Highlights
-
•
Description of 4 cases outside Asia of invasive infection by hypervirulent K. pneumoniae.
-
•
These are patients from the community without any type of epidemiological background or previous trips to the endemic area.
-
•
Unlike other series in our case, these are patients without one of the classic risk factors: no patient is diabetic.
-
•
Patients present both serotype K1 and K2, not finding a prevalent serotype in our series.
Keywords: Hypermucoviscous Klebsiella pneumoniae, Liver abscess, Community acquired infection, MLST
Abstract
In 1986, a new syndrome was described in Taiwan secondary to hypervirulent K. pneumoniae (hvKP), and its main feature was the ability to cause severe infection in young and immunocompetent hosts. Their virulence is explained by the efficient acquisition of iron and an increase in capsule production, which confer the characteristic hypermucoviscous phenotype. Most of these cases have been described in Asia and subsequently spread to America and Europe, where their prevalence is much lower. We present four cases of bacteremia and liver abscesses secondary to hypervirulent K. pneumoniae, two of them associated with endophthalmitis. K. pneumoniae isolates recovered from two of the patients belonged to capsular serotype K1 (genes wzx_K1 and magA), while the other two were K2 (gene wzy_K2). Both of the K1 isolates were classified into a ST23, and isolates of serotype K2 belonged to the ST375 and ST881 clones.
In Europe, hvKP isolates are less frequently recovered, mostly associated with Asian citizens or travelers, which was not the case in our patients. K1 capsular serotype is a major cause of primary liver abscess and secondary septic embolus, and K2 is associated with secondary liver abscess. Although these hypervirulent variants usually affect immunocompetent patients as in our cases, diabetes mellitus is a major risk factor for the most invasive cases, with concomitant poor prognosis. Identification of hypervirulent K. pneumoniae serotypes K1 and K2 should be considered as part of the microbiological diagnosis of community-acquired liver abscess due to their clinical implications.
Introduction
Klebsiella pneumoniae is a Gram-negative bacillus, which can be a member of the indigenous intestinal and nasopharyngeal microbiota in humans. However, it is also responsible for both community acquired and nosocomial infections, such as urinary tract infections, bacteremia, pneumonia and intraabdominal infections, acting as an opportunistic pathogen.
In 1986, Liu et al. described a new syndrome in Taiwan caused by K. pneumoniae which consisted in the presence of liver abscess associated with septic endophthalmitis [1]. Almost 20 years later, Fang et al. identified a novel virulence gene, magA, in K. pneumoniae isolates causing primary liver abscess and septic metastatic complications [2]. These authors also found that the hypermucoviscous phenotype (defined as the ability of forming a viscous string >5 mm in length) was significantly associated with K. pneumoniae invasive isolates.
This new organism was identified as hypervirulent K. pneumoniae (hvKP), and its main feature was the ability to cause severe infection in young and immunocompetent hosts. These hvKP are responsible for a syndrome that includes pyogenic liver abscess and metastatic spread to eyes, central nervous system and lungs. First in Asia, and then in America, Africa, Australia and Europe, an increasing number of infections caused by this organism are being reported [3].
The majority of these hvKP belong to capsular serotypes K1 and K2. Their virulence seems to be explained by the efficient acquisition of iron and an increase in capsule production, which confer the characteristic hypermucoviscous phenotype.
Case reports
We present clinical and microbiological features of four cases of invasive infection in Caucasian patients without relevant epidemiological history, caused by two different serotypes of hvKP (K1 and K2) in an 1160 beds tertiary hospital in Madrid (Spain):
-
•
Patient 1: An 86-year-old female with a history of hypertension and atrial fibrillation attended the emergency room with 3-day fever, ocular pain and decreased vision in her right eye. Endogenous endophthalmitis was suspected. The patient was hospitalized and intravitreous vancomycin and ceftazidime treatment was administered. After admission, abdominal Computed Tomography (CT) showed hepatic abscesses involving the right lobe of the liver, which were drained. K. pneumoniae was isolated from blood cultures, liver abscess, urine culture and vitreous fluid cultures. Intravenous cefotaxime (2 g every 4 h) was administered for 4 weeks. After completing the antimicrobial treatment, the liver abscess was resolved but her vision remained diminished.
-
•
Patient 2:A 72-year-old male with chronic hepatopathy due to hepatitis C virus attended the emergency room with fever (38.5 °C) and pain in the right hypochondrium. Abdominal CT-scan showed an abscess of 10 cm in diameter in the right hepatic lobe. Drainage was performed, obtaining purulent material that was sent for culture. K. pneumoniae was obtained from blood and liver abscess cultures. The patient received ceftriaxone 2 g every 24 h iv during 4 weeks, achieving complete recovery.
-
•
Patient 3: A 57-year-old male with primary hyperaldosteronism attended the emergency room with fever (39 °C), cough and pleuritic chest pain, treated empirically with ceftriaxone. An infiltrate in the right upper lobe with nodular opacities was observed in his chest x-ray. Immediately after admission, he began to present ocular pain and decreased vision in his right eye. After diagnosis of endogenous endophthalmitis, intravitreous treatment with vancomycin, ceftazidime and corticosteroids was administered. Abdominal CT-scan showed two hepatic abscesses involving the right lobe. Drainage was performed, and intravenous cefotaxime (2 g every 4 h) was administered. K. pneumoniae was recovered from blood and liver abscess cultures. After 4 weeks of antimicrobial treatment, improvement of the hepatic abscesses and total recovery of vision was achieved.
-
•
Patient 4: An 82-year-old male with a history of Parkinson's disease, chronic pancreatitis and hypertension attended the emergency room with fever (40 °C), deterioration of general condition, abdominal pain, dysuria and frequency. An abdominal CT-scan showed findings suggestive of cholangitis and multiloculated liver abscess in the left lobe. Drainage of the lesion was not performed due to expectation of limited yield when a loculated abscess is present. K. pneumoniae was recovered from blood cultures. The patient initially received meropenem (1 g every 8 h) and linezolid (600 mg every 12 h) and after four days, was de-escalated to intravenous ceftriaxone (2 g every 24 h). He completed 3 weeks, followed by 3 weeks of oral cefixime. Complete recovery was achieved.
Microbiological data
Identification (ID) and antimicrobial susceptibility testing (AST) following EUCAST criteria (EUCAST breakpoint version 9.0, www.eucast.org) were carried out by the automated system MicroScan® Walkaway (Beckman Coulter, West Sacramento, CA, United States) using negative combo panel type 53. All IDs were confirmed by MALDI-TOF Microflex Biotyper (Bruker Daltonics, Bremen, Germany).
In order to determine the capsular serotype K1 and K2, polymerase chain reactions (PCRs) were performed using specific primers for the detection of the genes wzx_K1, wzy_K2 and magA [4]. Genetic material from K. pneumoniae isolates was extracted using commercial kit QIAamp DNA Mini Kit (Qiagen, Venlo, The Netherlands). Pulsed-field ground electrophoresis (PFGE) was performed according to PulseNet PFGE protocol for E. coli O157:H7, E. coli non-O157 (STEC), Salmonella, Shigella sonnei and Shigella flexneri to study genetic relatedness [5]. To analyze the clonality of the specimens a multilocus sequence typing (MLST) scheme was performed following the protocol described by Diancourt et al [6] and the alleles and sequence types (STs) were assigned according to the MLST international scheme of the Institut Pasteur, Paris, France (http://bigsdb.pasteur.fr/perl/bigsdb/bigsdb.pl?db=pubmlst_klebsiella_seqdef_public).
K. pneumoniae isolates recovered from patient 1 and 2, belonged to capsular serotype K1 (genes wzx_K1 and magA) while the other two (patient 3 and 4) were K2 (gene wzy_K2). Both of the K1 isolates were classified as ST23, which is one of the major clonal complexes that includes only K1 isolates, and has been described as more virulent than other STs according to in-vitro studies [7]. These ST23 strains were not related by PFGE, indicating that a specific clone may not cause K. pneumoniae liver abscess. K. pneumoniae isolates of serotype K2 belonged to the ST375 and ST881 clones.
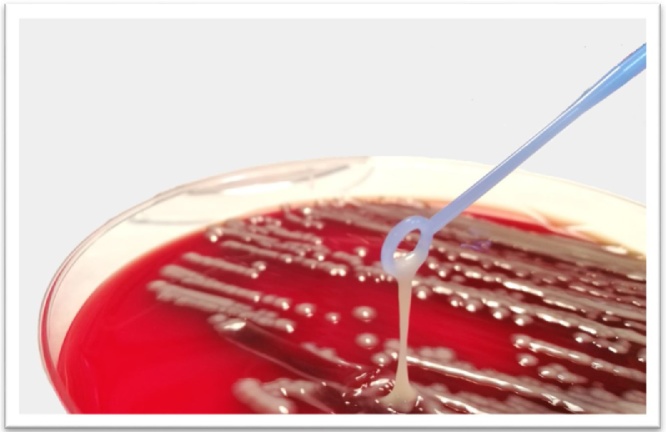
The hypermucoviscous phenotype can be measured semiquantitatively by the “string test”, which consists in the formation of a viscous string >5 mm in length when bacterial colonies on an agar plate are stretched by an inoculation loop. All isolates were positive for this test (Fig. 1). Both serotypes were highly susceptible to all antimicrobials tested including amoxicillin/clavulanate, extended spectrum cephalosporins, carbapenems, aminoglycosides, fluoroquinolones, rifampin, and colistin.
Fig. 1.
“String Test” confirming the hypermucoviscosity of a K. pneumoniae isolate recovered from blood culture (patient 4). A positive result is defined as the formation of a viscous rope greater than 5 mm when a bacterial colony is touched with a loop on an agar plate.
Discussion
Since 1980, especially in Southeast Asia, there has been an increase in the number of reported cases of community infections due to K. pneumoniae specifically by hypermucoviscous strains causing liver abscesses [2,8]. In Europe, K1 and K2 K. pneumoniae isolates are less frequently recovered, and some cases have been associated with Asian citizens or travelers, which was not the case in our patients [3,9].
K1 capsular serotype is a major cause of primary liver abscess and secondary septic embolus and K2 is related to secondary liver abscess. The expression of these capsular serotype antigens confers a mayor resistance to phagocytosis. The gen magA in K1 provides the formation of a protective exopolysaccharide associated with hypermucoviscosity, and the capacity to develop liver abscess and septic metastasis. Moreover aerobactine, an iron chelating siderophore, present in these isolates, potentiates the virulence of hvKP, as has been demonstrated in animal models [8]. In routine laboratory practice, the string test is a useful screening method for subsequent molecular characterization in order to detect possible hypervirulent strains (Fig. 1). Although these hypervirulent variants can affect immunocompetent patients as in the cases presented herein, diabetes mellitus seems to be a major risk factor for the most invasive cases with concomitant poor prognosis, especially in cases of endophthalmitis [10].
Because of the potential for causing metastatic infections, clinicians should be aware of the possibility of serious complications. Among others, it has been suggested that strict glycemic control could help to avoid the development of septic metastatic complications, but more clinical studies are still necessary to definitively suggest the benefit of strict glucose control in these cases [11]. Lungs, central nervous system, and eyes are the most common metastatic sites, but only a third of them are diagnosed on admission. Meningitis and endophthalmitis are associated with poorer outcome in 10–12% of cases, and meningitis is associated with high mortality rates [1,12]. Prognosis for patients with endophthalmitis caused by K. pneumoniae is very poor; more than 85% of patients had a severe visual deficit, however prognosis improves with early diagnosis and early intravenous and intravitreal treatment [13].
Finally, hvKP strains usually show high antimicrobial susceptibility, but this pattern seems to be decreasing over time [14]. Selection of antimicrobial treatment should be guided by in-vitro AST. Adequate drainage of abscesses is recommended for better clinical response. Three weeks of treatment has been recommended, as shorter courses of treatment are responsible for a high rate of relapses.
Conclusions
Outside Asian countries, isolation of hypermucoviscous K. pneumoniae isolates is uncommon. However, the incidence is growing, and is being isolated in individuals without the usual risk factors (diabetes mellitus or Asian origin) associated with infection due to these types of strains. Unlike some recently reported cases, our isolates are of community origin and present with high antimicrobial susceptibility. It is important to improve detection of hvKP isolates in order to optimize outcomes and avoid potential metastatic complications.
Funding
No funding sources have been received by any of the authors.
Conflict of interest
Authors have no conflicts of interest to declare with respect to the contents of this manuscript.
Acknowledgements
RC research is partially supported by Plan Nacional de I+D+i 2013‐2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/0016/0011) ‐ cofinanced by European Development Regional Fund “A way to achieve Europe”, Operative program Intelligent Growth 2014‐2020 and Fundación Soria Melguizo (Madrid, Spain).
MDA was partially supported by the Innovative Medicines Initiative (IMI), European Commission-funded project [iABC grant 115721-2] and the Fundación Francisco Soria Melguizo (Madrid, Spain).
We thank Mary Harper for English correction of the manuscript.
References
- 1.Liu Y.C., Cheng D.L., Lin C.L. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med. 1986;146:1913–1916. [PubMed] [Google Scholar]
- 2.Fang C.-T., Chuang Y.-P., Shun C.-T., Chang S.-C., Wang J.-T. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med. 2004;199:697–705. doi: 10.1084/jem.20030857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Decré D., Verdet C., Emirian A., Le Gourrierec T., Petit J.-C. Emerging severe and fatal infections due to Klebsiella pneumoniae in two university hospitals in France. J Clin Microbiol. 2011;49:3012–3014. doi: 10.1128/JCM.00676-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang C.T., Lai S.Y., Yi W.C., Hsueh P.R., Liu K.L., Chang S.C. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007;45:284–293. doi: 10.1086/519262. [DOI] [PubMed] [Google Scholar]
- 5.Han H., Zhou H., Li H., Gao Y., Lu Z., Hu K. Optimization of pulse-field gel electrophoresis for subtyping of Klebsiella pneumoniae. Int J Environ Res Public Health. 2013;10:2720–2731. doi: 10.3390/ijerph10072720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diancourt L., Passet V., Verhoef J., Grimont P.A.D., Brisse S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol. 2005;43:4178–4182. doi: 10.1128/JCM.43.8.4178-4182.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siu L.K., Fung C.-P., Chang F.-Y., Lee N., Yeh K.-M., Koh T.H. Molecular typing and virulence analysis of serotype K1 Klebsiella pneumoniae strains isolated from liver abscess patients and stool samples from noninfectious subjects in Hong Kong, Singapore, and Taiwan. J Clin Microbiol. 2011;49:3761–3765. doi: 10.1128/JCM.00977-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeh K.-M., Kurup A., Siu L.K., Koh Y.L., Fung C.-P., Lin J.-C. Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J Clin Microbiol. 2007;45:466–471. doi: 10.1128/JCM.01150-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cubero M., Grau I., Tubau F., Pallarés R., Dominguez M.A., Liñares J. Hypervirulent Klebsiella pneumoniae clones causing bacteraemia in adults in a teaching hospital in Barcelona, Spain (2007-2013) Clin Microb Infect. 2016;22:154–160. doi: 10.1016/j.cmi.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 10.Sheu S.-J., Kung Y.-H., Wu T.-T., Chang F.-P., Horng Y.-H. Risk factors for endogenous endophthalmitis secondary to klebsiella pneumoniae liver abscess. Retina. 2011;31:2026–2031. doi: 10.1097/IAE.0b013e31820d3f9e. [DOI] [PubMed] [Google Scholar]
- 11.Lin J.-C., Siu L.K., Fung C.-P., Tsou H.-H., Wang J.-J., Chen C.-T. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniaein type 2 diabetes mellitus patients with poor glycemic control. J Clin Endocrinol Metab. 2006;91:3084–3087. doi: 10.1210/jc.2005-2749. [DOI] [PubMed] [Google Scholar]
- 12.SS-J Lee, Chen Y.-S., Tsai H.-C., Wann S.-R., Lin H.-H., Huang C.-K. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 2008;47:642–650. doi: 10.1086/590932. [DOI] [PubMed] [Google Scholar]
- 13.Siu L.K., Yeh K.-M., Lin J.-C., Fung C.-P., Chang F.-Y. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis. 2012;12:881–887. doi: 10.1016/S1473-3099(12)70205-0. [DOI] [PubMed] [Google Scholar]
- 14.Arena F., De Angelis L.H., D’Andrea M.M., Cannatelli A., Fossati L. Infections caused by carbapenem-resistant Klebsiella pneumoniae with hypermucoviscous phenotype: a case report and literature review. Virulence. 2017;8(November (8)):1900–1908. doi: 10.1080/21505594.2017.1286439. [DOI] [PMC free article] [PubMed] [Google Scholar]