Abstract
Silicone oil tamponade is a frequent treatment for retinal detachment. Intraventricular migration of this agent is rare, but was described previously in patients with chronic glaucoma and atrophy of the optic disc. We describe a patient with prior silicone oil tamponade in the left eye with a noncontrast computed tomography demonstrating hyperattenuating material along the course of the left optic nerve and in the frontal horns of the lateral ventricles, and emphasize the use of prone noncontrast computed tomography as an important diagnostic tool in order to confirm the low specific gravity of the oil agent.
Keywords: Prone CT, Silicone oil tamponade, Silicone oil intraventricular migration
Abbreviations: NCCT, non-contrast computed tomography; MRI, magnetic resonance imaging; T1WI, T1 weighted images; T2WI, T2 weighted images; CSF, cerebrospinal fluid
Introduction
Silicone oil tamponade is a frequent treatment for retinal detachment. Intraventricular migration of this agent is uncommon [1], [2], but has been described in patients with chronic glaucoma and atrophy of the optic disc [2], [3], [4]. Due to its hyperattenuating appearance on non-contrast computed tomography (NCCT) intraventricular silicone oil has been misdiagnosed previously as intracranial hemorrhage [5], [6], with potential for further invasive investigation. We describe a case of silicone oil intraventricular migration in a patient previously treated for retinal detachment with silicone oil tamponade and emphasize the use of prone NCCT as an important diagnostic tool in order to confirm the low specific gravity of the oil agent.
Case report
A 54-year-old man with a history of chronic liver disease Child-Pugh B was admitted due to disorientation and drowsiness. Neurological examination demonstrated no focal deficit except for left eye blindness. He had been treated with vitrectomy and silicone oil tamponade for retinal detachment on the left. A diagnosis of hepatic encephalopathy was clinically suspected, but a NCCT was performed to rule out other causes.
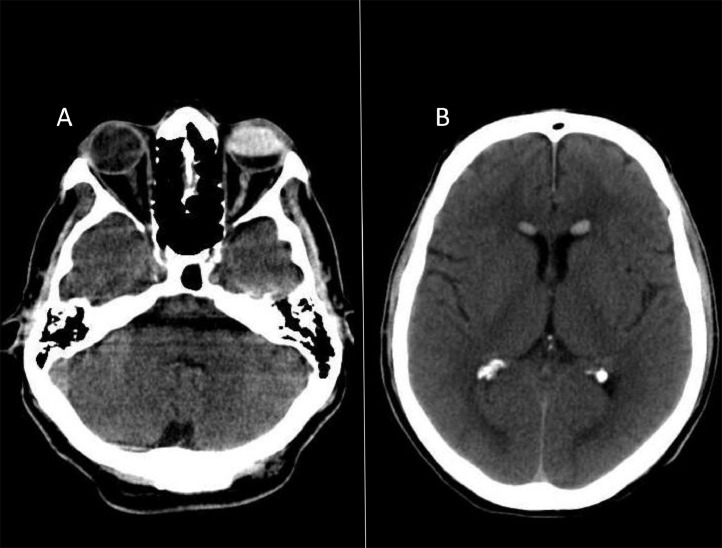
The NCCT demonstrated hyperattenuating material in the left eye vitreous space, along the course of the ipsilateral optic nerve, and in the frontal horns of the lateral ventricles (Fig. 1).
Fig. 1.
Head NCCT demonstrates hyperattenuating materials in the anterior portion of the left globe, along the course of ipsilateral optic nerve (A) and in the frontal horns of the lateral ventricles (B).
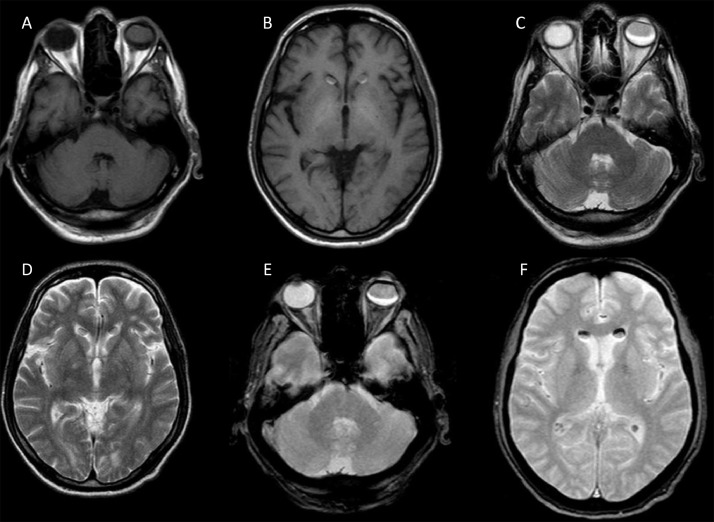
On magnetic resonance imaging (MRI), the material within the left eye and lateral ventricles demonstrated identical signal characteristics, with hyperintensity on T1 weighted images and hypointensity on T2 weighted images. Both T1 weighted images and T2 weighted images depicted crescent-shaped bands in the material-aqueous interface representing a chemical shift artifact, which was more evident on gradient-recalled echo sequence (Fig. 2). No diffusion restriction or contrast enhancement was demonstrated.
Fig. 2.
Brain MRI demonstrates identical signal of the substance in the left eye vitreous space and anterior horns of lateral ventricles, with hyperintensity on T1WI (A, B) and hypointensity on T2WI (C, D). Both T1WI and T2WI depicted crescent-shaped bands in the silicone oil-aqueous interface representing a chemical shift artifact, more evident on gradient-recalled echo sequence (E, F).
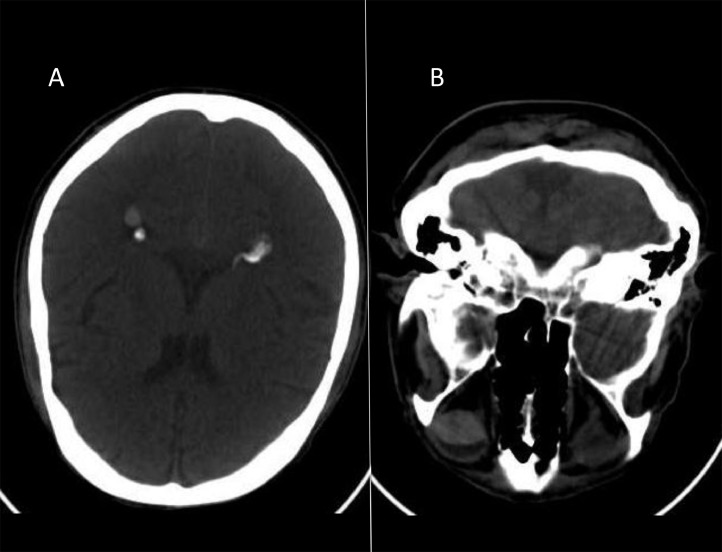
On prone NCCT, the hyperattenuating substance that was previously located in the frontal horns of the lateral ventricles migrated to the occipital horns, and also the hyperattenuating material in the left globe, which was located anteriorly in the vitreous space, moved posteriorly (Fig. 3). This confirmed the lower specific gravity of the hyperattenuating substance in comparison to the cerebrospinal fluid and vitreous humor, consistent with silicone oil.
Fig. 3.
Prone head NCCT shows the hyperattenuating substance located in the occipital horns of the lateral ventricles (A) and in the posterior aspect of the left eye vitreous space (B), demonstrating the material moved from a gravity nondependent location to another gravity nondependent location, which confirms the relative lower specific gravity of the hyperattenuating substance, consistent with silicone oil.
The patient was treated for hepatic encephalopathy and returned to his baseline in 2 days.
Discussion
Silicone oil is a popular agent to treat retinal detachment. Intraventricular migration is rare [1], [2], but has been reported in the medical literature [2], [3], [4], [5], [6], [7], [8]. The mechanism is not entirely clear, but some authors have suggested that atrophy of the optic disc associated with elevated intraocular pressure could lead to migration of the silicone oil along the optic nerve sheath that communicates with the subarachnoid space [3], [4]. In a pathologic study of 74 enucleated eyes after silicone oil tamponade, Budde et al. demonstrated 14 nerves with coalescent vacuoles regarded as silicone vacuoles [9]. This study raised the possibility of silicone oil migration through the nervous tissue of the optic nerve itself and not only along the cerebrospinal fluid space of the optic nerve sheath as hypothesized previously. The vacuolization of the optic nerve parenchyma in the context of chronic glaucoma is termed pseudocavernous optic atrophy [9]. The vast majority of case reports detailing intraventricular migration of silicone oil were incidental and without neurological complication [2]. However, there is 1 case report in the literature in which the patient presented with headache and third ventricular involvement, with increased intracranial pressure necessitating ventriculoperitoneal shunt catheter placement, which subsequently improved that patient's symptoms [8]. This suggests that neurological complications may rarely occur.
Our MRI findings are in accordance to the ones described previously [3], [4], [5], [6], [7]. However, MRI findings are variable depending on sequences parameters, field strength, and the different densities of silicone oil that are available for retinal tamponade [7]. Specific MRI sequences and MR spectroscopy for silicone oil have been described [6], and might show high specificity if investigated further.
Silicone oil has been described as hyperattenuating on NCCT with Hounsfield units from 50 s to 130 s [6], which encompasses the range of blood. Jabbour et al. and Potts et al. described each one a case of intraventricular migration of silicone oil, which initially had a NCCT misdiagnosed as intraventricular hemorrhage [5], [6]. This illustrates that it may lead to confusion, with potential for unnecessary invasive examinations, if this rare condition is not considered.
Nondependent intraventricular CT hyperattenuation likely will not be misdiagnosed as hemorrhagic, particularly if one notes the orbital findings and patient history. Prone CT is able to confirm the low specific gravity of the oil agent. Due to its relative low cost and less complexity in comparison to MRI and magnetic resonance spectroscopy (MRS) techniques the combination of supine and prone NCCT should be the first option in order to confirm the presence of silicone oil in the ventricular system.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Kiilgaard J.F., Milea D., Løgager V., la Cour M. Cerebral migration of intraocular silicone oil: an MRI study. Acta Ophthalmol. 2011;89:522–525. doi: 10.1111/j.1755-3768.2009.01793.x. [DOI] [PubMed] [Google Scholar]; Kiilgaard J.F., Milea D., Logager V., et al. Cerebral migration of intraocular silicone oil: an MRI study. Acta Ophthalmol2011;89:522-525 [DOI] [PubMed]
- 2.Grzybowski A., Pieczynski J., Ascaso F.J. Neuronal complications of intravitreal silicone oil: an updated review. Acta Ophthalmol. 2014;92(3):201–204. doi: 10.1111/aos.12212. [DOI] [PubMed] [Google Scholar]; Grzybowski A., Pieczynski J., Ascaso F.J.Neuronal complications of intravitreal silicone oil: an updated review. Acta Ophthalmol2014;92(3):201-204 [DOI] [PubMed]
- 3.Williams R.L., Beatty R.L., Kanal E., Weissman J.L. MR imaging of intraventricular silicone: case report. Radiology. 1999;212:151–154. doi: 10.1148/radiology.212.1.r99jl27151. [DOI] [PubMed] [Google Scholar]; Williams R.L., Beatty R.L., Kanal E., et al. MR imaging of intraventricular silicone: case report. Radiology1999;212:151-154 [DOI] [PubMed]
- 4.Eller A.W., Friberg T.R., Mah F. Migration of silicone oil into the brain: a complication of intraocular silicone oil for retinal tamponade. Am J Ophthalmol. 2000;129:685–688. doi: 10.1016/s0002-9394(00)00368-8. [DOI] [PubMed] [Google Scholar]; Eller A.W., Friberg T.R., Mah F.Migration of silicone oil into the brain: a complication of intraocular silicone oil for retinal tamponade. Am J Ophthalmol2000;129:685-688 [DOI] [PubMed]
- 5.Jabbour P., Hanna A., Rosenwasser R. Migration of silicone oil in the cerebral intraventricular system. Neurologist. 2011;17:109–110. doi: 10.1097/NRL.0b013e31820a9dc3. [DOI] [PubMed] [Google Scholar]; Jabbour P., Hanna A., Rosenwasser R.Migration of silicone oil in the cerebral intraventricular system. Neurologist2011;17:109-110 [DOI] [PubMed]
- 6.Potts M.B., Wu A.C., Rusinak D.J., Kesavabhotla K., Jahromi B.S. Seeing floaters – a case report and literature review of intraventricular migration of silicone oil tamponade material for retinal detachment. World Neurosurg. 2018;115(July):201–205. doi: 10.1016/j.wneu.2018.04.049. [DOI] [PubMed] [Google Scholar]; Potts M.B., Wu A.C., Rusinak D.J., Kesavabhotla K., Jahromi B.S.Seeing floaters – a case report and literature review of intraventricular migration of silicone oil tamponade material for retinal detachment. World Neurosurg. 2018, (July);115:201-205 [DOI] [PubMed]
- 7.Tatewaki Y., Kurihara N., Sato A., Suzuki I., Ezura M., Takahashi S. Silicone oil migrating from intraocular tamponade into the ventricles: case report with magnetic resonance image findings. J Comput Assist Tomogr. 2011;35:43–45. doi: 10.1097/RCT.0b013e3181fc938d. [DOI] [PubMed] [Google Scholar]; Tatewaki Y., Kurihara N., Sato A., et al. Silicone oil migrating from intraocular tamponade into the ventricles: case report with magnetic resonance image findings. J Comput Assist Tomogr2011;35:43-45 [DOI] [PubMed]
- 8.Hruby P.M., Poley P.R., Terp P.A., Thorell W.E., Margalit E. Headaches secondary to intraventricular silicone oil successfully managed with ventriculoperitoneal shunt. Retin Cases Brief Rep. 2013;7(3):288–290. doi: 10.1097/ICB.0b013e31828eeffe. [DOI] [PubMed] [Google Scholar]; Hruby P.M., Poley P.R., Terp P.A., Thorell W.E., Margalit E.Headaches secondary to intraventricular silicone oil successfully managed with ventriculoperitoneal shunt. Retin Cases Brief Rep. 2013;7(3):288-90 [DOI] [PubMed]
- 9.Budde M., Cursiefen C., Holbach L.M., Naumann G.O. Silicone oil-associated optic nerve degeneration. Am J Ophthalmol. 2001;131:392–394. doi: 10.1016/s0002-9394(00)00800-x. [DOI] [PubMed] [Google Scholar]; Budde M., Cursiefen C., Holbach L.M., et al. Silicone oil-associated optic nerve degeneration. Am J Ophthalmol2001;131:392-394 [DOI] [PubMed]