Abstract
Objectives
The objective of this study was to assess the impact of endometriosis on the quality of life.
Patients and methods
Study group of 205 women, aged between 18-45 years old, hospitalized in the “Cuza-Voda” Hospital of Iasi, between 2013-2015. We used the Fertility Problem Inventory, the Endometriosis Health Profile and the Beck Depression Inventory.
Results
We first realized a descriptive analyses of patients’ health related quality of life - 60% of women reported higher infertility distress associated with relationship issues caused by difficulties to conceive. The descriptive analysis over the quality of life in patients with endometriosis suggests that the high level of stress related factors, are: the loss over the control of the symptoms, dyspareunia and altered emotional status. Regarding the sexual aspect of life, almost a quarter of the women complained about an altered sexual status, due to both fear of failing in conceiving and dyspareunia caused by the endometriosis. The descriptive analysis over the infertility related stress suggests that the factors associated with a high level of stress are: sadness, pessimism, feeling of failure, irritability, lack of confidence, self-hatred and fatigue.
Conclusions
Patients with endometriosis are dealing daily with a large spectrum of symptoms, including pain, dyspareunia, emotional instability and high levels of stress, which have a negative impact upon the quality of life, by lowering it on different levels. Also, within the present study we showed a significant presence of high infertility stress in patients of all ages that lead to depression and social anxiety.
Keywords: endometriosis, infertility, patient questionnaire, psychological involvement, quality of life
INTRODUCTION
Endometriosis (EM) is a condition characterised by the implantation of endometrial stroma and glands outside the uterus, mainly on the ovaries and peritoneum (1-3), by this, inducing a chronic inflammatory reaction. What exactly triggers this process is not fully known and understood until this point, in spite all the years of research regarding the matter, endometriosis being still considered a “disease of theories”. Even that a remarkable number of studies have been investigating this topic, there is no known explanation that can provide an exact pathophysiologic pathway of the illness or sufficient evidence for why this disease is associated with infertility (4-6).
EM is considered being amongst the most frequently encountered diseases in women of reproductive age, having a major impact upon all the aspects of the patient’s life (4, 7).
The incidence of EM is rising, it's values at this moment being around 2% of the general population, representing a major cause of infertility, chronic pelvic pain, dyspareunia and dysmenorrhea. This disease affects 7-15% of women of reproductive age, accounting for 25-30% of cases of infertility, with an important social impact (3, 8).
The health status is directly correlated with the quality of life in a multidimensional concept that implies physical, psychological and social aspects of life, and the reports of these with the disease and its treatment.
One of the best methods to prevent the suffering of the patients is an early diagnosis that would improve the management of the disease and thus the quality of life. However, there are various reasons that can delay the diagnosis, and, by that, reaching an unfavourable outcome (9).
The EM symptom spectrum includes chronic pelvic pain, dyspareunia and infertility, disorders that can have a significant impact upon the patients, in terms of quality of life (QoL) (8).
The aim of the study is to explore some of the psychological reactions associated to EM and depression. We hypothesise that women with EM will show high levels of stress because of their infertility problems. We also expect that a lower quality of life and higher infertility stress will correlate with a higher frequency of depressive symptoms.
PATIENTS AND METHODS
We conducted a cross-sectional study that included a group of 205 women hospitalized in the “Cuza-Voda” University Hospital of Iasi, between 2014-2015. The inclusion criteria were: women aged between 18-42 years diagnosed with endometriosis-caused infertility, thus the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse, male partner being excluded as cause after evaluation for infertility or subfertility using a variety of clinical interventions, also from a laboratory evaluation of semen. The study did not include women with infertility of other causes except endometriosis, body mass index >30 Kg/m2, neoplasia, autoimmune diseases, diabetus mellitus, infectious disease, pregnancy in evolution, under anti-inflammatory or hormonal treatment, depression and treatment for depressive disorders, Cushing syndrome, Turner syndrome.
Every patient enrolled in the study signed a written informed consent. A form of the consent was approved by the Commission for Medical Ethics of the “Grigore T. Popa” University of Medicine and Pharmacy, Iasi.
Statistical methods
The scores principle- the same questionnaire is applied to all the participants in the study, and a primary score is calculated for each patient. In the statistical analysis, there were used both descriptive methods and analytical methods, with a threshold of significance of 95%. The data was centralised in SPSS18.0 data bases and processed with the specific statistical functions: t-Student test, Kruskal-Wallis test.
All patients underwent treatment with desogestrel, 6 months prior to surgery, which time coincides with the completing of the questionnaires.
As research tools, we used the following methods:
Fertility Problem Inventory (FPI) – Infertility Stress: This questionnaire was conceived to measure the patients’ level of stress, the faiths and attitudes regarding infertility. The Fertility Problem Inventory (FPI) was used to assess the stress caused by the infertility problems (10). The questionnaire has 46 items and generates scores on five domains associated to infertility stress: social concern (10 items), sexual concern (8 items), relationship concern (10 items), rejection of childfree lifestyle (8 items) and need for parenthood (10 items). Scores can be summed up to generate a global stress score. Women were asked to assess their agreement to the 46 statements on a Likert scale ranging from 1 – strongly disagree to 6 strongly agree. Higher scores indicate higher infertility stress. We calculated uniform scores by dividing the total scores by the maximum possible and multiplying the results by 100. The final scale ranges from 0 to 100;
Endometriosis Health Profile (EHP-30) - Health related quality of life. The use of this questionnaire in the clinical trials ought to evaluate the impact and benefits of the medical and surgical therapeutic interventions upon the quality of life, in women diagnosed with EM. We used Endometriosis Health Profile (EHP-30) to measure health related quality of life in women with EM (11). This was the first questionnaire designed to measure quality of life in this selected group. The items and scales were developed using interviews with patients addressing the complex consequences of EM on physical, psychological and social aspects of quality of life. The instrument consists of a core questionnaire and six modular parts. The core questionnaire is relevant to all patients with EM and has 30 items and five scales measuring pain, control and powerlessness, emotional well-being, social support and self-image. The modular parts count together 23 items assessing quality of life in areas of work, relationship with children, sexual intercourse, infertility, medical profession and treatment;
Beck Depression Inventory – Depression symptoms: The Beck-BDI depression inventory is a questionnaire that can provide valuable information over the existence of depression-associated manifestations and their severity. Beck Depression Inventory (BDI) is one of the most widely used measures for assessing depression symptoms (12).
All questionnaires were applied after being translated into Romanian and validated.
The questionnaires were translated from English in to Romanian by three different translators and we chose the best match for each item. We pretested the questionnaires on a sample of 30 women and computed Cronbach’s Alpha for each scale and for the total scores. Cronbach’s Alpha scores varied between 0.50 and 0.98. For Beck’s Depression Inventory, we had to eliminate items 10 and 16 assessing sleeping and crying habits, for a Cronbach’s Alpha of 0.50.
RESULTS
The Skewness test (p=-0.19) suggests that the age distribution was homogeneous, recording a mean value of 35.46±2.34 years, close to the median value of 35 years, age that we choose as a tee to apply the tests of signification.
The demographic analysis of our patients showed us that 85.37% of them were living in an urban environment, 80.48% have followed a superior cycle of study. 87.8% of the women were married. 82.92% of women were diagnosed with primary infertility due to endometriosis and 17.08% with secondary infertility. These last ones had this diagnosis founded on the fact that they had at least one child back home.
In the studied group of patients, only 2.4% had two live-births, spontaneous, the percent of the nulliparous women included in the study being of 82.9%. 81% of the women under 35 years old and 85% of those older than 35 years old were nulliparous (p=0.441). Body Mass Index (BMI) of the patients varied between 16kg/m2 and 31.10kg/m2, 12.2% of the patients being overweight, 4.9% of them being diagnosed with class I obesity. In the under 35 years group, BMI was slightly smaller compared with the group of women over 35 years old (22.13 vs. 22.96 kg/m2; p=0.066).
The fertility problem inventory consisted of 5 series of questions, each of 10 questions, divided as following domains: social, sexual, partner relationship, child-free lifestyle rejection and need of parenthood.
In the matter of social domain, almost half of the women questioned (43.9%) declared they could not help to compare themselves with their friends who had at least one child.
In the sexual domain, 22% of the women declared they felt anger if they missed a critical day for sexual intercourse. The stress score for the sexual domain varied between 18 and 30, a median value of 22.66±2.81 being registered, representing 47.21% out of the maximal score of 48. Also, 47.92% of the patients over 35 years old compared with 46.46% of the ones under 35 years old, have a slightly higher stress score related to the sexual domain.
Regarding the partner relationship issue, 22% of the women interrogated considered that their partner does not offer them enough support and understanding in the matter of the fertility problem as they would like to.
In the matter of childfree lifestyle rejection, a major percent of 63.3 women questioned considered that a couple without children could not be as happy as a couple with children.
We must take notice of the fact that 52.38% of the patients under 35 years old compared with 44.38% of those over 35 years old, had a significant higher level of stress, related to the child-free lifestyle (p=0.001).
Regarding the ‘need of parenthood’ domain, 92.7% of the women opinionated that pregnancy and birth are two of the most important events in a relationship. The same percent of women considered that being a parent is a much more important objective than having a successful career and, for a healthy marriage it is required for a couple to have at least one child. They also found it difficult to feel like a real adult without children of their own; 75.6% of the patients interviewed declared themselves frightened by a future without children in their life.
All the patients agreed that having at least one child is the main pursuit of their life. Also, more than half of the women declared that they always wanted to be a parent, and an impressive 100 percent of the women declared that they would do anything to get pregnant and give birth to a baby.
The stress score for the need of parenthood domain varied between 32 and 46, registering a median value of 40.10±2.90, representing 66.83% out of the maximum score of 60. In the matter of age, 67.38% of the women under 35 years old have a slightly higher stress score related to the need of parenthood, compared with the 66.25% of the ones over 35 years old.
Concluding, the highest scores in the matter of infertility are found in the need of parenthood domain (66.83%), respectively the social domain (50.53%), significantly higher compared to the sexual domain (47.21%), partner relationship (49.63%) or childfree lifestyle rejection domain (48.48%).
The uniform FPI score varied between 43.48% and 63.41%, showing infertility related stress in 52.94% of the questioned women. Depending on the epidemiological characteristics, the amount of stress generated by infertility was significantly higher in the women that had no children (54.66% vs. 52.59%; p=0.008), smokers (53.53% vs. 47.46%; p=0.001) and overweight or obese women (53.28% vs. 51.29%; p=0.011).
The Endometriosis Health Profile (EHP)
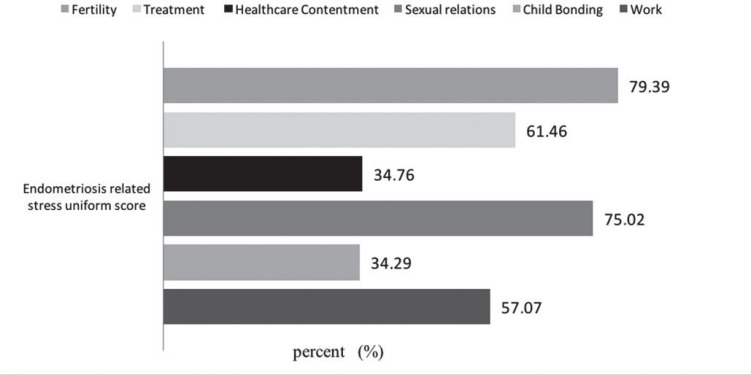
The endometriosis health profile was based on the analysis of two main domains: the quality of life and the EM related stress. The Quality of Life domain was divided into five subdomains, as follows: Pain, Symptoms Control, Emotion Control, Social Support and Self-Care. The Endometriosis Related Stress domain was divided into six subdomains: Work, Children Bonding, Sexual Relationship, Healthcare Contentment, Treatment and Fertility.
The descriptive analysis over the quality of life in patients with EM suggested that the high level of stress related factors are: the loss over the control of the symptoms, pain and altered emotional status.
The EM stress related domain was divided in six sub-domains: Work, Children Bonding, Sexual Relationship, Healthcare Contentment, Treatment and Fertility.
Synthesizing, the highest scores for the EM caused stress are found in the Fertility (79.39%), Treatment (61.46%) and Work (57.07%) subdomains, significantly higher compared with the Child Bonding (34.29%) and Healthcare Contentment (34.76%) subdomains (Fig. 1).
Figure 1.
Endometriosis related stress.
The BECK-BDI depression inventory consisted of 21 questions, that evaluated the feelings of sadness, failure, dissatisfaction, guilt, self-punishment, self-hatred, pessimism, suicidal thoughts, loss of control, irritability, introversion, lack of confidence, sleep disorders, fatigue, anorexia, weight loss and libido loss.
The total BDI score varied in between 21 to 40 showing severe depression in 98.5% of the patients and moderate depression in 1.5%.
DISCUSSION
For measuring the health-related quality of life on women with EM, we used the Endometriosis Health Profile questionnaire. Various studies showed the appliance of this study on assessing the health-related quality of life. Jones G. et al. showed that EHP questionnaire was very understandable by the respondents, making it suitable for measuring the health-related quality of life on patients with EM (13). Analysing the data extracted from the study group, we consider that the results are relevant and should raise concern. Patients with EM are dealing daily with a large spectrum of symptoms, including pain, dyspareunia, emotional instability and high levels of stress, which have a negative impact upon the quality of life, by lowering it on different levels.
Fauconnier et al. suggested in their study that different mechanisms could be responsible for the pain related to EM. These mechanisms could be the set of the variability in perception, description and interpretation of the same pain experience by different patients. By further studying this, we ought to get to explain and fix the difficulties for building efficient questionnaires (14).
We clearly underlined the effect of EM on work, with 87.8% of the women saying they feel guilty they are missing work or that they cannot complete their work duties because of their disease. The percentage is comparable with other studies that found a 51% of women stating that EM affected their work (15).
Other studies (16) have demonstrated that the inability to conceive generates a high level of stress in infertile women, facts stated in our study as well. Unsuccessful fertility treatments have a big impact on the psychological state of these women, especially if they do not have the desired outcome. Fagervold et al. 2009 stated that 7.7% suffered from a broken relationship due to the disease, results that are comparable to our study. We estimated the percentage of women that had an altered relationship with their partner at 22%, including the ones that said they felt anger if they missed a critical day for conception and the ones that stated they don’t feel like getting enough support from their partner (15, 17).
We must underline the importance of the sexual aspect of life and its impact over the women’s life. Dyspareunia, lack of desire for engaging in sexual intercourse, especially due the fear of not being able to conceive, summarize the large affected field of the sexual domain. Most of the times, the main concern of the physician is to treat the somatic symptoms of EM, as in pain, dyspareunia, spotting and of course, infertility. Literature data suggests that women with EM have impaired quality of life associated with their condition, fact that is also supported by our findings (15). As it can be seen, the total BDI score showed severe depression in 98.5% of the patients and moderate depression in 1.5%. These are extremely alarming numbers, showing us that EM and the associated infertility are powerful triggers of depression in women. We agree that a further exploration of the relationship between EM and infertility and depression is required. More information is surfacing, supporting the idea that infertility, along with the stress and depression generated by it, ought to be seen as a whole and not as separate parts in matter of diagnosis and treatment (18).
The main purposes of this study were on the one hand to better understand the physical and psychological needs of these patients and to offer them a bigger palette of options in terms of social and psychological support to overcome these obstacles and, on the other hand, to improve the therapeutic options available as we speak. This may prove to be no easy work, because as Fauconnier et al. said in their study, the common concept of severe dysmenorrhea should be expanded to “atypical cyclical pelvic pain syndrome”, for a better approach of the disease in a low prevalence population (14).
Within the present study, we showed a significant presence of high infertility stress in patients of all ages that lead to depression and social anxiety. One other note that the authors would like to make, is regarding the comparison between the two age groups, under 35 years old and over 35 years old. It is yet to be proven which are the external contributing factors that act over the 35 years old women, compared with the ones under 35 years old, considering that, in the majority cases, the women under 35 years old were much more affected that the ones over this age limit. In correlation with our results, the Centre for Disease Control and Prevention in the United States, reports a percentage of women affected by infertility, according to their age as follows: 11% of women aged between 15-29 years old, 17% of women aged 30-34 years old, 23% of women aged between 35-39 years old and 27% of women aged 40-44 years old (18). Thus, these studies showed that infertility is age-dependent and the probability to spontaneously conceive is inversely proportional with age.
Many studies conducted on different continents showed that the most negative impact upon the QoL in patients diagnosed with endometriosis are mainly lack of control and the feeling of powerlessness. (13, 19-22). Our study found the same results in matter of control, this symptom being cataloged as one of the most disturbing for the patients. We also found out that besides lack of control, high levels of stress were issued by pain and an altered emotional status.
The physician along the patient play two different but intricate roles in the diagnosis and treatment of EM, a first step in the correct approach of the disease being a clearer exposure of the symptoms by the patient and a better understanding of them, by the practitioner. Infertility, both a symptom and a disease by itself, can have dangerous consequences on women, affecting them physically and mentally. Prescribing a treatment according to protocols does not necessarily mean that it suits every patient, thus we must take notice that not only infertility, but also its treatment comes with a cost in terms of stress, emotions and mental health (23, 24).
Study limits
One major limitation of the study is the fact that we do not have a control group of women with infertility of other causes, thus we could not study the psychological impact of infertility on them. This happened because we included in the study only a specific group of women with endometriosis. For our further studies, a control group will be included, for a more explicit comparison and a better exposure of the psychological influence of infertility on them. Another limitation of the study is that the patients included in the study were not observed during the period of their therapy, the questionnaires being applied only at the end of the 6 months of treatment, at the moment of surgery. This was due the fact that all the patients had an increased compliance with treatment, fact sustained by a very good communication between both medical and patient sides. If a contrary situation had happened, the patients would have been monitored more closely.
Conflict of interest
None of the authors has any conflicts of interest to declare.
Author contributions
Daniela-Roxana Albu (Matasariu) applied the questionnaires to the patients, did the statistics and wrote the manuscript. Maria Iacob applied the questionnaires to the patients and worked on the data base, Alexandra Mihaila worked on the statistics and helped with the writing of the manuscript, Irina Dumitrascu and Mircea Onofriescu diagnosed endometriosis and did the patient selection, Irina Crumpei Tanasa found the appropriate questionnaires and translated them, Carmen Vulpoi supervised the entire study, with all its steps.
Authors agree to allow the journal to review the data if requested.
We are very grateful to Professor Corin Badiu for excellent advice and the critical review of this article.
Acknowledgement
“This paper was published under the frame of European Social fund, Human Resources Development Operational Programme 2007-2013, project no. POSDRU/ 159/1.5/136893”.
References
- 1.Bulun SE. Endometriosis. N. Engl. J. Med. 2009;360:268–279. doi: 10.1056/NEJMra0804690. [DOI] [PubMed] [Google Scholar]
- 2.Giudice LC. Clinical practice. Endometriosis. N. Engl. J. Med. 2010;362:2389–2398. doi: 10.1056/NEJMcp1000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil Steril. 1997;68:585–596. doi: 10.1016/s0015-0282(97)00191-x. [DOI] [PubMed] [Google Scholar]
- 4.Malutan A, Drugan T, Georgescu C, Ciortea R, Bucuri C, Bobric A, Rada MP, Mihu D. Vascular Endothelial Growth Factor serum levels in women with advanced endometriosis. Acta Endo (Buc) 2016;12(1):7–13. doi: 10.4183/aeb.2016.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li YZ, Wang LJ, Li X, Li SL, Wang JL, Wu ZH, Gong L, Zhang XD. Vascular endothelial growth factor gene polymorphisms contribute to the risk of endometriosis: an updated systematic review and meta-analysis of 14 case-control studies. Genet Mol Res. 2013;12(2):1035–1044. doi: 10.4238/2013.April.2.20. [DOI] [PubMed] [Google Scholar]
- 6.Hayrabedyan S, Kyurkchiev S, Kehayov I. FGF1 and S100A13 possibly contribute to angiogenesis in endometriosis. J Reprod Immunol. 2005;67(1-2):87–101. doi: 10.1016/j.jri.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Rižner TL. Noninvasive biomarkers of endometriosis: myth or reality? Expert Rev Mol Diagn. 2014;14(3):365–385. doi: 10.1586/14737159.2014.899905. [DOI] [PubMed] [Google Scholar]
- 8.Albu (Matasariu) DR, Iacob M, Dumitrascu I, Onofriescu M, Vulpoi C. Desogestrel in the preoperative treatment of endometriosis cysts. Rev Med Chir Soc Med Nat Iasi. 2015;119(3):710–714. [Google Scholar]
- 9.Oehmke F, Weyand J, Hackethal A, Konrad L, Omwandho C, Tinneberg HR. Impact of endometriosis on quality of life: a pilot study. Gynecol Endocrinol. 2009;25(11):722–725. doi: 10.3109/09513590903159607. [DOI] [PubMed] [Google Scholar]
- 10.Newton CR, Sherard W, Glavac I. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil.Steril. 1999;72(1):54–62. doi: 10.1016/s0015-0282(99)00164-8. [DOI] [PubMed] [Google Scholar]
- 11.Jones G, Kennedy S, Barnard A, Wong J, Jenkinson C. Development of an endometriosis quality-of life instrument: the Endometriosis Health Profile–30. Obstet Gynecol. 2001;98:258–264. doi: 10.1016/s0029-7844(01)01433-8. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin. Psychol Rev. 1988;8:77–100. [Google Scholar]
- 13.Jones G, Jenkinson C, Taylor N, Mills A, Kennedy S. Measuring quality of life in women with endometriosis: tests of data quality, score reliability, response rate and scaling assumptions of the Endometriosis Health Profile Questionnaire. Hum Reprod. 2006;21(10):2686–2693. doi: 10.1093/humrep/del231. [DOI] [PubMed] [Google Scholar]
- 14.Fauconnier A, Staraci S, Huchon C, Roman H, Panel P, Descamps P. Comparison of patient- and physician- based descriptions of symptoms of endometriosis: a qualitative study. Hum Reprod. 2013;28(10):2686–2694. doi: 10.1093/humrep/det310. [DOI] [PubMed] [Google Scholar]
- 15.De Graaff AA, D’Hooghe TM, Dunselman GA, Dirksen CD, Hummelshoj L, WERF EndoCost Consortium. Simoens S. The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. 2013;28(10):2677–2685. doi: 10.1093/humrep/det284. [DOI] [PubMed] [Google Scholar]
- 16.Xiaoli S, Mei L, Junjun B, Shu D, Zhaolian W, Jin W, Ju Q, Wanli S, Huali Z, Li J, Dong L, Li P, Xiaojin H. Assessing the quality of life of infertile Chinese women: a cross – sectional study. Taiwan J Obstet Gynecol. 2016;55:244–250. doi: 10.1016/j.tjog.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Fagervold B, Jenssen M, Hummelshoj L, Moen MH. Life after a diagnosis with endometriosis – a 15 years follow-up study. Acta Obstet Gynecol ScandI. 2009;88:914–919. doi: 10.1080/00016340903108308. [DOI] [PubMed] [Google Scholar]
- 18.De Berardis D, Mazza M, Marini S, Del Nibletto L, Pino MC, Valchera A, Ortolanis C, Ciarrocchi F, Martinotti G, Di Giannantonio M. Psychopathology, emotional aspects and psychological counselling in infertility: a review. Clin Ter. 2014;165(3):1–7. doi: 10.7417/CT.2014.1716. [DOI] [PubMed] [Google Scholar]
- 19.Jia SZ, Leng JH, Sun PR, Lang JH. Translation and psychometric evaluation of the simplified Chinese-version Endometriosis Health Profile-30. Hum Reprod. 2013;28(3):691–697. doi: 10.1093/humrep/des426. [DOI] [PubMed] [Google Scholar]
- 20.Jenkinson C, Kennedy S, Jones G. Evaluation of the American version of the 30-item Endometriosis Health Profile (EHP-30) Qual Life Res. 2008;17:1147–1152. doi: 10.1007/s11136-008-9403-9. [DOI] [PubMed] [Google Scholar]
- 21.Khong SY, Lam A, Luscombe G. Is the 30-item Endometriosis Health Profile (EHP-30) suitable as a self-report health status instrument for clinical trials? Fertil Steril. 2010;94:1928–1932. doi: 10.1016/j.fertnstert.2010.01.047. [DOI] [PubMed] [Google Scholar]
- 22.van de Burgt TJ, Hendriks JC, Kluivers KB. Quality of life in endometriosis: evaluation of the Dutch-version Endometriosis Health Profile-30 (EHP-30) Fertil Steril. 2011;95:1863–1865. doi: 10.1016/j.fertnstert.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Coughlan C, Walters S, Ledger W, Li TC. A comparison of psychological stress among women with and without reproductive failure. Int J Gynaecol Obstet. 2014;124:143–147. doi: 10.1016/j.ijgo.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Catherino WH. Stress relief to augment fertility: the pressure mounts. Fertil Steril. 2011;95(8):2462–2463. doi: 10.1016/j.fertnstert.2011.05.067. [DOI] [PubMed] [Google Scholar]