Abstract
Introduction:
Tumors are the second-most common cause of death after cardiovascular diseases. Due to the high prevalence and mortality rate, brain tumors are of great importance and makeup about 5% of all tumors. Different types of brain tumors have their special pattern based on age, sex, complaints on admission, radiological signs and sometimes, their family history and seem these patterns are changing according to the geographic region over time. In this study, we evaluate the incidence of brain tumors in the northwest of Iran.
Materials and Methods:
All patients with brain tumor diagnosis that were hospitalized between April 2011 and March 2016 evaluated. Exclusion criteria were considered as secondary tumors of the central nervous system (CNS) (metastases) and duplicate records for the recurrent disease of the same patient. Data collected from their documents and analyzed with SPSS version 16.
Results:
In the present study, male to female (M: F) ratio is 1:1. 92.5% of tumors are primary in which meningiomas (22%) and glioblastoma multiforme (GBM) (19.6%) are the most common types. The rarest tumor types are neurocytoma (0.3%) and chondroid chordoma (0.3%). GBM is the most common tumor in the male population and meningiomas are most common in females. Medulloblastoma and meningioma with a median age of 11 and 58 years, respectively, were known as the most common primary CNS malignancy of the youngest and oldest age of study group.
Conclusion:
The obtained data from this study revealed that age and sex are associated with the tumor types, which is consistent with the previous results. Brain tumors involvement pattern is changing in male patients somehow there is a tendency of involving more aggressive and malignant tumor types in male individuals could be seen.
Keywords: Brain tumor, epidemiology, primary central nervous system tumors, prevalence, tumor types
Introduction
Primary central nervous system tumors (PCNST) are known as all primary tumors which were arise from the main tissue or envelopes of the central nervous system (CNS).[1,2,3,4] These tumores are categorized into, benign, malignant or uncertain evolution. PCNST indicates a heterogeneous group of tumors, including 143 histological subtypes based on the World Health Organization (WHO) classification.[1,2] The overall incidence rate of all PCNST showes a range from 17.6/105 to 22.0/105 in American and European literatures.[5,6,7,8] Because of these tumors are responsible for high mortality and morbidity they are considered as a major public health issue whole over the world.[9] There is lack of Epidemiological data on PCNST in many countries including Iran because of the lack of a registration system on PCNT. There are numerous difficulties for tumor registries. Since data recording requires collecting all data from a high number of sources: data from neurosurgeons, radiologists, pathologists and death certificates, its time-consuming and not applicable in all facilities.[7] However, few national registries have provided theese type of information in their database. Among them, the Central Brain Tumor Registry of the United States (CBTRUS) provides valuable data on PCNST, classified based on the histology-grouping scheme.[5]
Despite the importance of epidemiologic studies on brain tumors, based on what mentioned above, there is a lack of such data in our area as a referral center of the northwest of Iran. Therefore, we decided to collect the epidemiologic data on PCNST based on a 5-year retrospective study.
Primary objective of our study was to provide descriptive epidemiological data of all histologically confirmed subtypes of PCNST in the East Azerbaijan province in Iran. It can provide a pile of valuable information for future epidemiological studies.
Materials and Methods
In this retrospective study, all patients (no age limit) with a histologically proven PCNST hospitalized between April 2011 and March 2016 in Tabriz were included (includes all hospitals of Tabriz University of Medical Science) and variables such as age, sex, and family history were retrospectively collected by referring to the hospital records of patients and entered into the data collection form. All tumors were assorted based on the WHO classification. It should be noted that according to the WHO classification, pituitary tumors do not belong to the PCNST.[1] However, these types of tumors are included in a few registries, such as the CBTRUS, and in the present study, as well.
Exclusion criteria were considered as secondary tumors of the CNS (metastases) and duplicate records for the recurrent disease of the same patient; in that case, data from the first surgery were recorded if within the inclusion criteria.
The sex ratio and average age of patients at the time of diagnosis were provided for each histological subtype. Data collected from the registered documents of all patients and analyzed with SPSS by using frequency, cumulative frequency, independent sample t-test, analysis of variance, Chi-square, and Fisher's statistical tests. In this study, P < 0.05 was considered statistically significant.
Patients who had no definitive pathologist diagnosis after mass removal had been excluded from the study.
Ethical consideration
Patients information entered into this study from archival records of individuals with a codename without mentioning true names of any participants. None of the patients’ personal information was included in this research.
Results
In this study, 610 patients with a primary diagnosis of brain tumor were examined. After modifying samples based on inclusion and exclusion criteria, there were 373 incident cases of CNS tumors were recorded between 2011 and 2016; among them, 347 was PCNST that includes 92.5% of all CNS tumors. The case distribution according to the tumor type and to prevalence was meningioma (22%), GBM (19.2%), astrocytoma (15.5%), oligodendroglioma (8.5%), metastatic tumors (7.5%), Schwannoma (7%), pituitary adenoma (5.9%), medulloblastoma (4.3%), ependymoma (3.2%), primary brain lymphoma (1.3%), hemangioblastoma (1.3%), papilloma (1.3%), craniopharyngioma (1.1%), primitive neuroectodermal tumor (0.8%), hemangiopericytoma (0.5%), neurocytoma (0.3%), and chondroid chordoma (0.3%) of all.
The tumor distribution according to the histology group is shown in Table 1 and Chart 1.
Table 1.
Case distribution according to the tumor type
| Sex | Total | ||
|---|---|---|---|
| Male | Female | ||
| Tumor type | |||
| GBM | |||
| Count | 52 | 21 | 73 |
| Percentage within tumor type | 71.2 | 28.8 | 100.0 |
| Percentage within sex | 27.7 | 11.4 | 19.6 |
| Astrocytoma | |||
| Count | 34 | 24 | 58 |
| Percentage within tumor type | 58.6 | 41.4 | 100.0 |
| Percentage within sex | 18.1 | 13.0 | 15.5 |
| Lymphoma | |||
| Count | 3 | 2 | 5 |
| Percentage within tumor type | 60.0 | 40.0 | 100.0 |
| Percentage within sex | 1.6 | 1.1 | 1.3 |
| Ependymoma | |||
| Count | 5 | 7 | 12 |
| Percentage within tumor type | 41.7 | 58.3 | 100.0 |
| Percentage within sex | 2.7 | 3.8 | 3.2 |
| Pituitary adenoma | |||
| Count | 15 | 7 | 22 |
| Percentage within tumor type | 68.2 | 31.8 | 100.0 |
| Percentage within sex | 8.0 | 3.8 | 5.9 |
| Meningioma | |||
| Count | 20 | 62 | 82 |
| Percentage within tumor type | 24.4 | 75.6 | 100.0 |
| Percentage within sex | 10.6 | 33.5 | 22.0 |
| Sechwannoma | |||
| Count | 12 | 14 | 26 |
| Percentage within tumor type | 46.2 | 53.8 | 100.0 |
| Percentage within sex | 6.4 | 7.6 | 7.0 |
| Craniopharyngioma | |||
| Count | 3 | 1 | 4 |
| Percentage within tumor type | 75.0 | 25.0 | 100.0 |
| Percentage within sex | 1.6 | 0.5 | 1.1 |
| Medulloblastoma | |||
| Count | 7 | 9 | 16 |
| Percentage within tumor type | 43.8 | 56.3 | 100.0 |
| Percentage within sex | 3.7 | 4.9 | 4.3 |
| Hemangioblastoma | |||
| Count | 4 | 1 | 5 |
| Percentage within tumor type | 80.0 | 20.0 | 100.0 |
| Percentage within sex | 2.1 | 0.5 | 1.3 |
| Metastatic tumor | |||
| Count | 15 | 13 | 28 |
| Percentage within tumor type | 53.6 | 46.4 | 100.0 |
| Percentage within sex | 8.0 | 7.0 | 7.5 |
| Oligodendroglioma | |||
| Count | 15 | 15 | 30 |
| Percentage within tumor type | 50.0 | 50.0 | 100.0 |
| Percentage within sex | 8.0 | 8.1 | 8.0 |
| PNET | |||
| Count | 1 | 2 | 3 |
| Percentage within tumor type | 33.3 | 66.7 | 100.0 |
| Percentage within sex | 0.5 | 1.1 | 0.8 |
| Papilloma | |||
| Count | 1 | 4 | 5 |
| Percentage within tumor type | 20.0 | 80.0 | 100.0 |
| Percentage within sex | 0.5 | 2.2 | 1.3 |
| Hemangiopericytoma | |||
| Count | 1 | 1 | 2 |
| Percentage within tumor type | 50.0 | 50.0 | 100.0 |
| Percentage within sex | 0.5 | 0.5 | 0.5 |
| Neurocytoma | |||
| Count | 0 | 1 | 1 |
| Percentage within tumor type | 0.0 | 100.0 | 100.0 |
| Percentage within sex | 0.0 | 0.5 | 0.3 |
| Chondroid chordoma | |||
| Count | 0 | 1 | 1 |
| Percentage within tumor type | 0.0 | 100.0 | 100.0 |
| Percentage within sex | 0.0 | 0.5 | 0.3 |
| Total | |||
| Count | 188 | 185 | 37 3 |
| Percentage within tumor type | 50.4 | 49.6 | 100.0 |
| Percentage within sex | 100.0 | 100.0 | 100.0 |
PNET – Primitive neuroectodermal tumor; GBM – Glioblastoma multiforme
Chart 1.
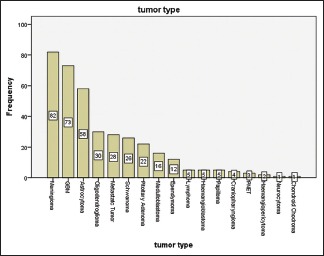
Tumor distribution tumor distribution according to the histology group
According to the WHO Grading of brain tumors in the current study, 47.5% of patients classified as Grade I, 13.3 were in Grade II, Grade III, and Grade IV accounted for 11.9% and 27.2% of cases, respectively.
At the time of diagnosis, 37 (9.6%) patients were aged fewer than 15 years. There was a significant difference in the relationship between types of brain tumors with the age of the patients was found in this study (P < 0.01). Based on that, medulloblastoma was the tumor type that most commonly affected young individuals, and hemangioblastoma was the most common tumors of elderly patients.
The age characteristics of all the cases according to the histological subtype are presented in Chart 2 and Table 2.
Chart 2.
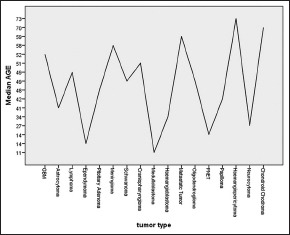
The middle age of patients involved by primary central nervous system tumors
Table 2.
Age distribution of cases based on tumor type
| Tumor type | n | Mean | SD | Median |
|---|---|---|---|---|
| Hemangiopericytoma | 2 | 73.00 | 19.799 | 73.00 |
| Chondroid chordoma | 1 | 70.00 | . | 70.00 |
| Metastatic tumor | 28 | 60.29 | 14.251 | 59.00 |
| Meningioma | 82 | 57.10 | 14.349 | 58.00 |
| Pitoitary adenoma | 22 | 53.00 | 15.185 | 47.50 |
| GBM | 73 | 50.38 | 17.403 | 52.00 |
| Craniopharyngioma | 4 | 49.50 | 13.528 | 50.50 |
| Schwannoma | 26 | 49.00 | 14.489 | 48.50 |
| Oligodendroglioma | 30 | 44.67 | 16.089 | 48.50 |
| Astrocytoma | 58 | 39.78 | 22.092 | 41.00 |
| Lymphoma | 5 | 38.00 | 22.338 | 49.00 |
| Papilloma | 5 | 37.20 | 30.417 | 42.00 |
| PNET | 3 | 36.33 | 42.194 | 14.00 |
| Hemangioblastoma | 5 | 33.80 | 5.718 | 34.00 |
| Neurocytoma | 1 | 27.00 | . | 27.00 |
| Ependymoma | 12 | 16.25 | 13.712 | 13.50 |
| Medulloblastoma | 16 | 15.19 | 9.005 | 11.00 |
| Total | 373 | 47.37 | 20.288 | 49.00 |
PNET – Primitive neuroectodermal tumor; GBM – Glioblastoma multiforme; SD – Standard deviation
Among the patients, 59.4% were male, corresponding to a ratio male/female of 1.19. The mean age was 52.6 years (51.9 for males and 53.3 for females).
In the present study, the most common brain tumor in male patients is GBM and astrocytoma with a prevalence of 27.7% and 18.1% respectively, and meningioma is the most frequent tumor type of females with a frequency of 33.5%.
Regarding the correlation between gender and tumor type also a meaningful relationship was found (P < 0.01). These findings reveal that hemangioblastoma, craniopharyngioma, and GBM mostly affect male patients and on the other hand papilloma and meningioma are more likely diagnosed in females. In addition, neurocytoma and chondroid chordoma were seen with the frequency of one case in female individuals [Table 1 and Charts 3, 4].
Chart 3.
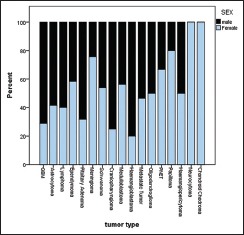
Tumor distribution according to the sex and histology group
Chart 4.
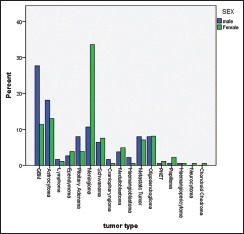
Tumor distribution according to the sex and histology group
Discussion
In the current study, from April 2011 to March 2016, 373 cases of CNS tumors were found in Tabriz University of Medical Science healthcare provider centers among them PCNST accounts for 92.5% of all cases. This huge imbalance between primary and metastatic CNS tumors is caused due to choosing of nonsurgical and palliative approaches for metastatic tumors because of the end stage nature of this situation as well as the technical limitation of using routine biopsy for all individuals with CNS masses.
As it has been mentioned earlier astrocytic tumors are the most common form of PCNST, and among them, GBM is the most common type which is account for approximately 25% of all primary CNS neoplasms. Astrocytomas also include 15%–20% of all PCNST.[5,10,11]
The obtained data of the present study revealed a prevalence rate of 19.6% for GBMs and 15.5% for astrocytomas, that is, close to the international statistics.
Meningiomas include 20% of PCNST and more commonly occurs in the last decades of life and is more commonly involved females.[9,10] In our study, it has been shown that meningeal tumors account for 22% of PCNST and has a high incidence after the 6th decade of life, and also more common in female individuals as well. The frequency was more than twice greater in females than in males. These results are in favor of other studies performed in Europe and the US.[12,13]
In addition, many studies count the female gender as a known risk factor for meningioma.[14]
In other related investigations have been done by researchers around the world a different male: female ratio among CNS tumors was reported, which can be explained by the environmental and racial differences among different ethnic groups.[10,11,15]
In our study, this proportion was almost equal with a slightly high presentation in male individuals.
Based on the results of the present study, medulloblastoma has the highest frequency rate among children with a median age of 11 years. This finding is similar to reports in the northeast of Iran, which explained that medulloblastoma is at the top list of PCNST incidence in children.[16]
Based on literature Medduloblastomas are mostly known to occure among pediatric population. Data collected from the SEER database revealed that this type of brain tumor represents a tendency to affect children (9.6 versus 0.54 children and adult respectively per million).[17]
In compare with a similar study in East Azerbaijan province which was done almost 10 years ago, a noticeable alteration in the pattern of CNS malignancies has seen. Based on the study done by Meshkini et al.,[18] hypophyseal adenomas account for the most common type of PCNS malignancy while in our study GBM was the most common type of malignancy.
Primary brain lymphomas also have shown a greater incidence in the current study as compared to the past. This increase in incidence is important because that very type of CNS malignancies just involved and related with immunodeficiency state.
Conclusion
Despite the high frequency of brain neoplasms in Iran, there are a few studies have been performed in order to evaluate the distribution of CNS tumors based on demographic and histopathologic types. The current retrospective study demonstrates important pathologic and epidemiologic features of primary CNS tumors in hospitals of the Tabriz University of Medical Science as the most dominant referral center of north-west of Iran. Therefore, this data can provide a preliminary information for upcoming researches.
In general, we can conclude that the incidence and prevalence rate of more invasive CNS tumors is highly increased in the East-Azerbaijan area in comparison with the past decades.
With the importance of CNS tumors and its influence and effect on health care and social systems, also psychological impression on the patients based on the findings of the current study it is clear that the more invasive types of CNS malignancies are growing. Therefore, the necessity of supplementary studies for determining of potential risk factors and rule of today's technology in getting involved with this kind of disease is completely clear.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131:803–20. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 2.Methodology Statistical Applications Branch, Surveillance Research Program, National Cancer Institute. Joinpoint Regression Program, Version. 2013;4(1.4) [Google Scholar]
- 3.Fisher JL, Schwartzbaum JA, Wrensch M, Wiemels JL. Epidemiology of brain tumors. Neurol Clin. 2007;25:867–90, vii. doi: 10.1016/j.ncl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Sahyoun NR, Lentzner H, Hoyert D, Robinson KN. Hyattsville, Maryland: National Center for Health Statistics; 2001. Trends in Causes of Death Among the Elderly. Aging Trends No. 1. [DOI] [PubMed] [Google Scholar]
- 5.Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol. 2015;17(Suppl 4):iv1–62. doi: 10.1093/neuonc/nov189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wöhrer A, Waldhör T, Heinzl H, Hackl M, Feichtinger J, Gruber-Mösenbacher U, et al. The austrian brain tumour registry: A cooperative way to establish a population-based brain tumour registry. J Neurooncol. 2009;95:401–11. doi: 10.1007/s11060-009-9938-9. [DOI] [PubMed] [Google Scholar]
- 7.Baldi I, Gruber A, Alioum A, Berteaud E, Lebailly P, Huchet A, et al. Descriptive epidemiology of CNS tumors in france: Results from the gironde registry for the period 2000-2007. Neuro Oncol. 2011;13:1370–8. doi: 10.1093/neuonc/nor120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crocetti E, Trama A, Stiller C, Caldarella A, Soffietti R, Jaal J, et al. Epidemiology of glial and non-glial brain tumours in Europe. Eur J Cancer. 2012;48:1532–42. doi: 10.1016/j.ejca.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 9.DeAngelis LM. Brain tumors. N Engl J Med. 2001;344:114–23. doi: 10.1056/NEJM200101113440207. [DOI] [PubMed] [Google Scholar]
- 10.Fuller GN, Ribalta T. Brain Tumors: An Overview of Current Histopathologic Classification. In: Winn HR, editor. Youmans Neurological Surgery. 6th ed. Philadelphia PA: Elsevier Health Science; 2011. pp. 1077–86. [Google Scholar]
- 11.Stiller CA, Desandes E, Danon SE, Izarzugaza I, Ratiu A, Vassileva-Valerianova Z, et al. Cancer incidence and survival in European adolescents (1978-1997). Report from the automated childhood cancer information system project. Eur J Cancer. 2006;42:2006–18. doi: 10.1016/j.ejca.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99:307–14. doi: 10.1007/s11060-010-0386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michaud DS, Gallo V, Schlehofer B, Tjønneland A, Olsen A, Overvad K, et al. Reproductive factors and exogenous hormone use in relation to risk of glioma and meningioma in a large European cohort study. Cancer Epidemiol Biomarkers Prev. 2010;19:2562–9. doi: 10.1158/1055-9965.EPI-10-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krampla W, Newrkla S, Pfisterer W, Jungwirth S, Fischer P, Leitha T, et al. Frequency and risk factors for meningioma in clinically healthy 75-year-old patients: Results of the transdanube ageing study (VITA) Cancer. 2004;100:1208–12. doi: 10.1002/cncr.20088. [DOI] [PubMed] [Google Scholar]
- 15.DeAngelis LM, Bruce JN. Tumors of the Skull and Cranial Nerves. In: Rowland LP, Pedley TA, editors. Merrit's Neurology. 12th ed. Philadelphia PA: Wolters Kluwer Lippincott Williams & Wilkins; 2010. pp. 378–86. [Google Scholar]
- 16.Jafarzadeh N, Faal A, Izanloo A, Farrokhi F, Ziaolhagh R, Hashemian HR, et al. Epidemiology of nervous system tumors according to WHO 2007 classification: A report of 1,164 cases from a single hospital. Int J Cancer Manage. 2018;11:e11462. [Google Scholar]
- 17.Smoll NR, Drummond KJ. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci. 2012;19:1541–4. doi: 10.1016/j.jocn.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Meshkini A, Fakhrjou A, Fathi A. Prevalence of central nervous system tumors – A single center ten-year study in Tabriz Imam Khomeini hospital. Med J Tabriz Univ Med Sci. 2010;31:76–82. [Google Scholar]


