Abstract
Background
Dentistry is a profession with a high prevalence of work‐related musculoskeletal disorders (WMSD) among practitioners, with symptoms often starting as early in the career as the student phase. Ergonomic interventions in physical, cognitive, and organisational domains have been suggested to prevent their occurrence, but evidence of their effects remains unclear.
Objectives
To assess the effect of ergonomic interventions for the prevention of work‐related musculoskeletal disorders among dental care practitioners.
Search methods
We searched CENTRAL, MEDLINE PubMed, Embase, PsycINFO ProQuest, NIOSHTIC, NIOSHTIC‐2, HSELINE, CISDOC (OSH‐UPDATE), ClinicalTrials.gov, and the World Health Organization International Clinical Trials Registry Platform (ICTRP) Search Portal to August 2018, without language or date restrictions.
Selection criteria
We included randomised controlled trials (RCTs), quasi‐RCTs, and cluster RCTs, in which participants were adults, aged 18 and older, who were engaged in the practice of dentistry. At least 75% of them had to be free from musculoskeletal pain at baseline. We only included studies that measured at least one of our primary outcomes; i.e. physician diagnosed WMSD, self‐reported pain, or work functioning.
Data collection and analysis
Three authors independently screened and selected 20 potentially eligible references from 946 relevant references identified from the search results. Based on the full‐text screening, we included two studies, excluded 16 studies, and two are awaiting classification. Four review authors independently extracted data, and two authors assessed the risk of bias. We calculated the mean difference (MD) with 95% confidence intervals (CI) for continuous outcomes and risk ratios (RR) with 95% confidence intervals for dichotomous outcomes. We assessed the quality of the evidence for each outcome using the GRADE approach.
Main results
We included two RCTs (212 participants), one of which was a cluster‐randomised trial. Adjusting for the design effect from clustering, reduced the total sample size to 210. Both studies were carried out in dental clinics and assessed ergonomic interventions in the physical domain, one by evaluating a multi‐faceted ergonomic intervention, which consisted of imparting knowledge and training about ergonomics, work station modification, training and surveying ergonomics at the work station, and a regular exercise program; the other by studying the effectiveness of two different types of instrument used for scaling in preventing WMSDs. We were unable to combine the results from the two studies because of the diversity of interventions and outcomes.
Physical ergonomic interventions. Based on one study, there is very low‐quality evidence that a multi‐faceted intervention has no clear effect on dentists' risk of WMSD in the thighs (RR 0.57, 95% CI 0.23 to 1.42; 102 participants), or feet (RR 0.64, 95% CI 0.29 to 1.41; 102 participants) when compared to no intervention over a six‐month period. Based on one study, there is low‐quality evidence of no clear difference in elbow pain (MD −0.14, 95% CI −0.39 to 0.11; 110 participants), or shoulder pain (MD −0.32, 95% CI −0.75 to 0.11; 110 participants) in participants who used light weight curettes with wider handles or heavier curettes with narrow handles for scaling over a 16‐week period.
Cognitive ergonomic interventions. We found no studies evaluating the effectiveness of cognitive ergonomic interventions.
Organisational ergonomic interventions. We found no studies evaluating the effectiveness of organisational ergonomic interventions.
Authors' conclusions
There is very low‐quality evidence from one study showing that a multi‐faceted intervention has no clear effect on dentists' risk of WMSD in the thighs or feet when compared to no intervention over a six‐month period. This was a poorly conducted study with several shortcomings and errors in statistical analysis of data. There is low‐quality evidence from one study showing no clear difference in elbow pain or shoulder pain in participants using light weight, wider handled curettes or heavier and narrow handled curettes for scaling over a 16‐week period.
We did not find any studies evaluating the effectiveness of cognitive ergonomic interventions or organisational ergonomic interventions.
Our ability to draw definitive conclusions is restricted by the paucity of suitable studies available to us, and the high risk of bias of the studies that are available. This review highlights the need for well‐designed, conducted, and reported RCTs, with long‐term follow‐up that assess prevention strategies for WMSDs among dental care practitioners.
Plain language summary
Ergonomic interventions to prevent musculoskeletal disorders among dental care practitioners
What is the aim of this review?
Dental care providers are more prone to injuries and disorders of the bones, muscles, and joints, which are known as musculoskeletal disorders (MSDs), due to the physically and mentally stressful nature of their work. Various measures or solutions have been suggested to prevent work‐related MSDs (WMSDs). These are known as ergonomic interventions, which means harmonising things with which people interact, in order to meet people's needs, abilities, and limitations. Ergonomic interventions fall under physical, cognitive (mental), or organisational domains. The aim of this Cochrane Review was to find out if any of these ergonomic interventions were effective in preventing WMSDs among dental care practitioners. We collected and analysed all relevant studies to answer this question. We found two relevant studies.
Key messages
There is very low‐quality evidence from one study, that a comprehensive ergonomics intervention, consisting of training, work station modification, and a regular exercise program has no effect on dentists' risk of WMSDs in the thighs or feet, over a period of six months. There is low‐quality evidence from one study that changing the tools used for scraping off dental plaque has no clear effect on dentists' elbow pain or shoulder pain over a four‐month period. Both included studies have several shortcomings, and did not follow‐up with participants for a sufficiently long period of time. We found no studies that evaluated the effectiveness of cognitive or organisational ergonomics interventions. We need better studies to evaluate the effectiveness of ergonomic interventions in dental care practitioners. It is very likely that including the results of new studies will change the conclusions of this review.
What was studied in the review?
Dental practitioners are highly susceptible to occupational hazards like MSDs, which have been attributed to deteriorating quality of life, burnout, and poor health, which often result in some practitioners quitting the profession. It has been suggested that introducing ergonomic interventions, by making improvements in working style, instruments used, dental office designs, physical activity, work posture, mental stress levels, appointment scheduling, or work environment may help to prevent WMSDs. Our review evaluated the effectiveness of all of these interventions in preventing WMSDs among those who practiced dentistry, be it dentists, dental hygienists, dental auxiliaries, dental nurses, or dental students. We assessed how well these measures prevented the occurrence of new WMSDs, not how they reduced the severity, or how they eliminated WMSDs that already existed. We evaluated the effectiveness of ergonomic interventions on the number of physician‐diagnosed WMSDs, self‐reported pain, or work ability.
What are the main results of the review?
We found two studies, involving 212 participants, that were conducted in dental practices or clinics in Iran and the United States. Both studies assessed physical ergonomic interventions. One study assessed a comprehensive ergonomics intervention, consisting of training, work station modification, and a regular exercise program, and the other study assessed two different types of instruments used for carrying out a dental procedure. The first study found that the comprehensive ergonomics intervention did not reduce musculoskeletal pain in the thighs or feet. The second study found that people using the two different kinds of tools for scraping off dental plaque had similar levels of elbow and shoulder pain. These studies had shortcomings, like poor methodology and short follow‐up times, hence we could not draw any definitive conclusions based on their findings.
We found no studies that assessed the effectiveness of cognitive or organisational ergonomics interventions. We need studies that are designed, conducted, and reported better to evaluate the effects of physical, cognitive, and organisational ergonomics interventions.
How up to date is this review?
We searched for studies published up to August 2018.
Summary of findings
Summary of findings for the main comparison. Physical ergonomic intervention compared to no intervention for prevention of musculoskeletal disorders in dental care practitioners.
| Multi‐faceted ergonomic interventions compared to no intervention | ||||||
| Patient or population: Dentists Setting: Private dental clinics in Tehran Intervention: Multi‐faceted ergonomic interventions Comparison: No intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with multi‐faceted ergonomic interventions | |||||
| Number of workers with newly diagnosed WMSD (incident cases) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not measure this outcome |
| Self‐reported complaints of MSD pain in thighs (Nordic musculoskeletal questionnaire) 6‐month follow‐up | 212 per 1000 | 121 per 1000 (49 to 300) | RR 0.57 (0.23 to 1.42) | 102 (1 RCT) | ⊕⊝⊝⊝ very low a, b, c | |
| Self‐reported complaints of MSD pain in feet (Nordic musculoskeletal questionnaire) 6‐month follow‐up | 250 per 1000 | 160 per 1000 (73 to 353) | RR 0.64 (0.29 to 1.41) | 102 (1 RCT) | ⊕⊝⊝⊝ very low a, b, c | |
| Work functioning or disability | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not measure this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | ||||||
a Downgraded by one level because we judged study to be at a high risk of bias.
b Downgraded by one level due to imprecision, since results were derived from a single small study.
c Downgraded by one level due to indirectness, since trial included measurements pertaining only to thighs and feet (as they alone met the inclusion criteria), instead of the most common sites of WMSD in dentistry, such as neck, shoulder, lower back, wrists, or hands.
Summary of findings 2. Physical ergonomic intervention compared to alternative instrument design to prevent musculoskeletal disorders among dentists and dental hygienists.
| Light weight Instruments with wide handles compared to heavy weight instruments with narrow handles for scaling | |||||
| Patient or population: Dentists and dental hygienists who performed scaling, root planing, or dental prophylaxis procedures Setting: Private dental clinics in San Fransisco Intervention: Light weight scaling instrument with a wide handle Comparison: Heavy weight scaling instrument with a narrow handle | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with heavy weight and narrow handle | Risk with instruments with light weight and wide handle | ||||
| Number of workers with newly diagnosed WMSD (incident cases) | ‐ | ‐ | ‐ | ‐ | The study did not measure this outcome |
| Self‐reported complaints of MSD pain in right upper extremity – elbow, forearm (0‐ to 10‐point scale; 0 = no pain, 10 = unbearable pain) 16‐week follow‐up | The mean change in self‐reported pain in the right elbow and forearm in the heavy instrument group was 0.06 | The mean change in self‐reported pain in the right elbow and forearm in the light instrument group was 0.14 lower (0.39 lower to 0.11 higher) | 108a (1 RCT) | ⊕⊕⊝⊝ low b, c | |
| Self‐reported complaints of MSD pain in right upper extremity – shoulder (0‐ to 10‐point scale; 0 = no pain, 10 = unbearable pain) 16‐week follow‐up | The mean change in self‐reported pain in the right shoulder in the heavy instrument group was 0.19 | The mean change in self‐reported pain in the right shoulder in the light instrument group was 0.32 lower (0.75 lower to 0.11 higher) | 108a (1 RCT) | ⊕⊕⊝⊝ low b,c | |
| Work functioning or disability | ‐ | ‐ | ‐ | ‐ | The study did not measure this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; ICC: intraclass correlation coefficient | |||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | |||||
a Study population adjusted to account for design effect of clustering in methodology; applied an assumed ICC of 0.1. Original study sample size = 110; adjusted sample size after accounting for design effect = 108.
b Downgraded by one level since study has an unclear risk of bias due to use of self‐reported assessment for outcomes (detection bias).
c Downgraded by one level due to imprecision, since results are derived from one small study alone.
Background
Description of the condition
Work‐related musculoskeletal disorders (WMSDs) have been identified as a significant occupational health problem among dental professionals (Hayes 2010; Leggat 2007). WMSDs can be defined as any injury to the human support system, including the bones, cartilage, muscles, ligaments, tendons, blood vessels, or nerves, caused or aggravated primarily by the performance of work and by the effects of the working environment (EASHW 2008; Lalumandier 2001; NIOSH 1997; Rolander 2001). Musculoskeletal disorders are considered to be work‐related when the environment and performance of work contribute significantly to the condition, the condition is made worse or persists longer due to work conditions, or both (Bernard 1997). General examples of work conditions that may lead to WMSDs include: routine lifting of heavy objects, daily exposure to whole body vibration, routine overhead work, work with the neck in a constantly flexed position, or performing repetitive forceful tasks (Bernard 1997). In dentistry, many cases of WMSDs are related to cumulative trauma, and are considered repetitive strain injuries. Risk factors for repetitive strain injuries among dental practitioners include gripping and using slender instruments in repetitive motions (such as for plaque removal and cavity preparation), and using vibratory instruments, such as hand pieces and ultrasonic scalers (Liskiewicz 1997; Morse 2003). The work environment also poses a risk for developing WMSDs, as the nature of dental work requires that dental practitioners sustain awkward postures and non‐neutral wrist positions. Furthermore, psychosocial factors, such as job satisfaction, level of support, and balance between work and private life have also been shown to be associated with WMSDs (Hayes 2012; Ylipaa 1999).
WMSDs are not limited to any specific region of the body; however, for dental professionals, they commonly occur in the neck, shoulder, lower back, and wrists (Hayes 2009). Sufferers of WMSDs may experience numbness, tingling, pain, decreased strength, or swelling of the affected area (Michalak‐Turcotte 2000). These symptoms can manifest through a variety of mechanisms, including decreased muscle function, impaired nerve conduction, strains, and ruptures of muscles, tendons, and ligaments, or degeneration or microfracture of the bones (ASCC 2006). Many specific WMSDs have been identified in the literature, including carpal tunnel syndrome (Hayes 2010), tendonitis (Conrad 1990; Hawn 2006), thoracic outlet syndrome (Sanders 2002), and de Quervians disease (Simmer‐Beck 2006).
The prevalence of non‐specific WMSDs among dental professionals is estimated to be between 49% and 92% (Moodley 2018). However, the prevalence of site‐specific WMSD varies greatly. In the same review of occupational health problems in dentistry, it was reported that prevalence of back pain ranged from 22.2‐91.0 %, neck pain from 20‐84.9% and shoulder pain from 18.9‐73.5% (Moodley 2018). An earlier review, which focused on neck and shoulder disorders, found that dentists reported a period prevalence of 26‐73% for neck symptoms and 20‐65% for shoulder symptoms over the previous year, while dental hygienists reported a higher prevalence ranging from 54‐83% for neck and 35‐76% for shoulder, and dental assistants reported prevalence of 38‐62% for neck and 27‐62% for shoulder (Morse 2010). Dental hygienists and therapists seemed to also have higher prevalence rates for WMSDs in wrists and hands as compared to dentists (Hayes 2013; Moodley 2018).
It is troubling that students undergoing training in dental professions also appear to be suffering from WMSDs at considerably high rates. A Dutch study reported that 95% of the dental students had suffered from pain in muscles and joints in the last 12 months (Breurs 2017) and a Malaysian study found that 93% of dental students in clinical training years developed WMSDs (Khan 2013). A 3‐year longitudinal study on dental hygiene students in Australia found that WMSD symptoms in neck, shoulder and wrists got progressively worse in the clinical training years, with a marked increase in the final year of training (Hayes 2014a). Given this early development of symptoms, career satisfaction and longevity may be a concern for these future dental professionals, especially since they are yet to embark on the rigours of full‐time clinical practice.
WMSDs can have a significant impact on the career of a dental professional. Researchers have identified that many sufferers seek medical attention for their WMSDs (Al Wazzan 2001; Hayes 2012; Leggat 2006). These injuries and illnesses acquired in the workplace not only have direct costs, in terms of seeking medical attention and compensation, but also indirect costs, such as decreased productivity, lost wages, and reduced quality of life. In the United States, lost income due to WMSDs in the dental profession has been estimated to be around USD 41 million annually (Michalak‐Turcotte 2000).
Description of the intervention
The International Ergonomic Association defines ergonomics as the scientific discipline concerned with the understanding of the interactions among humans and other elements of a system, and the profession that applies theory, principles, data, and methods to design, in order to optimise human well‐being and overall system performance. Ergonomics is intended to help to harmonise things with which people interact, in terms of people's needs, abilities, and limitations (IEA 2014). The European Society for Dental Ergonomics defines dental ergonomics as the adaptation of the working environment and methods for the dentist and his or her team, with respect to their physical and psychological capacity for healthy, safe, and comfortable functioning in their professional activity. Ergonomics maximises efficiency in time, space, and motion (Goldstep 1998), and aims to minimise the amount of physical and mental stress during the practice of dentistry for all involved (ADA 2004). The main objective of ergonomic interventions in dentistry is to prevent the occurrence of WMSDs, since they are difficult to treat once they occur, and tend to reoccur if the same work patterns are continued (Yamalik 2007).
The International Ergonomic Association categorises ergonomics into three specific domains of physical ergonomics, cognitive ergonomics, and organisational ergonomics (IEA 2014):
-
Physical ergonomics, with respect to dental professionals, consists of:
interventions aimed at operator factors (e.g. adopting right work posture, appropriate use of patient and dentist chair, or correct method of instrumentation and tool handling);
interventions aimed at office design factors (e.g. workstation layout, or set‐up of space for positioning of operators, patients, machines, delivery systems, and their inter‐relationships);
interventions aimed at dental equipment design factors (e.g. ergonomically designed operator and patient chairs, instruments, and visual aids).
Cognitive ergonomics consists of interventions aimed at interactions among humans and other elements of a system (e.g. mental workload or skilled performance).
Organisational ergonomics optimises organisational structures, policies, and processes (e.g. organisation of workflow or appointment scheduling).
How the intervention might work
The practice of dentistry is highly demanding and challenging, due to the amount of manual dexterity, visual acuity, and endurance required to carry out procedures in a narrow, confined, complex, and restricted work area, like the oral cavity. Ergonomic interventions seek to prevent the development of WMSDs, by focusing on the worker and factors within the work space or area, and by reducing, modifying, or eliminating both worker‐related and work‐related factors, during one's dental practice (Buckle 2002; Rucker 2002).
-
Physical ergonomic interventions
-
interventions aimed at operator factors:
the Standard ISO 11226, 'Ergonomics – evaluation of static working postures', provides ideal postures for dental work, such as sitting in an active, symmetrical upright posture, with upper body bent forward, if necessary, from the hip joints, at a maximum of 10 to 20 degrees. However, in practice, these ideal postures are not always adopted by practitioners. Clinical ergonomic training and education, which sought to rectify such poor work postures, were found to reduce the occurrence of WMSDs (Droeze 2005; Rucker 2002).
-
interventions aimed at dental office design factors:
poor ergonomic design of work area leads to WMSDs and decreased productivity at work. An ergonomically designed office facilitates more ideal body movements, postures, and working style. In turn, more ideal postures lead to fewer WMSDs (ADA 2004; Ahearn 2010).
-
interventions aimed at dental equipment design factors:
ergonomically designed operator and patient chairs allow the operator to adopt a better position during work. Suitable lighting and magnification devices eliminate the need to bend, and use less ideal postures of the trunk and neck, thus preventing the development of WMSDs. Hand instruments, designed according to ergonomic specifications, reduce muscle force, awkward postures, and movements, such as the pinching effect, or forces over the pads of fingers, thus reducing fatigue and WMSDs (Michalak‐Turcotte 2005; Morse 2007; Rempel 2012).
-
-
Cognitive ergonomic interventions
psychosocial stress, caused by job demands, such as the number of patients seen, or hours worked, and job control, is associated with WMSDs in dental practitioners (Morse 2010; Ylipaa 1999). Ergonomic interventions to reduce stress, by incorporating appropriate job control and working style measures, as well as relaxation techniques to offset stress levels, can prevent WMSDs (Kierklo 2011; Valachi 2003).
-
Organisational ergonomic interventions
better or different organisation of the work, such as working with dental assistants, eliminates less than ideal movements and postures, thus preventing WMSDs. Appointment scheduling, by alternating easy and difficult cases, and providing buffer periods and breaks for rest and stretching, reduce the likelihood of WMSDs for the operator and supporting staff. Task rotation also can prevent WMSDs, and reduces stress caused by repetitive procedures.
Among dental care practitioners, the effects of these ergonomic interventions on WMSDs were found to be dependent on gender, type of practice, and number of hours of work (Droeze 2005; Yamalik 2007; Ylipaa 1999).
Why it is important to do this review
A review on WMSDs in oral healthcare providers found neck symptoms in the range of 17% to 73% in dentists, 54% to 83% in dental hygienists, and 38% to 62% in dental assistants, and shoulder symptoms in the range of 20% to 65% in dentists, 27% to 76% in dental hygienists, 62% in dental assistants, and 6% in a single study of dental and dental hygiene students (Morse 2010). A recent review quantifies prevalence of non‐specific WMSDs among dental professionals to be between 49% and 92% (Moodley 2018). WMSDs also reached an alarming rate in dental students at 93‐95% (Breurs 2017; Khan 2013) and seem to get worse over the course of clinical training (Hayes 2014a). According to a 1987 estimate, dentists lost over USD 40 million (in 1987 dollars), and cancelled 1.3 million patient visits, due to WMSDs. Dental hygienists with WMSDs reported a reduction in number of days worked, decreased speed and quality of work, and increased sick leave, which also increased in relation to role ambiguity and poor social and work climates (Miller 1989; Osborn 1990; Petren 2007). It has been reported that 18% to 30% of practitioners cited WMSDs and work‐related disability among determining factors for quitting the profession (Burke 1997; Miller 1991). The American Dental Association stated that one out of four dentists would be disabled long enough to collect benefits at some point before retirement, according to the odds of disability determined by Great‐West Life in 2013, after studying years of disability claims by members (ADA 2014).
Studies have explained the occurrence of WMSDs in dental practitioners, as a function of gender, age, sitting or standing position of practice, posture, use of assistants, number of work hours per day, number of years worked, intensity of work done, force used, nature of procedures carried out, type of instruments, work‐rest cycles, office design, equipment used, organisational set‐up, stress, work environment, and pre‐disposing factors, like weight, smoking, physical fitness, and pre‐existing systemic conditions (Kierklo 2011; Morse 2010; Valachi 2003; Yamalik 2007). The available data are scattered, and often obtained through subjective, self‐reported surveys and questionnaires, or observation, and thus, lack objective measurements and defined criteria. No definitive or specific guidelines are available for dental care providers with respect to WMSDs, and in spite of the condition being so widespread, the few recommendations that are available are based on the adaptation of general ergonomic guidelines to dentistry. Our review aimed to investigate the available evidence for ergonomic interventions, in order to provide a basis for sound, scientific, and evidence‐based decision‐making, for formulating and implementing guidelines on dental ergonomics, to address an issue that is so crucial to the safety, health, and well‐being of the oral health practitioners in their professional and personal lives.
Objectives
To assess the effect of ergonomic interventions for the prevention of work‐related musculoskeletal disorders (WMSD) among dental care practitioners.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), quasi‐RCTs (methods of allocating participants to a treatment, which are not strictly at random, e.g. date of birth, hospital record number or alternative), and cluster‐RCTs (i.e. the unit of randomisation is a group of people, such as people working in the same specialty, or performing the same type of procedures, rather than individual practitioners). We included studies reported as full‐text, abstract only, or unpublished data.
Types of participants
We included adults, aged 18 and older, who were engaged in the practice of dentistry. At least 75% of the participants in a trial should have been free from musculoskeletal pain at baseline, and should not have sought active treatment for MSDs.
We excluded studies with participants with the following characteristics or comorbidities:
diseases of the central nervous system;
inflammatory rheumatic diseases;
degenerative muscular disorders; and
acute traumatic events of known etiology (like accidents or injury), caused specifically by non‐work‐related factors, in the past three months.
Types of interventions
We included trials that evaluated the effects of the following types of interventions.
Ergonomic interventions in the physical domain, aimed at either the operator or working environment. Operator‐directed interventions included: training to implement ideal postures and movements during work, training to use instruments in the ideal manner, using aids, and instruments that were ergonomically designed, while operating on patients, such as magnification devices, special lighting, intra‐oral cameras. Working environment interventions included modifications to operatory design, workstation layout, or set‐up.
Ergonomic interventions in the cognitive domain included: stress management and relaxation techniques, improving communication with co‐workers and patients, support systems to handle family‐work conflicts, training to master precision skills, prioritisation of operator preferences, and role‐designation to increase job satisfaction.
Ergonomic interventions in the organisational domain included: organisation of workflow, appointment scheduling, patient‐management systems, pace and variety of workload, sequence and administration of procedures, taking breaks between works, stretching, exercising, and mobilising after prolonged static postures, assistant support, task rotation, work‐rest cycles, and time management.
We included studies that compared these interventions with no intervention, a sham ergonomic intervention, or any other alternative intervention.
Types of outcome measures
We only included trials that had measured at least one of the primary outcomes of interest.
Primary outcomes
-
Number of workers with newly diagnosed WMSD (incident cases)
WMSDs refered to injuries that affected the musculoskeletal, peripheral nervous, and neurovascular systems, which were caused or aggravated by occupational exposure to ergonomic hazards (NIOSH 1997)
-
Self‐reported complaints of pain related to the musculoskeletal system
This could be measured using a dichotomy scale (yes or no), a Likert scale, a visual analogue scale (VAS), or any similar scale
Work functioning or disability, assessed in terms of level of functioning, limitation of movement, decrease in productivity, number of hours worked, total number of work days lost, loss or change of job, or work‐related disability, measured by outcome measures instruments, like the Oswestry Disability Index (ODI), Roland‐Morris Disability Questionnaire (RMDQ), Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH), Work Ability Index (WAI), or other similar instruments
Secondary outcomes
-
Change in posture
This could be measured by posture assessment scales, photometry, videometry, pressure sensors, precision stadiometers, inclinometers, electrogoniometers, angle transducers, force plates, dynamometers, or any other posture measurement techniques
-
Change in muscular load
This could be measured by electromyogram, strain gauge force transducers, or any another validated method
Change in nerve function, measured by neurological tests, or nerve conduction measurement
Costs for implementation of intervention, and treatment, or rehabilitation for affected workers
Compliance with interventions
We excluded trials that only measured one or more of the secondary outcomes of interest (without measuring our primary outcomes).
Search methods for identification of studies
Electronic searches
We conducted a systematic literature search to identify all published and unpublished trials that could be considered eligible for inclusion in this review. We searched the following electronic databases for identifying potential studies:
Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 8) in the Cochrane Library (searched 22 August 2018; Appendix 1);
MEDLINE PubMed (23 August 2018; Appendix 2);
EMBASE (www.elsevier.com/; 22 August 2018; Appendix 3);
PsycINFO ProQuest (24 August 2018; Appendix 4);
NIOSHTIC and NIOSHTIC‐2, searchable bibliographic databases of occupational safety and health publications, supported in whole or in part by the National Institute for Occupational Safety and Health (NIOSH; OSH‐UPDATE; 24 August 2018; Appendix 5);
HSELINE, database of bibliographic references to published documents on health and safety at work by the Health and Safety Executive (OSH‐UPDATE; 24 August 2018; Appendix 5);
CISDOC, a database by the Health and Safety Information Centre (CIS) of the International Labour Office in Geneva, Switzerland database (OSH‐UPDATE; 24 August 2018; Appendix 5);
ClinicalTrials.gov (clinicaltrials.gov/; 22 August 2018; Appendix 6);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) Search Portal (apps.who.int/trialsearch/; 22 August 2018; Appendix 6).
We searched all databases from their inception to the present, and we imposed no restrictions on language of publication. In future updates, if we identify any potentially eligible papers in languages other than those familiar to the review team, we will either arrange for the translation of key sections prior to assessment, or arrange for their full assessment by people who are proficient in the publications’ language(s).
Searching other resources
We checked reference lists of all articles that we retrieved as full‐text articles, related systematic, and narrative reviews, in order to identify additional potentially eligible studies. We contacted experts in the field, but they were also unable to identify additional unpublished materials.
Data collection and analysis
Selection of studies
Three review authors (PM, VHCW, and JJI) independently screened titles and abstracts of all the potential studies we identified as a result of the search, and coded them as 'retrieve' (eligible or potentially eligible, unclear) or 'do not retrieve'. We coded studies as ’do not retrieve’ if the title and abstract provided sufficient information to decide that the study did not fulfil our inclusion criteria. We excluded studies in this phase only if the study clearly was not randomised or clearly did not assess ergonomic interventions in dental care practitioners.
We retrieved the relevant full‐text study reports or publications. Three review authors (PM, VHCW, and MJH) independently screened the full‐text, and selected studies for inclusion, while identifying and recording reasons for exclusion of the ineligible studies. We resolved all disagreements by mutual discussion. We resolved any unresolved disagreements by consulting the fourth and fifth review authors (ABLA and LK). We identified and excluded duplicates, and collated multiple reports of the same study, so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009) and a 'Characteristics of excluded studies' table.
Data extraction and management
VHCW and MH used Covidence, and PM and JJI used a data extraction form, based on the sample form provided by Cochrane Work, to independently extract study characteristics and outcome data. First, we pilot tested the data extraction form on one included study. Thus, four review authors, in pairs (PM, JJI, VHCW, and MJH), independently extracted the following study characteristics from included studies.
Methods: study design, total duration of study, study location, study setting, withdrawals, and date of study.
Participants: number enrolled, mean age or age range, gender, severity of condition, diagnostic criteria if applicable, inclusion and exclusion criteria.
Interventions: Type, duration, intensity, frequency and content of both intervention and control intervention, and co‐interventions if any.
Outcomes: description of primary and secondary outcomes specified and collected, and time points reported.
Notes: funding for trial, and notable conflicts of interest of trial authors.
We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way. We resolved disagreements by discussion and consensus. Data extraction forms were used to finally collate and compile data extraction findings of all four review authors, particularly since lack of flexibility in customising data entry and editing made Covidence unamenable for this purpose. One review author (JJI) transferred data from data extraction forms into Review Manager 2014, and another review author (PM) double‐checked and made corrections as necessary.
Assessment of risk of bias in included studies
Two review authors (PM and ABLA) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by mutual discussion. We assessed the risk of bias according to the following items:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting;
other bias.
We graded each potential source of bias as high, low, or unclear, and provided a justification in the 'Risk of bias in included studies' section. We considered random sequence generation, allocation concealment, selective outcome reporting, and incomplete outcome data to be key items. We judged a study to have a high overall risk of bias when we judged one or more key items to have a high risk of bias. We considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for musculoskeletal disorder diagnosis may be different than for a self‐reported pain scale). Where information on risk of bias was based on unpublished data or correspondence with an author of a study, we made a note of it in the 'Risk of bias' table. When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Assesment of bias in conducting the systematic review
We conducted the review according to the published protocol (Mulimani 2014). We describe deviations from this in the Differences between protocol and review section.
Measures of treatment effect
We entered the outcome data for each study into the data tables in Review Manager 2014 to calculate the treatment effects. We used relative risks (RRs) for dichotomous outcomes, and mean differences (MDs) for continuous outcomes. We ensured that higher scores for continuous outcomes had the same meaning for the particular outcome, explained the direction to the reader, and reported where the directions were reversed, if this was necessary. We displayed the results in graphs (see Data collection and analysis). In future updates, if we come across any results that cannot be expressed in graphs, we will describe them in the 'Characteristics of included studies' table, or enter the data into 'Additional tables'.
Unit of analysis issues
For studies that used a cluster‐randomised design, and reported sufficient data to be included in the meta‐analysis, but did not make an allowance for the design effect, we calculated the design effect based on a fairly large assumed intra‐cluster correlation of 0.10. We assumed that 0.10 was a realistic estimate, based on studies about implementation research (Campbell 2001). We followed the methods stated in the Cochrane Handbook for Systematic Reviews of Interventions for the calculations (Higgins 2011).
Dealing with missing data
We contacted investigators or study sponsors in order to verify key study characteristics and obtain missing numerical outcome data, where possible. If we can include studies with missing data in future updates of this review and we think the missing data may introduce a serious bias, we will conduct a sensitivity analysis to explore the impact of including these studies in the overall assessment of results.
Where numerical outcome data were missing, such as standard deviations or correlation coefficients, and they could not be obtained from the study authors, we calculated them from other available statistics, such as P values, according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We assessed the clinical homogeneity of the results of included studies, based on similarity of population, intervention, outcome, and follow‐up. We considered populations as similar, based on the nature and type of procedures or work carried out by the practitioners, which would be associated with causing WMSDs in specific areas of the body.
We considered the three ergonomic domains (physical, cognitive and organisational) as dissimilar. However, we considered interventions under each of the ergonomic domains to be similar according to the following criteria.
In the physical domain, we considered interventions similar based on the size of the muscle groups being targeted with the intervention. We considered interventions to be similar if they aimed to improve either overall body posture, or positioning and balance (such as appropriate use of patient and dentist chair, operatory design, workstation layout, dental operatory lighting, magnification devices, visual aids). We also considered interventions targeted at smaller and more intricate muscle groups (such as correct method of instrumentation and tool handling, changing the grip of hand‐held instruments, instrument design factors) to be similar.
In the cognitive domain, we considered interventions similar if they aimed to provide relaxation, improve social interactions and provide support systems, or improve precision skills.
In the organisational domain, we considered interventions similar if they aimed to streamline the organisation of workflow (such as appointment scheduling, patient‐handling system, time management), or were aimed at mobilisation and rest during work (such as stretching, exercising, and mobilising after prolonged static posture, i.e. work‐rest cycles).
We considered all scales measuring pain to be similar (e.g. dichotomy scale (yes, no), Likert scale, visual analogue scale). For measurement of physical disability, we considered all self‐reported or subjective techniques to be similar (e.g. questionnaires), and all objective techniques to be similar (e.g. physical movement, mobility restriction, muscular activity measurement, nerve function). We also considered all methods to record productivity and functioning to be similar (e.g. number of hours worked, patients treated, work days lost, change of job).
We regarded follow‐up times up to six weeks as short‐term, from six weeks to six months as medium‐term, and more than six months as long‐term meaning that we would analyse them separately.
However, the two included studies did not have comparable interventions or duration of follow‐up, so we did not perform a meta‐analysis, or assess heterogeneity.
If we include sufficiently similar studies in future updates of this review to conduct meta‐analyses, we will assess heterogeneity by visual inspection of forest plots, and by using the Chi² and I² statistics for heterogeneity with a statistical significance level of P < 0.10. We will interpret the I² as follows: values ≤ 40% will indicate a low level of heterogeneity, values between 40% and 75% indicate moderate heterogeneity and ≥ 75% will represent very high heterogeneity. If we identify substantial heterogeneity (I² > 50), we will report it, and explore possible causes through subgroup analyses as described in Subgroup analysis and investigation of heterogeneity.
Assessment of reporting biases
We tried to prevent location bias by searching across multiple databases, and language bias by including all eligible articles, regardless of publication language. We did not formally assess publication bias, as there were no comparisons for which we included more than ten studies.
Data synthesis
Since the two included studies were clearly dissimilar with respect to their PICO elements as described above in Assessment of heterogeneity, we did not pool their results. Instead we analysed the results separately for each study, using Review Manager 5 software (Review Manager 2014). In future updates of this review, we will pool data from studies we judge to be clinically homogeneous. If more than one study provides usable data in any single comparison, we will perform a meta‐analysis using a fixed‐effect model. If we find statistical heterogeneity, we will use a random‐effect model to determine differences in results. If we use random‐effect model, in the presence of at least moderate statistical heterogeneity, then we will conduct subgroup analyses, as described below, to investigate the source of heterogeneity (Subgroup analysis and investigation of heterogeneity). We will include 95% CIs for all estimates. We will narratively describe skewed data, reported as medians and interquartile ranges. If multiple trial arms are reported in a single trial, we will include only the relevant arms. If two comparisons are combined in the same meta‐analysis, we will halve the control group to avoid double‐counting.
Quality of the evidence
We used the GRADE approach, as described in the Cochrane Handbook for Systematic Reviews of Interventions, to assess the quality of the body of evidence for the primary outcomes (Higgins 2011). The quality of a body of evidence for a specific outcome is based on five factors: 1) limitations of the study designs; 2) indirectness of evidence; 3) inconsistency of results; 4) imprecision of results; and 5) publication bias. The GRADE approach specifies four levels of quality (high, moderate, low, and very low), incorporating the factors noted above. Quality of evidence by GRADE should be interpreted as follows:
• High‐quality: We are very confident that the true effect lies close to that of the estimate of the effect; • Moderate‐quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; • Low‐quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect; • Very low‐quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
'Summary of findings' table
We created a 'Summary of findings' table that included the primary outcomes:
Number of workers with newly diagnosed WMSD (incident cases);
Self‐reported complaints of pain related to the musculoskeletal system;
Work functioning or disability.
We omitted secondary outcomes from the table, since the primary outcomes sufficiently represented the most compelling issues needed to be addressed by the interventions in this review.
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence generated from our two included studies. We used methods and recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions, using the GRADEpro GDT software (Higgins 2011). We justified all of our decisions to down‐ or up‐grade the quality of studies using footnotes, and we made comments to aid readers' understanding of the review, where necessary.
Subgroup analysis and investigation of heterogeneity
Given the limited number of studies included in this review, we could not perform subgroup analyses. If there are sufficient data in future updates of this review, we will undertake subgroup analyses based on gender, type of setting or practice (e.g. small, large, individual, group, hospital), and number of work hours.
Sensitivity analysis
We had planned to perform a sensitivity analysis to investigate whether our findings could be affected by the high risk of bias of some of the included studies. However, since we were unable to pool results from the studies, the need to perform a sensitivity analysis did not arise. Given there is sufficient data in future updates of this review, we will conduct a sensitivity analysis by including only high quality studies. We will define 'high quality' as studies having adequate random sequence generation and allocation concealment, and they report less than 20% of their data being missing , given the stated importance of attrition as a quality measure. We will consider only the primary outcome in the sensitivity analyses. If we identify statistical heterogeneity in our analyses, we will also pursue sensitivity analyses to explore the differences in results obtained from a fixed‐effect versus a random‐effects model.
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of included studies for this review. We avoided making recommendations for practice based on more than just the evidence, such as values and available resources. Our implications for research suggest priorities for future research, and outline what the remaining uncertainties are in the area.
Results
Description of studies
Results of the search
Our searches of databases and clinical trial registries identified 946 potentially relevant references, after we removed duplicates. Three review authors (PM, VCWH, and JJI) assessed the titles, keywords, and abstracts of these references, and identified 17 studies and three registered trials as potentially eligible. We obtained the full‐text publications for the 17 studies, and abstracts of the three ongoing trials (IRCT2016062128529N2; IRCT2014051117649N1; IRCT2015113024199N2).
We did not identify any additional references by searching the following databases: the NIOSHTIC, NIOSHTIC‐2, CISDOC, and HSELINE.
We checked the reference lists of all articles that we retrieved as full‐text papers, in an attempt to identify potentially eligible studies. We did not identify any additional studies through this approach. Of the 17 studies we considered, we included two in the review. Of the three ongoing studies assessed, we excluded one study, and we are still waiting for additional information from the researchers of two ongoing studies (IRCT2014051117649N1; IRCT2015113024199N2), which we have therefore categorized under “Studies awaiting classification”. To summarise, out of a total of 20 potentially eligible studies assessed, we excluded 16, two are awaiting classification, and we included two (see Figure 1 for the PRISMA study flow diagram).
1.
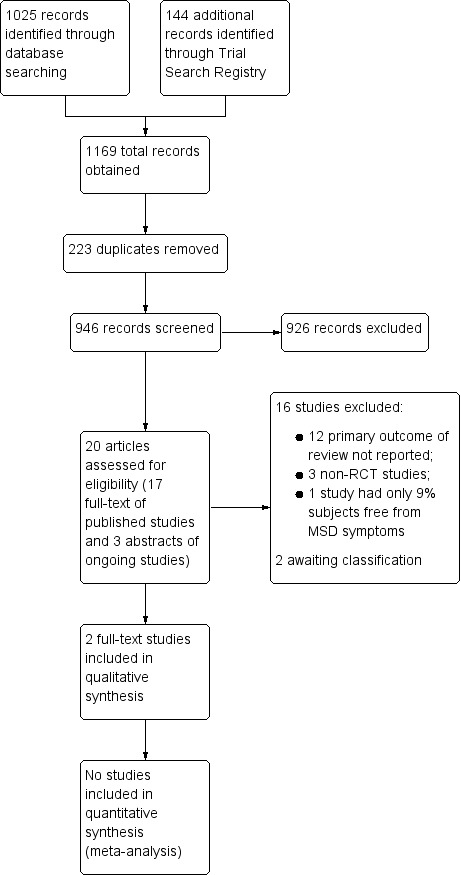
PRISMA study flow diagram
We wrote to the authors of one published study (von Thiele Schwarz 2008), and three ongoing clinical trials to get additional data (IRCT2014051117649N1; IRCT2016062128529N2; IRCT2015113024199N2). We received a response from the authors of IRCT2016062128529N2 and von Thiele Schwarz 2008, based on which we decided to exclude these studies.
Included studies
We included two studies, consisting of a total of 212 participants, both of which assessed physical ergonomic interventions (Dehghan 2016; Rempel 2012). We did not find any studies that evaluated either cognitive or organisational ergonomic interventions.
One of the included studies was cluster‐randomised (Rempel 2012). In order to evaluate the design effect (DEFF) on analyses, we re‐analysed the sample size, taking into account the intracluster correlation (ICC) and adjusting the sample size accordingly. We calculated the DEFF, based on an assumed ICC of 0.10. We used the formula 1 + (M −1)x ICC to calculate the design effect, where M is the average cluster size that results from dividing the total number of study participants by the number of units of randomisation or clusters. In this case, the design effect was 1.02. After adjusting for the design effect from clustering, the sample size was reduced to 210. For further details regarding these studies, see "Characteristics of included studies"
Location and settings
Dehghan 2016 was conducted among dentists working in the dentistry clinics of Tehran's hospitals in Iran; Rempel 2012 was carried out in the United States, and recruited private practitioners from dental offices in the San Francisco Bay area.
Types of participants
Dehghan 2016 recruited 102 dentists residing in Tehran, who were willing to fully participate in the study, and avoid using analgesics during the course of the study. Dentists with a history of spinal surgery, and pregnant females were excluded. The mean age was 39.82 ± 4.61 (mean ± SD) years in the intervention group, and 40.01 ± 4.12 years in the control group. Ratio of males to females was not reported. At baseline, the number of participants free from MSD symptoms in the thighs were 82% in the control group and 84% in the intervention group; for feet, there were 75% MSD symptom‐free in the control group and 76% in the intervention group. Less than 75% of the participants were free from MSDs in the knee, back, wrist, arm, shoulder and neck, hence, we did not assess outcomes for these parts in the current review on prevention.
Rempel 2012 included 110 dental hygienists and dentists, by selecting those who performed scaling, root planing, or teeth cleaning for more than 10 hours per week, and had been doing this work for more than one year. They excluded those who were receiving care from a physician for treatment of an upper‐extremity disorder. Out of the 110 participants, 10 were male and 100 were female, they were 44.7 ± 10.4 (mean ± SD) years, and their ethnicity was: Asian or Pacific Islander (23), African American, not of Hispanic origin (3), Hispanic (11), White, not of Hispanic origin (68), and other (5). After we adjusted for the cluster design effect with a DEFF of 1.02, the sample size reduced in the intervention group (light, wide instrument), from 54 to 53; in the control group (heavy, narrow instrument), from 56 to 55; and in total, from 110 to 108.
For the shoulder region, 91.1% in the heavy and narrow curette group, and 81.5 % in the light and wide curette group were free from MSD symptoms; for the elbow and forearm area, the figures were 87.5% in the heavy and narrow curette group, and 83.3% in the light and wide curette group. Only 73.2% of participants were symptom‐free in the hand and wrist region, so we did not assess outcomes for this region.
Types of interventions
Physical ergonomic interventions
Interventions targeting muscles for posture and balance were assessed in the Dehghan 2016 study for six months post‐intervention. The intervention group (N = 52) completed an eight‐week multi‐faceted ergonomic intervention, involving four key components of 1) Knowledge and training about ergonomics; 2) Work station modification; 3) Training and surveying ergonomics at the work station; and 4) A regular exercise program. Dentists in the control group (N = 50) did not receive any interventions.
Interventions targeting finer muscles involved in instrumentation were evaluated in the Rempel 2012 study by randomly assigning participants to work with one of two types of custom‐made periodontal instruments: instrument one was made from black plastic (acetal resin, Delrin, DuPont, Wilmington, Del.), weighed 14 g, and had an 11 mm diameter handle (N = 54); instrument two was made from steel, plated with black coating, weighed 34 g, and had an 8 mm diameter handle (N = 56). The instruments were surfaced with a medium diamond texture, and fitted with an R3S and an R4S tip (Ratcliff stainless steel universal scalers, G. Hartzell & Son, Concord, Calif.). Instrument weights and handle diameters were designed to provide a practical range that would have an effect on pinch force, based on results of previous laboratory studies. Participants were required to use the periodontal instruments in practice for a period of 16 weeks.
Cognitive ergonomic interventions
We found no studies that evaluated the effectiveness of cognitive ergonomic interventions.
Organisational ergonomic interventions
We found no studies that evaluated the effectiveness of organisational ergonomic interventions.
Types of Outcomes
Dehghan 2016 measured musculoskeletal pain at various locations in the body, by using the Nordic Musculoskeletal Questionnaire at baseline, three months, and six months.
Rempel 2012 collected self‐reported mean pain score of the right wrist, elbow, and shoulder weekly, using an online questionnaire, beginning one month before the start of the intervention, until the end of the intervention at 16 weeks. They also recorded the number of hours during the week that the participant performed different dental tasks; the number of nights during which they awakened with numbness in the right thumb, index finger, or middle finger; and the number of days during which the participant used pain medication for right upper extremity symptoms. Although the secondary outcome of numbness was relevant for our review, we decided not to include it, because the way this outcome was reported and assessed, was more in line with treatment than prevention of musculoskeletal disorders. The secondary outcome of compliance was also documented by participants self‐reporting that they used the allocated instruments approximately 82% of the time during scaling and root planing procedures.
Overall, we analysed data from 212 participants (210 after adjusting sample size) from these two studies for self‐reported pain, out of which, on average, 82.6% were free from MSD (range = 75% to 91.1%) at baseline.
Excluded studies
We excluded a total of 16 studies (including one ongoing study), primarily for three reasons: not reporting primary outcomes of the review, using non‐RCT designs, or having less than 75% participants free from MSD at baseline. We excluded twelve studies for failing to report any of the primary outcomes, i.e. physician‐diagnosed musculoskeletal disorder, self‐reported pain, or disability. These studies measured posture differences or improvements (Branson 2004; Maillet 2008; Ouivirach 2014; Thanathornwong 2014; Thanathornwong 2015); muscle activity (Cosaboom‐FitzSimons 2008; McCombs 2014; Simmer‐Beck 2006; grip strength (James 2010); body inclinations, perceived exertion, and discomfort (Lindegård 2012); and tactile sensitivity or discrimination (Ryan 2005; Simmer‐Beck 2007), which were not our primary outcome of interest. Three studies were non‐RCT (including one ongoing study) (Aghilinejad 2016; Hayes 2014b; IRCT2016062128529N2), and one study had only 9% participants free from MSD at baseline (von Thiele Schwarz 2008).
Risk of bias in included studies
Of the two included studies, we judged Dehghan 2016 to be at high risk, and Rempel 2012 to be at unclear risk. For the judgement of unclear risk of bias due to lack of reporting, we did not seek additional information from trial authors due to resource and time concerns. Instead, we completed the "Risk of Bias" assessment based on existing information in the published reports. The results are summarised in Figure 2, which shows review authors' judgements about each 'Risk of bias' item for each included study. Figure 3 shows review authors' judgements about each risk of bias item, presented as percentages across all included studies.
2.
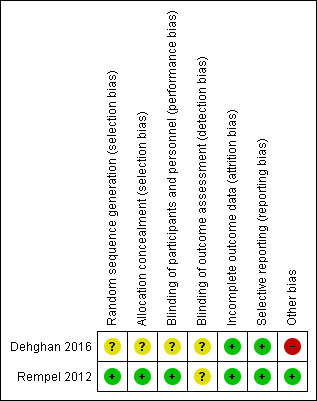
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
3.
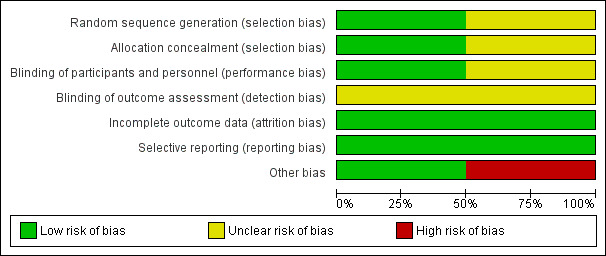
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
Both included trials reported the use of randomisation techniques. However, only Rempel 2012 provided further details of the technique used, and hence, we judged it as having a low risk of bias. We rated Dehghan 2016 as having an unclear risk of bias, due to lack of information. Only Rempel 2012 reported adequate allocation concealment, and we judged it as having a low risk of bias. Dehghan 2016 did not describe the method of allocation concealment and so we judged it as having an unclear risk of bias.
Blinding
Dehghan 2016 did not report details of the blinding procedure. Hence we categorised it as having an unclear risk of bias. Whereas Rempel 2012 reported blinding participants and personnel, and so we rated it as having a low risk of bias.
Since both studies used self‐reported outcome measures, the participants were themselves the outcome assessors, and thus impossible to blind. Since it was not possible to say whether this self‐reporting led participants to report effects of interventions favourably or unfavourably, we assigned an unclear risk of bias judgement for the domain of detection bias.
Incomplete outcome data
We judged both studies to be at low risk of attrition bias. Dehghan 2016 indicated that all 102 participants completed the study, whereas Rempel 2012 accounted for dropouts, and performed an intention‐to‐treat (ITT) analysis.
Selective reporting
We categorised both studies as having a low risk of reporting bias since all outcomes in the objectives of these trials were analysed and presented in the results section.
Other potential sources of bias
We found serious errors in the choice of statistical tests used to assess data in Dehghan 2016. In the text, they stated that they used a paired t‐test to compare differences in prevalence and in the data tables they stated that they used repeated measures ANOVA. . As these were dichotomous data, the authors should have used Chi² or logistic regression for the categorical outcome variables they measured in this study (prevalence of musculoskeletal disorders requiring a yes or no response), Consequently, the results and conclusions they reported are incorrectand so we classified this as an additional high risk of bias.
We detected no other potential source of bias in Rempel 2012.
Effects of interventions
Physical ergonomic interventions
1. Multi‐faceted ergonomic intervention compared to no intervention
Dehghan 2016 studied the effects of an eight‐week multi‐faceted intervention program over a period of six months. One of our inclusion criterion was that at baseline, 75% of participants had to be free from MSD. Since this criterion was fulfilled only by participants with thigh and foot MSD, we excluded outcome data related to other body parts.
We found that a multi‐faceted ergonomic intervention had no clear effect on the risk of WMSD in the thighs (risk ratio (RR) 0.57, 95% confidence interval (CI) 0.23 to 1.42; 102 participants; Analysis 1.1), or the feet (RR 0.64, 95% CI 0.29 to 1.41; 102 participants; Analysis 1.2) when compared to no intervention.
1.1. Analysis.
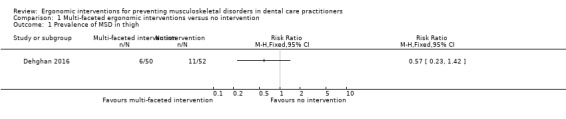
Comparison 1 Multi‐faceted ergonomic interventions versus no intervention, Outcome 1 Prevalence of MSD in thigh.
1.2. Analysis.
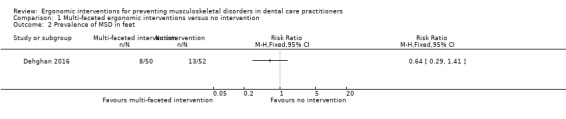
Comparison 1 Multi‐faceted ergonomic interventions versus no intervention, Outcome 2 Prevalence of MSD in feet.
2. Light weight and wide handled instruments compared to heavy weight and narrow handled instruments for scaling
Rempel 2012 evaluated the effects of a change in instrument design for a period of 16 weeks. We only included the measurements for elbow or forearm and shoulder pain from this study, since 75% of these participants were free from MSD at baseline. There was no clear difference in mean pain scores between participants using the lighter instrument with a wider handle and those using the heavier instrument with a narrower handle (elbow pain mean difference (MD) −0.14, 95% CI −0.39 to 0.11; 110 participants; Analysis 2.1; shoulder pain MD −0.32, 95% CI −0.75 to 0.11; 110 participants; Analysis 2.2). When change score (post‐intervention pain score minus pre‐intervention pain score) was positive, it indicated a decrease in pain. Mean difference (MD) was measured as change score with heavy instrument usage minus change score with light instrument usage. Therefore, a negative MD indicated a decrease in pain when participants used the lighter, wider handled instrument.
2.1. Analysis.

Comparison 2 Light instrument (curette) with wide handle versus heavy curette with narrow handle, Outcome 1 Self‐reported pain in right elbow, forearm.
2.2. Analysis.

Comparison 2 Light instrument (curette) with wide handle versus heavy curette with narrow handle, Outcome 2 Self‐reported pain in right shoulder.
Cognitive ergonomic interventions
We found no studies that evaluated the effectiveness of cognitive ergonomic interventions.
Organisational ergonomic interventions
We found no studies that evaluated the effectiveness of organisational ergonomic interventions.
Discussion
Summary of main results
We included one parallel‐arm and one cluster‐randomised controlled trial (RCT) in this review, both of which assessed physical ergonomic interventions for preventing work‐related musculoskeletal disorders (WMSD) in dental care practitioners. There is very low‐quality evidence from one trial, conducted with 102 dentists, showing that a multi‐faceted ergonomic intervention with modules on ergonomic awareness, training, workstation layout modifications, posture correction during working, and physical exercise has no clear effect on the prevalence of WMSD in thighs and feet over a six‐month period, when compared to no intervention. There is also low‐quality evidence from another single trial, conducted with 110 dentists and dental hygienists, showing that using instruments with lighter weight and a wider diameter handle for scaling have no clear effect on mean elbow or shoulder pain scores, when compared to instruments of heavier weight and with a narrower handle, over a 16‐week period.
We found no studies assessing the effectiveness of cognitive or organisational ergonomic interventions.
Overall completeness and applicability of evidence
We searched the literature extensively for this review, without language or date restrictions. We strictly applied appropriate inclusion and exclusion criteria to filter the studies that truly addressed the review question. Hence, we believe the results of our review represent the best evidence currently available for assessing ergonomic interventions for prevention of WMSDs among dental care practitioners.
Since the interventions and outcomes in both included studies were dissimilar, we were unable to combine them in a meta‐analysis. For the work‐related musculoskeletal disorder (WMSD) outcomes in both studies, we only included results of measurements where 75% or more participants were free from any symptoms of MSD at baseline, since our goal was to assess the effectiveness of prevention, not treatment.
Physical ergonomic interventions
The study by Dehghan 2016 found that a multi‐faceted ergonomic intervention program that included modules on ergonomic awareness, training, workstation layout modifications, posture correction during working, and physical exercise did not successfully prevent WMSDs in thighs and feet among dentists. A possible explanation for the lack of effect is that the trialists banded many interventions together, and they did not report compliance. Given that WMSDs among dental care practitioners are most prevalent in the neck, shoulder, lower back, and wrists or hands, we were unclear why this study decided to assess WMSDs in thighs, knees, and feet as well. We judged this study to be at high risk of bias, due to its flawed methodology and questionable use of statistics in their data analysis.
Rempel 2012, the cluster‐randomised study, compared the effectiveness of using lighter instruments with wider handles with heavier instruments and narrower handles, in reducing arm and shoulder WMSDs. The results showed no clear difference between the two kinds of instruments. However, the study's follow‐up time was only four months; longer‐term data would have helped us to draw better conclusions.
Based on these findings, the use of multi‐faceted ergonomic interventions or differently designed instruments by dental care practitioners in day‐to‐day practice to prevent WMSDs, can neither be dismissed nor validated. Studies that are methodologically sound and assess longer follow‐up times, which investigate the effects of individual interventions on areas that are at the highest at risk for WMSDs, are necessary to determine the effectiveness of these interventions with more clarity and accuracy.
Cognitive ergonomic interventions
Ergonomic interventions in the cognitive domain include measures, such as stress management and relaxation techniques, improving communication with co‐workers and patients, support systems to handle family‐work conflicts, training to master precision skills, prioritisation of operator preferences, role‐designation to increase job satisfaction. We found no studies that evaluated any of these interventions, which highlights the need to generate research in this area.
Organisational ergonomic interventions
Clinical experts have theorised that ergonomic interventions in this domain, such as organisation of workflow, appointment scheduling, patient‐management system, pace and variety of workload, sequence and administration of procedures, taking breaks, stretching, exercising and mobilising after prolonged static posture, assistant support, task rotation, work‐rest cycles, and time management could prevent WMSDs by reducing stress resulting from repetitive procedures and tasks. In our full‐text screening, we found one study by von Thiele Schwarz 2008, which assessed an intervention in this domain in female dental employees in Sweden, but we excluded it since only 9% of the participants were free from MSD at baseline. The paucity of studies highlights the need to generate research in this area.
Quality of the evidence
We included two studies in our review, both of which assessed interventions in the physical ergonomic domain; one by combining multiple interventions, and another by evaluating instrument features best suited for reducing musculoskeletal strain while performing scaling. We were unable to combine the results of these studies, due to diverse interventions and outcomes. We assessed the quality of evidence for each outcome using the GRADE criteria and GRADEpro GDT software.
Very low‐quality evidence, provided by Dehghan 2016, shows that a multi‐faceted ergonomic intervention leads to no significant difference in WMSDs in the thighs and feet, when compared to no intervention. We downgraded our assessment of the quality of the evidence by one level due to risks of bias evident in several methodological issues including: the lack of reporting of sequence generation, allocation concealment, blinding of participants and assessors, small sample size, inappropriate use of statistical tests and calculations, and failure to account for possible confounding factors in their follow‐up data. We downgraded the quality of evidence by another level for imprecision arising from the small sample size. We downgraded the quality of evidence by yet another level due to indirectness, since we were only able to include data from measurements pertaining to thighs and feet, since only participants for these outcomes met the inclusion criteria, rather than data for the neck, shoulder, lower back, and wrists or hands, which are considered to be the most common sites of WMSD in dentistry.
Low‐quality evidence, provided by Rempel 2012, shows no significant difference in reported pain in elbows or shoulders when using lighter instruments with wider handles, compared to heavier instruments with narrower handles. Overall, this study had sound methodology, but we downgraded the quality of evidence two levels; one level because of the unclear risk of bias following the use of a self‐reported outcome for the assessment of WMSDs, and one level for imprecision, because there was only a single study with a small sample size.
Potential biases in the review process
We conducted our review in a comprehensive manner, based on the peer‐reviewed and pre‐approved exhaustive methodology laid out in our protocol to eliminate arbitrariness or bias (Mulimani 2014). Three or four review authors independently carried out the important steps of the review, such as study selection, data extraction, and assessment of risk of bias; they resolved disagreements through discussion and consensus decision‐making. We carried out a comprehensive search strategy without restrictions on time and language, screened the references of identified trials, and contacted experts in the field of research. Nothwithstanding the thoroughness of the search, there still exists the risk that we may have inadvertently missed relevant studies for our review.
To strengthen the quality of evidence, we only included RCTs, and eliminated other study designs which are less methodologically rigorous and prone to bias. We only included RCTs if they had 75% of participants or more free from MSDs at baseline. For example, we excluded the study by von Thiele Schwarz 2008, since only 9% of the participants were free from MSD at baseline. We only included studies that measured one of the three primary outcomes, so the included studies were truly reflective of their potential to counter real‐life occurrence of WMSDs. As a result, we eliminated a large number of studies that reported secondary outcomes of interest, but not primary outcomes. We rejected twelve of the fourteen excluded studies for this reason, since they measured surrogate outcomes like body inclination, posture, muscle strength, muscle activity, and tactile sensations, and did not directly assess the WMSD outcomes in practitioners. These strict criteria significantly reduced the number of studies we could include in our review, but were necessary to stay true to the objectives of the review question.
Agreements and disagreements with other studies or reviews
Most reviews in this area have been non‐systematic and narrative in nature, mainly detailing the prevalence of WMSDs in various populations, or probable risk factors, causative mechanisms, and anecdotal suggestions or proposals for implementing ergonomic interventions (Gupta 2014; Khalekar 2016; Pirvu 2014; Sakzewski 2014). An umbrella review; 'Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment' assessed these reviews (De Sio 2018). It included 29 studies: 16 narrative reviews and 13 original articles. Of the original articles, 10 were cross‐sectional studies, two were clinical trials, and one was a case study. The inclusion criteria for this review were non‐specific; "articles included in this review focus on disorders related to ergonomics, and on the most effective preventive measures adopted in the dental profession" (De Sio 2018). The authors did not define, and hence did not apply the parameters that would make a study 'preventive'. The two clinical trials included in the review were non‐randomised, and measured a surrogate posture outcome in dental students, using ergonomically designed dental chairs. Based on their included narrative reviews and non‐randomised study designs, this umbrella review's results stated that 75% of the reviews highlighted the importance of stretching after each working session and at the end of the working day, while 61.5% of the original articles emphasised the use of modern and ergonomic instruments.
Since our review includes only RCTs, it would not be appropriate to compare our results with this umbrella review, whose conclusions were based on other study designs and reviews.
Authors' conclusions
Implications for practice.
Currently, there is insufficient evidence to conclude whether ergonomic interventions in the physical domain are effective in preventing musculoskeletal disorders among dental care practitioners.
There is very low‐quality evidence, provided by one study, indicating that a multi‐faceted ergonomic intervention has no clear effect on musculoskeletal pain in the thighs and feet.
There is low quality evidence, provided by another study, showing that changing instrument weight and handle size for scaling has no clear effect on pain in the elbows or shoulders.
Considering the methodological flaws and high risk of bias of the first study, and short follow‐up period and unclear risk of bias of the second study, we could not draw any reliable conclusions, or make recommendations for practice.
There is no evidence available to determine effectiveness of ergonomic interventions in the cognitive and organisational domains. Future studies will very likely affect the conclusions of this review.
Implications for research.
Given that this review identified only two studies – one with high and another with unclear risk of bias – both of which assessed the effectiveness of physical ergonomics interventions, there is a clear need for high‐quality randomised controlled trials (RCTs) that examine the effectiveness of ergonomic interventions in all three ergonomics domains: physical, cognitive and organisational, in the prevention of work‐related musculoskeletal disorders (WMSDs) among dental care practitioners.
Participants. Future studies should have sufficient numbers of participants to detect statistically significant differences. Sample size determination for these trials should be based on Type 1 error (alpha value), adequate power (probability of correctly rejecting null hypothesis), and expected effect size acquired from previous literature. For example, to assess the prevalence of WMSD related to intervention effects would require a sample size of 369, at 5% width of a 95% confidence interval, assuming the expected prevalence was an average of 60%, based on values seen in the literature. To detect a 0.5 unit change in mean pain score with a standard deviation of 1.5, would need a total sample size of 284, with 142 for each arm of the study. As there are no trials of cognitive and organisational ergonomics interventions, researchers undertaking such studies may need to conduct initial pilot studies to acquire the effect size needed to estimate the final sample size for the larger parent projects.
From the outset, studies should be clear whether they are testing interventions for prevention or treatment. Prevention studies should recruit participants with minimum (not more than 25%, as a rough guideline) to no baseline MSD levels, and studies assessing treatment should include not less than 75% of participants with MSDs. As we explained in the background of our review, the occurrence of WMSDs in dental practitioners is a function of: gender, age, sitting or standing position of practice, posture, use of assistants, number of work hours per day, number of years worked, intensity of work done, force used, nature of procedures carried out, type of instruments, work‐rest cycles, office design, equipment used, organisational set‐up, stress, work environment, and pre‐disposing factors like weight, smoking, physical fitness, and pre‐existing systemic conditions. These participant attributes should be matched across experimental and control groups, in order to generate comparable and meaningful results. The best way to achieve this could be stratified randomisation, adjusting for stratification factors instead of simple randomisation. Conducting multiple‐centre studies, in both high‐ and low‐income countries, will further increase the usefulness of the findings.
Interventions. Instead of grouping interventions as an intervention unit, a better understanding of intervention effects could be obtained by assessing individual interventions over longer follow‐up times. We found no studies that assessed the effectiveness of cognitive or organisational interventions, and these need to be planned in the future. These must include trials to evaluate cognitive interventions such as: stress management and relaxation techniques, improving communication with co‐workers and patients, support systems to handle family‐work conflicts, training to master precision skills, prioritisation of operator preferences, role designation to increase job satisfaction, and organisational ergonomic interventions like: organisation of workflow, appointment scheduling, patient‐management system, pace and variety of workload, sequence and administration of procedures, taking breaks, stretching, exercising and mobilising after prolonged static posture, assistant support, task rotation, work‐rest cycles, and time management.
Comparisons. Interventions of the same domain, and within the domain, of similar types, should be compared with each other. For example, in the physical domain, comparisons can be made between interventions aimed at improving overall body posture or aimed at positioning and balance (such as appropriate use of patient and dentist chair, operatory design, workstation layout, dental operatory lighting, magnification devices, visual aids), or those targeting smaller and more intricate muscle groups (such as correct method of instrumentation and tool handling, changing the grip of hand‐held instruments, or instrument design factors). Within the cognitive domain, comparisons could be made between interventions aiming to provide relaxation, or between interventions aimed at improving social interactions and providing support systems, or between interventions aimed at improving precision skills. In the organisational domain, comparisons could be drawn between interventions aimed at streamlining organisation of workflow (such as appointment scheduling, patient‐handling system, time management), or between interventions aimed at mobilisation and rest during work (such as stretching, exercising and mobilising after prolonged static posture, or work‐rest cycles).
Outcomes. Objective measures to diagnose WMSDs are better than self‐assessments. Future studies might consider including independent medical examinations for diagnosis, or other institutional or workplace injury reporting systems as objective measures. Workers' compensation records can indicate number of hours lost due to WMSD, but it has to be borne in mind that not all workers may report WMSD or claim compensation for it, especially if they are self‐employed. We excluded many studies on ergonomic interventions, since they assessed surrogate outcomes, like grip strength, muscle activity, tactile discrimination, posture, tilt angle of body, neck and back extensions, or kinematics, instead of measuring the real clinical manifestation of a musculoskeletal disorder. A surrogate end point, or marker, has been defined as a laboratory measurement or physical sign that is used in therapeutic trials as a substitute for a clinically meaningful end point that is a direct measure of how a patient feels, functions, or survives, and that is expected to predict the effect of the therapy (Twadell 2009). Since surrogate outcomes do provide a good objective assessment of risk factors, it is important to first establish the validity of these outcome measures in predicting or representing the WMSD, through extensive research, and only then use them as authentic predictors of WMSDs. Until that time, we recommend that future studies use direct measurement of resulting WMSD, instead of measuring surrogate outcomes, to provide more meaningful results.
Appropriate randomisation methodology, with sequence generation, allocation concealment, and blinding should be executed and reported. The main risk for bias we identified in this review was blinding (performance and detection bias). Although blinding of participants and personnel (performance bias) is difficult to achieve for ergonomic interventions, researchers should consider minimising detection bias, by having independent, blinded assessors diagnosing upper limb and neck WMSDs. Trialists should also include objective measures to monitor compliance.
Acknowledgements
We thank Jani Ruotsalainen, Managing Editor, Cochrane Work Group for providing administrative and logistical support for the conduct of this review, and Leena Isotalo, Information Specialist, Cochrane Work Group for developing and testing the search strategies for our protocol.
We would also like to thank the Cochrane Work Group's Co‐ordinating Editor, Jos Verbeek, Editors Esa‐Pekka Takala and Wim van Veelen, and external peer referee Erja Sormunen, for their comments on the protocol. We also thank Managing Editor, Jani Ruotsalainen, Editor Esa‐Pekka Takala, and external peer referees Arianne Verhagen, Erja Sormunen, and Giovanni Lodi for their comments on the review. We thank Joey Kwong for copy editing the protocol, and Victoria Pennick for copy editing the review.
We thank Dr. Sumanth Nagraj, Professor and Head of Department of Oral Medicine and Radiology, Melaka Manipal Medical College, and Clinical Editor of the Cochrane Oral Health group, for his valuable advice and input in carrying out this review, and for carrying out part of the search for studies. We also thank the institutional support and encouragement we received from Melaka‐Manipal Medical College to enable us to write this review.
Appendices
Appendix 1. CENTRAL search strategy
(2018, Issue 7. the Cochrane Library) #1 MeSH descriptor: ["Dentists"] explode all trees (159) #2 "dental profession*":ti,ab OR "dental hygienist*":ti,ab OR dentist*:ti,ab OR "dental care personnel":ti,ab OR "dental assistant*":ti,ab OR "dental therapist*":ti,ab OR "oral health therapist*":ti,ab OR "dental student*":ti,ab OR "dental hygiene student*":ti,ab OR (("oral health care":ti,ab) AND (personnel:ti,ab OR practitioner*:ti,ab OR student*:ti,ab)) (2142) #3 #1 OR #2 (2218) #4MeSH descriptor: ["Human Engineering"] explode all trees (65968) #5 biomechanic*:ti,ab OR "ergonomic intervention*":ti,ab OR "ergonomic design*":ti,ab OR "ergonomic training":ti,ab OR ergonomic*:ti,ab OR "dental office design":ti,ab OR "work station design":ti,ab OR "office layout":ti,ab OR "job posture*":ti,ab OR "work posture*":ti,ab OR "working posture*":ti,ab OR position*:ti,ab OR "rest period*":ti,ab OR "taking break*":ti,ab OR "work schedul*":ti,ab OR "workplace practic*":ti,ab OR lighting:ti,ab OR magnification*:ti,ab OR "patient chair":ti,ab OR "dental chair*":ti,ab OR ((chair:ti,ab OR chairs:ti,ab OR furnish*:ti,ab OR furniture:ti,ab OR tool*:ti,ab OR equipment*:ti,ab OR instrument*:ti,ab) AND (ergon*:ti,ab OR design*:ti,ab)) OR exercise*:ti,ab OR "physical fitness*":ti,ab OR "stress management":ti,ab OR "human factor*":ti,ab (92918) #6 #4 OR #5 (132683) #7 MeSH descriptor: ["Cumulative Trauma Disorders"] explode all trees (52200) #8 "occupational overuse syndrome":ti,ab OR "tension neck syndrome":ti,ab OR "tension neck":ti,ab OR "work related":ti,ab OR "cumulative trauma*":ti,ab OR ((repetiti*:ti,ab) AND (strain:ti,ab OR stress:ti,ab OR motion:ti,ab OR movement:ti,ab) AND (injur*:ti,ab OR disorder*:ti,ab)) OR "musculoskeletal disorder*":ti,ab OR "carpal tunnel syndrome":ti,ab OR "back pain":ti,ab OR discomfort:ti,ab (20298) #9 #7 OR #8 (67376) #10 #3 AND #6 AND #9 (57)
Appendix 2. MEDLINE search strategy
| Steps | Strategy | Hits | Time |
| #15 | Search (#12) OR #14 | 515 | 03:31:10 |
| #14 | Search (#10) AND #13 | 466 | 03:21:17 |
| #13 | Search ((effect*[Text Word]) OR (control[Text Word]) OR (controls*[Text Word]) OR (controla*[Text Word]) OR (controle*[Text Word]) OR (controli*[Text Word]) OR (controll*[Text Word]) OR (evaluation*[Text Word]) OR (program*[Text Word])) AND ((work[Text Word]) OR (works*[Text Word]) OR (work'*[Text Word]) OR (worka*[Text Word]) OR (worke*[Text Word]) OR (workg*[Text Word]) OR (worki*[Text Word]) OR (workl*[Text Word]) OR (workp*[Text Word]) OR (occupation*[Text Word]) OR (prevention*[Text Word]) OR (protect*[Text Word])) | 2433683 | 03:20:57 |
| #12 | Search (#10) AND #11 | 123 | 03:20:35 |
| #11 | Search ((((((((randomized controlled trial[Publication Type]) OR controlled clinical trial[Publication Type]) OR randomized[Title/Abstract]) OR placebo[Title/Abstract]) OR drug therapy[MeSH Subheading]) OR randomly[Title/Abstract]) OR trial[Title/Abstract]) OR groups[Title/Abstract]) NOT (("animals"[MeSH Terms]) NOT ("humans"[MeSH Terms])) | 3739120 | 03:20:06 |
| #10 | Search ((#3) AND #6) AND #9 | 786 | 03:19:29 |
| #9 | Search (#7) OR #8 | 577625 | 03:19:07 |
| #8 | Search ((((((((occupational overuse syndrome[Text Word]) OR tension neck syndrome[Text Word]) OR work related[Text Word]) OR cumulative trauma*[Text Word]) OR ((repetiti*) AND (strain OR stress OR motion OR movement) AND (injur* OR disorder*)) OR musculoskeletal disorder*[Text Word]) OR carpal tunnel syndrome[Text Word]) OR back pain[Text Word]) OR discomfort[Text Word]) | 128596 | 03:18:49 |
| #7 | Search (((((((((((((("cumulative trauma disorders"[MeSH Terms]) OR "occupational diseases"[MeSH:noexp]) OR "occupational health"[MeSH Terms]) OR "musculoskeletal diseases"[MeSH:noexp]) OR "back pain"[MeSH Terms]) OR "neck pain"[MeSH Terms]) OR "shoulder pain"[MeSH Terms]) OR "musculoskeletal pain"[MeSH Terms]) OR "hand injuries"[MeSH Terms]) OR "wrist injuries"[MeSH Terms]) OR "arm injuries"[MeSH Terms]) OR "upper extremity"[MeSH Terms]) OR "lower extremity"[MeSH Terms]) OR "back injuries"[MeSH Terms]) OR "carpal tunnel syndrome"[MeSH Terms] | 507588 | 03:18:12 |
| #6 | Search (#4) OR #5 | 1788923 | 03:17:46 |
| #5 | Search (((((((((((((((((((((((biomechanics[Text Word]) OR ergonomic intervention*[Text Word]) OR ergonomic design*[Text Word]) OR ergonomic training[Text Word]) OR ergonomics[Text Word]) OR dental office design[Text Word]) OR work station design[Text Word]) OR office layout[Text Word]) OR job posture*[Text Word]) OR work posture*[Text Word]) OR working posture*[Text Word]) OR position[Text Word]) OR rest period*[Text Word]) OR taking break*[Text Word]) OR work schedul*[Text Word]) OR workplace practic*[Text Word]) OR lighting[Text Word]) OR magnification*[Text Word]) OR patient chair[Text Word]) OR dental chair*[Text Word]) OR (((chair[Text Word]) OR (chairs[Text Word]) OR (furnish*[Text Word]) OR (furniture[Text Word]) OR (tool*[Text Word]) OR (equipment*[Text Word]) OR (instrument*[Text Word])) AND (ergon* OR design*)) OR exercise*[Text Word]) OR physical fitness*[Text Word]) OR stress management[Text Word]) OR human factors[Text Word] | 1118313 | 03:17:21 |
| #4 | Search ((((((((((("human engineering"[MeSH Terms]) OR "posture"[MeSH:noexp]) OR "movement"[MeSH:noexp]) OR "mechanics"[MeSH Terms]) OR "instrumentation"[MeSH Subheading]) OR "equipment design"[MeSH:noexp]) OR "user computer interface"[MeSH Terms]) OR "workload"[MeSH Terms]) OR "workplace"[MeSH Terms]) OR "exercise"[MeSH Terms]) OR "exercise movement techniques"[MeSH Terms]) OR "physical therapy modalities"[MeSH Terms] | 1097658 | 03:16:27 |
| #3 | Search (#1) OR #2 | 136614 | 03:16:01 |
| #2 | Search (((((((((dental profession*[Text Word]) OR dental hygienist*[Text Word]) OR dentist*[Text Word]) OR dental care personnel[Text Word]) OR dental assistant*[Text Word]) OR dental therapist*[Text Word]) OR oral health therapist*[Text Word]) OR dental student*[Text Word]) OR dental hygiene students*[Text Word]) OR ((oral health care[Text Word]) AND (personnel OR practitioner* OR student*)) | 133188 | 03:15:32 |
| #1 | Search (("dentists"[MeSH Terms]) OR "dental staff"[MeSH Terms]) OR "dental auxiliaries"[MeSH Terms] | 30765 | 03:15:04 |
Appendix 3. Embase Ovid search strategy
1. (dental profession* or dental hygienist* or dentist* or dental care personnel or dental assistant* or dental therapist* or oral health therapist* or dental student* or dental hygiene student* or ('oral health care' and (personnel or practitioner* or student*))).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (106983) 2(Dentists or Dental Staff or Dental Auxillaries).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (20711) 3. 1 or 2 (107084) 4. (Human engineering or Posture or movement or mechanical processes or Instrumentation or equipment design or User‐computer interface or workload or workplace or Exercise or Exercise movement techniques or physical therapy modalities).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (1191066) 5. (biomechanics or ergonomic intervention* or ergonomic design* or 'ergonomic training' or ergonomics or 'dental office design' or 'work station design' or 'office layout' or job posture* or work posture* or working posture* or position or rest period* or taking break* or work schedul* or workplace practic* or lighting or magnification* or 'patient chair' or dental chair* or ((chair or chairs or furnish* or furniture or tool* or equipment* or instrument*) and (ergon* or design*)) or exercise* or physical fitness* or 'stress management' or human factors).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (1318874) 6. 4 or 5 (1895207) 7. (cumulative trauma disorders or Occupational diseases or Occupational health or musculoskeletal diseases or back pain or neck pain or shoulder pain or musculoskeletal pain or hand injuries or wrist injuries or arm injuries or upper extremity or lower extremity or back injuries or Carpal Tunnel syndrome).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (259024) 8. (occupational overuse syndrome or tension neck syndrome or work related or cumulative trauma or (repetit* and (stain or stress or motion or movement) and (injur* or disorder*)) or musculoskeletal disorder* or carpal tunnel syndrome or back pain or discomfort).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (189433) 9. 7 or 8 (347167) 10. 3 and 6 and 9 (559) 11. (randomised controlled trial or controlled clinical trial or randomized or placebo or drug therapy or randomly or trial or groups).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (7116327) 12. limit 11 to human (5680025) 13. 11 and 12 (5680025) 14. 10 and 13 (146) 15. ((effect* or control* or evaluation* or program*) and (work* or occupation* or prevention* or protect*)).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (2571536) 16. 10 and 15 (242) 17. 14 and 16 (76)
Appendix 4. PsycINFO search strategy
#1 (dentist* OR "dental staff" OR "dental auxiliar*" OR "dental profession*" OR "dental hygienist*" OR "dental care personnel" OR "dental assistant*" OR "dental therapist*" OR "oral health therapist*" OR "dental student*" OR "dental hygiene student*").mp. (2842) #2 ("oral health care" AND (personnel OR practitioner* OR student*)).mp. (36) #3 #1 OR #2 (2860) #4 ("human engineering" OR posture OR movement OR "mechanical process*" OR instrumentation OR "equipment design" OR "user‐computer interface" OR workload OR workplace OR exercise OR "exercise movement technique*" OR "physical therapy modalit*" OR biomechanic* OR "ergonomic intervention*" OR "ergonomic design*" OR "ergonomic training" OR ergonomic* OR "dental office design" OR "work station design" OR "office layout" OR "job posture*" OR "work posture*" OR "working posture*" OR position* OR "rest period*" OR "taking break*" OR "work schedul*" OR "workplace practic*" OR lighting OR magnification* OR "patient chair" OR "dental chair*").mp. (320267) #5 ((chair OR chairs OR furnish* OR furniture OR tool* OR equipment* OR instrument*) AND (ergon* OR design*)).mp. (53569) #6 (exercise* OR "physical fitness*" OR "stress management" OR "human factor*").mp. (86307) #7 #4 OR #5 OR #6 (394180) #8 ("cumulative trauma disorder*" OR "occupational disease*" OR "occupational health" OR "musculoskeletal disease*" OR "back pain" OR "neck pain" OR "shoulder pain" OR "musculoskeletal pain" OR "hand injur*" OR "wrist injur*" OR "arm injur*" OR "upper extremit*" OR "lower extremit*" OR "back injur*" OR "carpal tunnel syndrome" OR "occupational overuse syndrome" OR "tension neck syndrome" OR "tension neck" OR "work related" OR "cumulative trauma*" OR "musculoskeletal disorder*" OR discomfort).mp. (35514) #9 (repetiti* AND (strain OR stress OR motion OR movement) AND (injur* OR disorder*)).mp. (1486) #10 #8 OR #9 (36812) #11 #3 AND #7 AND #10 (40)
Appendix 5. OSH update search strategy
OSH Update (databases NIOSHTIC, NIOSHTIC‐2, HSELINE, CISDOC)
| Step | Hits | Strategy |
| #1 | 2090 | GW{dentist* OR "dental staff" OR "dental auxiliar*" OR "dental profession*" OR "dental hygienist*" OR "dental care personnel" OR "dental assistant*" OR "dental therapist*" OR "oral health therapist*" OR "dental student*" OR "dental hygiene student*"} |
| #2 | 0 | GW{"oral health care" AND (personnel OR practitioner* OR student*)} |
| #3 | 2090 | #1 OR #2 |
| #4 | 121958 | GW{"human engineering" OR posture OR movement OR "mechanical process*" OR instrumentation OR "equipment design" OR "user‐computer interface" OR workload OR workplace OR exercise OR "exercise movement technique*" OR "physical therapy modalit*" OR biomechanic* OR "ergonomic intervention*" OR "ergonomic design*" OR "ergonomic training" OR ergonomic* OR "dental office design" OR "work station design" OR "office layout" OR "job posture*" OR "work posture*" OR "working posture*" OR position* OR "rest period*" OR "taking break*" OR "work schedul*" OR "workplace practic*" OR lighting OR magnification* OR "patient chair" OR "dental chair*"} |
| #5 | 39759 | GW{(chair OR chairs OR furnish* OR furniture OR tool* OR equipment* OR instrument*) AND (ergon* OR design*)} |
| #6 | 16891 | GW{exercise* OR "physical fitness*" OR "stress management" OR "human factor*"} |
| #7 | 142771 | #4 OR #5 OR #6 |
| #8 | 3380 | GW{"cumulative trauma disorder*" OR "occupational disease*" OR "occupational health" OR "musculoskeletal disease*" OR "back pain" OR "neck pain" OR "shoulder pain" OR "musculoskeletal pain" OR "hand injur*" OR "wrist injur*" OR "arm injur*" OR "upper extremit*" OR "lower extremit*" OR "back injur*" OR "carpal tunnel syndrome" OR "occupational overuse syndrome" OR "tension neck syndrome" OR "tension neck" OR "work related" OR "cumulative trauma*" OR "musculoskeletal disorder*" OR discomfort} |
| #9 | 4196 | GW{repetiti* AND (strain OR stress OR motion OR movement) AND (injur* OR disorder*)} |
| #10 | 7131 | #8 OR #9 |
| #11 | 135 | #3 AND #7 AND #10 |
| #12 | 581216 | DC{OUNIOC OR OUNIOS OR OUHSEL OR OUCISD} |
| #13 | 27 | #11 AND #12 |
Appendix 6. Other databases search strategy
| Search site | Date of search: from inception to | Type of Search | Keywords used | Results | Relevant RCTs from results |
| WHO ICTRP (www.who.int/ictrp/search/en/) |
22 August 2018 | Basic | Ergonomic | 91 | 3 |
| 22 August 2018 | Advanced | Dentist (in "Title") AND musculoskeletal (in "Condition") | 3 | 3 | |
| 22 August 2018 | Advanced | Dentist (in "Title") AND ergonomic (in "Intervention") | 2 | 2 | |
| ClincialTrials.gov (ClinicalTrials.gov) |
22 August 2018 | Basic | Ergonomic | 112 | 0 |
| 22 August 2018 | Advanced | Musculoskeletal disease or condition (in "Condition") AND Ergonomic (in " Intervention / Treatment") AND Dentist (in "Title acronym / Titles") | 0 | 0 | |
| 22 August 2018 | Advanced | Ergonomic (in " Intervention / Treatment") AND Dentist (in "Title acronym / Titles") | 0 | 0 |
Data and analyses
Comparison 1. Multi‐faceted ergonomic interventions versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Prevalence of MSD in thigh | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Prevalence of MSD in feet | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. Light instrument (curette) with wide handle versus heavy curette with narrow handle.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Self‐reported pain in right elbow, forearm | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Self‐reported pain in right shoulder | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Dehghan 2016.
| Methods | Randomised parallel group study carried out among private dental practitioners in Tehran, Iran | |
| Participants | Inclusion criteria: dentists residing in Tehran, willing to fully participate in the study, and avoid the use of pain relievers during the study Exclusion criteria: Female dentists who were pregnant while the study was being conducted, and history of any spine surgery Age at baseline: 39.82 ± 4.61 (mean ± SD) years in the intervention group, and 40.01 ± 4.12 years in the control group Sociodemographics: not reported Total number: 102 Number randomised ‐ intervention group 50; control group 52 Number evaluated ‐ intervention group 50; control group 52 At baseline, the number of participants free from symptoms in the control (82%) and intervention (84%) groups for thigh MSDs; free from foot MSDs in the control (75%) and intervention (76%) groups. Less than 75% participants were free from MSDs in knee, back, wrist, arm, shoulder, and neck, |
|
| Interventions | The study compared an 8‐week multi‐faceted ergonomic intervention program which included modification in both operator factors (work posture, chair position, method of instrument usage), and office design factors (workstation layout, set‐up of operatory and chairs, delivery systems) with a control group, which did not receive any intervention. Intervention consisted of: 1. Knowledge and training about ergonomics: Training sessions provided to participating dentists at the start of the multi‐faceted ergonomic program, which covered the basic ergonomic principles, ergonomic risk factors in dental occupation, and intervention components of the ergonomic program. 2. Workstation modification: At this stage, keeping in mind the risk factors in the dental occupation, participants were instructed on how to ergonomically modify their working postures in different situations at the workplace. For example, the correct working posture and correct alignment of the equipment was explained to the dentists. 3. Training and surveying ergonomics at the workstation: At this stage, working conditions were evaluated during the working shift for each dentist, and ergonomic risk factors associated with workstations were identified. To mitigate the risk factors, active discussions and workstation modifications were carried out. 4. A regular exercise program: A physiotherapist introduced exercises involving stretching movements targeting the neck, shoulder, waist, and bottom. These exercises continued regularly during the study. Participants were also asked to note their daily sports activities in the logbook. |
|
| Outcomes | The General Nordic Questionnaire of musculoskeletal symptoms was used to assess MSDs at baseline, 3 months, and 6 months, in various locations of the body, such as knees, thighs, back, wrist, arm, shoulder, neck, and feet. The text of the article stated that paired t‐test was used to compare differences in prevalence; data tables stated that repeated measure ANOVA was used to determine statistical significance. Only outcomes for thighs and feet were used in the current review, since all other sites had more than 75% participants with MSD. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided into 2 groups". Did not describe the method of randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Work ability was assessed by using self‐reported outcomes. Essentially, the participants were also the outcome assessors, thus blinding to prevent detection bias was not feasible. It remained unclear how self‐reporting would have influenced the subjective outcome reporting, either favourably or unfavourably, hence, we rated this as unclear risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 102 participants completed the study. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in methods reported in results |
| Other bias | High risk | Two components were assessed in this item – compliance and statistical tests used. Compliance was neither measured nor reported, if measured. There were errors in the statistical tests used to assess data in this study. The text stated paired t‐test, the graphs stated repeated measure ANOVA were used to determine statistical significance. As this was a parallel design RCT, which involved independent groups, the correct tests should have been Chi² or logistic regression for categorical outcome variables (as per outcomes measured in this study, in which they measured prevalence of musculoskeletal, which required a yes or no response) or independent t‐test for numerical outcome response. Paired t‐test and repeated measure ANOVA are best used in within groups instances; the outcome response in this study (prevalence of musculoskeletal disorder) was dichotomous. This inappropriate use of statistical test may have resulted in serious errors and statistically significant results where none existed, thus making us classify this as high risk of bias. |
Rempel 2012.
| Methods | A cluster‐randomised, blinded, controlled trail was carried out among private practitioners in the San Fransisco Bay area in the USA to evaluate the effects of periodontal instrument handle diameter and weight on arm pain among dentists and dental hygienists who performed scaling and root planing. Participants were recruited at local dental professional meetings. | |
| Participants | Inclusion criteria: dentists and dental hygienists were eligible to participate if they performed scaling and root planing or teeth cleaning for more than 10 hours per week, and had been doing this work for more than one year. Exclusion criteria: they were not eligible if they were receiving care from a physician for treatment of an upper‐extremity disorder. Age at baseline 44.7 ± 10.4 years (mean ± SD); gender: males 10; females 100; occupation: dentists 13, dental hygienists 97; years in practice: 1 to 5 years 23, more than 5 years 87; ethnicity: Asian or Pacific Islander 23, African American, not of Hispanic origin 3, Hispanic 11, White, not of Hispanic origin 68, other 5. Total number: 110 participants from 90 dental offices Number randomised:
Five participants dropped out of the study between 2 and 12 weeks after receiving the allocated intervention as follows:
Their data were included in the analysis following intention to treat methods (the last observation was carried forward to the 16th week). Number evaluated:‐
After adjusting for cluster design effect, sample size reduced by one:
The two intervention groups were compared by using general linear models (SAS version 10, SAS, Cary, N.C.), and by controlling for age, sex, occupation, and hours of instrument use per week, with an intention to treat approach. The effect of interaction between instrument and sex, instrument and age, and instrument and occupation, were also tested. The following participants were free from MSD symptoms at baseline:
|
|
| Interventions | The study was carried out between April 2009 and Feb 2011 and the duration of the intervention was 16 weeks. Participants were randomly assigned to one of two types of periodontal instruments:
The instrument diameters and weights were selected on the basis of previous laboratory study results to provide a practical range that would have an effect on pinch force. The instruments were custom manufactured, and surfaced with a medium diamond texture. Instrument 1 was made from black plastic (acetal resin, Delrin, DuPont, Wilmington, Del.), and instrument 2 was made from steel plated with black coating. All instruments were fitted with an R3S and an R4S tip (Ratcliff stainless steel universal scalers, G. Hartzell & Son, Concord, Calif.). Participants reported using the assigned instrument approximately 82% of the time during scaling and root planing procedures |
|
| Outcomes | The primary outcomes measured were change in mean pain score, in the right wrist, elbow, and shoulder; the secondary outcomes measured were nights awakened by finger numbness, days of medication use for pain, in practitioners with newly diagnosed MSDs. For subjects reporting complaints of pain, trialists recorded a change in mean pain score, in the right wrist, elbow, and shoulder, from the month before the intervention to the last month of the study, after adjusting for important covariates. Participants completed an online baseline questionnaire, from which trialists collected demographic data and work history information, and an online questionnaire at the end of every work week (Thursday or Friday) for the next five months. The weekly questionnaire assessed the participant’s maximum pain level (on a 0‐ to 10‐point scale, with anchors at 0 (no pain) and 10 (unbearable pain) for the right wrist and hand, right elbow and forearm, and right shoulder. The questionnaire also assessed the number of hours during the week that the participant performed different dental tasks, the number of nights during which he or she awakened with numbness in the right thumb, index finger, or middle finger, and the number of days during which the participant used pain medication for right upper‐extremity symptoms. We decided not to include the secondary outcome of numbness in our review, since the way this outcome was reported and assessed, was more related to treatment than the prevention of musculoskeletal disorders. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A postdoctoral fellow made computer‐generated random assignments. Comment: Done |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was at the level of the dental office." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "they did not know what design elements were being compared" Quote: "participants were effectively masked to the intervention" Quote: "We concealed intervention allocation from the researchers…" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Since self‐reported outcomes were used, it remained unclear how self‐reporting would have influenced outcome reporting, either favourably or unfavourably. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 110 participants completed the study. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in methods reported in results |
| Other bias | Low risk | We did not identify any other sources of potential bias. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aghilinejad 2016 | Not RCT |
| Branson 2004 | None of the primary outcomes of review measured. Study presented only posture differences, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Cosaboom‐FitzSimons 2008 | None of the primary outcomes of review measured. Study measured muscle activity, using surface electromyography, which was a secondary outcome for our review, hence, not eligible for inclusion. Study conducted in a simulated setting in a lab on typodonts, and not in a real workplace. |
| Hayes 2014b | Not RCT |
| IRCT2016062128529N2 | Ongoing clinical trial, additional information sought; excluded since it was not an RCT. |
| James 2010 | None of the primary outcomes of review measured. Study measured grip strength, which was a secondary outcome of our review, hence not eligible for inclusion. |
| Lindegård 2012 | None of the primary outcomes of review measured. Study measured body inclinations, perceived exertion, and discomfort, which were secondary outcomes of our review, hence, not eligible for inclusion. |
| Maillet 2008 | None of the primary outcomes of review measured. Study assesses posture improvement, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| McCombs 2014 | None of the primary outcomes of review measured. Study quantified electrical muscle activity during simulated dental polishing with 3 different types of hand pieces, using electromyography, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Ouivirach 2014 | None of the primary outcomes of review measured. Study assessed posture of the neck and upper back, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Ryan 2005 | None of the primary outcomes of review measured. Study assessed tactile sensitivity score, using Vibratory Sensory Analyzer (VSA), which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Simmer‐Beck 2006 | None of the primary outcomes of review measured. Study measured muscle activity using surface electromyography, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Simmer‐Beck 2007 | None of the primary outcomes of review measured. Study assessed tactile discrimination, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Thanathornwong 2014 | None of the primary outcomes of review measured. Study measured tilt angle of the neck and upper back, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| Thanathornwong 2015 | None of the primary outcomes of review measured. Study measured tilt angle of the upper back, which was a secondary outcome of our review, hence, not eligible for inclusion. |
| von Thiele Schwarz 2008 | Only 9% participants were free from WMSD. |
Characteristics of studies awaiting assessment [ordered by study ID]
IRCT2014051117649N1.
| Methods | Randomised, single arm study |
| Participants | Dentists with 5 years or more working backgrounds |
| Interventions | Training the dentist with 5 years or more working backgrounds about ergonomic principles |
| Outcomes | Musculoskeletal disorders measured using Nordic questionnaire. Time points: before intervention, and 1 month after intervention |
| Notes | Since data available from the WHO ICTRP abstract were limited to make appropriate decision regarding inclusion or exclusion of this clinical trial, we sought additional information regarding trial methodology, randomisation, any data collected thus far, etc. from authors. No response received as of now. |
IRCT2015113024199N2.
| Methods | Randomised, single arm study |
| Participants | Dentists |
| Interventions | Multi‐faceted intervention program consisting of five components – group training on ergonomic principles and safe practices, work and equipment modification, supervise onsite ergonomic training, regular exercise program, and typing training and computer workstation evaluation and advice. |
| Outcomes | Musculoskeletal disorders measured using Nordic questionnaire Time points: before intervention, and 1 month after intervention |
| Notes | Since data available from the WHO ICTRP abstract were limited to make appropriate decision regarding inclusion or exclusion of this clinical trial, we sought information regarding trial methodology, randomisation, any data collected thus far, etc. from the trial authors. No response received as of now. |
Differences between protocol and review
In our protocol, we did not mention our methodology for assessing the overall risk of bias for a study, which we did for the review. We considered random sequence generation, allocation concealment, selective outcome reporting, and incomplete outcome data to be key items. We judged a study to have a high overall risk of bias when we judged one or more key items to have a high risk of bias. We intended to consider blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, the risk of bias for a musculoskeletal disorder diagnosis may be different than for a self‐reported pain scale). Where information on risk of bias was based on unpublished data, or correspondence with an author of a study, we made a note of it in the 'Risk of bias' table. When considering treatment effects, we took into account the risk of bias in the studies that contributed to that outcome.
In Assessment of heterogeneity, we added the sentence: "If we identify substantial heterogeneity (I² > 50), we will report it, and explore possible causes through subgroup analyses as, described in Subgroup analysis and investigation of heterogeneity". As we could not pool results of studies in meta‐analysis in this version of the review due to clinical heterogeneity, this will only apply to data we might include in future updates of this review.
Contributions of authors
Conceiving the protocol: PM, LK
Designing the protocol: PM, VHCW, MJH, JJI, LK, ABL
Coordinating the protocol: PM, VHCW, MJH
Designing search strategies: PM (based on work by CIS, Leena Isotalo)
Writing the protocol: PM, VHCW, MJH, JJI, LK, ABL
Providing general advice on the protocol: LK, ABL, VHCW
Sources of support
Internal sources
-
University of Malaya Research Grant UMRG (RG467‐12HTM), Malaysia.
RM10,000 grant received by Victor Hoe to conduct this Cochrane review.
External sources
No sources of support supplied
Declarations of interest
Priti Mulimani: None known.
Victor Hoe: I have been invited as a speaker by Pfizer to deliver a one‐hour lecture on the topic, 'The GP in Occupational Health', on three occasions.
Melanie Hayes: I have published research papers and presented conference papers on the topic of musculoskeletal disorders in the dental profession.
Jose Idiculla: None known.
Adinegara Abas: None known.
Laxminarayan Karanth: None known.
New
References
References to studies included in this review
Dehghan 2016 {published data only}
- Dehghan N, Aghilinejad M, Nassiri‐Kashani MH, Amiri Z, Talebi A. The effect of a multifaceted ergonomic intervention program on reducing musculoskeletal disorders in dentists. Medical Journal of The Islamic Republic of Iran 2016;30(472):1‐5. [PMC free article] [PubMed] [Google Scholar]
Rempel 2012 {published data only}
- Rempel D, Lee DL, Dawson K, Loomer P. The effects of periodontal curette handle weight and diameter on arm pain: a four‐month randomized controlled trial. Journal of American Dental Association 2012 Oct;143(10):1105‐13. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aghilinejad 2016 {published data only}
- Aghilinejad M, Kabir‐Mokamelkhah E, Talebi A, Soleimani R, Dehghan N. The effect of magnification lenses on reducing musculoskeletal discomfort among dentists. Medical Journal of The Islamic Republic of Iran 2016;30:473. [PMC free article] [PubMed] [Google Scholar]
Branson 2004 {published data only}
- Branson BG, Bray KK, Gadbury‐Amyot C, Holt LA, Keselyak NT, Mitchell TV, et al. Effect of magnification lenses on student operator posture. Journal of Dental Education 2004;68(3):384‐9. [PubMed] [Google Scholar]
Cosaboom‐FitzSimons 2008 {published data only}
- Cosaboom‐FitzSimons ME, Tolle SL, Darby ML, Walker ML. Effects of 5 different finger rest positions on arm muscle activity during scaling by dental hygiene students. Journal of Dental Hygiene 2008;82(4):34. [PubMed] [Google Scholar]
Hayes 2014b {published data only}
- Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of loupes on neck pain and disability among dental hygienists. Work 2016;53:755‐62. [DOI] [PubMed] [Google Scholar]
- Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. International Journal of Dental Hygiene 2014;12(3):174‐9. [DOI] [PubMed] [Google Scholar]
IRCT2016062128529N2 {unpublished data only}
- IRCT2016062128529N2. Effect of educational intervention according to theory of planned behavior‐based new media on promoting health work and ergonomic status in the dentists. en.irct.ir/trial/23131 (first registered 07 May 2016).
James 2010 {published data only}
- James DM, Branson BG, Simmer‐Beck M, Bray KK. Examining the effect of the Flextend Orthotic device on grip strength: a pilot study. Work 2010;35(4):487‐94. [DOI] [PubMed] [Google Scholar]
Lindegård 2012 {published data only}
- Lindegård A, Gustafsson M, Hansson GÅ. Effects of prismatic glasses including optometric correction on head and neck kinematics, perceived exertion and comfort during dental work in the oral cavity – a randomised controlled intervention. Applied Ergonomics 2012;43(1):246‐53. [DOI] [PubMed] [Google Scholar]
Maillet 2008 {published data only}
- Maillet JP, Millar AM, Burke JM, Maillet MA, Maillet WA, Neish NR. Effect of magnification loupes on dental hygiene student posture. Journal of Dental Education 2008;72(1):33‐44. [PubMed] [Google Scholar]
McCombs 2014 {published data only}
- McCombs G, Russell DM. Comparison of corded and cordless handpieces on forearm muscle activity, procedure time and ease of use during simulated tooth polishing. Journal of Dental Hygiene 2014;88(6):386‐93. [PubMed] [Google Scholar]
Ouivirach 2014 {published data only}
- Thanathornwong B, Suebnukarn S, Ouivirach K. A system for predicting musculoskeletal disorders among dental students. International Journal of Occupational Safety and Ergonomics 2014;20(3):463‐75. [DOI] [PubMed] [Google Scholar]
Ryan 2005 {published data only}
- Ryan DL, Darby M, Bauman D, Tolle SL, Naik D. Effects of ultrasonic scaling and hand‐activated scaling on tactile sensitivity in dental hygiene students. Journal of Dental Hygiene 2005;79(1):9. [PubMed] [Google Scholar]
Simmer‐Beck 2006 {published data only}
- Simmer‐Beck M, Bray KK, Branson B, Glaros A, Weeks J. Comparison of muscle activity associated with structural differences in dental hygiene mirrors. Journal of Dental Hygiene 2006;80(1):8. [PubMed] [Google Scholar]
Simmer‐Beck 2007 {published data only}
- Simmer‐Beck M, Branson BG, Mitchell TV, Holt L. Comparison of tactile discrimination associated with varying weights of explorers. Journal of Dental Education 2007;71(5):687‐93. [PubMed] [Google Scholar]
Thanathornwong 2014 {published data only}
- Thanathornwong B, Suebnukarn S, Songpaisan Y, Ouivirach K. A system for predicting and preventing work‐related musculoskeletal disorders among dentists. Computer Methods in Biomechanics and Biomedical Engineering 2014;17(2):177‐85. [DOI] [PubMed] [Google Scholar]
Thanathornwong 2015 {published data only}
- Thanathornwong B, Suebnukarn S. The improvement of dental posture using personalized biofeedback. Studies in Health Technology and Informatics 2015;216:756‐60. [PubMed] [Google Scholar]
von Thiele Schwarz 2008 {published data only}
- Thiele Schwarz U, Lindfors P, Lundberg U. Health‐related effects of worksite interventions involving physical exercise and reduced workhours. Scandinavian Journal of Work, Environment & Health 2008;34(3):179‐88. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
IRCT2014051117649N1 {unpublished data only}
- IRCT2014051117649N1. Clinical trial of evaluation the effect of ergonomic trainings in reducing the musculoskeletal disorders comparing to pre‐training measurements in dentists with at least 5‐years working background. en.irct.ir/trial/16177 (first registered 18 November 2014).
IRCT2015113024199N2 {unpublished data only}
- IRCT2015113024199N2. Investigate the effectiveness of ergonomic interventions to reduce the prevalence of musculoskeletal disorders with participatory ergonomics approach to dentists and their assistants in Milad hospital at 2015. en.irct.ir/trial/20488 (first registered 09 December 2015).
Additional references
ADA 2004
- Ergonomics and Disability Support Advisory Committee (EDSAC). An introduction to ergonomics: risk factors, MSDs, approaches and interventions. A report of the EDSAC to Council on Dental Practice (CDP). https://cdn.shopify.com/s/files/1/1171/2566/files/topics_ergonomics_paper_2.pdf. American Dental Association, 2004 (accessed 5 October 2018).
ADA 2014
- American Dental Association. ADA members insurance plans: Income protection plan. insurance.ada.org/ada‐insurance‐plans/disability‐insurance.aspx 2014 (accessed 5 October 2018).
Ahearn 2010
- Ahearn DJ, Sanders MJ, Turcotte C. Ergonomic design for dental offices. Work 2010;35(4):495‐503. [DOI] [PubMed] [Google Scholar]
Al Wazzan 2001
- Al Wazzan KA, Almas K, Shethri SE, Al Quahtani MQ. Back and neck problems among dentists and dental auxiliaries. Journal of Contemporary Dental Practice 2001;2(3):1‐10. [PubMed] [Google Scholar]
ASCC 2006
- Australian Safety and Compensation Council. Work‐related Musculoskeletal Disorders in Australia. https://www.safeworkaustralia.gov.au/system/files/documents/1702/workrelatedmusculoskeltaldisorders_2006australia_2006_archivepdf.pdf (accessed 5 October 2018).
Bernard 1997
- Bernard BP. Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work‐related musculoskeletal disorders of the neck, upper extremity, and lower back. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute of Occupational Safety and Health July 1997, issue DHHS (NIOSH) Publication No. 97‐141.
Breurs 2017
- Bruers JJM, Trommelen LECM, Hawi P, Brand HS. Musculoskeletal disorders among dentists and dental students in the Netherlands. Nederlands Tijdschrift voor Tandheelkunde 2017;124(11):581‐7. [DOI] [PubMed] [Google Scholar]
Buckle 2002
- Buckle P. Adapting work to people: new approaches to preventing musculoskeletal disorders. Sharpening the Focus on Performance. Proceedings of the Safety & Health at Work Congress; 2002 May 13‐16; Birmingham, UK. Birmingham: Royal Society for the Prevention of Accidents, 2002.
Burke 1997
- Burke FJ, Main JR, Freeman R. The practice of dentistry: an assessment of reasons for premature retirement. British Dental Journal 1997;182(7):250‐4. [DOI] [PubMed] [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
Conrad 1990
- Conrad J, Osborn J, Conrad K, Jetzer T. Peripheral nerve dysfunction in practicing hygienists. Journal of Dental Hygiene 1990;64(8):382‐7. [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation. Covidence systematic review software. Melbourne: Veritas Health Innovation, 2014.
De Sio 2018
- Sio S, Traversini V, Rinaldo F, Colasanti V, Buomprisco G, Perri R, et al. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: an umbrella review. PeerJ 15 Jan 2018;6:e4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Droeze 2005
- Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work 2005;25:211‐20. [PubMed] [Google Scholar]
EASHW 2008
- Podniece Z, Taylor TN, Takala E, David G, Kudasz F, Heuvel, et al. Work‐related musculoskeletal disorders: prevention report. https://osha.europa.eu/en/publications/reports/en_TE8107132ENC.pdf/view. European Agency for Safety and Health at Work, 2008 (accessed 5 October 2018).
Goldstep 1998
- Goldstep F. Designing the esthetic dental environment. Dental Clinics of North America 1998;42:643‐51. [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed 5 October 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Gupta 2014
- Gupta A, Bhat M, Mohammed T, Bansal N, Gupta G. Ergonomics in dentistry. International Journal of Clinical Pediatric Dentistry 2014;7(1):30‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawn 2006
- Hawn C, Tolle S, Darby M, Walker M. A laboratory study to determine the effects of universal and rotating ultrasonic inserts on wrist movement and scaling time efficiency of dental hygienists. International Journal of Dental Hygiene 2006;4(1):15‐23. [DOI] [PubMed] [Google Scholar]
Hayes 2009
- Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. International Journal of Dental Hygiene 2009;7(3):159‐65. [DOI] [PubMed] [Google Scholar]
Hayes 2010
- Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. International Dental Journal 2010;60:343‐52. [PubMed] [Google Scholar]
Hayes 2012
- Hayes MJ, Smith DR, Taylor JA. Predictors of work‐related musculoskeletal disorders among dental hygienists. International Journal of Dental Hygiene 2012;10(4):265‐9. [DOI] [PubMed] [Google Scholar]
Hayes 2013
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Research Notes 2013;6:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2014a
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal Disorders in a 3 Year Longitudinal Cohort of Dental Hygiene Students. Journal of Dental Hygiene 2014;88(1):36‐41. [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
IEA 2014
- International Ergonomics Association. What is ergonomics – definition and domains of ergonomics. www.iea.cc/whats/index.html (accessed 10 July 2014).
Khalekar 2016
- Khalekar Y, Zope A, Chaudahari L, Brahmankar U, Gadge H, Deore S. Prevention is better than cure: ergonomics in dentistry. Journal of Applied Dental and Medical Sciences 2016;2:209–16. [Google Scholar]
Khan 2013
- Khan SA, Chew KY. Effect of working characteristics and taught ergonomics on the prevalence of musculoskeletal disorders amongst dental students.. BMC Musculoskelet Disorders 2013;14:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kierklo 2011
- Kierklo A, Kobus A, Jaworska M, Botulinski B. Work‐related musculoskeletal disorders among dentists – a questionnaire survey. Annals of Agricultural and Environmental Medicine 2011;18(1):79‐84. [PubMed] [Google Scholar]
Lalumandier 2001
- Lalumandier JA, McPhee SD. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. Journal of Dental Hygiene 2001;75(2):130‐4. [PubMed] [Google Scholar]
Leggat 2006
- Leggat PA, Smith DR. Musculoskeletal disorders self‐reported by dentists in Queensland, Australia. Australian Dental Journal 2006;51(4):324‐7. [DOI] [PubMed] [Google Scholar]
Leggat 2007
- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry. Industrial Health 2007;45:611‐21. [DOI] [PubMed] [Google Scholar]
Liskiewicz 1997
- Liskiewicz S, Kerschbaum W. Cumulative trauma disorders: an ergonomic approach for prevention. Journal of Dental Hygiene 1997;71(4):162‐7. [PubMed] [Google Scholar]
Michalak‐Turcotte 2000
- Michalak‐Turcotte C. Controlling dental hygiene work‐related musculoskeletal disorders: the ergonomic process. Journal of Dental Hygiene 2000;74(1):41‐8. [PubMed] [Google Scholar]
Michalak‐Turcotte 2005
- Michalak‐Turcotte C, Sanders MJ. A problem‐solving approach to ergonomic intervention in dental hygiene: part I. Dimensions of Dental Hygiene 2005;3(9):18, 20‐1. [Google Scholar]
Miller 1989
- Miller DJ, Shugars DA. Back pain in dentists: current research and prevention. Revista Odontologica de Puerto Rico 1989;27(3):22‐5. [PubMed] [Google Scholar]
Miller 1991
- Miller DL. An investigation into attrition of dental hygienists from the work force. Journal of Dental Hygiene 1991;65(1):25‐31. [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moodley 2018
- Moodley R, Naidoo S, Wyk J. The prevalence of occupational health‐related problems in dentistry: A review of the literature. Journal of Occupational Health 2018;60(2):111‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morse 2003
- Morse TF, Michalak‐Turcotte C, Atwood‐Sanders M, Warren N, Peterson DR, Bruneau H, et al. A pilot study of hand and arm musculoskeletal disorders in dental hygiene students. Journal of Dental Hygiene 2003;77(3):173‐9. [PubMed] [Google Scholar]
Morse 2007
- Morse T, Bruneau T, Michalak‐Turcotte C, Sanders M, Warren N. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. Journal of Dental Hygiene 2007;81(1):1‐20. [PubMed] [Google Scholar]
Morse 2010
- Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 2010;35(4):419‐29. [DOI] [PubMed] [Google Scholar]
NIOSH 1997
- The National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. Musculoskeletal disorders and workplace factors – A critical review of epidemiologic evidence for work‐related musculoskeletal disorders of the neck, upper extremity, and low back. www.cdc.gov/niosh/docs/97‐141/ 1997 (accessed 5 October 2018).
Osborn 1990
- Osborn JB, Newell KJ, Rudney JD, Stoltenberg JL. Musculoskeletal pain among Minnesota dental hygienists. Journal of Dental Hygiene 1990;64(3):132‐8. [PubMed] [Google Scholar]
Petren 2007
- Petren V, Petzall K, Preber H, Bergstrom J. The relationship between working conditions and sick leave in Swedish dental hygienists. International Journal of Dental Hygiene 2007;5(1):27‐35. [DOI] [PubMed] [Google Scholar]
Pirvu 2014
- Pîrvu C, Pătraşcu I, Pîrvu D, Ionescu C. The dentist’s operating posture – ergonomic aspects. Journal of Medicine and Life 2014;7(2):177‐82. [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rolander 2001
- Rolander B, Bellner A. Experience of musculoskeletal disorders, intensity of pain, and general conditions in work – the case of employees in non‐private dental clinics in a county in southern Sweden. Work 2001;17(1):65‐73. [PubMed] [Google Scholar]
Rucker 2002
- Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. Journal of California Dental Association 2002;30(2):139‐46. [PubMed] [Google Scholar]
Sakzewski 2014
- Sakzewski L, Naser‐ud‐Din S. Work‐related musculoskeletal disorders in dentists and orthodontists: a review of the literature. Work 2014;48(1):37‐45. [DOI] [PubMed] [Google Scholar]
Sanders 2002
- Sanders MA, Turcotte CM. Strategies to reduce work‐related musculoskeletal disorders in dental hygienists: two case studies. Journal of Hand Therapy 2002;15(4):363‐74. [DOI] [PubMed] [Google Scholar]
Twadell 2009
- Twadell S. Surrogate outcome markers in research and clinical practice. Australian Prescriber 2009;32:47‐50. [Google Scholar]
Valachi 2003
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. Journal of American Dental Association 2003;134(10):1344‐50. [DOI] [PubMed] [Google Scholar]
Yamalik 2007
- Yamalik N. Musculoskeletal disorders (MSDs) and dental practice. Part 2. Risk factors for dentistry, magnitude of the problem, prevention, and dental ergonomics. International Dental Journal 2007;57(1):45‐54. [DOI] [PubMed] [Google Scholar]
Ylipaa 1999
- Ylippa V, Arnetz BB, Preber H. Predictors of good general health, well‐being, and musculoskeletal disorders in Swedish dental hygienists. Acta Odontologica Scandinavica 1999;57(5):277‐82. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Mulimani 2014
- Mulimani P, Hoe VCW, Hayes MJ, Idiculla JJ, Abas ABL, Karanth L. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD011261] [DOI] [PMC free article] [PubMed] [Google Scholar]


