Abstract
Workforce shortages pose major obstacles to delivering adequate mental health care and scaling up services to address the global treatment gap. There is mounting evidence demonstrating the clinical effectiveness of having non-specialist health workers, such as community health workers, lay health workers, midwives, or nurses, deliver brief psychosocial treatments for common mental disorders in primary care settings. With rapidly increasing access to and use of digital technology worldwide, there may be new opportunities to leverage these emerging digital technologies to support non-specialist health workers and increase mental health workforce capacity. In this perspectives article, we consider the potential that digital technology holds for supporting non-specialist health workers in delivering evidence-based mental health care. Specifically, from our search of the academic literature, we identified seven promising examples from primary care settings in different low-income and middle-income countries (including India, Pakistan, Zimbabwe, Peru, China, and Nigeria) where digital platforms are being used to support delivery of mental health care from a variety of non-specialist providers by offering training, digital tools for diagnosis, guiding treatment, facilitating supervision, and integrating services. We summarize these examples and discuss future opportunities to use digital technology for supporting the development of a trained, effective, and sustainable mental health workforce. We also consider the potential to leverage these technologies for integrating mental health care into existing health systems in low resource settings.
Keywords: mental health, task-sharing, task-shifting, non-specialist health worker, community health worker, primary care, mHealth, digital technology
Background
Worldwide, mental disorders are a leading cause of disability1, accounting for over 8 million deaths annually2 and an estimated one in every 10 lost years of health.3 Healthcare systems in all countries are overwhelmed by the growing burden of mental disorders and face significant shortfalls in providing even basic mental health services.4 Workforce shortages pose major obstacles to delivering adequate mental health care, with the paucity of mental health providers being most severe in low-income and middle-income countries.3,4 Expanding the capacity and reach of the mental health workforce thus represents an urgent public health priority.
Integrating mental health services into primary care and shifting the provision of evidence-based psychosocial treatments to non-specialist health workers such as community health workers, lay persons, and other frontline health workers has emerged as a highly promising approach.5,6 However, there remain significant challenges with ensuring that non-specialist health workers can acquire the necessary competencies and skills to deliver evidence-based psychosocial treatments for common mental disorders, that these providers can access necessary support and assistance to continue delivering high quality care over time, and that such capacity building efforts can be scaled up and sustained within under-resourced national health systems. With rapidly increasing access to and use of digital technology worldwide, there may be new opportunities to support non-specialist health workers and increase the mental health workforce capacity.
In this perspectives article, we consider the potential to leverage digital technology for supporting non-specialist health workers in delivering evidence-based mental health care in low-income and middle-income countries. Specifically, we review the literature and summarize recent examples using digital platforms. We then discuss future opportunities to use digital technology for supporting the development of a trained, effective, and sustainable mental health workforce. We also reflect on the potential challenges and barriers to the successful evaluation and implementation of these digital programs.
Task-sharing for mental health care
There is widespread consensus that integrating mental health services into primary and community healthcare settings and task-sharing are essential for addressing the global treatment gap.7,8 Task-sharing (also referred to as task-shifting) involves training non-specialists, lay health workers, and other community health providers in the delivery of evidence-based mental health services.9 Non-specialist providers such as community health workers typically do not have any specialized training in mental health interventions.10 Numerous studies support the acceptability and effectiveness of adapting brief psychosocial treatments for delivery by non-specialist health workers in primary care and community-based settings for treatment of common mental disorders in lower income countries.11 A recent review of 27 trials involving delivery of psychosocial treatments for common mental disorders in adults by non-specialist health workers in low-income and middle-income countries demonstrated effectiveness of these interventions as reflected by a pooled effect size of 0.49 (95% confidence interval 0.36–0.62), favoring the interventions compared to control conditions.10 Importantly, several recent large-scale randomized controlled trials have demonstrated the effectiveness of task-sharing mental health care to non-specialist health workers for the treatment of depression in India12, common mental disorders in Zimbabwe13, and psychological distress in conflict-affected regions of Pakistan.14 In this perspectives article, we use the term “non-specialist health worker” to refer to a broad range of health workers without specialized training for delivering mental health care, including community health workers, lay health workers, midwives, nurses, primary care providers, village health workers, auxiliary health staff, and frontline health workers.
Despite successful task-sharing efforts, a key challenge is the need for effective training programs tailored to the culture and context of non-specialist health workers from diverse settings. It is necessary to recruit sufficient personnel to train and supervise these providers.15 Training programs need to be designed to ensure successful uptake of skills and knowledge for detecting and treating a range of mental disorders in different settings. Additionally, non-specialist health workers require ongoing supervision and support to prevent fatigue and worker burnout, and to ensure sustainability and continued delivery of high quality care. Strategies are also needed to extend the reach of the limited number of mental health specialists such as psychiatrists, psychiatric nurses, or psychologists to assist non-specialist health workers by offering treatment advice, routine consultation, and being available to intervene when patients present with severe cases or crises. Unconventional approaches such as peer-delivered services or novel workforce training programs may be critical for overcoming these diverse challenges towards developing a proficient and sustainable mental health workforce. As we highlight in the following section, the widespread access to and use of digital technology across most settings globally may yield new opportunities to achieve this aim.
Opportunities for digital technology to support the mental health workforce
The access to and use of digital technology, ranging from mobile phones to web applications, continues to increase rapidly in most countries worldwide. In this perspectives article, we define digital technology as mobile devices such as cellphones or smartphones, mobile applications, wearable devices and sensors, telepsychiatry applications, and online platforms. By early 2018, it was estimated that there were over 5.1 billion unique mobile users, representing over two thirds of the world’s population, over 3.1 billion social media users, and over 4 billion Internet users.16 While access to digital technology remains lower in rural areas or in highly impoverished settings, a substantial proportion of the global population has gained access to mobile devices, web platforms, smartphones, and other digital applications in recent years, thereby highlighting new opportunities to make evidence-based mental health interventions available to those in need.
Many studies, largely from higher income countries, have demonstrated the acceptability and early effectiveness of digital technologies, such as mobile phones, telepsychiatry applications, online programs or remote sensors, for improving the quality, reach and impact of mental health care.17 Use of digital technologies for mental health is not as common in most lower income countries18, though this has been an important area of increasing interest and growth in recent years.19,20 However, across most lower income settings, there have been few efforts to employ digital technologies for specifically supporting task-sharing and developing the capacity of non-specialist health workers to meet the care needs of individuals living with mental disorders.
Methods
Search strategy
In this perspectives article, we conducted a narrative review of the academic literature, with our search guided by four recent comprehensive reviews. Three of these reviews were on the topic of non-specialist health worker-delivered interventions for common mental disorders, and one review summarized the evidence on the use of digital technology for supporting mental health care in low-income and middle-income countries. Specifically, these prior reviews include: (1) Singla et al.’s (2017) systematic review and meta-analysis of the effectiveness of psychological treatments for common mental disorders delivered by non-specialist health workers10; (2) Barnett et al.’s (2018) systematic review of studies involving community health workers providing or supporting the delivery of psychosocial interventions targeting mental health outcomes21; (3) Kohrt et al.’s (2018) meta review of community interventions and the competencies of community-based providers in low-income and middle-income countries22; and (4) Naslund et al.’s (2017) review of the evidence on the use of mobile, online, and other digital technologies for treatment and prevention of mental disorders in low-income and middle-income countries.19
To begin, we searched the lists of included studies from each of these four reviews. Then, we searched MEDLINE/PubMed and Google Scholar to determine if there were any additional recent studies published since the searches conducted in these reviews. We used a combination of search headings including ‘low-income and middle-income countries’ or ‘global health’, ‘mental health’ or ‘mental disorders’, ‘community health worker’, ‘digital technology’ or ‘mobile technology’. Our goal was to identify studies from low-income and middle-income countries involving the use of digital technology for supporting non-specialist health workers in the delivery of mental health care. We allowed for very broad inclusion criteria, though studies had to describe a program or intervention involving non-specialist health workers including community health workers, primary care providers or other frontline health workers, and the use of digital technology for the treatment or prevention of mental disorders. Therefore, only articles describing an evaluation of an intervention were eligible. This included all study designs as well as papers describing study protocols. Commentaries, editorials, or review articles were excluded.
Synthesis of results
For studies that met our inclusion criteria, we extracted the following information: program name, country, study population and setting, description of the program or intervention, details about how digital technology was used to support non-specialist health workers, and main outcome measures. Furthermore, in the framework proposed by Agarwal and colleagues (2015), the ways in which digital technology can support frontline health workers is conceptualized according to a hierarchical framework along the duration of their professional careers.23 For example, digital technology can initially support training and skill building of non-specialist health workers. This is followed by using digital technology for providing non-specialist health workers with on-the-job support and diverse strategies for enhancing job performance and completing tasks and responsibilities. Lastly, digital technology can potentially be used to promote motivation and job retention through ongoing supervision, remote access to specialists and other health care providers, and opportunities for continuing education. In this perspectives articles, we grouped relevant studies according to this framework to support our interpretation of the findings and the role of digital technology for supporting non-specialist health workers.
Results
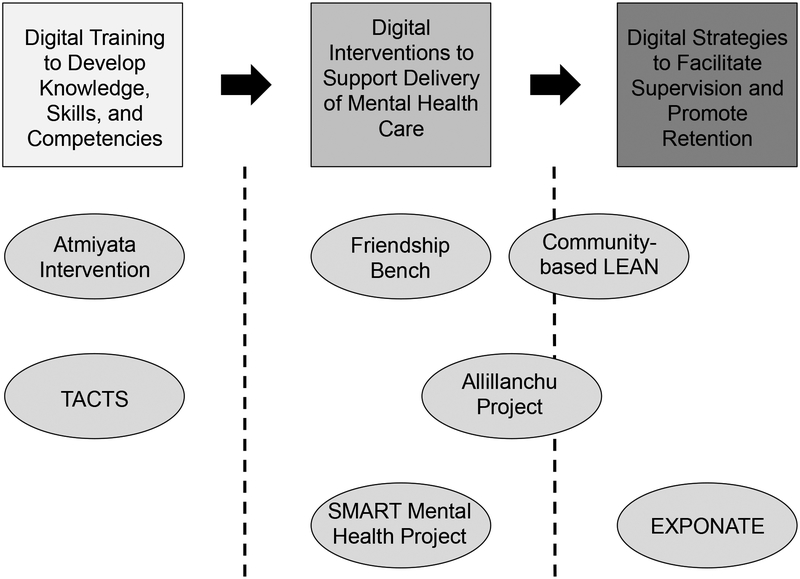
We identified seven examples of interventions using digital technology for supporting non-specialist health workers in the delivery of mental health care. These studies were from six low-income and middle-income countries, including India, Pakistan, Zimbabwe, Peru, China, and Nigeria. In Figure 1, we grouped these studies along the hierarchy proposed by Agarwal et al. (2015) in their framework and describe each example in the sections that follow. See Table 1 for a detailed summary of each study.
Figure 1.
Hierarchical framework depicting how digital technology can support the roles of non-specialist health workers in delivering evidence-based mental health carea
aThis framework is adapted from Agarwal and colleagues (2015) to illustrate the role of mobile technology for supporting non-specialist health workers in low-resource settings23
Table 1.
Examples demonstrating how digital platforms can support non-specialist health workers in the delivery of mental health care in low-resource settings
| Program Name | Country | Population and Setting | Program Description | Use of Digital Technology | Main Outcomes |
|---|---|---|---|---|---|
| Atmiyata Intervention24 | India | CMDs in rural villages | Community volunteers trained as “Atmiyata champions” or “Atmiyata mitras” to support detection of CMDs, provide basic support and counseling, facilitate referral to mental health professionals, and help individuals access social benefits. | Atmiyata champions and mitras provided smartphones to access Android mobile app with videos for training about mental health and questions to test knowledge; separate mobile app with videos for the community covering topics at the village level and available government welfare resources. | Program implemented in 41 rural villages; 59 Atmiyata champions were trained and 264 Atmiyata mitras were trained; there were 1–2 champions and 4–5 mitras assigned to each village. |
| TACTS for Thinking Healthy Program25 | Pakistan | Perinatal depression in a post-conflict rural area | Digital tablet-based program for supporting the training of community health workers to deliver the evidence-based and culturally tailored Thinking Healthy Program involving psychological treatment for perinatal depression. | TACTS system consists of tablet-based package with five training sessions covering core techniques of the Thinking Healthy Program, use of animated ‘avatars’ to narrate the sessions and convey instructional content, and includes role-plays, peer assessment and opportunities to practice problem solving strategies. | Effectiveness of the program for developing community health worker competence is currently being evaluated compared with in person training delivered by mental health specialists as part of a non-inferiority randomized controlled trial. |
| Friendship Bench13 | Zimbabwe | CMDs within primary care clinics | Trained lay health workers deliver the 6-session intervention focused on problem solving techniques on a bench outside the clinic; patients can access peer groups and referral to additional support and treatment. | Lay health workers use text messages and phone calls to reinforce program content and to promote adherence among patients; clinical team used voice calls and text messaging to provide supervision and guidance to lay health workers. | In RCT (n=573), participants in Friendship Bench intervention (n=286) showed significant reductions in symptoms and depression compared to participants standard care control group (n=287) at 6-month follow up. |
| SMART Mental Health Project28 | India | CMDs in rural villages | Community health workers and primary care doctors trained to screen, diagnose and manage common mental disorders using electronic decision support system based on guidelines outlined in the mhGAP program. | Mobile decision support system developed for use on Android tablets with OpenMRS platform to allow community health workers and primary care doctors to share clinical data securely over cloud-based servers; pre-recorded messages sent to individuals who screened positive to promote adherence and continuation of care. | Over 2 year period: 21 community health workers and 2 primary care doctors trained across 30 villages; over 5000 patients screened for CMDs of which 238 screened positive and were referred for treatment; reduction in symptoms and increased mental health services use. |
| Allillanchu Project32 | Peru | CMDs in primary care settings in urban setting | Primary care providers trained to use multi-component digital platform to support early detection, referral and access to treatment for CMDs | Digital program includes mobile screening tool for detection and management CMDs; mobile app provides guidance to primary care providers regarding treatment recommendations and follow up; web-based data collection for monitoring progress; sending patients motivational and reminder text messages to support treatment adherence. | 22 primary care providers, including midwives (n=12), nurses (n=8) and nursing assistants (n=2), were trained to use the program; 733 patients were screened, 159 (22%) screened positive for CMDs; most (n=155) referred to mental health care, and all received follow up text messages. |
| Community-based LEAN34 | China | People living with schizophrenia in rural areas | Program involves lay health supporters who are mostly family members or community volunteers to assist with supervising medication use, monitoring relapse and side effects, and supporting referrals and access to urgent hospital care. | Lay providers supported by a digital e-platform that allows mobile text and voice messaging to provide medication reminders to patients with schizophrenia and to alert when patients are non-adherent and at risk of relapse. E-platform integrates efforts of lay health supporters and their patients with the local village doctors, and the mental health system and psychiatrists. | Program effectiveness is currently being evaluated compared to usual community care as part of a large scale randomized controlled trial in 9 villages in rural townships, with medication adherence as the primary outcome, and symptoms and functioning as secondary outcomes |
| EXPONATE for Perinatal Depression37 | Nigeria | Perinatal depression in primary maternal care clinics in both rural and urban areas settings | Community midwives trained in psychoeducation, problem solving, and parenting skills to deliver 8 weekly sessions to pregnant women who screen positive for depression. Additional sessions provided during pregnancy or after childbirth as needed. | Mobile technology platform used to provide midwives with ongoing monitoring and supervision, connect them with physicians and mental health specialists, and allow them to provide automated text and voice messages to their patients with appointment reminders, promote engagement and reinforce session content. | Effectiveness and cost-effectiveness of the EXPONATE program is currently being evaluated compared to enhanced usual care as part of a pragmatic randomized controlled cluster trial enrolling 29 primary maternal care clinics in Oyo State. |
CMD = common mental disorders
RCT = randomized controlled trial
1). The Atmiyata Intervention in India
Atmiyata is a community-based mental health program focused on promoting wellness, raising awareness, and reducing distress by training and mobilizing community volunteers.24 This project aimed at complementing volunteer groups, which are an existing grassroots-level community resource across many villages in rural India including self-help groups or farmer’s clubs. This approach expands on prior successful efforts for addressing maternal health needs in various settings in India and Nepal as participation in local community groups is a common activity in many villages. Therefore, these groups may afford opportunities to identify individuals affected by mental health concerns and to create a supportive space for addressing their mental health needs.
The program involved training community volunteers as “Atmiyata champions” to support the detection of mental health problems, provide basic support and counseling to community members with common mental health disorders, and to facilitate referral to mental health professionals when necessary. The types of support involved evidence-based low-intensity techniques such as active listening, problem solving, and behavioral activation. The Atmiyata champions were also trained to help individuals access social benefits offered by the government, such as small financial contributions to households, as a means of alleviating poverty that can further exacerbate mental health problems. The program also facilitated a care pathway by providing shorter trainings to other community members, called mitras, so that they can identify individuals experiencing mental health issues for referral to the Atmiyata champions.
The program involves training and building capacity among ordinary community members, while leveraging existing community resources to improve awareness of mental health issues and to promote well-being. Atmiyata champions and mitras were provided smartphones to access videos for ongoing training tools to learn about mental health concepts and to refresh their knowledge and skills. The program also includes Android mobile applications, with one version for the Atmiyata champions and a separate version for the general public and community members. The mobile app contains basic e-learning videos on mental health for the Atmiyata champions with questions built into the app following each training video to test knowledge of mental health topics. The community videos covered important social situations at the village level (e.g., unemployment, problematic alcohol use, marital strife, violence against women), and one video was about available government welfare resources.
This project was developed and implemented in 41 villages across rural Maharashtra, India. In total, 59 Atmiyata champions were trained and 264 Atmiyata Mitras were trained. There were 1–2 champions and 4–5 Mitras assigned to each village. This program relies on utilizing resources that are already in place in rural communities and simultaneously strengthening existing public health linkages by developing working relationships, and referral pathways with district level and rural hospitals, primary health care centers, and non-governmental organizations working in rural communities.24 Furthermore, low-cost digital tools were used to enhance learning and feedback. Evaluation of the effectiveness and lasting impact of this community-model is necessary, as well as ongoing efforts to support supervision, and to overcome implementation challenges including health worker turnover and resistance from public sector mental health specialists.
2). TACTS for Thinking Healthy Program in Pakistan
The Technology-assisted Cascade Training and Supervision (TACTS) is a digital tablet-based program for supporting the training of community health workers, referred to as lady health workers in Pakistan, to deliver the evidence-based Thinking Healthy Program for perinatal depression.25 The Thinking Healthy Program is a culturally adapted intervention involving psychosocial treatment delivered by lady health workers that has previously demonstrated effectiveness at successfully treating perinatal depression in Pakistan.26 Drawing from these prior efforts, it is clear that human resource requirements such as training health workers to deliver the Thinking Healthy Program is a major barrier to scaling up and implementing the intervention. Therefore, the TACTS system was developed to leverage digital technology to facilitate training of lady health workers.
TACTS consists of a tablet-based package with five training sessions covering core techniques and principles of the Thinking Healthy Program. Animated ‘avatars’ depict culturally appropriate characters that narrate the sessions and convey the instructional content. The sessions are interactive, and include role-plays to address real-life challenging situations and to reinforce the content and key skills. Additional educational strategies include use of peer assessment of role-plays, self-reflection, sharing relevant experiences, and opportunities to practice problem solving strategies. There is also a separate module focused on supervision, where more experienced lady health workers learn skills for supervising their peers in delivery of the program. This program is currently being evaluated compared to in-person training delivered by mental health specialists as part of a non-inferiority randomized controlled trial in a post-conflict rural area of Pakistan. The primary outcome is competence of the lady health workers for delivering the intervention.25
3). The Friendship Bench in Zimbabwe
The Friendship Bench intervention is delivered by lay health workers and focuses on individual problem-solving, and is based on an extensive body of prior research and community efforts focused on targeting depression and other common mental disorders in Zimbabwe.27 Trained lay health workers deliver a manualized intervention to patients on a bench situated outside the clinic.27 In total, there are 6 sessions aimed at teaching the participating patients effective techniques for problem solving. After the fourth session, participating patients can choose to access a peer group led by prior participants in the Friendship Bench program. The lay health workers can then refer patients who do not improve following the initial 6 sessions to a supervisor with training in mental health for additional support and treatment.
Mobile technology in the form of text messages and phone calls is used to reinforce program content and to promote adherence among patients enrolled in the intervention.27 Lay health workers send patients up to 6 text messages or phone calls during the program. Technology was identified as a promising approach for reaching patients given that most individuals (90%) accessing primary care services own mobile phones.27 Lay health workers can also use text messaging to reach patients who missed sessions. The clinical team also used mobile phones, including voice calls and text messaging, to provide supervision to the lay health workers as well as guidance and support for responding to challenging cases.
In a randomized controlled trial with 573 patients, those randomized to the Friendship Bench intervention (n=286) showed significant reductions in symptoms measured using the 14-item Shona Symptom Questionnaire (SSQ-14) compared to patients in the standard care control group (n=287) at 6-months follow up (adjusted mean difference in SSQ-14 score, −4.86; 95% CI, −5.63 to −4.10; P < 0.001).13 Friendship Bench participants also showed significant reduction in depressive symptoms measured using the 9-item Patient Health Questionnaire (PHQ-9) compared to control group participants at 6-months follow up (adjusted mean difference in PHQ-9 score, −6.36; 95% CI, −6.45 to −5.27; P < 0.001).13
4). The SMART Mental Health Project in India
The Systematic Medical Appraisal Referral and Treatment (SMART) Mental Health project involved task-sharing and use of mobile technology to support primary care health workers in providing evidence-based mental health care in remote villages in Andhra Pradesh, India. In this project, community health workers referred to as Accredited Social Health Activists (ASHAs) and primary care doctors were trained to screen, diagnose and manage common mental disorders using an electronic decision support system.28,29 This mobile decision support system was developed for use on basic Android devices, and used an OpenMRS platform allowing community health workers and primary care doctors to share clinical data securely using the cloud-based servers.28 The algorithm to support decision-making related to diagnosis and management was based on guidelines outlined in the World Health Organization (WHO) mhGAP program.30 Pre-recorded messages were also sent to individuals who screened positive to promote adherence and continuation of care as recommended by the community health workers and primary care doctors.
As part of the program, 21 community health workers and two primary care doctors were trained over a two-year period across 30 villages. During this time, over 5000 patients were screened for common mental disorders of which 238 were identified as being positive and were referred to the primary care doctors for treatment. Among individuals who screened positive for depression or anxiety at the beginning of the study, there was a reduction in scores by the end of the intervention. At 3-months follow up, there was a reduction in depression measured using the PHQ-9 (adjusted mean difference in PHQ-9, −3.6; SE = 0.6; P < 0.001) and a reduction in anxiety measured using the 7-item Generalized Anxiety Disorder (GAD-7) questionnaire (adjusted mean difference in GAD-7, −1.3; SE = 0.4; P = 0.004).28 A key finding was that individuals increased their use of mental health services following screening and referral to the primary care doctor.31 The SMART program supported with mobile technology was considered both feasible and acceptable for use in this rural setting.
5). The Allillanchu Project in Peru
The Allillanchu Project is based in low-income areas of Lima, Peru, and employs task-sharing through use of a multi-component digital platform for supporting primary care providers, including midwives, nurses, and nursing assistants, in promoting early detection, referral and access to treatment for patients with common mental disorders in primary care settings.32 This program involves training primary care providers to use a mobile screening tool for the detection and management of depression, anxiety, psychosis, convulsive disorders, and problematic alcohol use. The mobile screening app yields immediate results about patients’ symptoms that may require treatment, and provides guidance regarding treatment recommendations and follow up to ensure that effective action was taken. When primary care providers screen patients using the mobile application, data is captured in real time using a web-based data collection platform that allows the research team to continuously monitor progress. The platform can also send patients in need of treatment for common mental disorders motivational and reminder text messages to support treatment adherence. Patients who screened positive are sent text messages over a 2-week period designed to further motivate them to seek mental health care. The messages consisted of reminders about where and when to find mental health care, as well as motivation and encouragement to seek help to address potential barriers to help seeking.33
As part of an implementation evaluation of this program, 22 primary care providers, consisting of midwives (n=12), nurses (n=8) and nursing assistants (n=2), were trained to deliver this care model. Training involved instruction for using the digital platform and mental health content based on the mhGAP training modules.30 Over a 9-week period, 1772 patients were enrolled in the primary care facility, of which 733 were screened by the primary care providers using the digital platform. Of these, 159 (22%) screened positive for a mental disorder, primarily depression or anxiety (n=125). Most (n=155) were referred to mental health care, and all patients who screened positive received follow up text messages from the digital platform. The primary care providers reported that they felt more aware of the importance of caring for their patients’ mental health concerns, and indicated that they had more knowledge and skills needed to provide mental health care. The digital platform appeared to be a successful tool for optimizing detection and referral processes, and for supporting primary care providers in a low-resource setting.32
6). Community-based LEAN in China
The community-based LEAN program aims to improve medication adherence and relapse prevention among people living with schizophrenia in rural China.34 The program seeks to capitalize on the recent ‘686’ countrywide initiative in China to provide practical community-based mental healthcare services35, and address ongoing challenges with poor medication adherence and high rates of relapse.36 The LEAN program actively involves lay health supporters who are mostly family members or community volunteers to assist with supervising medication use, monitoring relapse and side effects, and supporting referrals and access to urgent hospital care. The lay providers are supported by a digital e-platform that allows mobile text and voice messaging to provide medication reminders to patients with schizophrenia and to alert the lay providers when patients are non-adherent and at risk of relapse. Through the digital platform, checklists are used to assist lay health supporters and patients in detecting signs of relapse, monitoring medication use, and delivering general educational content about schizophrenia, treatment, and rehabilitation.34 In this program, there is an award system to promote motivation by allowing patients to earn points that can be redeemed for small prizes for responding to reminder text messages sent from the e-platform. Lastly, the e-platform integrates the efforts of the lay health supporters and their patients with the local village doctors, as well as the mental health system and psychiatrists.
The effectiveness of this program is currently being evaluated compared to usual community care within a large scale randomized controlled trial in 9 villages in rural townships of Hunan province, with medication adherence as the primary outcome, and symptoms and functioning as secondary outcomes.34 This program is novel because it leverages mobile technology as an approach for strengthening the health system by integrating care provided by lay health supporters, village doctors, mental health administrators, and psychiatrists. The digital platform specifically enhances task-sharing by facilitating structured digital communication and information sharing between patients and lay health supporters, who are then connected with mental health administrators and village doctors, and then with municipal psychiatrists. This approach is also unique because technology provides an opportunity to facilitate the engagement of family members in supporting care for relatives living with schizophrenia.
7). EXPONATE for Perinatal Depression in Nigeria
EXPONATE (Expanding Care for Perinatal Women with Depression) is a multicomponent stepped care intervention for perinatal depression in Nigeria supported with mobile technology.37 The program is delivered by community midwives who are trained in psychoeducation, problem-solving treatment, and parenting skills. The midwives deliver eight weekly sessions to pregnant women who screen positive for depression. Additional sessions are provided during pregnancy or after childbirth depending on severity of depressive symptoms. The EXPONATE intervention was adapted from a stepped care program for depression in primary care previously developed and tested in Nigeria38, and incorporated key treatment recommendations outlined in the mhGAP program.30
Mobile technology was integrated into the EXPONATE intervention as a way to provide ongoing monitoring and supervision for the midwives.37 A technological support platform was developed for this project, incorporating a network of mobile telephones linked to an online record system posted on a secure server. Through this platform, the community midwives were connected to physicians and mental health specialists. The physicians and mental health specialists could then use the mobile network to provide support to the midwives using text or voice messages. Additionally, the midwives could connect with their patients using mobile phones, and provide automated text and voice messages with reminders about clinic appointments to promote engagement and reinforce content covered during the in-person sessions. The EXPONATE program is currently being evaluated compared to enhanced usual care as part of a pragmatic randomized controlled cluster trial enrolling 29 primary maternal care clinics in Oyo State, covering clinics in both rural and urban areas of Nigeria.37 The primary outcome for this trial is recovery from depression, and secondary outcomes include mothers’ disability, parenting skills, experience of stigma, health services utilization, and infant development outcomes.37
DISCUSSION
Task-sharing mental health care to non-specialist health workers represents a highly promising approach for overcoming workforce shortages to support detection and treatment of common mental disorders. In this perspectives article, we consider how digital technology can support task-sharing efforts in low-resource settings. We summarized seven promising examples from six different countries with evidence ranging from large-scale randomized controlled trials, cohort studies, and early stage demonstration and implementation projects. Four projects were focused in rural settings24,25,28,34, one study was based in both urban and rural settings37, and two projects were based in urban areas.13,32 Four projects focused on common mental disorders in the primary care or community setting24,27,28,32, two projects focused on perinatal depression25,37, and one project leveraged community contacts for supporting care for persons living with schizophrenia.34 Importantly, digital technology was largely used to support or strengthen the delivery of existing evidence-based programs for mental health care. The success of new strategies involving use of digital technology likely will depend on whether these technologies can integrate seamlessly into already fragmented and heavily under-resourced health systems. It will also be essential for future efforts using digital technology to extend beyond supporting the delivery of existing services or programs, and to identify new models for deploying digital interventions to empower non-specialist health workers in ways that were previously not considered possible.39 This could include smartphone-based systems offering real-time decision support to non-specialist health workers deployed in remote areas, digital platforms that facilitate peer supervision and continuing education among health workers, and wearable sensors for monitoring high-risk patients and enabling non-specialist health workers to track treatment progress and respond to crises or signs of relapse.40
We found that few studies reported clinically meaningful effectiveness outcomes. This is consistent with a systematic review of 42 studies broadly using digital technology to support the roles of frontline health workers for delivering care for a range of health conditions.23 This prior review showed that despite considerable support for the feasibility and acceptability of using digital approaches, robust evidence on effectiveness was lacking.23 Importantly, for three of the interventions using digital technology that we summarized here, large-scale evaluations of effectiveness are currently ongoing (published protocols for these studies were included).25,34,37 We identified the different clinical functions of the digital technology in each study and summarized these as a matrix in Table 2. Many of the projects leveraged technology that is widely available, such as text messaging, voice calls, and smartphones to facilitate supervision of non-specialist health workers, and to allow non-specialist health workers to send reminders and supportive messages to their patients. Several projects also introduced more sophisticated platforms to support supervision, care coordination, and ongoing support for non-specialist health workers.
Table 2.
The clinical functions of digital platforms for supporting non-specialist health workers in the delivery of mental health care in low-resource settings
| Program Name | Type of health worker | Clinical Function of Digital Technologya | |||||
|---|---|---|---|---|---|---|---|
| Care coordination | Education | Supervision | Data collection and sharing | Alerts and reminders | Decision support, screening, and referrals | ||
| Atmiyata Intervention24 | Community volunteers | X | |||||
| TACTS for Thinking Healthy Program25 | CHWs referred to as Lady Health Workers | X | |||||
| Friendship Bench13 | Lay health workers | X | X | X | |||
| SMART Mental Health Project28 | CHWs and primary care doctors | X | X | X | |||
| Allillanchu Project32 | Primary care providers (e.g., midwives, nurses, nurse assistants) | X | X | X | X | ||
| Community-based LEAN34 | Lay health supporters who are mostly family members or community volunteers | X | X | X | X | ||
| EXPONATE for Perinatal Depression37 | Community midwives | X | X | X | |||
CHW = community health worker
The selection of different clinical functions of the digital technology were informed by a prior review of the evidence on the use of mobile health (mHealth) strategies among frontline health workers in low-income and middle-income countries.23
As highlighted in the examples here, technology largely served as a tool for enhancing the role of non-specialist health workers by allowing them to connect with and support their patients, access opportunities for training and skill development, receive supervision and support from more specialized providers, and improve data collection and care coordination. In comparison, a 2016 report summarizing over 140 projects using mobile technology for supporting frontline health workers in lower income countries found that mobile technology was primarily used for supporting data collection and electronic decision support, as well as facilitating provider training and education and provider-to-provider communication.41 Roughly 40% of the projects included in this prior report used smartphones, yet only one project targeted mental health.41 Among the studies summarized here we found that technology played an important role in facilitating communication, either directly between non-specialist health workers and their patients, or between non-specialist health workers and their supervisors or more specialized providers. As many evidence-based treatments for common mental disorders involve a high degree of human contact, emphasis on using technology for communication may offer an alternative to facilitate these connections. Consistent with the 2016 report41, we observed that technology did not act as a replacement for human capacity, but rather served as an important tool for supporting non-specialist health workers in their roles.
In countries where there is an established cadre of non-specialist health workers, digital technology could serve an especially important role for developing skills and competencies among these health workers to deliver evidence-based mental health care. We identified two studies that employed digital approaches for supporting skill building and knowledge acquisition among non-specialist health workers. In the Atmiyata program in a rural setting in India, basic educational videos were disseminated to community members using mobile applications accessible through a smartphone.24 In another example, a tablet-based system is currently being used to train community health workers to deliver the evidence-based and culturally tailored Thinking Healthy Program involving psychological treatment for perinatal depression in Pakistan.25 Continued efforts will be essential for determining whether digital training programs are effective at achieving clinical competence among non-specialist health workers, whether these digital programs are as effective as traditional face-to-face training programs, and the costs associated with developing and delivering these digital programs.
It will also be important to ensure the careful design of digital training programs by taking into account the perceptions and views of non-specialist health workers, as well as the local context where they work. For instance, this could involve eliciting non-specialist health workers’ explanatory models for mental disorders, referring to their understanding of the causes, symptoms, and treatments for mental disorders framed within the context of their cultural beliefs and local social norms.42 In contrast to specialist mental health clinicians, non-specialist health workers are typically embedded within the same communities as the patients they treat, and are therefore ideally situated to tailor treatments to the culture and explanatory models of illness of their patients.43,44 Through iterative design processes, it is possible to extend beyond simply transmitting clinical information and to adapt digital content to non-specialist health workers’ existing explanatory models, diverse contexts, and local language, which could support the cultural relevance of the program materials and promote ownership and engagement among users.45 By working closely with non-specialist health workers to develop digital interventions, it could also yield opportunities to identify misperceptions and stigmatizing views about mental disorders, making it possible to include content aimed at responding to these concerns.
Limitations with this perspectives article warrant discussion. First, our search of the literature was not systematic as we intentionally employed a narrative review expanding on four recent relevant reviews to identify the selection of highly promising examples summarized here. Further, we only considered examples from the published peer-reviewed literature. Therefore, we may not have fully captured the scope of evidence and possible unpublished projects. Second, there are several concerns related to generalizability. In research with digital technology, recruitment typically favors people who are already interested in using these technologies, which may only represent a small portion of the broader target population.39 This concern is especially prominent in the evaluation of digital interventions for persons living with mental illness, whereby technologies are usually designed for people who will use them, rather than for the larger population of individuals who need them and who are most likely to benefit from them.39 We may have observed the same concern here, where non-specialist health workers who agree to use digital technology for supporting delivery of mental health care are likely already interested and willing to use these technologies in their work, and may also be aware of the importance of treating or preventing mental disorders. Third, safety and ethical considerations related to technology use among non-specialist health workers also requires greater attention. None of the studies described here specifically mentioned efforts to uphold safety or minimize risks.
There remain several challenges ahead that require consideration. Integration of mental health care into existing health care systems is essential46, and digital technology can potentially support these efforts. Drawing from the examples summarized here, digital technology can facilitate communication, data collection, patient tracking and monitoring, and training and skill development, all of which are necessary for successfully integrating evidence-based mental health care within existing services for other non-communicable diseases.46 This is especially relevant for non-specialist health workers, as they typically encounter a large burden of chronic health conditions in their work.47 Furthermore, technology holds promise for maximizing available human resources capacity by allowing non-specialist health workers to screen patients and triage the mental health concerns encountered during their visits with patients. For example, individuals who are distressed or who have less severe forms of depression or other common mental disorders may be treated directly by non-specialist health workers, while individuals with increasingly complex mental disorders may be referred to more specialized providers. Digital interventions using mobile technology could facilitate patient screening and contact with supervisors, thereby making it possible to maximize the skill level of the limited number of available specialists, while empowering non-specialist health workers to effectively address the cases within the purvue of their training, clinical competence and skills.48 Furthermore, digital technology could serve an important function for enabling real-time program evaluation and capturing data to inform quality improvement efforts. As digital technologies support non-specialist health workers in data collection, outcome reporting, surveillance, and communication with patients and supervisors, there are important opportunities to inform continuous improvements to the efficiency of health systems and the quality of care delivered.23,49
Another consideration is the importance of having consistent and reliable wireless internet access, which remains a key challenge in many regions despite increasing device ownership. For example, fluctuations in wireless connectivity are common in impoverished settings and rural areas, and during poor weather conditions.50,51 To ensure the success of digital interventions for supporting non-specialist health workers, it will be important to consider how these technologies can function when wireless connectivity is poor, such as relying on asynchronous communication or data sharing as opposed to direct approaches, or by accessing content stored on the devices rather than streaming content over the internet.50 Such approaches will be needed to overcome immediate challenges with wireless connectivity until more robust mobile broadband networks become more widely available.
A final consideration is the need for economic models to ensure sustainability of digital interventions to support non-specialist health workers in delivering evidence-based mental health care. The increasing availability and decreasing costs of digital devices combined with recognition of mental health care as a priority within health systems are important. However, assessing costs will be essential for informing health systems, policy makers, and governments towards ensuring sustainability of digital efforts to support non-specialist health workers in delivering effective mental health care. Therefore, it will be necessary to ensure collection and reporting of the costs of developing digital interventions, the costs associated with delivering and implementing these programs, and the potential cost savings generated through task-sharing, increased efficiency and improved patient outcomes.
CONCLUSION
There is immense potential to leverage the increasing availability and reach of digital technologies to enhance the capacity, skills, and support for non-specialist health workers in low-resource settings towards alleviating the global burden of mental disorders. The examples described in this perspectives article contribute to mounting evidence demonstrating that non-specialist health workers can effectively deliver a wide range of evidence-base mental health treatments across diverse settings globally.5,10 Importantly, we found that technology appears to offer an important tool for supporting task-sharing of mental health care. Ongoing work will be critical to explore new opportunities for digital technology to drive innovative models of care delivery necessary to enhance the impact and reach of non-specialist health workers, to demonstrate the effectiveness and cost-effectiveness of these efforts, and to determine the scalability and sustained delivery of digital interventions in low-resource settings.
Acknowledgements:
This project was supported by a grant from the National Institute of Mental Health (U19MH113211). The funders played no role in the study design; collection, analysis, or interpretation of data; writing of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Competing Interests: None for any author.
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. The Lancet Psychiatry. 2016;3(2):171–178. [DOI] [PubMed] [Google Scholar]
- 2.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72(4):334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel V, Chisholm D, Parikh R, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities. The Lancet. 2016;387(10028):1672–1685. [DOI] [PubMed] [Google Scholar]
- 4.Kakuma R, Minas H, van Ginneken N, et al. Human resources for mental health care: current situation and strategies for action. The Lancet. 2011;378(9803):1654–1663. [DOI] [PubMed] [Google Scholar]
- 5.Hoeft TJ, Fortney JC, Patel V, Unützer J. Task-Sharing Approaches to Improve Mental Health Care in Rural and Other Low-Resource Settings: A Systematic Review. The Journal of rural health. 2018;34(1):48–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroenke K, Unutzer J. Closing the false divide: sustainable approaches to integrating mental health services into primary care. Journal of general internal medicine. 2017;32(4):404–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baingana F, Al’Absi M, Becker AE, Pringle B. Global research challenges and opportunities for mental health and substance-use disorders. Nature. 2015;527(7578):S172–S177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairburn CG, Patel V. The global dissemination of psychological treatments: a road map for research and practice. American Journal of Psychiatry. 2014;171(5):495–498. [DOI] [PubMed] [Google Scholar]
- 9.Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Social science & medicine. 2013;97:82–86. [DOI] [PubMed] [Google Scholar]
- 10.Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: Lessons from low-and middle-income countries. Annual review of clinical psychology. 2017;13:149–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Ginneken N, Tharyan P, Lewin S, et al. Non‐specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low-and middle-income countries. The Cochrane Library. 2013;11(11):CD009149. [DOI] [PubMed] [Google Scholar]
- 12.Patel V, Weobong B, Weiss HA, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. The Lancet. 2017;389(10065):176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chibanda D, Weiss HA, Verhey R, et al. Effect of a primary care–based psychological intervention on symptoms of common mental disorders in Zimbabwe: a randomized clinical trial. Jama. 2016;316(24):2618–2626. [DOI] [PubMed] [Google Scholar]
- 14.Rahman A, Hamdani SU, Awan NR, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. Jama. 2016;316(24):2609–2617. [DOI] [PubMed] [Google Scholar]
- 15.Kazdin AE. Addressing the treatment gap: A key challenge for extending evidence-based psychosocial interventions. Behaviour research and therapy. 2017;88:7–18. [DOI] [PubMed] [Google Scholar]
- 16.Kemp S Digital in 2018: World’s Internet Users Pass the 4 Billion Mark. 2018; https://wearesocial.com/blog/2018/01/global-digital-report-2018. Accessed May 9, 2018.
- 17.Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health. 2015;24(5):321–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farrington C, Aristidou A, Ruggeri K. mHealth and global mental health: still waiting for the mH 2 wedding? Globalization and health. 2014;10(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naslund JA, Aschbrenner KA, Araya R, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. The Lancet Psychiatry. 2017;4(6):486–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fairburn CG, Patel V. The impact of digital technology on psychological treatments and their dissemination. Behaviour research and therapy. 2017;88:19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing Community Health Workers to Address Mental Health Disparities for Underserved Populations: A Systematic Review. Adm Policy Ment Health. 2018:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kohrt BA, Asher L, Bhardwaj A, et al. The role of communities in mental Hhalth care in low-and middle-income countries: a meta-review of components and competencies. International journal of environmental research and public health. 2018;15(6):1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal S, Perry HB, Long LA, Labrique AB. Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Tropical medicine & international health. 2015;20(8):1003–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shields-Zeeman L, Pathare S, Walters BH, Kapadia-Kundu N, Joag K. Promoting wellbeing and improving access to mental health care through community champions in rural India: the Atmiyata intervention approach. International journal of mental health systems. 2017;11(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zafar S, Sikander S, Hamdani SU, et al. The effectiveness of Technology-assisted Cascade Training and Supervision of community health workers in delivering the Thinking Healthy Program for perinatal depression in a post-conflict area of Pakistan–study protocol for a randomized controlled trial. Trials. 2016;17(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. The Lancet. 2008;372(9642):902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chibanda D, Bowers T, Verhey R, et al. The Friendship Bench programme: a cluster randomised controlled trial of a brief psychological intervention for common mental disorders delivered by lay health workers in Zimbabwe. International journal of mental health systems. 2015;9(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maulik PK, Kallakuri S, Devarapalli S, Vadlamani VK, Jha V, Patel A. Increasing use of mental health services in remote areas using mobile technology: a pre–post evaluation of the SMART Mental Health project in rural India. Journal of global health. 2017;7(1):010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maulik PK, Tewari A, Devarapalli S, Kallakuri S, Patel A. The Systematic Medical Appraisal, Referral and Treatment (SMART) Mental Health Project: development and testing of electronic decision support system and formative research to understand perceptions about mental health in rural India. PloS one. 2016;11(10):e0164404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. mhGAP training manuals for the mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings-version 2.0 (for field testing). Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 31.Tewari A, Kallakuri S, Devarapalli S, Jha V, Patel A, Maulik PK. Process evaluation of the systematic medical appraisal, referral and treatment (SMART) mental health project in rural India. BMC psychiatry. 2017;17(1):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diez-Canseco F, Toyama M, Ipince A, et al. Integration of a Technology-Based Mental Health Screening Program Into Routine Practices of Primary Health Care Services in Peru (The Allillanchu Project): Development and Implementation. Journal of medical Internet research. 2018;20(3):e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Toyama M, Diez-Canseco F, Busse P, Del Mastro I, Miranda J. Design and content validation of a set of SMS to promote seeking of specialized mental health care within the Allillanchu Project. Global Health, Epidemiology and Genomics. 2018;3:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu DR, Gong W, Caine ED, et al. Lay health supporters aided by a mobile phone messaging system to improve care of villagers with schizophrenia in Liuyang, China: protocol for a randomised control trial. BMJ open. 2016;6(1):e010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Good BJ, Good M-JD. Significance of the 686 Program for China and for global mental health. Shanghai archives of psychiatry. 2012;24(3):175–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Q, Huang X, Wen H, Liang X, Lei L, Wu J. Retrospective analysis of treatment effectiveness among patients in Mianyang Municipality enrolled in the national community management program for schizophrenia. Shanghai archives of psychiatry. 2012;24(3):131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gureje O, Oladeji BD, Araya R, et al. Expanding care for perinatal women with depression (EXPONATE): study protocol for a randomized controlled trial of an intervention package for perinatal depression in primary care. BMC psychiatry. 2015;15(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oladeji BD, Kola L, Abiona T, Montgomery AA, Araya R, Gureje O. A pilot randomized controlled trial of a stepped care intervention package for depression in primary care in Nigeria. BMC psychiatry. 2015;15(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mohr DC, Weingardt KR, Reddy M, Schueller SM. Three problems with current digital mental health research… and three things we can do about them. Psychiatric services. 2017;68(5):427–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. The Lancet. 2018. [DOI] [PubMed] [Google Scholar]
- 41.Agarwal S, Rosenblum L, Goldschmidt T, Carras M, Labrique A. Mobile technology in support of frontline health workers. A comprehensive overview of the landscape knowledge gaps and future directions. Johns Hopkins University Global mHealth Initiative;2016. [Google Scholar]
- 42.Kleinman A Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine. Part B: Medical Anthropology. 1978;12:85–93. [DOI] [PubMed] [Google Scholar]
- 43.Witmer A, Seifer SD, Finocchio L, Leslie J, O’neil EH. Community health workers: integral members of the health care work force. American journal of public health. 1995;85(8_Pt_1):1055–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mendenhall E, De Silva MJ, Hanlon C, et al. Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Social science & medicine. 2014;118:33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Källander K, Tibenderana JK, Akpogheneta OJ, et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low-and middle-income countries: a review. Journal of medical Internet research. 2013;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J. Grand challenges: integrating mental health services into priority health care platforms. PloS medicine. 2013;10(5):e1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patel V, Chatterji S. Integrating mental health in care for noncommunicable diseases: an imperative for person-centered care. Health Affairs. 2015;34(9):1498–1505. [DOI] [PubMed] [Google Scholar]
- 48.Patel V Talking sensibly about depression. PLoS medicine. 2017;14(4):e1002257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laktabai J, Platt A, Menya D, et al. A mobile health technology platform for quality assurance and quality improvement of malaria diagnosis by community health workers. PloS one. 2018;13(2):e0191968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wallis L, Blessing P, Dalwai M, Shin SD. Integrating mHealth at point of care in low-and middle-income settings: the system perspective. Global health action. 2017;10(sup3):1327686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siedner MJ, Lankowski A, Musinga D, et al. Optimizing network connectivity for mobile health technologies in sub-Saharan Africa. PLoS One. 2012;7(9):e45643. [DOI] [PMC free article] [PubMed] [Google Scholar]