Abstract
Thoracic outlet syndrome, a group of diverse disorders, is a collection of symptoms in the shoulder and upper extremity area that results in pain, numbness, and tingling. Identification of thoracic outlet syndrome is complex and a thorough clinical examination in addition to appropriate clinical testing can aide in diagnosis. Practitioners must consider the pathology of thoracic outlet syndrome in their differential diagnosis for shoulder and upper extremity pain symptoms so that patients are directed appropriately to timely therapeutic interventions. Patients with a definitive etiology who have failed conservative management are ideal candidates for surgical correction. This manuscript will discuss thoracic outlet syndrome, occurrence, physical presentation, clinical implications, diagnosis, and management.
Keywords: Brachial plexus, Neurogenic thoracic outlet syndrome, Subclavian vein, Thoracic outlet syndrome
Introduction
Thoracic outlet syndrome (TOS) constitutes a group of diverse disorders that result in compression of the neurovascular bundle exiting the thoracic outlet. The thoracic outlet is an anatomical area in the lower neck defined as a group of three spaces between the clavicle and the first rib through which several important neurovascular structures pass; more detailed anatomical descriptions will correspond with discussions of the relevant pathology [1]. These structures include the brachial plexus, subclavian artery, and subclavian vein. Compression of this area causes a constellation of distinct symptoms, which can include upper extremity pallor, paresthesia, weakness, muscle atrophy, and pain [2].
TOS classifications are based on the pathophysiology of symptoms with subgroups consisting of neurogenic (nTOS), venous (vTOS), and arterial (aTOS) etiologies [3]. Furthermore, each one of these subgroups can be related to either congenital, traumatic, or functionally acquired causes [4]. Examples of congenital etiologies include the presence of a cervical rib or an anomalous first rib. Traumatic causes most commonly include whip-lash injuries and falls. Functional acquired causes can be related to vigorous, repetitive activity associated with sports or work. Diagnosis of TOS is generally dependent on clinician familiarity of TOS coupled with an evaluation of symptoms and patient-specific risk factors. Clinical suspicion can then be confirmed with provocative physical exam maneuvers, radiographic, and/or vascular studies. Because of the wide range of etiologies and lack of expert consensus for diagnostic testing, the true incidence of TOS is difficult to discern. Several articles report an incidence of 3–80/1000 [4]. Neurogenic TOS accounts for over 90% of the cases, followed by venous and arterial etiologies [3]. Historically, TOS presents with symptom onset between the ages of 20–50 years old and is more prevalent in women [5].
With the wide range of multifactorial etiologies, it also makes sense that best-practice treatments for TOS involve a comprehensive and multi-disciplinary approach. Management options can include surgery, lifestyle modification, pain management, anticoagulation, physical therapy, and rehabilitation [6]. This article therefore intends to review the most relevant, noteworthy, and up-to-date literature, and to provide clinicians with a concise summary of both diagnosis and management for TOS. A comprehensive electronic literature search (1970–2018) process was conducted that included PubMed, EMBASE, and MEDLINE databases, and Google Scholar. Previous materials published in peer-reviewed journals and grey literature were reviewed in a systematic manner. References cited in relevant articles were also reviewed. Search terms used included “thoracic outlet syndrome” AND “imaging” OR “angiography” OR “diagnosis” OR “neurogenic” OR “venous” OR “arterial” OR “NSAIDs” OR “physical therapy” OR “surgery” OR “antidepressants” OR “Raynaud’s” OR “neuropathy.”
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Occurrence, Physical Presentation
Epidemiology
As previously stated, TOS may be subcategorized into neurogenic, venous, or arterial, depending on the structure responsible for producing symptoms. nTOS is by far the most common, representing about 95% of cases [3]. The brachial plexus trunks or cords, originating from nerve roots C5 to T1, are responsible. nTOS can be further divided into true or disputed TOS, with disputed reportedly representing 95–99% of all neurogenic cases [7]. The symptoms of true and disputed nTOS are largely the same, though objective findings from motor nerve conduction studies and needle electromyography are notably absent in the disputed variety. Venous TOS accounts for 3–5% of cases and arterial TOS the final 1–2% [3]. The subclavian and axillary vasculature is implicated in arterial and venous TOS.
Both true and disputed nTOS are more common in women [3]. Teenaged to 60-year-old females are most frequently affected by true nTOS [3]. Whereas true nTOS is primarily unilateral, the disputed variety is often bilateral [7]. The lower brachial plexus is affected in about 80% of patients with the disputed subtype, while the upper brachial plexus is compromised in the other 20% [7]. Arterial TOS, a predominantly unilateral condition, affects both genders equally and more often affects young adults [8]. Venous TOS also tends to be unilateral and is more common in men than women. Due to its association with repetitive upper extremity activity, vTOS is more common in younger, able-bodied individuals, and most often affects the dominant upper extremity [8].
Anatomy
Clinicians need to maintain familiarity with the relevant anatomy to fully conceptualize TOS. The thoracic outlet comprises the space from the supraclavicular fossa to the axilla. The symptoms of TOS arise from compression of the brachial plexus nerves, subclavian artery and vein, and axillary artery and vein.
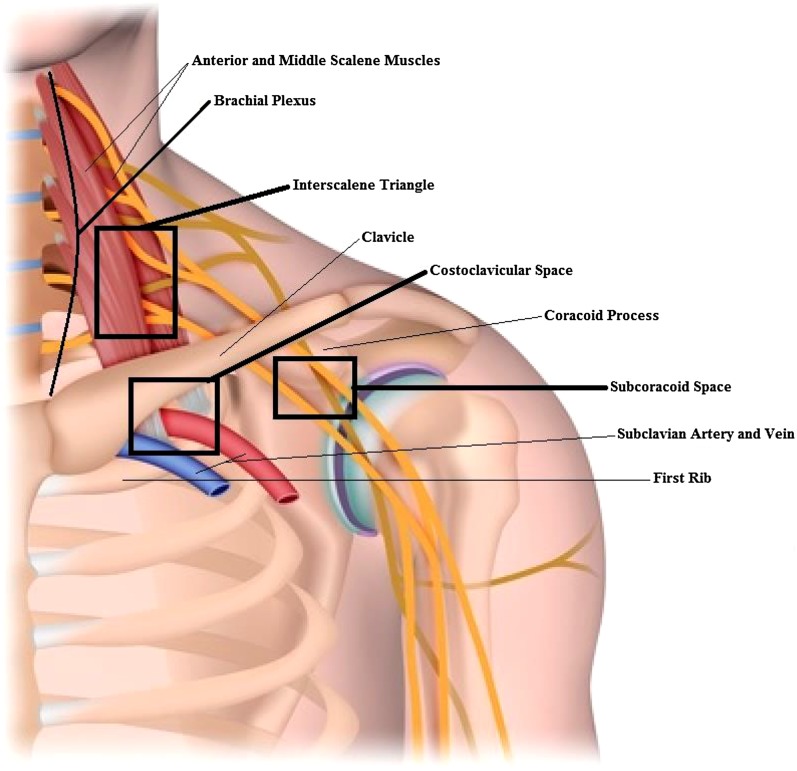
Described in Table 1 and diagrammatically represented in Fig. 1, the areas within the thoracic outlet where compression of nerves or vasculature occurs include the interscalene triangle, costoclavicular space, and subcoracoid space [7]. The interscalene triangle is the most medial compartment, and its borders are created by the anterior scalene muscle anteriorly, middle scalene muscle posteriorly, and first rib inferiorly. The brachial plexus and subclavian artery pass through the interscalene triangle, however the subclavian vein courses anterior to the compartment [9]. The second compartment, the costoclavicular space, is bordered by the subclavius muscle anteriorly and clavicle superiorly. The first rib and anterior scalene muscle form the inferior and posterior borders. The brachial plexus, subclavian artery, and subclavian vein all pass through this compartment. The final and most lateral compartment is the subcoracoid space. This space has alternatively been labeled as the retropectoralis space or the subcoracoid pectoralis minor space [9, 10]. The pectoralis minor muscle forms the anterior border of this space, and the ribs form the posterior boundary. As its name would suggest, the coracoid is located superior to this space. The brachial plexus passes through the subcoracoid space, and the subclavian artery and vein continue through it as the axillary artery and vein.
Table 1.
Anatomic spaces of thoracic outlet syndrome
| Compartment | Borders | Contents |
|---|---|---|
| Interscalene triangle |
Anterior: anterior scalene muscle Posterior: middle scalene muscle Inferior: first rib |
Brachial plexus Subclavian artery |
| Costoclavicular space |
Anterior: subclavius muscle Inferoposterior: first rib and anterior scalene muscle Superior: clavicle |
Brachial plexus Subclavian artery Subclavian vein |
| Subcoracoid space |
Anterior: pectoralis minor muscle Posterior: ribs 2–4 Superior: coracoid |
Brachial plexus Axillary artery Axillary vein |
Fig. 1.
Thoracic outlet and relevant anatomy
Etiology
Numerous mechanisms elicit the characteristic pathology of TOS, including trauma, repetitive motions, and anatomic variations. Traumatic events are typically high velocity, most often in the setting of a motor vehicle accident. Hemorrhage, hematoma or displaced fracture can directly compress the nerves or vasculature. Midshaft clavicular fracture in particular is a recognized cause [8]. Even after the initial insult, fibrosis can develop and produce symptoms [7]. Whiplash injuries exhibit a known association with TOS, most often of the neurogenic subtype; patients with a cervical rib are reportedly predisposed to this outcome [11].
Repetitive motions can lead to muscle hypertrophy that contributes to compression. Additionally, overuse injury in the setting of repetitive movements can cause swelling, small hemorrhages, and subsequent fibrosis, which can also account for symptoms. Venous TOS is also possible following repetitive motion. Paget–Schroetter disease, also called “effort thrombosis,” involves axillary or subclavian venous thrombosis following strenuous repeated activity with the arms [12].
Myriad anatomic variations incite TOS. One such variation, the presence of a cervical rib, bears an estimated prevalence of 1–2% of the general population but remains asymptomatic for most people. Patients with a cervical rib are at higher risk of nTOS, with up to 20% of nTOS cases attributable solely to the presence of a cervical rib [7]. Presence of a cervical rib is also a predisposing factor in the development of arterial TOS, as it can compress the subclavian artery and cause stenosis or aneurysm [11]. Congenital variations in musculature have also been reported to cause TOS. For instance, a supernumerary scalene muscle may contribute to compression within the interscalene triangle [7].
Malignancy causing compression is another well-documented etiology of TOS. Pancoast tumors, also known as superior pulmonary sulcus tumors, can invade and compress the brachial plexus [13]. Benign tumors are also capable of producing the characteristic symptoms, as illustrated by a rare case of multiple hereditary exostosis causing combined venous, arterial, and nTOS secondary to large osteochondromas [14].
Clinical Implications
Prompt recognition of the presenting signs of TOS is crucial to prevent long-term sequelae, specifically chronic upper extremity pain and severe disability. In each subtype of TOS, an understanding of the causative anatomic aberrancy can guide diagnosis.
Neurogenic TOS is caused by compression of the C5 through T1 brachial plexus nerve roots and comprises up to 90% of total TOS cases [15]. Compression of the nerve roots most often occurs within the scalene triangle but can also occur in the subarachnoid space as the nerve roots traverse beneath the pectoralis minor tendon. In this scenario, congenitally anomalous anatomy such as aberrant scalene musculature, cervical ribs, and connective tissue may compress and entrap nerve roots [16]. Additionally, acquired anatomical variation, e.g., scarring from injury, can affect these nerve roots. Accordingly, nTOS is often seen in young, active individuals who participate in athletic activities that involve repetitive overhead upper extremity motion and heavy lifting [11]. Diagnosis of nTOS is thereby based on the history of symptom presentation and clinical exam findings. Patients with nTOS often report consistently reproducible symptoms when performing the responsible activities and demonstrate positional exacerbation when mimicking these specific upper extremity motions. Symptoms generally correspond secondary to the level of nerve compression, with the most common being upper extremity heaviness with above-the-shoulder activities. A systematic review by Sanders et al. [11] described symptom distribution in neurogenic TOS to include upper extremity paresthesia (98%), neck pain (88%), trapezius pain (92%), shoulder and/or arm pain (88%), supraclavicular pain (76%), chest pain (72%), occipital headache (76%), and paresthesias in all five fingers (58%), the fourth and fifth fingers only (26%), or the first, second, and third fingers. In upper plexus TOS, involving compression of the C5, C6, and C7 nerves, pain is most often described in the lateral neck, with radiation superior to the ear and occiput. Pain may also radiate posteriorly to the rhomboid area, anteriorly across the clavicle into the upper pectoral region, laterally through the deltoid and trapezius muscle areas, and down the outer aspect of the arm [17]. In general, patients present with lower plexus TOS rather than upper, which corresponds to compression of the C8 and T1 nerves. Pain is typically distributed along the posterior of anterior shoulder with radiculopathy down the arm in a medio-brachial distribution along the inner aspect of the arm. Paresthesia tends to affect an ulnar nerve distribution along the ring and little fingers. Despite this etiological understanding of pathoanatomy, differentiation from other cervicobrachial symptoms may still prove challenging difficult [18].
Venous TOS, also referred to as Paget–von Schroetter syndrome, comprises 10–15% of cases, and is caused by subclavian compression within the costoclavicular space [19]. Mechanical compression and repetitive injury of the subclavian vein between the clavicle and first rib can lead to abrupt blood flow stagnation and subsequent effort thrombosis. This causes the pathognomonic presentation of acute upper extremity swelling, cyanosis, heaviness, and ultimately pain. Raynaud’s-like symptoms may be appreciated with vTOS but are typically unilateral, unlike the former disease [20]. It is important to remember, however, that Raynaud’s itself may present as unilateral in ~ 7% of cases, thus the clinician need maintain awareness of other causes of vascular compromise in their approach [21]. Like nTOS, venous TOS occurs frequently in physically active individuals, aged 15–45, many of whom participate in work or recreational activities that involve heavy lifting and repetitive upper extremity overhead motion. Pulmonary embolism is an important complication of venous and occurs in 10–20% of patients. In comparison to lower extremity DVT, however, clot burden is typically minimal and infrequently life-threatening, as extrinsic mechanical obstruction of blood flow theoretically prevents proximal embolization of venous blood clot. Though patients with effort thrombosis may initially present with an abnormal coagulation profile, genetic hypercoagulable parameters are typically negative, thusly distinguishing vTOS as a mechanical problem rather than a pro-coagulative hematologic disorder [22, 23]. As subclavian vein thrombosis may arise from alternative etiologies, imaging such as venous duplex, MRI, and CT can assess the proximal subclavian vein status to confirm the mechanical diagnosis [19]. Differentiation from nTOS is clinical; in contrast to pain exacerbated by overhead upper arm positioning, the symptomatology of venous thrombosis is stable.
Arterial TOS is by far the most rarely observed, occurring in 2–5% of TOS cases. Subclavian artery compression within the scalene triangle may be caused by an anomalous first rib, which ultimately developing an aneurysm distally. Acquired types may also be seen in physically active patients and athletes in whom arterial entrapment may occur at the level of the pectoralis minor tendon and the humeral head [24]. Arterial compression incites intimal damage, turbulent blood flow, and vessel dilation. Eventual arterial thrombosis and distal embolization may result in acute distal upper extremity ischemia. Clinical features are primarily vascular, as discussed, with secondary neurologic abnormalities as sequelae.
Clinicians should recall TOS on their differential diagnosis when confronted with a patient suffering from upper extremity pain and supporting physical exam findings. Adult patients who present with features of TOS necessitate a low threshold for imaging, as delay in treatment can lead to irreversible changes and chronic pain. While nTOS is the most frequent subtype, its diagnosis may be the most challenging by the lack of readily apparent clinical findings, such as vascular abnormalities on radiography [18].
Diagnosis of TOS is further complicated by alternative disorders with similar presentation. Nerve compression at the cervical spine or elbow and wrist, involving the median and ulnar nerve, may occur in conjunction with TOS. A presentation as such is referred to as double crush syndrome and may mask the presentation of TOS [25]. In these patients, careful consideration of multiple imaging modalities, electromyographic studies, and detailed physical examination are crucial to discern the foci of neurovascular compromise. Despite this, in as many as 29% of patients who present with symptoms consistent with distal peripheral nerve entrapment syndromes (e.g., carpal tunnel syndrome), there is no evidence of clinical or physical exam findings supporting a distal nerve lesion [26]. Furthermore, in patients with electrophysiologically proven distal entrapment syndrome, proximal neurological lesions at the level of the cervical spine may contribute to symptoms; in a review of 1000 cases of carpal tunnel syndrome, 89% of patients exhibited concomitant cervical arthritis, which is capable of eliciting similar symptoms [27]. Likewise, in a study of cyclists with ulnar nerve neuropathy, proximal neural lesions contributing to a double crush syndrome were symptomatically contributory [28]. The prevalence and diagnosis of nTOS is controversial, and much debate surrounds the role of nTOS to upper limb entrapment neuropathies. Careful consideration should, therefore, be given to compressive neuropathies at distinct, alternative sites which can lead to similarly disabling upper extremity pain and weakness.
Owing to the high prevalence of carpal tunnel syndrome (CTS), the concurrence of TOS with CTS has been extensively examined. However, controversy remains in terms of double crush phenomenon pathology, diagnosis, and treatment of these two syndromes. TOS is rare, and diagnosis often lacks specificity. Moreover, carpal tunnel syndrome is often inaccurately diagnosed. Compounded, the occurrence of simultaneous TOS and CTS becomes exceedingly rare. As such, it is unlikely that the combination would precipitate double crush syndrome [29]. In patients with persistent symptoms following decompression of distal nerve entrapment, though TOS may not be entirely excluded, proximal nerve compression stemming from cervical radiculopathy may be the more likely etiology. While reports have demonstrated TOS as a contributing factor to double crush phenomena with distal entrapment neuropathies, the prevalence of TOS in CTS is around 1% [30–33]. Furthermore, although the presence of double crush syndrome is difficult to confidently diagnose, the fact that CTS is a highly accepted diagnosis may explain the elevated incidence of reported coincident CTS with TOS. The association of TOS with CTS is both plausible and previously documented, but the unpredictability of both syndromes warrants surgical treatment of the distal compressive neuropathy first [32]. Persistent entrapment neuropathy following surgical treatment for TOS should raise suspicion for distal nerve entrapment syndrome [34]. Complete resolution of symptoms is achievable only by addressing all points of suspected neural compression [35, 36].
Though inherently distinct etiologically, the three forms of TOS share a fundamental mechanism of extrinsic neurovascular compression that ultimately produces severe pain and disability. In all cases, early recognition and diagnosis is crucial to initiation of the proper treatment. TOS remains a challenging and highly controversial diagnosis, and alternative, and possibly coincidental, proximal or distal compressive neuropathies must be excluded.
Diagnosis and Management
Relevant Physical Examination
When suspecting TOS, a general physical exam should focus on a thorough examination of not only the shoulder and upper extremity but the cervical spine as well, with particular attention to head and neck posture. A careful comparison between the affected and contralateral extremity can reveal obvious signs of wasting and weakness, while more subtle differences in skin color, temperature, and hair distribution may also be evident. Depending on the underlying etiology, patients may present with varied yet characteristic physical exam findings of the underlying cause of obstruction. Vascular TOS can cause large differences in blood pressure readings between arms (> 20 mmHg); the shoulder and chest may appear edematous in vTOS, while the upper extremity may appear pale or cyanotic with aTOS [37]. Not surprisingly, nTOS yields more obvious signs of muscular atrophy such as the Gilliatt–Sumner hand, which is a constellation of atrophic abductor pollicis brevis, hypothenar, and interossei muscles [38]. Other notable physical exam findings may include supraclavicular fullness or aneurismal pulsations [39].
While the use of individual provocative maneuvers for the diagnosis of TOS has led to a high number of false positives, studies indicate that reliance on multiple tests in conjunction may increase the specificity of TOS identification. Table 2 below describes commonly used maneuvers in the physical exam [39, 40]. A study by Gillard et al. demonstrated that combining the Adson and Roos test increased the specificity from 76 to 30% when used alone to 82% when both are positive [41].
Table 2.
Common provocative diagnostic tests for thoracic outlet syndrome
| Test | Maneuver | Result |
|---|---|---|
| ADSON TEST | Affected arm is abducted 30° at the shoulder while maximally extended. While extending the neck and turning head towards ipsilateral shoulder, patient inhales deeply | Decrease or absence of ipsilateral radial pulse |
| Elevated Arm Stress Test (EAST) or ROOS | Arms are placed in the surrender position with shoulders abducted to 90° and in external rotation, with elbows flexed to 90°. Patient slowly opens and closes hand for 3 min | Precipitates pain, paresthesias, heaviness or weakness |
| Upper Limb Tension Test (ULTT) or ELVEY |
Position 1: arms abducted to 90° with elbows flexed Position 2: active dorsiflexion of both wrists Position 3: head is tilted ear to shoulder, in both directions |
Positions 1 and 2 elicit symptoms on the ipsilateral side, while position 3 years elicits symptoms on the contralateral side |
Diagnostic Modalities
Further diagnostic testing is directed predominantly by clinical symptoms and the type of suspected TOS. While testing is often equivocal or negative in nTOS, making it a diagnosis of exclusion, testing for vTOS focuses on the demonstration of stenosis or occlusion of subclavian vessels. Below are tests commonly used in diagnosis and surgical planning for appropriate candidates.
Electrodiagnostic Testing
Although a majority of patients will have normal or negative results, electrophysiological evaluation via nerve conduction and EMG is indicated for those suspected of nTOS. However, when positive nTOS presents with a characteristic pattern of nerve conduction abnormalities. Sensory response may be normal in the median distribution but diminished or absent in medial antebrachial cutaneous and ulnar sensory responses. Additionally, diminished or absent median and ulnar motor response may be seen, typically with a more profound decrease in the median response. These findings are highly suggestive of nerve conduction abnormalities involving the C8 and T1 fibers (T1 usually more affected than C8) and serve to rule out cervical radiculopathy and myelopathy [10, 42, 43].
Injection of local anesthetic into the anterior scalene muscle has been used to successfully diagnose nTOS. Temporary relief of symptoms following medication injection decreases muscular tension on the neural bundle and may predict response to surgical decompression. In those with a positive response to the block, 94% were shown to have a positive outcome following surgical correction as compared to only 50% of patients who underwent decompression following a failed block [39].
Imaging
Imaging can also be helpful in confirming suspected cases of TOS. Anatomical abnormalities or defects, such as prominent cervical ribs, fracture calluses, or compressive tumors are commonly demonstrated on chest, shoulder, or spine radiographs. Conventional arteriography and venography, while they may demonstrate extrinsic compression, do not permit a clear depiction of the impinging anatomic structure, and they tend to be replaced by less invasive procedures (CT, MR imaging, sonography) as described below [17]. In addition to electrodiagnostic testing, MR neurogram can provide further detail to identify anatomical relationships or particular sites of compression.
For suspected vascular TOS, ultrasound maintains high sensitivity and specificity, is noninvasive and inexpensive, and should be the initial imaging test of choice. CT or MR angiography can differentiate equivocal cases or provide additional anatomic detail required for surgical planning [37].
Conservative Management Strategies
Management strategies depend on the underlying etiology of TOS. Initial treatment of nTOS consists of conservative measures, whereas vTOS or nTOS with refractory symptoms may undergo surgical management. Treatment is reserved only for symptomatic patients, as the presence of a cervical rib exists in 0.5% of the population but only a small fraction develop symptoms [38].
A consensus on the appropriate conservative regimen for nTOS remains controversial. However, a multimodal treatment approach including patient education, TOS-specific rehabilitation, and pharmacologic therapies have shown positive results. Rehab is recommended as the initial nonsurgical management for nTOS and should include patient education (postural mechanics, weight control, relaxation techniques), activity modification, and TOS-focused physical therapy (active stretching, targeted muscle strengthening, etc.) [38]. One study demonstrated symptomatic relief in 25 of 42 patients with nTOS following 6 months of physical therapy [37].
Pharmacologic interventions often provide symptomatic relief, and primarily include analgesics (NSAIDs and/or opioids) for neuropathic pain, as well as muscle relaxants, anticonvulsants, and/or antidepressants as adjuvants [6]. Additionally, injection of local anesthetic, steroids, or botulinum toxin type A into the anterior scalene and/or pectoralis muscle have demonstrated varying levels of success in observational studies [44], although the use of BTX-A failed to demonstrate significant benefit in a randomized trial [45].
Surgical Management Strategy in Failed Conservative Management and Treatment Outcomes
Surgery for TOS is reserved for patients who have failed conservative management. The threshold for decompression varies widely for mild to moderate symptoms, but certain symptoms require surgery.
As previously discussed, physical therapy and conservative management of nTOS should persist for at least 4–6 months prior to consideration of surgical intervention [46]. However, for patients with arterial or venous TOS, the initial intervention is most often surgical. A trial of anticoagulation via catheter-directed thrombolysis and systemic heparin therapy may be first attempted for patients with arterial or vascular TOS [47]. In cases of mild upper extremity ischemia, catheter-directed thrombolysis may restore perfusion. Symptoms refractory to these measures require surgery.
Surgical candidates should have failed conservative management [40]. Most surgical candidates exhibit nTOS with uncontrolled pain or progressively worsening upper extremity weakness. The surgery of choice is a first rib resection aimed at brachial plexus decompression, typically performed by vascular surgeons. The operation can also be performed by thoracic surgeons, neurosurgeons, orthopedic surgeons, and plastic surgeons [46]. In nTOS, the first rib is removed in addition to a scalenectomy or scalenotomy.
The three approaches to brachial plexus decompression by first rib removal include transaxillary, supraclavicular, and infraclavicular techniques. Each approach has achieved good outcomes, with no definitively superior technique [48]. While the transaxillary and supraclavicular approaches are utilized more frequently, technique is often chosen based on the individual patient and unique anatomical considerations. The supraclavicular approach requires a scalenectomy of the middle and anterior scalene muscles to expose a small portion of the first rib. The compression is thereby easily exposed, allowing for access to the brachial plexus if neurolysis is indicated. The transaxillary approach is performed by accessing the first rib between the pectoralis major and latissimus dorsi in the axilla. With the patient in the lateral position, careful dissection of the axillary vasculature and nerves may expose the first rib. In this approach, exposure is limited and potential brachial plexopathy may occur through over-manipulation and retraction. Less common, the infraclavicular approach allows for vascular reconstruction in patients with venous or arterial TOS and should be pursued if central venous exposure is required.
Brachial plexus injury after first rib resection does occur, but reporting varies widely [49]. In a multi-institution database study, brachial plexus injuries were reported in 0.6% patients with nTOS following transaxillary first rib resection [50]. However, another study of transaxillary first rib resections in patients with nTOS reported a brachial plexus injury incidence of 9%, with an incidence of 4% after supraclavicular first rib resection [51].
More recently, the introduction of minimally invasive techniques has achieved superior outcomes in first rib removal, as both robotic and thoracoscopically assisted approaches minimize brachial plexus manipulation [46]. Additional training, equipment, and expertise is required but may limit the overall surgical risk.
Overall outcomes from surgical decompression are very positive. Following surgical intervention, 95% of patients with nTOS reported “excellent” results [52]. In a 5-year follow-up study of patients with vTOS, patency rates were better than 95% [53]. Impediments to successful outcomes include major depression or comorbid conditions that skew the initial diagnosis [53].
Recent Developments
As more patients receive diagnosis and treatment for TOS, the referral pattern has changed. Instead of evaluation and treatment by multiple disciplines before consideration of TOS, patients are now referred sooner despite a shorter duration of symptoms, which improves the predicted response to surgical treatment [3]. Additionally, a rise in the number of adolescent cases has been described, owing to repetitive or vigorous activity such as musical instrument or athletic endeavors. More common in adolescents than adults, first rib resection has been successfully and safely performed for vTOS and aTOS with good outcomes and fast recovery [54].
Since TOS is a rare and complex group of disorders with potentially severe and disabling symptoms, care can be challenging for health care providers. Therefore, a systematic, organized approach to the diagnosis and treatment of TOS provides an opportunity for specialists to deliver patient-centered care and achieve optimal results. This specialized type of care is best delivered through the efforts of a multi-disciplinary team that consists of various specialists, including vascular surgery, thoracic surgery, neurology/neurosurgery, orthopedics, radiology, anesthesiology, pain management, physical therapy, and occupational therapy [55]. For this reason, centers of excellence for TOS have been established around the country with demonstrable improvements in outcomes [3].
Venous and arterial TOS are diagnosed by a combination of clinical presentation and imaging. Ongoing developments in the diagnosis of TOS include dynamic CT angiography, MR neurography, and Diffusion Tensor Imaging (DTI). These imaging modalities can be used to identify brachial plexus branching variants in which susceptibility to compression by the scalene muscle is increased. Neurogenic TOS is generally more difficult to diagnose as nerve and tissue inflammation lack consistent radiographic evidence. However, as imaging studies evolve, newer modalities with higher quality allow for improved diagnostic objectivity [56]. MRI can evaluate the anatomy of the thoracic outlet, the soft tissue structures causing compression, and allow direct visualization of brachial plexus compression [40]. Magnetic resonance neurography (MRN) is an imaging modality that allows non-invasive visualization of nerve morphology and signal. In this technique, signals from surrounding soft tissue such as adipose are suppressed, and pulsation artifact from pulsating blood is removed. Continued improvements in high-resolution MRN may, therefore, augment current diagnostic modalities by facilitating prompt identification of brachial plexus compression across the thoracic outlet in patients with nTOS [57].
While MRN denotes a class of techniques intended for assessment of peripheral nerves, diffusion tension imaging (DTI) or tractography is reserved for the CNS [58]. Short tau inversion recovery (STIR) sequences and the spectral adiabatic inversion recovery (SPAIR) preparatory module are variations of MRN and deliver a more complete anatomical description of the nerves comprising the brachial plexus. DTI sequences to visualize nerve fascicles are employed in the modeling technique of tractography, allowing for a more comprehensive assessment of peripheral nerve injury [57]. One study regarding MRN demonstrated a 100% positive predictive value in all 30 patients involved; however, ultrasound also identified compression all patients with nerve lesions visualized on MRN [59].
Current mainstays of diagnosis include duplex ultrasound, arteriography, hemodynamic testing (finger plethysmography) at rest and with symptom-producing maneuvers, as well as CT and MR angiography [60]. Invasive arteriography and angiography are useful in the detection of complications from aTOS such as thrombosis, embolization, and aneurysm. The invasive nature of these techniques limits their use to surgical planning rather than pure diagnostics. Other non-invasive tests such as MR and CT angiography are more readily employed for their diagnostic utility outside of surgical planning. Dynamic testing allows the clinician to evaluate arterial compression with provocative maneuvers, while imaging helps to define the anatomic source of compression and confirm the diagnosis of arterial, venous, or nTOS [40].
Surgical Advancements
As noted above, first rib resection with scalenectomy remains the operation of choice for decompression, but as surgical advancements continue to emphasize minimally invasive approaches, some institutions now employ VATS in order to achieve a clearer visualization of the operative field and potentially minimize injury to the neurovascular bundle [61]. Two additional strategies, the robotic-assisted and endoscopic-assisted trans-axillary approaches, are novel techniques with potential benefit, the latter aiming to decrease risk of pneumothorax [56].
Future Directions
The past 50 years have welcomed substantial progress in terms of our understanding and treatment of TOS, but several knowledge gaps remain elusive. Diagnosis, for instance, presents a considerable challenge to this day. A reliable and objective diagnostic tool, such as imaging, would herald a new era for patients with TOS [3]. Preoperative MRI or CTA comparison of patients with TOS to control patients has been suggested as a promising avenue of research. Similarly, timing of post-operative imaging is a subject of debate, with various schedules employed across institutions. For example, venograms at 2 weeks after first rib resection and scalenectomy may encounter residual post-surgical inflammation; the precise timing post-surgical venography requires further investigation [3].
Lastly, the impact of prosthetic versus autologous tissue for aTOS reconstruction has yet to be elucidated. Comparative patency rates and need for reoperation have not been firmly delineated, are further research in this area would provide significant benefit, although the inherent rarity of aTOS renders large, multicenter investigations complex [3].
Conclusions
Since the first use of the term TOS by Peet et al., there have been significant advancements in the understanding and treatment of the syndrome. The upper extremity pain and numbness typical of the condition have been subcategorized into distinct disorders based on the structures involved. A history of trauma or repetitive motions combined with supportive physical exam findings suggests the correct diagnosis. Other diagnostic modalities such as MRI, ultrasound, and nerve conduction studies can further support the diagnosis, and ongoing developments in this sphere are currently underway.
Despite advances, substantial controversy regarding the diagnosis remains. This is evidenced by the lack of objective findings surrounding nTOS, the most common and widely disputed form of TOS. The challenges associated with diagnosis complicate the selection of the appropriate treatment option. In some cases, e.g., acute vascular insufficiency or progressive neurologic dysfunction, surgical decompression is clearly indicated. Prompt recognition and treatment of TOS provide the greatest opportunity for optimal recovery. Unfortunately, the multitude of nonspecific symptoms and challenges in diagnosis can delay treatment and increase the risk of complications.
Surgical intervention for TOS syndrome is reserved for patients who have failed conservative management. Conservative treatment including physical therapy need be trialed for at least 4–6 months prior to consideration of surgical intervention [46]. Definitive therapy for patients with refractory aTOS or vTOS, however, remains surgical intervention.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Alan D. Kaye is a speaker for Depomed, Inc. and Merck, Inc. Mark R. Jones, Amit Prabhakar, Omar Viswanath, Ivan Urits, Jeremy B. Green, Julia B. Kendrick, Andrew J. Brunk, Matthew R. Eng, Vwaire Orhurhu and Elyse M. Cornett have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to: 10.6084/m9.figshare.7951541.
References
- 1.Aljabri B, Al-Omran M. Surgical management of vascular thoracic outlet syndrome: a teaching hospital experience. Ann Vasc Dis. 2013;6(1):74–79. doi: 10.3400/avd.oa.12.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact. J Occup Rehabil. 2011;21(3):366–373. doi: 10.1007/s10926-010-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freischlag J, Orion K. Understanding thoracic outlet syndrome. Scientifica (Cairo). 2014;2014:1–6. doi: 10.1155/2014/248163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Citisli V. Assessment of diagnosis and treatment of thoracic outlet syndrome, an important reason of pain in upper extremity, based on literature. J Pain Relief. 2015;04(02):1–7. [Google Scholar]
- 5.Maru S, Dosluoglu H, Dryjski M, Cherr G, Curl GR, Harris LM. Thoracic outlet syndrome in children and young adults. Eur J Vasc Endovasc Surg. 2009;38(5):560–564. doi: 10.1016/j.ejvs.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Brooke BS, Freischlag JA. Contemporary management of thoracic outlet syndrome. Curr Opin Cardiol. 2010;25(6):535–540. doi: 10.1097/HCO.0b013e32833f028e. [DOI] [PubMed] [Google Scholar]
- 7.Stewman C, Vitanzo PC, Harwood MI. Neurologic thoracic outlet syndrome: summarizing a complex history and evolution. Curr Sports Med Rep. 2014;13(2):100–106. doi: 10.1249/JSR.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 8.Ferrante MA, Ferrante ND. The thoracic outlet syndromes: Part 2. The arterial, venous, neurovascular, and disputed thoracic outlet syndromes. Muscle Nerve. 2017;56(4):663–673. doi: 10.1002/mus.25535. [DOI] [PubMed] [Google Scholar]
- 9.Raptis CA, Sridhar S, Thompson RW, Fowler KJ, Bhalla S. Imaging of the patient with thoracic outlet syndrome. RadioGraphics. 2016;36(4):984–1000. doi: 10.1148/rg.2016150221. [DOI] [PubMed] [Google Scholar]
- 10.Ferrante MA. The thoracic outlet syndromes. Muscle Nerve. 2012;45(6):780–795. doi: 10.1002/mus.23235. [DOI] [PubMed] [Google Scholar]
- 11.Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg. 2007;46(3):601–604. doi: 10.1016/j.jvs.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 12.Ibrahim R, Dashkova I, Williams M, et al. Paget–Schroetter syndrome in the absence of common predisposing factors: a case report. Thromb J. 2017;15:20. doi: 10.1186/s12959-017-0146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis GA, Knight SR. Pancoast Tumors. Neurosurg Clin N Am. 2008;19(4):545–557. doi: 10.1016/j.nec.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Abdolrazaghi H, Riyahi A, Taghavi M, Farshidmehr P, Mohammadbeigi A. Concomitant neurogenic and vascular thoracic outlet syndrome due to multiple exostoses. Ann Card Anaesth. 2018;21(1):71–73. doi: 10.4103/aca.ACA_119_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutherford RB. Vascular Surgery. 6th ed. Saunders; 2005.
- 16.Hooper TL, Denton J, McGalliard MK, Brismée J-M, Sizer PS. Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/diagnosis. J Man Manip Ther. 2010;18(2):74–83. doi: 10.1179/106698110X12640740712734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demondion X, Herbinet P, Van Sint Jan S, Boutry N, Chantelot C, Cotten A. Imaging assessment of thoracic outlet syndrome. RadioGraphics. 2006;26(6):1735–1750. doi: 10.1148/rg.266055079. [DOI] [PubMed] [Google Scholar]
- 18.Campbell WW, Landau ME. Controversial entrapment neuropathies. Neurosurg Clin N Am. 2008;19(4):597–608. doi: 10.1016/j.nec.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Thompson RW. Comprehensive management of subclavian vein effort thrombosis. Semin Intervent Radiol. 2012;29(1):44–51. doi: 10.1055/s-0032-1302451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooke RA. Thoracic outlet syndrome–aspects of diagnosis in the differential diagnosis of hand-arm vibration syndrome. Occup Med (Lond). 2003;53(5):331–6. http://www.ncbi.nlm.nih.gov/pubmed/12890833. Accessed 31 Mar 2019. [DOI] [PubMed]
- 21.Ingegnoli F, Gualtierotti R, Orenti A, et al. Uniphasic blanching of the fingers, abnormal capillaroscopy in nonsymptomatic digits, and autoantibodies: expanding options to increase the level of suspicion of connective tissue diseases beyond the classification of Raynaud’s phenomenon. J Immunol Res. 2015;2015:371960. doi: 10.1155/2015/371960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson R. Challenges in the treatment of thoracic outlet syndrome. Texas Hear Inst J. 2012;39(6):842–843. [PMC free article] [PubMed] [Google Scholar]
- 23.Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome. Neurologist. 2008;14(6):365–373. doi: 10.1097/NRL.0b013e318176b98d. [DOI] [PubMed] [Google Scholar]
- 24.Duwayri YM, Emery VB, Driskill MR, et al. Positional compression of the axillary artery causing upper extremity thrombosis and embolism in the elite overhead throwing athlete. J Vasc Surg. 2011;53(5):1329–1340. doi: 10.1016/j.jvs.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 25.William J, Molinari M, John C, Elfar M. The double crush syndrome. J Hand Surg Am. 2013;38(4):799–801. doi: 10.1016/j.jhsa.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Upton ARM, Mccomas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;302(7825):359–362. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 27.Hurst LC, Weissberg D, Carroll RE. The relationship of the double crush to carpal tunnel syndrome (an analysis of 1000 cases of carpal tunnel syndrome) J Hand Surg Br. 1985;10(2):202–204. doi: 10.1016/0266-7681(85)90018-x. [DOI] [PubMed] [Google Scholar]
- 28.Smith TM, Sawyer SF, Sizer PS, Brismée J-M. The double crush syndrome: a common occurrence in cyclists with ulnar nerve neuropathy—a case–control study. Clin J Sport Med. 2008;18(1):55–61. doi: 10.1097/JSM.0b013e31815c1d7a. [DOI] [PubMed] [Google Scholar]
- 29.Carroll RE, Hurst LC. The relationship of thoracic outlet syndrome and carpal tunnel syndrome. Clin Orthop Relat Res. 1982;164:149–153. [PubMed] [Google Scholar]
- 30.Seror P. Frequency of neurogenic thoracic outlet syndrome in patients with definite carpal tunnel syndrome: an electrophysiological evaluation in 100 women. Clin Neurophysiol. 2005;116(2):259–263. doi: 10.1016/j.clinph.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 31.Seror P. Symptoms of thoracic outlet syndrome in women with carpal tunnel syndrome. Clin Neurophysiol. 2005;116(10):2324–2329. doi: 10.1016/j.clinph.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 32.Narakas AOO. The role of thoracic outlet syndrome in the double crush syndrome. 1990;9(5):331–340. doi: 10.1016/s0753-9053(05)80506-x. [DOI] [PubMed] [Google Scholar]
- 33.Putters JL, Kaulesar Sukul DM, Johannes EJ. Bilateral thoracic outlet syndrome with bilateral radial tunnel syndrome: a double-crush phenomenon. Case report. Arch Orthop Trauma Surg. 1992;111(4):242–243. doi: 10.1007/BF00571487. [DOI] [PubMed] [Google Scholar]
- 34.Wood VE, Biondi J. Double-crush nerve compression in thoracic-outlet syndrome. J Bone Joint Surg Am. 1990;72(1):85–87. [PubMed] [Google Scholar]
- 35.Galarza M, Gazzeri R, Gazzeri G, Zuccarello M, Taha J. Cubital tunnel surgery in patients with cervical radiculopathy: double crush syndrome? Neurosurg Rev. 2009;32(4):471–478. doi: 10.1007/s10143-009-0219-z. [DOI] [PubMed] [Google Scholar]
- 36.Osterman AL. The double crush syndrome. Orthop Clin North Am. 1988;19(1):147–155. [PubMed] [Google Scholar]
- 37.Kuhn JE, Lebus GF, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015;23(4):222–232. doi: 10.5435/JAAOS-D-13-00215. [DOI] [PubMed] [Google Scholar]
- 38.Huang JH, Zager EL. Thoracic outlet syndrome. Neurosurgery. 2004;55(4):897–902. doi: 10.1227/01.neu.0000137333.04342.4d. [DOI] [PubMed] [Google Scholar]
- 39.Narayanasamy N, Rastogi R. Thoracic outlet syndrome (TOS): an enigma in pain medicine. In: Kaye AD, Shah RV, editors. Case studies in pain management. Cambridge: Cambridge University Press; 2014. pp. 102–108. 10.1017/cbo9781107281950.014.
- 40.Povlsen S, Povlsen B. Diagnosing thoracic outlet syndrome: current approaches and future directions. Diagnostics. 2018 doi: 10.3390/diagnostics8010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gillard J, Pérez-Cousin M, Hachulla E, et al. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint Bone Spine. 2001;68(5):416–424. doi: 10.1016/s1297-319x(01)00298-6. [DOI] [PubMed] [Google Scholar]
- 42.Le Forestier N, Moulonguet A, Maisonobe T, Léger JM, Bouche P. True neurogenic thoracic outlet syndrome: electrophysiological diagnosis in six cases. Muscle Nerve. 1998;21(9):1129–1134. doi: 10.1002/(sici)1097-4598(199809)21:9<1129::aid-mus3>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 43.Tsao BE, Ferrante MA, Wilbourn AJ, Shields RW. Electrodiagnostic features of true neurogenic thoracic outlet syndrome. Muscle Nerve. 2014;49(5):724–727. doi: 10.1002/mus.24066. [DOI] [PubMed] [Google Scholar]
- 44.Foley JM, Finlayson H, Travlos A. A review of thoracic outlet syndrome and the possible role of botulinum toxin in the treatment of this syndrome. Toxins (Basel). 2012;4(11):1223–1235. doi: 10.3390/toxins4111223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Finlayson HC, O’Connor RJ, Brasher PMA, Travlos A. Botulinum toxin injection for management of thoracic outlet syndrome: a double-blind, randomized, controlled trial. Pain. 2011;152(9):2023–2028. doi: 10.1016/j.pain.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 46.Burt BM. Thoracic outlet syndrome for thoracic surgeons. J Thorac Cardiovasc Surg. 2018;5:5. doi: 10.1016/j.jtcvs.2018.02.096. [DOI] [PubMed] [Google Scholar]
- 47.Vemuri C, McLaughlin LN, Abuirqeba AA, Thompson RW. Clinical presentation and management of arterial thoracic outlet syndrome. J Vasc Surg. 2017 doi: 10.1016/j.jvs.2016.11.039. [DOI] [PubMed] [Google Scholar]
- 48.Povlsen B, Hansson T, Povlsen SD. Treatment for thoracic outlet syndrome. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD007218.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buller L, Jose J, Baraga M, Lesniak B. Thoracic outlet syndrome: current concepts, imaging features, and therapeutic strategies. Am J Orthop. 2015 [PubMed] [Google Scholar]
- 50.Chang DC, Lidor AO, Matsen SL, Freischlag JA. Reported in-hospital complications following rib resections for neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2007 doi: 10.1016/j.avsg.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 51.Hosseinian MA, Loron AG, Soleimanifard Y. Evaluation of complications after surgical treatment of thoracic outlet syndrome. Korean J Thorac Cardiovasc Surg. 2017 doi: 10.5090/kjtcs.2017.50.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Urschel HC, Razzuk MA. Upper plexus thoracic outlet syndrome: optimal therapy. Ann Thorac Surg. 1997 doi: 10.1016/s0003-4975(97)00188-4. [DOI] [PubMed] [Google Scholar]
- 53.Schneider DB, Dimuzio PJ, Martin ND, et al. Combination treatment of venous thoracic outlet syndrome: open surgical decompression and intraoperative angioplasty. J Vasc Surg. 2004 doi: 10.1016/j.jvs.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 54.Kevin Chang BEGKD, et al. Spectrum of thoracic outlet syndrome presentation in adolescents. JAMA Surg. 2011;146(12):1383–1387. doi: 10.1001/archsurg.2011.739. [DOI] [PubMed] [Google Scholar]
- 55.Emery, VB, Thompson RW. Thoracic outlet syndrome pathways of care and treatment options for patients with NTOS. London: Springer; 2013. 10.1007/978-1-4471-4366-6_22.
- 56.Weaver M, Lum Y. New diagnostic and treatment modalities for neurogenic thoracic outlet syndrome. Diagnostics. 2017;7(2):28. doi: 10.3390/diagnostics7020028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Magill ST, Brus-Ramer M, Weinstein PR, Chin CT, Jacques L. Neurogenic thoracic outlet syndrome: current diagnostic criteria and advances in MRI diagnostics. Neurosurg Focus. 2015;39(3):E7. doi: 10.3171/2015.6.FOCUS15219. [DOI] [PubMed] [Google Scholar]
- 58.Filler A. Magnetic resonance neurography and diffusion tensor imaging: origins, history, and clinical impact of the first 50,000 cases with an assessment of efficacy and utility in a prospective 5000-patient study group. Neurosurgery. 2009 doi: 10.1227/01.NEU.0000351279.78110.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baumer P, Kele H, Kretschmer T, Koenig R, Pedro M, Bendszus M, Pham M. Thoracic outlet syndrome in 3T MR neurography-fibrous bands causing discernible lesions of the lower brachial plexus. Eur Radiol. 2014;24:756–761. doi: 10.1007/s00330-013-3060-2. [DOI] [PubMed] [Google Scholar]
- 60.Illig KA, Donahue D, Duncan A, et al. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. J Vasc Surg. 2016;64(3):e23–e35. doi: 10.1016/j.jvs.2016.04.039. [DOI] [PubMed] [Google Scholar]
- 61.Hwang J, Min B-J, Jo W-M, Shin JS. Video-assisted thoracoscopic surgery for intrathoracic first rib resection in thoracic outlet syndrome. J Thorac Dis. 2017;9(7):2022–2028. doi: 10.21037/jtd.2017.06.122. [DOI] [PMC free article] [PubMed] [Google Scholar]