Abstract
Background
Central venous catheters can help with diagnosis and treatment of the critically ill. The catheter may be placed in a large vein in the neck (internal jugular vein), upper chest (subclavian vein) or groin (femoral vein). Whilst this is beneficial overall, inserting the catheter risks arterial puncture and other complications and should be performed in as few attempts as possible.
In the past, anatomical ‘landmarks’ on the body surface were used to find the correct place to insert these catheters, but ultrasound imaging is now available. A Doppler mode is sometimes used to supplement plain ‘two‐dimensional’ ultrasound.
Objectives
The primary objective of this review was to evaluate the effectiveness and safety of two‐dimensional ultrasound (US)‐ or Doppler ultrasound (USD)‐guided puncture techniques for subclavian vein, axillary vein and femoral vein puncture during central venous catheter insertion in adults and children. We assessed whether there was a difference in complication rates between traditional landmark‐guided and any ultrasound‐guided central vein puncture.
When possible, we also assessed the following secondary objectives: whether a possible difference could be verified with use of the US technique versus the USD technique; whether there was a difference between using ultrasound throughout the puncture ('direct') and using it only to identify and mark the vein before starting the puncture procedure ('indirect'); and whether these possible differences might be evident in different groups of patients or with different levels of experience among those inserting the catheters.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 1), MEDLINE (1966 to 15 January 2013), EMBASE (1966 to 15 January 2013), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 15 January 2013), reference lists of articles, 'grey literature' and dissertations. An additional handsearch focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings. We attempted to identify unpublished or ongoing studies by contacting companies and experts in the field, and we searched trial registers. We reran the search in August 2014. We will deal with any studies of interest when we update the review.
Selection criteria
Randomized and quasi‐randomized controlled trials comparing two‐dimensional ultrasound or Doppler ultrasound versus an anatomical ‘landmark’ technique during insertion of subclavian or femoral venous catheters in both adults and children.
Data collection and analysis
Three review authors independently extracted data on methodological quality, participants, interventions and outcomes of interest using a standardized form. We performed a priori subgroup analyses.
Main results
Altogether 13 studies enrolling 2341 participants (and involving 2360 procedures) fulfilled the inclusion criteria. The quality of evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most of the trials had unclear risk of bias across the six domains, and heterogeneity among the studies was significant.
For the subclavian vein (nine studies, 2030 participants, 2049 procedures), two‐dimensional ultrasound reduced the risk of inadvertent arterial puncture (three trials, 498 participants, risk ratio (RR) 0.21, 95% confidence interval (CI) 0.06 to 0.82; P value 0.02, I² = 0%) and haematoma formation (three trials, 498 participants, RR 0.26, 95% CI 0.09 to 0.76; P value 0.01, I² = 0%). No evidence was found of a difference in total or other complications (together, US, USD), overall (together, US, USD), number of attempts until success (US) or first‐time (US) success rates or time taken to insert the catheter (US).
For the femoral vein, fewer data were available for analysis (four studies, 311 participants, 311 procedures). No evidence was found of a difference in inadvertent arterial puncture or other complications. However, success on the first attempt was more likely with ultrasound (three trials, 224 participants, RR 1.73, 95% CI 1.34 to 2.22; P value < 0.0001, I² = 31%), and a small increase in the overall success rate was noted (RR 1.11, 95% CI 1.00 to 1.23; P value 0.06, I² = 50%). No data on mortality or participant‐reported outcomes were provided.
Authors' conclusions
On the basis of available data, we conclude that two‐dimensional ultrasound offers small gains in safety and quality when compared with an anatomical landmark technique for subclavian (arterial puncture, haematoma formation) or femoral vein (success on the first attempt) cannulation for central vein catheterization. Data on insertion by inexperienced or experienced users, or on patients at high risk for complications, are lacking. The results for Doppler ultrasound techniques versus anatomical landmark techniques are uncertain.
Plain language summary
Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization
People who are critically ill sometimes need a central venous catheter to help with diagnosis and treatment. The catheter may be placed in a large vein in the neck (internal jugular vein), upper chest (subclavian/axillary vein) or groin (femoral vein). However, this procedure carries risks such as arterial puncture and other complications and should be performed with as few attempts as possible. Traditionally, anatomical ‘landmarks’ on the body surface were used to find the correct place to insert catheters, but ultrasound imaging is now available.
This Cochrane systematic review compared landmark techniques versus ultrasound guidance. The evidence is current to´January 2013. We included in the review 13 studies enrolling 2341 participants (and involving 2360 procedures). The studies were varied, and their quality was not high. We reran the search in August 2014. We will deal with any studies of interest when we update the review. Nevertheless, ultrasound offered some benefits, as it reduced the risk of arterial puncture and severe bruising in subclavian vein catheterization. Fewer data were available for femoral vein catheterization, but success rates seemed to be higher with ultrasound. No evidence showed a significant difference in complication rates or in time taken to cannulate at either site.
On the basis of available data, we conclude that two‐dimensional ultrasound offers small advantages in safety and quality when compared with an anatomical landmark technique for subclavian vein (reduced arterial puncture and haematoma formation) or femoral vein (reduced success on the first attempt) cannulation for central vein catheterization, but these findings do not necessarily hold for all groups of ultrasound users or for patients at high risk for complications. The results for Doppler ultrasound techniques versus anatomical landmark techniques are uncertain.
Summary of findings
Background
Description of the condition
Insertion of catheters into blood vessels for diagnostic or therapeutic purposes is often a vital component of perioperative or intensive care patient management. Approximately six million central venous catheterizations are performed each year in Europe and the USA (Calvert 2003; FDA Drug Bull 1989).
The benefits of central venous catheters (CVCs) lie in their ability to allow the recording of central venous pressure or other haemodynamic measures (Rajaram 2013), the infusion of agents that are too potent (e.g. catecholamines) or too irritating (e.g. cytotoxic chemotherapy, parenteral nutrition (Joffe 2009)) to be given through peripheral veins and the possibility of dialysis in acute renal failure.
Puncture of the vessels for central venous catheterization was originally guided by anatomical landmarks on or near the surface of the body through palpation of bones and/or arteries. This method can be unsuccessful in up to 35% of cases (Bernard 1971; Defalque 1974; Sznajder 1986), and the total rate of complications is reported in the literature as up to 19% (Merrer 2001). Further, 9% of people have abnormalities of the anatomy of their central veins, which make the puncture or catheterization difficult, dangerous or impossible to perform (Denys 1991). Many puncture‐ and catheter‐related complications of all degrees of severity have been described (Bodenham 2011; Cook 2011; Pikwer 2012; van Miert 2012). The US Food and Drug Administration (FDA) described a total puncture‐related rate of complications of 5% to 20% (FDA Drug Bull 1989), Johnson a rate of arterial punctures up to 37.8% (Johnson 1994) and Polderman a rate of catheter‐related infection (CRI) of 1% to 40% (Polderman 2002). Different sites of insertion carry different rates of risk, for instance, catheters in the femoral vein are more likely to lead to thrombotic or infectious complications than those in the subclavian vein (Ge 2012).
Puncture‐related complications can result from patient‐specific features such as an abnormal weight‐to‐height ratio (obesity, cachexia), variations in anatomical structure (the probability of which is given in the literature as up to 29%), thrombosis‐related changes in wall structure (Caridi 1998; Denys 1991; Ferral 1998; McIntyre 1992), existing hypovolaemia or coagulopathy (Bernard 1971). In addition, the experience of the practitioner (Bernard 1971), the environment in which the insertion is performed (Bo‐Linn 1982) and the position and the risk inherent in the particular puncture procedure contribute to the occurrence of complications.
Many attempts have been made to reduce the number of complications associated with central venous catheterizations. These attempts have involved the development of ever newer kinds of access and puncture techniques and materials, as well as the utilization of various ultrasound procedures (two‐dimensional ultrasound (US) or Doppler ultrasound (USD), direct or indirect, with or without needle guide).
Description of the intervention
Use of Doppler ultrasound to locate the subclavian vein was first reported in 1982 (Peters 1982), and its use in locating the internal jugular vein was reported two years later (Legler 1984). Two‐dimensional ultrasound was tried in subsequent investigations (Yonei 1986; Yonei 1988). Ultrasound can be performed during vein puncture ('direct' puncture), or it can be used to identify and mark the vessel before puncture ('indirect' use). Sterile sheaths prevent skin contamination by the ultrasound probe and can be filled with sterile ultrasonic transmitting gel. A needle guide—a piece of plastic that angles the needle so it will intersect the centre of the vessel—can be attached to the probe to ensure optimal positioning of the needle during vessel puncture. Passage of the introducer needle into the vein can be performed with a transverse (short axis, or 'out of plane') view or a longitudinal (long axis, or 'in plane') view. Benefits of the transverse view are that it is generally associated with a shorter learning curve and it can make it easier for the clinician to visualize small vessels. The primary advantage of the longitudinal view is that it allows better visualization of the advancing needle tip, which may reduce perforation of the posterior vessel wall (Atkinson 2005). For this reason the American College of Emergency Physicians has recommended the longitudinal view (American College of Emergency Physicians 2007).
How the intervention might work
Ultrasound guidance clarifies and makes 'visible' the relative position of the needle and the vein and surrounding structures. It can help the clinician predict anatomical variants (transposition of the vein and the artery, overlap of the artery and the vein), can clarify the site of target veins in the presence of abnormal patient features (e.g. morbid obesity, cachexia, local scarring) and can facilitate assessment of the patency of a target vein (thrombosis, small diameter) before and during the procedure. Scanning during changes in the patient's position allows the operator to find the best conditions for puncture, and assessing the internal diameter of different veins allows selection of one for which the catheter does not exceed one‐third the internal diameter of the vein. This is thought to reduce the likelihood of catheter‐related thrombosis (Debordeau 2009; Lamperti 2012).
The last paper related to USD guidance was published in 2000 (Verghese 2000). This study was published first as a congress poster in 1995 (Verghese 1995). As causes for this a lower effectiveness in comparison with the US techniques and the increasing distribution from ultrasonic apparatuses as well as the various use possibilities (provision of the vessel diameter, control of the catheter's tip position, peripheral venous and arterial cannulation, doing regional anaesthesia with the help of ultrasound and much more) being able to be suspected. Some of the studies evaluated by review authors for inclusion in this review permit the conclusion that Doppler ultrasound for vascular access is associated with a longer learning curve, longer insertion times and higher costs than B‐mode ultrasound (Bold 1998; Gilbert 1995; Legler 1984). Other studies found it "easy to learn, and efficient ..." (Branger 1995), and still others state: “Finally, training did not influence the course of the study...This suggests that training had no influence on Doppler guidance procedure and that it could be learned easily and quickly” (Lefrant 1998).
Why it is important to do this review
Several reviews (Calvert 2003; Hind 2003; Keenan 2002; Randolph 1996; Rothschild 2001) have compared the effectiveness of ultrasound guidance versus that of the landmark technique for central vein catheterization, but these reviews are now quite old. Techniques have changed, new studies have been performed and evidence shows slow uptake of the newer technique by some clinicians (Howard 2007). Therefore, we have systematically reviewed the literature to assess both efficacy and safety outcomes of sonographic techniques for vessel puncture during CVC instillation to see whether this approach makes the procedure safer, faster, freer of complications and more often successful. This review is one of a pair of Cochrane reviews on this topic. The other focuses on evidence for ultrasound in catheterization of the internal jugular vein (Brass 2013a).
Objectives
Primary objective
The primary objective of this review was to evaluate the effectiveness and safety of two‐dimensional ultrasound (US)‐ or Doppler ultrasound (USD)‐guided puncture techniques for subclavian vein, axillary vein and femoral vein puncture during central venous catheter insertion in adults and children. We assessed whether there was a difference in complication rates between traditional landmark‐guided and any ultrasound‐guided central vein puncture.
Secondary objectives
When possible, we also assessed the following secondary objectives: whether a possible difference could be verified with use of the US technique versus the USD technique; whether there was a difference between using ultrasound throughout the puncture ('direct') or only to identify and mark the vein before starting the puncture procedure ('indirect'); and whether these possible differences might be evident in different groups of patients or with different levels of experience among those inserting the catheters.
Methods
Criteria for considering studies for this review
Types of studies
We considered randomized controlled trials (RCTs) in all languages that were eligible for inclusion in the review, with an RCT defined as a study in which participants were allocated to treatment groups on the basis of a random or quasi‐random method (e.g. using random number tables, hospital number, date of birth). We also included controlled clinical trials (CCTs).
Types of participants
We included all patients (children and adults) who required the insertion of a central venous catheter via the subclavian, the axillary or the femoral vein.
We applied no restrictions with respect to specific population characteristics (such as age, gender, race or presence of a particular condition, for example, risk factors), settings (intensive care unit (ICU), operation room, patient awake/sedated/anaesthetized) or practitioners' experience.
Types of interventions
We included all studies in which conventional techniques oriented to anatomical landmarks (LMs) for puncture of the subclavian vein, the axillary vein and the femoral vein (control intervention) were compared with techniques in which punctures were performed with the help of imaging (US) or Doppler (USD) sonographic devices (experimental intervention). We included all studies, irrespective of whether the puncture was performed directly (under sonographic control) or indirectly (while searching for the vessel by means of ultrasound and marking the puncture site on the skin; the following puncture was performed without sonographic guidance).
Types of outcome measures
The outcome measures did not constitute criteria for inclusion of studies.
Primary outcomes
The primary outcome measured was the total number of perioperative and postoperative complications/adverse events (*absolute numbers (n/N) and expressed as percentages (%) (*)).
Secondary outcomes
Secondary outcomes included the following.
Overall success rate (*).
Number of attempts until success (*).
Number of participants with an arterial puncture (*).
Number of participants with significant haematoma formation (*).
Number of participants with other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (*).
Time needed for success (*).
Success with attempt number 1, 2, 3 (*).
Participant discomfort (*).
Mortality (*).
All outcomes were defined as stated by the study authors. We differentiated between intraoperative, postoperative and long‐term complications. We included studies irrespective of whether all of this information was available.
Search methods for identification of studies
We employed the standard methods of The Cochrane Anaesthesia Review Group.
Two review authors (PB, GS) independently assessed the titles and abstracts (when available) of all reports identified by electronic searching, manual searching, snowballing and making contact with experts and industry.
We assessed all reports as follows.
Patrick Brass (PB) assessed all reports.
Guido Schick (GS) assessed all reports.
We retrieved and evaluated full‐text versions of potentially relevant studies chosen by at least one review author. We masked all selected studies by obscuring study authors' names and institutions, locations of studies, reference lists, journals of publication and any other potential identifiers.
Electronic searches
We searched the following databases for relevant trials: the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 1; see Appendix 1 for detailed search strategy); Ovid MEDLINE (1966 to 15 January 2013; see Appendix 2); Ovid EMBASE (1980 to 15 January 2013; see Appendix 3); the Cumulative Index to Nursing and Allied Health Literature (CINAHL via EBSCOhost) (1982 to 15 January 2013; see Appendix 4), MedPilot (1980 to 15 January 2013; see Appendix 5) and other medical databases (Current Contents, Science Citation Index; registers of clinical trials (from the International Clinical Trials Registry; registers compiled by Current Science)).
We reran the search in August 2014. We will deal with any studies of interest when we update the review.
We did not limited the search by language or publication status.
We combined the MEDLINE search strategy with the Cochrane Highly Sensitive Search Strategy as contained in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We adapted our MEDLINE search strategy for searching the other databases.
We attempted to identify unpublished or ongoing studies by searching the following three trial registries (searched on 20 March 2012) for all years available in all possible fields using the basic search function (using separately the following keyword terms: "ultrasound", "central vein catheterization", "central vein catheter").
Current Controlled Trials: www.controlled‐trials.com.
ClinicalTrials.gov: www.clinicaltrials.gov.
Searching other resources
We performed an additional handsearch, which focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings (e.g. proceedings of the Annual Congress of the European Society of Intensive Care Medicine (ESICM), the Annual Congress of the German Society of Anaesthesia (DAK) or the Annual Congress of the European Society of Anaesthesia (ESA)) (2003 to 2013; last search 20 January 2013); references lists; 'grey literature' (System for Information on Grey Literature in Europe (SIGLE and ZETOC)); the Index to Scientific and Technical Proceedings (from the Institute for Scientific Information) and dissertations.
We attempted to identify unpublished or ongoing studies by contacting the companies medilab GmbH (SiteRite®; Dymax Corporation), Medimex (P.D. Access®/SmartNeedle®) and SonoSite.
We contacted experts in the field to identify unpublished studies and studies presented in abstract form at major international meetings.
We (PB, GS) checked the bibliographies of all identified studies. We repeated this approach until no further studies could be identified.
Data collection and analysis
Selection of studies
Two review authors (PB, GS) independently screened the titles and abstracts of reports identified by electronic searching, manual searching, snowballing and making contact with experts and industry for relevance. We excluded any citations that were clearly irrelevant at this stage. We obtained full copies of all potentially relevant papers.
Two review authors (PB, GS) independently screened the full papers, identified relevant studies and assessed eligibility of studies for inclusion. We selected trials that met the inclusion criteria, using a checklist designed in advance for that purpose. We resolved disagreements on the eligibility of studies through discussion. When resolution was not possible, we consulted a third review author (LK).
We assessed all studies that met the inclusion criteria for quality and extracted data from them. We excluded all irrelevant records and recorded details of the studies and reasons for exclusion.
Data extraction and management
Two review authors (PB, GS) independently extracted data using specially designed data extraction forms. We divided the workload as follows.
PB extracted data from all reports.
GS extracted data from all reports.
We resolved disagreements by discussion; when necessary we consulted a third review author (LK). Once we had resolved disagreements, we recorded the extracted data onto the final data extraction form.
We contacted study authors to ask for clarification or missing information. If further clarification was not available, if we could not get the missing information or if we reached no agreement, we placed these studies under the heading Studies awaiting classification to allow review authors the opportunity to use these data in the future.
One review author (PB) transcribed data into RevMan 5.2 (RevMan 5.2), and another review author (GS) checked the data entered to look for discrepancies.
In addition to details related to the risk of bias of included studies, we extracted two sets of data.
Study characteristics: place of publication; date of publication; population characteristics; setting; detailed nature of intervention; detailed nature of comparator; and detailed nature of outcomes. A key purpose of these data was to define unexpected clinical heterogeneity in included studies independently from the analysis of results.
Results of included studies with respect to each of the main outcomes indicated in the review question: We carefully recorded reasons why an included study did not contribute data on a particular outcome and considered the possibility of selective reporting of results on particular outcomes.
We recorded for each trial the following data.
Authors.
Year of publication.
Study design.
Population.
Inclusion procedure: (‐) means non‐consecutive/unknown, (+) means consecutive.
Setting: university/other/unknown.
Participant characteristics (age, gender, height, weight, body mass index (BMI)) recorded as stated in the study.
Punctured vessel/punctured side.
Intervention (US or USD, puncture occurred directly (DUS or DUSD) or indirectly (IDUS or IDUSD) (puncture method: US: information on the applied ultrasound procedure and on the position in which the puncture was performed; LM: information on the position in which the puncture was performed. Puncture method +: standardized, ‐: not standardized).
Study design: P: prospective; R: randomized; C: controlled; Cr‐o: cross‐over; information on randomization method; exclusion of participants after randomization: +: yes, ‐: no; intention‐to‐treat evaluation plan +: yes, ‐: no.
Number and experience of practitioner(s).
Numbers of punctures and participants.
LM/US: number of conventional/sonographic punctures.
Details of the outcome (all studies included, irrespective of whether they contained complete information on overall success rate, total number of attempts needed until success, number of punctures that were successful at first, second, third, etc. attempt, overall complication rate or numbers of individual complications and time required until success, or whether some of this information was lacking).
Conclusions of study authors.
Assessment of risk of bias in included studies
Two review authors (PB, GS) independently and in duplicate assessed the methodological quality of each included study using a simple form and following the domain‐based evaluation as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed the following domains as having low, unclear or high risk of bias.
Random sequence generation.
Allocation concealment.
Participant/subject blinding.
Provider/physician blinding.
Outcome assessor blinding.
Incomplete outcome data addressed.
Selective outcome reporting.
Other source of bias.
We reviewed the assessments and discussed inconsistencies between the review authors in interpreting inclusion criteria and their significance for selected studies. We resolved disagreements through discussion with a third review author.
We did not automatically exclude any study as a result of a rating of ’unclear risk of bias’ or ’high risk of bias.’ A summary of bias was given for each study, and the results were summarized in the Risk of bias in included studies portion of the Results section of this review. We predicted that, given the nature of the intervention, blinding of the practitioner would not be possible. We noted measures of clinical performance, for instance, when given, we recorded the experience and number of practitioners performing the procedures during a trial.
Second, we assessed the quality of evidence at the outcome level using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
Within each study, we described what was reported for each domain and contacted the study authors for additional information when necessary. We evaluated the risk of bias for each domain as follows.
Yes: criteria appropriately applied and described in the report or ascertained in communication with the primary author of the study.
Unclear: criteria not described and impossible to acquire from or clarify with the study authors.
No: criteria inappropriately applied.
Included studies were then classified into one of the following categories.
Low risk of bias: all criteria met.
Moderate risk of bias: one or more criteria unclear.
High risk of bias: one or more criteria not applied or met.
At each stage, we compared results. We discussed the impact of methodological quality on the results and resolved disagreements by discussion.
We had planned to perform a sensitivity analyses to test how sensitive the results are to reasonable changes in assumptions made during the review process and in the protocol for combining data (Lau 1998). We performed sensitivity analysis regarding randomized versus quasi‐randomized and good quality versus poor quality studies. We defined a good quality study as one that has all of the following domains: adequate allocation concealment; blinding of outcome assessment; and data analysis performed according to the 'intention‐to‐treat' principle. We defined a poor quality study as one that lacks one or more of these key domains. We reviewed the assessments and discussed inconsistencies between review authors in interpreting inclusion criteria and their significance for selected studies. We resolved disagreements through discussion with a third review author.
Measures of treatment effect
We analysed extracted data using Review Manager (RevMan 5.2).
For dichotomous data, we described results both as a relative measure (risk ratio (RR)) with 95% confidence intervals (CIs) and as an absolute measure (number needed to treat for an additional beneficial outcome and risk difference). Relative measures can be used to combine studies; absolute measures can be more informative than relative measures because they reflect baseline risk as well as changes in risk seen with the intervention. The test for overall pooled effect used the Z statistic, with a P value less than 0.05 taken to be significant. We used, for continuous outcomes, mean difference (MD) and standard deviation (SD) to summarize the data for each group. This conferred the advantage of summarizing results in natural units that are easily understood. We performed a meta‐analysis for studies that made similar comparisons and reported the same outcome measures.
Unit of analysis issues
We include cross‐over studies in this review, but we did not analyse the endpoint of success rate after cross‐over.
The unit of analysis was the individual participant.
Dealing with missing data
No simple solution is known for the problem of missing data. We handled this problem by contacting investigators, when possible, to request clarification of methodological issues and to ask for additional data. In addition, assumptions regarding the method used to cope with missing data were made explicit. We included studies irrespective of whether all of the outcome information was available. However, to date, we have not received data beyond those presented in the primary reports. If we subsequently receive additional information, we plan to incorporate these data into the next update of this review.
Assessment of heterogeneity
We assessed heterogeneity between trials by visually inspecting forest plots, and we quantified statistical heterogeneity by calculating the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than to chance (Higgins 2003). We regarded heterogeneity as low when I2 was less than 25%, as moderate when I2 was between 25% and 50% and as substantial when I2 was greater than 50%. If evidence of substantial heterogeneity was found, we investigated and reported possible reasons for this.
The predetermined significance level of heterogeneity included a P value of .05. Both the typical effect size and the effect size relative to specific study characteristics will be interpreted cautiously when heterogeneity is significant.
Assessment of reporting biases
We made a great effort to identify unpublished studies and to minimize the impact of possible publication bias by using a comprehensive research strategy.
Publication bias occurs when published studies are not representative of all studies that have been done, usually because positive results tend to be submitted and published more often than negative results. Because detecting publication bias is difficult, we tried to minimize this risk by performing comprehensive literature searching, using study registries and contacting the manufacturers of ultrasound devices (Glasziou 2001).
We assessed reporting bias by trying to identify whether the study was included in a trial registry, whether a protocol was available and whether the Methods section provided a list of outcomes. We compared the list of outcomes from those sources versus outcomes reported in the published paper.
We planned to use a graphical display (funnel plot) on the size of the treatment effect against the precision of the trial (one/standard error) and to investigate publication bias by examining for signs of asymmetry. Publication bias is associated with asymmetry (Light 1984). In the absence of publication bias, a plot of study sample size (or study weight) versus outcome (i.e. log relative risk) should have a bell or inverted funnel shape, with the apex near the summary effect estimate (funnel plot). If asymmetry was noted, we searched for reasons other than publication bias, such as poor methodological quality of smaller studies, true heterogeneity, artefactual reasons or chance (Egger 1997).
We did not use funnel plots to assess publication bias when we found fewer than 10 trials for an endpoint, as asymmetry is difficult to detect when a small number of studies are included.
Data synthesis
We reviewed the data from included studies qualitatively and then, if possible, combined the data quantitatively by population, intervention and outcome, using the statistical software of The Cochrane Collaboration—Review Manager (RevMan 5.2).
We performed a meta‐analysis when studies of similar comparisons reported the same outcome measures. We used models with random effects (i.e. the Mantel‐Haenszel (MH) method for dichotomous data (using risk ratio as effect measure) and the inverse variance (IV) method for continuous data (using standardized mean difference as effect measure)) because of apparent between‐study heterogeneity, as assessed by Q and I2 statistics. Confidence intervals were calculated at level 95%, and corresponding P values equal to or less than 5% (two‐sided alpha) were considered statistically significant.
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses of different sonographic techniques ((D)/(ID)/US/USD), puncture sites, groups of participants (adults, children) and practitioners (experienced and inexperienced, as described by study authors). Because some data were missing, we could not perform a subgroup analysis.
Sensitivity analysis
A priori, we planned sensitivity analyses to test how sensitive the results are to reasonable changes in assumptions made and to changes in the protocol for combining data (Lau 1998).
We planned to perform sensitivity analysis regarding 'randomized versus quasi‐randomized' and possibly 'good quality' studies versus 'poor quality' studies. We defined a good quality study as one that includes all of the following domains: adequate allocation concealment, blinding of outcome assessment and data analysis performed according to the intention‐to‐treat principle. A poor quality study was defined as one that lacks one or more of these key domains.
We have not performed a sensitivity analysis, as almost all of the included studies have high risk of bias. For example, in no study was the outcome assessor blinded. In only one study adequate sequence generation and adequate allocation concealment were reported (Aouad 2010), and in six trials the method of randomization or concealment of allocation was not made clear (Alic 2009; Branger 1994; Branger 1995; Gualtieri 1995; Lefrant 1998; Mansfield 1994). Inclusion and exclusion criteria were clearly defined in eight studies, and treatment and control groups were adequately described at entry in only four studies. No intention‐to‐treat analyses were performed in seven studies (Aouad 2010; Branger 1994; Branger 1995; Fragou 2011; Gualtieri 1995; Palepu 2009; Prabhu 2010). Whether this was done remains unclear in one study (Mansfield 1994).
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies.
Results of the search
The January 2013 search coupled with our previous search identified a total of 197 citations in electronic databases. Searches of other sources yielded a total of 13 citations: zero from an additional handsearch focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings (e.g. proceedings of the Annual Congress of the European Society of Intensive Care Medicine (ESICM) or the Annual Congress of the European Society of Anaesthesia (ESA)); three from reference lists; and 10 from the companies that we contacted to ask for references. Upon reviewing the titles and abstracts, we identified and retrieved for review 10 references in full text (see Figure 1). Altogether, 210 citations, including 183 duplicates, were identified. After screening the titles and abstracts of 27 unique citations, we excluded seven citations. We screened the remaining 20 texts in full, from which we excluded seven reports. We screened the remaining 20 texts in full and excluded seven of them. Reasons for their exclusion are as follows: One was not randomized; in one, the study authors randomly assigned the technique and the initial side of the puncture; in another, the study authors made no statements on punctured vessels; and in two studies, different vessels were punctured and evaluated together. One study was published twice—first as a congress poster (Thompson 1994), then as an article (Gualtieri 1995).
1.

Study flow diagram.
We reran the search in August 2014. We found eight new citations, of which five studies were of interest (Eldabaa 2012; Enany 2013; Lam 2013; Oh 2014; Xu 2013) (see Characteristics of studies awaiting classification). We will deal with studies of interest when we update the review.
We identified no ongoing studies. Altogether we included 13 studies in the quantitative synthesis.
Included studies
We included 13 studies enrolling 2341 participants (see Characteristics of included studies) (involving 2360 procedures [landmark 1194, ultrasound 1166]) published between 1994 and 2010: nine studying the subclavian vein (2030 participants, 2049 procedures [landmark 1033, ultrasound 1016]). Of these, five used two‐dimensional ultrasound (US) (Alic 2009; Fragou 2011; Gualtieri 1995; Mansfield 1994; Palepu 2009) and four used Doppler mode (USD) (Bold 1998; Branger 1994; Branger 1995; Lefrant 1998)). Four trials studied insertion into the femoral vein (311 participants, 311 procedures [landmark 161, ultrasound 150]); all used US (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010)). The individual studies involved sample sizes of 45 (Palepu 2009) to 821 participants (Mansfield 1994). The studies took place in different hospital settings all over the world. Participants were adults of both sexes in eight studies; children in one study (Aouad 2010); and adults and children in one study (Iwashima 2008); no details were given on three studies.
Of 13 eligible studies, eight were RCTs (six subclavian vein (Alic 2009; Bold 1998; Fragou 2011; Gualtieri 1995; Lefrant 1998; Palepu 2009), two femoral vein (Aouad 2010; Prabhu 2010)), and three were quasi‐RCTs (one subclavian vein (Mansfield 1994), two femoral vein (Iwashima 2008; Kwon 1997)). It was unclear whether two studies were RCTs or CCTs (two subclavian vein (Branger 1994; Branger 1995)). Inclusion and exclusion criteria were clearly defined in eight studies, and treatment and control groups were adequately described at entry in only four studies. No intention‐to‐treat analyses were performed in seven studies (Aouad 2010; Branger 1994; Branger 1995; Fragou 2011; Gualtieri 1995; Palepu 2009; Prabhu 2010). This detail remains unclear in one study (Mansfield 1994). In none of the studies was the outcome assessor blinded.
In nine studies the subclavian vein was used. Five of the nine studies used imaging ultrasound (US). (Of those five studies, four used direct (D) imaging ultrasound (Alic 2009; Fragou 2011; Gualtieri 1995; Palepu 2009) and the remaining study indirect (ID) imaging ultrasound (Mansfield 1994). The other four studies used sonographic techniques (Doppler (USD), direct (D) ultrasound (Bold 1998; Branger 1994; Branger 1995; Lefrant 1998), and indirect (ID) ultrasound in zero)).
In four studies the femoral vein was used; all used direct puncture with two‐dimensional ultrasound (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010). Among the four studies in which direct (D) ultrasound was used for subclavian vein cannulation (Alic 2009; Fragou 2011; Gualtieri 1995; Palepu 2009), passage of the introducer needle into the vein was performed with the transverse (short axis) view in two studies (Gualtieri 1995; Palepu 2009) and with the longitudinal (long axis) view in one study (Fragou 2011). Among the four studies in which direct (D) ultrasound was used for femoral vein cannulation (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010), passage of the introducer needle into the vein was performed with the transverse (short axis) view in all studies. In three studies the subclavian vein and the internal jugular vein were used (one US (Palepu 2009), two USD (Branger 1994; Branger 1995)). Information about the puncture side was given in five studies (subclavian vein in three (Lefrant 1998; Mansfield 1994; Palepu 2009) and femoral vein in two (Aouad 2010; Prabhu 2010)).
Among studies in which the subclavian vein was used, six studies evaluated the primary outcome complication rate total (Bold 1998; Branger 1994; Gualtieri 1995; Lefrant 1998; Mansfield 1994; Palepu 2009), three the numbers of arterial puncture and haematoma formation (Fragou 2011; Gualtieri 1995; Palepu 2009) and six the number of other complications ((Bold 1998; Branger 1994; Fragou 2011; Gualtieri 1995; Lefrant 1998; Palepu 2009); in two (Alic 2009; Branger 1995) the rate of complications was not evaluated. Among studies in which the femoral vein was used, no study evaluated the primary outcome complication rate total. All 13 studies evaluated the overall success rate and the failure rate. Eight studies (Alic 2009; Aouad 2010; Branger 1995; Fragou 2011; Gualtieri 1995; Lefrant 1998; Palepu 2009; Prabhu 2010) evaluated the number of attempts until success, but only four studies (Alic 2009; Branger 1995; Fragou 2011; Prabhu 2010) stated the standard deviation and therefore could be included in the analysis. Six studies evaluated time to successful cannulation, six success with attempt number one to five and seven the success rate after cross‐over.
In four studies (two subclavian, two femoral) no details on the number of operators who carried out the procedure were provided (given N = 9). In one study (Iwashima 2008) no details on the experience of the operators who carried out the procedure were provided (given N = 12). Exact details on the training experience of the operators with each method were absent or inaccurate in some studies (Alic 2009; Lefrant 1998; Mansfield 1994), and operators did not have similar experience with both techniques in most of the studies.
Three of six trials in which puncture of the subclavian vein was guided by ultrasound are almost 20 years old. All studies in which puncture was performed using Doppler were older than 15 years. Trials studying insertion into the femoral vein were dated from 1997, 2008 and 2010. Gualtieri (Gualtieri 1995) and possibly Palepu (Palepu 2009) used the axillary vein for cannulation.
Excluded studies
We excluded six studies from the review for the following reasons. One was an observational study with a sequential protocol. The ultrasound device was used for one week, and the landmark technique was used the following week; this was done alternately for eight weeks (Kwon 1997). In one study (Hilty 1997) each participant received bilateral femoral lines—one by ultrasound guidance and the other by the landmark approach. A computer‐generated randomization chart predetermined the choice of initial technique (landmark vs ultrasound) and the side approached first (left vs right). In one study the study authors made no statement regarding the punctured vessels (Woody 2001); in two studies the study authors used different vessels but stated the results together (Froehlich 2009; Miller 2002); and one study was published twice—first as a congress poster (Thompson 1994), then as a full paper (Gualtieri 1995). See Characteristics of excluded studies.
Awaiting classification
Five studies are awaiting classification (Eldabaa 2012; Enany 2013; Lam 2013; Oh 2014; Xu 2013). See Characteristics of studies awaiting classification.
Risk of bias in included studies
We used the domain‐based evaluation table of The Cochrane Collaboration as provided in RevMan 5.2 to assess the validity and quality of included trials. We have detailed the methods of randomization and outcome assessment as well as exclusion criteria in the Characteristics of included studies table. A summary of our assessment of methodological quality of included studies is given in Figure 2 and Figure 3. Most trials had unclear risk of bias across the six domains, and heterogeneity among the studies was significant.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
We believe that the inability to blind the practitioner performing the puncture, especially when the same person was performing all punctures, was a potential source of performance bias. One further source of potential bias was that in none of the studies was the outcome assessor blinded. For this reason, all included trials should be considered as having at least unclear risk of bias. Because of the nature of the intervention, blinding of the practitioner was never going to be possible; this is an unavoidable source of bias. We are aware that these studies present a potential risk of bias and have taken this into account when assessing study results.
Inclusion and exclusion criteria were clearly defined in eight studies, and treatment and control groups were adequately described at entry in only three studies (Aouad 2010; Fragou 2011; Lefrant 1998). No intention‐to‐treat analyses were performed in seven studies (Aouad 2010; Branger 1994; Branger 1995; Fragou 2011; Gualtieri 1995; Palepu 2009; Prabhu 2010). This detail remains unclear in one study (Mansfield 1994). The stated exclusion criteria were nearly similar in all included trials. We believe that the potential for exclusion bias was therefore low.
The experience of practitioners and their faculties in both ultrasound techniques and control techniques, as well as the number of practitioners involved, varied across trials. In four trials the number of practitioners performing the procedures was not stated (Aouad 2010; Fragou 2011; Palepu 2009; Prabhu 2010). In one study (Iwashima 2008) no details on the experience of the operators who carried out the procedure were provided.
Allocation
In six trials, the allocation sequence was adequately generated (Aouad 2010; Bold 1998; Fragou 2011; Gualtieri 1995; Palepu 2009; Prabhu 2010), it was unclear in four trials (Alic 2009; Iwashima 2008; Lefrant 1998; Mansfield 1994) and in three trials researchers used inadequate allocation generation (Branger 1994; Branger 1995; Kwon 1997). In one study allocation concealment was adequate (Aouad 2010).
Blinding
None of the studies was free from other problems that could put them at risk of bias. Given the nature of the intervention, blinding to the intervention was not always (participants) or was not (personnel) feasible; however, we assessed the risk of bias according to whether outcome assessors were independent from those involved in participant care management decisions. In none of the 13 trials was it stated that the outcome assessors were blinded. Procedures were carried out when participants were anaesthetized (Aouad 2010), sedated (Fragou 2011), sedated or anaesthetized (Gualtieri 1995; Iwashima 2008) or anaesthetized or awake (Branger 1994; Branger 1995), or in any of these three states (Lefrant 1998). None of the four studies in which participants were awake (Bold 1998; Kwon 1997; Mansfield 1994; Prabhu 2010) attempted to blind participants to the technique used. This may present a potential source of detection bias, as several of the assessed outcomes may be subjective (e.g. complication rate, participant satisfaction). No details on level of consciousness of participants during insertion were provided in two studies (Alic 2009; Palepu 2009).
Incomplete outcome data
Completeness of data on the main outcomes
In eight of the 13 studies, data on the main outcomes were reported completely (Alic 2009; Aouad 2010; Bold 1998; Fragou 2011; Gualtieri 1995; Mansfield 1994; Palepu 2009; Prabhu 2010). In five studies no main outcomes were defined (Branger 1994; Branger 1995; Iwashima 2008; Kwon 1997; Lefrant 1998). We believe that the potential for attrition bias is nevertheless low in these studies. Incomplete outcome data were addressed in three studies (Branger 1995; Gualtieri 1995; Mansfield 1994) with high risk of attrition bias. In these three trials, incomplete outcome data were not adequately addressed (outcomes of participants who withdrew or were excluded after allocation were neither detailed separately nor included in an intention‐to‐treat analysis, or the text stated no withdrawals). We believe that the potential for attrition bias is therefore high in these studies.
Among studies in which the subclavian vein was used, six studies evaluated the primary outcome complication rate total and three did not (Gualtieri 1995; Branger 1995; Fragou 2011); three evaluated the numbers of arterial punctures and haematomas formed (Fragou 2011; Gualtieri 1995; Palepu 2009) and six did not (Alic 2009; Bold 1998; Branger 1994; Branger 1995; Lefrant 1998; Mansfield 1994); and six evaluated the number of other complications (Bold 1998; Branger 1994; Fragou 2011; Gualtieri 1995; Lefrant 1998; Palepu 2009) and three did not (Alic 2009; Branger 1995; Mansfield 1994). Among studies in which the femoral vein was used, no study evaluated the primary outcome complication rate total. Eight studies (Alic 2009; Aouad 2010; Branger 1995; Fragou 2011; Gualtieri 1995; Lefrant 1998; Palepu 2009; Prabhu 2010) evaluated the number of attempts until success, but only four studies (Alic 2009; Branger 1995; Fragou 2011; Prabhu 2010) stated the standard deviation and therefore could be included for analysis. Five studies (Bold 1998; Branger 1994; Iwashima 2008; Kwon 1997; Mansfield 1994) did not evaluate the number of attempts until success. Seven studies did not evaluate the time to successful cannulation, seven did not evaluate success with attempt number one to five and six did not evaluate the success rate after cross‐over. None of the study authors indicated why these endpoints were not recorded.
A comparison of outcomes mentioned in the publication versus endpoints planned in the study protocol was not possible in any of the studies because not a single protocol was published.
Selective reporting
In no study can selective reporting (selective availability of data, selective reporting of outcomes, time points, subgroups or analyses) be excluded because none of the studies had a published protocol. However, in all studies with a Methods section, all outcomes specified therein were reported in the Results section.
Other potential sources of bias
A priori sample size calculations were conducted in none of the studies. No studies were stopped early, for example, by the data monitoring committee. Conflicts of interest were not reported in any studies.
In four studies (Alic 2009; Fragou 2011; Gualtieri 1995; Lefrant 1998) it remains unclear whether there were withdrawals, one study reported withdrawals (Mansfield 1994) and three studies reported a postrandomization exclusion (Branger 1995; Fragou 2011; Gualtieri 1995). In none of the studies did we find an excessive dropout rate.
Effects of interventions
Summary of findings for the main comparison. Ultrasound or Doppler guidance compared with anatomical landmark for subclavian vein cannulation for central vein catheterization.
| Ultrasound or Doppler guidance compared with anatomical landmark for subclavian vein cannulation for central vein catheterization | ||||||
| Patient or population: patients with the need for subclavian vein cannulation for central vein catheterization Settings: Intervention: ultrasound or Doppler guidance Comparison: anatomical landmark | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Anatomical landmark | Ultrasound or doppler guidance | |||||
| Complication rate total | Study population | RR 0.52 (0.23 to 1.17) | 1478 (6 studies) | ⊕⊝⊝⊝ Very lowa,b,c,d | ||
| 111 per 1000 | 58 per 1000 (26 to 130) | |||||
| Moderate | ||||||
| 155 per 1000 | 81 per 1000 (36 to 181) | |||||
| Overall success rate | Study population | RR 1.05 (0.97 to 1.13) | 1809 (8 studies) | ⊕⊕⊝⊝ Lowd,e,f,g | ||
| 877 per 1000 | 921 per 1000 (851 to 991) | |||||
| Moderate | ||||||
| 899 per 1000 | 944 per 1000 (872 to 1000) | |||||
| Number of attempts until success | Mean number of attempts until success in the intervention groups was 0.38 lower (1.26 lower to 0.5 higher) | 471 (2 studies) | ⊕⊝⊝⊝ Very lowd,h,i,j | |||
| Arterial puncture | Study population | RR 0.21 (0.06 to 0.82) | 498 (3 studies) | ⊕⊕⊝⊝ Lowd,j,k,l | ||
| 59 per 1000 | 12 per 1000 (4 to 48) | |||||
| Moderate | ||||||
| 55 per 1000 | 12 per 1000 (3 to 45) | |||||
| Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) | Study population | RR 0.29 (0.07 to 1.21) | 1058 (6 studies) | ⊕⊝⊝⊝ Very lowb,d,j,m | ||
| 97 per 1000 | 28 per 1000 (7 to 117) | |||||
| Moderate | ||||||
| 105 per 1000 | 30 per 1000 (7 to 127) | |||||
| Time to successful cannulation | Mean time to successful cannulation in the intervention groups was 10.48 higher (56.92 lower to 77.87 higher) | 471 (2 studies) | ⊕⊕⊝⊝ Lowb,c,d,n | |||
| Success with attempt number 1 | Study population | RR 1.08 (0.85 to 1.36) | 115 (2 studies) | ⊕⊕⊕⊕ Highd,g,o | ||
| 683 per 1000 | 737 per 1000 (580 to 928) | |||||
| Moderate | ||||||
| 686 per 1000 | 741 per 1000 (583 to 933) | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aLack of allocation concealment: unclear in 3 of 6 studies, inadequate in no studies. Incomplete outcome data addressed in 2 studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 3 of 6 studies, unclear in 2 studies. Treatment and control groups were adequately described at entry in 1 of 6 studies. bUnexplained substantial heterogeneity: P value 0.03, I² = 60%. cAn imprecise result including appreciable benefit or harm. dFewer than 10 trials for this endpoint, eLack of allocation concealment: unclear in 5 of 8 studies, inadequate in no studies. Incomplete outcome data addressed in 3 studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 2 of 8 studies, unclear in 3 studies. Treatment and control groups were adequately described at entry in 2 of 6 studies. fUnexplained substantial heterogeneity: P value < 0.0001, I² = 78%. gA precise result of no appreciable difference between treatments. hLack of allocation concealment: unclear in 2 of 2 studies. Incomplete outcome data addressed in no studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which patients are allocated in none of the studies. Free of other bias in 0 of 2 studies, unclear in 1 study. Treatment and control groups were adequately described at entry in 1 of 2 studies. iUnexplained substantial heterogeneity: P value 0.0005, I² = 92%. jAn imprecise result of appreciable or no appreciable effect. kLack of allocation concealment: unclear in 3 of 3 studies. Incomplete outcome data addressed in 1 study, unclear in 1 study. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 1 of 3 studies, unclear in no studies. Treatment and control groups were adequately described at entry in 1 of 3 studies. lNo heterogeneity: P value 0.53, I² = 0%. mLack of allocation concealment: unclear in 6 of 6 studies. Incomplete outcome data addressed in 1 study, unclear in 1 study. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 3 of 6 studies, unclear in 1 study. Treatment and control groups were adequately described at entry in 2 of 6 studies. nUnexplained substantial heterogeneity: P value 0.02, I² = 81%. oNo heterogeneity: P value 0.54, I² = 0%.
Summary of findings 2. Ultrasound guidance compared with anatomical landmarks for femoral vein cannulation for central vein catheterization.
| Ultrasound guidance compared with anatomical landmarks for femoral vein cannulation for central vein catheterization | ||||||
| Patient or population: patients with femoral vein cannulation for central vein catheterization Settings: Intervention: ultrasound guidance Comparison: anatomical landmarks | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Anatomical landmarks | ultrasound guidance | |||||
| Overall success rate | Study population | RR 1.11 (1 to 1.23) | 311 (4 studies) | ⊕⊕⊕⊝ Moderatea,b,c,d | ||
| 789 per 1000 | 876 per 1000 (789 to 970) | |||||
| Moderate | ||||||
| 847 per 1000 | 940 per 1000 (847 to 1000) | |||||
| Arterial puncture | Study population | RR 0.4 (0.14 to 1.16) | 311 (4 studies) | ⊕⊕⊝⊝ Lowd,e,f,g | ||
| 168 per 1000 | 67 per 1000 (23 to 195) | |||||
| Moderate | ||||||
| 134 per 1000 | 54 per 1000 (19 to 155) | |||||
| Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) | Study population | RR 0.49 (0.11 to 2.12) | 311 (4 studies) | ⊕⊕⊝⊝ Lowd,h,i,j | ||
| 31 per 1000 | 15 per 1000 (3 to 66) | |||||
| Moderate | ||||||
| 13 per 1000 | 6 per 1000 (1 to 28) | |||||
| Success with attempt number 1 | Study population | RR 1.73 (1.34 to 2.22) | 224 (3 studies) | ⊕⊕⊕⊕ Highd,k,l,m | ||
| 487 per 1000 | 843 per 1000 (653 to 1000) | |||||
| Moderate | ||||||
| 546 per 1000 | 945 per 1000 (732 to 1000) | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aLack of allocation concealment: unclear in 3 of 4 studies. Incomplete outcome data addressed in no studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 1 of 4 studies, unclear in 3 studies. Treatment and control groups were adequately described at entry in 1 of 4 studies. bNo heterogeneity: P value 0.11, I² = 50%. cA precise result of no appreciable difference between treatments. dFewer than 10 trials for this endpoint. eLack of allocation concealment: unclear in 3 of 4 studies. Incomplete outcome data addressed in no studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 1 of 4 studies, unclear in 3 studies. Treatment and control groups were adequately described at entry in 1 of 4 studies. fNo heterogeneity: P value 0.18; I² = 39%. gAn imprecise result of appreciable or no appreciable effect. hLack of allocation concealment: unclear in 3 of 4 studies. Incomplete outcome data addressed in no studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 1 of 4 studies, unclear in 3 studies. Treatment and control groups were adequately described at entry in 1 of 4 studies. iNo heterogeneity: P value 0.95, I² = 0%. jNo explanation was provided. kLack of allocation concealment: unclear in 2 of 3 studies. Incomplete outcome data addressed in no studies. Lack of blinding: Participants, operators and outcome assessors are aware of the arm to which participants are allocated in none of the studies. Free of other bias in 1 of 3 studies, unclear in 2 studies. Treatment and control groups were adequately described at entry in 1 of 3 studies. lNo heterogeneity: P value 0.23, I² = 31%. mA precise result of appreciable benefit.
Almost all of the included studies had unclear risk of bias, and heterogeneity was substantial. Therefore our results must be interpreted with caution. Further, our planned sensitivity analyses were not feasible, as trials could not be separated into ‘high‐quality’ and ‘poor‐quality’ studies.
The results are presented in two sections.
A. Subclavian/axillary vein cannulation for subclavian vein catheterization. Landmark technique versus two‐dimensional or Doppler ultrasound.
B. Femoral vein catheterization. Landmark technique versus two‐dimensional ultrasound.
For each outcome, differential effects between studies in which ultrasound was used for puncture or indirectly to locate the vein before puncture, or in which the method was not reported, when available, can be found in the tables within the Data and analyses section later in the review. None of the studies assessed participant discomfort during the procedure, and none assessed mortality.
Section A. Subclavian/axillary vein cannulation for subclavian vein catheterization. Landmark technique versus two‐dimensional or Doppler ultrasound
Heterogeneity was substantial for all outcomes except 4 (number of participants with an arterial puncture), 5 (number of participants with significant haematoma formation) and 8 (success on first attempt). A random‐effects model was used for analysis throughout this section.
1. Total number of perioperative and postoperative complications/adverse events
The total number of perioperative and postoperative complications/adverse events was reported in three trials using ultrasound including 918 participants (Gualtieri 1995; Mansfield 1994; Palepu 2009), and in three trials using Doppler ultrasound including 560 participants (Bold 1998; Branger 1994; Lefrant 1998) (see Analysis 1.1; Figure 4). The quality of the evidence was very low for this outcome (Table 1). For use of ultrasound (two‐dimensional (US) or Doppler ultrasound (USD))‐guided puncture techniques, no evidence showed a difference in this outcome (risk ratio (RR) 0.52, 95% confidence interval (CI) 0.23 to 1.17; P value 0.11, I² = 60%) (see Analysis 1.1; Figure 4). For direct (Gualtieri 1995; Palepu 2009) and indirect (Mansfield 1994) puncture using ultrasound, no evidence was found of a difference between ultrasound and landmark techniques (RR 0.57, 95% CI 0.17 to 1.91; P value 0.36, I² = 63 %) (see Analysis 1.1; Figure 4). A comparison of the two techniques (short axis, long axis) was not possible, as only in the studies from Gualtieri and Palepu (Gualtieri 1995; Palepu 2009) (transverse (short axis) view) was the total number of complications given. For use of Doppler guidance, no evidence revealed a difference in this outcome (RR 0.40, 95% CI 0.15 to 1.09; P value 0.07, I² = 17%) (see Analysis 1.1; Figure 4).
1.1. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 1 Complication rate total.
4.

Forest plot of comparison: 1 Traditional landmark vs ultrasound or Doppler guidance for subclavian vein cannulation for central vein catheterization, outcome: 1.1 Complication rate total.
2. Overall success rate
The overall success rate was reported in five trials using ultrasound including 1389 participants (Alic 2009; Fragou 2011; Gualtieri 1995; Mansfield 1994; Palepu 2009) and in three trials using Doppler ultrasound including 420 participants (Branger 1994; Branger 1995; Lefrant 1998). The quality of the evidence was low (Table 1). For use of ultrasound (two‐dimensional (US) or Doppler ultrasound (USD))‐guided puncture techniques, no evidence showed a difference in this outcome (RR 1.05, 95% CI 0.97 to 1.13; P value 0.22, I² = 78%) (see Analysis 1.2). For direct (Alic 2009; Fragou 2011; Gualtieri 1995; Palepu 2009) and indirect (Mansfield 1994) puncture using ultrasound, no evidence suggested a difference between ultrasound and landmark techniques (RR 1.08, 95% CI 0.96 to 1.20; P value 0.19, I² = 84%) (see Analysis 1.2). Use of direct puncture and the transverse (short axis) view (Gualtieri 1995; Palepu 2009) did not increase the overall success rate (RR 1.46, 95% CI 0.52 to 4.15; P value 0.47, I² = 95%). Use of direct puncture and the longitudinal (long axis) view (Fragou 2011) did increase the overall success rate (RR 1.14, 95% CI 1.08 to 1.20; P value < 0.00007). For use of Doppler guidance, no evidence showed a difference in this outcome (RR 1.00, 95% CI 0.92 to 1.08; P value 0.99, I² = 27%) (Analysis 1.2).
1.2. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 2 Overall success rate.
3. Number of attempts until success
Usable data were obtained from two trials including 471 participants (Alic 2009; Fragou 2011). Data from two trials (Gualtieri 1995; Palepu 2009) could not be used, as no standard deviation (SD) was reported. No evidence showed a difference between landmark and direct puncture ultrasound in the number of attempts needed to succeed (mean difference (MD) ‐0.38, 95% CI ‐1.26 to 0.50; P value 0.39, I² = 92%) (see Analysis 1.3). The quality of the evidence was very low (Table 1). A comparison of short and long axis approaches was not possible, as insufficient data were given (Fragou 2011) and the standard deviation was not provided. For use of Doppler guidance, the number of attempts until success was reported in only one trial (Branger 1995).
1.3. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 3 Number of attempts until success.
4. Number of participants with an arterial puncture
This was reported in three trials including 498 participants (Fragou 2011; Gualtieri 1995; Palepu 2009). Direct ultrasound significantly reduced the risk of arterial puncture (RR 0.21, 95% CI 0.06 to 0.82; P value 0.02, I² = 0%) (see Analysis 1.4). The quality of the evidence was low (Table 1). The number of participants with an arterial puncture was reported in three trials (Bold 1998; Branger 1994; Lefrant 1998), but only Lefrant 1998 could be used for analysis because no arterial punctures were performed in the other two studies.
1.4. Analysis.
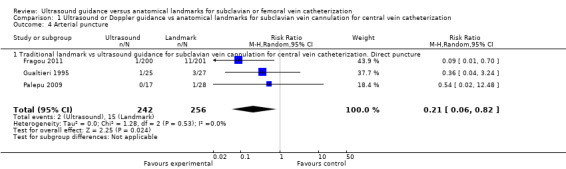
Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 4 Arterial puncture.
5. Number of participants with significant haematoma formation
The number of participants with significant haematoma formation was reported in three trials including 498 participants (Fragou 2011; Gualtieri 1995; Palepu 2009). Direct ultrasound significantly reduced the risk of haematoma (RR 0.26, 95% CI 0.09 to 0.76; P value 0.01, I² = 0%) (see Analysis 1.5). The quality of the evidence was moderate. None of the trials of Doppler ultrasound reported this outcome.
1.5. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 5 Haematoma formation.
6. Number of participants with other complications
The number of participants with other complications was reported in three trials using direct ultrasound including 498 participants (Fragou 2011; Gualtieri 1995; Palepu 2009) and in three trials using Doppler ultrasound including 560 participants (Bold 1998; Branger 1994; Lefrant 1998). The quality of the evidence was very low (Table 1). For use of ultrasound (two‐dimensional (US) or Doppler ultrasound (USD))‐guided puncture techniques, no evidence of a difference in this outcome was found (RR 0.29, 95% CI 0.07 to 1.21; P value 0.09, I² = 60%) (see Analysis 1.6). For use of direct ultrasound (two‐dimensional (US))‐guided puncture, no evidence showed a difference in this outcome (RR 0.18, 95% CI 0.01 to 4.73; P value 0.31, I² = 80%) (see Analysis 1.6). For use of a direct Doppler ultrasound (USD))‐guided puncture technique, no evidence revealed a difference in this outcome (RR 0.35, 95% CI 0.09 to 1.45; P value 0.15, I² = 33%) (see Analysis 1.6).
1.6. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 6 Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury).
Regarding comparison 1.6 (other complications), we conducted a sensitivity analysis to give greater weight to the studies by Fragou et al (2011) and Lefrant et al (1998), that is, both studies were larger in terms of most of the events. When models were fitted with fixed‐effect models, the treatment effect was slightly more in favour of ultrasound guidance, however with much higher imprecision reflected by larger 95% confidence intervals. Thus, we still derive a corresponding advantage for ultrasound guidance, however more cautiously so.
7. Time to successful cannulation
Times were reported in two trials using direct ultrasound including 471 participants: Alic 2009 (time to catheterization) and Fragou 2011 (time between penetration of skin and aspiration of venous blood into the syringe). No evidence was found of a difference in this outcome (MD 10.48 seconds, 95% CI ‐56.92 to 77.87; P value 0.76, I² = 81%) (see Analysis 1.7). The quality of the evidence was low. This outcome was reported in only two trials using Doppler ultrasound (USD) (Branger 1995; Lefrant 1998); only Branger 1995 could be used for analysis because the standard deviation was missing from the other study.
1.7. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 7 Time to successful cannulation.
8. Success on first attempt
This outcome was reported in two trials (Alic 2009; Palepu 2009). No evidence suggested a difference in this outcome (RR 1.08, 95% CI 0.85 to 1.36; P value 0.53, I² = 0%) (see Analysis 1.8). The quality of the evidence was high (Table 1). A comparison of short and long axis approaches was not possible, as only in the study from Palepu (Palepu 2009) (transverse (short axis) view) was the success rate on the first attempt given. This outcome was reported in only one trial using Doppler ultrasound (USD) (Lefrant 1998).
1.8. Analysis.

Comparison 1 Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization, Outcome 8 Success with attempt number 1.
Section B. Femoral vein catheterization. Landmark technique versus two‐dimensional ultrasound
The quality of the evidence was moderate to low for all outcomes.
1. Total number of perioperative and postoperative complications/adverse events
This was reported in only one trial (Prabhu 2010).
2. Overall success rate
This was reported in four trials including 311 participants (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010). A small increase in the overall success rate was reported (RR 1.11, 95% CI 1.00 to 1.23; P value 0.06, I² = 50%) (see Analysis 2.1). The quality of the evidence was moderate (Table 2).
2.1. Analysis.

Comparison 2 Ultrasound guidance vs anatomical landmarks for femoral vein cannulation for central vein catheterization, Outcome 1 Overall success rate.
3. Number of attempts until success
This was reported in only one trial (Prabhu 2010).
4. Number of participants with an arterial puncture
This was reported in four trials (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010). No evidence of a difference was found (RR 0.40, 95% CI 0.14 to 1.16; P value 0.09, I² = 39%) (see Analysis 2.2). The quality of the evidence was low (Table 2).
2.2. Analysis.

Comparison 2 Ultrasound guidance vs anatomical landmarks for femoral vein cannulation for central vein catheterization, Outcome 2 Arterial puncture.
5. Number of participants with significant haematoma formation
None of the trial authors reported this outcome.
6. Number of participants with other complications
This was reported in four trials (Aouad 2010; Iwashima 2008; Kwon 1997; Prabhu 2010), but only Kwon 1997 and Prabhu 2010 could be used for analysis because no events were reported in the other two studies. No evidence of a difference was found (RR 0.49, 95% CI 0.11 to 2.12; P value 0.34, I² = 0%) (see Analysis 2.3). The quality of the evidence was low (Table 2).
2.3. Analysis.
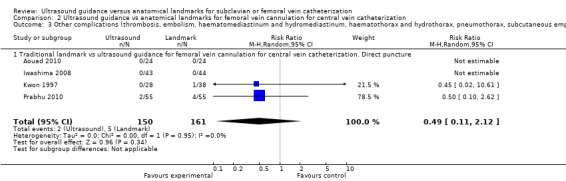
Comparison 2 Ultrasound guidance vs anatomical landmarks for femoral vein cannulation for central vein catheterization, Outcome 3 Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury).
7. Time to successful cannulation
This was reported in two trials (Aouad 2010; Kwon 1997), but only Kwon 1997 could be used for analysis because the standard deviation was missing from the other study.
8. Success on first attempt
This was reported in three trials including 224 participants (Aouad 2010; Kwon 1997; Prabhu 2010). Ultrasound used during puncture increased the rate of success on the first attempt (RR 1.73, 95% CI 1.34 to 2.22; P value < 0.0001, I² = 31) (see Analysis 2.4). The quality of the evidence was high (Table 2).
2.4. Analysis.

Comparison 2 Ultrasound guidance vs anatomical landmarks for femoral vein cannulation for central vein catheterization, Outcome 4 Success with attempt number 1.
We did not perform all planned subgroup analyses. For instance, it was not possible to separate out the experience of practitioners, as this varied across trials. In 11 of 12 trials, the level of experience in performing the procedures was stated (not in Iwashima 2008). The level of detail varied from 'technically inexperienced house officers' (Thompson 1994) or 'experienced in both techniques' (Alic 2009) up to very clear descriptions (Aouad 2010; Bold 1998; Gualtieri 1995). The definitions of both 'experienced' and 'inexperienced' operators varied widely. Both Fragou (Fragou 2011) and Bold (Bold 1998) characterized their operators as 'experienced.' However, the descriptions vary. Fragou states: 'All physicians who performed the procedures had at least >6 yrs of experience in central venous catheter placement,' whereas Bold appears to suggest more recent training: '..highly experienced fellows from the Department of Surgical Oncology (postgraduate year 6‐10). Eighteen physicians participated in the study, inserting from 1 to 27 catheters each (median, 13 catheters). All physicians underwent rigorous instruction in the use of the SmartNeedle and had demonstrated competence in the use of the Doppler probe and appropriate recognition of vascular flow signal characteristics prior to initiation of the study.' Similarly, for 'inexperienced' operators, Lefrant stated: '... operator was not trained in Doppler guidance before the beginning of this study' (Lefrant 1998), and Aouad wrote: '... anesthesia resident with no experience in US guidance and minimal experience with femoral line insertion using the landmark technique attempted cannulation under the supervision of a cardiac anaesthesiologist. The residents were instructed about the use of US guidance for femoral line insertion by watching 3 cases before the beginning of the study' (Aouad 2010).
Likewise, we did not perform a sensitivity analysis of 'high‐quality' versus 'low‐quality' studies, as almost all of the included studies had unclear risk of bias. For example, in no study was the outcome assessor blinded; in only six studies was an adequate sequence generation or adequate allocation concealment reported. Inclusion and exclusion criteria were clearly defined in only eight studies, and treatment and control groups were adequately described at entry in only three studies.
Discussion
Summary of main results
Our analyses of available data suggest that two‐dimensional ultrasound improves some, but not all, aspects of the effectiveness and safety of central venous catheter insertion.
For the subclavian vein, two‐dimensional ultrasound reduced the risk of arterial puncture and haematoma formation. No evidence showed a difference in total or other complications, overall or first‐time success rates, the number of attempts until success or time taken to insert the catheter. No evidence of a difference for any outcome was found when Doppler ultrasound was used.
For the femoral vein fewer data were available for analysis. No evidence was found of a difference in complication rates, time taken for insertion, arterial puncture or haematoma formation when two‐dimensional ultrasound was used. However, success on the first attempt was more likely with two‐dimensional ultrasound, and a small increase in the overall success rate was noted.
None of the studies addressed the impact of ultrasound guidance on mortality, length of stay or patient‐reported outcomes such as pain or discomfort during insertion. Last, whether the infection rate is increased by the use of ultrasonic apparatus because the transducer is brought into the puncture field possibly leading to local infection, or whether the reduced number of required puncture attempts, the shorter puncture duration and the smaller numbers of punctures of the arteria carotis and formed haematomas lead to a reduction in the infection rate was investigated by none of the reviewed studies and therefore remains unanswered. It should be paid attention in an aseptic procedure to avoid infections. The current CDC guidelines suggest the use of sterile US cover shields in order to reduce the risk of CLABSI.
Because of missing data, we did not compare the effects of experienced versus inexperienced operators, and so the relative utility of ultrasound in these groups remains unclear, and no data are available on use of the technique in patients at high risk of complications.
The following points should be taken into account to keep the complication rate low upon application of the ultrasound‐guided technique. Use of US for vascular access requires training (Feller‐Kopman 2007; Resnick 2008). The operator should learn the physical fundamentals of the procedure and its limitations and should learn to deal with the equipment used (image optimization, probe manipulation, imaging techniques), the simultaneous handling of the transducer and the presence of the needle both within and outside of the plane (French 2008). He or she should then have the possibility of applying learned principles under the supervision of an experienced colleague. The influence of the operator's experience on the complication rate during the ultrasound guided‐puncture technique could be proved in a variety of studies. Approaches used during the landmark technique should not be disregarded. The needle tip should be visualized at every time point of the puncture to avoid accidental puncture of adjacent arterial vessels or the pleura. Attention should be paid to operator experience in an aseptic procedure to avoid infection. Current Centers for Disease Control and Prevention (CDC) guidelines suggest the use of sterile US cover shields to reduce the risk of central line–associated bloodstream infection (CLABSI).
The results of our analyses must be interpreted with caution for several reasons.
The methodological quality of the evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most trials had unclear risk of bias across the six domains, with many items necessary to judge bias not reported in the studies. Heterogeneity among the studies was significant. Possible causes of this are the various access approaches, patient positions and techniques used for both puncture and cannulation. Another major problem in evaluating the studies was that exact details on training and experience of the operators for each method were absent or inaccurate, and their experience with each method was seldom uniform. Many studies included operators with limited experience in US‐guided vascular access techniques. However, US‐guided vascular access requires training and experience to maximize the benefits of this technique, and even more so to decrease potential complications. Experience with the landmark technique and limited practice with US‐guided vascular access will lead to an underestimation of the potential beneficial effects of the US‐guided technique. Nevertheless, only one study described the 'learning curve' of operators within the study, and this only for the US technique. Additional limitations included the unblinded design (operator bias, outcome assessor bias) and failure to clearly define measured outcomes. It is not clear whether the results mentioned above and the conclusions derived from them are also valid for emergency procedures. Unfortunately none of the studies that we evaluated contains a cost‐benefit analysis for ultrasound guidance. In addition, more than half of the 13 studies reviewed are older than 15 years. So they were performed at a time when the technology of the equipment and experience in dealing with it remained significantly limited.
It will become more difficult to argue for the puncture of different vessels without the use of an ultrasound‐guided technique in the future (Bodenham 2006), as these techniques appear to offer some safety gains. In time, the use of ultrasound for invasive procedures is likely to become as fundamental a part of anaesthetic practice as preoperative fasting (Smith 1997). However, two of our key questions—whether ultrasound improves safety and effectiveness of insertion in patients who are at higher risk of complications, and whether it helps inexperienced practitioners more (or indeed less) than experienced staff—remain unanswered. No evidence was found to suggest whether it should be used from the outset, or whether it should be a 'fall‐back' technique to be used when the landmark approach has failed, and opinions vary (Atkinson 2005; Calvert 2003; Scott 2004; Watters 2002; Muhm 2002). Formal guidance advocating the use of ultrasound‐guided catheterization is available from the US Agency for Healthcare Research and Quality in the United States (Shojania 2001), the National Institute for Health and Care Excellence (NICE) in the UK (NICE 2002), the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists (Troianos 2012) and the American Society of Anesthesiologists (Rupp 2012). Likewise, we do not accept economic arguments against the widespread introduction of ultrasound‐guided methods; although none of our review data allow us to comment further on this, others have explored this aspect in greater detail (Calvert 2003; Calvert 2004; Kinsella 2009).
Overall completeness and applicability of evidence
The 13 included studies recruited patients with a variety of underlying diseases, in a variety of settings, along with a variety of operators (different disciplines and experience); this should increase the applicability of the results.
Our systematic approach to the literature search, study selection and data extraction should have minimized the likelihood of missing relevant studies. Because of our comprehensive search strategy, the additional handsearch and the contact with different companies and experts in the field, we are confident that we have identified all randomized trials comparing ultrasound techniques for subclavian and femoral vein puncture during central venous catheter instillation in adults with landmark‐guided puncture techniques.
Quality of the evidence
The quality of the evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most trials had unclear risk of bias across the six domains, with many items necessary to judge bias not reported in the studies.
We originally planned to undertake exploratory subgroup analysis to find out whether contextual factors (types of operators, settings) or intervention factors (type of protocol or approach) were the cause of the heterogeneity. However, because of the small number of studies and the wide variety of procedures, operators and circumstances under which the cannulations took place, we could not justify performing such analyses.
It is not easy to isolate reasons for heterogeneity because the puncture of vessels and the insertion of catheters is a complex process. It is plausible that discordance in results among studies may be due to contextual factors (differences in patient populations and practice) or to intervention factors. In relation to intervention factors, many methodological differences among the studies may have contributed to heterogeneity. In relation to risk of bias within studies, methodological quality ranged from very low to high. The intervention could not be blinded to personnel; this is understandable. It is plausible therefore that the unblinded nature of the intervention may have prompted a change in behaviour, and this may have affected the results.
The methodological quality of the trials was high at best. Allocation concealment was described adequately in one of the 13 trials. In all studies outcome assessment was not blinded, or it was unclear. Clearly blinding of the operator is not possible in this type of work; however no trial except the one in which the participants were sedated or in narcosis attempted to blind the participant. Clinical heterogeneity in terms of the range of participants and operators studied, the approaches used and the ultrasound machines and probes used was considerable. Further, different studies used different methods and time periods for puncturing the vein and placing the catheter.
Performance of central venous catheterization is clearly dependent on the expertise of the operator for the landmark and for the ultrasound method and technique used. Advances in medicine do not result simply from the availability of new technology but depend on how the technology is actually applied (Guimares 2009). The experience of practitioners and their faculties in both ultrasound techniques and control techniques as well as the number of practitioners involved varied across the trials. In four trials the number of practitioners performing the procedures was not stated. Most trials reported the level of experience of the operator, but the data could not be combined. Furthermore, whatever the experience of the operator, certain 'tacit' factors involved in performing practical procedures are not (and indeed cannot be) recorded in the report of a clinical trial but nevertheless influence the effectiveness and safety of the procedure (Goodwin 2005; Mort 2009). Some of these include non‐technical skills; although less obvious, they are an essential part of expert performance (Smith 2009; Smith 2010; Smith 2011).
The included studies cover a period of 17 years, during which considerable change has occurred in the technology of ultrasound devices and the availability of ultrasound in anaesthetic practice.
Potential biases in the review process
Our systematic approach to searching, study selection and data extraction should have minimized the likelihood of missing relevant studies. A very comprehensive search strategy was applied to identify all potential studies and their reports. However, although 13 studies were identified, several relevant outcome data prespecified in our protocol were not always or were never (participant discomfort) reported. Several of these outcome measures are important for an informed and balanced decision on which technique should be used in which situation. Some of these outcome measures most likely were not ascertained during the trial; however, others could have well been collected but not reported. Unfortunately, even after contacting the primary investigators, to date we have not been able to obtain additional data. We followed the methodology for systematic reviews outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) (e.g. extracting data independently in duplicate to minimize errors and reduce bias) in the process of doing this systematic review.
Because of the lag time between the date of the search (January 2013) and publication of the review, studies of interest may not have been considered. We reran the search in August 2014 and found five eligible studies (Eldabaa 2012; Enany 2013; Lam 2013; Oh 2014; Xu 2013), which are now awaiting classification. We will deal with them when we update the review.
Agreements and disagreements with other studies or reviews
Five meta‐analyses (Calvert 2003; Hind 2003; Keenan 2002; Randolph 1996;Wu 2013) have compared the effectiveness of ultrasound guidance versus the traditional landmark technique for central vein catheterization. Our review includes more recent studies than were included in any of these.
Calvert and Hind et al conducted a meta‐analysis to assess the evidence for clinical effectiveness of ultrasound‐guided central venous cannulation (Calvert 2003; Hind 2003). This meta‐analysis included only studies in which investigators used real‐time two‐dimensional ultrasonography or Doppler needles and probes and compared these methods with the anatomical landmark method of cannulation. The review authors did not report any subgroup analysis, excluded all non‐English language papers and excluded trials with a quasi‐randomized design. The review authors included 18 RCTs that had been published up to 2001.
Their systematic review showed benefit from two‐dimensional ultrasound guidance for subclavian vein catheterization in adults compared with the landmark method. With limited evidence (52 insertions), two‐dimensional ultrasound guidance reduced the relative risk of failed catheter placements by 86% and the relative risk for complications by 90%. When Doppler ultrasound guidance was compared with the landmark method for cannulation of the subclavian vein, results significantly favoured the landmark method for relative risk of failed catheter placement and mean number of seconds to successful catheterization.
Randolph et al conducted a meta‐analysis to evaluate the effects of real‐time ultrasound guidance by using a regular or Doppler ultrasound technique for placement of central venous catheters (Randolph 1996). They included eight RCTs that had been published between 1990 and 1995. Studies were included if they were randomized clinical trials of adult or paediatric participants that evaluated real‐time ultrasound (USD or US). Their results were similar to those of the previous meta‐analysis.
Keenan et al (Keenan 2002) evaluated a total of 18 trials of US or USD in comparison with the landmark technique for central venous catheter insertion. Their subgroup analysis for subclavian catheters included only five studies, and they found no differences in insertion success rates and complication rates, as well as no difference in rates of arterial puncture.
A recent meta‐analysis from Wu and colleagues (Wu 2013) compared the use of anatomical landmark techniques for central venous cannulation versus real‐time, two‐dimensional ultrasound guidance, but it did not include all of the outcomes we have used and did not include Doppler mode studies or those that adopted an 'indirect' approach.
Authors' conclusions
Implications for practice.
Several important implications for practice have arisen from our systematic review and meta‐analysis.
Our systematic review shows the beneficial effects of using two‐dimensional ultrasound techniques for cannulation of the subclavian vein on the risk of accidental arterial puncture and on the risk of haematoma formation. It shows also the beneficial effects of using two‐dimensional ultrasound techniques for cannulation of the femoral vein on success with the first attempt and the overall success rate.
Our systematic review does not generally support the use of ultrasound guidance for insertion of subclavian or femoral catheters.
Implications for research.
In many studies important details were not described in sufficient detail. These include the nature of the landmarks used, the experience of the person inserting the catheter and some of the outcomes. Furthermore, important outcomes such as patient‐reported outcomes, infection (at the site of insertion or in the bloodstream) and bleeding and haematoma formation in patients with coagulopathy have not been addressed. Likewise, it would be possible to compare 'in‐plane' and 'out‐of‐plane' approaches.
However, two of our key questions—whether ultrasound improves safety and effectiveness of insertion in patients who are at higher risk of complications, and whether it helps inexperienced practitioners more (or indeed less) than experienced staff—remain unanswered. Further, differences in infection rates with and without ultrasound should be sought. Future studies should also compare techniques used in the emergency setting (including in those with poor or absent pulses) and those performed by operators equally experienced in both techniques. It would also be useful to know whether arterial puncture and haematoma are less likely in patients with disorders of coagulation.
Opinions are divided over whether further trials are actually necessary. Some argue that current evidence is sufficient to support the use of ultrasound (Bodenham 2006; Scott 2004). However, given that the studies we have identified are not of optimum quality and do not address all unanswered questions about the technique, we believe that this view is premature and is somewhat nihilistic. Future trials should be designed with the methodological issues we have highlighted in this review in mind, as well as the gaps in knowledge that need to be filled. A broader, mixed‐methods approach might be better suited to some aspects of this complex intervention, incorporating process evaluation to understand how context influences outcome and to provide insights to aid implementation in other settings. In addition, an economic evaluation that takes into consideration the cost‐effectiveness of the method (previously largely neglected with one exception (Calvert 2003)), not only from the payer's perspective but also from perspective of service users and of society as a whole, would be useful for decision makers.
What's new
| Date | Event | Description |
|---|---|---|
| 13 December 2018 | Amended | Editorial team changed to Cochrane Emergency and Critical Care |
History
Review first published: Issue 1, 2015
| Date | Event | Description |
|---|---|---|
| 28 May 2010 | Amended | Contact details updated |
| 4 November 2008 | Amended | List of review authors changed |
Acknowledgements
We would like to thank Harald Herkner (content editor); Nathan Pace (statistical editor); and Andrew Davidson, Bernard Cornel, Massimo Lamperti and Cliff Shelton (peer reviewers) for help and editorial advice provided during preparation of this systematic review. Many special thanks to Jane Cracknell for her great patience, help and editorial advice during preparation of this systematic review and protocol.
We would also like to thank Harald Herkner, Daniel Hind, Bernard Coronel, Janet Wale and Mark Edward for help and editorial advice provided during preparation of the protocol for the review, and Karen Hovhannisyan for help in preparing the search strategies.
We would like to acknowledge Prof. Dr. med. Ulf Börner's contribution to the protocol (Brass 2008). Prof. Dr. med. Ulf Börner was listed as an author of the protocol for a systematic review before the time of his death in 2008.
Appendices
Appendix 1. Search strategy for CENTRAL (Wiley Interscience)
#1 MeSH descriptor Catheterization, Central Venous explode all trees #2 MeSH descriptor Central Venous Pressure explode all trees #3 central venous line* #4 central venous pressure:TI,AB #5 (venous or vein*) near (cannulation or access or catheter*) #6 pulmonary art* flotation* #7 central line* insertion* #8 hickman near line* #9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8) #10 MeSH descriptor Ultrasonics explode all trees #11 MeSH descriptor Ultrasonography explode all trees #12 (imag* near guid*) #13 (ultrasound* or ultrasonic* or doppler) #14 (#10 OR #11 OR #12 OR #13) #15 (#9 AND #14)
Appendix 2. Search strategy for MEDLINE (Ovid SP)
1. (zentralveno?s* kathet* or (venostrom* or venenkathe*) or hickman line* or central line* insertion* or pulmonary arter* flotation* or ((venous or vein*) adj4 (cannulation or access or catheter* puncture)) or central venous line* or central venous pressure).mp. or exp Venous Cutdown/ or Central Venous Pressure/ or exp Catheterization Central Venous/ 2. (ultrasound* or ultrasonic* or Doppler or echography or ultrasonograpgh*).mp. or exp Ultrasonography Doppler Color/ or exp Echocardiography Doppler/ or exp Ultrasonography/ or exp Ultrasonics/ 3. 1 and 2 4. ((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or drug therapy.fs. or randomly.ab. or trial.ab. or groups.ab.) not (animals not (humans and animals)).sh. 5. 3 and 4
Appendix 3. Search strategy for EMBASE (Ovid SP)
1. central venous catheterization/ or central venous pressure/ or zentralveno?s* kathet*.mp. or (venostrom* or venenkathe*).mp. or hickman line*.mp. or central line* insertion*.mp. or pulmonary arter* flotation*.mp. or ((venous or vein*) adj4 (cannulation or access or catheter* puncture)).mp. or central venous line*.mp. or central venous pressure.mp. 2. ultrasound/ or explode echography/ or (ultrasound* or ultrasonic* or Doppler or echography or ultrasonograpgh*).mp. 3. 1 and 2 4. (randomized‐controlled‐trial/ or randomization/ or controlled‐study/ or multicenter‐study/ or phase‐3‐clinical‐trial/ or phase‐4‐clinical‐trial/ or double‐blind‐procedure/ or single‐blind‐procedure/ or (random* or cross?over* or factorial* or placebo* or volunteer* or ((singl* or doubl* or trebl* or tripl*) adj3 (blind* or mask*))).ti,ab.) not (animals not (humans and animals)).sh. 5. 3 and 4
Appendix 4. Search strategy for CINAHL (EBSCOhost)
S1 ( (MH "Catheterization, Peripheral Central Venous") OR (MH "Central Venous Pressure") OR (MH "Venous Cutdown") ) OR ( (zentralveno?s* kathet* or (venostrom* or venenkathe*) or hickman line* or central line* insertion* or pulmonary arter* flotation* or ((venous or vein*) and (cannulation or access or catheter* puncture)) or central venous line* or central venous pressure) ) S2 ( (MH "Ultrasonography, Doppler, Color") OR (MH "Echocardiography, Doppler") OR (MH "Ultrasonography") OR (MH "Ultrasonics") ) OR AB ( ultrasound* or ultrasonic* or Doppler or echography or ultrasonograpgh* ) S3 S1 and S2
Appendix 5. Search strategy for GRIPWEB search (DIMDI)
1 KL97; SM78; SPPP; SP97; CA66; CL63; MEOO; ME66; MEOA; ME6O; T165; MK77; GE79; EU93; PX97; PY81; HN69; CB85; SU88; SV88; AZ72; EM74; EM83; EM9O; PT85; TV01 2 ct d ultrasonics 3 ft=(ultrasound; ultrasonic) 4 ct d ultrasonography 5 cc d A##lus 6 cc d A1/us 7 cc d A2/us 8 cc d A3/us 9 cc d A4/us 10 cc d A5/us 11 cc d A6/us 12 cc d A7/us 13cc d A8/us 14 cc d A9/us 15 cc d A14/us 16 cc d c1/us 17 cc d c2/us 18 cc d c3/us 19 cc d c4/us 20 cc d c5/us 21 cc d c6/us 22 cc d c7/us 23 cc d c8/us 24 cc d c9/us 25 cc d c10us 26 cc d c11/us 27 cc d c12/us 28 cc d c13/us 29 cc d c14/us 30 cc d e15/us 31 cc d c16/us 32 co d e17/us 33 cc d c18/us 34 cc d c19/us 35 cc d c20/us 36 co d c21/us 37 cc d c23/us 38 cc d f3/us 39 ct d catheterization 40 ct=venous cutdown 41 ft=(vein cutdown; venostom?; venenkathe?) 42 ft=(central venous cathe?; zentralveno#s?kath?) 43 (cathether AND venous) /same sent 44 (Kathe? AND ven?) /same sent 45 (cathet? AND ven?) /same sent 46 S=45 OR S=44 OR S=43 OR S=42 OR S=41 OR S=40 OR S=39 47 S=46 OR S=38 OR S=37 OR S=36 OR S=35 OR S=34 OR S=33 OR S=32 OR S=31 OR S=30 OR S=29 OR S=28 OR S=27 OR S=26 OR S=25 OR S=24 OR S=23 OR S=22 OR S=21 OR S=20 OR S=19 OR S=18 OR S=17 OR S=16 OR S=15 OR S=14 OR S=13 OR S=12 OR S=11 OR S=10 OR S=9 OR S=8 OR S=7 OR S=6 OR S=5 OR S=4 OR S=3 OR S=2 48 S=47 AND S=46 49 48 AND (study; studie#) 50 49 AND (zufall?; random?) 51 50 and prospe#tiv? 52 CT="RANDOMIZED CONTROLLED TRIAL" 53 CT="CLINICAL TRIAL" 54 CT="CENTRAL VENOUS CATHETER" 55 CT=' PROSPECTIVE STUDIES" 56 CT="CATHETERIZATION" 57 CT="CATHETERIZATION, CENTRAL VENOUS" 58 CT="PROSPECTIVE STUDY" 59 S=58 OR S=57 OR S=56 OR S=55 OR S=54 OR S=53 OR S=52 60 S=59 AND S=51 61 check duplicates: unique in s=60 62 doppler/(ti; ct; ab) 63 vein puncture 64 venous puncture 65 cannulation 66 zentralveno#ese punktion 67 S=66 OR S=65 OR S=64 OR S=63 68 ultras? 69 S=68 OR S=62 70 67 AND 69 71 70 NOT 61 72 71 AND (studie#; study) 73 check duplicates: unique in s=72 74 73 AND Prospe#tiv?
Data and analyses
Comparison 1. Ultrasound or Doppler guidance vs anatomical landmarks for subclavian vein cannulation for central vein catheterization.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Complication rate total | 6 | 1478 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.23, 1.17] |
| 1.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct and indirect puncture | 3 | 918 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.17, 1.91] |
| 1.2 Traditional landmark vs Doppler guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 560 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.15, 1.09] |
| 2 Overall success rate | 8 | 1809 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.97, 1.13] |
| 2.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct and indirect puncture | 5 | 1389 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.96, 1.20] |
| 2.2 Traditional landmark vs Doppler guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 420 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.92, 1.08] |
| 3 Number of attempts until success | 2 | 471 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.26, 0.50] |
| 3.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 2 | 471 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.26, 0.50] |
| 4 Arterial puncture | 3 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.06, 0.82] |
| 4.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.06, 0.82] |
| 5 Haematoma formation | 3 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.09, 0.76] |
| 5.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.09, 0.76] |
| 6 Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) | 6 | 1058 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.07, 1.21] |
| 6.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 4.73] |
| 6.2 Traditional landmark vs Doppler guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 3 | 560 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.09, 1.45] |
| 7 Time to successful cannulation | 2 | 471 | Mean Difference (IV, Random, 95% CI) | 10.48 [‐56.92, 77.87] |
| 7.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture. Time between penetration of skin and aspiration of venous blood into the syringe | 2 | 471 | Mean Difference (IV, Random, 95% CI) | 10.48 [‐56.92, 77.87] |
| 8 Success with attempt number 1 | 2 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.85, 1.36] |
| 8.1 Traditional landmark vs ultrasound guidance for subclavian vein cannulation for central vein catheterization. Direct puncture | 2 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.85, 1.36] |
Comparison 2. Ultrasound guidance vs anatomical landmarks for femoral vein cannulation for central vein catheterization.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Overall success rate | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [1.00, 1.23] |
| 1.1 Traditional landmark vs ultrasound guidance for femoral vein cannulation for central vein catheterization. Direct puncture | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [1.00, 1.23] |
| 2 Arterial puncture | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.16] |
| 2.1 Traditional landmark vs ultrasound guidance for femoral vein cannulation for central vein catheterization. Direct puncture. | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.16] |
| 3 Other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.11, 2.12] |
| 3.1 Traditional landmark vs ultrasound guidance for femoral vein cannulation for central vein catheterization. Direct puncture | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.11, 2.12] |
| 4 Success with attempt number 1 | 3 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.34, 2.22] |
| 4.1 Traditional landmark vs ultrasound guidance for femoral vein cannulation for central vein catheterization. Direct puncture | 3 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.34, 2.22] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alic 2009.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: no details in the text Congress poster |
|
| Participants | ICU patients Inclusion and exclusion criteria not clearly defined in the text Treatment and control groups not adequately described at study entry Admission details not described, only “equal demographic data” No information on whether participants were anaesthetised, sedated or awake Operators: number: 1. All procedures were performed by the same physician Experience: who was experienced in both techniques |
|
| Interventions | Technique: LM: no details vs US: no details LM Unclear whether direct or indirect puncture Technique standardized: unclear Head‐up (anti‐Trendelenburg/down (Trendelenburg)/flat head rotation no details) Seldinger technique: catheter over needle, no details Vessel and side: SV no details US Direct puncture Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique: catheter over needle, no details Vessel and side: SV no details |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Number of attempts until success (n, SD) Complication rate total (n) Time to successful cannulation (seconds) Success with attempt number 1 (n, %) Outcome measures not defined |
|
| Notes | No cross‐over landmark‐guided puncture or ultrasound‐guided puncture Congress poster |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Prospectively randomized controlled trial (RCT) Randomization method: no details in the text |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Unclear _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Unclear _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Aouad 2010.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: Participants were randomly assigned using a computer‐generated table of random numbers to group LM or US. Results of randomization were concealed in sealed opaque envelopes and were opened after participants provided consent. Of note, our study was not sufficiently powered to detect any differences in the incidence of femoral artery puncture (A) |
|
| Participants | A total of 48 children birth to 12 years of age, ASA physical status III or IV, with congenital heart disease undergoing cardiac surgery were enrolled in a prospective randomized clinical trial. Exclusion criteria were haemodynamic instability and allergy to the US gel Inclusion and exclusion criteria clearly defined in the text Treatment and control groups adequately described at study entry. Minimum of 4 admission details described. 5 admission details described (sex, weight, height, age, underlying disorders) Participants were anaesthetized Operators: number: no details Experience: A CA‐3‐level anaesthesia resident with no experience in US guidance and minimal experience with femoral line insertion using the landmark technique attempted cannulation under the supervision of a cardiac anaesthesiologist. Residents were instructed on the use of US guidance for femoral line insertion by watching 3 cases before the beginning of the study |
|
| Interventions | Technique: LM: See text vs US: 10‐ to 5‐MHz ultrasound covered by a sterile sheath LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein right side US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein right side |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %): Shifting to the opposite side was considered a failure of insertion Number of attempts until success (n) Arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Time to successful cannulation (seconds): Time to successful wire insertion was calculated from the time of skin penetration until successful wire insertion, time from wire insertion to complete cannulation with the triple‐lumen catheter was calculated, time to complete cannulation was the sum of both times Success with attempt number 1 (n, %) |
|
| Notes | No cross‐over landmark‐guided puncture or ultrasound‐guided puncture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization method: computer‐generated table |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes opened after participants' consent was received |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | Low risk | Yes |
Bold 1998.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: computer‐generated block randomization 240 participants were enrolled in the study. Participants were stratified for 3 known risk factors: (1) prior surgery in the subclavian vein region, (2) prior radiotherapy at the attempted catheterization site and (3) an abnormal weight‐height ratio |
|
| Participants | At our institution, 8 to 20 patients per day undergo subclavian vein catheter insertion in a dedicated procedure suite The primary indication for placement of long‐term venous access catheters in our participants is administration of chemotherapy. All catheters were inserted under sterile, non‐emergency, controlled conditions 240 participants were enrolled in the study. All participants had at least 1 factor that may be associated with increased risk for failure or complication (body mass index [determined by weight in kilograms divided by square of the height in meters] of < 20 kg/m2 or > 30 kg/m2, prior surgery in the region adjacent to the subclavian vein or prior radiotherapy at the attempted catheterization site). Participants were stratified with regard to prior surgery within the region of the subclavian vein catheterization (e.g. mastectomy, axillary node dissection, thoracotomy) and body mass index to minimize any effect these confounding variables might have on the success rate Inclusion and exclusion criteria were clearly defined in the text Treatment and control groups were not adequately described at entry 4 admission details described (sex, BMI, age, anatomical distinctiveness) Participants awake Operators: number: 18 Experience: highly experienced fellows from the Department of Surgical Oncology (postgraduate year 6‐10). Eighteen physicians participated in the study, inserting from 1 to 27 catheters each (median, 13 catheters). All physicians underwent rigorous instruction in use of the SmartNeedle and had demonstrated competence in use of the Doppler probe and appropriate recognition of vascular flow signal characteristics before study initiation |
|
| Interventions | Technique: LM: described in the text vs US: SmartNeedle LM Unclear whether direct or indirect puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: SV no details |
|
| Outcomes | Complication rate total, arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Success with attempt number 1 or 2 (n, %) Success rate after cross‐over (n, %) |
|
| Notes | Cross‐over landmark‐guided puncture and ultrasound‐guided puncture LM: If catheterization of the subclavian vein was unsuccessful after 2 attempts, the participant was crossed over to the other catheterization technique. After 4 unsuccessful attempts (2 attempts using each technique), a chest radiograph was obtained to evaluate for complications, and the participant was declared a failure of subclavian vein cannulation 21 LM → 18 (85.7%) success with SN US: If catheterization of the subclavian vein was unsuccessful after 2 attempts, the participant was crossed over to the other catheterization technique. After 4 unsuccessful attempts (2 attempts using each technique), a chest radiograph was obtained to evaluate for complications, and the participant was declared a failure of subclavian vein cannulation 34 SN → 27 (79.4%) success with LM |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Prospectively randomized controlled trial (RCT) Randomization method: computer‐generated block randomization |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Yes _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | Unclear risk | No. 4 admission details described (sex, BMI, age, anatomical distinctiveness) |
Branger 1994.
| Methods | Controlled clinical trial (CCT) Randomization method: predetermined list; no other details in the text (C) |
|
| Participants | Consecutive patients requiring central venous catheter for haemodialysis, apheresis or parenteral nutrition; patients with known risk factors were excluded Inclusion and exclusion criteria not clearly defined in the text Treatment and control groups not adequately described at study entry No admission details described Participants awake Operators: number: no details Experience: junior residents, senior staff members (LM 6J 4S, US 5J 6S) |
|
| Interventions | Technique: LM: no details vs US: 5 MHz with needle guide, developed by study authors LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: IJV and SV no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: IJV and SV side no details |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %): failure defined in the text; see text Complication rate total, arterial puncture, haematoma formation (n, %) Success rate after cross‐over (n, %) |
|
| Notes | Cross‐over landmark‐guided puncture and ultrasound‐guided puncture LM: cross‐over after failure of initial technique after 30 minutes 3 LM → 2 (66.7%) successes with US US: cross‐over after failure of initial technique after 30 minutes 1 Do → (100%) success with senior |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomization method: predetermined list; no other details in the text |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Branger 1995.
| Methods | Controlled clinical trial (CCT) Randomization method: 100 consecutive patients with subclavian vein catheterization and 30 patients with IJV catheterization were included in the study. The choice of the vessel, puncture site and catheter was made according to the patient's history and clinical status before the non‐Doppler or Doppler technique was selected from random tables (with separate tables for subclavian and IJV catheterization) |
|
| Participants | Consecutive patients requiring central venous catheter for haemodialysis, apheresis or parenteral nutrition; patients with known risk factors such as thoracic abnormality, respiratory distress, major obesity or restlessness were excluded Inclusion and exclusion criteria not clearly defined in the text Treatment and control groups not adequately described at study entry 2 admission details described (sex, age) Participants awake and anaesthetized Operators: number: 22 Experience: 14 junior residents (postgraduate students < 5 years of clinical experience), 8 senior staff members (> 5 years of clinical experience), members of the nephrology, emergency and intensive care departments. They were taught the Doppler technique over a 2‐week period by the 2 senior members, who were previously involved in animal experimental study; participants had to achieve at least 1 venous catheterization with the non‐Doppler technique and with the Doppler technique before entering the study. The operator for each venous catheterization was chosen according to a random table (LM 10J 5S, US 6J 8S) |
|
| Interventions | Technique: LM: no details vs US: hand‐held pulsed Doppler probe for co‐axial guidance of the puncture needle and a dedicated 4‐MHz pulsed Doppler, probe sterilized, developed by study authors LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: IJV and SV no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: IJV and SV side no detail |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %): failure defined as inability to obtain venous blood after longer than 30 minutes after the onset of local anaesthesia or after more than 4 attempts at venous puncture Number of attempts until success (n, SD) Time to successful cannulation (seconds) Success rate after cross‐over (n, %) |
|
| Notes | Cross‐over landmark‐guided puncture and ultrasound‐guided puncture LM: cross‐over after failure of initial technique In case of failure of the initial attempt at catheterization by the non‐Doppler technique, the operator was allowed to use the Doppler technique 1 J LM → 1 (100%) success with Doppler 4 S LM → 2 (50%) success with Doppler US: cross‐over after failure of initial technique In case of failure of the Doppler technique used by a junior staff member, a senior staff member was asked to perform Doppler venous catheterization 1 J Do → 1 (100%) success with senior |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled clinical trial (CCT) Randomization method: random tables (C) |
| Allocation concealment (selection bias) | Unclear risk | Controlled clinical trial (CCT) Randomization method: random tables (C) |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: Yes _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Fragou 2011.
| Methods | Prospectively randomized controlled trial (RCT) Computer‐generated random numbers table (A); patients were stratified with regard to age, gender and body mass index. Block randomization was used to ensure equal numbers of patients in these groups 29% of patients in the ultrasound group were not in the Trendelenburg position as a result of increased intracranial pressure; however, catheterization was attempted in these cases. 42 patients who were not in the Trendelenburg position as a result of increased intracranial pressure and 20 patients in whom cannulation was not possible as a result of thrombosis, in the landmark group, were converted to the ultrasound group and were excluded from the analysis. Hence, only 401 patients were included in the final analysis. Notably, several patients in the landmark group were converted to the ultrasound group and were excluded from the analysis (e.g. patients who were not in the Trendelenburg position as a result of increased intracranial pressure) |
|
| Participants | Sedated and mechanically ventilated critical care patients. Catheterization was performed under non‐emergency conditions in the intensive care unit. 463 enrolled, 401 included in the final analysis Inclusion and exclusion criteria clearly defined in the text Treatment and control groups adequately described at entry. Minimum of 4 admission details described. 6 admission details described (sex, BMI, age, underlying disorders, coagulation status, anatomical distinctiveness) Participants sedated Operators: number: no details Experience: All physicians who performed the procedures had at least 6 years of experience in central venous catheter placement |
|
| Interventions | Technique: LM: well described in the text, with finder needle Notably, all participants underwent ultrasound scanning of the infraclavicular area to look for the presence of venous thrombosis. Participants in whom cannulation was not possible with the landmark method as a result of thrombosis were excluded from the study and subsequently had the procedure performed with ultrasound on the contralateral side. vs US: 7.5‐MHz US, probe wrapped in a sterile sheath LM Unclear whether direct or indirect puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details 29% not in the Trendelenburg position 29% of participants in the ultrasound group were not in the Trendelenburg position as a result of increased intracranial pressure; however, catheterization was attempted in these cases. 42 participants who were not in the Trendelenburg position as a result of increased intracranial pressure and 20 participants in whom cannulation was not possible as a result of thrombosis, in the landmark group, were converted to the ultrasound group and were excluded from the analysis. Hence, only 401 participants were included in the final analysis. Notably, several participants in the landmark group were converted to the ultrasound group and were excluded from the analysis (e.g. participants who were not in the Trendelenburg position as a result of increased intracranial pressure) Seldinger technique Vessel and side: SV no details |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Number of attempts until success (n, SD): average number of attempts before successful placement (defined as separate skin punctures) Complication rate total, arterial puncture (subclavian artery puncture was noted by forceful pulsatile expulsion of bright red blood from the needle), local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Time to successful cannulation (seconds): Access time was defined as the time between penetration of skin and aspiration of venous blood into the syringe. Preparation times for both techniques were not similar, taking into account that in the ultrasound group 118 ± 23 seconds was added in as a result of scanning the area before performing the actual penetration |
|
| Notes | No cross‐over landmark‐guided puncture and ultrasound‐guided puncture In most participants in whom the first attempt (1 pass of the introducing needle) at catheterization failed, another physician made the next attempt |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table; participants were stratified with regard to age, gender and body mass index. Block randomization was used to ensure equal numbers of participants in these groups |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcomes of participants who withdrew or were excluded after allocation were NEITHER detailed separately NOR included in an intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | Participant selection: Yes _X_ Withdrawals: Unclear _X_ Postrandomization exclusion: Yes _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | Low risk | Yes |
Gualtieri 1995.
| Methods | Prospectively randomized controlled trial Randomization method: random number table (A) |
|
| Participants | 53 placement procedures were attempted in 33 critically ill adult patients from the combined trauma‐surgical‐medical intensive care unit 1 procedure was excluded from data analysis Patients were excluded from the study if they required central venous access after cardiopulmonary arrest and other emergency situations, or when informed Inclusion and exclusion criteria not clearly defined in the text Treatment and control groups not adequately described at study entry Admission details not described, only “equal demographic data” No admission details described Participants anaesthetized or sedated Experience: All residents were in year 1 or 2 of their postgraduate study. Operators who had placed < 30 CVCs were supervised by an experienced physician |
|
| Interventions | Technique: LM: standard infraclavicular approach vs US: 7.5‐MHz ultrasound device (SiteRite) covered with a sterile sheath, needle guide used LM Unclear whether direct or indirect puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique: catheter over needle, no details Vessel and side: SV no details US Direct puncture Technique standardized Head down (Trendelenburg), head rotation, no details Seldinger technique: catheter over needle, no details Vessel and side: SV no details |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Number of attempts until success (n) Complication rate total, arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Success rate after cross‐over (n, %): In the landmark group, if venipuncture did not occur after 3 attempts by the less experienced operator, ultrasound salvage was attempted by the same operator. The number of venipuncture attempts with ultrasound was also recorded. If after 3 attempts with ultrasound venipuncture was not accomplished, the physician investigator attempted the procedure using ultrasound Outcomes measures not defined |
|
| Notes | Cross‐over landmark‐guided puncture: cross‐over after failure of initial technique 15 LM → cross‐over 12 (80%) successes with US No cross‐over ultrasound‐guided puncture |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization method: random number table (A) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcomes of participants who withdrew or were excluded after allocation were NEITHER detailed separately NOR included in an intention‐to‐treat analysis 1 catheterization attempt was excluded as a result of the participant's extreme agitation and inability to remain quiet, thus making it unsafe to proceed. This participant suffered no complications and did not have a catheter placed by the subclavian vein route |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | High risk | Participant selection: Unclear _X_ Withdrawals: Unclear _X_ Postrandomization exclusion: Yes _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Iwashima 2008.
| Methods | Prospectively quasi‐randomized controlled trial (Q‐RCT ) Randomization method: 87 consecutive patients. Patients were assigned to an ultrasound‐guided (US) group or a landmark‐guided (LM) group on an alternating basis |
|
| Participants | 87 consecutive patients with a median age of 2 years (range 1 month to 19 years) who had congenital or other heart disease Inclusion and exclusion criteria clearly defined in the text Treatment and control groups not adequately described at study entry 4 admission details described (sex, weight, age, underlying disorders). No significant differences in age, weight or gender observed between the 2 groups 82 participants in sedation; 5 participants anaesthetized Operators: number: 2 Experience: The operator and the assistant stood opposite one another. The operator and the assistant observed the monitor while the operator performed the needle puncture |
|
| Interventions | Technique: LM: See text vs US: 12‐MHz ultrasound covered by a sterile sheath LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein no details |
|
| Outcomes | Overall success rate (n, %): Successful access was defined as attempted needle puncture in which the guide wire entered the femoral vein within the first 2 attempts Failure rate (n, %): Lack of success was defined as 3 or more unsuccessful attempts or puncture of the femoral artery Arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Time to successful cannulation (seconds): Procedure time, defined as the time between penetration of the skin and aspiration of venous blood into the syringe, was classified as to whether or not it required less than 5 minutes |
|
| Notes | No cross‐over landmark‐guided puncture and ultrasound‐guided puncture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization method: alternating basis (C) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Yes _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Kwon 1997.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: sequential protocol (C) To allow for a fair comparison of the 2 techniques, a sequential protocol was used. As we perform a similar number of procedures each week, the ultrasound device was used 1 week and the landmark technique was used the following week, alternately for 8 weeks |
|
| Participants | Patients undergoing femoral vein cannulation for acute haemodialysis access were studied prospectively Inclusion and exclusion criteria not clearly defined in the text Treatment and control groups not adequately described at study entry 4 admission details described (sex, weight, age, underlying disorders) Participants awake Operators: number: 2 Experience: Operators had more than 4 years of extensive experience in landmark‐guided femoral vein access |
|
| Interventions | Technique: LM: described in the text vs US: 7.5‐MHz ultrasound, covered by a sterile sheath LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique: catheter over needle, no details Vessel and side: femoral vein no details US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique: catheter over needle, no details Vessel and side: femoral vein no details |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Time to successful cannulation (seconds): Access time was defined as the time between penetration of skin and aspiration of venous blood into the syringe. Total procedure time was defined as the time between the start of localization of femoral vein by ultrasound or external landmark technique and completion of insertion of the guide wire. When multiple sticks were required, only the time when the needle was on the skin or was advanced was taken into account Success with attempt number 1 (n, %) |
|
| Notes | Cross‐over landmark‐guided puncture, no cross‐over ultrasound‐guided puncture 4 of 38 participants randomly assigned to external landmark technique could not be cannulated during 2 needle passes, and hence were crossed over to attempts with ultrasound |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Prospectively randomized controlled trial (RCT) Randomization method: sequential protocol (C) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Yes _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | Unclear risk | No. 4 admission details described (sex, weight, age, underlying disorders) |
Lefrant 1998.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: table of random numbers (C) |
|
| Participants | Inclusion and exclusion criteria clearly defined in the text Treatment and control groups adequately described at study entry. Minimum of 4 admission details described. 6 admission details described (sex, weight, height, BMI, age, underlying disorders) Participants awake, sedated or anaesthetized Operators: number: 1 Experience: Because the operator was not trained in Doppler guidance before the beginning of this study, we looked for a potential effect of training during the study, comparing failure and immediate complication rates during first and second halves of the study |
|
| Interventions | Technique: LM: details described in the text vs US: hand‐held pulsed Doppler probe for co‐axial guidance of the puncture needle and a dedicated 4‐MHz pulsed Doppler, probe sterilized, developed by study authors, see Branger et al LM Unclear whether direct or indirect puncture Technique standardized: yes Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV right side n = 73, left n = 70 US Direct puncture Technique standardized: yes Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV right side n = 105, left n = 38 |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Number of attempts until success (n) Complication rate total, arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Time to successful cannulation (seconds) Success with attempt number 1 (n, %) Outcome measures not defined |
|
| Notes | No cross‐over landmark‐guided puncture or ultrasound‐guided puncture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization method: table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Yes _X_ Withdrawals: Unclear _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Yes _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | Low risk | Yes |
Mansfield 1994.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: block randomization (C) 3 withdrawals: Patients were unable to maintain supine position. Outcomes of patients who were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis |
|
| Participants | Most patients had breast cancer or lymphoma, catheter for administration of chemotherapy All catheters were inserted under controlled, non‐emergency conditions Inclusion and exclusion criteria clearly defined in the text Treatment and control groups not adequately described at study entry 3 admission details described (sex, BMI, anatomical distinctiveness) Participants awake Operators: number: 49 Experience: Physicians inserting the catheters ranged from surgical interns to surgical staff with 12 years of experience, each inserting 1 to 62 catheters in the study |
|
| Interventions | Technique: LM: no details vs US: 7.5‐MHz ultrasound LM Unclear whether direct or indirect puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV right 75% (n = 613), left 25% (n = 208) US Indirect puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: SV right 75% (n = 613), left 25% (n = 208) |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %) Complication rate total (n, %) |
|
| Notes | No cross‐over landmark‐guided puncture or ultrasound‐guided puncture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization method: block randomization (C) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Yes _X_ Withdrawals: Yes _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: Unclear _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No. 3 admission details described (sex, BMI, anatomical distinctiveness) |
Palepu 2009.
| Methods | Randomized controlled trial (RCT) Randomization method: computer‐generated randomization table All patients admitted to ICUs between April 2007 and September 2008 and requiring central venous access as part of their management were enrolled in the study. Patients younger than 18 years of age and those who refused to give consent for inclusion in the study were excluded. As the number of femoral vein catheterizations was small in both groups, they were not included in the analysis |
|
| Participants | Patients requiring central venous catheterization for difficult peripheral venous access, need for invasive haemodynamic monitoring and delivery of inotropic medications or antibiotics in a medical and surgical ICU Inclusion and exclusion criteria clearly defined in the text Treatment and control groups not adequately described at study entry 2 admission details described (sex, age) Admission details not described, only “equal demographic data” Participants awake? ...after giving local anaesthesia... Operators: number: no details Experience: registrars with less than 6 years of experience, consultants with more than 6 years of experience in the field of anaesthesia and critical care |
|
| Interventions | Technique: LM: technique; see picture in the article, without finder needle Cannulation using the landmark technique was performed as per standard guidelines vs US: 6‐ to 13‐MHz ultrasound probe covered with sterile sheath, without finder needle LM Direct puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: Right internal jugular vein (IJV) was the first choice for cannulation. Other sites such as left IJV or left or right subclavian (SCV) or femoral veins were cannulated only if the right IJV was not available for cannulation because of the presence of a previously inserted CVC or dialysis catheter IJV 194 (86,2%): right side 178 (91.8%) SCV 28 (12.4%): right side 23(82.1%) Femoral vein 3 (1.3%) US Direct puncture Technique standardized: unclear Head down (Trendelenburg), head rotation, no details Seldinger technique Vessel and side: IJV 205 (91.1%): right side 182 (88.8%) SCV 17 (7.6%): right side 16 (94.1%) Femoral vein 3 (1.3%) |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %): failure: Operator was unable to cannulate the vein within 3 attempts Number of attempts until success (n, SD): Attempt needle`s entry into the skin and its removal from the skin Complication rate total, arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Success with attempt number 1 (n, %) Success rate after cross‐over (n, %) |
|
| Notes | Cross‐over landmark‐guided puncture, no cross‐over ultrasound‐guided puncture If the initial method was unsuccessful after a maximum of 3 attempts, an alternative method was used, viz., USG was used if the insertion was done by the ALT technique, help was taken from a more experienced operator or an alternative site was chosen LM: 10/10 success with US and 7/7 success on the same side by a more experienced operator |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization table (A) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Low risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
Prabhu 2010.
| Methods | Prospectively randomized controlled trial (RCT) Randomization method: computer‐generated randomization (A) |
|
| Participants | Study on 110 patients requiring dialysis catheters into the femoral vein (FV). All patients requiring FV DC insertion for initiation of dialysis as part of their management between April and November 2008 were enrolled in the study. Excluded were patients 18 years of age, those who had undergone FV catheterization previously on the same side and those who did not give consent for participation in the study Inclusion and exclusion criteria clearly defined in the text Treatment and control groups not adequately described at study entry 2 admission details described (sex, age) Participants awake Operators: number: no details Experience: Operators were classified into 2 groups according to experience. Operators with 6 or fewer years of experience were classified as “registrars,” and operators with more than 6 years of experience were classified as “consultants” |
|
| Interventions | Technique: LM: performed per standard guidelines vs US: 13‐ to 6‐MHz ultrasound covered by a sterile sheath LM Unclear whether direct or indirect puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein right side (N = 52) (96.4%) US Direct puncture Technique standardized: unclear Head up (anti‐Trendelenburg)/down (Trendelenburg)/flat, head rotation, no details Seldinger technique Vessel and side: femoral vein right side (N = 52) (96.4%) |
|
| Outcomes | Overall success rate (n, %) Failure rate (n, %): The procedure was considered a failure if the operator was unable to perform venous catheterization after 3 attempts, with an attempt defined as entry of the introducer needle into the skin and its removal from the skin Number of attempts until success (n, SD) Complication rate total, arterial puncture, local bleeding, haematoma formation, cardiac complications, malpositioned catheter tips, rate of catheter‐related infection, mortality, rate of other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) (n, %) Success with attempt number 1 (n, %) Success rate after cross‐over (n, %) LM: If the initial method was unsuccessful after a maximum of 3 attempts, USG was used. if the insertion was done by ALT technique, help was taken LM: 11 failures: 11/11 (100%) success with US US: In 1 patient from the USG group in whom initial cannulation failed, catheterization had to be done on the other side because the guide wire could not be passed after successful needle puncture under USG guidance |
|
| Notes | Cross‐over landmark‐guided puncture; no cross‐over ultrasound‐guided puncture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization method: computer‐generated randomization (A) |
| Allocation concealment (selection bias) | Unclear risk | No details in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ Outcome assessor blinded: Unclear__X__ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes of participants who withdrew or were excluded after allocation were EITHER detailed separately OR included in an intention‐to‐treat analysis OR the text stated no withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Participant selection: Yes _X_ Withdrawals: No _X_ Postrandomization exclusion: No _X_ Intention‐to‐treat analysis: No _X_ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subject blinded: Unclear__X__ Physician blinded: No__X__ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor blinded: Unclear__X__ |
| Treatment and control groups were adequately described at entry. | High risk | No |
ALT: anatomical landmark‐guided technique.
ASA: American Society of Anesthesiologists.
BMI: body mass index.
CCT: controlled clinical trial.
CVC: central venous catheter.
DC: dialysis catheter.
Do: Doppler.
FV: femoral vein.
ICU: intensive care unit.
IJV: internal jugular vein.
LM: landmark.
Q‐RCT: quasi‐randomized controlled trial.
RCT: randomized controlled trial.
SCV: subclavian vein.
SD: standard deviation.
SN: SmartNeedle.
SV: subclavian vein.
US: ultrasound.
USG: ultrasound‐guided.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Froehlich 2009 | Different vessels were punctured and were statistically analysed together |
| Hilty 1997 | Each participant received bilateral femoral lines, 1 by ultrasound guidance and 1 by the landmark approach (control). Randomization determined which technique and which side would be attempted first. A computer‐generated randomization chart predetermined the choice of initial technique (landmark vs ultrasound) and the initial side of approach (left vs right) |
| Kwon 1996 | Randomization: no details |
| Miller 2002 | Prospectively randomized controlled trial; different vessels were punctured and were statistically analysed together |
| Thompson 1994 | Published twice (Congress poster → article); see Gualtieri 1995 |
| Woody 2001 | Prospectively randomized study. No details given on punctured vessels; no usable data provided |
Characteristics of studies awaiting assessment [ordered by study ID]
Eldabaa 2012.
| Methods | |
| Participants | Infants who had been prepared for major elective surgery |
| Interventions | Group I, in which femoral vein cannulation was guided by anatomical landmarks in optimally positioned participants, or Group II, in which the ultrasound‐guided technique was used for cannulation |
| Outcomes | Success, number of needle passes, first‐pass success |
| Notes |
Enany 2013.
| Methods | Prospective randomized trial |
| Participants | 60 paediatric participants with congenital heart disease ranging from 3 days to 15 years and weight range from 2800 to 50 kg for cardiac catheterization |
| Interventions | Femoral vein and artery punctures using an ultrasound‐guided technique or a landmark‐guided technique on external anatomical landmarks |
| Outcomes | Overall rate of success, access rate, procedure time, rate of puncture site complications |
| Notes |
Lam 2013.
| Methods | Quasi‐randomized controlled trial (on alternating days of the week) |
| Participants | Participants requiring temporary femoral vein catheters for haemodialysis |
| Interventions | Ultrasound localization of the femoral vein before cannulation vs conventional landmark localization. |
| Outcomes | Number of attempts, first attempt success rates, failure and complication rates |
| Notes |
Oh 2014.
| Methods | Prospective randomized controlled study |
| Participants | 60 adult participants who required subclavian venous catheterization for neurosurgery |
| Interventions | Real‐time ultrasound‐guided infraclavicular subclavian venous cannulation vs landmark‐guided cannulation |
| Outcomes | Misplacement of the guide wire, complications |
| Notes |
Xu 2013.
| Methods | Randomized study |
| Participants | 1369 patients with central venous catheterization |
| Interventions | Ultrasound‐guided central venous catheterization via the axillary vein vs the anatomical landmark method |
| Outcomes | Operation time, 1‐attempt success rate, complications, malposition rate |
| Notes |
Differences between protocol and review
Differences between the published protocol (Brass 2008) and the review must be noted.
As described in our published protocol, we planned to compare the effectiveness and safety of traditional landmark‐ and ultrasound‐guided techniques (ultrasound (UGP)‐ or Doppler (DGP)‐guided puncture techniques) for central vein catheterization. Because of the large number of eligible studies, we decided to split the review (Brass 2008) into two reviews: "Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization" and "Ultrasound guidance versus anatomical landmarks for subclavian and femoral vein catheterization."
We used the new domain‐based evaluation of The Cochrane Collaboration to assess the validity and quality of included studies. This was released after publication of the protocol.
We planned to perform sensitivity analysis regarding 'randomized versus quasi‐randomized' and possibly 'good quality studies versus poor quality studies' to test how sensitive the results are to reasonable changes in the assumptions made and in the protocol for combining data. We have not undertaken the sensitivity analysis, as almost all included studies have unclear risk of bias across the six domains.
We planned to consider the following additional outcomes: number of participants with significant local bleeding, number of participants with significant cardiac complications, rate of malpositioned catheter tips, number of participants with a significant pneumothorax, rate of catheter‐related infection and success rate after cross‐over. During our evaluation, we have determined that it is more useful to look at the number of participants with other complications (thrombosis, embolism, haematomediastinum and hydromediastinum, haematothorax and hydrothorax, pneumothorax, subcutaneous emphysema, nerve injury) all together. We planned to examine the costs connected with application of the new method and whether the additional financial expenditure is reasonably proportionate to the possibly ensuring improvement/advantages. We have not undertaken these analyses, as none of the studies assessed costs.
We planned to use a fixed‐effect model when heterogeneity between studies is negligible; otherwise we would use a random‐effects model that takes into account between‐study variability as well as within‐study variability. We have used a random‐effects model for all analyses regardless of heterogeneity, as in most comparisons, the heterogeneity that cannot readily be explained is > 25%. This is the more conservative approach.
Contributions of authors
Patrick Brass (PB), Martin Hellmich (MH), Laurentius Kolodziej (LK), Guido Schick (GS), Andrew F Smith (AFS)
Conceiving of the review: PB. Designing the review: PB. Co‐ordinating the review: PB. Undertaking manual searches: PB. Undertaking electronic searches: PB. Screening search results: PB, LK. Organizing retrieval of papers: PB, LK. Screening retrieved papers against inclusion criteria: PB, LK, GS. Appraising quality of papers: PB, LK, GS. Abstracting data from papers: PB, LK, GS. Writing to authors of papers to ask for additional information: PB. Providing additional data about papers: PB. Obtaining and screening data on unpublished studies: PB, LK. Managing data for the review: MH. Entering data into Review Manager (RevMan 5.2): PB, LK, GS. Analysing data: PB, GS. Interpreting data: PB, GS, MH, AFS. Writing the review: PB, AFS. Performing previous work that served as the foundation of the present study: PB. Serving as guarantor for the review (one review author): PB. Performing statistical analysis: PB, MH.
Sources of support
Internal sources
Professor M Hellmich, Institute of Medical Statistics, Informatics and Epidemiology, University of Cologne, Germany.
External sources
Jane Cracknell, Managing Editor, Cochrane Anaesthesia Review Group, Denmark.
Karen Hovhannisyan, Trial Search Co‐ordinator, Cochrane Anaesthesia Review Group, Denmark.
Declarations of interest
Patrick Brass: none known.
Martin Hellmich: none known.
Laurentius Kolodziej: none known.
Guido Schick: none known.
Andrew F Smith: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Alic 2009 {published data only}
- Alic Y, Torgay A, Pirat A. Ultrasound‐guided catheterization of the subclavian vein: a prospective comparison with the landmark technique in ICU patients. Critical Care. 2009; Vol. 13:S80.
Aouad 2010 {published data only}
- Aouad MT, Kanazi GE, Abdallah FW, Moukaddem FH, Turbay MJ, Obeid MY, et al. Femoral vein cannulation performed by residents: a comparison between ultrasound‐guided and landmark technique in infants and children undergoing cardiac surgery. Anesthesia and Analgesia 2010;111(3):724‐8. [DOI] [PubMed] [Google Scholar]
Bold 1998 {published data only}
- Bold RJ, Winchester DJ, Madary AR, Gregurich MA, Mansfield PF. Prospective, randomized trial of Doppler‐assisted subclavian vein catheterization. Archives of Surgery 1998;133(10):1089‐93. [DOI] [PubMed] [Google Scholar]
Branger 1994 {published data only}
- Branger B, Zabadani B, Vecina F, Juan JM, Dauzat M. Continuous guidance for venous punctures using a new pulsed Doppler probe: efficiency, safety [Guidage continu des ponctions veineuses par une nouvelle sonde Doppler pulsee: efficacite, securite]. Nephrologie 1994;15(2):137‐40. [PubMed] [Google Scholar]
Branger 1995 {published data only}
- Branger B, Dauzat M, Zabadani B, Vecina F, Lefranc JY. Pulsed Doppler sonography for the guidance of vein puncture: a prospective study. Artificial Organs 1995;19(9):933‐8. [DOI] [PubMed] [Google Scholar]
Fragou 2011 {published data only}
- Fragou M, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, Karabinis A, et al. Real‐time ultrasound‐guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Critical Care Medicine 2011;39(7):1607‐12. [DOI] [PubMed] [Google Scholar]
Gualtieri 1995 {published data only}
- Gualtieri E, Deppe SA, Sipperly ME, Thompson DR. Subclavian venous catheterization: greater success rate for less experienced operators using ultrasound guidance. Critical Care Medicine 1995;23(4):692‐7. [PMID: 7661944] [DOI] [PubMed] [Google Scholar]
Iwashima 2008 {published data only}
- Iwashima S, Ishikawa T, Ohzeki T. Ultrasound‐guided versus landmark‐guided femoral vein access in pediatric cardiac catheterization. Pediatric Cardiology 2008;29:339‐42. [DOI] [PubMed] [Google Scholar]
Kwon 1997 {published data only}
- Kwon TH, Kim YL, Cho DK. Ultrasound‐guided cannulation of the femoral vein for acute haemodialysis access. Nephrology, Dialysis, Transplantation 1997;12(5):1009‐12. [DOI] [PubMed] [Google Scholar]
Lefrant 1998 {published data only}
- Lefrant JY, Cuvillon P, Bénézet JF, Dauzat M, Peray P, Saïssi G, et al. Pulsed Doppler ultrasonography guidance for catheterization of the subclavian vein. Anesthesiology 1998;88(5):1195‐201. [DOI] [PubMed] [Google Scholar]
Mansfield 1994 {published data only}
- Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian‐vein catheterization. New England Journal of Medicine 1994;331(26):1735‐8. [DOI] [PubMed] [Google Scholar]
Palepu 2009 {published data only}
- Palepu GB, Deven J, Subrahmanyam M, Mohan S. Impact of ultrasonography on central venous catheter insertion in intensive care. The Indian Journal of Radiology & Imaging 2009;19(3):191‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prabhu 2010 {published data only}
- Prabhu MV, Juneja D, Gopal PB, Sathyanarayanan M, Subhramanyam S, Gandhe S, et al. Ultrasound‐guided femoral dialysis access placement: a single‐center randomized trial. Clinical Journal of the American Society of Nephrology 2010;5(2):235‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Froehlich 2009 {published data only}
- Froehlich CD, Rigby MR, Rosenberg ES, Li R, Roerig PL, Easley KA, et al. Ultrasound‐guided central venous catheter placement decreases complications and decreases placement attempts compared with the landmark technique in patients in a paediatric intensive care unit. Critical Care Medicone 2009;37(3):1090‐6. [DOI] [PubMed] [Google Scholar]
Hilty 1997 {published data only}
- Hilty WM, Hudson PA, Levitt MA, Hall JB. Real‐time ultrasound guided femoral vein catheterization during cardiopulmonary resuscitation. Annals of Ernergency Medicine 1997;29:331‐7. [DOI] [PubMed] [Google Scholar]
Kwon 1996 {published data only}
- Kwon TH, Kim YL, Cho DK. Ultrasound‐guided cannulation of the femoral vein for acute haemodialysis access. Nephrology, Dialysis and Transplantation 1997;12:1009‐12. [DOI] [PubMed] [Google Scholar]
Miller 2002 {published data only}
- Miller AH, Roth BA, Mills TJ, Woody JR, Longmoor CE, Foster B. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Academic Emergency Medicine 2002;9(8):800‐5. [DOI] [PubMed] [Google Scholar]
Thompson 1994 {published data only}
- Thompson DR, Gualtieri E, Deppe S, Sipperly ME. Greater success in subclavian vein cannulation using ultrasound for inexperienced operators. Critical Care Medicine 1994;22:A190. [DOI] [PubMed] [Google Scholar]
Woody 2001 {published data only}
- Woody JR, Miller AH, Mills TJ, Roth BA. Using ultrasound for central venous line placement (CVP) in the emergency department. Academic Emergency Medicine 2001;8:580. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Eldabaa 2012 {published data only}
- Eldabaa AA, Elgebaly AS, Elhafz AAA, Bassuni AS. Comparison of ultrasound‐guided vs. anatomical landmark‐guided cannulation of the femoral vein at the optimum position in infant. South African Journal of Anaesthesia and Analgesia 2012;18(3):162‐6. [Google Scholar]
Enany 2013 {published data only}
- Enany B, Elsayed M, Elshahed G, Abdelhaleem Z. Ultrasound versus landmark‐guided femoral vein, artery access in pediatric cardiac catheterization. Abstracts view online. www.summit‐tctap.com. 2013.
Lam 2013 {published data only}
- Lam KK, Ng HY, Wu CH, Wu MT, Chen JB, Lee CT. Ultrasound localization of the femoral vein facilitates successful cannulation for hemodialysis. Biomedical Journal 2013;36(5):237‐42. [DOI: 10.4103/2319-4170.113193] [DOI] [PubMed] [Google Scholar]
Oh 2014 {published data only}
- Oh AY, Jeon YT, Choi EJ, Ryu JH, Hwang JW, Park HP, et al. The influence of the direction of J‐tip on the placement of a subclavian catheter: real time ultrasound‐guided cannulation versus landmark method, a randomized controlled trial. BioMed Central Anesthesiology 2014;14(1):11. [DOI: 10.1186/1471-2253-14-11; PUBMED: 24581318] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2013 {published data only}
- Xu JX, Wand HZ, Ren H, Shen YF, Dong J, Li Q. Clinical application of ultrasound guided central venous catheterization via the axillary vein. Chinese Journal of Clinical Nutrition 2013;3:163‐7. [Google Scholar]
Additional references
American College of Emergency Physicians 2007
Atkinson 2005
- Atkinson P, Boyle A, Robinson S, Campbell‐Hewson G. Should ultrasound guidance be used for central venous catheterisation in the emergency department?. Emergency Medicine Journal 2005;22:158‐64. [DOI: 10.1136/emj.2003.011288] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernard 1971
- Bernard RW, Stahl WM. Subclavian vein catheterization: a prospective study. I. Non‐infectious complications. Annals of Surgery 1971;173(2):184‐90. [PUBMED: 5100094] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bo‐Linn 1982
- Bo‐Linn GW, Anderson DJ, Anderson KC, McGoon MD. Percutaneous central venous catheterization performed by medical house officers: a prospective study. Catheterization and Cardiovascular Diagnosis 1982;8(1):23‐9. [PUBMED: 7060113] [DOI] [PubMed] [Google Scholar]
Bodenham 2006
- Bodenham AR. Can you justify not using ultrasound guidance for central venous access?. Critical Care 2006;10(6):175. [PUBMED: 17129362] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodenham 2011
- Bodenham A. Reducing major procedural complications from central venous catheterisation. Anaesthesia 2011;66:6‐9. [PUBMED: 21198502] [DOI] [PubMed] [Google Scholar]
Brass 2013a
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Traditional landmark versus ultrasound guidance for internal jugular vein catheterization. Cochrane Database of Systematic Reviews in editorial process, Issue in editorial process. [DOI: 10.1002/14651858.CD006962] [DOI] [Google Scholar]
Calvert 2003
- Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A. The effectiveness and cost‐effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technology Assessment 2003;7(12):1‐84. [PUBMED: 12709290] [DOI] [PubMed] [Google Scholar]
Calvert 2004
- Calvert N, Hind D, McWilliams R, Davidson A, Beverley C, Thomas SM. Ultrasound for central venous cannulation: economic evaluation of cost‐effectiveness. Anaesthesia 2004;59(11):1116‐20. [PUBMED: 15479322] [DOI] [PubMed] [Google Scholar]
Caridi 1998
- Caridi JG, Hawkins IF Jr, Wiechmann BN, Pevarski DJ, Tonkin JC. Sonographic guidance when using the right internal jugular vein for central vein access. American Journal of Roentgenology 1998;171(5):1259‐63. [PUBMED: 9798857] [DOI] [PubMed] [Google Scholar]
Cook 2011
- Cook TM. Litigation related to central venous access by anaesthetists: an analysis of claims against the NHS in England 1995‐2009. Anaesthesia 2011;66:56‐7. [PUBMED: 21198504] [DOI] [PubMed] [Google Scholar]
Debordeau 2009
- Debordeau P, Kassab Chahmi D, Gal G, Kriegel I, Desruennes E, Douard MC, et al. 2008 SOR guidelines for the prevention and treatment of thrombosis associated with central venous catheters inpatients with cancer: report from the working group. Annals of Oncology 2009;20(9):1459–71. [DOI: 10.1093/annonc/mdp052; PUBMED: 19525362] [DOI] [PubMed] [Google Scholar]
Defalque 1974
- Defalque RJ. Percutaneous catheterization of the internal jugular vein. Anesthesia and Analgesia 1974;53(1):116‐21. [PUBMED: 4589503] [PubMed] [Google Scholar]
Denys 1991
- Denys BG, Uretsky BF. Anatomical variations of internal jugular vein localisation: impact on central venous access. Critical Care Medicine 1991;42(3):218‐23. [PUBMED: 1959371] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Phillips AN. Meta‐analysis: principles and procedures. BMJ 1997;315(7121):1533‐7. [PUBMED: 9432252] [DOI] [PMC free article] [PubMed] [Google Scholar]
FDA Drug Bull 1989
- Food, Drug Administration. Precautions necessary with central venous catheters. FDA Drug Bulletin 1989;July:15‐6. [Google Scholar]
Feller‐Kopman 2007
- Feller‐Kopman D. Ultrasound‐guided internal jugular access: a proposed standardized approach and implications for training and practice. Chest 2007;132(1):302‐9. [PUBMED: 17625091] [DOI] [PubMed] [Google Scholar]
Ferral 1998
- Ferral H. US‐guided puncture of the internal jugular vein: an unexpected anatomic relationship. Journal of Vascular and Interventional Radiology 1998;9(5):854‐5. [PUBMED: 9756083] [DOI] [PubMed] [Google Scholar]
French 2008
- French J, Raine‐Fenning N, Hardmann J. Pitfalls of ultrasound guided vascular access: the use of three/four‐dimensional ultrasound. Anaesthesia 2008;63:806–13. [DOI] [PubMed] [Google Scholar]
Ge 2012
- Ge X, Cavallazzi R, Li C, Pan SM, Wang YW, Wang FL. Central venous access sites for the prevention of venous thrombosis, stenosis and infection. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD004084.pub3; PUBMED: 22419292] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gilbert 1995
- Gilbert TB, Seneff MG, Becker RB. Facilitation of internal jugular venous cannulation using an audio‐guided Doppler ultrasound vascular access device: results from a prospective, dual‐center, randomized, crossover clinical study. Critical Care Medicine 1995;23(1):60‐5. [PUBMED: 8001387] [DOI] [PubMed] [Google Scholar]
Glasziou 2001
- Glasziou P, Irwig L, Bain C, Colditz G. Systematic Reviews in Health Care: A Practical Guide. 1st Edition. Cambridge, UK: Cambridge University Press, 2001. [NLM ID: 101133142] [Google Scholar]
Goodwin 2005
- Goodwin D, Pope C, Mort M, Smith AF. Access, boundaries and their effects: legitimate participation in anaesthesia. Sociology of Health and Illness 2005;27:855‐71. [PUBMED: 16283902] [DOI] [PubMed] [Google Scholar]
Guimares 2009
- Guimaraes MM, Dib R, Smith AF, Matos D. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD006058.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Altman DG editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org. Chichester, UK: John Wiley & Sons, Ltd. [Google Scholar]
Hind 2003
- Hind D, Calvert N, McWilliams R, Davidson A, Paisley S. Ultrasonic locating devices for central venous cannulation: meta‐analysis. BMJ 2003;327(7411):361. [PUBMED: 12919984] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howard 2007
- Howard S. A survey measuring the impact of NICE guidance 49: the use of ultrasound locating devices for placing central venous catheters. http://www.nice.org.uk/pdf/Final_CVC_placement_survey_report.pdf (accessed 4 June 2007).
Joffe 2009
- Joffe A, Anton N, Lequier L, Vandermeer B, Tjosvold L, Larsen B, et al. Nutritional support for critically ill children. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD005144.pub2] [DOI] [PubMed] [Google Scholar]
Johnson 1994
- Johnson PF. Central venous catheter placement and complications. Critical Care Medicine 1994;22(9):1515‐6. [PUBMED: 7980790] [PubMed] [Google Scholar]
Keenan 2002
- Keenan SP. Use of ultrasound to place central lines. Journal of Critical Care 2002;17(2):126‐37. [PUBMED: 12096376] [DOI] [PubMed] [Google Scholar]
Kinsella 2009
- Kinsella S, Young N. Ultrasound‐guided central line placement as compared with standard landmark technique: some unpleasant arithmetic for the economics of medical innovation. Value Health 2009;12(1):98‐100. [DOI: 10.1111/j.1524-4733.2008.00427.x; PUBMED: 18647249] [DOI] [PubMed] [Google Scholar]
Lamperti 2012
- Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, et al. International evidence‐based recommendations on ultrasound‐guided vascular access. Intensive Care Medicine 2012;38(7):1105‐17. [DOI: 10.1007/s00134-012-2597-x; PUBMED: 22614241] [DOI] [PubMed] [Google Scholar]
Lau 1998
- Lau J, Ioannidis JPA, Schmid CH. Quantitative synthesis in systematic reviews. In: Mulrow C, Cook D editor(s). Systematic Reviews: Synthesis of Best Evidence for Healthcare Decisions. 1st Edition. Philadelphia: American College of Physicians, 1998:91‐101. [Google Scholar]
Legler 1984
- Legler D, Nugent M. Doppler localization of the internal jugular vein facilitates its cannulation. Anesthesiology 1984;59:A 179. [DOI] [PubMed] [Google Scholar]
Light 1984
- Light RJ, Pillemer DB. Summing Up: The Science of Reviewing Research. Cambridge, Massachusetts: Harvard University Press, 1984. [NLM ID: 8505340] [Google Scholar]
McIntyre 1992
- McIntyre AS, Levison RA, Wood S, Phillips RK, Lennard‐Jones JE. Duplex Doppler ultrasound identifies veins suitable for insertion of central feeding catheters. Journal of Parenteral and Enteral Nutrition 1992;16(3):264‐7. [PUBMED: 1501358] [DOI] [PubMed] [Google Scholar]
Merrer 2001
- Merrer J, Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA 2001;286(6):700‐7. [PUBMED: 11495620] [DOI] [PubMed] [Google Scholar]
Mort 2009
- Mort M, Smith AF. Beyond Information: intimate relations in sociotechnical practice. Sociology 2009;43:215‐31. [DOI: 10.1177/0038038508101162] [DOI] [Google Scholar]
Muhm 2002
- Muhm M. Ultrasound guided central venous access. BMJ 2002;325(7377):1373‐4. [PUBMED: 12480829] [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2002
- National Institute for Health and Clinical Excellence Appraisal Committee Members. Guidance on the use of ultrasound locating devices for placing central venous catheters. Technology Appraisal No. 49 September 2002;49:1‐24. [Google Scholar]
Peters 1982
- Peters JL, Belsham PA, Garrett CP, Kurzer M. Doppler ultrasound technique for safer percutaneous catheterization of the infraclavicular subclavian vein. American Journal of Surgery 1982;143(3):391‐3. [PUBMED: 7065360] [DOI] [PubMed] [Google Scholar]
Pikwer 2012
- Pikwer A, Åkeson J, Lindgren S. Complications associated with peripheral or central routes for central venous cannulation. Anaesthesia 2012;67:65‐71. [PUBMED: 19370617] [DOI] [PubMed] [Google Scholar]
Polderman 2002
- Polderman KH, Girbes ARJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Medicine 2002;28(1):1‐17. [PUBMED: 11818994] [DOI] [PubMed] [Google Scholar]
Rajaram 2013
- Rajaram SS, Desai NK, Kalra A, Gajera M, Cavanaugh SK, Brampton W, et al. Pulmonary artery catheters for adult patients in intensive care. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD003408.pub3; PUBMED: 23450539] [DOI] [PMC free article] [PubMed] [Google Scholar]
Randolph 1996
- Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta‐analysis of the literature. Critical Care Medicine 1996;24(12):2053‐8. [PUBMED: 8968276] [DOI] [PubMed] [Google Scholar]
Resnick 2008
- Resnick JR, Cydulka RK, Donato J. Success of ultrasound‐guided peripheral intravenous access with skin marking. Academic Emergency Medicine 2008;15(8):723‐30. [PUBMED: 18637084] [DOI] [PubMed] [Google Scholar]
RevMan 5.2 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, November 8, 2012.
Rothschild 2001
- Rothschild JM. Ultrasound guidance of central vein catheterization. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ editor(s). Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Vol. 43, Rockville, MD: Agency for Healthcare Research and Quality, 2001:244‐52. [AHRQ Publication No. 01‐E058] [Google Scholar]
Rupp 2012
- American Society of Anesthesiologists Task Force on Central Venous Access, Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, Connis RT, Domino KB, et al. Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology 2012;116(3):539‐73. [DOI: 10.1097/ALN.0b013e31823c9569; PUBMED: 22307320] [DOI] [PubMed] [Google Scholar]
Scott 2004
- Scott DHT. Editorial II: the king of the blind extends his frontiers. British Journal of Anaesthesia 2004;93:175‐7. [DOI: 10.1093/bja/aeh183] [DOI] [PubMed] [Google Scholar]
Shojania 2001
- Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment. 2001;43(i‐x):1‐668. [PUBMED: 11510252] [PMC free article] [PubMed] [Google Scholar]
Smith 1997
- Smith AF, Vallance H, Slater RM. Shorter fluid fasts reduce postoperative emesis. BMJ 1997;314:1486. [PUBMED: 9167597] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2009
- Smith AF. In search of excellence in anesthesiology. Anesthesiology 2009;110:4‐5. [DOI: 10.1097/ALN.0b013e318190b263] [DOI] [PubMed] [Google Scholar]
Smith 2010
- Smith AF, Greaves JD. Beyond competence: defining and promoting excellence in anaesthesia. Anaesthesia 2010;65:184‐91. [PUBMED: 20003114] [DOI] [PubMed] [Google Scholar]
Smith 2011
- Smith AF, Glavin R, Greaves JD. Defining excellence in anaesthesia: the role of personal qualities and practice environment. British Journal of Anaesthesia 2011;106:38‐43. [PUBMED: 21118845] [DOI] [PubMed] [Google Scholar]
Sznajder 1986
- Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Archives of Internal Medicine 1986;146(2):259‐61. [PUBMED: 3947185] [DOI] [PubMed] [Google Scholar]
Troianos 2012
- Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesthesia and Analgesia 2012;114(1):46‐72. [DOI: 10.1213/ANE.0b013e3182407cd8; PUBMED: 22127816] [DOI] [PubMed] [Google Scholar]
van Miert 2012
- Miert C, Hill R, Jones L. Interventions for restoring patency of occluded central venous catheter lumens. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD007119.pub2; PUBMED: 22513946] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verghese 1995
- Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Approaches to internal jugular vein cannulation in infants: seeing, hearing vs. feeling. Anesthesia and Analgesia 1995;80:S525. [Google Scholar]
Verghese 2000
- Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Comparison of three techniques for internal jugular vein cannulation in infants. Paediatric Anaesthesia 2000;10(5):505‐11. [PUBMED: 11012954] [DOI] [PubMed] [Google Scholar]
Watters 2002
- Watters MP. Where is the harm in using ultrasound guidance?. BMJ; http://www.bmj.com/rapid‐response/2011/10/29/where‐harm‐using‐ultrasound‐guidance; accessed November 2013 2002.
Wu 2013
- Wu SY, Ling Q, Cao LH, Wang J, Xu MX, Zeng WA. Real‐time two‐dimensional ultrasound guidance for central venous cannulation: a meta‐analysis. Anesthesiology 2013;118(2):361‐75. [DOI: 10.1097/ALN.0b013e31827bd172; PUBMED: 23249991] [DOI] [PubMed] [Google Scholar]
Yonei 1986
- Yonei A, Nonoue T, Sari A. Real‐time ultrasonic guidance for percutaneous puncture of the internal jugular vein. Anesthesiology 1986;64(6):830‐1. [PUBMED: 3717653] [DOI] [PubMed] [Google Scholar]
Yonei 1988
- Yonei A, Yokota K, Yamashita S, Sari A. Ultrasound‐guided catheterization of the subclavian vein. Journal of Clinical Ultrasound 1988;16(7):499‐501. [PUBMED: 3152446] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Brass 2008
- Brass P, Hellmich M, Kolodziej L, Kullmer B, Schick G, Schregel W. Traditional landmark versus ultrasound guidance for central vein catheterization. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD006962] [DOI] [Google Scholar]


