Immune checkpoint inhibitors (ICIs) have improved outcomes for patients with cancer but related hematologic toxicities have been poorly described. Using VigiBase, the World Health Organization's pharmacovigilance database of individual case safety reports of adverse drug reactions, this study aimed to identify such cases of hematologic toxicities.
Abstract
Immune checkpoint inhibitors have improved outcomes for patients with numerous hematological and solid cancers. Hematologic toxicities have been described, but the spectrum, timing, and clinical presentation of these complications are not well understood. We used the World Health Organization's pharmacovigilance database of individual‐case‐safety‐reports (ICSRs) of adverse drug reactions, VigiBase, to identify cases of hematologic toxicities complicating immune checkpoint inhibitor therapy. We identified 168 ICSRs of immune thrombocytopenic purpura (ITP), hemolytic anemia (HA), hemophagocytic lymphohistiocytosis, aplastic anemia, and pure red cell aplasia in 164 ICSRs. ITP (n = 68) and HA (n = 57) were the most common of these toxicities and occurred concomitantly in four patients. These events occurred early on treatment (median 40 days) and were associated with fatal outcome in 12% of cases. Ipilimumab‐based therapy (monotherapy or combination with anti‐programmed death‐1 [PD‐1]) was associated with earlier onset (median 23 vs. 47.5 days, p = .006) than anti‐PD‐1/programmed death ligand‐1 monotherapy. Reporting of hematologic toxicities has increased over the past 2 years (98 cases between January 2017 and March 2018 vs. 70 cases before 2017), possibly because of increased use of checkpoint inhibitors and improved recognition of toxicities. Future studies should evaluate incidence of hematologic toxicities, elucidate risk factors, and determine the most effective treatment algorithms.
Key Points.
Immune‐mediated hematologic toxicities are a potential side effect of immune checkpoint inhibitors (ICIs).
Providers should monitor complete blood counts during treatment with ICIs.
Corticosteroids are the mainstay of treatment for immune‐mediated hematologic toxicities.
Further research is needed to define patient‐specific risk factors and optimal management strategies for hematologic toxicities.
Introduction
Immune checkpoint inhibitors (ICIs) have dramatically changed treatment paradigms and outcomes for patients with various malignancies. These therapies may trigger immune‐related adverse events (irAEs), which stem from aberrant activation of T cells against self‐antigens. Common irAEs, including dermatological, gastrointestinal, pulmonary, and endocrine, are well characterized. However, hematologic toxicities have been poorly described, partially because of their uncommon nature but also possibly because of lack of recognition.
A number of isolated case reports and case series have demonstrated that uncommon severe and even fatal hematologic toxicities may complicate immune checkpoint inhibitor therapy [1], [2], [3], [4], [5], [6]. However, no series has evaluated more than 10 cases; thus, the timing, spectrum, and clinical presentation of hematologic irAEs are poorly understood. In this report, we present a case of presumed immune‐mediated hypoproliferative anemia diagnosed at Vanderbilt University Medical Center and discuss management strategies. We then describe our interrogation of an international pharmacovigilance database to characterize 168 individual‐case‐safety‐reports (ICSRs) of hematologic toxicities complicating immune checkpoint inhibitor therapy.
Case Vignette
A 77‐year‐old man with metastatic Merkel cell carcinoma (MCC) being treated with pembrolizumab presented with new lightheadedness and fatigue. He was diagnosed with MCC 2.5 years earlier and had undergone amputation and four cycles of concurrent carboplatin and etoposide and external beam radiation to 5,040 cGy. He did well 6 six months before developing axillary disease necessitating lymph node dissection. Within 3 months, he developed multiple skin nodules and was treated with two cycles of concurrent carboplatin/etoposide and external beam radiation to 6,600 cGy. Treatment toxicities precluded administration of further chemotherapy.
Shortly after completing therapy, he developed additional chest wall disease. He was started on pembrolizumab 2 mg/kg every 3 weeks. Upon starting pembrolizumab, his white blood cell count (WBC) was 4 × 103/mcL, hemoglobin was 10.8 g/dL, and platelets were 52 × 103/mcL. With the next three cycles, blood counts were stable with slight increase in the platelet count. Prior to cycle 5 of pembrolizumab, when the patient presented with new lightheadedness and fatigue, the hemoglobin was 7.4 g/dL with a mean corpuscular volume of 101. WBC was 5.4 × 103/mcL, and platelets were 90 × 103/mcL. Pembrolizumab was held, and the patient was transfused 2 units of packed red blood cells (prbcs). Hemoglobin increased to 8.3 g/dL. Anemia work‐up did not reveal evidence of iron or B12 deficiency, hemolysis, thyroid dysfunction, or parvovirus. Two weeks later, without additional pembrolizumab, hemoglobin decreased further to 6.1 g/dL. Bone marrow biopsy demonstrated a hypocellular bone marrow (5% cellular) with marked erythroid hypoplasia and no evidence of erythroid precursors. He was treated with 2 additional units of prbcs, prednisone 40 mg b.i.d., and then 20 mg b.i.d. with improvement of his hemoglobin to 9.5 g/dL. His prednisone was tapered weekly over the next month; however, he was admitted for dyspnea, and because of concern for pneumonitis, he was reinitiated on high‐dose prednisone. This was tapered over 1 month, during which the hemoglobin was stable in the range of 9–11 g/dL. When prednisone was discontinued, hemoglobin decreased to 7.4 g/dL, and he was transfused 2 units of prbcs and prednisone 20 mg daily was resumed. Prednisone was tapered, and the patient received one additional dose of pembrolizumab. However, he developed gastric outlet obstruction and transitioned to hospice care.
This case highlights the difficulty in diagnosing and managing hematologic complications during immunotherapy treatment. Although this patient may have had some underlying decrease of his red blood cell count from prior treatment, the primary etiology of his anemia was thought to be an immune‐mediated, hypoproliferative anemia closely resembling pure red cell aplasia (PRCA), given the hematologic work‐up and the hemoglobin's response to steroids.
Materials and Methods
VigiBase Analysis
We accessed the World Health Organization's pharmacovigilance database of ICSRs, VigiBase [7], to examine reported hematologic toxicities associated with immune checkpoint inhibitor therapy. VigiBase contains information concerning adverse drug reactions, with >16,000,000 reports from >130 countries (http://www.vigiaccess.org/). We performed a search for severe adverse events associated with anti‐cytotoxic T lymphocyte antigen‐4 (CTLA‐4; ipilimumab, tremelimumab), anti‐programmed death‐1 (PD‐1; nivolumab, pembrolizumab), and anti‐programmed death ligand‐1 (PD‐L1; avelumab, durvalumab, and atezolizumab). We searched the following hematologic conditions using MEDdra preferred terms through March 2018: hemophagocytic lymphohistiocytosis (HLH), aplastic anemia (AA), autoimmune hemolytic anemia (AIHA), hemolytic anemia (HA), immune thrombocytopenic purpura (ITP), and PRCA. We selected these as examples of potentially immune‐mediated conditions that have been previously described with ICIs. We did not include other hematologic complications (e.g., neutropenia, anemia, disseminated intravascular coagulation) as these are often multifactorial and complications of malignancy or critical illness rather than of ICIs (which are not myelosuppressive). All cases in VigiBase are self‐reported according to MedDRA terms; additional clinical data regarding diagnostic criteria and toxicity management are not reported. We collected demographic and clinical data including sex, age, cancer type, reporting region, immunotherapy agents administered, time to onset of hematologic toxicity, recovery from hematologic toxicity, concurrent irAEs, fatal outcomes, and year of toxicity reporting.
Results and Discussion
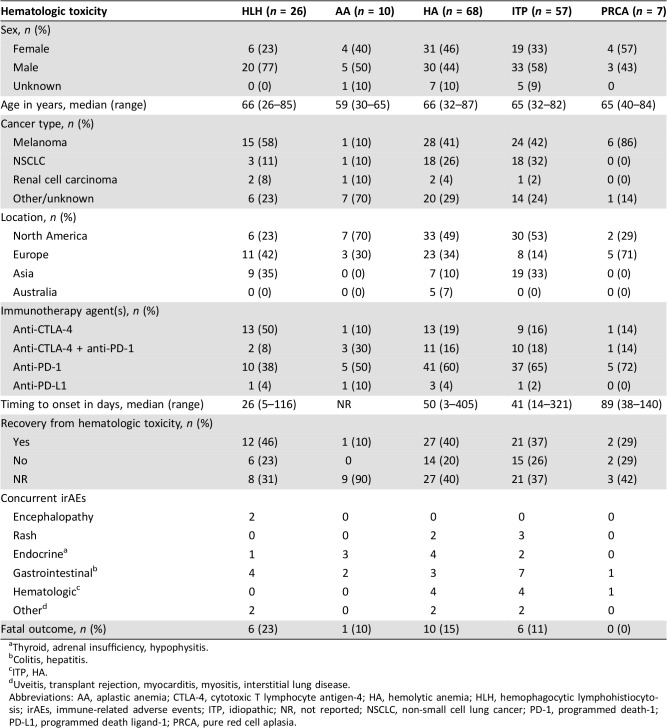
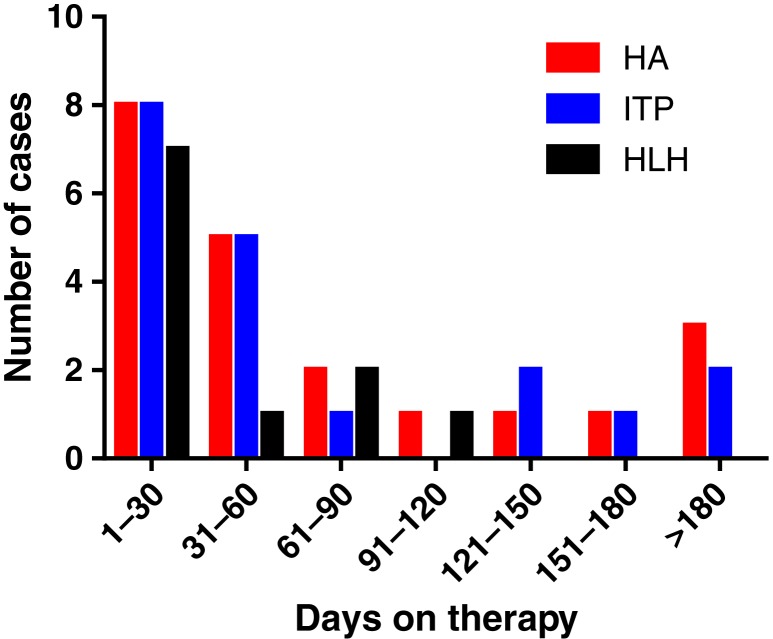
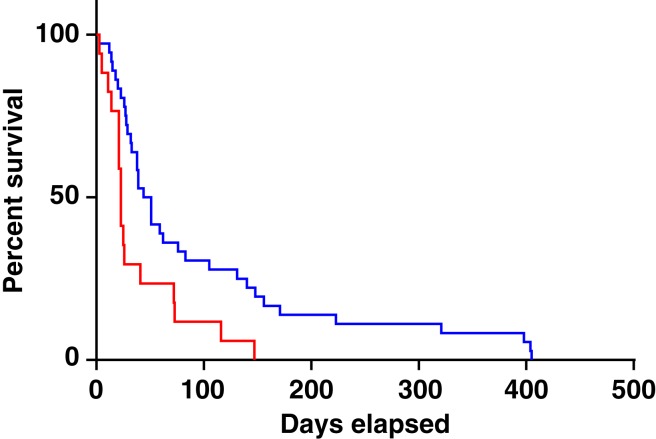
Using these criteria, 168 hematologic toxicities associated with ICIs were identified in 164 ICSRs (Table 1). Of these, 54% of cases occurred in males, and most commonly in melanoma and lung cancer. The median age of onset differed by hematologic toxicity but ranged from 59 to 66 years. Seventy‐six percent of cases were reported from North America and Europe. HA/AIHA (hereafter referred to as “HA”) was the most commonly reported hematologic toxicity (n = 68), followed by ITP (n = 57). Both of these conditions occurred concurrently in four ICSRs. Among all toxicities, the median time to onset was 40 days (range 3–405 days; Fig. 1). Toxicities related to anti‐CTLA‐4‐based therapy (either monotherapy or in combination with anti‐PD‐1) occurred earlier than those associated with anti‐PD‐1/PD‐L1 inhibitors (median 23 vs. 47.5 days, p = .006; Fig. 2).
Table 1. Characteristics of patients with hematologic toxicities.
Thyroid, adrenal insufficiency, hypophysitis.
Colitis, hepatitis.
ITP, HA.
Uveitis, transplant rejection, myocarditis, myositis, interstitial lung disease.
Abbreviations: AA, aplastic anemia; CTLA‐4, cytotoxic T lymphocyte antigen‐4; HA, hemolytic anemia; HLH, hemophagocytic lymphohistiocytosis; irAEs, immune‐related adverse events; ITP, idiopathic; NR, not reported; NSCLC, non‐small cell lung cancer; PD‐1, programmed death‐1; PD‐L1, programmed death ligand‐1; PRCA, pure red cell aplasia.
Figure 1.
Number of cases of hematologic toxicity by time on therapy. Time to development of toxicity based upon hematologic toxicity.
Abbreviations: HA, hemolytic anemia; HLH, hemophagocytic lymphohistiocytosis; ITP, immune thrombocytopenic purpura.
Figure 2.
Time to development of hematologic toxicity by therapy. Time to development of toxicity related to anti‐cytotoxic T lymphocyte antigen‐4 (CTLA‐4)‐based therapy (either monotherapy or in combination with anti‐programmed death‐1 [PD‐1]) versus anti‐PD‐1/programmed death ligand‐1 inhibitors. Red line: CTLA‐4; Blue line: PD‐1.
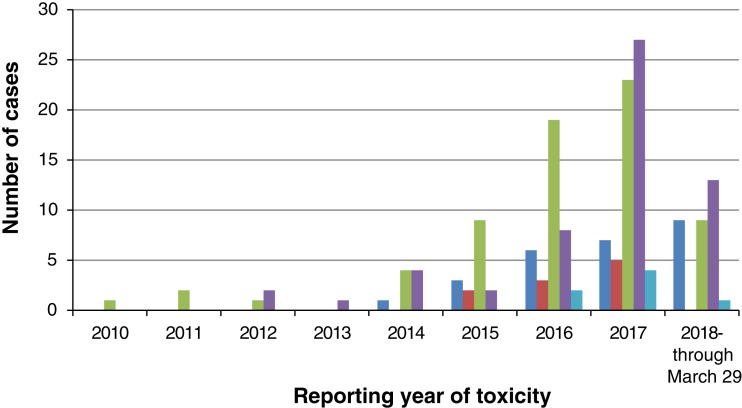
Toxicities were nonoverlapping with the exception of four ICSRs with ITP and concurrent HA, consistent with Evan's syndrome. There was also one patient who developed both PRCA and warm AIHA [2]. Concurrent, nonhematologic irAEs occurred in 23% of these patients. We also noted an increased number of cases of hematologic toxicity reported since 2017, as there were 98 cases between January 2017 and March 2018 versus 70 cases prior to January 2017 (Fig. 3). This may be attributed to increased use of ICIs as well as improved recognition of toxicities.
Figure 3.
Reporting year of hematologic toxicity. Dark blue: hemophagocytic lymphohistiocytosis; Red: aplastic anemia; Green: hemolytic anemia; Purple: immune thrombocytopenic purpura; Light blue: pure red cell aplasia.
We then evaluated individual hematologic toxicities. HA was the most common hematologic toxicity reported, although this database did not distinguish between warm and cold AIHA. Most cases in our study were associated with anti‐PD‐1/PD‐L1 treatment and occurred at a median of 50 days (range 3–405 days). Fatality was reported in 15% of HA cases; although definitive causality of HA (vs. other toxicities vs. cancer) cannot be definitively established based on VigiBase reporting. ITP, the second most common toxicity, occurred at a median of 41 days but also varied widely (range 14–321 days). Death was reported in 11% of cases.
HLH, an uncommon but previously described and potentially fatal hematologic disorder [8], [9], [10], was also reported in 26 cases. HLH can be triggered by underlying malignancy but has also been described as complicating ICIs. T‐cell activation may play a role in the development of HLH [11] and may explain this association. In contrast to other hematologic toxicities, most cases complicated CTLA‐4‐based regimens rather than anti‐PD‐1/PD‐L1 (58% vs. 34%; p = .02) Furthermore, HLH occurred earlier (median 26 days) and had a numerically higher rate of fatalities (23%; 6 of 26 cases) than with other hematologic toxicities. In 19% of cases in our study, concomitant Epstein‐Barr virus infection was reported, suggesting a potential augmented immune response in the setting of a chronic underlying infection. AA and PRCA occurred uncommonly (10 and 7 cases, respectively), mostly from anti‐PD‐1 therapy, and were associated with a single fatality.
There are a variety of hematologic conditions that have been associated with ICIs. Although the specific mechanisms of hematologic irAEs are not known, several studies have suggested that activated T cells and potentially removal of immune checkpoints may play a role in the pathogenesis of these hematologic disorders outside the context of ICI [11], [12], [13]. Further detailed mechanistic studies to explore the triggers and pathogenesis of hematologic irAEs are needed, and may give broader insights into the broader nature of these events. Understanding the etiology of abnormal blood counts can be challenging given confounding effects of chronic disease and prior treatment. A thorough hematologic work‐up potentially including bone marrow biopsy should be undertaken. There is no standard treatment for immune‐mediated hematologic toxicities. It is reasonable to start prednisone 1–2 mg/kg daily for severe hematologic toxicities along with transfusion support as needed. Similar to other immune‐mediated toxicities, steroids are generally tapered over 4–6 weeks.
Conclusion
Although this is, by far, the largest characterization of hematologic irAEs arising from ICIs, there are limitations to our study. First, the absolute frequency of hematologic toxicities cannot be assessed because VigiBase does not capture the number of individuals exposed to a given drug. Second, missing data in some cases precludes definitive characterization of demographic and clinical features. For example, it is important to define the diagnostic criteria for hematologic conditions to truly understand their frequency and to derive optimal management strategies. Also, database reporting is voluntary; thus, not all data fields are included in every report. This also may result in underestimation of the number of hematologic side effects, as many cases likely go unreported. Here, we excluded conditions such as pancytopenia and neutropenic fever from our report as it is not clear that immunotherapy agents alone result in these conditions and confounding factors may contribute. Ultimately, this study demonstrates that hematologic toxicities from ICIs occur fairly early on therapy, have regimen‐specific patterns, and may result in life‐threatening consequences. Future studies should focus on elucidating patient‐specific risk factors for development of these events and on describing optimal management strategies.
Acknowledgments
The supplied data from VigiBase come from a variety of sources. The likelihood of a causal relationship is not the same in all reports. The information does not represent the opinion of the World Health Organization. This study was supported by The Cancer ITMO of the French National Alliance for Life and Health Sciences (AVIESAN): “Plan Cancer 2014‐2019” (J.E.S., B.L.V.) by NIH/NCI K23 CA204726 (D.B.J.), the James C. Bradford Jr. Melanoma Fund (D.B.J.), and the Melanoma Research Foundation (D.B.J.), NIH/NHLBI K23 HL138291 (P.B.F.).
Author Contributions
Conception/design: Elizabeth J. Davis, Douglas B. Johnson
Provision of study material or patients: Joe‐Elie Salem, Kristin K. Ancell
Collection and/or assembly of data: Elizabeth J. Davis, Joe‐Elie Salem, Douglas B. Johnson
Data analysis and interpretation: Elizabeth J. Davis, Joe‐Elie Salem, Arissa Young, Jennifer R. Green, P. Brent Ferrell, Kristin K. Ancell, Benedicte Lebrun‐Vignes, Javid J. Moslehi, Douglas B. Johnson
Manuscript writing: Elizabeth J. Davis, Joe‐Elie Salem, Arissa Young, Jennifer R. Green, P. Brent Ferrell, Kristin K. Ancell, Benedicte Lebrun‐Vignes, Javid J. Moslehi, Douglas B. Johnson
Final approval of manuscript: Elizabeth J. Davis, Joe‐Elie Salem, Arissa Young, Jennifer R. Green, P. Brent Ferrell, Kristin K. Ancell, Benedicte Lebrun‐Vignes, Javid J. Moslehi, Douglas B. Johnson
Disclosures
Elizabeth J. Davis: Five Prime, Genentech, Bristol‐Myers Squibb, Incyte (RF); P. Brent Ferrell: Incyte (RF); Javid J. Moslehi: Pfizer, Bristol‐Myers Squibb, Novartis (C/A), Pfizer, Bristol‐Myers Squibb (RF); Douglas B. Johnson: Array, Bristol‐Myers Squibb, Incyte, Merck, Novartis (C/A), Bristol‐Myers Squibb, Incyte (RF). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Kong BY, Micklethwaite KP, Swaminathan S et al. Autoimmune hemolytic anemia induced by anti‐PD‐1 therapy in metastatic melanoma. Melanoma Res 2016;26:202–204. [DOI] [PubMed] [Google Scholar]
- 2.Nair R, Gheith S, Nair SG. Immunotherapy‐associated hemolytic anemia with pure red‐cell aplasia. N Engl J Med 2016;374:1096–1097. [DOI] [PubMed] [Google Scholar]
- 3.Palla AR, Kennedy D, Mosharraf H et al. Autoimmune hemolytic anemia as a complication of nivolumab therapy. Case Rep Oncol 2016;9:691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwab KS, Heine A, Weimann T et al. Development of hemolytic anemia in a nivolumab‐treated patient with refractory metastatic squamous cell skin cancer and chronic lymphatic leukemia. Case Rep Oncol 2016;9:373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tardy MP, Gastaud L, Boscagli A et al. Autoimmune hemolytic anemia after nivolumab treatment in Hodgkin lymphoma responsive to immunosuppressive treatment. A case report. Hematol Oncol 2017;35:875–877. [DOI] [PubMed] [Google Scholar]
- 6.Shiuan E, Beckermann KE, Ozgun A et al. Thrombocytopenia in patients with melanoma receiving immune checkpoint inhibitor therapy. J Immunother Cancer 2017;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindquist M. VigiBase, the WHO global ICSR database system: Basic facts. Ther Innov Regul Sci 2008;42:409–419. [Google Scholar]
- 8.Satzger I, Ivanyi P, Langer F et al. Treatment‐related hemophagocytic lymphohistiocytosis secondary to checkpoint inhibition with nivolumab plus ipilimumab. Eur J Cancer 2018;93:150–153. [DOI] [PubMed] [Google Scholar]
- 9.Malissen N, Lacotte J, Du‐Thanh A et al. Macrophage activation syndrome: A new complication of checkpoint inhibitors. Eur J Cancer 2017;77:88–89. [DOI] [PubMed] [Google Scholar]
- 10.Shah D, Shrestha R, Ramlal R et al. Pembrolizumab associated hemophagocytic lymphohistiocytosis. Ann Oncol 2017;28:1403. [DOI] [PubMed] [Google Scholar]
- 11.Ammann S, Lehmberg K, Zur Stadt U et al. Primary and secondary hemophagocytic lymphohistiocytosis have different patterns of T‐cell activation, differentiation and repertoire. Eur J Immunol 2017;47:364–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosokawa K, Muranski P, Feng X et al. Memory stem T cells in autoimmune disease: High frequency of circulating CD8+ memory stem cells in acquired aplastic anemia. J Immunol 2016;196:1568–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollinger MK, Giudice V, Cummings NA et al. PD‐1 deficiency augments bone marrow failure in a minor‐histocompatibility antigen mismatch lymphocyte infusion model. Exp Hematol 2018;62:17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]