Abstract
Enhanced recovery pathways are a novel approach focused on enhancing the care of surgical patients. “Prehabilitation” is the term applied to any intervention administered before surgery to reduce surgery-related morbidity, decrease the length of hospital stay, expedite the return of organ function, and facilitate the patient's return to normal life. A PubMed search was performed with the following key words: enhanced recovery, preoperative preparation, cessation of smoking and euvolemia. The results from this Pubmed search revealed that female patients may have higher levels of anxiety than male patients. Intensive smoking and alcohol cessation 6–8 weeks before elective surgery may reduce the incidence of postoperative morbidity. Preoperative exercise can be effective for reducing the postoperative complications like pulmonary complications and shortening the length of hospital stay. It is safe to allow patients to drink clear fluids up until 2 h before elective surgery (Level II evidence). Perioperative normoglycemia is the single most important factor to prevent surgical site infection. Intermittent pneumatic compression devices and low molecular weight heparin are effective in preventing postoperative thromboembolism. No advantage is gained by preoperative mechanical bowel preparation in elective colorectal surgery. The goal of preoperative fluid management is for the patient to arrive in the operating room in a hydrated and euvolemic state. Mild perioperative hypothermia may promote surgical wound infection by triggering thermoregulatory vasoconstriction, which decreases subcutaneous oxygen tension.
Keywords: Cessation of smoking, enhanced recovery, euvolemia, preoperative preparation
Introduction
Enhanced recovery after surgery (ERAS ®) is a novel approach to the care of the surgical patient. ERAS implementation involves a team consisting of surgeons, anesthesiologists, an ERAS coordinator, and staff in the preoperative evaluation clinic, preanesthesia-holding area nurse, operating room nurse, as well as staff in the surgical ward and/or the intensive care unit (ICU).[1] “Fast-track” programs evolved into ERAS pathways, which implement a series of perioperative interventions to expedite recovery after major operations. Patient outcomes are influenced by the type and extensiveness of surgical insults, patient susceptibility to perioperative stress, and quality of perioperative care.[2] The patients' inability to perform a preoperative cardiopulmonary exercise test or demonstrate an anaerobic threshold is associated with increased complications or death after surgery.[3] ERAS programs previously termed “fast-track surgery” are now part of standard care pathways to improve postoperative outcomes in most surgical services. “Prehabilitation” is the term applied to any intervention administered before surgery to reduce surgery-related morbidity, decrease the length of hospital stay, expedite the return of organ function, and facilitate the patient's return to normal life. The goal of prehabilitation is to accept responsibility and assume appropriate self-care.[4] Incorporating prehabilitation interventions with ERAS programs may further improve surgical outcomes. Optimal prehabilitation is a multicomponent process including exercise, diet, cessation of smoking, alcohol, and recreational drug consumptions, psychological, and clinical components.[4] Using ERAS protocols has also resulted in cost savings of US$2806-US$5898 per patient who underwent ERAS protocol of colorectal surgery.[5] Types of interventions that can change the surgery patient outcome are illustrated in Table 1.
Table 1.
Types of prehabilitation interventions
| Physical activity | Educational | Nutritional | Psychological | Clinical |
|---|---|---|---|---|
| Strength training | Advice | Diet plans for weight loss | Anxiety reducing intervention | Optimizing medication |
| Aerobics | Guidance | Optimizing nutrition for malnourished | Any cognitive or behavior intervention | Diabetes/blood glucose control |
| Specific exercises to areas being operated on | Self-care strategies | Oral supplementation including micro and macro nutrients | Combined cognitive or behavioral | Treating anemia and interventions to obtain good baseline status |
General Principles of ERAS
-
The aims of ERAS programs are as follows:
- Decrease the stress response to surgery: metabolic, endocrine, and inflammatory response as well as reduce protein catabolism
- Standardize and optimize perioperative medical care
- To decrease hospital stay and expedite return to normal life
- Promote pain control, avoid immobility due to inadequate analgesia, and decrease immobility-related complications
- Improve gastrointestinal function recovery
Enhanced recovery protocol (ERP) vs. conventional care protocol (CCP): A brief comparison between ERP and CCP is illustrated in Table 2
-
Perioperative process re-engineering: The re-engineered perioperative pathway is shown in Figure 1.[6] Re-engineering pathway by Grocott et al. utilizes three interventions
- Collaborative behavioral change offers a route to improving modifiable behavioral characteristics prior to surgery through active programs of alcohol cessation, activity/exercise, smoking cessation, and dietary intervention
- Collaborative decision-making ensures that each patient is confident about choosing available treatment options, including surgery
- Surgery schools allow for management of expectations about the in-hospital surgical journey and improve psychological preparation for surgery
Types of clinical outcomes after surgery are summarized in Table 3.
Table 2.
Comparison between enhanced recovery protocols and conventional care protocol
| Preoperative period | |
|---|---|
| ERAS | Conventional |
| Give patient 100 g oral carbohydrate drink | No carbohydrate drink |
| Minimize starvation (stop solids 6 h and liquids 2 h before procedure) | Overnight starvation (8 h or more) |
| Do not utilize routine mechanical bowel preparation | Routine mechanical bowel preparation |
| Encourage exercise, decreased smoking, and decreased alcohol consumption | Parenteral hydration (overnight bowl preparation) |
| Obtain informed consent | |
| Provide information about the ERAS protocol | |
| Identify comorbidities | |
| Antibiotic administered preoperatively | |
| Intraoperative period | |
| ERAS | Conventional |
| Neuraxial anesthesia plus general anesthesia | Spinal or general anesthesia only |
| Only when necessary: Nasogastric tubes, abdominal drains, and urinary catheters | Routine utilization of nasogastric tubes, abdominal drains, and urinary catheters |
| Goal-directed fluid therapy | Empirical/liberal hydration |
| Optimal oxygen maintenance | |
| minimal tissue handling | |
| Central and arterial lines should be used only if necessary | |
| Avoidance of hypothermia | |
| Postoperative period | |
| ERAS | Conventional |
| Early removal of tubes, drains, and catheters | Removal of tubes contingent on bowel motility |
| Early patient mobilization and enteral nutrition | No enforced patient mobilization and enteral nutrition only given when bowel motility is restored |
| Multimodal PONV prophylaxis | PONV prophylaxis |
| Day 2 removal of epidural catheter | |
| Maintenance of analgesia after epidural removal | |
| Postdischarge period | |
| ERAS | Conventional |
| 30 days follow up should include | |
| 48 h phone call | Minimal follow up, usually limited to day 7 clinic visit or as needed |
| Clinic visit on 7th day | |
| Emergency room visits | |
ERAS=Enhanced recovery after surgery, PONV=Postoperative nausea and vomiting
Figure 1.
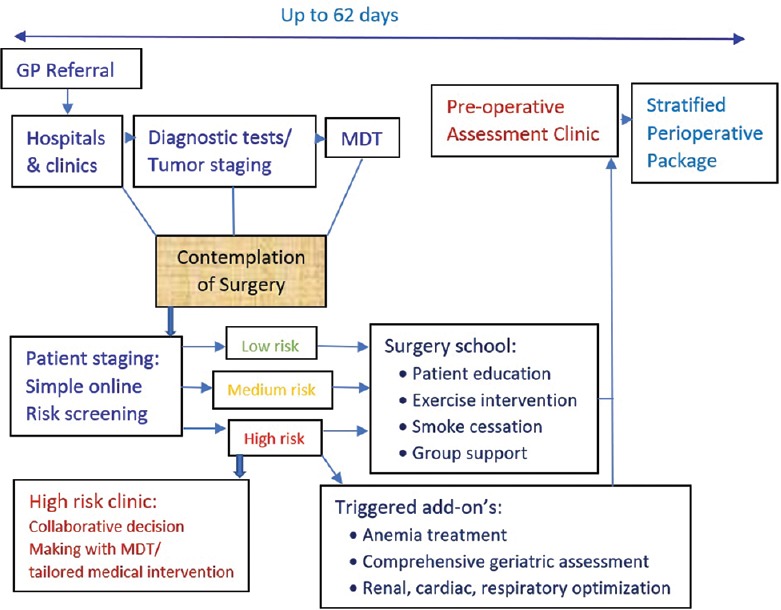
The pathway “re-engineered” – a model of process evolution in perioperative pathways. This re-engineered model is aimed at the timing of pre-assessment to much earlier in the pathway using simple online risk stratification tools, and also early staging by using objective physiological assessments. The purposes are to make sure that patients have detailed information prior to any medical decision and to operate with true collaborative decision-making to take center stage. Surgery school and any “bolt-ons” occur in conjunction with aims to have everything optimized prior to final decisions regarding surgery (Reproduced with permission from Springer Publisher)
Table 3.
Types of clinical outcomes
| Primary outcomes | Secondary outcomes |
|---|---|
| Postoperative infective complications (pneumonia, chest infection, and wound infection) | Length of stay in ICU or HDU |
| Postoperative noninfective complications (anastomotic leakage, wound dehiscence, or thromboembolism) | Perioperative morbidity (acute coronary event, stroke) |
| Length of hospital stay | Postoperative pain |
| All cause perioperative mortality | Hospital readmission |
ICU=Intensive care unit, HDU=High dependency unit
Family Counseling and Education
The purpose of a counseling session is to supplement information provided by the patient's surgeon in a purposeful and tailored manner.[7] Butler et al. found out through their investigation in 1996 that gender is a significant predictor of preoperative anxiety. Female patients demonstrated significantly higher levels of anxiety and had obviously longer hospitalization periods than the male participants.[8] Preoperative information and instructions about surgery and possible complications have been shown to reduce emotional and psychological distress. Tremendous fears exist in patients before surgery: postoperative pain, nausea and vomiting, fear of dying, awareness/awakening during surgery, not waking up from anesthesia, mental decline, and other postoperative complications.
Patients who have received preoperative counseling before admission would have increased knowledge and understanding, thus reduced anxiety levels and more realistic expectations.[9] Different methods of providing preoperative information to patients are illustrated in Table 4. While using videos offers a reflective situation that increases patients' ability to face the real challenge, verbal communications can allow the patients to ask questions and clarify certain patients' concerns. Ghoneim et al. used tape-recorded hypnosis instruction to reduce anxiety in presurgical patients. The audiotape contained a hypnotic and relaxing induction in which patients are guided to mental and physical relaxation.[10]
Table 4.
American Society of Anesthesiologists fasting recommendations
| Ingested material | Minimum fasting period |
|---|---|
| Clear liquid | 2 h |
| Breast milk | 4 h |
| Infant formula | 6 h |
| Nonhuman milk | 6 h |
| Light meal | 6 h |
| Fried food, fatty foods, or meat | 8 or more h |
Commonly used methods for information disclosure include video recordings, preadmission group teaching classes, preadmission booklets and brochures, postadmission individual/group teaching sessions, and individual preoperative visits from theater nurse/anesthesiologist.[9] A “stages of change” model shows how different behavioral theories and constructs can be applied to various stages of the model [Figure 2].
Figure 2.
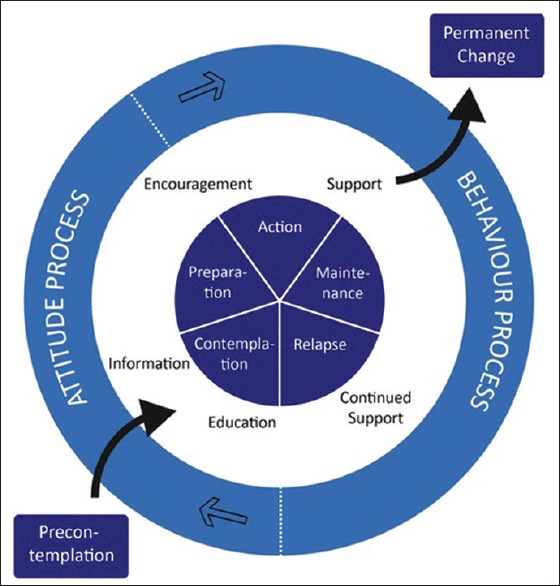
The stages of change model (Reproduced from Lauridsen et al. with permission)
Preoperative Cessation of Smoking, Drinking, and Recreational Drugs
Smoking
Smoking-related complications cost approximately $193 billion every year.[11] Cigarette smokers are at an increased risk of postoperative healing of surgical wounds and bones and severe pulmonary or/and cardiovascular complications.[12,13] Increased duration of preoperative smoking abstinence leads to fewer postoperative pulmonary complications.[14] Zaballos et al. recorded anesthesiologist-delivered interventions to help quit smoking before surgery.[15] Studies showed intensive smoking and alcohol cessation intervention 6–8 weeks before elective surgery could reduce postoperative morbidity by about 50%.[16] Postoperative smoking-cessation in elective surgery and after fractured surgery might likewise reduce complications.[17] Stop smoking before surgery is a collaborative program initiated for preoperative patients in Canada. This program has following goals:[18]
Increase patient's awareness of the benefits of quitting smoking preoperatively
Encourage healthcare professionals to provide brief interventions to support smoke cessation in surgical patients
Increase the number of patients who indeed quit smoking for surgery.
Nicotine replacement therapy increases short-term smoking cessation and may reduce postoperative morbidity. Varenicline, a drug used to treat smoke addiction, administered shortly before surgery has shown some benefits in long-term cessation but no obvious benefit on postoperative complications.[14] A randomized clinical trial involving smoking and alcohol cessation before urinary bladder cancer surgery significantly decreased the postoperative complications.[19] A study in Japan showed that “smoking cessation for at least two weeks before gastric cancer surgery helps reduce postoperative complications such as wound complications, pulmonary complications, and leakage” (Level II evidence).[20]
Alcohol
Alcohol intake increases the risk of postoperative complications after major and minor surgery, both elective and emergency procedures for both men and women. Heavy drinkers were 73% more likely to suffer from postoperative infection, 80% more likely to get difficulty breathing, and 29% more likely to need ICU admission than non-drinkers.[21] The likely pathophysiological mechanisms include a variety of subclinical cardiac dysfunction, an extreme stress-related endocrine response to surgical intervention.[21] A perioperative 6-week gold standard alcohol abstinence program was evaluated in patients with heavy alcohol use to undergoing ankle fracture surgery. Randomized clinical trials have shown that heavy-drinkers with ankle fracture will have a very high complication rate.[22] Clinical studies also showed that interventions reduced infections but not mortality in patients with alcohol abuse. However, the impact on lesser alcohol drinkers is unknown.[23] Alcohol abstinence before surgery results in a significant reduction in alcohol withdrawal, delirium, surgical site infection, and wound dehiscence, likely due to improved immune function and tissue healing.[24] Eliasen et al. showed preoperative alcohol consumption is associated with more complications, as infections, wound dehiscence, bleeding, cardiovascular and pulmonary complications, anastomotic leakage, and neurological complications. Alcohol and smoke cessation 6–8 weeks before elective surgery could reduce postoperative morbidity by about 50%.[16]
Cocaine
Cocaine is an illicit psychostimulant possessing some local anesthetic properties. Cocaine stimulates the sympathetic nervous system by inhibiting catecholamine reuptake transporters at the synaptic junction. Selective β1 adrenergic antagonists (esmolol) with a direct vasodilator (nitroprusside) and opioids may be needed to manage hypertension and tachycardia induced by cocaine.[25] Acute use of cocaine before surgery may predispose patient to significantly higher risk for cardiac complications. Chronic user of cocaine may require more analgesic agents to achieve adequate analgesia. Nontoxic cocaine-abusing patient can be administered general anesthesia with no greater risk than comparable age.[26]
Methamphetamine
Methamphetamine is also a psychostimulant with a duration up to 12 h, versus cocaine's 20 min.[27] Methamphetamine can cause long-term neuronal damage and cell death leading to coma, hypertension, hyperthermia, psychosis, tachyarrhythmia, and myocardial ischemia/infarction.[28] Careful preoperative evaluation by the anesthesiologist is pivotal. Methamphetamine use should be discontinued several days before elective surgery.[29]
Preoperative Exercise
Preoperative exercise can reduce postoperative hospital stay, pulmonary, and other complications in abdominal and cardiovascular surgery.[30] PaO2 was significantly increased in the intervention group during the preoperative period following training. Exercise improves inspiratory muscle endurance, functional mobility, reduces postoperative pain scores and anxiety, and improves quality of life.[31] Matassi et al. indicated that preoperative exercise of the arthritic knee facilitates immediate postoperative recovery following primary total knee replacement.[32] Preoperative exercise therapy might also improve physical fitness of patients prior to major surgery, and preoperative chest physiotherapy seems to be effective in reducing pulmonary complications.[33,34]
Preoperative Fasting
Preoperative fasting was first introduced a few years after the application of general anesthesia in 1848, after a 15-year-old child died potentially due to aspiration.[35] This dogma of overnight fasting has been the routine until 1980s when pediatric anesthesiologists first questioned overnight fasting.[36] Their study showed that it was perfectly safe to allow patients to drink clear fluids up until 2 h before elective surgery. The American Society of Anesthesiologists (ASA) fasting recommendations are illustrated in Table 5.
Table 5.
Natural diurnal pattern of metabolism in humans
| Day | Night | |
|---|---|---|
| Hormones | Insulin positive | Insulin negative |
| Glucagon positive | ||
| Glucocorticoids positive | ||
| Substrates | Storage | Breakdown |
| Utilization | Carbohydrates | Fat |
Bowel Preparation for Gastroenterological Procedures
Routine mechanical bowel preparation (MBP) contributes to preoperative dehydration and is unpleasant for the patients.[37] A systematic review of 18 randomized clinical trials (5805 patients enrolled) found no statistically significant benefit from either bowel preparation or rectal enemas.[38] Bhat et al. reported that MBP in elective colorectal surgery can be easily avoided to save patients from unwanted exhaustion, distress, and adverse effects related to MBP.[39]
Disadvantages of MBP are as follows:[40]
Troublesome, time consuming, and could be expensive
Requirement for admission before surgery in some hospitals
It can result in abdominal pain, bloating, and fatigue
It can cause fluid and electrolyte imbalance
Poor preparation may result in liquid stools, which increases intraoperative spillage
MBP causes histological changes in the colorectal mucosa
Potential bacterial translocation and anastomotic disruption[41]
Certain bowel preparations may produce explosive gases and increase the incidence of wound infection due to overgrowth of Escherichia coli.
The disadvantages of MBP may be ameliorated by some oral antibiotics.[42] Additionally, patients are encouraged to drink clear fluids up to 2 h before the induction of anesthesia.[43]
Preoperative Metabolic Preparation
Optimization of metabolic state prior to major surgery leads to improved surgical outcomes. Most of the perioperative metabolic preparation strategies aim at reducing or blocking the activation of inflammatory reactions by corticosteroids, non-steroidal anti-inflammatory drugs, and minimally invasive surgery.
-
Carbohydrate Loading: The natural diurnal pattern of metabolism in humans is illustrated in Table 4
Since the effects of insulin last for about 4–5 h after food intake, the body remains in a substrate-storing state from the first intake of food in the morning, until it is time to sleep in the evening. Studies showed if a patient is operated under the influence of insulin after giving carbohydrates load preoperatively results in attenuation of glucagon release, complete abolition of cortisol release, thus far less catabolic in postoperative period[44]
Metabolic Syndrome: A cluster of conditions as increased blood pressure, high blood sugar, excess body fat around waist, and abnormal cholesterol or triglyceride level can cause metabolic syndrome which may play a role in cancer growth such as colorectal carcinoma.[45] Preoperative metabolic syndrome, especially hyperglycemia, is a robust predictor for colorectal carcinoma (CRC) mortality[46]
Perioperative Glycemic Control: Perioperative maintenance of normoglycemia is the single most important factor to prevent surgical site infection. This is true regardless of the patient being diagnosed with diabetes or not.[47] An intraoperative infusion of 20% glucose with insulin improves the glycemic control, reducing insulin levels at the induction of anesthesia and minimizing hyperglycemia in surgery. Meta-analysis has shown that this strategy attenuates postoperative insulin resistance[48]
Preoperative Enteral Feeding: The American Society for Parenteral and Enteral Nutrition and the Society of Critical Care Medicine nutrition guidelines state that for those who cannot take adequate calories with oral supplementation alone, enteral nutrition via feeding tube should be considered and is preferred over parenteral nutrition if the gastrointestinal tract is functional. Feeding jejunotomy tube placement is common now in head and neck cancers and esophageal neoplastic diseases
-
Immune-modulating nutrition: Biochemical effects of immune-modulating formulas include increased cell membrane stability, enhanced cell-mediated immune responses, improved gastrointestinal mucosal integrity, attenuation of the inflammatory response to stress, and improved blood flow to poorly vascularized and ischemic tissues.[49] The short-term benefits of immune-nutrition have mainly been demonstrated in patients undergoing gastrointestinal surgery, particularly patients diagnosed with malnutrition or cancer.[50] Immune nutrition should be started 5–7 days preoperatively (500–1000 mL per day) and continued in the postoperative period[51]
Commonly used immune-modulating agents include combination of fish oils, eicosapentanoic acid (EPA), docosahexaenoic acid (DHA), arginine, nucleic acids, and antioxidants[49]
Vitamins and Trace Minerals: Preoperative use of multivitamins is not frequently discussed in the literature. Vitamin A and zinc levels are low in patients following gastrointestinal surgery. Both have known roles in wound healing. Decreased rates of pneumonia in burn patients are associated with administration of copper, selenium, and zinc supplementation.[52]
Prophylaxis of Infection
Surgical site infection is the most common perioperative infection leading to increased hospital stay, higher costs, and increased morbidity and mortality. Infection occurs within 30 days postoperatively or within 1 year if surgical implant is in place. Classification of operation and incidence of surgical infection is illustrated in Table 6.[53]
Table 6.
Classifications of surgery and wound infection rate
| Classification | Description | Incidence of surgical site infection (%) |
|---|---|---|
| Class I clean | Uninfected including incisional surgery wound | <2 |
| Class II clean-contaminated | Elective operation of visceral organ | 5-15 |
| Class III contaminated | Open surgical wound with nonpurulent inflammation | 15-30 |
| Class IV dirty | Surgery involving old wounds with dead tissue or wounds that involve a perforated bowel or a preexisting clinical infection | >30 |
Antibiotic prophylaxis refers to the preoperative introduction of short-term antibiotics in surgical patients. The decision to administer antibiotic prophylaxis should be made by utilization of the the National Nosocomial Infections Surveillance score system which considers three factors: classification in Table 6, ASA Physical status, duration of surgery.[53] Antibiotic prophylaxis should be administered when the the National Nosocomial Infections Surveillance score is ≥1.[54] Routine prophylaxis with intravenous antibiotics should be given 30–60 min before initiating colorectal surgery.[55]
Prophylaxis of Thromboembolic Events
The estimated annual incidence of venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is 1–2/1000/year among the general population.[56] Risk factors for VTE include previous VTE, reduced mobility, already known thrombophilic condition, elderly age >70, heart or respiratory failure, acute infarction or stroke, and obesity.[57]
Mechanical measures
Graduated compression stockings
1. They are believed to work by compressing both superficial and deep venous systems, increasing venous flow, and opening the venous valves.[58]
Intermittent pneumatic compression devices
2. Increased pulsatile venous flow can result from the sequential application of external compression on lower extremities, leading to enhanced vasodilatory, antithrombotic, and profibrinolytic effects including the release of tissue plasminogen activator (tPA).[59]
Pharmacological measures
Heparin
Low-molecular-weight heparins (LMWHs) include dalteparin, tinzaparin, and enoxaparin. Heparin is administered at 5000 units every 8–12 h, subcutaneously. The LMWHs have different structures and pharmacologic properties, therefore not interchangeable with each other or with heparin.[58] Antidotes are indicated in potential life-threatening bleeding or risk of recurrent bleeding. Idarucizumab is a specific reversal agent for dabigatran.[60] Standard perioperative antithrombotic therapy protocols are as below:[61]
Assess patients for perioperative anticoagulant management >7 days before surgery
Provide a calendar to the patinet and healthcare provider that outlines the perioperative timing of warfarin and antiplatelet drug discontinuation and resumption, dose and timing of LMWH bridging, and international normalized ratio (INR) measurement schedule
Ensure patient and caregiver education on injection techniques when administering outpatient LMWH bridging
INR testing on the day before surgery to identify patients with elevated INRs and permit the timely use of corrective vitamin K
Assessing postoperative hemostasis to facilitate the safe resumption of anticoagulant drugs.
Other Preoperative Considerations
Temperature
Mild perioperative hypothermia may promote surgical wound infection by triggering thermoregulatory vasoconstriction, which decreases subcutaneous oxygen tension. Low oxygen tension impairs oxidative killing by neutrophils and decreases the strength of wound healing by reducing the deposition of collagen.[62] Using forced-air warmer devices during surgery can help reduce catabolism, blood loss, and untoward cardiac events.[63] Intravenous fluids should be warmed using a suitable device.[64,65]
Prevention of aspiration
Orally administered histamine 2 receptor antagonist (as ranitidine) is effective in reducing gastric volume and acidity; the frequency of gastric pH levels <2.5; the frequency of gastric volume >25 mL; and the risk of aspiration (i.e., gastric volume >25 mL and pH <2.5) during the perioperative period.[66] ASA preoperative pharmacologic practice guidelines are illustrated in Table 7.[67]
Table 7.
American Society of Anesthesiologists preoperative pharmacologic practice guidelines
| Agents | Preoperative Administration |
|---|---|
| Antacids (cimetidine, famotidine, ranitidine) | Antacids may be preoperatively administered to patients at increased risk of pulmonary aspiration Only administer nonparticulate antacids Do not routinely administer preoperative antacids to reduce the risk of pulmonary aspiration in patients with no apparent increased risk for pulmonary aspiration |
| Antiemetics (ondansetron) | Antiemetics may be preoperatively administered to patients at increased risk of PONV The consultants and ASA members both disagree that preoperative antiemetics should be routinely administered before elective procedures requiring general anesthesia, regional anesthesia, or procedural sedation |
| Anticholinergics (atropine, scopolamine) | The administration of preoperative anticholinergics to reduce the risk of pulmonary aspiration is not recommended |
| GIT stimulants (metoclopramide) | The routine administration of preoperative multiple agents is not recommended for patients with no apparent increased risk for pulmonary aspiration |
| Multiple agents (sodium citrate) | The routine administration of preoperative multiple agents is not recommended for patients with no increased risk for developing pulmonary aspiration |
Adopted from ASA guideline 2017. ASA=American Society of Anesthesiologists, PONV=Postoperative nausea and vomiting, GIT=Gastrointestinal tract
Mental/psychological preparedness
Mental therapy is the form of breathing relaxation, stress management, and education. Patients are provided with information booklets about relaxation and stress. Psychological preparation should include two fundamental aspects, information about the details of experience and the teaching of effective coping strategies.[1]
Fluid management
Preoperative fluid management is an important component of ERAS pathway. The goal of preoperative fluid management is for the patient to be in a hydrated and euvolemic state.[34] Perioperatively, a near-zero fluid balance should be achieved.[50] Patients undergoing surgery within an ERAS protocol are less likely to be fluid responsive after induction of anesthesia.[68] Fluid balance should be optimized by targeting cardiac output or cardiac index.
Prevention of postoperative nausea and vomiting
Female patients, non-smokers, patients with a history of motion sickness, and patients using opioids are at high risk for postoperative nausea and vomiting (PONV). Multimodal antiemetic prophylaxis should be adopted. The second strategy is to decrease PONV risk by avoiding general anesthesia, using propofol infusions, avoiding nitrous oxide and volatile anesthetics, reducing opioid use, and decreasing the neostigmine dose.[69]
Prevention of postoperative ileus
Postoperative ileus is defined as a disruption of the normal peristaltic motion of the gut. Major contributing factors include surgical stress, secretion of inflammatory mediators, inhaled anesthetics, fluids, endogenous opioids in GI tract, and electrolyte balance and use of opioids for postoperative analgesia. The greatest advance in limiting postoperative ileus to date has probably resulted from the expanded use of laparoscopic surgery.[1,70]
Optimization of preoperative hemoglobin level
Over the last few decades, the hemoglobin level triggering blood transfusion has been steadily trending down. There are numerous complications associated with allogenic blood transfusion including the risk of disease transmission, fluid and hemodynamic overload, hemolytic reaction, acute lung injury, coagulopathy, allergic reaction, and febrile non-hemolytic reactions. Generally, surgical patients will not need hemoglobin optimization preoperatively, optimization of hemoglobin concentration was only attempted in <40% of patients in Spain.[71] Some patients, as anemic elderly patients, patient with coronary artery disease and borderline hemoglobin level, and members of the Jehovah's Witness, will benefit from preoperative hemoglobin optimization. Pharmacological optimization of hemoglobin level includes erythropoietin and iron supplement, obviously this optimization process is highly individualized.[71]
Summary
ERAS has been adopted in many medical institutions in the United States. In this review, we discussed the general principles of ERAS, and the multiple aspects related to preoperative preparations pertinent to ERAS. These preoperative preparations include patient and family education and counseling, preoperative cessation of smoking, drinking, and recreational drugs, preoperative exercise, appropriate preoperative fasting, avoidance of routine preoperative MBP and enema, optimization of preoperative metabolism, prophylaxis of infection and thromboembolic events, and maintenance of euvolemia and normothermia. These preoperative preparations are pivotal to the success of any ERAS protocol.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: A Review. JAMA Surg. 2017;152:292–8. doi: 10.1001/jamasurg.2016.4952. [DOI] [PubMed] [Google Scholar]
- 2.Moonesinghe SR, Mythen MG, Grocott MP. Patient-related risk factors for postoperative adverse events. Curr Opin Crit Care. 2009;15:320–7. doi: 10.1097/MCC.0b013e32832e067c. [DOI] [PubMed] [Google Scholar]
- 3.Lai CW, Minto G, Challand CP, Hosie KB, Sneyd JR, Creanor S, et al. Patients' inability to perform a preoperative cardiopulmonary exercise test or demonstrate an anaerobic threshold is associated with inferior outcomes after major colorectal surgery. Br J Anaesth. 2013;111:607–11. doi: 10.1093/bja/aet193. [DOI] [PubMed] [Google Scholar]
- 4.Wright S, Wiechula R, McLiesh P. The effectiveness of prehabilitation for adults having elective surgery: A systematic review protocol. JBI Database System Rev Implement Rep. 2016;14:78–92. doi: 10.11124/jbisrir-2016-2460. [DOI] [PubMed] [Google Scholar]
- 5.Altman AD, Nelson GS. Society of Gynecologic Oncology of Canada Annual General Meeting, Continuing Professional Development, and Communities of Practice Education Committees. The Canadian gynaecologic oncology perioperative management survey: Baseline practice prior to implementation of enhanced recovery after surgery (ERAS) society guidelines. J Obstet Gynaecol Can. 2016;38:1105–900. doi: 10.1016/j.jogc.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Grocott MP, Plumb JO, Edwards M, Fecher-Jones I, Levett DZ. Re-designing the pathway to surgery: Better care and added value. Perioper Med (Lond) 2017;6:9. doi: 10.1186/s13741-017-0065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shenson JA, Craig JN, Rohde SL. Effect of preoperative counseling on hospital length of stay and readmissions after total laryngectomy. Otolaryngol Head Neck Surg. 2017;156:289–98. doi: 10.1177/0194599816671695. [DOI] [PubMed] [Google Scholar]
- 8.Butler GS, Hurley CA, Buchanan KL, Smith-VanHorne J. Prehospital education: Effectiveness with total hip replacement surgery patients. Patient Educ Couns. 1996;29:189–97. doi: 10.1016/0738-3991(96)00883-x. [DOI] [PubMed] [Google Scholar]
- 9.Lepczyk M, Raleigh EH, Rowley C. Timing of preoperative patient teaching. J Adv Nurs. 1990;15:300–6. doi: 10.1111/j.1365-2648.1990.tb01817.x. [DOI] [PubMed] [Google Scholar]
- 10.Ghoneim MM, Block RI, Sarasin DS, Davis CS, Marchman JN. Tape-recorded hypnosis instructions as adjuvant in the care of patients scheduled for third molar surgery. Anesth Analg. 2000;90:64–8. doi: 10.1097/00000539-200001000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Morbidity and Mortality Weekly Report. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥18 Years – United States; 2009-2010. [PubMed] [Google Scholar]
- 12.Theocharidis V, Katsaros I, Sgouromallis E, Serifis N, Boikou V, Tasigiorgos S, et al. Current evidence on the role of smoking in plastic surgery elective procedures: A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2018;71:624–36. doi: 10.1016/j.bjps.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Turan A, Mascha EJ, Roberman D, Turner PL, You J, Kurz A, et al. Smoking and perioperative outcomes. Anesthesiology. 2011;114:837–46. doi: 10.1097/ALN.0b013e318210f560. [DOI] [PubMed] [Google Scholar]
- 14.Theadom A, Cropley M. Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: A systematic review. Tob Control. 2006;15:352–8. doi: 10.1136/tc.2005.015263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaballos M, Canal MI, Martínez R, Membrillo MJ, Gonzalez FJ, Orozco HD, et al. Preoperative smoking cessation counseling activities of anesthesiologists: A cross-sectional study. BMC Anesthesiol. 2015;15:60. doi: 10.1186/s12871-015-0036-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oppedal K, Møller AM, Pedersen B, Tønnesen H. Preoperative alcohol cessation prior to elective surgery. Cochrane Database Syst Rev. 2012 doi: 10.1002/14651858.CD008343.pub2. CD008343. doi: 10.1002/14651858.CD008343. [DOI] [PubMed] [Google Scholar]
- 17.Nåsell H, Adami J, Samnegård E, Tønnesen H, Ponzer S. Effect of smoking cessation intervention on results of acute fracture surgery: A randomized controlled trial. J Bone Joint Surg Am. 2010;92:1335–42. doi: 10.2106/JBJS.I.00627. [DOI] [PubMed] [Google Scholar]
- 18.Bottorff JL, Seaton CL, Viney N, Stolp S, Krueckl S, Holm N, et al. The stop smoking before surgery program: Impact on awareness of smoking-related perioperative complications and smoking behavior in Northern Canadian Communities. J Prim Care Community Health. 2016;7:16–23. doi: 10.1177/2150131915604827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lauridsen SV, Thomsen T, Thind P, Tønnesen H. STOP smoking and alcohol drinking before OPeration for bladder cancer (the STOP-OP study), perioperative smoking and alcohol cessation intervention in relation to radical cystectomy: Study protocol for a randomised controlled trial. Trials. 2017;18:329. doi: 10.1186/s13063-017-2065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung KH, Kim SM, Choi MG, Lee JH, Noh JH, Sohn TS, et al. Preoperative smoking cessation can reduce postoperative complications in gastric cancer surgery. Gastric Cancer. 2015;18:683–90. doi: 10.1007/s10120-014-0415-6. [DOI] [PubMed] [Google Scholar]
- 21. [Last accessed on 2018 Aug 16]. Available from: https://www.reuters.com/article/us-drinkers-surgery-problem-idUSBRE95Q0TF20130627 .
- 22.Tønnesen H, Egholm JW, Oppedal K, Lauritzen JB, Madsen BL, Pedersen B, et al. Patient education for alcohol cessation intervention at the time of acute fracture surgery: Study protocol for a randomised clinical multi-centre trial on a gold standard programme (Scand-ankle) BMC Surg. 2015;15:52. doi: 10.1186/s12893-015-0035-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shabanzadeh DM, Sørensen LT. Alcohol consumption increases post-operative infection but not mortality: A Systematic review and meta-analysis. Surg Infect (Larchmt) 2015;16:657–68. doi: 10.1089/sur.2015.009. [DOI] [PubMed] [Google Scholar]
- 24.Kaka AS, Zhao S, Ozer E, Agrawal A, Kang S, Rocco J, et al. Comparison of clinical outcomes following head and neck surgery among patients who contract to abstain from alcohol vs patients who abuse alcohol. JAMA Otolaryngol Head Neck Surg. 2017;143:1181–6. doi: 10.1001/jamaoto.2017.0553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Voigt L. Anesthetic management of the cocaine abuse patient. AANA J. 1995;63:438–43. [PubMed] [Google Scholar]
- 26.Hill GE, Ogunnaike BO, Johnson ER. General anaesthesia for the cocaine abusing patient. Is it safe? Br J Anaesth. 2006;97:654–7. doi: 10.1093/bja/ael221. [DOI] [PubMed] [Google Scholar]
- 27.West PL, McKeown NJ, Hendrickson RG. Methamphetamine body stuffers: An observational case series. Ann Emerg Med. 2010;55:190–7. doi: 10.1016/j.annemergmed.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Booker RJ, Smith JE, Rodger MP. Packers, pushers and stuffers – Managing patients with concealed drugs in UK emergency departments: A clinical and medicolegal review. Emerg Med J. 2009;26:316–20. doi: 10.1136/emj.2008.057695. [DOI] [PubMed] [Google Scholar]
- 29.Bahrami-Motlagh H, Hassanian-Moghaddam H, Behnam B, Arab-Ahmadi M. Failure of surgical treatment in methamphetamine body-stuffers. J Forensic Leg Med. 2015;32:70–2. doi: 10.1016/j.jflm.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 30.Valkenet K, van de Port IG, Dronkers JJ, de Vries WR, Lindeman E, Backx FJ, et al. The effects of preoperative exercise therapy on postoperative outcome: A systematic review. Clin Rehabil. 2011;25:99–111. doi: 10.1177/0269215510380830. [DOI] [PubMed] [Google Scholar]
- 31.Lemanu DP, Singh PP, MacCormick AD, Arroll B, Hill AG. Effect of preoperative exercise on cardiorespiratory function and recovery after surgery: A systematic review. World J Surg. 2013;37:711–20. doi: 10.1007/s00268-012-1886-4. [DOI] [PubMed] [Google Scholar]
- 32.Matassi F, Duerinckx J, Vandenneucker H, Bellemans J. Range of motion after total knee arthroplasty: The effect of a preoperative home exercise program. Knee Surg Sports Traumatol Arthrosc. 2014;22:703–9. doi: 10.1007/s00167-012-2349-z. [DOI] [PubMed] [Google Scholar]
- 33.Pouwels S, Stokmans RA, Willigendael EM, Nienhuijs SW, Rosman C, van Ramshorst B, et al. Preoperative exercise therapy for elective major abdominal surgery: A systematic review. Int J Surg. 2014;12:134–40. doi: 10.1016/j.ijsu.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 34.Miller TE, Roche AM, Mythen M. Fluid management and goal-directed therapy as an adjunct to enhanced recovery after surgery (ERAS) Can J Anaesth. 2015;62:158–68. doi: 10.1007/s12630-014-0266-y. [DOI] [PubMed] [Google Scholar]
- 35.Knight PR, 3rd, Bacon DR. An unexplained death: Hannah greener and chloroform. Anesthesiology. 2002;96:1250–3. doi: 10.1097/00000542-200205000-00030. [DOI] [PubMed] [Google Scholar]
- 36.Maltby JR, Sutherland AD, Sale JP, Shaffer EA. Preoperative oral fluids: Is a five-hour fast justified prior to elective surgery? Anesth Analg. 1986;65:1112–6. [PubMed] [Google Scholar]
- 37.Jung B, Påhlman L, Nyström PO, Nilsson E Mechanical Bowel Preparation Study Group. Multicentre randomized clinical trial of mechanical bowel preparation in elective colonic resection. Br J Surg. 2007;94:689–95. doi: 10.1002/bjs.5816. [DOI] [PubMed] [Google Scholar]
- 38.Güenaga KF, Matos D, Wille-Jørgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD001544.pub4. doi:10.1002/14651858.CD001544.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389:2105–16. doi: 10.1016/S0140-6736(17)30638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saha AK, Chowdhury F, Jha AK, Chatterjee S, Das A, Banu P. Mechanical bowel preparation versus no preparation before colorectal surgery: A randomized prospective trial in a tertiary care institute. J Nat Sci Biol Med. 2014;5:421–4. doi: 10.4103/0976-9668.136214. doi: 10.4103/0976-9668.136214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ballantyne GH. The experimental basis of intestinal suturing. Effect of surgical technique, inflammation, and infection on enteric wound healing. Dis Colon Rectum. 1984;27:61–71. doi: 10.1007/BF02554084. [DOI] [PubMed] [Google Scholar]
- 42.Gupta R, Gan TJ. Peri-operative fluid management to enhance recovery. Anaesthesia. 2016;71(Suppl 1):40–5. doi: 10.1111/anae.13309. [DOI] [PubMed] [Google Scholar]
- 43.Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, et al. Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American society of colon and rectal surgeons and society of American gastrointestinal and endoscopic surgeons. Dis Colon Rectum. 2017;60:761–84. doi: 10.1097/DCR.0000000000000883. [DOI] [PubMed] [Google Scholar]
- 44.Ljungqvist O. To fast or not to fast before surgical stress. Nutrition. 2005;21:885–6. doi: 10.1016/j.nut.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Micucci C, Valli D, Matacchione G, Catalano A. Current perspectives between metabolic syndrome and cancer. Oncotarget. 2016;7:38959–72. doi: 10.18632/oncotarget.8341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peng F, Hu D, Lin X, Chen G, Liang B, Zhang H, et al. Preoperative metabolic syndrome and prognosis after radical resection for colorectal cancer: The Fujian prospective investigation of cancer (FIESTA) study. Int J Cancer. 2016;139:2705–13. doi: 10.1002/ijc.30404. [DOI] [PubMed] [Google Scholar]
- 47.Ata A, Lee J, Bestle SL, Desemone J, Stain SC. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg. 2010;145:858–64. doi: 10.1001/archsurg.2010.179. [DOI] [PubMed] [Google Scholar]
- 48.Li L, Wang Z, Ying X, Tian J, Sun T, Yi K, et al. Preoperative carbohydrate loading for elective surgery: A systematic review and meta-analysis. Surg Today. 2012;42:613–24. doi: 10.1007/s00595-012-0188-7. [DOI] [PubMed] [Google Scholar]
- 49.Evans DC, Martindale RG, Kiraly LN, Jones CM. Nutrition optimization prior to surgery. Nutr Clin Pract. 2014;29:10–21. doi: 10.1177/0884533613517006. [DOI] [PubMed] [Google Scholar]
- 50.Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced recovery after surgery (ERAS®) society recommendations. World J Surg. 2013;37:240–58. doi: 10.1007/s00268-012-1771-1. [DOI] [PubMed] [Google Scholar]
- 51.Ali Abdelhamid Y, Chapman MJ, Deane AM. Peri-operative nutrition. Anaesthesia. 2016;71(Suppl 1):9–18. doi: 10.1111/anae.13310. [DOI] [PubMed] [Google Scholar]
- 52.Berger MM, Eggimann P, Heyland DK, Chioléro RL, Revelly JP, Day A, et al. Reduction of nosocomial pneumonia after major burns by trace element supplementation: Aggregation of two randomised trials. Crit Care. 2006;10:R153. doi: 10.1186/cc5084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Setiawan B. The role of prophylactic antibiotics in preventing perioperative infection. Acta Med Indones. 2011;43:262–6. [PubMed] [Google Scholar]
- 54.Parsons DP. Preoperative evaluation and risk management. Clin Colon Rectal Surg. 2009;22:5–13. doi: 10.1055/s-0029-1202870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced recovery after surgery (ERAS(®)) society recommendations. World J Surg. 2013;37:259–84. doi: 10.1007/s00268-012-1772-0. [DOI] [PubMed] [Google Scholar]
- 56.Goldhaber SZ. Venous thromboembolism: Epidemiology and magnitude of the problem. Best Pract Res Clin Haematol. 2012;25:235–42. doi: 10.1016/j.beha.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 57.Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141:e195S–226S. doi: 10.1378/chest.11-2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Laryea J, Champagne B. Venous thromboembolism prophylaxis. Clin Colon Rectal Surg. 2013;26:153–9. doi: 10.1055/s-0033-1351130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen AH, Frangos SG, Kilaru S, Sumpio BE. Intermittent pneumatic compression devices – Physiological mechanisms of action. Eur J Vasc Endovasc Surg. 2001;21:383–92. doi: 10.1053/ejvs.2001.1348. [DOI] [PubMed] [Google Scholar]
- 60.Lai A, Davidson N, Galloway SW, Thachil J. Perioperative management of patients on new oral anticoagulants. Br J Surg. 2014;101:742–9. doi: 10.1002/bjs.9485. [DOI] [PubMed] [Google Scholar]
- 61.Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141:e326S–50S. doi: 10.1378/chest.11-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of wound infection and temperature group. N Engl J Med. 1996;334:1209–15. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- 63.Nelson G, Altman AD, Nick A, Meyer LA, Ramirez PT, Achtari C, et al. Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced recovery after surgery (ERAS®) society recommendations – Part II. Gynecol Oncol. 2016;140:323–32. doi: 10.1016/j.ygyno.2015.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ma H, Lai B, Dong S, Li X, Cui Y, Sun Q, et al. Warming infusion improves perioperative outcomes of elderly patients who underwent bilateral hip replacement. Medicine (Baltimore) 2017;96:e6490. doi: 10.1097/MD.0000000000006490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Horosz B, Nawrocka K, Malec-Milewska M. Anaesthetic perioperative management according to the ERAS protocol. Anaesthesiol Intensive Ther. 2016;48:49–54. doi: 10.5603/AIT.2016.0006. [DOI] [PubMed] [Google Scholar]
- 66.Manchikanti L, Colliver JA, Marrero TC, Roush JR. Ranitidine and metoclopramide for prophylaxis of aspiration pneumonitis in elective surgery. Anesth Analg. 1984;63:903–10. [PubMed] [Google Scholar]
- 67.Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures: An updated report by the American society of anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–93. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 68.Srinivasa S, Taylor MH, Singh PP, Yu TC, Soop M, Hill AG, et al. Randomized clinical trial of goal-directed fluid therapy within an enhanced recovery protocol for elective colectomy. Br J Surg. 2013;100:66–74. doi: 10.1002/bjs.8940. [DOI] [PubMed] [Google Scholar]
- 69.Perry R, Scott LJ, Richards A, Haase AM, Savović J, Ness AR, et al. Pre-admission interventions to improve outcome after elective surgery-protocol for a systematic review. Syst Rev. 2016;5:88. doi: 10.1186/s13643-016-0266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures: An updated report by the American society of anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–93. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 71.Bisbe E, Basora M, Colomina MJ Spanish Best Practice in Peri-operative Anaemia Optimisation Panel. Peri-operative treatment of anaemia in major orthopaedic surgery: A practical approach from spain. Blood Transfus. 2017;15:296–306. doi: 10.2450/2017.0177-16. [DOI] [PMC free article] [PubMed] [Google Scholar]


