Abstract
Background
Diabetes Mellitus is a progressive, chronic and multifactorial endocrine disorder characterized by elevated serum glucose levels. It has a direct effect to social and health related quality of life.
Objective
This study aimed to determine the health-related quality of life among patients with type II diabetes mellitus (T2DM) using insulin therapy.
Methods
Cross-sectional observational study design was used to collect data from Malaysian patients with T2DM. Subjective and objective assessments were made either by using several questionnaires or each patient's specific medication profile registered to care sites. Study participants were recruited from both public hospitals and community health clinics located in Kuala Lumpur, Malaysia.
Results
A total of 430 patients with T2DM were recruited in this study with a response rate of 94.7%. The oral antidiabetic medication (OAM) group consisted of 63.0% of the study population and the rest (37.0%) were Insulin users. The body mass index and glycosylated hemoglobin patterns were significantly different between groups (P < 0.011 and P < 0.001). Insulin users showed high percentages of healthy body mass index index (44.7%) compared with OAM users (35.8%) and controlled glycemic index (glycosylated hemoglobin ≤7.5%) was significantly (P = 0.001) better among the insulin-user group compared with the OAM group. The Euro Quality of Life–5 dimension domain analysis indicated significant differences with domains of usual work (P < 0.047), pain and discomfort (P < 0.041), and anxiety and depression (P < 0.001) among insulin users versus OAM users. We also observed a significant difference between the groups regarding diet, monitoring, and disease-specific knowledge. The mean (SD) adherence score showed that insulin users were significantly (P < 0.001) more adherent (6.09 [2.98]) than OAM were nonadherent (4.19 [4.68]).
Conclusions
This study suggests the valuable effect of insulin therapy among patients with T2DM compared with OAMs on health-related quality of life, medication adherence, and health state. Insulin users reported they had better diabetes-related knowledge and treatment adherence characteristics than noninsulin users.
Key words: Adherence, Cross-sectional study, Diabetes knowledge, Health perception, Health care quality of life, Insulin use
Introduction
Diabetes mellitus (both type I and type II) is categorized as a progressive metabolic disorder consequently leading to serious morbidities and mortality.1 The International Diabetes Federation reported 366 million patients with diabetes in 2011 and predict that number to double by 2030.2 The prevalence of type II diabetes mellitus (T2DM) is predominant over type I diabetes across the globe. The previous scientific literature reported several clinical morbidities associated with T2DM3 that indeed deteriorate patients' social and general health conditions.4 Thus, T2DM induces high risk to public health and a threat to health care systems.5 The age-exposure effects of T2DM show that adult-age incidence increases the development of severe complications (both micro- and macrovascular), leading to a reduction in health-related quality of life (HRQoL).6, 7, 8
HRQoL is a multidimensional construct consisting of several characteristics to determine the role of emotional and physical functioning of patients with diabetes.9 The management of diabetes is based on a multifactorial concept and several demographic parameters, with disease and social factors strongly influencing the treatment management outcomes.7, 10 Monitoring and control of blood glucose is a viable tool to determine disease control and rational therapy.3, 6 However, several studies reported a strong influence of patient-related factors on blood glucose intolerance, including perception and self-care behavior.3, 6, 8, 11 Self-care, including self-monitoring of blood glucose, showed a positive effect on controlled glycemic levels,4, 7,9, 10, 11 considering the fact that diabetes-related disease knowledge plays a vital role in association with self-care behaviors of a patient.12 In addition, the long-term adverse effects of the disease reduce the self-care behaviors of patients and result in poor health state and HRQoL.13, 14
Medication adherence, diabetes-related knowledge, and patient satisfaction are the potential parameters for improving HRQoL.15 None of the studies have discussed these factors among Malaysian populations. Malaysia is a multiethnic society with different lifestyle patterns and religious practices,2, 3, 8, 9 mainly consisting of Malay, Chinese, and Indian ethnicity. In this diverse population, it is essential to determine the HRQoL multiconstruct model. Likewise, the literature suggests that treatment modality may influence the outcome of the disease, but not a single study has compared and/or contrasted the parameters of HRQoL between different modalities of treatment to date. Therefore, this study aimed to evaluate and determine the predictors of HRQoL among patients with T2DM based on treatment with oral antidiabetic medication (OAM) versus insulin users (combination therapy).
Materials and Methods
Study design and setting
This cross-sectional observational study used a multidimensional assessment method to collect data from Malaysian patients with T2DM. Subjective and objective assessments were made by using multiple questionnaires or the specific medication profiles of patients registered at care sites. Study participants were recruited from both public hospitals (2 general hospitals) and community health clinics (4 tertiary care clinics) located in Kuala Lumpur, Malaysia.
Ethics statement
The Ministry of Health and clinical research committees approved the study protocol. Study participants were requested to provide the signatory for the mandatory consent form upon acceptance. Participants were also informed about the voluntary participation and that they could leave the study at any time. All the publications/reports generated from this study were elusive to anonymity and privacy policy.
Sample size, inclusion criteria, and technique
The sample size was calculated by using the prevalence-based sampling method.16 Approximately 16.7%17 was the prevalence of T2DM in Malaysia (latest data available is 2015). A cumulative double design was applied to study sample size, where
Z = CI, p = prevalence of T2DM, and d = margin of error:
n = Z2 × p (1 – p)/d2
n = 1.962 × 0.167 (0.833) / 0.052
n = 214.3 × DEFF(2) (Design effect = reduce sampling bias)18
n = 428.6 ≈ 429
The health clinic computerized database was used to select the potential eligible patients. A random numbers of table in Excel software (Microsoft Corp, Redmond, Washington) were used to identify the participants to enroll in the study for further research applications. Stratified random sampling technique was used to enroll patients into the study. The inclusion criteria focused on age >18 years, registered for treatment at least 12 months (ie, 365 days), and language understanding (ie, read and speak) in Malay or English. Patients with severe clinical complications were excluded; for example, end-stage renal failure, liver cirrhosis, cancer (any type), physical disability, and mental impairment/condition (such complications influence HRQoL so the finding will not be truly representative of diabetes-related HRQoL). Special conditions were also not eligible because of temporary or specific low HRQoL and health status predeterminations; for example, pregnant women, geriatric patients (age >75 years) and patients claiming herbal supplement use (due to low clinical evidence).
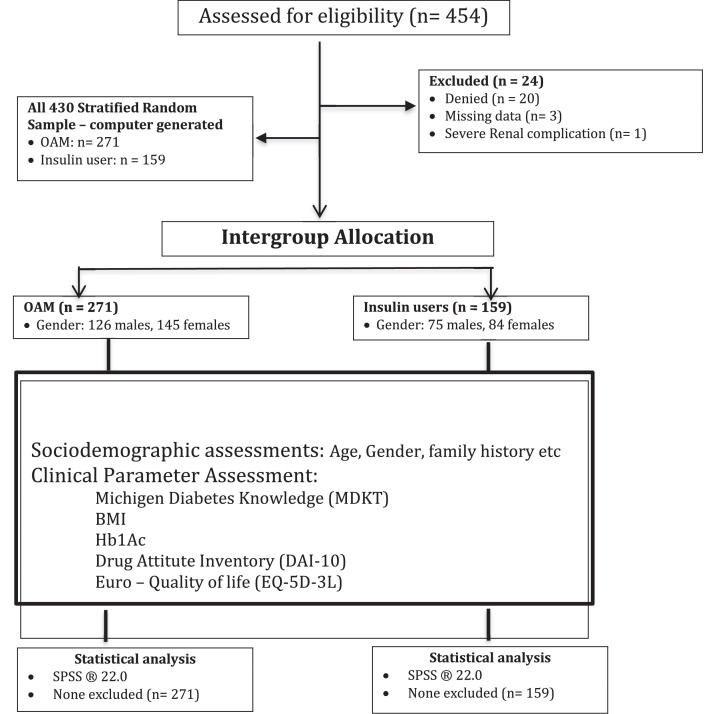
A total of 454 patients were contacted and approached, among them, 20 patients denied participating, 3 patients had missing data, and 1 had severe renal complications. Therefore, after exclusions/dropouts, data for 430 participants were compiled for analysis. Patients were then sorted into 2 groups on the basis of their treatment modality: OAM (n = 271; 63.0%) and insulin users (n = 159; 37.0%) (see the Figure).
Figure.
Consolidated standards of reporting trials diagram. BMI = body mass index; HbA1c = glycosylated hemoglobin; OAM = oral antidiabetic mediation.
Study tools and data collection
Participants were stratified according to treatment modality (insulin users vs noninsulin users). Intergroup assessments of sociodemographic characteristics, clinical parameters, diabetes-related knowledge, treatment adherence, and satisfaction were independent variables to predict the effect on HRQoL and differentiate the response among insulin users in the multivariate analysis. Prevalidated questionnaires were used for assessments and the developer and/or validator obtained the informed consents before ethics approval.
Sociodemographic and clinical parameters
A self-developed data collection form was used to obtain the sociodemographic and medical history data from patients' medication profile. The sociodemographic section consists of 7 items, including smoking and alcohol intake. However, clinical data like family history of diabetes, duration of diabetes, comorbidities, body mass index (BMI), and glycosylated hemoglobin (HbA1c) values were collected from the patients’ medical profiles. Both BMI and HbA1c values indicated the latest reported values. A treatment satisfaction statement was included in this form to rate overall satisfaction levels to a 3-point Likert scale, where 1 = satisfied, 2 = neutral, and 3 = dissatisfied. This was among the subjective assessments based on participants' experiences with the availability of health professionals and services in health care settings.
Michigan Diabetes Knowledge Test
The Michigan Diabetes Knowledge Test (MDKT)19 tool consists of 23 knowledge test items; however, the first 14 items were only appropriate for noninsulin users. Hence, to avoid analysis bias this study only used 14 items for both insulin versus noninsulin users to compare and contrast base knowledge. MDKT scoring was based on correct or wrong response to the specific item; therefore, scores ranged from 0 to 14. Further classification of knowledge scores was poor knowledge < 7, average 7–11, and good > 11. The MDKT tool was prevalidated and considered as a reliable tool for Malaysia populations.20 Permission to use the Malaysian version of the MDKT was obtained.
Drug Attitude Inventory
The Drug Attitude Inventory (DAI-10)21 instrument consists of 10 statements with the possible response of yes or no, and negative markings were assigned based on the wrong answer. Therefore, the score ranges from –10 to 10. Participant score < 0 was considered nonadherent, 0 to 5 conditional adherent, and 6 to 10 adherent. DAI-10 is a valid and reliable tool for Malaysian populations21; thus, no potential analytical bias was suspected in this study.
Euro-Quality of Life tool
The Euro-Quality of Life (EQ-5D-3L)22, 23 tool consists of 5 characteristic dimensions; each corresponds to a 3-point Likert scale on level of severity from no problem to extreme problem. A 5-digit code shows the state of health and reflects problems in the specific 5-domain construct. EQ-5D-3L index value was calculated by deducting the appropriate weights from 1 (eg, 11,111 state value for full health). Also, participants' self-rated health status was determined by using a visual analog scale, where 0 = worst imaginable health to 100 = best health. The 5-dimension index and the visual analog scale score were converted to substantial value score ranging between 0 = worst state and 1 = best state. This assessment can be used as a quantitative assessment of health status and treatment outcome. A pilot study among 35 patients was conducted to validate EQ-5D-3L and to ensure readability and understandability of the translated version. Cronbach α of 0.84 internal consistency was achieved, so this a reliable tool for this study.
Statistical analysis
The Statistical Package for the Social Sciences version 22.0 (IBM-SPSS Inc, Armonk, NY) was used for data analysis and findings at P < 0.05 were considered significant. Descriptive statistics were used to present sociodemographic and clinical parameters. Nominal variables were presented with frequency and percentage, the intergroup association among variables was compared through χ2 test. Continuous variables were presented with mean and SD and the intergroup association was evaluated by Student t test. Scoring of MDKT, DAI-10, and HRQoL was calculated per descriptive guidelines provided by the respective developers of the instruments. The association between study variables and HRQoL among insulin users versus noninsulin users were evaluated by χ2 and Cramér V/φ test was used to interpret the effect. The significant factors were then further assessed for predictive model expressed as odds ratio (OR) with 95% CI with a P value < 0.05.
Results and Findings
Sociodemographic and clinical characteristics
A total of 430 patients with T2DM were recruited into the study with a response rate of 94.7%. The OAM group represented 63.0% of the study population and the remaining 37.0% were sorted out for an insulin user with OAM combination group. There was no significant difference observed in between the groups with the sociodemographic variables except marital status (P < 0.002). Insulin users had a high frequency (34.0%) of singles (ie, never married) compared with OAM users (22.1%). BMI and HbA1c patterns were significantly different between groups (P < .011 and P < 0.001). Insulin users showed high percentages of healthy BMI values (44.7%) compared with OAM users (35.8%). Controlled glycemic index was also reported to be exceedingly high (64.2%) among insulin users compared with OAM users (44.6%). The distribution patterns are presented in Table 1. Overall satisfaction with current treatment did not show any significant difference between groups, although insulin users reported slightly higher percentages in both upper and lower end responses (satisfaction and dissatisfaction) than noninsulin users.
Table 1.
Demographic and clinical characteristics of the study population.
| Characteristic | OAM only* (n = 271) | OAM + insulin* (n = 159) | P value† |
|---|---|---|---|
| Sociodemographic | |||
| Gender | 0.541 | ||
| Male | 126 (46.5) | 75 (47.2) | |
| Female | 145 (53.5) | 84 (52.8) | |
| Age‡ (y) | 0.022 | ||
| ≤ 40 | 79 (29.1) | 35 (22.0) | |
| 40–60 | 164 (60.5) | 87 (54.7) | |
| > 61 | 28 (10.4) | 37 (23.3) | |
| Education | 0.713 | ||
| Primary | 29 (10.7) | 18 (11.3) | |
| Secondary | 86 (31.7) | 66 (41.5) | |
| University | 142 (52.4) | 51 (32.1) | |
| Higher | 14 (5.2) | 24 (15.1) | |
| Marital status | 0.002 | ||
| Ever married | 211 (77.9) | 105 (66.0) | |
| Never married | 60 (22.1) | 54 (34.0) | |
| Smoking habit | 0.413 | ||
| Ever smoked | 204 (75.3) | 111 (69.8) | |
| Never smoked | 67 (24.7) | 48 (30.2) | |
| Alcohol consumption | 0.225 | ||
| Ever drink | 107 (39.5) | 52 (32.7) | |
| Never drink | 164 (60.5) | 107 (67.3) | |
| Employment status | 0.343 | ||
| Governmental | 148 (54.6) | 101 (63.5) | |
| Nongovernmental | 123 (45.4) | 58 (36.5) | |
| Overall, satisfaction with current treatment | 0.087 | ||
| Satisfied | 122 (45.0) | 79 (49.7) | |
| Neutral response | 91 (33.6) | 34 (21.4) | |
| Dissatisfied | 58 (21.4) | 46 (28.9) | |
| Clinical parameters | |||
| Family history of diabetes | 0.741 | ||
| Yes | 218 (80.4) | 131 (82.4) | |
| No | 53 (19.6) | 28 (17.6) | |
| Duration of diabetes (y) | 0.512 | ||
| 0–5 | 64 (23.6) | 21 (13.2) | |
| 6–10 | 139 (51.3) | 87 (54.7) | |
| > 10 | 68 (25.1) | 51 (32.1) | |
| Comorbidities | 0.814 | ||
| Congestive heart disease | 42 (15.5) | 27 (17.0) | |
| Mild liver disease | 23 (8.5) | 18 (11.3) | |
| Hyperlipidemia | 55 (20.3) | 21 (13.2) | |
| Others | 4 (1.5) | 8 (5.0) | |
| None | 147 (54.2) | 85 (53.5) | |
| Body mass index | 0.011 | ||
| < 18.5/underweight | 113 (41.7) | 67 (42.1) | |
| 18.5-24.9/Healthy | 97 (35.8) | 71 (44.7) | |
| 25.0-29.9/overweight | 61 (22.5) | 21 (13.2) | |
| HbA1c (%) | 0.001 | ||
| ≤ 7.5 | 121 (44.6) | 102 (64.2) | |
| > 7.5 | 150 (55.4) | 57 (35.8) | |
HbA1c = glycosylated hemoglobin; OAM = oral antidiabetic medications.
Values are presented as n (%).
Boldface type indicates significance at P < 0.05 based on χ2 test for the nominal variables.
Median age (SD): 49.31 (10.42) years.
§Body mass index and HbA1c values were the last reported values in the medical profile.
HRQoL pattern and profiling
The HRQoL scores and patterns among groups are presented in Table 2. The EQ-5D-3L mean (SD) index value showed a significantly better quality of life (0.63 [0.14]) among insulin users than noninsulin users (0.49 [0.25]) (P < 0.001). Similarly, participants’ self-reported QoL was overall good and better among insulin users than noninsulin users (64.53% and 51.68% visual analog scale; P < 0.001). The EQ-5D-3L domain analysis reported significant differences in the domains of usual work (P < 0.047), pain and discomfort (P < 0.041) and anxiety and depression (P < 0.001) among insulin users versus OAM users. Mobility and self-care domains showed similar patterns between groups.
Table 2.
Assessment of health-related quality of life among participants.
| Euro Quality of Life–5 dimensions domain* | Health state | OAM only† | OAM + insulin† | P value‡ |
|---|---|---|---|---|
| Mobility | 0.811 | |||
| No problems with walking | 1 | 214 (79.0) | 118 (74.2) | |
| Some problems with walking | 2 | 40 (14.8) | 29 (18.2) | |
| Confined to bed | 3 | 17 (6.2) | 12 (7.6) | |
| Self-care | 0.745 | |||
| No problems with self-care | 1 | 231 (85.2) | 139 (87.4) | |
| Some problem washing or dressing | 2 | 37 (13.7) | 18 (11.3) | |
| Unable to wash or dress myself | 3 | 3 (1.1) | 2 (1.3) | |
| Usual work | 0.041 | |||
| No problem with daily activities | 1 | 189 (69.7) | 124 (78.0) | |
| Some problem with the usual activities | 2 | 67 (24.7) | 28 (17.6) | |
| Unable to perform usual activities | 3 | 15 (5.6) | 7 (4.4) | |
| Pain and discomfort | 0.047 | |||
| No pain or discomfort | 1 | 166 (61.3) | 81 (50.9) | |
| Moderate pain or discomfort | 2 | 64 (23.6) | 55 (34.6) | |
| Extreme pain or discomfort | 3 | 41 (15.1) | 23 (14.5) | |
| Anxiety and depression | 0.001 | |||
| No anxiety or depression | 1 | 33 (12.2) | 59 (37.1) | |
| Moderately anxious or depressed | 2 | 178 (65.7) | 82 (51.6) | |
| Extremely anxious or depressed | 3 | 60 (22.1) | 18 (11.3) | |
| Euro Quality of Life–5 dimensions index value§ | 0.49 (0.25) | 0.63 (0.14) | 0.001 | |
| Visual analog scale§ | 51.68 (18.79) | 64.53 (15.21) | 0.001 |
Domains are briefly discussed in the Methods. Five domains were evaluated on the basis of 3 levels of severity coded as 1, 2, 3; therefore, each health state has 5-digit code (eg, 11,111 reflects no problem in any domain).
Values are presented as n (%).
Boldface type indicates significance at P < 0.05 based on χ2 test for nominal variable and Student t test for comparing means.
Values are presented as mean (SD).
Health state assessment
A total of 63 OAM and 57 insulin users reported different health states in the study population. Top-10 health states based on frequency are shown in Table 3. A total of 135 (49.8%) participants in the OAM and 84 (52.8%) participants in the insulin-users group constituted top-10 health states (Table 3) in term of frequency and percentage distribution.
Table 3.
Top-10 health states.*
| Health state | OAM only† | Health state | OAM + insulin† |
|---|---|---|---|
| 11,111 | 52 (19.2) | 11,111 | 33 (20.8) |
| 11,122 | 23 (8.5) | 12,123 | 11 (6.9) |
| 11,221 | 14 (5.2) | 11,232 | 9 (5.7) |
| 11,233 | 11 (4.1) | 11,223 | 9 (5.7) |
| 12,223 | 9 (3.3) | 11,212 | 7 (4.4) |
| 12,231 | 7 (2.6) | 21,221 | 5 (3.1) |
| 22,331 | 7 (2.6) | 22,232 | 3 (1.9) |
| 22,333 | 5 (1.8) | 22,122 | 3 (1.9) |
| 21,233 | 4 (1.5) | 21,233 | 2 (1.3) |
| 23,332 | 3 (1.1) | 23,233 | 2 (1.3) |
OAM = oral antidiabetic medication.
Domains are briefly discussed in the Methods. Five domains were evaluated on the basis of 3 levels of severity coded as 1, 2, or 3; therefore, each state has 5-digit code (eg, 11,111 reflects no problem in any domain).
Values are presented as frequency (%).
Diabetes-related knowledge test assessment
Knowledge test score patterns are provided in Table 4. It was found that most OAM participants (n = 191; 70.5%) had poor diabetes-related knowledge compared with insulin users (n = 43; 27.0%) (P < .001). The poor knowledge reflects issues related to diet and diabetes-related management knowledge. Our findings also revealed significant differences between groups regarding diet, monitoring, and disease-specific knowledge. Overall mean (SD) knowledge score reported that insulin users had a better level of knowledge (8.22 [1.97]) than OAM participants (6.13 [2.29]) (P < 0.001).
Table 4.
Diabetes-related knowledge among study participants.
| Characteristic* | OAM only† | OAM + insulin† | P value‡ |
|---|---|---|---|
| Suitable diet for diabetic patients | 113 (41.7) | 79 (49.7) | 0.051 |
| High carbohydrate foods | 109 (40.2) | 71 (44.7) | 0.022 |
| High fat content | 159 (58.7) | 122 (76.7) | 0.001 |
| Free food for patients with diabetes | 94 (34.7) | 68 (42.8) | 0.013 |
| HbA1c interpretation | 148 (54.6) | 134 (84.3) | 0.001 |
| Method for blood glucose monitoring | 183 (67.5) | 129 (81.1) | 0.001 |
| Unsweetened fruit effect on blood glucose | 109 (40.2) | 61 (38.4) | 0.134 |
| Treatment of low blood glucose | 92 (34.0) | 84 (52.8) | 0.017 |
| Effect of exercise on controlled glucose levels | 209 (77.1) | 139 (87.4) | 0.001 |
| Effect of infection on blood glucose | 77 (28.4) | 51 (32.1) | 0.367 |
| Foot care practice | 162 (59.8) | 133 (83.6) | 0.001 |
| Low-fat food reduces disease risks | 126 (46.5) | 89 (56.0) | 0.034 |
| Numbness and tingling interpretation | 192 (70.8) | 108 (67.9) | 0.231 |
| Problem not associated with diabetes | 201 (74.2) | 135 (84.9) | 0.011 |
| Knowledge score | 6.13 (2.29) | 8.22 (1.97) | 0.001 |
HbA1c = glycosylated hemoglobin; OAM = oral antidiabetic medication.
True answers only.
Values are presented as n (%).
Boldface type indicates significance at P < 0.05 based on χ2 test for the nominal variable, Student t test for comparing means.
§The knowledge score was calculated by awarding 1 score to the right answer and 0 to wrong response. Therefore, total score = 14 (< 7 = poor level, 7–11 = average level, and > 11 good knowledge level). Knowledge score is presented as mean (SD).
Medication adherence assessment
The drug attitude inventory tool was used to evaluate the adherence level among insulin users and noninsulin users. Table 5 provides the data on the level of adherence among the study population. Intergroup assessment showed that only item 7, “Medication makes me feel better,” was not statistically significant between groups. Otherwise, all the other 9 items reported significant differences among insulin users versus OAM users. The overall mean (SD) adherence score showed that insulin users were significantly (P < 0.001) more adherent (6.09 [2.98]) than OAM users (4.19 [4.68]).
Table 5.
Medication adherence profiling.
| Drug adherence item* | OAM only† | OAM + insulin† | P value‡ |
|---|---|---|---|
| Medication outweighs the bad | 121 (44.6) | 113 (71.1) | 0.001 |
| Feel uncomfortable with medication | 83 (30.6) | 74 (46.5) | 0.001 |
| Medication of my own choice | 252 (93.0) | 123 (77.3) | 0.010 |
| Medications make me more relaxed | 211 (77.8) | 139 (87.4) | 0.001 |
| Medication makes me tired and sluggish | 164 (60.5) | 58 (36.5) | 0.001 |
| Medication used only when I feel sick | 141 (52.0) | 49 (30.8) | 0.001 |
| Feel better on medication | 209 (77.1) | 112 (70.4) | 0.314 |
| Unnatural for mind and body to be controlled by medication | 147 (54.2) | 31 (19.5) | 0.001 |
| Medication makes thoughts clearer | 227 (83.7) | 78 (49.0) | 0.001 |
| Medications prevent me to get sick | 239 (88.1) | 126 (79.2) | 0.027 |
| Adherence score§ | 4.19 (4.68) | 6.09 (2.98) | 0.001 |
True answers only.
Values are presented as n (%).
Boldface type indicates significance at P < 0.05 based on χ2 for the nominal variable and Student t test for comparing means.
Adherence score was calculated by using a negative mark for the wrong answer where score < 0 = nonadherent, 0–5 = conditional adherent, and 6–10 = adherent. Adherence score is presented as mean (SD).
Predictors of HRQoL among Insulin users versus noninsulin users
The association between HRQoL among OAM users and study variables showed that age, treatment satisfaction, family history of diabetes, duration of diabetes, comorbidities, and medication adherence were significantly associated variables, with Cramér V strong positive association effect range from 0.543 to 0.617. In addition to these variables, Insulin users also reported effect on education level, marital status, BMI, and HbA1c, with the Cramér V test revealing a strong positive association effect range from 0.510 to 0.639. Table 6 shows the detailed analytical data.
Table 6.
Predictors of health-related quality of life (HRQoL) among insulin and noninsulin users.*
| Characteristic | OAM – HRQoL P value |
OAM + Insulin HRQoL P value |
|---|---|---|
| Gender | 0.421 | 0.835 |
| Age | 0.011 (φc = 0.562) | 0.013 (φc = 0.588) |
| Education | 0.083 | 0.017 (φc = 0.544) |
| Marital status | 0.163 | 0.027 (φc = 0.565) |
| Smoking | 0.302 | 0.411 |
| Alcohol use | 0.078 | 0.107 |
| Employment | 0.648 | 0.883 |
| Treatment satisfaction | 0.022 (φc = 0.581) | 0.003 (φc = 0.639) |
| Family history | 0.011 (φc = 0.547) | 0.001 (φc = 0.622) |
| Duration of diabetes | 0.007 (φc = 0.543) | 0.024 (φc = 0.559) |
| Comorbidities | 0.010 (φc = 0.557) | 0.001 (φc = 0.597) |
| BMI | 0.149 | 0.011 (φc = 0.553) |
| HbA1c | 0.246 | 0.018 (φc = 0.510) |
| Diabetes-related knowledge | 0.647 | 0.546 |
| Medication adherence | 0.031 (φc = 0.617) | 0.021 (φc = 0.632) |
BMI = body mass index; HbA1c = glycosylated hemoglobin; OAM = oral antidiabetic medication.
Boldface type indicates significance at P < 0.05 based on χ2 or Cramér V test. Values in parentheses are the interpretation of effect (0.50–0.99 strongly predicting effect).
Logistic regression modeling was used with the significantly associated independent variables and compared with HRQoL (insulin vs OAM). The Omnibus test of model significance was highly significant, indicating the models were advisable. Treatment satisfaction had significant association (adjusted OR = 2.25; 95% CI = 1.49–2.78; P < 0.001) with insulin users. However, medication adherence (adjusted OR = 1.83; 95% CI = 1.22–1.97; P < 0.001) showed a significant association among OAM users. Thus, a 1-point increase in treatment satisfaction would improve HRQoL among patients with T2DM with insulin use about 2.25 times, and similarly, a 1-point increase in medication adherence would predict to improve approximately 1.83 times HRQoL among patients with T2DM using OAM only. These predictors reflected the improvement in HRQoL among insulin users in comparison to noninsulin users provided that the other factors remained constant.
Discussion
Although several clinical literature works have reported profiling and predicting the effect of multiple variables on HRQoL among patients with T2DM, the data from Malaysia are scarce and none have reported treatment-specific predicting factors. Therefore, in this study we showed a true reflection of the Malaysian community and created a global benchmark to compare HRQoL among insulin and noninsulin users.
The findings reported OAM with poor HRQoL than insulin therapy. The value score of the EQ-5D-3L visual analog scale index also indicated significantly low indices among OAM users.10, 13 The negative influence of T2DM on HRQoL and health state is widely reported across the world,15, 24, 25 but current apprehension focuses on the reversibility of such deteriorating effects with rational treatment modalities. This study also reported that insulin users had a better and improved HRQoL compared with OAM use only.
Several previous studies have reported that factors like age, treatment satisfaction, demographic characteristics, and number of diabetes-related medications have an influence on HRQoL.5 Redekop et al26 reported that treatment satisfaction was the only key independent predictor for HRQoL among patients with T2DM.26 In our study, we evaluated the predicting effects of sociodemographic, clinical, and behavior parameters. Our findings were significantly associated with age, treatment satisfaction, and medication adherence as well as BMI and HbA1c value. Such predicting effects were limited to the treatment modalities, insulin users have more confounding predictors compared with noninsulin users. Our findings also reported that the strongest predictor for improved HRQoL amongst insulin users was treatment satisfaction and treatment adherence when compared with noninsulin users. These findings are first of its kind reported, although previous literature has reported similar findings with a single cohort of patients with T2DM without sorting for treatment line.14, 21, 24 Jamie et al27 reported that premixed 70/30 insulin controlled postprandial glycemic index and improved HRQoL among patients with T2DM in relation to hypoglycemic events.
Family history of diabetes,28 duration of diabetes,25 comorbidities,29 and medication adherence 13, 14, 30 were also significant contributing factors for reducing HRQoL and health state among patients with T2DM. This study reported a strong positive effect of these variables on the diabetes-related QOL, regardless of the patient using insulin or OAM. Pichon et al31 reported the positive influence of insulin use in low–middle income countries on high HRQoL and improved health status among patients with T2DM,31 and recommended early clinical management of diabetes with insulin therapy. The present study validated these findings for primary diabetes care. Longer duration of diabetes results in cardiovascular diseases and substantially reduced cardiac output in patients. Patients receiving insulin therapy are likely to increase muscle perfusion through redistribution of regional blood flow instead of increasing cardiac output.32 Such findings prefer insulin therapy over OAM in primary care settings. Our study supports the argument that insulin users have improved HRQoL compared with OAM users.
Medication adherence reported the highest OR in predicting the HRQoL among patients with OAM, but treatment satisfaction showed the directly proportional among insulin users. Past studies casually discussed the role of medication adherence to HRQoL among patients with T2DM.12, 33, 34 However, this study concisely discussed the factor effect and association pattern among patients regardless of treatment modalities and demographic distribution. This study also reported a negative effect of nonadherence on HRQoL among patients with T2DM provided other conditions remained constant, and these findings are in concordance with the previous literature.35, 36, 37 Insulin users reported a significant association with BMI and, on the other hand, such effect was undetermined among OAM patients. A study conducted by Redekop et al26 concluded the potential effect of Insulin therapy together with obesity on HRQoL among Dutch patients with T2DM. High HbA1c index was also reported as a potential predictor to reduce QoL.38 This supports previous findings in a Malaysian population and determines the extent of the predictor's effect on HRQoL among patients with insulin versus noninsulin users. Our findings will help health care professionals design and improve health care plans for patients with specific characteristics and will promote the individualization of treatment models.
Treatment satisfaction, self-care behavior, and drug adherence are key determinants of patients’ diabetes management outcomes, treatment-specific glucose tolerance, HRQoL, social functioning, and disease management costs.39 Optimal adherence will tend to make patients feel better about health state and differentiate the effect. Subsequently, this will improve the subjective perception of HRQoL on desired outcomes, as well as overall improvement in patient response and treatment satisfaction.
Limitations of the study
The cross-sectional observational study design has limitations, but in this study, we tried to reduce bias by sorting patients to treatment modality. Data collected from a single city cannot be generalized, but Kuala Lumpur is the capital of Malaysia and in fact, most Malaysians living in this city come from various parts of Malaysia. Further research required to completely address the beneficial results of insulin therapy. Finally, different assessment tools might reveal different findings; thus, concerns should focus on comparison and validation of specific clinical tools to the Malaysian population and also contrast the findings to provide better information to optimize treatment protocol in health care settings.
Conclusions
The results of this study suggest the valuable effect of insulin therapy among patients with T2DM compared with OAM on HRQoL, medication adherence, and health state. Insulin users reported better diabetes-related knowledge and treatment adherent characteristics than noninsulin users. This study also showed a strong association of age, education, marital status, BMI, HbA1c, adherence, and treatment satisfaction in the model prediction to improve HRQoL among insulin users with T2DM.
Acknowledgments
Acknowledgments
The authors thank the nursing staff for arranging patients’ records and managing the scheduling of follow-ups. The authors also thank the College of Pharmacy administration for continued support on administrative approvals.
Dr Gillani was the principal investigator and drafted the manuscript. Drs Ansari and Zaghloul were responsible for content analysis and data validation. Drs Abdul, Rathore, and Sulaiman participated in data collection and data analysis. Drs Baig, Rathore, and Althagfan participated in study content analysis and helped to draft the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors have indicated that they have no conflicts of interest regarding the content of this article.
Contributor Information
Syed Wasif Gillani, Email: sgillani@taibahu.edu.sa.
Hassaan Anwar Rathore, Email: hassaan@usm.my.
References
- 1.Gillani Syed Wasif. Determining Effective Diabetic Care; A Multicentre - Longitudinal Interventional Study. Current Pharmaceutical Design. 2016;22:1–8. doi: 10.2174/1381612822666160813235704. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. About diabetes. 2013. http://www.idf.org/about-diabetes. Accessed 05-04-2017.
- 3.Gillani Syed Wasif, Sulaiman Syed Azhar Syed, Abdul Mohi Iqbal Mohammad, Baig Mirza R. Combined effect of metformin with ascorbic acid versus acetyl salicylic acid on diabetes-related cardiovascular complication; a 12–month single blind multicenter randomized control trial. Cardiovasc Diabetol. 2017;16:103. doi: 10.1186/s12933-017-0584-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lamand D.W., LeRoith D. The worldwide diabetes epidemic. Current Opinion in Endocrinology, Diabetes & Obesity. 2012;19(2):93–96. doi: 10.1097/MED.0b013e328350583a. [DOI] [PubMed] [Google Scholar]
- 5.Alberti K.G.M.M., Zimmet P., Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabetic Medicine. 2006;23(5):469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 6.Gillani Syed Wasif, Azeem Eman, Siddiqui Ammar, Mian Rashid Iqbal, Poh Vinci, Sulaiman Syed Azhar Syed, Baig Mirza Rafiullah. Oxidative Stress Correlates (OSC) in Diabetes Mellitus Patients. Current Diabetes Reviews. 2016;12:279–284. doi: 10.2174/1573399811666150520094631. [DOI] [PubMed] [Google Scholar]
- 7.Whiting D.R., Guariguata L., Weil C., Shaw J. IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Research and Clinical Practice. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 8.Gillani Syed Wasif, Abdul Mohi Iqbal Mohammad. Public health care system, a quasi-experimental study: Acceptance and attitude to implicate clinical services. Acta Pharm. 2017;67:71–83. doi: 10.1515/acph-2017-0008. [DOI] [PubMed] [Google Scholar]
- 9.Grey M., Jaser S.S., Whittenore R., Jeon S., Lindemann E. Coping skills training for parents of children with type 1 diabetes: 12-month outcomes. Nursing Research. 2011;60(3):173–181. doi: 10.1097/NNR.0b013e3182159c8f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillani Syed Wasif, Abdul Mohi Iqbal Mohammad, Ansari Irfan A, Zaghlou Hisham A., SS Syed Azhar, Baig Mirza. Predicting relationship of Eating Behavior, Physical Activity & Smoking with Type II Diabetes and related Comorbidities among Saudi Citizens; Cross-sectional Observational Study. Journal of diabetes in Developing countries (JDDC) 2018 [Google Scholar]
- 11.Gillani Syed Wasif, Sulaiman Syed Azhar Syed, Abdul Mohi Iqbal Mohammad, Saad Sherif Y. A qualitative study to explore the perception and behavior of patients towards diabetes management with physical disability. Diabetol Metab Syndr. 2017;9:58. doi: 10.1186/s13098-017-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zabaleta A., Forbes A., While A., Mold F., Armayor N.C. Relationship between diabetes knowledge, glycemic control and quality of life: pilot study. Prim Care Diabetes. 2010;12:374–381. [Google Scholar]
- 13.Lee W.J., Song K.H., Noh J.H., Choi Y.J., Jo M.W. Health-related quality of life using the EuroQOL 5D questionnaire in Korean patients with type 2 diabetes. J Korean Med Sci. 2012;27:255–260. doi: 10.3346/jkms.2012.27.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Maskari F., El-Sadig M., Al-Kaabi J.M., Afandi B., Nagelkerke N., Yeatts K.B. Knowledge, attitude and practices of diabetic patients in the united Arab Emirates. PLoS ONE. 2013;8:e52857. doi: 10.1371/journal.pone.0052857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gillani Syed Wasif, Ansari Irfan A, Zaghloul Hisham A., MA Mohi Iqbal, SS Syed Azhar, Baig Mirza. Women with Type 1 Diabetes Mellitus; Effect of Disease and Psychosocial-related Correlates on Health related Quality of Life. Journal of Diabetes Research. 2018 doi: 10.1155/2018/4079087. Article ID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniel W.W. John Wiley & Sons; New York: 2010. Biostatistics: basic concepts and methodology for the health sciences. [Google Scholar]
- 17.Tee E.-S., Yap R.W.K. Type 2 diabetes mellitus in Malaysia: current trends and risk factors. European Journal of Clinical Nutrition. 2017;71:844–849. doi: 10.1038/ejcn.2017.44. [DOI] [PubMed] [Google Scholar]
- 18.Indicators and methods for cross-sectional surveys of vitamin and mineral status of populations. The Micronutrient Initiative (Ottawa) and the Centers for Disease Control and Prevention (Atlanta) [http://www.who.int/vmnis/toolkit/mcn-micronutrient-surveys.pdf] Accessed 8 January 2017.
- 19.Fitzgerald J.T., Funnell M.M., Anderson R.M., Nwankwo R., Stansfield R.B., Piatt G.A. Validation of the Revised Brief Diabetes Knowledge Test (DKT2) The Diabetes Educator. 2016;42(2):178–187. doi: 10.1177/0145721715624968. [DOI] [PubMed] [Google Scholar]
- 20.Al-Qazaz H., Hassali M., Shafie A., Sulaiman S., Sundram S. The 14-item Michigan Diabetes Knowledge Test: translation and validation study of the Malaysian version. Pract Diab Int. 2010;27:238–241a. doi: 10.1016/j.diabres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad Nur Sufiza, Ramli Azuana, Islahudin Farida, Paraidathathu Thomas. Medication adherence in patients with type 2 diabetes mellitus treated at primary health clinics in Malaysia. Patient Prefer Adherence. 2013;7:525–530. doi: 10.2147/PPA.S44698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.EuroQOL Euro-QOL – a new facility for the measurement of health-related quality of life. Health Policy. 1990;13(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 23.O Solli, Stavem K., Kristiansen I.S. Health-related quality of life in diabetes: the associations of complications with EQ-5D scores. Health and Quality of Life Outcomes. 2010;8:E18. doi: 10.1186/1477-7525-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Porojan M., Poanta L., Dumitrascu D. Assessing health related quality of life in diabetic patients. Romanin J Int Med. 2012;50:27–31. [PubMed] [Google Scholar]
- 25.Eljedi A., Mikolajczyk R.T., Kraemer A., Laaser U. Health-related quality of life in diabetic patients and controls without diabetes in refugee camps in the Gaza strip: a cross-sectional study. BMC Public Health. 2006;6:268. doi: 10.1186/1471-2458-6-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ken Redekop W., Koopmanschap Marc A., Stolk Ronald P., Rutten Guy E.H.M., Wolffenbuttel Bruce H.R., Niessen Louis W. Health-Related Quality of Life and Treatment Satisfaction in Dutch Patients With Type 2 Diabetes. Diabetes Care. Mar 2002;25(3):458–463. doi: 10.2337/diacare.25.3.458. [DOI] [PubMed] [Google Scholar]
- 27.Davidson Jaime A., Einhorn Daniel, Allweiss Pamela, Flood Thomas M., FACE, Garber Alan J., MD, Garcia Mariano J., Kahn Charles B., Soler Norman G., White John R., Jr, Huster William J. Effect of Premixed Nph and Regular Insulin On Glucose Control and Health-Related Quality of Life in Patients with Type 2 Diabetes Mellitus. Endocrine Practice. 1997;3(6):331–336. doi: 10.4158/EP.3.6.331. [DOI] [PubMed] [Google Scholar]
- 28.Sepúlveda E., Poínhos R., Constante M., Pais-Ribeiro J., Freitas P., Carvalho D. Health-related quality of life in type 1 and type 2 diabetic patients in a Portuguese central public hospital. Diab Metab Syndr Obes: Targets Therapy. 2015;8:219–226. doi: 10.2147/DMSO.S80472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larkin M.E., Walders-Abramson N., Hirst K. Effects of comorbid conditions on health-related quality of life in youth with Type 2 diabetes: the TODAY clinical trial. Diabetes management (London, England) 2015;5(6):431–439. doi: 10.2217/dmt.15.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gillani Syed Wasif, Ansari Irfan A, Zaghloul Hisham A., MA Mohi Iqbal, SS Syed Azhar, Baig Mirza. Bridging Glycated Hemoglobin With Quality of Life & Health State; A Randomized Case-Control Study Among Type 2 Diabetes. BMC Diabetology & Metabolic syndrome. 2018;10(23):1–10. doi: 10.1186/s13098-018-0325-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pichon-Riviere A., Irazola V., Beratarrechea A., Alcaraz A., Carrara C. Quality of life in type 2 diabetes mellitus patients requiring insulin treatment in Buenos Aires, Argentina: a cross-sectional study. International Journal of Health Policy and Management. 2015;4(7):475–480. doi: 10.15171/ijhpm.2015.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parsonage W., Hetmanski D., Cowley A. Beneficial haemodynamic effects of insulin in chronic heart failure. Heart. 2001;85(5):508–513. doi: 10.1136/heart.85.5.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Faria H.T.G., Veras V.S., Xavier A.T., Teixeira C.R., Zanetti M.L., Santos M.A. Quality of life in patients with diabetes mellitus before and after their participation in an educational program. Rev Esc Enferm USP. 2013;47:348–354. doi: 10.1590/s0080-62342013000200011. [DOI] [PubMed] [Google Scholar]
- 34.Saleh F., Mumu S.J., Ara F., Hafez M.A., Ali L. Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: a cross-sectional study. BMC Public Health. 2014;14:31. doi: 10.1186/1471-2458-14-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perwitasari D., Urbayatun S. Treatment adherence and quality of life in diabetes mellitus patients in Indonesia. SAGE Open. 2016;6:1–7. [Google Scholar]
- 36.Chaveepojnkamjorn W., Pichainarong N., Schelp F.-P., Mahaweerawat U. Quality of life and compliance among type 2 diabetic patients. South East Asian J Trop Med Public Health. 2008;39:328–334. [PubMed] [Google Scholar]
- 37.Honish A., Westerfield W., Ashby A., Momin S., Phillippi R. Health-related quality of life and treatment compliance with diabetes care. Dis Manag. 2006;9:195–200. doi: 10.1089/dis.2006.9.195. [DOI] [PubMed] [Google Scholar]
- 38.Wändell P. Quality of life of patients with diabetes mellitus. An overview of research in primary health care in the Nordic countries. Scand J Prim Health Care. 2005;23:68–74. doi: 10.1080/02813430510015296. [DOI] [PubMed] [Google Scholar]
- 39.Jimmy B., Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26:155–159. doi: 10.5001/omj.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]