Abstract
Background
There has been a recent surge in the creation and adaptation of instruments to measure physical functioning (PF) in the intensive care unit (ICU). Selecting the right measurement instrument depends on understanding the core constructs that it measures in terms of the International Classification of Functioning, Disability and Health (ICF) domains.
Purpose
The purpose of this study was to map systematically the ICF domains and subdomains included in the PF measurement instruments used for adult patients during the ICU stay.
Data Sources
A systematic search was carried out in Cochrane CENTRAL, PubMed, CINAHL, and LILACS as well as a hand search up to May 17, 2017.
Study Selection
Study selection included all types of research articles that used at least 1 PF measurement instrument in adult patients within the ICU.
Data Extraction
Study design, year of publication, study population, and the measurement instruments reported were recorded. A consensus of experts analyzed the ICF domains included in each instrument.
Data Synthesis
We found 181 articles containing 60 PF measurement instruments used during the ICU stay. Twenty-six ICF domains were identified, 38 instruments included Mobility, and 13 included Muscle function.
Limitations
Studies not written in English or Spanish were excluded.
Conclusions
There are numerous PF measurement instruments used in adult patients in the ICU. The most frequent ICF domain measured is Mobility. This study highlights the ICF domains contained in the instruments that can be used clinically, providing a complete database of instruments that could facilitate selection of the most appropriate measure based on the patients’ needs.
Technological advances and interdisciplinary management in intensive care units (ICUs) have led to higher survival rates of patients who are critically ill1,2; however, survival can be associated with deterioration in physical functioning (PF),3,4 cognitive impairment, and decreased quality of life long after ICU discharge.5,6
PF is conceptualized as those physical abilities that allow functional independence and those related to movement.7,8 In 2001, the World Health Organization (WHO) introduced the International Classification of Functioning, Disability and Health (ICF).9 This was intended to provide a unified and standard language as a conceptual framework for the description of health and health-related well-being. The ICF framework describes human functioning as an umbrella concept of the interaction of 4 basic components: (1) body functions and structures, (2) activities and participation, (3) environmental factors, and (4) personal factors.9 Each of these components systematically groups various domains and subdomains to describe PF.9 For example, the domain “Mobility” is defined as bodily movement in daily activities; the subdomains of mobility include rolling over, sitting, standing, and walking.9
In clinical practice, PF should be assessed early in order to identify changes in PF that occur during the ICU stay, to evaluate the success of the interventions, and to aid in discharge planning and identify patients with risk of subsequent physical deterioration.10,11 This has led to the creation, clinimetric evaluation, and adaptation of various PF measurement instruments for use in the ICU.12 However, there is evidence of heterogeneity in the use of outcomes within clinical trials in patients in the ICU.13 A systematic review by Parry et al identified 33 measurement instruments designed to assess muscle mass, muscle strength, and PF in critically ill patients, and evidenced considerable variability in the instruments used to measure different ICF domains.14 This makes it difficult to know how to select the best measure for use in clinical practice and research.
A key step in correctly understanding the contents of the instruments is identifying the domains included in each one.10 The aim of this scoping review was to identify the ICF domains and subdomains included in the PF measurement instruments used with adult patients during the ICU stay.
Methods
Study Design
A scoping review was conducted to identify the PF measurement instruments applied to adult patients in the ICU that have been reported in published scientific articles, and subsequently identify the ICF domains included within these instruments. In this study, the Joanna Briggs Institute methodological guide for carrying out scoping reviews was used.15
Research Question
What are the ICF domains included in the PF measurement instruments used with the adult ICU patient population reported in the scientific literature?
Data Sources and Systematic Search
A systematic search was conducted in the Cochrane CENTRAL, PubMed, CINAHL, and LILACS electronic databases using a strategy with keywords and MeSH terms associated with “Measurement Instrument,” “Intensive Care Units,” and “Physical Function” (see Appendix) from inception to May 17, 2017, to identify the PF measurement instruments of the adult ICU patient population reported in the scientific literature. It was filtered by language (English and Spanish), and all types of study design were considered. To incorporate the largest number of PF measurement instruments, database searches were supplemented by a hand search of articles related to ICU measurement instruments.
Selection of Articles
Articles were included if in the methodology the full text described the use of at least 1 PF measurement instrument at any time point during the ICU stay.
The following exclusion criteria were applied: (1) articles that did not report measuring PF in the ICU, such as those that assess long-term results, contextual factors, or quality of life (ie, SF-36, EQ5D, satisfaction questionnaires, anxiety, cognitive deficiencies, etc); (2) articles that targeted populations other than adult patients in the ICU (ie, ICU survivors, post-ICU poutpatient, ward, emergency, pediatric, neonatal); (3) articles that did not specify if the measurements were completed during the ICU stay; and (4) laboratory articles (in vitro) or performed in animal models.
A researcher (F.G-S.) carried out the article selection process in 3 stages, applying filter by title, abstract, and full text according to the eligibility criteria. A second researcher (C.M-O.) performed a quality control check by randomly selecting 12 (10%) excluded articles in each of the selection stages and reviewing them to validate this filtering process. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement,16 and the “include rather than exclude” methodology were used to review the full text of potentially relevant articles.17 This meant that if at least 1 of the excluded articles was considered appropriate for inclusion after the quality control check (C.M-O.), all articles excluded at that stage were reviewed again (F.G-S.).
Data Extraction
The included articles were collated in a Microsoft Excel data extraction spreadsheet by F.G-S. A second researcher (C.M-O.) performed the same process as a quality control check at this stage. These data were then inputted into a consensus matrix between the 2 researchers (C.M-O. and F.G-S.). The following study information was extracted: (1) study design (observational, clinical trials, validation, others); (2) year of publication (inception to 1999, 2000–2009, 2010–2017); (3) study population (Medical/Respiratory, Surgical, Neurocritical care/Neurosurgical, Cardiothoracic/Cardio-surgical, Trauma, Burns, and Mixed/General); and (4) PF instruments used or named in the ICU setting, including scales and scores (defined as instruments or tests that capture current physical performance measures through the evaluator observation and scoring), questionnaires (defined as self-report surveys, in which the patient or family must report their previous or current condition), and biophysical instruments (defined as technological devices that use concepts from physics to measure function, structure, or activity).
Synthesis and Analysis of Measurement Instruments
The PF instruments used within ICU studies were extracted from the full-text articles included in the review and were analyzed according to the following ICF domains and subdomains (available at http://apps.who.int/classifications/icfbrowser/) based on the definitions of the ICF components:
Body Functions: defined as the physiological functions of body systems (including psychological functions).
Body Structures: defined as anatomical parts of the body such as organs, limbs, and their components.
Activities and Participation: activity corresponds to the execution of a task or action by an individual, and participation is the involvement of a person in a life situation.
Environmental Factors: These comprise the physical, social, and attitudinal environment in which people live and conduct their lives.
Two researchers (E.J.C. and F.G-S.) independently analyzed the content of the full version of PF measurement instruments to identify the ICF domains represented within them. This was done using a preconstructed data spreadsheet in Microsoft Excel; the presence or absence of each domain in the instruments according to the definitions of the ICF was recorded within the spreadsheet.9,18 If the instruments included other ICF domains or subdomains, they were recorded and analyzed.
The classification of all PF instruments by both researchers (E.J.C. and F.G-S.) was then compared; any differences were resolved by discussion until a consensus was reached. Finally, another researcher (C.M-O.) performed a third quality control check on 15 (25%) randomly selected instruments to verify the classification of the domains and subdomains that had been identified.
Results
Study Selection
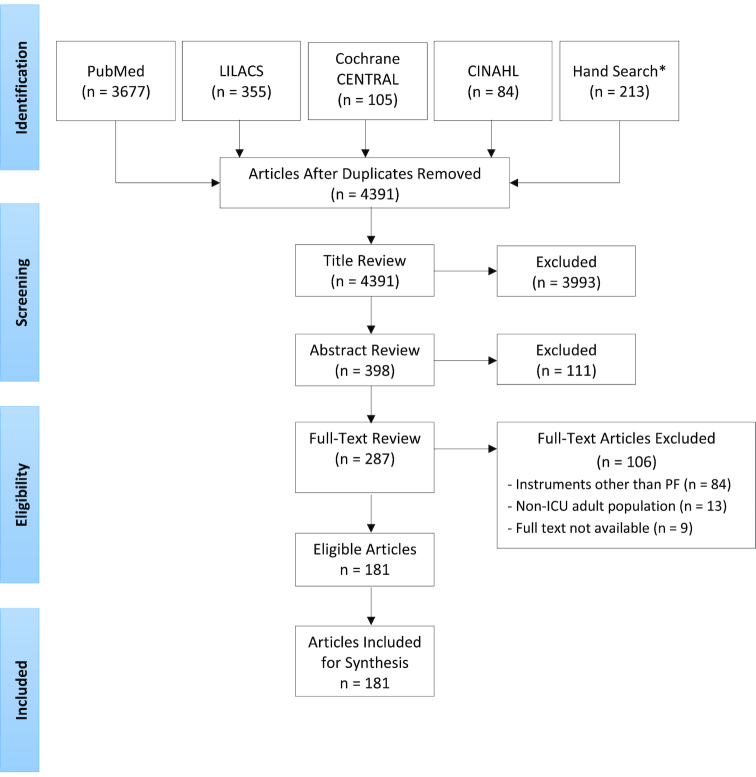
The initial search yielded 4434 citations that were filtered through removal of duplicates and irrelevant articles (Figure). The 181 full-text articles that met the eligibility criteria were analyzed to extract the PF measurement instruments.
Figure.
Flow diagram of the included articles. Asterisk (*), twenty-seven articles were selected by hand search from author's personal files reviewed by title (see supplementary material online, available at https://academic.oup.com/ptj). CENTRAL = Cochrane Controlled Trials Registry; CINAHL = Cumulative Index of Nursing and Allied Health Literature; LILACS = Literatura Latinoamericana de Información en Ciencias de la Salud; PF = physical functioning; ICU = intensive care unit.
Characteristics of Included Articles
Table 1 summarizes the bibliometric information of the included studies. The first research article that included a measure of PF in the ICU (maximal inspiratory pressure) was published in 1990. Articles published between 1990 and 1999 represent only 2.8% of all the articles included in this scoping review; between 2000 and 2009 this increased to 10.5%, whereas most (86.7%) were published between 2010 and 2017.
Table 1.
Characteristics of the Articles Included in This Scoping Review (n = 181)
| Characteristic | n (%) |
|---|---|
| Year of publication | |
| 1990–1999 | 5 (2.8) |
| 2000–2009 | 19 (10.5) |
| 2010–2017 | 157 (86.7) |
| Study design | |
| Observational study | 76 (42) |
| Clinical trial | 27 (15) |
| Validation study | 27 (15) |
| Othera | 51 (28) |
| Type of intensive care unit | |
| Mixed/general | 72 (40) |
| Medical/respiratory | 16 (8.8) |
| Surgical | 13 (7.2) |
| Neurocritical/neurosurgical | 7 (4) |
| Cardiothoracic/cardiosurgical | 5 (2.8) |
| Burn | 2 (1.1) |
| Traumatology | 1 (0.6) |
| Intensive care unit not specified | 65 (36) |
aIncludes systematic reviews, narrative reviews, editorials, surveys, pilot studies, consensus and expert recommendations.
Of the research articles included in this review, 42% were observational studies and 15% were clinical trials (8.7% of these were randomized clinical trials). The validation studies identified were on psychometric properties and cross-cultural adaptation of different instruments (15%). Forty percent of studies were conducted in a mixed or general ICU, whereas 36% did not explicitly report the type of ICU (Tab. 1).
Physical Functioning Measurement Instruments in the ICU
There were 60 PF measurement instruments used within the ICU setting discussed within the 181 selected articles. Thirty-three of the instruments were scales or scores, 18 were biophysical instruments, and 9 were questionnaires. Two other instruments were found, the Swedish Simple Early Mobility Scale19 and the ICU Patient-Reported Functional Scale20; these do not yet have the full version available to identify the ICF domains and for this reason they were not included for the analysis.
The only measurement instruments reported in the burn intensive care unit setting were the Chelsea Critical Care Physical Assessment Tool (CPAx), the Barthel Index, the Functional Independence Measure, and goniometry. The instruments that were reported in the neurological/neurosurgical intensive care unit setting were the Functional Status Score for the Intensive Care Unit, Barthel Index, Glasgow Outcome Score, Disability Rating Scale, handheld dynamometry, computed tomography muscle scan (CT muscle scan), and the Critical Care Functional Rehabilitation Outcome Measure. In the cardiovascular/cardio-surgical intensive care unit setting the Medical Research Council Sum Score, Perme Intensive Care Unit Mobility Scale, peripheral muscle ultrasound, handgrip dynamometry, and maximal inspiratory pressure were identified.
We found 26 domains related to the PF within 60 instruments: 14 Body Functions, 8 Activities and Participation, 3 Body Structures, and 1 domain related to Environmental Factors. In addition to the 12 ICF domains related to PF, 14 other domains were identified (Tab. 2). The most frequently identified domains in the PF measurement instruments were: Mobility (n = 38, 63.3%), Muscle function (strength, resistance, and tone) (n = 13, 21.7%), and Movement functions (postural reactions, reactions of balance, walking pattern, and sensations related to muscles) (n = 12, 20%). Of the 60 instruments described in this review, none included all 4 components of the ICF (Body Functions and Structures, Activities and Participation, Environmental Factors, and Personal Factors). Table 3 shows the ICF domains included in the 42 scales, scores, and questionnaires, and Table 4 shows the ICF domains included in the 18 biophysical instruments.
Table 2.
International Classification of Functioning, Disability and Health (ICF) Domains Included in the Measurement Instruments of This Scoping Review (n = 26)
| Related to Physical Functioning (n = 12) | Other ICF domains (n = 14) |
|---|---|
| Body Functions | |
| Respiratory muscle functions (b445) Exercise tolerance functions (b455) Functions of joints and bones (b710–b729) Muscle functions (b730–b749) Movement functions (b750–b789) | Mental functions (b1) Sensory functions and pain (b2) Maintenance of blood pressure (b4202) Respiration functions (b440) Additional respiratory functions (b450) Ingestion functions (b510) Defecation functions (b525) Urinary functions (b610–b639) Functions of the skin (b810–b849) |
| Body Structures | |
| Muscles of respiration (s4303) Structures related to movement (s710–s799) | Structure of areas of skin (s810) |
| Activities and Participation | |
| General tasks and demands (d2) Mobility (d4) Self-care (d5) Domestic life (d6) | Learning and applying knowledge (d1) Communication (d3) Major life areas (d8) Community, social, and civic life (d9) |
| Environmental Factors | |
| Products and technology for personal use in daily living (e115) | |
Table 3.
ICF Domains of the 42 Physical Functioning Scales, Scores, and Questionnaires Used in the Adult ICUa
| Functions of the Joints and Bones (b710-b729) | Muscle Functions (b730-b749) | Movement Functions (b750-b789) | Respiratory Muscle Functions (b445) | Exercise Tolerance Functions (b455) | Respiration Functions (b440) | Other Body Functionsb | Structures Related to Movement (s7) | Muscles of Respiration (s433) | General Tasks and Demands (d2) | Mobility (d4) | Self-Care (d5) | Domestic Life (d6) | Community, Social, and Civic Life (d9) | Other Activities and Participationc | Products and Technology for Personal Use in Daily Living (e115) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scales/scores | MRC Sum Score/MMT | x | |||||||||||||||
| MRC 4-point Scale | x | ||||||||||||||||
| FSS-ICU | x | ||||||||||||||||
| DEMMI | x | x | |||||||||||||||
| SOMS | x | ||||||||||||||||
| MMS | x | ||||||||||||||||
| ICU Mobility Scale | x | ||||||||||||||||
| 5-point Mobility Scale | x | ||||||||||||||||
| Mobilization Scale | x | ||||||||||||||||
| CPAx | x | x | x | x | x | ||||||||||||
| PFIT | x | x | x | ||||||||||||||
| PFIT-s | x | x | x | ||||||||||||||
| Perme ICU Mobility Scale | x | x | x | x | x | x | x | ||||||||||
| CcFROM | x | x | x | ||||||||||||||
| ACIF | x | x | x | x | |||||||||||||
| mRMI | x | x | |||||||||||||||
| FAC | x | ||||||||||||||||
| SPPB | x | x | x | ||||||||||||||
| 6MWD | x | x | |||||||||||||||
| 2MWD | x | x | |||||||||||||||
| 4-m Walking Test | x | ||||||||||||||||
| 30-s Sit-to-Stand Test | x | x | x | ||||||||||||||
| FTSST | x | x | |||||||||||||||
| Timed Up & Go | x | ||||||||||||||||
| COMHON Index | x | x | x | ||||||||||||||
| FIM | x | x | x | x | x | x | |||||||||||
| mmFIM | x | ||||||||||||||||
| NSAd | x | x | |||||||||||||||
| Modified Ashworth Scale | x | ||||||||||||||||
| Berg Balance Scale | x | x | |||||||||||||||
| Modified Rankin Scale | x | x | x | x | x | ||||||||||||
| Borg Scale | x | x | |||||||||||||||
| Fatigue Resistance Index | x | x | |||||||||||||||
| Questionnaires | Barthel Index | x | x | x | x | ||||||||||||
| ERBI | x | x | x | x | x | x | |||||||||||
| Clinical Frailty Scale | x | x | x | x | x | x | |||||||||||
| KPS | x | x | x | x | x | ||||||||||||
| Katz ADL Scale | x | x | x | x | |||||||||||||
| Lawton IADL Scale | x | x | x | ||||||||||||||
| GOS/eGOS | x | x | x | x | x | ||||||||||||
| DisabilityRating Scale | x | x | x | x | x | x | x | x | |||||||||
| HACC | x | x | x | x | x | x | x |
aACIF = Acute Care Index of Function; ADL = Activities of Daily Living; CcFROM = Critical Care Functional Rehabilitation Outcome Measure; COMHON = Conscious level, Mobility, Hemodynamics, Oxygenation, Nutrition Index; CPAx = Chelsea Critical Care Physical Assessment Tool; DEMMI = de Morton Mobility Index; ERBI = Early Rehabilitation Barthel Index; FAC = Functional Ambulation Categories; FIM = Functional Independence Measure; FSS-ICU = Functional Status Score for the Intensive Care Unit; FTSST = Five Times Sit-to-Stand Test; GOS/eGOS = Glasgow Outcome Score/extended Glasgow Outcome Score; HACC = Home And Community Care functional assessment scale; IADL = Instrumental Activities of Daily Living Scale; ICF = International Classification of Functioning, Disability and Health; ICU = intensive care unit, KPS = Karnofsky Performance Scale; mmFIM = mini-modified Functional Independence Measure Score; MMS = Manchester Mobility Score; MMT = manual muscle test; MRC = Medical Research Council; mRMI = Modified Rivermead Mobility Index; MWD = minute walking distance; NSA = Modified Nottingham Sensory Assessment; PFIT-s = Physical Function in Intensive Care Test Score; SOMS = SICU Optimal Mobilisation Score; SPPB = Short Physical Performance Battery.
bOther Body functions were identified in the following measurement instruments: Mental functions (b1): Perme Intensive Care Unit Mobility Scale (Perme IMS), Acute Care Index of Function (ACIF), COMHON, FIM, ERBI, and Disability Rating Scale; Sensory functions and pain (b2): NSA and Perme IMS; Maintenance of blood pressure (b422): COMHON; Additional respiratory functions (b450): CPAx (cough); Ingestion functions (b510): COMHON and ERBI; Defecation functions (b525): FIM, Barthel Index, ERBI, Katz ADL scale, and HACC; Urinary functions (b610-b639) and Functions of the skin (b810-b849): NSA.
cOther Activities and participation were identified in the following measurement instruments: Learning and applying knowledge (d1): ACIF, FIM, and Clinical Frailty scale; Communication (d3): FIM, ERBI, Lawton IADL Scale, Disability Rating Scale, and HACC; Major life areas (d8): Lawton IADL Scale and Disability Rating Scale.
dIncludes Structure of areas of skin (s810).
Table 4.
ICF Domains of 18 Physical Functioning Biophysical Instruments Used in the Adult ICUa
| Biophysical Instruments | Functions of the Joints and Bones (b710-b729) | Muscle Functions (b730-b749) | Movement Functions (b750-b789) | Respiratory Muscle Functions (b445) | Exercise Tolerance Functions (b455) | Respiration Functions (b440) | Other Body Functions | Structures Related to Movement (s7) | Muscles of Respiration (s433) | General Tasks and Demands (d2) | Mobility (d4) | Self-Care (d5) | Domestic Life (d6) | Community, Social, and Civic Life (d9) | Other Activities and Participation | Products and Technology for Personal Use in Daily Living (e115) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Goniometry | x | x | ||||||||||||||
| Dynamometryb | x | |||||||||||||||
| Peripheral muscle ultrasound | x | |||||||||||||||
| Diaphragm ultrasound | x | x | ||||||||||||||
| Accelerometryc | x | x | x | |||||||||||||
| SWA-MF | x | x | x | |||||||||||||
| Noninvasive mobility sensor | x | |||||||||||||||
| MIP/NIF | x | |||||||||||||||
| Maximal expiratory pressure | x | |||||||||||||||
| DxA | x | |||||||||||||||
| Bioimpedance spectroscopy | x | |||||||||||||||
| CT muscle scan | x | x | ||||||||||||||
| Muscle circumference | x | |||||||||||||||
| Muscle biopsy | x | |||||||||||||||
| Electromyographyd | x | |||||||||||||||
| PdiTw | x | |||||||||||||||
| Quadriceps twitch tension | x | |||||||||||||||
| Peroneal nerve test | x |
aCT = computed tomography; DxA = dual-energy X-ray absorptiometry; ICF = International Classification of Functioning, Disability and Health; ICU = intensive care unit; MIP = maximal inspiratory pressure; NIF = negative inspiratory force; PdiTw = transdiaphragmatic pressure in response to phrenic nerve stimulation; SWA-MF = Sensewear armband mini-fly motion sensor.
bIncludes handgrip and handheld dynamometry.
cIncludes sensor movement, accelerometry, and physical activity monitor.
dIncludes electromyography, nerve conduction studies, and electrophysiological studies.
Mobility Measurement Instruments in the ICU
Because mobility was the most commonly reported domain, the description of 19 Mobility subdomains identified in the instruments has been included (Tab. 5). The subdomain identified most frequently was Walking short distances (n = 26), and the subdomains identified the least (ie, in only 1 instrument) were Reaching (on Berg Balance Scale), Jumping (on the de Morton Mobility Index [DEMMI]), and Walking on different surfaces (on Functional Ambulation Categories).
Table 5.
ICF Mobility Subdomains of 38 Physical Functioning Instruments Used in the Adult ICUa
| Lying Down (d4100) | Sitting (d4103) | Standing (d4104) | Bending (d4105) | Shifting the Body's CoG (d4106) | Rolling Over (d4107)b | Maintaining a Lying Position (d4150) | Maintaining a Sitting Position (d4153) | Maintaining a Standing Position (d4154) | Transferring Oneself While Sitting (d4200) | Transferring Oneself While Lying (d4201) | Fine Hand Use – Picking Up (d4400) | Reaching (d4452) | Walking Short Distances (d4500) | Walking on Different Surfaces (d4502) | Walking, Other Specified (d4508)c | Climbing (d4551) | Jumping (d4553) | Moving Around Using Equipment: Wheelchair (d465) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure Mobility | CPAx | x | x | x | x | x | x | x | x | |||||||||||
| DEMMI | x | x | x | x | x | x | x | x | x | x | ||||||||||
| PFIT | x | x | ||||||||||||||||||
| PFIT-s | x | x | ||||||||||||||||||
| Perme ICU Mobility Scale | x | x | x | x | x | x | x | |||||||||||||
| CcFROM | x | x | x | x | x | x | x | x | ||||||||||||
| ACIF | x | x | x | x | x | x | x | x | x | x | ||||||||||
| MRMi | x | x | x | x | x | x | x | x | x | |||||||||||
| SPPB | x | x | x | x | x | |||||||||||||||
| 6MWD | x | |||||||||||||||||||
| 2MWD | x | |||||||||||||||||||
| 30-s Sit to Stand Test | x | x | ||||||||||||||||||
| FTSST | x | x | ||||||||||||||||||
| COMHON Index | x | x | x | x | x | x | ||||||||||||||
| FIM | x | x | x | x | x | x | ||||||||||||||
| Berg Balance Scale | x | x | x | x | x | x | x | x | x | |||||||||||
| Modified Rankin Scale | x | |||||||||||||||||||
| Barthel Index | x | x | x | x | x | x | ||||||||||||||
| ERBI | x | x | x | x | x | x | ||||||||||||||
| Katz ADL Scale | x | |||||||||||||||||||
| HACC | x | x | x | x | ||||||||||||||||
| Clinical Frailty Scale | Not specified | |||||||||||||||||||
| KPS | Not specified | |||||||||||||||||||
| GOS/eGOS | Not specified | |||||||||||||||||||
| Disability Rating Scale | Not specified | |||||||||||||||||||
| Accelerometryd | Not specified | |||||||||||||||||||
| SWA-MF | Not specified | |||||||||||||||||||
| ONLY Measure Mobility | FSS-ICU | x | x | x | x | x | x | x | ||||||||||||
| SOMS | x | x | x | x | x | x | ||||||||||||||
| MMS | x | x | x | x | x | x | x | |||||||||||||
| ICU Mobility Scale | x | x | x | x | x | x | x | x | x | x | ||||||||||
| 5-point Mobility Scale | x | x | x | x | x | |||||||||||||||
| Mobilization Scale | x | x | x | x | x | x | x | |||||||||||||
| FAC | x | x | ||||||||||||||||||
| mmFIM | x | x | x | |||||||||||||||||
| 4-m Walking Test | x | |||||||||||||||||||
| Timed “Up & Go” | x | x | x | |||||||||||||||||
| Noninvasive Mobility Sensor | Not specified | |||||||||||||||||||
aACIF = Acute Care Index of Function; ADL = Activities of Daily Living; CcFROM = Critical Care Functional Rehabilitation Outcome Measure; COMHON = Conscious level, Mobility, Hemodynamics, Oxygenation, Nutrition Index; CPAx = Chelsea Critical Care Physical Assessment Tool; DEMMI = de Morton Mobility Index; FAC = Functional Ambulation Categories; FIM = Functional Independence Measure; FSS-ICU = Functional Status Score for the Intensive Care Unit; FTSST = Five Times Sit-to-Stand Test; GOS/eGOS = Glasgow Outcome Score/extended Glasgow Outcome Score; HACC = Home And Community Care functional assessment scale; ICF = International Classification of Functioning, Disability and Health; ICU = intensive care unit, KPS = Karnofsky Performance Scale; mmFIM = mini-modified Functional Independence Measure Score; MMS = Manchester Mobility Score; mRMI = Modified Rivermead Mobility Index; MWD = minute walking distance; PFIT-s = Physical Function in Intensive Care Test Score; SOMS = SICU Optimal Mobilisation Score; SPPB = Short Physical Performance Battery; SWA-MF = Sensewear armband mini-fly motion sensor.
bImplemented ICF Update Proposals 2012 (https://extranet.who.int/icfrevision/nr/loginICF.aspx).
cIncludes: marching on the spot, stepping, or steps-in-place.
dIncludes: sensor movement, accelerometry, and physical activity monitor.
In 7 instruments (Clinical Frailty Scale, Karnofsky Performance Scale, Glasgow Outcome Score/extended Glasgow Outcome Score, Disability Rating Scale, accelerometry, Sensewear armband mini-fly motion sensor, and Noninvasive Mobility Sensor) the Mobility subdomain could not be identified, so “not specified” was used.
The biophysical instruments capable of measuring Mobility in the ICU were accelerometry, the Sensewear armband mini-fly motion sensor, and the Noninvasive Mobility Sensor. Of all instruments that measure Mobility, those that included the most Mobility subdomains (10 subdomains each) were the Intensive Care Unit Mobility Scale, the Acute Care Index of Function, and DEMMI.
Of the 38 instruments that measured Mobility, 11 measured this domain exclusively, whereas others integrated different Function and Activities in the same measurement instrument, such as the CPAx, Physical Function in Intensive Care Test-scored, Short Physical Performance Battery, DEMMI, Critical Care Functional Rehabilitation Outcome Measure, Berg Balance Scale, and Perme Intensive Care Unit Mobility Scale. All instruments that measured Mobility exclusively measured Walking short distances, and only the Functional Status Score for the Intensive Care Unit, Intensive Care Unit Mobility Scale, and Mini-Modified Functional Independence Measure Score included the Moving around using equipment subdomain (ie, wheelchair mobility). The detailed results of the Mobility subdomains are shown in Table 5.
Discussion
This scoping review aimed to identify the ICF domains and subdomains included in the PF measurement instruments used in adult patients during the ICU stay. The purpose was to provide a quick reference guide for researchers and clinicians when selecting measures of PF in practice.
Sixty PF measurement instruments were identified, covering 26 ICF domains and 19 Mobility subdomains. Of the 181 articles selected, 2.8% (n = 5) were published between 1990 and 1999, whereas 86.7% (n = 153) were published between 2010 and 2017. This highlights the rapid increase in the number of publications of articles that include PF measurement instruments in the adult ICU since the beginning of the 21st century. This is consistent with the increasing interest in morbidity as an important outcome of critical illness, and not merely mortality.6,21 The multiple constructs included within these instruments also demonstrate how multifaceted and complex the physical impairments of patients in the ICU are, and the variation in tools reflects the lack of consensus on the most robust and important measurement instruments.10,22
This scoping review provides a quick reference guide to assist clinicians and researchers in the selection of PF measurement instruments available based on the ICF framework. The World Health Organization and the World Confederation for Physical Therapy have proposed the use of the ICF as a universal framework for interdisciplinary teams and physical therapist practice.8,23 The ICF can be used for clinical, educational, and/or research purposes and as a planning tool for service-level decision-makers.18 Therefore, using measurement instruments mapped to the ICF domains will be beneficial in both clinical practice and research.22 No studies to date have mapped all PF measures used in critical care research to the ICF domains. Parry et al published a systematic review that identified 33 instruments that measure muscle mass, muscle strength, and PF at any point in the recovery from critical illness (from ICU to posthospitalization),14 but this was not mapped against the specific ICF domains and subdomains for each instruments. Subsequently, in 2017 Parry et al identified the ICF domains included in 11 of the best-known PF instruments (all of them included in our review), and highlighted important differences in the contents of the instruments when the ICF subdomains are considered24; however, this was not an exhaustive list.
The most frequent domain identified in our study was Mobility (included in 38 instruments), which reflects the importance placed on mobility in the ICU. Mobility includes more than 80 subdomains,9 19 of which were included in the PF measures in ICU. Systematic reviews have shown the importance of the measurement of Mobility in acute hospital settings and in elderly patients, because independence in mobility is a key factor in determining discharge after acute hospitalization and has been identified as a predictor of many important outcomes.25,26
Mobility is measured in different ways within the instruments: (1) by measuring the duration of a position or activity (ie, Berg Balance Scale, Short Physical Performance Battery, DEMMI); (2) achieving a specific mobility level (ie, Intensive Care Unit Mobility Scale, Manchester Mobility Score, Physical Function in Intensive Care Test-scored); (3) measuring the distance or time walked (ie, 6-minute walking distance, 2-minute walking distance, 4-meter walking test, Timed Up & Go); or (4) measuring the level of assistance required by the patient for a specific activity (ie, Functional Status Score for the Intensive Care Unit , CPAx, Perme Intensive Care Unit Mobility Scale). Selecting the most appropriate measurement instrument will depend on available clinical resources/expertise, and the reason for assessment (ie, research, education, clinical practice).27
Rolling over is a fundamental component of Mobility in the ICU because it is one of the first activities that can be performed safely by a critical care patient. Rolling over requires good trunk control and limb strength,28 and its execution has repercussions for higher activities, such as standing and walking.29 Despite this only 8 instruments measure Rolling over (CPAx, DEMMI, Critical Care Functional Rehabilitation Outcome Measure, Acute Care Index of Function, Modified Rivermead Mobility Index, Functional Status Score for the Intensive Care Unit, Intensive Care Unit Mobility Scale, and Mobilization Scale).
Walking has been shown to improve lung function in mechanically ventilated patients and can facilitate ventilatory weaning, and minimize the problems associated with prolonged bed rest.30 In the present study, Walking short distances (<1 km) is the Mobility subdomain most frequently identified (n = 26), which demonstrates the importance of walking as part of the evaluation in the ICU.31
It has been argued that measurement using scores or ordinal scales can present problems in the accuracy of the results, so it is necessary to use biophysical instruments to better quantify Mobility in the ICU32; of these only 3 such instruments were identified in this review (accelerometry, Sensewear armband mini-fly motion sensor, and Noninvasive Mobility Sensor).
The second domain most frequently identified in this study was Muscle function (n = 13). The development of muscle weakness of the extremities is associated with a prolonged duration on mechanical ventilation, a prolonged stay in the ICU, and an increased risk of morbidity and mortality.33,34 The evaluation of muscle strength is important in selecting the “dosage” of physical exercise and evaluating the effect of clinical interventions.35 The Muscle function domain includes mainly the measurement of Muscle strength functions (ie, Medical Research Council Sum Score, handheld dynamometry, handgrip dynamometry, Physical Function in Intensive Care Test-scored, CPAx), Muscle tone functions (ie, Modified Ashworth Scale), and Muscle endurance functions (ie, Perme Intensive Care Unit Mobility Scale, Short Physical Performance Battery). Unlike the other instruments, the CPAx includes domains of Mobility, Balance (nonvestibular), Respiration function (respiratory support), and Additional respiratory functions (cough effectiveness), with this being the only scale that includes the measurement of muscle strength through a biophysical instrument (handgrip dynamometry), which makes it possible to quantify grip strength in kilograms.28
Strengths and Limitations
The consensus to identify the ICF domains was carried out via email and not in person, and the researchers had no formal training on the ICF framework. However, in this scoping review the application of a quality control check by a third researcher36 ensured that the selected domains were chosen according to the ICF definitions. Another weakness of this review was that studies not written in English or Spanish were excluded. This might mean that relevant studies were omitted. However, compared with previous studies, this study includes the largest number of PF measurement instruments used in adult ICU, and classifies in detail the ICF domains included. It also reveals the domains most commonly used in critically ill adult patients to facilitate the use of measurement instruments in clinical practice.
Recommendations for Future Research
The ICF tool adds structure to the description and understanding of PF-related domains in acute care settings.37–39 Despite its wide applicability, the ICF framework has not been integrated into common practice in the ICU40; this could be because not all of the ICF domains are considered relevant within the ICU. Work on a core outcome measurement set is currently underway,41–43 so future studies or consensus could define an ICF core set relevant in critical illness.44
Currently, it is not known whether a single instrument is capable of covering all of the relevant domains within the ICF while retaining robust measurement properties, so it is likely that more than 1 instrument will be needed at any given time to measure PF.24,45 When selecting a PF measurement instrument for the ICU, it is recommended that future studies carefully choose the instruments and outcomes to be evaluated13 based on the core constructs that the researchers wish to measure in terms of ICF domains and subdomains.22 Future research should investigate the several outcome measures that are likely required to capture patients’ recovery trajectory, and the questionnaires, scores, scales, and biophysical instruments that capture different aspects of PF.
Conclusion
There are numerous PF measurement instruments used in the adult ICU that contain different ICF domains, the most frequent being Mobility. This scoping review categorizes PF measures and their ICF domains, providing a quick reference guide for clinicians and researchers to assist in instrument selection.
Supplementary Material
Appendix 1.
Search Terms for the Identification of Articles Eligible for Scoping Review
| Database | Search Terms | Results |
|---|---|---|
| PubMed (May 17, 2017) | ((“Outcome Assessment (Health Care)”[Mesh] OR “Patient Outcome Assessment”[Mesh] OR “measurement instrument” OR psychometrics OR clinimetric OR “functional outcomes” OR validity OR validation OR reliability OR “cross cultural” OR “clinicophysiologic evaluation” OR) AND (“Intensive Care Units”[Mesh] OR “critical care” OR “critical patient” OR “intensive care” OR “Critical Illness”[Mesh]) OR “mechanically ventilated patients”)) AND (“Early Ambulation”[Mesh] OR “physical funct*” OR “functional status” OR rehabilitation OR “Mobility Limitation”[Mesh] OR Mobili* OR “exercise capacity” OR “functional capacity” OR “functional independence” OR muscle OR “physical impairment” OR disability OR walking OR “Activities of Daily Living”[Mesh] OR “limb strength”) Limits: to present Language filters: English and Spanish | 3677 |
| LILACS (May 17, 2017) | (“Evaluación del resultado del paciente” OR “instrumento de medición” OR psicometría OR “resultados funcionales” clinimétricos OR validez OR validación OR confiabilidad OR “adaptación transcultural” OR “evaluación clinicofisiológica”) AND (“unidad de cuidado intensivo” OR “cuidado crítico” OR “paciente crítico” OR “cuidado intensivo” OR “enfermedad crítica” OR “pacientes ventilados mecánicamente”) AND (“deambulación temprana” OR “función física” OR “estado funcional” OR rehabilitación OR “Limitación de movilidad” OR Mobili* OR “capacidad de ejercicio” OR “capacidad funcional” OR “independencia funcional” OR músculo OR “impedimento físico” OR discapacidad OR caminar OR “Actividades de la vida diaria” OR “fuerza de la extremidad”) Limits: from inception to present Language filters: English and Spanish | 355 |
| Cochrane CENTRAL (May 17, 2017) | (“Patient Outcome Assessment” OR “measurement instrument” OR psychometrics OR clinimetric OR “functional outcomes” OR validity OR validation OR reliability OR “cross cultural” OR “clinicophysiologic evaluation”) AND (“Intensive Care Units” OR “critical care” OR “critical patient” OR “intensive care” OR “Critical Illness” OR “mechanically ventilated patients”) AND (“Early Ambulation” OR “physical funct*” OR “functional status” OR rehabilitation OR “Mobility Limitation” OR Mobili* OR “exercise capacity” OR “functional capacity” OR “functional independence” OR muscle OR “physical impairment” OR disability OR walking OR “Activities of Daily Living” OR “limb strength”) Limits: from inception to present Language filters: English and Spanish | 105 |
| CINAHL (May 17, 2017) | (“Patient Outcome Assessment” OR “measurement instrument” OR psychometrics OR clinimetric OR “functional outcomes” OR validity OR validation OR reliability OR “cross cultural” OR “clinicophysiologic evaluation”) AND (“Intensive Care Units” OR “critical care” OR “critical patient” OR “intensive care” OR “Critical Illness” OR “mechanically ventilated patients”) AND (“Early Ambulation” OR “physical funct*” OR “functional status” OR rehabilitation OR “Mobility Limitation” OR Mobili* OR “exercise capacity” OR “functional capacity” OR “functional independence” OR muscle OR “physical impairment” OR disability OR walking OR “Activities of Daily Living” OR “limb strength”) Limits: from inception to present Language filters: English | 84 |
Author Contributions and Acknowledgments
Concept/idea/research design: F. González-Seguel, C. Merino-Osorio
Writing: F. González-Seguel, C. Merino-Osorio
Data collection: F. González-Seguel, C. Merino-Osorio
Data analysis: F. González-Seguel, E. Corner, C. Merino-Osorio
Project management: F. González-Seguel
Providing institutional liaisons: F. González-Seguel, E. Corner
Consultation (including review of manuscript before submitting): F. González-Seguel, E. Corner, C. Merino-Osorio
The authors acknowledge the School of Physical Therapy, Facultad de Medicina Clínica Alemana Universidad del Desarrollo and the Master's program in Physical Therapy and Rehabilitation of the Universidad del Desarrollo for academic support during this study.
Disclosures
The authors completed the ICMJE Form for Disclosures of Potential Conflicts of Interest. E.J. Corner was the primary developer of the Chelsea critical care physical assessment tool (CPAx). No further conflicts of interest were disclosed.
References
- 1. Spragg RG, Bernard GR, Checkley W et al.. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010;181:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Needham DM, Davidson J, Cohen H et al.. Improving long-term outcomes after discharge from intensive care unit. Crit Care Med. 2012;40:502–509. [DOI] [PubMed] [Google Scholar]
- 3. Fan E, Dowdy DW, Colantuoni E et al.. Physical complications in acute lung injury survivors: A two-year longitudinal prospective study. Crit Care Med. 2014;42:849–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pfoh ER, Wozniak AW, Colantuoni E et al.. Physical declines occurring after hospital discharge in ARDS survivors: a 5-year longitudinal study. Intensive Care Med. 2016;42:1557–1566. [DOI] [PubMed] [Google Scholar]
- 5. Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9:277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Herridge MS, Tansey CM, Matté A et al.. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. [DOI] [PubMed] [Google Scholar]
- 7. Painter P, Stewart AL Carey S. Physical functioning: definitions, measurement, and expectations. Adv Ren Replace Ther. 1999;6:110–123. [DOI] [PubMed] [Google Scholar]
- 8. Tomey KM, Sowers MR. Assessment of physical functioning: a conceptual model encompassing environmental factors and individual compensation strategies. Phys Ther. 2009;89:705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. The International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 10. Turnbull AE, Rabiee A, Davis WE et al.. Outcome measurement in ICU survivorship research from 1970 to 2013. Crit Care Med. 2016;44:1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hoyer EH, Young DL, Klein LM et al.. Toward a common language for measuring patient mobility in the hospital: reliability and construct validity of interprofessional mobility measures. Phys Ther. 2018;98:133–142. [DOI] [PubMed] [Google Scholar]
- 12. Parry SM, Denehy L, Beach LJ, Berney S, Williamson HC, Granger CL. Functional outcomes in ICU – what should we be using? An observational study. Crit Care. 2015;19:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of early rehabilitation during intensive care unit stay on functional status: Systematic review and meta-analysis. PLoS One. 2015;10:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Parry SM, Granger CL, Berney S et al.. Assessment of impairment and activity limitations in the critically ill: a systematic review of measurement instruments and their clinimetric properties. Intensive Care Med. 2015;41:744–762. [DOI] [PubMed] [Google Scholar]
- 15. Jordan Z, Munn Z, Aromataris E, Lockwood C. Now that we're here, where are we? The JBI approach to evidence-based healthcare 20 years on. Int J Evid Based Healthc. 2015;13:117–120. [DOI] [PubMed] [Google Scholar]
- 16. Liberati A, Altman DG, Tetzlaff J et al.. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Collaboration; 2011. [Google Scholar]
- 18. World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF. WHO, Geneva; 2002. [Google Scholar]
- 19. Koo KK, Lord T, Huerta KK et al.. Validity and inter-rater reliability of the Swedish simple early mobility (SEA) scale: a simple activity scale to measure highest level of daily mobility in intensive care units. Am J Respir Crit Care Med. 2017;195:A2736. [Google Scholar]
- 20. Cohn J, Rizvi A, Lorenzo J. Interrater reliability and responsiveness of the ICU patient reported functional scale. Crit Care Med. 2016;44:283. [Google Scholar]
- 21. Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43:171–183. [DOI] [PubMed] [Google Scholar]
- 22. Nordon-Craft A, Moss M, Quan D, Schenkman M. Intensive care unit-acquired weakness: Implications for physical therapist management. Phys Ther. 2012;92:1494–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Van der Wees PJ, Moore AP, Powers CM, Stewart A, Nijhuis-van der Sanden MWG, de Bie RA. Development of clinical guidelines in physical therapy: Perspective for international collaboration. Phys Ther. 2011;91:1551–1563. [DOI] [PubMed] [Google Scholar]
- 24. Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. Crit Care. 2017;21:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pinto-Carral A, Fernández-Villa T, Molina de la Torre AJ. Patient-reported mobility: A systematic review. Arch Phys Med Rehabil. 2016;97:1182–1194. [DOI] [PubMed] [Google Scholar]
- 26. de Morton NA, Berlowitz DJ, Keating JL. A systematic review of mobility instruments and their measurement properties for older acute medical patients. Health Qual Life Outcomes. 2008;6:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Parry SM, Nydahl P, Needham DM. Implementing early physical rehabilitation and mobilisation in the ICU: institutional, clinician, and patient considerations. Intensive Care Med. 2018;44:470–473. [DOI] [PubMed] [Google Scholar]
- 28. Alexander NB, Grunawalt JC, Carlos S, Augustine J. Bed mobility task performance in older adults. J Rehabil Res Dev. 2000;37:633–638. [PubMed] [Google Scholar]
- 29. Burns JR, Jones FL. Letter: Early ambulation of patients requiring ventilatory assistance. Chest. 1975;68:608. [DOI] [PubMed] [Google Scholar]
- 30. Mehrholz J, Mückel S, Oehmichen F, Pohl M. First results about recovery of walking function in patients with intensive care unit-acquired muscle weakness from the General Weakness Syndrome Therapy (GymNAST) cohort study. BMJ Open. 2015;5:e008828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ma AJ, Rawat N, Reiter A et al.. Measuring patient mobility in the ICU using a novel noninvasive sensor. Crit Care Med. 2017;45:630–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370:1626–1635. [DOI] [PubMed] [Google Scholar]
- 33. Volaklis KA, Halle M, Meisinger C. Muscular strength as a strong predictor of mortality: A narrative review. Eur J Intern Med. 2015;26:303–310. [DOI] [PubMed] [Google Scholar]
- 34. Vanpee G, Hermans G, Segers J, Gosselink R. Assessment of limb muscle strength in critically ill patients: a systematic review. Crit Care Med. 2014;42:701–711. [DOI] [PubMed] [Google Scholar]
- 35. Corner EJ, Wood H, Englebretsen C et al.. The Chelsea Critical Care Physical Assessment Tool (CPAx): Validation of an innovative new tool to measure physical morbidity in the general adult critical care population. An observational proof-of-concept pilot study. Physiother (United Kingdom). 2013;99:33–41. [DOI] [PubMed] [Google Scholar]
- 36. Bown MJ, Sutton AJ. Quality control in systematic reviews and meta-analyses. Eur J Vasc Endovasc Surg. 2010;40:669–677. [DOI] [PubMed] [Google Scholar]
- 37. Grill E, Huber EO, Gloor-Juzi T, Stucki G. Intervention goals determine physical therapists’ workload in the acute care setting. Phys Ther. 2010;90:1468–1478. [DOI] [PubMed] [Google Scholar]
- 38. Boldt C, Grill E, Wildner M et al.. ICF Core Set for patients with cardiopulmonary conditions in the acute hospital. Disabil Rehabil. 2005;27:375–380. [DOI] [PubMed] [Google Scholar]
- 39. Grill E, Müller M, Stier-Jarmer M et al.. Validation of the comprehensive ICF Core Sets for patients receiving rehabilitation interventions in the acute care setting. J Rehabil Med. 2011;43:92–101. [DOI] [PubMed] [Google Scholar]
- 40. Allet L, Bürge E, Monnin D. ICF: Clinical relevance for physiotherapy? A critical review. Adv Physiother. 2008;10:127–137. [Google Scholar]
- 41. González-Seguel F, Arriagada-Bravo A, Lee-Goic J, Ugarte S. Feasibility and clinical utility of ICF framework in critically ill patients: Case report. Ann Musc Disord. 2017;1:1002. [Google Scholar]
- 42. Turnbull AE, Sepulveda KA, Dinglas VD, Chessare CM, Bingham CO, Needham DM. Core domains for clinical research in acute respiratory failure survivors. Crit Care Med. 2017;45:1001–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Needham DM, Sepulveda KA, Dinglas VD et al.. Core outcome measures for clinical research in acute respiratory failure survivors: An international modified Delphi consensus study. Am J Respir Crit Care Med. 2017;196:1122–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jette AM. Invited commentary on the ICF and physical therapist practice. Phys Ther. 2010;90:1064–1065. [DOI] [PubMed] [Google Scholar]
- 45. Libuy MH, Szita CP, Hermosilla PJ, Arellano SD, Rodríguez-Núñez I, Báez RC. Validez y confiabilidad de las escalas de evaluación funcional en pacientes críticamente enfermos. Revisión sistemática. Rev Med Chil. 2017;145:1137–1144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.