Abstract
In 2012, the provincial cancer agency in Alberta initiated a provincial quality improvement project to develop, implement, and evaluate a provincial navigation program spanning 15 sites across over 600,000 square kilometres. This project was selected for two years of funding (April, 2012–March 31, 2014) by the Alberta Cancer Foundation (ACF) through an Enhanced Care Grant process. A series of articles has been created to capture the essence of this quality improvement project, the processes that were undertaken, the standards developed, the educational framework that guided the orientation of new navigator staff, and the outcomes that were measured. This first article in the series focuses on establishing the knowledge base that guided the development of this provincial navigation program and describing the methodology undertaken to implement the program across 15 rural and isolated urban cancer care delivery sites. The second article in this series will delve into the educational framework that was developed to guide the competency development and orientation process for the registered nurses who were hired into the newly developed cancer patient navigator roles. The third and final article will explore the outcomes that were achieved through this quality improvement project culminating with a discussion section highlighting key learnings, adaptations made, and next steps underway to broaden the scope and impact of the provincial navigation program.
INTRODUCTION
Developing, implementing, and evaluating a provincial navigation program spanning 15 sites across over 600,000 square kilometres is no small feat, but that is what was undertaken within the Alberta provincial cancer agency. Work on this provincial quality improvement project began in April 2012, and is ongoing. However, the grant-funded portion of the work was from 2012–2014 and is the focus of this series of articles. Capturing the essence of this program work, the processes that were undertaken, the standards developed, the educational framework that guided the orientation of new navigator staff, and the outcomes that were measured in the initial two-year grant-funded project required the development of a series of articles.
The intention of this series of articles is to share the learnings gleaned from the multiple stages of this project with others who may be considering the implementation of a similar program. As well, these articles will contribute to the knowledge base regarding the impact that a cancer patient navigator program such as this can have on the patient experience, team functioning, care coordination, and health system utilization.
In this first article, the focus is on describing the knowledge base that guided the development of the navigation program and the methodology undertaken to implement the program across 15 rural and isolated urban cancer care delivery sites. The second article will delve into the educational framework that was developed to guide the competency development and orientation for registered nurses who were hired into the newly developed cancer patient navigator roles. The third and final article will explore the outcomes that were achieved through this quality improvement project culminating with a discussion section highlighting key learning, adaptations made, and the next steps underway to broaden the scope and impact of the provincial navigation program.
BACKGROUND
Cancer patient navigation can be defined as a “proactive, intentional process of collaborating with a person and his or her family to provide guidance, as they negotiate the maze of treatments, services and potential barriers throughout the cancer journey” (Canadian Partnership Against Cancer [CPAC], 2012, p. 5). The central concept within this definition includes an individual (navigator) being available to support a patient at any point throughout his or her cancer journey. Patients have reported that the continuity of their relationship with a navigator, being able to access one resource person at any point throughout their cancer journey, and being able to discuss whatever concerns they have is valuable (Hébert & Fillion, 2011; Pedersen & Hack, 2010; Skrutkowski, Saucier, Ritchie, Tran, & Smith, 2011; Walsh et al., 2011).
The concept of navigation originated in the United States, in 1990, when Dr. Harold P. Freeman founded the first patient navigation program in Harlem, New York. The original program targeted improving navigation support to low socioeconomic status, African American women with breast cancer to eliminate barriers to early diagnosis and timely treatment (Freeman, Muth, & Kerner, 1995). This initial project produced dramatic improvements in mortality amongst participants, increasing five-year survival rates from 39% to 70% (Freeman, 2013). Since then, cancer patient navigation programs have evolved in scope and application, to improve care for patients of all socioeconomic and ethnically diverse backgrounds and may be found at specific points or across the entire cancer journey (Freeman, 2013; McMullen, 2013; Wilcox & Bruce, 2010).
Although navigation has existed in some form for more than 25 years, variations remain within navigation models. Navigator roles may be fulfilled by lay people, including cancer survivors, as well as health care professionals, such as social workers and nurses, and may possess differing levels of education and training (Wells et al., 2008). Additionally, navigation roles may be designed with different parameters such as specialized navigation roles focused on supporting patients with a specific cancer type, or a particular population of patients such as young adults or aboriginals. There are also generalist navigation roles with a geographical scope of responsibility, designed to ensure all patients in their catchment areas have equitable access to services, or navigation roles that are focused on supporting patients at a specific timepoint on their cancer journey, such as a survivorship navigator (Thomas & Peters, 2014).
Navigation is recognized as an effective strategy and key enabler to enhancing the delivery of person-centred care as navigators promote the delivery of individualized care and support (CPAC, 2012). Currently the majority of navigation programs in Canada focus on patients who are newly diagnosed, have complex needs, or who are from rural and remote communities (CPAC, 2012). Cancer patient navigation programs have been shown to influence system efficiencies through improved continuity and coordination of care and facilitating timely access to services, thus improving the overall patient experience of care (CPAC, 2012; Fillion et al., 2012; McMullen, 2013). In addition to these system benefits, numerous studies have shown direct benefits to patient outcomes such as decreasing patient reported anxiety, enabling patient access to the right service at the right time, empowering patients to self-manage and cope with their diagnosis, and self-reports of patients’ feeling better prepared for consultations and treatments (CPAC, 2012; Fillion et al., 2012). The four key themes regarding patient needs addressed by improved navigation supports are emotional, practical and informational, family, and other complex needs (Lorhan et al., 2014).
A diagnosis of cancer is always an unexpected and challenging event for patients and families (Fitch, 2008). However, those who live in rural and isolated urban centres face additional challenges in accessing and coordinating care. Often, patients must travel significant distances to access specialized care. As well, their home community may have a limited number of health care providers with oncology expertise and knowledge (Cantril & Haylock, 2013). Research has demonstrated that rural patients who are followed by a navigator experience statistically significantly less distress after being connected to a navigator (Swanson & Koch, 2010).
In Canada, the first provincial professional navigation programs emerged in the early 2000s in the provinces of Nova Scotia and Quebec (Fillion et al., 2012). Since then, numerous navigation programs have been initiated across the country and by 2011, every province and one territory in Canada had instituted some type of professional cancer patient navigator supports (CPAC, 2012; Pedersen & Hack, 2010). Nationally, these roles have most often been taken on by oncology nurses (CPAC, 2012).
In Alberta, work towards a navigation program began in 2006 with an initial provincial needs assessment (Miller, 2006). This process involved focus groups with cancer patients and survivors, as well as a Delphi survey with health professionals, health care leaders, volunteers, and patient advocates. Based on the cumulative findings of this needs assessment, a provincial cancer patient navigation framework was developed. As approximately one third of Albertans live outside of the major cities of Calgary and Edmonton (Finance Alberta, 2015), and as the needs assessment highlighted numerous unmet needs in the rural areas, a decision was made to focus efforts to implement cancer patient navigation in the 15 community oncology settings (11 community cancer centres [CCCs] and four regional cancer centres [RCCs]). A pilot project which tested the impact of adding a part-time cancer patient navigator to one RCC and two CCC sites was undertaken in 2007. In 2008, based on strong positive evaluation results, a recommendation was made to expand the cancer patient navigator program to include navigator support at all community and regional cancer centres (AHS, 2008).
Due to provincial health care restructuring in Alberta at that time, moving the recommendation forward was not possible. However, in 2012, through the generous support of the Alberta Cancer Foundation (ACF) a proposal to implement the cancer patient navigator role in all CCCs and RCCs was selected for funding. In alignment with the provincial goal of creating a comprehensive and coordinated cancer care system (AHS, 2013), the goals for this newly formed cancer patient navigation program included enhancing integration with primary care; improved access for rural patients to psychological, physical and supportive care services; and developing a strong cancer workforce to meet the needs of cancer patients and their families, specifically in rural and isolated urban areas of Alberta.
PROJECT METHODOLOGY
This project was designed as a continual quality improvement (QI) project, as the core goal of the project was to implement the navigation role into the existing clinical environment at each setting and evaluate its impact. The implementation guide for cancer patient navigation developed by the Canadian Partnership Against Cancer (CPAC, 2012) was utilized as a guiding document, as it is well established that successful QI requires a comprehensive and effective change management strategy (Langley, Moen, Nolan, Nolan, Norman, & Provost, 2009).
The implementation strategy included several key elements including: a current state review, provincial program coordination and standards, co-design of the navigation role with cancer care operational leaders, development and utilization of a standardized training and coaching program, identification of barriers in each setting with associated strategies to manage them, and the development of program metrics. As per the QI methodology, the approach for optimizing the navigator role once implemented included routine small-scale, site-specific Plan, Study, Do, Act (PSDA) cycles (Langley et al., 2009). This project complied with the Helsinki Declaration (World Medical Association, 2008) and the Alberta Research Ethics Community Consensus Initiative (ARECCI) ethics guidelines for quality improvement and evaluation (ARECCI, 2012). A project screen established by ARECCI identified this project as within the scope of QI and waived the need for a full REB review. No harm was anticipated or actually reported in relation to this project.
Hiring a program coordinator/educator
The provincial scope, fixed timeline, and the need for rigorous evaluation necessitated the creation of a program coordinator/educator to manage the day to day aspects of program development, implementation planning, creation of an orientation program, and to support navigators in their roles’ development, role integration, and ongoing professional development. Due to population distribution and diverse geographical locations, individual navigators would be practising in isolated locations across the province. Provincial oversight and guidance was required to ensure that similar practice standards and role parameters existed across sites and to conduct the evaluation of impact of the role. Therefore, the first project activity was the creation of a job description for a project coordinator/educator with subsequent recruitment. Role requirements included being a registered nurse with a strong oncology knowledge base, preferably Master’s prepared, with teaching, project management, evaluation planning, and change management experience. Once hired, the program coordinator/educator began conducting a current state assessment and literature review.
Establishing a standard navigation role description
A review of literature regarding navigation, current navigation programs within the province, as well as consultation with other provincial navigation programs across Canada provided an understanding of the scope and function of navigation roles, both provincially and nationally. Based on this review and input from key operational stakeholders, the overall vision for the navigator program and role in Alberta was established. A standard job description was developed, which outlined the scope and function of the role, as well as the corresponding aptitude and skill set necessary to be successful in the role. Key elements of the provincial standardized role description revolved around the navigation competency framework, which defined cancer patient navigation as a bi-dimensional role. Competency development was required in two areas: facilitation of continuity of care, including informational, management, and relational continuity; and promotion of patient and family empowerment, including facilitating active coping, cancer self-management skills, and delivering supportive care (Fillion et al., 2012). Once the standardized role description was vetted with operational management and provincial Human Resources, the standardized scope and description allowed for the development of a provincial orientation program.
Developing the navigation orientation curriculum
The development of an orientation framework was facilitated by previous provincial work initiated in 2006, in which a Cancer Patient Navigation course had been developed. This course consisted of eight modules: 1. Introduction—history and benefits of patient navigation, 2. Effective and compassionate communication, 3. Culturally competent patient care, 4. Assessing patient needs, 5. Navigating patients to resources and support, 6. Managing stress and avoiding burnout, 7. Documentation and, 8. Toolkit (Dozois, 2010). With further direction and understanding of the navigator role now being offered by the more recently developed navigation national competency framework described above (Cook et al., 2013; Fillion et al., 2012) several modules were updated, and several new learning modules were added to further enhance navigators’ competency development and knowledge base. These included how to utilize the provincial EMR for navigation documentation, the inclusion of cultural safety in the module on providing culturally competent care, and how to conduct resource mapping within their catchment areas. The modules were used to deliver the key content in the navigator orientation through self-study, group review, and facilitated discussions. Part 2 in this series of articles will delve more deeply into the structure, content and facilitated learning within the provincial navigation orientation framework.
Recruitment and hiring
The program team worked closely with site managers to interview and hire navigators at each RCC and CCC. The decision was made that all navigators would report to their local manager, and the primary function of the program team would be to support the development, integration, standardization, evaluation, and ongoing professional development of nurses in the navigator roles across sites. As the program team could not orientate all 15 navigators simultaneously, a staggered hiring process was established with the site manager group. Approximately four sites per month recruited and hired their navigators, resulting in a cohort of four navigators to orientate monthly. In this way, all 15 navigator positions were filled within four months. This staggered hiring approach allowed the new navigators to form cohesive groups where collective learning, problem solving, and professional growth were facilitated. It also allowed the program staff to conduct multiple PSDA cycles to continually improve the navigation orientation.
Whenever possible, navigators were recruited from existing site oncology teams, as these nurses were already familiar with their local community, had established relationships with local health care providers, and were familiar with what supports and services were available. Because the cancer care sites recruiting for navigators were based in rural and isolated urban areas, some managers found it challenging to recruit experienced oncology nurses to these roles. When navigators were hired without previous oncology experience, additional efforts were taken to support these candidates due to the steep learning curve. Partnering the navigator with the oncology nursing education team to establish a baseline of oncology knowledge, as well as extending their practicum in the clinic setting prior to taking on the navigator orientation were both strategies utilized to support this cohort. However, even with these additional efforts, it was quickly discovered that navigators hired from existing oncology teams were more likely to stay in the role and required less time for orientation. During the course of this project, 20 navigators were hired and orientated, with 15 of those having oncology experience. Five navigators left their roles in the first year of the program, three of which had no previous oncology experience. The two experienced oncology nurses who left their navigation roles in that same year did so because they moved out of the community.
Delivering the orientation
Orientation was led by the coordinator/educator and included both lecture, self-study modules, and online learning. Due to geographic distance, the majority of orientation was done virtually through videoconferencing with the new staff doing self-study prior to the group discussions. In the first few cohorts of new navigators, some orientation was done face to face or in small groups but, as the orientation became more refined and established, more and more content was delivered via videoconferencing. Depending on location, each navigator also had the opportunity to visit either the North Tertiary Cancer Centre in Edmonton or the South Tertiary Cancer Centre in Calgary. It was important for navigators to establish connections with key resources at these sites and to understand the journey their patients would undergo should they need to have components of their treatment at these sites.
As access to oncology-specific providers and resources is often limited in smaller communities, supporting the navigator to build a network of local, non-cancer-specific providers and services who were able and willing to support cancer patients and their families closer to home, was an essential part of role development. As part of their orientation, each navigator was supported to conduct an environmental scan of providers, resources, and supports in their geographical area of responsibility, with the final step of their orientation process being to host a community stakeholder presentation. This provided an additional opportunity for community and health care partners to learn about the new navigation role in their community and for new collaborations to be formed between community partners, cancer care teams, and health care providers outside of the cancer system. Community stakeholders included community- or hospital-based social workers, hospital inpatient managers, primary care physicians, chaplains, family services, home care, palliative care, dietitians, physiotherapists, aboriginal case managers, mental health workers, and non-for-profit community agencies such as the Canadian Cancer Society.
Role implementation
Creating a standardized navigator role description was essential. However, it was recognized that an important element of success of this provincial program was the ability to tailor each role to the local and geographical context, population base, cultural groups, resources accessible, and practice setting. As part of the initial implementation planning, local site managers were consulted to better understand both the centre in which the navigator would be based and some of the unique needs of the population and communities for which they would be caring. Some facilities already had specialized oncology social workers as part of the clinical teams. In those sites, understanding how the navigator role would interface and collaborate daily with this social worker role was important. Other smaller centres had remote access to an oncology social worker via telephone or telehealth, which required a different approach to collaboration. Addressing this important collaboration upfront allowed for management strategies to be developed that minimized role confusion and managed overlapping functions between roles.
The provincial project team supported role implementation in several ways. The first was by travelling to sites to co-present with the local navigator to the clinical teams about the new navigator role. During these site visits smaller meetings were also conducted with the site manager and key supportive care team members, such as the site social worker, nurse practitioners, and the navigators. These meetings allowed for discussion about role clarity, scope, effective strategies for collaboration, and shared care to occur. The project coordinator/educator also set up individual weekly meetings with all navigators for the first three months of their role development/implementation and monthly teleconference meetings for the navigation team, as a whole. These structured meetings allowed for mentorship, collective learning, and reinforced provincial standards. In addition to these structured supports the coordinator/educator was available to the navigators on an as-needed basis to support problem solving and complex care coordination issues. In this way, the coordinator/educator acted as a navigator for the navigators. As the program has matured and navigators have begun to move from novice towards expert (Benner, Tanner, & Chesla, 2009), establishing a peer preceptorship/mentorship relationship between new navigators and more experienced navigators within the program became feasible (Watson, Raffin, Melnick, & Whyte, 2012). As it is challenging to take on a new role, especially a role that is not already established or well understood by the clinical team, supporting individual navigators with their role development and integration of their role in their local site was a core activity of the program team.
Communication planning
In an effort to increase the visibility of the navigator role and program, the provincial project team developed provincial brochures, posters, and promotional letters with information about navigation that could be used by navigators to promote awareness of their role within their community settings. Information about cancer patient navigation was also integrated into patient orientation and chemotherapy teaching classes. A webpage was created on the external Alberta Health Services (AHS) site that lists the navigators, what they do, where they are located, and how they can be accessed (AHS, 2015). Several formal navigation communications were created to facilitate provincial awareness of the program. For example, the navigation program was featured in the Alberta Cancer Foundation annual report (ACF, 2015) and in an Alberta Health Services communications media release at the end of March 2013. This media release included a number of news stories about the program airing on television, radio, and in a variety of newspapers across the province (AHS, 2013). Additionally, the program team presented to various groups and connections were made to ensure key strategic partners including tumour triage and first contact programs; Aboriginal, Métis and Inuit health; and primary care, to ensure all stakeholders were aware of the navigation program and how they could access the support for their cancer patients.
Practice standards
To ensure consistent practice across sites, as well as to facilitate continuity of care across providers and sites, practice standards for all navigators within the program were established. One key standard developed was that all navigation documentation was to be completed electronically using the cancer-specific electronic medical record (EMR). Standardized documentation tools were created within the EMR to facilitate easy identification of navigation interventions to other providers. Documentation tools also provided guidelines for new navigators regarding the components of a navigation assessment and provided a way to support standard practice across sites. As this was a QI project, program metrics were also required to show the impact of navigation interventions and evaluate outcomes. Within the EMR, a navigation workload measurement tool was created that, when completed by the navigator, would capture the number of unique patients cared for by the navigator, the number of visits required for each patient, the mode of connection with the patient, what navigation interventions were enacted, and the timepoint in the cancer journey the care was delivered. Connecting this workload to the EMR also meant the program team was able to collect basic aggregate demographic data and distinguish each community’s unique data to identify trends. The workload reports also acted as a quality improvement tool, as monthly reports generated through the EMR provided a snapshot of the navigator’s work in each community and allowed for the identification of areas in practice where PDSA cycles of improvement could be targeted.
The workload and documentation tools evolved significantly over the course of the initial grant-funded project. As navigators began to use the tools, and workload data began to accumulate, revisions were made to ensure usability for the providers and that data captured were useful and meaningful to the program’s overall goals. Involving the navigators in these PSDA cycles was essential, as it reinforced that the project team valued their contribution, allowing them to identify what data points were meaningful to represent their work. This collaborative work also ensured that navigators understood why data were being collected. This process of review and engagement also served to improve utilization of the workload measurement tool because when the navigators saw their own data presented back and compared their data to other sites, they were more motivated to ensure their data accurately represented their work and contributions to patient care.
Professional development support
After initial work to integrate the navigator role was completed in each site, the program team’s focus shifted to understanding what structures were needed to support ongoing education and professional development for continued competency development in the highly skilled navigator team. Due to the isolated nature of their work, an important element of ongoing professional development has been a virtual Community of Practice established and jointly facilitated by the navigation program’s coordinator/educator and by a specialized oncology social worker. The navigator team continues to meet monthly to discuss practice issues, share resources, and find solutions to common challenges they faced across the province. This also provides a consistent venue for other programs to present relevant provincial information to the navigator team.
At the onset of the QI project it was clear that the navigators were not the only oncology providers with a navigation function in their role. To support ongoing professional development and cross-provider connections, an annual provincial care coordination forum was established. This annual forum consists of two days, the first of which focuses on providing opportunity for the provincial navigator group and provincial social work teams to meet within their professional groups to discuss issues revolving around their program standards and profession-specific topics of interest in person. The second day is an inter-professional day where the two provincial groups and other professionals involved in care coordination/navigation of cancer patients explore larger common issues such as conducting difficult conversations, integrating palliative care, developing cultural competencies, role clarity, and improving team collaboration. This annual face-to-face care coordination meeting has been pivotal to creating connections and role clarity across disciplines both within the cancer system and beyond.
Evaluation
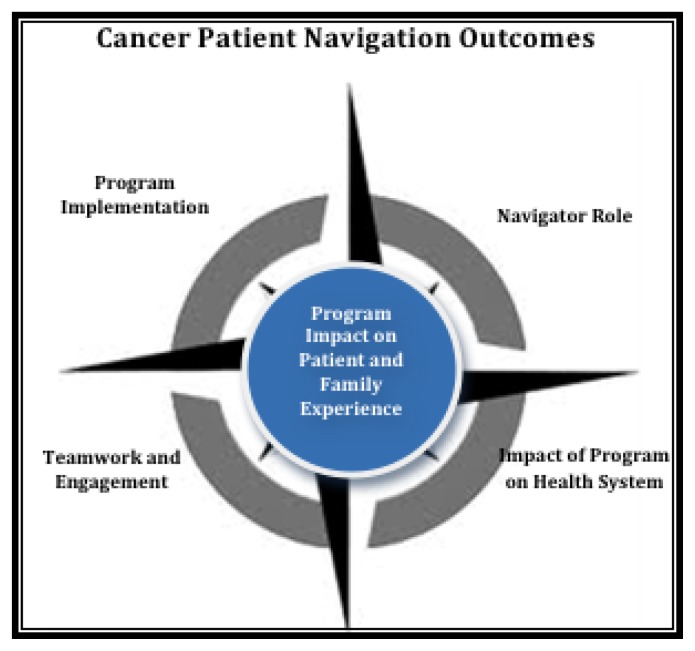
As the initial project was grant-funded and there was a requirement to demonstrate how this program enhanced care coordination, impacted the patient and family experience and the health care system overall, a robust evaluation strategy was developed. The evaluation focused on five key outcomes: patient and family experience, effectiveness of program design and implementation, success of the navigation orientation framework, impact on teamwork and engagement, and the influence of this program on health system utilization and functioning (see Figure 1). The third and final article in this series will explore the outcomes that were achieved through this quality improvement project and will culminate with a discussion section highlighting key learnings, adaptations made to the program, and next steps underway to broaden the scope and impact of the program.
Figure 1.
Model of Key Outcomes
CONCLUSION
In 2012, the provincial cancer care agency in Alberta undertook a daunting task to develop, implement, and evaluate the impact of a provincial navigation program spanning 15 isolated urban cancer care delivery centres. In order to achieve this goal, a provincial plan was required, followed by a robust implementation phase. The focus of this article was to describe the knowledge base that guided the development of this navigation program and the methodology undertaken to implement the program across all sites. Much collective learning has occurred in the process of undertaking this work. It is hoped that through sharing the learnings achieved from the multiple stages of this project with others who are considering the implementation of a similar program, they will have a more informed starting place to begin their program planning and development, thus leveraging health system transformation forward. The next article in this series will delve more deeply into the structure, content, and facilitated learning processes within the provincial navigation orientation framework. The third and final article will report on the findings from the program evaluation and demonstrate how these findings add to the knowledge base regarding the impact that a cancer patient navigation program can have on the patient experience, team functioning, care coordination, and health system utilization.
Footnotes
This manuscript was written on the basis of the presentation offered as the Helene Hudson Lectureship at the annual conference of the Canadian Association of Nursing in Oncology held in Toronto, 2015.
REFERENCES
- Alberta Cancer Foundation (ACF) Annual Progress Report. 2015. Retrieved from http://albertacancer.ca/progress-report/spring-2015/patient-navigators.
- Alberta Health (AH) Changing our future: Alberta’s cancer plan to 2030. 2013. Retrieved from http://www.health.alberta.ca/documents/Cancer-Plan-Alberta-2013.pdf.
- Alberta Health Services (AHS) Evaluation Report: Provincial cancer patient navigation demonstration project. 2008. Internal document, AHS [Google Scholar]
- Alberta Health Services (AHS) Media release: Cancer patient navigators lend a helping hand. 2013. Retrieved from http://www.albertahealthservices.ca/news/releases/2013/Page8182.aspx.
- Alberta Health Services (AHS) Cancer Patient Navigation and Tumour Triage Resources. 2015. Retrieved from http://www.albertahealthservices.ca/info/service.aspx?id=1025354.
- Alberta Research Ethics Community Consensus Initiative (ARECCI) ARECCI guidelines for quality improvement and evaluation projects. 2012. Retrieved from http://www.aihealthsolutions.ca/initiatives-partnerships/arecci-a-project-ethics-community-consensus-initiative/ [PMC free article] [PubMed]
- Benner P, Tanner C, Chesla C. Expertise in nursing practice: Caring, clinical judgment and ethics. New York, NY: Springer; 2009. [Google Scholar]
- Canadian Partnership Against Cancer (CPAC) Navigation: A guide to implementing best practices in person-centred care. 2012. Retrieved from http://www.cancerview.ca/idc/groups/public/documents/webcontent/guide_implement_nav.pdf.
- Cantril C, Haylock PJ. Patient navigation in the oncology care setting. Seminars In Oncology Nursing. 2013;29(2):76–90. doi: 10.1016/j.soncn.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Cook S, Fillion L, Fitch MI, Veillette AM, Matheson T, Aubin M, Rainville F. Core areas of practice and associated competencies for nurses working as professional cancer navigators. Canadian Oncology Nursing Journal/Revue canadienne de soins infirmiers en oncologie. 2013;23(1):44–52. doi: 10.5737/1181912x2314452. [DOI] [PubMed] [Google Scholar]
- Dozois E. Alberta Health Services (AHS) Cancer Patient Navigation Course. 2010. Internal AHS document [Google Scholar]
- Fillion L, Cook S, Veillette A, Aubin M, de Serres M, Rainville F, Doll R. Professional navigation framework: Elaboration and validation in a Canadian context. Oncology Nursing Forum. 2012;39(1):58–69. doi: 10.1188/12.ONF.E58-E69A. [DOI] [PubMed] [Google Scholar]
- Finance Alberta. Alberta Population Projections by Census Divisions, 2015–2041. 2015. Retrieved from http://finance.alberta.ca/aboutalberta/population-projections/2015-2041-alberta-populationprojections.pdf.
- Fitch M. Supportive care framework. Canadian Oncology Nursing Journal/Revue canadienne de soins infirmiers en oncologie. 2008;18(1):6–14. doi: 10.5737/1181912x181614. [DOI] [PubMed] [Google Scholar]
- Freeman H. The history, principles, and future of patient navigation: Commentary. Seminars in Oncology Nursing. 2013;29(2):72–75. doi: 10.1016/j.soncn.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Freeman H, Muth B, Kerner J. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Practice. 1995;3(1):19–30. [PubMed] [Google Scholar]
- Hébert J, Fillion L. Gaining a better understanding of the support function of oncology nurse navigators from their own perspective and that of people living with cancer: Part 1. Canadian Oncology Nursing Journal. 2011;21(1):33–38. doi: 10.5737/1181912x2113338. [DOI] [PubMed] [Google Scholar]
- Langley G, Moen R, Nolan K, Nolan T, Norman C, Provost L. The Improvement Guide: A Practical Approach to Enhancing Organisational Performance. San Francisco, CA: Jossey Bass; 2009. [Google Scholar]
- Lorhan S, Dennis D, van der Westhuizen M, Hodgson S, Berrang T, Daudt H. The experience of people with lung cancer with a volunteer-based lay navigation intervention at an outpatient cancer center. Patient Education & Counseling. 2014;96(2):237–248. doi: 10.1016/j.pec.2014.05.002. [DOI] [PubMed] [Google Scholar]
- McMullen L. Oncology nurse navigators and the continuum of cancer care. Seminars In Oncology Nursing. 2013;29(2):105–117. doi: 10.1016/j.soncn.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Miller J. Cancer patient navigation needs assessment: Project report. 2006. Alberta Cancer board: Medical Affairs and Community Oncology Division, Internal Document [Google Scholar]
- Pedersen A, Hack T. Pilots of oncology health care: A concept analysis of the patient navigator role. Oncology Nursing Forum. 2010;37(1):55–60. doi: 10.1188/10.ONF.5560. [DOI] [PubMed] [Google Scholar]
- Skrutkowski M, Saucier A, Ritchie JA, Tran N, Smith K. Intervention patterns of pivot nurses in oncology. Canadian Oncology Nursing Journal. 2011;21(4):218–222. doi: 10.5737/1181912x214218222. [DOI] [PubMed] [Google Scholar]
- Swanson J, Koch L. The role of the oncology nurse navigator in distress management of adult inpatients with cancer: A retrospective study. Oncology Nursing Forum. 2010;37(1):69–76. doi: 10.1188/10.ONF.69-76. [DOI] [PubMed] [Google Scholar]
- Thomas M, Peters E. Setting-Specific Navigation. In: Blaseg K, Daughtery P, Gamblin K, editors. Oncology nurse navigation: Delivering patient-centered care across the continuum. Pittsburgh, PA: Oncology Nursing Society; 2014. [Google Scholar]
- Walsh J, Young J, Harrison J, Butow P, Solomon M, Masya L, White K. What is important in cancer care coordination? A qualitative investigation. European Journal of Cancer Care. 2011;20(2):220–227. doi: 10.1111/j.1365-2354.2010.01187.x. [DOI] [PubMed] [Google Scholar]
- Watson L, Raffin S, Melnick A, Whyte D. Designing and implementing an ambulatory oncology nursing peer preceptorship program: Using grounded theory research to guide program development. Nursing Research and Practice. 2012 doi: 10.1155/2012/451354.. Article ID 451354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, … &, Raich PC. Patient navigation: State of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox B, Bruce S. Patient navigation: A “win-win” for all involved. Oncology Nursing Forum. 2010;37(1):21–25. doi: 10.1188/10.ONF.21-25. [DOI] [PubMed] [Google Scholar]
- World Medical Association (WMA) Declaration of Helsinki: Ethical principles for medical research involving human subjects. 2008. Retrieved from http://www.wma.net/en/30publications/10policies/b3/17c.pdf. [PubMed]