There is no statistically significant association between methylation in the promoter region of the serotonin transporter gene (SLC6A4) and amygdala activation during negative emotion processing in individuals with alcohol dependence or healthy controls.
Abstract
Aims
Differences in DNA methylation of the serotonin transporter gene (SLC6A4) have been shown to alter SLC6A4 expression and predict brain functions in healthy individuals. This study investigated the association between SLC6A4 promoter methylation and threat-related amygdala activation in individuals with alcohol dependence (AD).
Methods
Methylation of the SLC6A4 promoter region was assessed using peripheral blood DNA from 45 individuals with AD and 45 healthy controls (HCs). All participants completed an emotional face matching task in a 3-T magnetic resonance imaging (MRI) scanner.
Results
Results did not reveal any association between SLC6A4 promoter methylation variation and threat-related amygdala activation in HCs or individuals with AD. Furthermore, methylation in the promoter region of SLC6A4 did not significantly differ between the groups.
Conclusions
Our results do not replicate a previous finding that increased methylation in the promoter region of SLC6A4 is associated with threat-related amygdala activation in healthy individuals and further show that there is no such association in individuals with AD. Given that the number of imaging epigenetics studies on SLC6A4 is very limited to date, these inconsistent results indicate that future research is needed to clarify its association with amygdala reactivity in both healthy and clinical populations.
INTRODUCTION
Alcohol use disorder (AUD) affects 15.1 million Americans 18 years and older (SAMHSA, 2015). This chronic disorder is defined by compulsive alcohol use, tolerance to its effects, and the development of negative affective states during withdrawal (Koob, 2014). Both genetic and environmental factors contribute to the complex etiology of AUD, with heritability ranging from 40 to 70% (Kendler et al., 2012; Rietschel and Treutlein, 2013). Despite this large genetic component, the identification of genes involved in the pathophysiology of AUD has been challenging, in part due to the complex mode of inheritance, small effect size of putative genes, multiple genes or functional networks involved and clinical heterogeneity.
One approach to dissect this clinical heterogeneity is to focus on endophenotypes or clinical subdomains, such as negative affect (e.g. anxiety, depressive symptoms or anhedonia) and negative emotion processing in AUD. The gene encoding the serotonin transporter (SERT, 5-HTT), SLC6A4, is one of the most prominent and studied candidate genes involved in mood and affect regulation (Hariri and Holmes, 2006; Lohoff, 2010; Thompson and Kenna, 2016). The SERT mediates presynaptic reuptake of serotonin, thus determining the duration and magnitude of serotonin signaling. Genetic variation in the promoter region of SLC6A4, including the serotonin-transporter-linked polymorphic region (5-HTTLPR) polymorphism, has been shown to affect the gene’s transcriptional rate both in vitro and in vivo (Lesch et al., 1996; Pezawas et al., 2005). Moreover, 5-HTTLPR has been demonstrated to have functional relevance for fear and anxiety-related behaviors in functional magnetic resonance imaging (fMRI) studies, where carriers of the short allele showed increased amygdala activity in response to aversive stimuli compared to individuals with two long alleles (Smolka et al., 2007; Murphy et al., 2013). This may be relevant to AUD as studies on the neurobiology of AUD have found that altered amygdala activation and integrity in conjunction with altered corticolimbic emotion regulation may contribute to the negative reinforcement aspects of alcohol craving, as well as future relapse (Koob and Le Moal, 2008; Wrase et al., 2008). Given the amygdala’s crucial involvement in the processing of fearful stimuli (Phan et al., 2002) and emotional distress (van Marle et al., 2009), altered amygdala reactivity and consequently altered corticolimbic top-down regulation may contribute to compulsive drinking behavior through negative reinforcement mechanisms. However, despite initial evidence for a role of the 5-HTTLPR, several replication studies have resulted in inconsistent findings and recent meta-analyses have concluded that other factors, such as epigenetic modulation, may play an important role that requires further research (Murphy et al., 2013; Bastiaansen et al., 2014, 2015; Kaufman, 2015).
The field of epigenetics is rapidly developing in AUD and might help explain some of the environmental components as they interact with the genetic architecture (Schuebel et al., 2016; Palmisano and Pandey, 2017; Lohoff et al., 2018). There is increasing evidence that chronic alcohol use may alter gene expression in neurons through changes in DNA methylation (Zhang and Gelernter, 2017). While research on the role of epigenetic regulation of SLC6A4 in amygdala reactivity is still limited, one study found that DNA methylation was associated with differences in SLC6A4 mRNA expression and in vivo amygdala function. That is, Nikolova et al. (2014) showed that increased promoter methylation correlated with increased threat-related amygdala reactivity in healthy individuals, as measured by blood oxygen level-dependent (BOLD) fMRI. Interestingly, these epigenetic effects were greater than, and independent of the 5-HTTLPR polymorphism. Therefore, further research on the association between methylation and amygdala reactivity is needed, particularly in clinical populations, such as AUD patients, as epigenetic mechanisms adaptively regulate gene expression in response to environmental influences, such as alcohol use or stress (Jirtle and Skinner, 2007). While some studies have shown differential SLC6A4 methylation in major depressive disorder, where higher promoter methylation correlated with family history of depression and more severe depressive symptoms, little is known about the role of SLC6A4 methylation in AUD (Kang et al., 2013; Zhao et al., 2013). Investigating the role of SLC6A4 methylation in AUD will improve our understanding of functional mechanisms of altered emotion processing in AUD and might uncover new treatment targets.
In this study, we investigated SLC6A4 promoter methylation variation in individuals with alcohol dependence (AD) and healthy controls (HCs). First, we hypothesized that methylation in the SLC6A4 promoter would be associated with threat-related amygdala activation in the HCs but that this relationship would significantly differ in individuals with AD. Second, we hypothesized that methylation levels in the SLC6A4 promoter would be significantly different in AD cases compared to HCs.
METHOD
Participants
Ninety individuals with AD and HCs (45 each, mean age = 39.78, SD = 11.33) provided written informed consent in compliance with the Declaration of Helsinki and the Institutional Review Board of the National Institutes of Health (NIH)/National Institute on Alcohol Abuse and Alcoholism (NIAAA). Detailed information about the sample and recruitment can be found elsewhere (Muench et al., 2018). For sample demographics and characteristics, see Table 1. All participants underwent the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 1995). Exclusion criteria included left-handedness, pregnancy, claustrophobia, or significant neurological or medical diagnoses, as determined by a history and physical exam. While other drug dependence diagnoses were not exclusionary, it should be noted that only one participant met DSM-IV criteria for cannabis and cocaine dependence. Excluding this participant’s data did not affect the results, therefore, they were included in the analyses reported here. All participants were free from any psychotropic medications on the day of the fMRI scan.
Table 1.
Demographics and characteristics of the sample
| Alcohol-dependent subjects N = 45 | Healthy controls N = 45 | P-value | |
|---|---|---|---|
| Gender, N (%) | |||
| Male | 35 (77.8) | 22 (48.9) | 0.004 |
| Female | 10 (22.2) | 23 (51.1) | |
| Age, mean years (SD) | 43.25 (10.73) | 36.30 (10.94) | 0.003 |
| Ethnicity, N (%) | |||
| Black/African American | 24 (53.3) | 18 (40.0) | 0.088 |
| European American | 17 (37.8) | 16 (35.6) | |
| Asian | 0 (0.0) | 6 (13.3) | |
| Multiracial | 1 (2.2) | 3 (6.7) | |
| Unknown | 3 (6.7) | 2 (4.4) | |
| Smokers, N (%) | 26 (57.8) | 0 (0.0) | <0.0001 |
| Average number of drinking days in past 90 days, mean (SD) | 69.60 (25.19) | 18.76 (16.08) | <0.0001 |
| Number of heavy drinking days in past 90 days, mean (SD) | 59.49 (30.65) | 2.42 (7.19) | <0.0001 |
| Average number of drinks per drinking day, mean (SD) | 13.11 (8.84) | 1.80 (1.78) | <0.0001 |
| Montgomery–Asberg Depression Score, mean (SD) | 12.13 (10.21) | 0.87 (1.67) | <0.0001 |
| Any Anxiety Disorder—Current N, (%) | 8 (9.0) | 1 (1.1) | 0.010 |
| Any Anxiety Disorder—Lifetime N, (%) | 11 (12.4) | 1 (1.1) | 0.002 |
| Generalized Anxiety Disorder—Current | 3 (3.4) | 1 (1.1) | 0.030 |
| Generalized Anxiety Disorder—Lifetime N, (%) | 3 (3.4) | 1 (1.1) | 0.030 |
| Posttraumatic Stress Disorder—Current N, (%) | 2 (2.3) | 0 (0.0) | 0.150 |
| Posttraumatic Stress Disorder—Lifetime N, (%) | 2 (2.3) | 0 (0.0) | 0.150 |
| Any Mood Disorder—Current N, (%) | 5 (5.6) | 0 (0.0) | 0.020 |
| Any Mood Disorder—Lifetime N, (%) | 10 (11.2) | 8 (9.0) | 0.560 |
| Major Depressive Disorder—Current N, (%) | 3 (3.4) | 0 (0.0) | 0.070 |
| Major Depressive Disorder—Lifetime N, (%) | 9 (10.1) | 8 (9.0) | 0.750 |
Note: SD = standard deviation. Boldface indicates significant differences between cases and controls.
Additional exclusion criteria for the HC group included positive urine drug screens or alcohol breathalyzer on the day of the scan, as well as any DSM-IV-TR diagnosis of current or past AD. There were no alcohol abstainers in this group.
All participants completed the Face Matching task (a modified version of the Fearful Faces task, Hariri et al., 2002) in a 3-T MRI scanner, as well as the Timeline Followback (TLFB) interview, a measure of alcohol consumption over the previous 90 days (Sobell and Sobell, 1992), and the Montgomery–Asberg Depression scale (MADRS) (Svanborg and Åsberg, 1994), a measure of depressive symptoms.
Face matching task
All participants were administered a Face Matching task (Hariri et al., 2002). Participants were presented with a target picture at the top of the screen and two pictures at the bottom of the screen and asked to identify which picture at the bottom matched the target picture via button press. Pictures belonged to one of the following six categories: angry faces, sad faces, fearful faces, happy faces, neutral faces and geometric shapes. The task consisted of two interleaved blocks of each picture category. Each block started with a 2-s display of instructions that indicated the task (i.e. ‘match shapes’ vs. ‘match faces’). Each block was 30 s long and consisted of six images from the same category, shown for five seconds each. There was no inter-stimulus interval, and there was an equal number of male and female faces.
MRI data acquisition and preprocessing
A Siemens 3-T Skyra scanner (Siemens Medical Solutions USA, Inc., Malvern, PA) was used to obtain structural (MPRGE) and functional neuroimaging data. Functional scans were obtained using an echoplanar-imaging pulse sequence (TR: 2000 ms, TE: 30 ms, flip angle: 90°, FOV: 24 × 24 cm2, 38 mm slice thickness, 36 slices, multi-slice mode: interleaved). Presentation® software (Version 19.0, Neurobehavioral Systems, Inc., Berkeley, CA, www.neurobs.com) was used to present the Face Matching task. Analysis of Functional NeuroImages (AFNI) version 5 (Cox et al., 2015) was used to process each subject’s fMRI data. Following removal of the first three repetition times (TRs) from each time course, AFNI’s 3dDespike was used to smooth spikes in signal over time course, and detrend and interpolate time series to shift time courses for each voxel to be aligned with the same temporal origin. Next, each time series’ volumes were aligned to the base volume and to the participant’s skull-stripped anatomy. Subsequently, AFNI’s 3dAllineate was employed to transform the volumes into the standardized Talairach and Tournoux space (Talairach and Tournoux, 1988). Images were smoothed with a 4-mm full-width half-maximum Gaussian kernel, and motion parameters and their derivates were regressed to eliminate movement-associated variance. For the Face Matching task data, stimulus onset times were regressed to detect the signal that was associated with each of the conditions prior to motion regression, and TRs with motion derivatives of 0.3 or greater were excluded from further analysis. All individual masks and registrations underwent visual inspection to verify quality.
BOLD fMRI data and region of interest analyses
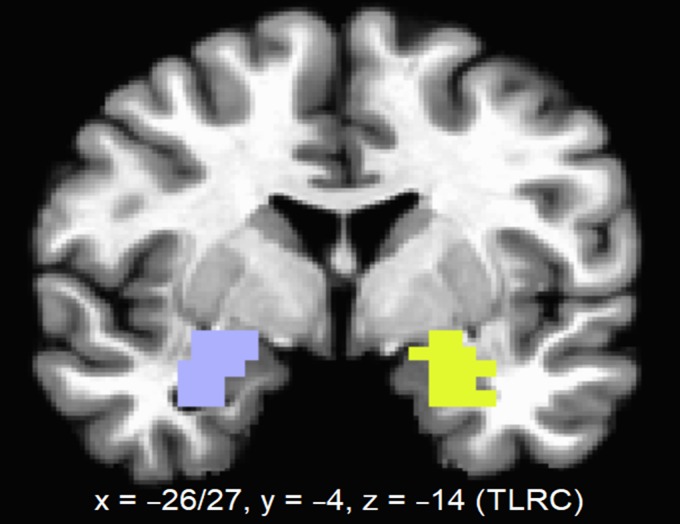
Single-subject level analyses on BOLD responses were performed based on the experimental condition blocks and contrast of interest. The contrast of interest was [Angry + Fearful] > Shapes. Beta values corresponding to the contrast of interest in the regions of interest (ROI) were extracted for each subject. The ROIs were left and right amygdala. These were extracted using AFNI’s 3Dmask_tool. See Fig. 1 for an image of the ROIs used.
Fig. 1.
Amygdala regions of interest (ROIs).
DNA extraction and methylation analysis
The National Institute on Alcohol Abuse and Alcoholism Laboratory of Neurogenetics used the Illumina OmniExpress BeadChip (Illumina, San Diego, CA) to extract ancestry informative markers for the purpose of calculating ancestral proportions for all participants. Ancestry scores for six ethnic factors (Africa, Europe, Asia, Far East Asia, Oceania, and Americas) were calculated for each subject using a panel of 2500 ancestry informative markers present on the Illumina array by Structure, version 2.2 (https://web.stanford.edu/group/pritchardlab/structure.html) that performs individual comparison to the CEPH Diversity panel of 1051 subjects from 51 worldwide populations (http://www.cephb.fr/en/hgdp_panel.php) (Wiers et al., 2018). Given the ethnic distribution of the present sample (see Table 1), AIM scores for Africa, Europe and Asia were used as covariates in the main regression analysis.
For DNA methylation analysis, blood samples were obtained from all participants and genomic DNA was extracted using the QIAamp DNA Blood Maxi Kit (Qiagen, Santa Clarita, CA). DNA methylation levels of 37 CpG sites in the promoter region of SLC6A4 were measured using quantitative bisulfite pyrosequencing by EpigenDx (Hopkinton, MA) following standard EpigenDx protocols. Specifically, 500 ng of genomic DNA was treated with bisulfite using EZ DNA methylation kits (Zymo Research, Inc., Irvine, CA), purified following the manufacturer’s protocol, and eluted to a volume of 46 μL. Next, polymerase chain reaction (PCR) was conducted with 1 μL of bisulfite-treated DNA and 0.2 μM of each primer. One of the primers was biotin-labeled and purified with high performance liquid chromatography (HPLC) to achieve purification of the final PCR product with Sepharose beads. After the resulting PCR products were bound to Streptavidin Sepharose High Performance (GE Healthcare Life Sciences, Marlborough, MA), they were purified, washed and denatured with a 0.2 μM NaOH solution. Subsequently, the Pyrosequencing Vacuum Prep Tool (Pyrosequencing, Qiagen, Gaithersburg, MD) was used for rewashing in accordance with the manufacturer’s protocol. After 5 μM of sequencing primer was annealed, 10 μL of the resulting PCR products were sequenced by Pyrosequencing on the PSQ96 HS System (Pyrosequencing).
Methylation status of each CpG site was assessed using QCpG software (Pyrosequencing) and determined as an artificial C/T single nucleotide polymorphism (SNP). Methylation levels were computed by dividing the percentage of the methylated alleles by the total number of alleles (methylated and unmethylated). For quality control purposes, non-CpG cytosines were included as internal controls in each experiment to reveal incomplete bisulfite conversion of the input DNA, and additional samples of low, medium, and high methylated DNA were included to serve as controls in each PCR. Lastly, PCR bias testing was conducted by combining unmethylated control DNA with in vitro methylated DNA at different ratios (0%, 5%, 10%, 25%, 50%, 75%, 100%) and performing bisulfite modification, PCR and Pyrosequencing analysis.
Five SLC6A4 assays were employed to analyze 37 CpG dinucleotides across the gene ranging from −1532 to 203 base pairs from the TSS, based on Ensembl Transcript ID ENST00000261707. Ten CpG sites where more than 40% of samples showed zero percent methylation were excluded from further analysis. Consequently, 27 CpG sites were analyzed, 15 of which coincided with the 20 CpG sites examined in the study by Nikolova et al. (2014). Supplementary Table S1 provides detailed information on the location of all 37 CpG sites, including their genomic location and position relative to the translational start codon (ATG) and TSS following Genome Reference Consortium Human Build 38 (GRCh38/hg38), as well as mean methylation and the number of participants with 0% methylation for both groups. When comparing the present study’s data to the original study, it should be noted that CpG site data from Nikolova et al. (2014) follows Genome Reference Consortium Human Build 37 [GRCh37/hg19].
Statistical analysis
A personal computer-based statistical software package (IBM SPSS Statistics® 20, IBM Corp., Armonk, NY) was used to perform all statistical analyses. Differences on demographic variables were examined using t-tests for continuous variables and chi-square tests for categorical variables. As a dimension reduction approach, principal component analysis was carried out to estimate principal component scores (PCS) accounting for the observed correlation among methylation at SLC6A4 promoter CpG sites and summarizing the maximum variability among them. The top PCS was used for further analysis.
The main outcome measure in the present study was unilateral amygdala activation as measured by BOLD fMRI during the presentation of angry and fearful faces in the Face Matching task. This contrast was chosen to be consistent with Nikolova et al. (2014). Fearful and angry facial expressions are considered to indicate an ecologically valid threat, therefore, amygdala responses to fearful and angry facial expressions are hereafter referred to as threat-related amygdala activation (Carré et al., 2013). Shapiro–Wilk tests showed normal distributions for BOLD responses to fearful and angry faces in the left (P = 0.830) and right (P = 0.112) amygdala. For the main analysis, a linear regression model was used to test associations between the first PCS of promoter methylation and threat-related amygdala BOLD responses in both groups while controlling for age, gender and AIM scores for European, Asian, and African ancestry. Next, linear regression models were used to investigate associations between the percentage of methylation at individual CpG sites in the SLC6A4 promoter region and unilateral threat-related amygdala BOLD responses in both groups while controlling for age, gender and AIM scores. Between-group differences in regression slopes for the AD and HC groups were tested by including interaction terms (group × PC1/SLC6A4 CpG site) in the regression models. To examine differences in overall SLC6A4 methylation, defined as the average percentage of methylated cytosines, and differences in amygdala BOLD responses, one-way analyses of covariance (ANCOVAs) were conducted. Given prior reports of associations between age and methylation (Muench et al., 2018), as well as between gender and methylation (Philibert et al., 2008), these ANCOVAs included age and gender as covariates. Statistical significance was set at P < 0.05 (two-tailed) for all analyses. Analyses were adjusted for multiple comparisons using the Benjamini–Hochberg procedure. Specifically, the Benjamini–Hochberg procedure was applied across CpG sites within each hemisphere.
RESULTS
Association between serotonin transporter gene methylation and threat-related amygdala activation
The top PCS captured 36% of the methylation variance among all 27 CpG locations in the promoter with a robust eigenvalue of 9.66. A linear regression model was used to examine associations between the top PCS and amygdala BOLD responses in both groups while controlling for age, gender and AIM scores. Analyses found that the top PCS was not significantly associated with amygdala BOLD responses in the left (P = 0.434) or the right hemisphere (P = 0.942). There was no significant group × PC1 interaction effect in the left (P = 0.498) or right (P = 0.999) amygdala.
Next, linear regression analyses were employed to examine associations between SLC6A4 CpG site methylation and threat-related amygdala activation while controlling for age, gender and AIM scores (Table 2). Analyses showed that promoter methylation of the serotonin transporter gene did not correlate with amygdala activation in response to fearful and angry faces in either group (AD and HC). There were no significant group × SLC6A4 CpG site methylation interaction effects in the left (all Ps ≥ 0.085) or the right (all Ps ≥ 0.103) hemisphere. It should be noted that methylation at two CpG sites (CpG site 14 and CpG site 23) was initially associated with threat-related amygdala activation in the left hemisphere. However, these associations did not survive correction for multiple comparisons (CpG site 14: adjusted P = 0.621; CpG site 23: adjusted P = 0.621). Furthermore, average methylation across all 27 CpG sites was not associated with amygdala BOLD responses in the right or left hemisphere.
Table 2.
Summary of results from linear regression models predicting amygdala activation from group, percentage methylation at each of the 27 individual CpG sites, and their interaction term while controlling for age, gender and ancestry informative markers
| CpG Site | CpG ID | Distance to TSS | Left amygdala | Right amygdala | ||
|---|---|---|---|---|---|---|
| b | P-value | b | P-value | |||
| 1 | 311 | −1532 | −0.016 | 0.916 | −0.061 | 0.695 |
| 2 | 312 | −1525 | −0.021 | 0.886 | −0.136 | 0.379 |
| 3 | 313 | −1519 | −0.051 | 0.738 | −0.139 | 0.381 |
| 4 | 299 | −1061 | 0.152 | 0.361 | −0.104 | 0.548 |
| 5 | 298 | −1059 | −0.050 | 0.767 | −0.142 | 0.415 |
| 6 | 297 | −1057 | −0.072 | 0.664 | −0.221 | 0.194 |
| 7 | 296 | −1046 | −0.101 | 0.501 | −0.052 | 0.736 |
| 8 | 295 | −1030 | 0.210 | 0.145 | 0.230 | 0.125 |
| 9 | 294 | −1022 | 0.268 | 0.069 | 0.247 | 0.106 |
| 10 | 293 | −994 | 0.070 | 0.632 | 0.047 | 0.755 |
| 11 | 291 | −977 | 0.053 | 0.709 | −0.051 | 0.727 |
| 12 | 272 | −200 | −0.119 | 0.540 | 0.155 | 0.438 |
| 13 | 252 | 59 | 0.102 | 0.527 | 0.132 | 0.426 |
| 14 | 251 | 63 | 0.310 | 0.040 | 0.097 | 0.541 |
| 15 | 250 | 65 | 0.188 | 0.228 | 0.175 | 0.282 |
| 16 | 249 | 72 | 0.085 | 0.603 | −0.206 | 0.223 |
| 17 | 248 | 77 | −0.010 | 0.945 | −0.012 | 0.936 |
| 18 | 247 | 82 | −0.061 | 0.686 | −0.199 | 0.206 |
| 19 | 246 | 84 | 0.198 | 0.200 | 0.189 | 0.239 |
| 20 | 245 | 98 | −0.027 | 0.894 | −0.080 | 0.706 |
| 21 | 244 | 102 | 0.124 | 0.420 | 0.084 | 0.598 |
| 22 | 243 | 117 | 0.115 | 0.463 | −0.144 | 0.380 |
| 23 | 239 | 133 | 0.282 | 0.050 | 0.004 | 0.978 |
| 24 | 236 | 160 | −0.071 | 0.639 | 0.137 | 0.378 |
| 25 | 235 | 173 | −0.022 | 0.885 | 0.127 | 0.420 |
| 26 | 234 | 200 | 0.072 | 0.632 | −0.111 | 0.473 |
| 27 | 233 | 203 | −0.103 | 0.495 | −0.011 | 0.946 |
Note: Boldface indicates significance. Negative numbers in the distance to TSS column indicate that the CpG site is located downstream of the transcriptional start site (TSS), while positive numbers indicate that the CpG site is located upstream of the TSS.
Group differences in serotonin transporter methylation and threat-related amygdala activation
Analyses controlling for age and gender showed no significant differences between the AD and HC group on threat-related amygdala activation (left amygdala: F(1,86) = 1.74, P = 0.191; right amygdala: F(1,86) = 1.09, P = 0.299) or average methylation across the 27 CpG sites examined in this study (F(1,86) = 0.91, P = 0.342). Furthermore, analyses comparing the AD and HC group on age- and gender-adjusted single CpG site methylation found no significant differences (data not shown).
DISCUSSION
This case–control study investigated the relationship between methylation variation in the promoter region of the SLC6A4 gene and amygdala activation during negative emotion processing in individuals with AD and HCs. Results did not reveal any association between SLC6A4 promoter methylation variation and threat-related amygdala activation in healthy individuals or those with AD. Furthermore, methylation in the promoter of SLC6A4 did not significantly differ between groups.
Our results do not replicate the previous finding by Nikolova et al. (2014) that increased methylation in the promoter region of SLC6A4 was associated with amygdala activation in healthy individuals. Two additional studies have found associations between SLC6A4 promoter methylation and amygdala reactivity to negative emotional stimuli in healthy adolescents and adults (Frodl et al., 2015; Swartz et al., 2017). Our discrepant finding may be due to clinical heterogeneity in our HC population, such as presence of early life stress or anxiety levels. In addition, it should be noted that the present study’s sample was ethnically mixed with only 33 Caucasian participants (16 HC and 17 AD; see Table 1), while participants in the prior study by Nikolova et al. (2014) were of European ancestry only. While we did control for ancestry informative markers in our analyses, the power to detect associations that may only be present in individuals of European ancestry might have been reduced. Future studies in larger, well-balanced samples are needed to investigate this association in individuals of different ancestries. Furthermore, future studies should consider that several additional factors affect threat-related amygdala reactivity, including multiple serotoninergic genes, environmental factors, and corticolimbic neurocircuitry (Fisher and Hariri, 2012; Kaufman, 2015). However, a more recent study reported an interaction effect of methylation of the retrotransposonal Alu element (AluJb) in the SLC6A4 promoter region and major depressive disorder on right amygdala responsiveness to emotional faces but no association between amygdala reactivity and methylation among HCs (Schneider et al., 2018), which is consistent with the present study. Given that the number of imaging epigenetics studies on SLC6A4 is very limited to date, these inconsistent results indicate that future research is needed to clarify its association with amygdala reactivity in both healthy and clinical populations.
There was no significant difference in age- and gender-adjusted SLC6A4 overall or single CpG site methylation levels between AD cases and controls. This is consistent with a previous study that found no difference in methylation at 7 SLC6A4 CpG sites in 27 AD cases and 15 controls (Park et al., 2011). In contrast, preclinical data has shown brain region-specific effects of prenatal alcohol exposure, including increased SLC6A4 mRNA expression in the hippocampus, as well as increased SLC6A4 methylation (upstream of a putative TSS) and decreased mRNA expression in the hypothalamus (Ngai et al., 2015). Furthermore, a clinical study found altered SLC6A4 methylation levels in newborns of mothers who were drinking lightly before or during pregnancy (Lee et al., 2015). These mixed findings on the association between alcohol use and SLC6A4 methylation may be explained by methodological differences, a lack of power due to the small sample sizes in the present study and Park et al. (2011), or the fact that methylation varies at different CpG sites. Taken together, these findings indicate that epigenetic variation in the SLC6A4 promoter might be affected by alcohol exposure and that multiple CpG sites may work in concert to contribute to the pathogenesis of AUD, with each single CpG site contributing only a small effect to the clinical phenotype. Further research is required to improve our understanding of how alcohol use affects methylation at different SLC6A4 CpG sites and how these changes relate to alcohol-related phenotypes. In addition, studies with individuals at different stages of AUD might contribute to a deeper insight into epigenetic methylation dynamics at SLC6A4 CpG sites.
Some limitations in this study should be noted. First, our study may have lacked statistical power to detect the possibly small effect size of SLC6A4 CpG site methylation on threat-related amygdala reactivity. Based on our sample size of 90, we had a power of 78% with a moderate effect size (R2 = 0.3) and Bonferroni-corrected alpha (0.05/54), indicating that there is a possibility of false negatives due to a lack of power. Second, AD cases and controls were not well matched for smoking status (i.e. current smokers vs. non-smokers) with a smoking rate of 57.8% in AD cases and 0% in controls. However, an ANCOVA controlling for age and gender showed that there was no difference in threat-related amygdala activation between smokers and non-smokers in the AD group [left amygdala: F(1,41) = 2.04, P = 0.161; right amygdala: F(1,41) = 0.04, P = 0.843]. Nevertheless, future studies in samples balanced for smoking status are needed that might also examine other potential confounds, such as diet, exercise, and circadian rhythms. Furthermore, heterogenous blood cell types between participants could have confounded methylation levels. It should be noted that we used targeted pyrosequencing to examine 37 CpG sites only. Therefore, we were unable to employ deconvolution algorithms, which require genome-wide methylation data, to adjust for cell type heterogeneity. Finally, as it was not possible to directly measure methylation levels in the brain, we used DNA extracted from peripheral blood samples. However, a recent study has reported a strong correlation between mean methylation levels in the blood and brain (= 0.90; Horvath et al., 2012). While blood-brain correlations of methylation levels vary across different brain regions, methylation in promoter CpG island sites has been shown to be largely conserved across brain tissue and blood from the same individuals (Davies et al., 2012). For the serotonin transporter gene, associations between peripheral SLC6A4 promoter methylation and in vivo serotonin synthesis in the orbitofrontal cortex, as well as correlations between SLC6A4 methylation in peripheral blood leukocytes and postmortem amygdala tissue have been reported (Wang et al., 2012; Riese et al., 2014), supporting the potential of peripheral tissues, such as blood, to serve as proxies for methylation levels in neural tissues. Importantly, blood samples are easily obtainable and could thus be collected repeatedly to track changes in epigenetic variation prior to detoxification and after varying periods of abstinence. This approach could greatly improve our understanding of epigenetic mechanisms in AUD. Lastly, age and gender were included as covariates in all analyses because cases and controls were not well matched for these variables.
In summary, our study did not replicate a previous finding of an association between SLC6A4 methylation and threat-related amygdala activation in healthy individuals and further showed that there was no such association in individuals with AD. Moreover, there was no significant difference in SLC6A4 promoter methylation levels between individuals with and without AD. However, given the small number of available studies on neuroimaging epigenetics studies of SLC6A4 in clinical and healthy populations, future research is needed. The continued exploration of the role of epigenetic mechanisms, such as DNA methylation and histone acetylation, in disease-related endophenotypes may uncover gene-environment interactions that contribute to psychopathology, which could lead to more precise treatments for individuals with AUD.
Supplementary Material
FUNDING
This work was supported by the National Institutes of Health (NIH) intramural funding (Grant number ZIA-AA000242 to F.W.L., Section on Clinical Genomics and Experimental Therapeutics and grant number ZIA-AA000125 to R.M., Clinical NeuroImaging Research Core), Division of Intramural Clinical and Biological Research of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), as well as by a grant of the German Research Foundation (Grant number DFG CH1936/1-1 to K.C.).
CONFLICT OF INTEREST STATEMENT
None.
REFERENCES
- Bastiaansen JA, De Vries YA, Munafò MR (2015) Citation distortions in the literature on the serotonin-transporter-linked polymorphic region and amygdala activation. Biol Psychiatry 78:E35–6. [DOI] [PubMed] [Google Scholar]
- Bastiaansen JA, Servaas MN, Marsman JBC, et al. (2014) Filling the gap: relationship between the serotonin-transporter-linked polymorphic region and amygdala activation. Psychol Sci 25:2058–66. [DOI] [PubMed] [Google Scholar]
- Carré JM, Hyde LW, Neumann CS, et al. (2013) The neural signatures of distinct psychopathic traits. Soc Neurosci 8:122–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox SM, Frank MJ, Larcher K, et al. (2015) Striatal D1 and D2 signaling differentially predict learning from positive and negative outcomes. Neuroimage 109:95–101. [DOI] [PubMed] [Google Scholar]
- Davies MN, Volta M, Pidsley R, et al. (2012) Functional annotation of the human brain methylome identifies tissue-specific epigenetic variation across brain and blood. Genome Biol 13:R43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. (1995) Structured Clinical Interview for DSM-IV Axis I Disorders. New York: New York State Psychiatric Institute. [Google Scholar]
- Fisher PM, Hariri AR (2012) Linking variability in brain chemistry and circuit function through multimodal human neuroimaging. Genes Brain Behav 11:633–42. [DOI] [PubMed] [Google Scholar]
- Frodl T, Carballedo A, Vaisheva F, et al. (2015) DNA methylation of the serotonin transporter gene (SLC6A4) is associated with brain function involved in processing emotional stimuli. J Psychiatry Neurosci 40:296–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri AR, Holmes A (2006) Genetics of emotional regulation: the role of the serotonin transporter in neural function. Trends Cogn Sci 10:182–91. [DOI] [PubMed] [Google Scholar]
- Hariri AR, Tessitore A, Mattay VS, et al. (2002) The amygdala response to emotional stimuli: a comparison of faces and scenes. Neuroimage 17:317–23. [DOI] [PubMed] [Google Scholar]
- Horvath S, Zhang Y, Langfelder P, et al. (2012) Aging effects on DNA methylation modules in human brain and blood tissue. Genome Biol 13:R97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jirtle RL, Skinner MK (2007) Environmental epigenomics and disease susceptibility. Nat Rev Genet 8:253–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HJ, Kim JM, Stewart R, et al. (2013) Association of SLC6A4 methylation with early adversity, characteristics and outcomes in depression. Prog Neuropsychopharmacol Biol Psychiatry 44:23–8. [DOI] [PubMed] [Google Scholar]
- Kaufman J. (2015) Reply To: Citation distortions in the literature on the serotonin-transporter-linked polymorphic region and amygdala activation. Biol Psychiatry 78:e37–38. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Chen XN, Dick D, et al. (2012) Recent advances in the genetic epidemiology and molecular genetics of substance use disorders. Nat Neurosci 15:181–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF. (2014) Chapter 3—Neurocircuitry of alcohol addiction: synthesis from animal models In Sullivan EV, Pfefferbaum A (eds). Handbook of Clinical Neurology. Amsterdam, Netherlands: Elsevier, 33–54. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M (2008) Neurobiological mechanisms for opponent motivational processes in addiction. Philos Trans R Soc Lond B Biol Sci 363:3113–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee BY, Park SY, Ryu HM, et al. (2015) Changes in the methylation status of DAT, SERT, and MeCP2 gene promoters in the blood cell in families exposed to alcohol during the periconceptional period. Alcohol Clin Exp Res 39:239–50. [DOI] [PubMed] [Google Scholar]
- Lesch KP, Bengel D, Heils A, et al. (1996) Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274:1527–31. [DOI] [PubMed] [Google Scholar]
- Lohoff FW. (2010) Overview of the genetics of major depressive disorder. Curr Psychiatry Rep 12:539–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohoff FW, Sorcher JL, Rosen AD, et al. (2018) Methylomic profiling and replication implicates deregulation of PCSK9 in alcohol use disorder. Mol Psychiatry 23:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muench C, Wiers CE, Cortes CR, et al. (2018) Dopamine transporter gene methylation is associated with nucleus accumbens activation during reward processing in healthy but not alcohol-dependent individuals. Alcohol Clin Exp Res 42:21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S, Norbury R, Godlewska B, et al. (2013) The effect of the serotonin transporter polymorphism (5-HTTLPR) on amygdala function: a meta-analysis. Mol Psychiatry 18:512–20. [DOI] [PubMed] [Google Scholar]
- Ngai YF, Sulistyoningrum DC, O’Neill R, et al. (2015) Prenatal alcohol exposure alters methyl metabolism and programs serotonin transporter and glucocorticoid receptor expression in brain. Am J Physiol Regul Integr Comp Physiol 309:R613–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolova YS, Koenen KC, Galea S, et al. (2014) Beyond genotype: serotonin transporter epigenetic modification predicts human brain function. Nat Neurosci 17:1153–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmisano M, Pandey SC (2017) Epigenetic mechanisms of alcoholism and stress-related disorders. Alcohol 60:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park BY, Lee BC, Jung KH, et al. (2011) Epigenetic changes of serotonin transporter in the patients with alcohol dependence: methylation of an serotonin transporter promoter CpG island. Psychiatry Investig 8:130–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezawas L, Meyer-Lindenberg A, Drabant EM, et al. (2005) 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci 8:828–34. [DOI] [PubMed] [Google Scholar]
- Phan KL, Wager T, Taylor SF, et al. (2002) Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI. Neuroimage 16:331–48. [DOI] [PubMed] [Google Scholar]
- Philibert RA, Sandhu H, Hollenbeck N, et al. (2008) The relationship of 5HTT (SLC6A4) methylation and genotype on mRNA expression and liability to major depression and alcohol dependence in subjects from the Iowa Adoption Studies. Am J Med Genet B Neuropsychiatr Genet 147:543–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riese H, Van Den Heuvel ER, Snieder H, et al. (2014) Association between methylation of the SLC6A4 promoter region in peripheral blood leukocytes and methylation in amygdala tissue. Psychosom Med 76:244–6. [DOI] [PubMed] [Google Scholar]
- Rietschel M, Treutlein J (2013) The genetics of alcohol dependence. Ann N Y Acad Sci 1282:39–70. [DOI] [PubMed] [Google Scholar]
- Schneider I, Kugel H, Redlich R, et al. (2018) Association of serotonin transporter gene alujb methylation with major depression, amygdala responsiveness, 5-HTTLPR/rs25531 polymorphism, and stress. Neuropsychopharmacology 43:1308–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuebel K, Gitik M, Domschke K, et al. (2016) Making sense of epigenetics. Int J Neuropsychopharmacol 19:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolka M, Bühler M, Schumann G, et al. (2007) Gene–gene effects on central processing of aversive stimuli. Mol Psychiatry 12:307–17. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline Follow-back: a technique for assessing self-reported ethanol consumption In Raye Z, Litten JPA (eds). Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press, 41–72. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2015) 2015 National Survey on Drug Use and Health (NSDUH). Table 5.6B—Substance Use Disorder in Past Year among Persons Aged 18 or Older, by Demographic Characteristics: Percentages, 2014 and 2015 https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm#tab5-6b.
- Svanborg P, Åsberg M (1994) A new self‐rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr Scand 89:21–8. [DOI] [PubMed] [Google Scholar]
- Swartz JR, Hariri AR, Williamson DE (2017) An epigenetic mechanism links socioeconomic status to changes in depression-related brain function in high-risk adolescents. Mol Psychiatry 22:209–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talairach J, Tournoux P (1988) Co-planar Stereotaxic Atlas of the Human Brain: 3-Dimensional Proportional System: An Approach to Cerebral Imaging. Stuttgart; New York: G. Thieme, New York: Thieme Medical Publishers. [Google Scholar]
- Thompson MD, Kenna GA (2016) Variation in the serotonin transporter gene and alcoholism: risk and response to pharmacotherapy. Alcohol Alcohol 51:164–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Marle HJ, Hermans EJ, Qin S, et al. (2009) From specificity to sensitivity: how acute stress affects amygdala processing of biologically salient stimuli. Biol Psychiatry 66:649–55. [DOI] [PubMed] [Google Scholar]
- Wang D, Szyf M, Benkelfat C, et al. (2012) Peripheral SLC6A4 DNA methylation is associated with in vivo measures of human brain serotonin synthesis and childhood physical aggression. PLoS One 7:e39501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiers CE, Towb PC, Hodgkinson CA, et al. (2018) Association of genetic ancestry with striatal dopamine D2/D3 receptor availability. Mol Psychiatry 23:1711–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrase J, Makris N, Braus DF, et al. (2008) Amygdala volume associated with alcohol abuse relapse and craving. Am J Psychiatry 165:1179–84. [DOI] [PubMed] [Google Scholar]
- Zhang H, Gelernter J (2017) Review: DNA methylation and alcohol use disorders: progress and challenges. Am J Addict 26:502–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Goldberg J, Bremner JD, et al. (2013) Association between promoter methylation of serotonin transporter gene and depressive symptoms: a monozygotic twin study. Psychosom Med 75:523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.