Cardiopulmonary interactions in chronic obstructive pulmonary disease (COPD) involve many pathophysiologic mechanisms and are thus a complex field of research (1, 2). An increasingly studied mechanism over the last decade is the effect of lung hyperinflation on cardiac filling and the associated consequences for exercise tolerance and physical activity (3–6).
Because all available long-acting bronchodilators used for maintenance therapy in chronic obstructive pulmonary disease (COPD) are effective lung deflators, it would be logical to also look for the positive effects of lung deflation on cardiac filling. However, hurdles related to technology and uncertainties about the appropriate endpoints have prevented a timely development of protocols. Such protocols would be much more complex than simply measuring lung volumes by body plethysmography. It was only 3 years ago that Stone and colleagues, in a landmark study, showed that lung deflation by monobronchodilator therapy plus an inhaled corticosteroid improves biventricular filling and cardiac output in patients with COPD and hyperinflation (7). Last year, Hohlfeld and colleagues confirmed these findings by using dual bronchodilation in patients with COPD whose lungs were slightly more hyperinflated than those examined in the study by Stone and colleagues (8). Through careful patient selection based on hyperinflation, and a more effective lung deflation therapy by dual bronchodilation, Hohlfeld and colleagues showed even more pronounced effects on cardiac filling and cardiac output (8). These impressive improvements in the study of cardiac filling, which might indirectly imply an improved pulmonary blood volume circulation, allowed the authors to also study the effects of lung deflation on pulmonary perfusion. In a follow-up study presented in this issue of the Journal, Vogel-Claussen and colleagues (pp. 1086–1096) used functional lung magnetic resonance imaging to measure regional pulmonary ventilation (9).
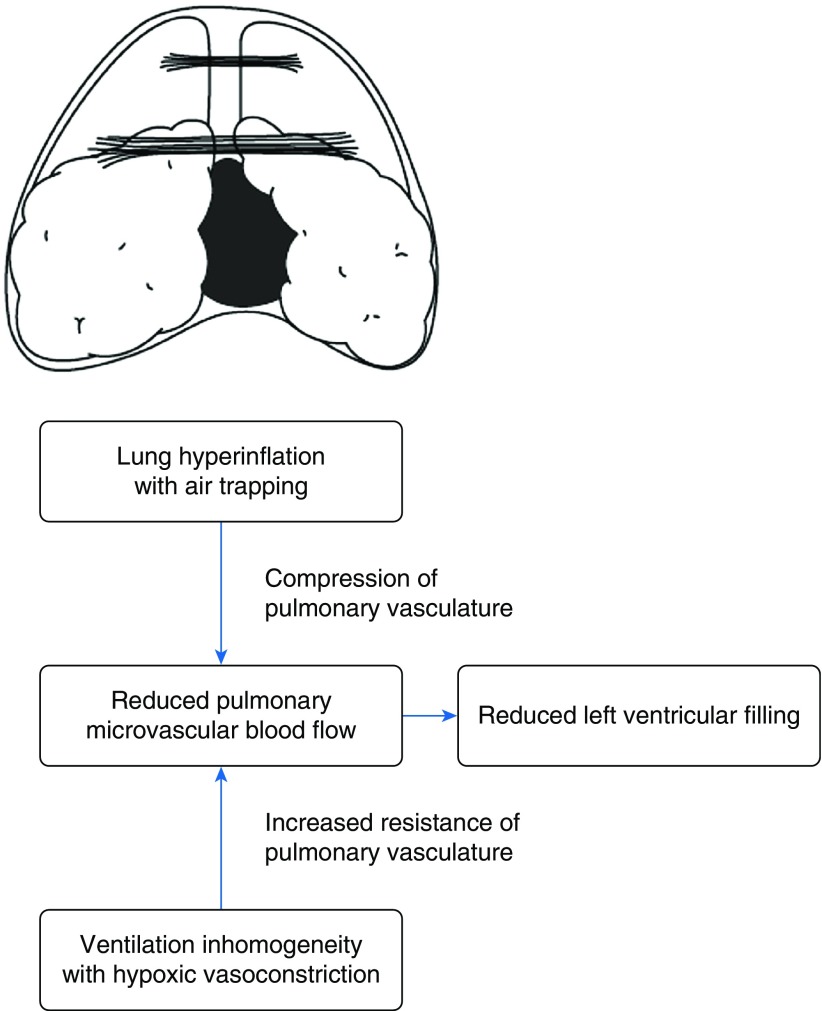
For me, the current (“secondary”) analyses are even more important than the previous primary analyses, which confirmed what had been shown before. So why are the current analyses important and clearly not secondary, as formally stated in the statistical analysis plan in the protocol? It is because they help us understand the mechanisms by which bronchodilators improve cardiac filling. Based on data derived from chest X-ray imaging and right heart catheterization with wedge pressure measurements, it was previously speculated that lung hyperinflation prevents the extension of the heart within the cardiac fossa during diastolic filling (10). It now seems that this is an effect of lung hyperinflation on pulmonary perfusion rather than an improvement in the anatomical position of the heart. Furthermore, the improvements of pulmonary perfusion seen with lung deflation in the current analyses by Vogel-Claussen and colleagues seem to occur predominantly at the microvasculature site rather than at the macrovasculature site (9). This implies that reduced air trapping with less compression of the pulmonary microvasculature mediates the effects of bronchodilation on cardiac filling due to increased perfusion (Figure 1). A second mechanism closely related to the first is the improved regional ventilation with bronchodilation. Increased regional ventilation might in turn result in an improved ventilation–perfusion mismatch, which again improves the venous blood flow to the left heart (Figure 1).
Figure 1.
Schematic diagram showing the potential mechanisms of lung hyperinflation on reduced left ventricular filling, which is mediated by reduced pulmonary microvascular blood flow. The drawing of the hyperinflated lung is reproduced by permission from Reference 10.
Can the book now be closed on the effects of bronchodilation on cardiac filling? The answer to this question is clearly no! We need to find out how far the results of this single-center study in a highly selected population can be generalized, as not all patients with COPD have markedly hyperinflated lungs. Furthermore, patients with COPD are frequently affected by cardiac comorbidities. In particular, arterial hypertension affects diastolic function and filling. Would the results be the same in patients with less hyperinflation and a “stiff heart” due to hypertensive heart disease and other cardiovascular conditions, such as coronary artery disease and atrial fibrillation? I don’t think so. Striking results in a paper by the COPDGene investigators show that reduction of exacerbation by the use of β-blockers occurs primarily in patients with COPD and a low left ventricular volume (11). Is this a COPD-specific cardiac effect of β-blockers with a longer filling time due to heart rate reduction and consequently a better cardiac filling? We don’t know yet, but I am sure we will find out in the near future. This landmark paper by Vogel-Claussen and colleagues will help us design future studies to address these questions.
Supplementary Material
Acknowledgments
Acknowledgment
The author thanks Mary McKenney for a critical review of this paper.
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.201901-0061ED on January 29, 2019
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Kovacs G, Agusti A, Barberà JA, Celli B, Criner G, Humbert M, et al. Pulmonary vascular involvement in chronic obstructive pulmonary disease: is there a pulmonary vascular phenotype? Am J Respir Crit Care Med. 2018;198:1000–1011. doi: 10.1164/rccm.201801-0095PP. [DOI] [PubMed] [Google Scholar]
- 2.Rocha A, Arbex FF, Sperandio PA, Souza A, Biazzim L, Mancuso F, et al. Excess ventilation in chronic obstructive pulmonary disease-heart failure overlap: implications for dyspnea and exercise intolerance. Am J Respir Crit Care Med. 2017;196:1264–1274. doi: 10.1164/rccm.201704-0675OC. [DOI] [PubMed] [Google Scholar]
- 3.Watz H, Waschki B, Boehme C, Claussen M, Meyer T, Magnussen H. Extrapulmonary effects of chronic obstructive pulmonary disease on physical activity: a cross-sectional study. Am J Respir Crit Care Med. 2008;177:743–751. doi: 10.1164/rccm.200707-1011OC. [DOI] [PubMed] [Google Scholar]
- 4.Watz H, Waschki B, Meyer T, Kretschmar G, Kirsten A, Claussen M, et al. Decreasing cardiac chamber sizes and associated heart dysfunction in COPD: role of hyperinflation. Chest. 2010;138:32–38. doi: 10.1378/chest.09-2810. [DOI] [PubMed] [Google Scholar]
- 5.Watz H. The lungs and the heart. Am J Respir Crit Care Med. 2015;192:7–8. doi: 10.1164/rccm.201505-0888ED. [DOI] [PubMed] [Google Scholar]
- 6.Watz H. Chronic obstructive pulmonary disease: when pulmonologists do something good for the heart. Am J Respir Crit Care Med. 2016;193:703–704. doi: 10.1164/rccm.201512-2340ED. [DOI] [PubMed] [Google Scholar]
- 7.Stone IS, Barnes NC, James WY, Midwinter D, Boubertakh R, Follows R, et al. Lung deflation and cardiovascular structure and function in chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2016;193:717–726. doi: 10.1164/rccm.201508-1647OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hohlfeld JM, Vogel-Claussen J, Biller H, Berliner D, Berschneider K, Tillmann HC, et al. Effect of lung deflation with indacaterol plus glycopyrronium on ventricular filling in patients with hyperinflation and COPD (CLAIM): a double-blind, randomised, crossover, placebo-controlled, single-centre trial. Lancet Respir Med. 2018;6:368–378. doi: 10.1016/S2213-2600(18)30054-7. [DOI] [PubMed] [Google Scholar]
- 9.Vogel-Claussen J, Schönfeld C-O, Kaireit TF, Voskrebenzev A, Czerner CP, Renne J, et al. Effect of indacaterol/glycopyrronium on pulmonary perfusion and ventilation in hyperinflated patients with chronic obstructive pulmonary disease (CLAIM): a double-blind, randomized, crossover trial Am J Respir Crit Care Med 20191991086–1096 [DOI] [PubMed] [Google Scholar]
- 10.Butler J, Schrijen F, Henriquez A, Polu JM, Albert RK. Cause of the raised wedge pressure on exercise in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1988;138:350–354. doi: 10.1164/ajrccm/138.2.350. [DOI] [PubMed] [Google Scholar]
- 11.Bhatt SP, Vegas-Sánchez-Ferrero G, Rahaghi FN, MacLean ES, Gonzalez-Serrano G, Come CE, et al. Cardiac morphometry on computed tomography and exacerbation reduction with β-blocker therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;196:1484–1488. doi: 10.1164/rccm.201702-0399LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.