Abstract
Background
Early accurate detection of all skin cancer types is important to guide appropriate management and improve morbidity and survival. Basal cell carcinoma (BCC) is usually a localised skin cancer but with potential to infiltrate and damage surrounding tissue, whereas cutaneous squamous cell carcinoma (cSCC) and melanoma are higher risk skin cancers with the potential to metastasise and ultimately lead to death. When used in conjunction with clinical or dermoscopic suspicion of malignancy, or both, reflectance confocal microscopy (RCM) may help to identify cancers eligible for non‐surgical treatment without the need for a diagnostic biopsy, particularly in people with suspected BCC. Any potential benefit must be balanced against the risk of any misdiagnoses.
Objectives
To determine the diagnostic accuracy of RCM for the detection of BCC, cSCC, or any skin cancer in adults with any suspicious lesion and lesions that are difficult to diagnose (equivocal); and to compare its accuracy with that of usual practice (visual inspection or dermoscopy, or both).
Search methods
We undertook a comprehensive search of the following databases from inception to August 2016: Cochrane Central Register of Controlled Trials; MEDLINE; Embase; CINAHL; CPCI; Zetoc; Science Citation Index; US National Institutes of Health Ongoing Trials Register; NIHR Clinical Research Network Portfolio Database; and the World Health Organization International Clinical Trials Registry Platform. We studied reference lists and published systematic review articles.
Selection criteria
Studies of any design that evaluated the accuracy of RCM alone, or RCM in comparison to visual inspection or dermoscopy, or both, in adults with lesions suspicious for skin cancer compared with a reference standard of either histological confirmation or clinical follow‐up, or both.
Data collection and analysis
Two review authors independently extracted data using a standardised data extraction and quality assessment form (based on QUADAS‐2). We contacted authors of included studies where information related to the target condition or diagnostic threshold were missing. We estimated summary sensitivities and specificities using the bivariate hierarchical model. For computation of likely numbers of true‐positive, false‐positive, false‐negative, and true‐negative findings in the 'Summary of findings' tables, we applied summary sensitivity and specificity estimates to lower quartile, median and upper quartiles of the prevalence observed in the study groups. We also investigated the impact of observer experience.
Main results
The review included 10 studies reporting on 11 study cohorts. All 11 cohorts reported data for the detection of BCC, including 2037 lesions (464 with BCC); and four cohorts reported data for the detection of cSCC, including 834 lesions (71 with cSCC). Only one study also reported data for the detection of BCC or cSCC using dermoscopy, limiting comparisons between RCM and dermoscopy. Studies were at high or unclear risk of bias across almost all methodological quality domains, and were of high or unclear concern regarding applicability of the evidence. Selective participant recruitment, unclear blinding of the reference test, and exclusions due to image quality or technical difficulties were observed. It was unclear whether studies were representative of populations eligible for testing with RCM, and test interpretation was often undertaken using images, remotely from the participant and the interpreter blinded to clinical information that would normally be available in practice.
Meta‐analysis found RCM to be more sensitive but less specific for the detection of BCC in studies of participants with equivocal lesions (sensitivity 94%, 95% confidence interval (CI) 79% to 98%; specificity 85%, 95% CI 72% to 92%; 3 studies) compared to studies that included any suspicious lesion (sensitivity 76%, 95% CI 45% to 92%; specificity 95%, 95% CI 66% to 99%; 4 studies), although CIs were wide. At the median prevalence of disease of 12.5% observed in studies including any suspicious lesion, applying these results to a hypothetical population of 1000 lesions results in 30 BCCs missed with 44 false‐positive results (lesions misdiagnosed as BCCs). At the median prevalence of disease of 15% observed in studies of equivocal lesions, nine BCCs would be missed with 128 false‐positive results in a population of 1000 lesions. Across both sets of studies, up to 15% of these false‐positive lesions were observed to be melanomas mistaken for BCCs. There was some suggestion of higher sensitivities in studies with more experienced observers. Summary sensitivity and specificity could not be estimated for the detection of cSCC due to paucity of data.
Authors' conclusions
There is insufficient evidence for the use of RCM for the diagnosis of BCC or cSCC in either population group. A possible role for RCM in clinical practice is as a tool to avoid diagnostic biopsies in lesions with a relatively high clinical suspicion of BCC. The potential for, and consequences of, misclassification of other skin cancers such as melanoma as BCCs requires further research. Importantly, data are lacking that compare RCM to standard clinical practice (with or without dermoscopy).
Plain language summary
What is the diagnostic accuracy of reflectance confocal microscopy for the detection of basal or squamous cell carcinoma of the skin in adults?
What is the aim of the review?
The aim of this Cochrane Review was to find out how accurate reflectance confocal microscopy (RCM) is on its own or compared to inspection of a skin lesion with the naked eye alone or using a hand‐held microscope called dermoscopy for diagnosing two common forms of keratinocyte skin cancer: basal cell carcinoma (BCC) or cutaneous squamous cell carcinoma (cSCC) in adults. Review authors in Cochrane included 10 studies to answer this question.
Why is improving the diagnosis of BCC or cSCC important?
There are a number of different types of skin cancer. BCC and cSCC are usually localised skin cancers. Making the correct diagnosis is important because mistaking one skin cancer for another can lead to the wrong treatment being used or lead to a delay in effective treatment. A missed diagnosis of BCC (known as a false‐negative result) can result in the missed BCC growing and causing disfigurement. A missed diagnosis of cSCC is more serious as it could spread to other parts of the body. Diagnosing a skin cancer when it is not actually present (a false‐positive result) may result in unnecessary biopsy or treatment and can cause discomfort and worry to patients.
What was studied in the review?
Microscopic techniques are used by skin cancer specialists to provide a more detailed, magnified examination of suspicious skin lesions than can be achieved using the naked eye alone. Currently, dermoscopy is used by doctors as part of the examination of suspicious skin lesions. RCM is a new microscopic technique to increase the magnification. It is a hand‐held device or static unit using infrared light that can visualise deeper layers of the skin when compared with dermoscopy. Both techniques are painless procedures, but RCM is more expensive, time consuming, and requires additional specialised training. Dermoscopy can be used by general practitioners (GP) whereas RCM is likely to only be used by hospital specialists for people who have been referred with a skin lesion that is suspected to be a skin cancer. We wanted to see if RCM should be used instead of, or as well as, inspection of a skin lesion with the naked eye alone or using dermoscopy to diagnose BCC or cSCC. The accuracy of the test was looked at when used on people with any suspicious skin lesion and also in people with skin lesions that were tricky to diagnose.
What are the main results of the review?
We found 10 studies that included information on 11 groups of people with lesions suspicious for skin cancer. The main results were based on seven of the 11 sets of data: four in any lesion suspicious for skin cancer and three in particularly difficult to diagnose skin lesions.
For the comparison of RCM versus dermoscopy, we found four sets of data that included 912 suspicious skin lesions. The results suggested that in a group of 1000 people with any suspicious lesion, of whom 125 (12.5%) really do have BCC:
‐ an estimated 139 people will have an RCM result indicating BCC is present;
‐ of these, 44 (32%) people will not have BCC (false‐positive results) including one person with a melanoma mistaken for a BCC;
‐ of the 861 people with an RCM result indicating that BCC is not present, 30 (3%) will actually have BCC.
The review also included three sets of data on people that had 668 particularly difficult to diagnose skin lesions, one comparing RCM to dermoscopy. The results suggested that if RCM was to be used by skin specialists in a group of 1000 people, of whom 150 (15%) really do have BCC:
‐ an estimated 269 people will have an RCM result indicating BCC is present;
‐ of these, 128 (48%) people will not have a BCC (known as a false‐positive result), including as many as 19 people with melanomas mistaken for BCCs;
‐ of the 732 people with an RCM result indicating that BCC is not present, nine (1%) will actually have BCC.
There was not enough evidence to determine the accuracy of RCM for the detection of cSCC in either population group.
How reliable are the results of this review?
There was a lot of variation in the results of the studies in this review. Poor reporting of study conduct made assessment of the reliability of studies difficult. It was unclear whether studies were representative of populations eligible for testing with RCM, and test interpretation was often undertaken using images, remotely from the patient and the interpreter blinded to clinical information that would normally be available in practice. Only one study compared the accuracy of dermoscopy and RCM. Most studies were conducted by specialist research teams with high levels of training and experience with RCM, meaning that RCM may appear better than it would be when used in everyday practice. Most studies reported diagnosis based on observers' subjective views, which might not be the same for people using the technique in everyday practice. In nine studies, the diagnosis of skin cancer was made by a skin biopsy or by following up those people over time to make sure they remained negative for skin cancer*. This is likely to have been a reliable method for deciding whether patients really had skin cancer. In one study, the absence of skin cancer was made by experts looking at the skin, a method that may be less reliable for deciding whether patients really had skin cancer.
Who do the results of this review apply to?
Five studies were carried out in Europe (61%), and the rest in Asia, Oceania, North America, or more than one continent. The average ages of people who took part ranged from 41 to 65 years. The percentage of people with BCC in these studies ranged from 6% to 83% (a middle value of 12% for any suspicious lesion and 15% for difficult to diagnose skin lesions). For studies of RCM used for cSCC, the percentage of people with cSCC ranged between 4% and 13%. In many studies it was not clear what tests people taking part had received before RCM.
What are the implications of this review?
There was not enough good evidence to support the use of RCM for the diagnosis of BCC or cSCC outside of research studies. There was a lot of variation and uncertainty in results and in the ways studies were carried out, reducing the reliability of findings. Using RCM might avoid the need for a diagnostic biopsy in people who see a doctor with a high suspicion of a BCC lesion, but more research is needed to confirm this. Such research should compare RCM to dermoscopy in well‐described groups of people with suspicious skin lesions and they must say whether other skin cancers end up being missed or being wrongly classified as BCC.
How up‐to‐date is this review?
The review authors searched for and used studies published up to August 2016.
*In these studies, biopsy or clinical follow‐up were the reference standards (means of establishing final diagnoses).
Summary of findings
Summary of findings'. 'Summary of findings table.
| Question: | What is the diagnostic accuracy of reflectance confocal microscopy for the detection of keratinocyte skin cancers in adults? | |||||
| Population: | Adults with lesions suspicious for skin cancer, including:
|
|||||
| Index test: | RCM | |||||
| Comparator test: | Visual inspection or dermoscopy, or both | |||||
| Target condition: |
|
|||||
| Reference standard: | Histology with or without long‐term follow‐up | |||||
| Action: | If accurate, negative results of RCM will stop patients having unnecessary excision of skin lesions; positive results could inform the use of non‐surgical management options. | |||||
| Quantity of evidence | Target condition | Number of studies | Total lesions | Total cases | ||
| — | BCC | 10 (11 cohorts) | 2037 | 464 | ||
| — | cSCC | 4 (4 cohorts) | 834 | 71 | ||
| Limitations | ||||||
| Risk of bias: | High (4/11) or unclear (3/11) risk for participant selection with exclusion on image quality and use of a case‐control design. Low risk for index test (11/11). High risk from inadequate reference standard (2/11) and unclear blinding of the reference standard to the RCM result (8/11). Differential verification in 3/11, timing of tests not mentioned in 7/11, and exclusions due to technical difficulties in 4/11. | |||||
| Applicability of evidence to question: | High (8/11) or unclear (3/11) concern for participants and setting with narrowly defined populations (3/11) or multiple lesions per patient (5/11). High concern for index test (7/11) with remote RCM interpretation (5/11) blinded to clinical information (3/11), lack of detail on the diagnostic threshold (2/11), and novice RCM users (2/11). The studies were dominated by 1 particularly expert research group (8/11). Little information given concerning the expertise of the histopathologist. | |||||
| FINDINGS: | ||||||
| 10 studies providing data for 11 cohorts of lesions were eligible for inclusion, 7 in our target populations of interest. All 7 cohorts reported data for detection of BCC and 2 reported data for detection of cSCC. The findings presented were based on results from these 7 cohorts. Insufficient data were available to compare RCM with visual inspection or dermoscopy or to consider the effect of using formally developed algorithms to assist RCM diagnosis. There was some evidence of melanomas or SCCs being misdiagnosed as BCCs and of higher sensitivity in cohorts using more experienced observers. | ||||||
| Test: RCM for detection of BCC using any or no algorithm at any threshold in any suspicious lesion | ||||||
| Datasets (n) | Lesions (n) | Cases (n) | Sensitivity (95% CI) | Specificity (95% CI) | ||
| 4 | 912 | 107 | 76% (45% to 92%) | 95% (66% to 99%) | ||
| Numbers in a cohort of 1000 lesionsa | True positives | False positives | False negatives | True negatives | PPV | NPV |
| At median prevalence 12.5% | 95 (56; 115) |
44 (298; 9) |
30 (69; 10) |
831 (578; 866) |
68% (16; 93) |
97% (89; 99) |
| At lower quartile prevalence 10% | 75 (45; 91) |
45 (306; 9) |
24 (54; 8) |
856 (595; 892) |
63% (13; 91) |
97% (92; 99) |
| At upper quartile prevalence 15% | 118 (70; 143) |
42 (287; 8) |
37 (85; 12) |
803 (558; 837) |
74% (20; 94) |
96% (87; 99) |
| Test: RCM for detection of BCC using any or no algorithm at any threshold in equivocal lesions | ||||||
| Datasets (n) | Lesions (n) | Cases (n) | Sensitivity (95% CI) | Specificity (95% CI) | ||
| 3 | 668 | 148 | 94% (79% to 98%) | 85% (72% to 92%) | ||
| Numbers in a cohort of 1000 lesionsa |
True positives |
False positives |
False negatives |
True negatives |
PPV | NPV |
| At median prevalence 15% | 141 (119; 147) |
128 (238; 68) |
9 (32; 3) |
723 (612; 782) |
53% (33; 68) |
99% (95; 100) |
| At lower quartile prevalence 11% | 100 (84; 104) |
134 (250; 72) |
6 (22; 2) |
760 (644; 822) |
43% (25; 59) |
99% (97; 100) |
| At upper quartile prevalence 29% | 276 (232; 288) |
106 (198; 56) |
18 (62; 6) |
600 (508; 650) |
72% (54; 84) |
97% (89; 99) |
| Test: RCM for detection of cSCC using any or no algorithm | ||||||
| — | Lesions (n) | Cases (n) | Sensitivity (95% CI) | Specificity (95% CI) | ||
| In any suspicious lesion (1 study) | 323 | 42 | 74% (58% to 86%) | 92% (88% to 95%) | ||
| In equivocal lesions (1 study) | 260 | 13 | 77% (46% to 95%) | 98% (96% to 100%) | ||
aNumber of true positives, false positives, false negatives, and true negatives have been estimated at the median and interquartile ranges of prevalence, at mean sensitivity and specificity and using the lower and upper limits of the 95% confidence intervals, denoted in brackets (lower limit; upper limit)
BCC: basal cell carcinoma; CI: confidence interval; cSCC: cutaneous squamous cell carcinoma; n: number; NPV: negative predictive value; PPV: positive predictive value; RCM: reflectance confocal microscopy; SCC: squamous cell carcinoma.
Background
This review is one of a series of Cochrane Diagnostic Test Accuracy (DTA) Reviews on the diagnosis and staging of melanoma and keratinocyte skin cancers as part of the National Institute for Health Research (NIHR) Cochrane Systematic Reviews Programme. Appendix 1 shows the content and structure of the programme.
Target condition being diagnosed
The most commonest skin cancers in white populations are those arising from keratinocyte cells: basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) (Gordon 2013; Madan 2010). BCC is the more common of the two keratinocyte carcinomas, and approximately around one third of people with a BCC will develop a second BCC (Flohil 2013). In 2003, the World Health Organization estimated that between two and three million 'non‐melanoma' skin cancers (of which BCC and cSCC are estimated to account for around 80% and 16% of cases respectively) and 132,000 melanoma skin cancers occur globally each year (WHO 2003).
In this diagnostic test accuracy (DTA) review, we collectively referred to BCC and cSCC using the new preferred and more accurate term of 'keratinocyte carcinoma' (Karimkhani 2015). Rather than defining BCC and cSCC by what they are not (i.e. non‐melanoma skin cancer), we collectively refer to these conditions using the preferred and more accurate term of 'keratinocyte carcinoma' in this DTA review (Karimkhani 2015). We define (a) BCC and (b) cSCC as the primary target conditions for this review. We also examine accuracy for the target condition of (c) any skin cancer, including keratinocyte skin cancer, melanoma or atypical intraepidermal melanocytic variants and any other skin cancer. We have examined the accuracy of reflectance confocal microscopy (RCM) for the diagnosis of melanoma in another review (Dinnes 2018a), which is one of a series of systematic reviews of diagnostic tests for the diagnosis of keratinocyte skin cancers (Dinnes 2015a). A table of acronyms used is provided in Appendix 2.
Basal cell carcinoma
BCC can arise from multiple stem cell populations, including from the follicular bulge and interfollicular epidermis (Grachtchouk 2011). Growth is usually localised, but it can infiltrate and damage surrounding tissue, which if left untreated can cause considerable destruction and disfigurement, particularly when located on the face (Figure 1). The four main types of BCC are superficial, nodular, morphoeic (infiltrative), and pigmented. Lesions typically present as slow‐growing asymptomatic papules, plaques, or nodules which may bleed or form ulcers that do not heal (Firnhaber 2012). People with a BCC often present themselves to healthcare professionals with a non‐healing lesion rather than specific symptoms such as pain. Many lesions are diagnosed incidentally (Gordon 2013).
1.

Sample photographs of superficial spreading melanoma (left), basal cell carcinoma (centre) and cutaneous squamous cell carcinoma (right). Copyright © 2012 Dr Rubeta Matin: reproduced with permission.
BCC most commonly occurs on sun‐exposed areas of the head and neck (McCormack 1997), and are more common in men and in people over the age of 40. A rising incidence of BCC in younger people has been attributed to increased recreational sun exposure (Bath‐Hextall 2007a; Gordon 2013; Musah 2013). Other risk factors include Fitzpatrick skin types I and II (Fitzpatrick 1975; Lear 1997; Maia 1995); previous skin cancer history; immunosuppression; arsenic exposure; and genetic predisposition, such as in basal cell naevus (Gorlin's) syndrome (Gorlin 2004; Zak‐Prelich 2004). Annual incidence is increasing worldwide; Europe has experienced a mean increase of 5.5% per year since the 1970s, the USA 2% per year, while estimates for the UK show incidence appears to be increasing more steeply at a rate of an additional 6 per 100,000 persons per year (Lomas 2012). The rising incidence has been attributed to an ageing population; changes in the distribution of known risk factors, particularly ultraviolet radiation; and improved detection due to the increased awareness among both practitioners and the general population (Verkouteren 2017). Hoorens 2016 points to evidence for a gradual increase in the size of BCCs over time, with delays in diagnosis ranging from 19 to 25 months.
According to National Institute for Health and Care Excellence (NICE) guidance (NICE 2010), low risk BCCs are nodular lesions occurring in people older than 24 years who are not immunosuppressed and do not have Gorlin's syndrome. Furthermore, lesions should be located below the clavicle; should be small (less than 1 cm) with clinically well‐defined margins; not recurrent following incomplete excision or other treatment; and not in awkward or highly visible locations (NICE 2010). Superficial BCCs are also typically low risk and may be amenable to medical treatments such as cryotherapy, photodynamic therapy (PDT) or topical immunomodulatory therapy, e.g. 5% Imiquimod cream (Kelleners‐Smeets 2017). Assigning BCCs as low or high risk influences the management options (Batra 2002; Randle 1996).
Advanced locally destructive BCC can be found on the H‐area of the face (Lear 2014), can arise from long‐standing untreated lesions or from a recurrence of aggressive BCC after primary treatment (Lear 2012). Very rarely, BCC may metastasize to regional and distant sites resulting in death; this is particularly true for large neglected lesions in people who are immunosuppressed, or those with Gorlin syndrome (McCusker 2014). Rates of metastasis are reported at 0.0028% to 0.55% (Lo 1991), with very poor survival rates. It is recognised that basosquamous carcinoma (more like a high‐risk SCC in behaviour and not considered a true BCC) is likely to have accounted for many cases of apparent metastases of BCC, hence, the spuriously high reported incidence in some studies of up to 0.55%, which is not seen in clinical practice (Garcia 2009).
Squamous cell carcinoma of the skin
Primary cSCC arises from the keratinising cells of the epidermis or its appendages. People with cSCC often present with an ulcer or firm (indurated) papule, plaque, or nodule (Griffin 2016), often with an adherent crust (Madan 2010) (Figure 1). cSCC can arise in the absence of a precursor lesion or may develop from pre‐existing lesions, such as actinic keratosis or Bowen's disease (considered by some clinicians to be cSCC in situ) with an estimated annual risk of progression of less than 1% to 20% for newly‐arising lesions (Alam 2001) and 5% for pre‐existing lesions (Kao 1986). It remains locally invasive for a variable length of time, but has the potential to spread to the regional lymph nodes or via the bloodstream to distant sites, especially in immunosuppressed individuals (Lansbury 2010). High risk lesions are those arising on the lip or ear; recurrent cSCC; lesions arising on non‐exposed sites; within scars, or chronic ulcers; tumours more than 20 mm in diameter and depth of invasion more than 4 mm; and poor differentiation on pathological examination (Motley 2009). Perineural nerve invasion (PNI) of at least 0.1 mm in diameter is a further documented risk factor for high‐risk cSCC (Carter 2013).
Chronic ultraviolet light exposure through recreation or occupation is strongly linked to cSCC occurrence (Alam 2001). It is particularly common in people with fair skin and in less common genetic disorders of pigmentation, such as albinism, xeroderma pigmentosum, and recessive dystrophic epidermolysis bullosa (RDEB) (Alam 2001). Other recognised risk factors include immunosuppression; chronic wounds; arsenic or radiation exposure; certain drug treatments, such as voriconazole and BRAF mutation inhibitors; and previous skin cancer history (Baldursson 1993; Chowdri 1996; Dabski 1986; Fasching 1989; Lister 1997; Maloney 1996; O'Gorman 2014). In solid organ transplant recipients, cSCC is the most common form of skin cancer; the risk of developing cSCC has been estimated at 65 to 253 times that of the general population (Hartevelt 1990; Jensen 1999; Lansbury 2010). Overall, local and metastatic recurrence of cSCC at five years is estimated at 8% and 5% respectively. The five‐year survival rate of metastatic cSCC of the head and neck is around 60% (Moeckelmann 2018).
Treatment
Treatment options for BCC and cSCC include surgery, other destructive techniques, and topical chemotherapy. One Cochrane Review of 27 randomised controlled trials (RCTs) of interventions for BCC found very little good‐quality evidence for any of the interventions used (Bath‐Hextall 2007b). Complete surgical excision of primary BCC has a reported five‐year recurrence rate of less than 2% (Griffiths 2005 (data 1998 to 2003); Walker 2006 (review paper)), leading to significantly fewer recurrences than treatment with radiotherapy (Bath‐Hextall 2007b). After apparent clear histopathological margins (serial vertical sections) after standard excision biopsy with 4 mm surgical peripheral margins taken, there is a five‐year reported recurrence rate of around 4% (Drucker 2017). Mohs micrographic surgery, whereby horizontal sections of the tumour are microscopically examined perioperatively and re‐excision is undertaken until the margins are tumour‐free, can be considered for high risk lesions on the face where standard wider excision margins might lead to considerable functional or cosmetic impairment (Bath‐Hextall 2007b; Motley 2009; Lansbury 2010; Stratigos 2015). Bath‐Hextall 2007b found a single trial comparing Mohs micrographic surgery with a 3 mm surgical margin excision in BCC (Smeets 2004); the update of this study showed non‐significantly lower recurrence at 10 years with Mohs micrographic surgery (4.4% compared to 12.2% after surgical excision; P = 0.10) (van Loo 2014).
The main treatments for high risk BCC are wide local excision, Mohs micrographic surgery and radiotherapy. For low risk or superficial subtypes of BCC, or for small or multiple BCCs, or both, at low risk sites (Marsden 2010), destructive techniques other than excisional surgery may be used (e.g. electrodessication and curettage or cryotherapy (Alam 2001; Bath‐Hextall 2007b)). Alternatively non‐surgical (or non‐destructive) treatments may be considered (Bath‐Hextall 2007b; Drew 2017; Kim 2014), including topical chemotherapy such as imiquimod (Williams 2017), 5‐fluorouracil (5‐FU) (Arits 2013), ingenol mebutate (Nart 2015) and PDT (Roozeboom 2016). Non‐surgical treatments are most frequently used for superficial forms of BCC, with one head to head trial suggesting topical imiquimod is superior to PDT and 5‐FU (Jansen 2018). Although non‐surgical techniques are increasingly used, they do not allow histological confirmation of tumour clearance, and their use is dependent on accurate characterisation of the histological subtype and depth of tumour. The 2007 systematic review of BCC interventions found limited evidence from very small RCTs for these approaches (Bath‐Hextall 2007b), which have only partially been filled by subsequent studies (Bath‐Hextall 2014; Kim 2014; Roozeboom 2012). Most BCC trials have compared interventions within the same treatment class, and few have compared medical versus surgical treatments (Kim 2014).
Vismodegib, a first‐in‐class Hedgehog signalling pathway inhibitor, is now available for the treatment of metastatic or locally advanced BCC based on the pivotal study ERIVANCE BCC (Sekulic 2012). It is licensed for use in people with BCC where surgery or radiotherapy is inappropriate, e.g. for treating locally advanced periocular and orbital BCCs with orbital salvage of people who otherwise would have required exenteration (Wong 2017). However, in 2017, NICE recommended against the use of vismodegib based on cost‐effectiveness and uncertainty of evidence (NICE 2017).
A systematic review of interventions for primary cSCC found only one RCT eligible for inclusion (Lansbury 2010). Current practice therefore relies on evidence from observational studies, as reviewed in Lansbury 2013, for example. Surgical excision with predetermined margins is usually the first‐line treatment (Motley 2009; Stratigos 2015). Estimates of recurrence after Mohs micrographic surgery, surgical excision, or radiotherapy, which are likely to have been evaluated in higher risk populations, have shown pooled recurrence rates of 3% (Mohs), 5.4% (surgical excision), and 6.4% (radiotherapy) with overlapping confidence intervals (CI); the review authors advise caution when comparing results across treatments (Lansbury 2013).
Index test(s)
RCM, also known as confocal laser scanning microscopy or confocal microscopy, was first developed for skin imaging in the early 1990s (Rajadhyaksha 1995), and is emerging as a potential alternative or adjunct to dermoscopy for the diagnosis of skin cancer. It is a non‐invasive technology, which can be used to visualise horizontally sectioned images of the skin at a cellular lateral resolution of about 1 μm, in vivo to the depth of the upper dermis. The contrast for the monochrome images produced is achieved by the variation of the optical properties within the skin when illuminated by a near‐infrared light (830 nm) (see Figure 2). The greatest contrast is achieved from melanin, so that RCM is advocated as being particularly useful for assessing pigmented lesions.
2.
RCM images of normal skin (top) and of lentigo maligna (bottom). Copyright © 2017 Dr Rakesh Patalay: reproduced with permission.
The Caliber ID VivaScope imaging systems are the only commercially available RCM devices (distributed by MAVIG in Europe; www.vivascope.de/en/home.html). The Vivascope 1500 (and the previously available 1000 version) is a console‐based unit with a dermoscopic attachment, whereas the Vivascope 3000 is a hand‐held device designed for superior ergonomics, allowing imaging of lesions inaccessible for the 1500 version (Figure 3). Imaging can be undertaken by clinicians or technicians following appropriate training (Edwards 2016). The length of time required for diagnosis has been estimated at 15 minutes for the Vivascope 1500 (10 minutes of a technician's time for imaging and five minutes of a dermatologist's time for image interpretation) and 10 minutes for the Vivascope 3000 (Edwards 2016). The company has estimated the mean cost per use of the 1500 system, including dermoscopy, as GBP 120 based on 2014 National Health Service (NHS) reference costs and an indicative price for Vivascope 1500 of GBP 95,224 (Edwards 2016).
3.

Caliber ID Vivascope 1500 with 3000 attachment. Copyright © 2017 Guy's & St Thomas' NHS Foundation Trust: reproduced with permission.
Various algorithms have been proposed for the interpretation of RCM images, particularly for the diagnosis of melanoma (Dinnes 2018a); however, evaluation of lesion characteristics associated with other types of skin cancer, especially BCC, is ongoing (Gonzalez 2002; Guitera 2012). The lesion characteristics most recently proposed to be associated with BCC include the presence of 'dark silhouettes' or 'bright tumour islands' plus at least one of: 'streaming' polarisation of nuclei in neoplastic aggregates along the same axis of orientation; 'peripheral palisading' of nuclei at the tumour islands' periphery; dark 'peritumoral clefts' around the tumour islands; fibrotic stroma with 'thickened collagen bundles;' dilated and tortuous 'linear blood vessels' and 'coiled blood vessels'; 'bright dendritic structures' within tumour islands; and 'bright round cells' in the stroma. Nevertheless, BCC and cSCC specific criteria have yet to be fully established, with some suggestion that the keratotic surface of SCC may prohibit the use of imaging techniques (Edwards 2016).
Clinical pathway
The diagnosis of skin lesions occurs in primary, secondary, and tertiary care settings by both generalist and specialist healthcare providers. In the UK, people with concerns about a new or changing lesion will present to their GP rather than directly to a specialist in secondary care. If the GP has concerns then he/she usually refers the person to a specialist in secondary care – usually a dermatologist but sometimes to a surgical specialist such as a plastic surgeon or an ophthalmic surgeon. Suspicious skin lesions may also be identified in a referral setting, for example, by a general surgeon, and referred for a consultation with a skin cancer specialist (Figure 4). Skin cancers identified by other specialist surgeons (such as an ear, nose, and throat (ENT) specialist or maxillofacial surgeon) will usually be diagnosed and treated without further referral.
4.

Current clinical pathway for people with skin lesions.
Current UK guidelines recommend that all suspicious pigmented lesions presenting in primary care should be assessed by taking a clinical history and visual inspection using the seven‐point checklist (MacKie 1990); lesions suspected to be melanoma or cSCC (London Cancer Alliance 2013) should be referred for appropriate specialist assessment within two weeks (Chao 2013; Marsden 2010; NICE 2015). However, evidence is emerging to suggest that excision of melanoma by GPs is not associated with increased risk compared with outcomes in secondary care (Murchie 2017). In the UK, low risk BCC are usually recommended for routine referral, with urgent referral for those in whom a delay could have a significant impact on outcomes, for example, due to large lesion size or critical site (NICE 2015). Appropriately qualified generalist care providers increasingly undertake management of low risk BCC in the UK (NICE 2010) and Australia (CCAAC Network 2008).
For referred lesions, the specialist clinician will use history‐taking, visual inspection of the lesion (in conjunction with other skin lesions), and palpation of the lesion and associated lymph nodes in conjunction with dermoscopic examination to inform a clinical decision. If melanoma is suspected, then urgent 2 mm excision biopsy is recommended (Lederman 1985; Lees 1991); for cSCC, predetermined surgical margin excision or a diagnostic biopsy may be considered. BCC and premalignant lesions potentially eligible for non‐surgical treatment may undergo a diagnostic biopsy before initiation of therapy if there is diagnostic uncertainty. Equivocal (or more difficult to diagnose) melanocytic lesions for which a definitive clinical diagnosis cannot be reached may undergo surveillance to identify any lesion changes that would indicate excision biopsy or reassurance and discharge for those that remain stable over a period of time.
Theoretically, teledermatology consultations may aid appropriate triage of lesions into urgent referral; non‐urgent secondary care referral (e.g. for suspected BCC); or where available, referral to an intermediate care setting (e.g. clinics run by GPs with a special interest in dermatology). The distinction between setting and examiner qualifications and experience is important as specialist clinicians might work in primary care settings (e.g. in the UK, GPs with a special interest in dermatology and skin surgery who have undergone appropriate training), and generalists might practice in secondary care settings (e.g. plastic surgeons who do not specialise in skin cancer). The level of skill and experience in skin cancer diagnosis will vary for both generalist and specialist care providers and will also impact on test accuracy.
Prior test(s)
The diagnosis of skin cancer is based on history‐taking and clinical examination. In the UK, this is typically undertaken at two decision points – first in the GP surgery where a decision is made to refer or not to refer, and then a second time by a dermatologist or other secondary care clinician where a decision is made to biopsy or excise or not. Visual inspection of the skin is undertaken iteratively, using both implicit pattern recognition (non‐analytical reasoning) and more explicit 'rules' based on conscious analytical reasoning (Norman 2009), the balance of which will vary according to experience and familiarity with the diagnostic question. Various attempts have been made to formalise the 'mental rules' involved in analytical pattern recognition for melanoma (Friedman 1985; Grob 1998; MacKie 1985; MacKie 1990; Sober 1979; Thomas 1998); however, visual inspection for keratinocyte skin cancers relies primarily on pattern recognition. Accuracy varies according to the expertise of the clinician. Primary care physicians have been found to miss over half of BCC (Offidani 2002) and to inappropriately diagnose one third of BCC (Gerbert 2000). In contrast, one Australian study found that trained dermatologists were able to detect 98% of BCC, but with a specificity of only 45% (Green 1988).
A range of technologies have emerged to aid diagnosis to reduce the number of diagnostic biopsies or inappropriate surgical procedures. Dermoscopy using a hand‐held microscope has become the most widely used tool for clinicians to improve diagnostic accuracy of pigmented lesions, in particular for melanoma (Argenziano 1998; Argenziano 2012; Haenssle 2010; Kittler 2002), although is less well established for the diagnosis of BCC or cSCC. The diagnostic accuracy, and comparative accuracy, of visual inspection and dermoscopy for keratinocyte skin cancer has been evaluated in a further review in this series (Dinnes 2018b).
Role of index test(s)
RCM is most likely to have a role as an additional test to better identify lesions that can be monitored or reassured as being benign, instead of being sent for urgent excision (Edwards 2016), or for low risk BCC to identify those eligible for non‐surgical treatment without the need for a diagnostic biopsy. RCM could also be considered as a primary diagnostic test (i.e. as a potential replacement for dermoscopy).
Delay in diagnosis of a BCC as a result of a false‐negative test is not as serious as for melanoma because BCCs are usually slow growing and very unlikely to metastasise (Betti 2017). However, delayed diagnosis can result in a larger and more complex excision with consequent greater morbidity. Very sensitive diagnostic tests for BCC, however, may compromise on lower specificity leading to a higher false‐positive rate, and an enormous burden of skin surgery, such that a balance between sensitivity and specificity is needed. The situation for cSCC is more similar to melanoma in that the consequences of falsely reassuring a person that they do not have skin cancer can be serious and potentially fatal. Thus, a good diagnostic test for cSCC should demonstrate high sensitivity and a corresponding high negative predictive value. A test that can reduce false‐positive clinical diagnoses without missing true cases of disease has patient and resource benefits. False‐positive clinical diagnoses not only cause unnecessary morbidity from the biopsy, but could lead to initiation of inappropriate therapies and also increase patient anxiety.
A further postulated advantage of RCM is its ability to non‐invasively differentiate seborrhoeic keratoses or non‐melanocytic lesions from a population of pigmented lesions (de Carvalho 2015; Nascimento 2014; Menge 2016). RCM could also develop a role in guiding definitive therapeutic margins (Edwards 2016), both pre‐ and intraoperatively and to estimate response to topical chemotherapy for lentigo maligna and potentially BCCs; however, these uses are not under consideration in this review.
Alternative test(s)
A number of other tests have been reviewed as part of our series of Cochrane DTA reviews on the diagnosis of keratinocyte skin cancers, including visual inspection and dermoscopy (Dinnes 2018b), teledermatology (Chuchu 2018a), mobile phone applications (Chuchu 2018b), computer‐assisted diagnosis (CAD) techniques (Ferrante di Ruffano 2018a), optical coherence tomography (OCT) (Ferrante di Ruffano 2018b), exfoliative cytology (Ferrante di Ruffano 2018c), and high‐frequency ultrasound (Dinnes 2018c).
OCT is an emerging optical imaging technology based on interferometry using a near infra‐red light source. It exploits differences in the refractive index in the skin to create vertically sectioned images in vivo, in real time, and has a relatively high depth of penetration, allowing dermal lesions to be delineated (Olsen 2015). OCT is considered to be particularly useful for the differentiation of non‐pigmented lesions. Pigmented lesions produce regular scattering patterns which inhibit the differentiation of malignant from benign lesions (Olsen 2015; Gambichler 2015). The use of high‐frequency ultrasound has been advocated in diagnosing a range of skin conditions, including skin cancer, infection, and inflammatory conditions (Kleinerman 2012), with malignant lesions reportedly appearing as hypoechogenic areas surrounded by a hyperechogenic dermis. Melanomas in particular also reportedly appear homogenous and with well‐defined margins (e.g. Harland 2000). CAD or artificial intelligence‐based techniques process and manipulate lesion data using predefined algorithms to identify the features that discriminate malignant from benign lesions (Rajpara 2009; Esteva 2017). These techniques have been incorporated into commercially available hand‐held devices for ease of use in a clinic setting, including SIAscopy (Moncrieff 2002; Walter 2012), MelaFind (Monheit 2011; Wells 2012; Hauschild 2014), and the Nevisense Electrical Impedance Spectroscopy system (Malvehy 2014). However, CAD has most commonly been applied to digital dermoscopy images (Rajpara 2009; Esteva 2017).
We also did not assess histopathological confirmation following lesion excision, because it is the established reference standard for skin cancer diagnosis and will be one of the standards against which the index tests are evaluated in these reviews
Rationale
This series of reviews of diagnostic tests used to assist the clinical diagnosis of BCC and cSCC, aims to identify the most accurate approaches to diagnosis and to provide clinical and policy decision‐makers with the highest possible standard of evidence on which to base decisions. With the increasing availability of a wider range of tests, there is a need to differentiate and appropriately triage keratinocyte skin cancers to avoid sending too many people with benign or low risk lesions for a specialist opinion and possible excision or biopsy, while not missing those people who have lesions that require treatment.
Although a set of billing codes for the USA have been agreed since January 2016 (Rajadhyaksha 2017), RCM is not recommended for routine use in the UK (Edwards 2016), Australia (Guitera 2017), or New Zealand (Sobarun 2015). To date, the use of RCM has been limited by expense (in terms of both equipment and staff time) and the need for specialised training. Some studies have demonstrated high sensitivity and specificity among experienced RCM users, however, in at least one study, the accuracy of the group on average was higher than that of any one individual observer (Farnetani 2015). Our own systematic review of 18 studies of RCM for the diagnosis of melanoma suggested that although RCM may augment diagnostic sensitivity when used in conjunction with clinical inspection and dermoscopy, its main contribution was an increase in specificity, reducing the number of people receiving unnecessary surgery by up to three‐quarters compared to dermoscopy (Dinnes 2018a).
Available systematic reviews of RCM for keratinocyte skin cancers are limited by out of date searches and methods. Xiong 2016 failed to consider differences in study populations and varying definitions of the target condition, and used an out of date meta‐analytic approach. Mogensen 2007 did not report the use of systematic methods for study inclusion or extraction and did report undertaking quality assessment, while Edwards 2016 focused on selected studies considered to be more applicable to a UK setting. In this rapidly advancing field, there is a need for an up‐to‐date analysis of the accuracy of RCM for the diagnosis of keratinocyte skin cancer.
This review follows a generic protocol which covers the full series of Cochrane DTA Reviews for the diagnosis of keratinocyte skin cancer (Dinnes 2015a). The Background and Methods sections of this review therefore use some text that was originally published in the protocol (Dinnes 2015a) and text that overlaps some of our other reviews (Dinnes 2018a; Dinnes 2018b).
Objectives
To determine the diagnostic accuracy of RCM for the detection of BCC, cSCC, or any skin cancer in adults with any suspicious lesion and lesions that are difficult to diagnose (equivocal); and to compare its accuracy with that of usual practice (visual inspection or dermoscopy, or both).
Accuracy was estimated separately according to the point in the clinical pathway at which RCM was evaluated:
in participants with any suspicious lesion, where RCM might have been used as an alternative to dermoscopy or to supplement visual inspection alone;
in participants with equivocal (or more difficult to diagnose) lesions in whom a clear management decision could not be made following visual inspection and dermoscopy, where RCM might have been used as an addition to visual inspection or dermoscopy, or both.
Studies that did not clearly fit into either of these two groups were considered as 'other lesion' studies. The terms equivocal and 'difficult to diagnose' have been used, and should be interpreted, interchangeably throughout this review.
Secondary objectives
To determine the diagnostic accuracy of RCM for the detection of any skin cancer in adults, where keratinocyte skin cancers made up at least 50% of included skin cancers, and to compare its accuracy with visual inspection or dermoscopy, or both.
Accuracy was estimated separately according to the point in the clinical pathway at which RCM was evaluated:
where it might have been used as an alternative to dermoscopy in participants with any lesion suspicious for melanoma;
where it might have been used as an addition to visual inspection or dermoscopy, or both, in participants with equivocal lesions in whom a clear management decision could not be made following visual inspection and dermoscopy alone.
For the detection of BCC or cSCC (the primary target conditions):
to compare the accuracy of RCM to dermoscopy where both tests were evaluated in the same studies (direct test comparisons);
to determine the diagnostic accuracy of individual algorithms for RCM;
to determine the effect of observer experience.
Investigation of sources of heterogeneity
We set out to address a range of potential sources of heterogeneity for investigation across our series of reviews, as outlined in our generic protocol (Dinnes 2015a) and described in Appendix 3; however, our ability to investigate these was necessarily limited by the available data on each individual test reviewed.
Methods
Criteria for considering studies for this review
Types of studies
We included test accuracy studies that allow comparison of the result of the index test with that of a reference standard, including the following:
studies where all participants received a single index test and a reference standard;
studies where all participants received more than one index test(s) and reference standard;
studies where participants were allocated (by any method) to receive different index tests or combinations of index tests and all received a reference standard (between‐person comparative (BPC) studies);
studies that recruited series of participants unselected by true disease status (referred to as case series for the purposes of this review);
diagnostic case‐control studies that separately recruited diseased and non‐diseased groups (see Rutjes 2005);
both prospective and retrospective studies; and
studies where previously acquired clinical or dermoscopic images were retrieved and prospectively interpreted for study purposes.
We excluded studies from which we could not extract 2×2 contingency data, or if they included fewer than five cases of BCC or cSCC or fewer than five benign lesions. The size threshold of five is arbitrary. However such small studies are unlikely to add precision to estimate of accuracy.
Studies available only as conference abstracts were excluded; however, attempts were made to identify full papers for potentially relevant conference abstracts (Searching other resources).
Participants
We included studies in adults with lesions suspicious for skin cancer.
We excluded studies that recruited only participants with malignant diagnoses and studies that compared test results in participants with malignancy compared with test results based on 'normal' skin as controls, due to the bias inherent in such comparisons (Rutjes 2006).
We excluded studies conducted in children or which clearly reported more than 50% of participants aged 16 years and under.
Index tests
We included studies evaluating RCM alone, or RCM in comparison to usual practice (visual inspection or dermoscopy, or both).
We included all established algorithms or checklists to assist diagnosis by RCM. We included studies developing new algorithms or methods of diagnosis (i.e. derivation studies) if they:
used a separate independent 'test set' of participants or images to evaluate the new approach, or
investigated lesion characteristics that had previously been suggested as associated with BCC or cSCC and the study reported accuracy based on the presence or absence of particular combinations of characteristics.
We excluded studies if they:
used a statistical model to produce a data driven equation, or algorithm based on multiple diagnostic features, with no separate test set;
used cross‐validation approaches such as 'leave‐one‐out' cross‐validation (Efron 1983);
evaluated the accuracy of the presence or absence of individual lesion characteristics or morphological features, with no overall diagnosis of malignancy.
There were no exclusions made according to test observer.
Target conditions
Two primary target conditions were defined as the detection of:
basal cell carcinoma (BCC), including all subtypes;
invasive cutaneous squamous cell carcinoma (cSCC) (we did not consider cSCC in situ or Bowen's disease as disease positive).
An additional definition of the target condition was considered in secondary analysis, the detection of:
any skin cancer, including BCC, cSCC, melanoma, or any rare skin cancer (e.g. Merkel cell cancer), as long as skin cancers other than melanoma made up more than 50% of the disease positive group. Data from studies in which melanoma accounted for more than 50% of skin cancers were included in the review of RCM for the diagnosis of melanoma (Dinnes 2018a).
Reference standards
The ideal reference standard was histopathological diagnosis in all eligible lesions. A qualified pathologist or dermatopathologist should have performed histopathology. Ideally, reporting should have been standardised detailing a minimum dataset to include the type of skin cancer (BCC, cSCC) and subtype of BCC and may also have referred to the TNM (tumour, node, and metastasis) classification of staging for cSCC (Royal College of Pathologists 2014). We did not apply the reporting standard as a necessary inclusion criterion, but extracted any pertinent information.
Partial verification (applying the reference test only to a subset of participants undergoing the index test) was of concern given that lesion excision or biopsy were unlikely to be carried out for all benign‐appearing lesions within a representative population sample. Therefore, we accepted clinical follow‐up of benign‐appearing lesions as an eligible reference standard, while recognising the risk of differential verification bias (as misclassification rates of histopathology and follow‐up will differ).
Additional eligible reference standards included cancer registry follow‐up and 'expert opinion' with no histology or clinical follow‐up. Cancer registry follow‐up is considered less desirable than active clinical follow‐up, as it is not carried out within the control of the study investigators. Furthermore, if participant‐based analyses as opposed to lesion‐based analyses are presented (as for cancer registry follow‐up), it may be difficult to determine whether the detection of a malignant lesion during follow‐up was the same lesion that originally tested negative on the index test.
All of the above were eligible reference standards with the following caveats:
all study participants with a final diagnosis of the target disorder must have had a histological diagnosis, either subsequent to the application of the index test or after a period of clinical follow‐up, and
at least 50% of all participants with benign lesions must have either had a histological diagnosis or clinical follow‐up to confirm benignity.
Search methods for identification of studies
Electronic searches
The Information Specialist (SB) carried out a comprehensive search for published and unpublished studies. A single large literature search was conducted to cover all topics in the programme grant (see Appendix 1 for a summary of reviews included in the programme grant). This allowed for the screening of search results for potentially relevant papers for all reviews at the same time. A search combining disease related terms with terms related to the test names, using both text words and subject headings was formulated. The search strategy was designed to capture studies evaluating tests for the diagnosis or staging of skin cancer. As the majority of records were related to the searches for tests for staging of disease, a filter using terms related to cancer staging and to accuracy indices was applied to the staging test search, to try to eliminate irrelevant studies, for example, those using imaging tests to assess treatment effectiveness. A sample of 300 records that would be missed by applying this filter was screened and the filter adjusted to include potentially relevant studies. When piloted on MEDLINE, inclusion of the filter for the staging tests reduced the overall numbers by around 6000. The final search strategy, incorporating the filter, was subsequently applied to all bibliographic databases as listed below (Appendix 4). The final search result was cross‐checked against the list of studies included in five systematic reviews; our search identified all but one of the studies, and this study was not indexed on MEDLINE. The Information Specialist devised the search strategy, with input from the Information Specialist from Cochrane Skin. No additional limits were used.
We searched the following bibliographic databases to 29 August 2016 for relevant published studies:
MEDLINE via Ovid (from 1946);
MEDLINE In‐Process & Other Non‐Indexed Citations via Ovid; and
Embase via Ovid (from 1980).
We searched the following bibliographic databases to 30 August 2016 for relevant published studies:
the Cochrane Central Register of Controlled Trials (CENTRAL) 2016, Issue 7, in the Cochrane Library;
the Cochrane Database of Systematic Reviews (CDSR) 2016, Issue 8, in the Cochrane Library;
Cochrane Database of Abstracts of Reviews of Effects (DARE) 2015, Issue 2;
CRD HTA (Health Technology Assessment) database 2016, Issue 3; and
CINAHL (Cumulative Index to Nursing and Allied Health Literature via EBSCO from 1960).
We searched the following databases for relevant unpublished studies using a strategy based on the MEDLINE search:
CPCI (Conference Proceedings Citation Index), via Web of Science™ (from 1990; searched 28 August 2016); and
SCI Science Citation Index Expanded™ via Web of Science™ (from 1900, using the 'Proceedings and Meetings Abstracts' Limit function; searched 29 August 2016).
We searched the following trials registers using the search terms 'melanoma', 'squamous cell', 'basal cell' and 'skin cancer' combined with 'diagnosis':
Zetoc (from 1993; searched 28 August 2016).
The US National Institutes of Health Ongoing Trials Register (www.clinicaltrials.gov); searched 29 August 2016.
NIHR Clinical Research Network Portfolio Database (www.nihr.ac.uk/research‐and‐impact/nihr‐clinical‐research‐network‐portfolio/); searched 29 August 2016.
The World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch/); searched 29 August 2016.
We aimed to identify all relevant studies regardless of language or publication status (published, unpublished, in press, or in progress). We applied no date limits.
Searching other resources
We screened relevant systematic reviews identified by the searches for their included primary studies, and included any missed by our searches. We checked the reference lists of all included papers, and subject experts within the author team reviewed the final list of included studies. There was no electronic citation searching.
Data collection and analysis
Selection of studies
At least one review author (JD or NC) screened titles and abstracts with any queries discussed and resolved by consensus. A pilot screen of 539 MEDLINE references showed good agreement (89% with a kappa of 0.77) between screeners. Primary test accuracy studies and test accuracy reviews (for scanning of reference lists) of any test used to investigate suspected melanoma, BCC, or cSCC were included at initial screening. Both a clinical reviewer (from one of a team of 12 clinician reviewers) and a methodologist reviewer (JD or NC) independently applied inclusion criteria to all full text articles (Appendix 3). We resolved disagreements by consensus or by a third party (JDD, CD, HW, and RM). We contacted authors of eligible studies when insufficient data were presented to allow for the construction of 2×2 contingency tables.
Data extraction and management
One clinical (as detailed above) and one methodologist reviewer (JD, NC or LFR) independently extracted data concerning details of the study design; participants; index test(s) or test combinations; and criteria for index test positivity, reference standards, and data required to populate a 2×2 diagnostic contingency table for each index test using a piloted data extraction form. We extracted data at all available index test thresholds. We resolved disagreements by consensus or by a third party (JDD, CD, HW, and RM). We entered data into Review Manager 5 (Review Manager 2014).
We contacted authors of included studies where information relating to the diagnostic threshold was missing. We contacted authors of conference abstracts published from 2013 to 2015 to ask whether full data were available. If we identified no full paper, we marked conference abstracts as 'pending' and will revisit them in a future review update.
Dealing with multiple publications and companion papers
Where we identified multiple reports of a primary study, we maximised yield of information by collating all available data. Where there were inconsistencies in reporting or overlapping study populations, we contacted study authors for clarification in the first instance. If this contact with authors was unsuccessful, we used the most complete and up‐to‐date data source where possible.
Assessment of methodological quality
We assessed risk of bias and applicability of included studies using the QUADAS‐2 checklist (Whiting 2011), tailored to the review topic (see Appendix 6). The modified QUADAS‐2 tool was piloted on a small number of included full text articles. One clinical and one methodologist reviewer (JD, NC, or LFR) independently assessed quality for the remaining studies; we resolved any disagreement by consensus or by a third party where necessary (JDD, CD, HW, and RM).
Statistical analysis and data synthesis
For the detection of each definition of the target condition, we conducted separate analyses according to the point in the clinical pathway that RCM was applied. There were three groups of studies formed:
RCM used in participants with any lesion suspicious for skin cancer (i.e. no attempt to exclude cancers diagnosed as obvious BCCs or SCCs or as clearly benign on visual inspection or dermoscopy was described (denoted as studies in 'any suspicious lesion'));
RCM used as an addition to dermoscopy in participants with equivocal lesions in whom a clear management decision could not be made following visual inspection and dermoscopy (denoted as studies in 'equivocal' lesions);
'Other' studies which did not fit into either of these categories.
Our unit of analysis for all analyses was the lesion rather than the participant. This is because 1. in skin cancer initial treatment is directed to the lesion rather than systemically (thus it is important to be able to correctly identify cancerous lesions for each person), and 2. it is the most common way in which the primary studies reported data. Although there was a theoretical possibility of correlations of test errors when the same people contributed data for multiple lesions, most studies included very few people with multiple lesions and any potential impact on findings was likely to be very small, particularly in comparison with other concerns regarding risk of bias and applicability. For each analysis undertaken, we included only one dataset per study to avoid overcounting of lesions. Where an individual study assessed multiple thresholds, we selected datasets for correct diagnosis of each type of malignancy as opposed to data for the decision to excise lesions. If studies reported data for multiple observers, we used data from the most experienced observer, and used data for a single observer's diagnosis in preference to a consensus or mean across observers. If we were unable to choose a dataset based on the above 'rules,' we made a random selection of one dataset per study.
For each index test, algorithm or checklist under consideration, we plotted estimates of sensitivity and specificity on coupled forest plots and in receiver operating characteristic (ROC) space. For tests that reported commonly used thresholds, we estimated summary operating points (summary sensitivities and specificities) with 95% confidence and prediction regions using the bivariate hierarchical model (Chu 2006; Reitsma 2005). Where there were inadequate data available for the model to converge, we simplified the model, first by assuming no correlation between estimates of sensitivity and specificity and second by setting estimates of near zero variance terms to zero (Takwoingi 2017). Where all studies reported 100% sensitivity (or 100% specificity), we summed the number with disease (or no disease) across studies and used this to compute a binomial exact 95% CI. We assessed heterogeneity in estimates of sensitivity and specificity by inspection of the magnitude and statistical significance of the estimates of variance terms in the bivariate model.
We included data on the accuracy of visual inspection or dermoscopy, to allow comparisons of tests, only if reported in the studies of RCM due to the known substantial unexplained heterogeneity in all studies of the accuracy of these tests (Dinnes 2018a). We made comparisons between tests using RCM data from all RCM studies, and then only using RCM data from studies that also reported visual inspection or dermoscopy data for the same participants to enable a robust direct comparison (Takwoingi 2013).
For computation of likely numbers of true‐positive, false‐positive, false‐negative, and true‐negative findings in the 'Summary of findings' tables, we applied summary sensitivity and specificity estimates to lower, median, and upper quartiles of the prevalence observed in the study groups.
We fitted bivariate models using the meqrlogit command in STATA 13.
Investigations of heterogeneity
We initially examined heterogeneity between studies by visually inspecting the forest plots of sensitivity and specificity and summary ROC plots. Where there were a sufficient number of studies, we performed meta‐regression by adding the potential source of heterogeneity as a covariate to a hierarchical model.
Sensitivity analyses
We performed no sensitivity analyses.
Assessment of reporting bias
Because of uncertainty about the determinants of publication bias for diagnostic accuracy studies and the inadequacy of tests for detecting funnel plot asymmetry (Deeks 2005), we performed no tests to detect publication bias.
Results
Results of the search
The search identified and screened 34,517 unique references for inclusion. Of these, 1051 full text papers were reviewed for eligibility for any one of the suite of reviews of tests to assist in the diagnosis of melanoma or keratinocyte skin cancer. Of the 1051 full text papers assessed, 848 were excluded from all reviews in our series (see Figure 5 PRISMA flow diagram of search and eligibility results).
5.
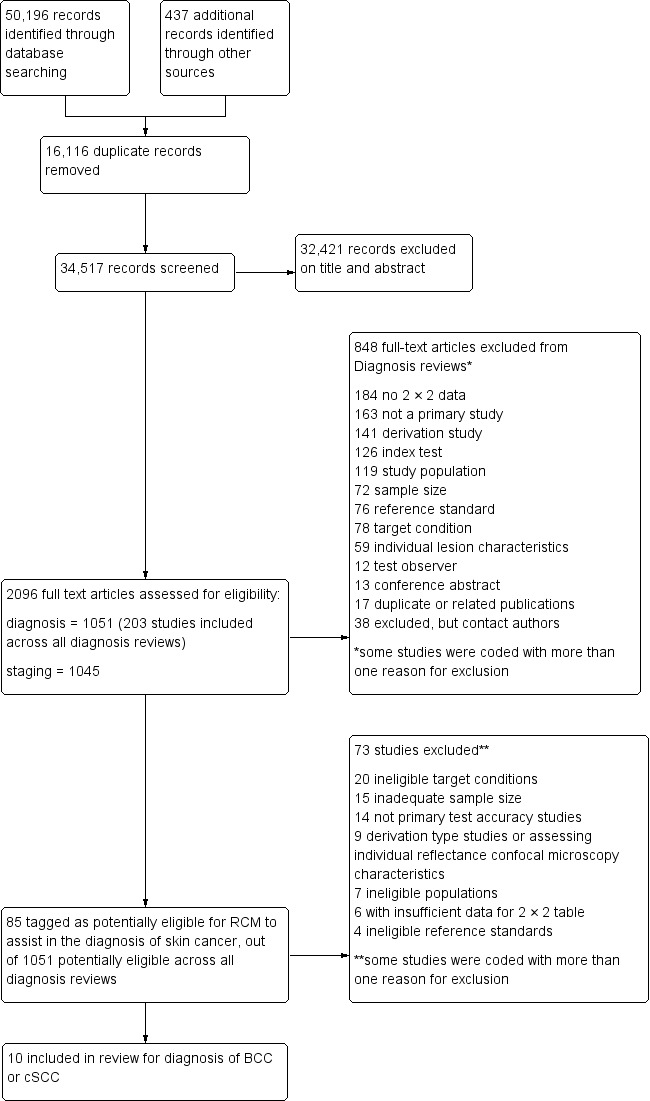
PRISMA flow diagram.
Of the 83 studies tagged as potentially eligible for the two RCM reviews, 22 publications were included, reporting 22 individual studies: 10 in this review and 18 in the review of RCM for the detection of melanoma (six were included in both). Reasons for exclusion included publications not being primary test accuracy studies (14 studies); lack of test accuracy data (six studies); because they were derivation studies developing new algorithms or approaches to diagnosis without the use of separate training and test sets of data (five studies); included ineligible populations (e.g. including only malignant lesions (six studies); did not assess eligible target conditions or did not adequately define the target condition (20 studies); inadequate sample size (15 studies); assessed the accuracy of individual RCM characteristics (four studies); or used ineligible reference standards (i.e. less than 50% of benign group with final diagnosis established by histology or follow‐up; four studies). A list of the 73 studies excluded from this review with reasons for exclusion is provided in the Characteristics of excluded studies table, with a list of all studies excluded from the full series of reviews available as a separate pdf (please contact skin.cochrane.org for a copy of the pdf).
We contacted the corresponding authors of six publications and asked them to supply further information for the purposes of this review. To date, responses have been received from only one author to allow study inclusion (Incel 2015). In addition, Professor Pellacani provided information on lesion overlap between several identified studies that were coauthored by him.
This review reported on 11 cohorts of participants with lesions suspected of skin cancer, published in 10 study publications, providing 91 datasets for RCM and four for usual practice (visual inspection (one cohort) or dermoscopy (three cohorts)). A total of 2037 lesions with 464 BCCs were included in the 11 datasets reporting data for BCC, and 834 lesions with 71 cSCCs were included in the four datasets reporting data for cSCC. The total number of study participants could not be estimated due to lack of reporting in study publications. The Pellacani 2014 study was split into two cohorts for the purposes of this review: one cohort of lesions equivocal on dermoscopy denoted as the RCM 'consultation' group by the study authors (Pellacani 2014a (cons)); and the other cohort of lesions recommended for excision on the basis of clear cut clinical or dermoscopic findings, denoted as the RCM 'documentation' group by the study authors (Pellacani 2014b (doc)). There is a description of the various algorithms and thresholds used for diagnosis across the studies in Appendix 7.
Methodological quality of included studies
The overall methodological quality of all 11 included study cohorts is summarised in Figure 6 and Figure 7. Studies were generally at high or unclear risk of bias across all domains apart from the index test and of high or unclear concern regarding applicability of the evidence.
6.
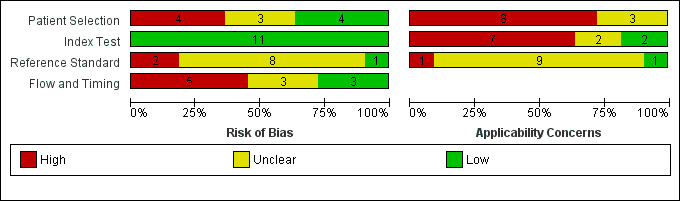
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies.
7.
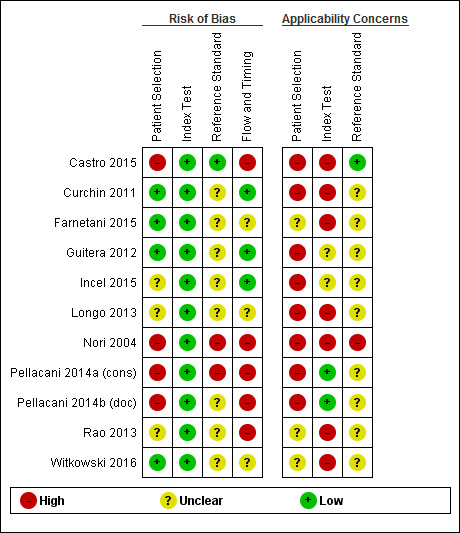
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study.
Almost two‐thirds of cohorts were at high (four cohorts) or unclear (three cohorts) risk of bias for participant selection due to exclusion of poor‐quality images (three cohorts), use of a case‐control type design (one cohort) or unclear participant selection (three cohorts). All cohorts were at high (eight cohorts) or unclear (three cohorts) concern regarding applicability of included participants and setting, due to restricted study populations (with four studies including only participants with lesions suspected of melanoma, two including only those with high clinical suspicion of BCC, and two with more narrowly defined populations such as nodular lesions or proliferative lesions) and inclusion of multiple lesions per participant (five cohorts). Eight of the 11 cohorts included lesions selected for excision based on the clinical or dermoscopic diagnosis or selected retrospectively from histopathology databases; this was not considered of high concern regarding applicability for RCM studies as the primary role for RCM is to reduce unnecessary excisions.
All cohorts were at low risk of bias in the index test domain. Over half of studies were high concern for the applicability of the index test (seven cohorts), due to remote RCM interpretation (five cohorts), blinding to clinical information (three cohorts), presentation of consensus diagnoses only (one cohort), lack of detail regarding the diagnostic threshold used (two cohorts), or interpretation by a non‐expert observer (two cohorts). It is of note that eight of the 11 cohorts were produced by, or in collaboration with, the same expert research team, led by Professor Pellacani which may further reduce the generalisability of results.
One cohort was at low risk of bias for the reference standard, two at high risk due to inadequate reference standards (greater than 20% of the disease negative group with final diagnosis by follow‐up or expert opinion), and eight at unclear risk due to unclear blinding of the reference standard to the RCM result. None of the cohorts reported blinding of histology to the referral diagnosis (based on clinical examination or dermoscopy), but this was not incorporated into the overall risk of bias for this domain. For the applicability of the reference standard, one cohort was at high risk due to the use of expert observer diagnosis as the reference standard and nine cohorts were unclear regarding histopathology interpretation by an experienced histopathologist or by a dermatopathologist.
For participant flow and timing, three cohorts were at low risk of bias, five at high risk, and three at unclear risk. Three cohorts did not use the same reference standard for all participants (differential verification), seven cohorts were unclear on the interval between the application of the index test and excision for histology, and four cohorts did not include all participants in the analysis primarily due to technical difficulties in imaging.
Findings
1. Target condition: basal cell carcinoma
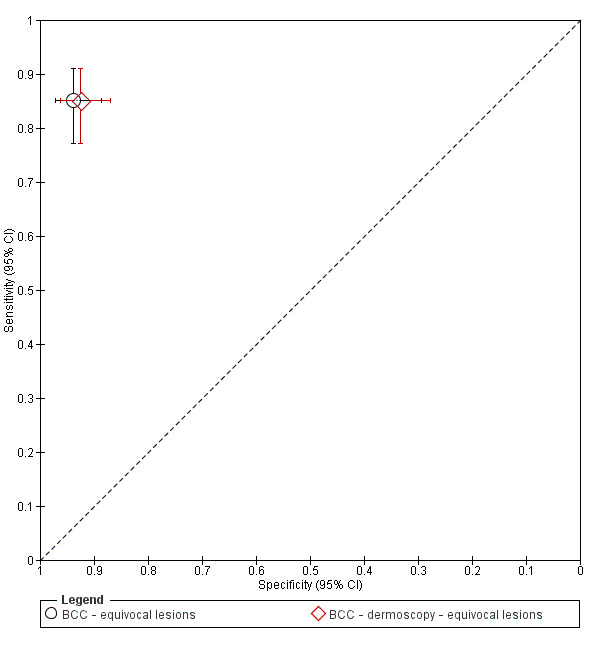
In this section, we presented the results for studies of RCM versus visual inspection or dermoscopy for the target condition of BCC, according to the study population: studies in participants with any lesions suspicious for melanoma versus those in participants with equivocal lesions. The included studies used a number of different approaches to RCM diagnosis; see Appendix 7 for details. Appendix 8 provides summary characteristics of studies. Table 2 presents the results for the primary analyses. Figure 8 gives forest plots of study data for each analysis in this table with studies plotted in ROC space in Figure 9 and Figure 10. Table 3 and Figure 11 compare results between observers.
1. Comparison of reflectance confocal microscopy with dermoscopy for the detection of basal cell carcinoma.
| Test | Studies | Lesions (cases) | Sensitivity (95% CI) | Specificity (95% CI) |
| Any suspicious lesion studies (all studies) | ||||
| RCM | 4 | 912 | 0.76 (0.45 to 0.92) | 0.95 (0.66 to 0.99) |
| Dermoscopy | 0 | — | — | — |
| Any suspicious lesion studies (direct comparisons) | ||||
| RCM | 0 | — | — | — |
| Dermoscopy | 0 | — | — | — |
| Equivocal lesion studies (all studies) | ||||
| RCM | 3 | 668 | 0.94 (0.79 to 0.98) | 0.85 (0.72 to 0.92) |
| Dermoscopy | 1 | 260 | 0.85 (0.77 to 0.91) | 0.92 (0.87 to 0.96) |
| Equivocal lesion studies (direct comparisons) | ||||
| RCM | 1 | 260 | 0.85 (0.77 to 0.91) | 0.94 (0.89 to 0.97) |
| Dermoscopy | 1 | 260 | 0.85 (0.77 to 0.91) | 0.92 (0.87 to 0.96) |
CI: confidence interval; RCM: reflectance confocal microscopy.
8.
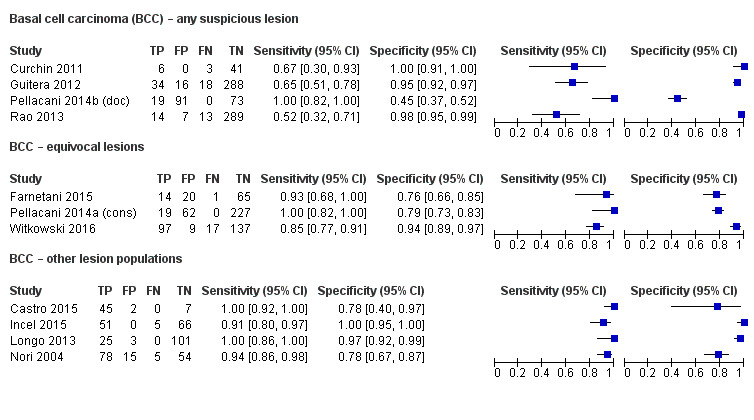
Forest plot of tests: RCM for the detection of BCC in any suspicious lesion (top), equivocal lesions (centre), other lesion (bottom) populations. CI: confidence interval; FN: false negative; FP: false positive; TN: true negative; TP: true positive.
9.
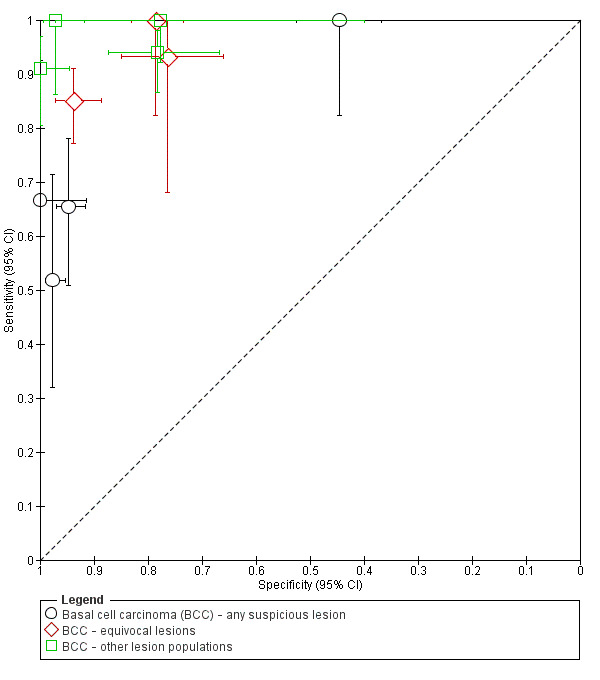
ROC Plot of tests: RCM for the detection of BCC in any suspicious lesion, equivocal lesions, other lesion populations.
10.
ROC Plot of tests: reflectance confocal microscopy versus dermoscopy in equivocal lesions (Witkowski 2016). BCC: basal cell carcinoma; CI: confidence interval.
2. Results by observer experience.
| Person/image | Observer experience | Studies (n) | Lesions (cases) | Pooled sensitivity (95% CI) |
Pooled specificity (95% CI) |
| Detection of BCC | |||||
| In person | High | 3 | 545 (83) | 1.00 (0.96 to 1.00) | 0.67 (0.45 to 0.83) |
| Image | High | 4 | 908 (119) | 0.86 (0.50 to 0.97) | 0.94 (0.86 to 0.98) |
| Both | High | 7 | 1453 (202) | 0.98 (0.74 to 1.00) | 0.87 (0.71 to 0.95) |
| In person | Low | 2 | 368 (34) | 0.75 (0.53 to 0.88) | 0.97 (0.64 to 1.00) |
| Image | Low | 2 | 252 (98) | 0.92 (0.82 to 0.97) | 0.84 (0.75 to 0.90) |
| Both | Low | 4 | 620 (132) | 0.85 (0.69 to 0.93) | 0.91 (0.81 to 0.96) |
| In person | NR | 1 | 122 (56) | 0.91 (0.80 to 0.97) | 1.00 (0.95 to 1.00) |
| Image | NR | 1 | 260 (114) | 0.85 (0.77 to 0.91) | 0.94 (0.78 to 0.97) |
| Both | NR | 2 | 382 (170) | 0.88 (0.80 to 0.93) | 0.98 (0.74 to 1.00) |
| Detection of cSCC | |||||
| In person | High | 0 | 0 | — | — |
| Image | High | 2 | 452 (47) | 0.95 (0.06 to 1.00) | 0.99 (0.40 to 1.00) |
| Both | High | 2 | 452 (47) | 0.95 (0.06 to 1.00) | 0.99 (0.40 to 1.00) |
| In person | Low | 1 | 318 (39) | 0.41 (0.26 to 0.58) | 0.97 (0.95 to 1.00) |
| Image | Low | 0 | 0 | — | — |
| Both | Low | 1 | 318 (39) | 0.41 (0.26 to 0.58) | 0.97 (0.95 to 1.00) |
| In person | NR | 1 | 122 (11) | 0.82 (0.48 to 0.98) | 0.96 (0.91 to 0.99) |
| Image | NR | 1 | 260 (13) | 0.77 (0.46 to 0.95) | 0.98 (0.96 to 1.00) |
| Both | NR | 2 | 382 (24) | 0.79 (0.59 to 0.91) | 0.98 (0.96 to 0.99) |
| Detection of KER | |||||
| In person | High | 0 | 0 | — | — |
| Image | High | 3 | 552 (161) | 0.94 (0.70 to 0.99) | 0.86 (0.82 to 0.90) |
| Both | High | 3 | 552 (161) | 0.94 (0.70 to 0.99) | 0.86 (0.82 to 0.90) |
| In person | Low | 2 | 368 (95) | 0.80 (0.71 to 0.87) | 0.85 (0.81 to 0.89) |
| Image | Low | 1 | 90 (35) | 0.83 (0.66 to 0.93) | 0.85 (0.74 to 0.92) |
| Both | Low | 3 | 458 (130) | 0.81 (0.73 to 0.87) | 0.85 (0.81 to 0.89) |
| In person | NR | 0 | 0 | — | — |
| Image | NR | 1 | 260 (140) | 0.91 (0.85 to 0.95) | 0.80 (0.72 to 0.87) |
| Both | NR | 1 | 260 (140) | 0.91 (0.85 to 0.95) | 0.80 (0.72 to 0.87) |
BCC: basal cell carcinoma; CI: confidence interval; cSCC: cutaneous squamous cell carcinoma; KER: any keratinocyte skin cancer; n: number; NR: not reported.
11.

Forest plot of accuracy of reflectance confocal microscopy to detect basal cell carcinoma (BCC) by experience (separately for in‐person and image‐based studies). CI: confidence interval; FN: false negative; FP: false positive; TN: true negative; TP: true positive.
Any suspicious lesion
The following section documents studies where RCM appeared to have been evaluated in participants with any lesion scheduled for excision. These populations are likely to include both clinically or dermoscopically obvious BCCs, along with a proportion of more difficult to diagnose (equivocal) lesions so that RCM was being evaluated as an addition to visual inspection alone or visual inspection with dermoscopy.
Four studies provided data for the detection of BCC with RCM (Curchin 2011; Guitera 2012; Pellacani 2014b (doc); Rao 2013). A total of 912 lesions were included with 107 cases of BCC. One study provided data for expert and non‐expert observers; however, only 284 of the 334 included lesions were evaluated by both readers (Rao 2013). The total number of participants could not be reported due to lack of reporting in two of the four studies (Guitera 2012; Rao 2013; Guitera 2012 reported overall number of participants but not the number with lesions included in the test set of data).
All studies were case series and undertaken in secondary or specialist clinic settings. Lesions were scheduled for excision reportedly for cosmetic or medical reasons (Rao 2013), reasons not reported (Curchin 2011), to rule out an 'epithelial tumour' or melanoma (Guitera 2012), or due to clinical or dermoscopy suspicion of melanoma (Pellacani 2014b (doc)). Three studies included any type of lesion, and one restricted to pigmented lesions only (Pellacani 2014b (doc)). Sample sizes ranged from 50 to 356 lesions. The median lesion to participant ratio in three studies was 1.19 (range 1.07 to 1.20). The mean prevalence of BCC was 13% (range 8% to 18%); the mean prevalence of any malignancy (BCC, cSCC, or melanoma) was 34% (range 22% to 56%). All studies also reported data for the diagnosis of melanoma (Dinnes 2018a). Studies generally included a varied spectrum of benign lesions including benign melanocytic naevi (Guitera 2012; Pellacani 2014b (doc); Rao 2013), Spitz naevi (Guitera 2012; Pellacani 2014b (doc); Rao 2013), and seborrhoeic or actinic keratoses (Guitera 2012; Pellacani 2014b (doc); Rao 2013), or both. All studies made the reference standard diagnosis by histology alone (i.e. all lesions either excised or biopsied).
All four studies used the Vivascope 1500 imaging system; three reporting the use of dermoscopic images to help guide acquisition of RCM images (Curchin 2011; Guitera 2012; Rao 2013). The studies reported diagnosis for a single observer rather than for a consensus of observers or mean value. Only Guitera 2012 reported observer qualifications (dermatologists). Three studies presented data for expert observers (Guitera 2012; Pellacani 2014b (doc); Rao 2013) and one for novice observers (Curchin 2011). Studies undertook diagnosis in person with real‐time interpretation of RCM images (Curchin 2011; Pellacani 2014b (doc)), or remotely based on RCM images alongside the dermoscopic image of the same lesion (Guitera 2012; Rao 2013). Rao 2013 also presented data for in‐person diagnosis by a less experienced observer but this was not included in the primary analysis for detection of BCC.
One study developed a new algorithm for detection of melanoma and BCC (data for the BCC element are reported here) (Guitera 2012), and the other three reported data for the correct diagnosis of each type of malignancy (Curchin 2011; Pellacani 2014b (doc); Rao 2013). Estimates of sensitivities ranged from 52% to 100% and specificities from 45% to 100% (Figure 8). The high sensitivity of 100% and low specificity of 45% in Pellacani 2014b (doc) appeared as outliers, all other studies having sensitivities at or below 67% and specificities above 95% (Figure 9). Pellacani 2014b (doc) was the only study to restrict inclusion to pigmented lesions, and all lesions had "consistent clinical and or dermoscopic criteria for melanoma diagnosis;" it also included no cSCCs in the disease negative group.
Summary sensitivity and specificity for the detection of BCC were 76% (95% CI 45% to 92%) and 95% (95% CI 66% to 99%) (Table 2). Two studies incorrectly identified other skin cancers as BCCs (8/114 false‐positive diagnoses), including two melanomas and two cSCCs in Guitera 2012 and four cSCCs in Rao 2013. The other study which included cSCCs reported correct diagnosis of all six cSCCs or cSCC precursors (Curchin 2011).
Equivocal lesion studies
We defined equivocal lesion studies as those in which RCM was used in participants with equivocal lesions in whom a clear management decision could not be made following visual inspection or dermoscopy (i.e. RCM was being evaluated as a potential addition to dermoscopy).
Three studies provided data for the detection of BCC with RCM (Farnetani 2015; Pellacani 2014a (cons); Witkowski 2016), one providing data for nine different observers (Farnetani 2015), and one comparing the diagnosis of the same lesions with RCM and using dermoscopic images (Witkowski 2016). A total of 668 lesions were included with 148 cases of BCC; the total number of participants could not be reported due to lack of reporting in two studies.
All studies were case series, two of which reinterpreted previously acquired RCM images (Farnetani 2015; Witkowski 2016), and were undertaken in secondary or specialist clinic settings. Two studies included lesions suspected of being melanoma. Farnetani 2015 included any clinically equivocal lesion excised due to clinical or dermoscopic suspicion of melanoma, and Pellacani 2014a (cons) included pigmented lesions from participants requesting a mole check or with suspicion of melanoma for which an outcome decision could not be reached based on clinical or dermoscopic criteria. One study included clinically equivocal 'pink' cutaneous lesions with no pigmentation or containing less than 10% pigment and the absence of pigment network (Witkowski 2016). Sample sizes ranged from 100 to 308 lesions. The prevalence of BCC was 6% (Pellacani 2014a (cons)), 15% (Farnetani 2015), and 44% (Witkowski 2016), and prevalence of any malignancy was 8% for BCC, 35% for cSCC, and 53% for melanoma (only Witkowski 2016 included any cSCC). Two studies also reported data for the diagnosis of melanoma (Farnetani 2015; Pellacani 2014a (cons); see also Dinnes 2018a). Studies included a varied spectrum of benign lesions, Farnetani 2015 and Pellacani 2014a (cons) including predominantly benign melanocytic naevi and Witkowski 2016 included a relatively larger proportion of benign keratotic lesions and dermatofibromas (Appendix 8). Two studies made the reference standard diagnosis by histology alone (Farnetani 2015; Witkowski 2016); Pellacani 2014a (cons) reported histological diagnosis for the 81 lesions initially recommended for excision, with sequential digital follow‐up in the remaining 74% (227/308) of lesions; 28 of these (all found to be benign) were later excised due to changes identified on follow‐up.
All studies used the Vivascope 1500 imaging system and reported diagnosis for single observers, with Farnetani 2015 also reporting the mean across nine observers and for the majority diagnosis (five of nine evaluators in agreement). Observers were dermatologists (Farnetani 2015), assumed to be dermatologists (Witkowski 2016), or RCM described as conducted in a 'confocal unit' (Pellacani 2014a (cons)). Diagnosis was undertaken in person with real‐time interpretation of RCM (Pellacani 2014a (cons)) or remotely based on RCM images either alongside the dermoscopic image of the same lesion (Farnetani 2015), or blinded to all other clinical information (Witkowski 2016).
All three studies reported data for observer diagnosis of BCC. Estimates of sensitivities ranged from 85% to 100% and specificities from 76% to 94% (Figure 8). The high specificity of 94% (95% CI 89% to 97%) in Witkowski 2016 appeared as an outlier (non‐overlapping CIs), the other two studies having specificities of 76% (95% CI 66% to 85%) (Farnetani 2015) and 79% (95% CI 73% to 83%) (Pellacani 2014a (cons)). Of note, Witkowski 2016 had a markedly different participant population to the other two studies, including only non‐pigmented lesions with a markedly different spectrum of lesion types (see above).
Summary sensitivity and specificity for the detection of BCC were 94% (95% CI 79% to 98%) and 85% (95% CI 72% to 92%) (Table 2). Two studies incorrectly identified other skin cancers as BCCs (15/91 false‐positive diagnoses) including 14 melanomas in Farnetani 2015 and one cSCC in Witkowski 2016.
Witkowski 2016 also presented data for the diagnosis of non‐pigmented lesions based on the dermoscopic image alone (different observers interpreting the RCM and dermoscopic images). Sensitivity and specificity estimates were almost identical, with test sensitivity of 85% (95% CI 77% to 91%) for both tests and specificity of 94% (95% CI 89% to 97%) for RCM compared to 92% (95% CI 87% to 96%) for dermoscopy (Table 2; Figure 10).
Analyses by algorithms used to assist reflectance confocal microscopy
The 11 included cohorts of lesions provided 12 datasets evaluating the accuracy of different approaches to diagnosis with RCM for the detection of BCC. Appendix 7 provides a description of these approaches.
Only one eligible study used a formally developed algorithm for the detection of BCC in an 'any suspicious lesion' population. Guitera 2012 randomly allocated lesions to a training set for algorithm development and a test set for validation to develop a new two‐step algorithm for the detection of melanoma and BCC. Lesions were predominantly melanocytic or suspicious for BCC. Applying the features independently significant for BCC, sensitivity was 65% (95% CI 51% to 78%) and specificity was 95% (95% CI 92% to 97%). These results were largely similar to those of the other studies in 'any suspicious lesion' (Figure 8), all of which reported observers' correct diagnosis of BCC. All data for 'equivocal lesion' populations was also based on observers' correct diagnosis of BCC without the use of any formal algorithm.
Two studies reported accuracy for features found to be independently significant for BCC but did not use a separate training set to ascertain the relevant features (Castro 2015; Longo 2013). Two studies selected lesion characteristics thought to assist the correct diagnosis of BCC based on previously published literature (Appendix 7) (Incel 2015; Nori 2004). All four studies were classified as 'other lesion population' studies, and are covered in more detail below. All studies reported sensitivities and specificities at or above 90%, apart from specificities of 78% (95% CI 40% to 97%) reported in Castro 2015, which included only nine 'benign' lesions, and of 78% (95% CI 67% to 87%) in Nori 2004, which reported only that control group lesions had a 'range of common diagnoses' to BCC (Figure 8).
Analyses by observer experience
The 11 included studies provided 19 datasets evaluating the accuracy of observers with different levels of expertise; nine datasets coming from the same study (Farnetani 2015).
Figure 11 provides forest plots of all studies by observer experience, separately for in‐person and image‐based studies. Table 3 presents meta‐analytical estimates for each group. Data for two of the nine observers (one for high experience and one for low experience) were randomly sampled from Farnetani 2015. One further study provided a comparison of a less experienced (in‐person diagnosis) observer compared to a more experienced (but image‐based diagnosis) observer; however, the two observers did not examine the same lesions (overlap of 284/334 lesions) (Rao 2013). We did not formally make any comparisons between subgroups due to the small number of studies available.
Seven cohorts presented data for observers judged to be expert or experienced in RCM: three were based on in‐person evaluations (Pellacani 2014a (cons); Pellacani 2014b (doc)), or assumed to be in person (Castro 2015); four were from image‐based evaluations, two where observers were provided with the dermoscopic image of the same lesion (Farnetani 2015; Rao 2013), and two where observers were blinded to all clinical information (Guitera 2012; Longo 2013). The pooled sensitivity for the seven datasets was 98% (95% CI 74% to 100%) and pooled specificity was 87% (95% CI 71% to 95%) (Table 3). Sensitivities were at or above 90% in all studies apart from Guitera 2012 (65%, 95% CI 51% to 78%) and Rao 2013 (52%, 95% CI 32% to 71%). Specificities were more variable (45% to 98%), likely due to variations in the spectrum of disease (Figure 11).
Four cohorts presented for observers judged to be less experienced or novice: two were based on in‐person evaluations (Curchin 2011; Rao 2013), and two were image based, one providing observers with the dermoscopic image of the same lesion (Farnetani 2015), and one blinding observers to all clinical information (Nori 2004). The pooled sensitivity for the four datasets was 85% (95% CI 69% to 93%) and specificity was 91% (95% CI 81% to 96%) (Table 3).
Two studies did not report the experience of RCM observers (Incel 2015; Witkowski 2016) (Table 3).
Investigations of heterogeneity
We were unable to undertake investigations of heterogeneity for other characteristics listed in the protocol due to lack of data.
2. Target condition: cutaneous squamous cell carcinoma
Two studies reported data for RCM for the target condition of cSCC: one conducted in participants with any lesion suspicious for melanoma (Rao 2013), and one in comparison to dermoscopy participants with equivocal lesions (Witkowski 2016). Appendix 8 provides summary characteristics of studies. Table 4 presents study results and Figure 12 presents forest plots of study data. Two further studies present data for cSCC in 'other' lesion populations (see 'Other lesion populations' section below).
3. Comparison of reflectance confocal microscopy with dermoscopy for the detection of squamous cell carcinoma.
| Test | Studies | Lesions (cases) | Sensitivity (95% CI) | Specificity (95% CI) |
| All lesion studies (all studies) | ||||
| RCM | 1 | 323 (42) | 0.74 (0.58 to 0.86) | 0.92 (0.88 to 0.95) |
| Dermoscopy | 0 | — | — | — |
| All lesion studies (direct comparisons) | ||||
| RCM | 0 | — | — | — |
| Dermoscopy | 0 | — | — | — |
| Equivocal lesion studies (all studies) | ||||
| RCM | 1 | 260 (13) | 0.77 (0.46 to 0.95) | 0.98 (0.96 to 1.00) |
| Dermoscopy | 1 | 260 (13) | 0.77 (0.46 to 0.95) | 0.99 (0.96 to 1.00) |
| Equivocal lesion studies (direct comparisons) | ||||
| RCM | 1 | 260 (13) | 0.77 (0.46 to 0.95) | 0.98 (0.96 to 1.00) |
| Dermoscopy | 1 | 260 (13) | 0.77 (0.46 to 0.95) | 0.99 (0.96 to 1.00) |
CI: confidence interval; RCM: reflectance confocal microscopy.
12.

Forest plot of tests: reflectance confocal microscopy for the detection of cSCC in any suspicious lesion (top), equivocal lesions (centre), and other lesion (lower) populations. CI: confidence interval; FN: false negative; FP: false positive; TN: true negative; TP: true positive.
Rao 2013 included lesions scheduled for excision for cosmetic or medical reasons and presented results for the correct diagnosis of cSCC for two observers with varying levels of experience based on in‐person diagnosis and interpretation of RCM images alongside dermoscopic images. For the experienced observer assessing RCM images (42/323 assessed were cSCC), sensitivity for the detection of cSCC was 74% (95% CI 58% to 86%) and specificity was 92% (95% CI 88% to 95%). For the less experienced observer, in‐person RCM interpretation (39/318 assessed were cSCC) had a lower sensitivity of 41% (95% CI 26% to 58%) and higher specificity of 97% (95% CI 95% to 99%).
Witkowski 2016 included 260 clinically equivocal 'pink' cutaneous lesions and presented results for the correct diagnosis of cSCC (13 lesions) for one observer based on RCM image interpretation and for another observer based on the dermoscopic image alone; there was no other clinical information. Sensitivity was the same for both tests 77% (95% CI 46% to 95%), and specificities were almost identical at 98% for RCM (95% CI 96% to 100%) and 99% for dermoscopy (95% CI 96% to 100%).
3. Target condition: any skin cancer
Four studies reported data for RCM for the target condition of any skin cancer: two were conducted in participants with any lesion suspicious for melanoma (Curchin 2011; Rao 2013), and two in participants with equivocal lesions (Farnetani 2015; Witkowski 2016). Appendix 8 presents summary characteristics of studies. Table 5 present study results and Figure 13 presents forest plots of study data.
4. Comparison of reflectance confocal microscopy with dermoscopy for the detection of any skin cancer.
| KER | Studies | Lesions (cases) | Sensitivity (95% CI) | Specificity (95% CI) |
| Any suspicious lesion studies (all studies) | ||||
| RCM | 2 | 373 (100) | 0.85 (0.77 to 0.91) | 0.86 (0.82 to 0.98) |
| Dermoscopy | 0 | — | — | — |
| Any suspicious lesion studies (direct comparisons) | ||||
| RCM | 0 | — | — | — |
| Dermoscopy | 0 | — | — | — |
| Equivocal lesion studies (all studies) | ||||
| RCM | 2 | 360 (175) | 0.89 (0.82 to 0.94) | 0.85 (0.75 to 0.92) |
| Dermoscopy | 1 | 260 (140) | 0.91 (0.86 to 0.95) | 0.79 (0.71 to 0.86) |
| Equivocal lesion studies (direct comparisons) | ||||
| RCM | 1 | 260 (140) | 0.91 (0.85 to 0.95) | 0.80 (0.72 to 0.87) |
| Dermoscopy | 1 | 260 (140) | 0.91 (0.86 to 0.95) | 0.79 (0.71 to 0.86) |
CI: confidence interval; KER: any keratinocyte skin cancer; RCM: reflectance confocal microscopy.
13.
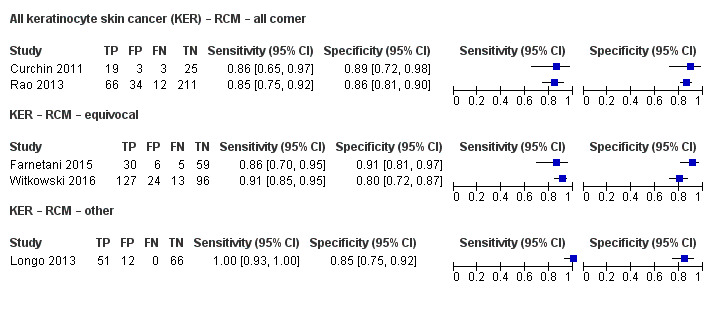
Forest plot of tests: reflectance confocal microscopy for the detection of any skin cancer (KER) in any suspicious lesion (top), equivocal lesions (centre), other lesion (lower) populations. CI: confidence interval; FN: false negative; FP: false positive; TN: true negative; TP: true positive
Both studies in the any suspicious lesion group included lesions scheduled for excision, with diagnosis undertaken in person by a novice RCM reader (Curchin 2011), or remotely by an RCM expert based on RCM images (Rao 2013). Both studies reported data for the observer's correct diagnosis of each malignancy, and Rao 2013 reported data for the correct diagnosis of each type of malignancy and for the decision to excise a lesion. Rao 2013 also reported data for in‐person evaluation with RCM by a less experienced observer (data not included due to a prior stated preference for more experienced observer data). A total of 373 lesions were included with 100 skin cancers (22 melanoma, 36 BCC, and 42 cSCCs), pooled sensitivity was 85% (95% CI 0.77% to 0.91%) and specificity was 86% (95% CI 82% to 98%).
One of the two studies in equivocal lesions was conducted in participants with lesions excised due to suspicion for melanoma (Farnetani 2015), and one in non‐pigmented or 'pink' lesions (Witkowski 2016). A total of 360 lesions were included with 175 malignant cases (32 melanomas, 129 BCCs (114 of which were from the Witkowski 2016 dataset), 13 cSCCs, and one syringoid eccrine carcinoma). Despite differences in the spectrum of included lesions, results from the two studies were similar (Figure 13), and pooled sensitivity was 89% (95% CI 0.82% to 0.94%) and specificity was 85% (95% CI 75% to 92%).
One study from each of these two groups provided data both for correct diagnosis of each malignancy and for the decision to excise suspicious lesions (Rao 2013; Witkowski 2016). Figure 14 and Figure 15 demonstrate the trade‐off between higher sensitivity and lower specificity from the lower excision threshold.
14.

ROC plot of tests: reflectance confocal microscopy for the detection of any skin cancer (KER) for correct diagnosis of each malignancy and decision to excise a lesion (image‐based evaluations).
15.

ROC plot of tests: reflectance confocal microscopy for the detection of any skin cancer (KER) for correct diagnosis of each malignancy and decision to excise a lesion (in‐person evaluations).
4. Other lesion populations
Four evaluations of RCM in other study populations were identified. Appendix 8 provides summary characteristics of studies, with forest plots in Figure 8 and ROC plots in Figure 9.
Two studies included lesions with a high index of suspicion for BCC (Castro 2015; Nori 2004). Castro 2015 included excised lesions suspicious for BCC based on clinical and dermoscopic examination and that were amenable to RCM examination using a hand‐held RCM probe (Vivascope 3000) to allow comparison with the standard approach (Vivascope 1500); 83% (45/54) of included lesions were histological confirmed to be BCC. The presence of RCM lesion characteristics selected from previous studies was assessed; however, it was not clear whether this was an image‐based or in‐person evaluation. Sensitivity was 100% (95% CI 92% to 100%) using the Vivascope 1500 system compared to 93% (95% CI 82% to 99%) using the Vivascope 3000, and specificity estimates were both 78% (95% CI 40% to 97%). There were no melanomas or cSCCs in this study.
Nori 2004 included 83 biopsy confirmed BCCs and a convenience sample of non‐BCC with 'range of common diagnoses;' the prevalence of BCC was 55% (83/152). Diagnosis based on images acquired using the Vivascope 1000 and based on the presence of morphological RCM characteristics previously investigated by the same group was compared to visual inspection of clinical images (latter reported for only 105/152 lesions). Sensitivity and specificity were both higher using RCM (based on the presence of three or more RCM criteria) compared to visual inspection: sensitivity was 94% (95% CI 86% to 98%) with RCM versus 48% (95% CI 35% to 62%) with visual inspection and specificity was 78% (95% CI 67% to 87%) with RCM compared to 62% (95% CI 46% to 75%) with visual inspection. Results for the four included cSCCs could not be disaggregated from the benign diagnoses; there were no melanomas.
Incel 2015 examined 122 non‐pigmented suspected malignant lesions or proliferative skin lesions with a vascular structure on dermoscopic examination with the hand‐held Vivascope 3000 system, using selected characteristics considered to be indicative of BCC and characteristics considered to be indicative of cSCC. The prevalence of BCC was 46% (56/122); of cSCC was 7% (9/122); with keratoacanthoma, seborrhoeic, actinic keratosis, or Bowen's disease making up half of the benign group (29/57). Sensitivity for the detection of BCC was 91% (95% CI 80% to 97%) and specificity was 100% (95% CI 95% to 100%). All nine SCCs were test negative (i.e. not mistaken for BCCs). Sensitivity for the detection of cSCC was 82% (95% CI 48% to 98%) and specificity was 96% (95% CI 91% to 99%). Similarly, this study mistook no BCCs for SCCs.
Longo 2013 included 140 clinically nodular lesions that underwent excision including 23 nodular melanomas (16%), 28 BCCs (20%), six cSCC (5%), and nine with cutaneous melanoma metastases (7.5%). An experienced dermatologist interpreted RCM images blinded to dermoscopy using RCM pattern analysis. Excluding non‐evaluable results (including one BCC and one SCC), sensitivities were 100% for detection of BCC and SCC, and specificities were 97% (95% CI 92% to 99%) for BCC and 100% (95% CI 97% to 100%) for SCC. For the detection of any malignant lesion (excluding melanoma metastases), sensitivity was 100% (95% CI 93% to 100%) and specificity was 85% (95% CI 75% to 92%).
Discussion
Summary of main results
RCM has been evaluated in a range of study populations and using a number of different approaches to assist diagnosis. Most of the data related to the detection of BCC, with few studies recruiting sufficient numbers of participants with cSCC (i.e. five or more) to allow accuracy to be reliably estimated. Both sensitivity and specificity for the detection of BCC appeared to vary with the spectrum of included lesions. Sensitivity was relatively low in participants with any suspicious lesion but was higher in studies of more selected populations. Studies were generally at high or unclear risk of bias across almost all domains and of high or unclear concern regarding applicability of the evidence, limiting the strength of conclusions that could be drawn. The Table 1 presents key results for the primary target conditions of BCC and cSCC.
For the detection of BCC in participants with any suspicious lesion, RCM summary sensitivity was 76% and specificity was 95%. Applying these estimates to a hypothetical cohort of 1000 lesions at the median prevalence of BCC of 12.5%, the Table 1 showed that RCM would miss 30/125 BCCs with 44 false‐positive diagnoses. On the evidence observed, only one of these false‐positive results might be a melanoma with up to two misdiagnosed cSCCs. The wide CIs for both estimates mean that the number of BCCs missed could range from 10 to 69, and number of false positives from nine to 298. A single cohort of lesions with a high clinical or dermoscopic suspicion of being melanomas was responsible for most of the variation in results (Pellacani 2014b (doc)). The other studies in this group had sensitivities between 52% and 67% and specificities above 95%, which would correspond with numbers of BCCs missed at the higher end of the 10 to 69 per 1000 range, and false positives at the lower end of the nine to 298 per 1000 range (with a corresponding reduction in the potential for melanomas being misclassified as BCCs).
RCM sensitivity was higher (94%) for the detection of BCC in participants with equivocal lesions, but with a lower specificity of 85%. Applying these estimates to a hypothetical cohort of 1000 lesions at the median prevalence of BCC of 15%, the Table 1 showed that RCM would miss 9/150 BCCs with 128 false‐positive diagnoses. On the evidence observed for equivocal lesions, there is a much greater potential for misdiagnosis of melanomas as BCCs, with up to 19 of these false‐positive results potentially being melanomas. The CIs around these estimates were not as wide as for any suspicious lesion: the number of BCCs missed at this disease prevalence could range between three and 32, and number of false positives from 68 to 238. The lowest sensitivity (85%) and highest specificity (94%) in this group were produced from the cohort of non‐pigmented lesions (Witkowski 2016), as opposed to the other two studies recruiting lesions equivocal for melanoma diagnosis.
There were insufficient data available to compare RCM with visual inspection or dermoscopy or to consider the effect of using formally developed algorithms to assist RCM diagnosis of BCC. However, there was some evidence of higher sensitivity from more experienced observers.
Data for the detection of cSCC were limited but suggested sensitivity in the range of 74% to 77% with high specificity of 92% to 98%.
Strengths and weaknesses of the review
The strengths of this review included an in‐depth and comprehensive electronic literature search, systematic review methods including double extraction of papers by both clinicians and methodologists, and contact with authors to allow study inclusion or clarify data. A clear analysis structure according to patient pathway was adopted to allow test accuracy in different study populations to be estimated, and a detailed and replicable analysis of methodological quality was undertaken.
The main concerns for the review were a result of the small number of studies, variation in the spectrum of included lesions, and poor reporting of primary studies, hindering the assessment of study quality and limiting the conclusions that could be drawn from the data. Despite some evidence of high sensitivity or specificity, or both, depending on the study population, research in the field has been dominated by a single expert group and results obtained from a more typical range of specialists in different countries, healthcare systems, and settings are needed. Our analysis by observer experience across algorithms and study populations lends support to the consensus that experience and observer familiarity with the diagnostic question is a key element of any diagnostic process that requires interpretation by the human eye (Norman 2009). Only one eligible study evaluated a formally developed algorithm to assist RCM interpretation; however, we excluded four studies from our review that examined individual RCM characteristics only or did not use separate training and test sets of data (Amjadi 2011; Eichert 2010; Peppelman 2015; Rishpon 2009). Further work in this area may be warranted.
Given these limitations, our results should be considered as exploratory rather than conclusive. Our results are in contrast to those of other recently published systematic reviews (Xiong 2016; Edwards 2016), one of which was conducted as part of a technology assessment report for NICE (Edwards 2016). However, our review extends the time period searched for eligible studies from 2014 in Edwards 2016 and from 2015 in Xiong 2016, considers the impact of different study populations and target conditions, and uses currently recommended methods for DTA systematic reviews (Deeks 2013). Xiong 2016 did not consider varying definitions of the target condition in their primary analysis but pooled all studies regardless of detection of melanoma, BCC, or SCC. In a secondary analysis, three studies were pooled for the detection of BCC, producing estimates of sensitivity of 91.7% (95% CI 86.5% to 95.4%) and specificity of 91.3% (95% CI 93.6% to 96.2%); two of the three studies with high percentages of BCC lesions were included in our 'other population' analysis (Castro 2015; Nori 2004); and one was excluded from this review due to the presentation of individual RCM features for detection of BCC rather than for an overall diagnosis (Peppelman 2013). The Edwards 2016 review did not conduct a meta‐analysis, instead selecting studies considered to be more applicable to a UK setting. Using the Castro 2015 study, which was included in our review as an 'other lesion population' study, economic modelling showed RCM to be a dominant strategy when used in populations with a high clinical suspicion of being BCCs in comparison to diagnostic biopsy, whether used in lesions positive or equivocal for BCC on dermoscopy. The potential for misdiagnosis of any melanomas or cSCCs as BCCs does not appear to have been considered.
Applicability of findings to the review question
There were insufficient data available to compare the accuracy of RCM with visual inspection or dermoscopy as planned. Similarly there was a lack of data to assess the use different algorithms to aid diagnosis. It is not clear how applicable the data included in this review were regarding the routine use of RCM in a usual clinic setting as opposed to a highly specialist centre with expert RCM observers. Data were lacking regarding specific uses of the test, for example, to confirm a clinical diagnosis of BCC before initiation of non‐surgical treatment. Most of the studies used the current version of the only commercially available RCM system, the Vivascope 1500. The use of remote image‐based diagnosis largely by RCM experts may restrict the transferability of results to a clinical setting.
Authors' conclusions
Implications for practice.
It is unclear whether reflectance confocal microscopy (RCM) has a role in clinical practice for the diagnosis of basal cell carcinoma (BCC), although some studies suggest it has the potential to improve diagnoses. There are as yet insufficient data to support its use as a tool for avoidance of diagnostic biopsies in lesions with high clinical suspicion of BCC. In populations with a wider spectrum of lesions, there is potential for both missed BCCs and for misclassification of benign lesions, or other malignant skin cancers such as melanoma, as BCCs. Evidence for the detection squamous cell carcinoma (cSCC) is even more scarce; however, there is a clear suggestion that cSCCs could be missed with RCM. Importantly, data are lacking that compare RCM to usual practice (whether with or without dermoscopy), such that the diagnostic impact of RCM cannot be clearly estimated.
Implications for research.
Further prospective evaluation of RCM in populations with a high clinical suspicion of BCC is warranted. Research should be conducted in a standard healthcare setting with a clearly defined and representative population of participants with dermoscopically equivocal lesions. RCM results should be interpreted in a usual care setting by healthcare staff representative of those who would be likely to interpret images in practice, in order to confirm the suggested increase in accuracy over dermoscopy. A multicentre approach would allow confirmation that results can be replicated across centres and that the technology can be implemented across a health service. Prospective recruitment of consecutive series of participants, with test interpretation blinded to the reference standard diagnosis and with prespecified and clearly defined diagnostic thresholds for determining test positivity is easily achieved. Systematic follow‐up of non‐excised lesions avoids over‐reliance on a histological reference standard and allows results to be more generalisable to routine clinical practice. A standardised approach to diagnosis, and clear identification of the level of training and experience required to achieve good results is also required. Any future research study needs to be clear about the diagnostic pathway followed by study participants prior to study enrolment, and should conform to the updated Standards for Reporting of Diagnostic Accuracy (STARD) guideline (Bossuyt 2015).
What's new
| Date | Event | Description |
|---|---|---|
| 19 December 2018 | Amended | Affiliations, Disclaimer and Sources of support updated |
Acknowledgements
Members of the Cochrane Skin Cancer Diagnostic Test Accuracy Group include:
the full project team (Susan Bayliss, Naomi Chuchu, Clare Davenport, Jonathan Deeks, Jac Dinnes, Kathie Godfrey, Rubeta Matin, Colette O'Sullivan, Yemisi Takwoingi, Hywel Williams);
our 12 clinical reviewers (Rachel Abbott, Ben Aldridge, Oliver Bassett, Sue Ann Chan, Alana Durack, Monica Fawzy, Abha Gulati, Jacqui Moreau, Lopa Patel, Daniel Saleh, David Thompson, Kai Yuen Wong) and two methodologists (Lavinia Ferrante di Ruffano and Louise Johnston) who assisted with full text screening, data extraction, and quality assessment across the entire suite of reviews of diagnosis and staging and skin cancer;
our expert advisor and co‐author for this review, Rakesh Patalay, and on the protocol for keratinocyte skin cancer, Fiona Bath‐Hextall; and
all members of our Advisory Group (Jonathan Bowling, Seau Tak Cheung, Colin Fleming, Matthew Gardiner, Abhilash Jain, Susan O'Connell, Pat Lawton, John Lear, Mariska Leeflang, Richard Motley, Paul Nathan, Julia Newton‐Bishop, Miranda Payne, Rachael Robinson, Simon Rodwell, Julia Schofield, Neil Shroff, Hamid Tehrani, Zoe Traill, Fiona Walter, Angela Webster).
Cochrane Skin would like to thank Robert Dellavalle, who was the Dermatology Editor for this review; and a clinical referee who wishes to remain anonymous. We also wish to thank the Cochrane DTA editorial base and colleagues, as well as Anne Lawson, who copy‐edited this review.
Appendices
Appendix 1. Current content and structure of the Programme Grant
| LIST OF REVIEWS | Number of studies | |
| Diagnosis of melanoma | ||
| 1 | Visual inspection | 49 |
| 2 | Dermoscopy +/‐ visual inspection | 104 |
| 3 | Teledermatology | 22 |
| 4 | Smartphone applications | 2 |
| 5a | Computer‐assisted diagnosis – dermoscopy‐based techniques | 42 |
| 5b | Computer‐asssisted diagnosis – spectroscopy‐based techniques | Review amalgamated into 5a |
| 6 | Reflectance confocal microscopy | 18 |
| 7 | High‐frequency ultrasound | 5 |
| Diagnosis of keratinocyte skin cancer (BCC and cSCC) | ||
| 8 | Visual inspection +/‐ Dermoscopy | 24 |
| 5c | Computer‐asssisted diagnosis – dermoscopy‐based techniques | Review amalgamated into 5a |
| 5d | Computer‐asssisted diagnosis – spectroscopy‐based techniques | Review amalgamated into 5a |
| 9 | Optical coherence tomography | 5 |
| 10 | Reflectance confocal microscopy | 10 |
| 11 | Exfoliative cytology | 9 |
| Staging of melanoma | ||
| 12 | Imaging tests (ultrasound, CT, MRI, PET‐CT) | 38 |
| 13 | Sentinel lymph node biopsy | 160 |
| Staging of cSCC | ||
| Imaging tests review | Review dropped; only one study identified | |
| 13 | Sentinel lymph node biopsy | Review amalgamated into 13 above (n = 15 studies) |
Appendix 2. Table of acronyms used in review text
| Acronym | Definition |
| BCC | Basal cell carcinoma |
| BPC | Between‐person comparative (study) |
| CAD | Computer‐assisted diagnosis |
| cSCC | Cutaneous squamous cell carcinoma |
| DEJ | Dermoepidermal junction |
| DTA | Diagnostic test accuracy |
| ENT | Ear, nose, and throat |
| FP | False positive |
| GP | General practitioner |
| KER | Any keratinocyte skin cancer |
| LM | Lentigo maligna |
| MEL | Invasive melanoma or melanoma in situ |
| MM | Malignant melanoma |
| NHS | National Health Service |
| NICE | National Institute for Health and Care Excellence |
| NIHR | National Institute for Health Research |
| NML | Non‐melanocytic lesion |
| OCT | Optical coherence tomography |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta‐Analyses |
| QUADAS | Quality Assessment of Diagnostic Accuracy Studies |
| RCM | Reflectance confocal microscopy |
| RCT | Randomised controlled trial |
| RDEB | Recessive dystrophic epidermolysis bullosa |
| ROC | Receiver operating characteristic |
| SCC | Squamous cell carcinoma |
| TN | True negative |
Appendix 3. Proposed sources of heterogeneity
1. Population characteristics
general versus higher risk populations
participant population: primary/secondary/specialist unit
lesion suspicion: general suspicion/atypical/equivocal/not reported
lesion type: any pigmented; melanocytic
inclusion of multiple lesions per participant
ethnicity
2. Index test characteristics
type of test or algorithm used for test interpretation within each 'group' of tests
the nature of and definition of criteria for test positivity
diagnosis in‐person versus image‐based diagnosis
observer experience with the index test
approaches to lesion preparation (e.g. the use of oil or antiseptic gel for dermoscopy)
3. Reference standard characteristics
reference standard used
whether histology reporting meets pathology reporting guidelines
use of excisional versus diagnostic biopsy
whether two independent dermatopathologists reviewed histological diagnosis
4. Study quality
consecutive or random sample of participants recruited
index test interpreted blinded to the reference standard result
index test interpreted blinded to the result of any other index test
presence of partial or differential verification bias (whereby only a sample of those subject to the index test were verified by the reference test or by the same reference test with selection dependent on the index test result)
use of an adequate reference standard
overall risk of bias
Appendix 4. Final search strategies
Melanoma search strategies to August 2016
Database: Ovid MEDLINE(R) 1946 to August week 3 2016
Search strategy:
1 exp melanoma/
2 exp skin cancer/
3 exp basal cell carcinoma/
4 basalioma$1.ti,ab.
5 ((basal cell or skin) adj2 (cancer$1 or carcinoma$1 or mass or masses or tumour$1 or tumor$1 or neoplasm$1 or adenoma$1 or epithelioma$1 or lesion$1 or malignan$ or nodule$1)).ti,ab.
6 (pigmented adj2 (lesion$1 or mole$ or nevus or nevi or naevus or naevi or skin)).ti,ab.
7 (melanom$1 or nonmelanoma$1 or non‐melanoma$1 or melanocyt$ or non‐melanocyt$ or nonmelanocyt$ or keratinocyt$).ti,ab.
8 nmsc.ti,ab.
9 (squamous cell adj2 (cancer$1 or carcinoma$1 or mass or masses or tumor$1 or tumour$1 or neoplasm$1 or adenoma$1 or epithelioma$1 or epithelial or lesion$1 or malignan$ or nodule$1) adj2 (skin or epiderm$ or cutaneous)).ti,ab.
10 (BCC or CSCC or NMSC).ti,ab.
11 keratinocy$.ti,ab.
12 Keratinocytes/
13 or/1‐12
14 dermoscop$.ti,ab.
15 dermatoscop$.ti,ab.
16 photomicrograph$.ti,ab.
17 exp epiluminescence microscopy/
18 (epiluminescence adj2 microscop$).ti,ab.
19 (confocal adj2 microscop$).ti,ab.
20 (incident light adj2 microscop$).ti,ab.
21 (surface adj2 microscop$).ti,ab.
22 (visual adj (inspect$ or examin$)).ti,ab.
23 ((clinical or physical) adj examin$).ti,ab.
24 3 point.ti,ab.
25 three point.ti,ab.
26 pattern analys$.ti,ab.
27 ABCD$.ti,ab.
28 menzies.ti,ab.
29 7 point.ti,ab.
30 seven point.ti,ab.
31 (digital adj2 (dermoscop$ or dermatoscop$)).ti,ab.
32 artificial intelligence.ti,ab.
33 AI.ti,ab.
34 computer assisted.ti,ab.
35 computer aided.ti,ab.
36 neural network$.ti,ab.
37 exp diagnosis, computer‐assisted/
38 MoleMax.ti,ab.
39 image process$.ti,ab.
40 automatic classif$.ti,ab.
41 image analysis.ti,ab.
42 SIAscop$.ti,ab.
43 Aura.ti,ab.
44 (optical adj2 scan$).ti,ab.
45 MelaFind.ti,ab.
46 SIMSYS.ti,ab.
47 MoleMate.ti,ab.
48 SolarScan.ti,ab.
49 VivaScope.ti,ab.
50 (high adj3 ultraso$).ti,ab.
51 (canine adj2 detect$).ti,ab.
52 ((mobile or cell or cellular or smart) adj ((phone$1 adj2 app$1) or application$1)).ti,ab.
53 smartphone$.ti,ab.
54 (DermoScan or SkinVision or DermLink or SpotCheck).ti,ab.
55 Mole Detective.ti,ab.
56 Spot Check.ti,ab.
57 (mole$1 adj2 map$).ti,ab.
58 (total adj2 body).ti,ab.
59 exfoliative cytolog$.ti,ab.
60 digital analys$.ti,ab.
61 (image$1 adj3 software).ti,ab.
62 (teledermatolog$ or tele‐dermatolog$ or telederm or tele‐derm or teledermoscop$ or tele‐dermoscop$ or teledermatoscop$ or tele‐dermatoscop$).ti,ab.
63 (optical coherence adj (technolog$ or tomog$)).ti,ab.
64 (computer adj2 diagnos$).ti,ab.
65 exp sentinel lymph node biopsy/
66 (sentinel adj2 node).ti,ab.
67 nevisense.mp. or HFUS.ti,ab.
68 electrical impedance spectroscopy.ti,ab.
69 history taking.ti,ab.
70 patient history.ti,ab.
71 (naked eye adj (exam$ or assess$)).ti,ab.
72 (skin adj exam$).ti,ab.
73 physical examination/
74 ugly duckling.mp. or UD.ti,ab.
75 ((physician$ or clinical or physical) adj (exam$ or triage or recog$)).ti,ab.
76 ABCDE.mp. or VOC.ti,ab.
77 clinical accuracy.ti,ab.
78 Family Practice/ or Physicians, Family/ or clinical competence/
79 (confocal adj2 microscop$).ti,ab.
80 diagnostic algorithm$1.ti,ab.
81 checklist$.ti,ab.
82 virtual imag$1.ti,ab.
83 volatile organic compound$1.ti,ab.
84 dog$1.ti,ab.
85 gene expression analy$.ti,ab.
86 reflex transmission imag$.ti,ab.
87 thermal imaging.ti,ab.
88 elastography.ti,ab.
89 or/14‐88
90 (CT or PET).ti,ab.
91 PET‐CT.ti,ab.
92 (FDG or F18 or Fluorodeoxyglucose or radiopharmaceutical$).ti,ab.
93 exp Deoxyglucose/
94 deoxy‐glucose.ti,ab.
95 deoxyglucose.ti,ab.
96 CATSCAN.ti,ab.
97 exp Tomography, Emission‐Computed/
98 exp Tomography, X‐ray computed/
99 positron emission tomograph$.ti,ab.
100 exp magnetic resonance imaging/
101 (MRI or fMRI or NMRI or scintigraph$).ti,ab.
102 exp echography/
103 Doppler echography.ti,ab.
104 sonograph$.ti,ab.
105 ultraso$.ti,ab.
106 doppler.ti,ab.
107 magnetic resonance imag$.ti,ab.
108 or/90‐107
109 (stage$ or staging or metasta$ or recurrence or sensitivity or specificity or false negative$ or thickness$).ti,ab.
110 "Sensitivity and Specificity"/
111 exp cancer staging/
112 or/109‐111
113 108 and 112
114 89 or 113
115 13 and 114
Database: Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations 29 August 2016
Search strategy:
1 basalioma$1.ti,ab.
2 ((basal cell or skin) adj2 (cancer$1 or carcinoma$1 or mass or masses or tumour$1 or tumor$1 or neoplasm$1 or adenoma$1 or epithelioma$1 or lesion$1 or malignan$ or nodule$1)).ti,ab.
3 (pigmented adj2 (lesion$1 or mole$ or nevus or nevi or naevus or naevi or skin)).ti,ab.
4 (melanom$1 or nonmelanoma$1 or non‐melanoma$1 or melanocyt$ or non‐melanocyt$ or nonmelanocyt$ or keratinocyt$).ti,ab.
5 nmsc.ti,ab.
6 (squamous cell adj2 (cancer$1 or carcinoma$1 or mass or masses or tumor$1 or tumour$1 or neoplasm$1 or adenoma$1 or epithelioma$1 or epithelial or lesion$1 or malignan$ or nodule$1) adj2 (skin or epiderm$ or cutaneous)).ti,ab.
7 (BCC or CSCC or NMSC).ti,ab.
8 keratinocy$.ti,ab.
9 or/1‐8
10 dermoscop$.ti,ab.
11 dermatoscop$.ti,ab.
12 photomicrograph$.ti,ab.
13 (epiluminescence adj2 microscop$).ti,ab.
14 (confocal adj2 microscop$).ti,ab.
15 (incident light adj2 microscop$).ti,ab.
16 (surface adj2 microscop$).ti,ab.
17 (visual adj (inspect$ or examin$)).ti,ab.
18 ((clinical or physical) adj examin$).ti,ab.
19 3 point.ti,ab.
20 three point.ti,ab.
21 pattern analys$.ti,ab.
22 ABCD$.ti,ab.
23 menzies.ti,ab.
24 7 point.ti,ab.
25 seven point.ti,ab.
26 (digital adj2 (dermoscop$ or dermatoscop$)).ti,ab.
27 artificial intelligence.ti,ab.
28 AI.ti,ab.
29 computer assisted.ti,ab.
30 computer aided.ti,ab.
31 neural network$.ti,ab.
32 MoleMax.ti,ab.
33 image process$.ti,ab.
34 automatic classif$.ti,ab.
35 image analysis.ti,ab.
36 SIAscop$.ti,ab.
37 Aura.ti,ab.
38 (optical adj2 scan$).ti,ab.
39 MelaFind.ti,ab.
40 SIMSYS.ti,ab.
41 MoleMate.ti,ab.
42 SolarScan.ti,ab.
43 VivaScope.ti,ab.
44 (high adj3 ultraso$).ti,ab.
45 (canine adj2 detect$).ti,ab.
46 ((mobile or cell or cellular or smart) adj ((phone$1 adj2 app$1) or application$1)).ti,ab.
47 smartphone$.ti,ab.
48 (DermoScan or SkinVision or DermLink or SpotCheck).ti,ab.
49 Mole Detective.ti,ab.
50 Spot Check.ti,ab.
51 (mole$1 adj2 map$).ti,ab.
52 (total adj2 body).ti,ab.
53 exfoliative cytolog$.ti,ab.
54 digital analys$.ti,ab.
55 (image$1 adj3 software).ti,ab.
56 (teledermatolog$ or tele‐dermatolog$ or telederm or tele‐derm or teledermoscop$ or tele‐dermoscop$ or teledermatoscop$ or tele‐dermatoscop$).ti,ab.
57 (optical coherence adj (technolog$ or tomog$)).ti,ab.
58 (computer adj2 diagnos$).ti,ab.
59 (sentinel adj2 node).ti,ab.
60 nevisense.mp. or HFUS.ti,ab.
61 electrical impedance spectroscopy.ti,ab.
62 history taking.ti,ab.
63 patient history.ti,ab.
64 (naked eye adj (exam$ or assess$)).ti,ab.
65 (skin adj exam$).ti,ab.
66 ugly duckling.mp. or UD.ti,ab.
67 ((physician$ or clinical or physical) adj (exam$ or triage or recog$)).ti,ab.
68 ABCDE.mp. or VOC.ti,ab.
69 clinical accuracy.ti,ab.
70 (Family adj (Practice or Physicians)).ti,ab.
71 (confocal adj2 microscop$).ti,ab.
72 clinical competence.ti,ab.
73 diagnostic algorithm$1.ti,ab.
74 checklist$.ti,ab.
75 virtual imag$1.ti,ab.
76 volatile organic compound$1.ti,ab.
77 dog$1.ti,ab.
78 gene expression analy$.ti,ab.
79 reflex transmission imag$.ti,ab.
80 thermal imaging.ti,ab.
81 elastography.ti,ab.
82 or/10‐81
83 (CT or PET).ti,ab.
84 PET‐CT.ti,ab.
85 (FDG or F18 or Fluorodeoxyglucose or radiopharmaceutical$).ti,ab.
86 deoxy‐glucose.ti,ab.
87 deoxyglucose.ti,ab.
88 CATSCAN.ti,ab.
89 positron emission tomograph$.ti,ab.
90 (MRI or fMRI or NMRI or scintigraph$).ti,ab.
91 Doppler echography.ti,ab.
92 sonograph$.ti,ab.
93 ultraso$.ti,ab.
94 doppler.ti,ab.
95 magnetic resonance imag$.ti,ab.
96 or/83‐95
97 (stage$ or staging or metasta$ or recurrence or sensitivity or specificity or false negative$ or thickness$).ti,ab.
98 96 and 97
99 82 or 98
100 9 and 99
Database: Embase 1974 to 29 August 2016
Search strategy:
1 *melanoma/
2 *skin cancer/
3 *basal cell carcinoma/
4 basalioma$.ti,ab.
5 ((basal cell or skin) adj2 (cancer$1 or carcinoma$1 or mass or masses or tumour$1 or tumor$1 or neoplasm$ or adenoma$ or epithelioma$ or lesion$ or malignan$ or nodule$)).ti,ab.
6 (pigmented adj2 (lesion$1 or mole$ or nevus or nevi or naevus or naevi or skin)).ti,ab.
7 (melanom$1 or nonmelanoma$1 or non‐melanoma$1 or melanocyt$ or non‐melanocyt$ or nonmelanocyt$ or keratinocyt$).ti,ab.
8 nmsc.ti,ab.
9 (squamous cell adj2 (cancer$1 or carcinoma$1 or mass or tumor$1 or tumour$1 or neoplasm$1 or adenoma$1 or epithelioma$1 or epithelial or lesion$1 or malignan$ or nodule$1) adj2 (skin or epiderm$ or cutaneous)).ti,ab.
10 (BCC or cscc).mp. or NMSC.ti,ab.
11 keratinocyte.ti,ab.
12 keratinocy$.ti,ab.
13 or/1‐12
14 dermoscop$.ti,ab.
15 dermatoscop$.ti,ab.
16 photomicrograph$.ti,ab.
17 *epiluminescence microscopy/
18 (epiluminescence adj2 microscop$).ti,ab.
19 (confocal adj2 microscop$).ti,ab.
20 (incident light adj2 microscop$).ti,ab.
21 (surface adj2 microscop$).ti,ab.
22 (visual adj (inspect$ or examin$)).ti,ab.
23 ((clinical or physical) adj examin$).ti,ab.
24 3 point.ti,ab.
25 three point.ti,ab.
26 pattern analys$.ti,ab.
27 ABCD$.ti,ab.
28 menzies.ti,ab.
29 7 point.ti,ab.
30 seven point.ti,ab.
31 (digital adj2 (dermoscop$ or dermatoscop$)).ti,ab.
32 artificial intelligence.ti,ab.
33 AI.ti,ab.
34 computer assisted.ti,ab.
35 computer aided.ti,ab.
36 neural network$.ti,ab.
37 MoleMax.ti,ab.
38 exp diagnosis, computer‐assisted/
39 image process$.ti,ab.
40 automatic classif$.ti,ab.
41 image analysis.ti,ab.
42 SIAscop$.ti,ab.
43 (optical adj2 scan$).ti,ab.
44 Aura.ti,ab.
45 MelaFind.ti,ab.
46 SIMSYS.ti,ab.
47 MoleMate.ti,ab.
48 SolarScan.ti,ab.
49 VivaScope.ti,ab.
50 confocal microscop$.ti,ab.
51 (high adj3 ultraso$).ti,ab.
52 (canine adj2 detect$).ti,ab.
53 ((mobile or cell$ or cellular or smart) adj ((phone$1 adj2 app$1) or application$1)).ti,ab.
54 smartphone$.ti,ab.
55 (DermoScan or SkinVision or DermLink or SpotCheck).ti,ab.
56 Spot Check.ti,ab.
57 Mole Detective.ti,ab.
58 (mole$1 adj2 map$).ti,ab.
59 (total adj2 body).ti,ab.
60 exfoliative cytolog$.ti,ab.
61 digital analys$.ti,ab.
62 (image$1 adj3 software).ti,ab.
63 (optical coherence adj (technolog$ or tomog$)).ti,ab.
64 (teledermatolog$ or tele‐dermatolog$ or telederm or tele‐derm or teledermoscop$ or tele‐dermoscop$ or teledermatoscop$).mp. or tele‐dermatoscop$.ti,ab.
65 (computer adj2 diagnos$).ti,ab.
66 *sentinel lymph node biopsy/
67 (sentinel adj2 node).ti,ab.
68 nevisense.ti,ab.
69 HFUS.ti,ab.
70 electrical impedance spectroscopy.ti,ab.
71 history taking.ti,ab.
72 patient history.ti,ab.
73 (naked eye adj (exam$ or assess$)).ti,ab.
74 (skin adj exam$).ti,ab.
75 *physical examination/
76 ugly duckling.ti,ab.
77 UD sign$.ti,ab.
78 ((physician$ or clinical or physical) adj (exam$ or recog$ or triage)).ti,ab.
79 ABCDE.ti,ab.
80 clinical accuracy.ti,ab.
81 *general practice/
82 (confocal adj2 microscop$).ti,ab.
83 clinical competence/
84 diagnostic algorithm$.ti,ab.
85 checklist$1.ti,ab.
86 virtual image$1.ti,ab.
87 volatile organic compound$1.ti,ab.
88 VOC.ti,ab.
89 dog$1.ti,ab.
90 gene expression analys$.ti,ab.
91 reflex transmission imaging.ti,ab.
92 thermal imaging.ti,ab.
93 elastography.ti,ab.
94 dog$1.ti,ab.
95 gene expression analys$.ti,ab.
96 reflex transmission imaging.ti,ab.
97 thermal imaging.ti,ab.
98 elastography.ti,ab.
99 or/14‐93
100 PET‐CT.ti,ab.
101 (CT or PET).ti,ab.
102 (FDG or F18 or Fluorodeoxyglucose or radiopharmaceutical$).ti,ab.
103 exp Deoxyglucose/
104 CATSCAN.ti,ab.
105 deoxyglucose.ti,ab.
106 deoxy‐glucose.ti,ab.
107 *positron emission tomography/
108 *computer assisted tomography/
109 positron emission tomograph$.ti,ab.
110 *nuclear magnetic resonance imaging/
111 (MRI or fMRI or NMRI or scintigraph$).ti,ab.
112 *echography/
113 Doppler.ti,ab.
114 sonograph$.ti,ab.
115 ultraso$.ti,ab.
116 magnetic resonance imag$.ti,ab.
117 or/100‐116
118 (stage$ or staging or metasta$ or recurrence or sensitivity or specificity or false negative$ or thickness$).ti,ab.
119 "Sensitivity and Specificity"/
120 *cancer staging/
121 or/118‐120
122 117 and 121
123 99 or 122
124 13 and 123
Database: Cochrane Library (Wiley) 2016 searched 30 August 2016 CDSR Issue 8 of 12 2016 CENTRAL Issue 7 of 12 2016 HTA Issue 3 of 4 July 2016 DARE Issue 3 of 4 2015
Search strategy:
#1 melanoma* or nonmelanoma* or non‐melanoma* or melanocyt* or non‐melanocyt* or nonmelanocyt* or keratinocyte*
#2 MeSH descriptor: [Melanoma] explode all trees
#3 "skin cancer*"
#4 MeSH descriptor: [Skin Neoplasms] explode all trees
#5 skin near/2 (cancer* or carcinoma* or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*)
#6 nmsc
#7 "squamous cell" near/2 (cancer* or carcinoma* or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*) near/2 (skin or epiderm* or cutaneous)
#8 "basal cell" near/2 (cancer* or carcinoma* or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*)
#9 pigmented near/2 (lesion* or nevus or mole* or naevi or naevus or nevi or skin)
#10 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9
#11 dermoscop*
#12 dermatoscop*
#13 Photomicrograph*
#14 MeSH descriptor: [Dermoscopy] explode all trees
#15 confocal near/2 microscop*
#16 epiluminescence near/2 microscop*
#17 incident next light near/2 microscop*
#18 surface near/2 microscop*
#19 "visual inspect*"
#20 "visual exam*"
#21 (clinical or physical) next (exam*)
#22 "3 point"
#23 "three point"
#24 "pattern analys*"
#25 ABDC
#26 menzies
#27 "7 point"
#28 "seven point"
#29 digital near/2 (dermoscop* or dermatoscop*)
#30 "artificial intelligence"
#31 "AI"
#32 "computer assisted"
#33 "computer aided"
#34 AI
#35 "neural network*"
#36 MoleMax
#37 "computer diagnosis"
#38 "image process*"
#39 "automatic classif*"
#40 SIAscope
#41 "image analysis"
#42 "optical near/2 scan*"
#43 Aura
#44 MelaFind
#45 SIMSYS
#46 MoleMate
#47 SolarScan
#48 Vivascope
#49 "confocal microscopy"
#50 high near/3 ultraso*
#51 canine near/2 detect*
#52 Mole* near/2 map*
#53 total near/2 body
#54 mobile* or smart near/2 phone*
#55 cell next phone*
#56 smartphone*
#57 "mitotic index"
#58 DermoScan or SkinVision or DermLink or SpotCheck
#59 "Mole Detective"
#60 "Spot Check"
#61 mole* near/2 map*
#62 total near/2 body
#63 "exfoliative cytolog*"
#64 "digital analys*"
#65 image near/3 software
#66 teledermatolog* or tele‐dermatolog* or telederm or tele‐derm or teledermoscop* or tele‐dermoscop* or teledermatoscop* or tele‐dermatolog*
#67 "optical coherence" next (technolog* or tomog*)
#68 computer near/2 diagnos*
#69 sentinel near/2 node*
#70 #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 or #66 or #67 or #68 or #69
#71 ultraso*
#72 sonograph*
#73 MeSH descriptor: [Ultrasonography] explode all trees
#74 Doppler
#75 CT or PET or PET‐CT
#76 "CAT SCAN" or "CATSCAN"
#77 MeSH descriptor: [Positron‐Emission Tomography] explode all trees
#78 MeSH descriptor: [Tomography, X‐Ray Computed] explode all trees
#79 MRI
#80 MeSH descriptor: [Magnetic Resonance Imaging] explode all trees
#81 MRI or fMRI or NMRI or scintigraph*
#82 "magnetic resonance imag*"
#83 MeSH descriptor: [Deoxyglucose] explode all trees
#84 deoxyglucose or deoxy‐glucose
#85 "positron emission tomograph*"
#86 #71 or #72 or #73 or #74 or #75 or #76 or #77 or #78 or #79 or #80 or #81 or #82 or #83 or #84 or #85
#87 stage* or staging or metasta* or recurrence or sensitivity or specificity or "false negative*" or thickness*
#88 MeSH descriptor: [Neoplasm Staging] explode all trees
#89 #87 or #88
#90 #89 and #86
#91 #70 or #90
#92 #10 and #91
#93 BCC or CSCC or NMCS
#94 keratinocy*
#95 #93 or #94
#96 #10 or #95
#97 nevisense
#98 HFUS
#99 "electrical impedance spectroscopy"
#100 "history taking"
#101 "patient history"
#102 naked next eye near/1 (exam* or assess*)
#103 skin next exam*
#104 "ugly duckling" or (UD sign*)
#105 MeSH descriptor: [Physical Examination] explode all trees
#106 (physician* or clinical or physical) near/1 (exam* or recog* or triage*)
#107 ABCDE
#108 "clinical accuracy"
#109 MeSH descriptor: [General Practice] explode all trees
#110 confocal near microscop*
#111 "diagnostic algorithm*"
#112 MeSH descriptor: [Clinical Competence] explode all trees
#113 checklist*
#114 "virtual image*"
#115 "volatile organic compound*"
#116 dog or dogs
#117 VOC
#118 "gene expression analys*"
#119 "reflex transmission imaging"
#120 "thermal imaging"
#121 elastography
#122 #97 or #98 or #99 or #100 or #101 or #102 or #103 or #104 or #105 or #106 or #107 or #108 or #109 or #110 or #111 or #112 or #113 or #114 or #115 or #116 or #117 or #118 or #119 or #120 or #121
#123 #70 or #122
#124 #96 and #123
#125 #96 and #90
#126 #125 or #124
#127 #10 and #126
Database: CINAHL Plus (EBSCO) 1937 to 30 August 2016
Search strategy:
S1 (MH "Melanoma") OR (MH "Nevi and Melanomas+")
S2 (MH "Skin Neoplasms+")
S3 (MH "Carcinoma, Basal Cell+")
S4 basalioma*
S5 (basal cell) N2 (cancer* or carcinoma* or mass or masses or tumor* or tumour* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*)
S6 (pigmented) N2 (lesion* or mole* or nevus or nevi or naevus or naevi or skin)
S7 melanom* or nonmelanoma* or non‐melanoma* or melanocyt* or non‐melanocyt* or nonmelanocyt*
S8 nmsc
S9 TX BCC or cscc or NMSC
S10 (MH "Keratinocytes")
S11 keratinocyt*
S12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11
S13 dermoscop* or dermatoscop* or photomicrograph* or (3 point) or (three point) or ABCD* or menzies or (7 point) or (seven point) or AI or Molemax or SIASCOP* or Aura or MelaFind or SIMSYS or MoleMate or SolarScan or smartphone* or DermoScan or SkinVision or DermLink or SpotCheck
S14 (epiluminescence or confocal or incident or surface) N2 (microscop*)
S15 visual N1 (inspect* or examin*)
S16 (clinical or physical) N1 (examin*)
S17 pattern analys*
S18 (digital) N2 (dermoscop* or dermatoscop*)
S19 (artificial intelligence)
S20 (computer) N2 (assisted or aided)
S21 (neural network*)
S22 (MH "Diagnosis, Computer Assisted+")
S23 (image process*)
S24 (automatic classif*)
S25 (image analysis)
S26 SIAScop*
S27 (optical) N2 (scan*)
S28 (high) N3 (ultraso*)
S29 elastography
S30 (mobile or cell or cellular or smart) N2 (phone*) N2 (app or application*)
S31 (mole*) N2 (map*)
S32 total N2 body
S33 exfoliative cytolog*
S34 digital analys*
S35 image N3 software
S36 teledermatolog* or tele‐dermatolog* or telederm or tele‐derm or teledermoscop* or tele‐dermoscop* or teledermatoscop* or tele‐dermatoscop* teledermatolog* or tele‐dermatolog* or telederm or tele‐derm or teledermoscop*
S37 (optical coherence) N1 (technolog* or tomog*)
S38 computer N2 diagnos*
S39 sentinel N2 node
S40 (MH "Sentinel Lymph Node Biopsy")
S41 nevisense or HFUS or checklist* or VOC or dog*
S42 electrical impedance spectroscopy
S43 history taking
S44 "Patient history"
S45 naked eye
S46 skin exam*
S47 physical exam*
S48 ugly duckling
S49 UD sign*
S50 (physician* or clinical or physical) N1 (exam*)
S51 clinical accuracy
S52 general practice
S53 (physician* or clinical or physical) N1 (recog* or triage)
S54 confocal microscop*
S55 clinical competence
S56 diagnostic algorithm*
S57 checklist*
S58 virtual image*
S59 volatile organic compound*
S60 gene expression analys*
S61 reflex transmission imag*
S62 thermal imaging
S63 S13 or S14 or S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62
S64 CT or PET
S65 PET‐CT
S66 FDG or F18 or Fluorodeoxyglucose or radiopharmaceutical*
S67 (MH "Deoxyglucose+")
S68 deoxy‐glucose or deoxyglucose
S69 CATSCAN
S70 CAT‐SCAN
S71 (MH "Deoxyglucose+")
S72 (MH "Tomography, Emission‐Computed+")
S73 (MH "Tomography, X‐Ray Computed")
S74 positron emission tomograph*
S75 (MH "Magnetic Resonance Imaging+")
S76 MRI or fMRI or NMRI or scintigraph*
S77 echography
S78 doppler
S79 sonograph*
S80 ultraso*
S81 magnetic resonance imag*
S82 S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81
S83 stage* or staging or metasta* or recurrence or sensitivity or specificity or (false negative*) or thickness
S84 (MH "Neoplasm Staging")
S85 S83 OR S84
S86 S82 AND S85
S87 S63 OR S86
S88 S12 AND S87
Database: Science Citation Index SCI Expanded (Web of Science) 1900 to 30 August 2016
Conference Proceedings Citation Index (Web of Science) 1900 to 1 September 2016
Search strategy:
#1 (melanom* or nonmelanom* or non‐melanoma* or melanocyt* or non‐melanocyt* or nonmelanocyt* or keratinocyt*)
#2 (basalioma*)
#3 ((skin) near/2 (cancer* or carcinoma or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*))
#4 ((basal) near/2 (cancer* or carcinoma* or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*))
#5 ((pigmented) near/2 (lesion* or mole* or nevus or nevi or naevus or naevi or skin))
#6 (nmsc or BCC or NMSC or keratinocy*)
#7 ((squamous cell (cancer* or carcinoma* or mass or masses or tumour* or tumor* or neoplasm* or adenoma* or epithelioma* or lesion* or malignan* or nodule*))
#8 (skin or epiderm* or cutaneous)
#9 #8 AND #7
#10 #9 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
#11 ((dermoscop* or dermatoscop* or photomicrograph* or epiluminescence or confocal or "incident light" or "surface microscop*" or "visual inspect*" or "physical exam*" or 3 point or three point or pattern analy* or ABCDE or menzies or 7 point or seven point or dermoscop* or dermatoscop* or AI or artificial or computer aided or computer assisted or neural network* or Molemax or image process* or automatic classif* or image analysis or siascope or optical scan* or Aura or melafind or simsys or molemate or solarscan or vivascope or confocal microscop* or high ultraso* or canine detect* or cellphone* or mobile* or phone* or smartphone or dermoscan or skinvision or dermlink or spotcheck or spot check or mole detective or mole map* or total body or exfoliative psychology or digital or image software or optical coherence or teledermatology or telederm* or teledermoscop* or teledermatoscop* or computer diagnos* or sentinel))
#12 ((nevisense or HFUS or impedance spectroscopy or history taking or patient history or naked eye or skin exam* or physical exam* or ugly duckling or UD sign* or physician* exam* or physical exam* or ABCDE or clinical accuracy or general practice or confocal microscop* or clinical competence or diagnostic algorithm* or checklist* or virtual image* or volatile organic or VOC or dog* or gene expression or reflex transmission or thermal imag* or elastography))
#13 #11 or #12
#14 ((PET or CT or FDG or deoxyglucose or deoxy‐glucose or fluorodeoxy* or radiopharma* or CATSCAN or positron emission or computer assisted or nuclear magnetic or MRI or FMRI or NMRI or scintigraph* or echograph* or Doppler or sonograph* or ultraso* or magnetic reson*))
#15 ((stage* or staging or metast* or recurrence or sensitivity or specificity or false negative* or thickness*))
#16 #14 AND #15
#17 #16 OR #13
#18 #10 AND #17
Refined by: DOCUMENT TYPES: ( MEETING ABSTRACT OR PROCEEDINGS PAPER )
Appendix 5. Full text inclusion criteria
| Criterion | Inclusion | Exclusion |
| Study design |
For diagnostic and staging reviews
|
|
| Target condition |
|
|
| Population |
For diagnostic reviews
For staging reviews
|
|
| Index tests |
For diagnosis
For staging
Any test combination and in any order Any test positivity threshold Any variation in testing procedure (e.g. radioisotope used) |
|
| Reference standard |
For diagnostic studies
For studies of imaging tests for staging
For studies of SLNB accuracy for staging
|
For diagnostic studies
|
| BCC: basal cell carcinoma; cSCC: cutaneous squamous cell carcinoma; CT: computed tomography; FNAC: fine needle aspiration cytology; LND: lymph node dissection; MRI: magnetic resonance imaging; PET: positron emission tomography; PET‐CT: positron emission tomography computed tomography; RCT: randomised controlled trial; SCC: squamous cell carcinoma; SLN+: positive sentinel lymph node; SLn: negative sentinel lymph node; SLNB: sentinel lymph node biopsy. | ||
Appendix 6. Quality assessment (based on QUADAS‐2)
The QUADAS‐2 checklist (Whiting 2011) was tailored to the review topic as follows below.
Participant selection domain (1)
Selective recruitment of study participants can be a key influence on test accuracy. In general terms, all participants eligible to undergo a test should be included in a study, allowing for the intended use of that test within the context of the study. We considered studies that separately sampled malignant and benign lesions to have used a case‐control design; and those that supplemented a series of suspicious lesions with additional malignant or benign lesions to be at unclear risk of bias
In terms of exclusions, we considered studies that excluded particular lesion types, particular lesion sites, or that excluded lesions on the basis of image quality or lack of observer agreement (e.g. on histopathology) to be at high risk of bias.
In judging the applicability of participant populations to the review question, we considered restriction to particular lesion populations, such as melanocytic, nodular, high risk, or restrictions by size to be of high concern for applicability.
Given that diagnosis of skin cancer is primarily lesion‐based, there is the potential for study participants with multiple lesions to contribute disproportionately to estimates of test accuracy, especially if they are at particular risk of having skin cancer. We considered studies that include a high number of lesions in relation to the number of study to be less representative than studies conducted in a more general population participants (i.e. if the difference between the number of included lesions and number of included participants is greater than 5%).
Index test domain (2)
Given the potential for subjective differences in test interpretation, the interpretation of the index test blinded to the result of the reference standard is a key means of reducing bias. For prospective studies and retrospective studies that used the original index test interpretation, the diagnosis will by nature be interpreted and recorded before the result of the reference standard is known; however, studies using previously acquired images could be particularly susceptible to information bias. For these studies to be at low risk of bias, we required a clear indication that observers were unaware of the reference standard diagnosis at time of test interpretation. An item was also added to assess the presence of blinding between interpretations of different algorithms, however this item was not included in the overall assessment of risk of bias.
Prespecification of the index test threshold was considered present if the study clearly reported that the threshold used was not data driven (i.e. was not based on study results). Studies that did not clearly describe the threshold used but that required clinicians to record a diagnosis or management decision for a lesion were considered to be unclear on this criterion. Studies reporting accuracy for multiple numeric thresholds, where receiver operating characteristic (ROC) analysis was used to select the threshold, or that reported accuracy for the presence of independently significant lesion characteristics with no separate test set of lesions were considered at high risk of bias.
In terms of applicability of the index test to the review question, we required the test to be applied and interpreted as it would be in a clinical practice setting (i.e. in person or face‐to‐face with the participant), and by a single observer as opposed to a consensus decision or mean across multiple observers. Image‐based studies were considered to be high concern, although RCM image interpretations where the observer was also supplied with a clinical or dermoscopic image of the lesion along with some participant characteristics were considered 'unclear.'
Despite the often subjective nature of test interpretation, it is also important for study authors to outline the particular lesion characteristics that were considered to be indicative for skin cancer, particularly where established algorithms or checklists were not used. Studies were considered of low concern if the threshold used was established in a prior study or sufficient threshold details were presented to allow replication.
The experience of the examiner will also impact on the applicability of study results. We required studies to describe the test interpreter as 'experienced' or 'expert' in RCM to have low concern about applicability.
Reference standard domain (3)
In an ideal study, consecutively recruited participants should all undergo incisional or excisional biopsy of the skin lesion regardless of level of clinical suspicion. In reality, both partial and differential verification bias are likely. Partial verification bias may occur where histology is the only reference standard used, and only those participants with a certain degree of suspicion of malignancy based on the result of the index test undergo verification, the others either being excluded from the study or defined as being disease negative without further assessment or follow‐up, as discussed above.
Differential verification bias will be present where other reference standards are used in addition to histological verification of suspicious lesions. A typical example of verification bias in skin cancer occurs when investigators do not biopsy people with benign‐appearing lesions but instead follow them up for a period of time to determine whether any malignancy subsequently develops (these would be false negatives on the index test). We defined an 'adequate' reference standard as: all disease positive participants having a histological reference standard either at the time of application of the index test or after a period of clinical follow‐up; and at least 80% of disease negative participants have received a histological diagnosis, with up to 20% undergoing at least three months' follow‐up of benign‐appearing lesions.
A further challenge is the potential for incorporation bias (i.e. where the result of the index test is used to help determine the reference standard diagnosis). It is normal practice for the clinical diagnosis (usually by visual inspection or dermoscopy) to be included on pathology request forms and for the histopathologist to use this diagnosis to help with the pathology interpretation. Although inclusion of such clinical information on the histopathology request form is theoretically a form of incorporation bias, blinded interpretation of the histopathology reference standard is not normal practice, and enforcement of such conditions would significantly limit the generalisability of the study results. For studies evaluating RCM, this item was divided into two questions, first whether the reference standard was blinded to the index test result (RCM), and second whether it was blinded to the clinical diagnosis. Only the response to the first part (i.e. blinding to RCM) was included in our overall assessment of risk of bias for the reference standard domain.
In judging the applicability of the reference standard to our review question, scored studies as high concern around applicability if they used expert diagnosis (with no follow‐up) as a reference standard in any participant, or did not report histology interpretation by a dermatopathologist.
Flow and timing domain (4)
In the ideal study, the diagnosis based on the index test and reference standard should be made consecutively or as near to each other in time as possible to avoid changes in lesion over time. For lesions with a histological reference standard, we have defined a one‐month period as an appropriate interval between application of the index test and the reference standard. For studies using clinical follow‐up, a minimum three‐month follow‐up period has been defined as at low risk of bias for detecting false negatives.
In assessing whether all participants were included in the analysis, we considered studies at high risk of bias if participants were excluded following recruitment.
Comparative domain
A comparative domain was added to the QUADAS‐2 checklist for studies comparing the accuracy of RCM and dermoscopy. Items were included to assess the presence of blinding of interpretation between tests, and to specify a maximum of one month interval between application of index tests, as intervals greater than these may be accompanied by changes in tumour characteristics. As it would not be normal practice for RCM to be interpreted blinded to the clinical or dermoscopic diagnosis, the scoring of this item did not contribute to our overall assessment of risk of bias. We also considered whether both tests were applied and interpreted in a clinically applicable manner.
The following tables use text that was originally published in the QUADAS‐2 tool by Whiting and colleagues (Whiting 2011).
| Item | Response (delete as required) |
| Participant selection (1) risk of bias | |
| 1) Was a consecutive or random sample of participants or images enrolled? |
Yes – if paper states consecutive or random No – if paper describes other method of sampling Unclear – if participant sampling not described |
| 2) Was a case‐control design avoided? |
Yes – if consecutive or random or case‐control design clearly not used No – if study described as case‐control or describes sampling specific numbers of participants with particular diagnoses Unclear – if not described |
3) Did the study avoid inappropriate exclusions, e.g.
|
Yes – if inappropriate exclusions were avoided No – if lesions were excluded that might affect test accuracy, e.g. 'difficult to diagnose' lesions, or where disagreement between evaluators was observed Unclear – if not clearly reported but there is suspicion that difficult to diagnose lesions may have been excluded |
4) For between‐person comparative studies only (i.e. allocating different tests to different study participants):
|
For A)
For B)
For C)
|
| Could the selection of participants have introduced bias? For non‐comparative and within‐person comparative studies
For between‐person comparative studies
|
For non‐comparative and within‐person comparative studies
For between‐person comparative studies
|
| Participant selection (1) concerns regarding applicability | |
1) Are the included participants and chosen study setting appropriate to answer the review question, i.e. are the study results generalisable?
|
A) For studies that will contribute to the analysis of participants with a primary presentation of a skin lesion (i.e. test naive) Yes – if participants included in the study appear to be generally representative of those who might present in a usual practice setting No – if study participants appear to be unrepresentative of usual practice, e.g. in terms of severity of disease, demographic features, presence of differential diagnosis or comorbidity, setting of the study, and previous testing protocols Unclear – if insufficient details are provided to determine the generalisability of study participants B) For studies that will contribute to the analysis of referred participants (i.e. who have already undergone some form of testing) Yes – if study participants appear to be representative of those who might be referred for further investigation. If the study focuses only on those with equivocal lesions, for example, we would suggest that this is not representative of the wider referred population No – if study participants appear to be unrepresentative of usual practice, e.g. if a particularly high proportion of participants have been self‐referred or referred for cosmetic reasons. Other factors to consider include severity of disease, demographic features, presence of differential diagnosis or comorbidity, setting of the study, and previous testing protocols Unclear – if insufficient details are provided to determine the generalisability of study participants |
| 2) Did the study avoid including participants with multiple lesions? |
Yes – if the difference between the number of included lesions and number of included participants is less than 5% No – if the difference between the number of included lesions and number of included participants is greater than 5% Unclear – if it is not possible to assess |
Is there concern that the included participants do not match the review question?
|
|
| Index test (2) risk of bias (to be completed per test evaluated) | |
| 1) Was the index test or testing strategy result interpreted without knowledge of the results of the reference standard? |
Yes – if index test described as interpreted without knowledge of reference standard result or, for prospective studies, if index test is always conducted and interpreted prior to the reference standard No – if index test described as interpreted in knowledge of reference standard result Unclear – if index test blinding is not described |
| 2) Was the diagnostic threshold at which the test was considered positive prespecified? |
Yes – if threshold was prespecified (i.e. prior to analysing study results) No – if threshold was not prespecified Unclear – if not possible to tell whether or not diagnostic threshold was prespecified |
| 3) For within‐person comparisons of index tests or testing strategies (i.e. > 1 index test applied per participant): was each index test result interpreted without knowledge of the results of other index tests or testing strategies? |
Yes – if all index tests were described as interpreted without knowledge of the results of the others No – if the index tests were described as interpreted in the knowledge of the results of the others Unclear – if it is not possible to tell whether knowledge of other index tests could have influenced test interpretation N/A – if only 1 index test was evaluated |
| Could the conduct or interpretation of the index test have introduced bias? For non‐comparative and between‐person comparison studies
For within‐person comparative studies
|
For non‐comparative and between‐person comparison studies
For within‐person comparative studies
|
| Index test (2) concern about applicability | |
| 1) Was the diagnostic threshold to determine presence or absence of disease established in a previously published study? E.g. previously evaluated/established
|
Yes – if a previously evaluated/established tool to aid diagnosis was used or if the diagnostic threshold used was established in a previously published study No – if an unfamiliar/new tool to aid diagnosis was used, if no particular algorithm was used, or if the objective threshold reported was chosen based on results in the current study Unclear – if insufficient information was reported |
| 2) Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? Study results can only be reproduced if the diagnostic threshold is described in sufficient detail. This item applies equally to studies using pattern recognition and those using checklists or algorithms to aid test interpretation |
Yes – If the criteria for diagnosis were reported in sufficient detail to allow replication No – if the criteria for diagnosis were not reported in sufficient detail to allow replication Unclear – If some but not sufficient information on criteria for diagnosis to allow replication were provided |
| 3) Was the test interpretation carried out by an experienced examiner? |
Yes – if the test was interpreted by 1 or more speciality‐accredited dermatologists, or by examiners of any clinical background with special interest in dermatology and with any formal training in the use of the test No – if the test was not interpreted by an experienced examiner (see above) Unclear – if the experience of the examiner(s) was not reported in sufficient detail to judge or if examiners were described as 'Expert' with no further detail given N/A – if system‐based diagnosis, i.e. no observer interpretation |
Is there concern that the index test, its conduct, or interpretation differ from the review question?
|
|
| Reference standard (3) risk of bias | |
| 1) Is the reference standard likely to correctly classify the target condition? A) Disease positive – 1 or more of the following:
B) Disease negative – 1 or more of the following:
|
A) Disease positive Yes – if all participants with a final diagnosis of malignancy underwent 1 of the listed reference standards No – If a final diagnosis of malignancy for any participant was reached without histopathology Unclear – if the method of final diagnosis was not reported for any participant with a final diagnosis of malignancy or if the length of clinical follow‐up used was not clear or if a clinical follow‐up reference standard was reported in combination with a participant‐based analysis and it was not possible to determine whether the detection of a malignant lesion during follow‐up is the same lesion that originally tested negative on the index test B) Disease negative Yes – If at least 80% of benign diagnoses were reached by histology and up to 20% were reached by clinical follow‐up for a minimum of 3 months following the index test No – if more than 20% of benign diagnoses were reached by clinical follow‐up for a minimum of 3 months following the index test or if clinical follow‐up period was less than 3 months Unclear – if the method of final diagnosis was not reported for any participant with benign or non‐melanoma diagnosis |
| 2) Were the reference standard results interpreted without knowledge of the results of the index test? Please score this item for all studies even though histopathology interpretation is usually conducted with knowledge of the clinical diagnosis (from visual inspection or dermoscopy or both). We will deal with this by not including the response to this item in the 'Risk of bias' assessment for these tests. For reviews of all other tests, this item will be retained |
Yes – if the reference standard diagnosis was reached blinded to the index test result No – if the reference standard diagnosis was reached with knowledge of the index test result Unclear – if blinded reference test interpretation was not clearly reported |
| Could the reference standard, its conduct, or its interpretation have introduced bias? For visual inspection/dermoscopy evaluations
For all other tests
|
For visual inspection/dermoscopy evaluations
For all other tests
|
| REFERENCE STANDARD (3) CONCERN ABOUT APPLICABILITY | |
| 1) Expert opinion (with no histological confirmation) was not used as a reference standard 'Expert opinion' means diagnosis based on the standard clinical examination, with no histology or lesion follow‐up ***do not complete this item for teledermatology studies |
Yes – if expert opinion was not used as a reference standard for any participant No – if expert opinion was used as a reference standard for any participant Unclear – if not clearly reported |
| 2) Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? |
Yes – if histology interpretation was reported to be carried out by an experienced histopathologist or dermatopathologist No – if histology interpretation was reported to be carried out by a less experienced histopathologist Unclear – if the experience/qualifications of the pathologist were not reported |
Is there concern that the target condition as defined by the reference standard does not match the review question?
***For teledermatology studies only
|
***For teledermatology studies only
|
| Flow and timing (4): risk of bias | |
| 1) Was there an appropriate interval between index test and reference standard? A) For histopathological reference standard, was the interval between index test and reference standard ≤ 1 month? B) If the reference standard includes clinical follow‐up of borderline/benign‐appearing lesions, was there at least 3 months' follow‐up following application of index test(s)? |
A) Yes – if study reports ≤ 1 month between index and reference standard No – if study reports > 1 month between index and reference standard Unclear – if study does not report interval between index and reference standard B) Yes – if study reports ≥ 3 months' follow‐up No – if study reports < 3 months' follow‐up Unclear – if study does not report the length of clinical follow‐up |
| 2) Did all participants receive the same reference standard? |
Yes – if all participants underwent the same reference standard No – if more than 1 reference standard was used Unclear – if not clearly reported |
| 3) Were all participants included in the analysis? |
Yes – if all participants were included in the analysis No – if some participants were excluded from the analysis Unclear– if not clearly reported |
| 4) For within‐person comparisons of index tests Was the interval between application of index tests ≤ 1 month? |
Yes – if study reports ≤ 1 month between index tests No – if study reports > 1 month between index tests Unclear – if study does not report the interval between index tests |
| Could the participant flow have introduced bias? For non‐comparative and between‐person comparison studies
For within‐person comparative studies
|
For non‐comparative and between‐person comparison studies
For within‐person comparative studies
|
| BCC: basal cell carcinoma; cSCC: cutaneous squamous cell carcinoma. | |
Appendix 7. Details of RCM algorithms and diagnostic thresholds for diagnosis
|
Castro 2015 BCC |
Guitera 2012 (2 step algorithm to identify BCC then MM) |
Longo 2013 BCC (and MM) |
Nori 2004 (based on Gonzalez 2002) BCC |
| Previously published RCM criteria assessed (cites Agero 2006; Nori 2004; Guitera 2012) Selected characteristics chosen; ≥ c3 RCM criteria present, including either presence of:
Additional criteria assessed:
|
Evaluated 47 RCM features (referenced to a number of prior studies) and conducted multivariate analysis on the training set of lesions to identify independently significant features for MM and for BCC; assume presence of any one indicated T+) Correct identification as MM or BCC (based on independently significant features as identification from training set) For BCC:
|
47 RCM features recorded; multivariate analysis id 4 positive independent significant features for BCC
|
Selected 5 criteria from a number of morphologic characteristics previously investigated by the same group, on the basis that they were 'easily and unambiguously detected by non‐dermatopathologists and a novice reviewer' Data presented for ≥ 2, ≥ 3, ≥ 4, 5 characteristics present
|
|
Incel 2015 BCC/SCC |
Results based on 'observer diagnosis' | ||
| Selected characteristics from to assist correct diagnosis of different lesion types (cites Malvehy 2012; Eichert 2010; Ahlgrimm‐Siess 2010; Röwert‐Huber 2007; Ahlgrimm‐Siess 2011) Characteristics listed for BCC included:
Characteristics listed for SCC included: refractile squam/crust in stratum corneum and nucleated cells with dark centre (parakeratotic)cells;
|
Curchin 2011: applied RCM score: ≥ 3 for suspected melanomas and LM score for suspected LM of the face (Guitera 2010); reported observer correct diagnosis of BCC; no further details presented Farnetani 2015: evaluators completed a 'pattern description' (presence/absence of a number of RCM features) and gave an overall diagnosis of malignant (melanoma or BCC) or benign. Discriminant analysis also used to identify features independently associated with malignancy (and with MM and BCC separately). 3 more frequently observed in BCC were:
Pellacani 2014: NR; Pellacani 2005 algorithm used for diagnosis of melanoma Rao 2013: observers gave diagnosis (MM/BCC/SCC) and excise decision (no further details) Witkowski 2016: report correct diagnosis (MM/BCC/SCC) and excise decision (no further details) |
||
| BCC: basal cell carcinoma; DEJ: dermoepidermal junction; LM: lentigo maligna; MM: malignant melanoma; RCM: reflectance confocal microscopy; SCC: squamous cell carcinoma; T+: test positive. | |||
Appendix 8. Summary study details by lesion population
| Study author Outcomes reported |
Study type Country Setting |
Inclusion criteria | n participants/lesions |
Index tests (algorithm) Diagnostic approach |
Observer qual (n); expe Additional data available |
Reference standard Final diagnoses |
Exclusions |
| Any suspicious lesion | |||||||
|
Curchin 2011 BCC KER (MEL) |
NC P‐CS Australia Secondary |
People scheduled for minor excision | 42/50 | Vivascope 1500; Observer dx (RCM score for suspected melanomas) In person (single observer) |
Observer qual NR; n = NR Described as novice to RCM analysis after completing a RCM analysis course in Modena, Italy. Dermoscopic and RCM images were aligned over the top of each other. |
Histology alone MM 12; MiS 1; BCC: 9; cSCC: 6 (included SK or AK, or both); 'benign' diagnoses: 23 |
Reported correct dx of all 6 SCC or precursors (not disaggregated) |
|
Guitera 2012 BCC (MEL) |
WPC NR‐CS Australia/ Italy Specialist clinic/secondary |
People with suspicious lesions, including those on face and neck suspicious for LM, and requiring histology to rule out an epithelial tumour or an MM; predominantly melanocytic or suspicious for BCC | 663/710 356 lesions randomised to 'test set' included here |
Vivascope 1500; No algorithm (independently significant features for BCC) Image‐based (single observer) |
Dermatologist (n = 2); described as expert observers RCM guided by dermoscopic findings but interpretation blinded to all but lesion location and participant age |
Histology alone MEL 105; BCC: 52; cSCC: 9; BN 132; SN 16; AK 8; 31 benign macule of the face and 3 DF |
BCC: 2 MM and 2 SCC were FP |
|
Pellacani 2014b (doc) BCC (MEL) |
NC P‐CS Italy Specialist clinic |
People requesting a mole check or with suspicion of melanoma who were referred to PLC clinic. Documentation group (doc) included lesions with consistent clinical or dermoscopic criteria, or both, for melanoma dx | 171/184 (1/184 did not undergo RCM) |
Vivascope 1500; observer dx (assumed RCM score for suspected melanomas) In person (single observer) |
Observer qual NR (n = 1); dx made at 'confocal unit' RCM reader was aware that lesions were dermoscopically atypical but blinded to 'RCM documentation' or 'RCM consultation' |
Histology alone (documentation group) MM 13; MiS 9; BCC: 19; 1 melanoma metastases; BN 121; SN 8; SK or other keratotic 7; other benign 5 |
— |
|
Rao 2013 BCC SCC KER (MEL) |
NC NR‐CS USA Secondary |
All lesions removed for cosmetic or medical reasons that were imaged using a confocal scanning microscope | NR/334 Reader 1 (novice) evaluated 318 lesions; reader 2 (expert) evaluated 323 lesions; 284 were examined by both readers |
Vivascope 1500; No algorithm (correct dx of each malignancy; overall observer dx of malignancy) Image‐based (single observer) |
Observer qual NR (n = 2); reader 1 had 1 year' RCM experience at the start of the study; reader 2 had > 9 years' experience with RCM. dx was based on the dermoscopic image and confocal microscopy evaluation. |
Histology alone MM 8; melanoma (in situ); 1; BCC: 27; cSCC: 42; BN 176; SK 22; AK 24; 23 other |
BCC: 4 SCC were FP; SCC: 9 BCCs picked up as SCCs were considered TN as per Methods |
| Equivocal lesion studies | |||||||
|
Farnetani 2015 BCC (MEL) |
NC R‐CS Italy Secondary |
Diagnostically equivocal lesions excised due to clinical or dermoscopic suspicion of melanoma, where a specific clinical and dermoscopic dx could not be rendered with certainty. | NR/100 | Vivascope 1500; no algorithm (observer dx – pattern description and diagnostic judgment) Image based (single observer) |
Dermatologist (n = 9); 6 experienced (≥ 3 years' RCM experience) and 3 'recent' RCM users. Experienced reader randomly selected for primary analysis. Dermoscopic image provided; no additional clinical information (e.g. age and melanoma or lesion history) |
Histology alone MEL 20; BCC: 15; SK 7; BN 55; AK 3 |
BCC: 14 MM FP |
|
Pellacani 2014a (cons) BCC (MEL) |
NC P‐CS Italy Specialist clinic |
People requesting a mole check or with suspicion of melanoma who were referred to PLC clinic. Consultation group (cons) included lesions requiring an outcome decision from RCM (dx could not be reached on clinical or dermoscopic criteria, or both) | 252/309 1/308 did not undergo RCM |
Vivascope 1500; observer dx (assumed RCM score for suspected melanomas) In person (single observer) |
Observer qual NR (n = 1); dx made at 'confocal unit' RCM reader was aware that lesions were dermoscopically atypical but blinded to 'RCM documentation' or 'RCM consultation' |
Histology plus FU (cons group); 227/308 referred for sequential digital FU; 28 later excised; MM 2; MiS 4; BCC: 19; BN 71; SN 5; benign NML 8; 199 benign on FU | — |
|
Witkowski 2016 BCC SCC MM |
WPC‐tests R‐CS Italy Secondary |
Clinically equivocal 'pink' cutaneous lesions with absent pigmentation or containing < 10% pigment and absence of pigment network | NR/260 | Vivascope 1500; no algorithm (correct dx of each malignancy) Dermoscopy Image‐based (single observer) |
Dermatologist (assumed; n = 2, 1 dermoscopy 1 RCM); experience NR No additional information provided |
Histology alone MEL 12; BCC: 114; cSCC: 13; 1 syringoid eccrine carcinoma; benign keratotic 25; BN 47; SN 6; DF 18; other benign 24 |
BCC: 1 SCC FP |
| Other lesion populations | |||||||
|
Castro 2015 BCC |
WPC NR‐CS Brazil and USA Specialist clinic |
People with ≥ 1 skin lesions deemed suspicious for BCC based on clinical and dermoscopic examination. | NR/54 | Vivascope 1500 vs Vivascope 3000 (no algorithm; ≥ 3 characteristics present) Unclear if image based; consensus of 2 |
Dermatologist (n = 1); experienced with RCM examination and supervised by skin cancer expert Clinical, dermoscopic and RCM imaging performed by same dermatologist |
Histology BCC: 45; 'benign' diagnoses: 9 |
38 of original 92 lesions excluded as only accessible to Vivascope 3000 (mostly facial). |
|
Incel 2015 BCC SCC |
NC P‐CS Turkey Secondary |
People with non‐pigmented suspected tumoural lesions or proliferative skin lesions and with a vascular structure on dermoscopic examination | 114/122 | Vivascope 3000 (no algorithm; selected characteristics; correct dx of BCC/SCC) Unclear if image‐based; unclear if single observer) |
Observer qual NR (n = NR); states "First 60 lesions subjected to blinded evaluation by 2 observers," no further details provided | Histology BCC: 56; cSCC: 9; KA 3; SK 11; AK 8; BD 7; and 22 other benign non‐pigmented tumours |
BCC: all SCCs considered test negative |
|
Longo 2013 BCC SCC KER (MEL) |
NC R‐CS Italy Specialist clinic/secondary |
Clinically nodular lesions (defined as cutaneous palpable/superficial seated lesions and not subcutaneous ones) that underwent excision | 140/140 | Vivascope 1500 (NR but assumed to be used; correct dx of BCC/SCC) Image‐based (single observer) |
Dermatologist (n = 1); 5 years' experience in RCM Blinded to dermoscopy |
Histology NM 23; BCC: 28; cSCC: 6; Other malignant: 9 melanoma metastases; SK 14; BN 32 including 7 SN); 5 vascular; 6 other benign |
Non evaluable and non‐specific results excluded (n = 11); including 1 BCC and 1 SCC |
|
Nori 2004 BCC |
WPC CCS USA and Spain Secondary/private clinic |
Biopsy confirmed BCC and convenience sample of non‐BCC with 'range of common diagnoses' | 145/152 105 had VI dx |
Vivascope 1000 (no algorithm; selected characteristics; ≥ 3 present) VI (clinical photographs; high/medium/low probability BCC) Image‐based (single observer) |
Observer qual NR (n = 1); 'novice confocal reviewer' Blinded interpretation |
Histology or expert dx; 15/65 benign had clinical dx BCC: 83 ( 58 in VI analysis); cSCC: 4; 'benign' dx: 65 |
BCC: could not disaggregate SCC result (n = 4) from rest of D‐ group |
| AK: actinic keratosis; BCC: basal cell carcinoma; BD: Bowen's disease; BN: benign naevi; BPC: between‐person comparison (of tests); CCS: case‐control study; Cons: consensus diagnosis; CS: case series; cSCC: cutaneous squamous cell carcinoma; DF: dermatofibroma; dx: diagnosis; exp: experience; FP: false positive; FU: follow‐up; LS: lentigo simplex; n: number; NC: non‐comparative; NR: not reported; P: prospective; PLC: pigmented lesion clinic; MEL: invasive melanoma or atypical intraepidermal melanocytic variants; MiS: melanoma in situ (or lentigo maligna); MM: malignant (invasive) melanoma; qual: qualification; R: retrospective; RCM: reflectance confocal microscopy; SK: seborrhoeic keratosis; SN: Spitz nevi; VI: visual inspection; WPC: within‐person comparison (of tests). | |||||||
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
1. Test.
Basal cell carcinoma (BCC) – any suspicious lesion.
2. Test.
BCC – equivocal lesions.
3. Test.
BCC – other lesion populations.
4. Test.
BCC – reflectance confocal microscopy (RCM) – other – Vivascope 3000.
5. Test.
BCC – dermoscopy – equivocal lesions.
6. Test.
BCC – visual inspection – other lesion populations.
7. Test.
Squamous cell carcinoma (SCC) – RCM – all comer.
8. Test.
SCC – RCM – equivocal.
9. Test.
SCC – RCM – other.
10. Test.
SCC – dermoscopy – equivocal.
11. Test.
All keratinocyte skin cancer (KER) – RCM – all comer.
12. Test.
KER – RCM – equivocal.
13. Test.
KER – RCM – other.
14. Test.
KER – dermoscopy – equivocal.
15. Test.
Malignant melanoma (MM)2 – RCM – equivocal (non‐pigmented) not in melanoma review.
16. Test.
BCC – RCM score at ≥ 3 – in person.
17. Test.
BCC – RCM score at NR (likely ≥ 3) – in person.
18. Test.
BCC – Guitera 2‐step algorithm (significant chars for BCC) – image based.
19. Test.
BCC – no algorithm (significant characteristics) – in person.
20. Test.
BCC – no algorithm (significant characteristics) – image based.
21. Test.
BCC – no algorithm (selected characteristics) – in person.
22. Test.
BCC – no algorithm (selected characteristics) – image based.
23. Test.
BCC – no algorithm (observer diagnosis) – in person.
24. Test.
BCC – no algorithm (observer diagnosis) – image based.
25. Test.
BCC – hand‐held RCM – no algorithm (significant characteristics).
28. Test.
SCC – no algorithm (selected characteristics) in person.
29. Test.
SCC – no algorithm (observer diagnosis) – in person.
30. Test.
SCC – no algorithm (observer diagnosis) – image based.
33. Test.
KER – RCM at ≥ 3 – in person.
36. Test.
KER – no algorithm (observer diagnosis) – in person.
37. Test.
KER – no algorithm (observer diagnosis) – image based.
38. Test.
KER – no algorithm (excise decision) – in person.
39. Test.
KER – no algorithm (excise decision) – image based.
40. Test.
BCC – by observer – high – in person.
41. Test.
BCC – by observer – high – image based.
42. Test.
BCC – by observer – low – in person.
43. Test.
BCC – by observer – low – image based.
44. Test.
BCC – by observer – NR – in person.
45. Test.
BCC – by observer – NR – image based.
47. Test.
SCC – by observer – low – in person.
48. Test.
SCC – by observer – NR – in person.
49. Test.
SCC – by observer – high – image based.
50. Test.
SCC – by observer – NR – image based.
52. Test.
KER – by observer – low – in person.
53. Test.
KER – by observer – high – image based.
54. Test.
KER – by observer – low – image based.
55. Test.
KER – by observer – NR – image based.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Castro 2015.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: NR Period of data collection: NR Country: Brazil and USA |
||
| Patient characteristics and setting |
Inclusion criteria: participants recruited were those presenting with ≥ 1 skin lesions that were highly suspicious for BCC based on clinical and dermoscopic examination. All lesions underwent biopsy. Setting: specialist unit (skin cancer/pigmented lesions clinic) Prior testing: clinical or dermatoscopic suspicion, or both Setting for prior testing: unspecified Exclusion criteria: poor‐quality index test image; from discussion: "HH‐RCM imaging was successfully performed in all lesions in which imaging was attempted, while TWP‐RCM was technically applicable in only 59% of lesions in which imaging was attempted." Sample size (participants): number eligible: 73 Sample size (lesions): number eligible: 92. number included: 54 Participant characteristics: mean age 65 years (range 30–89 years). Fitzpatrick phototype: 24 participants with type II; 8 participants with type III Lesion characteristics: site reported for BCCs only – head/neck: 9, trunk: 26, upper limbs/shoulder: 4, lower limbs/hip: 6 |
||
| Index tests |
RCM: Vivascope 3000; using 2 different ways of assessment using HH‐RCM and TWP‐RCM No algorithm. Previously published RCM criteria assessed (cites Guitera 2012; Nori 2004; Agero 2006) and selected criteria chosen Method of diagnosis: not clearly reported; may be in person. "All examinations, including clinical, dermoscopic and RCM imaging, were made by a dermatologist experienced with RCM examination (RPRC) with supervision by a skin cancer expert (GGR or HR)." However, also stated that, "All RCM images were evaluated jointly by two readers blinded to the results of the histopathological examination." Not clear whether this was undertaken at the time of RCM examination or subsequently. Prior test data: clinical examination and dermoscopy. "All examinations, including clinical, dermoscopic and RCM imaging, were made by a dermatologist experienced with RCM examination (RPRC) with supervision by a skin cancer expert (GGR or HR)." Diagnostic threshold: ≥ 3 RCM criteria present Diagnosis based on: consensus (2 observers); (n = 2) Observer qualifications: dermatologist Experience in practice: high experience or 'expert' Experience with index test: high experience/'expert' users (not stated but both observers coauthored studies developing RCM) Other detail: attempted imaging with HH‐RCM and TWP‐RCM using a standardised protocol, however, TWP‐RCM imaging is restricted to anatomic locations that allow contact and is not feasible in some anatomic locations such as the eyelids Derivation aspect to study: images were evaluated for the presence of previously published RCM criteria for identification of BCC; approach to selection of characteristics indicative of skin cancer was not described. Characteristics selected: "at least one of the criteria had to be the presence of 'dark silhouettes' or 'bright tumor islands'; these latter criteria denote the presence of neoplastic aggregates of BCC and hence need to be observed in all cases identified as BCC by RCM." Additional criteria assessed were:
|
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 45 BCCs; disease negative: 9 Target condition (final diagnoses): BCC: 45; 'benign' diagnoses: 9 |
||
| Flow and timing | Excluded participants: imaging with both TWP‐RCM and HH‐RCM was attempted in 92 lesions from 73 participants; however, 38 (41%) of the lesions, mostly facial, were excluded as they were only accessible to HH‐RCM imaging. Time interval to reference test: NR |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Are the included participants and chosen study setting appropriate? | No | ||
| Did the study avoid including participants with multiple lesions? | Unclear | ||
| High | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | No | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | Yes | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Yes | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Low | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| High | |||
Curchin 2011.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: prospective Period of data collection: January 2010 to May 2010 Country: Australia |
||
| Patient characteristics and setting |
Inclusion criteria: people from Dermatology Department's minor excision booking list; not further described Setting: secondary (general dermatology) Prior testing: selected for excision (no further detail) Setting for prior testing: unspecified Exclusion criteria: none reported Sample size (participants): number included: 42 Sample size (lesions): number included: 50 Participant characteristics: none reported Lesion characteristics: none reported |
||
| Index tests |
RCM: Vivascope 1500; RCM score (Pellacani 2007) and LM score for suspected LM of the face (Guitera 2010) Method of diagnosis: in‐person diagnosis Prior test data: dermoscopy "dermoscopic and RCM images were aligned over the top of each other so that correlation between the two could be made." Diagnostic threshold: for melanoma – RCM score: ≥ 3; threshold for LM score for suspected LM of the face was not described (Guitera 2010). Observer diagnosis for SCC/BCC; RCM features listed Diagnosis based on: single observer; (n = 1?) Observer qualifications: NR Experience in practice: not described Experience with index test: low experience/novice users; analysis was performed by a novice to RCM analysis after completing an RCM analysis course in Modena, Italy. |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 21; disease negative: 29 Target condition (final diagnoses): melanoma (invasive): 12; melanoma (in situ): 1; BCC: 9; cSCC: 6 (included SK or AK, or both); 'benign' diagnoses: 23 |
||
| Flow and timing | Time interval to reference test: NR | ||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | No | ||
| Low | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Yes | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | No | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Low | |||
Farnetani 2015.
| Study characteristics | |||
| Patient sampling |
Study design: case series; series of cases consecutively and retrospectively selected by an expert dermoscopist for a web based interobserver reliability study Data collection: retrospective image selection/prospective interpretation Period of data collection: NR Country: Italy (lesion image acquisition); observers were located in the USA (3), Europe (4), Australia (1), and Israel (1). |
||
| Patient characteristics and setting |
Inclusion criteria: diagnostically equivocal lesions excised due to clinical or dermoscopic suspicion of melanoma, where a specific clinical and dermoscopic diagnosis could not be rendered with certainty. Lesions selected by an expert dermoscopist blinded to final diagnosis. Setting: secondary (general dermatology); all included RCM images were collected at the Department of Dermatology of the University of Modena and ReggioEmilia (Modena, Italy) Prior testing: clinical or dermatoscopic suspicion, or both Setting for prior testing: secondary (general dermatology) Exclusion criteria: poor‐quality index test image; "No additional selection criteria were considered in case selection such as the presence or lack of pigmentation, diameter, elevation, or other clinical or dermoscopic attribute. Sample size (participants): number included: NR Sample size (lesions): number included: 100 Participant characteristics: none reported Lesion characteristics: none reported |
||
| Index tests |
RCM: Vivascope 1500; no algorithm – evaluators completed a 'pattern description' (presence/absence of a number of RCM features) Method of diagnosis: confocal images (remote); 3 RCM mosaic images presented per lesion Prior test data: dermoscopy. "Each case for evaluation had a high‐resolution dermoscopic image obtained with a dermoscopic lens that was attached to a digital camera." "No additional clinical information (eg, age and melanoma or lesion history) was provided to evaluators." Diagnostic threshold: evaluators completed a 'pattern description' (presence/absence of a number of RCM features) and gave an overall diagnosis of malignant (melanoma or BCC) or benign. Diagnosis based on: single observer (results presented for each of 9 observers); consensus (≥ 5 of 9 evaluators); mean (across 9 observers and across 6 more experienced and 3 less experienced observers) (n = 9) Observer qualifications: dermatologist Experience in practice: not described Experience with index test: low experience/novice users (3 with < 3 years' RCM experience). High experience/'expert' users (6 with ≥ 3 years' RCM experience) Derivation aspect to study: in addition to pattern analysis described above, discriminant analysis was used to identified RCM features independently associated with malignancy, melanoma, and BCC. 3 of 6 discriminatory RCM features were more frequently observed in melanoma: the presence of pagetoid cells, the presence of atypical cells at the DEJ, and irregular epidermal architecture; 3 of 6 discriminatory RCM features were more frequently observed in BCCs: basaloid cord‐like structures, presence of ulceration, and a specific DEJ pattern. Accuracy was not estimated for combinations of these particular features. |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 35; disease negative: 65 Target condition (final diagnoses): melanoma (in situ and invasive, or NR): 20; BCC: 15; seborrhoeic keratosis: 7; other: 55 melanocytic nevi, 3 AK |
||
| Flow and timing | Excluded participants: excised lesions only included Time interval to reference test: NR Time interval between index test(s): N/A |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | Yes | ||
| Did the study avoid including participants with multiple lesions? | Unclear | ||
| Low | Unclear | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | No | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Unclear | ||
| Was the test interpretation carried out by an experienced examiner? | Yes | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Unclear | |||
Guitera 2012.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: NR Period of data collection: NR Country: Australia and Italy Test set derived: randomly split into training and test sets |
||
| Patient characteristics and setting |
Inclusion criteria: consecutive participants presenting or found with suspicious lesions, including all macules of the face and neck suspicious for LM, and which would be subjected to biopsy or excision to rule out an epithelial tumour or an MM following conventional clinical and dermoscopy diagnosis and with lesion location amenable to RCM; described as predominantly melanocytic or suspicious for BCC. Setting: mixed, lesions recruited from Modena (general dermatology) and Sydney (skin cancer/pigmented lesions clinic) Prior testing: clinical or dermatoscopic suspicion, or both Exclusion criteria: location/site of lesion keratotic, sole, and palm lesions were excluded. Sample size (participants): number eligible: 663 Sample size (lesions): number eligible: 710 / number included: 356 in test set, 253 melanocytic Participant characteristics: median age (full sample): 53, IQR 39 to 66 (for full sample), range: 6–90; male: 354 (53.4%) (of full sample) Lesion characteristics: NR |
||
| Index tests |
RCM: RCM score and Segura algorithm; also derived own independently significant features for MM and BCC. Vivascope 1500 Method of diagnosis: confocal images (remote) Prior test data: lesion site or participant age only, or both: "RCM features were described by two expert observers (GP and PG), blinded from any clinical information, dermoscopy, and clinical aspects, but not for the location and age of the patient." Diagnostic threshold: 2 established algorithms assessed: Pellacani scoring system for melanoma (Pellacani 2007), score > 3; and Segura 2‐step algorithm (Segura 2009), score of 0; own new 2‐step model identified 7 independently significant features for MM (assume presence of any one indicated T+):
8 independently significant features for BCC:
Derivation aspect to study: lesion characteristics assessed a series of 48 features, corresponding to previous observations (Pellacani 2007; Guitera 2009), and new descriptors were considered at 3 different depth levels. Descriptions and definitions provided. Selection of characteristics indicative of skin cancer by multivariate discriminant analysis performed on the training set. Diagnosis based on: single observer (n = 2) Observer qualifications: dermatologist Experience in practice: high experience or 'expert' Experience with index test: high experience/'expert' users |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: not further described; full sample Disease positive: 335/disease negative: 375 Target condition (final diagnoses): test set only; melanoma (in situ and invasive, or NR): 105; BCC: 52; cSCC: 9 benign nevus 132; Spitz nevus 16; AK 8; 31 benign macule of the face; and 3 dermatofibroma |
||
| Flow and timing | No exclusions Imaged prior to biopsy |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | No | ||
| Low | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Unclear | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | Unclear | ||
| Low | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Low | |||
Incel 2015.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: prospective (assumed); "Written consent was obtained from all participants before enrolment." Period of data collection: NR Country: Turkey |
||
| Patient characteristics and setting |
Inclusion criteria: people with non‐pigmented suspected tumoral lesions or proliferative skin lesions and with a vascular structure on dermoscopic examination Setting: secondary (not further described) Istanbul Training and Research Hospital Prior testing: clinical or dermatoscopic suspicion, or both – all participants underwent clinical evaluations "following guidelines of the visual inspection and diagnosis of nonpigmented skin tumor;" those with a vascular structure on dermoscopic examination underwent RCM Setting for prior testing: secondary (general dermatology); specialist unit (skin cancer/pigmented lesions clinic) Exclusion criteria: prominent hyperkeratosis; history of significant other skin disease, kidney, liver, heart disease, surgery, or invasive procedure on the localisation of tumour in the last 6 months, sunbathing or indoor tanning in the last 3 months, and people receiving therapy that has angiogenic effects such as systemic/topical steroids Sample size (participants): number included: 114 Sample size (lesions): number included: 122 Participant characteristics: median age 61 years, range 18‐87 years; male: 57% Lesion characteristics: site – head and neck: 76.2%; extremities: 10.2%; back, abdomen, and chest: 13.6% |
||
| Index tests |
RCM: characteristics from previous studies selected to assist correct diagnosis of different lesion types; also assessed vascularity of lesions using RCM but this did not inform diagnosis. Vivascope 3000 Method of diagnosis: unclear; images of first 60 lesions subjected to blinded evaluation by 2 observers to identify vascular morphology; unclear whether overall diagnoses reported were based on images or in‐person assessments Prior test data: unclear Diagnostic threshold: characteristics listed for BCC included: dark silhouettes in dermis, bright tumour islands at DEJ and in the dermis; cleft‐like dark areas; dendritic cells, bright rond cells, canalicular vessels. Characteristics listed for SCC included: refractile squam/crust in stratum corneum and nucleated cells with dark centre (parakeratotic) cells; atypical honeycomb pattern, disarranged pattern at stratum granulosum layer; large, round, nucleated cells at the granular layer (dyskeratotic cells); dendritic cells at the granular layer and small edged papillae at DEJ; dendritic cells (referenced to Ahlgrimm‐Siess 2010; Ahlgrimm‐Siess 2011; Eichert 2010; Malvehy 2012; Röwert‐Huber 2007) Derivation aspect to study: study assessed vascularity of lesions with RCM but diagnoses of each lesion type reportedly based on above characteristics. Diagnosis based on: NR Observer qualifications: NR Experience in practice: NR Experience with index test: NR |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: clinically, dermoscopically, and confocally suspected malignant lesions, recurrent, and therapy resistant lesions were excised; benign appearing but suspected lesions were punch biopsied. Formalin fixed paraffin embedded tissue sections were stained with haematoxylin–eosin. Histopathological examination was conventionally operated by light microscopy Target condition (final diagnoses): BCC: 56; cSCC: 9; keratoacanthoma 3; SK 11; AK 8; Bowen's disease 7; and 24 other non‐pigmented tumours that included sebaceous hyperplasia 4, eccrine poroma 4, pyogenic granuloma 3, amelanotic melanoma 2, sebaceous adenoma 2, trichilemmoma 2, warty dyskeratoma 1, pilomatrixoma 1, kaposi sarcoma 1, fibrohistiocytic tumour 1, eccrine spiradenoma 1, and eccrine porocarcinoma 1 |
||
| Flow and timing | Index to reference interval: appears consecutive "Biopsy was taken for routine histology from selected patients, and was examined with RCM." No exclusions reported |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | No | ||
| Unclear | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Unclear | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | Unclear | ||
| Low | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Low | |||
Longo 2013.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: retrospective image selection/prospective interpretation Period of data collection: NR Country: Italy |
||
| Patient characteristics and setting |
Inclusion criteria: clinically nodular lesions (defined as cutaneous palpable/superficial seated lesions and not subcutaneous ones) that underwent excision Setting: secondary (general dermatology); specialist unit (skin cancer/pigmented lesions clinic) Prior testing: selected for excision (no further detail) Setting for prior testing: secondary (general dermatology); specialist unit (skin cancer/pigmented lesions clinic) Exclusion criteria: none reported (not evaluable and non‐specific RCM results excluded; see below) Sample size (participants): number included: 140 Sample size (lesions): number included: 140 Participant characteristics: mean age 50 years (SD 19.7). Male: 64; 45.7% Lesion characteristics: all clinically nodular; site – 'most' on the trunk; dermatofibroma mainly located on extremities. Mean thickness 2.16 mm (SD 82); 23 'pure' nodular melanomas |
||
| Index tests |
RCM: model NR; likely Vivascope 1500. No algorithm – reports observer diagnosis and independently significant features Method of diagnosis: confocal images (remote) Prior test data: no further information used; blinded to dermoscopic image Diagnostic threshold: a diagnosis was formulated based on 'RCM pattern analysis' (Longo 2011; Pellacani 2007; and several others cited) Diagnosis based on: single observer (n = 1) Observer qualifications: dermatologist Experience in practice: high experience or 'expert'; 5 years' experience in RCM and, therefore, presumably in practice Experience with index test: high experience/'expert' users; 5 years' experience in RCM Derivation aspect to study: main study data included relate to observer's interpretation of RCM characteristics and diagnostic classification. Univariate and then multivariate discriminant analysis was also performed to identify independently significant RCM criteria (total of 36 assessed) for NM+Mets (nodular melanoma + metastasis) vs all other diagnoses, BCC vs all other diagnoses, SCC vs all other diagnoses. However, the data presented relate to only 130 lesions, and the melanoma metastases cannot be separated from the nodular melanoma, therefore melanoma data not included. Characteristics selected for nodular melanoma or melanoma mets were: widespread pagetoid distribution; many atypical cells; and cerebriform nests. Characteristics selected for BCC were: tumour islands; cauliflower architecture; bright filaments within the tumour islands; and presence of bright collagen. Not clearly reported for SCC. |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 66; disease negative: 57 Target condition (final diagnoses): melanoma (invasive): 23 nodular; BCC: 28; cSCC: 6; other malignant: 9 melanoma metastases; SK: 14; benign naevus: 32 (14 compound, 8 intradermal, 3 blue naevi, 7 Spitz naevi); other: 5 vascular and 6 other benign lesions |
||
| Flow and timing | Excluded participants: 8 not evaluable and 3 'non‐specific' RCM results reported (appear to be excluded from derivation of independently significant characteristics) Not evaluable: lesions where all the 3 levels (epidermis, DEJ, and upper dermis) were not explorable for any reason that hampered the collection of quality images or the exploration of DEJ/superficial dermis. Non‐specific: lesions where a diagnosis could not be formulated, despite the possibility of exploring all 3 levels, because of the impossibility of recognising diagnostic features with enough confidence. |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | No | ||
| Did the study avoid including participants with multiple lesions? | Yes | ||
| Unclear | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | No | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Unclear | ||
| Was the test interpretation carried out by an experienced examiner? | Yes | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Unclear | |||
Nori 2004.
| Study characteristics | |||
| Patient sampling |
Study design: case control; appears to be case‐control type design sampling BCC and non‐BCC Data collection: retrospective image selection/prospective interpretation Period of data collection: 2 years – date range not specified Country: USA and Spain |
||
| Patient characteristics and setting |
Inclusion criteria: biopsy‐confirmed BCC and convenience sample of non‐BCC with 'range of common diagnoses' (only 7 of the 69 non‐BCC had BCC on the list of possible differential diagnoses); of these 105 images were selected for clinical assessment based on superior clinical image quality. Setting: secondary (general dermatology) Division of Dermatology, Loma Linda Uni Med School; Dermatology Service, Madrid, Spain; Private care (Dermatology and Dermatologic surgery private practice); Wellmann Laboratories of Photomedicine, Massachusetts General Hospital Prior testing: NR Setting for prior testing: unspecified Exclusion criteria: none reported Sample size (participants): number included: 145 Sample size (lesions): number included: 152; 105 in VI analysis Participant characteristics: male: 98; 64% Lesion characteristics: lesion site: face/ears: 35%; trunk: 13%; limbs: extremities 45%; back 7% |
||
| Index tests |
VI: no algorithm Method of diagnosis: clinical photographs Prior test data: no further information used Diagnostic threshold: NR. Lesions assigned to: high probability (BCC until confirmed otherwise), medium probability (would biopsy to rule out BCC), and low probability (no biopsy needed). Diagnosis based on: single observer (n = 2) Observer qualifications: dermatologist Experience in practice: not described Experience with index test: not described RCM: Vivascope 1000 (plus prototype device built in Wellman Laboratories (n = 20)). No algorithm; selected characteristics assessed (referenced to Gonzalez 2002) Method of diagnosis: confocal images (remote) Prior test data: no further information used; images from all 152 lesions was retrospectively analysed in a blinded fashion Diagnostic threshold: ≥ 2, 3, 4 or 5 present of 5 features selected based on prior study by same authors (elongated monomorphic basaloid nuclei; polarisation of these nuclei along the same axis of orientation; prominent inflammatory infiltrate; increased dermal vasculature; pleomorphism of the overlying epidermis indicative of actinic changes) Diagnosis based on: single observer (n = 1) Observer qualifications: 'novice confocal reviewer' reviewed all images Experience in practice: not described Experience with index test: low experience/novice users; novice confocal reviewer Other detail: the images produced by Vivascope 1000 and prototype device reportedly similar, with no measurable differences between them. Derivation aspect to study: the 5 criteria were chosen as they were "easily and unambiguously detected by non dermatopathologists and our novice reviewer so that the applicability of our results would be useful to the dermatology community as a whole." |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis plus other Details: 15 lesions were not biopsied (e.g. lesions like SK) because the clinical diagnosis was considered diagnostic Histology: disease positive: 83; disease negative: 54 Expert opinion: disease positive: 0; disease negative: 15 Target condition (final diagnoses): BCC: 83; 58 in VI analysis; cSCC: 4; 'benign' diagnoses: 65 |
||
| Flow and timing | — | ||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Are the included participants and chosen study setting appropriate? | No | ||
| Did the study avoid including participants with multiple lesions? | Yes | ||
| High | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | No | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | No | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | No | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | Unclear | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| High | |||
Pellacani 2014a (cons).
| Study characteristics | |||
| Patient sampling |
Study design: case series (consultation group documented here) Data collection: prospective Period of data collection: January 2010 to December 2010 Country: Italy |
||
| Patient characteristics and setting |
Inclusion criteria: people requesting a mole check or with suspicion of melanoma who were referred to PLC and who were then found to have atypical lesions on dermoscopy. Those in whom diagnosis could not be determined on dermoscopy were referred for an 'outcome decision' (consultation group). Participants were referred on the basis of both urgent access (melanoma suspected in a single lesion by GP or other dermatologist) and scheduled access (referred for dermoscopy and total body examination). Setting: specialist unit (skin cancer/pigmented lesions clinic) Prior testing: dermatoscopic suspicion in all cases. All participants underwent dermoscopy in the PLC; those with dermoscopically atypical lesions were referred for RCM, either to document a lesion already selected for excision (documentation group, reported in Pellacani 2014b (doc)) or for an 'outcome decision' (consultation group), i.e. diagnosis could not be determined on dermoscopy. Setting for prior testing: specialist unit (skin cancer/pigmented lesions clinic) Exclusion criteria: clinically or dermatoscopically clear‐cut epithelial tumours, or both, were not enrolled; poor‐quality index test image. In 9 cases, RCM could not be performed (5 RCM documentation and 4 RCM consultation) due to the presence of artefacts, hyperkeratosis, or ulcerations, impeding imaging. Sample size (participants): number eligible: 1005 examined with dermoscopy; number included: 252 referred for RCM consultation Sample size (lesions): number eligible: NR; number included: 308 for RCM documentation Participant characteristics: median age 41.7 years (IQR 31.9 to 52.1 years); for all 1005 referred participants: 443 male (44%); consultation group only: history of melanoma/skin cancer 23 (7%); family history of melanoma 30 (10%). Fitzpatrick phototype I to II: 150 (49%); Type III to IV 116 (38%) Lesion characteristics: lesion site (full sample) head/neck: 9%; trunk: 59%; upper limbs/shoulder: 12%; lower limbs/hip: 20% |
||
| Index tests |
RCM: RCM score. Vivascope 1500 Method of diagnosis: in person Prior test data: participants were "referred to confocal unit;" confocal reader was blinded to the participant pathway and aware that lesions were dermoscopically atypical for 'RCM documentation' or for 'RCM consultation.' Diagnostic threshold: NR, Pellacani 2005 cited Diagnosis based on: single observer (n = 1) Observer qualifications: dermatologist (assumed; participants were "referred to confocal unit") Experience in practice: not described Experience with index test: not described but 'confocal unit' described Other detail: dermatoscopy examinations were conducted using the Dermlite HR (3Gen LLC, San Juan Capistrano, CA, USA). Lesions that were scheduled for digital monitoring were also acquired by means of FotoFinder (TeachScreen GmbH, Bad Birnbach, Germany) using 20‐fold magnification. |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis plus FU and cancer registry FU Histology (not further described): 81 (consultation group); overall dataset – 292 excised (see Pellacani 2014b (doc)) Clinical FU: 227. 28 of which were subsequently excised because of observed dermatoscopic changes (all benign). Most non‐excised lesions (178/199 (89.4%)) were followed up for 1 year; the others were lost at the 1‐year FU. Cancer registry FU: those lost to clinical FU were checked on the tumour registry; no melanomas were diagnosed in participants scheduled for FU after baseline examinations. Target condition (final diagnoses): melanoma (invasive): 13; melanoma (in situ): 9; BCC: 19; 1 melanoma metastasis; Clark naevus 71; Spitz nevus 5; solar lentigo, SK or lichen planus‐like keratosis 0; other benign 207 (8 with histological diagnosis (25 Clark naevi, 2 Spitz naevi and 1 benign non‐melanocytic lesion) and 199 benign on FU) |
||
| Flow and timing | Excluded participants: 9 excluded due to RCM failure | ||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | No | ||
| High | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Yes | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | No | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| High | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | Yes | ||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| High | |||
Pellacani 2014b (doc).
| Study characteristics | |||
| Patient sampling |
Study design: case series (documentation group described here) Data collection: prospective Period of data collection: January 2010 to December 2010 Country: Italy |
||
| Patient characteristics and setting |
Inclusion criteria: people requesting a mole check or with suspicion of melanoma who were referred to PLC and who were then found to have atypical lesions on dermoscopy. Those in whom excision was required on dermoscopy were referred for RCM documentation (documentation group). Participants were referred on the basis of both urgent access (melanoma suspected in a single lesion by GP or other dermatologist) and scheduled access (referred for dermoscopy and total body examination). Setting: specialist unit (skin cancer/pigmented lesions clinic) Prior testing: dermatoscopic suspicion in all cases. All participants underwent dermoscopy in the PLC; those with dermoscopically atypical lesions were referred for RCM, either to document a lesion already selected for excision (documentation group, as reported here) or for an 'outcome decision' (consultation group, reported in Pellacani 2014a (cons)), i.e. diagnosis could not be determined on dermoscopy. Setting for prior testing: specialist unit (skin cancer/pigmented lesions clinic) Exclusion criteria: clinically or dermatoscopically clear‐cut epithelial tumours, or both, were not enrolled; poor‐quality index test image. In 9 cases, RCM could not be performed (5 RCM documentation and 4 RCM consultation) due to the presence of artefacts, hyperkeratosis, or ulcerations, impeding imaging Sample size (participants): number eligible: 1005 examined with dermoscopy; number included: 171 referred for RCM documentation Sample size (lesions): number eligible: NR; number included: 183 for RCM documentation Participant characteristics: median age 41.2 years (IQR 35 to 63 years); for all 1005 referred participants: 443 male (44%); history of melanoma/skin cancer 8 (5%); family history of melanoma 13 (8%). Fitzpatrick phototype I to II: 99 (58%); Type III to IV 72 (42%) Lesion characteristics: lesion site (full sample) head/neck: 9%; trunk: 59%; upper limbs/shoulder: 12%; lower limbs/hip: 20% |
||
| Index tests |
RCM: RCM score. Vivascope 1500 Method of diagnosis: in person Prior test data: participants were "referred to confocal unit;" confocal reader was blinded to the participant pathway and aware that lesions were dermoscopically atypical for 'RCM documentation' or for 'RCM consultation.' Diagnostic threshold: NR, Pellacani 2005 cited Diagnosis based on: single observer (n = 1) Observer qualifications: dermatologist (assumed; participants were "referred to confocal unit") Experience in practice: not described Experience with index test: not described but 'confocal unit' described Other detail: dermatoscopy examinations were conducted using the Dermlite HR (3Gen LLC, San Juan Capistrano, CA, USA). Lesions that were scheduled for digital monitoring were also acquired by means of FotoFinder (TeachScreen GmbH, Bad Birnbach, Germany) using 20‐fold magnification. |
||
| Target condition and reference standard(s) |
Type of reference standard: histology alone for documentation group; 227 from consultation group were referred for FU (see Pellacani 2014a (cons)) Target condition (final diagnoses): melanoma (invasive): 13; melanoma (in situ): 9; BCC: 19; 1 melanoma metastasis; Clark naevus 121; Spitz nevus 8; solar lentigo, SK or lichen planus‐like keratosis 7; other benign 5 (haemosiderotic dermatofibroma, xanthogranuloma, viral wart, and 2 non‐specific inflammatory dermatoses) |
||
| Flow and timing | Excluded participants: 9 due to RCM failure | ||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | No | ||
| High | High | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Yes | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | Yes | ||
| Was the test interpretation carried out by an experienced examiner? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | No | ||
| Were all patients included in the analysis? | No | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | Yes | ||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| High | |||
Rao 2013.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: NR. Appeared to be prospective but not explicitly stated Period of data collection: June 2010 to September 2011 Country: USA |
||
| Patient characteristics and setting |
Inclusion criteria: all lesions removed for cosmetic or medical reasons that were imaged using a confocal scanning microscope Setting: secondary (general dermatology) based on author institutions Prior testing: NR Setting for prior testing: unspecified Exclusion criteria: none reported Sample size (participants): NR Sample size (lesions): number eligible: 340; number included: 334 Participant characteristics: none reported Lesion characteristics: none reported |
||
| Index tests |
RCM: Vivascope 1500. No algorithm; overall diagnosis Method of diagnosis: in‐person diagnosis USA (reader 1; less experienced) Confocal images (remote) Modena, Italy; reader 2 (more experienced) Prior test data: for image based, "diagnosis was based on the dermoscopic image and confocal microscopy evaluation before excision." Diagnostic threshold: NR; observers gave diagnosis and excise decision (no further details) Diagnosis based on: single observer (n = 2) Observer qualifications: NR; presume dermatologists Experience in practice: not described Experience with index test: low experience/novice users reader 1 (USA) had 1 year of experience at the beginning of the study; High experience/'expert' users reader 2 (Italy) had over 9 years of experience with RCM. Other detail: images were sent via Vivanet (CaliberID, Rochester, NY, USA), a Health Insurance Portability and Accountability Act compliant server. |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 78; disease negative: 256 Target condition (final diagnoses): melanoma (invasive): 8; melanoma (in situ); 1; BCC: 27; cSCC: 42; Benign nevi 176; SK 22; AK 24; other 23 |
||
| Flow and timing | Excluded participants: 6 described as excluded because of insufficient information. Furthermore, 318/334 reported for reader 1 and 323/334 reported for reader 2. | ||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Are the included participants and chosen study setting appropriate? | Unclear | ||
| Did the study avoid including participants with multiple lesions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | Unclear | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | No | ||
| Was the test interpretation carried out by an experienced examiner? | Unclear | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| High | |||
Witkowski 2016.
| Study characteristics | |||
| Patient sampling |
Study design: case series Data collection: retrospective image selection/prospective interpretation Period of data collection: January 2009–2011 Country: Italy |
||
| Patient characteristics and setting |
Inclusion criteria: consecutive clinically equivocal 'pink' cutaneous lesions with absent pigmentation or containing < 10% pigment and absence of pigment network. All lesions were excised at first visit or FU videodermoscopy control visit and had available digital dermoscopy images and a complete standard set of RCM images, with histopathology reports Setting: secondary (general dermatology) Prior testing: clinical suspicion of malignancy without dermatoscopic suspicion Setting for prior testing: secondary (general dermatology) Exclusion criteria: unequivocal appearance/diagnosis benign diagnosis made with high confidence; lack of histological report as a result of the lesion not being excised. Sample size (participants): NR Sample size (lesions): number eligible: 3869 consecutive cases were reviewed; number included: 260 Participant characteristics: none reported Lesion characteristics: none reported |
||
| Index tests |
Dermoscopy: no algorithm Method of diagnosis: dermoscopic images Prior test data: no further information used Diagnostic threshold: not described in detail, but accuracy presented for 2 diagnostic decisions: correct diagnosis (of BCC, MM, and SCC) and correct management decision (excise or not) Diagnosis based on: single observer (n = 2; 1 reader evaluated only dermoscopic images while the second reader evaluated RCM images) Observer qualifications: NR; likely dermatologist Experience in practice: not described Experience with index test: not described RCM: Vivascope 1500; no algorithm – overall diagnosis Method of diagnosis: confocal images (remote) Prior test data: no further information used "The first reader (JL) evaluated only dermoscopic images while the second reader (AW) evaluated RCM images." Diagnostic threshold: NR. Not described in detail, but accuracy presented for 2 diagnostic decisions: correct diagnosis (of BCC, MM, and SCC) and correct management decision (excise or not) Diagnosis based on: single observer (n = 1) Observers: as described above |
||
| Target condition and reference standard(s) |
Type of reference standard: histological diagnosis alone Details: no further details provided Disease positive: 140; disease negative: 120 Target condition (final diagnoses): melanoma (in situ and invasive, or NR): 12; BCC: 114; cSCC: 13; 1 syringoid eccrine carcinoma; SK plus other: 25 (solar lentigo/SK/lichen planus‐like keratosis/AK); 47 nevi; 6 Spitz nevi; 18 dermatofibromas, 4 vascular lesions, and 20 other type benign lesions (1 clear cell acanthoma, 1 discoid lupus, 10 inflammatory lesions, 1 perivascular hyperplasia, 4 granulomatous hyperacanathosis reactions, 1 papulous fibrosis, 1 eccrine poroma, and 1 eczematous lesion). |
||
| Flow and timing | Excluded participants: around 357 cases excluded due to the lack of a histopathology report, as a result of the lesion not being excised, or a benign diagnosis was made with high confidence. Time interval to reference test: NR Time interval between index test(s): NR |
||
| Comparative | |||
| Notes | — | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Are the included participants and chosen study setting appropriate? | Yes | ||
| Did the study avoid including participants with multiple lesions? | Unclear | ||
| Low | Unclear | ||
| DOMAIN 2: Index Test Reflectance confocal microscopy | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| For studies reporting the accuracy of multiple diagnostic thresholds, was each threshold or algorithm interpreted without knowledge of the results of the others? | |||
| Was the test applied and interpreted in a clinically applicable manner? | No | ||
| Were thresholds or criteria for diagnosis reported in sufficient detail to allow replication? | No | ||
| Was the test interpretation carried out by an experienced examiner? | Unclear | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Expert opinion (with no histological confirmation) was not used as a reference standard | Yes | ||
| Was histology interpretation carried out by an experienced histopathologist or by a dermatopathologist? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the referral diagnosis? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the minimum clinical follow‐up after application of index test(s) adequate? | |||
| If more than one algorithm evaluated for the same test, was the interval between application of the different algorithms 1 month or less? | |||
| Unclear | |||
AK: actinic keratosis; BCC: basal cell carcinoma; cSCC: cutaneous squamous cell carcinoma; DEJ: dermoepidermal junction; FU: follow‐up; GP: general practitioner; HH‐RCM: hand‐held reflectance confocal microscopy; IQR: interquartile range; LM: lentigo maligna; MM: malignant melanoma; N/A: not applicable/available; NR: not reported; PLC: pigmented lesion clinic; RCM: reflectance confocal microscopy; SCC: squamous cell carcinoma; SD: standard deviation; SK: seborrhoeic keratosis; TWP‐RCM: traditional wide‐probe reflectance confocal microscopy; VI: visual inspection.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agero 2006 | Excluded on sample size; only 5 lesions |
| Ahlgrimm‐Siess 2010 | Excluded on study population; BCC only Excluded on sample size; only 2 cases |
| Ahlgrimm‐Siess 2011 | Excluded on study population; SCC only Excluded on sample size; only 2 cases |
| Alarcon 2014 | Excluded on sample size; target condition (eligible for melanoma review only) |
| Amjadi 2011 | Excluded on target population; included only BCC (82)/SCC (48) and 8 AK/SK lesions; primary aim appeared to be to differentiate BCC and SCC despite describing inclusion of clinically difficult to diagnose non‐pigmented lesions. Excluded on derivation study |
| Bassoli 2012 | Excluded on target condition; aimed to identify criteria for specific diagnosis of LPLK using in vivo RCM |
| Benati 2015 | Excluded on individual lesion characteristics |
| Braga 2009 | Excluded on sample size; case reports |
| Carrera 2015 | Excluded as not a primary study |
| de Carvalho 2015 | Excluded on individual lesion characteristics Excluded on 2×2 data |
| de Carvalho 2016 | Excluded on target condition Excluded on sample size |
| Edwards 2016 | Excluded as not a primary study; systematic review |
| Eichert 2010 | Excludes on individual lesion characteristics; looked at accuracy of previously identified RCM features for melanoma, BCC and SCC in a cohort of 100 lesions but did not give accuracy for overall diagnosis of each group |
| Ferrari 2015 | Excluded on target condition (eligible for melanoma review only) |
| Figueroa‐Silva 2016 | Excluded on target condition (eligible for melanoma review only) |
| Gareau 2009 | Excluded on study population; only BCC cases |
| Gerger 2005 | Excluded on reference standard; only 1/3 of disease negative group had adequate reference test Excluded; duplicate or related publication; data reported as training set in Koller 2011 (#860) |
| Gerger 2006 | Excluded on reference standard Only 30/120 benign were excised (30/90 benign nevi and 0/30 SK) |
| Gerger 2008 | Excluded on reference standard All MMs were excised plus 14/50 benign; remainder diagnosed on clinical/dermoscopic criteria |
| Giambrone 2015 | Excluded on target condition Excluded but contacted authors they do not give information on the target condition other than describing malignant and benign cutaneous lesions. Contacted 8 May 2017 |
| Gill 2014 | Excluded as derivation study; looking for correlation with histological features Excluded on 2×2 data; looked at correlation between RCM features and histological features; not test accuracy Excluded duplicate or related publication; same lesions reportedly included in Pellacani 2012 |
| Gonzalez 2002 | Excluded on population included only BCC |
| Gonzalez 2013 | Excluded not a primary study |
| Guida 2015 | Excluded not a primary study; systematic review |
| Guitera 2009 | Excluded on target condition (eligible for melanoma review only) |
| Guitera 2010 | Excluded on target condition; only looking at LM and not LMM |
| Guitera 2013 | Excluded on study population; LM and LMM only Excluded on target condition; data only available for LM Excluded on 2×2 data |
| Haenssle 2006 | Excluded on index test; surveillance study estimating accuracy of different approaches to follow‐up |
| Hennessy 2010 | Excluded on 2×2 data |
| Hofmann‐Wellenhof 2008 | Excluded on reference standard; included 70 melanocytic lesions; 20 MM (all histologically verified); 70 benign naevi (28% histologically verified, and the rest diagnosed with dermoscopy only) |
| Hoogedoorn 2014 | Excluded; conference abstract |
| Hoogedoorn 2015 | Excluded on sample size |
| Humphrey 2006 | Excluded on study population Excluded as derivation study; assessed lesion vascularity |
| Kadouch 2015a | Systematic review |
| Kadouch 2015b | Excluded not a primary study; clinical trial protocol |
| Koller 2011 | Excluded on target condition (eligible for melanoma review only) |
| Kose 2014 | Excluded not a test accuracy study Excluded on 2×2 data |
| Langley 2001 | Excluded on 2×2 Excluded, contacted authors for RCM 2×2 data; could only get 2×2 for clinical diagnosis |
| Langley 2006 | Excluded on sample size |
| Langley 2007 | Excluded on target condition (eligible for melanoma review only) |
| Losi 2014 | Excluded if individual lesion characteristics Excluded on 2×2 data |
| Lovatto 2015 | Excluded on target condition (eligible for melanoma review only) |
| Maier 2013 | Excluded on study population; all study participants had final diagnosis of melanoma |
| Malvehy 2012 | Excluded not a primary study; review paper |
| Menge 2016 | Excluded on target population; included participants with primary possible recurrent and or previously treated lesions and did not disaggregate results. Also included multiple lesions per participant (63 'sites' from 17 participants; unclear how many of the 39 LM positive on histology had melanoma) |
| Miller 2011 | Excluded on target condition Excluded on 2×2 data; not an accuracy study |
| Nobre Moura 2011 | Excluded on sample size; case report |
| Pellacani 2005 | Excluded if derivation study; used leave 1 out |
| Pellacani 2007 | Excluded on target condition (eligible for melanoma review only) |
| Pellacani 2008 | Excluded on 2×2 data; no accuracy data provided in the study, looked at correlation of RCM features to dermoscopy and histology |
| Pellacani 2009 | Excluded on 2×2 data; study tested concordance of terminology used in RCM; not accuracy |
| Pellacani 2012 | Excluded on target condition (eligible for melanoma review only) |
| Peppelman 2013 | Excluded on study population; only present data for subtypes of BCC Excluded on 2×2 data; did not give accuracy data |
| Peppelman 2015 | Excluded if derivation study Excluded on 2×2 data; no data for overall accuracy |
| Peppelman 2016 | Excluded as not a primary study; RCT protocol |
| Puig 2012 | Excluded on sample size; case report |
| Pupelli 2013 | Excluded on target condition (eligible for melanoma review only) |
| Reggiani 2015 | Excluded not a primary study; systematic review |
| Rishpon 2009 | Excluded on sample size; only 3 invasive SCC Excluded if derivation study RCM characteristics for SCC |
| Röwert‐Huber 2007 | Excluded not a primary study; review paper |
| Salerni 2011 | Excluded on sample size; < 5 cases |
| Scope 2009 | Excluded on sample size |
| Scope 2014 | Excluded as not a primary study; editorial paper |
| Segura 2009 | Excluded on target condition (eligible for melanoma review only) |
| Soyer 2013 | Excluded as not a primary study; comment on a primary study (Longo 2013) |
| Stanganelli 2015 | Excluded on target condition (eligible for melanoma review only) |
| Steiner 1992 | Excluded on sample size; only 2 melanomas |
| Stephens 2013 | Excluded on sample size |
| Stevenson 2013 | Excluded not a primary study; systematic review of RCM |
| Tannous 2009 | Excluded on sample size; only 2 malignant melanomas |
| Willard 2011 | Excluded on sample size; case study |
| Xiong 2016 | Excluded as not a primary study; systematic review of RCM |
| Yelamos 2016 | Excluded as not a primary study |
AK: actinic keratosis; BCC: basal cell carcinoma; LM: lentigo maligna; LMM: lentigo maligna melanoma; LPLK: lichen planus‐like keratosis; RCM: reflectance confocal microscopy; RCT: randomised controlled trial; SCC: squamous cell carcinoma; SK: solar keratosis. See also Appendix 2.
Characteristics of studies awaiting classification [ordered by study ID]
Borsari 2016.
| Study characteristics | |||
| Patient sampling | Not yet assessed | ||
| Patient characteristics and setting | Not yet assessed | ||
| Index tests | Not yet assessed | ||
| Target condition and reference standard(s) | Not yet assessed | ||
| Flow and timing | Not yet assessed | ||
| Comparative | Not yet assessed | ||
| Notes | Published October 2016; after search dates | ||
Guitera 2016.
| Study characteristics | |||
| Patient sampling | Not yet assessed | ||
| Patient characteristics and setting | Not yet assessed | ||
| Index tests | Not yet assessed | ||
| Target condition and reference standard(s) | Not yet assessed | ||
| Flow and timing | Not yet assessed | ||
| Comparative | Not yet assessed | ||
| Notes | Published October 2016; after search dates | ||
Jain 2017.
| Study characteristics | |||
| Patient sampling | Not yet assessed | ||
| Patient characteristics and setting | Not yet assessed | ||
| Index tests | Not yet assessed | ||
| Target condition and reference standard(s) | Not yet assessed | ||
| Flow and timing | Not yet assessed | ||
| Comparative | Not yet assessed | ||
| Notes | Published March 2017; conference abstract only | ||
Ludzik 2016.
| Study characteristics | |||
| Patient sampling | Not yet assessed | ||
| Patient characteristics and setting | Not yet assessed | ||
| Index tests | Not yet assessed | ||
| Target condition and reference standard(s) | Not yet assessed | ||
| Flow and timing | Not yet assessed | ||
| Comparative | Not yet assessed | ||
| Notes | Published September 2016; after search dates | ||
Differences between protocol and review
For the primary objective, study populations that could not be clearly identified as either 'any suspicious lesion' or 'equivocal lesions' were considered separately as 'other lesion' studies.
Secondary objectives have been tailored to the individual test, with three objectives added: to compare the accuracy of RCM to dermoscopy where both tests have been evaluated in the same studies; to determine the diagnostic accuracy of individual algorithms for RCM; and to determine the effect of observer experience.
The secondary objective has been changed from "for the detection of any skin cancer" to "for the detection of any skin cancer in adults, where keratinocyte skin cancers make up at least 50% of included skin cancers" in order to keep the focus on keratinocyte skin cancers for this review and in order not to replicate analyses conducted for the review of RCM for melanoma. These changes also affect the definition of the secondary target condition in the Methods section. Heterogeneity investigations were limited by the data available.
Population inclusion criteria amended from inclusion of adults with lesions suspicious for keratinocyte skin cancer to inclusion of adults with lesions suspicious for any skin cancer, on the basis that studies targeting those with pigmented skin lesions or with lesions suspicious for melanoma also reported 2×2 contingency data for the detection of BCC or cSCC within these populations. We added a requirement for a minimum of five benign lesions as well as five malignant lesions. The size threshold of five was arbitrary. However, such small studies are unlikely to add precision to estimates of accuracy.
We amended the text to clarify that studies available only as conference abstracts would be excluded from the review unless full papers could be identified; studies available only as conference abstracts do not allow a comprehensive assessment of study methods or methodological quality.
We proposed to supplement the database searches by searching the annual meetings of appropriate organisations (e.g. British Association of Dermatologists Annual Meeting, American Academy of Dermatology Annual Meeting, European Academy of Dermatology and Venereology Meeting, Society for Melanoma Research Congress, World Congress of Dermatology, European Association of Dermato Oncology); however, due to volume of evidence retrieved from database searches and time restrictions, we were unable to do this.
For quality assessment, the QUADAS‐2 tool was further tailored according to the review topic. In terms of analysis, restriction to analysis of per participant data was not performed due to lack of data. Sensitivity analyses were not performed as planned due to lack of data.
We intended to analyse studies separately according to in‐ person and image‐based assessments; however, we were unable to do so due to lack of data.
Studies using cross‐validation, such as 'leave‐one‐out' cross‐validation were excluded rather than included as these methods are not sufficiently robust and are likely to produce unrealistic estimates of test accuracy.
To improve clarity of methods and to allow inclusion of studies presenting simple algorithms consisting of lesion characteristics that had previously been suggested as associated with BCC or cSCC: this text from the protocol, "We will include studies developing new algorithms or methods of diagnosis (i.e. derivation studies) if they use a separate independent 'test set' of participants or images to evaluate the new approach. We will also include studies using other forms of cross validation, such as 'leave‐one‐out' cross‐validation (Efron 1983). We will note for future reference (but not extract) any data on the accuracy of lesion characteristics individually, e.g. the presence or absence of a pigment network or detection of asymmetry," has been replaced with "We included studies developing new algorithms or methods of diagnosis (i.e. derivation studies) if they:
used a separate independent 'test set' of participants or images to evaluate the new approach, or
investigated lesion characteristics that had previously been suggested as associated with BCC or cSCC and the study reported accuracy based on the presence or absence of particular combinations of characteristics.
We excluded studies if they:
used a statistical model to produce a data driven equation, or algorithm based on multiple diagnostic features, with no separate test set;
used cross‐validation approaches such as 'leave‐one‐out' cross‐validation (Efron 1983);
evaluated the accuracy of the presence or absence of individual lesion characteristics or morphological features, with no overall diagnosis of malignancy."
Although we extracted any reporting of special interest or accreditation in skin cancer according to observer expertise, we were unable to analyse the effect on accuracy due to lack of data.
As per the change to secondary objectives, this text from the protocol "For our secondary objective, the target condition will include any skin lesion requiring excision. We will include studies reporting data for keratinocyte skin cancer combined, and not differentiated according to BCC or cSCC, in this analysis, along with any melanoma or rare skin cancer (e.g. Merkel or amelanotic melanoma) that may be detected. We will not consider in situ cancers or actinic keratosis as disease‐positive" has been changed to "An additional definition of the target condition was considered in secondary analysis, the detection of:
any skin cancer, including BCC, cSCC, melanoma, or any rare skin cancer (e.g. Merkel cell cancer), as long as skin cancers other than melanoma made up more than 50% of the disease positive group. Data from studies in which melanoma accounted for more than 50% of skin cancers were included in the review of RCM for the diagnosis of melanoma (Dinnes 2018a)."
Added the following as possible sources of heterogeneity in Appendix 1:
participant population: primary/secondary/specialist unit;
lesion suspicion: general suspicion/atypical/equivocal/not reported;
lesion type: any pigmented; melanocytic;
inclusion of multiple lesions per participant.
Contributions of authors
JD was the contact person with the editorial base. JD co‐ordinated contributions from the coauthors and wrote the final draft of the review. SB conducted the literature searches. JD, NC, DS, and LP screened papers against eligibility criteria. JD and NC obtained data on ongoing and unpublished studies. JD, NC, DS, and LP appraised the quality of papers. JD, NC, DS, and LP extracted data for the review and sought additional information about papers. JD entered data into Review Manager 5. JD and JJD analysed and interpreted data. JD, JJD, NC, YT, and CD worked on the methods sections. JD, DS, RP, RNM, and HCW drafted the clinical sections of the background and responded to the clinical comments of the referees. JD, JJD, CD, and YT responded to the methodology and statistics comments of the referees. KG was the consumer coauthor and checked the review for readability and clarity, as well as ensuring outcomes are relevant to consumers. JD is the guarantor of the update.
Disclaimer
This project presents independent research supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Skin Group and Cochrane Programme Grant funding, and the NIHR Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health and Social Care.
Sources of support
Internal sources
No sources of support supplied
External sources
-
The National Institute for Health Research (NIHR), UK.
The NIHR, UK, is the largest single funder of the Cochrane Skin Group
-
NIHR Systematic Review Programme, UK.
This project was funded by an NIHR Cochrane Systematic Reviews Programme Grant (13/89/15)
-
NIHR Birmingham Biomedical Research Centre, UK.
JD, JJD and YT receive support from the NIHR Birmingham Biomedical Research Centre
Declarations of interest
JD: nothing to declare. JJD: nothing to declare. NC: nothing to declare. DS: nothing to declare. SB: nothing to declare. YT: nothing to declare. CD: nothing to declare. LP: nothing to declare. RM: "my institution received a grant for a BARCO NV commercially sponsored study to evaluate digital dermoscopy in the skin cancer clinic and Oxfordshire Health Services Research Charitable Funds for carrying out a study of feasibility of using the SCQOLIT tool in non‐melanoma skin cancer; I have received payment from the UK Photopheresis Society for a lecture on cutaneous graft versus host disease October 2017; and royalties for Oxford Handbook of Medical Dermatology (Oxford University Press). I have no conflicts of interest to declare that directly relate to the publication of this work." COS: nothing to declare. RP: nothing to declare. HCW: "I am director of the NIHR HTA Programme. HTA is part of the NIHR which also supports the NIHR systematic reviews programme from which this work is funded."
Edited (no change to conclusions)
References
References to studies included in this review
Castro 2015 {published data only}
- Castro RP, Stephens A, Fraga‐Braghiroli NA, Oliviero MC, Rezze GG, Rabinovitz H, et al. Accuracy of in vivo confocal microscopy for diagnosis of basal cell carcinoma: a comparative study between handheld and wide‐probe confocal imaging. Journal of the European Academy of Dermatology and Venereology 2015;29(6):1164‐9. [DOI: 10.1111/jdv.12780; ER4:20569441; PUBMED: 25338750] [DOI] [PubMed] [Google Scholar]
Curchin 2011 {published data only}
- Curchin CE, Wurm EM, Lambie DLj, Longo C, Pellacani G, Soyer HP. First experiences using reflectance confocal microscopy on equivocal skin lesions in Queensland. Australasian Journal of Dermatology 2011;52(2):89‐97. [ER4:15465900; PUBMED: 21605091] [DOI] [PubMed] [Google Scholar]
Farnetani 2015 {published data only}
- Farnetani F, Scope A, Braun RP, Gonzalez S, Guitera P, Malvehy J, et al. Skin cancer diagnosis with reflectance confocal microscopy: reproducibility of feature recognition and accuracy of diagnosis. JAMA Dermatology 2015;151(10):1075‐80. [ER4:25233569; PUBMED: 25993262] [DOI] [PubMed] [Google Scholar]
Guitera 2012 {published data only}
- Guitera P, Menzies SW, Longo C, Cesinaro AM, Scolyer RA, Pellacani G. In vivo confocal microscopy for diagnosis of melanoma and basal cell carcinoma using a two‐step method: analysis of 710 consecutive clinically equivocal cases. Journal of Investigative Dermatology 2012;132(10):2386‐94. [ER4:15465942; PUBMED: 22718115] [DOI] [PubMed] [Google Scholar]
Incel 2015 {published data only}
- Incel P, Gurel MS, Erdemir AV. Vascular patterns of nonpigmented tumoral skin lesions: confocal perspectives. Skin Research & Technology 2015;21(3):333‐9. [PUBMED: 25345376] [DOI] [PubMed] [Google Scholar]
Longo 2013 {published data only}
- Longo C, Farnetani F, Ciardo S, Cesinaro AM, Moscarella E, Ponti G, et al. Is confocal microscopy a valuable tool in diagnosing nodular lesions? A study of 140 cases. British Journal of Dermatology 2013;169(1):58‐67. [ER4:15465992; PUBMED: 23374159] [DOI] [PubMed] [Google Scholar]
Nori 2004 {published data only}
- Nori S, Rius‐Diaz F, Cuevas J, Goldgeier M, Jaen P, Torres A, et al. Sensitivity and specificity of reflectance‐mode confocal microscopy for in vivo diagnosis of basal cell carcinoma: a multicenter study. Journal of the American Academy of Dermatology 2004;51(6):923‐30. [ER4:15466027; PUBMED: 15583584] [DOI] [PubMed] [Google Scholar]
Pellacani 2014a (cons) {published data only}
- Pellacani G, Pepe P, Casari A, Longo C. Reflectance confocal microscopy as a second‐level examination in skin oncology improves diagnostic accuracy and saves unnecessary excisions: a longitudinal prospective study. British Journal of Dermatology 2014;171(5):1044‐51. [PUBMED: 24891083] [DOI] [PubMed] [Google Scholar]
Pellacani 2014b (doc) {published data only}
- Pellacani G, Pepe P, Casari A, Longo C. Reflectance confocal microscopy as a second‐level examination in skin oncology improves diagnostic accuracy and saves unnecessary excisions: a longitudinal prospective study. British Journal of Dermatology 2014;171(5):1044‐51. [PUBMED: 24891083] [DOI] [PubMed] [Google Scholar]
Rao 2013 {published data only}
- Rao BK, Mateus R, Wassef C, Pellacani G. In vivo confocal microscopy in clinical practice: comparison of bedside diagnostic accuracy of a trained physician and distant diagnosis of an expert reader. Journal of the American Academy of Dermatology 2013;69(6):e295‐300. [ER4:15466076; PUBMED: 24035553] [DOI] [PubMed] [Google Scholar]
Witkowski 2016 {published data only}
- Witkowski AM, Ludzik J, DeCarvalho N, Ciardo S, Longo C, DiNardo A, et al. Non‐invasive diagnosis of pink basal cell carcinoma: how much can we rely on dermoscopy and reflectance confocal microscopy?. Skin Research & Technology 2016;22(2):230‐7. [ER4:25012281; PUBMED: 26338448] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agero 2006 {published data only}
- Agero AL, Busam KJ, Benvenuto‐Andrade C, Scope A, Gill M, Marghoob AA, et al. Reflectance confocal microscopy of pigmented basal cell carcinoma. Journal of the American Academy of Dermatology 2006;54(4):638‐43. [DOI] [PubMed] [Google Scholar]
Ahlgrimm‐Siess 2010 {published data only}
- Ahlgrimm‐Siess V, Cao T, Oliviero M, Hofmann‐Wellenhof R, Rabinovitz HS, Scope A. The vasculature of nonmelanocytic skin tumors in reflectance confocal microscopy: vascular features of basal cell carcinoma. Archives of Dermatology 2010;146(3):353‐4. [DOI] [PubMed] [Google Scholar]
Ahlgrimm‐Siess 2011 {published data only}
- Ahlgrimm‐Siess V, Cao T, Oliviero M, Hofmann‐Wellenhof R, Rabinovitz HS, Scope A. The vasculature of nonmelanocytic skin tumors on reflectance confocal microscopy: vascular features of squamous cell carcinoma in situ. Archives of Dermatology 2011;147(2):264. [DOI] [PubMed] [Google Scholar]
Alarcon 2014 {published data only}
- Alarcon I, Carrera C, Turegano P, Malvehy J, Puig S. Basal cell carcinoma with spontaneous regression: added value of reflectance confocal microscopy when the dermoscopic diagnosis is uncertain. Journal of the American Academy of Dermatology 2014;71(1):e7‐9. [DOI] [PubMed] [Google Scholar]
Amjadi 2011 {published data only}
- Amjadi M, Coventry BJ, Greenwood JE. Reflectance confocal microscopy in the diagnosis of non‐melanoma skin cancer and benign lesions versus normal skin: a blinded prospective trial. Internet Journal of Plastic Surgery 2011;7(2):1‐6. [ER4:21450593] [Google Scholar]
Bassoli 2012 {published data only}
- Bassoli S, Rabinovitz HS, Pellacani G, Porges L, Oliviero MC, Braun RP, et al. Reflectance confocal microscopy criteria of lichen planus‐like keratosis. Journal of the European Academy of Dermatology & Venereology 2012;26(5):578‐90. [DOI] [PubMed] [Google Scholar]
Benati 2015 {published data only}
- Benati E, Argenziano G, Kyrgidis A, Moscarella E, Ciardo S, Bassoli S, et al. Melanoma and naevi with a globular pattern: confocal microscopy as an aid for diagnostic differentiation. British Journal of Dermatology 2015;173(5):1232‐8. [DOI] [PubMed] [Google Scholar]
Braga 2009 {published data only}
- Braga JC, Scope A, Klaz I, Mecca P, Gonzalez S, Rabinovitz H, et al. The significance of reflectance confocal microscopy in the assessment of solitary pink skin lesions. Journal of the American Academy of Dermatology 2009;61(2):230‐41. [DOI] [PubMed] [Google Scholar]
Carrera 2015 {published data only}
- Carrera C. High‐risk melanoma patients: can unnecessary naevi biopsies be avoided?. British Journal of Dermatology 2015;172(2):313‐5. [DOI] [PubMed] [Google Scholar]
de Carvalho 2015 {published data only}
- Carvalho N, Farnetani F, Ciardo S, Ruini C, Witkowski AM, Longo C, et al. Reflectance confocal microscopy correlates of dermoscopic patterns of facial lesions help to discriminate lentigo maligna from pigmented nonmelanocytic macules. British Journal of Dermatology 2015;173(1):128‐33. [DOI] [PubMed] [Google Scholar]
de Carvalho 2016 {published data only}
- Carvalho N, Guida S, Spagnol AL, Cesinaro AM, Farnetani F, Bonamonte D, et al. Pink melanocytic and non‐melanocytic lesions: how reflectance confocal microscopy can help in differential diagnosis. Journal of the European Academy of Dermatology & Venereology 2016;30(6):1026‐9. [DOI] [PubMed] [Google Scholar]
Edwards 2016 {published data only}
- Edwards SJ, Mavranezouli I, Osei‐Assibey G, Marceniuk G, Wakefield V, Karner C. VivaScope 1500 and 3000 systems for detecting and monitoring skin lesions: a systematic review and economic evaluation. Health Technology Assessment (Winchester, England) 2016;20(58):1‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eichert 2010 {published data only}
- Eichert S, Mohrle M, Breuninger H, Rocken M, Garbe C, Bauer J. Diagnosis of cutaneous tumors with in vivo confocal laser scanning microscopy. Journal der Deutschen Dermatologischen Gesellschaft 2010;8(6):400‐10. [DOI] [PubMed] [Google Scholar]
Ferrari 2015 {published data only}
- Ferrari B, Pupelli G, Farnetani F, Carvalho NT, Longo C, Reggiani C, et al. Dermoscopic difficult lesions: an objective evaluation of reflectance confocal microscopy impact for accurate diagnosis. Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(6):1135‐40. [DOI: 10.1111/jdv.12769; ER4:20569458; PUBMED: 25303304] [DOI] [PubMed] [Google Scholar]
Figueroa‐Silva 2016 {published data only}
- Figueroa‐Silva O, Cinotti E, Almeida Silva T, Moscarella E, Lallas A, Ciardo S, et al. Diagnostic accuracy of reflectance confocal microscopy for lesions typified by dermoscopic island. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(9):1594‐8. [ER4:25012335; PUBMED: 27109574] [DOI] [PubMed] [Google Scholar]
Gareau 2009 {published data only}
- Gareau DS, Karen JK, Dusza SW, Tudisco M, Nehal KS, Rajadhyaksha M. Sensitivity and specificity for detecting basal cell carcinomas in Mohs excisions with confocal fluorescence mosaicing microscopy. Journal of Biomedical Optics 2009;14(3):034012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gerger 2005 {published data only}
- Gerger A, Koller S, Kern T, Massone C, Steiger K, Richtig E, et al. Diagnostic applicability of in vivo confocal laser scanning microscopy in melanocytic skin tumors. Journal of Investigative Dermatology 2005;124(3):493‐8. [DOI] [PubMed] [Google Scholar]
Gerger 2006 {published data only}
- Gerger A, Kerl H, Samonigg H, Langsenlehner U, Krippl P, Smolle J. Sensitivity and specificity of confocal laser scanning microscopy for in vivo diagnosis of malignant skin tumors. Journal of Investigative Dermatology 2006;126(Suppl 3):s114. [DOI] [PubMed] [Google Scholar]
Gerger 2008 {published data only}
- Gerger A, Wiltgen M, Langsenlehner U, Richtig E, Horn M, Weger W, et al. Diagnostic image analysis of malignant melanoma in in vivo confocal laser‐scanning microscopy: a preliminary study. Skin Research & Technology 2008;14(3):359‐63. [DOI] [PubMed] [Google Scholar]
Giambrone 2015 {published data only}
- Giambrone D, Alamgir M, Masud A, Bronsnick T, Rao B. The diagnostic accuracy of in vivo confocal microscopy in clinical practice. Journal of the American Academy of Dermatology 2015;73(2):317‐9. [DOI] [PubMed] [Google Scholar]
Gill 2014 {published data only}
- Gill M, Longo C, Farnetani F, Cesinaro AM, Gonzalez S, Pellacani G. Non‐invasive in vivo dermatopathology: identification of reflectance confocal microscopic correlates to specific histological features seen in melanocytic neoplasms. Journal of the European Academy of Dermatology & Venereology 2014;28(8):1069‐78. [DOI] [PubMed] [Google Scholar]
Gonzalez 2002 {published data only}
- Gonzalez S, Tannous Z. Real‐time in vivo confocal reflectance microscopy of basal cell carcinoma. Journal of the American Academy of Dermatology 2002;47:869‐74. [DOI] [PubMed] [Google Scholar]
Gonzalez 2013 {published data only}
- Gonzalez S. Should reflectance confocal microscopy be the gold standard for basal cell carcinoma diagnosis?. Imaging in Medicine 2013;5(4):299‐301. [Google Scholar]
Guida 2015 {published data only}
- Guida S, Longo C, Casari A, Ciardo S, Manfredini M, Reggiani C, et al. Update on the use of confocal microscopy in melanoma and non‐melanoma skin cancer. Giornale Italiano di Dermatologia e Venereologia 2015;150(5):547‐63. [PubMed] [Google Scholar]
Guitera 2009 {published data only}
- Guitera P, Pellacani G, Longo C, Seidenari S, Avramidis M, Menzies SW. In vivo reflectance confocal microscopy enhances secondary evaluation of melanocytic lesions. Journal of Investigative Dermatology 2009;129(1):131‐8. [ER4:15465945; PUBMED: 18633444] [DOI] [PubMed] [Google Scholar]
Guitera 2010 {published data only}
- Guitera P, Pellacani G, Crotty KA, Scolyer RA, Li L‐X, Bassoli S, et al. The impact of in vivo reflectance confocal microscopy on the diagnostic accuracy of lentigo maligna and equivocal pigmented and nonpigmented macules of the face. Journal of Investigative Dermatology 2010;130(8):2080‐91. [DOI] [PubMed] [Google Scholar]
Guitera 2013 {published data only}
- Guitera P, Moloney FJ, Menzies SW, Stretch JR, Quinn MJ, Hong A, et al. Improving management and patient care in lentigo maligna by mapping with in vivo confocal microscopy. JAMA Dermatology 2013;149(6):692‐8. [DOI] [PubMed] [Google Scholar]
Haenssle 2006 {published data only}
- Haenssle HA, Krueger U, Vente C, Thoms K‐M, Bertsch HP, Zutt M, et al. Results from an observational trial: digital epiluminescence microscopy follow‐up of atypical nevi increases the sensitivity and the chance of success of conventional dermoscopy in detecting melanoma. Journal of Investigative Dermatology 2006;126(5):980‐5. [DOI] [PubMed] [Google Scholar]
Hennessy 2010 {published data only}
- Hennessy R, Jacques S, Pellacani G, Gareau D. Clinical feasibility of rapid confocal melanoma feature detection. Proceedings of the SPIE 2010;7548:75480Q. [Google Scholar]
Hofmann‐Wellenhof 2008 {published data only}
- Hofmann‐Wellenhof R, Langsenlehner U, Richtig E, Koller S, Weger W, Ahlgrimm‐Siess V, et al. In vivo confocal laser scanning microscopy of melanocytic skin tumours: diagnostic applicability using unselected tumour images. British Journal of Dermatology 2008;158(2):329‐33. [DOI] [PubMed] [Google Scholar]
Hoogedoorn 2014 {published data only}
- Hoogedoorn L, Peppelman M, Erp PE, Gerritsen MJ. The use of in vivo reflectance confocal microscopy in clinical practice: prospective differentiation of difficult to distinguish nodular basal cell carcinomas and intradermal nevi. Nederlands Tijdschrift voor Dermatologie en Venereologie 2014;24(1):48. [Google Scholar]
Hoogedoorn 2015 {published data only}
- Hoogedoorn L, Peppelman M, Blokx WA, Erp PE, Gerritsen M‐JP. Prospective differentiation of clinically difficult to distinguish nodular basal cell carcinomas and intradermal nevi by non‐invasive reflectance confocal microscopy: a case series study. Journal of the European Academy of Dermatology and Venereology 2015;29(2):330‐6. [DOI] [PubMed] [Google Scholar]
Humphrey 2006 {published data only}
- Humphrey S, Walsh NM, Delaney L, Propperova I, Langley RG. Prognostic significance of vascularity in cutaneous melanoma: pilot study using in vivo confocal scanning laser microscopy. Journal of Cutaneous Medicine and Surgery 2006;10(3):122‐7. [DOI] [PubMed] [Google Scholar]
Kadouch 2015a {published data only}
- Kadouch DJ, Schram ME, Leeflang MM, Limpens J, Spuls PI, Rie MA. In vivo confocal microscopy of basal cell carcinoma: a systematic review of diagnostic accuracy. Journal of the European Academy of Dermatology & Venereology 2015;29(10):1890‐7. [DOI] [PubMed] [Google Scholar]
Kadouch 2015b {published data only}
- Kadouch DJ, Wolkerstorfer A, Elshot Y, Zupan‐Kajcovski B, Crijns MB, Starink MV, et al. Treatment of basal cell carcinoma using a one‐stop‐shop with reflectance confocal microscopy: study design and protocol of a randomized controlled multicenter trial. JMIR Research Protocols 2015;4(3):e109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koller 2011 {published data only}
- Koller S, Wiltgen M, Ahlgrimm‐Siess V, Weger W, Hofmann‐Wellenhof R, Richtig E, et al. In vivo reflectance confocal microscopy: automated diagnostic image analysis of melanocytic skin tumours. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25(5):554‐8. [ER4:15465979; PUBMED: 20735518] [DOI] [PubMed] [Google Scholar]
Kose 2014 {published data only}
- Kose K, Cordova M, Duffy M, Flores ES, Brooks DH, Rajadhyaksha M. Video‐mosaicing of reflectance confocal images for examination of extended areas of skin in vivo. British Journal of Dermatology 2014;171(5):1239‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Langley 2001 {published data only}
- Langley RG, Rajadhyaksha M, Dwyer PJ, Sober AJ, Flotte TJ, Anderson RR. Confocal scanning laser microscopy of benign and malignant melanocytic skin lesions in vivo. Journal of the American Academy of Dermatology 2001;45(3):365‐76. [DOI] [PubMed] [Google Scholar]
Langley 2006 {published data only}
- Langley RG, Burton E, Walsh N, Propperova I, Murray SJ. In vivo confocal scanning laser microscopy of benign lentigines: comparison to conventional histology and in vivo characteristics of lentigo maligna. Journal of the American Academy of Dermatology 2006;55(1):88‐97. [DOI] [PubMed] [Google Scholar]
Langley 2007 {published data only}
- Langley RG, Walsh N, Sutherland AE, Propperova I, Delaney L, Morris SF, et al. The diagnostic accuracy of in vivo confocal scanning laser microscopy compared to dermoscopy of benign and malignant melanocytic lesions: a prospective study. Dermatology 2007;215(4):365‐72. [ER4:15465985; PUBMED: 17912001] [DOI] [PubMed] [Google Scholar]
Losi 2014 {published data only}
- Losi A, Longo C, Cesinaro AM, Benati E, Witkowski A, Guitera P, et al. Hyporeflective pagetoid cells: a new clue for amelanotic melanoma diagnosis by reflectance confocal microscopy. British Journal of Dermatology 2014;171(1):48‐54. [DOI] [PubMed] [Google Scholar]
Lovatto 2015 {published data only}
- Lovatto L, Carrera C, Salerni G, Alos L, Malvehy J, Puig S. In vivo reflectance confocal microscopy of equivocal melanocytic lesions detected by digital dermoscopy follow‐up. Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(10):1918‐25. [ER4:25012311; PUBMED: 25752663] [DOI] [PubMed] [Google Scholar]
Maier 2013 {published data only}
- Maier T, Sattler EC, Braun‐Falco M, Korting HC, Ruzicka T, Berking C. Reflectance confocal microscopy in the diagnosis of partially and completely amelanotic melanoma: report on seven cases. Journal of the European Academy of Dermatology & Venereology 2013;27(1):e42‐52. [DOI] [PubMed] [Google Scholar]
Malvehy 2012 {published data only}
- Malvehy J, Hanke‐Martinez M, Costa J, Salerni G, Carrera C, Puig S. Semiology and pattern analysis in nonmelanocytic lesions. In: Hofmann‐Wellenhof R, Pellacani G, Malvehy J, Soyer HP editor(s). Reflectance Confocal Microscopy for Skin Diseases. Berlin, Heidelberg: Springer Berlin Heidelberg, 2012:239‐52. [Google Scholar]
Menge 2016 {published data only}
- Menge TD, Hibler BP, Cordova MA, Nehal KS, Rossi AM. Concordance of handheld reflectance confocal microscopy (RCM) with histopathology in the diagnosis of lentigo maligna (LM): a prospective study. Journal of the American Academy of Dermatology 2016;74(6):1114‐20. [DOI] [PubMed] [Google Scholar]
Miller 2011 {published data only}
- Miller JH, Chrisler WB, Wang X, Sowa MB. Confocal microscopy for modeling electron microbeam irradiation of skin. Radiation & Environmental Biophysics 2011;50(3):365‐9. [DOI] [PubMed] [Google Scholar]
Nobre Moura 2011 {published data only}
- Nobre Moura F, Dalle S, Depaepe L, Durupt F, Balme B, Thomas L. Melanoma: early diagnosis using in vivo reflectance confocal microscopy. Clinical & Experimental Dermatology 2011;36(2):209‐11. [DOI] [PubMed] [Google Scholar]
Pellacani 2005 {published data only}
- Pellacani G, Cesinaro AM, Seidenari S. Reflectance‐mode confocal microscopy of pigmented skin lesions – improvement in melanoma diagnostic specificity. Journal of the American Academy of Dermatology 2005;53(6):979‐85. [DOI] [PubMed] [Google Scholar]
Pellacani 2007 {published data only}
- Pellacani G, Guitera P, Longo C, Avramidis M, Seidenari S, Menzies S. The impact of in vivo reflectance confocal microscopy for the diagnostic accuracy of melanoma and equivocal melanocytic lesions. Journal of Investigative Dermatology 2007;127(12):2759‐65. [ER4:15466047; PUBMED: 17657243] [DOI] [PubMed] [Google Scholar]
Pellacani 2008 {published data only}
- Pellacani G, Longo C, Malvehy J, Puig S, Carrera C, Segura S, et al. In vivo confocal microscopic and histopathologic correlations of dermoscopic features in 202 melanocytic lesions. Archives of Dermatology 2008;144(12):1597‐608. [DOI] [PubMed] [Google Scholar]
Pellacani 2009 {published data only}
- Pellacani G, Vinceti M, Bassoli S, Braun R, Gonzalez S, Guitera P, et al. Reflectance confocal microscopy and features of melanocytic lesions: an internet‐based study of the reproducibility of terminology. Archives of Dermatology 2009;145(10):1137‐43. [DOI] [PubMed] [Google Scholar]
Pellacani 2012 {published data only}
- Pellacani G, Farnetani F, Gonzalez S, Longo C, Cesinaro AM, Casari A, et al. In vivo confocal microscopy for detection and grading of dysplastic nevi: a pilot study. Journal of the American Academy of Dermatology 2012;66(3):e109‐21. [ER4:15466043; PUBMED: 21742408] [DOI] [PubMed] [Google Scholar]
Peppelman 2013 {published data only}
- Peppelman M, Wolberink EA, Blokx WA, Kerkhof PC, Erp PE, Gerritsen MJ. In vivo diagnosis of basal cell carcinoma subtype by reflectance confocal microscopy. Dermatology 2013;227(3):255‐62. [DOI] [PubMed] [Google Scholar]
Peppelman 2015 {published data only}
- Peppelman M, Nguyen KP, Hoogedoorn L, Erp PE, Gerritsen MJ. Reflectance confocal microscopy: non‐invasive distinction between actinic keratosis and squamous cell carcinoma. Journal of the European Academy of Dermatology & Venereology 2015;29(7):1302‐9. [DOI] [PubMed] [Google Scholar]
Peppelman 2016 {published data only}
- Peppelman M, Nguyen KP, Alkemade HA, Maessen‐Visch B, Hendriks JC, Erp PE, et al. Diagnosis of basal cell carcinoma by reflectance confocal microscopy: study design and protocol of a randomized controlled multicenter trial. JMIR Research Protocols 2016;5(2):e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Puig 2012 {published data only}
- Puig S, Giacomo TB, Serra D, Cabrini F, Alos L, Palou J, et al. Reflectance confocal microscopy of blue nevus. European Journal of Dermatology 2012;22(4):552‐3. [DOI] [PubMed] [Google Scholar]
Pupelli 2013 {published data only}
- Pupelli G, Longo C, Veneziano L, Cesinaro AM, Ferrara G, Piana S, et al. Small‐diameter melanocytic lesions: morphological analysis by means of in vivo confocal microscopy. British Journal of Dermatology 2013;168(5):1027‐33. [ER4:15466070; PUBMED: 23301553] [DOI] [PubMed] [Google Scholar]
Reggiani 2015 {published data only}
- Reggiani C, Manfredini M, Mandel VD, Farnetani F, Ciardo S, Bassoli S, et al. Update on non‐invasive imaging techniques in early diagnosis of non‐melanoma skin cancer. Giornale Italiano di Dermatologia e Venereologia 2015;150(4):393‐405. [PubMed] [Google Scholar]
Rishpon 2009 {published data only}
- Rishpon A, Kim N, Scope A, Porges L, Oliviero MC, Braun RP, et al. Reflectance confocal microscopy criteria for squamous cell carcinomas and actinic keratoses. Archives of Dermatology 2009;145(7):766‐72. [DOI] [PubMed] [Google Scholar]
Röwert‐Huber 2007 {published data only}
- Röwert‐Huber J, Patel MJ, Forschner T, Ulrich C, Eberle J, Kerl H, et al. Actinic keratosis is an early in situ squamous cell carcinoma: a proposal for reclassification. British Journal of Dermatology 2007;156:8‐12. [DOI] [PubMed] [Google Scholar]
Salerni 2011 {published data only}
- Salerni G, Lovatto L, Carrera C, Palou J, Alos L, Puig‐Butille JA, et al. Correlation among dermoscopy, confocal reflectance microscopy, and histologic features of melanoma and basal cell carcinoma collision tumor. Dermatologic Surgery 2011;37(2):275‐9. [DOI] [PubMed] [Google Scholar]
Scope 2009 {published data only}
- Scope A, Mecca PS, Marghoob AA. skINsight lessons in reflectance confocal microscopy: rapid diagnosis of pigmented basal cell carcinoma. Archives of Dermatology 2009;145(1):106‐7. [DOI] [PubMed] [Google Scholar]
Scope 2014 {published data only}
- Scope A, Longo C. Recognizing the benefits and pitfalls of reflectance confocal microscopy in melanoma diagnosis. Dermatology Practical & Conceptual 2014;4(3):67‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Segura 2009 {published data only}
- Segura S, Puig S, Carrera C, Palou J, Malvehy J. Development of a two‐step method for the diagnosis of melanoma by reflectance confocal microscopy. Journal of the American Academy of Dermatology 2009;61(2):216‐29. [ER4:20569494; PUBMED: 19406506] [DOI] [PubMed] [Google Scholar]
Soyer 2013 {published data only}
- Soyer HP, Prow TW. Reflectance confocal microscopy in the diagnosis of nodular skin lesions. British Journal of Dermatology 2013;169(1):4. [DOI] [PubMed] [Google Scholar]
Stanganelli 2015 {published data only}
- Stanganelli I, Longo C, Mazzoni L, Magi S, Medri M, Lanzanova G, et al. Integration of reflectance confocal microscopy in sequential dermoscopy follow‐up improves melanoma detection accuracy. British Journal of Dermatology 2015;172(2):365‐71. [ER4:20569496; PUBMED: 25154446] [DOI] [PubMed] [Google Scholar]
Steiner 1992 {published data only}
- Steiner A, Pehamberger H, Binder M, Wolff K. Pigmented Spitz nevi: improvement of the diagnostic accuracy by epiluminescence microscopy. Journal of the American Academy of Dermatology 1992;27(5 Pt 1):697‐701. [DOI] [PubMed] [Google Scholar]
Stephens 2013 {published data only}
- Stephens A, Fraga‐Braghiroli N, Oliviero M, Rabinovitz H, Scope A. Spoke wheel‐like structures in superficial basal cell carcinoma: a correlation between dermoscopy, histopathology, and reflective confocal microscopy. Journal of the American Academy of Dermatology 2013;69(5):e219‐21. [DOI] [PubMed] [Google Scholar]
Stevenson 2013 {published data only}
- Stevenson AD, Mickan S, Mallett S, Ayya M. Systematic review of diagnostic accuracy of reflectance confocal microscopy for melanoma diagnosis in patients with clinically equivocal skin lesions. Dermatology Practical & Conceptual 2013;3(4):19‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tannous 2009 {published data only}
- Tannous Z, Al‐Arashi M, Shah S, Yaroslavsky AN. Delineating melanoma using multimodal polarized light imaging. Lasers in Surgery & Medicine 2009;41(1):10‐6. [DOI] [PubMed] [Google Scholar]
Willard 2011 {published data only}
- Willard K, Warschaw KE, Swanson DL. Use of reflectance confocal microscopy to differentiate hidrocystoma from basal cell carcinoma. Dermatologic Surgery 2011;37(3):392‐4. [DOI] [PubMed] [Google Scholar]
Xiong 2016 {published data only}
- Xiong YD, Ma S, Li X, Zhong X, Duan C, Chen Q. A meta‐analysis of reflectance confocal microscopy for the diagnosis of malignant skin tumours. Journal of the European Academy of Dermatology & Venereology 2016;30(8):1295‐302. [DOI] [PubMed] [Google Scholar]
Yelamos 2016 {published data only}
- Yelamos O, Nehal KS. Integrating clinical information, dermoscopy and reflectance confocal microscopy to improve the diagnostic accuracy and confidence of amelanotic and lightly pigmented melanomas. British Journal of Dermatology 2016;175(6):1147‐8. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Borsari 2016 {published data only}
- Borsari S, Pampena R, Lallas A, Kyrgidis A, Moscarella E, Benati E, et al. Clinical indications for use of reflectance confocal microscopy for skin cancer diagnosis. JAMA Dermatology 2016;152(10):1093‐8. [PUBMED: 27580185] [DOI] [PubMed] [Google Scholar]
Guitera 2016 {published data only}
- Guitera P, Menzies SW, Argenziano G, Longo C, Losi A, Drummond M, et al. Dermoscopy and in vivo confocal microscopy are complementary techniques for diagnosis of difficult amelanotic and light‐coloured skin lesions. British Journal of Dermatology 2016;175(6):1311‐9. [PUBMED: 27177158 ] [DOI] [PubMed] [Google Scholar]
Jain 2017 {published data only}
- Jain M, Pulijal SV, Rajadhyaksha M. The bedside diagnostic accuracy of a novice reflectance confocal microscopy reader for skin cancer detection in vivo in real‐time: understanding challenges and potential pitfalls. Proceedings of SPIE. 2017; Vol. 10060. [DOI: 10.1117/12.2255685] [DOI]
Ludzik 2016 {published data only}
- Ludzik J, Witkowski AM, Roterman‐Konieczna I, Bassoli S, Farnetani F, Pellacani G. Improving diagnostic accuracy of dermoscopically equivocal pink cutaneous lesions with reflectance confocal microscopy in telemedicine settings: double reader concordance evaluation of 316 cases. PloS One 2016;11(9):e0162495. [PUBMED: 27606812] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Alam 2001
- Alam M, Ratner D. Cutaneous squamous‐cell carcinoma. New England Journal of Medicine 2001;344(13):975‐83. [PUBMED: 11274625] [DOI] [PubMed] [Google Scholar]
Argenziano 1998
- Argenziano G, Fabbrocini G, Carli P, Giorgi V, Sammarco E, Delfino M. Epiluminescence microscopy for the diagnosis of doubtful melanocytic skin lesions. Comparison of the ABCD rule of dermatoscopy and a new 7‐point checklist based on pattern analysis. Archives of Dermatology 1998;134(12):1563‐70. [PUBMED: 9875194] [DOI] [PubMed] [Google Scholar]
Argenziano 2012
- Argenziano G, Albertini G, Castagnetti F, Pace B, Lernia V, Longo C, et al. Early diagnosis of melanoma: what is the impact of dermoscopy?. Dermatologic Therapy 2012;25(5):403‐9. [PUBMED: 23046019] [DOI] [PubMed] [Google Scholar]
Arits 2013
- Arits AH, Mosterd K, Essers BA, Spoorenberg E, Sommer A, Rooij MJ, et al. Photodynamic therapy versus topical imiquimod versus topical fluorouracil for treatment of superficial basal‐cell carcinoma: a single blind, non‐inferiority, randomised controlled trial. Lancet Oncology 2013;14(7):647‐54. [DOI: 10.1016/S1470-2045(13)70143-8; PUBMED: 23683751] [DOI] [PubMed] [Google Scholar]
Baldursson 1993
- Baldursson B, Sigurgeirsson B, Lindelof B. Leg ulcers and squamous cell carcinoma. An epidemiological study and a review of the literature. Acta Dermato‐Venereologica 1993;73(3):171‐4. [PUBMED: 8105611] [DOI] [PubMed] [Google Scholar]
Bath‐Hextall 2007a
- Bath‐Hextall F, Leonardi‐Bee J, Smith C, Meal A, Hubbard R. Trends in incidence of skin basal cell carcinoma. Additional evidence from a UK primary care database study. International Journal of Cancer 2007;121(9):2105‐8. [PUBMED: 17640064] [DOI] [PubMed] [Google Scholar]
Bath‐Hextall 2007b
- Bath‐Hextall FJ, Perkins W, Bong J, Williams HC. Interventions for basal cell carcinoma of the skin. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD003412.pub2] [DOI] [PubMed] [Google Scholar]
Bath‐Hextall 2014
- Bath‐Hextall F, Ozolins M, Armstrong SJ, Colver GB, Perkins W, Miller PS, et al. Surgical excision versus imiquimod 5% cream for nodular and superficial basal‐cell carcinoma (SINS): a multicentre, non‐inferiority, randomised controlled trial. Lancet Oncology 2014;15(1):96‐105. [PUBMED: 24332516] [DOI] [PubMed] [Google Scholar]
Batra 2002
- Batra RS, Kelley LC. A risk scale for predicting extensive subclinical spread of nonmelanoma skin cancer. Dermatologic Surgery 2002;28(2):107‐12; discussion 112. [PUBMED: 11860418] [DOI] [PubMed] [Google Scholar]
Betti 2017
- Betti R, Moneghini L, Mapelli ET, Bulfamante G, Cerri A. Growth rate of different basal cell carcinoma subtypes. European Journal of Dermatology 2017;27(5):544‐5. [PUBMED: 29084641] [DOI] [PubMed] [Google Scholar]
Bossuyt 2015
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015;351:h5527. [DOI: 10.1136/bmj.h5527] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2013
- Carter JB, Johnson MM, Chua TL, Karia PS, Schmults CD. Outcomes of primary cutaneous squamous cell carcinoma with perineural invasion: an 11‐year cohort study. JAMA Dermatology 2013;149(1):35‐41. [DOI: 10.1001/jamadermatol.2013.746; PUBMED: 23324754] [DOI] [PubMed] [Google Scholar]
CCAAC Network 2008
- Cancer Council Australia & Australian Cancer Network. Basal cell carcinoma, squamous cell carcinoma (and related lesions) – a guide to clinical management in Australia, 2008. www.cancer.org.au/content/pdf/HealthProfessionals/ClinicalGuidelines/Basal_cell_carcinoma_Squamous_cell_carcinoma_Guide_Nov_2008‐Final_with_Corrigendums.pdf. Sydney: Cancer Council Australia & Australian Cancer Network, (accessed 19 May 2015).
Chao 2013
- Chao D, London Cancer North and East. London cancer, guidelines for cutaneous malignant melanoma management August 2014. www.londoncancer.org/media/76373/london‐cancer‐melanoma‐guidelines‐2013‐v0.pdf. London: London Cancer North and East Alliance, (accessed 25 February 2015).
Chowdri 1996
- Chowdri NA, Darzi MA. Postburn scar carcinomas in Kashmiris. Burns 1996;22(6):477‐82. [PUBMED: 8884010] [DOI] [PubMed] [Google Scholar]
Chu 2006
- Chu H, Cole S. Bivariate meta‐analysis for sensitivity and specificity with sparse data: a generalized linear mixed model approach (letter to the editor). Journal of Clinical Epidemiology 2006;59(12):1331. [PUBMED: 17098577] [DOI] [PubMed] [Google Scholar]
Chuchu 2018a
- Chuchu N, Dinnes J, Takwoingi Y, Matin RN, Bayliss SE, Davenport C, et al. Teledermatology for diagnosing skin cancer in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013193] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chuchu 2018b
- Chuchu N, Takwoingi Y, Dinnes J, Matin RN, Bassett O, Moreau JF, et al. Smartphone applications for triaging adults with skin lesions that are suspicious for melanoma. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013192] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dabski 1986
- Dabski K, Stoll HL Jr, Milgrom H. Squamous cell carcinoma complicating late chronic discoid lupus erythematosus. Journal of Surgical Oncology 1986;32(4):233‐7. [PUBMED: 3736067] [DOI] [PubMed] [Google Scholar]
Deeks 2005
- Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. Journal of Clinical Epidemiology 2005;58(9):882‐93. [PUBMED: 16085191] [DOI] [PubMed] [Google Scholar]
Deeks 2013
- Deeks JJ, Bossuyt PM, Gatsonis C, editor(s). Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration, 2013. Available from srdta.cochrane.org.
Dinnes 2018a
- Dinnes J, Deeks JJ, Saleh D, Chuchu N, Bayliss SE, Patel L, et al. Reflectance confocal microscopy for diagnosing cutaneous melanoma in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013190] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinnes 2018b
- Dinnes J, Deeks JJ, Chuchu N, Matin RN, Wong KY, Aldridge RB, et al. Visual inspection and dermoscopy, alone or in combination, for diagnosing keratinocyte skin cancers in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD011901.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinnes 2018c
- Dinnes J, Bamber J, Chuchu N, Bayliss SE, Takwoingi Y, Davenport C, et al. High‐frequency ultrasound for diagnosing skin cancer in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013188] [DOI] [PMC free article] [PubMed] [Google Scholar]
Drew 2017
- Drew BA, Karia PS, Mora AN, Liang CA, Schmults CD. Treatment patterns, outcomes, and patient satisfaction of primary epidermally limited nonmelanoma skin cancer. Dermatologic Surgery 2017;43(12):1423‐30. [DOI: 10.1097/DSS.0000000000001225; PUBMED: 28661992] [DOI] [PubMed] [Google Scholar]
Drucker 2017
- Drucker A, Adam GP, Langberg V, Gazula A, Smith B, Moustafa F, et al. Treatments for Basal Cell and Squamous Cell Carcinoma of the Skin. Comparative Effectiveness Reviews, No. 199. Rockville (MD): Agency for Healthcare Research and Quality (US), 2017. [PubMed] [Google Scholar]
Efron 1983
- Efron B. Estimating the error rate of a prediction rule: improvement on cross‐validation. Journal of the American Statistical Association 1983;78(382):316‐31. [DOI: 10.1080/01621459.1983.10477973] [DOI] [Google Scholar]
Esteva 2017
- Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist‐level classification of skin cancer with deep neural networks. Nature 2017;542(7639):115‐8. [PUBMED: 28117445] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fasching 1989
- Fasching MC, Meland NB, Woods JE, Wolff BG. Recurrent squamous‐cell carcinoma arising in pilonidal sinus tract – multiple flap reconstructions. Report of a case. Diseases of the Colon & Rectum 1989;32(2):153‐8. [PUBMED: 2914529] [DOI] [PubMed] [Google Scholar]
Ferrante di Ruffano 2018a
- Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C, et al. Computer‐assisted diagnosis techniques (dermoscopy and spectroscopy‐based) for diagnosing skin cancer in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013186] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferrante di Ruffano 2018b
- Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C, et al. Optical coherence tomography for diagnosing skin cancer in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013189] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferrante di Ruffano 2018c
- Ferrante di Ruffano L, Dinnes J, Chuchu N, Bayliss SE, Takwoingi Y, Davenport C, et al. Exfoliative cytology for diagnosing basal cell carcinoma and other skin cancers in adults. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD013187] [DOI] [PMC free article] [PubMed] [Google Scholar]
Firnhaber 2012
- Firnhaber JM. Diagnosis and treatment of basal cell and squamous cell carcinoma. American Family Physician 2012;86(2):161‐8. [PUBMED: 22962928] [PubMed] [Google Scholar]
Fitzpatrick 1975
- Fitzpatrick TB. Soleil et peau. Journal de Médecine Esthétique 1975;2:33‐4. [Google Scholar]
Flohil 2013
- Flohil SC, Leest RJ, Arends LR, Vries E, Nijsten T. Risk of subsequent cutaneous malignancy in patients with prior keratinocyte carcinoma: a systematic review and meta‐analysis. European Journal of Cancer 2013;49(10):2365‐75. [PUBMED: 23608733] [DOI] [PubMed] [Google Scholar]
Friedman 1985
- Friedman HI, Cooper PH, Wanebo HJ. Prognostic and therapeutic use of microstaging of cutaneous squamous cell carcinoma of the trunk and extremities. Cancer 1985;56(5):1099‐105. [PUBMED: 4016700] [DOI] [PubMed] [Google Scholar]
Gambichler 2015
- Gambichler T, Schmid‐Wendtner MH, Plura I, Kampilafkos P, Stucker M, Berking C, et al. A multicentre pilot study investigating high‐definition optical coherence tomography in the differentiation of cutaneous melanoma and melanocytic naevi. Journal of the European Academy of Dermatology & Venereology 2015;29(3):537‐41. [PUBMED: 25073788] [DOI] [PubMed] [Google Scholar]
Garcia 2009
- Garcia C, Poletti E, Crowson AN. Basosquamous carcinoma. Journal of the American Acadademy of Dermatology 2009;60(1):137‐43. [PUBMED: 19103364] [DOI] [PubMed] [Google Scholar]
Gerbert 2000
- Gerbert B, Bronstone A, Maurer T, Hofmann R, Berger T. Decision support software to help primary care physicians triage skin cancer: a pilot study. Archives of Dermatology 2000;136(2):187‐92. [PUBMED: 10677094] [DOI] [PubMed] [Google Scholar]
Gordon 2013
- Gordon R. Skin cancer: an overview of epidemiology and risk factors. Seminars in Oncology Nursing 2013;29(3):160‐9. [PUBMED: 23958214] [DOI] [PubMed] [Google Scholar]
Gorlin 2004
- Gorlin RJ. Nevoid basal cell carcinoma (Gorlin) syndrome. Genetics in Medicine 2004;6(6):530‐9. [PUBMED: 15545751] [DOI] [PubMed] [Google Scholar]
Grachtchouk 2011
- Grachtchouk M, Pero J, Yang SH, Ermilov AN, Michael LE, Wang A, et al. Basal cell carcinomas in mice arise from hair follicle stem cells and multiple epithelial progenitor populations. Journal of Clinical Investigation 2011;121(5):1768‐81. [PUBMED: 21519145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Green 1988
- Green A, Leslie D, Weedon D. Diagnosis of skin cancer in the general population: clinical accuracy in the Nambour survey. Medical Journal of Australia 1988;148(9):447‐50. [PUBMED: 3283506] [DOI] [PubMed] [Google Scholar]
Griffin 2016
- Griffin LL, Ali FR, Lear JT. Non‐melanoma skin cancer. Clinical Medicine 2016;16(1):62‐5. [PUBMED: 26833519] [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffiths 2005
- Griffiths RW, Suvarna SK, Stone J. Do basal cell carcinomas recur after complete conventional surgical excision?. British Journal of Plastic Surgery 2005;58(6):795‐805. [PUBMED: 16086990] [DOI] [PubMed] [Google Scholar]
Grob 1998
- Grob JJ, Bonerandi JJ. The 'ugly duckling' sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Archives of Dermatology 1998;134(1):103‐4. [PUBMED: 9449921] [DOI] [PubMed] [Google Scholar]
Guitera 2017
- Guitera P, Menzies S, Chamberlain A, Soyer P, Cancer Council Australia Melanoma Guidelines Working Party. What is the role of confocal microscopy in melanoma diagnosis?. www.wiki.cancer.org.au/australia/Guidelines:Melanoma/Confocal_microscopy (accessed prior to 28 November 2017).
Haenssle 2010
- Haenssle HA, Korpas B, Hansen‐Hagge C, Buhl T, Kaune KM, Rosenberger A, et al. Seven‐point checklist for dermatoscopy: performance during 10 years of prospective surveillance of patients at increased melanoma risk. Journal of the American Academy of Dermatology 2010;62(5):785‐93. [PUBMED: 20226567] [DOI] [PubMed] [Google Scholar]
Harland 2000
- Harland CC, Kale SG, Jackson P, Mortimer PS, Bamber JC. Differentiation of common benign pigmented skin lesions from melanoma by high‐resolution ultrasound. British Journal of Dermatology 2000;143(2):281‐9. [PUBMED: 10951134] [DOI] [PubMed] [Google Scholar]
Hartevelt 1990
- Hartevelt MM, Bavinck JN, Kootte AM, Vermeer BJ, Vandenbroucke JP. Incidence of skin cancer after renal transplantation in The Netherlands. Transplantation 1990;49(3):506‐9. [PUBMED: 2316011] [DOI] [PubMed] [Google Scholar]
Hauschild 2014
- Hauschild A, Chen SC, Weichenthal M, Blum A, King HC, Goldsmith J, et al. To excise or not: impact of MelaFind on German dermatologists' decisions to biopsy atypical lesions. Journal der Deutschen Dermatologischen Gesellschaft 2014;12(7):606‐14. [PUBMED: 24944011] [DOI] [PubMed] [Google Scholar]
Hoorens 2016
- Hoorens I, Vossaert K, Pil L, Boone B, Schepper S, Ongenae K, et al. Total‐body examination vs lesion‐directed skin cancer screening. JAMA Dermatology 2016;152(1):27‐34. [DOI] [PubMed] [Google Scholar]
Jansen 2018
- Jansen MH, Mosterd K, Arits AH, Roozeboom MH, Sommer A, Essers BA, et al. Five‐year results of a randomized controlled trial comparing effectiveness of photodynamic therapy, topical imiquimod, and topical 5‐fluorouracil in patients with superficial basal cell carcinoma. Journal of Investigative Dermatology 2018;138(3):527‐33. [DOI: 10.1016/j.jid.2017.09.033; PUBMED: 29045820] [DOI] [PubMed] [Google Scholar]
Jensen 1999
- Jensen P, Hansen S, Moller B, Leivestad T, Pfeffer P, Geiran O, et al. Skin cancer in kidney and heart transplant recipients and different long‐term immunosuppressive therapy regimens. Journal of the American Academy of Dermatology 1999;40(2 Pt 1):177‐86. [PUBMED: 10025742] [DOI] [PubMed] [Google Scholar]
Kao 1986
- Kao GF. Carcinoma arising in Bowen's disease. Archives of Dermatology 1986;122(10):1124‐6. [PUBMED: 3767398] [PubMed] [Google Scholar]
Karimkhani 2015
- Karimkhani C, Boyers LN, Dellavalle RP, Weinstock MA. It's time for "keratinocyte carcinoma" to replace the term "nonmelanoma skin cancer". Journal of the American Academy of Dermatology 2015;72(1):186‐7. [PUBMED: 25497921] [DOI] [PubMed] [Google Scholar]
Kelleners‐Smeets 2017
- Kelleners‐Smeets NW, Mosterd K, Nelemans PJ. Treatment of low‐risk basal cell carcinoma. Journal of Investigative Dermatology 2017;137(3):539‐40. [PUBMED: 28235442] [DOI] [PubMed] [Google Scholar]
Kim 2014
- Kim DD, Tang JY, Ioannidis JP. Network geometry shows evidence sequestration for medical vs. surgical practices: treatments for basal cell carcinoma. Journal of Clinical Epidemiology 2014;67(4):391‐400. [PUBMED: 24491794] [DOI] [PubMed] [Google Scholar]
Kittler 2002
- Kittler H, Pehamberger H, Wolff K, Binder M. Diagnostic accuracy of dermoscopy (review). Lancet Oncology 2002;3(3):159‐65. [PUBMED: 11902502] [DOI] [PubMed] [Google Scholar]
Kleinerman 2012
- Kleinerman R, Whang TB, Bard RL, Marmur ES. Ultrasound in dermatology: principles and applications. Journal of the American Academy of Dermatology 2012;67(3):478‐87. [PUBMED: 22285673] [DOI] [PubMed] [Google Scholar]
Lansbury 2010
- Lansbury L, Leonardi‐Bee J, Perkins W, Goodacre T, Tweed JA, Bath‐Hextall FJ. Interventions for non‐metastatic squamous cell carcinoma of the skin. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD007869.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lansbury 2013
- Lansbury L, Bath‐Hextall F, Perkins W, Stanton W, Leonardi‐Bee J. Interventions for non‐metastatic squamous cell carcinoma of the skin: systematic review and pooled analysis of observational studies. BMJ 2013;347:f6153. [PUBMED: 24191270] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lear 1997
- Lear JT, Tan BB, Smith AG, Bowers W, Jones PW, Heagerty AH, et al. Risk factors for basal cell carcinoma in the UK: case‐control study in 806 patients. Journal of the Royal Society of Medicine 1997;90(7):371‐4. [PUBMED: 9290417] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lear 2012
- Lear JT. Oral hedgehog‐pathway inhibitors for basal‐cell carcinoma. New England Journal of Medicine 2012;366(23):2225‐6. [PUBMED: 22670909] [DOI] [PubMed] [Google Scholar]
Lederman 1985
- Lederman JS, Sober AJ. Does biopsy type influence survival in clinical stage I cutaneous melanoma?. Journal of the American Academy of Dermatology 1985;13(6):983‐7. [PUBMED: 4078105] [DOI] [PubMed] [Google Scholar]
Lees 1991
- Lees VC, Briggs JC. Effect of initial biopsy procedure on prognosis in stage I invasive cutaneous malignant melanoma: review of 1086 patients. British Journal of Surgery 1991;78(9):1108‐10. [PUBMED: 1933198] [DOI] [PubMed] [Google Scholar]
Lister 1997
- Lister RK, Black MM, Calonje E, Burnand KG. Squamous cell carcinoma arising in chronic lymphoedema. British Journal of Dermatology 1997;136(3):384‐7. [PUBMED: 9115922] [PubMed] [Google Scholar]
Lo 1991
- Lo JS, Snow SN, Reizner GT, Mohs FE, Larson PO, Hruza GJ. Metastatic basal cell carcinoma: report of twelve cases with a review of the literature. Journal of the American Academy of Dermatology 1991;24(5 Pt 1):715‐9. [PUBMED: 1869642] [DOI] [PubMed] [Google Scholar]
Lomas 2012
- Lomas A, Leonardi‐Bee J, Bath‐Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. British Journal of Dermatology 2012;166(5):1069‐80. [PUBMED: 22251204] [DOI] [PubMed] [Google Scholar]
London Cancer Alliance 2013
- London Cancer Alliance. Guidelines for the treatment and referral of squamous cell carcinoma (SCC) of the skin. www.londoncancer.org/media/76391/london‐cancer‐scc‐guidelines‐2013‐v1.0.pdf. London: London Cancer Alliance, (accessed prior to 25 May 2018).
Longo 2011
- Longo C, Rito C, Beretti F, Cesinaro AM, Piñeiro‐Maceira J, Seidenari S, et al. De novo melanoma and melanoma arising from pre‐existing nevus: in vivo morphologic differences as evaluated by confocal microscopy. Journal of the American Academy of Dermatology 2011;65(3):604‐14. [PUBMED: 21715047] [DOI] [PubMed] [Google Scholar]
MacKie 1985
- MacKie RM, English J, Aitchison TC, Fitzsimons CP, Wilson P. The number and distribution of benign pigmented moles (melanocytic naevi) in a healthy British population. British Journal of Dermatology 1985;113(2):167‐74. [PUBMED: 4027184] [DOI] [PubMed] [Google Scholar]
MacKie 1990
- MacKie RM. Clinical recognition of early invasive malignant melanoma. BMJ 1990;301(6759):1005‐6. [PUBMED: 2249043] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madan 2010
- Madan V, Lear JT, Szeimies RM. Non‐melanoma skin cancer. Lancet 2010;375(9715):673‐85. [PUBMED: 20171403] [DOI] [PubMed] [Google Scholar]
Maia 1995
- Maia M, Proenca NG, Moraes JC. Risk factors for basal cell carcinoma: a case‐control study. Revista de Saude Publica 1995;29(1):27‐37. [PUBMED: 8525311] [DOI] [PubMed] [Google Scholar]
Maloney 1996
- Maloney ME. Arsenic in dermatology. Dermatologic Surgery 1996;22(3):301‐4. [PUBMED: 8599743] [DOI] [PubMed] [Google Scholar]
Malvehy 2014
- Malvehy J, Hauschild A, Curiel‐Lewandrowski C, Mohr P, Hofmann‐Wellenhof R, Motley R, et al. Clinical performance of the Nevisense system in cutaneous melanoma detection: an international, multicentre, prospective and blinded clinical trial on efficacy and safety. British Journal of Dermatology 2014;171(5):1099‐107. [PUBMED: 24841846] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marsden 2010
- Marsden JR, Newton‐Bishop JA, Burrows L, Cook M, Corrie PG, Cox NH, et al. BAD guidelines: revised UK guidelines for the management of cutaneous melanoma 2010. British Journal of Dermatology 2010;163(2):238‐56. [PUBMED: 20608932] [DOI] [PubMed] [Google Scholar]
McCormack 1997
- McCormack CJ, Kelly JW, Dorevitch AP. Differences in age and body site distribution of the histological subtypes of basal cell carcinoma. A possible indicator of differing causes. Archives of Dermatology 1997;133(5):593‐6. [PUBMED: 9158412] [PubMed] [Google Scholar]
McCusker 2014
- McCusker M, Basset‐Seguin N, Dummer R, Lewis K, Schadendorf D, Sekulic A, et al. Metastatic basal cell carcinoma: prognosis dependent on anatomic site and spread of disease. European Journal of Cancer 2014;50(4):774‐83. [PUBMED: 24412051] [DOI] [PubMed] [Google Scholar]
Moeckelmann 2018
- Moeckelmann N, Ebrahimi A, Dirven R, Liu J, Low TH, Gupta R, et al. Analysis and comparison of the 8th Edition American Joint Committee on Cancer (AJCC) nodal staging system in cutaneous and oral squamous cell cancer of the head and neck. Annals of Surgical Oncology 2018;25(6):1730‐6. [DOI: 10.1245/s10434-018-6340-x; PUBMED: 29352431] [DOI] [PubMed] [Google Scholar]
Mogensen 2007
- Mogensen M, Jemec GB. Diagnosis of nonmelanoma skin cancer/keratinocyte carcinoma: a review of diagnostic accuracy of nonmelanoma skin cancer diagnostic tests and technologies.. Dermatologic Surgery 2007;33(10):1158‐74. [PUBMED: 17903149] [DOI] [PubMed] [Google Scholar]
Moncrieff 2002
- Moncrieff M, Cotton S, Claridge E, Hall P. Spectrophotometric intracutaneous analysis: a new technique for imaging pigmented skin lesions. British Journal of Dermatology 2002;146(3):448‐57. [PUBMED: 11952545] [DOI] [PubMed] [Google Scholar]
Monheit 2011
- Monheit G, Cognetta AB, Ferris L, Rabinovitz H, Gross K, Martini M, et al. The performance of MelaFind: a prospective multicenter study. Archives of Dermatology 2011;147(2):188‐94. [PUBMED: 20956633] [DOI] [PubMed] [Google Scholar]
Motley 2009
- Motley RJ, Preston PW, Lawrence CM. Multi‐professional guidelines for the management of the patient with primary cutaneous squamous cell carcinoma. www.bad.org.uk/healthcare‐professionals/clinical‐standards/clinical‐guidelines/scc (accessed prior to 28 November 2017).
Murchie 2017
- Murchie P, Amalraj Raja E, Brewster DH, Iversen L, Lee AJ. Is initial excision of cutaneous melanoma by general practitioners (GPs) dangerous? Comparing patient outcomes following excision of melanoma by GPs or in hospital using national datasets and meta‐analysis. European Journal of Cancer 2017;86:373‐84. [PUBMED: 29100192] [DOI] [PubMed] [Google Scholar]
Musah 2013
- Musah A, Gibson JE, Leonardi‐Bee J, Cave MR, Ander EL, Bath‐Hextall F. Regional variations of basal cell carcinoma incidence in the U.K. using The Health Improvement Network database (2004‐10). British Journal of Dermatology 2013;169(5):1093‐9. [PUBMED: 23701520] [DOI] [PubMed] [Google Scholar]
Nart 2015
- Nart IF, Armayones SG, Medina FV, Orti MB, Orpinell XB. Basal cell carcinoma treated with ingenol mebutate. Journal of the American Academy of Dermatology 2015;5(Suppl 1):AB180. [Google Scholar]
Nascimento 2014
- Nascimento MM, Shitara D, Enokihara MM, Yamada S, Pellacani G, Rezze GG. Inner gray halo, a novel dermoscopic feature for the diagnosis of pigmented actinic keratosis: clues for the differential diagnosis with lentigo maligna. Journal of the American Academy of Dermatology 2014;71(4):708‐15. [PUBMED: 24947988] [DOI] [PubMed] [Google Scholar]
NICE 2010
- National Institute for Health and Clinical Excellence. NICE guidance on cancer services. Improving outcomes for people with skin tumours including melanoma (update). www.nice.org.uk/guidance/csgstim. NICE, (accessed 19 May 2015).
NICE 2015
- National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. www.nice.org.uk/guidance/ng12. London: National Institute for Health and Clinical Excellence, (accessed prior to 25 May 2018).
NICE 2017
- National Institute for Health and Care Excellence. Vismodegib for treating basal cell carcinoma. www.nice.org.uk/guidance/ta489. London: NICE, (accessed prior to 25 May 2018).
Norman 2009
- Norman G, Barraclough K, Dolovich L, Price D. Iterative diagnosis. BMJ 2009;339:b3490. [DOI: 10.1136/bmj.b3490] [DOI] [PubMed] [Google Scholar]
O'Gorman 2014
- O'Gorman SM, Murphy GM. Photosensitizing medications and photocarcinogenesis. Photodermatology, Photoimmunology & Photomedicine 2014;30(1):8‐14. [PUBMED: 24393207] [DOI] [PubMed] [Google Scholar]
Offidani 2002
- Offidani A, Simonetti O, Bernardini ML, Alpagut A, Cellini A, Bossi G. General practitioners' accuracy in diagnosing skin cancers. Dermatology 2002;205(2):127‐30. [PUBMED: 12218226] [DOI] [PubMed] [Google Scholar]
Olsen 2015
- Olsen J, Themstrup L, Jemec GB. Optical coherence tomography in dermatology. Giornale Italiano di Dermatologia e Venereologia 2015;150(5):603‐15. [PUBMED: 26129683] [PubMed] [Google Scholar]
Pellacani 2014
- Pellacani G, Pepe P, Casari A, Longo C. Reflectance confocal microscopy as a second‐level examination in skin oncology improves diagnostic accuracy and saves unnecessary excisions: a longitudinal prospective study. British Journal of Dermatology 2014;171(5):1044‐51. [PUBMED: 24891083] [DOI] [PubMed] [Google Scholar]
Rajadhyaksha 1995
- Rajadhyaksha M, Grossman M, Esterowitz D, Webb RH, Anderson RR. In vivo confocal scanning laser microscopy of human skin: melanin provides strong contrast. Journal of Investigative Dermatology 1995;104(6):946‐52. [PUBMED: 7769264] [DOI] [PubMed] [Google Scholar]
Rajadhyaksha 2017
- Rajadhyaksha M, Marghoob A, Rossi A, Halpern AC, Nehal KS. Reflectance confocal microscopy of skin in vivo: from bench to bedside. Lasers in Surgery and Medicine 2017;49(1):7‐19. [PUBMED: 27785781] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rajpara 2009
- Rajpara SM, Botello AP, Townend J, Ormerod AD. Systematic review of dermoscopy and digital dermoscopy/artificial intelligence for the diagnosis of melanoma. British Journal of Dermatology 2009;161(3):591‐604. [PUBMED: 19302072] [DOI] [PubMed] [Google Scholar]
Randle 1996
- Randle HW. Basal cell carcinoma. Identification and treatment of the high‐risk patient. Dermatologic Surgery 1996;22(3):255‐61. [PUBMED: 8599737] [DOI] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58(10):982‐90. [PUBMED: 16168343] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roozeboom 2012
- Roozeboom MH, Arits AH, Nelemans PJ, Kelleners‐Smeets NW. Overall treatment success after treatment of primary superficial basal cell carcinoma: a systematic review and meta‐analysis of randomized and nonrandomized trials. British Journal of Dermatology 2012;167(4):733‐56. [PUBMED: 22612571] [DOI] [PubMed] [Google Scholar]
Roozeboom 2016
- Roozeboom MH, Arits AH, Mosterd K, Sommer A, Essers BA, Rooij MJ, et al. Three‐year follow‐up results of photodynamic therapy vs. imiquimod vs. fluorouracil for treatment of superficial basal cell carcinoma: a single‐blind, noninferiority, randomized controlled trial. Journal of Investigative Dermatology 2016;136(8):1568‐74. [PUBMED: 27113429] [DOI] [PubMed] [Google Scholar]
Royal College of Pathologists 2014
- Royal College of Pathologists. Standards and datasets for reporting cancers. Dataset for the histological reporting of primary invasive cutaneous squamous cell carcinoma and regional lymph nodes. www.rcpath.org/Resources/RCPath/Migrated%20Resources/Documents/G/G124_DatasetSquamous_May14.pdf. London: Royal College of Pathologists, (accessed 19 May 2015).
Rutjes 2005
- Rutjes AW, Reitsma JB, Vandenbroucke JP, Glas AS, Bossuyt PM. Case‐control and two‐gate designs in diagnostic accuracy studies. Clinical Chemistry 2005;51(8):1335‐41. [PUBMED: 15961549] [DOI] [PubMed] [Google Scholar]
Rutjes 2006
- Rutjes AW, Reitsma JB, Nisio M, Smidt N, Rijn JC, Bossuyt PM. Evidence of bias and variation in diagnostic accuracy studies. CMAJ 2006;174(4):469‐76. [PUBMED: 16477057] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sekulic 2012
- Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, et al. Efficacy and safety of vismodegib in advanced basal‐cell carcinoma. New England Journal of Medicine 2012;366(23):2171‐9. [PUBMED: 22670903] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smeets 2004
- Smeets NW, Krekels GA, Ostertag JU, Essers BA, Dirksen CD, Nieman FH, et al. Surgical excision vs Mohs' micrographic surgery for basal‐cell carcinoma of the face: randomised controlled trial. Lancet 2004;364(9447):1766‐72. [PUBMED: 15541449] [DOI] [PubMed] [Google Scholar]
Sobarun 2015
- Sobarun P. Reflectance confocal microscopy. www.dermnetnz.org/topics/reflectance‐confocal‐microscopy/ (accessed 18 May 2017).
Sober 1979
- Sober AJ, Fitzpatrick TB, Mihm MC, Wise TG, Pearson BJ, Clark WH, et al. Early recognition of cutaneous melanoma. JAMA 1979;242(25):2795‐9. [PUBMED: 501893] [PubMed] [Google Scholar]
Stratigos 2015
- Stratigos A, Garbe C, Lebbe C, Malvehy J, Marmol V, Pehamberger H, et al. Diagnosis and treatment of invasive squamous cell carcinoma of the skin: European consensus‐based interdisciplinary guideline. European Journal of Cancer 2015;51(14):1989‐2007. [PUBMED: 26219687] [DOI] [PubMed] [Google Scholar]
Takwoingi 2013
- Takwoingi Y, Leeflang MM, Deeks JJ. Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Annals of Internal Medicine 2013;158(7):544‐54. [PUBMED: 23546566] [DOI] [PubMed] [Google Scholar]
Takwoingi 2017
- Takwoingi Y, Guo B, Riley RD, Deeks JJ. Performance of methods for meta‐analysis of diagnostic test accuracy with few studies or sparse data. Statistical Methods in Medical Research 2017;26(4):1896‐911. [DOI: 10.1177/0962280215592269; PUBMED: 26116616] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 1998
- Thomas L, Tranchand P, Berard F, Secchi T, Colin C, Moulin G. Semiological value of ABCDE criteria in the diagnosis of cutaneous pigmented tumors. Dermatology 1998;197(1):11‐7. [PUBMED: 9693179] [DOI] [PubMed] [Google Scholar]
van Loo 2014
- Loo E, Mosterd K, Krekels GA, Roozeboom MH, Ostertag JU, Dirksen CD, et al. Surgical excision versus Mohs' micrographic surgery for basal cell carcinoma of the face: a randomised clinical trial with 10 year follow‐up. European Journal of Cancer 2014;50(17):3011‐20. [PUBMED: 25262378] [DOI] [PubMed] [Google Scholar]
Verkouteren 2017
- Verkouteren JA, Ramdas KH, Wakkee M, Nijsten T. Epidemiology of basal cell carcinoma: scholarly review. British Journal of Dermatology 2017;177(2):359‐72. [DOI: 10.1111/bjd.15321.; PUBMED: 28220485] [DOI] [PubMed] [Google Scholar]
Walker 2006
- Walker P, Hill D. Surgical treatment of basal cell carcinomas using standard postoperative histological assessment. Australasian Journal of Dermatology 2006;47(1):1‐12. [PUBMED: 16405477] [DOI] [PubMed] [Google Scholar]
Walter 2012
- Walter FM, Morris HC, Humphrys E, Hall PN, Prevost AT, Burrows N, et al. Effect of adding a diagnostic aid to best practice to manage suspicious pigmented lesions in primary care: randomised controlled trial. BMJ 2012;345:e4110. [PUBMED: 22763392] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wells 2012
- Wells R, Gutkowicz‐Krusin D, Veledar E, Toledano A, Chen SC. Comparison of diagnostic and management sensitivity to melanoma between dermatologists and MelaFind: a pilot study. Archives of Dermatology 2012;148(9):1083‐4. [PUBMED: 22986873] [DOI] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529‐36. [PUBMED: 22007046] [DOI] [PubMed] [Google Scholar]
WHO 2003
- World Health Organization. INTERSUN: the Global UV Project. A guide and compendium. www.who.int/uv/publications/en/Intersunguide.pdf. Geneva: World Health Organisation, (accessed 20 May 2015).
Williams 2017
- Williams HC, Bath‐Hextall F, Ozolins M, Armstrong SJ, Colver GB, Perkins W, et al. Surgery versus 5% imiquimod for nodular and superficial basal cell carcinoma: 5‐year results of the SINS randomized controlled trial. Journal of Investigative Dermatology 2017;137(3):614‐9. [DOI: 10.1016/j.jid.2016.10.019; PUBMED: 27932240] [DOI] [PubMed] [Google Scholar]
Wong 2017
- Wong KY, Fife K, Lear JT, Price RD, Durrani AJ. Vismodegib for locally advanced periocular and orbital basal cell carcinoma: a review of 15 consecutive cases. Plastic and Reconstructive Surgery 2017;5(7):e1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zak‐Prelich 2004
- Zak‐Prelich M, Narbutt J, Sysa‐Jedrzejowska A. Environmental risk factors predisposing to the development of basal cell carcinoma. Dermatologic Surgery 2004;30(2 Pt 2):248‐52. [PUBMED: 14871217] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Dinnes 2015a
- Dinnes J, Wong KY, Gulati A, Chuchu N, Leonardi‐Bee J, Bayliss SE, et al. Tests to assist in the diagnosis of keratinocyte skin cancers in adults: a generic protocol. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD011901] [DOI] [Google Scholar]
Dinnes 2015b
- Dinnes J, Matin RN, Moreau JF, Patel L, Chan SA, Wong KY, et al. Tests to assist in the diagnosis of cutaneous melanoma in adults: a generic protocol. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD011902] [DOI] [Google Scholar]


