Abstract
Background:
Conventionally, intradural spinal tumor excision requires longer skin incision, bilateral subperiosteal muscle stripping, and total laminectomy, thereby decreasing the stability of the spine and increasing the morbidity. Minimally invasive surgery (MIS) for intradural spinal tumor excision preserves the posterior supporting structures of the spine in the midline and on the contralateral side and decreases morbidity and achieves the resection of the tumor.
Aims:
The aim is to analyze the surgical technique and outcome of the thoracic and lumbar intradural spinal tumor excision using minimally invasive tubular retractor system.
Patients and Methods:
A retrospective study was conducted in patients admitted with thoracic and lumbar intradural spinal tumors who had undergone tumor excision using minimally invasive tubular retractor system and satisfied the inclusion and exclusion criteria. Intradural tumors involving one or two vertebral levels were included in the study. Intramedullary spinal tumor, intradural tumor extending into intervertebral foramen, and intradural tumor involving more than two vertebral levels were excluded from the study. The study included the data of the 13 patients, who were operated between January 2017 and October 2018. The age and sex of the patients were noted. Gadolinium-enhanced magnetic resonance imaging scan and X-ray of the spine were taken in all the patients. The pre- and postoperative data analyzed include pain using visual analog scale (VAS), power using Medical Research Council (MRC) grading, myelopathy using Nurick's grade, sensory changes, and bowel and bladder symptoms. The steps involved in the surgical technique, extent of resection, intraoperative blood loss, duration of surgery, postoperative complications, duration of stay after the surgery, and postoperative X-ray were analyzed.
Results:
Out of 13 patients, one case of dorsally placed meningioma was converted to open laminectomy and excision due to nonvisualization of the spinal cord and increased bleeding from the tumor. Hence, data of the remaining 12 patients were analyzed. The histopathology of these cases was meningioma (6), schwannoma (5), and neurenteric cyst (1). There were 5 men and 7 women with age group of 27–70 years (mean: 48 years). There were 8 thoracic and 4 lumbar tumors. The duration of symptoms was 2 days to 72 months (mean: 35 months). Eight cases were predominantly occupying on the right side and 4 cases on the left side within the spinal canal. The skin incision length was 25 mm to 35 mm (mean: 28 mm). We used tubular retractors with diameter ranging from 22 mm to 30 mm (mean: 24 mm). Expandable retractors were used in 9 cases (75%) and nonexpandable in 3 cases (25%). Tubular retractor of company Jayon (India) was used in 5 cases and PITKAR (India) in 7 cases. We have not found any significant difference in the usage of both the systems. The tumor size (craniocaudal) was ranging from 9.5 mm to 38 mm (mean: 19 mm). Intraoperative blood loss was 75–200 ml (mean: 115 ml). Gross total resection was achieved in 8 cases and near-total resection in 4 cases. Dura was sutured primarily in all the cases. The dural closure was done with continuous sutures in 6 (50%) cases and interrupted in 6 (50%) cases. Polypropylene suture was used in 10 cases and polyglactin suture in 2 cases of dural closure. The authors found it easy to suture the dura using 7-0 polypropylene. Fibrin sealant was used in 9 (75%) cases. The duration of the surgery was ranging from 160 min to 390 min (mean: 260 min). Cerebrospinal fluid leak and pseudomeningocele were noted in one case. One patient developed suture site infection. VAS for pain, sensory symptoms, Nurick's grade for myelopathy, and MRC grading for power were improved in all the affected patients. Out of two patients with constipation, one patient improved and the other developed incontinence, which was recovered on follow-up after 2 weeks. Out of the 4 patients with urinary symptoms, 3 were improved. Another patient of preoperative normal micturition developed urinary retention due to exacerbation of benign prostatic hypertrophy. Postoperative X-ray showed preserved spinous process and facet joints in all cases. The duration of the hospital stay was ranging from 2 days to 11 days (mean: 6 days).
Conclusion:
Anteriorly or laterally placed intradural spinal tumors confined to the spinal canal can be excised safely and effectively using tubular retractor system, with adding the advantages of the MIS surgery. When in doubt, always convert the MIS to open surgery to avoid injury to vital structures.
Keywords: Intradural tumor, minimally invasive surgery, spinal tumor, tubular retractor
Introduction
Laminectomy is the most commonly performed approach for excision of the intradural spinal tumor. Conventionally, intradural spinal tumor excision requires longer skin incision, bilateral subperiosteal muscle stripping, and total laminectomy. Hence, it decreases the stability of the spine and increases the morbidity.
Unilateral hemilaminectomy is a good corridor for the removal of intradural extramedullary spinal tumors. This approach offers the advantage of less postoperative pain and no postoperative deformity.[1] As the field of minimally invasive surgery (MIS) has developed, it has been implemented for the treatment of increasingly difficult and complex pathologies, including trauma, spinal malignancies, and spinal deformity in adults.[2] MIS for the resection of intradural extramedullary tumors is safe and effective and offers a reduction in operative blood loss, lower risk of cerebrospinal fluid (CSF) leak, and shorter hospital stay for select patients.[3]
Intradural extramedullary and extradural tumors can be completely and safely resected through a minimally invasive approach using the nonexpandable tubular retractor.[4] Most common intradural tumors are schwannomas and meningiomas. The authors analyzed the surgical technique and outcome of the thoracic and lumbar intradural spinal tumor excision using minimally invasive tubular retractor system.
Patients and Methods
The study was conducted in the Department of Neurosurgery, Government Medical College, Thrissur, India, and approved by the Institutional Review Board of the institution. The authors retrospectively analyzed prospectively collected data of 13 patients with thoracic and lumbar intradural spinal tumors, who had undergone hemilaminectomy and tumor excision using minimally invasive tubular retractor system, between January 2017 and October 2018. Patients satisfying the inclusion and exclusion criteria were selected. Intradural tumors involving one or two vertebral levels were included in the inclusion criteria. Intramedullary spinal tumor, intradural tumor extending into intervertebral foramen, and intradural tumor involving more than two vertebral levels were considered for exclusion criteria. Preoperative diagnosis of the tumor was done using 1.5-Tesla gadolinium-enhanced magnetic resonance imaging (MRI). Preoperative anteroposterior and lateral X-ray of the thoracic or lumbar spine was taken in all the cases. Computed tomography scan was taken in few cases. All the patients underwent surgery using expandable or nonexpendable tubular retractor system. Tubular retractor system of either Jayon (India) company or PITKAR (India) company was used depending on the availability. For single-level spinal tumor, it was the preference of the neurosurgeon to use expandable or nonexpendable retractor system. For two-level spinal tumor, only expandable tubular retractor system was used. Tubular retractors of various diameter and length were available. Preoperative, intraoperative, and postoperative parameters were analyzed.
Parameters analyzed
The parameters analyzed include age, sex, pain using visual analog scale (VAS), power using Medical Research Council (MRC) grading, myelopathy using Nurick's grade, sensory changes, bowel and bladder symptoms, spinal tumor level, size of the tumor, side of the tumor in spinal canal, skin incision length, tubular retractor type and diameter used, hemilaminectomy side and level, intraoperative blood loss, intraoperative extent of tumor resection (gross total/near total), dural closure technique (primary/secondary), dural suturing technique (continuous/interrupted), suture material used for dural closure, use of fibrin glue, duration of surgery, and histopathology. Complications noted include skin necrosis, surgical site infection (SSI), CSF leak, pseudomeningocele, intraoperative wrong level, and intraoperative conversion to open surgery. The postoperative outcomes which were assessed include changes in sensory symptoms, VAS, MRC grading, and Nurick's grade. Changes in urinary and bowel symptoms were noted. Findings in spine X-ray (anteroposterior and lateral) taken in the postoperative period were noted. The timing of mobilization and discharge from the hospital were recorded. Any other complications whether intraoperative or postoperative occurring during the admission period were recorded. The data for the study were collected from medical records of the patients available in the medical records library and in the Neurosurgery department. Surgical videos of the patients were also analyzed.
Operative technique
Preoperative marker X-ray was taken in all the patients to decide for the site of skin incision. Urinary catheter was inserted before surgery. All the patients were operated in prone position under general anesthesia with endotracheal intubation. Radiolucent operation table was used for facilitating the anteroposterior and lateral C-arm image. Intraoperative neurophysiological monitoring was not used in any case. After confirming the incision site using C-arm image, a vertical skin incision was placed in paramedian position around 1.5 cm from the midline. The side of the skin incision was determined by the side of the maximum bulk of the tumor in MRI scan. Subcutaneous plane was dissected and thoracolumbar fascia was incised vertically. Smallest dilator was docked on the hemilamina. Serial dilators were sequentially inserted over the smaller dilator [Figure 1]. The dilators were moved over the hemilamina to separate the muscles from the underlying lamina. The position was confirmed using anteroposterior and lateral C-arm image. The desired tubular retractor (expandable or nonexpendable) was placed over the largest positioned dilator [Figure 2a–c]. Then, all the dilators were removed. The shortest length tubular retractor which can fit to just above the skin level was used. Longer length tube was avoided since it was increasing working distance for the instruments. The tubular retractor was angulated according to the need and fixed to the table-mounted retractor holder [Figure 3]. The retractor holder can be loosened at any time to reposition the tubular retractor. Now, the position of the retractor was again confirmed using C-arm image. Neurosurgical operating microscope (Leica F40) was now brought into the scene. The remaining minimal muscles over the hemilamina were removed. Hemilaminectomy was done using high-speed drill (Anspach, Johnson & Johnson) and Kerrison punch. Ligamentum flavum was excised. Spinous process, interspinous, and supraspinous ligaments were preserved. Whenever required, the base of the spinous process was drilled for the wider exposure. Minimal facetectomy was done, whenever required to expose the tumor. Bayonetted instruments were used to avoid visual obscuration during surgery. Dura was opened longitudinally using No. 11 scalpel blade and held widely separated using tack sutures, which are put using 5-0 polypropylene. Arachnoid was opened. The spinal cord, roots, and tumor were identified. Tumor capsule was opened and tumor was decompressed. Ultrasonic aspirator (CUSA, Integra, Inc.) was used whenever required. After decompression, capsule was removed. Small schwannomas were removed en bloc without decompression. In meningioma, excision of the tumor and coagulation of the dura was considered as the gross total resection (GTR). Small part of the tumor inseparable from the root or cord was left behind in near-total resection (NTR). Dura was sutured using continuous or interrupted sutures. Dural closure was a difficult step. The authors used bayonetted toothed forceps and bayonetted needle holder for suturing the dura. Fat pieces were layered and fibrin sealant (Tisseel, Baxter, India or Evicel, Johnson and Johnson) was applied. Tubular retractor was removed. Separated muscles were reapproximated. Subcutaneous sutures put and skin stapled.
Figure 1.
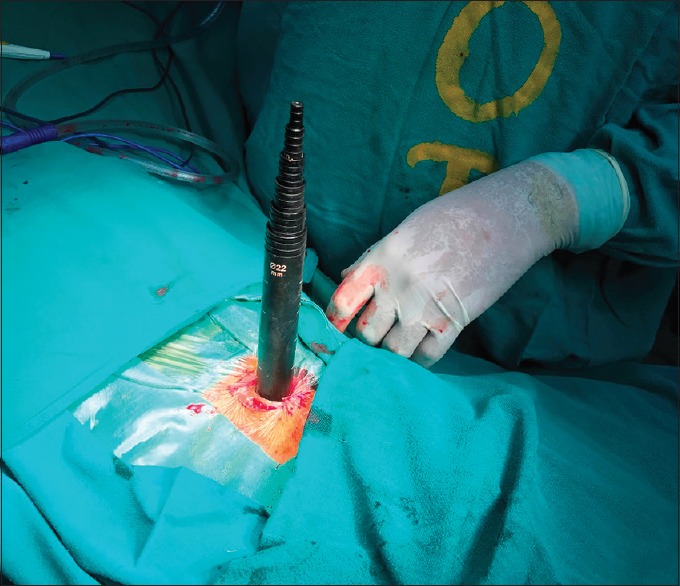
Serial dilators were sequentially inserted over the smaller dilator in minimally invasive surgery surgery
Figure 2.
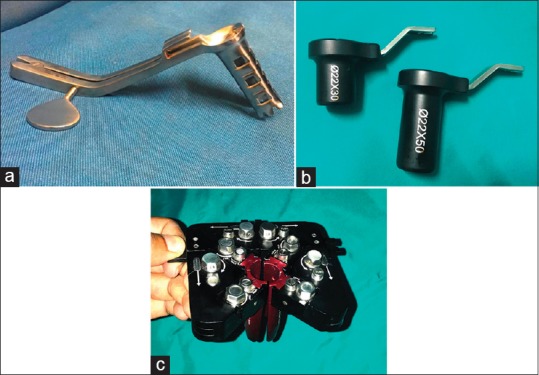
(a) Jayon (India) expandable tubular retractor. (b) PITKAR (India) nonexpandable tubular retractor. (c) PITKAR (India) expandable tubular retractor
Figure 3.
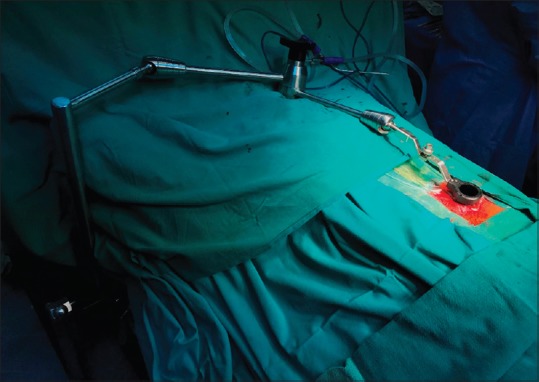
The tubular retractor was fixed to the table-mounted retractor holder
Results
There were 13 patients with thoracic and lumbar intradural spinal tumors, who underwent surgery using minimally invasive tubular retractor system, and satisfied the inclusion and exclusion criteria. The histopathology of these cases was meningioma (7), schwannoma (5), and neurenteric cyst (1). Among them, one case of 22-year-old female meningioma at T9–10 level was converted to open laminectomy. It was arising from the dorsal and lateral surface of the dura mater. Spinal cord was not visualized due to the dorsal attachment and increased bleeding from the meningioma. Hence, this case was converted to open laminectomy and excision. The data were analyzed in the remaining 12 patients. There were 5 men and 7 women with age group of 27–70 years (mean age: 48 years). There were 8 thoracic and 4 lumbar tumors. The duration of symptoms was ranging from 2 days to 72 months (mean: 35 months) [Table 1].
Table 1.
Distribution of age, sex, and duration of symptoms in 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
| Case number | Age | Sex | Duration of symptoms (months) |
|---|---|---|---|
| 1 | 31 | Male | 5 |
| 2 | 36 | Female | 18 |
| 3 | 48 | Female | 2 |
| 4 | 58 | Male | 60 |
| 5 | 42 | Female | 24 |
| 6 | 55 | Female | 72 |
| 7 | 46 | Female | 36 |
| 8 | 48 | Male | 60 |
| 9 | 70 | Female | 48 |
| 10 | 45 | Female | 24 |
| 11 | 65 | Male | 72 |
| 12 | 27 | Male | 2 days |
Back pain and radiculopathy were noted in 10 patients, sensory symptoms in 12 patients, constipation in 2 patients, and urinary symptoms in 4 patients. On examination, spasticity was noted in 3 patients and lower limb weakness was noted in 12 patients [Figure 4].
Figure 4.
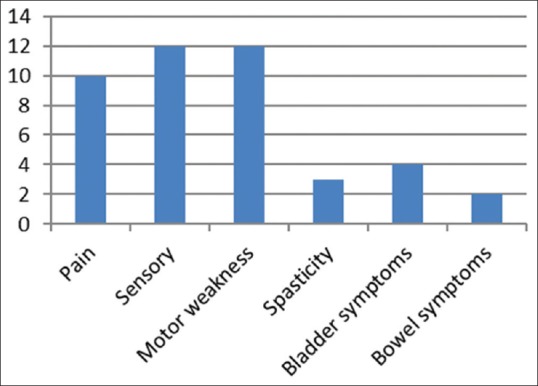
Clinical features of 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
Eight cases were predominantly occupying on the right side and four cases on the left side within the spinal canal. The tumor had pushed the spinal cord to the opposite direction. The side for the surgery was approached from the side of the tumor within the spinal canal. The incision length was ranging from 25 mm to 35 mm (mean: 28 mm). We used tubular retractors with diameter ranging from 22 mm to 30 mm (mean: 24 mm). Expandable retractors were used in 9 cases and nonexpendable in 3 cases. For two-level hemilaminectomy, the authors preferred to use expandable retractor. The authors used either Jayon, India, or PITKAR, India, tubular retractor system depending on the availability. We have not found any significant difference in the usage of both the systems for one level tumor [Table 2].
Table 2.
Operative findings of 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
| Case number | Tumor location | Side of tumor | Incision length (mm) | Tubular retractor | Tubular retractor diameter (mm) | Implant used | Hemilaminectomy side | Hemilaminectomy |
|---|---|---|---|---|---|---|---|---|
| 1 | L4-5 | Right | 30 | Expandable | 25 | Jayon | Right | L4, upper L5 |
| 2 | L3-4 | Left | 25 | Expandable | 22 | Jayon | Left | Lower L3, upper L4 |
| 3 | T11 | Left | 25 | Expandable | 22 | Jayon | Left | T11 |
| 4 | L4-5 | Left | 25 | Expandable | 23 | Jayon | Left | Lower L4, L5 |
| 5 | L3 | Right | 28 | Nonexpandable | 22 | PITKAR | Right | L3 |
| 6 | T10 | Right | 30 | Expandable | 25 | Jayon | Right | T10 |
| 7 | T12 | Right | 30 | Expandable | 25 | PITKAR | Right | T12 |
| 8 | T9 | Right | 25 | Expandable | 22 | PITKAR | Right | T9 |
| 9 | T10-11 | Left | 25 | Nonexpandable | 22 | PITKAR | Left | T10 |
| 10 | T12 | Right | 30 | Expandable | 25 | PITKAR | Right | T12 |
| 11 | T11-12 | Right | 35 | Expandable | 30 | PITKAR | Right | T11, T12 |
| 12 | T8 | Right | 30 | Nonexpandable | 22 | PITKAR | Right | T8 |
The tumor size (craniocaudal) was ranging from 9.5 mm to 38 mm (mean: 19 mm). Intraoperative blood loss was 75–200 ml (mean: 115 ml). GTR was achieved in 8 (67%) cases and NTR in 4 (33%) cases. Small part of the tumor adhering to the spinal cord and roots were intentionally left behind in the four cases of NTR. Dura was sutured primarily in all the cases. Dural closure was done with continuous sutures in 6 (50%) cases and interrupted in 6 (50%) cases. Polypropylene sutures were used in 10 (83%) cases (5-0 in 5 cases, 6-0 in 3 cases, and 7-0 in 2 cases) and polyglactin in 2 (17%) cases (5-0 in 1 case and 6-0 in 1 case). There was no difference in the result on using continuous or interrupted sutures. We found that it was easy to put sutures continuously using 7-0 polypropylene. Fibrin sealant was used in 9 cases. Intraoperatively, fibrin sealant was found to seal the dura along the suture line. The duration of the surgery was ranging from 160 min to 390 min (mean: 260 min) [Table 3].
Table 3.
Operative findings, histopathology, and duration of hospital stay after the surgery of 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
| Case number | Tumor size (mm) (AP × TR × CC) | Blood loss (ml) | Excision | Dural closure | Dural suturing | Suture material | Fibrin sealant usage | Duration of surgery (minutes) | Histopathology | Duration of stay (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 10×11×17 | 150 | GTR | Primary | Interrupted | 5-0 polypropylene | + | 390 | Schwannoma | 3 |
| 2 | 8×11×9.5 | 75 | NTR | Primary | Interrupted | 5-0 polypropylene | - | 300 | Schwannoma | 7 |
| 3 | 9×11×12 | 100 | GTR | Primary | Continuous | 6-0 polypropylene | - | 160 | Schwannoma | 2 |
| 4 | 15×25×30 | 150 | NTR | Primary | Interrupted | 5-0 polyglactin | - | 210 | Schwannoma | 9 |
| 5 | 10×10×12 | 90 | GTR | Primary | Continuous | 6-0 polypropylene | + | 200 | Meningioma | 7 |
| 6 | 8×8 × 11 | 150 | GTR | Primary | Interrupted | 5-0 polypropylene | + | 300 | Meningioma | 3 |
| 7 | 12×16×14 | 100 | GTR | Primary | Continuous | 7-0 polypropylene | + | 200 | Meningioma | 3 |
| 8 | 14×15×26 | 200 | NTR | Primary | Interrupted | 5-0 polypropylene | + | 360 | Meningioma | 7 |
| 9 | 12×13×26 | 70 | GTR | Primary | Interrupted | 6-0 polyglactin | + | 165 | Meningioma | 8 |
| 10 | 12×16×15 | 75 | GTR | Primary | Continuous | 5-0 polypropylene | + | 220 | Meningioma | 7 |
| 11 | 14×17×38 | 150 | NTR | Primary | Continuous | 6-0 polypropylene | + | 360 | Schwannoma | 11 |
| 12 | 13×10×18 | 75 | GTR | Primary | Continuous | 7-0 polypropylene | + | 255 | Neurenteric cyst | 7 |
+: Used, -: Not used. GTR – Gross total resection; NTR – Near-total resection
Pseudomeningocele and CSF leak were noted in one case of T11–T12 laminectomy and schwannoma excision. In this case, dura was sutured continuously using 6-0 polypropylene and fibrin sealant was applied. It was subsided after 10 days of conservative treatment. One patient had SSI, which was treated with antibiotics and resuturing [Table 4].
Table 4.
Complications of 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
| Case number | Skin necrosis | Suture site infection | CSF leak | Pseudo meningocele | Wrong level |
|---|---|---|---|---|---|
| 1 | - | - | - | - | - |
| 2 | - | - | - | - | - |
| 3 | - | - | - | - | - |
| 4 | - | + | - | - | - |
| 5 | - | - | - | - | - |
| 6 | - | - | - | - | - |
| 7 | - | - | - | - | - |
| 8 | - | - | - | - | - |
| 9 | - | - | - | - | - |
| 10 | - | - | - | - | - |
| 11 | - | - | + | + | - |
| 12 | - | - | - | - | - |
+: Present, -: Absent. CSF – Cerebrospinal fluid
All the patients were treated with oral acetaminophen 500 mg twice daily for 3 days and oral gabapentin 100 mg once daily for 2 weeks. Minimal pain was noted at the surgery site in postoperative period. All the affected patients (100%) were improved in VAS (preoperative mean: 8.6; postoperative mean: 1.5). Sensory symptom of paresthesia or numbness was improved in all patients (100%). Nurick's grade was improved in all 3 affected patients (100%). Lower limb power was grossly assessed using MRC grading. Power was improved in all the affected 12 patients (100%). Ten patients were mobilized in 24 h. In the remaining two, one patient with preoperative paraplegia started walking with support on the 6th postoperative day. The other patient with severe lower limb weakness (right: Grade 2, left: Grade 0) had improved in power (right: Grade 4, left: Grade 1) without able to walk. Out of 2 patients with constipation, one was improved but the other developed incontinence, which was recovered on follow-up after 2 weeks. Out of 4 patients with urinary symptoms, 3 were recovered. However, one patient of retention was discharged with urinary catheter. Another preoperatively normal patient developed urinary retention in the postoperative period. On evaluation by urologist, he was found to have Grade II benign prostatic hypertrophy. Hence, he was discharged with urinary catheter on urologist advice [Table 5]. Postoperative anteroposterior and lateral X-ray was showing preserved spinous process and facet joints. The duration of the hospital stay was ranging from 2 days to 11 days (mean: 6 days).
Table 5.
Preoperative and postoperative clinical findings of 12 patients undergoing minimally invasive resection of thoracic and lumbar intradural spinal tumors
| Case number | VAS preoperative | VAS postoperative | Sensory preoperative | Sensory postoperative | Lower limb power preoperative | Lower limb power postoperative | Nurick’s preoperative | Nurick’s postoperative | Bowel symptoms preoperative | Bowel symptoms postoperative | Bladder symptoms preoperative | Bladder symptoms postoperative |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 7 | 1 | + | Decr | R4+, L5 | R5, L5 | NA | NA | N | N | N | N |
| 2 | 9 | 2 | + | Decr | R4-, L4 | R5, L5 | NA | NA | N | N | N | N |
| 3 | 9 | 2 | + | Decr | R5, L4+ | R5, L5 | NA | NA | N | N | N | N |
| 4 | 10 | 2 | + | Decr | R5, L4 | R5, L4+ | NA | NA | N | N | N | Reten |
| 5 | 10 | 0 | + | Decr | R5, L4 | R4+, L4+ | NA | NA | N | N | N | N |
| 6 | 8 | 1 | + | Decr | R4-, L4+ | R4+, L4+ | 3 | 1 | N | N | N | N |
| 7 | 8 | 2 | + | Decr | R4, L5 | R5, L5 | NA | NA | N | N | Reten | N |
| 8 | 8 | 1 | + | Decr | R4-, L4 | R5, L5 | 4 | 1 | N | N | N | N |
| 9 | 0 | 0 | + | Decr | R2, L0 | R4, L1 | NA | NA | Consti | Inconti | Reten | Reten |
| 10 | 9 | 0 | + | Decr | R4, L5 | R5, L5 | NA | NA | N | N | Inconti | N |
| 11 | 8 | 1 | + | Decr | R4, L4; foot R0, L3 | R4+, L4; foot R2, L4 | NA | NA | N | N | N | N |
| 12 | 0 | 0 | + | Decr | R 0, L 0 | R4, L4 | 5 | 3 | Consti | N | Reten | N |
VAS – Visual analog scale; Decr – Decrease; R – Right; L – Left; NA – Not applicable; N – Normal; Consti – Constipation; Reten – Retension
Illustrative case 1
A 70-year-old female patient presented with a history of walking difficulty and lower limbs numbness for 4 years. Walking difficulty had gradually progressed. After a trivial fall 10 days back, the patient had become bedridden and also developed urinary retention and constipation. Examination revealed the right lower limb Grade 2 power and left lower limb Grade 0 power. Sensation was decreased in the lower limbs, lower limb tone was normal, and urinary bladder catheterized. Gadolinium-enhanced MRI scan revealed contrast-enhancing lesion at T10–11 level arising from anterior and left lateral dura of the spinal canal. Radiologically, it was diagnosed as a case of meningioma [Figure 5a and b]. The patient underwent surgery in prone position. A 2.5-cm left paramedian incision was put at T10 lamina level. Serial dilators were placed and the patient underwent T10 left hemilaminectomy using 22-mm nonexpandable PITKAR tubular retractor system [Figure 6a]. The base of the T10 spinous process was drilled. Dura was opened longitudinally. Arachnoid was opened. Meningioma, cord, and roots were defined [Figure 6b]. Tumor was removed in piecemeal and gross total excision was done. Anterior and lateral dural inner surface was coagulated using bipolar diathermy. Dura was closed using 6-0 polyglactin interrupted sutures [Figure 6c]. Bone pieces removed during laminectomy were replaced back on the dural surface along with fat pieces [Figure 6d]. Fibrin sealant was applied and wound closed in layers.
Figure 5.
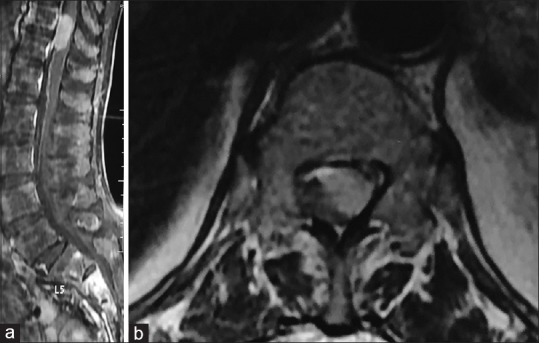
(a) Gadolinium-enhanced magnetic resonance imaging scan sagittal image showing meningioma occupying the anterior part of the spinal canal at T10–11 level. (b) Gadolinium-enhanced magnetic resonance imaging scan axial image showing meningioma occupying the anterior and left lateral part of the spinal canal at T10–11 level
Figure 6.
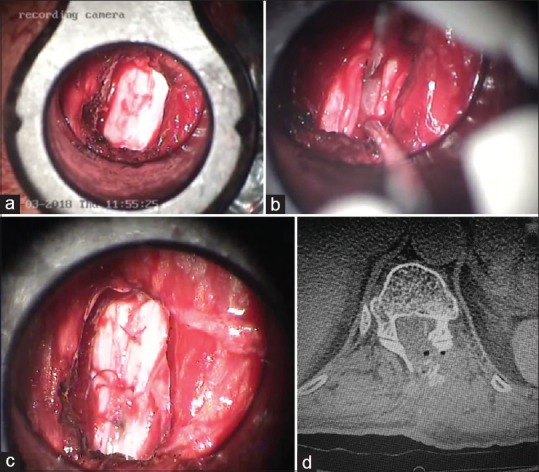
(a) Visualization of the dura after hemilaminectomy using nonexpendable retractor system. (b) Tumor and roots were visualized through the tubular retractor system. (c) Dura was closed using 6-0 polyglactin interrupted sutures. (d) Postoperative computed tomography scan showing the left hemilaminectomy in minimally invasive surgery for tumor excision. Bone pieces removed during laminectomy were replaced back on the dural surface
Illustrative case 2
A 22-year-old female patient was presented with a history of walking difficulty for 1 year, paresthesia and backache for 1 month. Examination revealed the right lower limb Grade 4 power and left lower limb Grade 5 power. Tone was increased in both the lower limbs. Gadolinium-enhanced MRI scan revealed contrast-enhancing lesion at T9–10 level arising from posterior and right lateral dura of the spinal canal. Radiologically, it was diagnosed as a case of meningioma [Figure 7a–c]. The patient underwent surgery using PITKAR expandable tubular retractor system. On opening the dura, meningioma was seen arising from dorsal and lateral surface of the dura. Hence, the spinal cord was not visualized. Furthermore, there was increased bleeding from the tumor. Hence, the case was converted to open laminectomy and excision of the tumor.
Figure 7.
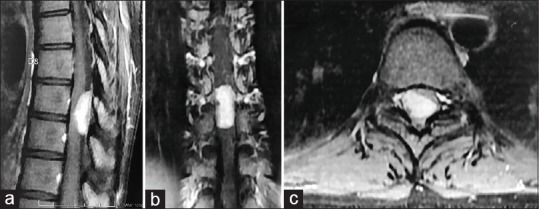
(a) Gadolinium-enhanced magnetic resonance imaging scan sagittal image showing contrast-enhancing meningioma occupying the posterior aspect of the spinal canal at T9–10 level. (b) Gadolinium-enhanced magnetic resonance imaging scan coronal image showing contrast-enhancing meningioma occupying the posterior aspect of the spinal canal at T9–10 level. (c) Gadolinium-enhanced magnetic resonance imaging scan axial image showing contrast-enhancing meningioma occupying the right lateral and posterior aspect of the spinal canal at T9–10 level
Discussion
Nzokou et al. operated 13 patients with thoracic and lumbar spinal tumors using a nonexpandable tubular retractor system. There were 4 patients with intradural (2 lumbar and 2 thoracic) and 9 patients with extradural spinal tumors. There was mean blood loss of 180 ml and mean operative time of 194 min in intradural tumors.[4]
Mannion et al. operated on 13 intradural extramedullary tumors using minimally invasive tube-assisted paramedian oblique approach. Satisfactory tumor resection was achieved in all but 1 case. Mean blood loss was 155 ml and mean operative time was 180 min. The surgical incision was inaccurately placed by one level in 2 cases. In 1 case, the approach was converted to open when the tumor could not be found, and postoperatively, there was a CSF leak with infection that required readmission.[5]
Haji et al. retrospectively reviewed 15 intradural and 7 extradural neoplasms in 20 patients operated on between September 2005 and May 2009 using METRx MAST Quadrant expandable (22–52 mm) tubular retractors (Medtronics). Mean intraoperative time was 210 min, blood loss 428 mL, and average length of hospital stay was 3 days. Four patients required postoperative patient-controlled analgesia for pain control, and an average of 5.8 doses of narcotic were given per patient. One patient developed CSF leak and another patient developed foot drop and urinary retention. About 15 of 22 tumors (68%) were completely resected, with only one patient requiring repeat operation for residual tumor.[6]
Gandhi et al. retrospectively reviewed a prospectively collected surgical database of 14 intradural spinal tumors operated using expandable retractors. Mean intraoperative time was 218 min, estimated blood loss was 280 mL, and average length of hospital stay was 3 days. There was 1 case of wound dehiscence. GTR was achieved in 79% of cases and patients improved neurologically in 71% of cases.[7]
Pham et al. reviewed the literature to find all studies involving minimally invasive resection of intradural extramedullary spinal tumors through the use of a tubular retractor system. Nine studies were found for a total of 114 patients with reported mean ages from 46.5 to 63.8 years and follow-up times from 1.5 months to 24 months. Studies reported their GTR rates (range: 75%–100%), mean operative time (range: 184.9–256.3 min), mean estimated blood loss (range: 56–238.8 ml), and hospital length of stays (range: 2.4–6.9 days). The most common surgery-related complication was CSF leak or pseudomeningocele in 6 patients (5.3%) of which 4 patients (3.5%) required a reoperation. MIS for the resection of intradural extramedullary tumors is safe and effective and offers a reduction in operative blood loss, lower risk of CSF leak, and shorter hospital stay for select patients.[3]
In our study, there were 5 men and 7 women with mean age 48 years. There were 8 thoracic and 4 lumbar tumors with mean duration of symptoms of 35 months. Eight cases were predominantly occupying on the right side (67%) and 4 cases on the left side (33%) within the spinal canal. The mean skin incision length was 28 mm. We used tubular retractors with diameter ranging from 22 mm to 30 mm (mean: 24 mm). Expandable retractors were used in 75% of cases and nonexpandable in 25% of cases. The mean tumor size (craniocaudal) was 19 mm and intraoperative blood loss was 115 ml. GTR was achieved in 67% of cases and NTR in 33% of cases. Dural closure was done with continuous sutures in 50% of cases and interrupted in 50% of cases. Polypropylene sutures were used in 83% of cases and polyglactin in 17% of cases. There was no difference in the outcome on using any particular suture or suturing technique. We found that it was easy to put sutures continuously using 7-0 polypropylene. Fibrin sealant was used in 75% of cases. The authors believe that fibrin sealant reduces the chances of CSF leak. The mean duration of the surgery was 260 min. Pseudomeningocele and CSF leak was noted in one case. The authors believe that chance of CSF leak is more in case of long dural incision. One patient had SSI. One case of dorsally placed meningioma was converted to open surgery. Minimal pain was noted at the surgery site in postoperative period. Motor power, VAS, sensory symptoms, and Nurick's grade were improved in 100% of cases. Long-term follow-up is not available for assessing the development of kyphosis. The mean duration of the hospital stay was 6 days.
Conclusion
Meningiomas arising from the posterior part of spinal dura are preferably operated by open technique. Selection of the ideal patient and experience with open surgery is the paramount factor for the success of MIS tumor excision. Correct C-arm localization of the level of tumor is the most important step in MIS surgery. Bayonetted-shaped instruments will help in avoiding the visual obscuration by the instruments during the surgery. Tumors occupying one spinal level can be operated with either expandable or nonexpandable tubular retractors. However, two-level spinal tumors will require expandable tubular retractors. Gross total excision of the anteriorly or laterally placed intradural tumors confined to the spinal canal can be done safely and effectively using tubular retractor system, with adding the advantages of the MIS surgery. Longer length of the dural opening has higher chances of CSF leak. MIS reduces the blood loss, soft-tissue injury, bone removal, skin incision, and the hospital stay.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.KrishnanKutty R, Sreemathyamma SB, Sivanandapanicker JL, Asher P, Prabhakar RB, Peethambaran A, et al. Hemilaminectomy for spinal cord intradural tumors: An institutional experience. Asian J Neurosurg. 2018;13:760–5. doi: 10.4103/ajns.AJNS_106_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith ZA, Fessler RG. Paradigm changes in spine surgery: Evolution of minimally invasive techniques. Nat Rev Neurol. 2012;8:443–50. doi: 10.1038/nrneurol.2012.110. [DOI] [PubMed] [Google Scholar]
- 3.Pham MH, Chang KE, Liu JC, Hsieh PC. Minimally invasive surgery for intradural extramedullary spinal tumors: A comprehensive review with illustrative clinical cases. World Spinal Column J. 2016;2:84–96. [Google Scholar]
- 4.Nzokou A, Weil AG, Shedid D. Minimally invasive removal of thoracic and lumbar spinal tumors using a nonexpandable tubular retractor. J Neurosurg Spine. 2013;19:708–15. doi: 10.3171/2013.9.SPINE121061. [DOI] [PubMed] [Google Scholar]
- 5.Mannion RJ, Nowitzke AM, Efendy J, Wood MJ. Safety and efficacy of intradural extramedullary spinal tumor removal using a minimally invasive approach. Neurosurgery. 2011;68:208–16. doi: 10.1227/NEU.0b013e318207b3c7. [DOI] [PubMed] [Google Scholar]
- 6.Haji FA, Cenic A, Crevier L, Murty N, Reddy K. Minimally invasive approach for the resection of spinal neoplasm. Spine (Phila Pa 1976) 2011;36:E1018–26. doi: 10.1097/BRS.0b013e31820019f9. [DOI] [PubMed] [Google Scholar]
- 7.Gandhi RH, German JW. Minimally invasive approach for the treatment of intradural spinal pathology. Neurosurg Focus. 2013;35:E5. doi: 10.3171/2013.5.FOCUS13163. [DOI] [PubMed] [Google Scholar]


