Abstract
Background
Gingival recession is defined as the oral exposure of the root surface due to a displacement of the gingival margin apical to the cemento‐enamel junction and it is regularly linked to the deterioration of dental aesthetics. Successful treatment of recession‐type defects is based on the use of predictable root coverage periodontal plastic surgery (RCPPS) procedures. This review is an update of the original version that was published in 2009.
Objectives
To evaluate the efficacy of different root coverage procedures in the treatment of single and multiple recession‐type defects.
Search methods
Cochrane Oral Health's Information Specialist searched the following databases: Cochrane Oral Health's Trials Register (to 15 January 2018), the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 12) in the Cochrane Library (searched 15 January 2018), MEDLINE Ovid (1946 to 15 January 2018), and Embase Ovid (1980 to 15 January 2018). The US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials (15 January 2018). No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) only of at least 6 months' duration evaluating recession areas (Miller's Class I or II ≥ 3 mm) and treated by means of RCPPS procedures.
Data collection and analysis
Screening of eligible studies, data extraction and risk of bias assessment were conducted independently and in duplicate. Authors were contacted for any missing information. We expressed results as random‐effects models using mean differences (MD) for continuous outcomes and odds ratios (OR) for dichotomous outcomes with 95% confidence intervals (CI). We used GRADE methods to assess the quality of the body of evidence of our main comparisons.
Main results
We included 48 RCTs in the review. Of these, we assessed one as at low risk of bias, 12 as at high risk of bias and 35 as at unclear risk of bias. The results indicated a greater reduction in gingival recession for subepithelial connective tissue grafts (SCTG) + coronally advanced flap (CAF) compared to guided tissue regeneration with resorbable membranes (GTR rm) + CAF (MD ‐0.37 mm; 95% CI ‐0.60 to ‐0.13, P = 0.002; 3 studies; 98 participants; low‐quality evidence). There was insufficient evidence of a difference in gingival recession reduction between acellular dermal matrix grafts (ADMG) + CAF and SCTG + CAF or between enamel matrix protein (EMP) + CAF and SCTG + CAF. Regarding clinical attachment level changes, GTR rm + CAF promoted additional gains compared to SCTG + CAF (MD 0.35; 95% CI 0.06 to 0.63, P = 0.02; 3 studies; 98 participants; low‐quality evidence) but there was insufficient evidence of a difference between ADMG + CAF and SCTG + CAF or between EMP + CAF and SCTG + CAF. Greater gains in the keratinized tissue were found for SCTG + CAF when compared to EMP + CAF (MD ‐1.06 mm; 95% CI ‐1.36 to ‐0.76, P < 0.00001; 2 studies; 62 participants; low‐quality evidence), and SCTG + CAF when compared to GTR rm + CAF (MD ‐1.77 mm; 95% CI ‐2.66 to ‐0.89, P < 0.0001; 3 studies; 98 participants; very low‐quality evidence). There was insufficient evidence of a difference in keratinized tissue gain between ADMG + CAF and SCTG + CAF. Few data exist on aesthetic condition change related to patients' opinion and patients' preference for a specific procedure.
Authors' conclusions
Subepithelial connective tissue grafts, coronally advanced flap alone or associated with other biomaterial and guided tissue regeneration may be used as root coverage procedures for treating localised or multiple recession‐type defects. The available evidence base indicates that in cases where both root coverage and gain in the width of keratinized tissue are expected, the use of subepithelial connective tissue grafts shows a slight improvement in outcome. There is also some weak evidence suggesting that acellular dermal matrix grafts appear as the soft tissue substitute that may provide the most similar outcomes to those achieved by subepithelial connective tissue grafts. RCTs are necessary to identify possible factors associated with the prognosis of each RCPPS procedure. The potential impact of bias on these outcomes is unclear.
Plain language summary
Root coverage procedures for the treatment of localised and multiple recession‐type defects
Review question
The aim of this review was to evaluate the efficacy of different surgical procedures to cover exposed tooth roots, when the gum tissue has receded away from the tooth.
Background
Receding gums (also known as gingival recession) is the gradual loss of gum tissue, and if left untreated it can result in exposure of the tooth root, between the gum and the tooth. It can involve one tooth (single recession‐type defect) or many teeth (multiple recession‐type defects). It can affect the look of the teeth, and is also linked to tooth sensitivity. Exposure of the tooth root can be treated by cosmetic surgery; techniques include grafting and gum regeneration. Grafting involves taking tissue from another place in the mouth and stitching it over the area of the exposed root. With gum regeneration, biomaterials are used to regenerate gum tissue without the need for taking it from the roof of the mouth. Procedures used in gum grafting and gum regeneration include: free gingival grafts, coronally advanced flaps, acellular dermal matrix grafts, laterally positioned flaps and guided tissue regeneration. This review is an update of the original version that was published in 2009.
Study characteristics
Authors from Cochrane Oral Health carried out this review and the evidence is up to date to 15 January 2018. A total of 48 randomised controlled trials on 1227 adults were included with five studies evaluating multiple recession‐type defects and the rest single gingival recessions. Most trials followed participants for 6 months to 12 months. The review looked at different interventions: free gingival grafts (FGG), coronally advanced flap (CAF) alone or associated to acellular dermal matrix grafts (ADMG), enamel matrix protein (EMP), guided tissue regeneration with resorbable membranes (GTR rm), guided tissue regeneration with non‐resorbable membranes (GTR nrm), GTR rm associated with bone substitutes, platelet‐rich plasma or fibrin (PRP or PRF), growth factors (rhPDGF‐BB) associated to bone substitutes (b‐TCP), subepithelial connective tissue grafts (SCTG) or xenogeneic collagen matrix (XCM). We did not find any trials evaluating laterally positioned flaps (LPF).
Key results
The results of this review have shown that most root coverage periodontal plastic surgery procedures led to gains in reduction of gingival recession. However, we are uncertain about which intervention is the most effective as all studies were judged to be at unclear or high risk of bias. Preferably, subepithelial connective tissue grafts, coronally advanced flap alone or associated with another graft or biomaterial and guided tissue regeneration can be used as root coverage procedures for treating recession‐type defects. Limited data exist on how these interventions affect the appearance of the teeth. Adverse effects reported in the studies included discomfort and pain, but these were mainly related to the site where the tissue graft was taken, and occurred mainly within the first week after surgery with no influence on root coverage outcomes. Further research is needed on the results to be achieved from each root coverage periodontal plastic procedure.
Quality of the evidence
We judged the quality of the evidence to be low or very low mainly due to problems with the design of the studies.
Summary of findings
Summary of findings for the main comparison. Acellular dermal matrix graft (ADMG) + coronally advanced flap (CAF) compared to subepithelial connective tissue graft (SCTG) + CAF for treating adult patients with single recession‐type defects (short term).
| ADMG + CAF compared to SCTG + CAF for adult patients with localised recession‐type defects (short term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: university dental departments Intervention: ADMG + CAF Comparison: SCTG + CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SCTG + CAF | Risk with ADMG + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Sites with complete root coverage Follow‐up: range 6 months to 12 months | 520 per 1000 | 245 per 1000 (123 to 597) | OR 0.43 (0.13 to 1.37) | 50 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | Only parallel‐design studies were included |
| Gingival recession change Follow‐up: range 6 months to 12 months | The mean gingival recession change ranged from 2.48 to 4.20 mm | MD 0.36 mm lower (1.03 lower to 0.3 higher) | ‐ | 100 (4 RCTs) | ⊕⊕⊝⊝ LOW2 | Subgroup analyses were undertaken for parallel‐design and split‐mouth studies |
| Clinical attachment level change Follow‐up: range 6 months to 12 months | The mean clinical attachment level change ranged from 2.23 to 4.40 mm | MD 0.53 mm lower (1.14 lower to 0.08 higher) | ‐ | 100 (4 RCTs) | ⊕⊕⊝⊝ LOW2 | Subgroup analyses were undertaken for parallel‐design and split‐mouth studies |
| Keratinized tissue change Follow‐up: range 6 months to 12 months | The mean keratinized tissue change ranged from ‐0.15 to ‐3.30 mm | MD 0.59 mm lower (1.27 lower to 0.10 higher) | ‐ | 100 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW3 | Subgroup analyses were undertaken for parallel‐design and split‐mouth studies.There was a clear inconsistence in the results according to the study design |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ADMG: acellular dermal matrix graft; CAF: coronally advanced flap; CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial; SCTG: subepithelial connective tissue graft. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
|
1Downgraded 2 levels for imprecision.
2Downgraded 1 level for inconsistency and 1 for imprecision. 3Downgraded 2 levels for inconsistency and 1 for imprecision. | ||||||
Summary of findings 2. Acellular dermal matrix graft (ADMG) + coronally advanced flap (CAF) compared to CAF for treating adult patients with single recession‐type defects (short term).
| ADMG + CAF compared to CAF for adult patients with single recession‐type defects (short term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: university/dental hospital Intervention: ADMG + CAF Comparison: CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with CAF | Risk with ADMG + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Sites with complete root coverage Follow‐up: range 6 months to 12 months | 280 per 1000 | 607 per 1000 (72 to 969) | OR 3.97 (0.20 to 80.50) | 50 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW1 | 1 parallel‐design and 1 split‐mouth studies were included. There was a clear inconsistence in the results according to the study design |
| Gingival recession depth change Follow‐up: range 6 months to 12 months | The mean gingival recession depth change ranged from 2.19 to 2.50 mm | MD 0.61 mm higher (0.52 lower to 1.73 higher) | ‐ | 50 (2 RCTs) | ⊕⊕⊝⊝ LOW2 | 1 parallel‐design and 1 split‐mouth studies were included |
| Clinical attachment level change Follow‐up: range 6 months to 12 months | The mean clinical attachment level change ranged from 1.92 to 2.64 mm | MD 0.51 mm higher (0.25 lower to 1.27 higher) | ‐ | 50 (2 RCTs) | ⊕⊕⊝⊝ LOW2 | 1 parallel‐design and 1 split‐mouth studies were included |
| Keratinized tissue width change Follow‐up: range 6 months to 12 months | The mean keratinized tissue width change ranged from ‐0.33 to ‐0.46 mm | MD 0.28 mm higher (0.08 lower to 0.64 higher) | ‐ | 50 (2 RCTs) | ⊕⊕⊝⊝ LOW2 | 1 parallel‐design and 1 split‐mouth studies were included |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ADMG: acellular dermal matrix graft; CAF: coronally advanced flap; CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
|
1Downgraded 2 levels for inconsistency and 1 level for imprecision. 2Downgraded 1 level for inconsistency and 1 level for imprecision. | ||||||
Summary of findings 3. Enamel matrix protein (EMP) + coronally advanced flap (CAF) compared to CAF for treating adult patients with single recession‐type defects (short term).
| EMP + CAF compared to CAF for adult patients with single recession‐type defects (short term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: university/dental hospital Intervention: EMP + CAF Comparison: CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with CAF | Risk with EMP + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Gingival recession depth change Follow‐up: range 6 months to 12 months | The mean gingival recession depth change ranged from 2.16 to 3.80 mm | MD 0.07 mm higher (0.25 lower to 0.40 higher) | ‐ | 136 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 2 split‐mouth studies were included |
| Clinical attachment level change Follow‐up: range 6 months to 12 months | The mean clinical attachment level change ranged from 2.18 to 3.80 mm | MD 0.22 mm higher (0.02 lower to 0.45 higher) | ‐ | 136 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 2 split‐mouth studies were included |
| Keratinized tissue width change Follow‐up: range 6 months to 12 months | The mean keratinized tissue width change ranged from ‐0.30 to ‐0.53 mm | MD 0.35 mm higher (0.13 higher to 0.56 higher) | ‐ | 136 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 2 split‐mouth studies were included |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAF: coronally advanced flap; CI: confidence interval; EMP: enamel matrix protein; MD: mean difference; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded 1 level for inconsistency and 1 level for imprecision. | ||||||
Summary of findings 4. Enamel matrix protein (EMP) + coronally advanced flap (CAF) compared to subepithelial connective tissue graft (SCTG) + CAF for treating adult patients with single recession‐type defects (short/medium term).
| EMP + CAF compared to SCTG + CAF for adult patients with single recession‐type defects (short/medium term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: private practice Intervention: EMP + CAF Comparison: SCTG + CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SCTG + CAF | Risk with EMP + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | (1 RCT) | ⊕⊝⊝⊝ VERY LOW1 | McGuire 2012 10 years after surgery asked their patients to respond to questions related to aesthetic satisfaction. 6 patients had no preference for a particular type of treatment, 2 favoured aesthetic results with the test treatment (i.e. EMD + CAF), and 1 favoured results with the control treatment (SCTG + CAF) (P = 0.564) |
| Sites with complete root coverage Follow‐up: range 6 months to 24 months | 742 per 1000 | 527 per 1000 (141 to 1000) | OR 0.61 (0.05 to 7.86) | 62 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW2 | 1 of the studies provided 6‐month data, while the other 24‐month outcomes |
| Gingival recession change Follow‐up: range 6 months to 12 months | The mean gingival recession change ranged from 4.01 to 4.33 mm | MD 0.39 mm lower (1.27 lower to 0.48 higher) | ‐ | 62 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW2 | ‐ |
| Clinical attachment change Follow‐up: range 6 months to 12 months | The mean clinical attachment change ranged from 4.21 to 4.51 mm | MD 0.25 mm lower (0.69 lower to 0.20 higher) | ‐ | 62 (2 RCTs) | ⊕⊕⊝⊝ LOW3 | ‐ |
| Keratinized tissue change Follow‐up: range 6 months to 12 months | The mean keratinized tissue change ranged from ‐1.56 to ‐1.83 mm | MD 1.06 mm lower (1.36 lower to 0.76 lower) | ‐ | 62 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW2 | ‐ |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAF: coronally advanced flap; CI: confidence interval; EMP: enamel matrix protein; MD: mean difference; RCT: randomised controlled trial; SCTG: subepithelial connective tissue graft. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
|
1Downgraded 1 level for risk of bias, 1 level for inconsistency and 2 levels for imprecision. 2Downgraded 1 level for inconsistency and 2 levels for imprecision. 3Downgraded 2 levels for imprecision. | ||||||
Summary of findings 5. Guided tissue regeneration resorbable membrane (GTR rm) + coronally advanced flap (CAF) compared to subepithelial connective tissue graft (SCTG) + CAF for treating adult patients with single recession‐type defects (short term).
| GTR rm + CAF compared to SCTG + CAF for adult patients with localised recession‐type defects (short term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: university dental departments Intervention: GTR rm + CAF Comparison: SCTG + CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SCTG + CAF | Risk with GTR rm + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Sites with complete root coverage Follow‐up: range 6 months to 12 months | 571 per 1000 | 449 per 1000 (286 to 623) | OR 0.61 (0.30 to 1.24) | 98 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | ‐ |
| Gingival recession change Follow‐up: range 6 months to 12 months | The mean gingival recession change ranged from 2.80 to 5.30 mm | MD 0.37 mm lower (0.60 lower to 0.13 lower) | ‐ | 98 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | ‐ |
| Clinical attachment level change Follow‐up: range 6 months to 12 months | The mean clinical attachment level change ranged from 2.30 to 4.70 | MD 0.35 higher (0.06 higher to 0.63 higher) | ‐ | 98 (3 RCTs) | ⊕⊕⊝⊝ LOW1 | ‐ |
| Keratinized tissue change Follow‐up: range 6 months to 12 months | The mean keratinized tissue change ranged from ‐1.10 to ‐3.10 mm | MD 1.77 mm lower (2.66 lower to 0.89 lower) | ‐ | 98 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW2 | ‐ |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAF: coronally advanced flap; CI: confidence interval; GTR rm: guided tissue regeneration resorbable membrane; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial; SCTG: subepithelial connective tissue graft. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
|
1 Downgraded 2 levels for imprecision. 2 Downgraded 1 level for inconsistency and 2 levels for imprecision. | ||||||
Summary of findings 6. Xenogeneic collagen matrix (XCM) + coronally advanced flap (CAF) compared to CAF for treating adult patients with single recession‐type defects (short term).
| XCM + CAF compared to CAF for adult patients with single recession‐type defects (short term) | ||||||
| Patient or population: adult patients with single recession‐type defects Setting: university/dental hospital Intervention: XCM + CAF Comparison: CAF | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with CAF | Risk with XCM + CAF | |||||
| Aesthetic condition change related to patient's opinion | ‐ | ‐ | ‐ | (1 RCT) | ⊕⊕⊝⊝ LOW1 | Sangiorgio 2017 compared XCM + CAF versus CAF alone in the treatment of single gingival recessions. Root coverage aesthetics and overall aesthetic results were evaluated by each patient with the assistance of a VAS. Similar findings were found for both outcomes, irrespective of the type of treatment applied |
| Sites with complete root coverage Follow‐up: range 6 months to 12 months | 404 per 1000 | 762 per 1000 (614 to 866) | OR 4.73 (2.35 to 9.50) | 104 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 1 split‐mouth studies were included |
| Gingival recession depth change Follow‐up: range 6 months to 12 months | The mean gingival recession depth change ranged from 2.16 to 2.36 mm | MD 0.40 mm higher (0.11 higher to 0.68 higher) | ‐ | 104 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 1 split‐mouth studies were included |
| Clinical attachment level change Follow‐up: range 6 months to 12 months | The mean clinical attachment level change ranged from 2.47 to 2.80 mm | MD 0.37 mm higher (0.09 lower to 0.83 higher) | ‐ | 104 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 1 split‐mouth studies were included |
| Keratinized tissue width change Follow‐up: range 6 months to 12 months | The mean keratinized tissue width change ranged from ‐0.30 to ‐0.51 mm | MD 0.44 mm higher (0.04 higher to 0.85 higher) | ‐ | 104 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | 1 parallel‐design and 1 split‐mouth studies were included |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAF: coronally advanced flap; CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; OR: odds ratio; VAS: visual analogue scale; XCM: xenogeneic collagen matrix. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| 1Downgraded 1 level for inconsistency and 1 level for imprecision. | ||||||
Background
Description of the condition
Gingival recession is a term that designates the oral exposure of the root surface due to a displacement of the gingival margin apical to the cemento‐enamel junction (Camargo 2001; Wennström 1996). Reports from diverse epidemiological surveys revealed that gingival recession may affect most of the adult population (Richmond 2007; Susin 2004; Thomson 2006). The development of a gingival recession may be associated to diverse aetiological factors (Camargo 2001; Chambrone 2003; Khocht 1993; Yoneyama 1988), such as: a) disease‐related factors (i.e. plaque‐induced periodontal disease (Löe 1992; Yoneyama 1988) and viruses (Pini Prato 2002)); b) inadequate dental procedures (i.e. presence of composite/prosthetic restorations invading the biological width (Donaldson 1973; Parma‐Benefati 1985)); c) tooth and periodontal anatomical features (i.e. inadequate tooth alignment (Stoner 1980), presence of muscle inserts close to margin of gingiva (Camargo 2001), lack of an adequate band of attached keratinized gingiva (Chambrone 2016; Tenenbaum 1982), and the reduced buccal‐lingual thickness of the alveolar bone plate (Steiner 1981; Wennström 1987)); and d) trauma‐factors (i.e. presence of lip/tongue piercings (Chambrone 2003) and incorrect toothbrushing procedures (Khocht 1993; Smukler 1984)). Gingival recession is also regularly linked to the deterioration of dental aesthetics as well as buccal cervical dentine hypersensitivity (Chambrone 2006; Chambrone 2016). In such cases, the goals of periodontal therapy should be to address the needs and wishes of each patient, and treatment options should be made available to them (Caffesse 1995).
Description of the intervention
Preferably, treatment options should be based on systematic, unbiased and objective evaluations of the literature (McGuire 1995). Moreover, the introduction of specific objectives, inclusion criteria and search strategies based on evidence and scientifically valid information may reduce the variation in clinical outcomes, establish the application and predictability of a specific procedure and improve the effectiveness of clinical practice (McGuire 1995). Consequently, scientific evidence‐based information should be achieved by well delineated systematic reviews (Needleman 2002).
Currently, successful treatment of recession‐type defects is based on the use of clinically predictable root coverage periodontal plastic surgery (RCPPS) procedures. As first proposed by Miller in 1988, the term periodontal plastic surgery comprises different surgical techniques intended to correct and prevent anatomical, developmental, traumatic or plaque disease‐induced defects of the gingiva, alveolar mucosa or bone (AAP 1996).
Historically, these procedures originated at the beginning of the 20th century, presented by Younger in 1902, Harlan in 1906 and Rosenthal in 1911 (Baer 1981) who first described the use of pedicle or free soft tissue grafts to cover denuded root surfaces. However, these techniques were abandoned for a long time. During recent decades, different surgical procedures were proposed. Coronally advanced flaps, laterally repositioned flaps, free gingival grafts and subepithelial connective tissue grafts appeared as novel approaches to achieve improvements in recession depth, clinical attachment level and width of keratinized tissue (Bernimoulin 1975; Björn 1963; Cohen 1968; Grupe 1956; Grupe 1966; Harris 1992; Harvey 1965; Harvey 1970; Langer 1985; Nabers 1966; Patur 1958; Sullivan 1968; Sumner 1969; Wennström 1996). Concomitantly, in the mid1980s Miller's classification of recession defects (Miller 1985) appeared as an adequate and useful tool providing surgical predictability, especially for the correction of Class I and II recession (e.g. defects without loss of interproximal bone or soft tissue).
Why it is important to do this review
Different systematic reviews and overviews of systematic reviews have been published focusing on the effect of RCPPS procedures on the treatment of localised gingival recessions (Buti 2013; Chambrone 2008; Chambrone 2010b; Chambrone 2012; Chambrone 2015; Oates 2003; Pini Prato 2014; Roccuzzo 2002). These authors reported that different surgical techniques and flap designs had been described and used in an attempt to correct localised gingival recessions producing statistically significant improvements in gingival recession, clinical attachment level and in the width of keratinized tissue band (when indicated). Also, it was recommended for clinical practice that when root coverage is indicated, subepithelial connective tissue grafts, should be considered as the 'gold standard' procedures (Buti 2013; Chambrone 2008; Chambrone 2010b; Chambrone 2012; Chambrone 2015; Oates 2003; Pini Prato 2014; Roccuzzo 2002). Moreover, the use of other biomaterials of allogenous (i.e. adermal matrix grafts (Woodyard 2004)); xenogenous (i.e. collagen membranes (Roccuzzo 1996; Zucchelli 1998), enamel matrix derivative (Del Pizzo 2005) and collagen bilayer matrix (McGuire 2016)) has been broadly studied since the late 1990s to treat gingival recession.
The previous version of this Cochrane Review (Other published versions of this review) endorsed these outcomes, and also emphasised the importance of subepithelial connective tissue grafts in improving the keratinized tissue band to maintain the results achieved with therapy long term. Also, it was highlighted and demonstrated the importance of the different surgical techniques as an important tool in clinical decision making. This review is an update of the original version that was published in 2009 (Chambrone 2009b).
Objectives
To evaluate the efficacy of different root coverage procedures in the treatment of localised and multiple recession‐type defects.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) only of at least 6 months' duration and reporting patient‐based analysis.
Types of participants
Studies were included if the participants met the following criteria.
A clinical diagnosis of localised or multiple recession‐type defects.
Recession areas selected for treatment classified as Miller's (Miller 1985) Class I (marginal tissue recession not extending to the mucogingival junction and no loss of interproximal bone or soft tissue) or Class II (marginal tissue recession extending to or beyond the mucogingival junction and no loss of interproximal bone or soft tissue) of at least 3 mm, and that were surgically treated by means of periodontal plastic surgery (PPS) procedures. Studies including Miller's Class III (marginal tissue recession extending to or beyond the mucogingival junction with loss of bone or soft tissue, apical to the cemento‐enamel junction but coronal to the level of the recession defect), Class IV (marginal tissue recession extending to or beyond the mucogingival junction with loss of bone or soft tissue apical to the level of the recession defect), and restored root surfaces were not included.
At least 10 participants per group at final examination.
Types of interventions
The interventions of interest were:
free gingival grafts (FGG);
laterally positioned flap (LPF);
coronally advanced flap (CAF);
subepithelial connective tissue grafts (SCTG) alone or in combination with LPF or CAF;
CAF in association with allograft (e.g. acellular dermal matrix grafts (ADMG), others), guided tissue regeneration (GTR), enamel matrix protein (EMP), xenogeneic matrix grafts (XMG) or other biomaterial.
In addition, RCTs comparing variations of the same procedure (e.g. CAF with vertical incisions versus CAF without vertical incisions, etc.) were also considered eligible for inclusion in the review.
Types of outcome measures
Primary outcomes
Aesthetic condition change related to patient's opinion (satisfactory, non‐satisfactory or not reported, or using standardised methods of assessment (i.e. visual analogue scale (VAS)).
Number and percentage of sites with complete root coverage, and gingival recession depth change (mm).
Secondary outcomes
Clinical attachment level change (mm).
Keratinized tissue width change (mm).
Mean root coverage (%).
Patients' preference for a specific PPS procedure (in split‐mouth trials).
Occurrence of adverse effects (yes/no) or postoperative complications (yes/no) or both.
In addition, we separated outcome measures into short term (as evaluated 6 months to 12 months following interventions), medium term (13 months to 59 months) or long term (60 or more months (≥ 5 years)).
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials without language or publication status restrictions:
Cochrane Oral Health's Trials Register (searched 15 January 2018) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 12) in the Cochrane Library (searched 15 January 2018) (Appendix 2);
MEDLINE Ovid (1946 to 15 January 2018) (Appendix 3);
Embase Ovid (1980 to 15 January 2018) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
The following trial registries were searched for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 15 January 2018) (Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 15 January 2018) (Appendix 6).
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
Details regarding screening of titles, abstracts, and full texts of papers published until October 2008 were reported previously (Chambrone 2009b; Chambrone 2010). Identification of studies conducted from November 2008 to January 2018 were similarly performed by two independent review authors (Leandro Chambrone (LC) and Maria Aparecida Salinas Ortega (MASO)) who independently screened titles, abstracts and full texts of the search results. The search was designed to be sensitive and include controlled clinical trials, these were filtered out early in the selection process if they were not randomised. Agreement between review authors was assessed calculating Kappa scores. The review authors remained unblinded regarding the author(s), their institutional affiliations and the site of publication of reports. The full report was obtained for all studies appearing to meet the inclusion criteria or in instances where there was insufficient information from the title, keywords and abstract to make a clear decision. Both review authors assessed all studies independently for eligibility. Disagreement between the review authors was resolved by discussion with the inclusion of another review author (Roberto Rotundo (RR)). In case of missing data, authors were contacted to resolve eventual doubts and provide further details from the trial. Data were excluded until further clarification was available if agreement could not be reached. The studies meeting the inclusion criteria underwent validity assessment and data extraction. We recorded studies rejected at this or subsequent stages in a table of excluded studies.
Data extraction and management
For this update LC and MASO independently and in duplicate extracted data using specially designed data extraction forms.
Data were extracted and loaded onto Review Manager 5 software (Review Manager 2014) and checked. Data on the following issues were extracted and recorded:
citation, publication status and year of publication;
location of trial: country and place where the patients were treated (e.g. private practice or university dental hospitals);
study design: randomised controlled trial;
characteristics of participants: sample size, gender, age, local and systemic conditions;
methodological quality of trials: patient/defect selection bias, selection of a control group, adequate inclusion criteria, statistical analysis, randomisation selection, validity of conclusions and clinical variables analysed;
characteristics of interventions: 1) free gingival grafts (FGG); 2) laterally positioned flap (LPF); 3) coronally advanced flap (CAF); 4) subepithelial connective tissue grafts (SCTG) alone or in combination with LPF or CAF; or 5) CAF in association with acellular dermal matrix grafts (ADMG), guided tissue regeneration (GTR), enamel matrix protein (EMP), xenogeneic matrix grafts (XMG) or other biomaterial;
source of funding and conflict of interest.
We contacted trial authors when necessary for clarification of data or, where possible, to obtain missing data. We excluded data until further clarification was available if agreement could not be reached.
Assessment of risk of bias in included studies
Two review authors (LC and MASO) independently assessed the risk of bias of each included study using the Cochrane domain‐based, two‐part tool as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We contacted study authors for clarification or missing information where necessary and feasible. We resolved any disagreements through discussion, consulting a third review author to achieve consensus when necessary.
We completed a 'Risk of bias' table for each included study. For each domain of risk of bias, we first described what was reported to have happened in the study. This provided the rationale for our judgement of whether that domain was at low, high, or unclear risk of bias.
We assessed the following domains:
sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessment (detection bias);
incomplete outcome data (attrition bias);
selective outcome reporting (reporting bias);
other bias.
We categorised the overall risk of bias of individual studies. Studies were categorised as being at low, high, or unclear risk of bias according to the following criteria:
low risk of bias (plausible bias unlikely to seriously alter the results) if all domains were at low risk of bias;
high risk of bias (plausible bias that seriously weakens confidence in the results) if one or more domains were at high risk of bias; or
unclear risk of bias (plausible bias that raises some doubt about the results) if one or more domains were at unclear risk of bias.
These assessments are reported in the Characteristics of included studies table and also graphically.
Data synthesis
We collated data into evidence tables and grouped them according to type of intervention. Descriptive summary was performed to determine the quantity of data, checking further for study variations in terms of study characteristics, study quality and results. This assisted in confirming the similarity of studies and suitability of further synthesis methods, including possible meta‐analysis.
We used random‐effects meta‐analyses throughout. For continuous data, we expressed pooled outcomes as weighted mean differences (MD) with their associated 95% confidence intervals (CI). For dichotomous data, these were predominately pooled odds ratios (OR) and associated 95% CI. The analyses were conducted using the generic inverse variance statistical method where the MD or log[OR] and standard error (SE) are entered for all studies. We used the Becker‐Balagtas method (Stedman 2011) to calculate log ORs, as indicated by Curtin 2002 to accommodate data pooling from split‐mouth and parallel‐group studies in a single meta‐analysis, and facilitate data synthesis (Stedman 2011). For split‐mouth trials it was assumed a intracluster correlation co‐efficient of 0.05, while for parallel trials a co‐efficient of 0 for the calculation of SE. Statistical heterogeneity was assessed by calculation of the Q statistic. We performed analyses using Review Manager software (Review Manager 2014).
Variance imputation methods were conducted to estimate appropriate variance estimates in some split‐mouth studies, where the appropriate standard deviation of the differences was not included in the trials (Follmann 1992). The significance of discrepancies in the estimates of the treatment effects from the different trials was assessed by means of Cochran's test for heterogeneity and the I2 statistic.
Publication bias
Publication bias would be investigated, especially as its presence was detected in a previous review (Roccuzzo 2002), by graphical methods and via the Begg and Mazumdar (Begg 1994) adjusted rank correlation test and the Egger regression asymmetry test (Egger 1997). However, the available number of studies and heterogeneity of reported procedures prevented such evaluation.
Summary of findings
We produced 'Summary of findings' tables for our main comparisons on single recession defects involving the 'gold‐standard' procedure (i.e. SCTG‐based procedures versus other root coverage procedures) (Buti 2013; Chambrone 2008; Chambrone 2009b; Chambrone 2010; Chambrone 2010b; Chambrone 2012; Chambrone 2015; Oates 2003; Pini Prato 2014; Richardson 2015; Roccuzzo 2002; Tatakis 2015) and the currently used alternative approaches (i.e. CAF, CAF + ADMG, CAF + enamel matrix derivative (EMD) and CAF + xenogeneic collagen matrix (XCM) indicated by the American Academy of Periodontology (Chambrone 2015; Richardson 2015; Tatakis 2015) for the following outcomes: aesthetic condition change related to patient's opinion, sites with complete root coverage, gingival recession depth change; clinical attachment level change; and keratinized tissue width change.
We used GRADE methods (GRADE 2004), and the GRADEproGDT online tool for developing 'Summary of findings' tables (gradepro.org/). We assessed the quality of the body of evidence for each comparison and outcome by considering the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates, and the risk of publication bias. We categorised the quality of each body of evidence as high, moderate, low, or very low.
Results
Description of studies
Results of the search
A total of 1714 records were retrieved from the electronic searches. After the removal of duplicates, 724 records were screened for eligibility. 530 records were discarded, and the full‐texts of 194 articles were assessed. From the 194 papers, 137 did not meet the criteria of eligibility and the reasons for exclusion were reported in the Characteristics of excluded studies table. 48 studies (reported in 57 papers) were included in the review, with 20 providing data for meta‐analyses (Figure 1). Kapa scores for the searches conducted up to 2008 are described in the previous version of this review (Chambrone 2009b). Kappa scores for inter‐reviewer agreement for title or abstract review or both, and full texts screening were 0.88 (95% confidence interval (CI) 0.83 to 0.94) and 0.87 (95% CI 0.75 to 0.99), respectively.
1.
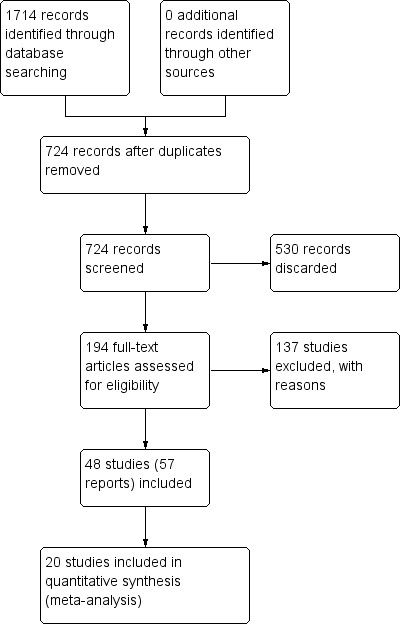
Study flow diagram.
Included studies
We included 48 randomised controlled trials (RCTs) reported in 57 papers in this review. Nine RCTs had their data reported in two articles each (i.e. according to the follow‐up period or type of data (i.e. clinical or patient‐reported outcomes). Consequently, the papers with a shorter follow‐up period were included under the one study name (e.g. papers with the longer follow‐up) (Costa 2016; de Queiroz 2006; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Rosetti 2013; Spahr 2005), while one article reporting patient‐reported outcomes was included under the name of the clinical outcomes paper (Sangiorgio 2017).
Out of the 48 included RCTs, 28 trials were conducted according to a split‐mouth design (Abolfazli 2009; Ayub 2012; Babu 2011; Barros 2015; Costa 2016; da Silva 2004; de Queiroz 2006; Del Pizzo 2005; Dodge 2000; Henderson 2001; Jankovic 2010; Jepsen 2013; Joly 2007; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Öncü 2017; Reino 2012; Reino 2015; Roccuzzo 1996; Rosetti 2013; Spahr 2005; Trombelli 1996; Tunali 2015; Wang 2001; Zucchelli 2003; Zucchelli 2009), and 20 according to a parallel design (Ahmedbeyli 2014; Bouchard 1994; Bouchard 1997; Jaiswal 2012; Keceli 2008; Keceli 2015; Matarasso 1998; Ozenci 2015; Paolantonio 1997; Paolantonio 2002; Paolantonio 2002b; Pendor 2014; Rasperini 2011; Sangiorgio 2017; Shori 2013; Tozum 2005; Woodyard 2004; Zucchelli 1998; Zucchelli 2014; Zucchelli 2014b). In total, 1227 patients were treated and all studies were published in full.
Eight RCTs were private practice based (Abolfazli 2009; Bouchard 1994; Bouchard 1997; Dodge 2000; McGuire 2012; McGuire 2014; McGuire 2016; Paolantonio 1997), 35 were based in universities or dental hospitals (Ahmedbeyli 2014; Ayub 2012; Babu 2011; Barros 2015; Costa 2016; da Silva 2004; de Queiroz 2006; Henderson 2001; Jaiswal 2012; Jankovic 2010; Joly 2007; Keceli 2008; Keceli 2015; Leknes 2005; Matarasso 1998; Öncü 2017; Ozenci 2015; Paolantonio 2002; Paolantonio 2002b; Pendor 2014; Reino 2012; Reino 2015; Roccuzzo 1996; Rosetti 2013; Shori 2013; Tozum 2005; Trombelli 1996; Tunali 2015; Wang 2001; Woodyard 2004; Zucchelli 1998; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b), and five were multicentre studies (Del Pizzo 2005; Jepsen 2013; Rasperini 2011; Sangiorgio 2017; Spahr 2005).
Thirteen trials were conducted in Italy (Del Pizzo 2005; Matarasso 1998; Paolantonio 1997; Paolantonio 2002; Paolantonio 2002b; Rasperini 2011, Roccuzzo 1996; Trombelli 1996; Zucchelli 1998; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b), 10 in Brazil (Ayub 2012; Barros 2015; Costa 2016; da Silva 2004; de Queiroz 2006; Joly 2007; Reino 2012; Reino 2015; Rosetti 2013; Sangiorgio 2017), seven in USA (Dodge 2000; Henderson 2001; McGuire 2012; McGuire 2014; McGuire 2016; Wang 2001; Woodyard 2004), seven in Turkey (Ahmedbeyli 2014; Keceli 2008; Keceli 2015; Öncü 2017; Ozenci 2015; Tozum 2005; Tunali 2015), four in India (Babu 2011; Jaiswal 2012; Pendor 2014; Shori 2013), two in France (Bouchard 1994; Bouchard 1997), one in Germany (Spahr 2005), one in Iran (Abolfazli 2009), one in Norway (Leknes 2005), one in Serbia (Jankovic 2010), and one in multiple countries: Germany, Italy, Sweden and Spain (Jepsen 2013).
Nine trials were supported, totally or in part, by governmental agencies or university programs (Ayub 2012; Keceli 2008; Paolantonio 2002; Paolantonio 2002b; Reino 2012; Reino 2015; Rosetti 2013; Sangiorgio 2017; Trombelli 1996), and 10 by companies who sponsored or provided products or both that were used as interventions in the RCTs (Ayub 2012; Henderson 2001; Jepsen 2013; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Reino 2015; Spahr 2005; Wang 2001).
Five studies evaluated multiple recession‐type defects (Ahmedbeyli 2014; Jaiswal 2012; Öncü 2017; Ozenci 2015; Tunali 2015), whereas the others single gingival recessions. Two studies (Costa 2016; Reino 2012) evaluated exclusively outcomes of smokers (i.e. 10 or more cigarettes per day for more than 5 years). In addition, the majority of trials followed participants during a short‐term period (6 months to 12 months). Only five publications with medium‐term follow‐up (Abolfazli 2009; Del Pizzo 2005; de Queiroz 2006; Rosetti 2013; Spahr 2005) and five with long‐term follow‐up (Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Paolantonio 1997) were included.
Treatment modalities
Different interventions have been evaluated: free gingival grafts (FGG), coronally advanced flap (CAF) alone or associated to acellular dermal matrix grafts (ADMG), enamel matrix protein (EMP), guided tissue regeneration with resorbable membranes (GTR rm), guided tissue regeneration with non‐resorbable membranes (GTR nrm), GTR rm associated with bone substitutes, platelet‐rich plasma or fibrin (PRP or PRF), growth factors (rhPDGF‐BB) associated to bone substitutes (b‐TCP), subepithelial connective tissue grafts (SCTG) or xenogeneic collagen matrix (XCM). We did not find any RCTs evaluating laterally positioned flaps (LPF).
Excluded studies
We excluded 137 studies, 28 on the grounds that they were not randomised controlled trials (Berlucchi 2005; Daniel 1990; Dembowska 2007; Erley 2006; Gunay 2008; Gupta 2006; Harris 1997; Harris 2000; Harris 2002; Harris 2005; Hirsch 2005; Jovicic 2013; Moses 2006; Muller 1998; Muller 1999; Nemcovsky 2004; Pini Prato 1992; Pini Prato 1996; Pini Prato 1999; Pini Prato 2005; Sallum 2003; Sbordone 1988; Scabbia 1998; Schlee 2011; Trombelli 1995; Trombelli 1997; Trombelli 2005; Wennström 1996).
One hundred and nine papers were classified as randomised trials; however, they did not fulfil the inclusion criteria. 77 articles included patients with recession defects < 3 mm (Abou‐Arraj 2017; Aichelmann Reidy 2001; Alexiou 2017; Alkan 2011; Alkan 2013; Andrade 2008; Aroca 2009; Aroca 2013; Azaripour 2016; Bajic 2014; Bansal 2016; Berlucchi 2002; Bherwani 2014; Bittencourt 2006; Bittencourt 2009; Borghetti 1999; Bozkurt Dogan 2015; Byun 2009; Caffesse 2000; Cairo 2016; Cardaropoli 2009; Cardaropoli 2012; Cardaropoli 2014; Castellanos 2006; Cheung 2004; Cordaro 2012; Cortellini 2009; Deshpande 2014; Dilsiz 2010; Dilsiz 2010b; Felipe 2007; Fernandes‐Dias 2015; Gholami 2013; Griffin 2009; Haghighati 2009; Han 2008; Huang 2005; Jahnke 1993; Jain 2017; Jankovic 2012; Jepsen 1998; Jepsen 2017; Jhaveri 2010; Kennedy 1985; Kuis 2013; Köseoglu 2013; Lins 2003; M 2016; Mazzocco 2011; Modica 2000; Moka 2014; Moslemi 2011; Nazareth 2011; Ozcelik 2011; Ozturan 2011; Pilloni 2006; Pini Prato 2011; Pourabbas 2009; Rebele 2014; Ricci 1996; Roman 2013; Salhi 2014; Santana 2010; Santana 2010b; Santamaria 2017; Santamaria 2017b; Singh 2015; Stefanini 2016; Tatakis 2000; Thombre 2013; Trabulsi 2004; Trombelli 1998; Wang 2014; Wang 2015; Zucchelli 2010; Zucchelli 2012; Zuhr 2013).
Five articles did not present a patient‐based analysis (Barros 2004; Barros 2005; Cetiner 2003; Cordioli 2001; Rahmani 2006) and two included both single and multiple recessions in the analyses (Milinkovic 2015; Ricci 1996b). Studies including Miller's Class III or Class IV recessions (Andrade 2010; Borghetti 1994), a follow‐up period < 6 months (Baghele 2012; Lafzi 2007), patients under 18 years of age (Mahajan 2012), interventions not of interest for this review (Wilson 2005; Yilmaz 2014) and that had counted less than 10 participants per group at final examination (Burkhardt 2005; Kimble 2004; Mahajan 2007; Tal 2002; Trombelli 1995b) were excluded as well.
The remaining papers were excluded due to the combination of two or more factors such as the treatment of recession < 3 mm and a follow‐up period < 6 months (Laney 1992; Pini Prato 2000); less than 10 patients per group at final examination and patient‐based analysis not presented (Banihashemrad 2009); inclusion of patients with recession depth < 3 mm, patient‐based analysis not presented (Khobragade 2016; Kumar 2017; Uzun 2018) and patients with Miller's Class III recessions (Ghahroudi 2013); inclusion of both single and multiple defects in the estimates and defects < 3 mm (Gobbato 2016); inclusion of gingival recession < 3 mm and defects not classified according to the Miller Classification System (Tonetti 2018); and less than 10 patients per group at final examination, recessions < 3 mm and patient‐based analysis not presented (Duval 2000; Ito 2000).
In addition, the author from one study was contacted to resolve doubts and provide further details from her trial (Romagna‐Genon 2001). However, this author did not provide the requested explanations, consequently, her paper was excluded from the review.
Risk of bias in included studies
Risk of bias in the included studies was evaluated using the data extracted from each trial (Figure 2; Figure 3). Moreover, all authors were contacted to provide complementary information by means of a questionnaire regarding the methodological quality of their trials.
2.
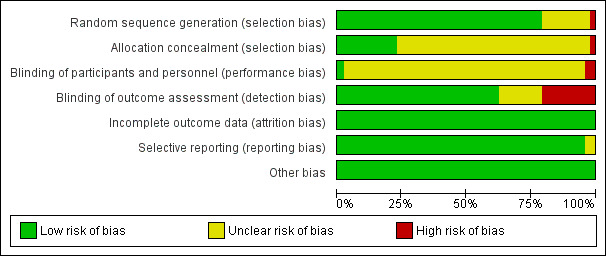
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
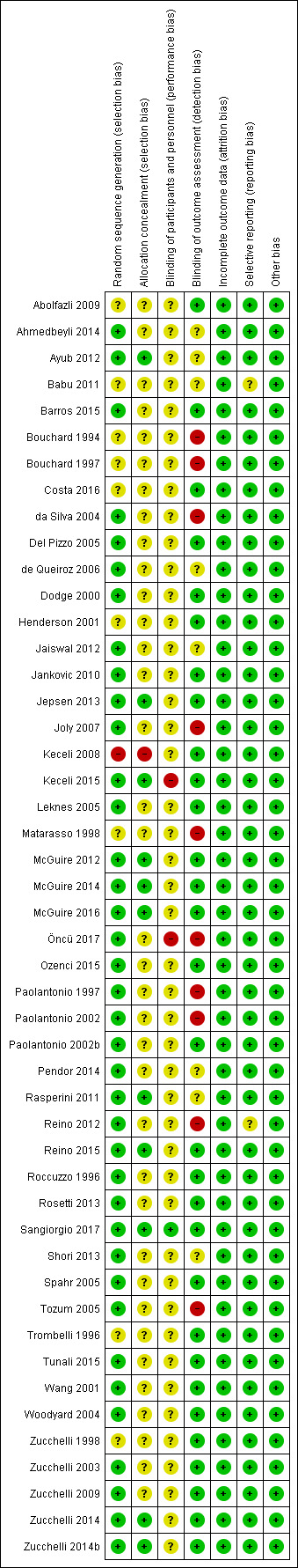
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
One study was assessed as at low overall risk of bias (Sangiorgio 2017), whereas 35 as at unclear overall risk of bias (Abolfazli 2009; Ahmedbeyli 2014; Ayub 2012; Babu 2011; Barros 2015; Costa 2016; Del Pizzo 2005; de Queiroz 2006; Dodge 2000; Henderson 2001; Jaiswal 2012; Jankovic 2010; Jepsen 2013; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Ozenci 2015; Paolantonio 2002b; Pendor 2014; Rasperini 2011; Reino 2015; Roccuzzo 1996; Rosetti 2013; Shori 2013; Spahr 2005; Trombelli 1996; Tunali 2015; Wang 2001; Woodyard 2004; Zucchelli 1998; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b), and 12 as at high overall risk of bias (Bouchard 1994; Bouchard 1997; da Silva 2004; Joly 2007; Keceli 2008; Keceli 2015; Matarasso 1998; Öncü 2017; Paolantonio 1997; Paolantonio 2002; Reino 2012; Tozum 2005).
Sequence generation
All the trials were described as RCTs, but not all reported randomisation and allocation methods in detail. Thirty‐eight trials (Ahmedbeyli 2014; Ayub 2012; Barros 2015; da Silva 2004; de Queiroz 2006; Del Pizzo 2005; Dodge 2000; Jaiswal 2012; Jankovic 2010; Jepsen 2013; Joly 2007; Keceli 2015; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Öncü 2017; Ozenci 2015; Paolantonio 1997; Paolantonio 2002; Paolantonio 2002b; Pendor 2014; Rasperini 2011; Reino 2012; Reino 2015; Roccuzzo 1996; Rosetti 2013; Sangiorgio 2017; Shori 2013; Spahr 2005; Tunali 2015; Wang 2001; Woodyard 2004; Tozum 2005; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b) presented an adequate method of randomisation, while one reported an inadequate method (Keceli 2008). In nine, the method of randomisation was considered unclear (Abolfazli 2009; Babu 2011; Bouchard 1994; Bouchard 1997; Costa 2016; Henderson 2001; Matarasso 1998; Trombelli 1996; Zucchelli 1998).
Allocation (selection bias)
Only 11 trials presented an adequate method of allocation concealment (Ayub 2012; Keceli 2015; Jepsen 2013; McGuire 2012; McGuire 2014; McGuire 2016; Rasperini 2011; Reino 2015; Sangiorgio 2017; Zucchelli 2014; Zucchelli 2014b). One trial reported an inadequate method of allocation concealment (Keceli 2008). All other trials were classified as unclear because the method of allocation was not described (Characteristics of included studies table).
Blinding (performance bias and detection bias)
Examiners were considered blinded in 30 studies (Abolfazli 2009; Barros 2015; Costa 2016; Del Pizzo 2005; Dodge 2000; Henderson 2001; Jankovic 2010; Jepsen 2013; Keceli 2008; Keceli 2015; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Ozenci 2015; Paolantonio 2002b; Reino 2015; Roccuzzo 1996; Rosetti 2013; Sangiorgio 2017; Spahr 2005; Trombelli 1996; Tunali 2015; Wang 2001; Woodyard 2004; Zucchelli 1998; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b), not blinded in ten studies (Bouchard 1994; Bouchard 1997; da Silva 2004; Joly 2007; Matarasso 1998; Öncü 2017; Paolantonio 1997; Paolantonio 2002; Reino 2012; Tozum 2005), and unclear in eight studies (Ahmedbeyli 2014; Ayub 2012; Babu 2011; de Queiroz 2006; Jaiswal 2012; Pendor 2014; Rasperini 2011; Shori 2013). Blindness of participants/patients was considered unclear for all the included trials, except for two trials (Keceli 2015; Öncü 2017) where the patients were considered not blinded to the surgical procedure and for Sangiorgio 2017 who reported that patients remained masked regarding which treatment they received
Whilst authors from three trials (Paolantonio 1997; Paolantonio 2002; Tozum 2005) have responded to the review enquiry (i.e. questionnaire regarding the methodological quality of each trial) that their study had blinded examiners, in practical terms this might have been impossible to achieve with very different interventions (i.e. SCTG versus free gingival grafts, GTR rm versus GTR rm with bone substitutes versus SCTG and modified tunnel procedures + SCTG versus SCTG + CAF). Consequently, where the intervention was very different and where the examiner could therefore guess the group allocation, the study was interpreted to be not blinded.
Incomplete outcome data (attrition bias), selective reporting (reporting bias), and potential sources of bias
Only seven studies (Costa 2016; Keceli 2008; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Spahr 2005) reported withdrawals and dropouts (see Characteristics of included studies table). Overall, all studies were at low risk of bias for this domain. Selective reporting was considered low for the majority of studies, except for two RCTs (Babu 2011; Reino 2012). In the first trial (Babu 2011) between‐groups comparisons regarding baseline recession depth were not reported (control group (SCTG): 4.00 mm; test group (GTRs): 4.50 mm). In the second trial (Reino 2012) baseline and follow‐up means regarding recession depth, clinical attachment level and keratinized tissue width were not reported in the study. Other sources of bias were not identified within all the included trials.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6
See Table 1; Table 2; Table 3; Table 4; Table 5; Table 6.
Aesthetic condition change, gingival recession depth change, clinical attachment level change and keratinized tissue width change
Aesthetic condition change related to patient's opinion was reported in 10 RCTs (Ahmedbeyli 2014; Bouchard 1994; McGuire 2012; McGuire 2014; McGuire 2016; Ozenci 2015; Rosetti 2013; Zucchelli 2003; Zucchelli 2014; Zucchelli 2014b). Given the heterogeneity of methods/criteria used to assess this outcome and types of procedures compared, formal pooling of data via meta‐analysis was precluded. Therefore, the individual studies results' are depicted below under the appropriate pooled estimates/comparisons or at Additional Table 7.
1. Outcome changes of trials not incorporated into meta‐analyses.
| Study | Interventions | MD RD decrease (95% CI) | MD CAL gain (95% CI) | MD KTW gain (95% CI) | Aesthetic condition change |
| Ahmedbeyli 2014 | ADMG + CAF | 3.08 (2.79 to 3.37)a, b | 2.74 (2.44 to 3.06)a, b | 1.21 (1.08 to 1.34)a, b | The authors asked each patient about different patient‐reported outcomes (i.e. root coverage attained, colour of gums, shape and contour of gums), and both procedures were rated equally in all aspects |
| CAF | 2.37 (1.90 to 2.84)a | 2.17 (1.71 to 2.63)a | 0.60 (0.40 to 0.80)a | ||
| Ayub 2012 | ADMG (positioned 1 mm apical to the CEJ) + CAF (extended flap) | 2.92 (2.73 to 3.11)a, b | 3.07 (2.70 to 3.44)a, b | 1.07 (0.82 to 1.32)a | Not reported |
| ADMG + CAF (extended flap) | 2.18 (2.00 to 2.36)a | 2.01 (1.73 to 2.29)a | 0.93 (0.59 to 1.27)a | ||
| Babu 2011 | GTR (collagen membrane) + CAF | 3.80 (3.25 to 4.35)a | Not reported | 1.50 (1.07 to 1.93)a | Not reported |
| SCTG + CAF | 3.40 (2.85 to 3.95)a | Not reported | 2.30 (1.88 to 2.72)a | ||
| Bouchard 1994 | SCTG + CAF + citric acid (graft without epithelial collar) | 2.93 (NA)a | 2.74 (NA)a | 1.00 (NA)a | Aesthetic evaluation was performed by 2 independent examiners who were blinded to the given treatment. Additionally, the authors commented that no patient was dissatisfied with the aesthetical results obtained |
| SCTG (graft with epithelial collar) | 2.93 (NA)a | 2.86 (NA)a | 0.93 (NA)a | ||
| Bouchard 1997 | SCTG + CAF + tetracycline hydrochloride | 3.80 (NA)a | 2.66 (NA)a | 1.00 (NA)a | Not reported |
| SCTG + CAF + citric acid | 3.47 (NA)a | 3.20 (NA)a | 0.93 (NA)a | ||
| Costa 2016 | ADMG + EMD + CAF (6 months) | 1.94 (1.45 to 2.43)a, b | 1.35 (0.90 to 1.80)a | 1.61 (1.03 to 2.19)a | Not reported |
| ADMG + CAF (6 months) | 1.52 (1.18 to 1.86)a | 1.07 (0.84 to 1.30)a | 1.55 (1.11 to 1.99)a | ||
| ADMG + EMD + CAF (12 months) | 2.17 (1.64 to 2.70)a, b | 1.64 (1.06 to 2.22)a | 1.61 (1.10 to 2.12)a | ||
| ADMG + CAF (12 months) | 1.83 (1.49 to 2.17)a | 1.43 (0.98 to 1.88)a | 1.63 (1.14 to 2.12)a | ||
| da Silva 2004 | SCTG + CAF | 3.16 (2.65 to 3.67)a | 2.53 (1.86 to 3.20)a | 0.55 (0.01 to 1.09)a, b | Not reported |
| CAF | 2.73 (2.14 to 3.32)a | 2.30 (1.68 to 2.92)a | ‐0.21 (‐0.58 to 0.16) | ||
| Henderson 2011 | ADMG (basement membrane side against the tooth) + CAF | 3.95 (2.59 to 5.31)a | 4.15 (2.78 to 5.52)a | 0.80 (0.23 to 1.37)# | Not reported |
| ADMG (connective tissue side against the tooth) + CAF | 3.55 (2.89 to 4.21)a | 3.65 (2.75 to 4.55)a | 0.80 (0.09 to 1.51)a | ||
| Jaiswal 2012 | EMD + CAF | 3.40 (2.80 to 4.00)a, b | 3.70 (3.08 to 4.32)a, b | 2.95 (2.60 to 3.30)a | Not reported |
| CAF | 2.81 (2.56 to 3.06)a | 2.79 (2.54 to 3.04)a | 2.66 (2.31 to 3.01)a | ||
| Jankovic 2010 | Platelet‐rich fibrin + CAF | 3.05 (2.72 to 3.38)a | Not reported | 0.17 (0.05 to 0.29) | Not reported |
| EMD + CAF | 2.75 (2.48 to 3.02)a | Not reported | 0.60 (0.42 to 0.78)b | ||
| Keceli 2008 | SCTG + platelet‐rich plasma + CAF | Data not reported in the trial (the results from this study were reported as median values (within‐groups comparisons P < 0.05; between‐groups comparison P > 0.05) | Data not reported in the trial (the results from this study were reported as median values (within‐groups comparisons P < 0.05; between‐groups comparison P > 0.05) | Data not reported in the trial (the results from this study were reported as median values (within‐groups comparisons P < 0.05; between‐groups comparison P > 0.05) | Not reported |
| SCTG + CAF | |||||
| Keceli 2015 | SCTG + platelet‐rich fibrin + CAF | 3.00 (2.78 to 3.22)a, b | 3.10 (2.75 to 3.45)a, b | 1.23 (0.94 to 1.52)a | Not reported |
| SCTG + CAF | 2.55 (2.33 to 2.77) | 2.50 (2.15 to 2.85)a | 0.83 (0.59 to 1.07)a | ||
| Leknes 2005 | GTR (polylactide membrane ‐ Guidor) (6 months) + CAF | 2.00 (1.52 to 2.48)a | 1.30 (0.55 to 2.05)a | 0.50 (0.19 to 0.81) | Not reported |
| CAF (6 months) | 2.30 (1.75 to 2.85)a | 1.50 (0.75 to 2.25)a | 0.40 (0.18 to 0.62)a | ||
| GTR (polylactide membrane ‐ Guidor) (12 months) + CAF | 2.00 (1.52 to 2.48)a | 1.50 (0.80 to 2.20)a | 0.60 (0.32 to 0.88)a | ||
| CAF (12 months) | 2.20 (1.65 to 2.75)a | 1.80 (1.10 to 2.50)a | 0.40 (0.18 to 0.62)a | ||
| GTR (polylactide membrane ‐ Guidor) (72 months) + CAF | 1.40 (0.63 to 2.17) | 1.70 (0.64 to 2.76)a | 0 | ||
| CAF (72 months) | 1.30 (0.53 to 2.07)a | 1.50 (0.41 to 2.59)a | 0 | ||
| Matarasso 1998 | GTR (polylactide membrane ‐ Guidor) + double papilla flap | 3.40 (3.16 to 3.64)a | 3.10 (2.84 to 3.36)a | 2.00 (1.77 to 2.23)a | Not reported |
| GTR (polylactide membrane ‐ Guidor) + CAF | 2.50 (2.22 to 2.78)a | 2.80 (2.50 to 3.10)a | 0.90 (0.49 to 1.31) | ||
| McGuire 2014 | B‐TCP + CD + rhPDGF‐BB + CAF (6 months) | 2.90 (2.71 to 3.09)a | 2.90 (2.71 to 3.09)a | 1.00 (0.81 to 1.19)a | At 6 months, patients aesthetic rating by 10 cm visual analogue scale did not identify differences in the clinical rating of colour/texture of the tissues observed between the treatments. At 5 years, of the 20 test and 20 control sites, "14 sites for each were rated as 'very satisfied.' In the test group, 4 sites were rated as 'satisfied,' 1 as 'unsatisfied,' and 1 as 'very unsatisfied.' In the control group, the remaining 6 sites were rated as 'satisfied' |
| SCTG + CAF (6 months) | 3.30 (3.11 to 3.49)a, b | 2.90 (2.51 to 3.29)a | 1.30 (1.11 to 1.49)a | ||
| B‐TCP + CD + rhPDGF‐BB + CAF (5 years) | 2.35 (1.82 to 2.88)a | 1.95 (1.53 to 2.37)a | 1.00 (0.6 to 1.40)a | ||
| SCTG + CAF (5 years) | 3.05 (2.67 to 3.43)a, b | 2.35 (1.89 to 2.81)a | 1.63 (1.17 to 2.09)a, b | ||
| McGuire 2016 | XCM + CAF (6 months) | 2.62 (2.33 to 2.91)a | 2.28 (1.95 to 2.71)a | 1.34 (0.92 to 1.76)a | Patients rated equivalent aesthetic changes from baseline to 6 months for XCM + CAF versus SCTG + CAF (overall, "for both test and control treatments, > 90% of subjects recorded improvement"). Similarly, approximately 90% of patients (15 XCM + CAF and 16 SCTG + CAF) remained "satisfied or very satisfied" 5 year after root coverage therapy and no statistical difference in satisfaction was reported |
| SCTG + CAF (6 months) | 3.10 (2.91 to 3.29)a, b | 2.70 (2.42 to 2.98)a | 1.26 (0.63 to 1.89)a | ||
| XCM + CAF (12 months) | 2.78 (2.51 to 3.06)a | 2.26 (1.76 to 2.76)a | 1.11 (0.77 to 1.45)a | ||
| SCTG + CAF (12 months) | 3.17 (3.01 to 3.33)a, b | 2.85 (2.59 to 3.11)a, b | 1.09 (0.43 to 1.75)a | ||
| XCM + CAF (5 years) | Not reported | Not reported | Not reported | ||
| SCTG + CAF (5 years) | Not reported | Not reported | Not reported | ||
| Ozenci 215 | ADMG + CAF (tunnel) | 2.45 (2.33 to 2.57)a | 2.33 (2.07 to 2.59)a | 0.87 (0.61 to 1.13)a | A similar overall patient satisfaction was recorded for patients with multiple recession‐type defects treated by ADMG + coronally advanced tunnel flap or ADMG + CAF (without vertical releasing incisions) (P > 0.05) |
| ADMG + CAF (without vertical realising incisions) | 3.10 (2.75 to 3.45)a, b | 2.75 (2.38 to 3.12)a, b | 1.25 (1.1. to 1.40)a, b | ||
| Paolantonio 1997 | SCTG + double papilla flap | 2.85 (2.71 to 2.99)a, b | Not reported | 3.51 (3.28 to 3.74)a | Not reported |
| FGG | 1.61 (1.50 to 1.72)a | Not reported | 3.66 (3.52 to 3.80)a | ||
| Pendor 2014 | SCTG + double papilla flap | 3.80 (2.75 to 4.85)a | 3.80 (2.64 to 4.96)a | 3.80 (2.76 to 4.84)a | Not reported |
| SCTG + CAF | 3.34 (2.91 to 3.77)a | 3.74 (3.27 to 4.21)a | 3.30 (3.00 to 3.60)a | ||
| Rasperini 2011 | SCTG + EMD + CAF | 3.90 (3.59 to 4.21)a | 3.90 (3.63 to 4.17)a | 2.00 (1.62 to 2.38)a | Not reported |
| SCTG + CAF | 3.60 (3.06 to 4.14)a | 3.50 (2.96 to 4.04)a | 2.00 (1.46 to 2.54)a | ||
| Reino 2012 | SCTG + CAF (extended flap) | Not reported | Not reported | Not reported | Not reported |
| SCTG + CAF | Not reported | Not reported | Not reported | ||
| Reino 2015 | XCM + CAF (extended flap) | 2.84 (2.54 to 3.14)a, b | 2.66 (2.20 to 3.12)a | ‐0.03 (‐0.34 to 0.28) | Not reported |
| XCM + CAF | 2.21 (1.95 to 2.47)a | 1.85 (1.41 to 2.29)a | 0.35 (0.03 to 0.67) | ||
| Tozum 2005 | SCTG + modified tunnel procedure | 3.36 (3.03 to 3.69)a, b | 3.93 (3.40 to 4.46)a, b | Not reported | Not reported |
| SCTG + CAF | 2.56 (2.19 to 2.93)a | 2.44 (1.77 to 3.11)a | Not reported | ||
| Trombelli 1996 | CAF + fibrin glue + tetracycline hydrochloride | 2.40 (2.10 to 2.70)a | 2.40 (1.93 to 2.87)a | ‐0.40 (‐0.75 to ‐0.05) | Not reported |
| CAF + tetracycline hydrochloride | 1.80 (1.21 to 2.39)a | 1.90 (1.43 to 2.37)a | ‐0.5 (‐1.21 to 0.21) | ||
| Zucchelli 2003 | SCTG (graft size equal to the bone dehiscence) + CAF | 3.90 (3.54 to 4.26)a | 3.90 (3.55 to 4.25)a, b | 2.30 (2.00 to 2.60)a | The results obtained at the 12‐month follow‐up visit showed that patients were more satisfied with the appearance of test‐treated recessions (i.e. graft dimension equal to the depth of the bone dehiscence), as well as, less satisfied with poor colour blending and excessive thickness of the control‐treated recessions (i.e. graft dimension 3 mm greater than the depth of the bone dehiscence) |
| SCTG (graft size 3 mm greater than the bone dehiscence) + CAF | 3.60 (3.24 to 3.96)a | 3.10 (2.73 to 3.47)a | 3.30 (2.94 to 3.66)a, b | ||
| Zucchelli 2009 | Ultrasonic scaling + CAF | 3.18 (2.74 to 3.62)a | 2.90 (2.49 to 3.31)a | 0.36 (‐0.04 to 0.76)a | Not reported |
| Manual/hand scaling + CAF | 3.54 (3.06 to 4.02)a | 3.36 (2.82 to 3.90)a | 0.55 (0.24 to 0.86)a | ||
| Zucchelli 2014 | SCTG (de‐epithelialized FGG (graft height of 4 mm and thickness < 2 mm)) + CAF | 3.66 (3.31‐4.02)a | 3.26 (2.97‐3.56)a | 2.17 (1.94 to 2.39)a | Based on a visual analogue scale, the authors did not identify differences in terms of patient root coverage aesthetic assessment 12 months after surgery between sites treated with SCTG (de‐epithelialized FGG (graft height of 4 mm and thickness < 2 mm)) + CAF versus SCTG (de‐epithelialized FGG (graft height > 4 mm and thickness > 2 mm)) + CAF. Overall, both procedures led to high aesthetic results, but colour match scores were higher for patients receiving reduced size grafts (P < 0.01) |
| SCTG (de‐epithelialized FGG (graft height > 4 mm and thickness > 2 mm) + CAF | 3.80 (3.45‐4.14)a | 3.60 (3.23‐4.03)a | 2.50 (2.22‐2.77)a | ||
| Zucchelli 2014b | SCTG + CAF (removal of the labial submucosal tissue) | 3.68 (3.24 to 4.12)a, b | 5.24 (4.55 to 5.93)a | 1.56 (1.13 to 1.99)a | The outcomes achieved with a visual analogue scale did not show differences between procedures in terms of root coverage, but colour match was identified by patients as better when the labial submucosal tissue was removed |
| SCTG + CAF | 3.08 (2.64 to 3.52)a | 4.60 (4.05 to 5.15)a | 2.20 (1.51 to 2.89)a, b |
ADMG: acellular dermal matrix graft; B‐TCP + CD + rhPDGF‐BB: Beta‐tricalcium phosphate + recombinant human platelet‐derived growth factor‐BB with a bioabsorbable collagen wound‐healing dressing; CAF: coronally advanced flap; CAL: clinical attachment level; CEJ: cemento‐enamel junction; CI: confidence interval; EMD: enamel matrix derivative; EMP: enamel matrix protein; FGG: free gingival graft; GR: gingival recession; GTR: guided tissue regeneration; KTW: keratinized tissue width; MD: mean difference; NA: CI are not available or could not be calculated; RD: recession depth; SCTG: subepithelial connective tissue graft; XCM: xenogeneic collagen matrix. aStatistically significant within‐groups. bStatistically significant between‐groups (superior group). cWithin‐group comparisons not evaluated.
Of the 48 included trials, 20 evaluating single and multiple recession‐type defects were included into the following meta‐analyses:
ADMG + CAF versus SCTG + CAF ‐ short term (Barros 2015; Joly 2007; Paolantonio 2002b; Shori 2013);
ADMG + CAF versus CAF ‐ short term (de Queiroz 2006; Woodyard 2004);
EMP + CAF versus CAF ‐ short term (Del Pizzo 2005; Sangiorgio 2017; Spahr 2005);
EMP + CAF versus CAF ‐ short/medium term (Del Pizzo 2005; Sangiorgio 2017; Spahr 2005);
EMP + CAF versus SCTG + CAF ‐ short/medium term (Abolfazli 2009; McGuire 2012);
GTR rm + CAF versus SCTG + CAF ‐ short term (Paolantonio 2002; Wang 2001; Zucchelli 1998);
GTR rm + CAF versus GTR nrm + CAF ‐ short term (Roccuzzo 1996; Zucchelli 1998);
GTR rm associated with bone substitutes + CAF versus SCTG + CAF ‐ short term (Paolantonio 2002; Rosetti 2013);
GTR rm associated with bone substitutes + CAF versus GTR rm + CAF ‐ short term (Dodge 2000; Paolantonio 2002);
XCM + CAF versus CAF ‐ short term (Jepsen 2013; Sangiorgio 2017); and
PRF + CAF versus SCTG + CAF ‐ short term (Öncü 2017; Tunali 2015).
(See Additional Table 8; Table 1; Table 2; Table 3; Table 4; Table 5; Table 6.)
2. Summary of meta‐analyses.
| Comparison | Studies | Outcome | Statistical method | Effect size | Chi2 | P value (Q) | I2 (%) |
| ADMG + CAF versus SCTG + CAF | Barros 2015; Joly 2007; Paolantonio 2002b; Shori 2013 | GR depth change | MD 95% CI | ‐0.36 (‐1.03, 0.30) | 15.06 | 0.002 | 80.0 |
| CAL change | MD 95% CI | ‐0.53 (‐1.14, 0.08) | 9.73 | 0.02 | 69.0 | ||
| KT width change | MD 95% CI | ‐0.59 (‐1.27, 0.10) | 17.17 | 0.0007 | 83.0 | ||
| SCRC | OR 95% CI | 0.43 (0.13, 1.37) | 0.00 | 0.96 | 0 | ||
| ADMG + CAF versus CAF | de Queiroz 2006; Woodyard 2004 | GR depth change | MD 95% CI | 0.61 (‐0.52, 1.73) | 7.45 | 0.006 | 87.0 |
| CAL change | MD 95% CI | 0.51 (‐0.25, 1.27) | 2.32 | 0.13 | 57.0 | ||
| KT width change | MD 95% CI | 0.28 (‐0.08, 0.64) | 0.30 | 0.59 | 0 | ||
| SCRC | OR 95% CI | 3.97 (0.20, 80.50) | 5.03 | 0.02 | 80.0 | ||
| EMP + CAF versus CAF (1) | Del Pizzo 2005; Sangiorgio 2017; Spahr 2005 | GR depth change | MD 95% CI | 0.07 (‐0.25, 0.40) | 5.62 | 0.06 | 64.0 |
| CAL change | MD 95% CI | 0.22 (‐0.02, 0.45) | 1.57 | 0.46 | 0 | ||
| KT width change | MD 95% CI | 0.35 (0.13, 0.56) | 0.64 | 0.73 | 0 | ||
| EMP + CAF versus CAF (2) | Del Pizzo 2005; Sangiorgio 2017; Spahr 2005 | GR depth change | MD 95% CI | 0.32 (0.10, 0.55) | 2.10 | 0.35 | 5.0 |
| CAL change | MD 95% CI | 0.35 (0.09, 0.61) | 1.25 | 0.53 | 0 | ||
| KT width change | MD 95% CI | 0.40 (0.17, 0.62) | 1.63 | 0.44 | 0 | ||
| EMP + CAF versus SCTG + CAF | Abolfazli 2009; McGuire 2012 | GR depth change | MD 95% CI | ‐0.39 (‐1.27, 0.48) | 25.79 | <0.00001 | 96.0 |
| CAL change | MD 95% CI | ‐0.25 (‐0.69, 0.20) | 2.95 | 0.09 | 66.0 | ||
| KT width change | MD 95% CI | ‐1.06 (‐1.36, ‐0.76) | 2.47 | 0.12 | 59.0 | ||
| SCRC | OR 95% CI | 0.61 (0.05, 7.86) | 7.86 | 0.005 | 87.0 | ||
| GTR rm + CAF versus SCTG + CAF | Paolantonio 2002; Wang 2001; Zucchelli 1998 | GR depth change | MD 95% CI | ‐0.37 (‐0.60, ‐0.13) | 0.25 | 0.88 | 0 |
| CAL change | MD 95% CI | 0.35 (0.06, 0.63) | 0.93 | 0.63 | 0 | ||
| KT width change | MD 95% CI | ‐1.77 (‐2.66, ‐0.89) | 15.84 | 0.0004 | 87.0 | ||
| SCRC | OR 95% CI | 0.61 (0.30, 1.24) | 2.01 | 0.37 | 0 | ||
| GTR rm + CAF versus GTR nrm + CAF | Roccuzzo 1996; Zucchelli 1998 | GR depth change | MD 95% CI | 0.23 (‐0.22, 0.68) | 1.59 | 0.21 | 37.0 |
| CAL change | MD 95% CI | 0.12 (‐0.37, 0.60) | 0.28 | 0.60 | 0 | ||
| KT width change | MD 95% CI | 0.12 (‐0.23, 0.48) | 0.03 | 0.86 | 0 | ||
| SCRC | OR 95% CI | 1.33 (0.46, 3.85) | 0.21 | 0.65 | 0 | ||
| GTR rm associated with bone substitutes + CAF versus SCTG + CAF | Paolantonio 2002; Rosetti 2000 | GR depth change | MD 95% CI | ‐0.82 (‐2.13, 0.49) | 9.92 | 0.002 | 90.0 |
| CAL change | MD 95% CI | ‐0.52 (‐1.34, 0.30) | 2.72 | 0.10 | 63.0 | ||
| KT width change | MD 95% CI | ‐2.38 (‐2.84, ‐1.92) | 1.86 | 0.17 | 46.0 | ||
| GTR rm associated with bone substitutes + CAF versus GTR rm + CAF | Dodge 2000; Paolantonio 2002 | GR depth change | MD 95% CI | 0.48 (0.09, 0.88) | 0.10 | 0.76 | 0 |
| CAL change | MD 95% CI | 0.76 (‐0.01, 1.54) | 2.83 | 0.09 | 65.0 | ||
| KT width change | MD 95% CI | 0.23 (‐0.21, 0.68) | 1.63 | 0.20 | 39.0 | ||
| SCRC | OR 95% CI | 1.87 (0.75, 4.64) | 0.03 | 0.87 | 0 | ||
| XCM + CAF versus CAF | Jepsen 2013; Sangiorgio 2017 | GR depth change | MD 95% CI | 0.40 (0.11, 0.68) | 0.86 | 0.35 | 0 |
| CAL change | MD 95% CI | 0.37 (‐0.09, 0.83) | 1.70 | 0.19 | 41.0 | ||
| KT width change | MD 95% CI | 0.44 (0.04, 0.85) | 1.16 | 0.28 | 14.0 | ||
| SCRC | OR 95% CI | 4.73 (2.35, 9.50) | 0.16 | 0.69 | 0 | ||
| PRF + CAF versus SCTG + CAF | Tunali 2015; Öncü 2017 | GR depth change | MD 95% CI | ‐0.01 (‐0.89, 0.86) | 14.71 | 0.0001 | 93.0 |
| CAL change | MD 95% CI | ‐0.37 (‐0.69, ‐0.06) | 0.58 | 0.45 | 0 | ||
| KT width change | MD 95% CI | ‐0.26 (‐0.98, 0.45) | 13.41 | 0.0003 | 93.0 |
ADMG: acellular dermal matrix graft; CAF: coronally advanced flap; CAL: clinical attachment level; CI: confidence interval; EMP: enamel matrix protein; GR: gingival recession; GTR rm: guided tissue regeneration resorbable membrane; GTR nrm: guided tissue regeneration non‐resorbable membrane; KT: keratinized tissue; MD: mean difference; OR: odds ratio; PRF: platelet‐rich fibrin; RR: risk ratio; SCRC: sites with complete root coverage; SCTG: subepithelial connective tissue graft; XCM: xenogeneic collagen matrix.
Comparisons 1 to 10 evaluated single defects, while comparison 11 multiple recession‐type defects. Moreover, analyses were performed according to the follow‐up evaluation (i.e. short term (6 months follow‐up preferably) in the majority of comparisons, except for two comparisons: EMP + CAF versus CAF (Comparison 4) where the data were derived from short term (6 months, Sangiorgio 2017) and medium term (24 months, Del Pizzo 2005; Spahr 2005) measurements; and EMP + CAF versus SCTG + CAF (Comparison 5) where the data from mean changes from baseline (i.e. gingival recession, clinical attachment level and keratinized tissue width) were derived from short‐term measurements, whereas sites with complete root coverage the data were derived from 6‐month (McGuire 2012) and 24‐month (Abolfazli 2009) measurements.
The study by Babu 2011 was not included into Comparison 6 because it was not clear whether test (GTR rm + CAF) and control (SCTG + CAF) displayed similar baseline recession depth, clinical attachment level and keratinized tissue means. In addition, data from studies not included in meta‐analyses are presented in Additional Table 7.
ADMG + CAF versus SCTG + CAF ‐ short term (Comparison 1)
Aesthetic condition change was not reported for this comparison.
-
Gingival recession depth, clinical attachment level and keratinized tissue width changes (Outcomes 1.1 to 1.3): there were four trials (Barros 2015; Joly 2007; Paolantonio 2002b; Shori 2013) reporting these outcomes measured as changes from the baseline values and there was insufficient evidence of a difference in these outcomes between ADMG + CAF and SCTG + CAF.
ADMG + CAF versus SCTG + CAF (Comparison 1, Outcome 1.1; Analysis 1.1): P = 0.28, mean difference ‐0.36 mm (95% confidence interval (CI) ‐1.03 to 0.30, Chi2 = 15.06, degrees of freedom (df) = 3, P = 0.002, I2 = 80%).
ADMG + CAF versus SCTG + CAF (Comparison 1, Outcome 1.2; Analysis 1.2): P = 0.09, mean difference ‐0.53 mm (95% CI ‐1.14 to 0.08, Chi2 = 9.73, df = 3, P = 0.02, I2 = 69%).
ADMG + CAF versus SCTG + CAF (Comparison 1, Outcome 1.3; Analysis 1.3): P = 0.10, mean difference ‐0.59 mm (95% CI ‐1.27 to 0.10, Chi2 = 17.17, df = 3, P = 0.0007, I2 = 83%).
1.1. Analysis.
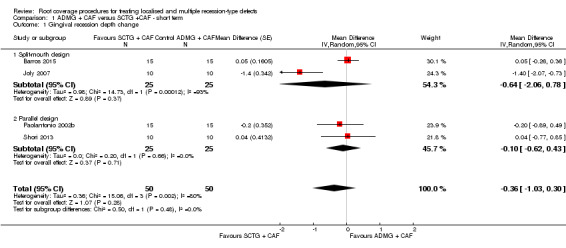
Comparison 1 ADMG + CAF versus SCTG +CAF ‐ short term, Outcome 1 Gingival recession depth change.
1.2. Analysis.
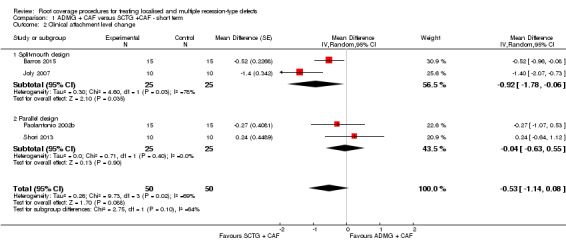
Comparison 1 ADMG + CAF versus SCTG +CAF ‐ short term, Outcome 2 Clinical attachment level change.
1.3. Analysis.
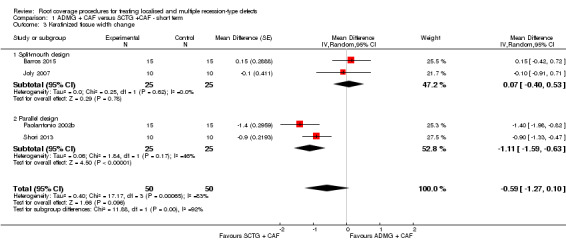
Comparison 1 ADMG + CAF versus SCTG +CAF ‐ short term, Outcome 3 Keratinized tissue width change.
ADMG + CAF versus CAF ‐ short term (Comparison 2)
Aesthetic condition change was not reported for this comparison.
-
Gingival recession depth, clinical attachment level and keratinized tissue width changes (Outcomes 2.1 to 2.3): there were two trials (de Queiroz 2006; Woodyard 2004) reporting these outcomes measured as changes from the baseline values and there was insufficient evidence of a difference in these outcomes between ADMG + CAF and CAF.
ADMG + CAF versus CAF (Comparison 2, Outcome 2.1; Analysis 2.1): P = 0.29, mean difference 0.61 mm (95% CI ‐0.52 to 1.73, Chi2 = 7.45, df = 1, P = 0.006, I2 = 87%).
ADMG + CAF versus CAF (Comparison 2, Outcome 2.2; Analysis 2.2): P = 0.19, mean difference 0.51 mm (95% CI ‐0.25 to 1.27, Chi2 = 2.32, df = 1, P = 0.13, I2 = 57%).
ADMG + CAF versus CAF (Comparison 2, Outcome 2.3; Analysis 2.3): P = 0.13, mean difference 0.28 mm (95% CI ‐0.08 to 0.64, Chi2 = 0.30, df = 1, P = 0.59, I2 = 0%).
2.1. Analysis.
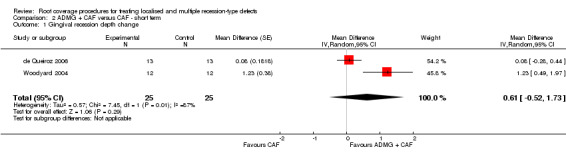
Comparison 2 ADMG + CAF versus CAF ‐ short term, Outcome 1 Gingival recession depth change.
2.2. Analysis.
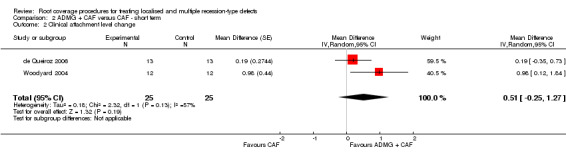
Comparison 2 ADMG + CAF versus CAF ‐ short term, Outcome 2 Clinical attachment level change.
2.3. Analysis.
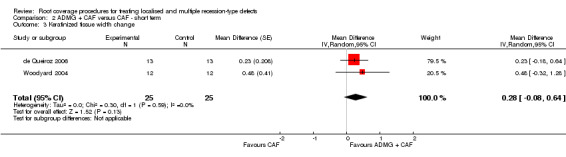
Comparison 2 ADMG + CAF versus CAF ‐ short term, Outcome 3 Keratinized tissue width change.
EMP + CAF versus CAF ‐ short term (Comparison 3)
Aesthetic condition change: Sangiorgio 2017 reported the results of root coverage aesthetics and overall aesthetic results evaluated by each patient with the assistance of a visual analogue scale (VAS). In terms of root coverage aesthetics both treatment approaches showed evidence of similar improvements between baseline and 6‐month evaluation. Regarding overall aesthetic results following treatment, there was evidence of equivalent outcomes for both groups (i.e. similar aesthetics).
-
Gingival recession depth and clinical attachment level changes (Outcomes 3.1 and 3.2): there was insufficient evidence of a difference in outcomes between EMP + CAF and CAF (three trials: Del Pizzo 2005; Sangiorgio 2017; Spahr 2005).
EMP + CAF versus CAF (Comparison 3, Outcome 3.1; Analysis 3.1): P = 0.67, mean difference 0.07 mm (95% CI ‐0.25 to 0.40, Chi2 = 5.62, df = 2, P = 0.06, I2 = 64%).
EMP + CAF versus CAF (Comparison 3, Outcome 3.2; Analysis 3.2): P = 0.07, mean difference 0.22 mm (95% CI ‐0.02 to 0.45, Chi2 = 1.57, df = 2, P = 0.46, I2 = 0%).
Keratinized tissue width change (Comparison 3, Outcome 3.3; Analysis 3.3): there was evidence of greater gain in the width of keratinized tissue for EMP + CAF when compared to CAF alone of 0.35 mm (95% CI 0.13 to 0.56, Chi2 = 0.64, df = 2, P = 0.73, I2 = 0%) (three trials: Del Pizzo 2005; Sangiorgio 2017; Spahr 2005).
3.1. Analysis.
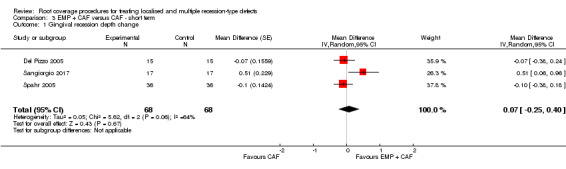
Comparison 3 EMP + CAF versus CAF ‐ short term, Outcome 1 Gingival recession depth change.
3.2. Analysis.
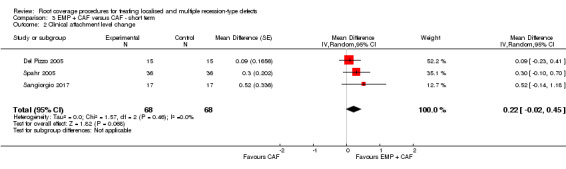
Comparison 3 EMP + CAF versus CAF ‐ short term, Outcome 2 Clinical attachment level change.
3.3. Analysis.
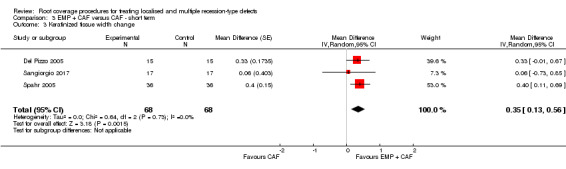
Comparison 3 EMP + CAF versus CAF ‐ short term, Outcome 3 Keratinized tissue width change.
EMP + CAF versus CAF ‐ short/medium term (Comparison 4)
Aesthetic condition change: Sangiorgio 2017 reported the results of root coverage aesthetics and overall aesthetic results evaluated by each patient with the assistance of a VAS. In terms of root coverage aesthetics both treatment approaches showed evidence of similar improvements between baseline and 6‐month evaluation. Regarding overall aesthetic results following treatment, there was evidence of equivalent outcomes for both groups (i.e. similar aesthetics).
-
Gingival recession depth, clinical attachment level and keratinized tissue width changes (Outcomes 4.1 and 4.3): there was evidence of greater reduction of gingival recession depth with concomitant gain in the clinical attachment level and width of keratinized tissue for EMP + CAF when compared to CAF alone (three trials: Del Pizzo 2005; Sangiorgio 2017; Spahr 2005).
EMP + CAF versus CAF (Comparison 4, Outcome 4.1; Analysis 4.1): P = 0.005, mean difference 0.32 mm (95% CI 0.10 to 0.55, Chi2 = 2.10, df = 2, P = 0.35, I2 = 5%).
EMP + CAF versus CAF (Comparison 4, Outcome 4.2; Analysis 4.2): P = 0.009, mean difference 0.35 mm (95% CI 0.09 to 0.61, Chi2 = 1.25, df = 2, P = 0.53, I2 = 0%).
EMP + CAF versus CAF (Comparison 4, Outcome 4.3; Analysis 4.3): P = 0.0005, mean difference 0.40 mm (95% CI 0.17 to 0.62, Chi2 = 1.63, df = 2, P = 0.44, I2 = 0%).
4.1. Analysis.
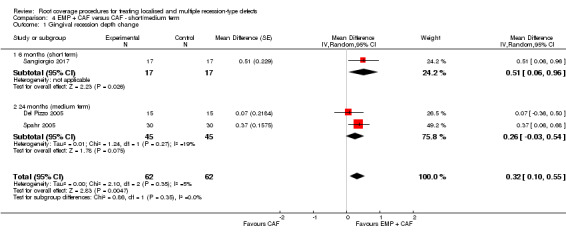
Comparison 4 EMP + CAF versus CAF ‐ short/medium term, Outcome 1 Gingival recession depth change.
4.2. Analysis.
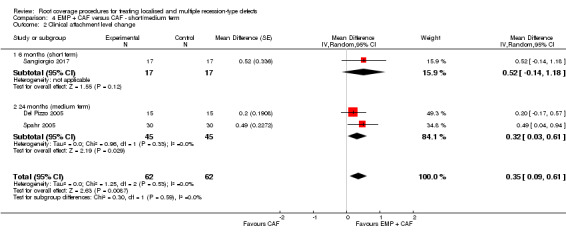
Comparison 4 EMP + CAF versus CAF ‐ short/medium term, Outcome 2 Clinical attachment level change.
4.3. Analysis.
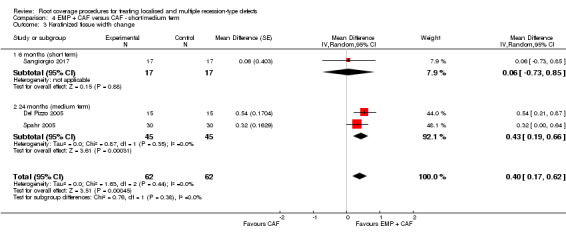
Comparison 4 EMP + CAF versus CAF ‐ short/medium term, Outcome 3 Keratinized tissue width change.
EMP + CAF versus SCTG + CAF ‐ short term (Comparison 5)
Aesthetic condition change: McGuire 2012 10 years after surgery asked their patients to respond to questions related to aesthetic satisfaction. Six patients had no preference for a particular type of treatment, two favoured aesthetic results with the test treatment (i.e. EMD + CAF), and one favoured results with the control treatment (SCTG + CAF) (P = 0.564).
-
Gingival recession depth and clinical attachment level changes (Outcomes 5.1 and 5.2): there was insufficient evidence of a difference between EMP + CAF and the SCTG + CAF (two trials: Abolfazli 2009; McGuire 2012).
EMP + CAF versus SCTG + CAF (Comparison 5, Outcome 5.1; Analysis 5.1): P = 0.38, mean difference ‐0.39 mm (95% CI ‐1.27 to 0.48, Chi2 = 25.79, df = 1, P < 0.00001, I2 = 96%).
EMP + CAF versus SCTG + CAF (Comparison 5, Outcome 5.2; Analysis 5.2): P = 0.28, mean difference ‐0.25 mm (95% CI ‐0.69 to 0.20, Chi2 = 2.95, df = 1, P = 0.09, I2 = 66%).
Keratinized tissue width changes (Comparison 5, Outcomes 5.3; Analysis 5.3): there was evidence of a difference between the EMP + CAF and the SCTG + CAF in keratinized tissue changes (P < 0.00001, mean difference ‐1.06 mm (95% CI ‐1.36 to ‐0.76, Chi2 = 2.47, df = 1, P = 0.12, I2 = 59%)) (two trials: Abolfazli 2009; McGuire 2012).
5.1. Analysis.
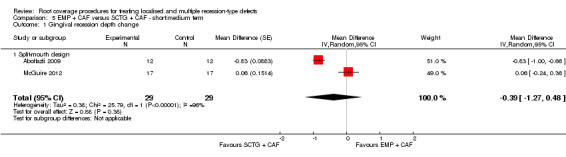
Comparison 5 EMP + CAF versus SCTG + CAF ‐ short/medium term, Outcome 1 Gingival recession depth change.
5.2. Analysis.
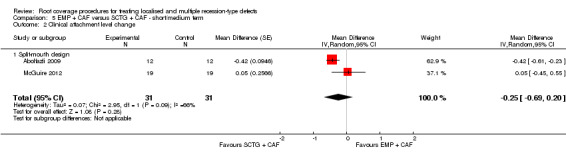
Comparison 5 EMP + CAF versus SCTG + CAF ‐ short/medium term, Outcome 2 Clinical attachment level change.
5.3. Analysis.
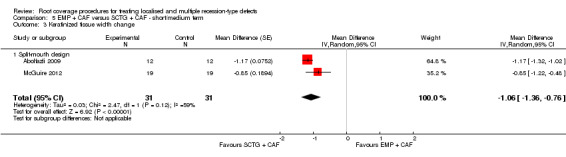
Comparison 5 EMP + CAF versus SCTG + CAF ‐ short/medium term, Outcome 3 Keratinized tissue width change.
GTR rm + CAF versus SCTG + CAF ‐ short term (Comparison 6)
Aesthetic condition change was not reported for this comparison.
-
Gingival recession depth and keratinized tissue changes (Outcomes 6.1 and 6.3): there were three trials (Paolantonio 2002; Wang 2001; Zucchelli 1998) for this outcome measured as change from the baseline values. There was evidence of a difference between GTR rm + CAF versus SCTG + CAF.
GTR rm + CAF versus SCTG + CAF (Comparison 6, Outcome 6.1; Analysis 6.1): P = 0.002, mean difference ‐0.37 mm (95% CI ‐0.60 to ‐0.13, Chi2 = 0.25, df = 2, P = 0.88, I2 = 0%).
GTR rm + CAF versus SCTG + CAF (Comparison 6, Outcome 6.3; Analysis 6.3): P < 0.0001, mean difference ‐1.77 mm (95% CI ‐2.66 to ‐0.89, Chi2 = 15.84, df = 2, P = 0.0004, I2 = 87%).
Clinical attachment level change (Comparison 6, Outcome 6.2; Analysis 6.2): there was evidence of a difference between GTR rm + CAF versus SCTG + CAF (mean difference of 0.35 mm, P = 0.02 (95% CI 0.06 to 0.63, Chi2 = 0.93, df = 2, P = 0.63, I2 = 0%)) (three trials: Paolantonio 2002; Wang 2001; Zucchelli 1998).
6.1. Analysis.
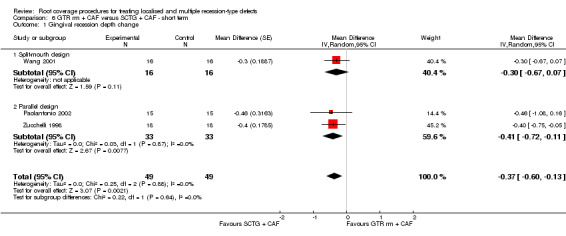
Comparison 6 GTR rm + CAF versus SCTG + CAF ‐ short term, Outcome 1 Gingival recession depth change.
6.3. Analysis.
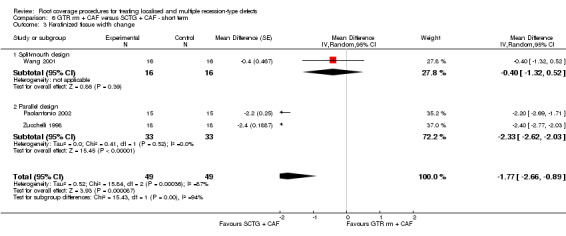
Comparison 6 GTR rm + CAF versus SCTG + CAF ‐ short term, Outcome 3 Keratinized tissue width change.
6.2. Analysis.
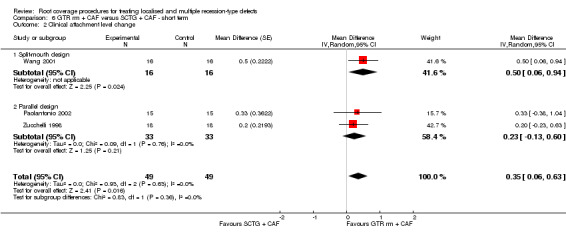
Comparison 6 GTR rm + CAF versus SCTG + CAF ‐ short term, Outcome 2 Clinical attachment level change.
GTR rm + CAF versus GTR nrm + CAF ‐ short term (Comparison 7)
Aesthetic condition change was not reported for this comparison.
-
Gingival recession depth, clinical attachment level and keratinized tissue width changes (Outcomes 7.1 to 7.3): there were two trials (Roccuzzo 1996; Zucchelli 1998) reporting these outcomes measured as changes from the baseline values and there was insufficient evidence of a difference in these outcomes between GTR rm + CAF and GTR nrm + CAF treatment.
GTR rm + CAF versus GTR nrm + CAF (Comparison 7, Outcome 7.1; Analysis 7.1): P = 0.32, mean difference 0.23 mm (95% CI ‐0.22 to 0.68, Chi2 = 1.59, df = 1, P = 0.21, I2 = 37%).
GTR rm + CAF versus GTR nrm + CAF (Comparison 7, Outcome 7.2; Analysis 7.2): P = 0.64, mean difference 0.12 mm (95% CI ‐0.37 to 0.60, Chi2 = 0.28, df = 1, P = 0.60, I2 = 0%).
GTR rm + CAF versus GTR nrm + CAF (Comparison 7, Outcome 7.3; Analysis 7.3): P = 0.50, mean difference 0.12 mm (95% CI ‐0.23 to 0.48, Chi2 = 0.03, df = 1, P = 0.86, I2 = 0%).
7.1. Analysis.
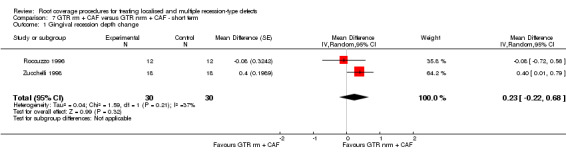
Comparison 7 GTR rm + CAF versus GTR nrm + CAF ‐ short term, Outcome 1 Gingival recession depth change.
7.2. Analysis.
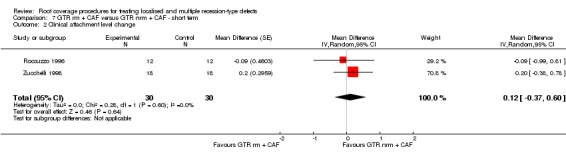
Comparison 7 GTR rm + CAF versus GTR nrm + CAF ‐ short term, Outcome 2 Clinical attachment level change.
7.3. Analysis.
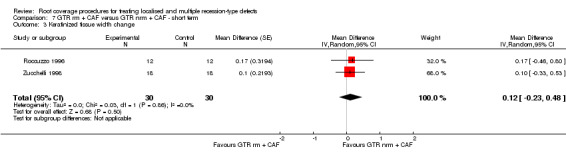
Comparison 7 GTR rm + CAF versus GTR nrm + CAF ‐ short term, Outcome 3 Keratinized tissue width change.
GTR rm associated with bone substitutes + CAF versus SCTG + CAF ‐ short term (Comparison 8)
Aesthetic condition change: Rosetti 2013 compared the GTR rm procedure associated with demineralized freeze‐dried bone allografts to SCTG in patients with bilateral gingival recessions. Similarly, aesthetical evaluation was performed by five examiners who were not participating in the study. In this study, the authors have mentioned only that the patient satisfaction survey indicated that all patients were satisfied with the aesthetic results achieved by both procedures at 18 months post‐surgery. In addition, no significant differences were identified between the 18 and 30 months assessments.
-
Gingival recession depth and clinical attachment level changes (Outcomes 8.1 and 8.2): two trials (Paolantonio 2002; Rosetti 2013) were evaluated and there was insufficient evidence of a difference between these procedures.
GTR rm + CAF associated with bone substitutes versus SCTG + CAF (Comparison 8, Outcome 8.1; Analysis 8.1): P = 0.22, mean difference ‐0.82 mm (95% CI ‐2.13 to 0.49, Chi2 = 9.92, df = 1, P = 0.002, I2 = 90%).
GTR rm + CAF associated with bone substitutes versus SCTG + CAF (Comparison 8, Outcome 8.2; Analysis 8.2): P = 0.21, mean difference ‐0.52 mm (95% CI ‐1.34 to 0.30, Chi2 = 2.72, df = 1, P = 0.10, I2 = 63%).
Keratinized tissue width change (Comparison 8, Outcome 8.3; Analysis 8.3): there was evidence of greater gain in keratinized tissue for SCTG + CAF when compared to GTR rm + CAF associated with bone substitutes of ‐2.38 mm (95% CI ‐2.84 to ‐1.92, Chi2 = 1.86, df = 1, P = 0.17, I2 = 46%) (two trials: Paolantonio 2002; Rosetti 2013).
8.1. Analysis.
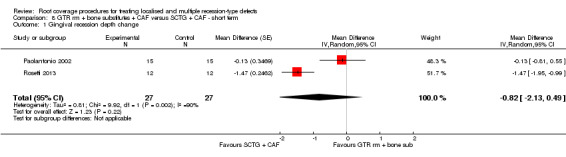
Comparison 8 GTR rm + bone substitutes + CAF versus SCTG + CAF ‐ short term, Outcome 1 Gingival recession depth change.
8.2. Analysis.
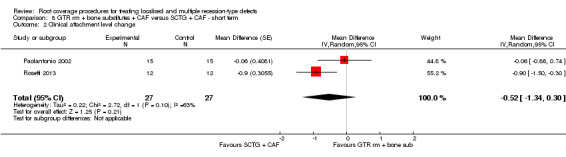
Comparison 8 GTR rm + bone substitutes + CAF versus SCTG + CAF ‐ short term, Outcome 2 Clinical attachment level change.
8.3. Analysis.
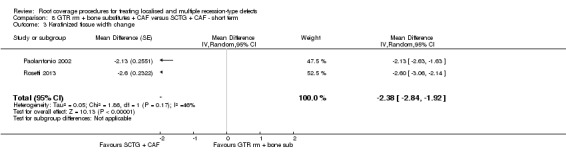
Comparison 8 GTR rm + bone substitutes + CAF versus SCTG + CAF ‐ short term, Outcome 3 Keratinized tissue width change.
GTR rm associated with bone substitutes + CAF versus GTR rm + CAF ‐ short term (Comparison 9)
Aesthetic condition change was not reported for this comparison.
Gingival recession depth change (Comparison 9, Outcome 9.1; Analysis 9.1): there was evidence of a difference between GTR rm + CAF associated with bone substitutes and GTR rm + CAF favouring GTR rm + CAF associated with bone substitutes (P = 0.02, mean difference 0.48 mm (95% CI 0.09 to 0.88, Chi2 = 0.10, df = 1, P = 0.76, I2 = 0%)) (two trials: Dodge 2000; Paolantonio 2002).
-
Clinical attachment level and keratinized tissue width changes (Outcomes 9.2 and 9.3): there were two trials (Dodge 2000; Paolantonio 2002) reporting these outcomes measured as changes from the baseline values and there was insufficient evidence of a difference in these outcomes between GTR rm + CAF associated with bone substitutes and GTR rm + CAF.
GTR rm + bone substitutes + CAF versus GTR rm + CAF (Comparison 9, Outcome 9.2; Analysis 9.2): P = 0.05, mean difference 0.76 mm (95% CI ‐0.01 to 1.54, Chi2 = 2.83, df = 1, P = 0.09, I2 = 65%).
GTR rm + bone substitutes + CAF versus GTR rm + CAF (Comparison 9, Outcome 9.3; Analysis 9.3): P = 0.31, mean difference 0.23 mm (95% CI ‐0.21 to 0.68, Chi2 = 1.63, df = 1, P = 0.20, I2 = 39%).
9.1. Analysis.
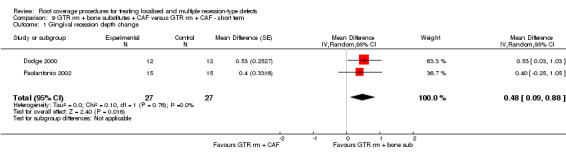
Comparison 9 GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term, Outcome 1 Gingival recession depth change.
9.2. Analysis.
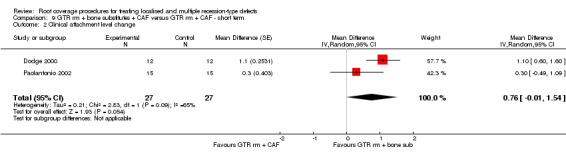
Comparison 9 GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term, Outcome 2 Clinical attachment level change.
9.3. Analysis.
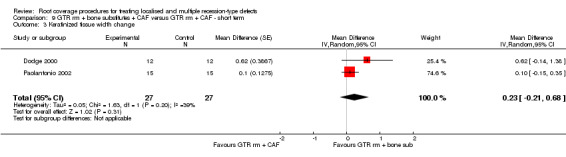
Comparison 9 GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term, Outcome 3 Keratinized tissue width change.
XCM + CAF versus CAF ‐ short term (Comparison 10)
Aesthetic condition change: Sangiorgio 2017 reported the results of root coverage aesthetics and overall aesthetic results evaluated by each patient with the assistance of a VAS. In terms of root coverage aesthetics both treatment approaches showed evidence of similar improvements between baseline and 6‐month evaluation. Regarding overall aesthetic results following treatment, there was evidence of equivalent outcomes for both groups (i.e. similar aesthetics).
-
Gingival recession depth and keratinized tissue level changes (Outcomes 10.1 and 10.3): there was evidence of a difference between XCM + CAF and the CAF alone favouring XCM + CAF (two trials: Jepsen 2013; Sangiorgio 2017).
XCM + CAF versus CAF (Comparison 10, Outcome 10.1; Analysis 10.1): P = 0.006, mean difference 0.40 mm (95% CI 0.11 to 0.68, Chi2 = 0.86, df = 1, P = 0.35, I2 = 0%).
XCM + CAF versus CAF (Comparison 10, Outcome 10.3; Analysis 10.3): P = 0.03, mean difference 0.44 mm (95% CI 0.04 to 0.85, Chi2 = 1.16, df = 1, P = 0.28, I2 = 14%).
Clinical attachment level change (Comparison 10, Outcome 10.2; Analysis 10.2): there was insufficient evidence of a difference between the XCM + CAF and the CAF alone (P = 0.11, mean difference 0.37 mm (95% CI ‐0.09 to 0.83, Chi2 = 1.70, df = 1, P = 0.19, I2 = 41%)) (two trials: Jepsen 2013; Sangiorgio 2017).
10.1. Analysis.
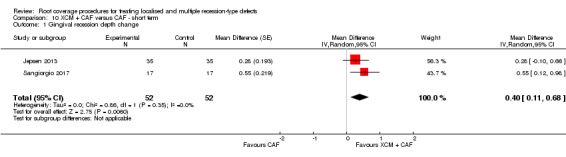
Comparison 10 XCM + CAF versus CAF ‐ short term, Outcome 1 Gingival recession depth change.
10.3. Analysis.
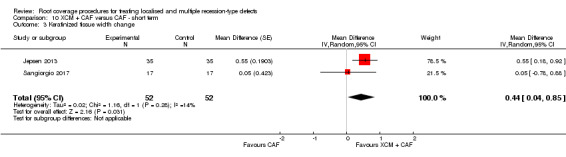
Comparison 10 XCM + CAF versus CAF ‐ short term, Outcome 3 Keratinized tissue width change.
10.2. Analysis.
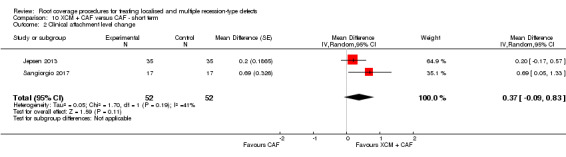
Comparison 10 XCM + CAF versus CAF ‐ short term, Outcome 2 Clinical attachment level change.
PRF + CAF versus SCTG + CAF ‐ short term (Comparison 11)
Aesthetic condition change was not reported for this comparison.
-
Gingival recession depth and keratinized tissue width changes (Outcomes 11.1 and 11.3): there were two trials (Öncü 2017; Tunali 2015) reporting these outcomes measured as changes from the baseline values and there was insufficient evidence of a difference in these outcomes between PRF + CAF and SCTG + CAF in the treatment of multiple recession‐type defects.
PRF + CAF versus SCTG + CAF (Comparison 11, Outcome 11.1; Analysis 11.1): P = 0.98, mean difference ‐0.01 mm (95% CI ‐0.89 to 0.86, Chi2 = 14.71, df = 1, P = 0.0001, I2 = 93%).
PRF + CAF versus SCTG + CAF (Comparison 11, Outcome 11.3; Analysis 11.3): P = 0.47, mean difference ‐0.26 mm (95% CI ‐0.98 to 0.45, Chi2 = 13.41, df = 1, P = 0.0003, I2 = 93%).
Clinical attachment level change (Comparison 11, Outcome 11.2; Analysis 11.2): there was evidence of a difference between PRF + CAF and SCTG + CAF favouring SCTG + CAF (P = 0.02, mean difference ‐0.37 mm (95% CI ‐0.69 to 0.06, Chi2 = 0.58, df = 1, P = 0.45, I2 = 0%)) (two trials: Öncü 2017; Tunali 2015).
11.1. Analysis.
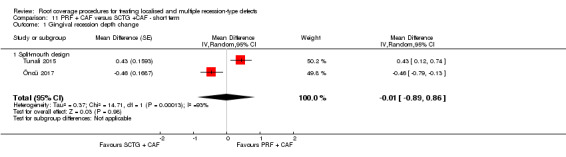
Comparison 11 PRF + CAF versus SCTG +CAF ‐ short term, Outcome 1 Gingival recession depth change.
11.3. Analysis.
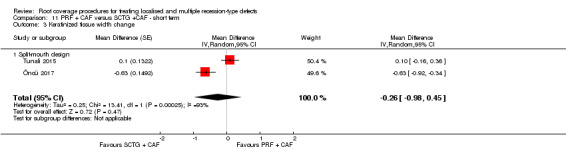
Comparison 11 PRF + CAF versus SCTG +CAF ‐ short term, Outcome 3 Keratinized tissue width change.
11.2. Analysis.
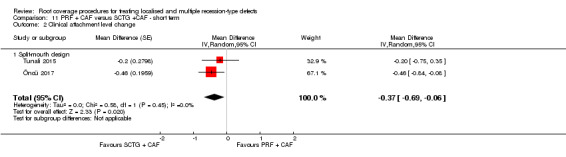
Comparison 11 PRF + CAF versus SCTG +CAF ‐ short term, Outcome 2 Clinical attachment level change.
Results from trials not included in meta‐analyses
Twenty‐eight trials could not be included into meta‐analyses because of the heterogeneity of root coverage procedures compared. Thus, their results (i.e. mean difference and 95% confidence intervals) are presented in additional Table 7. Likewise, some important issues of some of these studies are depicted bellow.
Babu 2011: although the authors of this study reported that "patients presented lesions with similar preoperative clinical parameters as shown by paired t test: RD (1.04), KG (1.08), and PD (1.09)", P values were not reported (Note of the review authors: the restricted number of defects included in the study suggests the need of non‐parametric analyses.).
Keceli 2008: the results from this study were reported as median values. The median value regarding the amount of root coverage achieved was 3.0 mm for both procedures, i.e. SCTG + platelet‐rich plasma and SCTG (Friedman test, within‐groups comparison P < 0.05). Differences between groups were not statistically significant (Mann–Whitney test ‐ P > 0.05). The median value regarding attachment gains values were 2.5 mm for SCTG + platelet‐rich plasma and 3.0 mm for SCTG (Friedman test, within‐groups comparison P < 0.05). Differences between groups were not statistically significant (Mann–Whitney test ‐ P > 0.05). The results from this study were reported as median values. However, the median values regarding keratinized tissue gains values were not reported. Only baseline and 12‐month medians values were reported. Differences within‐groups were considered statistically significant (Friedman test, P < 0.05). Conversely, differences between groups were not statistically significant (Mann–Whitney test ‐ P > 0.05).
McGuire 2016: with respect to the 5‐year follow‐up, changes from baseline were not reported. Overall, mean clinical attachment levels were of 2.35 mm and 1.65 mm for the test and control groups. Mean width of keratinized tissue of 3.41 mm and 4.12 mm were recorded for the test and control groups, respectively.
Pendor 2014: differences between groups in terms of keratinized tissue increase could not be accurately evaluated because baseline means were not statistically similar (Student t Test, P < 0.001).
Rasperini 2011: differences between groups in terms of keratinized tissue increase could not be accurately evaluated because baseline means were not statistically similar (Mann–Whitney U‐test, P = 0.01).
Reino 2012: baseline and final mean values regarding recession depth, clinical attachment level and width of keratinized tissue were not reported. Overall, both groups presented similar pre‐treatment clinical values (P > 0.05) for these outcome measures. There was a significant decrease in mean gingival recession and mean clinical attachment level for both SCTG + CAF (extended flap) and SCTG + CAF (ANOVA Two Way Test, within‐groups comparison P < 0.05). Differences between groups for both parameters were not statistically significant (ANOVA One Way Test, P < 0.01).The mean width of keratinized tissue increased for both SCTG + CAF (extended flap) and SCTG + CAF (ANOVA Two Way Test, within‐groups comparison P < 0.05). Differences between groups were not statistically significant (ANOVA One Way Test, P > 0.05).
Reino 2015: the mean gingival recession decreased from 3.47 mm to 0.63 mm for XCM + CAF (extended flap) and from 3.49 mm to 1.28 mm for XCM + CAF (Mann Whitney Test, intra‐group comparisons P < 0.001, comparison between groups P = 0.014). The mean clinical attachment level decreased from 5.29 mm to 2.63 mm for XCM + CAF (extended flap) and from 5.31 mm to 3.46 mm for XCM + CAF (ANOVA Two Way Test, intra‐group comparisons P < 0.01). Differences between groups were not statistically significant (P > 0.05). The mean width of keratinized tissue changed from 1.74 mm to 1.71 mm for XCM + CAF (extended flap) and from 1.66 mm to 2.01 mm for XCM + CAF (ANOVA Two Way Test, intra‐group comparisons P > 0.05). Differences between groups were not statistically significant (P > 0.05).
Sites with complete root coverage and percentage of complete root coverage
Data from the number and percentage of sites with complete root coverage were reported in 34 studies (Abolfazli 2009; Ahmedbeyli 2014; Ayub 2012; Bouchard 1994; Bouchard 1997; Costa 2016; da Silva 2004; de Queiroz 2006; Del Pizzo 2005; Dodge 2000; Henderson 2001; Jankovic 2010; Jepsen 2013; Leknes 2005; McGuire 2014; McGuire 2016; Ozenci 2015; Paolantonio 1997; Paolantonio 2002; Paolantonio 2002b; Pendor 2014; Rasperini 2011; Reino 2012; Roccuzzo 1996; Shori 2013; Trombelli 1996; Tunali 2015; Wang 2001; Woodyard 2004; Zucchelli 1998; Zucchelli 2003; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b). One study (Spahr 2005) reported only the percentage of sites with complete root coverage at 12‐ and 24‐month follow‐ups. Another trial (McGuire 2012) reported the percentage of sites with complete root coverage at 12‐month and 10‐year follow‐ups, whereas the number of sites was presented only at the final evaluation (Additional Table 9).
3. Root coverage outcomes ‐ complete root coverage and mean root coverage.
| Study | Interventions | SCRC | PCRC | MRC |
| Abolfazli 2009 | EMD + CAF (12 months) SCTG + CAF (12 months) EMD + CAF (24 months) SCTG + CAF (24 months) |
NR NR 3/12 8/12 |
NR NR 25.0 66.6 |
77.7 83.4 76.9 93.1 |
| Ahmedbeyli 2014 | ADMG + CAF CAF |
11/12 6/12 |
83.3 50.0 |
94.8 74.9 |
| Ayub 2012 | ADMG (positioned 1 mm apical to the CEJ) + CAF (extended flap) ADMG + CAF (extended flap) |
4/15 0/15 |
26.6 0 |
88.4 65.8 |
| Babu 2011 | GTR (collagen membrane) + CAF SCTG + CAF |
NR NR |
NR NR |
84.0 84.8 |
| Barros 2015 | ADMG + CAF (extended flap) SCTG + CAF (extended flap) |
NR NR |
NR NR |
80.7 78.7 |
| Bouchard 1994 | SCTG + CAF + citric acid (graft without epithelial collar) SCTG (graft with epithelial collar) |
3/15 5/15 |
20.0 33.3 |
69.7 64.7 |
| Bouchard 1997 | SCTG + CAF + tetracycline hydrochloride SCTG + CAF + citric acid |
6/15 8/15 |
40.0 53.3 |
79.3 84.0 |
| Costa 2016 | ADMG + EMD + CAF (6 months) ADMG + CAF (6 months) ADMG + EMD + CAF (12 months) ADMG + CAF (12 months) |
3/19 1/19 3/19 1/19 |
15.8 5.3 |
55.4 44.0 59.7 52.8 |
| da Silva 2004 | SCTG + CAF CAF |
2/11 1/11 |
18.1 9.0 |
75.3 68.8 |
| de Queiroz 2006 | ADMG + CAF (6 months) CAF (6 months) ADMG + CAF (12 months) CAF (12 months) ADMG + CAF (24 months) CAF (24 months) |
3/13 3/13 2/13 2/13 1/13 1/13 |
23.0 23.0 15.3 15.3 7.7 7.7 |
76.0 71.0 71.0 66.7 68.4 55.9 |
| Del Pizzo 2005 | EMD + CAF CAF |
11/15 9/15 |
73.3 60.0 |
90.7 86.7 |
| Dodge 2000 | GTR (polylactide membrane ‐ Guidor) + tetracycline hydrochloride + DFDBA + CAF GTR (polylactide membrane ‐ Guidor) + tetracycline hydrochloride + CAF |
6/12 4/12 |
50.0 33.3 |
89.9 73.7 |
| Henderson 2001 | ADMG (basement membrane side against the tooth) + CAF ADMG (connective tissue side against the tooth) + CAF |
7/10 8/10 |
70.0 80.0 |
94.9 95.5 |
| Jaiswal 2012 | EMD + CAF CAF |
NR NR |
NR NR |
86.3 79.6 |
| Jankovic 2010 | Platelet‐rich fibrin + CAF EMD + CAF |
12/20 13/20 |
60.0 65.0 |
72.1 70.5 |
| Jepsen 2013 | XCM + CAF CAF |
29/35 17/35 |
82.8 48.6 |
72.0 66.2 |
| Joly 2007 | ADMG + CAF (without vertical incisions) SCTG + CAF (without vertical incisions) |
NR NR |
NR NR |
50.0 79.5 |
| Keceli 2008 | SCTG + platelet‐rich plasma + CAF SCTG + CAF |
6/17 8/19 |
35.3 42.1 |
86.4 86.4 |
| Keceli 2015 | SCTG + platelet‐rich fibrin + CAF SCTG + CAF |
11/20 7/20 |
55.0% 35.0% |
89.6 79.9 |
| Leknes 2005 | GTR (polylactide membrane ‐ Guidor) (6 months) + CAF CAF (6 months) GTR (polylactide membrane ‐ Guidor) (12 months) + CAF CAF (12 months) GTR (polylactide membrane ‐ Guidor) (72 months) + CAF CAF (72 months) |
5/20 10/20 4/20 6/20 2/11 1/11 |
25.0 50.0 20.0 30.0 18.2 9.1 |
51.2 63.8 51.2 61.1 35.0 34.2 |
| Matarasso 1998 | GTR (polylactide membrane ‐ Guidor) + double papilla flap GTR (polylactide membrane ‐ Guidor) + CAF |
NR NR |
NR NR |
73.9 62.5 |
| McGuire 2012 | EMD + CAF (6 months) SCTG + CAF (6 months) EMD + CAF (10 years) SCTG + CAF (10 years) |
17/19 15/19 5/9 7/9 |
89.5 79.0 55.6 77.8 |
95.1 93.8 83.3 89.8 |
| McGuire 2014 | B‐TCP + CD with rhPDGF‐BB + CAF (6 months) SCTG + CAF (6 months) B‐TCP + CD with rhPDGF‐BB + CAF (5 years) SCTG + CAF (5 years) |
NR NR 12/20 15/20 |
NR NR 60.0 75.0 |
90.8 98.6 74.1 89.3 |
| McGuire 2016 | XCM + CAF (6 months) SCTG + CAF (6 months) XCM + CAF (12 months) SCTG + CAF (12 months) XCM + CAF (5 years) SCTG + CAF (5 years) |
15/25 23/25 17/23 22/23 9/17 15/17 |
60.0 92.0 73.9 95.6 52.9 88.2 |
83.5 97.0 88.5 99.3 77.6 95.5 |
| Öncü 2017 | Platelet‐rich fibrin + CAF (6 months) SCTG + CAF (6 months) |
15/30(t) 18/30(t) |
50.0 60.0 |
77.1 84.0 |
| Ozenci 2015 | ADMG + CAF (tunnel) ADMG + CAF (without vertical realising incisions) |
12/31(t) 23/27(t) |
37.4(t) 85.0(t) |
75.7 93.8 |
| Paolantonio 1997 | SCTG + double papilla flap FGG |
17/35 3/35 |
48.6 8.6 |
85.2 53.2 |
| Paolantonio 2002 | GTR (polylactide membrane ‐ Guidor) + CAF GTR (polylactic acid membrane ‐ Paroguide) + hydroxyapatite/collagen/chondroitin‐sulphate graft + CAF SCTG + double papilla flap |
6/15 8/15 9/15 |
40.0 53.3 60.0 |
81.0 87.1 90.0 |
| Paolantonio 2002b | ADMG + CAF SCTG + CAF |
4/15 7/15 |
26.6 46.6 |
83.3 88.8 |
| Pendor 2014 | SCTG + double papilla flap SCTG + CAF |
6/10 6/10 |
60.0 60.0 |
88.0 84.7 |
| Rasperini 2011 | SCTG + EMD + CAF SCTG + CAF |
16/26 14/30 |
61.5 46.6 |
90.7 76.6 |
| Reino 2012 | SCTG + CAF (extended flap) SCTG + CAF |
2/20 0/20 |
10.0 0 |
44.5 43.2 |
| Reino 2015 | XCM + CAF (extended flap) XCM + CAF |
NR NR |
NR NR |
81.9 62.8 |
| Roccuzzo 1996 | GTR (polylactic acid membrane ‐ Guidor) + CAF GTR (ePTFE membrane ‐ Gore‐Tex) + CAF |
5/12 5/12 |
41.6 41.6 |
82.4 82.4 |
| Rosetti 2013 | GTR (collagen membrane) + tetracycline hydrochloride + DFDBA + CAF (18 months) SCTG + tetracycline hydrochloride (18 months) GTR (collagen membrane) + tetracycline hydrochloride + DFDBA + CAF (30 months) SCTG + tetracycline hydrochloride (30 months) |
NR NR NR NR |
NR NR NR NR |
84.2 95.6 87.0 95.5 |
| Sangiorgio 2017 | XCM + CAF EMD + CAF XCM + EMD + CAF CAF |
9/17 12/17 10/17 4/17 |
52.9 70.6 58.8 23.5 |
87.2 88.8 91.6 68.0 |
| Shori 2013 | ADMG + CAF SCTG + CAF |
NR NR |
NR NR |
86.9 84.7 |
| Spahr 2005 | EMP + CAF (6 months) Placebo (propylene glycol alginate) + CAF (6 months) EMP + CAF (12 months) Placebo (propylene glycol alginate) + CAF (12 months) EMP + CAF (24 months) Placebo (propylene glycol alginate) + CAF (24 months) |
NR NR NR NR NR NR |
NR NR NR NR 53.0 23.0 |
80.0 79.0 80.0 79.0 84.0 67.0 |
| Tozum 2005 | SCTG + modified tunnel procedure SCTG + CAF |
NR NR |
NR NR |
96.4 77.1 |
| Trombeli 1996 | CAF + fibrin glue + tetracycline hydrochloride CAF + tetracycline hydrochloride |
1/11 2/11 |
9.1 18.2 |
63.1 52.9 |
| Tunali 2015 | Leukocyte‐ and platelet‐rich fibrin + CAF (6 months) SCTG + CAF (6 months) Leukocyte‐ and platelet‐rich fibrin + CAF (12 months) SCTG + CAF (12 months) |
4/22(t) 2/22(t) 3/22(t) 4/22(t) |
18.2 9.1 13.6 18.2 |
74.6 74.1 76.6 77.4 |
| Wang 2001 | GTR (reabsorbable double thickness collagen membrane ‐ Sulzer Dental Inc) + CAF SCTG + CAF |
7/16 7/16 |
43.8 43.8 |
73.0 84.0 |
| Woodyard 2004 | ADMG + CAF CAF |
11/12 4/12 |
91.6 33.3 |
96.0 67.0 |
| Zucchelli 1998 | GTR (polylactic acid membrane ‐ Guidor) + CAF GTR (ePTFE membrane ‐ Gore‐Tex) + CAF SCTG + CAF |
7/18 5/18 12/18 |
39.0 28.0 66.0 |
85.7 80.5 93.5 |
| Zucchelli 2003 | SCTG (graft size equal to the bone dehiscence) + CAF SCTG (graft size 3 mm greater than the bone dehiscence) + CAF |
13/15 12/15 |
86.7 80.0 |
97.3 94.7 |
| Zucchelli 2009 | Ultrasonic scaling + CAF Manual/hand scaling + CAF |
6/11 9/11 |
54.5 81.8 |
84.2 95.4 |
| Zucchelli 2014 | SCTG (de‐epithelialized FGG (graft height of 4 mm and thickness < 2 mm)) + CAF SCTG (de‐epithelialized FGG (graft height > 4 mm and thickness > 2 mm) ) + CAF |
25/30 24/30 |
83.3 80.0 |
96.3 96.7 |
| Zucchelli 2014b | SCTG + CAF (removal of the labial submucosal tissue) SCTG + CAF |
22/25 12/25 |
88.0 48.0 |
97.8 82.8 |
ADMG: acellular dermal matrix graft; B‐TCP: Beta‐tricalcium phosphate; CAF: coronally advanced flap; CEJ: cemento‐enamel junction; DFDBA: demineralized freeze‐dried bone allograft; EMD: enamel matrix derivative; EMP: enamel matrix protein; ePTFE: expanded polytetrafluorethylene; FGG: free gingival graft; GTR: guided tissue regeneration; MRC: mean root coverage; PCRC: percentage of complete root coverage; rhPDGF‐BB: recombinant human platelet‐derived growth factor‐BB; SCRC: sites with complete root coverage; SCTG: subepithelial connective tissue graft; t: teeth; XCM: xenogeneic collagen matrix.
Among the included RCTs designed to evaluate single recession type‐defects (excluding the data from the studies by Costa 2016 and Reino 2012 who included only heavy smokers) the percentage of complete root coverage varied from 0% (Ayub 2012) to 91.6% (Woodyard 2004) for ADMG; 18.1% (da Silva 2004) to 95.6% (McGuire 2016) for SCTG; 25% (Abolfazli 2009) to 89.5% (McGuire 2012) for EMP; 7.7 % (de Queiroz 2006) to 81.8% (Zucchelli 2009) for CAF; 33.3% (Dodge 2000) to 53.3% (Paolantonio 2002) for GTR rm; and 28% (Zucchelli 1998) to 41.6% (Roccuzzo 1996) for GTR nrm (Additional Table 9).
In addition, odds ratio (OR) analyses were available for six comparisons.
ADMG + CAF versus SCTG + CAF ‐ short term (Analysis 1.4), ADMG + CAF versus CAF ‐ short term (Analysis 2.4), EMP + CAF versus SCTG + CAF ‐ short/medium term (Analysis 5.4), GTR rm + CAF versus SCTG + CAF‐ short term (Analysis 6.4), GTR rm + CAF versus GTR nrm + CAF ‐ short term (Analysis 7.4), and GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term (Analysis 9.4): no statistical differences were found between procedures.
XCM + CAF versus CAF ‐ short term (Analysis 10.4): the combined therapy improved the achievement of sites displaying complete root coverage compared to the use of CAF alone (OR of 4.73 (95% CI 2.35 to 9.50; P < 0.0001; Chi2 = 0.16; I2 = 0%)).
1.4. Analysis.
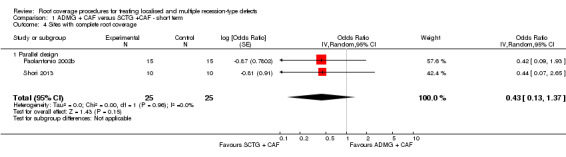
Comparison 1 ADMG + CAF versus SCTG +CAF ‐ short term, Outcome 4 Sites with complete root coverage.
2.4. Analysis.
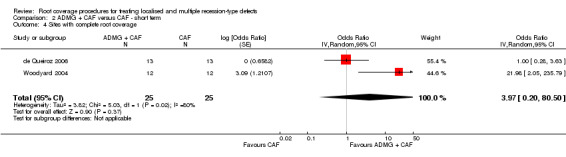
Comparison 2 ADMG + CAF versus CAF ‐ short term, Outcome 4 Sites with complete root coverage.
5.4. Analysis.
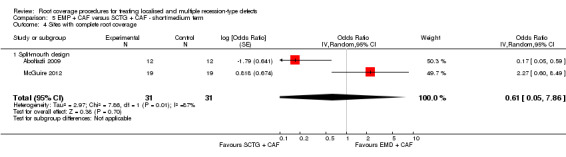
Comparison 5 EMP + CAF versus SCTG + CAF ‐ short/medium term, Outcome 4 Sites with complete root coverage.
6.4. Analysis.
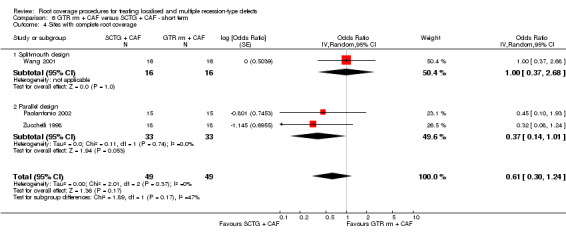
Comparison 6 GTR rm + CAF versus SCTG + CAF ‐ short term, Outcome 4 Sites with complete root coverage.
7.4. Analysis.
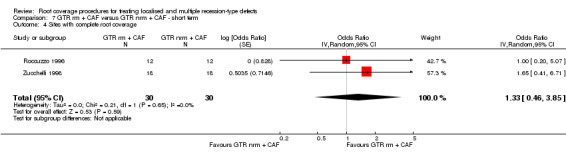
Comparison 7 GTR rm + CAF versus GTR nrm + CAF ‐ short term, Outcome 4 Sites with complete root coverage.
9.4. Analysis.
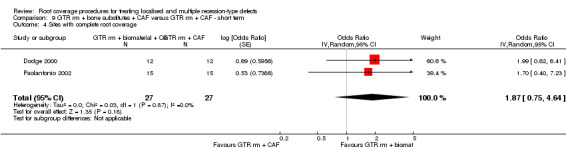
Comparison 9 GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term, Outcome 4 Sites with complete root coverage.
10.4. Analysis.
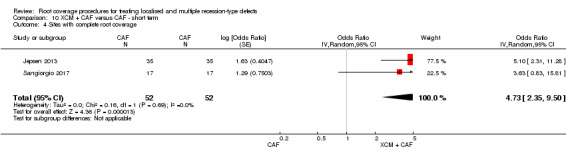
Comparison 10 XCM + CAF versus CAF ‐ short term, Outcome 4 Sites with complete root coverage.
Mean root coverage
All included trials reported the mean root coverage. Within studies evaluating single recession type‐defects (excluding the data from Costa 2016 and Reino 2012 who included only heavy smokers), this outcome varied from 50% (Joly 2007) to 96% (Woodyard 2004) for ADMG, 64.7% (Bouchard 1994) to 99.3% for SCTG (McGuire 2016), 70.5% (Jankovic 2010) to 95.1% (McGuire 2012) for EMP, 55.9% (de Queiroz 2006) to 95.4% (Zucchelli 2009) for CAF, 62.5% (Matarasso 1998) to 73.7% (Dodge 2000) for GTR rm, 84.2 % (Rosetti 2013) to 89.9% (Dodge 2000) for GTR rm associated with bone substitutes, and 80.5% (Zucchelli 1998) to 82.4% (Roccuzzo 1996) for GTR nrm (Additional Table 9).
Patients' preference for a specific periodontal plastic surgery (PPS) procedure
Patients' preference for a specific PPS procedure (in split‐mouth trials) was reported in three trials (Roccuzzo 1996; Wang 2001; Zucchelli 2003).
In the first study (Roccuzzo 1996), all patients preferred the GTR treatment only because it was a single‐step procedure.
The second trial (Wang 2001) comparing patient satisfaction with aesthetics (i.e. amount of root coverage, colour match and overall satisfaction) obtained by SCTG and GTR rm showed that the participants reported greater overall satisfaction with the GTR procedures, probably explained by the reduction in treatment time and elimination of the need for a second surgical intervention.
In the third (Zucchelli 2003), 12 patients (80%) preferred the treatment with reduced size SCTG (i.e. graft dimension equal to the depth of the bone dehiscence) due to the better aesthetics achieved.
Occurrence of adverse effects or postoperative complications or both
Occurrence of adverse effects and/or postoperative complications during the postsurgical period was reported in 15 trials (Ahmedbeyli 2014; Costa 2016; Dodge 2000; Jankovic 2010; Jepsen 2013; Keceli 2008; McGuire 2012; McGuire 2014; McGuire 2016; Roccuzzo 1996; Spahr 2005; Wang 2001; Zucchelli 2003; Zucchelli 2014; Zucchelli 2014b).
Ahmedbeyli 2014: patients rated ADMG + CAF and CAF equally in terms of the following conditions: pain during surgery, discomfort associated to the duration of procedure and handling by the operator, postsurgical pain/swelling and complications.
Ayub 2012: exposure of ADMG was reported in two cases (ADMG + CF group).
Dodge 2000; Roccuzzo 1996: reported membrane exposure between the first and second weeks of healing.
Jankovic 2010: recording based on a "healing index" showed statistically significantly superior results for EMP + CAF compared to platelet‐rich fibrin + CAF (P < 0.05) 1 week after surgery. Also, three patients in the EMP group and one in the platelet‐rich fibrin group experienced "severe pain". All patients in the EMP group indicated "greater discomfort", as well as pain intensity was "statistically significantly different between groups for the first 5 days" favouring the platelet‐rich fibrin group.
Jepsen 2013: patient evaluations via VAS exclusively for GR => 3 mm were not available. However, for all defects, there were no differences regarding pain and discomfort between XCM + CAF versus CAF.
Keceli 2008: there were minor complications related to postoperative swelling occurring within the first days after surgery, and immediate postoperative bleeding in one donor site of SCTG.
McGuire 2012: patient‐reported discomfort was considered statistically significantly higher for SCTG when compared to EMP + CAF, only at 1 month postoperatively.
McGuire 2014: all patients had mild or no discomfort due to bleeding, swelling, and sensitivity between the first and the fourth week after treatment. VAS did not identify statistically significant differences in pain scores between beta‐tricalcium phosphate (b‐TCP) + recombinant human platelet‐derived growth factor‐B with a bioabsorbable collagen wound‐healing dressing + CAF and SCTG + CAF. 6 months after treatment, 97% of the patients "commented that they experienced no difference in discomfort between the two treatment sites". 25 patients (78.1%) experienced 75 adverse events within the first 6 months (the most common ones were mild contusion (50%) and face swelling (40.6%)).
McGuire 2016: two subjects had trauma (a seizure) at 1 week, and 3 weeks (subject could not recall a specific injury) at test sites (XCM + CAF). There were no statistically significant differences between groups (XCM + CAF versus SCTG + CAF) in VAS in terms of pain score/discomfort scores at 1 week, 4 weeks or 6 months.
Öncü 2017: VAS showed evidence of less discomfort during the first postoperative week for PRF + CAF compared to SCTG + CF.
Spahr 2005: six patients felt moderate discomfort postoperatively, without differences between treatment modalities (CAF + EMP versus CAF).
Wang 2001: two patients treated with SCTG experienced adverse effects: one patient experienced postsurgical swelling and the other postsurgical ecchymosis.
Zucchelli 2003: greater covering flap dehiscence, more painful palate wound healing and necrosis of the primary palatal flap during the first period of healing was detected in patients treated with SCTG showing graft dimension 3 mm greater than the depth of the bone dehiscence.
Zucchelli 2014: 2 weeks after treatment, there was a statistically superior shrinkage of the covering flap with graft exposure at control sites (de‐epithelialized free gingival graft: graft height equal to the depth of bone dehiscence and thickness ≥ 2 mm) than at test sites (de‐epithelialized free gingival graft: graft height of 4 mm thickness < 2 mm).
Zucchelli 2014b: 2 weeks after surgery, shrinkage of the covering flap with graft exposure was noticed in 36% of control sites (SCTG + CAF without removal of the labial submucosal tissue) and 4% of test sites (SCTG + CAF with removal of the labial submucosal tissue). The difference was statistically significant (P < 0.01). VAS did not identify difference in patient pain and morbidity between the two procedures.
Discussion
Summary of main results
The objectives of the root coverage periodontal plastic surgery (RCPPS) procedures are to improve patients' aesthetic conditions and other clinical outcomes (e.g. clinical attachment level and the width of keratinized tissue) through the coverage of previously denuded root surfaces. Reported as primary and secondary outcomes, a summary of the main results is depicted below.
Primary outcomes
In spite of aesthetics being considered the primary goal of root coverage procedures, few studies had evaluated aesthetic condition change related to patients' opinion (Ahmedbeyli 2014; Bouchard 1994; McGuire 2012; McGuire 2014; McGuire 2016; Ozenci 2015; Rosetti 2013; Zucchelli 2003; Zucchelli 2014; Zucchelli 2014b). In these studies, the majority of the patients were satisfied with the final aesthetic result achieved. Also, procedures that make a reduction in the operatory time possible, that eliminate the need for a second surgical site and their associated morbidity (guided tissue regeneration with resorbable membranes (GTR rm)) (Wang 2001) and that use smaller palatal grafts (Zucchelli 2003; Zucchelli 2014) were better accepted by the patients.
In terms of recession depth reduction, results from meta‐analyses demonstrated evidence that at short term: subepithelial connective tissue grafts (SCTG) + coronally advanced flap (CAF) promoted additional gains to those achieved by GTR rm + CAF; xenogeneic collagen matrix (XCM) + CAF improved the gains obtained by CAF alone; enamel matrix derivative (EMD) + CAF led to better stability of the gingival margin after treatment than CAF alone; and GTR rm + bone substitutes + CAF provided better outcomes than GTR rm + CAF. While statistical analyses (i.e. meta‐analyses) did not reveal sufficient evidence of differences between other group comparisons, it was possible to demonstrate that the evaluated procedures were similarly efficient in reducing baseline mean gingival recession.
There was a marked variation between procedures in terms of the achievement of complete root coverage at short term (Additional Table 9): 0% to 95.6%. Odds ratio analyses on complete root coverage did not reveal evidence of differences between procedures in none of the available comparisons, except for XCM + CAF versus CAF (i.e. the combined therapy promoted better outcomes). In addition, some studies showed a decrease in the number of sites displaying complete root coverage over time (de Queiroz 2006; McGuire 2012; McGuire 2014; McGuire 2016).
Secondary outcomes
With respect to secondary outcomes, four comparisons showed evidence that SCTG + CAF promoted additional gains in the width of keratinized tissue compared to EMP + CAF, GTR rm + CAF, or GTR rm + bone substitutes + CAF. Similarly, the use of EMP + CAF or XCM + CAF promoted additional gains in the keratinized tissue compared to the use of CAF alone (Additional Table 8). Regarding clinical attachment level changes, there was evidence that SCTG + CAF promoted additional gains to those achieved by platelet‐rich fibrin (PRF) + CAF, and that GTR rm + CAF promoted additional gains compared to SCTG + CAF.
Only one trial reported results from free gingival grafts compared to SCTG after a follow‐up period of 5 years (Paolantonio 1997). The results of this study evidenced the superiority of connective grafts in terms of gains in root coverage and similarities in the amount of keratinized tissue achieved.
Also, there was a markedly variation in the amount of root coverage achieved. Mean root coverage varied from 44% to 99.3% (Additional Table 9). Additionally, data from some medium‐ and long‐term trials (de Queiroz 2006; McGuire 2012; McGuire 2014; McGuire 2016) showed that both mean and complete root coverage decreased over time.
Patients' preference for a specific periodontal plastic surgery procedure followed the same pattern as aesthetics condition change (Roccuzzo 1996; Zucchelli 2003).
Occurrence of an early discomfort with or without pain was related to donor sites of SCTG (McGuire 2012; Öncü 2017; Wang 2001; Zucchelli 2003). This aspect may be related to the size of the graft obtained from the palate and the surgical approach used (Zucchelli 2003). Moreover, 'bigger grafts' were more associated to shrinkage of the covering flap with graft exposure when compared to 'small grafts' (Zucchelli 2003; Zucchelli 2014). In terms of flap preparation, the removal of the labial submucosal tissue, in the area of lower incisors, led to a reduction in the number of sites experiencing covering flap shrinkage than sites where the submucosal tissue was not removed (Zucchelli 2014b).
With respect to guided tissue regeneration techniques, membrane exposure during healing was associated with primary postoperative complications (Dodge 2000; Roccuzzo 1996).
Overall findings and conditions
Although 48 randomised controlled trials (RCTs) were included in this Cochrane Review, it was difficult to combine data from these trials due to a great variability of comparisons between the various RCPPS procedures and the inexistence of a unique gold standard control group in all studies. Consequently, only 20 trials were incorporated into meta‐analyses (Abolfazli 2009; Barros 2015; de Queiroz 2006; Del Pizzo 2005; Dodge 2000; Jepsen 2013; Joly 2007; McGuire 2012; Öncü 2017; Paolantonio 2002; Paolantonio 2002b; Roccuzzo 1996; Rosetti 2013; Sangiorgio 2017; Shori 2013; Spahr 2005; Tunali 2015; Wang 2001; Woodyard 2004; Zucchelli 1998) in 11 different group comparisons (i.e. five analyses consisted of two studies, one of three studies, and one of four trials) (Additional Table 8). These aspects prevent us from drawing formal definitive conclusions.
Few studies reported a follow‐up period superior to 12 months (Abolfazli 2009; de Queiroz 2006; Del Pizzo 2005; Leknes 2005; McGuire 2012; McGuire 2014; McGuire 2016; Paolantonio 1997; Rosetti 2013; Spahr 2005). In six of these studies a chronological evaluation of the results evidenced loss in the amount of root coverage obtained (e.g. mean root coverage and sites with complete root coverage) between the 6 months to 12 months period of evaluation (de Queiroz 2006; Del Pizzo 2005; Spahr 2005) and between the first year and 5‐ and 10‐year follow‐ups (McGuire 2012; McGuire 2014; McGuire 2016). This assumption was evidenced by the findings of pooled estimates (Comparison 3, Outcome 3.1 and Comparison 4, Outcome 4.1). Long‐term period evaluations are probably linked to individual conditions such as changes in the periodontal health status, toothbrushing, habits and genetic and systemic conditions.
Two trials (Costa 2016; Reino 2012) evidenced the detrimental impact of smoking on root coverage outcomes (i.e. mean root coverage and complete root coverage decrease) within patients who smoke ≥ 10 cigarettes per day for more than 5 years.
Overall, both the individual studies' outcomes (i.e. within‐group comparisons reported by each individual trial) and findings of pooled estimates clearly demonstrated that all root coverage procedures included in this Cochrane Review promoted reduction in the extent of gingival recession and concomitant gain in the clinical attachment level for both single and multiple recession‐type defects. Likewise, it was evidenced that keratinized tissue augmentation of these sites was associated to the use of SCTG or allogenous (ADMG)/xenogenous (XCM) soft tissue substitutes.
Quality of the evidence
Based on the information contained in each individual article and on the details regarding the methodological quality of the trials provided after contact with original authors (e.g. method of randomisation, allocation concealment, blinding of examiners/patients and completeness of the follow‐up period), only one study was considered to be at a low overall risk of bias. Therefore the lack of allocation concealment or blinding or both and inadequate methods of randomisation, as well as the lack of similar inclusion criteria between trials and baseline characteristics of defects (as reported by some studies), can act as source of biases and can affect the accuracy of the results (Needleman 2002; Needleman 2005). GRADE methods (GRADE 2004) were used to assess the quality of the body of evidence of our main comparisons and our assessment is presented in the Table 1; Table 2; Table 3; Table 4; Table 5; Table 6 with all evidence considered to be of low to very low quality, mainly for imprecision and inconsistency.
Potential biases in the review process
In this review, only defects ≥ 3 mm were included in order to minimize heterogeneity between the trials. However, this inclusion criterion could have eliminated data from studies that could be incorporated into meta‐analyses (see Agreements and disagreements with other studies or reviews). In addition, the limited number of studies included in the meta‐analyses prevented formal testing for publication bias.
Agreements and disagreements with other studies or reviews
Data from the included studies in this review have shown that the percentage of success achieved by RCPPS procedures was regularly associated with improvements in the clinical parameters (i.e. outcomes measures), mainly evaluated by gains in the clinical attachment level and in the width of keratinized tissue and achieved mean root coverage. Nevertheless, different authors have pointed out that these currently used parameters only reflect the final clinical results expected and not the changes that had occurred in patient‐centred outcomes, such as changes in the aesthetic condition, functional limitations (e.g. limitations in chew and deglutition of food), discomfort, pain, alterations in the level of sociability after surgery (e.g. psychological and behavioural impact), and patients' preference for a specific RCPPS procedure in trials with a split‐mouth design (Needleman 2005b; Ng 2006; Ozcelik 2007; Roccuzzo 2002). Consequently, patients and professionals can present different points of view regarding the performed procedures and the achieved final result.
With respect to patient‐centred evaluations, some studies evaluated aesthetics and pain/discomfort through the use of visual scales or similar instruments (Ahmedbeyli 2014; Jankovic 2010; Jepsen 2013; McGuire 2014; McGuire 2016; Zucchelli 2014; Zucchelli 2014b). The visual analogue scale (VAS) is a tool that has been used to evaluate the levels of discomfort and pain subsequent to different modalities of periodontal treatment (Checchi 1993; Fardal 2002; Karadottir 2002; Matthews 1993). This resource can be applied to evaluate various aesthetic and functional individual outcomes. In another study (Jørnung 2007) the use of VAS showed that the opinion of the patients with respect to their own smile was statistically significantly better than the opinion of two different clinicians, highlighting that the patient's individual perception can influence clinical decision making choice. On the other hand, both patients and clinicians (i.e. general dentists and periodontists) seem to agree that, in terms of aesthetic perception, complete root coverage is perceived as the primary 'successful outcome' of a RCPPS procedure (Rotundo 2008). Another interesting scale developed for professional aesthetical evaluation, the root‐coverage esthetic score (RES) (Cairo 2009), might be adapted to assist patients in performing more accurate assessments of five important items: gingival margin, soft tissue texture, gingival colour, and marginal tissue contour. In addition, it is important to highlight that patients' perception of buccal recessions is not high (approximately half of the patients with one gingival recession do not perceive them), as well as that the majority of those defects do not lead to functional or aesthetic concerns (Nieri 2013).
The great variability in the percentages of sites with complete and mean root coverage is probably associated with a set of factors such as the type of defect, amount and quality of adjacent gingival tissue, sample size and the applied inclusion criteria (e.g. patients' selection, methodological quality, type of technique, devices used for measurements and differences between operators). It seems that the amount of root coverage obtained is associated with initial recession anatomy. Better results in terms of percentage of complete and mean root coverage can be expected when baseline recession defects are < 4 mm (Berlucchi 2005), at the same time flaps with < 1 mm thickness can harm the achievement of complete root coverage (Baldi 1999; Berlucchi 2005). It has been demonstrated by an individual patient data meta‐analysis of 602 Miller Class I and II recession defects (Chambrone 2012) that the greater the baseline recession depth, the smaller the chance of achieving complete root coverage. Moreover, another couple of studies (Nieri 2009; Pini Prato 2005) demonstrated that sites in which the gingival margin was sutured at the level of the cemento‐enamel junction the achievement of complete root coverage was inferior to those sites where the flap was sutured coronal (approximately 1 mm to 2 mm) (i.e. the more apical the gingival margin after surgery, the smaller the chance of complete root coverage). Thick and wide interproximal dental papillae can positively influence the percentage of complete root coverage (Berlucchi 2005; Saletta 2001), however, their baseline anatomy is directly associated with the distance from the contact point to the bone crest. When the measurement from the contact point to the bone crest is 5 mm or less, the papilla is present almost 100% of the time, whereas, when the distance is 6 mm, the papilla is present 56% of the time (Tarnow 1992). When this distance is between 7 mm to 10 mm the papilla is missing most of the time (Tarnow 1992). It should also be noted that the inclusion of studies with recession defects ≥ 4 mm tends to show greater differences between baseline and follow‐up means (i.e. outcome change), a factor that may influence the calculation of meta‐analyses.
With respect to flap tension, it has been suggested that the higher the flap tension, the lower the recession reduction (Pini Prato 2000). Consequently, all theses factors make comparisons and combination of data from different trials a critical issue. In this way, trials investigating the treatment of gingival recession with similar baseline characteristics or which have included baseline and final individual defects measurements will allow more effective evaluations of each surgical technique, as well as facilitating future meta‐analyses.
It has been shown that smoking can affect the results obtained by RCPPS procedures (Chambrone 2009). Two RCTs (Costa 2016; Reino 2012) evaluated only patients who smoked ≥ 10 cigarettes per day for at least 5 years, and their showed that heavy smokers may be benefited by root coverage therapy, as well. On the other hand, mean root coverage and complete root coverage were clearly inferior to the outcomes achieved by trials evaluating non‐smokers (Additional Table 9). Eight trials reported the inclusion of smokers (Bouchard 1994; Bouchard 1997; Jepsen 2013; McGuire 2012; Spahr 2005; Zucchelli 2009; Zucchelli 2014; Zucchelli 2014b) who smoked less than 10 cigarettes per day. None of them performed comparisons between smokers and non‐smokers. Zucchelli 1998 commented only that patients who smoke more than 10 cigarettes a day presented the worst percentage of root coverage. This is in line with included RCTs on smokers (Costa 2016; Reino 2012) and the data from other studies that have compared the amount of root coverage obtained by smokers and non‐smokers through CAF (Silva 2007) and SCTG (Erley 2006; Martins 2004). Similarly, root modification agents (e.g. tetracycline solution and citric acid) and the type of mechanical root scaling associated to the RCPPS procedure (i.e. CAF) were evaluated in few studies. Nevertheless, these RCTs have suggested that there is no significant clinical benefit of root conditioning in conjunction with root coverage procedures (Additional Table 7; Table 9).
Since 2002, some extensive systematic reviews have evaluated the effects of PPS procedures in the treatment of recession defects. Roccuzzo 2002 used stringent inclusion criteria, but it also included non‐randomised trials, gingival recessions < 3 mm and did not evaluate changes in the width of keratinized tissue or the use of biomaterial such as acellular dermal matrix grafts. Oates 2003 included only RCTs and its inclusion criteria were only based on the terms 'human study, English language, and therapeutic study including the use of a gingival surgical procedure to treat gingival recession'. Chambrone 2008 focused mainly on the treatment of recession defects with SCTG. These reviews did not include searches for unpublished data (i.e. grey literature), papers published in all languages (Chambrone 2008; Oates 2003; Roccuzzo 2002) or evaluation of the risk of bias (Oates 2003; Roccuzzo 2002). However, their results were similar to ours. Additionally, the present version of this Cochrane Review is also in completely line with data from the recent American Academy of Periodontology Regeneration Workshop systematic review that concluded that: 1. "all RCPPS procedures can provide significant reduction in recession depth and clinical attachment level gain without alteration of probing depth for Miller Class I and II localized recession‐type defects, but multiple recession‐type defects seems to be benefit as well despite the reduced quantity of information available;" 2. "SCTG‐based procedures provided the best outcomes for clinical practice because of their superior percentages of mean root coverage and complete root coverage and the significant increase of keratinized tissue when compared with most of the other procedures" (as reported by the individual studies' outcomes, additional Table 9); 3. "the use of CAF with ADMG, EMP, and XCM also provided gains, many of them similar to SCTG‐based procedures, and thus these may be considered as adequate substitute treatment approaches"; and 4. "smoking may decrease the expected results" (Chambrone 2015).
It is also important to highlight that recent evidence from two long‐term non‐randomised studies that followed patients for at least 20 years found that gingival recessions recurrence/relapse appears to be more associated to sites lacking an attached keratinized tissue band of at least 2 mm (Agudio 2017; Pini Prato 2018). Similarly, a recent systematic review (Chambrone 2016) evaluating the long‐term outcomes of untreated buccal recession‐type defects (in terms of associated reported aesthetic and functional alterations and factors influence the progression/worsening of dental and periodontal tissue conditions) found that: 1. untreated buccal recession defects in individuals with good oral hygiene are highly likely to experience recession depth increase during long‐term follow‐up (≥ 5 years) ‐ 78% of the defects displayed clinical worsening; and 2. the presence of keratinized tissue band and/or greater keratinized tissue width decrease the chance of recession depth increase or the development of new recessions. Nonetheless, individual data from some of the studies included in the systematic review suggest that SCTG promoted better stability of the gingival margin/some degree of creeping attachment over time, compared to other surgical approaches (Abolfazli 2009; Jepsen 2013; McGuire 2012; McGuire 2016; Tunali 2015).
Several trials on periodontal plastic surgery have been performed evaluating different procedures as control groups. They have evidenced the lack of a standard procedure that could be considered as gold standard (i.e. control group) for the majority of trials. In this review, the exclusion of non‐randomised studies and the use of stringent inclusion criteria may have led to the loss of evidence‐based information since only studies which compared two (or more) active treatments were studied (since a placebo or no control treatment group were not possible). Studies that evaluated recession defects < 3 mm were also excluded. Overall, data from the included studies indicate that the SCTG is the procedure that can become this gold standard; however, further research on this matter is needed.
In addition, similar to another Cochrane Review (Esposito 2005), the majority of included RCTs were often performed on patients presenting different clinical and systemic conditions from those currently found in a conventional private practice. These conditions can cause more variability of the results when extrapolated to daily practice.
Authors' conclusions
Implications for practice.
All the analysed root coverage periodontal plastic surgery (RCPPS) procedures led to gains in gingival recession (i.e. recession depth decrease and clinical attachment level gain) and thus can be used in clinical practice. However, there was a great variability in the percentages of complete root coverage and mean root coverage.
The available evidence base indicates that subepithelial connective tissue grafts (SCTG) plus coronally advanced flap (CAF), CAF alone or associated with biomaterial (e.g. acellular dermal matrix grafts (ADMG), enamel matrix protein (EMP) and xenogeneic collagen matrix (XCM) and guided tissue regeneration (GTR)) may be used as root coverage procedures for the treatment of recession‐type defects. The available information on the use of platelet‐rich fibrin associated to CAF is very scarce and it precludes formal accurate comparisons with CAF alone or CAF plus SCTG or other biomaterial. In case where both root coverage and gain in the width of keratinized tissue are expected, the available evidence base suggests the use of SCTG seems to be more adequate.
Individual studies' outcomes and some weak evidence obtained by the available pooled estimates suggest that SCTG plus CAF may be considered as 'gold standard' procedure for the treatment of recession‐type defects. Moreover, evidence suggests that SCTG promoted better stability of the gingival margin/some degree of creeping attachment over time, compared to other surgical approaches.
Acellular dermal matrix grafts (primarily) and XCM (secondly) may be considered as alternatives in cases where SCTG harvested from the palate could not be used.
Outcome measures of the evaluated surgical techniques were not improved by the use of root modification agents (e.g. citric acid or tetracycline solution) or the type of mechanical root scaling (i.e. ultrasonic or manual) during surgery. Overall, outcomes from few individual studies indicated equivalent improvements for sites treated with these chemical/mechanical procedures or not.
The incidence of adverse effects, such as discomfort with or without pain, was mainly related to donor sites of SCTG. However, these conditions occurred mainly within the first week after surgery and did not influence on root coverage outcomes.
The potential impact of bias on these outcomes (primary and secondary) is unclear.
Implications for research.
Limited data exist on aesthetic condition change related to patient's opinion, thus further randomised controlled trials (RCTs) are still required to evaluate this primary outcome variable.
Future split‐mouth trials should focus on patients' preference for a specific periodontal plastic surgery procedure.
Precise and objective aesthetic evaluations should be included in future studies. The use of the visual analogue scale (VAS) will allow more precise evaluations of patient‐based outcomes.
The inclusion of baseline and final individual defect measurements will allow more precise evaluations, as well as subgroup evaluations (e.g. patients presenting similar defects) and future comparisons via meta‐analyses. These outcome measures should include gingival recession depth and width, clinical attachment level, width and thickness of keratinized tissue, and root surface conditions (i.e. presence of caries, abrasions or restorations).
Comparisons between different operators (i.e. with respect to the degree of operator's experience) remain necessary to evaluate differences in the expected outcome measures.
Multicentre studies may favour the inclusion and evaluation of larger samples of patients and therefore the achievement of statistical power.
Considering the proposed inclusion criteria, no data were available for lateral positioned flaps and there is limited information for free gingival grafts and platelet‐rich fibrin. These procedures might be evaluated by future research.
More long‐term RCTs are necessary to adequately confirm and identify possible factors associated with the prognosis and indications of each root coverage periodontal plastic surgery procedure. CONSORT should be considered when designing and reporting future studies (www.consort‐statement.org/) .
What's new
| Date | Event | Description |
|---|---|---|
| 11 October 2018 | Amended | Co‐author name correction. |
History
Protocol first published: Issue 2, 2008 Review first published: Issue 2, 2009
| Date | Event | Description |
|---|---|---|
| 25 September 2018 | New citation required and conclusions have changed |
|
| 15 January 2018 | New search has been performed | Searches were updated up to 15 January 2018. |
Acknowledgements
The review authors would like to acknowledge Anne Littlewood for her assistance on the search strategy section and Helen Worthington, Ian Needleman, Luisa Fernandez Mauleffinch and Marco Esposito from Cochrane Oral Health for their help with the preparation of the protocol and full text of the review. We would like to thank Professor Kevin Seymour from Division of Dentistry, School of Medical Sciences, Faculty of Biology, Medicine and Health, the University of Manchester for providing comments on this update.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
1 ((recession and gingiva*) or (recession and defect*) or "recession‐type defect*"):ti,ab 2 ((exposure near root*) or (exposed near root*)):ti,ab 3 (denude* near "root surface*"):ti,ab 4 (gingiva* near defect*):ti,ab 5 #1 or #2 or #3 or #4 6 (tissue near regenerat*):ti,ab 7 ((gingiva* near esthetic*) or (gingiva* near aesthetic*)):ti,ab 8 (periodont* and "plastic surgery"):ti,ab 9 ("soft tissue graft" or "coronally advanced flap*"):ti,ab 10 ("laterally positioned flap*" or "laterally‐positioned flap*"):ti,ab 11 ("connective tissue graft*" or "connective‐tissue graft*"):ti,ab 12 (gingiva* near transplant*):ti,ab 13 ("dermal matrix" near graft*):ti,ab 14 "enamel matrix protein":ti,ab 15 #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 16 (#5 and #15) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 [mh ^"gingival recession"] #2 ((recession near gingiva*) or (recession near defect*) or "recession‐type defect*") #3 ((exposure near root*) or (exposed near root*)) #4 (gingiva* near defect*) #5 (denude* near "root surface*") #6 {or #1‐#5} #7 [mh ^"Guided tissue regeneration"] #8 (tissue near regenerat*) #9 ((gingiva* near esthetic*) or (gingiva* near aesthetic*)) #10 (periodont* and "plastic surgery") #11 ("soft tissue graft" or "coronally advanced flap*") #12 ("laterally positioned flap*" or "laterally‐positioned flap*") #13 ("connective tissue graft*" or "connective‐tissue graft*") #14 (gingiva* near transplant*) #15 ("dermal matrix" near graft*) #16 "enamel matrix protein" #17 {or #7‐#16} #18 #6 and #17
Appendix 3. MEDLINE Ovid search strategy
1. Gingival recession/ 2. ((recession adj5 gingiva$) or (recession adj5 defect$) or "recession‐type defect$").ti,ab. 3. ((exposure adj5 root$) or (exposed adj5 root$)).ti,ab. 4. (gingiva$ adj5 defect$).ti,ab. 5. (denude$ adj5 "root surface$").ti,ab. 6. or/1‐5 7. exp Guided tissue regeneration/ 8. (tissue adj5 regenerat$).ti,ab. 9. ((gingiva$ adj5 esthetic$) or (gingiva$ adj5 aesthetic$)).ti,ab. 10. (periodont$ and "plastic surgery").ti,ab. 11. ("soft tissue graft$" or "coronally advanced flap$").ti,ab. 12. "laterally positioned flap$".ti,ab. 13. "connective tissue graft$".ti,ab. 14. (gingiva$ adj5 transplant$).ti,ab. 15. ("dermal matrix" adj5 graft$).ti,ab. 16. "enamel matrix protein".ti,ab. 17. or/7‐16 18. 6 and 17
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐ maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of theCochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011) (Lefebvre 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. Gingiva disease/ 2. ((recession adj5 gingiva$) or (recession adj5 defect$) or "recession‐type defect$").ti,ab. 3. ((exposure adj5 root$) or (exposed adj5 root$)).ti,ab. 4. (gingiva$ adj5 defect$).ti,ab. 5. (denude$ adj5 "root surface$").ti,ab. 6. or/1‐5 7. Tissue regeneration/ 8. (tissue adj5 regenerat$).ti,ab. 9. ((gingiva$ adj5 esthetic$) or (gingiva$ adj5 aesthetic$)).ti,ab. 10. (periodont$ and "plastic surgery").ti,ab. 11. ("soft tissue graft$" or "coronally advanced flap$").ti,ab. 12. "laterally positioned flap$".ti,ab. 13. "connective tissue graft$".ti,ab. 14. (gingiva$ adj5 transplant$).ti,ab. 15. ("dermal matrix" adj5 graft$).ti,ab. 16. "enamel matrix protein".ti,ab. 17. or/7‐16 18. 6 and 17
The above subject search was linked to adapted version of the Cochrane Embase Project filter for identifying randomised controlled trials in Embase Ovid (see http://www.cochranelibrary.com/help/central‐creation‐details.html for information):
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomisation/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
recession AND tissue regeneration
Appendix 6. World Health Organization International Clinical Trials Registry Platform search strategy
recession AND tissue regeneration
root coverage
Data and analyses
Comparison 1. ADMG + CAF versus SCTG +CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 4 | 100 | Mean Difference (Random, 95% CI) | ‐0.36 [‐1.03, 0.30] |
| 1.1 Split‐mouth design | 2 | 50 | Mean Difference (Random, 95% CI) | ‐0.64 [‐2.06, 0.78] |
| 1.2 Parallel design | 2 | 50 | Mean Difference (Random, 95% CI) | ‐0.10 [‐0.62, 0.43] |
| 2 Clinical attachment level change | 4 | 100 | Mean Difference (Random, 95% CI) | ‐0.53 [‐1.14, 0.08] |
| 2.1 Split‐mouth design | 2 | 50 | Mean Difference (Random, 95% CI) | ‐0.92 [‐1.78, ‐0.06] |
| 2.2 Parallel design | 2 | 50 | Mean Difference (Random, 95% CI) | ‐0.04 [‐0.63, 0.55] |
| 3 Keratinized tissue width change | 4 | 100 | Mean Difference (Random, 95% CI) | ‐0.59 [‐1.27, 0.10] |
| 3.1 Split‐mouth design | 2 | 50 | Mean Difference (Random, 95% CI) | 0.07 [‐0.40, 0.53] |
| 3.2 Parallel design | 2 | 50 | Mean Difference (Random, 95% CI) | ‐1.11 [‐1.59, ‐0.63] |
| 4 Sites with complete root coverage | 2 | 50 | Odds Ratio (Random, 95% CI) | 0.43 [0.13, 1.37] |
| 4.1 Parallel design | 2 | 50 | Odds Ratio (Random, 95% CI) | 0.43 [0.13, 1.37] |
Comparison 2. ADMG + CAF versus CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 50 | Mean Difference (Random, 95% CI) | 0.61 [‐0.52, 1.73] |
| 2 Clinical attachment level change | 2 | 50 | Mean Difference (Random, 95% CI) | 0.51 [‐0.25, 1.27] |
| 3 Keratinized tissue width change | 2 | 50 | Mean Difference (Random, 95% CI) | 0.28 [‐0.08, 0.64] |
| 4 Sites with complete root coverage | 2 | 50 | Odds Ratio (Random, 95% CI) | 3.97 [0.20, 80.50] |
Comparison 3. EMP + CAF versus CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 3 | 136 | Mean Difference (Random, 95% CI) | 0.07 [‐0.25, 0.40] |
| 2 Clinical attachment level change | 3 | 136 | Mean Difference (Random, 95% CI) | 0.22 [‐0.02, 0.45] |
| 3 Keratinized tissue width change | 3 | 136 | Mean Difference (Random, 95% CI) | 0.35 [0.13, 0.56] |
Comparison 4. EMP + CAF versus CAF ‐ short/medium term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 3 | 124 | Mean Difference (Random, 95% CI) | 0.32 [0.10, 0.55] |
| 1.1 6 months (short term) | 1 | 34 | Mean Difference (Random, 95% CI) | 0.51 [0.06, 0.96] |
| 1.2 24 months (medium term) | 2 | 90 | Mean Difference (Random, 95% CI) | 0.26 [‐0.03, 0.54] |
| 2 Clinical attachment level change | 3 | 124 | Mean Difference (Random, 95% CI) | 0.35 [0.09, 0.61] |
| 2.1 6 months (short term) | 1 | 34 | Mean Difference (Random, 95% CI) | 0.52 [‐0.14, 1.18] |
| 2.2 24 months (medium term) | 2 | 90 | Mean Difference (Random, 95% CI) | 0.32 [0.03, 0.61] |
| 3 Keratinized tissue width change | 3 | 124 | Mean Difference (Random, 95% CI) | 0.40 [0.17, 0.62] |
| 3.1 6 months (short term) | 1 | 34 | Mean Difference (Random, 95% CI) | 0.06 [‐0.73, 0.85] |
| 3.2 24 months (medium term) | 2 | 90 | Mean Difference (Random, 95% CI) | 0.43 [0.19, 0.66] |
Comparison 5. EMP + CAF versus SCTG + CAF ‐ short/medium term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 58 | Mean Difference (Random, 95% CI) | ‐0.39 [‐1.27, 0.48] |
| 1.1 Split‐mouth design | 2 | 58 | Mean Difference (Random, 95% CI) | ‐0.39 [‐1.27, 0.48] |
| 2 Clinical attachment level change | 2 | 62 | Mean Difference (Random, 95% CI) | ‐0.25 [‐0.69, 0.20] |
| 2.1 Split‐mouth design | 2 | 62 | Mean Difference (Random, 95% CI) | ‐0.25 [‐0.69, 0.20] |
| 3 Keratinized tissue width change | 2 | 62 | Mean Difference (Random, 95% CI) | ‐1.06 [‐1.36, ‐0.76] |
| 3.1 Split‐mouth design | 2 | 62 | Mean Difference (Random, 95% CI) | ‐1.06 [‐1.36, ‐0.76] |
| 4 Sites with complete root coverage | 2 | 62 | Odds Ratio (Random, 95% CI) | 0.61 [0.05, 7.86] |
| 4.1 Split‐mouth design | 2 | 62 | Odds Ratio (Random, 95% CI) | 0.61 [0.05, 7.86] |
Comparison 6. GTR rm + CAF versus SCTG + CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 3 | 98 | Mean Difference (Random, 95% CI) | ‐0.37 [‐0.60, ‐0.13] |
| 1.1 Split‐mouth design | 1 | 32 | Mean Difference (Random, 95% CI) | ‐0.3 [‐0.67, 0.07] |
| 1.2 Parallel design | 2 | 66 | Mean Difference (Random, 95% CI) | ‐0.41 [‐0.72, ‐0.11] |
| 2 Clinical attachment level change | 3 | 98 | Mean Difference (Random, 95% CI) | 0.35 [0.06, 0.63] |
| 2.1 Split‐mouth design | 1 | 32 | Mean Difference (Random, 95% CI) | 0.5 [0.06, 0.94] |
| 2.2 Parallel design | 2 | 66 | Mean Difference (Random, 95% CI) | 0.23 [‐0.13, 0.60] |
| 3 Keratinized tissue width change | 3 | 98 | Mean Difference (Random, 95% CI) | ‐1.77 [‐2.66, ‐0.89] |
| 3.1 Split‐mouth design | 1 | 32 | Mean Difference (Random, 95% CI) | ‐0.4 [‐1.32, 0.52] |
| 3.2 Parallel design | 2 | 66 | Mean Difference (Random, 95% CI) | ‐2.33 [‐2.62, ‐2.03] |
| 4 Sites with complete root coverage | 3 | 98 | Odds Ratio (Random, 95% CI) | 0.61 [0.30, 1.24] |
| 4.1 Split‐mouth design | 1 | 32 | Odds Ratio (Random, 95% CI) | 1.0 [0.37, 2.68] |
| 4.2 Parallel design | 2 | 66 | Odds Ratio (Random, 95% CI) | 0.37 [0.14, 1.01] |
Comparison 7. GTR rm + CAF versus GTR nrm + CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 60 | Mean Difference (Random, 95% CI) | 0.23 [‐0.22, 0.68] |
| 2 Clinical attachment level change | 2 | 60 | Mean Difference (Random, 95% CI) | 0.12 [‐0.37, 0.60] |
| 3 Keratinized tissue width change | 2 | 60 | Mean Difference (Random, 95% CI) | 0.12 [‐0.23, 0.48] |
| 4 Sites with complete root coverage | 2 | 60 | Odds Ratio (Random, 95% CI) | 1.33 [0.46, 3.85] |
Comparison 8. GTR rm + bone substitutes + CAF versus SCTG + CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 54 | Mean Difference (Random, 95% CI) | ‐0.82 [‐2.13, 0.49] |
| 2 Clinical attachment level change | 2 | 54 | Mean Difference (Random, 95% CI) | ‐0.52 [‐1.34, 0.30] |
| 3 Keratinized tissue width change | 2 | Mean Difference (Random, 95% CI) | ‐2.38 [‐2.84, ‐1.92] |
Comparison 9. GTR rm + bone substitutes + CAF versus GTR rm + CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 54 | Mean Difference (Random, 95% CI) | 0.48 [0.09, 0.88] |
| 2 Clinical attachment level change | 2 | 54 | Mean Difference (Random, 95% CI) | 0.76 [‐0.01, 1.54] |
| 3 Keratinized tissue width change | 2 | 54 | Mean Difference (Random, 95% CI) | 0.23 [‐0.21, 0.68] |
| 4 Sites with complete root coverage | 2 | 54 | Odds Ratio (Random, 95% CI) | 1.87 [0.75, 4.64] |
Comparison 10. XCM + CAF versus CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | 104 | Mean Difference (Random, 95% CI) | 0.40 [0.11, 0.68] |
| 2 Clinical attachment level change | 2 | 104 | Mean Difference (Random, 95% CI) | 0.37 [‐0.09, 0.83] |
| 3 Keratinized tissue width change | 2 | 104 | Mean Difference (Random, 95% CI) | 0.44 [0.04, 0.85] |
| 4 Sites with complete root coverage | 2 | 104 | Odds Ratio (Random, 95% CI) | 4.73 [2.35, 9.50] |
Comparison 11. PRF + CAF versus SCTG +CAF ‐ short term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival recession depth change | 2 | Mean Difference (Random, 95% CI) | ‐0.01 [‐0.89, 0.86] | |
| 1.1 Split‐mouth design | 2 | Mean Difference (Random, 95% CI) | ‐0.01 [‐0.89, 0.86] | |
| 2 Clinical attachment level change | 2 | Mean Difference (Random, 95% CI) | ‐0.37 [‐0.69, ‐0.06] | |
| 2.1 Split‐mouth design | 2 | Mean Difference (Random, 95% CI) | ‐0.37 [‐0.69, ‐0.06] | |
| 3 Keratinized tissue width change | 2 | Mean Difference (Random, 95% CI) | ‐0.26 [‐0.98, 0.45] | |
| 3.1 Split‐mouth design | 2 | Mean Difference (Random, 95% CI) | ‐0.26 [‐0.98, 0.45] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abolfazli 2009.
| Methods | RCT, split‐mouth design, 2 treatment groups, 24 months' duration | |
| Participants | 12 individuals, 8 females, aged 28 to 51 years, with 2 bilateral Miller Class I buccal gingival recessions of at least 3 mm | |
| Interventions | 1. EMD + CAF 2. SCTG + CAF |
|
| Outcomes | GRC*(2) CALC*(2) KTC*(2) SCRC PCRC*(2) MRC*(2) (Manual probe) |
|
| Notes | Practice‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Ahmedbeyli 2014.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 24 individuals, 12 females, aged 22 to 40 years, with Miller Class I multiple buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + CAF 2. CAF |
|
| Outcomes | ACC GRC*(1) CALC*(1) KTC*(1) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other types of bias was not detected |
Ayub 2012.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 15 individuals, number of females not reported, aged 20 to 56 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG (positioned 1 mm apical to the cemento‐enamel junction) + CAF (extended flap) 2. ADMG + CAF (extended flap) |
|
| Outcomes | GRC*(1) CALC*(1) KTC SCRC PCRC MRC (Automated controlled force probe and manual probe) |
|
| Notes | University/hospital‐based and supported by the State of São Paulo Research Foundation and BioHorizons Inc | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomly permuted block |
| Allocation concealment (selection bias) | Low risk | Adequate ‐ sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Babu 2011.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 10 individuals, number of females not reported, age not reported, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. GTR + CAF (collagen membrane ‐ Bioproducts Lab) 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Unclear risk | Between groups comparisons regarding baseline recession depth were not reported |
| Other bias | Low risk | Evidence of other bias was not detected |
Barros 2015.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 15 individuals, 10 females, aged 23 to 54 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + CAF (extended flap) 2. SCTG + CAF (extended flap) |
|
| Outcomes | GRC CALC KTC MRC (Automated controlled force probe ‐ 0.50 N) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Bouchard 1994.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 30 individuals, 24 females, aged 21 to 62 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + CAF + CA (graft without epithelial collar) 2. SCTG (graft with epithelial collar) |
|
| Outcomes | ACC GRC CALC KTC SCRC PCRC MRC (Automated controlled force probe ‐ 0.50 N) |
|
| Notes | Practice‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Bouchard 1997.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 30 individuals, 25 females, aged 21 to 70 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + CAF + TTC‐HCl 2. SCTG + CAF + CA |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Automated controlled force probe ‐ 0.50 N) |
|
| Notes | Practice‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Costa 2016.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals (heavy smokers ‐ 10 or more cigarettes/day for over 5 years), 12 females, aged 30 to 50 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + EMD + CAF (extended flap) 2. ADMG + CAF (extended flap) |
|
| Outcomes | GRC*(1) CALC KTC SCRC PCRC MRC (Automated controlled force probe and compass) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "method of randomly allocating by simple draw" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 patient did not return for clinical evaluation at 6 months Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not be expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
da Silva 2004.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 11 individuals, 5 females, aged 18 to 43 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. SCTG + CAF 2. CAF |
|
| Outcomes | GRC CALC KTC*(1) SCRC PCRC MRC (Automated controlled force probe) |
|
| Notes | University/hospital‐based Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
de Queiroz 2006.
| Methods | RCT, split‐mouth design, 2 treatment groups, 24 months' duration | |
| Participants | 13 individuals, 7 females, mean age 32.8 years, with 2 bilateral Miller Class I buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + CAF 2. CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based Data from earlier article (de Queiroz 2004) were reported as part of this trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Del Pizzo 2005.
| Methods | RCT, split‐mouth design, 2 treatment groups, 24 months' duration | |
| Participants | 15 individuals, 11 females, aged 18 to 56 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. EMP + CAF 2. CAF |
|
| Outcomes | GRC CALC KTC*(1) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Dodge 2000.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 12 individuals, 8 females, aged 23 to 51 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) + TTC‐HCl + DFDBA 2. GTR (polylactic acid membrane ‐ Guidor) + TTC‐HCl |
|
| Outcomes | GRC CALC*(1) KTC*(1) SCRC PCRC MRC (Manual probe) |
|
| Notes | Practice‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Henderson 2001.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 10 individuals, 5 females, aged 24 to 68 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG (connective tissue side against the tooth) + CAF 2. ADMG (basement membrane side against the tooth) + CAF |
|
| Outcomes | GRC CALC KTC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Lifecore Biomedical | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Jaiswal 2012.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals, 8 females, aged 25 to 56 years, with Miller Class II multiple buccal gingival recessions of at least 3 mm | |
| Interventions | 1. EMD + CAF 2. CAF |
|
| Outcomes | GRC*(1) CALC*(1) KTC MRC (Automated controlled force probe ‐ 15g) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Jankovic 2010.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 20 individuals, 12 females, aged 21 to 48 years, with bilateral Miller Class I and II maxillary buccal gingival recessions of at least 3 mm | |
| Interventions | 1. Platelet‐rich fibrin + CAF 2. EMD + CAF |
|
| Outcomes | GRC KTC*(2) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Jepsen 2013.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 35 individuals, age > 18 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. XCM + CAF 2. CAF |
|
| Outcomes | GRC*(1) CALC KTC*(1) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Geistlich Pharma AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Joly 2007.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 10 individuals, 4 females, aged 24 to 68 years, with 2 Miller Class I or II maxillary buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + CAF (flap without vertical incisions) 2. SCTG + CAF (flap without vertical incisions) |
|
| Outcomes | GRC*(2) CALC*(2) KTC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Keceli 2008.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 40 individuals, 30 females, aged 18 to 60 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm. 36 individuals completed the study | |
| Interventions | 1. SCTG + platelet‐rich plasma + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by The Research Foundation of Hacettepe University | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The first patient was selected in one of the two experimental groups by coin toss, and the next patient was consecutively added to the opposite group by one of the authors" |
| Allocation concealment (selection bias) | High risk | Quote: "The first patient was selected in one of the two experimental groups by coin toss, and the next patient was consecutively added to the opposite group by one of the authors" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are missing in both intervention groups (4 patients discontinued the study between 6‐ to 12‐month evaluations due to moving to another city). Thus, decision to move house away from the geographical location to another is unlikely to be connected with their subsequent outcome |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Keceli 2015.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 40 individuals, 27 females, aged 22 to 50 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + platelet‐rich fibrin + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC*(1) (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Number‐labeled opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Patients were not blinded to the root coverage procedure |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Leknes 2005.
| Methods | RCT, split‐mouth design, 2 treatment groups, 72 months' duration | |
| Participants | 20 individuals, 10 females, mean age 38.4 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm. 11 individuals completed the study | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) 2. CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Automated controlled force probe and manual probe) |
|
| Notes | University/hospital‐based and membranes provided by Guidor AB Unpublished data were included following contact with author Data from earlier article (Amarante 2000) were reported as part of this trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 11 out of 20 subjects were available for the final evaluation (6 subjects rejected to complete the study and 3 moved to other part of Norway) Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other was not detected |
Matarasso 1998.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 20 individuals, 8 females, aged 18 to 42 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) + double papilla flap 2. GTR (polylactic acid membrane ‐ Guidor) + CAF |
|
| Outcomes | GRC CALC KTC MRC (Manual probe) |
|
| Notes | University/hospital‐based Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
McGuire 2012.
| Methods | RCT, split‐mouth design, 2 treatment groups, 5 years' duration | |
| Participants | 20 individuals, 10 females, aged 23 to 62 years, with 2 Miller Class II maxillary buccal gingival recessions of at least 4 mm. 19 individuals completed the 6‐month follow‐up, 17 completed the 12‐month follow‐up, and 9 the 5‐year follow‐up | |
| Interventions | 1. EMP + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC*(2) PCRC MRC (Manual probe) |
|
| Notes | Practice‐based and supported by BIORA AB (currently Straumann) Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Adequate ‐ sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 patients did not complete the 12‐month follow‐up: 1 participant dropped out because he had moved out of the country (where the RCT was conducted), 1 had a change in job and could not comply with study schedule and 1 was not compliant and was exited from the trial. Moreover, at the 10‐year final evaluation, just 9 out 17 patients available at short‐term assessment were available/agreed to be re‐evaluated (reasons were not reported) Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not to be expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
McGuire 2014.
| Methods | RCT, split‐mouth design, 2 treatment groups, 5 years' duration | |
| Participants | 30 individuals, 26 females, aged 18 to 70 years, with 2 Miller Class II buccal gingival recessions of at least 3 mm. 30 individuals completed the 6 months follow‐up, whereas 20 the 5 years follow‐up | |
| Interventions | 1. Beta‐tricalcium phosphate (b‐TCP) + recombinant human platelet‐derived growth factor‐B with a bioabsorbable collagen wound‐healing dressing + CAF 2. SCTG + CAF |
|
| Outcomes | ACC GRC*(2) CALC KTC*(2) SCC PCRC MRC (Manual probe) |
|
| Notes | Practice‐based and supported by Osteohealth Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Adequate ‐ sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the initial 6‐month evaluation, but 20 out 30 were available for follow‐up 5 years after the original recession‐related surgery (reasons were not reported) Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not to be expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
McGuire 2016.
| Methods | RCT, split‐mouth design, 2 treatment groups, 5 years' duration | |
| Participants | 25 individuals, 17 females, aged 18 to 70 years, with 2 Miller Class II buccal gingival recessions of at least 3 mm. 23 individuals completed the 12 months follow‐up, whereas 17 the 5 years follow‐up | |
| Interventions | 1. XCM + CAF 2. SCTG + CAF |
|
| Outcomes | ACC GRC*(2) CALC*(2) KTC SCC PCRC MRC (Manual probe) |
|
| Notes | Practice‐based and supported by Giestlich Pharma AG Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Adequate ‐ sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The 25 patients included in the study completed the initial 6‐month follow‐up, whereas 17 were available for a 5‐year recall (quote: "seven patients unavailable for recall had moved, were not reachable, or had conflicting engagements, and one had received a class 5 restoration that eradicated the baseline measurement reference point") Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not to be expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Ozenci 2015.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 20 individuals, 13 females, aged 22 to 42 years, with Miller Class I multiple buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + Tunnel (CAF) 2. ADMG + CAF |
|
| Outcomes | ACC*(2) GRC*(2) CALC*(2) KTC*(2) SCC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Paolantonio 1997.
| Methods | RCT, parallel design, 2 treatment groups, 60 months' duration | |
| Participants | 70 individuals, 38 females, aged 25 to 48 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + double papilla flap 2. FGG |
|
| Outcomes | GRC*(1) KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | Practice‐based Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Paolantonio 2002.
| Methods | RCT, parallel design, 3 treatment groups, 12 months' duration | |
| Participants | 45 individuals, 31 females, aged 27 to 51 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) 2. GTR (polylactic acid membrane ‐ Paroguide) + hydroxyapatite/collagen/chondroitin‐sulfate graft 3. SCTG + double papilla flap |
|
| Outcomes | GRC CALC KTC*(3) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Italian Ministry of University and Scientific Research Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Paolantonio 2002b.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 30 individuals, 19 females, aged 29 to 51 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. ADMG + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC*(2) SCRC PCRC MRC (Automated controlled force probe ‐ 20 g and calliper) |
|
| Notes | University/hospital‐based and supported by Italian Ministry of University and Scientific Research Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Pendor 2014.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals, 6 females, aged 25 to 46 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + double pedicle flap 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Automated controlled force probe ‐ 15 g and calliper) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Rasperini 2011.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 56 individuals, 39 females, mean 35.5 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. EMD + SCTG + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random permuted blocks |
| Allocation concealment (selection bias) | Low risk | Central registration |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Reino 2012.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 12 individuals (heavy smokers ‐ 20 or more cigarettes per day for more than 5 years), 10 females, aged 35 to 50 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. SCTG + CAF (extended flap) 2. SCTG + CAF |
|
| Outcomes | SCRC PCRC MRC (Automated controlled force probe and manual probe) |
|
| Notes | University/hospital‐based and supported by the State of São Paulo Research Foundation, São Paulo, Brazil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Unclear risk | Baseline and follow‐up means regarding recession depth, clinical attachment level and keratinized tissue width were not reported in the study |
| Other bias | Low risk | Evidence of other bias was not detected |
Reino 2015.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals, 14 females, aged 26 to 46 years, with 2 bilateral Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. XCM + CAF (extended flap) 2. XCM + CAF |
|
| Outcomes | GRC*(1) CALC KTC MRC (Automated controlled force probe and calliper) |
|
| Notes | University/hospital‐based and supported by the State of São Paulo Research Foundation, São Paulo, Brazil and Geistlich Pharma AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomly permuted block |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Roccuzzo 1996.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 12 individuals, 3 females, aged 21 to 31 years, with 2 Miller Class I or II buccal gingival recessions of at least 4 mm | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) 2. GTR (ePTFE membrane ‐ Gore‐Tex) |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Rosetti 2013.
| Methods | RCT, split‐mouth design, 2 treatment groups, 30 months' duration | |
| Participants | 12 individuals, 9 females, aged 25 to 60 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. GTR (collagen membrane) + TTC‐HCl + DFDBA 2. SCTG + HCl |
|
| Outcomes | ACC GRC CALC KTC*(2) MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Brazilian National Council for Scientific and Technologic Development | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Sangiorgio 2017.
| Methods | RCT, parallel design, 4 treatment groups, 6 months' duration | |
| Participants | 68 individuals, aged 18 to 60 years, with 1 maxillary Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. XCM + CAF 2. EMD + CAF 3. XCM + EMD + CAF 4. CAF |
|
| Outcomes | ACC GRC*(Groups 1, 2 and 3 were superior to 4) CALC KTC SCRC PCRC*(Groups 2 and 3 were superior to 4) MRC*(Groups 1, 2 and 3 were superior to 4) (Manual probe and digital calliper) |
|
| Notes | University/hospital‐based and supported by the State of São Paulo Research Foundation, São Paulo, Brazil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table |
| Allocation concealment (selection bias) | Low risk | Sealed and opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Patients remained unaware of the type of surgical procedures they received |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Shori 2013.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals, aged 18 to 50 years, with 1 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. ADMG + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC*(2) SCR PCRC MRC (Automated controlled force probe) |
|
| Notes | Universite/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Spahr 2005.
| Methods | RCT, split‐mouth design, 2 treatment groups, 24 months' duration | |
| Participants | 37 individuals, 17 females, aged 22 to 62 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm. 30 individuals completed the study | |
| Interventions | 1. EMP + CAF 2. Placebo (propylene glycol alginate) + CA |
|
| Outcomes | GRC CALC KTC PCRC MRC (Automated controlled force probe, calliper and manual probe) |
|
| Notes | University/hospital‐based and supported by BIORA AB (currently Straumann) Data from earlier article (Hagewald 2002) were reported as part of this trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 patients could not be recalled after the follow‐up period (they moved with address unknown) and 1 patient was excluded after enrolment in the study due to injuries of gingival tissues in the course of dental treatment by the referring dentist Data are equally missing in both intervention groups (split‐mouth design), but reasons for these are both reported and balanced across groups, then important bias is not to be expected |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Tozum 2005.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 31 individuals, 21 females, aged 16 to 59 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG + modified tunnel procedure 2. SCTG + CAF |
|
| Outcomes | GRC*(1) CALC*(1) MRC (Manual probe) |
|
| Notes | University/hospital‐based Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Trombelli 1996.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 15 individuals, 3 female, aged 25 to 51 years, with 2 Miller Class I or II maxillary buccal gingival recessions of at least 3 mm | |
| Interventions | 1. CAF (fibrin glue + TTC‐HCl) 2. CAF (TTC‐HCl) |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Italian Ministry of University and Scientific Research | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Tunali 2015.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 10 individuals, 6 female, aged 25 to 52 years, with 2 Miller Class I or II multiple buccal gingival recessions of at least 3 mm | |
| Interventions | 1. Leukocyte‐ and platelet‐rich fibrin + CAF 2. SCTG + CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based Unpublished data were included following contact with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Wang 2001.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 16 individuals, 10 females, aged 30 to 54 years, with 2 Miller Class I or II buccal gingival recessions of at least 3 mm | |
| Interventions | 1. GTR (reabsorbable double thickness collagen membrane ‐ Sulzer Dental Inc) 2. SCTG + CAF |
|
| Outcomes | ACC GRC CALC KTC MRC (Manual probe) |
|
| Notes | University/hospital‐based and supported by Sulzer Calcitek Inc | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Woodyard 2004.
| Methods | RCT, parallel design, 2 treatment groups, 6 months' duration | |
| Participants | 24 individuals, 14 females, mean age 34.6 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. ADMG + CAF 2. CAF |
|
| Outcomes | GRC*(1) CALC*(1) KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Zucchelli 1998.
| Methods | RCT, parallel design, 3 treatment groups, 12 months' duration | |
| Participants | 54 individuals, 29 females, aged 23 to 33 years, with 1 Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. GTR (polylactic acid membrane ‐ Guidor) 2. GTR (ePTFE membrane ‐ Gore‐Tex) 3. SCTG + CAF |
|
| Outcomes | GRC CALC KTC*(3) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Zucchelli 2003.
| Methods | RCT, split‐mouth design, 2 treatment groups, 12 months' duration | |
| Participants | 15 individuals, aged 18 to 35 years, with 2 Miller Class I or II maxillary buccal gingival recessions of at least 3 mm | |
| Interventions | 1. SCTG (graft size equal to the bone dehiscence) + CAF 2. SCTG (graft size 3 mm greater than the bone dehiscence) + CAF |
|
| Outcomes | ACC GRC CALC*(1) KTC*(2) SCRC PCRC MRC (Manual pressure sensitive probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Zucchelli 2009.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 11 individuals, aged 18 to 40 years, with 2 Miller Class I maxillary buccal gingival recessions of at least 3 mm | |
| Interventions | 1. Ultrasonic instrumentation ‐ CAF 2. Hand instrumentation ‐ CAF |
|
| Outcomes | GRC CALC KTC SCRC PCRC MRC (Manual pressure sensitive probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Zucchelli 2014.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 60 individuals, aged > 18 years, with 1 Miller Class I or II maxillary buccal gingival recession of at least 3 mm | |
| Interventions | 1. SCTG (de‐epithelialized free gingival graft: graft height equal to the depth of bone dehiscence and thickness ≥ 2 mm) + CAF 2. SCTG (de‐epithelialized free gingival graft: graft height of 4 mm thickness < 2 mm ) + CAF |
|
| Outcomes | ACC GRC CALC KTC SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table |
| Allocation concealment (selection bias) | Low risk | Sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Zucchelli 2014b.
| Methods | RCT, parallel design, 2 treatment groups, 12 months' duration | |
| Participants | 50 individuals, 28 females, age > 18 years, with 1 Miller Class I or II gingival recession of at least 3 mm at the buccal aspect of lower incisors | |
| Interventions | 1. SCTG + CAF ‐ with removal of the labial submucosal tissue 2. SCTG + CAF ‐ without removal of the labial submucosal tissue |
|
| Outcomes | ACC*(1) GRC*(1) CALC KTC*(2) SCRC PCRC MRC (Manual probe and calliper) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measurements were performed by 1 examiner not aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
Öncü 2017.
| Methods | RCT, split‐mouth design, 2 treatment groups, 6 months' duration | |
| Participants | 20 individuals, 11 females, age > 18 years, with maxillary bilateral multiple Miller Class I or II buccal gingival recession of at least 3 mm | |
| Interventions | 1. Platelet‐rich fibrin + CAF without vertical incisions 2. SCTG + CAF without vertical incisions |
|
| Outcomes | GRC CALC KTC*(2) SCRC PCRC MRC (Manual probe) |
|
| Notes | University/hospital‐based | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Patients remained unblinded to the root coverage procedure |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measurements were performed by 1 examiner aware of the type of surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients completed the follow‐up period |
| Selective reporting (reporting bias) | Low risk | Evidence of selective reporting of outcomes was not detected |
| Other bias | Low risk | Evidence of other bias was not detected |
ACC: aesthetic condition change; ADMG: acellular dermal matrix graft; CA: citric acid; CAF: coronally advanced flap; CALC: clinical attachment change; DFDBA: demineralized freeze‐dried bone allograft; EMD: enamel matrix derivative; EMP: enamel matrix protein; ePTFE: expanded polytetrafluorethylene; FGG: free gingival graft; GRC: gingival recession change; GTR: guided tissue regeneration; KTC: keratinized tissue change; MRC: mean root coverage; PCRC: percentage of complete root coverage; RCT: randomised controlled trial; SCRC: sites with complete root coverage; SCTG: subepithelial connective tissue graft; TTC‐HCl: tetracycline hydrochloride; XCM ‐ xenogeneic collagen matrix. *statistically significant between‐groups (superior group).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abou‐Arraj 2017 | Inclusion of patients with recession depth < 3 mm |
| Aichelmann Reidy 2001 | Inclusion of patients with recession depth < 3 mm |
| Alexiou 2017 | Inclusion of patients with recession depth < 3 mm |
| Alkan 2011 | Inclusion of patients with recession depth < 3 mm |
| Alkan 2013 | Inclusion of patients with recession depth < 3 mm |
| Andrade 2008 | Inclusion of patients with recession depth < 3 mm |
| Andrade 2010 | Inclusion of patients with Miller's Class III recessions |
| Aroca 2009 | Inclusion of patients with recession depth < 3 mm |
| Aroca 2013 | Inclusion of patients with recession depth < 3 mm |
| Azaripour 2016 | Inclusion of patients with recession depth < 3 mm |
| Baghele 2012 | Follow‐up period < 6 months |
| Bajic 2014 | Inclusion of patients with recession depth < 3 mm |
| Banihashemrad 2009 | Less than 10 patients per group at final examination and patient‐based analysis not presented |
| Bansal 2016 | Inclusion of patients with recession depth < 3 mm |
| Barros 2004 | Patient‐based analysis not presented |
| Barros 2005 | Patient‐based analysis not presented |
| Berlucchi 2002 | Inclusion of patients with recession depth < 3 mm |
| Berlucchi 2005 | Inclusion of patients with recession depth < 3 mm |
| Bherwani 2014 | Inclusion of patients with recession depth < 3 mm |
| Bittencourt 2006 | Inclusion of patients with recession depth < 3 mm |
| Bittencourt 2009 | Inclusion of patients with recession depth < 3 mm |
| Borghetti 1994 | Inclusion of patients with Miller's Class III or IV recession defects |
| Borghetti 1999 | Inclusion of patients with recession depth < 3 mm |
| Bozkurt Dogan 2015 | Inclusion of patients with recession depth < 3 mm |
| Burkhardt 2005 | Less than 10 patients per group at final examination |
| Byun 2009 | Inclusion of patients with recession depth < 3 mm |
| Caffesse 2000 | Inclusion of patients with recession depth < 3 mm |
| Cairo 2016 | Inclusion of patients with recession depth < 3 mm |
| Cardaropoli 2009 | Inclusion of patients with recession depth < 3 mm |
| Cardaropoli 2012 | Inclusion of patients with recession depth < 3 mm |
| Cardaropoli 2014 | Inclusion of patients with recession depth < 3 mm |
| Castellanos 2006 | Inclusion of patients with recession depth < 3 mm |
| Cetiner 2003 | Patient‐based analysis not presented |
| Chakraborthy 2015 | Randomised non‐controlled trial |
| Cheung 2004 | Inclusion of patients with recession depth < 3 mm |
| Cordaro 2012 | Inclusion of patients with recession depth < 3 mm |
| Cordioli 2001 | Patient‐based analysis not presented |
| Cortellini 2009 | Inclusion of patients with recession depth < 3 mm |
| Daniel 1990 | Not a randomised controlled trial |
| Dembowska 2007 | Not a randomised controlled trial |
| Deshpande 2014 | Inclusion of patients with recession depth < 3 mm |
| Dilsiz 2010 | Inclusion of patients with recession depth < 3 mm |
| Dilsiz 2010b | Inclusion of patients with recession depth < 3 mm |
| Duval 2000 | Inclusion of patients with recession depth < 3 mm, less than 10 patients per group at final examination and patient‐based analysis not presented |
| Erley 2006 | Not a randomised controlled trial |
| Felipe 2007 | Inclusion of patients with recession depth < 3 mm |
| Fernandes‐Dias 2015 | Inclusion of patients with recession depth < 3 mm |
| Ghahroudi 2013 | Inclusion of patients with recession depth < 3 mm, patient‐based analysis not presented, and patients with Miller's Class III recessions |
| Gholami 2013 | Inclusion of patients with recession depth < 3 mm |
| Gobbato 2016 | Inclusion of both single and multiple defects in the estimates and patients with recession depth < 3 mm |
| Griffin 2009 | Inclusion of patients with recession depth < 3 mm |
| Gunay 2008 | Not a randomised controlled trial |
| Gupta 2006 | Not a randomised controlled trial |
| Haghighati 2009 | Inclusion of patients with recession depth < 3 mm |
| Han 2008 | Inclusion of patients with recession depth < 3 mm |
| Harris 1997 | Not a randomised controlled trial |
| Harris 2000 | Not a randomised controlled trial |
| Harris 2002 | Not a randomised controlled trial |
| Harris 2005 | Not a randomised controlled trial |
| Hirsch 2005 | Not a randomised controlled trial |
| Huang 2005 | Inclusion of patients with recession depth < 3 mm |
| Ito 2000 | Inclusion of patients with recession depth < 3 mm, less than 10 patients per group at final examination and patient‐based analysis not presented |
| Jahnke 1993 | Inclusion of patients with recession depth < 3 mm |
| Jain 2017 | Inclusion of patients with recession depth < 3 mm |
| Jankovic 2012 | Inclusion of patients with recession depth < 3 mm |
| Jepsen 1998 | Inclusion of patients with recession depth < 3 mm |
| Jepsen 2017 | Inclusion of patients with recession depth < 3 mm |
| Jhaveri 2010 | Inclusion of patients with recession depth < 3 mm |
| Jovicic 2013 | Not a randomised controlled trial |
| Kennedy 1985 | Inclusion of patients with recession depth < 3 mm |
| Khobragade 2016 | Patient‐based analysis not reported and inclusion of patients with recession depth < 3 mm |
| Kimble 2004 | Less than 10 patients per group at final examination |
| Kuis 2013 | Inclusion of patients with recession depth < 3 mm |
| Kumar 2017 | Patient‐based analysis not reported and inclusion of patients with recession depth < 3 mm |
| Köseoglu 2013 | Inclusion of patients with recession depth < 3 mm |
| Lafzi 2007 | Follow‐up period < 6 months |
| Laney 1992 | Inclusion of patients with recession depth < 3 mm and follow‐up period < 6 months |
| Lins 2003 | Inclusion of patients with recession depth < 3 mm |
| M 2016 | Inclusion of patients with recession depth < 3 mm |
| Mahajan 2007 | Less than 10 patients per group at final examination |
| Mahajan 2012 | Inclusion of patient with age < 18 years |
| Mazzocco 2011 | Inclusion of patients with recession depth < 3 mm |
| Milinkovic 2015 | Patient‐based analysis not presented |
| Modica 2000 | Inclusion of patients with recession depth < 3 mm |
| Moka 2014 | Inclusion of patients with recession depth < 3 mm |
| Moses 2006 | Not a randomised controlled trial |
| Moslemi 2011 | Inclusion of patients with recession depth < 3 mm |
| Muller 1998 | Not a randomised controlled trial |
| Muller 1999 | Not a randomised controlled trial |
| Nazareth 2011 | Inclusion of patients with recession depth < 3 mm |
| Nemcovsky 2004 | Not a randomised controlled trial |
| Ozcelik 2011 | Inclusion of patients with recession depth < 3 mm |
| Ozturan 2011 | Inclusion of patients with recession depth < 3 mm |
| Pilloni 2006 | Inclusion of patients with recession depth < 3 mm |
| Pini Prato 1992 | Not a randomised controlled trial |
| Pini Prato 1996 | Not a randomised controlled trial |
| Pini Prato 1999 | Not a randomised controlled trial |
| Pini Prato 2000 | Inclusion of patients with recession depth < 3 mm and follow‐up period < 6 months |
| Pini Prato 2005 | Not a randomised controlled trial |
| Pini Prato 2011 | Inclusion of patients with recession depth < 3 mm |
| Pourabbas 2009 | Inclusion of patients with recession depth < 3 mm |
| Rahmani 2006 | Not a randomised controlled trial |
| Rebele 2014 | Inclusion of patients with recession depth < 3 mm |
| Ricci 1996 | Inclusion of patients with recession depth < 3 mm |
| Ricci 1996b | Patient‐based analysis not presented |
| Romagna‐Genon 2001 | Study author did not provide requested explanations |
| Roman 2013 | Inclusion of patients with recession depth < 3 mm |
| Salhi 2014 | Inclusion of patients with recession depth < 3 mm |
| Sallum 2003 | Not a randomised controlled trial |
| Santamaria 2017 | Inclusion of patients with recession depth < 3 mm |
| Santamaria 2017b | Inclusion of patients with recession depth < 3 mm |
| Santana 2010 | Inclusion of patients with recession depth < 3 mm |
| Santana 2010b | Inclusion of patients with recession depth < 3 mm |
| Sbordone 1988 | Not a randomised controlled trial |
| Scabbia 1998 | Not a randomised controlled trial |
| Schlee 2011 | Not a randomised controlled trial |
| Singh 2015 | Inclusion of patients with recession depth < 3 mm |
| Stefanini 2016 | Inclusion of patients with recession depth < 3 mm |
| Tal 2002 | Authors did not provide requested explanations |
| Tatakis 2000 | Inclusion of patients with recession depth < 3 mm |
| Thombre 2013 | Inclusion of patients with recession depth < 3 mm |
| Tonetti 2018 | Inclusion of patients with recession depth < 3 mm and defects were not classified according the Miller Classification System |
| Trabulsi 2004 | Inclusion of patients with recession depth < 3 mm |
| Trombelli 1995 | Not a randomised controlled trial |
| Trombelli 1995b | Less than 10 patients per group at final examination |
| Trombelli 1997 | Not a randomised controlled trial |
| Trombelli 1998 | Inclusion of patients with recession depth < 3 mm |
| Trombelli 2005 | Not a randomised controlled trial |
| Uzun 2018 | Patient‐based analysis not reported and inclusion of patients with recession depth < 3 mm |
| Wang 2014 | Inclusion of patients with recession depth < 3 mm |
| Wang 2015 | Inclusion of patients with recession depth < 3 mm |
| Wennström 1996 | Not a randomised controlled trial |
| Wilson 2005 | Intervention not of interest |
| Yilmaz 2014 | Intervention not of interest |
| Zucchelli 2010 | Inclusion of patients with recession depth < 3 mm |
| Zucchelli 2012 | Inclusion of patients with recession depth < 3 mm |
| Zuhr 2013 | Inclusion of patients with recession depth < 3 mm |
Differences between protocol and review
Changes to the original protocol.
Title: inclusion of 'multiple.'
Objectives: 'effectiveness' was changed to 'efficacy.'
Type of interventions: assessment of coronally advanced flap (CAF) + different biomaterial.
Type of outcomes: 'number/percentage of sites achieving complete root coverage' became a primary outcome.
Type of outcomes: studies with follow‐up > 12 months and ≤ 60 months were considered as medium‐term trials, whereas randomised controlled trials with follow‐up > 60 months as long term.
Contributions of authors
Leandro Chambrone: conceiving the review, designing the protocol, designing the review, undertaking searches, obtaining and screening data on unpublished studies, data collection and extraction for the review, writing to authors of papers for additional information, entering data into RevMan 5, analysis of data, interpretation of data and writing the review.
Maria Aparecida Salinas Ortega: undertaking searches, data collection and extraction for the review.
Flávia Sukekava: undertaking searches, data collection and extraction for the review, and analysis of data.
Roberto Rotundo: interpretation of data and writing the review.
Kalemaj Zamira: analysis and interpretation of data.
Jacopo Buti: designing the review, analysis of data, co‐ordinating and writing the review.
Giovan Paolo Pini Prato: interpretation of data and writing the review.
Sources of support
Internal sources
None, Other.
External sources
-
Cochrane Oral Health Global Alliance, Other.
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships‐alliances). Contributors over the past year have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and the Swiss Society for Endodontology, Switzerland.
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Leandro Chambrone, Giovan Paolo Pini Prato, Jacopo Buti and Roberto Rotundo acted as investigators of some trials considered in this review, but none of the authors report conflicts of interest related to this review. Maria Aparecida Salinas Ortega: no interests to declare. Flávia Sukekava: no interests to declare. Kalemaj Zamira: no interests to declare.
Edited (no change to conclusions)
References
References to studies included in this review
Abolfazli 2009 {published data only}
- Abolfazli N, Saleh‐Saber F, Eskandari A, Lafzi A. A comparative study of the long term results of root coverage with connective tissue graft or enamel matrix protein: 24‐month results. Medicina Oral, Patologia Oral y Cirugia Bucal 2009;14:E304‐9. [PubMed] [Google Scholar]
Ahmedbeyli 2014 {published data only}
- Ahmedbeyli C, Ipci SD, Cakar G, Kuru BE, Yılmaz S. Clinical evaluation of coronally advanced flap with or without acellular dermal matrix graft on complete defect coverage for the treatment of multiple gingival recessions with thin tissue biotype. Journal of Clinical Periodontology 2014;41:303‐10. [DOI] [PubMed] [Google Scholar]
Ayub 2012 {published data only}
- Ayub LG, Ramos UD, Reino DM, Grisi MFM, Taba Jr M, Souza SLS, et al. Randomized comparative clinical study of two surgical procedures to improve root coverage with the acellular dermal matrix graft. Journal of Clinical Periodontology 2012;39:871–8. [DOI] [PubMed] [Google Scholar]
Babu 2011 {published data only}
- Babu HM, Gujjari SK, Prasad D, Sehgal PK, Srinivasan A. Comparative evaluation of a bioabsorbable collagen membrane and connective tissue graft in the treatment of localized gingival recession: a clinical study. Journal of the Indian Society of Periodontology 2011;15(4):353‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barros 2015 {published data only}
- Barros RRM, Macedo GO, Queiroz AC, Novaes Jr AB. A modified surgical flap for root coverage in association with grafting materials. Journal of Esthetic and Restorative Dentistry 2015;27(2):84‐91. [DOI] [PubMed] [Google Scholar]
Bouchard 1994 {published data only}
- Bouchard P, Etienne D, Ouhayoun JP, Nilveus R. Subepithelial connective tissue grafts in the treatment of gingival recessions. A comparative study of 2 procedures. Journal of Periodontology 1994;65:929‐36. [DOI] [PubMed] [Google Scholar]
Bouchard 1997 {published data only}
- Bouchard P, Nilveus R, Etienne D. Clinical evaluation of tetracycline HCl conditioning in the treatment of gingival recessions. A comparative study. Journal of Periodontology 1997;68(3):262‐9. [DOI] [PubMed] [Google Scholar]
Costa 2016 {published data only}
- Alves LB, Costa PP, Souza SLS, Moraes Grisi MF, Palioto DB, Taba M Jr, et al. Acellular dermal matrix graft with or without enamel matrix derivative for root coverage in smokers: a randomised clinical study. Journal of Clinical Periodontology 2012;39:393‐9. [DOI] [PubMed] [Google Scholar]
- Costa PP, Alves LB, Souza SL, Grisi MF, Palioto DB, Taba M Jr, et al. Root coverage in smokers with acellular dermal matrix graft and enamel matrix derivative: a 12‐month randomized clinical trial. International Journal of Periodontics and Restorative Dentistry 2016;36(4):525‐31. [DOI] [PubMed] [Google Scholar]
da Silva 2004 {published data only}
- Silva RC, Joly JC, Lima AF, Tatakis DN. Root coverage using the coronally positioned flap with or without a subepithelial connective tissue graft. Journal of Periodontology 2004;75(3):413‐9. [DOI] [PubMed] [Google Scholar]
Del Pizzo 2005 {published data only}
- Pizzo M, Zucchelli G, Modica F, Villa R, Debernardi C. Coronally advanced flap with or without enamel matrix derivative for root coverage: a 2‐year study. Journal of Clinical Periodontology 2005;32(11):1181‐7. [DOI] [PubMed] [Google Scholar]
de Queiroz 2006 {published data only}
- Queiroz Cortes A, Martins AG, Nociti FH Jr, Sallum AW, Casati MZ, Sallum EA. Coronally positioned flap with or without acellular dermal matrix graft in the treatment of Class I gingival recessions: a randomized controlled clinical study. Journal of Periodontology 2004;75(8):1137‐44. [DOI] [PubMed] [Google Scholar]
- Queiroz Cortes A, Sallum AW, Casati MZ, Nociti FH Jr, Sallum EA. A two‐year prospective study of coronally positioned flap with or without acellular dermal matrix graft. Journal of Clinical Periodontology 2006;33(9):683‐9. [DOI] [PubMed] [Google Scholar]
Dodge 2000 {published data only}
- Dodge JR, Greenwell H, Drisko C, Wittwer JW, Yancey J, Rebitski G. Improved bone regeneration and root coverage using a resorbable membrane with physically assisted cell migration and DFDBA. International Journal of Periodontics & Restorative Dentistry 2000;20(4):398‐411. [PubMed] [Google Scholar]
Henderson 2001 {published data only}
- Henderson RD, Greenwell H, Drisko C, Regennitter FJ, Lamb JW, Mehlbauer MJ, et al. Predictable multiple site root coverage using an acellular dermal matrix allograft. Journal of Periodontology 2001;72(5):571‐82. [DOI] [PubMed] [Google Scholar]
Jaiswal 2012 {published data only}
- Jaiswal GR, Kumar R, Khatri PM, Jaiswal SG, Bhongade ML. The effectiveness of enamel matrix protein (Emdogain) in combination with coronally advanced flap in the treatment of multiple marginal tissue recession: a clinical study. Journal of the Indian Society of Periodontology 2012;16(2):224‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jankovic 2010 {published data only}
- Jankovic S, Aleksic Z, Milinkovic I, Dimitrijevic B. The coronally advanced flap in combination with platelet rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: a comparative study. European Journal of Esthetic Dentistry 2010;5:260‐73. [PubMed] [Google Scholar]
Jepsen 2013 {published data only}
- Jepsen K, Jepsen S, Zucchelli G, Stefanini M, Sanctis M, Baldini N, et al. Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: a multicenter randomized clinical trial. Journal of Clinical Periodontology 2013;40:82‐9. [DOI] [PubMed] [Google Scholar]
Joly 2007 {published data only}
- Joly JC, Carvalho AM, Silva RC, Ciotti DL, Cury PR. Root coverage in isolated gingival recessions using autograft versus allograft: a pilot study. Journal of Periodontology 2007;78(6):1017‐22. [DOI] [PubMed] [Google Scholar]
Keceli 2008 {published data only}
- Keceli HG, Sengun D, Berberoglu A, Karabulut E. Use of platelet gel with connective tissue grafts for root coverage: a randomized‐controlled trial. Journal of Clinical Periodontology 2008;35(3):255‐62. [DOI] [PubMed] [Google Scholar]
Keceli 2015 {published data only}
- Keceli HG, Kamak G, Erdemir EO, Evginer MS, Dolgun A. The adjunctive effect of platelet‐rich fibrin to connective tissue graft in the treatment of buccal recession defects: results of a randomized, parallel‐group controlled trial. Journal of Periodontology 2015;86(11):1221‐30. [DOI] [PubMed] [Google Scholar]
Leknes 2005 {published data only}
- Amarante ES, Leknes KN, Skavland J, Lie T. Coronally positioned flap procedures with or without a bioabsorbable membrane in the treatment of human gingival recession. Journal of Periodontology 2000;71(6):989‐98. [DOI] [PubMed] [Google Scholar]
- Leknes KN, Amarante ES, Price DE, Boe OE, Skavland RJ, Lie T. Coronally positioned flap procedures with or without a biodegradable membrane in the treatment of human gingival recession. A 6‐year follow‐up study. Journal of Clinical Periodontology 2005;32(5):518‐29. [DOI] [PubMed] [Google Scholar]
Matarasso 1998 {published data only}
- Matarasso S, Cafiero C, Coraggio F, Vaia E, Paoli S. Guided tissue regeneration versus coronally repositioned flap in the treatment of recession with double papillae. International Journal of Periodontics & Restorative Dentistry 1998;18(5):444‐53. [PubMed] [Google Scholar]
McGuire 2012 {published data only}
- McGuire MK, Nunn M. Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue. Part 1: comparison of clinical parameters. Journal of Periodontology 2003;74(8):1110‐25. [DOI] [PubMed] [Google Scholar]
- McGuire MK, Scheyer ET, Nunn M. Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue: comparison of clinical parameters at 10 years. Journal of Periodontology 2012;83:1353‐62. [DOI] [PubMed] [Google Scholar]
McGuire 2014 {published data only}
- McGuire MK, Scheyer ET, Schupbach P. Growth factor‐mediated treatment of recession defects: a randomized controlled trial and histologic and microcomputed tomography examination. Journal of Periodontology 2009;80(4):550‐64. [DOI] [PubMed] [Google Scholar]
- McGuire MK, Scheyer ET, Snyder MB. Evaluation of recession defects treated with coronally advanced flaps and either recombinant human platelet‐derived growth factor‐BB plus b‐tricalcium phosphate or connective tissue: comparison of clinical parameters at 5 years. Journal of Periodontology 2014;85(10):1361‐70. [DOI] [PubMed] [Google Scholar]
McGuire 2016 {published data only}
- McGuire MK, Scheyer ET. Long‐term results comparing xenogeneic collagen matrix and autogenous connective tissue grafts with coronally advanced flaps for treatment of dehiscence‐type recession defects. Journal of Periodontology 2016;87(3):221‐7. [DOI] [PubMed] [Google Scholar]
- McGuire MK, Scheyer ET. Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence‐type recession defects. Journal of Periodontology 2010;81(8):1108‐17. [DOI] [PubMed] [Google Scholar]
Öncü 2017 {published data only}
- Öncü E. The use of platelet‐rich fibrin versus subepithelial connective tissue graft in treatment of multiple gingival recessions: a randomized clinical trial. International Journal of Periodontics & Restorative Dentistry 2017;37(2):265‐71. [DOI] [PubMed] [Google Scholar]
Ozenci 2015 {published data only}
- Ozenci I, Ipci SD, Cakar G, Yilmaz S. Tunnel technique versus coronally advanced flap with acellular dermal matrix graft in the treatment of multiple gingival recessions. Journal of Clinical Periodontology 2015;42:1135–42. [DOI] [PubMed] [Google Scholar]
Paolantonio 1997 {published data only}
- Paolantonio M, Murro C, Cattabriga A, Cattabriga M. Subpedicle connective tissue graft versus free gingival graft in the coverage of exposed root surfaces. A 5‐year clinical study. Journal of Clinical Periodontology 1997;24(1):51‐6. [DOI] [PubMed] [Google Scholar]
Paolantonio 2002 {published data only}
- Paolantonio M. Treatment of gingival recessions by combined periodontal regenerative technique, guided tissue regeneration, and subpedicle connective tissue graft. A comparative clinical study. Journal of Periodontology 2002;73(1):53‐62. [DOI] [PubMed] [Google Scholar]
Paolantonio 2002b {published data only}
- Paolantonio M, Dolci M, Esposito P, D'Archivio D, Lisanti L, Luccio A, et al. Subpedicle acellular dermal matrix graft and autogenous connective tissue graft in the treatment of gingival recessions: a comparative 1‐year clinical study. Journal of Periodontology 2002;73(11):1299‐307. [DOI] [PubMed] [Google Scholar]
Pendor 2014 {published data only}
- Pendor S, Baliga V, Bhongade ML, Turakia V, Shori T. A comparison between connective tissue grafts combined with either double pedicle grafts or coronally positioned pedicle grafts: a clinical study. Journal of the Indian Society of Periodontology 2014;18(3):326‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rasperini 2011 {published data only}
- Rasperini G, Roccuzzo M, Francetti L, Acunzo R, Consonni D, Silvestri M. Subepithelial connective tissue graft for treatment of gingival recessions with and without enamel matrix derivative: a multicenter, randomized controlled clinical trial. International Journal of Periodontics & Restorative Dentistry 2011;31(2):133‐9. [PubMed] [Google Scholar]
Reino 2012 {published data only}
- Reino DM, Novaes Jr AB, Maia LP, Paioto DB, Grisi MFM, Taba Jr M, et al. Treatment of gingival recessions in heavy smokers using two surgical techniques: a controlled clinical trial. Brazilian Dental Journal 2012;23(1):59‐67. [DOI] [PubMed] [Google Scholar]
Reino 2015 {published data only}
- Reino DM, Maia LP, Fernandes PG, Souza SLS, Taba Jr M, Palioto DB, et al. A randomized comparative study of two techniques to optimize the root coverage using a porcine collagen matrix. Brazilian Dental Journal 2015;26(5):445‐50. [DOI] [PubMed] [Google Scholar]
Roccuzzo 1996 {published data only}
- Roccuzzo M, Lungo M, Corrente G, Gandolfo S. Comparative study of a bioresorbable and a non‐resorbable membrane in the treatment of human buccal gingival recessions. Journal of Periodontology 1996;67(1):7‐14. [DOI] [PubMed] [Google Scholar]
Rosetti 2013 {published data only}
- Rosetti EP, Marcantonio E Jr, Zuza EP, Marcantonio RAC. Root coverage stability of the subepithelial connective tissue graft and guided tissue regeneration: a 30‐month follow‐up clinical trial. Journal of Dentistry 2013;41:114‐20. [DOI] [PubMed] [Google Scholar]
- Rosetti EP, Marcantonio RA, Rossa C Jr, Chaves ES, Goissis G, Marcantonio E Jr. Treatment of gingival recession: comparative study between subepithelial connective tissue graft and guided tissue regeneration. Journal of Periodontology 2000;71(9):1441‐7. [DOI] [PubMed] [Google Scholar]
Sangiorgio 2017 {published data only}
- Rocha Dos Santos M, Sangiorgio JPM, Neves FLDS, França‐Grohmann IL, Nociti FH Jr, Silverio Ruiz KG, et al. Xenogenous collagen matrix and/or enamel matrix derivative for treatment of localized gingival recessions: a randomized clinical trial. Part II: patient‐reported outcomes. Journal of Periodontology 2017;88(12):1319‐28. [DOI] [PubMed] [Google Scholar]
- Sangiorgio JPM, Neves FLDS, Rocha Dos Santos M, França‐Grohmann IL, Casarin RCV, Casati MZ, et al. Xenogenous collagen matrix and/or enamel matrix derivative for treatment of localized gingival recessions: a randomized clinical trial. Part I: clinical outcomes. Journal of Periodontology 2017;88(12):1309‐18. [DOI] [PubMed] [Google Scholar]
Shori 2013 {published data only}
- Shori T, Kolte A, Kher V, Dharamthok S, Shrirao T. A comparative evaluation of the effectiveness of subpedicle acellular dermal matrix allograft with subepithelial connective tissue graft in the treatment of isolated marginal tissue recession: a clinical study. Journal of the Indian Society of Periodontology 2013;17(1):78‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spahr 2005 {published data only}
- Hagewald S, Spahr A, Rompola E, Haller B, Heijl L, Bernimoulin JP. Comparative study of Emdogain and coronally advanced flap technique in the treatment of human gingival recessions. A prospective controlled clinical study. Journal of Clinical Periodontology 2002;29(1):35‐41. [DOI] [PubMed] [Google Scholar]
- Spahr A, Haegewald S, Tsoulfidou F, Rompola E, Heijl L, Bernimoulin JP, et al. Coverage of Miller class I and II recession defects using enamel matrix proteins versus coronally advanced flap technique: a 2‐year report. Journal of Periodontology 2005;76(11):1871‐80. [DOI] [PubMed] [Google Scholar]
Tozum 2005 {published data only}
- Tozum TF, Keceli HG, Guncu GN, Hatipoglu H, Sengun D. Treatment of gingival recession: comparison of two techniques of subepithelial connective tissue graft. Journal of Periodontology 2005;76(11):1842‐8. [DOI] [PubMed] [Google Scholar]
Trombelli 1996 {published data only}
- Trombelli L, Scabbia A, Wikesjö UM, Calura G. Fibrin glue application in conjunction with tetracycline root conditioning and coronally positioned flap procedure in the treatment of human gingival recession defects. Journal of Clinical Periodontology 1996;23(9):861‐7. [DOI] [PubMed] [Google Scholar]
Tunali 2015 {published data only}
- Tunali M, Ozdemir H, Arabaci T, Pikdoken ML. Clinical evaluation of autologous platelet‐rich fibrin in the treatment of multiple adjacent gingival recession defects: a 12‐month study. International Journal of Periodontics & Restorative Dentistry 2015;35(1):105‐14. [DOI] [PubMed] [Google Scholar]
Wang 2001 {published data only}
- Wang HL, Bunyaratavej P, Labadie M, Shyr Y, MacNeil RL. Comparison of 2 clinical techniques for treatment of gingival recession. Journal of Periodontology 2001;72(10):1301‐11. [DOI] [PubMed] [Google Scholar]
Woodyard 2004 {published data only}
- Woodyard JG, Greenwell H, Hill M, Drisko C, Iasella JM, Scheetz J. The clinical effect of acellular dermal matrix on gingival thickness and root coverage compared to coronally positioned flap alone. Journal of Periodontology 2004;75(1):44‐56. [DOI] [PubMed] [Google Scholar]
Zucchelli 1998 {published data only}
- Zucchelli G, Clauser C, Sanctis M, Calandriello M. Mucogingival versus guided tissue regeneration procedures in the treatment of deep recession type defects. Journal of Periodontology 1998;69(2):138‐45. [DOI] [PubMed] [Google Scholar]
Zucchelli 2003 {published data only}
- Zucchelli G, Amore C, Sforzal NM, Montebugnoli L, Sanctis M. Bilaminar techniques for the treatment of recession‐type defects. A comparative clinical study. Journal of Clinical Periodontology 2003;30(10):862‐70. [DOI] [PubMed] [Google Scholar]
Zucchelli 2009 {published data only}
- Zucchelli G, Mounssif I, Stefanini M, Mele M, Montebugnoli L, Sforza NM. Hand and ultrasonic instrumentation in combination with root‐coverage surgery: a comparative controlled randomized clinical trial. Journal of Periodontology 2009;80(4):577‐85. [DOI] [PubMed] [Google Scholar]
Zucchelli 2014 {published data only}
- Zucchelli G, Mounssif I, Mazzotti C, Montebugnoli L, Sangiorgi M, Mele M, et al. Does the dimension of the graft influence patient morbidity and root coverage outcomes? A randomized controlled clinical trial. Journal of Clinical Periodontology 2014;41:708–16. [DOI] [PubMed] [Google Scholar]
Zucchelli 2014b {published data only}
- Zucchelli G, Marzadori M, Mounssif I, Mazzotti C, Stefanini M. Coronally advanced flap + connective tissue graft techniques for the treatment of deep gingival recession in the lower incisors. A controlled randomized clinical trial. Journal of Clinical Periodontology 2014;41:806–13. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abou‐Arraj 2017 {published data only}
- Abou‐Arraj RV, Kaur M, Vassilopoulos PJ, Geurs NC. Creation of a zone of immobile connective tissue with acellular dermal matrix allografts. International Journal of Periodontics & Restorative Dentistry 2017;37(4):571‐9. [DOI] [PubMed] [Google Scholar]
Aichelmann Reidy 2001 {published data only}
- Aichelmann‐Reidy ME, Yukna RA, Evans GH, Nasr HF, Mayer ET. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. Journal of Periodontology 2001;72(8):998‐1005. [DOI] [PubMed] [Google Scholar]
Alexiou 2017 {published data only}
- Alexiou A, Vouros I, Menexes G, Konstantinidis A. Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: a randomized controlled clinical study. Quintessence International 2017;48(5):381‐9. [DOI] [PubMed] [Google Scholar]
Alkan 2011 {published data only}
- Alkan EA, Parlar A. EMD or subepithelial connective tissue graft for the treatment of single gingival recessions: a pilot study. Journal of Periodontal Research 2011;46(6):637‐42. [DOI] [PubMed] [Google Scholar]
Alkan 2013 {published data only}
- Alkan EA, Parlar A. Enamel matrix derivative (Endogain) or subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessions: a pilot study. International Journal of Periodontics & Restorative Dentistry 2013;33(5):619‐25. [DOI] [PubMed] [Google Scholar]
Andrade 2008 {published data only}
- Andrade PF, Felipe MEMC, Novaes AB Jr, Souza SLS, Taba M Jr, Palioto DB, et al. Comparison between two surgical techniques for root coverage with an acellular dermal matrix graft. Journal of Clinical Periodontology 2008;35:263‐9. [DOI] [PubMed] [Google Scholar]
Andrade 2010 {published data only}
- Andrade PF, Grisi MFM, Marcaccini AM, Fernandes PG, Reino DM, Souza SLS, et al. Comparison between micro‐ and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. Journal of Periodontology 2010;81(11):1572‐9. [DOI] [PubMed] [Google Scholar]
Aroca 2009 {published data only}
- Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet‐rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6‐month study. Journal of Periodontology 2009;80(2):244‐52. [DOI] [PubMed] [Google Scholar]
Aroca 2013 {published data only}
- Aroca S, Molnar B, Windisch P, Gera I, Salvi GE, Nikolidakis D, et al. Treatment of multiple adjacent Miller Class I and II gingival recessions with a Modified Coronally Advanced Tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. Journal of Clinical Periodontology 2013;40:713‐20. [DOI] [PubMed] [Google Scholar]
Azaripour 2016 {published data only}
- Azaripour A, Kissinger M, Farina VSL, Noorden CJF, Gerhold‐Ay A, Willershausen B, et al. Root coverage with connective tissue graft associated with coronally advanced flap or tunnel technique: a randomized, double‐blind, mono‐centre clinical trial. Journal of Periodontology 2016;43:1142‐50. [DOI] [PubMed] [Google Scholar]
Baghele 2012 {published data only}
- Baghele ON, Pol DG. An evaluation of the effectiveness and predictability of transpositional flap vs connective tissue graft for coverage of Miller's Class‐I and Class‐II facial marginal tissue recession lesions: a clinical study. Indian Journal of Dental Research 2012;23(2):195‐202. [DOI] [PubMed] [Google Scholar]
Bajic 2014 {published data only}
- Bajić M, Janković S, Milinković I, Čakić S, Perunović N, Novaković N, et al. Utilization of two different surgical techniques in gingival recession treatment: a comparative study [Компаративна анализа примене двеју техникатрансплантата везивног ткива у лечењу рецесијагингиве]. Srpski Arhiv Za Celokupno Lekarstvo 2014;142(3‐4):155‐63. [DOI] [PubMed] [Google Scholar]
Banihashemrad 2009 {published data only}
- Banihashemrad A, Aghassizadeh E, Radvar M. Treatment of gingival recessions by guided tissue regeneration and coronally advanced flap. New York State Dental Journal 2009;75:54‐8. [PubMed] [Google Scholar]
Bansal 2016 {published data only}
- Bansal A, Kulloli A, Kathariya R, Shetty S, Jain H, Raikar S. Comparative evaluation of coronally advanced flap with and without bioactive glass putty in the management of gingival recession defects: a randomized controlled clinical trial. Journal of the International Academy of Periodontology 2016;18(1):7‐15. [PubMed] [Google Scholar]
Barros 2004 {published data only}
- Barros RR, Novaes AB, Grisi MF, Souza SL, Taba MJ, Palioto DB. A 6‐month comparative clinical study of a conventional and a new surgical approach for root coverage with acellular dermal matrix. Journal of Periodontology 2004;75(10):1350‐6. [DOI] [PubMed] [Google Scholar]
Barros 2005 {published data only}
- Barros RR, Novaes AB Jr, Grisi MF, Souza SL, Taba M Jr, Palioto DB. New surgical approach for root coverage of localized gingival recession with acellular dermal matrix: a 12‐month comparative clinical study. Journal of Esthetic and Restorative Dentistry 2005;17(3):156‐64. [DOI] [PubMed] [Google Scholar]
Berlucchi 2002 {published data only}
- Berlucchi I, Francetti L, Fabbro M, Testori T, Weinstein RL. Enamel matrix proteins (Emdogain) in combination with coronally advanced flap or subepithelial connective tissue graft in the treatment of shallow gingival recessions. International Journal of Periodontics & Restorative Dentistry 2002;22(6):583‐93. [PubMed] [Google Scholar]
Berlucchi 2005 {published data only}
- Berlucchi I, Francetti L, Fabbro M, Basso M, Weinstein RL. The influence of anatomical features on the outcome of gingival recessions treated with coronally advanced flap and enamel matrix derivative: a 1‐year prospective study. Journal of Periodontology 2005;76(6):899‐907. [DOI] [PubMed] [Google Scholar]
Bherwani 2014 {published data only}
- Bherwani C, Kulloli A, Kathariya R, Shetty S, Agrawal P, Gujar D, et al. Zucchelli's technique or tunnel technique with subepithelial connective tissue graft for treatment of multiple gingival recessions. Journal of the International Academy of Periodontology 2014;16(2):34‐42. [PubMed] [Google Scholar]
Bittencourt 2006 {published data only}
- Bittencourt S, Peloso Ribeiro E, Sallum EA, Sallum AW, Nociti FH Jr, Casati MZ. Comparative 6‐month clinical study of a semilunar coronary positioned flap and subepithelial connective tissue graft for the treatment of gingival recession. Journal of Periodontology 2006;77(2):174‐81. [DOI] [PubMed] [Google Scholar]
Bittencourt 2009 {published data only}
- Bittencourt S, Ribeiro Edel P, Sallum EA, Sallum AW, Nociti FH Jr, Casati MZ. Semilunar coronally positioned flap or subepithelial connective tissue graft for the treatment of gingival recession: a 30‐month follow‐up study. Journal of Periodontology 2009;80(7):1076‐82. [DOI] [PubMed] [Google Scholar]
Borghetti 1994 {published data only}
- Borghetti A, Louise F. Controlled clinical evaluation of the subpedicle connective tissue graft for the coverage of gingival recession. Journal of Periodontology 1994;65(12):1107‐12. [DOI] [PubMed] [Google Scholar]
Borghetti 1999 {published data only}
- Borghetti A, Glise JM, Monnet‐Corti V, Dejou J. Comparative clinical study of a bioabsorbable membrane and subepithelial connective tissue graft in the treatment of human gingival recession. Journal of Periodontology 1999;70(2):123‐30. [DOI] [PubMed] [Google Scholar]
Bozkurt Dogan 2015 {published data only}
- Bozkurt Dogan S, Ongoz Dede F, Balli U, Atalay EN, Durmuslar MC. Concentrated growth factor in the treatment of adjacent multiple gingival recessions: a split‐mouth randomized clinical trial. Journal of Clinical Periodontology 2015;42:868–75. [DOI] [PubMed] [Google Scholar]
Burkhardt 2005 {published data only}
- Burkhardt R, Lang NP. Coverage of localized gingival recessions: comparison of micro‐ and macrosurgical techniques. Journal of Clinical Periodontology 2005;32(3):287‐93. [DOI] [PubMed] [Google Scholar]
Byun 2009 {published data only}
- Byun H‐Y, Oh T‐J, Abuhussein HM, Yamashita J, Soehren SE, Wang H‐L. Significance of the epithelial collar on the subepithelial connective tissue graft. Journal of Periodontology 2009;80(6):924‐32. [DOI] [PubMed] [Google Scholar]
Caffesse 2000 {published data only}
- Caffesse RG, LaRosa M, Garza M, Munne‐Travers A, Mondragon JC, Weltman R. Citric acid demineralization and subepithelial connective tissue grafts. Journal of Periodontology 2000;71(4):568‐72. [DOI] [PubMed] [Google Scholar]
Cairo 2016 {published data only}
- Cairo F, Cortellini P, Pilloni A, Nieri M, Cincinelli S, Amunni F, et al. Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: a randomized controlled clinical trial. Journal of Clinical Periodontology 2016;43:849‐56. [DOI] [PubMed] [Google Scholar]
Cardaropoli 2009 {published data only}
- Cardaropoli D, Cardaropoli G. Healing of gingival recessions using a collagen membrane with a hemineralized xenograft: a randomized controlled clinical trial. International Journal of Periodontics & Restorative Dentistry 2009;29(1):59‐67. [PubMed] [Google Scholar]
Cardaropoli 2012 {published data only}
- Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: a randomized controlled clinical trial. Journal of Periodontology 2012;83(3):321‐8. [DOI] [PubMed] [Google Scholar]
Cardaropoli 2014 {published data only}
- Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Coronally advanced flap with and without a xenogenic collagen matrix in the treatment of multiple recessions: a randomized controlled clinical study. International Journal of Periodontics & Restorative Dentistry 2014;34(Supplement):S97‐S102. [DOI] [PubMed] [Google Scholar]
Castellanos 2006 {published data only}
- Castellanos A, Rosa M, Garza M, Caffesse RG. Enamel matrix derivative and coronal flaps to cover marginal tissue recessions. Journal of Periodontology 2006;77(1):7‐14. [DOI] [PubMed] [Google Scholar]
Cetiner 2003 {published data only}
- Cetiner D, Parlar A, Balos K, Alpar R. Comparative clinical study of connective tissue graft and two types of bioabsorbable barriers in the treatment of localized gingival recessions. Journal of Periodontology 2003;74(8):1196‐205. [DOI] [PubMed] [Google Scholar]
Chakraborthy 2015 {published data only}
- Chakraborthy S, Sambashivaiah S, Rithesh K, Bilchodmath S. Amnion and chorion allografts in combination with coronally advanced flap in the treatment of gingival recession: a clinical study. Journal of Clinical and Diagnostic Research 2015;9(9):ZC98‐ZC101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheung 2004 {published data only}
- Cheung WS, Griffin TJ. A comparative study of root coverage with connective tissue and platelet concentrate grafts: 8‐month results. Journal of Periodontology 2004;75(12):1678‐87. [DOI] [PubMed] [Google Scholar]
Cordaro 2012 {published data only}
- Cordaro L, Torresanto VM, Torsello F. Split‐mouth comparison of a coronally advanced flap with or without enamel matrix derivative for coverage of multiple gingival recession defects: 6‐ and 24‐month follow‐up. International Journal of Periodontics & Restorative Dentistry 2012;32:e10‐e20. [PubMed] [Google Scholar]
Cordioli 2001 {published data only}
- Cordioli G, Mortarino C, Chierico A, Grusovin MG, Majzoub Z. Comparison of 2 techniques of subepithelial connective tissue graft in the treatment of gingival recessions. Journal of Periodontology 2001;72(11):1470‐6. [DOI] [PubMed] [Google Scholar]
Cortellini 2009 {published data only}
- Cortellini P, Tonetti M, Baldi C, Francetti L, Rasperini G, Rotundo R, et al. Does placement of a connective tissue graft improve the outcomes of coronally advanced flap for coverage of single gingival recessions in upper anterior teeth? A multi‐centre, randomized, double blind, clinical trial. Journal of Clinical Periodontology 2009;36(1):68‐79. [DOI] [PubMed] [Google Scholar]
Daniel 1990 {published data only}
- Daniel A, Cheru R. Treatment of localised gingival recession with subpedicle connective tissue graft and free gingival auto graft‐‐a comparative clinical evaluation. Journal of the Indian Dental Association 1990;61(12):294‐7. [PubMed] [Google Scholar]
Dembowska 2007 {published data only}
- Dembowska E, Drozdzik A. Subepithelial connective tissue graft in the treatment of multiple gingival recession. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2007;104(3):1‐7. [DOI] [PubMed] [Google Scholar]
Deshpande 2014 {published data only}
- Deshpande A, Koudale SB, Bhongade ML. A comparative evaluation of rhPDGF‐BB + β‐TCP and subepithelial connective tissue graft for the treatment of multiple gingival recession defects in humans. International Journal of Periodontics & Restorative Dentistry 2014;34(2):241‐9. [DOI] [PubMed] [Google Scholar]
Dilsiz 2010 {published data only}
- Dilsiz A, Aydin T, Canakci V, Cicek Y. Root surface biomodification with Nd:YAG laser for the treatment of gingival recession with subepithelial connective tissue grafts. Photomedicine and Laser Surgery 2010;28(3):337‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dilsiz 2010b {published data only}
- Dilsiz A, Aydin T, Yavuz S. Root surface biomodification with an Er:YAG laser for the treatment of gingival recession with subepithelial connective tissue grafts. Photomedicine and Laser Surgery 2010;28(4):511‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duval 2000 {published data only}
- Duval BT, Maynard JG, Gunsolley JC, Waldrop TC. Treatment of human mucogingival defects utilizing a bioabsorbable membrane with and without a demineralized freeze‐dried bone allograft. Journal of Periodontology 2000;71(11):1687‐92. [DOI] [PubMed] [Google Scholar]
Erley 2006 {published data only}
- Erley KJ, Swiec GD, Herold R, Bisch FC, Peacock ME. Gingival recession treatment with connective tissue grafts in smokers and non‐smokers. Journal of Periodontology 2006;77(7):1148‐55. [DOI] [PubMed] [Google Scholar]
Felipe 2007 {published data only}
- Felipe ME, Andrade PF, Grisi MF, Souza SL, Taba M, Palioto DB, et al. Comparison of two surgical procedures for use of the acellular dermal matrix graft in the treatment of gingival recessions: a randomized controlled clinical study. Journal of Periodontology 2007;78(7):1209‐17. [DOI] [PubMed] [Google Scholar]
Fernandes‐Dias 2015 {published data only}
- Fernandes‐Dias SB, Marco AC, Santamaria M Jr, Kerbauy WD, Jardini MAN, Santamaria MP. Connective tissue graft associated or not with low laser therapy to treat gingival recession: randomized clinical trial. Journal of Clinical Periodontology 2015;42(1):54–61. [DOI] [PubMed] [Google Scholar]
Ghahroudi 2013 {published data only}
- Ghahroudi AAR, Khorsand A, Rokn AR, Sabounchi SS, Shayesteh YS, Soolari A. Comparison of amnion allograft with connective tissue graft for root coverage procedures: a double‐blind, randomized, controlled clinical trial. Journal of the International Academy of Periodontology 2013;15(4):101‐12. [PubMed] [Google Scholar]
Gholami 2013 {published data only}
- Gholami GA, Saberi A, Kadkhodazadeh M, Amid R, Karami D. Comparison of the clinical outcomes of connective tissue and acellular dermal matrix in combination with double papillary flap for root coverage: a 6‐month trial. Dental Research Journal 2013;10(4):506‐13. [PMC free article] [PubMed] [Google Scholar]
Gobbato 2016 {published data only}
- Gobbato L, Nart J, Bressan E, Mazzocco F, Paniz G, Lops D. Patient morbidity and root coverage outcomes after the application of a subepithelial connective tissue graft in combination with a coronally advanced flap or via a tunneling technique: a randomized controlled clinical trial. Clinical Oral Investigations 2016;20(8):2191‐202. [DOI] [PubMed] [Google Scholar]
Griffin 2009 {published data only}
- Griffin TJ, Cheung WS. Guided tissue regeneration‐based root coverage with a platelet concentrate graft: a 3‐year follow‐up case series. Journal of Periodontology 2009;80(7):1192‐9. [DOI] [PubMed] [Google Scholar]
Gunay 2008 {published data only}
- Gunay H, Dogan S, Geurtsen W. Harvesting technique using a mucotome and modified surgical procedure for root coverage with enamel matrix derivatives with and without a connective tissue graft. International Journal of Periodontics & Restorative Dentistry 2008;28(5):497‐507. [PubMed] [Google Scholar]
Gupta 2006 {published data only}
- Gupta R, Pandit N, Sharma M. Clinical evaluation of a bioresorbable membrane (polyglactin 910) in the treatment of Miller type II gingival recession. International Journal of Periodontics & Restorative Dentistry 2006;26(3):271‐7. [PubMed] [Google Scholar]
Haghighati 2009 {published data only}
- Haghighati F, Mousavi M, Moslemi N, Kebria MM, Golestan B. A comparative study of two root‐coverage techniques with regard to interdental papilla dimension as a prognostic factor. International Journal of Periodontics & Restorative Dentistry 2009;29(2):179‐89. [PubMed] [Google Scholar]
Han 2008 {published data only}
- Han JS, John V, Blanchard SB, Kowolik MJ, Eckert GJ. Changes in gingival dimensions following connective tissue grafts for root coverage: comparison of two procedures. Journal of Periodontology 2008;79(8):1346‐54. [DOI] [PubMed] [Google Scholar]
Harris 1997 {published data only}
- Harris RJ. A comparative study of root coverage obtained with guided tissue regeneration utilizing a bioabsorbable membrane versus the connective tissue with partial‐thickness double pedicle graft. Journal of Periodontology 1997;68(8):779‐90. [DOI] [PubMed] [Google Scholar]
Harris 2000 {published data only}
- Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: results of 107 recession defects in 50 consecutively treated patients. International Journal of Periodontics & Restorative Dentistry 2000;20(1):51‐9. [PubMed] [Google Scholar]
Harris 2002 {published data only}
- Harris RJ. Root coverage with connective tissue grafts: an evaluation of short‐ and long‐term results. Journal of Periodontology 2002;73(9):1054‐9. [DOI] [PubMed] [Google Scholar]
Harris 2005 {published data only}
- Harris RJ, Miller LH, Harris CR, Miller RJ. A comparison of three techniques to obtain root coverage on mandibular incisors. Journal of Periodontology 2005;76(10):1758‐67. [DOI] [PubMed] [Google Scholar]
Hirsch 2005 {published data only}
- Hirsch A, Goldstein M, Goultschin J, Boyan BD, Schwartz Z. A 2‐year follow‐up of root coverage using sub‐pedicle acellular dermal matrix allografts and subepithelial connective tissue autografts. Journal of Periodontology 2005;76(8):1323‐8. [DOI] [PubMed] [Google Scholar]
Huang 2005 {published data only}
- Huang LH, Neiva RE, Soehren SE, Giannobile WV, Wang HL. The effect of platelet‐rich plasma on the coronally advanced flap root coverage procedure: a pilot human trial. Journal of Periodontology 2005;76(10):1768‐77. [DOI] [PubMed] [Google Scholar]
Ito 2000 {published data only}
- Ito K, Oshio K, Shiomi N, Murai S. A preliminary comparative study of the guided tissue regeneration and free gingival graft procedures for adjacent facial root coverage. Quintessence International 2000;31(5):319‐26. [PubMed] [Google Scholar]
Jahnke 1993 {published data only}
- Jahnke PV, Sandifer JB, Gher ME, Gray JL, Richardson AC. Thick free gingival and connective tissue autografts for root coverage. Journal of Periodontology 1993;64(4):315‐22. [DOI] [PubMed] [Google Scholar]
Jain 2017 {published data only}
- Jain A, Jaiswal GR, Kumathalli K, Kumar R, Singh A, Sarwan A. Comparative evaluation of platelet rich fibrin and dehydrated amniotic membrane for the treatment of gingival recession ‐ a clinical study. Journal of Clinical and Diagnostic Research 2017;11(8):ZC24‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jankovic 2012 {published data only}
- Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, et al. Use of platelet‐rich fibrin membrane following treatment of gingival recession: a randomized clinical trial. International Journal of Periodontics & Restorative Dentistry 2012;32(2):e41‐e50. [PubMed] [Google Scholar]
Jepsen 1998 {published data only}
- Jepsen K, Heinz B, Halben JH, Jepsen S. Treatment of gingival recession with titanium reinforced barrier membranes versus connective tissue grafts. Journal of Periodontology 1998;69(3):383‐91. [DOI] [PubMed] [Google Scholar]
Jepsen 2017 {published data only}
- Jepsen K, Stefanini M, Sanz M, Zucchelli G, Jepsen S. Long‐term stability of root coverage by coronally advanced flap procedures. Journal of Periodontology 2017;88(7):1319‐28. [DOI] [PubMed] [Google Scholar]
Jhaveri 2010 {published data only}
- Jhaveri HM, Chavan MS, Tomar GB, Deshmukh VL, Wani MR, Miller PD Jr. Acellular dermal matrix seeded with autologous gingival fibroblasts for the treatment of gingival recession: a proof‐of‐concept study. Journal of Periodontology 2010;81(4):616‐25. [DOI] [PubMed] [Google Scholar]
Jovicic 2013 {published data only}
- Jovicic B, Lazic Z, Nedic M, Matijevic S, Gostovic‐Spadijer A. Therapeutic efficacy of connective tissue autotransplants with periosteum and platelet rich plasma in the management of gingival recession. Vojnosanitetski Pregled 2013;70(7):664‐9. [DOI] [PubMed] [Google Scholar]
Kennedy 1985 {published data only}
- Kennedy JE, Bird WC, Palcanis KG, Dorfman HS. A longitudinal evaluation of varying widths of attached gingiva. Journal of Clinical Periodontology 1985;12(8):667‐75. [DOI] [PubMed] [Google Scholar]
Khobragade 2016 {published data only}
- Khobragade S, Kolte A, Kolte R, Shrirao T, Potey A. Modified coronally advanced flap with and without orthodontic button application in management of multiple proximate gingival recession defects: a randomized clinical trial. Contemporary Clinical Dentistry 2016;7(4):544‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kimble 2004 {published data only}
- Kimble KM, Eber RM, Soehren S, Shyr Y, Wang HL. Treatment of gingival recession using a collagen membrane with or without the use of demineralized freeze‐dried bone allograft for space maintenance. Journal of Periodontology 2004;75(2):210‐20. [DOI] [PubMed] [Google Scholar]
Köseoglu 2013 {published data only}
- Köseoglu S, Duran I, Saglam M, Bozkurt SB, Kırtıloglu OS, Hakkı SS. Efficacy of collagen membrane seeded with autologous gingival fibroblasts in gingival recession treatment: a randomized, controlled pilot study. Journal of Periodontology 2013;84(10):1416‐24. [DOI] [PubMed] [Google Scholar]
Kuis 2013 {published data only}
- Kuis D, Sciran I, Lajnert V, Snjaric D, Prpic J, Pezelj‐Ribaric S, et al. Coronally advanced flap alone or with connective tissue graft in the treatment of single gingival recession defects: a long‐term randomized clinical trial. Journal of Periodontology 2013;84(11):1576‐85. [DOI] [PubMed] [Google Scholar]
Kumar 2017 {published data only}
- Kumar A, Bains VK, Jhingran R, Srivastava R, Madan R, Rizvi I. Patient‐centered microsurgical management of gingival recession using coronally advanced flap with either platelet‐rich fibrin or connective tissue graft: a comparative analysis. Contemporary clinical Dentistry 2017;8(2):293‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lafzi 2007 {published data only}
- Lafzi A, Mostofi Zadeh Farahani R, Abolfazli N, Amid R, Safaiyan A. Effect of connective tissue graft orientation on the root coverage outcomes of coronally advanced flap. Clinical Oral Investigations 2007;11(4):401‐8. [DOI] [PubMed] [Google Scholar]
Laney 1992 {published data only}
- Laney JB, Saunders VG, Garnick JJ. A comparison of two techniques for attaining root coverage. Journal of Periodontology 1992;63(1):19‐23. [DOI] [PubMed] [Google Scholar]
Lins 2003 {published data only}
- Lins LH, Lima AF, Sallum AW. Root coverage: comparison of coronally positioned flap with and without titanium‐reinforced barrier membrane. Journal of Periodontology 2003;74(2):168‐74. [DOI] [PubMed] [Google Scholar]
M 2016 {published data only}
- M Y, Mlv P, Bv K, N SJ. Comparison of extracellular matrix membrane and connective tissue graft for root coverage in Class I/II gingival recession defects: a split‐mouth study. Journal of the International Academy of Periodontology 2016;18(2):36‐44. [PubMed] [Google Scholar]
Mahajan 2007 {published data only}
- Mahajan A, Dixit J, Verma UP. A patient‐centered clinical evaluation of acellular dermal matrix graft in the treatment of gingival recession defects. Journal of Periodontology 2007;78(12):2348‐55. [DOI] [PubMed] [Google Scholar]
Mahajan 2012 {published data only}
- Mahajan A, Bharadwaj A, Mahajan P. Comparison of periosteal pedicle graft and subepithelial connective tissue graft for the treatment of gingival recession defects. Australian Dental Journal 2012;57:51‐7. [DOI] [PubMed] [Google Scholar]
Mazzocco 2011 {published data only}
- Mazzocco F, Comuzzi L, Stefani R, Milan Y, Favero G, Stellini E. Coronally advanced flap combined with a subepithelial connective tissue graft using full‐ or partial‐thickness flap reflection. Journal of Periodontology 2011;82(11):1524‐9. [DOI] [PubMed] [Google Scholar]
Milinkovic 2015 {published data only}
- Milinkovic I, Aleksic Z, Jankovic S, Popovic O, Bajic M, Cakic S, et al. Clinical application of autologous fibroblast cell culture in gingival recession treatment. Journal of Dental Research 2015;50:363‐70. [DOI] [PubMed] [Google Scholar]
Modica 2000 {published data only}
- Modica F, Pizzo M, Roccuzzo M, Romagnoli R. Coronally advanced flap for the treatment of buccal gingival recessions with and without enamel matrix derivative. A split‐mouth study. Journal of Periodontology 2000;71(11):1693‐8. [DOI] [PubMed] [Google Scholar]
Moka 2014 {published data only}
- Moka LR, Boyapati R, Srinivas M, Swamy DN, Swarna C, Putcha M. Comparison of coronally advanced and semilunar coronally repositioned flap for the treatment of gingival recession. Journal of Clinical and Diagnostic Research 2014;8(6):ZC04‐ZC08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moses 2006 {published data only}
- Moses O, Artzi Z, Sculean A, Tal H, Kozlovsky A, Romanos GE, et al. Comparative study of two root coverage procedure: a 24‐month follow‐up multicenter study. Journal of Periodontology 2006;77(2):195‐202. [DOI] [PubMed] [Google Scholar]
Moslemi 2011 {published data only}
- Moslemi N, Jazi MM, Haghighati F, Morovati SP, Jamali R. Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: a 5‐year randomized clinical study. Journal of Clinical Periodontology 2011;38(12):1122‐9. [DOI] [PubMed] [Google Scholar]
Muller 1998 {published data only}
- Muller HP, Eger T, Schorb A. Gingival dimensions after root coverage with free connective tissue grafts. Journal of Clinical Periodontology 1998;25(5):424‐30. [DOI] [PubMed] [Google Scholar]
Muller 1999 {published data only}
- Muller HP, Stahl M, Eger T. Root coverage employing an envelope technique or guided tissue regeneration with a bioabsorbable membrane. Journal of Periodontology 1999;70(7):743‐51. [DOI] [PubMed] [Google Scholar]
Nazareth 2011 {published data only}
- Nazareth CA, Cury PR. Use of anorganic bovine derived hydroxyapatite matrix/cell‐binding peptide (P‐15) in the treatment of isolated Class I gingival recession defects: a pilot study. Journal of Periodontology 2011;82(5):700‐7. [DOI] [PubMed] [Google Scholar]
Nemcovsky 2004 {published data only}
- Nemcovsky CE, Artzi Z, Tal H, Kozlovsky A, Moses O. A multicenter comparative study of two root coverage procedures: coronally advanced flap with addition of enamel matrix proteins and subpedicle connective tissue graft. Journal of Periodontology 2004;75(4):600‐7. [DOI] [PubMed] [Google Scholar]
Ozcelik 2011 {published data only}
- Ozcelik O, Haytac MC, Seydaoglu G. Treatment of multiple gingival recessions using a coronally advanced flap procedure combined with button application. Journal of Clinical Periodontology 2011;38:572–80. [DOI] [PubMed] [Google Scholar]
Ozturan 2011 {published data only}
- Ozturan S, Durukan SA, Ozcelik O, Seydaoglu G, Haytac MC. Coronally advanced flap adjunct with low intensity laser therapy: a randomized controlled clinical pilot study. Journal of Clinical Periodontology 2011;38(11):1055‐62. [DOI] [PubMed] [Google Scholar]
Pilloni 2006 {published data only}
- Pilloni A, Paolantonio M, Camargo PM. Root coverage with a coronally positioned flap used in combination with enamel matrix derivative: 18‐month clinical evaluation. Journal of Periodontology 2006;77(12):2031‐9. [DOI] [PubMed] [Google Scholar]
Pini Prato 1992 {published data only}
- Pini Prato G, Tinti C, Vincenzi G, Magnani C, Cortellini P, Clauser C. Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recession. Journal of Periodontology 1992;63(11):919‐28. [DOI] [PubMed] [Google Scholar]
Pini Prato 1996 {published data only}
- Pini Prato G, Clauser C, Cortellini P, Tinti C, Vincenzi G, Pagliaro U. Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal recessions. A 4‐year follow‐up study. Journal of Periodontology 1996;67(11):1216‐23. [DOI] [PubMed] [Google Scholar]
Pini Prato 1999 {published data only}
- Pini‐Prato G, Baldi C, Pagliaro U, Nieri M, Saletta D, Rotundo R, et al. Coronally advanced flap procedure for root coverage. Treatment of root surface: root planning versus polishing. Journal of Periodontology 1999;70(9):1064‐76. [DOI] [PubMed] [Google Scholar]
Pini Prato 2000 {published data only}
- Pini Prato G, Pagliaro U, Baldi C, Nieri M, Saletta D, Cairo F, et al. Coronally advanced flap procedure for root coverage. Flap with tension versus flap without tension: a randomized controlled clinical study. Journal of Periodontology 2000;71(2):188‐201. [DOI] [PubMed] [Google Scholar]
Pini Prato 2005 {published data only}
- Pini Prato GP, Baldi C, Nieri M, Franseschi D, Cortellini P, Clauser C, et al. Coronally advanced flap: the post‐surgical position of the gingival margin is an important factor for achieving complete root coverage. Journal of Periodontology 2005;76(5):713‐22. [DOI] [PubMed] [Google Scholar]
Pini Prato 2011 {published data only}
- Pini Prato G, Rotundo R, Franceschi D, Cairo F, Cortellini P, Nieri M. Fourteen‐year outcomes of coronally advanced flap for root coverage: follow‐up from a randomized trial. Journal of Clinical Periodontology 2011;38:715‐20. [DOI] [PubMed] [Google Scholar]
Pourabbas 2009 {published data only}
- Pourabbas R, Chitsazi MT, Kosarieh E, Olyaee P. Coronally advanced flap in combination with acellular dermal matrix with or without enamel matrix derivatives for root coverage. Indian Journal of Dental Research 2009;20(3):320‐5. [DOI] [PubMed] [Google Scholar]
Rahmani 2006 {published data only}
- Rahmani ME, Lades MA. Comparative clinical evaluation of acellular dermal matrix allograft and connective tissue graft for the treatment of gingival recession. Journal of Contemporary Dental Practice 2006;7(2):63‐70. [PubMed] [Google Scholar]
Rebele 2014 {published data only}
- Rebele SF, Zuhr O, Schneider D, Jung RE, Heurzeler MB. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions. Journal of Clinical Periodontology 2014;41:593‐603. [DOI] [PubMed] [Google Scholar]
Ricci 1996 {published data only}
- Ricci G, Silvestri M, Rasperini G, Cattaneo V. Root coverage: a clinical/statistical comparison between subpedicle connective tissue graft and laterally positioned full thickness flaps. Journal of Esthetic Dentistry 1996;8(2):66‐73. [DOI] [PubMed] [Google Scholar]
Ricci 1996b {published data only}
- Ricci G, Silvestri M, Tinti C, Rasperini G. A clinical/statistical comparison between the subpedicle connective tissue graft method and the guided tissue regeneration technique in root coverage. International Journal of Periodontics & Restorative Dentistry 1996;16(6):538‐45. [PubMed] [Google Scholar]
Romagna‐Genon 2001 {published data only}
- Romagna‐Genon C. Comparative clinical study of guided tissue regeneration with a bioabsorbable bilayer collagen membrane and subepithelial connective tissue graft. Journal of Periodontology 2001;72(9):1258‐64. [DOI] [PubMed] [Google Scholar]
Roman 2013 {published data only}
- Roman A, Soanca A, Kasaj A, Stratul S‐I. Subepithelial connective tissue graft with or without enamel matrix derivative for the treatment of Miller class I and II gingival recessions: a controlled randomized clinical trial. Journal of Periodontal Research 2013;48:563‐72. [DOI] [PubMed] [Google Scholar]
Salhi 2014 {published data only}
- Salhi L, Lecloux G, Seidel L, Rompen E, Lambert F. Coronally advanced flap versus the pouch technique combined with a connective tissue graft to treat Miller's class I gingival recession: a randomized controlled trial. Journal of Clinical Periodontology 2014;41:387‐95. [DOI] [PubMed] [Google Scholar]
Sallum 2003 {published data only}
- Sallum EA, Casati MZ, Caffesse RG, Funis LP, Nociti FH Jr, Sallum AW. Coronally positioned flap with or without enamel matrix protein derivative for the treatment of gingival recessions. American Journal of Dentistry 2003;16(5):287‐91. [PubMed] [Google Scholar]
Santamaria 2017 {published data only}
- Santamaria MP, Fernandes‐Dias SB, Araújo CF, Lucas da Silva Neves F, Mathias IF, Rebelato Bechara Andere NM, et al. 2‐year assessment of tissue biostimulation with low‐level laser on the outcomes of connective tissue graft in the treatment of single gingival recession: a randomized clinical trial. Journal of Periodontology 2017;88(4):320‐8. [DOI] [PubMed] [Google Scholar]
Santamaria 2017b {published data only}
- Santamaria MP, Neves FLDS, Silveira CA, Mathias IF, Fernandes‐Dias SB, Jardini MAN, et al. Connective tissue graft and tunnel or trapezoidal flap for the treatment of single maxillary gingival recessions: a randomized clinical trial. Journal of Clinical Periodontology 2017;44(5):540‐7. [DOI] [PubMed] [Google Scholar]
Santana 2010 {published data only}
- Santana RB, Furtado MB, Mattos CML, Mello Fonseca E, Dibart S. Clinical evaluation of single stage advanced versus rotated flaps in the treatment of gingival recessions. Journal of Periodontology 2010;81(4):485‐92. [DOI] [PubMed] [Google Scholar]
Santana 2010b {published data only}
- Santana RB, Mattos CML, Dibart S. A clinical comparison of two flap designs for coronal advancement of the gingival margin: semilunar versus coronally advanced flap. Journal of Clinical Periodontology 2010;37(7):651‐8. [DOI] [PubMed] [Google Scholar]
Sbordone 1988 {published data only}
- Sbordone L, Ramaglia L, Spagnuolo G, Luca M. A comparative study of free gingival and subepithelial connective tissue grafts. Periodontal Case Reports 1988;10(1):8‐12. [PubMed] [Google Scholar]
Scabbia 1998 {published data only}
- Scabbia A, Trombelli L. Long‐term stability of the mucogingival complex following guided tissue regeneration in gingival recession defects. Journal of Clinical Periodontology 1998;25(12):1041‐6. [DOI] [PubMed] [Google Scholar]
Schlee 2011 {published data only}
- Schlee M, Esposito M. Human dermis graft versus autogenous connective tissue grafts for thickening soft tissue and covering multiple gingival recessions: 6‐month results from a preference clinical trial. European Journal of Oral Implantology 2011;4(2):119‐25. [PubMed] [Google Scholar]
Singh 2015 {published data only}
- Singh N, Uppoor A, Naik D. Semilunar coronally advanced flap with or without low level laser therapy in treatment of human maxillary multiple adjacent facial gingival recessions: a clinical study. Journal of Esthetic and Restorative Dentistry 2015;27(6):355‐66. [DOI] [PubMed] [Google Scholar]
Stefanini 2016 {published data only}
- Stefanini M, Jepsen K, Sanctis M, Baldini N, Greven B, Heinz B, et al. Patient‐reported outcomes and aesthetic evaluation of root coverage procedures: a 12‐month follow‐up of a randomized controlled clinical trial. Journal of Clinical Periodontology 2016;43(12):1132‐41. [DOI] [PubMed] [Google Scholar]
Tal 2002 {published data only}
- Tal H, Moses O, Zohar R, Meir H, Nemcovsky C. Root coverage of advanced gingival recession: a comparative study between acellular dermal matrix allograft and subepithelial connective tissue grafts. Journal of Periodontology 2002;73(12):1405‐11. [DOI] [PubMed] [Google Scholar]
Tatakis 2000 {published data only}
- Tatakis DN, Trombelli L. Gingival recession treatment: guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. Journal of Periodontology 2000;71(2):299‐307. [DOI] [PubMed] [Google Scholar]
Thombre 2013 {published data only}
- Thombre V, Koudale SB, Bhongade ML. Comparative evaluation of the effectiveness of coronally positioned flap with or without acellular dermal matrix allograft in the treatment of multiple marginal gingival recession defects. International Journal of Periodontics & Restorative Dentistry 2013;33(3):e88‐e94. [DOI] [PubMed] [Google Scholar]
Tonetti 2018 {published data only}
- Tonetti MS, Cortellini P, Pellegrini G, Nieri M, Bonaccini D, Allegri M, et al. Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: randomized trial assessing non‐inferiority in root coverage and superiority in oral health‐related quality of life. Journal of Clinical Periodontology 2018;45(1):78‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trabulsi 2004 {published data only}
- Trabulsi M, Oh TJ, Eber R, Weber D, Wang HL. Effect of enamel matrix derivative on collagen guided tissue regeneration‐based root coverage procedure. Journal of Periodontology 2004;75(11):1446‐57. [DOI] [PubMed] [Google Scholar]
Trombelli 1995 {published data only}
- Trombelli L, Schincaglia GP, Scapoli C, Calura G. Healing response of human buccal gingival recessions treated with expanded polytetrafluoroethylene membranes. A retrospective report. Journal of Periodontology 1995;66(1):14‐22. [DOI] [PubMed] [Google Scholar]
Trombelli 1995b {published data only}
- Trombelli L, Schincaglia GP, Zangari F, Griselli A, Scabbia A, Calura G. Effects of tetracycline HCl conditioning and fibrin‐fibronectin system application in the treatment of buccal gingival recession with guided tissue regeneration. Journal of Periodontology 1995;66(5):313‐20. [DOI] [PubMed] [Google Scholar]
Trombelli 1997 {published data only}
- Trombelli L, Tatakis DN, Scabbia A, Zimmerman GJ. Comparison of mucogingival changes following treatment with coronally positioned flap and guided tissue regeneration procedures. International Journal of Periodontics & Restorative Dentistry 1997;17(5):448‐55. [PubMed] [Google Scholar]
Trombelli 1998 {published data only}
- Trombelli L, Scabbia A, Tatakis DN, Calura G. Subpedicle connective tissue graft versus guided tissue regeneration with bioabsorbable membrane in the treatment of human gingival recession defects. Journal of Periodontology 1998;69(11):1271‐7. [DOI] [PubMed] [Google Scholar]
Trombelli 2005 {published data only}
- Trombelli L, Minenna L, Farina R, Scabbia A. Guided tissue regeneration in human gingival recessions. A 10‐year follow‐up study. Journal of Clinical Periodontology 2005;32(1):16‐20. [DOI] [PubMed] [Google Scholar]
Uzun 2018 {published data only}
- Uzun BC, Ercan E, Tunali M. Effectiveness and predictability of titanium‐prepared platelet‐rich fibrin for the management of multiple gingival recessions. Clinical Oral Investigations 2018;22(3):1345‐54. [DOI] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang H‐L, Romanos GE, Geurs NC, Sullivan A, Amo FS‐L, Eber RM. Comparison of two differently processed acellular dermal matrix products for root coverage procedures: a prospective, randomized multicenter study. Journal of Periodontology 2014;85(12):1693‐701. [DOI] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang H‐L, Amo FS‐L, Layher M, Eber R. Comparison of freeze‐dried and solvent‐dehydrated acellular dermal matrix for root coverage: a randomized controlled trial. International Journal of Periodontics & Restorative Dentistry 2015;35:811‐7. [DOI] [PubMed] [Google Scholar]
Wennström 1996 {published data only}
- Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2‐year prospective clinical study. Journal of Clinical Periodontology 1996;23(8):770‐7. [DOI] [PubMed] [Google Scholar]
Wilson 2005 {published data only}
- Wilson TG Jr, McGuire MK, Nunn ME. Evaluation of the safety and efficacy of periodontal applications of a living tissue‐engineered human fibroblast‐derived dermal substitute. II. Comparison to the subepithelial connective tissue graft: a randomized controlled feasibility study. Journal of Periodontology 2005;76(6):881‐9. [DOI] [PubMed] [Google Scholar]
Yilmaz 2014 {published data only}
- Yilmaz E, Ozcelik O, Comert M, Ozturan S, Seydaoglu G, Teughels W, et al. Laser‐assisted laterally positioned flap operation: a randomized controlled clinical trial. Photomedicine and Laser Surgery 2014;32(2):67‐74. [DOI] [PubMed] [Google Scholar]
Zucchelli 2010 {published data only}
- Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, et al. Patient morbidity and root coverage outcome after subepithelial connective tissue and de‐epithelialized grafts: a comparative randomized‐controlled clinical trial. Journal of Clinical Periodontology 2010;37(8):728–38. [DOI] [PubMed] [Google Scholar]
Zucchelli 2012 {published data only}
- Zucchelli G, Marzadori M, Mele M, Stefanini M, Montebugnoli L. Root coverage in molar teeth: a comparative controlled randomized clinical trial. Journal of Clinical Periodontology 2012;39(11):1082–8. [DOI] [PubMed] [Google Scholar]
Zuhr 2013 {published data only}
- Zuhr O, Rebele SF, Schneider D, Jung RE, Hurzeler MB. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient‐centred outcomes. Journal of Clinical Periodontology 2013;41:582–92. [DOI] [PubMed] [Google Scholar]
Additional references
AAP 1996
- American Academy of Periodontology. Consensus report. Mucogingival therapy. Annals of Periodontology 1996;1(1):702‐6. [DOI] [PubMed] [Google Scholar]
Agudio 2017
- Agudio G, Chambrone L, Pini Prato G. Biologic remodeling of periodontal dimensions of areas treated with gingival augmentation procedure: a 25‐year follow‐up observation. Journal of Periodontology 2017;88(7):634‐42. [DOI] [PubMed] [Google Scholar]
Baer 1981
- Baer PN, Benjamin SD. Gingival grafts: a historical note. Journal of Periodontology 1981;52(4):206‐7. [DOI] [PubMed] [Google Scholar]
Baldi 1999
- Baldi C, Pini‐Prato G, Pagliaro U, Nieri M, Saletta D, Muzzi L, et al. Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage? A 19‐case series. Journal of Periodontology 1999;70(9):1077‐84. [DOI] [PubMed] [Google Scholar]
Begg 1994
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088‐101. [PubMed] [Google Scholar]
Bernimoulin 1975
- Bernimoulin JP, Luscher B, Muhlemann HR. Coronally repositioned periodontal flap. Clinical evaluation after one year. Journal of Clinical Periodontology 1975;2(1):1‐13. [DOI] [PubMed] [Google Scholar]
Björn 1963
- Björn H. Free transplantation of gingiva propria. Sveriges Tandlak Tidskr 1963;22:684. [Google Scholar]
Buti 2013
- Buti J, Baccini M, Nieri M, Marca M, Pini‐Prato GP. Bayesian network meta‐analysis of root coverage procedures: ranking efficacy and identification of best treatment. Journal of Clinical Periodontology 2013;40:372‐86. [DOI] [PubMed] [Google Scholar]
Caffesse 1995
- Caffesse RG, Mota LF, Morrison EC. The rationale periodontal therapy. Periodontology 2000 1995;9:7‐13. [DOI] [PubMed] [Google Scholar]
Cairo 2009
- Cairo F, Rotundo R, Miller PD, Pini Prato GP. Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. Journal of Periodontology 2009;80:705‐10. [DOI] [PubMed] [Google Scholar]
Camargo 2001
- Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontology 2000 2001;27:72‐96. [DOI] [PubMed] [Google Scholar]
Chambrone 2003
- Chambrone L, Chambrone LA. Gingival recessions caused by lip piercing: case report. Journal of the Canadian Dental Association 2003;69(8):505‐8. [PubMed] [Google Scholar]
Chambrone 2006
- Chambrone LA, Chambrone L. Subepithelial connective tissue grafts in the treatment of multiple recession‐type defects. Journal of Periodontology 2006;77(5):909‐16. [DOI] [PubMed] [Google Scholar]
Chambrone 2008
- Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession‐type defects?. Journal of Dentistry 2008;36(9):659‐71. [DOI] [PubMed] [Google Scholar]
Chambrone 2009
- Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. The influence of tobacco smoking on the outcomes achieved by root coverage procedures: a systematic review. Journal of the American Dental Association 2009;140(3):294‐306. [DOI] [PubMed] [Google Scholar]
Chambrone 2010b
- Chambrone L, Faggion CM Jr, Pannuti CM, Chambrone LA. Evidence‐based periodontal plastic surgery: an assessment of quality of systematic reviews in the treatment of recession‐type defects. Journal of Clinical Periodontology 2010;37(12):1110‐8. [DOI: 10.1111/j.1600-051X.2010.01634.x.] [DOI] [PubMed] [Google Scholar]
Chambrone 2012
- Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence‐based periodontal plastic surgery. II. An individual data meta‐analysis for evaluating factors in achieving complete root coverage. Journal of Periodontology 2012;83(4):477‐90. [DOI: 10.1902/jop.2011.110382] [DOI] [PubMed] [Google Scholar]
Chambrone 2015
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. Journal of Periodontology 2015;86(2 Suppl):S8‐51. [DOI: 10.1902/jop.2015.130674] [DOI] [PubMed] [Google Scholar]
Chambrone 2016
- Chambrone L, Tatakis DN. Long‐term outcomes of untreated buccal gingival recessions: a systematic review and meta‐analysis. Journal of Periodontology 2016;87:796‐808. [DOI] [PubMed] [Google Scholar]
Checchi 1993
- Checchi L, Trombelli L. Postoperative pain and discomfort with and without periodontal dressing in conjunction with 0.2% chlorhexidine mouthwash after apically positioned flap procedure. Journal of Periodontology 1993;64(12):1238‐42. [DOI] [PubMed] [Google Scholar]
Cohen 1968
- Cohen DW, Ross SE. The double papillae repositioned flap in periodontal therapy. Journal of Periodontology 1968;39(2):65‐70. [DOI] [PubMed] [Google Scholar]
Curtin 2002
- Curtin F, Elbourne D, Altman DG. Meta‐analysis combining parallel and cross‐over clinical trials. II: Binary outcomes. Statistics in Medicine 2002;21(15):2145‐59. [DOI] [PubMed] [Google Scholar]
Donaldson 1973
- Donaldson D. Gingival recession associated with temporary crowns. Journal of Periodontology 1973;44:691‐6. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Esposito 2005
- Esposito M, Grusovin MG, Coulthard P, Worthington HV. Enamel matrix derivative (Emdogain) for periodontal tissue regeneration in intrabony defects. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD003875.pub2] [DOI] [PubMed] [Google Scholar]
Fardal 2002
- Fardal O, Johannessen AC, Linden GJ. Patient perceptions of periodontal therapy completed in a periodontal practice. Journal of Periodontology 2002;73(9):1060‐6. [DOI] [PubMed] [Google Scholar]
Follmann 1992
- Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology 1992;45(7):769‐73. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grupe 1956
- Grupe HE, Warren RF Jr. Repair of gingival defects by a sliding flap operation. Journal of Periodontology 1956;27:92‐5. [Google Scholar]
Grupe 1966
- Grupe HE. Modified technique for the sliding flap operation. Journal of Periodontology 1966;37(6):491‐5. [DOI] [PubMed] [Google Scholar]
Harris 1992
- Harris RJ. The connective tissue and partial thickness double pedicle graft: a predictable method of obtaining root coverage. Journal of Periodontology 1992;63(5):477‐86. [DOI] [PubMed] [Google Scholar]
Harvey 1965
- Harvey PM. Management of advanced periodontitis. I. Preliminary report of a method of surgical reconstruction. New Zealand Dental Journal 1965;61(285):180‐7. [PubMed] [Google Scholar]
Harvey 1970
- Harvey PM. Surgical reconstruction of the gingiva. II. Procedures. New Zealand Dental Journal 1970;66(303):42‐52. [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jørnung 2007
- Jørnung J, Fardal Ø. Perceptions of patients' smiles: a comparison of patients' and dentists' opinions. Journal of the American Dental Association 2007;138(12):1544‐53. [DOI] [PubMed] [Google Scholar]
Karadottir 2002
- Karadottir H, Lenoir L, Barbierato B, Bogle M, Riggs M, Sigurdsson T, et al. Pain experienced by patients during periodontal maintenance treatment. Journal of Periodontology 2002;73(5):536‐42. [DOI] [PubMed] [Google Scholar]
Khocht 1993
- Khocht A, Simon G, Person P, Denepitiya JL. Gingival recession in relation to history of hard toothbrush use. Journal of Periodontology 1993;64(9):900‐5. [DOI] [PubMed] [Google Scholar]
Langer 1985
- Langer B, Langer L. Subephithelial connective tissue graft technique for root coverage. Journal of Periodontology 1985;56(12):715‐20. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Löe 1992
- Löe H, Anerud A, Boysen H. The natural history of periodontal disease in man: prevalence, severity, extent of gingival recession. Journal of Periodontology 1992;63:489‐95. [DOI] [PubMed] [Google Scholar]
Martins 2004
- Martins AG, Andia DC, Sallum AW, Sallum EA, Casati MZ, Nociti Júnior FH. Smoking may affect root coverage outcome: a prospective clinical study in humans. Journal of Periodontology 2004;75(4):586‐91. [DOI] [PubMed] [Google Scholar]
Matthews 1993
- Matthews DC, McCulloch CA. Evaluating patient perceptions as short‐term outcomes of periodontal treatment: a comparison of surgical and non‐surgical therapy. Journal of Periodontology 1993;64(10):990‐7. [DOI] [PubMed] [Google Scholar]
McGuire 1995
- McGuire MK, Newman MG. Evidence‐based periodontal treatment. I. A strategy for clinical decisions. International Journal of Periodontics & Restorative Dentistry 1995;15(1):70‐83. [PubMed] [Google Scholar]
Miller 1985
- Miller PD Jr. A classification of marginal tissue recession. International Journal of Periodontics & Restorative Dentistry 1985;5(2):8‐13. [PubMed] [Google Scholar]
Nabers 1966
- Nabers JM. Free gingival grafts. Periodontics 1966;4(5):243‐5. [PubMed] [Google Scholar]
Needleman 2002
- Needleman IG. A guide to systematic reviews. Journal of Clinical Periodontology 2002;29 Suppl 3:6‐9. [DOI] [PubMed] [Google Scholar]
Needleman 2005
- Needleman I, Moles DR, Worthington H. Evidenced‐based periodontology, systematic reviews and research quality. Periodontology 2000 2005;37:12‐28. [DOI] [PubMed] [Google Scholar]
Needleman 2005b
- Needleman I, Tucker R, Giedrys‐Leeper E, Worthington H. Guided tissue regeneration for periodontal infrabony defects ‐ a Cochrane Systematic Review. Periodontology 2000 2005;37:106‐23. [DOI] [PubMed] [Google Scholar]
Ng 2006
- Ng SK, Leung WK. Oral health‐related quality of life and periodontal status. Community Dentistry and Oral Epidemiology 2006;34(2):114‐22. [DOI] [PubMed] [Google Scholar]
Nieri 2009
- Nieri M, Rotundo R, Franceschi D, Cairo F, Cortellini P, Pini Prato G. Factors affecting the outcome of the coronally advanced flap procedure: a Bayesian network analysis. Journal of Periodontology 2009;80:405‐10. [DOI] [PubMed] [Google Scholar]
Nieri 2013
- Nieri M, Pini Prato GP, Giani M, Magnani N, Pagliaro U, Rotundo R. Patient perceptions of buccal gingival recessions and requests for treatment. Journal of Clinical Periodontology 2017;40:707‐12. [DOI] [PubMed] [Google Scholar]
Oates 2003
- Oates TW, Robinson M, Gunsolley JC. Surgical therapies for the treatment of gingival recession. A systematic review. Annals of Periodontology 2003;8(1):303‐20. [DOI] [PubMed] [Google Scholar]
Ozcelik 2007
- Ozcelik O, Haytac MC, Seydaoglu G. Immediate post‐operative effects of different periodontal treatment modalities on oral health‐related quality of life: a randomized clinical trial. Journal of Clinical Periodontology 2007;34(9):788‐96. [DOI] [PubMed] [Google Scholar]
Parma‐Benefati 1985
- Parma‐Benfenati S, Frigazzato PA, Ruben MP. The effect of restorative margins on the postsurgical development and nature of the periodontium. Part I. International Journal of Periodontics and Restorative Dentistry 1985;5:30‐51. [PubMed] [Google Scholar]
Patur 1958
- Patur B, Glickan I. Gingival pedicle flaps for covering root surfaces denuded by chronic destructive periodontal disease: a clinical experiment. Journal of Periodontology 1958;29:50‐2. [Google Scholar]
Pini Prato 2002
- Pini Prato GP, Rotundo R, Magnani C, Ficarra G. Viral etiology of gingival recession. A case report. Journal of Periodontology 2002;73:110‐4. [DOI] [PubMed] [Google Scholar]
Pini Prato 2014
- Pini Prato G, Nieri M, Pagliaro U, Giorgi TS, Marca M, Franceschi D, et al. Surgical treatment of single gingival recessions: clinical guidelines. European Journal of Oral Implantology 2014;7(1):9‐43. [PubMed] [Google Scholar]
Pini Prato 2018
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richardson 2015
- Richardson CR, Allen EP, Chambrone L, Langer B, McGuire MK, Zabalegui I, et al. Periodontal soft tissue root coverage procedures: practical applications from the AAP Regeneration Workshop. Clinical Advances in Periodontics 2015;5(1):2‐10. [DOI] [PubMed] [Google Scholar]
Richmond 2007
- Richmond S, Chestnutt I, Shennan J, Brown R. The relationship of medical and dental factors to perceived general and dental health. Community Dentistry and Oral Epidemiology 2007;35(2):89‐97. [DOI] [PubMed] [Google Scholar]
Roccuzzo 2002
- Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: a systematic review. Journal of Clinical Periodontology 2002;29 Suppl 3:178‐94. [DOI] [PubMed] [Google Scholar]
Rotundo 2008
- Rotundo R, Nieri M, Mori M, Clauser C, Pini Prato G. Aesthetic perception after root coverage procedure. Journal of Clinical Periodontology 2008;35:705‐12. [DOI] [PubMed] [Google Scholar]
Saletta 2001
- Saletta D, Pini Prato G, Pagliaro U, Baldi C, Mauri M, Nieri M. Coronally advanced flap procedure: is the interdental papilla a prognostic factor for root coverage?. Journal of Periodontology 2001;72(6):760‐6. [DOI] [PubMed] [Google Scholar]
Silva 2007
- Silva CO, Lima AF, Sallum AW, Tatakis DN. Coronally positioned flap for root coverage in smokers and non‐smokers: stability of outcomes between 6 months and 2 years. Journal of Periodontology 2007;78(9):1702‐7. [DOI] [PubMed] [Google Scholar]
Smukler 1984
- Smukler H, Landsberg J. The toothbrush and gingival traumatic injury. Journal of Periodontology 1984;55:713‐9. [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732‐4. [DOI] [PubMed] [Google Scholar]
Steiner 1981
- Steiner GC, Person JK, Ainamo J. Changes on the marginal periodontium as a result of labial tooth movement in monkeys. Journal of Periodontology 1981;52:314‐20. [DOI] [PubMed] [Google Scholar]
Stoner 1980
- Stoner J, Mazdyasna S. Gingival recession in the lower incisor region of 15‐year‐old subjects. Journal of Periodontology 1980;51:74‐6. [DOI] [PubMed] [Google Scholar]
Sullivan 1968
- Sullivan HC, Atkins JH. Free autogenous gingival grafts. 3. Utilization of grafts in the treatment of gingival recession. Periodontics 1968;6(4):152‐60. [PubMed] [Google Scholar]
Sumner 1969
- Sumner CF 3rd. Surgical repair of recession on the maxillary cuspid: incisally repositioning the gingival tissues. Journal of Periodontology 1969;40(2):119‐21. [DOI] [PubMed] [Google Scholar]
Susin 2004
- Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. Journal of Periodontology 2004;75(10):1377‐86. [DOI] [PubMed] [Google Scholar]
Tarnow 1992
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. Journal of Periodontology 1992;63(12):995‐6. [DOI] [PubMed] [Google Scholar]
Tatakis 2015
- Tatakis DN, Chambrone L, Allen EP, Langer B, McGuire MK, Richardson CR, et al. Periodontal soft tissue root coverage procedures: a consensus report from the AAP Regeneration Workshop. Journal of Periodontology 2015;86(2 Suppl):S52–5. [DOI] [PubMed] [Google Scholar]
Tenenbaum 1982
- Tenenbaum H. A clinical study comparing the width of attached gingiva on the prevalence of gingival recession. Journal of Clinical Periodontology 1982;9:86‐92. [DOI] [PubMed] [Google Scholar]
Thomson 2006
- Thomson WM, Broadbent JM, Poulton R, Beck JD. Changes in periodontal disease experience from 26 to 32 years of age in a birth cohort. Journal of Periodontology 2006;77(6):947‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wennström 1987
- Wennström JL, Lindhe J, Sinclair F, Theilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. Journal of Clinical Periodontology 1987;14:121‐9. [DOI] [PubMed] [Google Scholar]
Yoneyama 1988
- Yoneyama T, Okamoto H, Lindhe J, Socransky SS, Haffajee AD. Probing depth, attachment loss and gingival recession. Findings from a clinical examination in Ushiku, Japan. Journal of Clinical Periodontology 1988;15(9):581‐91. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Chambrone 2008b
- Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of recession‐type defects. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD007161] [DOI] [PubMed] [Google Scholar]
Chambrone 2009b
- Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localised recession‐type defects. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD007161.pub2] [DOI] [PubMed] [Google Scholar]
Chambrone 2010
- Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root‐coverage procedures for the treatment of localized recession‐type defects: a Cochrane systematic review. Journal of Periodontology 2010;81(4):452‐78. [DOI: 10.1902/jop.2010.090540] [DOI] [PubMed] [Google Scholar]


