Abstract
Background
During intensive care unit (ICU) admission, patients and their carers experience physical and psychological stressors that may result in psychological conditions including anxiety, depression, and post‐traumatic stress disorder (PTSD). Improving communication between healthcare professionals, patients, and their carers may alleviate these disorders. Communication may include information or educational interventions, in different formats, aiming to improve knowledge of the prognosis, treatment, or anticipated challenges after ICU discharge.
Objectives
To assess the effects of information or education interventions for improving outcomes in adult ICU patients and their carers.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, CINAHL, and PsycINFO from database inception to 10 April 2017. We searched clinical trials registries and grey literature, and handsearched reference lists of included studies and related reviews.
Selection criteria
We included randomised controlled trials (RCTs), and planned to include quasi‐RCTs, comparing information or education interventions presented to participants versus no information or education interventions, or comparing information or education interventions as part of a complex intervention versus a complex intervention without information or education. We included participants who were adult ICU patients, or their carers; these included relatives and non‐relatives, including significant representatives of patients.
Data collection and analysis
Two review authors independently assessed studies for inclusion, extracted data, assessed risk of bias, and applied GRADE criteria to assess certainty of the evidence.
Main results
We included eight RCTs with 1157 patient participants and 943 carer participants. We found no quasi‐RCTs. We identified seven studies that await classification, and three ongoing studies.
Three studies designed an intervention targeted at patients, four at carers, and one at both patients and carers. Studies included varied information: standardised or tailored, presented once or several times, and that included verbal or written information, audio recordings, multimedia information, and interactive information packs. Five studies reported robust methods of randomisation and allocation concealment. We noted high attrition rates in five studies. It was not feasible to blind participants, and we rated all studies as at high risk of performance bias, and at unclear risk of detection bias because most outcomes required self reporting.
We attempted to pool data statistically, however this was not always possible due to high levels of heterogeneity. We calculated mean differences (MDs) using data reported from individual study authors where possible, and narratively synthesised the results. We reported the following two comparisons.
Information or education intervention versus no information or education intervention (4 studies)
For patient anxiety, we did not pool data from three studies (332 participants) owing to unexplained substantial statistical heterogeneity and possible clinical or methodological differences between studies. One study reported less anxiety when an intervention was used (MD ‐3.20, 95% confidence interval (CI) ‐3.38 to ‐3.02), and two studies reported little or no difference between groups (MD ‐0.40, 95% CI ‐4.75 to 3.95; MD ‐1.00, 95% CI ‐2.94 to 0.94). Similarly, for patient depression, we did not pool data from two studies (160 patient participants). These studies reported less depression when an information or education intervention was used (MD ‐2.90, 95% CI ‐4.00 to ‐1.80; MD ‐1.27, 95% CI ‐1.47 to ‐1.07). However, it is uncertain whether information or education interventions reduce patient anxiety or depression due to very low‐certainty evidence.
It is uncertain whether information or education interventions improve health‐related quality of life due to very low‐certainty evidence from one study reporting little or no difference between intervention groups (MD ‐1.30, 95% CI ‐4.99 to 2.39; 143 patient participants). No study reported adverse effects, knowledge acquisition, PTSD severity, or patient or carer satisfaction.
We used the GRADE approach and downgraded certainty of the evidence owing to study limitations, inconsistencies between results, and limited data from few small studies.
Information or education intervention as part of a complex intervention versus a complex intervention without information or education (4 studies)
One study (three comparison groups; 38 participants) reported little or no difference between groups in patient anxiety (tailored information pack versus control: MD 0.09, 95% CI ‐3.29 to 3.47; standardised general ICU information versus control: MD ‐0.25, 95% CI ‐4.34 to 3.84), and little or no difference in patient depression (tailored information pack versus control: MD ‐1.26, 95% CI ‐4.48 to 1.96; standardised general ICU information versus control: MD ‐1.47, 95% CI ‐6.37 to 3.43). It is uncertain whether information or education interventions as part of a complex intervention reduce patient anxiety and depression due to very low‐certainty evidence.
One study (175 carer participants) reported fewer carer participants with poor comprehension among those given information (risk ratio 0.28, 95% CI 0.15 to 0.53), but again this finding is uncertain due to very low‐certainty evidence.
Two studies (487 carer participants) reported little or no difference in carer satisfaction; it is uncertain whether information or education interventions as part of a complex intervention increase carer satisfaction due to very low‐certainty evidence. Adverse effects were reported in only one study: one participant withdrew because of deterioration in mental health on completion of anxiety and depression questionnaires, but the study authors did not report whether this participant was from the intervention or comparison group.
We downgraded certainty of the evidence owing to study limitations, and limited data from few small studies.
No studies reported severity of PTSD, or health‐related quality of life.
Authors' conclusions
We are uncertain of the effects of information or education interventions given to adult ICU patients and their carers, as the evidence in all cases was of very low certainty, and our confidence in the evidence was limited. Ongoing studies may contribute more data and introduce more certainty when incorporated into future updates of the review.
Plain language summary
Information for adult intensive care unit patients and their carers
Background
During intensive care unit (ICU) admission, patients and their carers experience physical and psychological stressors that may lead to increased anxiety, depression, and post‐traumatic stress disorder (PTSD). Improving communication among patients, their carers, and doctors, nurses, and other ICU staff may improve these outcomes. Communication may include information or educational interventions, in different formats, which aim to improve knowledge of the patient's condition, their treatment plan, or challenges they may face after ICU discharge.
Study characteristics
The evidence is current up to 10 April 2017. We included eight studies with 1157 ICU patients and 943 carers of ICU patients. Seven studies are awaiting classification because we could not assess their eligibility, and three studies are ongoing. We included studies that assessed information given to patients or their carers compared to no information, and studies that assessed information as part of a more complex intervention compared to a complex intervention that did not include information or education. Studies included varied information: standardised or tailored to the individual, given regularly or on a single occasion, and that included verbal or written information, audio recordings, multimedia information, and interactive information packs.
Key results
Overall, it is uncertain whether information or education (given alone or as part of a more complex intervention) improves outcomes for patients and their carers following a stay in the ICU. For patients, it is uncertain whether or not information or education reduces anxiety or depression, or improves health‐related quality of life. One patient asked to withdraw from the study because they believed that their mental health worsened when they completed a questionnaire to assess anxiety and depression, but it is not clear whether this person received the information intervention or not. No studies reported PTSD in patients. For carers, it is uncertain whether or not information or education reduces anxiety or depression or improves carers' knowledge acquisition or their satisfaction with information provided.
Quality of the evidence
It was not possible for researchers to mask patients and carers to the intervention they received, and it was unclear whether this would affect the results, which relied on self assessments. Study authors did not consistently report rigorous methods for carrying out randomised trials, and we noted some losses of patients and carers during the studies. We found few small studies for this review, reporting limited data for many outcomes of interest. It is uncertain whether information or education is effective due to very low‐certainty evidence.
Conclusion
We are uncertain about the effects of information or education interventions given to adult ICU patients and their carers. The evidence was of very low certainty, and our confidence in the evidence was limited. We are aware of three ongoing studies and seven studies that were recently completed but not yet published. These studies may provide additional evidence or improve the certainty in the findings in future updates of the review.
Summary of findings
Background
Description of the condition
During intensive care unit (ICU) admission, patients experience a variety of physical and psychological stressors, which may result in psychological disorders including anxiety, depression, and post‐traumatic stress disorder (PTSD) (Hofhuis 2008; Ringdal 2005; Wang 2009). Elevated and prolonged stress can also have detrimental consequences on other health outcomes, affecting wound healing and susceptibility to infection (Herbert 1993; Walburn 2009). The duration of psychological disorders frequently extends beyond discharge from the ICU (Ringdal 2005), and can impact a patient’s recovery as well as the mental health of carers or relatives (Davidson 2007). For example, reported anxiety and depression prevalence among people treated in ICUs ranges from 12% to 43% (Eddleston 2000; Scragg 2001), and 10% to 30% (Davydow 2009; Eddleston 2000; Scragg 2001), respectively. A recent meta‐analysis estimated that PTSD occurs in 20% of people treated in ICUs (Parker 2015). Family members of critically ill patients are also at risk of depression, anxiety, PTSD, and complicated grief (Haines 2015; Kross 2015). The prevalence of anxiety, depression, and PTSD in carers of people treated in ICUs is reported as ranging from 15% to 24%, 5% to 36%, and 35% to 57%, respectively (Van Beusekom 2016). Ineffective communication between healthcare professionals and patients/carers, or a lack of information, can exacerbate psychological disorders, both during and after an ICU stay (Magnus 2006).
Description of the intervention
Information or education interventions represent one type of communication intervention and include structured information programmes, information leaflets, face‐to‐face briefings, recorded messages, or use of online resources. These interventions aim to improve knowledge (e.g. of the condition, care, expected length of stay, or sources of support during recovery) and comprehension in patients and their carers in order to reduce anxiety and ultimately improve health outcomes (Azoulay 2002; Hofhuis 2008; Linton 2008). Information or education interventions may involve communication of important information from healthcare provider to patient, but can also incorporate elements of patient‐to‐provider communication whereby the intervention is tailored to the patient’s needs. Patients and carers who are not fluent or literate in the dominant language used by information providers may face additional challenges (Joint Commission 2007; Riley 2006; Schyve 2007). Timing of the intervention is also an important factor (Fleischer 2014). For example, interventions delivered during ICU admission may focus on the delivery of information to the carer (if the patient is incapacitated or unconscious), who then relays the information to the patient. Such an intervention is reliant on the carer's ability to comprehend and relay the correct information. In comparison, delivery of interventions at the point of discharge may involve both the patient and their carer.
How the intervention might work
There are several potential mechanisms through which information and education interventions might reduce anxiety. The provision of information and education (as a component of supportive communication) can reduce both cardiovascular reactivity (Thorsteinsson 1999), and levels of stress hormones such as cortisol (Floyd 2008). Supportive communication may also serve to encourage a stressed person to reappraise recent traumatic experiences, such as time spent in an ICU. By altering how people appraise stressful events, communication can ameliorate physiological and emotional responses to stress (Chadwick 2016).
Why it is important to do this review
Clinical guidelines recommend effective communication with critically ill patients and their families during admission to, and discharge from, the ICU. Patient‐centred discussions regarding their condition and steps that can be taken during a patient's recovery are also encouraged (NICE CG50). A number of controlled trials have examined the effects of education interventions for reducing anxiety and improving outcomes in critically ill patients, Azoulay 2002; Fleischer 2014; Hwang 1998; Linton 2008, and their carers (Douglas 2005). However, the findings of these trials are conflicting, which may relate to the timing or duration of the intervention. For example, Fleischer 2014 found no benefit (in terms of a reduction in anxiety) of an ICU‐specific single episode intervention (comprising face‐to‐face verbal communication) versus a non‐specific conversation of comparable length. In contrast, Hwang 1998 reported a reduction in anxiety for cardiac ICU patients who received an information intervention via audio recording. Both of these studies examined the effect of the interventions on depression and anxiety, but only Fleischer 2014 examined longer‐term well‐being, reporting no effect of the intervention on postdischarge quality of life. Despite the availability of data from individual trials, there are no available up‐to‐date syntheses of the evidence on education and information interventions for improving outcomes for ICU patients and their carers. Scheunemann 2011 performed a systematic review of randomised controlled trials of interventions to improve communication in intensive care. The review authors concluded that the evidence supported the use of printed information and structured communication by the ICU team. The use of ethics consultation, or palliative care consultation (e.g. about the appropriateness of aggressive medical treatments), improved emotional outcomes in family members and reduced the length of stay in the ICU and treatment intensity. However, whilst the review included studies where the focus was on determining the effects of information interventions, the review authors highlighted that few studies considered patient‐centred outcomes beyond mortality.
Our review served to re‐evaluate the available relevant evidence. Furthermore, our review focused on one aspect of communication interventions: information or education interventions. Information may be given at different time points (before an expected stay in the ICU, during an ICU stay, or after discharge from an ICU), and with different purposes. The time of an ICU stay may be especially distressing for patients and their carers, and their information needs especially high. We therefore chose to focus the review on this period of high need, considering as eligible any interventions aiming to provide information or education to these patients and their carers during the ICU stay. We included studies that provided communication interventions to enhance knowledge of the patient's prognosis and treatment plan, and information related to expected transition from the ICU; we did not consider studies that were designed to improve communication of decisions related to end‐of‐life care. The aim of this review was to reduce the uncertainty around whether information or education interventions are effective in improving knowledge and understanding, and ultimately short‐ and long‐term psychological health outcomes, in patients and their carers during and after their stay in an ICU. Additionally, improvements in short‐term outcomes potentially result in a shorter duration of stay in the ICU, and may thus reduce resource use.
Objectives
To assess the effects of information or education interventions for improving outcomes in adult ICU patients and their carers.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs). We planned to include quasi‐RCTs (i.e. trials in which randomisation is attempted but subject to potential manipulation, such as allocating participants by day of the week, date of birth, or sequence of entry into trial), with a parallel design. We included cluster RCTs to enable inclusion of studies that assign the ICU, rather than individual patients, to the intervention or control group/arm.
Types of participants
Adult (aged 18 years and above) ICU patients and critically ill patients in high‐dependency care units regardless of their status (e.g. conscious, unconscious, intubated) or length of stay. We also included carers of these patients (whether relatives or non‐relatives), because the psychological status of both can be affected by a patient’s critical illness and stay in the ICU (Davidson 2007; Haines 2015; Kross 2015).
If studies included adults and children, we included the study if the mean age of participants was 18 years or above.
Types of interventions
We included information or education interventions, which we defined as any intervention designed to improve a patient or carer's knowledge or understanding of the prognosis, treatment plan, or challenges likely to affect the patient during their transition from the ICU. Information or education interventions were delivered in different formats, such as written (e.g. leaflet), verbal (e.g. counselling), or digital (e.g. phone or tablet application, recorded message). We acknowledge the difficulties associated with delineating the definitions of information and education interventions (Kaufman 2018); for the purposes of this review, we essentially considered them as variants of the same thing. The intervention was additional or different to that provided in the comparator group (e.g. information pamphlet versus no information pamphlet). We required the intervention to be delivered by treating healthcare professionals (clinicians, nurses, or support teams).
We also included studies of more complex interventions, if part of the intervention involved the provision of information with the aim of improving a patient’s knowledge or understanding of the topics listed above, and provision was more than that delivered in the comparator group (i.e. if the effects of the information or education intervention could be isolated from the rest of the complex intervention). Finally, we also included studies that employed ‘sham’ controls (e.g. where patients were assigned to receive an ICU‐specific pamphlet versus a non‐specific pamphlet).
We included studies in which the intervention was given whilst the patient was critically ill in the ICU. We excluded studies in which the intervention was given before the ICU stay (i.e. before critical illness) and after the ICU stay (i.e. to a survivor of critical illness).
We excluded studies that assessed the effectiveness of patient diaries because patient diaries provided retrospective information to the patient about what they had experienced during their stay, rather than the provision of information aiming to increase a patient or carer's knowledge about what they should expect whilst they are in the ICU and as they transition from the ICU. We excluded information that was provided as part of managing end‐of‐life care.
We included the following comparisons:
information or education intervention versus no information or education intervention; and
information or education intervention as a part of a complex intervention (e.g. information or education intervention plus support) versus complex intervention without information or education (e.g. support alone).
The intervention was presented to either the patient, carer, or both.
Types of outcome measures
Primary outcomes
Severity of anxiety in patients (assessed with the Hospital Anxiety and Depression Scale (HADS) or other validated method).
Severity of depression in patients (assessed with the HADS or other validated method).
Knowledge acquisition (patients and carers).
Secondary outcomes
Severity of PTSD in patients treated in ICUs (assessed using the Impact of Event Scale‐Revised (IES‐R) or other validated tool).
Severity of depression in carers (assessed using the HADS or other validated tool).
Severity of anxiety in carers (assessed using the HADS or other validated tool).
Patient or carer satisfaction with information provided (e.g. self reported).
Health‐related quality of life (HRQoL) (measured with a validated quality of life questionnaire such as EQ‐5D or Short Form‐36 (SF‐36)).
Length of stay in ICU.
Adverse effects.
Where more than one outcome measure was presented per outcome (for example, EQ‐5D and SF‐36 for HRQoL), we planned to select the primary outcome measure that was identified by the publication authors. Where no primary outcome measure was identified, we planned to select the measure specified in the sample size calculation. If there was no sample size calculation, we planned to rank the effect estimates (i.e. list them in order from largest to smallest) and select the median effect estimate; where there was an even number of outcome measures, we planned to select the measure whose effect estimate was ranked n/2 (where n is the number of outcomes).
We extracted data for all outcomes at their last reported time point.
The reporting of one or more of the outcomes listed above was not an inclusion criterion for this review.
Main outcomes for 'Summary of findings' tables
We reported the primary outcomes and the severity of PTSD in patients treated in ICUs, patient or carer satisfaction with the information provided, HRQoL, and adverse effects, in 'Summary of findings' tables.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
the Cochrane Central Register of Controlled Trials (CENTRAL), the Cochrane Library, issue 3, 2017;
MEDLINE OvidSP (1946 to 10 April 2017);
Embase OvidSP (1974 to 10 April 2017);
PsycINFO OvidSP (1806 to 10 April 2017); and
CINAHL (Cumulative Index to Nursing and Allied Health Literature) EBSCO (1937 to 10 April 2017).
We conducted a preliminary search in CENTRAL on 17 January 2017 using the CENTRAL scoping search strategy (Appendix 1) whilst the tailored database searches were being finalised. On 10 April 2017, we ran the finalised search strategies for the following databases: CENTRAL (Appendix 2), MEDLINE (Appendix 3), Embase (Appendix 4), PsycINFO (Appendix 5), and CINAHL (Appendix 6). The results from the CENTRAL scoping search were combined with results of the finalised search strategies, and all duplicates were removed.
We also searched the US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en/) on 24 March 2017 for ongoing and recently completed studies. We searched all databases with no restriction on region or language of publication.
Searching other resources
We checked the references of all relevant primary studies and review articles (from 2010 onwards) to identify additional studies that might have been relevant to the review. We contacted authors of included studies for advice about other relevant studies.
We conducted a grey literature search through OpenGrey (www.opengrey.eu./) on 31 August 2017.
Data collection and analysis
Selection of studies
Two review authors independently screened all titles and abstracts identified by the searches to determine which met the inclusion criteria, retrieving the full texts of any papers considered to be potentially relevant. Two review authors independently screened the full‐text articles for inclusion or exclusion. Any discrepancies were resolved by discussion until consensus was reached, or through consultation with a third review author where necessary. We categorised all potentially relevant papers excluded from the review at this stage as excluded studies and provided the reasons for their exclusion in the Characteristics of excluded studies table. We also provided citation details and any available information about ongoing studies, and collated and reported details of duplicate publications, so that each study (rather than each report) was the unit of interest in the review. We reported the screening and selection process in an adapted PRISMA flow chart (Liberati 2009).
Data extraction and management
Two review authors extracted data independently from included studies. Any discrepancies were resolved by discussion until consensus was reached, or through consultation with a third review author where necessary. We developed and piloted a data extraction template and used Covidence to extract the following details of the included studies: funding source, declaration of interests for the primary investigators, aim of intervention, study design and duration, study setting, description of intervention and comparator (to include whether it was generic or personalised and frequency of intervention); the following patient participant characteristics by intervention/comparator group: number randomised, number excluded from analyses, age, gender body mass index, measure of illness (e.g. Acute Physiologic Assessment and Chronic Health Evaluation (APACHE‐II) score, Glasgow Coma score, Sequential Organ Failure Assessment (SOFA) score), health literacy, and intubation status; and the following carer participant characteristics by intervention/comparator group: age, gender, relationship to patient participant, and health literacy status (Covidence). We used this information to populate Characteristics of included studies tables. We also extracted outcome data from the results of the included studies (see Primary outcomes and Secondary outcomes). We imported extracted data in Covidence into Review Manager 5 (Covidence; Review Manager 2014).
Assessment of risk of bias in included studies
We assessed and reported on the methodological risk of bias of included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and the Cochrane Consumers and Communication guidelines (Higgins 2011; Ryan 2013), which recommend the explicit reporting of the following individual elements for RCTs: random sequence generation; allocation sequence concealment; blinding (participants, personnel); blinding (outcome assessment); completeness of outcome data; selective outcome reporting; and other sources of bias (e.g. imbalances in baseline characteristics of intervention and comparator groups). We considered blinding separately for different outcomes where appropriate, and separately assessed risk of detection bias for patient‐related outcomes and carer‐related outcomes. We considered studies to have a high risk of bias if they reported a loss of more than 10% of patient or carer participants, and if the loss was not explained or was uneven between comparison groups. We considered risk of bias for selective recruitment in cluster RCTs, and whether analysis methods accounted for unit of randomisation, reporting this in the random sequence generation and other sources of bias domains. We did not complete 'Risk of bias' judgements for outcomes that were not reported. We judged each item as being at high, low, or unclear risk of bias as set out in the criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and provided a quote from the study report and a justification for our judgement for each item in the 'Risk of bias' table in Characteristics of included studies. We planned to assess and report quasi‐RCTs as being at a high risk of bias for the random sequence generation item of the 'Risk of bias' tool.
A study was deemed as at high risk of bias if it was considered to be at high or unclear risk of bias for either the sequence generation or allocation concealment domain, based on growing empirical evidence that these factors are particularly important potential sources of bias (Higgins 2011). We planned to conduct sensitivity analyses excluding studies at unclear or high risk to investigate the effects of this decision on effect estimates for studies in which meta‐analyses were conducted. However, as we did not combine any data in meta‐analysis, we did not conduct this sensitivity analysis.
Two review authors independently assessed the risk of bias of included studies, with any disagreements resolved by discussion to reach consensus. We contacted study authors for additional information about the included studies or for clarification of the study methods as required. We incorporated the results of the 'Risk of bias' assessment into the review through standard tables, and systematic narrative description and commentary about each of the elements, leading to an overall assessment of the risk of bias of included studies and a judgement about the internal validity of the results of the review.
Measures of treatment effect
Although we did not conduct meta‐analysis in this review, we calculated the mean difference (MD) and 95% confidence interval (CI) for continuous outcomes in each study using the mean, standard deviation (SD), and number of people assessed for both the intervention and comparison groups as reported by study authors. We calculated the MD and 95% CI using the Review Manager 5 calculator (Review Manager 2014). If studies did not report a mean and SD, we presented measures (e.g. median and range) as reported by study authors. Again, we were unable to conduct meta‐analysis on dichotomous outcomes in this review. We calculated a risk ratio (RR) and 95% CI using number of events and the number of people assessed in the intervention and comparison groups in each study; we calculated RRs and 95% CI using the Review Manager 5 calculator (Review Manager 2014). We provided a narrative description of data reported by study authors, and when data were available using an appropriate measure, we included effect estimates for each study using the calculated MDs or RRs.
Unit of analysis issues
We did not include cross‐over trials in this review. Where multiple trial arms were reported in a single trial, we included only the relevant arms. If two comparisons (e.g. intervention A versus no intervention and intervention B versus no intervention) were combined in the same meta‐analysis, we planned to halve the control group (e.g. no intervention) to avoid double‐counting. If we included cluster RCTs, we planned to check for unit of analysis errors. We reported data if the participant was the unit of randomisation (rather than the study centre), and we planned that if unit of analysis errors were present, we would not combine data from cluster RCTs in meta‐analysis.
Dealing with missing data
We contacted study authors to obtain missing data (participant, outcome, or summary data). For participant data, we conducted analysis on an intention‐to‐treat basis where possible; otherwise we analysed data as reported. We reported on the levels of loss to follow‐up and assessed this as a source of potential bias.
For missing outcome or summary data, we planned to impute missing data where possible (for methods relevant to dichotomous data, see Higgins 2008) and report any assumptions in the review. We planned to investigate through sensitivity analyses the effects of any imputed data on pooled effect estimates.
Assessment of heterogeneity
We considered whether studies were sufficiently similar (based on consideration of populations, interventions, and setting) and assessed the degree of statistical heterogeneity by visual inspection of forest plots and by examining the Chi² test for heterogeneity. We quantified statistical heterogeneity using the I² statistic. An I² value of 50% or more is considered to represent substantial levels of heterogeneity, but we interpreted this value in light of the size and direction of effects and the strength of the evidence for heterogeneity (based on consideration of populations, interventions, and setting), using the P value from the Chi² test (Higgins 2011).
Where we detected substantial clinical, methodological, or statistical heterogeneity across included studies, we did not report pooled results from meta‐analysis but instead used a narrative approach to data synthesis. We attempted to explore possible clinical or methodological reasons for this variation by grouping studies that were similar in terms of populations, intervention features, or other factors, to explore differences in intervention effects.
Assessment of reporting biases
We assessed reporting bias qualitatively based on the characteristics of the included studies (e.g. if only small studies that indicate positive findings were identified for inclusion), and if information obtained from contact with study authors suggested that there were relevant unpublished studies.
We did not identify sufficient included studies (at least 10) to justify construction of a funnel plot to investigate small‐study effects and to assess the presence of publication bias (Sterne 2011).
Data synthesis
Our decision whether to meta‐analyse data was based on whether the interventions in the included trials were similar enough in terms of participants, settings, intervention, comparison, and outcome measures to ensure meaningful conclusions from a statistically pooled result.
Because we were unable to pool the data statistically using meta‐analysis for some outcomes, we conducted a narrative synthesis of results, and when possible used effect estimates for each study calculated using the Review Manager 5 calculator (Review Manager 2014). We presented the major outcomes and results, organised by outcome for each main comparison, and we presented data in tables and narratively summarised the results as reported by study authors.
Subgroup analysis and investigation of heterogeneity
The effect of an information or education intervention might be expected to vary with different characteristics of the intervention itself, such as format (e.g. brochure versus one‐to‐one education session), frequency (e.g. a single verbal counselling session versus monthly sessions), specificity (e.g. tailored versus non‐tailored information), or information provider (e.g. doctor or nurse). The condition of the participant may also affect the participant's ability to receive or comprehend the information or education. For example, intubation status may influence the effectiveness of information interventions that are designed to be bidirectional between patient and healthcare provider, as the intubated patient would likely find it more difficult to communicate questions to the physician or nurse. We considered it unlikely that consciousness level would influence the results (and we did not perform a subgroup analysis by consciousness level) in as much as it would not be possible to deliver an information intervention to an unconscious patient. We did not exclude this population of patients, as the intervention may have a beneficial effect on the unconscious patient's carer. We therefore planned to perform subgroup analyses to investigate the following potential effect modifiers:
type of intervention: tailored versus non‐tailored;
type of intervention platform: verbal versus written versus digital;
category of information provider: doctor versus nurse versus psychologist versus support worker;
frequency of intervention: once (e.g. one‐off verbal counselling session) versus multiple sessions (e.g. monthly verbal counselling sessions); and
intubation status of the participant: intubated versus non‐intubated patients.
We presented a narrative form of subgroup analysis in the absence of pooled statistical data.
Sensitivity analysis
We did not carry out sensitivity analyses because we did not conduct meta‐analyses in this review.
'Summary of findings' tables
We prepared separate 'Summary of findings' tables to present the findings relating to each of the stated comparisons. We used the methods described in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011). For each table, we presented the results for the major comparisons of the review, for each of the major primary outcomes, including potential harms, as outlined in Types of outcome measures. We used the GRADE system to rank the certainty of the evidence using GRADEpro GDT software (GRADEpro GDT; Schünemann 2011). Through use of the GRADE system, we assessed the certainty of the evidence for each outcome on each of the following domains: study limitations, inconsistency, imprecision, indirectness, and publication bias. Two review authors independently assessed the certainty of the evidence as implemented and described in the GRADEpro software (GRADEpro GDT; Schünemann 2011). If meta‐analysis was not possible, we presented results in a narrative 'Summary of findings' table format, such as that used by Chan 2011.
Ensuring relevance to decisions in health care
The protocol and review received feedback from at least one consumer referee in addition to a health professional as part of the Cochrane Consumers and Communication Group’s standard editorial process. Additionally, a member of the review author team (DE) visited an ICU unit and ICU follow‐up clinic before drafting this protocol in order to better understand the challenges faced by critically ill patients and their relatives during the recovery process, and the types of education or information interventions currently available. The central theme of many of the discussions, that is that the provision of information was crucial to the psychological recovery of patients (and carers), emphasised the need for this review.
Results
Description of studies
Results of the search
We screened 18,073 titles and abstracts from database searches, backward citation searches of relevant reviews, forward citation searches of eligible studies, searches of clinical trials registers, and grey literature searches. We considered the full‐text of 48 records. See Figure 1.
1.
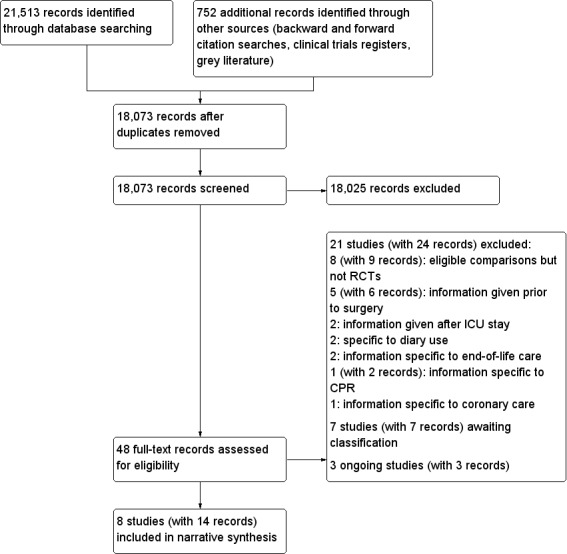
Study flow diagram.
Included studies
See Characteristics of included studies.
We included eight RCTs; seven used a parallel design (Azoulay 2002; Carson 2016; Curtis 2016; Demircelik 2016; Fleischer 2014; Hwang 1998; Torke 2016), and one used a cluster parallel design (Bench 2015). We found no quasi‐RCTs.
Study population
We included studies that recruited participants who were patients in the ICU (we refer to these as patient participants) or family members, carers, or significant representatives of patients in the ICU (we refer to these as carer participants).
Studies had 1157 randomised patient participants and 943 randomised carer participants.
Participants were adults; one study recruited patient participants from 16 years of age, although the mean age indicated that most patient participants were older than 18 years of age (Hwang 1998). Carer participants included related family members (spouses, parents, siblings, and children), and unrelated significant representatives. We collected data on education level of patient and carer participants when available. Azoulay 2002, which was conducted in France, reported that all carer participants were able to speak French and that nine of 204 carer participants were healthcare professionals. Curtis 2016 reported education levels of carer participants, with eight out of 268 participants educated below high school level. Demircelik 2016 included 38 out of 100 patient participants with university level education. Hwang 1998 reported that 29 out of 60 patient participants were educated below middle school level. Torke 2016 reported education level as number of years of education, with a mean (SD) of 12.3 years (± 1.5) in the intervention group, and 15.5 years (± 2.6) in the control group. The remaining studies did not report education levels.
Study authors recruited patient participants with primary diagnoses: acute respiratory failure, shock, acute renal failure, or coma (Azoulay 2002); cardiovascular diseases (Demircelik 2016); and heart disease (Hwang 1998). The remaining studies did not report primary diagnoses. All patient participants were mechanically ventilated in Carson 2016 and Curtis 2016, and approximately a third of patient participants were mechanically ventilated in Fleischer 2014. We assumed from information in the full report that patient participants were also mechanically ventilated in Hwang 1998. The remaining studies did not report ventilation status.
Setting
All studies were conducted in the ICU; types of ICU were surgical (Azoulay 2002; Bench 2015; Fleischer 2014; Hwang 1998), medical (Azoulay 2002; Bench 2015; Carson 2016; Fleischer 2014; Torke 2016), coronary (Demircelik 2016), and trauma (Bench 2015; Curtis 2016). The studies were conducted in France, the UK, the USA, Germany, Taiwan, and Turkey.
Interventions
Three studies designed an intervention targeted at the patient participant (Demircelik 2016; Fleischer 2014; Hwang 1998). Four studies designed an intervention targeted at the carer participant (Azoulay 2002; Carson 2016; Curtis 2016; Torke 2016). One study designed an intervention targeted at both the patient and carer participant (Bench 2015).
We included studies for the two comparison groups. In summary, types of intervention were as follows.
Comparison 1: information or education intervention versus no information or education intervention
Nurses gave multimedia education training to patient participants versus no provision of information (Demircelik 2016).
Study nurses gave standardised and structured verbal information about the specific aspects of the ICU to the patient participant on the first day of the ICU stay versus a standardised non‐specific conversation of the same length (Fleischer 2014).
Audio message about the ICU and treatment plan recorded by physician and played to patient participant after heart surgery versus no information (Hwang 1998).
A Family Navigator was appointed to each carer participant to provide individualised information and support versus usual care (Torke 2016).
Comparison 2: information or education intervention as part of a complex intervention versus complex intervention without information or education
A family information leaflet given to carer participants at ICU admission alongside standard information that included daily meetings with the physician versus standard information only (Azoulay 2002). Because study authors described "standard information" in this study, which we believe was more enhanced than the description of standard care in other studies, we categorised this standard care as a complex intervention.
A User Centred Critical Care Discharge Information Pack (UCCDIP) that encouraged active participation given to patient and carer participants by bedside nurses and ad hoc verbal discharge information from healthcare professionals versus a standard ICU information booklet without discussion with bedside nurses and ad hoc verbal discharge information versus only ad hoc verbal discharge information (Bench 2015).
Structured family meetings led by palliative care team plus standard brochure and routine family meetings led by ICU clinicians versus standard brochure and routine family meetings led by ICU clinicians (Carson 2016).
Trained communication facilitator provided personalised information and emotional support to carer participant and opportunities to discuss concerns, and included information sharing with clinicians versus standardised verbal information about time in the ICU and the ICU transition (Curtis 2016).
Funding sources
Funding sources were reported in six studies with no conflicts of interest (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016; Fleischer 2014; Torke 2016). Two studies did not report funding sources (Demircelik 2016; Hwang 1998).
Excluded studies
We excluded 21 studies. See Characteristics of excluded studies.
We excluded eight studies that described relevant information interventions given to carers or patients in the ICU and were not RCTs (Barnett 2011; Chien 2006; Daly 2010; Medland 1998; Mistraletti 2017; Mitchell 2004; Othman 2016; White 2012). We excluded five studies in which healthcare professionals provided information to elective surgical patients and their carers prior to the ICU stay (Berg 2006; Guo 2012; Lai 2016; Lynn‐McHale 1997; Shin 2017); these studies were not RCTs. We excluded two RCTs in which healthcare professionals provided information after the ICU stay (Jones 2003; Walsh 2012). We excluded two studies in which caregivers and family members used a diary during the ICU stay, which was equivalent to information provision after the ICU stay (Garrouste‐Orgeas 2010; Jones 2009). We excluded two RCTs in which healthcare professionals provided information to carers related to bereavement and end‐of‐life decisions for ICU patients (Kirchhoff 2008; Lautrette 2007). We excluded one RCT in which healthcare professionals provided information to carers related specifically to cardiopulmonary resuscitation of ICU patients (Wilson 2015), and one study in which patients were in a coronary care unit and information was related specifically to cardiac patient health and disease management (Weibel 2016).
Studies awaiting classification
We were unable to assess eligibility for seven studies (Herlihy 2014; IRCT201111148100N1; IRCT2014102819728N1; McCarthy 2017; NCT01147978; NCT02067559; NCT02415634). See Characteristics of studies awaiting classification.
We identified five studies during searches of clinical trials registers; these studies were completed, but published reports of the results were not available (IRCT201111148100N1; IRCT2014102819728N1; NCT01147978; NCT02067559; NCT02415634). Two studies were published as abstracts with insufficient information (Herlihy 2014; McCarthy 2017).
Ongoing studies
We identified three ongoing studies from clinical trial register searches (NCT01982877; NCT02445937; NCT02931851). See Characteristics of ongoing studies.
Study authors describe interventions that involve family meetings with trained healthcare professionals (NCT01982877; NCT02445937), and use of a website to provide information to patient and carer participants (NCT02931851).
Risk of bias in included studies
See 'Risk of bias' graph (Figure 2) and 'Risk of bias' summary (Figure 3).
2.
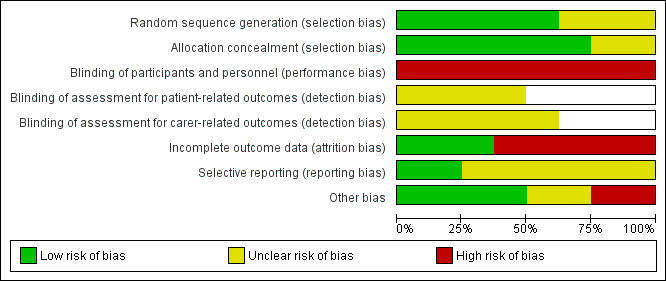
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
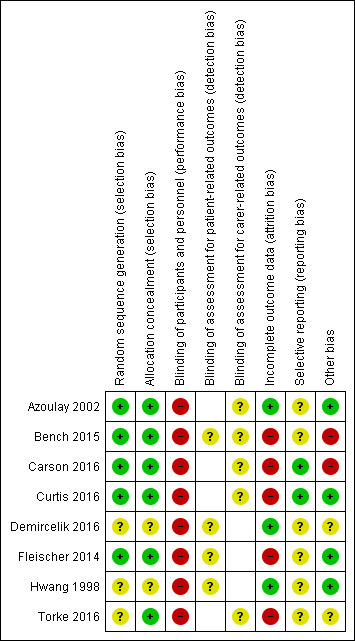
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Blank spaces indicate that outcome was not measured by study authors.
Allocation
All studies were described as randomised, and five studies provided sufficient details on the method of randomisation (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016; Fleischer 2014); we judged these studies as having a low risk of bias. Three studies provided no details on method of randomisation, and we judged risk of bias as unclear (Demircelik 2016; Hwang 1998; Torke 2016).
Six studies provided sufficient details about methods used to conceal allocation from healthcare professionals (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016; Fleischer 2014; Torke 2016); we judged these studies as having a low risk of bias. Two studies provided no details, and we judged risk of bias as unclear (Demircelik 2016; Hwang 1998).
Blinding
It was not feasible to blind participants and healthcare professionals to the intervention, and we judged all studies as having a high risk of performance bias. Most outcome assessments involved patient or carer responses to interview questions or self completion of questionnaires. We were unable to judge whether lack of participant blinding could influence outcome assessment, and assessed risk of detection bias as unclear for both patient participant‐ and carer participant‐related outcomes in all studies. We did not assess risk of bias for outcomes that were not reported; these are indicated by blank spaces in the 'Risk of bias' summary (Figure 3).
Incomplete outcome data
We judged three studies as having a low risk of bias because we noted few or no participant losses (Azoulay 2002; Demircelik 2016; Hwang 1998). We judged five studies as having a high risk of bias because they reported high attrition rates (loss of > 10%) among carer participants, and imbalance between groups or in reasons for participant loss (Bench 2015; Carson 2016; Curtis 2016; Fleischer 2014; Torke 2016).
Selective reporting
Two studies had prospective registration with clinical trials registers, and we noted that outcomes in clinical trials registration documents were the same as the reported outcomes (Carson 2016; Curtis 2016); we judged these studies as having a low risk of selective reporting bias. Two studies had retrospective registration with clinical trials registers, and it was not feasible to judge risk of selective reporting bias using these documents (Bench 2015; Fleischer 2014); we judged these studies as at unclear risk of selective reporting bias. We were unable to source clinical trials registration documents for four studies (Azoulay 2002; Demircelik 2016; Hwang 1998; Torke 2016), and it was not feasible to judge risk of bias; we assessed these studies as having an unclear risk of selective reporting bias.
Other potential sources of bias
In one study, the control group was given a verbal "ad hoc" intervention that was not standardised, which introduced a high risk of bias because participants in the control group may have received additional information (Bench 2015). In addition, we considered the effect of the cluster design of Bench 2015 in this review; study authors reported data with the participant as the unit of randomisation, but we did not combine these data with other studies, and we did not consider this to introduce risk of bias to the review. Overall, we judged Bench 2015 as having a high risk of other sources of bias due to the ad hoc information given to the control group.
We judged one study to be at a high risk of bias because the control group had opportunities to meet with a palliative care team, and it is feasible that some participant carers in that group received equivalent information to the intervention group (Carson 2016). One study had differences in gender and years of education between carer participants (Torke 2016); it was not feasible to judge whether this may have influenced the results, and we assessed this study as at unclear risk of bias. One study had limited detail in the study report relating to intervention and control groups (Demircelik 2016); we judged this study as at unclear risk of bias. We identified no other sources of bias in the remaining studies (Azoulay 2002; Curtis 2016; Fleischer 2014; Hwang 1998).
Effects of interventions
Summary of findings for the main comparison. Information or education intervention versus no information or education intervention.
| Information or education intervention versus no information or education intervention | ||||
|
Patient or population: adult ICU patients and their carers Settings: ICUs in Turkey, Germany, Taiwan, and the USA Intervention: information or education intervention Comparison: no information or education intervention | ||||
| Outcomes | Effects of information or education interventions for adult ICU patients and their carers | No. of analysed participants (studies) | Certainty of the evidence (GRADE) | Comments |
|
Severity of anxiety in patients HADS‐A (1 week after hospital discharge); scale from 0 to 20 CINT (admission to regular ward); scale from 0 to 100 BSRS (in ICU, time point not specified); scale from 0 to 20 Lower scores in all scales indicate less anxiety. |
In 1 study, mean anxiety scores in the intervention group were 3.20 lower (3.38 to 3.02 lower). 2 studies reported mean anxiety scores with little or no difference between groups (0.40 lower in the intervention group, 4.75 lower to 3.95 higher; and 1.00 lower in the intervention group, 2.94 lower to 0.94 higher). |
332 patient participants (3 studies) | ⊕⊝⊝⊝ very lowa |
We did not pool data: statistical heterogeneity was high (I² = 99%); we noted possible clinical differences in illness severity of participants (e.g. whether patient participants were intubated), and methodological differences in types of information provision (e.g. whether information was tailored, and what type, and how often, it was presented). |
|
Severity of depression in patients HADS‐D (1 week after hospital discharge); scale from 0 to 20 BSRS (in ICU, time point not specified); scale from 0 to 20 Lower scores in both scales indicate less depression. |
In 2 studies, mean depression scores in the intervention group were 2.90 lower (4.00 to 1.80 lower); and 1.27 lower (1.47 to 1.07 lower). | 160 patient participants (2 studies) | ⊕⊝⊝⊝ very lowb |
We did not pool data: statistical heterogeneity was high (I² = 99%); we noted possible clinical differences in illness severity of participants (e.g. whether patient participants were intubated), and methodological differences in types of information provision (e.g. what type, and how often the information was presented). |
| Knowledge acquisition (patients and carers) | Not measured | ‐ | ‐ | |
| Severity of PTSD in patients treated in ICUs | Not measured | ‐ | ‐ | |
| Patient or carer satisfaction with information provided (e.g. self reported) | Not measured | ‐ | ‐ | |
|
Health‐related quality of life (HRQoL) SF‐12 MCS (3 months after ICU discharge); scale from 0 to 100 Lower scores indicate reduced HRQoL. |
In 1 study, mean HRQoL score in the intervention group was 1.30 lower (4.99 lower to 2.39 higher). | 143 patient participants (1 study) | ⊕⊝⊝⊝ very lowc |
|
| Adverse effects | Not measured | ‐ | ‐ | |
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||
| BSRS: Brief Symptom Rating Scale; HADS‐A: Hospital Anxiety and Depression Scale ‐ anxiety subscale; HADS‐D: Hospital Anxiety and Depression Scale ‐ depression subscale; ICU: intensive care unit; MCS: mental health component summary; PTSD: post‐traumatic stress disorder; SF‐12: 12‐item Short Form Health Survey | ||||
aTwo studies reported insufficient information on randomisation methods and allocation concealment; we could not judge risk of selective reporting bias due to insufficient reporting; and we were unclear if lack of blinding would have influenced outcome assessment; we downgraded by one level for study limitations. Few studies with a small sample size reported outcome data, and we could not combine data; we downgraded one level for imprecision. We noted statistical heterogeneity in outcome data between studies; we downgraded one level for inconsistency. bBoth studies reported insufficient information on randomisation methods and allocation concealment; we could not judge risk of selective reporting bias due to insufficient reporting; and we were unclear if lack of blinding would have influenced outcome assessment; we downgraded by one level for study limitations. Few studies with a small sample size reported outcome data; we downgraded one level for imprecision. We noted statistical heterogeneity in outcome data between studies; we downgraded one level for inconsistency. cWe were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition; we downgraded by one level for study limitations. Data were from a single study with a small sample size, and wide confidence interval; we downgraded two levels for imprecision.
Summary of findings 2. Information or education intervention as part of a complex intervention versus complex intervention without information or education.
| Information or education intervention as part of a complex intervention versus complex intervention without information or education | ||||
|
Patient or population: adult ICU patients and their carers Settings: ICUs in France, the UK, and the USA Intervention: information or education intervention as part of a complex intervention Comparison: complex intervention without information or education intervention | ||||
| Outcomes | Effects of information or education interventions for adult ICU patients and their carers | No. of analysed participants (studies) | Certainty of the evidence (GRADE) | Comments |
|
Severity of anxiety in patients HADS‐A (at hospital discharge or at 28 days, whichever time point was soonest); scale from 0 to 20 Lower scores indicate less anxiety. |
In 1 study, mean anxiety score (using HADS‐A) in participants given a tailored information pack was 0.09 higher (‐3.29 lower to 3.47 higher), and in participants given a standardised general ICU information leaflet was 0.25 lower (4.34 lower to 3.84 higher). | 38 patient participants (1 study) |
⊕⊝⊝⊝ very lowa |
|
|
Severity of depression in patients HADS‐D (at hospital discharge or 28 days, whichever time point was soonest); scale from 0 to 20 Lower scores indicate less depression. |
In 1 study, mean depression score (using HADS‐D) in participants given a tailored information pack was 1.26 lower (4.48 lower to 1.96 higher), and in participants given a standardised general information leaflet was 1.47 lower (6.37 lower to 3.43 higher). | 38 patient participants (1 study) |
⊕⊝⊝⊝ very lowa |
|
| Knowledge acquisition (patients and carers) | In 1 study, fewer carer participants had poor comprehension if they were given an information leaflet (RR 0.28, 95% CI 0.15 to 0.53; absolute risk difference of 29.4% fewer carer participants with poor comprehension (41.6% to 17.1% fewer)). | 175 carer participants (1 study) |
⊕⊝⊝⊝ very lowb |
|
| Severity of PTSD in patients treated in ICUs | Not measured | ‐ | ‐ | |
|
Patient or carer satisfaction with information provided CCFNI (between day 3 and day 5); scale from 14 to 56 Lower scores indicate increased satisfaction. FS‐ICU 24 (90 days after randomisation); scale from 0 to 100 Lower scores indicate less satisfaction. |
1 study noted little or no difference in level of carer participant satisfaction when they were given an information leaflet. In 1 study, mean score of family satisfaction (using FS‐ICU 24) in the intervention group was 3.20 lower (7.27 lower to 0.87 higher). |
487 carer participants (2 studies) |
⊕⊝⊝⊝ very lowc |
We did not pool data: data in one study were reported as median scores; we could not calculate a mean difference with these data. |
| Health‐related quality of life | Not measured | ‐ | ‐ | |
| Adverse effects | 1 patient participant asked to be withdrawn from the trial because she believed that completion of the HADS triggered a deterioration in her mental health. It was not reported whether this participant came from the information intervention or comparison group. | 59 patient participants (1 study) | ⊕⊝⊝⊝ very lowd |
|
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||
| CCFNI: Critical Care Family Needs Inventory; CI: confidence interval; FS‐ICU 24: Family Satisfaction in the Intensive Care Unit 24‐item survey; HADS‐A: Hospital Anxiety and Depression Scale ‐ anxiety subscale; HADS‐D: Hospital Anxiety and Depression Scale ‐ depression subscale; ICU: intensive care unit; PTSD: post‐traumatic stress disorder; RR: risk ratio | ||||
aWe were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition; we downgraded by one level for study limitations. Data were from a single study with a very small sample size; we downgraded two levels for imprecision. bWe were unclear if lack of blinding would have influenced outcome assessment, and we could not judge risk of selective reporting bias due to insufficient reporting; we downgraded by one level for study limitations. Data were from a single study with a small sample size; we downgraded two levels for imprecision. cWe were unclear if lack of blinding would have influenced outcome assessment, and we noted some inconsistencies in attrition; we downgraded by one level for study limitations. Data were from two studies; we noted a wide range of scores in one study, and a wide CI in the other study; we downgraded two levels for imprecision. dWe were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition; we downgraded by one level for study limitations. Evidence was from a single study with a very small sample size, and study authors did not report whether the single event related to the intervention group or the control group; we downgraded two levels for imprecision.
Comparison 1: information or education intervention versus no information or education intervention
Primary outcomes
Severity of anxiety in patients
Three studies measured anxiety and analysed data for 332 patient participants (Demircelik 2016; Fleischer 2014; Hwang 1998). Demircelik 2016 used the Hospital Anxiety and Depression Scale ‐ anxiety subscale (HADS‐A) at one week after hospital discharge. Fleischer 2014 used three scoring systems for anxiety: a questionnaire for surgical ICU patients (called CINT) after admission to the regular ward; the State‐Trait Anxiety Inventory (STAI); and the visual analogue scale for anxiety (VAS‐A). We used the CINT questionnaire in this review because this was the primary outcome identified by the study authors. Hwang 1998 used the Brief Symptom Rating Scale (BSRS) postoperatively in the cardiosurgical unit. Lower scores in all scales indicate less anxiety. We found substantial statistical heterogeneity between studies (I² = 99%); we noted possible clinical differences between studies in illness severity of participants (e.g. whether patient participants were intubated) and methodological differences in types of information provision (e.g. whether information was tailored; and what type, and how often, it was presented). We therefore did not pool data for anxiety. See Analysis 1.1 for unpooled data.
1.1. Analysis.
Comparison 1 Information or education intervention versus no information or education intervention, Outcome 1 Anxiety in patient participants.
We calculated mean differences (MDs) for each study using the Review Manager 5 calculator (Review Manager 2014). Demircelik 2016 found that patient participants experienced reduced anxiety if they received multimedia information compared to no information (MD ‐3.20, 95% confidence interval (CI) ‐3.38 to ‐3.02); this was a score of 3.20 points lower (indicating less anxiety) in the intervention group (3.38 to 3.02 lower). However, Fleischer 2014 found little or no difference in anxiety when patient participants received standardised and structured information compared to a standardised non‐specific conversation (MD ‐0.40, 95% CI ‐4.75 to 3.95; a score of 0.40 points lower in the intervention group, 4.75 lower to 3.95 higher), and Hwang 1998 found little or no difference in anxiety when patient participants listened to an audio message about the ICU compared to no audio message (MD ‐1.00, 95% CI ‐2.94 to 0.94; 1.00 points lower in the intervention group, 2.94 lower to 0.94 higher).
Overall, it is uncertain whether an information or education intervention compared to no information or education intervention reduces anxiety in patients due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because some studies had unclear risk of selection bias; we were unable to assess risk of selective reporting bias in studies; and it was unclear if lack of blinding would have influenced outcome assessment); one level for imprecision (because the sample size was small); and one level for inconsistency (due to unexplained statistical heterogeneity). See Table 1.
Severity of depression in patients
Two studies measured depression and analysed data for 160 participants (Demircelik 2016; Hwang 1998). Tools used to measure depression were: Hospital Anxiety and Depression Scale ‐ depression subscale (HADS‐D) at one week after hospital discharge (Demircelik 2016), and the BSRS postoperatively in the cardiosurgical unit (Hwang 1998). Lower scores on both scales indicate less depression. We found substantial statistical heterogeneity between studies (I² = 99%); we noted possible clinical differences between studies in illness severity of participants (e.g. whether patient participants were intubated) and methodological differences in types of information provision (e.g. what type, and how often the information was presented). We therefore did not pool data for depression. See Analysis 1.2 for unpooled data.
1.2. Analysis.
Comparison 1 Information or education intervention versus no information or education intervention, Outcome 2 Depression in patient participants.
We calculated MDs for each study using the Review Manager 5 calculator (Review Manager 2014). Demircelik 2016 found that patient participants who received multimedia education training experienced a slight reduction in depression compared to those who received no information (MD ‐2.90, 95% CI ‐4.00 to ‐1.80); this was a score of 2.90 points lower (indicating less depression) in the intervention group (4.00 to 1.80 lower). Hwang 1998 also found that patient participants who received an information intervention (an audio message) experienced a reduction in depression compared to those who received no information (MD ‐1.27, 95% CI ‐1.47 to ‐1.07); this was a score of 1.27 points lower (indicating less depression) in the intervention group (1.47 to 1.07 lower).
However, it is uncertain whether information or education intervention compared to no information or education intervention reduces depression in patients due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because some studies had unclear risk of selection bias; we were unable to assess risk of selective reporting bias in studies; and it was unclear if lack of blinding would have influenced outcome assessment); one level for imprecision (because the sample size was small); and one level for inconsistency (due to unexplained statistical heterogeneity). See Table 1.
Knowledge acquisition (patients and carers)
No study reported this outcome.
Secondary outcomes
Severity of PTSD in patients treated in ICUs
No study reported this outcome.
Severity of depression in carers
One study reported depression in 26 carer participants six to eight weeks after ICU discharge using the Patient Health Questionnaire‐9 (PHQ‐9), with lower scores indicating less depression (Torke 2016). Calculating MD using the Review Manager 5 calculator (Review Manager 2014), we noted that using a Family Navigator to provide information to carer participants makes little or no difference to depression of carer participants (MD 2.90, 95% CI ‐1.84 to 7.64); this is a score of 2.90 higher (indicating more depression) in the intervention group (1.84 lower to 7.64 higher). See Table 3 for data reported by study authors.
1. Comparison 1: information or education intervention versus no information or education intervention.
| Outcome: severity of depression in carers | ||||
| Study | Measurement tool |
Data as mean (SD) Intervention |
Data as mean (SD) Control |
P value* |
| Torke 2016 | PHQ‐9, for depression (at 6 to 8 weeks postdischarge) |
7.1 (± 7.4); N = 13 | 4.2 (± 4.6); N = 13 | 0.34 |
| Outcome: severity of anxiety in carers | ||||
| Study | Measurement tool |
Data as mean (SD) Intervention |
Data as mean (SD) Control |
P value* |
| Torke 2016 | GAD‐7, for anxiety (at 6 to 8 weeks postdischarge) |
5.7 (± 5.7); N = 13 | 3.9 (± 5.0); N = 13 | 0.32 |
| Outcome: health‐related quality of life | ||||
| Study | Measurement tool |
Data as mean (SD) Intervention |
Data as mean (SD) Control |
P value* |
| Fleischer 2014 | SF‐12 MCS (at 3 months postdischarge) |
46.9 (± 11.3); N = 71 | 48.2 (± 11.2); N = 72 | ‐ |
| Outcome: length of ICU stay | ||||
| Study | Measurement tool |
Data as mean (SD) Intervention |
Data as mean (SD) Control |
P value* |
| Fleischer 2014 | length of stay, days | 4.3 (± 4.5); N = 104 | 4.9 (± 5.5); N = 107 | ‐ |
*P value as reported by study authors GAD‐7: Generalized Anxiety Disorder 7‐item scale ICU: intensive care unit MCS: mental health component summary (of SF‐12) N: number of analysed participants PHQ‐9: Patient Health Questionnaire‐9 SD: standard deviation SF‐12: 12‐item Short Form Health Survey
We did not use GRADEpro GDT to assess the certainty of this evidence (GRADEpro GDT), but noted that these data were from one pilot study with methodological limitations and a very small sample size, therefore our confidence in the effect was very low.
Severity of anxiety in carers
One study reported anxiety in 26 carer participants six to eight weeks after ICU discharge using the Generalized Anxiety Disorder seven‐item scale (GAD‐7), with lower scores indicating less anxiety (Torke 2016). We calculated MD using the Review Manager 5 calculator (Review Manager 2014), and noted that using a Family Navigator to provide information to carer participants makes little or no difference to the anxiety of carer participants (MD 1.80, 95% CI ‐2.32 to 5.92); this is 1.80 higher (indicating more anxiety) in the intervention group (2.32 lower to 5.92 higher). See Table 3 for data reported by study authors.
We did not use GRADEpro GDT to assess the certainty of this evidence (GRADEpro GDT), but noted that these data were from one pilot study with methodological limitations and a very small sample size, therefore our confidence in the effect was very low.
Patient or carer satisfaction with information provided
No study reported this outcome.
Health‐related quality of life
One study reported HRQoL in 143 patient participants three months after discharge (Fleischer 2014). This study used two assessment tools to measure HRQoL: the 12‐item Short Form Health Survey (SF‐12) and the Schedule for Evaluation of Individual Quality of Life (SEIQoL). We used data from the mental component score of the SF‐12 (SF‐12 MCS); this scoring system is a shortened version of the SF‐36, which is the most commonly used tool to assess HRQoL in critically ill people (Hofhuis 2009), with lower scores indicating worse health. Study authors reported no clinically relevant differences in HRQoL at three months between patient participants who received standardised and structured verbal information and those who received a standardised non‐specific conversation; we calculated MD using the Review Manager 5 calculator, which also showed little or no difference between groups (MD ‐1.30, 95% CI ‐4.99 to 2.39); this score is 1.30 lower (indicating worse HRQoL) in the intervention group (4.99 lower to 2.39 higher). See Table 3 for data reported by study authors.
It is uncertain whether using information or education intervention compared to no information or education intervention improves HRQoL (in relation to mental function) due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because we were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition in the study) and two levels for imprecision (because evidence was from a single study; the sample size was small; and the CI was wide) (GRADEpro GDT). See Table 1.
Length of stay in the ICU
One study reported length of ICU stay for 143 patient participants (Fleischer 2014). We calculated MD using the Review Manager 5 calculator (Review Manager 2014), and found little or no difference in length of ICU stay between those who received standardised and structured verbal information and those who received a standardised non‐specific conversation (MD ‐0.60 days, 95% CI ‐1.95 to 0.75); this is 0.60 days lower in the intervention group (1.95 lower to 0.75 higher). See Table 3 for data reported by study authors.
We did not use GRADEpro GDT to assess the certainty of the evidence (GRADEpro GDT), but noted that evidence for this outcome was from one study with methodological limitations and few participants, therefore our confidence in the effect was very low .
Adverse effects
No study reported this outcome.
Subgroup analyses
We did not perform meta‐analysis on any data and were not able to conduct formal statistical subgroup analyses on data for this comparison. We attempted to group studies and performed narrative assessment of the influence of potential effect modifiers for those outcomes where at least two studies with differences in potential effect modifiers contributed data. There were relatively few studies contributing data to this comparison, and narrative grouping according to potential effect modifiers did not reveal any clear patterns in the findings based on differential influences of these factors. A narrative synthesis is presented in Appendix 7.
Sensitivity analyses
We did not perform meta‐analysis on any data and were not able to conduct sensitivity analyses on data for this comparison.
Comparison 2: information or education intervention as part of a complex intervention (e.g. information or education intervention plus support) versus complex intervention without information or education (e.g. support alone)
Primary outcomes
Severity of anxiety in patients
One study assessed anxiety at hospital discharge or at 28 days after ICU discharge using HADS‐A in 38 patient participants (Bench 2015). This study was a cluster‐randomised study with three study arms. Study authors reported data as median and range scores; we contacted the study authors, who provided raw participant data, which we used to calculate mean and SDs. See Table 4 for median (range) scores in the published report, and mean (SD) scores as calculated by the review authors using participant data from the study authors (using the Review Manager 5 calculator) (Review Manager 2014). We found little or no difference in anxiety experienced by patient participants at hospital discharge or at 28 days after ICU discharge (study authors reported data at whichever time point was soonest) regardless of whether participants were given a tailored UCCDIP, a standard ICUsteps information booklet, or ad hoc information. For participants given the tailored UCCDIP versus those given ad hoc verbal information: MD 0.09, 95% CI ‐3.29 to 3.47; this is a score of 0.09 higher (indicating more anxiety) in the UCCDIP group (3.29 lower to 3.47 higher). For participants given standard ICUsteps information booklet versus those given ad hoc verbal information: MD ‐0.25, 95% CI ‐4.34 to 3.84; this is 0.25 lower (indicating less anxiety) in the ICUsteps group (4.34 lower to 3.84 higher).
2. Comparison 2: information or education intervention as part of a complex intervention versus complex intervention without information or education.
| Outcome: severity of anxiety in patients | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Bench 2015 | HADS‐A (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest) |
UCCDIP Mean (SD)a: 6.47 (± 5.04); N = 17 Median (range): 7.0 (18); N = 17 ICUsteps Mean (SD)a: 6.13 (± 4.79); N = 8 Median (range): 6.0 (13); N = 8 |
Mean (SD)a: 6.38 (± 4.39); N = 13 Median (range): 5.0 (16); N = 13 |
≥ 0.05 |
| Outcome: severity of depression in patients | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Bench 2015 | HADS‐D (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest) |
UCCDIP Mean (SD)a: 6.59 (± 3.71); N = 17 Median (range, reported by study authors as a single number): 6.0 (12); N = 17 ICUsteps Mean (SD)a: 6.38 (± 5.90); N = 8 Median (range, reported by study authors as a single number): 4.5 (12); N = 8 |
Mean (SD)a: 7.85 (± 4.96); N = 13 Median (range): 7.0 (15); N = 13 |
≥ 0.05 |
| Outcome: knowledge acquisition | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Azoulay 2002 | Carer participant comprehension (between day 3 and 5) | 10 participants had poor comprehension; N= 87 | 36 participants had poor comprehension; N = 88 | < 0.0001 |
| Outcome: severity of depression in carers | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Bench 2015 | HADS‐D (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest) |
UCCDIP Median (range, reported by study authors as a single number): 1.0 (8); N = 5 ICUsteps Median (range, reported by study authors as a single number): 7.0 (2); N = 2 |
Median (range, reported by study authors as a single number): 18 (0); N = 1 | 0.80 |
| Carson 2016 | HADS‐D (at 3 months) | Mean (SD): 4.9 (± 4.2); N = 163 | Mean (SD): 5.0 (± 4.5); N = 149 | ‐ |
| Curtis 2016 | PHQ‐9. Depression scores (at 6 months) | Mean: 3.59; N = 66 | Mean: 5.13; N = 49 | 0.017 |
| Outcome: severity of anxiety in carers | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Bench 2015 | HADS‐A (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest) |
UCCDIP Median (range, reported by study authors as a single number): 4.0 (13); N = 5 ICUsteps Median (range, reported by study authors as a single number): 7.50 (3); N = 2 |
Median (range, reported by study authors as a single number): 16.0 (0); N = 1 | 0.90 |
| Carson 2016 | HADS‐A (at 3 months) | Mean (SD): 7.2 (± 4.6); N = 163 | Mean (SD): 6.4 (± 4.7); N = 149 | ‐ |
| Curtis 2016 | GAD‐7. Anxiety scores (at 6 months) | Mean: 3.28; N = 67 | Mean: 3.94; N = 50 | 0.430 |
| Outcome: patient or carer satisfaction with information provided | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Azoulay 2002 | CCFNI for carer participants (between day 3 and day 5); lower scores indicate increased satisfaction | Median (range): 21 (18 to 26); N = 87 | Median (range): 23 (19 to 27); N = 88 | 0.08 |
| Carson 2016 | FS‐ICU 24 for carer participants (at 3 months); higher scores indicate increased satisfaction | Mean (95% CI): 81.1 (78.3 to 83.9); N = 163 | Mean (95% CI): 84.3 (81.3 to 87.3); N = 149 | 0.13 |
| Outcome: length of ICU stay | ||||
| Study | Measurement tool |
Data Intervention |
Data Control |
P value* |
| Azoulay 2002 | Length of stay, days | Median (range): 9 (6 to 18); N = 87 | Median (range): 10 (6 to 16); N = 88 | NS |
| Bench 2015 | Length of stay, days |
UCCDIP Median (range, reported by study authors as a single number): 7.0 (104); N = 51 ICUsteps Median (range, reported by study authors as a single number): 6.0 (62); N = 48 |
Median (range, reported by study authors as a single number): 6.0 (371); N = 59 | 0.24 |
| Carson 2016 | Length of stay, days | Median (IQR): 19 (15 to 26); N = 130 | Median (IQR): 20 (15 to 30); N = 126 | 0.51 |
| Curtis 2016 | Length of stay, days | Mean (SD not reported): 17.4; N = 82 | Mean (SD not reported): 21.4; N = 86 | 0.297 |
acalculated using participant data supplied by study authors *P value as reported by study authors CCFNI: Critical Care Family Needs Inventory CI: confidence interval FS‐ICU 24: Family Satisfaction in the Intensive Care Unit 24‐item survey GAD‐7: Generalized Anxiety Disorder 7‐item scale HADS‐A: Hospital Anxiety and Depression Scale ‐ anxiety subscale HADS‐D: Hospital Anxiety and Depression Scale ‐ depression subscale ICU: intensive care unit IQR: interquartile range N: number of analysed participants NS: not significant (term used by study authors to describe P value) PHQ‐9: Patient Health Questionnaire‐9 SD: standard deviation UCCDIP: User Centred Critical Care Discharge Information Pack
It is uncertain whether an information or education intervention as part of a complex intervention compared to a complex intervention without information or education reduces anxiety in patients due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because we were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition) and two levels for imprecision (because evidence was from a single study with a very small sample size). See Table 2.
Severity of depression in patients
One study assessed depression at hospital discharge or at 28 days after ICU discharge (study authors reported data at whichever time point was soonest) using HADS‐D in 38 patient participants (Bench 2015). This study was a cluster‐randomised study with three study arms. Study authors reported data as median and range scores; we contacted the study authors, who provided raw participant data, which we used to calculate mean and SDs. See Table 4 for median (range) scores in the published report, and mean (SD) scores as calculated by the review authors (using the Review Manager 5 calculator) (Review Manager 2014). We found little or no difference in depression experienced by patient participants at hospital discharge or at 28 days after ICU discharge regardless of whether participants were given a tailored UCCDIP, a standard ICUsteps information booklet, or ad hoc information. For participants given the tailored UCCDIP versus those given ad hoc verbal information: MD ‐1.26, 95% CI ‐4.48 to 1.96; this is a score of 1.26 lower (indicating less depression) in the UCCDIP group (4.48 lower to 1.96 higher). For participants given standard ICUsteps information booklet versus those given ad hoc verbal information: MD ‐1.47, 95% CI ‐6.37 to 3.43; this is 1.47 lower (indicating less depression) in the ICUsteps group (6.37 lower to 3.43 higher).
It is uncertain whether an information or education intervention as part of a complex intervention compared to a complex intervention without information or education reduces depression in patients due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because we were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition) and two levels for imprecision (because evidence was from a single study with a very small sample size). See Table 2.
Knowledge acquisition (patients and carers)
One study assessed knowledge acquisition in 175 carer participants (Azoulay 2002). See Table 4 for data as reported by study authors.
Study authors collected information from a standardised interview on carer participants' comprehension of diagnosis, prognosis, and treatment. Study authors reported that fewer intervention group carer participants had poor comprehension (10/87, 11.5%) than those who were not given an information leaflet (36/88, 41%). We calculated a risk ratio (RR) using the Review Manager 5 calculator (RR 0.28, 95% CI 0.15 to 0.53) (Review Manager 2014); this is an absolute risk difference of 29.4% fewer carer participants with poor comprehension when a family information leaflet was used (41% to 17% fewer).
It is uncertain whether an information or education intervention as part of a complex intervention compared to a complex intervention without information or education increases knowledge acquisition in carers due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because we were unclear if lack of blinding would have influenced outcome assessment, and we could not judge risk of selective reporting bias due to insufficient reporting) and by two levels for imprecision (because evidence was from a single study with a small sample size). See Table 2.
Secondary outcomes
Severity of PTSD in patients treated in ICUs
No study reported this outcome.
Severity of depression in carers
Four studies reported depression in 610 carer participants (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). Azoulay 2002 used HADS between day three and day five, and reported that 39% of carers suffered depression; the study authors did not report data by group and reported no difference between randomised groups.
Other studies used HADS‐D (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest in Bench 2015, and at three months in Carson 2016) and PHQ‐9 at six months (Curtis 2016), with lower scores indicating less depression in both scales. It was not feasible to pool data because studies reported data differently. Bench 2015 reported median scores, and noted little or no difference between groups (P = 0.80). Carson 2016 reported unadjusted and adjusted mean data; we reported unadjusted data and noted little or no difference in depression scores between groups (MD ‐0.10, 95% CI ‐1.07 to 0.87). Curtis 2016 noted no difference in adjusted mean depression scores between groups (but reported a significant difference between groups based on P = 0.017). We included data as reported by study authors in Table 4.
Overall, the evidence suggested that the effects of information or education as part of a complex intervention compared to a complex intervention without information or education are uncertain. We did not use GRADE to assess the certainty of this evidence, but noted study limitations from our 'Risk of bias' assessments (three studies had high risk of attrition bias; we were unable to assess risk of selective reporting bias in two studies; and it was unclear whether lack of blinding would have influenced outcome assessment), and data could not be statistically pooled, which limited our certainty in the evidence and ability to draw conclusions.
Severity of anxiety in carers
Four studies reported anxiety in 612 carer participants (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). Azoulay 2002 used HADS between day three and day five, and reported that 60% of carers suffered anxiety; the study authors did not report data by group and reported no difference between randomised groups.
Other studies used HADS‐A (at hospital discharge or at 28 days post‐ICU discharge, whichever time point was soonest in Bench 2015, and at three months in Carson 2016) and GAD‐7 at six months (Curtis 2016), with lower scores indicating less anxiety in both scales. It was not feasible to pool data because studies reported data differently. Bench 2015 reported median scores, and noted little or no difference between groups (P = 0.90). Carson 2016 reported unadjusted and adjusted mean data; we reported unadjusted data and noted little or no difference in anxiety scores between groups (MD 0.80, 95% CI ‐0.23 to 1.83). Curtis 2016 reported no difference in adjusted mean anxiety scores between groups (P = 0.430). We have included data as reported by study authors in Table 4.
Overall, the evidence from studies suggested that the effects of information or education as part of a complex intervention compared to a complex intervention without information or education are uncertain for anxiety in carers. We did not use GRADE to assess the certainty of this evidence, but noted study limitations from our 'Risk of bias' assessments (three studies had high risk of attrition bias; we were unable to assess risk of selective reporting bias in two studies; and it was unclear whether lack of blinding would have influenced outcome assessment), and data could not be statistically pooled, which limited our certainty in the evidence and ability to draw conclusions.
Patient or carer satisfaction with information provided
Two studies assessed satisfaction in 487 carer participants (Azoulay 2002; Carson 2016).
Azoulay 2002 assessed carer participant satisfaction with the information provided using the Critical Care Family Needs Inventory questionnaire (CCFNI) between day three and day five. Study authors reported median scores with little or no difference between groups (P = 0.08). See Table 4 for median data as reported by study authors.
Carson 2016 used the 24‐item Family Satisfaction in the Intensive Care Unit Survey Score in carer participants (with higher scores indicating increased satisfaction); the study authors reported little or no difference in levels of satisfaction between groups when analysis was adjusted for multiple respondents and study site (MD ‐3.1, 95% CI ‐7.3 to 1.0); this is a score of 3.1 lower (indicating less satisfaction) in the intervention group (7.3 lower to 1.0 higher). See Table 4 for mean data as reported by study authors. We calculated an unadjusted analysis with the Review Manager 5 calculator using data in Table 4 (Review Manager 2014), which also showed little or no difference in carer satisfaction between groups (MD ‐3.20, 95% CI ‐7.27 to 0.87); 3.20 lower (indicating less satisfaction) in the intervention group (7.27 lower to 0.87 higher).
We did not pool data because data in Azoulay 2002 were reported as median scores rather than mean scores, but evidence from studies showed little or no difference between groups in carer satisfaction. However, it is uncertain whether an information or education intervention as part of a complex intervention compared to a complex intervention without information or education changes carer satisfaction due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (because we were unclear if lack of blinding would have influenced outcome assessment, and we noted some inconsistencies in attrition) and by two levels for imprecision (evidence was from few studies, and we noted a wide range of scores in one study, and a wide CI in another study). See Table 2.
Health‐related quality of life
No study reported this outcome.
Length of stay in the ICU
Four studies reported length of stay in the ICU for 777 patient participants (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). We could not pool data due to differences in reporting. See Table 4 for individual study data.
Azoulay 2002 reported that differences in median length of ICU stay between participants who were given a family information leaflet and standard information compared to participants who were given only standard information were not significant. Bench 2015 reported median length of ICU and noted little or no difference in length of ICU stay between participants who were given a UCCDIP compared to ad hoc information or between participants who were given an ICUsteps booklet compared to ad hoc information (P = 0.24). Carson 2016 reported median length of ICU stay and noted little or no difference in length of ICU stay between participants who accessed structured family meetings led by a palliative care team with a standard brochure and routine family meetings with ICU clinicians compared to only routine family meetings with ICU clinicians (P = 0.51). Curtis 2016 reported mean lengths of ICU stay and noted little or no difference between participants who accessed a trained communication facilitator who provided personalised information and emotional support compared to standardised verbal information (P = 0.297).
The evidence suggests that the effects of an information or education intervention as part of a complex intervention are uncertain in terms of length of ICU stay. We did not use GRADE to assess the certainty of the evidence. We noted study limitations from our 'Risk of bias' assessments (three studies had a high risk of attrition bias; we were unable to assess risk of selective reporting bias in two studies; and it was unclear whether lack of blinding would have influenced outcome assessment), and we noted wide ranges in scores; it is likely that a larger sample size would be required to assess the effect of length of ICU stay due to the wide differences in participant conditions in the ICU.
Adverse effects
One study reported adverse effects (Bench 2015). One of 59 patient participants asked to be withdrawn from the trial because completion of the HADS triggered a deterioration in her mental health status. The study authors did not report to which group this patient participant belonged.
It is uncertain whether an information or education intervention as part of a complex intervention compared to a complex intervention without information or education reduces adverse events due to very low‐certainty evidence. Using the GRADE approach, we downgraded by one level for study limitations (we were unclear if lack of blinding would have influenced outcome assessment, and we noted high attrition) and two levels for imprecision (evidence was from a single study with a very small sample size and insufficient information as to which group the data belonged). See Table 2.
Subgroup analyses
We did not perform meta‐analysis on any data and were not able to conduct formal statistical subgroup analyses on data for this comparison. We attempted to group studies and performed narrative assessment of the influence of potential effect modifiers for those outcomes where at least two studies with differences in potential effect modifiers contributed data. There were relatively few studies contributing data to this comparison, and narrative grouping according to potential effect modifiers did not reveal any clear patterns in the findings based on differential influences of these factors. A narrative synthesis is presented in Appendix 7.
Sensitivity analyses
We did not perform meta‐analysis on any data and were not able to conduct sensitivity analyses on data for this comparison.
Discussion
Summary of main results
We included eight studies in this review. Four studies compared an information or education intervention versus no information or education intervention, and four studies compared information or education intervention as part of a complex intervention versus complex intervention without information or education. We identified a further seven studies awaiting classification (five studies were completed but without publication of full report, and two studies were published only as abstracts with insufficient information) and three ongoing studies.
Overall, the evidence for studies assessing the use of an information or education intervention versus no information or education was of very low certainty. We did not pool data from three studies, one of which showed less patient anxiety following the use of an information or education intervention, and two of which showed little or no difference in patient anxiety whether or not an information or education intervention was used. Similarly, we did not pool data from two studies that reported patient depression; both studies found less patient depression when an information or education intervention was used. It was uncertain whether the use of information or education interventions improved HRQoL; evidence from one study showed little or no difference in HRQoL between groups for this comparison. We found no studies that measured or reported knowledge acquisition, severity of PTSD, patient or carer satisfaction, or adverse effects for this comparison. Although we did not use the GRADE approach to assess the certainty of the evidence for carer depression and anxiety and length of stay in the ICU, we found that an information or education intervention may make little or no difference to these outcomes.
Overall, the evidence for studies assessing the use of an information or education intervention as part of a complex intervention versus a complex intervention without information or education was also of very low certainty. One multi‐arm study found little or no difference in patient anxiety or patient depression for each intervention compared with the control group, which had no information or education part. One study reported fewer carer participants with poor comprehension in the group given information or education, and two studies found little or no difference in carer satisfaction. One adverse effect was reported in one study in which a patient withdrew due to deterioration in mental health on completion of anxiety and depression questionnaires, but it is unclear whether this participant was from the information or comparison group. We found no studies that measured or reported severity of PTSD, or HRQoL. We did not use the GRADE approach to assess the certainty of the evidence for carer depression and anxiety and length of stay in the ICU, and found that an information or education intervention as part of a complex intervention may make little or no difference to these outcomes.
Overall completeness and applicability of evidence
We identified eight studies with 1157 patient participants who were admitted to the ICU with a range of diagnoses. In addition, studies included 943 carer participants, who were described as family members, carers, and significant representatives of the patient.
We did not specify type of information in the review criteria, and the included studies varied in specific type of intervention and illness severity of participant. Interventions were verbal information, which was standardised or tailored to the individual, or written information, multimedia information, or recorded audio information. Information interventions were presented as the main source of information or presented as part of a complex support system. Three studies presented information to the patient participant; four presented information to the carer participant; and one presented information to both. Studies that presented information to patient participants may have included patients with less severe illness or prognosis than those that presented information to carer participants. Heterogeneity in the different types of information presented to participants, the timing of the interventions, and the differences in the illness severity of patient participants is an important consideration in this review, and we could not be certain that interventions in each study were applicable to all people in the ICU setting (e.g. communication may be limited depending on level of consciousness of the patient, and definitions of standard care may differ between institutions). We were unable to clearly identify any features of the intervention or its delivery that influenced the results, but this examination was limited due to the small number of studies within each comparison.
Studies did not report all outcomes, and we found limited data for this review on knowledge acquisition, patient or carer satisfaction, HRQoL, and adverse events. No studies reported PTSD. We considered these to be important outcomes in measures of the effectiveness of information or education interventions, and lack of reporting of these outcomes limited the completeness of our evidence.
In this review, we chose to focus on information given during the ICU stay; this time point may be especially distressing for patients and their carers, and their information needs especially high. We excluded studies of information interventions given before or after the ICU stay, or studies of diary use, which provided retrospective information to patients. We excluded studies that were designed to improve communication of decisions related to end‐of‐life care because these were a specific subgroup of critically ill patients with communication interventions aiming to assist in the management of grief, bereavement, counselling, and after‐death decisions.
Quality of the evidence
We noted that some studies reported insufficient methods for sequence generation and allocation concealment, which are important sources of bias. We noted a large loss of participants during study follow‐up in some studies; loss to follow‐up also included carer participants and were not always explained by death of the patient participant as could be expected in studies in the critically ill setting. We were unable to judge risk of selective reporting bias in studies that did not provide clinical trials registration. It was not feasible to blind participants to the intervention, which introduced a high risk of performance bias and may have influenced self assessed outcome data. We used the GRADE approach to assess the certainty of the evidence, downgrading evidence for study limitations.
We identified few studies, with few patient and carer participants and limited data for each of our outcomes. We identified data from single studies for some outcomes. We considered the effect of small sample size and used the GRADE approach to reduce confidence in the effects on our outcomes due to imprecision. We also noted some inconsistencies in data between studies. We did not formally consider the impact of statistical heterogeneity, as described above, or the risk of publication bias as studies were too few.
Potential biases in the review process
We conducted a thorough search, and two review authors assessed study eligibility, extracted data, and assessed risk of bias in included studies. Despite two review authors independently searching for studies, we could not be certain that we found all published or unpublished studies.
Study authors reported limited descriptions of usual or standard care in the ICU, and we expect that 'standard care', particularly regarding provision of information in the ICU, could vary considerably between studies. We used two comparison groups as described in our protocol, and grouped studies according to a 'best fit' for each comparison. Our judgements were based on information provided in the study reports, and because of unknown differences in usual care, it is possible that some studies may fit better into the alternative comparison group, which may have influenced our findings. This was particularly problematic for studies in which we expected that standard care may have had features that were enhanced relative to other studies (e.g. in Azoulay 2002).
We made some post hoc decisions during the review process. We split a secondary outcome into two separate outcomes (severity of depression and severity of anxiety). We believed that this provided greater opportunity to explore the available data within the review for outcomes related to the carer participant.
Agreements and disagreements with other studies or reviews
We identified one systematic review that assessed the effects of communication interventions delivered in the ICU (Scheunemann 2011). The authors of this review concluded that structured family meetings improved patient‐ and carer‐related outcomes. However, the review authors did not perform meta‐analysis and evidence included non‐RCTs and RCTs, and the review focused on a more complex care intervention to improve communication. The earlier review also included a wider variety of interventions and populations, for example our review did not include interventions that targeted family members who were soon to be or who were recently bereaved. Differences in types of interventions or timing of interventions may have affected the outcome results and interpretation, for example bereaved carers may have different emotional responses than those who are supporting a patient who has just been admitted to the ICU. Recent guidelines for family‐centred care in the ICU recommended communication with family members using routine interdisciplinary conferences (Davidson 2017). The review authors noted that these recommendations were based on weak evidence, from both RCTs and non‐RCTs, and they did not conduct meta‐analysis due to heterogeneity between studies.
Authors' conclusions
Implications for practice.
We are uncertain about the effects of information or education presented to intensive care unit (ICU) patients or their carers on patient levels of anxiety and depression, knowledge acquisition, patient or carer satisfaction, health‐related quality of life, or adverse effects. We are also uncertain about the effects on carer levels of anxiety and depression or length of ICU stay, and we found no evidence to assess the effects on post‐traumatic stress disorder symptoms. The evidence was of very low certainty, and our confidence in the results is limited. Our review had few studies, and the types and delivery features of the information provided differed in each study. We are therefore unclear about the most effective ways of conveying information to ICU patients and their carers to improve outcomes.
Implications for research.
Research continues in the field of information provision to ICU patients and their carers, and we identified three ongoing studies and seven completed studies that are awaiting classification. These studies may contribute to future updates of this review. We acknowledge that future studies may have differences in type of information provision, or severity of illness of the included ICU patient participant. However, we hope that further studies would increase the potential for meta‐analyses, and differences can be explored through appropriate subgroup analyses; this might increase opportunities to explore and identify the most effective ways of conveying information. We propose that future studies incorporate robust methodology, particularly with methods used to allocate participants to interventions. This review did not report outcomes related to mortality and symptoms of post‐traumatic stress disorder experienced by carers; future updates should consider these additional outcomes in the assessment of communication interventions. Furthermore, this review did not include studies of communication interventions given before or after the ICU stay, nor studies specifically addressing communication for end‐of‐life care. Incorporation of a wider range of participants and timing of delivery relative to the ICU stay in future updates may increase the amount and certainty of evidence of the effects of communication interventions providing information or education related to the ICU stay.
Notes
This protocol is based on standard text and guidance provided by Cochrane Consumers and Communication (CCCG 2013).
Acknowledgements
We thank the editors and staff of the Cochrane Consumers and Communication Review Group, particularly Rebecca Ryan, Bronwyn Hemsley, and Ann Jones for their input into the protocol (Evans 2016), We thank Rebecca Ryan, Dianne Lowe, Bronwen Merner, Ann Jones of the Cochrane Consumers and Communication Review Group, and Dr Pauline Wong (Peer Reviewer) and Belinda Macleod Smith (Consumer Referee), for their input into this review. We thank Joanne McPeake and Tara Quasim for hosting a visit to the ICU follow‐up clinic at Queen Elizabeth Hospital, Glasgow to meet ICU patients and their families/carers. We thank study authors Dr J Randall Curtis and Dr Suzanne Bench, who provided additional information to the review authors.
Appendices
Appendix 1. CENTRAL search strategy (scoping)
#1MeSH descriptor: [Intensive Care Units] #2(icu or icus or intensive care):ti,ab,kw #3MeSH descriptor: [Critical Care] #4MeSH descriptor: [Critical Illness] #5MeSH descriptor: [Emergency Medical Services] #6MeSH descriptor: [Emergency Treatment] #7((intensive or critical or emergency or trauma) next care):ti,ab,kw #8(emergency near/2 (service* or treatment*)):ti,ab,kw #9MeSH descriptor: [Emergencies] #10#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 #11MeSH descriptor: [Patient Education as Topic] #12((patient or client or carer or caregiver or care giver or parent or family or providing or provision of or supplying or supplied) near/1 (education or information)):ti,ab,kw #13MeSH descriptor: [Health Communication] #14MeSH descriptor: [Counseling] #15MeSH descriptor: [Teaching Materials] #16#11 or #12 or #13 or #14 or #15 #17(audio* or video* or cassette* or tape? or dvd* or compact disc? or cd or cds or multimedia or multi media):ti,ab,kw #18MeSH descriptor: [Internet] #19MeSH descriptor: [Telecommunications] #20(internet or web or website* or online or on line or electronic* or computer* or email* or mail* or blog* or weblog* or podcast* or portal?):ti,ab,kw #21MeSH descriptor: [Computer‐Assisted Instruction] #22(telephon* or phone or phones):ti,ab,kw #23MeSH descriptor: [Mobile Applications] #24(mobile device* or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or text messag* or sms or ehealth or e‐health):ti,ab,kw #25(pamphlet* or booklet* or leaflet* or flyer* or poster? or brochure* or print* material*):ti,ab,kw #26((education* or teaching or instruction* or counsel?ing or advisory or information*) near/1 (material* or program* or session*)):ti,ab,kw #27MeSH descriptor: [Communication] #28MeSH descriptor: [Information Services] #29MeSH descriptor: [Information Dissemination] #30#17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 #31(patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or relatives):ti,ab,kw #32#30 and #31 #33#16 or #32 #34#10 and #33
Appendix 2. CENTRAL search strategy (final)
#1[mh "intensive care units"] #2(icu or icus or intensive care or ccu or ccus):ti,ab,kw #3(("special care" or burn or "coronary care" or cardiac or "respiratory care" or stroke) near/2 (unit* or room*)):ti,ab,kw #4[mh "emergency medical services"] #5[mh "emergency treatment"] #6((critical or emergency or trauma) next care):ti,ab,kw #7(emergency near/2 (service* or treatment*)):ti,ab,kw #8"critical* ill*":ti,ab,kw #9(emergency or emergencies):kw #10[mh "respiration artificial"] #11[mh "nutritional support"] #12(resuscitation or cpr or "life support" or (artificial near/1 (respiration or ventilation or feeding))):ti,ab,kw #13((heart or cardiac) near/2 (stimulation or massage)):ti,ab,kw #14("trauma cent*" or "emergency ward*"):ti,ab,kw #15{or #1‐#14} #16((patient* or client* or carer* or caregiver* or "care giver*" or parent* or family or families or providing or "provision of" or supplying or supplied) near/3 (educat* or inform*)):ti,ab,kw #17(counseling or "health communication"):kw #18[mh "teaching materials"] #19{or #16‐#18} #20(audio* or video* or cassette* or tape* or recording or dvd* or "compact dis*" or cd or cds or multimedia or "multi media"):ti,ab,kw #21[mh internet] #22[mh telecommunications] #23(internet or web or website* or online or "on line" or electronic* or digital* or computer* or email* or mail* or blog* or weblog* or podcast* or portal* or "social media" or facebook):ti,ab,kw #24(telephon* or phone or phones):ti,ab,kw #25("mobile application*" or "mobile device*" or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or "text messag*" or sms or ehealth or e‐health):ti,ab,kw #26(pamphlet* or booklet* or leaflet* or flyer* or poster or posters or brochure* or ((print* or written) next (material* or information or advice or communication or intervention*))):ti,ab,kw #27((education* or teaching or instruction* or counsel* or advisory or information*) next (material* or program* or session*)):ti,ab,kw #28[mh ^communication] #29"medical information":kw #30"interpersonal communication":kw #31[mh "professional patient relations"] #32[mh ^"professional family relations"] #33("doctor patient relation" or "nurse patient relationship"):kw #34[mh "verbal behavior"] #35(face‐to‐face or conversation* or ((verbal* or oral*) near/2 (communicat* or educat* or teach* or instruct* or inform* or advis* or advice* or intervention*))):ti,ab,kw #36"information service*":kw #37"information dissemination":kw #38{or #20‐#37} #39(patient* or client* or carer* or caregiver* or "care giver*" or parent* or family or families or relatives):ti,ab,kw #40#38 and #39 #41#19 or #40 #42#15 and #41
Appendix 3. MEDLINE search strategy
1. exp intensive care units/
2. (icu or icus or intensive care or ccu or ccus).ti,ab,kf.
3. ((special care or burn or coronary care or cardiac or respiratory care or stroke) adj2 (unit* or room*)).ti,ab,kf.
4. critical care/
5. critical illness/
6. exp emergency medical services/
7. exp emergency treatment/
8. ((critical or emergency or trauma) adj care).ti,ab,kf.
9. (emergency adj2 (service* or treatment*)).ti,ab,kf.
10. emergencies/
11. exp respiration artificial/
12. exp nutritional support/
13. (resuscitation or cpr or life support or (artificial adj (respiration or ventilation or feeding))).ti,ab,kf.
14. ((heart or cardiac) adj2 (stimulation or massage)).ti,ab,kf.
15. (trauma cent* or emergency ward*).ti,ab,kf.
16. or/1‐15
17. patient education as topic/
18. ((patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or providing or provision of or supplying or supplied) adj3 (educat* or inform*)).ti,ab,kf.
19. health communication/
20. counseling/
21. exp teaching materials/
22. or/17‐21
23. (audio* or video* or cassette* or tape? or recording* or dvd* or compact disc? or cd or cds or multimedia or multi media).ti,ab,kf.
24. exp internet/
25. exp telecommunications/
26. (internet or web or website* or online or on line or electronic* or digital* or computer* or email* or mail* or blog* or weblog* or podcast* or portal? or social media or facebook).ti,ab,kf.
27. computer assisted instruction/
28. (telephon* or phone or phones).ti,ab,kf.
29. mobile applications/
30. (mobile device* or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or text messag* or sms or ehealth or e‐health).ti,ab,kf.
31. pamphlets/
32. (pamphlet* or booklet* or leaflet* or flyer* or poster? or brochure* or ((print* or written) adj (material* or information or advice or communication or intervention*))).ti,ab,kf.
33. ((education* or teaching or instruction* or counsel?ing or advisory or information*) adj (material* or program* or session*)).ti,ab,kf.
34. communication/
35. information services/
36. exp professional patient relations/
37. professional family relations/
38. exp verbal behavior/
39. (face‐to‐face or conversation* or ((verbal* or oral*) adj2 (communicat* or educat* or teach* or instruct* or inform* or advis* or advice* or intervention*))).ti,ab,kf.
40. information dissemination/
41. or/23‐40
42. (patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or relatives).mp.
43. 41 and 42
44. 22 or 43
45. 16 and 44
46. randomized controlled trial.pt.
47. controlled clinical trial.pt.
48. randomized.ab.
49. placebo.ab.
50. clinical trials as topic.sh.
51. randomly.ab.
52. trial.ti.
53. or/46‐52
54. 45 and 53
Appendix 4. Embase search strategy
1. intensive care unit/
2. (icu or icus or intensive care or ccu or ccus).ti,ab,kw.
3. ((special care or burn or coronary care or cardiac or respiratory care or stroke) adj2 (unit* or room*)).ti,ab,kw.
4. intensive care/
5. intensive care nursing/
6. exp artificial feeding/
7. exp artificial ventilation/
8. resuscitation/
9. critical illness/
10. critically ill patient/
11. emergency health service/
12. exp emergency treatment/
13. ((intensive or critical or emergency or trauma) adj care).ti,ab,kw.
14. (emergency adj2 (service* or treatment*)).ti,ab,kw.
15. emergency/
16. (resuscitation or cpr or life support or (artificial adj (respiration or ventilation or feeding))).ti,ab,kw.
17. ((heart or cardiac) adj2 (stimulation or massage)).ti,ab,kw.
18. (trauma cent* or emergency ward*).ti,ab,kw.
19. or/1‐18
20. patient education/
21. patient information/
22. ((patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or providing or provision of or supplying or supplied) adj3 (educat* or inform*)).ti,ab,kw.
23. counseling/
24. or/20‐23
25. exp audiovisual equipment/
26. exp recording/
27. (audio* or video* or cassette* or tape? or dvd* or compact disc? or cd or cds or multimedia or multi media).ti,ab,kw.
28. internet/
29. e‐mail/
30. social media/
31. (internet or web or website* or online or on line or electronic* or digital* or computer* or email* or mail* or blog* or weblog* or podcast* or portal? or social media or facebook).ti,ab,kw.
32. telephone/
33. (telephon* or phone or phones).ti,ab,kw.
34. mobile application/
35. exp mobile phone/
36. text messaging/
37. (mobile device* or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or text messag* or sms or ehealth or e‐health).ti,ab,kw.
38. (pamphlet* or booklet* or leaflet* or flyer* or poster? or brochure* or ((print* or written) adj (material* or information or advice or intervention*))).ti,ab,kw.
39. ((education* or teaching or instruction* or counsel?ing or advisory or information*) adj (material* or program* or session*)).ti,ab,kw.
40. interpersonal communication/
41. information service/
42. doctor patient relation/
43. nurse patient relationship/
44. exp verbal communication/
45. (face‐to‐face or (verbal* adj2 (communicat* or educat* or teach* or instruct* or inform* or advis* or advice* or intervention*))).ti,ab,kw.
46. information dissemination/
47. or/25‐46
48. (patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or relatives).mp.
49. 47 and 48
50. 24 or 49
51. 19 and 50
52. randomized controlled trial/
53. controlled clinical trial/
54. single blind procedure/ or double blind procedure/
55. crossover procedure/
56. random*.tw.
57. placebo*.tw.
58. ((singl* or doubl*) adj (blind* or mask*)).tw.
59. (crossover or cross over or factorial* or latin square).tw.
60. (assign* or allocat* or volunteer*).tw.
61. or/52‐60
62. 51 and 61
63. limit 62 to embase
Appendix 5. PsycINFO search strategy
1. (icu or icus or intensive care or ccu or ccus).ti,ab,hw,id.
2. ((special care or burn or coronary care or cardiac or respiratory care or stroke) adj2 (unit* or room*)).ti,ab,hw,id.
3. ((critical or emergency or trauma) adj care).ti,ab,hw,id.
4. (emergency adj2 (service* or treatment*)).ti,ab,hw,id.
5. exp life sustaining treatment/
6. (resuscitation or cpr or life support or (artificial adj (respiration or ventilation or feeding))).ti,ab,hw,id.
7. ((heart or cardiac) adj2 (stimulation or massage)).ti,ab,hw,id.
8. (trauma cent* or emergency ward*).ti,ab,hw,id.
9. or/1‐8
10. ((patient* or client* or carer* or caregiver* or care giver* or parent* or family or families or providing or provision of or supplying or supplied) adj3 (educat* or inform*)).ti,ab,hw,id.
11. health knowledge/
12. counseling/
13. exp communications media/
14. or/10‐13
15. (audio* or video* or cassette* or tape? or recording* or dvd* or compact disc? or cd or cds or multimedia or multi media).ti,ab,id.
16. exp internet/
17. exp electronic communication/
18. (internet or web or website* or online or on line or electronic* or digital* or computer* or email* or mail* or blog* or weblog* or podcast* or portal? or social media or facebook).ti,ab,hw,id.
19. (telephon* or phone or phones).ti,ab,id.
20. exp mobile devices/
21. (mobile device* or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or text messag* or sms or ehealth or e‐health).ti,ab,id.
22. (pamphlet* or booklet* or leaflet* or flyer* or poster? or brochure* or ((print* or written) adj2 (material* or information or advice or communication or intervention*))).ti,ab,hw,id.
23. ((education* or teaching or instruction* or counsel?ing or advisory or information*) adj (material* or program* or session*)).ti,ab,hw,id.
24. communication/
25. exp interpersonal communication/
26. exp verbal communication/
27. (face‐to‐face or conversation* or ((verbal* or oral*) adj2 (communicat* or inform* or educat* or instruct* or teach* or advis* or advice* or intervention*))).ti,ab,hw,id.
28. information services/
29. information dissemination/
30. or/15‐29
31. (patient* or client* or carer* or caregiver* or care giver* or parent? or family or families or relatives).ti,ab,hw,id.
32. 30 and 31
33. 14 or 32
34. 9 and 33
35. random*.ti,ab,hw,id.
36. trial*.ti,ab,hw,id.
37. controlled stud*.ti,ab,hw,id.
38. placebo*.ti,ab,hw,id.
39. ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).ti,ab,hw,id.
40. (cross over or crossover or factorial* or latin square).ti,ab,hw,id.
41. (assign* or allocat* or volunteer*).ti,ab,hw,id.
42. treatment effectiveness evaluation/
43. mental health program evaluation/
44. exp experimental design/
45. "2100".md.
46. or/35‐45
47. 34 and 46
Appendix 6. CINAHL search strategy
S50 s49
S49 s38 and s48
S48 S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47
S47 TI (singl* or doubl* or tripl* or trebl*) and TI (blind* or mask*)
S46 AB (singl* or doubl* or tripl* or trebl*) and AB (blind* or mask*)
S45 AB (random* or trial or placebo*) or TI (random* or trial or placebo*)
S44 MH Quantitative Studies
S43 MH Placebos
S42 MH Random Assignment
S41 MH Clinical Trials+
S40 PT Clinical Trial
S39 "randomi?ed controlled trial" or PT randomized controlled trial
S38 s14 and s37
S37 s17 or s36
S36 s34 and s35
S35 patient* or client* or carer* or caregiver* or "care giver*" or parent* or family or families or relatives
S34 s18 or s19 or s20 or s21 or s22 or s23 or s24 or s25 or s26 or s27 or s28 or s29 or s30 or s31 or s32 or s33
S33 information N1 (service* or dissemination)
S32 face‐to‐face or conversation* or ((verbal* or oral*) N2 (communicat* or educat* or teach* or instruct* or inform* or advis* or advice* or intervention*))
S31 MH verbal behavior+
S30 MH professional‐family relations
S29 MH professional‐patient relations+
S28 "interpersonal communication"
S27 MH communication
S26 (education* or teaching or instruction* or counsel* or advisory or information*) N1 (material* or program* or session*)
S25 pamphlet* or booklet* or leaflet* or flyer* or poster or posters or brochure* or ((print* or written) N1 (material* or information or advice or communication or intervention*))
S24 "mobile application*" or "mobile device*" or app or apps or mhealth or m‐health or cellphone* or smartphone* or iphone* or "text messag*" or sms or ehealth or e‐health
S23 telephon* or phone or phones
S22 internet or web or website* or online or "on line" or electronic* or digital* or computer* or email* or mail* or blog* or weblog* or podcast* or portal* or "social media" or facebook
S21 MH telecommunications+
S20 MH internet+
S19 audio* or video* or cassette* or tape* or recording or dvd* or "compact dis*" or cd or cds or multimedia or "multi media"
S18 MH audiovisuals+
S17 s15 or s16
S16 counseling or "health communication"
S15 (patient* or client* or carer* or caregiver* or "care giver*" or parent* or family or families or providing or "provision of" or supplying or supplied) N3 (educat* or inform*)
S14 s1 or s2 or s3 or s4 or s5 or s6 or s7 or s8 or s9 or s10 or s11 or s12 or s13
S13 "trauma cent*" or "emergency ward*"
S12 (heart or cardiac) N2 (stimulation or massage)
S11 resuscitation or cpr or "life support" or (artificial N1 (respiration or ventilation or feeding)
S10 MH nutritional support+
S9 MH respiration, artificial+
S8 MW (emergency or emergencies)
S7 "critical* ill*"
S6 emergency N2 (service* or treatment*)
S5 (critical or emergency or trauma) N1 care
S4 MH emergency treatment+
S3 ("special care" or burn or "coronary care" or cardiac or "respiratory care" or stroke) N2 (unit* or room*)
S2 icu or icus or "intensive care" or ccu or ccus
S1 MH intensive care units+
Appendix 7. Subgroup analysis: narrative summary
Comparison 1: information or education intervention versus no information or education intervention
1. Type of intervention: tailored versus non‐tailored
Demircelik 2016 and Hwang 1998 presented non‐tailored, standardised information to participants. Fleischer 2014 presented non‐tailored, standardised information and information that was tailored to participants' needs.
Severity of anxiety in patients: degree of tailoring of the information did not appear to explain differences in effects of the intervention across three studies that measured patient anxiety (Demircelik 2016; Fleischer 2014; Hwang 1998). Two studies measured the effect of non‐tailored information (Hwang 1998), and both tailored and non‐tailored information (Fleischer 2014), and reported little or no difference in patient anxiety. However, one study that also assessed non‐tailored information reported a larger mean difference in the intervention group, which indicated a reduction in anxiety when non‐tailored information was given to participants (Demircelik 2016).
2. Type of intervention platform: verbal versus written versus digital
Demircelik 2016 used multimedia education materials, and Hwang 1998 used an audio recording. Torke 2016 used verbal information, and Fleischer 2014 used verbal information with the addition of prompt cards for individualised discussion.
Severity of anxiety in patients: type of information platform did not appear to explain differences in the effects of the intervention across three studies that measured patient anxiety (Demircelik 2016; Fleischer 2014; Hwang 1998). Two studies that both reported little or no difference in patient anxiety used primarily verbal information, Fleischer 2014, and audio information (Hwang 1998). Although one study used a different platform for information (multimedia education materials) and found a decrease in patient anxiety that favoured the intervention (Demircelik 2016), we did not have sufficient evidence to report whether type of intervention platform contributed to the difference in results between studies.
Severity of depression in patients: it was unclear whether information platform might explain findings for patient depression because data were limited to only two studies (Demircelik 2016; Hwang 1998). Both studies found that patient participants in the intervention group had reduced depression, however the types of platform for the information differed, with one more recent study using multimedia education materials (Demircelik 2016), and one using an audio recording (Hwang 1998).
3. Category of information provider: doctor versus nurse versus psychologist versus support worker
Demircelik 2016 and Fleischer 2014 used nurses to provide information. Hwang 1998 presented information recorded by the participant's physician.
Severity of anxiety in patients: category of information provider did not appear to explain differences in effects of the intervention across three studies that measured patient anxiety (Demircelik 2016; Fleischer 2014; Hwang 1998). Two studies reported little or no difference in patient anxiety, and the information providers in these studies differed: in Fleischer 2014 the information providers were nurses, and in Hwang 1998 they were the participant's physician. One study in which nurses were the information providers found a decrease in patient depression that favoured the intervention (Demircelik 2016).
Severity of depression in patients: it was unclear whether category of information provider might explain findings for patient depression because data were limited to only two studies (Demircelik 2016; Hwang 1998). Both studies found that patient participants in the intervention group had reduced depression, however category of provider differed, with one study using nurses (Demircelik 2016), and the other study using the participant's physician (Hwang 1998).
4. Frequency of intervention: once (e.g. one‐off verbal counselling session) versus multiple sessions (e.g. monthly verbal counselling sessions)
The information was presented on a single occasion in two studies (Fleischer 2014; Hwang 1998). Demircelik 2016 provided no information on intervention frequency.
Severity of anxiety in patients: we could not be certain whether frequency of the intervention might explain differences in findings for patient anxiety; whilst two studies that presented information on a single occasion reported little or no difference in patient anxiety (Fleischer 2014; Hwang 1998), one study that reported a reduction in anxiety in the intervention group did not provide information on the frequency of the intervention (Demircelik 2016).
Severity of depression in patients: similarly, we could not be certain whether frequency of the intervention might explain findings for patient depression in two studies (Demircelik 2016; Hwang 1998). Whilst both studies reported reduced depression in the intervention group, only one study reported frequency of intervention, which was on a single occasion (Hwang 1998).
5. Intubation status of the participant: intubated versus non‐intubated patients
Fleischer 2014 reported numbers of patient participants that were mechanically ventilated in each group; overall 65% of patient participants were ventilated. We assumed that some participants were mechanically ventilated in Hwang 1998 due to the reported details of the audio message, and this study reported little or no difference in patient anxiety. However, Demircelik 2016 reported no details of mechanical ventilation status.
Severity of anxiety in patients: we could not determine whether intubation status of the participant might explain differences in effects of the intervention for patient anxiety because it was not certain how many, or whether or not, participants were intubated during the ICU stay in two studies (Demircelik 2016; Hwang 1998), and because study authors reported that not all participants were intubated in Fleischer 2014.
Comparison 2: information or education intervention as part of a complex intervention (e.g. information or education intervention plus support) versus complex intervention without information or education (e.g. support alone)
1. Type of intervention: tailored versus non‐tailored
Three studies presented non‐tailored, standardised information and information that was tailored to participants' needs (Azoulay 2002; Carson 2016; Curtis 2016). Bench 2015 had two intervention groups: one group presented both non‐tailored, standardised information and information that was tailored to participants' needs; the other group presented only non‐tailored, standardised information to participants.
Severity of depression in carers: we could not be certain whether type of intervention might explain findings for depression in carers. Four studies used non‐tailored, standardised information and reported little or no difference in carer depression (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). However, Bench 2015, which was a multi‐arm study, also reported little or no difference in carer depression for participants who had received tailored information alongside non‐tailored information.
Severity of anxiety in carers: we could not be certain whether type of intervention might explain findings for anxiety in carers. Again, four studies used non‐tailored, standardised information and reported little or no difference in carer anxiety (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). However, Bench 2015, which was a multi‐arm study, also reported little or no difference in carer anxiety for participants who had received tailored information alongside non‐tailored information.
Length of stay in the ICU: we could not be certain whether type of intervention might explain findings for length of ICU stay. Again, four studies used non‐tailored, standardised information and reported little or no difference in length of ICU stay (Azoulay 2002; Bench 2015; Carson 2016; Curtis 2016). However, Bench 2015, which was a multi‐arm study, also reported little or no difference in length of ICU stay for participants who had received tailored information alongside non‐tailored information.
2. Type of intervention platform: verbal versus written versus digital
Curtis 2016 used a communication facilitator and presented all information verbally. Azoulay 2002 and Carson 2016 presented written information and verbal information. Bench 2015 had two intervention groups: one presented written and verbal information, and the other presented written information.
Severity of depression in carers: we could not be certain whether type of information platform might explain findings for depression in carers. Whilst each study reported little or no difference in carer depression, the type of platform differed between groups: one study presented information verbally (Curtis 2016); two studies presented both written and verbal information (Azoulay 2002; Carson 2016); and one multi‐arm study presented written and verbal information to one group, and written information to the other group (Bench 2015).
Severity of anxiety in carers: similarly, we could not be certain whether type of information platform might explain findings for anxiety in carers. Whilst each study reported little or no difference in carer anxiety, the type of platform differed between groups: one study presented information verbally (Curtis 2016); two studies presented both written and verbal information (Azoulay 2002; Carson 2016); and one multi‐arm study presented written and verbal information to one group, and written information to the other group (Bench 2015).
Length of stay in the ICU: we could not be certain whether type of intervention platform might explain findings for length of ICU stay. Whilst each study reported little or no difference in length of ICU stay, the type of platform differed between groups: one study presented information verbally (Curtis 2016); two studies presented both written and verbal information (Azoulay 2002; Carson 2016); and one multi‐arm study presented written and verbal information to one group, and written information to the other group (Bench 2015).
3. Category of information provider: doctor versus nurse versus psychologist versus support worker
Azoulay 2002 and Curtis 2016 used a doctor to present information. Carson 2016 used a physician and a nurse to present information with additional meetings with social workers, chaplains, or staff from other disciplines when needed. Bench 2015 had two intervention groups: one used a bedside nurse to present information, and the other did not use a nurse and gave no further details about the information provider.
Severity of depression in carers: we could not be certain whether category of information provider might explain findings for depression in carers. Whilst four studies reported little or no difference in carer depression, category of information provider differed or was not sufficiently reported in studies: two studies used a doctor to present information (Azoulay 2002; Curtis 2016); one study used a multi team approach that included both doctors and nurses (Carson 2016); and one multi‐arm study used a nurse in one group and did not specify who presented information in another arm (Bench 2015).
Severity of anxiety in carers: similarly, we could not be certain whether category of information provider might explain findings for anxiety in carers. Whilst four studies reported little or no difference in carer anxiety, category of information provider differed or was not sufficiently reported in these studies: two studies used a doctor to present information (Azoulay 2002; Curtis 2016); one study used a multi team approach that included both doctors and nurses (Carson 2016); and one multi‐arm study used a nurse in one group and did not specify who presented information in another arm (Bench 2015).
Patient or carer satisfaction with information provided: we could not be certain whether category of information provider might explain findings for carer satisfaction. Two studies reported little or no difference in carer satisfaction, but these studies differed with regard to category of provider: Azoulay 2002 used a doctor to present information, and Carson 2016 used a multi team approach that included both doctors and nurses.
Length of stay in the ICU: we could not be certain whether category of information provider might explain findings for length of ICU stay. Whilst four studies reported little or no difference in length of ICU stay, category of information provider differed or was not sufficiently reported in these studies: two studies used a doctor to present information (Azoulay 2002; Curtis 2016); one study used a multi team approach that included both doctors and nurses (Carson 2016); and one multi‐arm study used a nurse in one group and did not specify who presented information in another arm (Bench 2015).
4. Frequency of intervention: once (e.g. one‐off verbal counselling session) versus multiple sessions (e.g. monthly verbal counselling sessions)
Azoulay 2002 presented information at least once every day. Bench 2015 presented information on a single occasion for both intervention groups. Carson 2016 presented information on a minimum of two occasions, with the first and second occasion separated by 10 days. Curtis 2016 provided no information on intervention frequency apart from a 24‐hour follow‐up with the carer participant after the patient participant's discharge to acute care.
Severity of depression in carers: we could not be certain whether frequency of the intervention might explain findings for carer depression. Whilst four studies reported little or no difference in carer depression, the frequency of information provision differed or was not presented in these studies: one study presented information at least daily (Azoulay 2002); one study presented information at least twice during the ICU stay (Carson 2016); one study presented information on a single occasion in each of its two intervention groups (Bench 2015); and frequency was insufficiently reported in Curtis 2016.
Severity of anxiety in carers: similarly, we could not be certain whether frequency of the intervention might explain findings for carer anxiety. Whilst four studies reported little or no difference in carer anxiety, the frequency of information provision differed or was not presented in these studies: one study presented information at least daily (Azoulay 2002); one study presented information at least twice during the ICU stay (Carson 2016); one study presented information on a single occasion in each of its two intervention groups (Bench 2015); and frequency was insufficiently reported in Curtis 2016.
Patient or carer satisfaction with information provided: we could not be certain whether frequency of intervention might explain findings for carer satisfaction. Two studies that provided information at different frequencies (Azoulay 2002 provided information at least once, and Carson 2016 provided information at least twice) reported little or no difference in carer satisfaction (Azoulay 2002; Carson 2016).
Length of stay in the ICU: we could not be certain whether frequency of the intervention might explain findings for length of ICU stay. Whilst four studies reported little or no difference in length of ICU stay, the frequency of information provision differed or was not presented in these studies: one study presented information at least daily (Azoulay 2002); one study presented information at least twice during the ICU stay (Carson 2016); one study presented information on a single occasion in each of its two intervention groups (Bench 2015); and frequency was insufficiently reported in Curtis 2016.
5. Intubation status of the participant: intubated versus non‐intubated patients
Two studies provided no details of mechanical ventilation status (Azoulay 2002; Bench 2015). Carson 2016 required patient participants to have undergone at least seven days of mechanical ventilation uninterrupted for at least 96 hours. Curtis 2016 required patient participants to be mechanically ventilated at enrolment.
Severity of depression in carers: we could not be certain whether intubation status of the participant could explain findings for carer depression. Whilst four studies reported little or no difference in carer depression, two studies included patient participants who were intubated at enrolment (Carson 2016; Curtis 2016), and two studies provided no details of intubation status of patients (Azoulay 2002; Bench 2015).
Severity of anxiety in carers: similarly, we could not be certain whether intubation status of the participant could explain findings for carer anxiety. Whilst four studies reported little or no difference in carer anxiety, two studies included patient participants who were intubated at enrolment (Carson 2016; Curtis 2016), and two studies provided no details of intubation status of patients (Azoulay 2002; Bench 2015).
Patient or carer satisfaction with information provided: we could not be certain whether intubation status of the patient participants could explain findings for carer satisfaction. Two studies reported little or no difference, but only one study reported intubation status of patient participants (Carson 2016).
Length of stay in the ICU: we could not be certain whether intubation status of the patient participants could explain findings for length of ICU stay. Whilst four studies reported little or no difference in length of ICU stay, two studies included patient participants who were intubated at enrolment (Carson 2016; Curtis 2016), and two studies provided no details of intubation status of patients (Azoulay 2002; Bench 2015).
Data and analyses
Comparison 1. Information or education intervention versus no information or education intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anxiety in patient participants | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Depression in patient participants | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Azoulay 2002.
| Methods | RCT, parallel design, 2‐arm, multicentre study Aim of the study: to determine whether a standardised "family information leaflet" improved satisfaction and comprehension of the information provided to carer participants |
|
| Participants |
Total number of randomised patient participants: 204 Total number of randomised carer participants: 204 Inclusion criteria: patient in ICU, length of stay ≥ 48 hours Exclusion criteria: patient died within 48 hours after ICU admission, carers refused to participate in the study, or no carers visited within 5 days of ICU admission Participant baseline characteristics Patient: Intervention group Age, median (range): 57 (47 to 73) years Gender, M/F: 55/32 BMI: not reported SAPS II, median (range): 40 (27 to 54) Mechanically ventilated: not reported Primary diagnoses: acute respiratory failure (N = 51), shock (N = 28), acute renal failure (N = 20), coma (N = 35) Additional information (e.g. socio‐economic characteristics, nationality, primary language): 77.7% of French descent, 17% were unemployed Health literacy status (number correct on REALM‐SF): not reported Control group Age, median (range): 61 (51 to 70) years Gender, M/F: 58/30 BMI: not reported SAPS II, median (range): 42 (30 to 55) Mechanically ventilated: not reported Primary diagnoses: acute respiratory failure (N = 48), shock (N = 29), acute renal failure (N = 20), coma (N = 31) Additional information (e.g. socio‐economic characteristics, nationality, primary language): 77.3% were of French descent, 18.2% were unemployed Health literacy status (number correct on REALM‐SF): not reported Carer: Intervention group Age, median (range): 46 (35 to 63) years Gender, M/F: 61/26 Relationship to patient: spouse (N = 38), parent (N = 7), child (N = 24), sibling (N = 13), other relative (N = 3), not related (N = 2) Additional information (e.g. socio‐economic characteristics, nationality, primary language): 5 were healthcare professionals. All spoke French. Health literacy status (number correct on REALM‐SF): not reported Control group Age median (range): 50 (40 to 61) years Gender, M/F: 65/23 Relationship to patient: spouse (N = 44), parent (N = 6), child (N = 25), sibling (N = 8), other relative (N = 2), not relative (N = 3) Additional information (e.g. socio‐economic characteristics, nationality, primary language): 4 were healthcare professionals. All spoke French. Health literacy status (number correct on REALM‐SF): not reported Country: France Setting: multicentre, 51 ICUs (medical and surgical) |
|
| Interventions |
Recipient of the intervention: carer participant Intervention group Patient participants: N= 102; losses = 15 (reasons for losses included: death, patient received no visits in first 5 days, refusal to participate. Numbers for each loss not reported by group); analysed = 87 Carer participants: N = 102; losses = 15 (reasons include those for patient); analysed = 87 Details: carer participants given a standardised FIL plus standard information. Carer participant had at least 1 meeting with physician each day during the first week of ICU admission. Information was for ICU period. Content of FIL included: ICU information, healthcare professionals, visiting times, diagram of ICU room, glossary of commonly used terms, invitation for carer participants to talk to healthcare professionals. Control group Patient participants: N = 102; losses = 14 (reasons for losses included: death, patient received no visits in first 5 days, refusal to participate. Numbers for each loss not reported by group); analysed = 88 Carer participants: N = 102; losses = 14 (reasons include those for patient); analysed = 88 Details: carer participant given standard information on diagnosis, prognosis, and treatment, specific for the ICU period. Carer participant had at least 1 meeting with physician each day during first week of ICU admission. |
|
| Outcomes |
Outcomes reported in the review: Anxiety and depression of carer participant (using HADS‐A and HADS‐D; 7 items in each questionnaire, total scores range from 0 to 21; lower scores indicate less anxiety and less depression), comprehension and satisfaction (using CCFNI; scores range from 14 to 56; lower score indicates increased satisfaction), knowledge acquisition of carer participant (interview to assess comprehension of diagnosis, prognosis, and treatment; scale not reported; poor comprehension defined as failure to understand any of the 3 components, and good comprehension as understanding of any combination of these components). All outcomes measured between day 3 and day 5. Length of stay in the ICU Other outcomes reported in the study: none |
|
| Notes |
Funding/declarations of interest: supported by a grant from the French Society for Critical Care Study dates: start date July 2001, finish date not reported Note: we used the descriptions of the intervention and control group in the study report to categorise this study into Comparison group 2 in this review (information or education interventions as part of a complex intervention versus complex intervention without information or education). Because participants in the control group had at least daily meetings with a physician and were provided with more comprehensive information specific to the ICU, we categorised this 'standard care' as a complex intervention as it was more enhanced than the description of standard care in other studies. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators used computer‐generated random‐number tables. |
| Allocation concealment (selection bias) | Low risk | An independent organisation carried out randomisation using sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind personnel and participants to group allocation |
| Blinding of assessment for carer‐related outcomes (detection bias) | Unclear risk | Knowledge acquisition and anxiety and depression using HADS, and satisfaction using CCFNI. Investigators assessing comprehension (satisfactory comprehension of diagnosis, prognosis, and treatment) were blinded to group allocation, but carers were aware of group allocation; it is not clear whether awareness of group allocation would have influenced carer‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study authors reported loss of 6 carer participants after randomisation due to refusal to participate. It is unclear whether these losses were balanced between groups. However, overall loss was low (< 10%) and is unlikely to introduce attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | Prospective clinical trials registration or details of published protocol not reported. Not feasible to assess selective outcome reporting. We noted that study authors did not report data for HADS by group; it is not clear why these data were not reported by group, and selective outcome reporting may be present. |
| Other bias | Low risk | No other sources of bias identified. |
Bench 2015.
| Methods | RCT, cluster design, 3‐arm, single‐centre study Described as pilot study Aim of the study: to provide an initial evaluation of a User Centred Critical Care Discharge Information Pack, and also to inform decisions regarding its development and evaluation and estimate power calculation for further study |
|
| Participants |
Total number of randomised patient participants: 158 Total number of randomised carer participants: 80 Inclusion criteria: patients > 18 years of age, carers > 18 years of age, elective or emergency admissions in the ICU ≥ 72 hours, patients identified for discharge to a general ward setting within the hospital, and elective discharges between 8 a.m. and 8 p.m. Monday to Friday Exclusion criteria: patients for whom active treatment had been withdrawn, inability to verbally communicate in or read English, or involvement in a phase I focus group study Participant baseline characteristics Patient: Intervention group ‐ UCCDIP Age, mean (SD): 60 (± 15.19) years Gender, M/F: 26/25 BMI: not reported APACHE II, mean (SD): 17.75 (± 5.78) Mechanically ventilated: not reported Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, nationality, primary language): ethnicity (white British, N): 40 Health literacy status (number correct on REALM‐SF): not reported Intervention group ‐ attention control arm Age, mean (SD): 59 (± 15.26) years Gender, M/F: 25/23 BMI: not reported APACHE II, mean (SD): 16.83 (± 5.76) Mechanically ventilated: not reported Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, nationality, primary language): ethnicity (white British, N): 34 Health literacy status (number correct on REALM‐SF): not reported Control group: Age, mean (SD): 61 (± 17.48) years Gender, M/F: 31/28 APACHE II, mean (SD): 16.49 (± 5.48) Mechanically ventilated: not reported Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): not reported Carer: Carer baseline characteristics were not reported by group. Overall: Age, mean (SD): 55 (± 14.6) years Gender, M/F: 28/52 Relationship to patient: spouse or long‐term partner (N = 37) Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): ethnicity (white British, N): 41 Country: UK Setting: 2 ICUs in a single teaching hospital in London (medical, surgical, and trauma) |
|
| Interventions |
Recipient of the information: patient and carer participants Intervention group ‐ UCCDIP Patient participants: N = 51 (36 clusters); losses not clearly reported by group (overall: 27 patient participant losses); analysed at time point 1 = 31 (23 clusters), analysed at time point 2 = 17 (10 clusters) Carer participants: N = not reported by group; overall: 32 carer participant losses; study authors reported no carer participant outcome data Details: patient and carer participants each given a UCCDIP with a discussion with bedside nurse. Information pack was for ICU transition period. Information included a personal discharge summary and standard information about preparing for ICU discharge and transition to the ward. Pack included opportunity for active participation (e.g. diary pages for patient or carer participants to express thoughts or feelings). Intervention given on day of discharge decision. Study participants also received usual care and ad hoc verbal discharge information from a variety of healthcare professionals. Intervention group ‐ attention control arm Patient participants: N = 48 (31 clusters); losses not clearly reported by group (overall: 27 patient participant losses); analysed at time point 1 = 28 (17 clusters); analysed at time point 2 = 8 (6 clusters) Carer participants: N = not reported by group; overall: 32 carer participant losses; study authors reported no carer participant outcome data Details: patient and carer participants given standardised booklet provided by ICUsteps charity. No discussion with bedside nurse. Information was for ICU period and ICU transition. Information contained general ICU information and post‐ICU challenges. Information did not include opportunities to reflect or consider individual needs. Intervention given on day of discharge decision. Study participants also received usual care and ad hoc verbal discharge information from a variety of healthcare professionals. Control group Patient participants: N = 59 (33 clusters); losses not clearly reported (overall: 27 patient participant losses); analysed at time point 1 = 42 (23 clusters), analysed at time point 2 = 13 (5 clusters) Carer participants: N = not reported by group; overall 32 carer participant losses; study authors reported no carer participant outcome data Details: patient and carer participants given ad hoc verbal ICU discharge information provided by a variety of healthcare professionals. |
|
| Outcomes |
Outcomes reported in the review: Anxiety and depression of the patient participant and anxiety and depression of the carer participant at 28 days postdischarge (using HADS‐A and HADS‐D; 7 items in each questionnaire, total scores range from 0 to 21; lower scores indicate less anxiety and less depression), length of stay in the ICU, adverse effects (patient participant withdrawal from study at time point 1; 5 days (± 1 day)) Other outcomes reported in the study: Anxiety and depression of the patient participant and anxiety and depression of the carer participant at 5 days postdischarge (HADS‐A and HADS‐D), patient and carer perceptions of coping (BCOPE), discharge experience of patient and carer, patient's perceptions of self care, views of staff about UCCDIP |
|
| Notes |
Funding/declarations of interest: NIHR Study dates: August 2011 to May 2012 Note: study authors provided unpublished data for carer‐related outcomes, and raw patient data, which we used to calculate mean and standard deviations for APACHE II scores at baseline, and HADS‐A and HADS‐D (the published report included data as median and range scores for HADS‐A and HADS‐D). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cluster‐randomised study that involved randomisation by day of the week (cluster) depending on each ICU. Investigators used a computer‐generated random number sequence to conduct randomisation. |
| Allocation concealment (selection bias) | Low risk | Investigators concealed group allocation using sequentially numbered, sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel to group allocation |
| Blinding of assessment for patient‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression using HADS. Study investigators conducting interviews were blinded to group allocation. However, participants were aware of allocation, and it is not clear whether awareness of group allocation would have influenced patient‐reported outcome data. |
| Blinding of assessment for carer‐related outcomes (detection bias) | Unclear risk | Carer outcomes were collected but not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | We noted a large number of losses between recruitment and week 1 (overall loss is 17%). We also noted large numbers of losses for follow‐up at 28 days in unpublished data provided by study authors. |
| Selective reporting (reporting bias) | Unclear risk | Clinical trials registration: ISRCTN47262088. Study authors report that trial registration was completed after the start of recruitment due to administration difficulties. Not feasible to assess risk of selective outcome reporting. Study authors noted that they had not reported data for carer participants, although this was an outcome in the methods section. No explanation is given for this lack of data. |
| Other bias | High risk | Study included complex interventions that also included ad hoc information. Because of this it is possible that participants in each group received the same amount of information, and we judged this study to have a high risk of other bias. We also noted the cluster study design. Results were reported with the participant as the unit of randomisation; we reported results according to the study authors because we were not including data in meta‐analysis for this review, and therefore judged the cluster design as being at low risk of bias. Our overall judgement was that the study was at high risk of other sources of bias. |
Carson 2016.
| Methods | RCT, parallel design, 2‐arm, multicentre study Aim of the study: to determine the effect of informational and emotional support meetings for carer participants led by palliative care specialists on carer‐ and patient‐centred outcomes |
|
| Participants |
Total number of randomised patient participants: 256 Total number of randomised carer participants: 365 Inclusion criteria: patients ≥ 21 years of age, treated in medical ICUs, requiring ≥ 7 days of mechanical ventilation uninterrupted for ≥ 96 hours, not expected to be weaned or die within 72 hours. Carers who had the responsibility of healthcare decision making for patient (to include multiple family members if they participated together in decision‐making process) Exclusion criteria: patients mechanically ventilated at an outside hospital for > 7 days, or had chronic neuromuscular disease, trauma, or burns. Carer decision‐maker was unavailable or lacked English proficiency, primary clinician refused to grant permission to investigators to approach patient or carer, or investigators were the attending clinician. Patients previously admitted to the study ICU, or who had a palliative care consultation prior to screening Participant baseline characteristics Patient: Intervention group Age, mean (95% CI): 58 (55.2 to 60.8) years Gender, M/F: 64/66 BMI: not reported APACHE II, mean (95% CI): 26.2 (25.2 to 27.3) Mechanically ventilated: Y Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, ethnicity, primary language): Ethnicity, Hispanic or Latino, N = 17; non‐Hispanic or non‐Latino, N = 112; insurance status, Medicare, N = 60; Medicaid, N = 11; commercial, N = 47; none, N = 9; other, N = 3 Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (95% CI): 57 (54.0 to 59.7) years Gender, M/F: 61/65 BMI: not reported APACHE II, mean (95% CI): 25.8 (24.6 to 27.0) Mechanically ventilated: yes Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, ethnicity, primary language): ethnicity, Hispanic or Latino, N = 15; non‐Hispanic or non‐Latino, N = 111. Insurance status, Medicare, N = 57; Medicaid, N = 16; commercial, N = 36; none, N = 11; other, N = 6 Health literacy status (number correct on REALM‐SF): not reported Carer: Intervention group Age, mean (95% CI): 51 (48.8 to 52.8) years Gender, M/F: 56/128 Relationship to patient: spouse (N = 57), parent (N = 18), child (N = 41), sibling (N = 11), other (N = 3) Additional information (e.g. socio‐economic characteristics, nationality, primary language): ethnicity, Hispanic or Latino, N = 28; non‐Hispanic or non‐Latino, N = 155; employment status: employed, N = 103; unemployed, N = 15; homemaker, N = 10; retired, N = 40; disabled, N = 13; student, N = 1 Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (95% CI): 51 (48.6 to 52.7) years Gender, M/F: 50/131 Relationship to patient: spouse (N = 47), parent (N = 17), child (N = 41), sibling (N = 15), other (N = 6) Additional information (e.g. socio‐economic characteristics, nationality, primary language): ethnicity, Hispanic or Latino, N = 23; non‐Hispanic or non‐Latino, N = 158; employment status: employed, N = 93; unemployed, N = 22; homemaker, N = 16; retired, N = 25; disabled, N = 22; student, N = 3 Health literacy status (number correct on REALM‐SF): not reported Country: USA Setting: multicentre, 4 medical ICUs in 3 tertiary centres |
|
| Interventions |
Recipient of the information: carer participants Intervention group Patient participants: N = 130; no losses Carer participants: N = 184; losses = 21 (15 refused to participate, data unavailable for 6); analysed = 163 at 3 months Details: carer participants given standardised brochure plus minimum of 2 meetings with palliative care physician and nurse, to include social workers, chaplains, or other disciplines as needed. Meetings structured according to a set of objectives and recommended topics. Intensive care unit clinicians held additional family meetings according to usual practice. Information was for ICU period and ICU transition and included: the nature of the patient participant's illness and treatments; prognosis for outcomes including ventilator independence, function, and life quality; impact of treatment on patient participant experience (including symptom burden); potential complications of treatment; expected care needs after hospitalisation; and alternatives to continuation of treatment. Meetings were held after 7 days of mechanical ventilation, at onset of chronic illness, and when a tracheostomy was considered. First and second meetings separated by 10 days Control group Patient participants: N = 126; no losses Carer participants: N = 181; losses = 32 (15 refused to participate, data unavailable for 17); analysed = 149 at 3 months Details: carer participant given standardised and personalised intervention. Intensive care unit clinicians managed all formal and informal family meetings according to usual practice without input from palliative care specialists. Carers given the same brochure. Intensive care unit clinicians could consult with palliative care team if required. Information was for ICU period and ICU transition. Intervention given at least once after 10 days in the ICU. |
|
| Outcomes |
Outcomes reported in the review: Anxiety and depression of the carer participant measured at 3 months (using HADS‐A and HADS‐D, 7 items in each questionnaire, total scores range from 0 to 21; lower scores indicate less anxiety and less depression), satisfaction (FS‐ICU 24; scores from 0 to 100; higher score indicates increased satisfaction), ICU length of stay Other outcomes reported in the study: PTSD symptoms of the carer participant (IES‐R) patient‐focused communication regarding the goals of care measured (After‐Death Bereavement Family Interview), Quality of Communications scale score, number of days of mechanical ventilation, ICU length of stay, hospital length of stay, limitations of ICU therapies, hospital mortality, and 90‐day survival Outcomes assessed immediately after second support meeting, then followed up at 90 days. |
|
| Notes |
Funding/declarations of interest: funded by grant from the NINR. Funders had no role in the design and conduct of the study. One author (Dr Carson) reported a consulting agreement with the Research Triangle Institute related to quality of care in long‐term acute care hospitals. Study dates: October 2010 to November 2014 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators used a computer‐generated, web‐based randomisation method. |
| Allocation concealment (selection bias) | Low risk | Use of web‐based system ensured allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind personnel and participants to group allocation |
| Blinding of assessment for carer‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression using HADS, and assessment of satisfaction using FS‐ICU 24. Study authors report that the study primary outcome assessment was blinded, and that interview assessors were also blinded. However, the study authors do not report whether independent investigators were involved in the assessments of carer‐related outcomes. It is not clear whether awareness of group allocation would have influenced carer‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition of carer participants (overall loss of 14%). Loss is imbalanced between groups. |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration: NCT01230099. Relevant review outcomes all reported in trial register documents. |
| Other bias | High risk | The control group had opportunities to meet with the palliative care team, therefore it is feasible that some carer participants in the control group may have received equivalent information to the intervention group. |
Curtis 2016.
| Methods | RCT, parallel design, 2‐arm, multicentre study (5 ICUs in 2 hospitals) Aim of the study: to determine if an ICU communication facilitator reduces family distress and intensity of end‐of‐life care |
|
| Participants |
Total number of randomised patient participants: 168 Total number of randomised carer participants: 268 Inclusion criteria: patients in ICU > 24 hours, > 18 years of age, mechanically ventilated at enrolment, SOFA score ≥ 6 or diagnostic criteria predicting ≥ 30% risk of hospital mortality, legal carer decision‐maker consent for patient participation, and a family member able to come to the hospital. Carers > 18 years of age, and able to complete consent process and questionnaires in English Exclusion criteria: not reported Participant baseline characteristics Patient: Intervention group Age, mean (SD): 52.1 (± 17.2) years Gender, M/F: 55/27 BMI: not reported SOFA, mean (SD): 9.8 (± 3.4) Mechanically ventilated: yes Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (SD): 55.3 (± 18.8) years Gender, M/F: 53/33 BMI: not reported SOFA, mean (SD): 9.9 (± 2.9) Mechanically ventilated: yes Primary diagnoses: no details Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): not reported Carer: Intervention group Age, mean (SD): 49.5 (± 12.0) years Gender, M/F: 38/93 Relationship to patient: spouse (N = 39), parent (N = 27), child (N = 33), sibling (N = 16), other relative (N = 12), not a relative (N = 4) Additional information (e.g. socio‐economic characteristics, ethnicity, primary language): education levels of carer participants were as follows: below high school (N = 4); high school diploma (N = 19); trade school or college (N = 48); undergraduate degree (N = 32); and postcollege education (N = 19). Ethnicity: Hispanic, N = 12 Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (SD): 52.4 (± 14.2) years Gender, M/F: 41/96 Relationship to patient: spouse (N = 39), parent (N = 25), child (N = 40), sibling (N = 15), other relative (N = 15), not a relative (N = 3) Additional information (e.g. socio‐economic characteristics, nationality, primary language): education levels of carer participants were as follows: below high school (N = 4); high school diploma (N = 25); trade school or college (N = 40); undergraduate degree (N = 22); and postcollege education (N = 18). Ethnicity: Hispanic, N = 10 Health literacy status (number correct on REALM‐SF): not reported Country: USA Setting: 5 ICUs, 2 hospitals, level 1 trauma centre, community‐based hospital |
|
| Interventions |
Recipient of the information: carer participants Intervention group Patient participants: N = 82 Carer participants: N = 131; analysed = 76 at 3 months, 70 at 6 months Details: carer participant provided with a "communication facilitator". Verbal information included interviews to discuss concerns, needs, and communication characteristics. Meetings with clinicians to share family concerns and needs, provision of communication and emotional support tailored to carer participant, participation in family (carer) conferences, and a 24‐hour follow‐up with carer after discharge to acute care. Study title suggests that information is about ICU transition. Control group Patient participants: N = 86 Carer participants: N = 137; analysed = 57 at 3 months, 52 at 6 months Details: carer given standardised verbal intervention. Information was for ICU period and ICU transition. |
|
| Outcomes |
Outcomes reported in the review: Depression of carer participant at 6 months (using PHQ‐9; includes 9 criteria, total score from 0 to 21; lower scores indicate less depression), anxiety of carer participants at 6 months (using GAD‐7; includes 7 criteria, total score from 0 to 21; lower scores indicate less anxiety), length of stay in the ICU (in days) Other outcomes reported in the study: Depression and anxiety of carer participant at 3 months (PHQ‐9 and GAD‐7), PTSD of carer participant, length of hospital stay, hospital mortality, and time to withdrawal of life‐support |
|
| Notes |
Funding/declarations of interest: NINR. Study authors declare no conflicts of interest. Study dates: November 2008 to October 2013 Note: study aim was to assess information related to end‐of‐life care, but study includes 75% of patient participants who did not die. Study authors provided unpublished data for number of carer participants for outcomes measured with GAD‐7 and PHQ‐9. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants assigned on a 1:1 ratio based on computer‐generated random numbers (information taken from associated reference published by the study authors in 2012 (Curtis 2016)). |
| Allocation concealment (selection bias) | Low risk | Allocation concealed in sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind personnel or participants to intervention |
| Blinding of assessment for carer‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression using GAD‐7 and PHQ‐9. Study authors do not report whether independent investigators were involved in these assessments. It is not clear whether awareness of group allocation would have influenced carer‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition of carer participants at 3‐ and 6‐month follow‐up periods (overall loss of 54%). Imbalance between groups |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration: NCT00720200. All review outcomes reported in completed study report according to protocol. |
| Other bias | Low risk | No other sources of bias identified. |
Demircelik 2016.
| Methods | RCT, parallel design, 2‐arm, multicentre study Aim of the study: to investigate the effect of multimedia nursing education on the prognosis of patients with cardiovascular diseases in terms of the incidence of disease‐related and ICU‐related depression and anxiety |
|
| Participants |
Total number of randomised patient participants: 100 Inclusion criteria: patients admitted to a coronary care unit, no verbal communication problem, physically and psychologically comfortable while completing the questionnaire, and agreed to participate in the research Exclusion criteria: patients being treated for psychiatric disease at time of admission, had prior diagnosis of psychiatric disorders, or under the influence of alcohol or substance that might prevent the patient from co‐operating in the study or impair their ability to complete the questionnaire/telephone interview Intervention group Age, mean (SD): 59 (± 13) years Gender, M/F: 34/16 BMI: not reported Primary diagnoses: cardiovascular diseases Mechanically ventilated: not reported Additional information (e.g. socio‐economic characteristics, nationality, primary language): university education (N = 17) Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (SD): 62 (± 10) years Gender, M/F: 30/20 BMI: not reported Primary diagnoses: cardiovascular diseases Mechanically ventilated: not reported Additional information (e.g. socio‐economic characteristics, nationality, primary language): university education (N = 21) Health literacy status (number correct on REALM‐SF): not reported Country: Turkey Setting: 2 ICUs |
|
| Interventions |
Recipient of the information: patient participant Intervention group Patient participants: N = 50 Details: given multimedia nursing education, where nurses gave training to patients and technical materials were prepared. Patient participant received information. Information was standardised, and materials were the same for each patient participant. Information was intended for ICU period. Control group Patient participants: N = 50 Details: not given multimedia nursing education |
|
| Outcomes |
Outcomes reported in the review: Anxiety and depression of the patient participant assessed during ICU stay and at 1‐week post‐hospital discharge via telephone follow‐up (using HADS‐A and HADS‐D; 7 items in each questionnaire, total scores range from 0 to 21; lower scores indicate less anxiety and less depression). Other outcomes reported in the study: None |
|
| Notes |
Funding/declarations of interest: not reported Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible patients in each centre were allocated to a control or experimental group by unspecified random selection. |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It is not feasible to blind participants and personnel to the group allocation. |
| Blinding of assessment for patient‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression using HADS. Study authors do not report whether independent investigators were involved in these assessments. It is not clear whether awareness of group allocation would have influenced patient‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Prospective clinical trials registration or details of published protocol not reported. Not feasible to assess selective outcome reporting |
| Other bias | Unclear risk | Limited detail in study report relating to intervention and control groups |
Fleischer 2014.
| Methods | RCT, parallel design, 2‐arm, multicentre study Aim of the study: to evaluate whether a structured information programme via face‐to‐face communication compared to a non‐specific verbal face‐to‐face communication contributes to a reduction of anxiety experienced by patient participants |
|
| Participants |
Total number of randomised participants: 211 Inclusion criteria: patients with scheduled and unscheduled ICU stays > 24 hours from enrolment. Recruited at beginning of ICU stay (within first 24 hours of consciousness postadmission) Exclusion criteria: patients with an anticipated inability to complete the mailed follow‐up questionnaire, cognitive impairment, lack of German language ability, > 48 hours awake and clear in the ICU (because intervention was intended for the beginning of ICU stay), < 18 years of age, or who were placed in a room with another study participant Participant baseline characteristics Patient: Intervention group Age, mean (SD): 63.3 (± 14.5) years Gender, M/F: 66/38 BMI: not reported SAPS II, mean (SD): 23.8 (± 8.2) Mechanically ventilated, Y/N: 70/34 Primary diagnoses: cardiac surgery (N = 52), general surgery (N = 19), medical (N = 33) Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (SD): 65.8 (± 11.8) years Gender, M/F: 71/36 BMI: not reported SAPS II, mean (SD): 26.1 (± 10.2) Mechanically ventilated, Y/N: 67/40 Primary diagnoses: cardiac surgery (N = 50), general surgery (N = 22), medical (N = 35) Additional information (e.g. socio‐economic characteristics, nationality, primary language): not reported Health literacy status (number correct on REALM‐SF): not reported Country: Germany Setting: multicentre, 3 hospitals (cardiac surgery, general surgery, medical ICUs) |
|
| Interventions |
Recipient of the information: patient participant Intervention group Patient participants: N = 104; losses at admission to acute ward = 22, losses at 3 months postdischarge = 33; analysed at admission to acute ward = 82, analysed at 3 months postdischarge = 71 Details: patient participant given standardised and personalised verbal information by study nurse. Given in addition to standard care. Individualised information structured through use of a limited number of prompt cards available for selection, with structured questions to ask the participant if more information was required at each stage. Duration of information presentation was 10 to 15 minutes and contained standardised information related to specific ICU aspects (procedural, sensory, coping information). Individualised information addressed patient participant's fears and questions. Intervention given on day 1 of ICU stay. Control group Patient participants: N = 107; 2 were given intervention on insistence (included in intention‐to‐treat analysis), losses at admission to acute ward = 17, losses at 3 months postdischarge = 35; analysed at admission to acute ward = 90, analysed at 3 months postdischarge = 72 Details: patient participant given standardised non‐specific conversation of the same length that was semi‐structured, self directed, non‐specific, and excluded information on ICU stay. Given on day 1 of ICU stay |
|
| Outcomes |
Outcomes reported in the review: Anxiety on admission to regular ward (using CINT score; calculated on a Likert scale 0 to 100; lower scores indicate less anxiety), HRQoL assessed 3 months after discharge (SF‐12 MCS; 12 questions scored on a scale of 0 to 100; higher scores indicate better QoL), length of stay (in days) Other outcomes reported in the study: Anxiety (STAI, VAS‐A), HRQoL (SF‐12 PCS and SEIQoL) |
|
| Notes |
Funding/declarations of interest: funded by the German Federal Ministry of Education and Research. Study authors declare no competing interests. Study dates: December 2007 to December 2009 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators used a computer‐generated randomisation sequence. |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed in sequentially numbered, sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded to the intervention. |
| Blinding of assessment for patient‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety using VAS and STAI, and HRQoL using SF‐12. Study authors do not report whether independent investigators were involved in these assessments. It is not clear whether awareness of group allocation would have influenced patient‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rate of attrition (overall loss at end of follow‐up is 32%). Losses are balanced between groups. However, we noted some imbalances in reasons for loss that are not explained (e.g. there are more deaths in the intervention group, and more people withdrawing consent in the control group). |
| Selective reporting (reporting bias) | Unclear risk | Registration with clinical trials register: NCT00764933, and publication of a study protocol. However, both of these documents were available after start of study. Not feasible to assess selective outcome reporting effectively |
| Other bias | Low risk | No other sources of bias identified. |
Hwang 1998.
| Methods | RCT, parallel design, 2‐arm, single‐centre study Aim of the study: to investigate the effects of an audio‐recorded message from the attending cardiac surgeon that provides information and emotional support on the physiological and psychological reactions of heart surgery patients during the early recovery phase in the ICU |
|
| Participants |
Total number of randomised participants: 60 Inclusion criteria: patients > 16 years of age, alert and oriented, with no visual or auditory defects, and no psychiatric illness or cognitive impairment Exclusion criteria: not reported Participant baseline characteristics Patient: Age not reported by group. Overall age, mean (SD): 52.7 (± 15.5) years Intervention group Gender, M/F: 18/12 BMI: not reported Illness severity: not reported Mechanically ventilated: assumed patient participants were ventilated because of description of information included in recorded message Primary diagnoses: heart disease Additional information (e.g. socio‐economic characteristics, nationality, primary language): participant education levels: < middle school (N = 13), > middle school (N = 17); occupation: professional (N = 13), non‐professional (N = 17); social class I‐III (N = 7), social class IV (N = 8), social class V (N = 15) Health literacy status (number correct on REALM‐SF): not reported Control group Gender, M/F: 16/14 BMI: not reported Illness severity: not reported Mechanically ventilated: assumed patient participants were ventilated because of description of information included in recorded message Primary diagnoses: heart disease Additional information (e.g. socio‐economic characteristics, nationality, primary language): participant education levels: < middle school (N = 16), > middle school (N = 14); occupation: professional (N = 6), non‐professional (N = 24); social class I‐III (N = 4), social class IV (N = 3), social class V (N = 23) Health literacy status (number correct on REALM‐SF): not reported Country: Taiwan Setting: ICU in National Taiwan University Hospital (surgical) |
|
| Interventions |
Recipient of the information: patient participant Intervention group Patient participants: N = 30; no losses Details: patient participant given standardised audio message recorded by physician. Message played back to patient participant during ICU recovery. Duration of message was 6 to 10 minutes and was given 5 to 10 hours after heart surgery. Information included reassurance, general ICU information, rehabilitation information, and treatment plan. Intervention given once. Control group Patient participants: N = 30; no losses Details: patient participants given no information. Patient participants given earphones to block out other noises. |
|
| Outcomes |
Outcomes reported in the review: Anxiety and depression of patient participant, postoperatively in cardiosurgical unit (using BSRS; each symptom is scored from 1 to 7 with 18 to 24 possible symptoms; lower scores indicate less depression) Other outcomes reported in the study: Pain, tension, psychological reactions, and hostility of patient participant |
|
| Notes |
Funding/declarations of interest: not reported Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomly assigned, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No evidence of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not possible to blind participants. It may have been possible to blind personnel, but insufficient details were provided. |
| Blinding of assessment for patient‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression with BSRS. Study authors do not report whether independent investigators were involved in these assessments. It is not clear whether awareness of group allocation would have influenced patient‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No clinical trial registration or pre‐published protocol. Not feasible to judge selective outcome reporting |
| Other bias | Low risk | No other sources of bias identified. |
Torke 2016.
| Methods | RCT, parallel design, 2‐arm, single‐centre study Aim of the study: to conduct a pilot study of the "Family Navigator" role for carer participants' unmet communication needs |
|
| Participants |
Total number of randomised carer participants: 26 Inclusion criteria: patients ≥ 21 years of age, admitted to medical ICU, with severe cognitive impairment determined by chart review (sedated or comatose) or a score of ≥ 8 errors on the Short Portable Mental Status Questionnaire, and the ability to contact carer within 3 days of ICU admission. Carers who were the legally authorised decision‐makers according to a healthcare power of attorney document or Indiana surrogate decision‐making law Exclusion criteria: patients imminently dying or expected to be transferred out of ICU within 24 hours of admission Participant baseline characteristics Patient: Intervention group Age, mean (SD): 53.27 (± 14.18) years Gender, M/F: 4/9 BMI: not reported SOFA, N with score ≥ 8: 9 Mechanically ventilated: not reported Primary diagnoses: not reported Additional information (e.g. socio‐economic characteristics, nationality, primary language): education, mean (SD): 11.5 (± 1.6) years; ethnicity: Hispanic (N = 0) Health literacy status (number correct on REALM‐SF): not reported Control group Age, mean (SD): 57.42 (± 11.03) years Gender, M/F: 9/6 BMI: not reported SOFA, N with score ≥ 8: 12 Mechanically ventilated: not reported Primary diagnoses: not reported Additional information (e.g. socio‐economic characteristics, nationality, primary language): education, mean (SD): 13.5 (± 3.1) years; ethnicity: Hispanic (N = 0) Health literacy status (number correct on REALM‐SF): not reported Carer: Intervention group Age, mean (SD): 50.93 (± 12.01) years Gender, M/F: 9/4 Relationship to patient: spouse (N = 8), son/daughter (N = 3), grandchild (N = 0), other (N = 2) Additional information (e.g. socio‐economic characteristics, nationality, primary language): education, mean (SD): 12.3 (± 1.5) years; ethnicity: Hispanic (N = 0) Health literacy status (number correct on REALM‐SF), mean (SD): 7.4 (± 0.7) Control group Age, mean (SD): 46.16 (± 17.36) years Gender, M/F: 3/10 Relationship to patient: spouse (N = 6), son/daughter (N = 5), grandchild (N = 0), other (N = 2) Additional information (e.g. socio‐economic characteristics, nationality, primary language): education, mean (SD): 15.5 (± 2.6) years; ethnicity: Hispanic (N = 0) Health literacy status (number correct on REALM‐SF), mean (SD): 7.2 (± 0.4) Country: USA Setting: medical ICU |
|
| Interventions |
Recipient of the information: carer participant Intervention group Carer participants: N = 13 Details: given Family Navigator, a nursing role trained to address carer participants' unmet communication and support needs. Family Navigator provided and facilitated regular clinical updates, decision options, emotional and spiritual support, active listening, and information related to hospital resources; co‐ordinated discharge transitions; and reinforced information. Information was individualised and for the carer participant. Information was for the ICU stay, and included discharge transition information and postdischarge telephone contact. Intervention was daily. Control group Carer participants: N = 13 Details: given usual care, all carer participants eligible to receive ICU support services. ICU social worker provided psychosocial support and co‐ordinated family meetings. |
|
| Outcomes |
Outcomes reported in the review: Depression of carer participant measured at 6 to 8 weeks after ICU discharge (using PHQ‐9; includes 9 criteria, each scored 0 to 3; lower scores indicate less depression); anxiety of carer participant measured at 6 to 8 weeks after ICU discharge (using GAD‐7; includes 7 criteria, each scored 0 to 3; lower scores indicate less anxiety). Other outcomes reported in the study: Post‐traumatic stress symptoms of carer participant (using IES‐R) Decision quality (using Decision Conflict Scale) assessed during weekly interviews for up to 3 decisions made. All measured at 6 to 8 weeks after ICU discharge. |
|
| Notes |
Funding/declarations of interest: supported by the National Institute on Aging Study dates: October 2013 to March 2014 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly generated group assignment. No additional details provided. |
| Allocation concealment (selection bias) | Low risk | Carer participants allocated by research co‐ordinator using sequentially numbered, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind personnel and participant to group assignment |
| Blinding of assessment for carer‐related outcomes (detection bias) | Unclear risk | Assessment of anxiety and depression using GAD‐7 and PHQ‐9. Study authors do not report whether independent investigators were involved in these assessments. It is not clear whether awareness of group allocation would have influenced carer‐reported outcome data. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Overall rates of follow‐up were 81%. Study authors do not report number of losses by group, but overall loss is > 10%. |
| Selective reporting (reporting bias) | Unclear risk | Study authors do not report clinical trial registration or details of prospectively published protocol. Not feasible to assess selective outcome reporting without these documents |
| Other bias | Unclear risk | Study authors report differences in gender and years of education between carer participant groups; those in the intervention group were more likely to be male and to have lower education. Unclear whether this may have influenced results |
APACHE II: Acute Physiology and Chronic Health Evaluation II BMI: body mass index BCOPE: Brief Coping Orientations to Problems Experienced tool BSRS: Brief Symptom Rating Scale CCFNI: Critical Care Family Needs Inventory CI: confidence interval CINT: questionnaire for surgical ICU patients used in Fleischer 2014 FIL: family information leaflet FS‐ICU 24: Family Satisfaction in the Intensive Care Unit 24‐item survey GAD‐7: Generalized Anxiety Disorder 7‐item scale HADS: Hospital Anxiety and Depression Scale HADS‐A: Hospital Anxiety and Depression Scale ‐ anxiety subscale HADS‐D: Hospital Anxiety and Depression Scale ‐ depression subscale HRQoL: health‐related quality of life IES‐R: Impact of Event Scale‐Revised ICU: intensive care unit MCS: mental health component summary (of SF‐12) M/F: male/female NIHR: National Institute for Health Research NINR: National Institute of Nursing Research PCS: physical health component summary (of SF‐12) PEI: Patient Enablement Instrument PHQ‐9: Patient Health Questionnaire‐9 PTSD: post‐traumatic stress disorder RCT: randomised controlled trial REALM‐SF: Rapid Estimate of Adult Literacy in Medicine‐Short Form SAPS II: Simplified Acute Physiology Score II SD: standard deviation SEIQoL: Schedule for Evaluation of Individual Quality of Life SF‐12: 12‐item Short Form Health Survey SOFA: Sequential Organ Failure Assessment STAI: State‐Trait Anxiety Inventory UCCDIP: User Centred Critical Care Discharge Information Pack VAS‐A: visual analogue scale ‐ anxiety Y/N: yes/no
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barnett 2011 | Described as a quasi‐experimental cohort treatment reversal study. Information given to visitors of ICU patients regarding visitor orientation, visitor engagement, and general patient health information. |
| Berg 2006 | RCT. Participants scheduled for elective surgery given educational information about ICU stay on the day before surgery. |
| Chien 2006 | Pre‐ and post‐test study design. Family members received an individual education programme. |
| Daly 2010 | Pre‐ and post‐test study design. Family meetings were organised on a weekly basis to discuss prognosis and treatment options with ICU physicians and nurses versus family meetings organised if ICU physicians thought they were needed. |
| Garrouste‐Orgeas 2010 | Prospective study; abstract does not contain information about randomisation. Intervention involves caregivers and family members completing a diary during patient ICU stay. Diary is not equivalent to provision of information during ICU stay. |
| Guo 2012 | RCT. Participants scheduled for cardiac surgery given preoperative education intervention including information about ICU stay. |
| Jones 2003 | RCT. Intervention is given after the ICU stay. |
| Jones 2009 | RCT. Intervention involves completion of a diary with photographs as a memory tool, with the aim of reducing PTSD. Diary is not equivalent to provision of information during ICU stay. |
| Kirchhoff 2008 | RCT. Information related to preparation for withdrawal of life‐support |
| Lai 2016 | RCT. Participants scheduled for cardiac surgery were given educational package including video information, discussion, and tour of ICU on the day before surgery. Study is ongoing. |
| Lautrette 2007 | RCT. Information for family members related to bereavement management. |
| Lynn‐McHale 1997 | Pre‐ and post‐test study design. Elective surgical patients and family members given tour of ICU prior to surgery. |
| Medland 1998 | Pre‐ and post‐test study design. Structured communication with family members including discussion with nurse, information pamphlet, and daily telephone call from nurse |
| Mistraletti 2017 | Before‐and‐after study design. Family members given brochure and access to a website. Related to understanding of ICU environment, and anticipated emotional needs |
| Mitchell 2004 | Pre‐ and post‐test study design. Information given to family members relating to transfer from the ICU to the general ward. |
| Othman 2016 | Pre‐ and post‐test quasi‐experimental study design. Family members given information booklet related to the ICU. |
| Shin 2017 | Quasi‐experimental design. Information given to cardiac surgical patients prior to ICU admission. |
| Walsh 2012 | RCT. Provision of intervention after discharge from the ICU and during acute ward stay |
| Weibel 2016 | RCT. Patients in the coronary care unit ‐ not described as an ICU setting. Information related to management of specific cardiac patient health needs and disease management. |
| White 2012 | Not an RCT. Information given as part of a support programme for family members. Not related to transition from ICU |
| Wilson 2015 | RCT. Information was specifically related to teaching carer participants how to give CPR to the patient, rather than general information relating to prognosis, treatment, and transition from the ICU. |
CPR: cardiopulmonary resuscitation; ICU: intensive care unit; PTSD: post‐traumatic stress disorder; RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Herlihy 2014.
| Methods | RCT |
| Participants |
Total number of randomised participants: 246 (spokespersons for families of ICU patients) Setting: ICU (medical and surgical) |
| Interventions |
Intervention group Details: spokesperson for carers given an iPad app. App provided disease and care information for surrogates. Control group Details: participant given usual ICU care. |
| Outcomes | Satisfaction (measured using FS‐ICU 24 questionnaire) at end of participant's ICU stay |
| Notes | Published as an abstract. Insufficient information to include in this review; does not include number of participants by group, and data are not clearly reported. |
IRCT201111148100N1.
| Methods | RCT |
| Participants |
Total number of randomised participants: 64 Inclusion criteria: carer between 18 to 80 years of age, responsible for patient's care, able to read and understand Persian language, have no previous experience of caring for a patient undergoing open heart surgery, not being a professional person, the patient's surgery is elective Exclusion criteria: occurrence of any postoperative complications such as bleeding and reoperation; the patient is not able to be extubated in the first 24 hours after surgery; or patient or family member cannot participate in all educational sessions Country: Iran Setting: ICU Amir‐almomenin Hospital (surgical) |
| Interventions |
Intervention group Details: 1 day before surgery participant and carer given half‐hour ICU orientation tour, information about open heart surgery unit, and opportunity to discuss concerns and ask questions. Immediately after surgery participant and carer given an educational pamphlet including information about participant's clinical condition, treatment, and care. On second and third days, 30‐minute educational sessions held for patient participant and carer. Information included participant's clinical condition, ICU care, home care needs, diet and medications, wound care and infection prevention, referral time for follow‐up, and removing the sutures and postoperative activities. Participant and carer given additional opportunity to ask questions. Control group Details: no intervention in control group. Participants will not receive any structured and planned education. They will receive information about the rules, phone access, and visit hours just according to the hospital routine, as well as a brief verbal description of the participant's condition. |
| Outcomes | Anxiety (measured using Spielberger anxiety questionnaire) before and after intervention; satisfaction (using researcher‐designed questionnaire) postintervention |
| Notes | Funding/declarations of interest: funded by Tehran University of Medical Sciences Clinical trials registration documents state that this study is completed. We are awaiting publication of full report with results. |
IRCT2014102819728N1.
| Methods | RCT |
| Participants |
Inclusion criteria: carer 18 to 60 years of age, responsible for patient care, able to understand Persian language, not suffering from mental illness, patient undergoing open heart surgery Exclusion criteria: carer refuses to participate in the study; patient has postoperative complications such as bleeding, loss of consciousness, death, etc. Country: Iran Setting: ICU Amir‐almomenin Hospital (surgical) |
| Interventions |
Intervention group Details: carers given 3 face‐to‐face sessions of nursing consultation. Sessions lasted between half an hour and 1 hour depending on the carer's needs. Information included: preparation prior to surgery; explanation of different aspects of disease and treatment, including surgery, ICU, and cardiac surgery; treatment plan for hospitalisation; care plan for after discharge; and emotional support to families with opportunity to express feelings and ask questions. Control group Details: carer given routine care and information. |
| Outcomes | Anxiety (measured using STAI) before and after intervention; satisfaction (measured using unspecified questionnaire) after intervention |
| Notes | Funding/declarations of interest: sponsored by Social Welfare and Rehabilitation University Clinical trials register states that this study is completed. We are awaiting publication of full report with results. |
McCarthy 2017.
| Methods | RCT |
| Participants | Inclusion criteria: diary candidates (identified using CAM‐ICU screening tool) with need for mechanical ventilation > 14 hours |
| Interventions |
Intervention group Details: participant given ICU diary and PICS educational pamphlet and video in a 20‐bed multiservice ICU for 10 months. Video was made by staff and available 24/7. Programme champions on acute care units assist with maintaining the diary and ensuring that it accompanies patients upon discharge. |
| Outcomes | Not clearly reported in abstract |
| Notes | Conference abstract with limited information. We are awaiting publication of full report with results to assess eligibility. |
NCT01147978.
| Methods | RCT |
| Participants |
Target number of randomised participants: 303 Inclusion criteria: patients > 18 years of age, alive at the end of ICU stay, with > 48 hours of mechanical ventilation, consenting to be called back 3 months and 1 year after ICU discharge Exclusion criteria: patients with chronic cognitive deterioration before ICU admission, inclusion in another interventional randomised study, non French‐speaking, unable to give consent, end‐of‐life situation (survival at 3 months very improbable), deaf Country: France Setting: ICU (medical) |
| Interventions |
Intervention group Details: patient participant and carer participant given conference by the intensivist at end of ICU stay. Information included details on progress of ICU stay, orientation after discharge, and the possibility of consulting a general practitioner. Control group Details: participants given standard care without end‐of‐stay conference. |
| Outcomes | Anxiety and depression (measured using HADS and IES‐R). Patient participants and carer participants interviewed by phone 3 months and 1 year after ICU discharge. |
| Notes | Funding/declarations of interest: sponsored by Assistance Publique, University Paris 7, Institut National de la Santé et de la Recherche Médicale Study start date: April 2009 Clinical trials register states that this study is completed. We are awaiting publication of full report with results. |
NCT02067559.
| Methods | RCT |
| Participants |
Target number of randomised participants: 59 Inclusion criteria: patients > 17 years of age, enrolment < 72 hours of ICU admission, time of ICU stay predicted to be > 72 hours by ICU treatment team, mechanical ventilation required for > 24 hours, can understand verbal and written English Exclusion criteria: no carer available, terminal illness with life expectancy of < 6 months, pre‐existing cognitive impairment, mechanical ventilation for < 24 hours, reason for ICU admission is suicide attempt or overdose Country: Canada Setting: ICU |
| Interventions |
Intervention groups ICU diaries Details: patient participant given a bound empty journal to be stored at the bedside. All carers and ICU staff invited to write in ICU diary at any time. Procedure for diary writing followed previous research. Psycho‐education Details: patient participant given psycho‐education brochure. Brochure described procedures in ICU such as sedation and ventilation, and the delirium, hallucinations, and trauma that may result; as well as symptoms of PTSD post‐ICU. It provided instructions for follow‐up, information, and emergency care. Brochure instructed patient participants to contact their follow‐up healthcare provider if they had any questions. ICU diary plus psycho‐education Details: patient participant given both interventions. Control group Details: patient participant given usual treatment. |
| Outcomes |
|
| Notes | Study start date: March 2014 Clinical trials register states that this study is completed. We are awaiting publication of full report with results. |
NCT02415634.
| Methods | RCT |
| Participants |
Target number of randomised participants: 20 Inclusion criteria: patients ≥ 18 years of age, admitted to ICU > 4 days, indication for physiotherapy referral in the ICU, indication for follow‐up physiotherapy on ICU discharge, RASS score 0 at time of consent Exclusion criteria: ICU length of stay > 14 days, patients allocated a multidisciplinary team in advance of a planned ICU admission (e.g. liver transplant), pregnant mothers, palliation, expected discharge to another hospital, unable to understand English, patients who have direct access to condition‐specific multidisciplinary team follow‐up (e.g. stroke, neurology), psychiatric disease, unstable cardiac disease, where physiotherapy treatment is limited or maximal functional capacity is capped for duration of study (e.g. non‐weight‐bearing status due to orthopaedic limitation x 12 weeks), patients who are unable to give consent Country: Ireland Setting: ICU |
| Interventions |
Intervention group Details: patient participant given usual care plus information pack at ICU discharge called the RECAP. RECAP includes: critical care discharge summary (UCCDIP), rehabilitation goal‐setting care plan, patient communication forum, useful supports and contact information, and tailored exercise programme. Patient participant given a consultation with ICU physiotherapist before ICU discharge and once weekly thereafter for 3 weeks. Consultation used to discuss goal attainment and associated challenges. Intensive care unit therapist met once weekly with patient participant's primary physiotherapist to provide clinical support if necessary in determining the patient participant's needs post‐critical care. Control group Details: patient participant given standard physiotherapy intervention after ICU discharge. |
| Outcomes |
|
| Notes | Study start date: November 2014 Clinical trials register states that this study is completed. We are awaiting publication of full report with results. |
CAM‐ICU: Confusion Assessment Method for the Intensive Care Unit CINT: questionnaire for surgical ICU patients used in Fleischer 2014 CPAx: Chelsea Critical Care Physical Assessment Tool FIM: Functional Independence Measure FS‐ICU 24: Family Satisfaction in the Intensive Care Unit 24‐item survey HADS: Hospital Anxiety and Depression Scale ICU: intensive care unit ICUMT: ICU Memory Tool IES‐R: Impact of Event Scale‐Revised PICS: post‐intensive care unit syndrome PTSD: post‐traumatic stress disorder RASS: Richmond Agitation‐Sedation Scale RCT: randomised controlled trial RECAP: REhabilitation after Critical illness Assisted discharge Pack SAI: State Anxiety Inventory SF‐12: 12‐item Short Form Health Survey STAI: State‐Trait Anxiety Inventory UCCDIP: User Centred Critical Care Discharge Information Pack
Characteristics of ongoing studies [ordered by study ID]
NCT01982877.
| Trial name or title | The Four Supports Study: family support intervention in intensive care units |
| Methods | RCT |
| Participants |
Target number of randomised participants: 300 Inclusion criteria: patients ≥ 21 years of age, unable to make treatment decisions, have either an APACHE II score of ≥ 22 or, for patients with a primary neurologic diagnosis (e.g. intracranial haemorrhage, subdural haemorrhage, or subarachnoid haemorrhage), physician estimates the patient has at least a 40% risk of long‐term severe functional impairment or 40% risk of in‐hospital mortality Exclusion criteria: patients who do not have carers, do not have ≥ 1 family member who is willing to participate in the study, are awaiting organ transplantation Country: Pennsylvania, USA |
| Interventions |
Intervention group Details: carer participant given The Four Supports Intervention, which is a multifaceted intervention involving the addition of a trained nurse/social worker interventionist to the care team who delivers 4 kinds of support: emotional support, communication support, decision support, and anticipatory grief support. Carer participant also given usual care plus the control (as below). Control group Details: carer participant given usual care plus 2 × 15‐minute education sessions about critical illness and mechanical ventilation. Given on days 2 and 5 and delivered by a research staff co‐ordinator with education in critical care nursing |
| Outcomes | For carer participants: anxiety and depression (measured using HADS) and the impact of events (measured using IES), assessed 6 months after patient participant's death or discharge from hospital For patient participants: centredness of care (measured using PCC) |
| Starting date | January 2014 |
| Contact information | Douglas White, MD, University of Pittsburgh, whitedb@upmc.edu |
| Notes |
NCT02445937.
| Trial name or title | PARTNER II: improving patient and family centered care in advanced critical illness |
| Methods | RCT |
| Participants |
Target number of randomised participants: 690 patients and 690 surrogates Inclusion criteria: patients ≥ 18 years of age, carer decision‐maker for ICU patient in 1 of 5 UPMC ICUs Exclusion criteria: non‐English speaking, awaiting organ transplantation, not physically able to participate in family meeting Country: Pennsylvania, USA |
| Interventions |
Intervention group Details: participants are given the PARTNER intervention, which is a multifaceted intervention delivered by a trained "PARTNER Champion" who has undergone 16 hours of intense communication training, with audit and feedback, quarterly booster training, and expert implementation support. Additionally, there is academic detailing of ICU physicians and ICU bedside nurses to augment the intervention. The PARTNER intervention deploys 3 strategies to improve: the timeliness and frequency of clinician‐family communication; the emotional and decision support provided to families; and the appropriate involvement of palliative care specialists. Control group Details: participants are given ICU Family Communication intervention delivered by key nurse/social workers within the ICU. The nurse/social worker interventionist will have received 4 hours of training designed to aid in clinician‐family communication. The nurse/social worker will touch base with families daily, attend to emotion, and facilitate a clinician‐family meeting on or before day 4 of ICU admission with at least the physician and family and nurse/social worker who acts as their advocate. |
| Outcomes |
|
| Starting date | June 2015 |
| Contact information | Douglas B White, MD, University of Pittsburgh, whitedb@upmc.edu |
| Notes |
NCT02931851.
| Trial name or title | Family information management in the intensive care unit (ICU‐families) |
| Methods | RCT |
| Participants |
Target number of randomised participants: 110 Inclusion criteria: ICU patients ≥ 18 years of age, anticipated further ICU stay ≥ 3 days Exclusion criteria: lack of basic IT user knowledge, no basic German language skills, DNR order Country: Austria and Switzerland |
| Interventions |
Intervention group Details: carer given access to professionally developed website for relatives of ICU patients. Control group Details: carer given standard online information. |
| Outcomes |
|
| Starting date | August 2017 |
| Contact information | Magdalena Hoffmann, MA, magdalena.hoffmann@medunigraz.at |
| Notes |
APACHE II: Acute Physiology and Chronic Health Evaluation II DNR: do not resuscitate FS‐ICU 24: Family Satisfaction in the Intensive Care Unit 24‐item survey HADS: Hospital Anxiety and Depression Scale ICU: intensive care unit IES: Impact of Event Scale IT: information technology PARTNER: PAiring Re‐engineered ICU Teams with Nurse‐driven Education and OutReach PCC: Patient Centeredness of Care Scale PPPC: Patient‐Perceived Patient‐Centeredness of Care Scale PTSD: post‐traumatic stress disorder QOC: quality of communication RCT: randomised controlled trial UPMC: University of Pittsburgh Medical Center
Differences between protocol and review
Types of interventions
We edited this section to clarify exclusion of studies in which the intervention was given before the ICU stay (i.e. before critical illness) and after the ICU stay (i.e. to a survivor of critical illness). This was a clarification, because in the Types of participants section (and title of the review), we specified inclusion of patients who were in the ICU.
Types of interventions
We excluded studies that assessed the effectiveness of patient diaries because patient diaries provided retrospective information to the patient about what they had experienced during their stay. This review considered provision of information aiming to increase a patient or carer's knowledge about what they are currently experiencing (rather than what they have experienced), and what they should expect whilst they are in the ICU and as they transition from the ICU. This specific patient diary intervention is considered in another Cochrane Review (Ullman 2014). We excluded studies that provided information or education about managing end‐of‐life care, which are complicated by aspects of grief, bereavement, counselling, and after‐death management.
Types of outcome measures
We divided the outcome "severity of distress or anxiety or depression in carers" into "severity of depression" and "severity of anxiety". We added adverse effects to our reported outcomes.
Searches
We did not conduct database searches in ISI Web of Science and LILACS (Latin American and Caribbean Literature in Health Sciences) (BIREME). We included a grey literature search.
Data extraction and management
We extracted additional information regarding characteristics of carer participants, because outcomes related to carer participants, and it was important to assess whether there were differences between carer participant groups.
Data synthesis
We conducted a narrative synthesis of the results. We organised these results by comparison and outcome. We did not organise the results by type of intervention (verbal, written, digital) as described in the protocol. We calculated mean differences for single‐study data using the Review Manager 5 calculator (Review Manager 2014), and incorporated this information with a narrative summary of individual study data.
Sensitivity analysis
We did not conduct sensitivity analysis because we did not pool data. Planned sensitivity analyses were as follows: unpublished data (i.e. no peer‐reviewed full‐text paper available); trials with inadequate or unclear methods of random sequence generation or allocation concealment (i.e. high risk or unclear risk of selection bias); studies with missing data (e.g. to examine the effect of imputed data or data based on assumptions); treatment effect: random‐effects model versus fixed‐effect model; and dichotomous outcomes: Mantel‐Haenszel odds ratio versus Peto odds ratio.
'Summary of findings' tables
We added an additional outcome to the review (adverse effects), and considered this to be an important outcome to include in the 'Summary of findings' tables. We replaced length of ICU stay with adverse effects in the 'Summary of findings' tables.
Contributions of authors
David Evans (guarantor) drafted the protocol with critical input from Sharon Lewis, Andrew Smith, and Phil Alderson. Sharon Lewis led the review process (selecting studies, data extraction and management, writing the review) with input from Michael Pritchard (data extraction and management, writing the review), Oliver Schofield‐Robinson (selecting studies, data extraction and management), David Evans (selecting studies, providing advice on selection of studies, checking the final draft of the review), Phil Alderson (providing advice on selection of studies, checking the final draft of the review), and Andrew Smith (providing advice on selection of studies, checking the final draft of the review, guarantor for the review).
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research, UK.
This project was supported by the National Institute for Health Research (NIHR), via a Cochrane Programme Grant to the Anaesthesia, Critical and Emergency Care Group. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS), or the Department of Health, UK.
Declarations of interest
Sharon R Lewis: is funded by the National Institute for Health Research (NIHR) Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
Michael W Pritchard: is funded by the NIHR Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
Oliver Schofield‐Robinson: is funded by the NIHR Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
David JW Evans: was previously funded (at the time that development of the protocol was initiated) by the NIHR Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
Phil Alderson: My work on this review is funded, in part, by the NIHR Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
Andrew F Smith: My work on this review is funded, in part, by the NIHR Cochrane Collaboration Programme Grant 13/89/16 ‐ 'Back to normal': speed and quality of recovery after surgery, major injury, and critical care.
New
References
References to studies included in this review
Azoulay 2002 {published data only}
- Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. American Journal of Respiratory and Critical Care Medicine 2002;165(4):438‐42. [PUBMED: 11850333] [DOI] [PubMed] [Google Scholar]
Bench 2015 {published data only}
- Bench S, Day T, Heelas K, Hopkins P, White C, Griffiths P. Evaluating the feasibility and effectiveness of a critical care discharge information pack for patients and their families: a pilot cluster randomised controlled trial. BMJ Open 2015;5(11):e006852. [PUBMED: 26614615] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bench S, Griffiths P, Hopkins P, Day T, Milligan P, Yardley L, et al. Enhancing early critical illness recovery through the use of a 'user centred critical care discharge information pack'. Intensive Care Medicine 2012;38(Suppl):S231. [DOI: 10.1007/s00134-012-2683-0] [DOI] [Google Scholar]
- Bench SD, Day TL, Griffiths P. Developing user centred critical care discharge information to support early critical illness rehabilitation using the Medical Research Council's complex interventions framework. Intensive and Critical Care Nursing 2012;28(2):123‐31. [PUBMED: 22386848] [DOI] [PubMed] [Google Scholar]
Carson 2016 {published data only}
- Carson SS, Cox CE, Wallenstein S, Hanson LC, Danis M, Tulsky JA, et al. Effect of palliative care‐led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA 2016;316(1):51‐62. [PUBMED: 27380343] [DOI] [PMC free article] [PubMed] [Google Scholar]
Curtis 2016 {published data only}
- Curtis JR, Ciechanowski PS, Downey L, Gold J, Nielsen EL, Shannon SE, et al. Development and evaluation of an interprofessional communication intervention to improve family outcomes in the ICU. Contemporary Clinical Trials 2012;33(6):1245‐54. [PUBMED: 22772089] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis JR, Treece PD, Nielsen EL, Gold J, Ciechanowski PS, Shannon SE, et al. Randomized trial of communication facilitators to reduce family distress and intensity of end‐of‐life care. American Journal of Respiratory and Critical Care Medicine 2016;193(2):154‐62. [PUBMED: 26378963] [DOI] [PMC free article] [PubMed] [Google Scholar]
Demircelik 2016 {published data only}
- Demircelik MB, Cakmak M, Nazli Y, Şentepe E, Yigit D, Keklik M, et al. Effects of multimedia nursing education on disease‐related depression and anxiety in patients staying in a coronary intensive care unit. Applied Nursing Research 2016;29:5‐8. [PUBMED: 26856480] [DOI] [PubMed] [Google Scholar]
- Demircelik MB, Yigit D, Şentepe E, Keklik M, Cetin M, Cetin Z, et al. The effectiveness of multimedia nursing education on reducing illness‐related anxiety and depression in coronary care unit's patients. Journal of the American College of Cardiology 2013;2:C50. [DOI: 10.1016/j.jacc.2013.08.145] [DOI] [Google Scholar]
Fleischer 2014 {published data only}
- Fleischer S, Berg A, Behrens J, Kuss O, Becker R, Horbach A, et al. Does an additional structured information program during the intensive care unit stay reduce anxiety in ICU patients?: a multicenter randomized controlled trial. BMC Anesthesiology 2014;14(1):48. [PUBMED: 25071414] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischer S, Berg A, Neubert TR, Koller M, Behrens J, Becker R, et al. Structured information during the ICU stay to reduce anxiety: study protocol of a multicenter randomized controlled trial. Trials 2009;10:84. [DOI: 10.1186/1745-6215-10-84; PUBMED: 19751500] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hwang 1998 {published data only}
- Hwang SL, Chang Y, Ko WJ, Lee MB. Stress‐reducing effect of physician's tape‐recorded support on cardiac surgical patients in the intensive care unit. Journal of the Formosan Medical Association 1998;97(3):191‐6. [PUBMED: 9549270] [PubMed] [Google Scholar]
Torke 2016 {published data only}
- Torke AM, Wocial LD, Johns SA, Callahan CM, Sachs GA, Perkins SM, et al. The family navigator: pilot study of a new role to support family communication in the ICU. Journal of General Internal Medicine 2015;30:S272. [Google Scholar]
- Torke AM, Wocial LD, Johns SA, Sachs GA, Callahan CM, Bosslet GT, et al. The family navigator: a pilot intervention to support intensive care unit family surrogates. American Journal of Critical Care 2016;25(6):498‐507. [PUBMED: 27802950] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Barnett 2011 {published data only}
- Barnett B, Henderson M, Hochhalter A, Spradley C. Impact of videos in the intensive care unit: a novel approach to communication. Chest 2011;140:333A. [DOI: 10.1378/chest.1119235] [DOI] [Google Scholar]
Berg 2006 {published data only}
- Berg A, Fleischer S, Koller M, Neubert TR. Preoperative information for ICU patients to reduce anxiety during and after the ICU‐stay: protocol of a randomized controlled trial [NCT00151554]. BMC Nursing 2006;5:4. [PUBMED: 16524468] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chien 2006 {published data only}
- Chien WT, Chiu YL, Lam LW, Ip WY. Effects of a needs‐based education programme for family carers with a relative in an intensive care unit: a quasi‐experimental study. International Journal of Nursing Studies 2006;43(1):39‐50. [PUBMED: 16183062] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu YL, Chien WT, Lam LW. Effectiveness of a needs‐based education programme for families with a critically ill relative in an intensive care unit. Journal of Clinical Nursing 2004;13(5):655‐6. [PUBMED: 15189419] [DOI] [PubMed] [Google Scholar]
Daly 2010 {published data only}
- Daly BJ, Douglas SL, O'Toole E, Gordon NH, Hejal R, Peerless J, et al. Effectiveness trial of an intensive communication structure for families of long‐stay ICU patients. Chest 2010; Vol. 138, issue 6:1340‐8. [DOI] [PMC free article] [PubMed]
Garrouste‐Orgeas 2010 {published data only}
- Garrouste‐Orgeas M, Coquet I, Perier A, Timsit JF, Pochard F, Philippart F, et al. Impact of an ICU diary on family and patient's psychological symptoms after an ICU stay. Intensive Care Medicine 2010;36(Suppl):S154. [DOI: 10.1007/s00134-010-1999-x] [DOI] [Google Scholar]
Guo 2012 {published data only}
Jones 2003 {published data only}
- Jones C, Skirrow P, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, et al. Rehabilitation after critical illness: a randomized controlled trial. Critical Care Medicine 2003;31(10):2456‐61. [PUBMED: 14530751] [DOI] [PubMed] [Google Scholar]
Jones 2009 {published data only}
- Jones C, Backman C, Capuzo M, Egerod I, Flaatten H, Granja C, et al. ICU diaries reduce posttraumatic stress disorder after critical illness: a randomised controlled trial. Intensive Care Medicine 2009;35(Suppl):S115. [Google Scholar]
Kirchhoff 2008 {published data only}
- Kirchhoff KT, Palzkill J, Kowalkowski J, Mork A, Gretarsdottir E. Preparing families of intensive care patients for withdrawal of life support: a pilot study. American Journal of Critical Care 2008;17(2):113‐21. [PUBMED: 18310647] [PubMed] [Google Scholar]
Lai 2016 {published data only}
- Lai VK, Lee A, Leung P, Chiu CH, Ho KM, Gomersall CD, et al. Patient and family satisfaction levels in the intensive care unit after elective cardiac surgery: study protocol for a randomised controlled trial of a preoperative patient education intervention. BMJ Open 2016;6(6):e011341. [PUBMED: 27334883] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai VKW, Lee A, Leung P, Chiu CH, Ho KM, Gomersall CD, et al. Patient and family satisfaction levels in the intensive care unit after elective cardiac surgery. Anesthesia and Analgesia 2016;123(3 Suppl 2):143. [DOI: 10.1213/01.ane.0000492516.58705.24] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lautrette 2007 {published data only}
- Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. New England Journal of Medicine 2007;356(5):469‐78. [PUBMED: 17267907] [DOI] [PubMed] [Google Scholar]
Lynn‐McHale 1997 {published data only}
- Lynn‐McHale D, Corsetti A, Brady‐Avis E, Shaffer R, McGrory J, Rothenberger C. Preoperative ICU tours: are they helpful?. American Journal of Critical Care 1997;6(2):106‐15. [PUBMED: 9172847] [PubMed] [Google Scholar]
Medland 1998 {published data only}
- Medland JJ, Ferrans CE. Effectiveness of a structured communication program for family members of patients in an ICU. American Journal of Critical Care 1998;7(1):24‐9. [PUBMED: 9429680] [PubMed] [Google Scholar]
Mistraletti 2017 {published data only}
- Mistraletti G, Umbrello M, Mantovani ES, Moroni B, Formenti P, Spanu P, et al. A family information brochure and dedicated website to improve the ICU experience for patients' relatives: an Italian multicenter before‐and‐after study. Intensive Care Medicine 2017;43(1):69‐79. [PUBMED: 27830281] [DOI] [PubMed] [Google Scholar]
Mitchell 2004 {published data only}
- Mitchell ML, Courtney M. Reducing family members' anxiety and uncertainty in illness around transfer from intensive care: an intervention study. Intensive and Critical Care Nursing 2004;20(4):223‐31. [PUBMED: 15288876] [DOI] [PubMed] [Google Scholar]
Othman 2016 {published data only}
- Othman H, Subramanian P, Ali NAM, Hassan H, Haque M. The effect of information booklets on family members' satisfaction with decision making in an intensive care unit of Malaysia. Journal of Young Pharmacists 2016;8(2):128‐32. [DOI: 10.5530/jyp.2016.2.13] [DOI] [Google Scholar]
Shin 2017 {published data only}
- Shin KM, Choi HR. Effects of prior information about intensive care unit environment on anxiety and environmental stress in patients undergoing open heart surgery. Journal of Korean Academic Society of Nursing Education 2017;21(1):28‐35. [DOI: 10.5977/jkasne.2015.21.1.28] [DOI] [Google Scholar]
Walsh 2012 {published data only}
- Walsh TS, Salisbury LG, Boyd J, Ramsay P, Merriweather J, Huby G, et al. A randomised controlled trial evaluating a rehabilitation complex intervention for patients following intensive care discharge: the RECOVER study. BMJ Open 2012;2(4):e001475. [PUBMED: 22761291] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weibel 2016 {published data only}
- Weibel L, Massarotto P, Hediger H, Mahrer‐Imhof R. Early education and counselling of patients with acute coronary syndrome: a pilot study for a randomized controlled trial. European Journal of Cardiovascular Nursing 2016;15(4):213‐22. [PUBMED: 25341680] [DOI] [PubMed] [Google Scholar]
White 2012 {published data only}
- White DB, Cua SM, Walk R, Pollice L, Weissfeld L, Hong S, et al. Nurse‐led intervention to improve surrogate decision making for patients with advanced critical illness. American Journal of Critical Care 2012;21(6):396‐409. [PUBMED: 23117903] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2015 {published data only}
- Wilson ME, Akhoundi A, Hinds R, Krupa A, Kashani K. Use of a video to improve patient and surrogate understanding of cardiopulmonary resuscitation and resuscitation preference options in the ICU: a randomized controlled trial. American Journal of Respiratory and Critical Care Medicine 2013;187:A4962. [www.atsjournals.org/doi/abs/10.1164/ajrccm‐conference.2013.187.1_MeetingAbstracts.A4962] [Google Scholar]
- Wilson ME, Krupa A, Hinds RF, Litell JM, Swetz KM, Akhoundi A, et al. A video to improve patient and surrogate understanding of cardiopulmonary resuscitation choices in the ICU: a randomized controlled trial. Critical Care Medicine 2015;43(3):621‐9. [PUBMED: 25479118] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Herlihy 2014 {published data only}
- Herlihy J, Schaefer F, Smith C. Effect of mobile application providing information support on satisfaction of ICU patient families. Critical Care Medicine 2014;42(12):A1505‐6. [DOI: 10.1097/01.ccm.0000458103.59535.90] [DOI] [Google Scholar]
IRCT201111148100N1 {published data only}
- IRCT201111148100N1. Effectiveness of family centered informational support on anxiety and satisfaction of patients undergoing open heart surgery and their families. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT201111148100N1 (first received 5 June 2012).
IRCT2014102819728N1 {published data only}
- IRCT2014102819728N1. Nursing counseling on anxiety and satisfaction [The effect of nursing consultation on patient's family anxiety and satisfaction at the cardiac surgical intensive care unit]. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2014102819728N1 (first received 22 June 2014).
McCarthy 2017 {published data only}
- McCarthy M, Mount C, Eccleston S. Improving the post‐intensive care syndrome patient experience with an ICU diary program. Critical Care Medicine 2017;44(12 Suppl 1):283. [DOI: 10.1097/01.ccm.0000509503.57228.ab] [DOI] [Google Scholar]
NCT01147978 {published data only}
- NCT01147978. Proactive communication strategy in intensive care unit and post traumatic stress symptoms (FAMIREAXV) [Impact of a proactive strategy of communication with patients hospitalized in ICU and their families with the aim of reducing their anxious and depressive symptoms and their post traumatic stress symptoms]. clinicaltrials.gov/ct2/show/NCT01147978 (first received 18 June 2010).
NCT02067559 {published data only}
- NCT02067559. Preventing post‐traumatic stress in ICU survivors: a pilot randomized controlled trial of ICU diaries. clinicaltrials.gov/ct2/show/NCT02067559 (first received 18 February 2014).
NCT02415634 {published data only}
- NCT02415634. Rehabilitation after critical illness assisted discharge pack (RECAP) [Investigation of physiotherapy led ICU discharge facilitation using the rehabilitation after critical illness assisted discharge pack (RECAP) model; a pilot randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT02415634 (first received 6 April 2015).
References to ongoing studies
NCT01982877 {published data only}
- NCT01982877. The four supports study: family support intervention in intensive care units [A trial to improve surrogate decision‐making for critically ill older adults]. clinicaltrials.gov/ct2/show/NCT01982877 (first received 30 October 2013).
NCT02445937 {published data only}
- NCT02445937. PARTNER II: improving patient and family centered care in advanced critical illness [Stepped wedge trial of an intervention to support proxy decision makers in ICUs]. clinicaltrials.gov/ct2/show/NCT02445937 (first received 13 May 2015).
NCT02931851 {published data only}
- NCT02931851. Family information management in the intensive care unit (ICU‐families) [Family information management in the intensive care unit: a randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT02931851 (first received 11 October 2016).
Additional references
CCCG 2013
- Cochrane Consumers and Communication Group. Standard protocol text and additional guidance for review authors. cccrg.cochrane.org (accessed prior to 21 August 2018).
Chadwick 2016
- Chadwick AE, Zoccola PM, Figueroa WS, Rabideau EM. Communication and stress: effects of hope evocation and rumination messages on heart rate, anxiety, and emotions after a stressor. Health Communication 2016;31(12):1‐13. [DOI] [PubMed] [Google Scholar]
Chan 2011
- Chan RJ, Webster J, Marquart L. Information interventions for orienting patients and their carers to cancer care facilities. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD008273.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation. Covidence. Version accessed prior to 21 August 2018. Melbourne, Australia: Veritas Health Innovation.
Davidson 2007
- Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient‐centered intensive care unit: American College of Critical Care Medicine Task Force 2004‐2005. Critical Care Medicine 2007;35(2):605‐22. [PUBMED: 17205007] [DOI] [PubMed] [Google Scholar]
Davidson 2017
- Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family‐centered care in the neonatal, pediatric, and adult ICU. Critical Care Medicine 2017;45(1):103‐28. [PUBMED: 27984278] [DOI] [PubMed] [Google Scholar]
Davydow 2009
- Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Medicine 2009;35(5):796‐809. [DOI] [PMC free article] [PubMed] [Google Scholar]
Douglas 2005
- Douglas SL, Daly BJ, Kelley CG, O'Toole E, Montenegro H. Impact of a disease management program upon caregivers of chronically critically ill patients. Chest 2005;128(6):3925‐36. [DOI] [PubMed] [Google Scholar]
Eddleston 2000
- Eddleston JM, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Critical Care Medicine 2000;28(7):2293‐9. [DOI] [PubMed] [Google Scholar]
Floyd 2008
- Floyd K, Riforgiate S. Affectionate communication received from spouses predicts stress hormone levels in healthy adults. Communication Monographs 2008;75(4):351‐68. [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed prior to 21 August 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Haines 2015
- Haines KJ, Denehy L, Skinner EH, Warrillow S, Berney S. Psychosocial outcomes in informal caregivers of the critically ill: a systematic review. Critical Care Medicine 2015;43(5):1112‐20. [DOI] [PubMed] [Google Scholar]
Herbert 1993
- Herbert TB, Cohen S. Stress and immunity in humans: a meta‐analytic review. Psychosomatic Medicine 1993;55(4):364‐79. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JP, White IR, Wood AM. Imputation methods for missing outcome data in meta‐analysis of clinical trials. Clinical Trials 2008;5(3):225‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hofhuis 2008
- Hofhuis JG, Spronk PE, Stel HF, Schrijvers AJ, Rommes JH, Bakker J. Experiences of critically ill patients in the ICU. Intensive and Critical Care Nursing 2008;24(5):300‐13. [DOI] [PubMed] [Google Scholar]
Hofhuis 2009
- Hofhuis JG, Stel HF, Schrijvers AJ, Rommes JH, Bakker J, Spronk PE. Health‐related quality of life in critically ill patients: how to score and what is the clinical impact?. Current Opinion in Critical Care 2009;15(5):425‐30. [PUBMED: 19623059] [DOI] [PubMed] [Google Scholar]
Joint Commission 2007
- The Joint Commission. What did the doctor say?: Improving health literacy to protect patient safety. www.jointcommission.org/assets/1/18/improving_health_literacy.pdf. Oakbrook Terrace, IL, (accessed 15 June 2016).
Kaufman 2018
- Kaufman J, Ryan R, Walsh L, Horey D, Leask J, Robinson P, et al. Face‐to‐face interventions for informing or educating parents about early childhood vaccination. Cochrane Database of Systematic Reviews 2018, Issue 5. [DOI: 10.1002/14651858.CD010038.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kross 2015
- Kross E. The importance of caregiver outcomes after critical illness. Critical Care Medicine 2015;43(5):1149‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linton 2008
- Linton S, Grant C, Pellegrini J. Supporting families through discharge from PICU to the ward: the development and evaluation of a discharge information brochure for families. Intensive and Critical Care Nursing 2008;24(6):329‐37. [DOI] [PubMed] [Google Scholar]
Magnus 2006
- Magnus VS, Turkington L. Communication interaction in ICU ‐ patient and staff experiences and perceptions. Intensive and Critical Care Nursing 2006;22(3):167‐80. [DOI] [PubMed] [Google Scholar]
NICE CG50
- National Institute for Health and Care Excellence. Acutely ill patients in hospital. Recognition of and response to acute illness in adults in hospital. Clinical guideline [CG50]. 2007. www.nice.org.uk/guidance/cg50 (accessed 27 January 2016). [PubMed]
Parker 2015
- Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Critical Care Medicine 2015;43(5):1121‐9. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Riley 2006
- Riley JB, Cloonan P, Norton C. Low health literacy: a challenge to critical care. Critical Care Nursing Quarterly 2006;29(2):174‐8. [DOI] [PubMed] [Google Scholar]
Ringdal 2005
- Ringdal M, Plos K, Lundberg D, Johansson L, Bergbom I. Outcome after injury: memories, health‐related quality of life, anxiety, and symptoms of depression after intensive care. Journal of Trauma 2005;66(4):1226‐33. [DOI] [PubMed] [Google Scholar]
Ryan 2013
- Ryan R, Hill S, Prictor M, McKenzie J, Cochrane Consumers and Communication Group. Study quality guide. cccrg.cochrane.org/author‐resources (accessed prior to 21 September 2018).
Scheunemann 2011
- Scheunemann LP, McDevitt M, Carson SS, Hanson LC. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest 2011;139(3):543‐54. [DOI] [PubMed] [Google Scholar]
Schyve 2007
- Schyve PM. Language differences as a barrier to quality and safety in health care: the Joint Commission perspective. Journal of General Internal Medicine 2007;22(Suppl 2):360–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Scragg 2001
- Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesthesia 2001;56(1):9‐14. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta‐analyses of randomised controlled trials. BMJ 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
Thorsteinsson 1999
- Thorsteinsson EB, James JE. A meta‐analysis of the effects of experimental manipulations of social support during laboratory stress. Psychology and Health 1999;14(5):869‐86. [Google Scholar]
Ullman 2014
- Ullman AJ, Aitken LM, Rattray J, Kenardy J, Brocque R, MacGillivray S, et al. Diaries for recovery from critical illness. Cochrane Database of Systematic Reviews 2014, Issue 12. [DOI: 10.1002/14651858.CD010468.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Beusekom 2016
- Beusekom I, Bakhshi‐Raiez F, Keizer NF, Dongelmans DA, Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Critical Care 2016;20:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walburn 2009
- Walburn J, Vedhara K, Hankins M, Rixon L, Weinman J. Psychological stress and wound healing in humans: a systematic review and meta‐analysis. Journal of Psychosomatic Research 2009;67(3):253‐71. [DOI] [PubMed] [Google Scholar]
Wang 2009
- Wang K, Zhang B, Li C, Wang C. Qualitative analysis of patients' intensive care experience during mechanical ventilation. Journal of Clinical Nursing 2009;18(2):183‐90. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Evans 2016
- Evans DW, Lewis SR, Alderson P, Smith AF. Information or education interventions for adult intensive care unit (ICU) patients and their carers. Cochrane Database of Systematic Reviews 2016, Issue 12. [DOI: 10.1002/14651858.CD012471] [DOI] [PMC free article] [PubMed] [Google Scholar]


