Abstract
A sizable number of children are exposed to household member substance problems, an adverse childhood experience (ACE), yet little research uses a nationally representative sample of U.S. children to examine this association. We used newly released data from the 2016 National Survey of Children's Health (NSCH), a nationally representative sample of noninstitutionalized children in the United States, and logistic regression models to investigate the relationship between household member substance problems and 14 indicators of children's health. We find 9.0% of children in the United States have experienced household member substance problems. We also find children exposed to household member substance problems are more likely to have health problems than children not exposed to household member substance problems, but that most of these descriptive differences can be explained by household characteristics and other ACEs. Children exposed to household member substance problems are a vulnerable population. Given that household member substance problems are concentrated among socioeconomically disadvantaged children, children at a greater risk of health problems than their counterparts, this ACE may exacerbate existing socioeconomic inequalities in children's health.
Keywords: Children's health, Household member substance problems, National Survey of Children's Health
Highlights
-
•
Household member substance problems is an adverse childhood experience (ACE).
-
•
9.0% of U.S. children have experienced household member substance problems.
-
•
Household member substance problems are associated with health problems.
-
•
This ACE may exacerbate existing socioeconomic inequalities in children's health.
1. Introduction
A substantial proportion of the U.S. population has a substance use disorder, defined as clinically significant impairments resulting from the use of drugs or alcohol (Lipari & Van Horn, 2017a, 2017b). In 2016, approximately 20.1 million individuals over age 12 had a substance use disorder, including 7.4 million (2.7% of the population) with an illicit drug use disorder and 15.1 million (5.6% of the population) with an alcohol use disorder (Lipari & Van Horn, 2017a, 2017b). Accordingly, a sizable number of children reside with individuals who have impairments from drug or alcohol use. About one in eight—or 8.7 million—children live with at least one parent suffering from a substance use disorder (Lipari & Van Horn, 2017a, 2017b).
Household member substance problems is an adverse childhood experience (ACE) that may be consequential for children's health (Dube, Felitti, Dong, Files, & Anda, 2003; Felitti, 2009; Peleg-Oren & Teichman, 2006; Schilling, Aseltine, & Gore, 2007). The stress process perspective provides a theoretical lens for understanding the relationship between household member substance problems and children's health. This perspective suggests that stressors, such as household member substance problems, are concentrated among vulnerable populations and that these stressors can have deleterious consequences for physical and mental health (Pearlin, 1989; Pearlin, Menaghan, Lieberman, & Mullan, 1981).
Moreover, the stress process perspective suggests that stressors can proliferate across individuals, with the stressor experienced by one individual having deleterious consequences for the physical and mental health of those connected to the individual (Pearlin, Aneshensel, & LeBlanc, 1997). Children are especially important to the stress process perspective (Avison, 2010). Substance use problems can strain household economic resources (Rehm et al., 2009), fracture relationships between family members (Whisman, 1999), and have corresponding physical and mental health problems (Kessler, Chiu, Demler, & Walters, 2005; Whiteford et al., 2013), all of which are social determinants of children's health (Bloom, Cohen, & Freeman, 2009; Hardie & Landale, 2013; McLeod & Shanahan, 1993; Turney, 2011; Turney & Hardie, 2017). Therefore, in accordance with the stress process perspective, the stressor of household member substance problems may be associated with health impairments among children.
Despite good reasons to expect an association between household member substance problems and impairments in children's health, little research considers the health disparities between U.S. children exposed and not exposed to household member substance problems (Berg, Bäck, Vinnerljung, & Hjern, 2016; Jääskeläien, Holmila, Notkola, & Raitasalo, 2016; Kandel, 1990; Osborne & Berger, 2009; Raitasalo & Holmila, 2017; Thompson, Alonzo, Hu, & Hasin, 2017; Zebrak & Green, 2016). This is an important oversight given the sizable number of children exposed to household member substance problems, many of whom experience other vulnerabilities. Existing research generally finds that parental substance problems are linked to poor health in children. For example, one study used data from the Fragile Families and Child Wellbeing Study, a cohort of U.S. urban children born to mostly unmarried parents, and found that parental substance abuse is associated with an increased risk of behavioral problems and fair or poor overall health in children. This study also found that these associations are strongest when both parents abuse substances (Osborne & Berger, 2009). Another study, using data from a prospective cohort study of African Americans, finds that parental alcohol use is associated with problem behaviors in adolescence (Zebrak & Green, 2016). Research examining children in countries outside the United States come to similar conclusions about the deleterious consequences of parental or household member substance problems (Berg et al., 2016; Jääskeläien et al., 2016; Raitasalo & Holmila, 2017).
In this article, we use newly released data from the 2016 National Survey of Children's Health (NSCH) to provide one of the first examinations of the association between household member substance problems and children's health among a nationally representative sample of non-institutionalized children in the United States. We examine three global indicators (fair or poor overall health, activity limitations, chronic school absence) and nine specific indicators (including mental health [e.g., depression, anxiety] and physical health [e.g., asthma, obesity]) of children's health. We also examine two summary measures of children's health, one that indicates the child currently has any of the nine specific health conditions and another that indicates the number of specific health conditions. Our analyses isolate the relationship between household member substance problems and children's health by adjusting for a large number of child, parent, and household characteristics including poverty and exposure to other ACEs (e.g., parental divorce or separation, parental incarceration). Taken together, these analyses complement and extend prior research on this topic by using a nationally representative sample of U.S. children, by considering an array of general and specific measures of children's health, and by adjusting for factors that might render the relationship between household member substance problems and children's health spurious.
2. Methods
2.1. Participants
We estimate the relationship between household member substance problems and children's health using the newly released 2016 National Survey of Children's Health (NSCH), a cross-sectional survey funded and directed by the Health Resources and Services Administration Maternal and Child Health Bureau (HRSA MCHB). These data comprise a nationally representative sample of 50,212 non-institutionalized children ages 0 to 17. Between June 2016 and February 2017, researchers used the Census Master Address File to identify eligible households and, within each household, identified a focal child. Eligible households were first asked to participate in a web-based survey and, among those that did not respond to the first two web survey invitations, were then asked to participate in a mailed paper survey. The majority (80.6%) of completed surveys were web-based surveys. The overall weighted response rate was 40.7%. An analysis of non-response bias finds “no strong or consistent evidence of nonresponse bias” and our analyses employ survey weights to adjust for non-response (Census Bureau. 2017., 2017; Child and Adolescent Health Measurement Initiative Data Resource Center for Child and Adolescent Health, 2016).
2.2. Measures
2.2.1. Outcome variables
The outcome variables include 14 indicators of children's health, all reported by the parent respondent (the focal child's mother in 63% of observations). First, these include three global measures of children's health: (1) fair or poor overall health (compared to good, very good, or excellent health); (2) activity limitations (1 = limited or prevented in ability to do things most same-age children can do because of medical, behavioral, or other health condition); and (3) chronic school absence (1 = missed 11 or more school days because of illness or injury in past year). Fair or poor overall health provides an indication of the child's overall health. Though parent responses are skewed toward reporting favorable health, and the validity of parent-reported health is not understood in the same way as adult self-reported health, prior research collapses parent-reported fair and poor overall health (Bzostek & Beck, 2011; Case, Lubotsky, & Paxson, 2002; Chen, Martin, & Matthews, 2006; Idler & Benyamini, 1997; Turney, 2013). Additionally, analyses that instead estimate good, fair, or poor overall health (compared to very good or excellent health) and analyses that use the full distribution of response produce estimates consistent with those presented. Activity limitations and chronic school absence provide an indication of how the child's health interferes with his/her life.
Second, the outcome variables include nine specific measures of current health conditions: (1) learning disability; (2) Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder (ADD/ADHD); (3) depression; (4) anxiety problems; (5) behavioral or conduct problems; (6) developmental delay; (7) asthma; (8) obesity; and (9) speech or other language disorder. These measures were chosen because they are all relatively common childhood health conditions that have been at least partly attributed to the social environment. Third, the outcome variables include two summary measures of children's health: (1) a binary variable indicating the child had any of the nine current health conditions and (2) a count variable indicating the number of current health conditions the child had (ranging from 0 to 9).
2.2.2. Explanatory variable
A binary variable indicates exposure to household member substance problems. Parent respondents were asked to report on one indicator of household member substance problems: “To the best of your knowledge, has this child ever … lived with anyone who had a problem with alcohol or drugs?” Below we include a discussion of the limitations of this measure.
2.2.3. Control variables
The multivariate analyses adjust for three sets of control variables, as it is important to isolate the relationship between household member substance problems and children's health (Berg et al., 2016; Jääskeläien et al., 2016; Osborne & Berger, 2009). The first set includes demographic characteristics: child age, child gender (1 = female), child born low birth weight, child race/ethnicity (White [non-Hispanic], Black [non-Hispanic], Hispanic, other race [non-Hispanic]), child immigrant status (1 = first- or second-generation immigrant), household language (1 = English), mother's age (29 years or younger, 30–39 years, 40–49 years, 50 years and older), and parent's educational attainment (less than high school, high school diploma, some college, Bachelor's degree and higher).
The second set includes additional household characteristics: parent's marital status (1 = married), parent's employment status (1 = employed at least 50 of the last 52 weeks), mother's health (1 = fair or poor overall health), household member welfare receipt, household member WIC receipt, household income below the federal poverty line, household member smokes inside the home, and neighborhood safety (1 = neighborhood always safe for child).
The third set includes eight additional ACEs: (1) parental incarceration; (2) parental divorce or separation; (3) parental death; (4) witness of household member abuse (i.e., child saw or heard parents or adults slap, hit, kick, or punch one another); (5) violence exposure (i.e., child was a victim of violence or witnessed neighborhood violence); (6) household member mental illness; (7) racial discrimination; and (8) income difficulties (i.e., it was very often hard to get by on the family's income since the child was born). See Appendix Table 1 for a correlation matrix of ACEs.
2.3. Statistical analyses
The analyses proceed in two stages. The first analytic stage presents frequencies of the outcome variables by household member substance problems. Chi-square tests examine whether the differences among children exposed and not exposed to household member substance problems are statistically significant. The second analytic stage presents results from regression models that estimate each of the dependent variables as a function of household member substance problems. Logistic regression models estimate all dependent variables except for number of health conditions, which is estimated with a negative binomial regression model. Model 1 adjusts for a limited set of variables. Model 2 adjusts for additional parent and household variables. Model 3 further adjusts for ACEs to isolate the independent association between household member substance problems and children's health. By including a relatively limited set of control variables, Model 1 provides an upper-bound estimate of the association between household member substance problems and children's health. Conversely, by including an extended set of control variables that may precede or follow household member substance problems, Model 2 and especially Model 3 provide a lower-bound (and conservative) estimate of this association. We also estimate the association between household member substance problems and children's health separately for the following three groups: (1) children ages 0 to 5, (2) children ages 6 to 11, and (3) children ages 12 to 17. These models adjust for child, parent, and household control variables (the equivalent of Model 2 in the estimates of the full sample).
Relatively few observations were missing data (with control variables missing, on average, 3% of observations). We preserved missing observations by producing 20 imputed data sets, using the multivariate normal method, and averaging results across the data sets. All analyses employ survey weights to account for the complex sampling design and non-response. All analyses were conducted with Stata 13.0.
2.4. Sample description
Table 1 presents weighted frequencies of children's health. As expected, relatively few children are in fair or poor health (1.8%), have an activity limitation (5.2%), or have chronic school absence (3.9%). Among the nine specific health outcomes, obesity is most common (16.1%), followed by asthma (8.4%), ADD/ADHD (7.6%), behavioral or conduct problems (6.3%), anxiety problems (6.0%), learning disability (5.7%), speech or other language disorder (4.7%), developmental delay (4.5%), and depression (2.7%). More than one-quarter (27.1%) of children currently have any of the nine specific health conditions and, on average, children have 0.52 health conditions (range: 0 to 9).
Table 1.
Weighted frequencies of outcome variables: 2016 National Survey of Children's Health (NSCH).
| Measure | Age | % | N |
|---|---|---|---|
| Fair or poor health | 0 to 17 | 1.8% | 50,060 |
| Activity limitation | 0 to 17 | 5.2% | 50,125 |
| Chronic school absence | 6 to 17 | 3.9% | 34,961 |
| Learning disability | 0 to 17 | 5.7% | 50,005 |
| ADD/ADHD | 0 to 17 | 7.6% | 49,733 |
| Depression | 0 to 17 | 2.7% | 49,997 |
| Anxiety problems | 0 to 17 | 6.0% | 49,914 |
| Behavioral or conduct problems | 0 to 17 | 6.3% | 49,959 |
| Developmental delay | 0 to 17 | 4.5% | 49,973 |
| Asthma | 0 to 17 | 8.4% | 49,742 |
| Obesity | 10 to 17 | 16.1% | 24,405 |
| Speech or other language disorder | 0 to 17 | 4.7% | 49,990 |
| Any specific health condition | 0 to 17 | 27.1% | 50,211 |
| Number of specific health conditions | 0 to 17 | 0.52 | 50,211 |
Note: Any specific health condition defined as an affirmative response to any of the following nine indicators: (1) learning disability, (2) ADD/ADHD, (3) depression, (4) anxiety problems, (5) behavioral or conduct problems, (6) developmental delay, (7) asthma, (8) obesity, and (9) speech or other language disorder. Number of health conditions is a summary measure of these health conditions (ranging from 0 to 9).
Table 2 presents weighted descriptive statistics of the sample. About half (48.9%) of children are female. The majority are White (51.9%), followed by Hispanic (24.5%), Black (12.7%), and other race (10.9%). More than one-quarter (26.0%) are immigrants or children of immigrants. More than one-fifth (21.9%) are living in households with incomes below the poverty line. Among the eight additional ACEs considered, parental divorce or separation is most common (25.4%), followed by parental incarceration (8.0%), household member mental illness (7.8%), income difficulties (6.4%), witness of household member abuse (5.6%), witness of violence (3.7%), racial discrimination (3.6%), and parental death (3.2%).
Table 2.
Weighted frequencies and means of independent and control variables: 2016 National Survey of Children's Health (NSCH).
| Full sample | By household member drug or alcohol problem |
|||
|---|---|---|---|---|
| Yes | No | |||
| Child female | 48.9% | 51.7% | 48.7% | |
| Child born low birth weight | 8.3% | 10.8% | 8.0% | ** |
| English spoken at home | 85.8% | 93.1% | 85.0% | *** |
| Child race/ethnicity | ||||
| White (non-Hispanic) | 51.9% | 55.6% | 51.5% | * |
| Black (non-Hispanic) | 12.7% | 11.1% | 12.9% | |
| Hispanic | 24.5% | 24.0% | 24.6% | |
| Other (non-Hispanic) | 10.9% | 9.3% | 11.0% | |
| Child first or second generation immigrant | 26.0% | 12.6% | 27.4% | *** |
| Child age | 8.60 | 10.555 | 8.41 | *** |
| Child health insurance | ||||
| Private insurance | 57.1% | 35.5% | 59.2% | *** |
| Public insurance | 36.9% | 56.7% | 35.0% | *** |
| No insurance | 6.0% | 7.8% | 5.8% | * |
| Child saw doctor in past year | 85.9% | 87.0% | 85.8% | |
| Mother age | ||||
| 29 years or younger | 12.2% | 9.4% | 12.5% | ** |
| 30–39 years | 42.8% | 40.9% | 42.9% | * |
| 40–49 years | 35.4% | 35.3% | 35.5% | |
| 50 years or older | 9.6% | 14.4% | 9.1% | *** |
| Parent married to child's biological father | 61.0% | 25.2% | 64.6% | *** |
| Parent employed | 94.0% | 88.9% | 94.5% | *** |
| Parental educational attainment | ||||
| Less than high school | 9.0% | 8.5% | 9.1% | |
| High school diploma | 14.4% | 18.8% | 14.0% | *** |
| Some college | 28.0% | 38.6% | 26.9% | *** |
| Bachelor's degree or higher | 48.6% | 34.2% | 50.1% | *** |
| Mother in fair or poor health | 6.1% | 13.0% | 5.4% | *** |
| Household member receives welfare | 4.4% | 8.6% | 3.9% | *** |
| Household member receives WIC | 13.5% | 15.8% | 13.3% | |
| Household income below the poverty line | 21.9% | 28.7% | 21.3% | *** |
| Household member smokes inside home | 2.7% | 8.3% | 2.1% | *** |
| Neighborhood always safe for child | 63.8% | 52.5% | 64.9% | *** |
| Parental incarceration | 8.0% | 40.8% | 4.8% | *** |
| Parental divorce or separation | 25.4% | 68.0% | 21.1% | *** |
| Parental death | 3.2% | 10.0% | 2.5% | *** |
| Witness of household member abuse | 5.6% | 34.8% | 2.7% | *** |
| Witness of violence | 3.7% | 19.6% | 2.1% | *** |
| Household member mental illness | 7.8% | 39.5% | 4.7% | *** |
| Racial discrimination | 3.6% | 12.0% | 2.7% | *** |
| Income difficulties | 6.4% | 16.3% | 5.4% | *** |
| N | 50,212 | 4,468 | 45,744 | |
Note: Asterisks compare children exposed to household member drug or alcohol problem and children not exposed to household member drug or alcohol problem. *p < .05, **p < .01, ***p < .001.
Table 2 also shows demographic, socioeconomic, and household differences between children exposed and not exposed to household member substance problems. Children exposed to household member substance problems are less likely than others to have married parents (25.2% compared to 64.6%, p < .001), less likely to have employed parents (88.9% compared to 94.5%, p < .001), and more likely to be living in households with incomes below the poverty line (28.7% compared to 21.3%, p < .001). Children exposed to household member substance problems are also more likely to experience all of the eight other ACEs.
3. Results
3.1. Frequency of household member substance problems
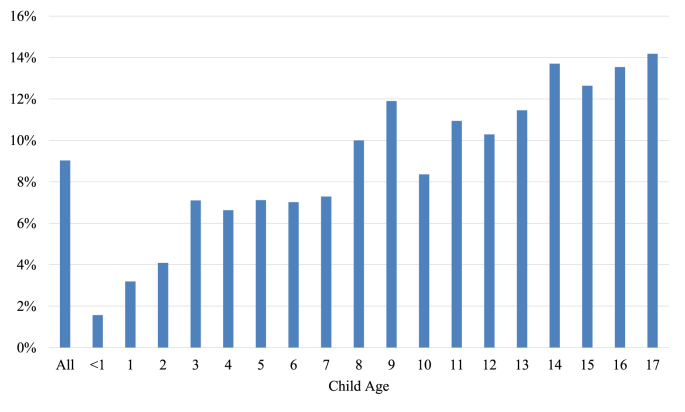
Fig. 1 documents the weighted frequencies of household member substance problems, first for the full sample and then by child age. Nearly one-tenth (9.0%) of children have been exposed to household member substance problems. As expected, the percentage of children exposed to household member substance problems increases with age. About 1.6% of children under age 1 have been exposed to household member substance problems, compared to 7.0% of 6-year-old children, 10.3% of 12-year-old children, and 14.2% of 17-year-old children.
Fig. 1.
Weighted frequencies of household member drug or alcohol problem, by child age (N = 50,212).
3.2. Descriptives of children's health, by household member substance problems
Table 3 presents frequencies and means of children's health by exposure to household member substance problems. Children exposed to household member substance problems, compared to other children, are nearly four times as likely to experience depression (8.1% compared to 2.1%, p < .001). These children are three times as likely to have anxiety problems (16.7% compared to 5.0%, p < .001), behavioral or conduct problems (17.1% compared to 5.3%, p < .001), and ADD/ADHD (18.1% compared to 6.5%, p < .001). They are also about twice as likely to have a learning disability (12.1% compared to 5.0%, p < .001), developmental delay (7.6% compared to 4.2%, p < .001), and asthma (12.8% compared to 8.0%, p < .001). Children exposed to household member substance problems are also more likely to have worse global indicators of health, measured by fair or poor health (3.5% compared to 1.6%, p < .01), activity limitations (9.1% compared to 4.8%, p < .001), and chronic school absence (8.1% compared to 3.4%, p < .001). They are also nearly twice as likely to have any specific health condition (47.2% compared to 25.1%, p < .001) and, on average, have about twice as many health conditions (1.09 compared to 0.46, p < .001).
Table 3.
Weighted descriptive statistics of children's health, by household member drug or alcohol problem: 2016 National Survey of Children's Health (NSCH).
| Household member drug or alcohol problem |
|||
|---|---|---|---|
| Yes | No | ||
| Fair or poor health | 3.5% | 1.6% | ** |
| Activity limitation | 9.1% | 4.8% | *** |
| Chronic school absence | 8.1% | 3.4% | *** |
| Learning disability | 12.1% | 5.0% | *** |
| ADD/ADHD | 18.1% | 6.5% | *** |
| Depression | 8.1% | 2.1% | *** |
| Anxiety problems | 16.7% | 5.0% | *** |
| Behavioral or conduct problems | 17.1% | 5.3% | *** |
| Developmental delay | 7.6% | 4.2% | *** |
| Asthma | 12.8% | 8.0% | *** |
| Obesity | 20.0% | 15.6% | ** |
| Speech or other language disorder | 6.4% | 4.5% | *** |
| Any specific health condition | 47.2% | 25.1% | *** |
| Number of specific health conditions | 1.09 | 0.46 | *** |
| N | 45,744 | 4,468 | |
Note: Asterisks compare children exposed to household member drug or alcohol problem and children not exposed to household member drug or alcohol problem. Ns vary across outcome variables (see Table 1). **p < .01, ***p < .001.
3.3. Estimating children's health as a function of household member substance problems
Table 4 presents results from logistic regression models (and, in the case of one outcome variable, negative binomial regression models) estimating children's health as a function of household member substance problems. Model 1, which adjusts for limited demographic characteristics, shows that children exposed to household member substance problems have worse health outcomes than their counterparts. The negative association between household member substance problems and children's health persists across all dependent variables. For example, children exposed to household member substance problems, compared to their counterparts, are more likely to be in fair or poor health (OR = 2.10; 95% CI = 1.17, 3.76), have an activity limitation (OR = 1.70; 95% CI = 1.37, 2.16), and have chronic school absence (OR = 2.05; 95% CI = 1.40, 2.98). These children are also more likely to have mental health conditions such as depression (OR = 2.59; 95% CI = 2.06, 3.26) and anxiety (OR = 2.81; 95% CI = 2.23, 3.54) and physical health conditions such as asthma (OR = 1.37; 95% CI = 1.09, 1.72) and obesity (OR = 1.31; 95% CI = 1.07, 1.67). They are also more likely to have any specific health condition (OR = 2.09, 95% CI = 1.78, 2.45) and, on average, have a greater number of specific health conditions (b = 0.65, 95% CI = 0.55, 0.76).
Table 4.
Regression models estimating children's health as a function of household member with drug or alcohol problem: 2016 National Survey of Children's Health (NSCH).
| Model 1 |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| limited controls |
extended controls |
extended controls + adverse childhood experiences |
|||||||
| OR or b | [CI] | OR or b | [CI] | OR or b | [CI] | ||||
| Fair or poor health | 2.10 | * | [1.17, 3.76] | 1.47 | [0.83, 2.60] | 1.11 | [0.63, 1.95] | ||
| Activity limitation | 1.70 | *** | [1.37, 2.16] | 1.18 | [0.93, 1.50] | 0.96 | [0.77, 1.29] | ||
| Chronic school absence | 2.05 | *** | [1.40, 2.98] | 1.62 | * | [1.07, 2.46] | 1.20 | [0.73, 1.98] | |
| Learning disability | 1.91 | *** | [1.55, 2.36] | 1.48 | *** | [1.18, 1.85] | 1.16 | [0.88, 1.54] | |
| ADD/ADHD | 2.34 | *** | [1.95, 2.80] | 1.69 | *** | [1.40, 2.05] | 1.25 | * | [1.00, 1.56] |
| Depression | 2.59 | *** | [2.06, 3.26] | 1.79 | ** | [1.40, 2.29] | 0.94 | [0.69, 1.28] | |
| Anxiety problems | 2.81 | *** | [2.23, 3.54] | 2.14 | *** | [1.70, 2.71] | 1.39 | * | [1.06, 1.83] |
| Behavioral or conduct problems | 3.10 | *** | [2.54, 3.78] | 2.07 | *** | [1.69, 2.54] | 1.15 | [0.90, 1.47] | |
| Developmental delay | 1.66 | *** | [1.32, 2.09] | 1.22 | [0.94, 1.57] | 1.01 | [0.76, 1.34] | ||
| Asthma | 1.37 | * | [1.09, 1.72] | 1.16 | [0.93, 1.46] | 0.95 | [0.73, 1.26] | ||
| Obesity | 1.31 | * | [1.07, 1.67] | 1.13 | [0.90, 1.43] | 1.09 | [0.82, 1.45] | ||
| Speech or other language disorder | 1.43 | ** | [1.07, 1.67] | 1.22 | [0.94, 1.58] | 0.96 | [0.71, 1.29] | ||
| Any specific health condition | 2.09 | *** | [1.78, 2.45] | 1.65 | ** | [1.40, 1.93] | 1.19 | [1.00, 1.43] | |
| Number of specific health conditions | 0.65 | *** | [0.55, 0.76] | 0.40 | *** | [0.29, 0.50] | 0.10 | [-0.02, 0.22] | |
| N | 50,212 | 50,212 | 50,212 | ||||||
Notes: Each row represents a separate dependent variable. Negative binomial regression models estimate number of specific health conditions. Logistic regression models estimate all other dependent variables. Odds ratios (OR) or coefficients and 95% confidence intervals (CI) presented for household member drug or alcohol problem. Model 1 adjusts for the following: child age, child gender, child born low birth weight, child race/ethnicity, child first- or second-generation immigrant, household language is English, mother age, and parent educational attainment. Model 2 adjusts for all variables in Model 1 and the following: parent married to child's biological father, parent employed, mother in fair or poor health, household member receives welfare, household member receives WIC, household income below the poverty line, household member smokes inside the home, and neighborhood always safe for child. Model 3 adjusts for all variables in Model 2 and the following: parental incarceration, parental divorce or separation, household member mental health problem, parental death, witness of household member abuse, witness of violence, racial discrimination, and income difficulties. All analyses account for complex sampling design. Ns vary across outcome variables (see Table 1). *p < .05, **p < .01, ***p < .001.
Model 2 further adjusts for parent and household characteristics. The magnitude of the association between household member substance problems and children's health is reduced across outcomes, with these additional characteristics explaining between 26% (anxiety problems) and 69% (activity limitations) of the association (coefficients not presented). The associations remain statistically significant for eight of the 14 outcomes. Children exposed to household member substance problems, compared to their counterparts, have a greater likelihood of chronic school absence (OR = 1.62; 95% CI = 1.07, 2.46), learning disability (OR = 1.48; 95% CI = 1.18, 1.85), ADD/ADHD (OR = 1.69; 95% CI = 1.40, 2.05), depression (OR = 1.79; 95% CI = 1.40, 2.29), anxiety problems (OR = 2.14; 95% CI = 1.70, 2.71), and behavioral or conduct problems (OR = 2.07; 95% CI = 1.69, 2.54). They also have a greater likelihood of any specific health condition (OR = 1.65, 95% CI = 1.40, 1.93) and have a greater number of specific health conditions (b = 0.40, 95% CI = 0.29, 0.50).
Model 3, which further adjusts for eight additional ACEs, shows household member substance problems is significantly associated with only two of the 14 outcomes. Children exposed to household member substance problems, compared to their counterparts, have 1.25 times the odds of ADD/ADHD (95% CI = 1.00, 1.56) and 1.39 times the odds of anxiety problems (95% CI = 1.06, 1.83). In supplemental analyses, we examined which of the eight additional ACEs explained the largest percentage of the association between household member substance problems and children's health. We found that household member mental health explained the largest share of the association (55% of the association, on average, across all of the outcome variables), followed by parental incarceration (17%), witness of household member abuse (16%), witness of violence (13%), income difficulties (9%), parental divorce or separation (8%), racial discrimination (6%), and parental death (0%).
The models presented combine children of all ages, but it is possible that the association between household member substance problems and children's health varies across children's age. We consider this possibility in Appendix Table 2, which presents results from regression models estimating children's health as a function of household member substance problems separately across the following three age groups: (1) children ages 0 to 5, (2) children ages 6 to 11, and (3) children ages 12 to 17. By and large, this table shows that the statistically significant associations between household member substance problems and children's health are consistent across children's age groups. However, there is some evidence that the magnitude of the association is larger among children ages 0 to 5 (compared to children ages 6 to 11 or children ages 12 to 17). For example, household member substance problems is associated with 1.96 times the odds of any specific health condition among children ages 0 to 5 (95% CI = 1.37, 2.81), compared to 1.65 times the odds among children ages 6 to 11 (95% CI = 1.25, 2.16) and 1.53 times the odds among children ages 12 to 17 (95% CI = 1.25, 1.88).
4. Discussion
Living with a household member who has problems with drugs or alcohol is considered an adverse childhood experience (ACE), defined as a potentially stressful or traumatic event (Felitti, 2009). Despite the sizable number of children exposed to household member substance problems, as well as reasons to believe that household member substance problems is a social determinant of children's health, little research examines differences in children's health among children exposed and not exposed to household member substance problems (Berg et al., 2016; Jääskeläien et al., 2016; Kandel, 1990; Osborne & Berger, 2009; Raitasalo & Holmila, 2017; Thompson et al., 2017; Zebrak & Green, 2016). This is an especially important oversight given the burgeoning research on the social determinants of children's health (Mehta, Lee, & Ylitalo, 2013; Turney, Lee, & Mehta, 2013) and the health consequences of ACE exposure more generally (Anda et al., 1999; Chapman et al., 2004; Corso, Edwards, Fang, & Mercy, 2008; Felitti, 2009; Felitti et al., 1998; Gilbert, Patel, Farmer, & Lu, 2015; Klassen, Chirico, O’Leary, Cairney, & Wade, 2016; Turney, 2018; Wade, Shea, Rubin, & Wood, 2014). In this article, we use newly released data from the 2016 National Survey of Children's Health (NSCH), a probability sample of U.S. children, to provide a nationally representative accounting of the association between household member substance problems and children's health.
Results suggest three conclusions. First, we find that a sizable percentage of U.S. children are exposed to household member substance problems (Lipari & Van Horn, 2017a, 2017b). Nearly one-tenth (9.0%) of children have lived with a household member who has drug or alcohol problems. By age 17, about one-seventh (14.2%) of children have experienced household member substance problems. Importantly, household member substance problems is the second most commonly reported ACE (following parental divorce or separation).
Second, in accordance with the stress process perspective, we find that children exposed to household member substance problems are more likely than other children to have health problems (Avison, 2010; Pearlin, 1989; Pearlin et al., 1981, 1997). These descriptive differences exist across all health outcomes considered. On average, children exposed to household member substance problems have worse global health (measured by fair or poor health, activity limitations, and chronic school absence) than other children. They are also between two and four times as likely to have mental health problems (such as depression and anxiety) and physical health problems (including obesity and asthma).
Third, for all but two of the 14 outcomes considered, the descriptive associations between household member substance problems and children's health fall from statistical significance in fully adjusted multivariate models. Adjusting for parent and household characteristics (such as parental marital status and educational attainment) explains some of the association between household member substance problems and children's health. Adjusting for additional ACEs (such as household member mental illness and parental incarceration) further explains the association between household member substance problems and children's health. Importantly, these models provide a conservative estimate of the relationship between household member substance problems and children's health, as they adjust for other ACEs that are both correlated with household member substance problems and are possibly endogenous to household member substance problems. For example, it is quite possible that household member substance problems engenders an additional ACE, parental incarceration, which then initiates and exacerbates health problems among children.
In the most rigorous models—those that adjust for child, parent, and household characteristics (including additional ACEs)—household member substance problems is only associated with an increased risk of ADD/ADHD and anxiety. This means that, for most health outcomes, the association between household member substance problems and children's health results not from household member substance problems but instead from characteristics correlated with household member substance problems (especially additional ACEs). This also means that household member substance problems are independently associated with ADD/ADHD and anxiety. The stress process perspective is non-specific in nature, so does not provide guidance as to why these two outcomes may be especially reactive to household member substance problems, but future research should work to understand how social determinants of children's health may be differentially associated with specific outcomes (Pearlin et al., 1981).
The analyses suggest some possible explanations for the descriptive association between household member substance problems and children's health. For example, the magnitude of these associations decreases after adjusting for socioeconomic characteristics such as parental educational attainment and household poverty. The relationship between household member substance problems and socioeconomic characteristics is likely bi-directional, and the cross-sectional data do not facilitate disentangling these bi-directional relationships, but this finding provides suggestive evidence that household economic instability is a pathway linking household member substance problems to children's health (Bloom et al., 2009; Rehm et al., 2009).
Similarly, the analyses provide suggestive evidence that additional ACEs—such as parental divorce or parental incarceration—may link household member substance problems to children's health. Recent research finds that children who experience parental incarceration are eight times as likely as their counterparts to experience household member substance problems (Corso et al., 2008). Again, the direction of causality is likely bi-directional, with parental incarceration and household member substance problems influencing one another, and these data do not allow us to consider these complexities. That said, the findings suggest a relationship between household member substance problems and other ACEs, which together may have deleterious consequences for children's health (Felitti, 2009; Jimenez, Wade, Lin, Morrow, & Reichman, 2016). Establishing proper time-ordering between the dependent, independent, and control variables, as well as untangling the mechanisms linking household member substance problems to children's health, are important directions for future research.
4.1. Limitations
We used nationally representative data that are appropriate to examine the association between household member substance problems and children's health. However, limitations exist. First, these observational data preclude causal conclusions, as it is possible there exist unobserved characteristics that would render the relationship between household member substance problems and children's health statistically non-significant. Unobserved characteristics may render the association between household member substance problems and children's ADD/ADHD and anxiety spurious. Relatedly, the cross-sectional data necessitate that household member substance problems is measured contemporaneously with the control variables; therefore, the analyses likely obscure some characteristics that link household member substance problems and children's health. Second, similar to other data sources, the measure of household member substance problems is reported by the parent respondent and is not a clinical or diagnostic indicator of alcohol or drug abuse (Osborne & Berger, 2009). Third, important information about household member substance problems remains unobserved. The data do not include information about who in the household has substance problems, how long the child was exposed to household member substance problems, and how frequently the child was exposed to substance use; these contingencies may be differentially associated with children's health. These limitations are outweighed by the large, recent, and nationally representative sample but provide important directions for future research.
5. Conclusions
These findings have important public health implications. Household member substance problems is a commonly experienced ACE, with nearly one-tenth of all children in the United States having lived with a household member with an alcohol or drug problem. Children exposed to household member substance problems are a vulnerable population, as these children have more health problems than their counterparts. Pediatricians should consider screening parents for substance problems and direct parents to appropriate resources for treatment and, in turn, alleviate stressors in children's lives. Pediatricians should also pay particular attention to the health of children living with family members who have substance problems. Given that household member substance problems are concentrated among socioeconomically disadvantaged children, children at a greater risk of health problems than their counterparts, this ACE may exacerbate existing socioeconomic inequalities in children's health (Bloom et al., 2009).
Ethics
This research does not involve human subjects. This research was deemed exempt from human subjects research by the institutional review board at the University of California, Irvine.
Acknowledgement
This project was funded by a small grant from the Center for Demographic and Social Analysis at the University of California, Irvine. The authors are grateful to Jessica Hardie and Anita Zuberi for their feedback on an earlier version of this manuscript. The authors have no conflicts of interests to report. The authors have no financial disclosures to report.
Footnotes
Table A1.
| Household member drug or alcohol problem | Parental incarceration | Parental divorce or separation | Parental death | Witness of household member abuse | Witness of violence | Household member mental illness | Racial discrimination | Income difficulties | |
|---|---|---|---|---|---|---|---|---|---|
| Household member drug or alcohol problem | 1.000 | ||||||||
| Parental incarceration | 0.398 | 1.000 | |||||||
| Parental divorce or separation | 0.325 | 0.331 | 1.000 | ||||||
| Parental death | 0.137 | 0.123 | 0.101 | 1.000 | |||||
| Witness of household member abuse | 0.365 | 0.345 | 0.295 | 0.086 | 1.000 | ||||
| Witness of violence | 0.262 | 0.242 | 0.188 | 0.089 | 0.344 | 1.000 | |||
| Household member mental illness | 0.360 | 0.193 | 0.230 | 0.093 | 0.267 | 0.240 | 1.000 | ||
| Racial discrimination | 0.097 | 0.093 | 0.080 | 0.046 | 0.108 | 0.100 | 0.094 | 1.000 | |
| Income difficulties | 0.117 | 0.119 | 0.147 | 0.038 | 0.127 | 0.110 | 0.148 | 0.063 | 1.000 |
Table A2.
| Ages 0 to 5 |
Ages 6 to 11 |
Ages 12 to 17 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR or b | [CI] | OR or b | [CI] | OR or b | [CI] | ||||
| Fair or poor health | 0.20 | * | [0.05, 0.77] | 1.81 | [0.68, 4.84] | – | – | ||
| Activity limitation | 1.43 | [0.80, 2.56] | 1.06 | [0.70, 1.58] | 1.14 | [0.80, 1.62] | |||
| Chronic school absence | – | – | 0.96 | [0.52, 1.78] | 1.85 | * | [1.45, 3.00] | ||
| Learning disability | 1.73 | [0.80, 3.72] | 1.68 | ** | [1.17, 2.40] | 1.28 | [0.93, 1.76] | ||
| ADD/ADHD | 1.69 | [0.75, 3.81] | 1.89 | *** | [1.40, 2.56] | 1.60 | *** | [1.25, 2.06] | |
| Depression | – | – | 1.26 | [0.75, 2.12] | 1.93 | *** | [1.45, 2.57] | ||
| Anxiety problems | 2.89 | * | [1.23, 6.77] | 2.25 | *** | [1.50, 3.38] | 1.94 | *** | [1.52, 2.49] |
| Behavioral or conduct problems | 2.10 | ** | [1.22, 3.62] | 2.32 | *** | [1.68, 3.22] | 1.78 | *** | [1.34, 2.38] |
| Developmental delay | 1.62 | [0.94, 2.79] | 1.45 | [0.96, 2.19] | 0.82 | [0.54, 1.23] | |||
| Asthma | 1.24 | [0.76, 2.04] | 1.15 | [0.79, 1.70] | 1.16 | [0.86, 1.56] | |||
| Obesity | – | – | – | – | 1.09 | [0.43, 1.43] | |||
| Speech or other language disorder | 1.65 | * | [1.01, 2.69] | 1.11 | [0.74, 1.67] | 1.00 | [0.62, 1.61] | ||
| Any specific health condition | 1.96 | *** | [1.37, 2.81] | 1.65 | *** | [1.25, 2.16] | 1.53 | *** | [1.25, 1.88] |
| Number of specific health conditions | 0.62 | *** | [0.29, 0.94] | 0.41 | *** | [0.25, 0.57] | 0.32 | *** | [0.19, 0.45] |
| N | 50,212 | 50,212 | 50,212 | ||||||
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Anda R.F., Croft J.B., Felitti V.J., Nordenberg D., Giles W.H., Williamson D.F. Adverse childhood experiences and smoking during adolescence and adulthood. Journal of the American Medical Association. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]; Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, Giovino GA. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652-1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed]
- Avison W.R. Incorporating children's lives into a life course perspective on stress and mental health. Journal of Health and Social Behavior. 2010;51(4):361–375. doi: 10.1177/0022146510386797. [DOI] [PubMed] [Google Scholar]; Avison WR. Incorporating children’s lives into a life course perspective on stress and mental health. J Health Soc Behav. 2010;51(4), 361-375. doi: 10.1177/0022146510386797 [DOI] [PubMed]
- Berg L., Bäck K., Vinnerljung B., Hjern A. Parental alcohol-related disorders and school performance in 16 year olds-a Swedish national cohort study. Addiction. 2016;111:1795–1803. doi: 10.1111/add.13454. [DOI] [PMC free article] [PubMed] [Google Scholar]; Berg L, Back K, Vinnerljung B, Hjern A. Parental alcohol-related disorders and school performance in 16 year olds-a Swedish national cohort study. Addict. 2016;111:1795-1803. doi: 10.1111/add.13454 [DOI] [PMC free article] [PubMed]
- Bloom B., Cohen R.A., Freeman G. Summary health statistics for U.S. children: National health interview survey, 2008. Vital Health Stat. 2009;10(244):1–81. https://www.cdc.gov/nchs/data/series/sr_10/sr10_244.pdf [PubMed] [Google Scholar]; Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National health interview survey, 2008. Vital Health Stat 10. 2009;(244):1-81. https://www.cdc.gov/nchs/data/series/sr_10/sr10_244.pdf [PubMed]
- Bzostek S.H., Beck A.N. Familial instability and young children's physical health. Social Science & Medicine. 2011;73(2):282–292. doi: 10.1016/j.socscimed.2011.04.014. [DOI] [PubMed] [Google Scholar]; Bzostek SH, Beck AN. Familial instability and young children’s physical health. Soc Sci Med. 2011;73(2):282-292. Doi: 10.1016/j.socscimed.2011.04.014 [DOI] [PubMed]
- Case A., Lubotsky D., Paxson C. Economic status and health in childhood: The origins of the gradient. The American Economic Review. 2002;92(5):1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]; Case A, Lubotsky D, Paxson C. Economic status and health in childhood: The origins of the gradient. Am Econ Rev. 2002;92(5):1308-1334. doi: 10.1257/000282802762024520 [DOI] [PubMed]
- Chapman M.V., Wall A., Barth R.P., Biemer P., Runyan D., Webb M. Children's voices: The perceptions of children in foster care. American Journal of Orthopsychiatry. 2004;74(3):293–304. doi: 10.1037/0002-9432.74.3.293. [DOI] [PubMed] [Google Scholar]; Chapman MV, Wall A, Barth RP, Biemer P, Runyan D, Webb M, et al. Children’s voices: The perceptions of children in foster care. Am J Orthopsychiatry. 2004;74(3):293-304. doi: 10.1037/0002-9432.74.3.293. [DOI] [PubMed]
- Chen E., Martin A.D., Matthews K.A. Understanding health disparities: The role of race and socioeconomic status in children's health. American Journal of Public Health. 2006;96(4):702–708. doi: 10.2105/AJPH.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chen E, Martin AD, Matthews KA. Understanding health disparities: The role of race and socioeconomic status in children’s health. Am J Public Health. 2006;96(4):702-708. doi: 10.2105/AJPH.2004.048124 [DOI] [PMC free article] [PubMed]
- Child and Adolescent Health Measurement Initiative, Data Resource Center for Child and Adolescent Health . Vol. 2018. 2016. www.childhealthdata.org (National Survey of Children's Health (NSCH) [Stata indicator data set]. Health resources and Services administration, maternal and child health Bureau in collaboration with the U.S. Census Bureau). Retrieved. [Google Scholar]; Child and Adolescent Health Measurement Initiative, Data Resource Center for Child and Adolescent Health. 2016 National Survey of Children’s Health (NSCH) [Stata Indicator Data Set]. Health Resources and Services Administration, Maternal and Child Health Bureau in collaboration with the U.S. Census Bureau. 2018. Retrieved December 1, 2017 from www.childhealthdata.org.
- Corso P.S., Edwards V.J., Fang X., Mercy J.A. Health-related quality of life among adults who experienced maltreatment during childhood. American Journal of Public Health. 2008;98(6):1094–1100. doi: 10.2105/AJPH.2007.119826. [DOI] [PMC free article] [PubMed] [Google Scholar]; Corso PS, Edwards VJ, Fang X, Mercy JA. Health-related quality of life among adults who experienced maltreatment during childhood. Am J Public Health. 2008;98(6):1094-1100. doi: 10.2105/AJPH.2007.119826. [DOI] [PMC free article] [PubMed]
- Dube S.R., Felitti V.J., Dong M., Files W.H., Anda R.F. The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Journal of Preventive Medicine. 2003;37(3):268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]; Dube SR, Felitti VJ, Dong M, Files WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. J Prev Med. 2003;37(3):268-277. doi: 10.1016/S0091-7435(03)00123-3. [DOI] [PubMed]
- Felitti V.J. Adverse childhood experiences and adult health. Academy of Pediatrics. 2009;9(3):131–132. doi: 10.1016/j.acap.2009.03.001. [DOI] [PubMed] [Google Scholar]; Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009;9(3):131-132. doi:10.1016/j.acap.2009.03.001. [DOI] [PubMed]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]; Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed]
- Gilbert B.J., Patel V., Farmer P.E., Lu C. Assessing development assistance for mental health in developing countries: 2007-2013. PLoS Medicine. 2015;12(6) doi: 10.1371/journal.pmed.1001834. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gilbert BJ, Patel V, Farmer PE, Lu C. Assessing development assistance for mental health in developing countries: 2007-2013. PLoS Med. 2015;12(6):e1001834. doi: 10.1371/journal.pmed.1001834. [DOI] [PMC free article] [PubMed]
- Hardie J.H., Landale N.S. Profiles of risk: Maternal health, socioeconomic status, and child health. Journal of Marriage and Family. 2013;75(3):651–666. doi: 10.1111/jomf.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hardie JH, Landale NS. Profiles of risk: maternal health, socioeconomic status, and child health. J Marriage Fam. 2013;75(3):651-666. doi: 10.1111/jomf.12021 [DOI] [PMC free article] [PubMed]
- Idler E.L., Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]; Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21-37. doi: 10.2307/2955359 [PubMed]
- Jääskeläien M., Holmila M., Notkola I.L., Raitasalo K. Mental disorders and harmful substance use in children of substance abusing parents: A longitudinal register-based study on a complete birth cohort born in 1991. Drug and Alcohol Review. 2016;35:728–740. doi: 10.1111/dar.12417. [DOI] [PubMed] [Google Scholar]; Jaaskelaien M, Holmila M, Notkola IL, Raitasalo K. Mental disorders and harmful substance use in children of substance abusing parents: A longitudinal register-based study on a complete birth cohort born in 1991. Drug Alc Rev. 2016;35:728-740. doi: 10.1111/dar.12417 [DOI] [PubMed]
- Jimenez M.E., Wade R., Lin Y., Morrow L.M., Reichman N.E. Adverse experiences in early childhood and kindergarten outcomes. Journal of Pediatrics. 2016;137(2) doi: 10.1542/peds.2015-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jimenez ME, Wade R, Lin Y, Morrow LM, Reichman NE. Adverse experiences in early childhood and kindergarten outcomes. J Pediatr. 2016;137(2):e20151839. doi: 10.1542/peds.2015-1839 [DOI] [PMC free article] [PubMed]
- Kandel D.B. Parenting styles, drug use, and children's adjustment in families of young adults. Journal of Marriage and Family. 1990;52(1):183–196. [Google Scholar]; Kandel DB. Parenting styles, drug use, and children's adjustment in families of young adults. J Marriage Fam. 1990;52(1):183-196. doi: 10.2307/352849
- Kessler R.C., Chiu W.T., Demler O., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatr. 2005;62(6): 617-627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed]
- Klassen S.A., Chirico D., O'Leary D.D., Cairney J., Wade T.J. Linking systemic arterial stiffness among adolescents to adverse childhood experiences. Child Abuse & Neglect. 2016;56:1–10. doi: 10.1016/j.chiabu.2016.04.002. [DOI] [PubMed] [Google Scholar]; Klassen SA, Chirico D, O’Leary DD, Cairney J, Wade TJ. Linking systemic arterial stiffness among adolescents to adverse childhood experiences. Child Abuse Negl. 2016;56:1-10. doi: 10.1016/j.chiabu.2016.04.002. [DOI] [PubMed]
- Lipari R.N., Van Horn S.L. The CBHSQ report. Rockville (MD): Substance abuse and mental health services administration (US) 2017. Trends in substance use disorders among adults aged 18 or older.https://www.ncbi.nlm.nih.gov/books/NBK447253/ [PubMed] [Google Scholar]; Lipari RN, Van Horn SL. Trends in substance use disorders among adults aged 18 or older. In: The CBHSQ Report. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2017. https://www.ncbi.nlm.nih.gov/books/NBK447253/. Accessed June 26, 2018. [PubMed]
- Lipari R.N., Van Horn S.L. The CBHSQ report. Rockville (MD): Substance abuse and mental health services administration (US) 2017. Children living with parents who have a substance use disorder.https://www.ncbi.nlm.nih.gov/books/NBK464590/ [PubMed] [Google Scholar]; Lipari RN, Van Horn SL. Children living with parents who have a substance use disorder. In: The CBHSQ Report. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2017. https://www.ncbi.nlm.nih.gov/books/NBK464590/. Accessed June 26, 2018. [PubMed]
- McLeod J.D., Shanahan M.J. Poverty, parenting, and children's mental health. American Sociological Review. 1993;58(3):351–366. [Google Scholar]; McLeod JD, Shanahan MJ. Poverty, parenting, and children’s mental health. Amer Soc Rev.1993;58(3):351-366. doi: 10.2307/2095905
- Mehta N.K., Lee H., Ylitalo K.R. Child health in the United States: Recent trends in racial/ethnic disparities. Social Science & Medicine. 2013;95:6–15. doi: 10.1016/j.socscimed.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mehta NK, Lee H, Ylitalo KR. Child health in the United States: recent trends in racial/ethnic disparities. Soc Sci Med. 2013;95:6-15. doi: 10.1016/j.socscimed.2012.09.011. [DOI] [PMC free article] [PubMed]
- Osborne C., Berger L.M. Parental substance abuse and child well-being: A consideration of parents' gender and coresidence. Journal of Family Issues. 2009;30(3):341–370. [Google Scholar]; Osborne C, Berger LM. Parental substance abuse and child well-being: a consideration of parents' gender and coresidence. J Fam Issues. 2009;30(3): 341-370. doi: 10.1177/0192513X08326225.
- Pearlin L.I. The sociological study of stress. Journal of Health and Social Behavior. 1989;30(1):241–256. [PubMed] [Google Scholar]; Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989; 30(1);241-256. doi: 10.2307/2136956 [PubMed]
- Pearlin L.I., Aneshensel C.S., LeBlanc A.J. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. Journal of Health and Social Behavior. 1997;38(3):223–236. [PubMed] [Google Scholar]; Pearlin LI, Aneshensel CS, LeBlanc AJ. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. J Health Soc Behav. 1997;38(3);223-236. doi: 10.2307/2955368 [PubMed]
- Pearlin L.I., Menaghan E.G., Lieberman M.A., Mullan J.T. The stress process. Journal of Health and Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]; Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4);337-356. doi: 10.2307/2136676 [PubMed]
- Peleg-Oren N., Teichman M. Young children of parents with substance use disorders (SUD): A review of the literature and implications for social work practice. Journal of Social Work Practice in the Addictions. 2006;6(1–2):49–61. [Google Scholar]; Peleg-Oren N, Teichman M. Young children of parents with substance use disorders (SUD): A review of the literature and implications for social work practice. J of Soc Work Pract Addict. 2006;6(1-2):49-61. doi: 10.1300/J160v06n01_03.
- Raitasalo K., Holmila M. Parental substance abuse and risks to children's safety, health and psychological development. Drugs. 2017;24(1):17–22. [Google Scholar]; Raitasalo K, Holmila M. Parental substance abuse and risks to children's safety, health and psychological development. Drugs. 2017;24(1):17-22. doi: 10.1080/09687637.2016.1232371
- Rehm J., Mathers C., Popova S., Tavorncharoensap M., Teerawattananon Y., Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373(9682):2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]; Rehm J, Mathers C, Popova S, Tavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373(9682):2223-2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed]
- Schilling E.A., Aseltine R.H., Gore S. Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health. 2007;7(1):30. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]; Schilling EA, Aseltine RH, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7(1):30. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed]
- Thompson R.G., Alonzo D., Hu M.C., Hasin D.S. The influences of parental divorce and maternal-versus parental alcohol abuse on offspring lifetime suicide attempt. Drug and Alcohol Review. 2017;36:408–414. doi: 10.1111/dar.12441. [DOI] [PubMed] [Google Scholar]; Thompson RG, Alonzo D, Hu MC, Hasin DS. The influences of parental divorce and maternal-versus parental alcohol abuse on offspring lifetime suicide attempt. Drug Alcohol Rev. 2017;36:408-414. doi: 10.1111/dar.12441. [DOI] [PubMed]
- Turney K. Maternal depression and childhood health inequalities. Journal of Health and Social Behavior. 2011;52(3):314–332. doi: 10.1177/0022146511408096. [DOI] [PubMed] [Google Scholar]; Turney K. Maternal depression and childhood health inequalities. J Health Soc Behav. 2011;52(3):314-332. doi: 10.1177/0022146511408096 [DOI] [PubMed]
- Turney K. Perceived instrumental support and children's health across the early life course. Social Science & Medicine. 2013;95:34–42. doi: 10.1016/j.socscimed.2012.08.017. [DOI] [PubMed] [Google Scholar]; Turney, K. (2013). Perceived instrumental support and children's health across the early life course. Soc Sci Med, 95, 34-42. Doi: 10.1016/j.socscimed.2012.08.017 [DOI] [PubMed]
- Turney K. Adverse childhood experiences among children of incarcerated parents. Children and Youth Services Review. 2018;89 [Google Scholar]; Turney K. Adverse childhood experiences among children of incarcerated parents. Child Youth Serv Rev. 2018;89: 10.1016/j.childyouth.2018.04.033.
- Turney K., Hardie J.H. Health limitations among mothers and fathers: Implications for parenting. Journal of Marriage and Family. 2017;80(1):219–238. doi: 10.1111/jomf.12425. [DOI] [PMC free article] [PubMed] [Google Scholar]; Turney K, Hardie JH. Health limitations among mothers and fathers: implications for parenting. J Marriage Fam. 2017;80(1):219-238. doi: 10.1111/jomf.12425 [DOI] [PMC free article] [PubMed]
- Turney K., Lee H., Mehta N.K. The social determinants of children's health. Social Science & Medicine. 2013;95:1–5. doi: 10.1016/j.socscimed.2013.07.015. [DOI] [PubMed] [Google Scholar]; Turney K, Lee H, Mehta NK. The social determinants of children’s health. Soc Sci Med. 2013;95:1-5. doi: 10.1016/j.socscimed.2013.07.015. [DOI] [PubMed]
- U.S. Census Bureau . 2017. 2016 National Survey of Children's Health: Nonresponse bias analysis.https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/nonresponse-bias-analysis/NSCH%202016%20Nonresponse%20Bias%20Analysis.pdf Retrieved. [Google Scholar]; U.S. Census Bureau. 2017. 2016 National Survey of Children’s Health: Nonresponse Bias Analysis. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/nonresponse-bias-analysis/NSCH%202016%20Nonresponse%20Bias%20Analysis.pdf. Retrieved July 6, 2018.
- Wade R., Shea J.A., Rubin D., Wood J. Adverse childhood experiences of low-income urban youth. Journal of Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]; Wade R, Shea JA, Rubin D, Wood J. Adverse childhood experiences of low-income urban youth. J Pediatr. 2014;134(1):e13-e20. doi:10.1542/peds.2013-2475. [DOI] [PubMed]
- Whisman M.A. Marital dissatisfaction and psychiatric disorders: Results from the National Comorbidity Survey. Journal of Abnormal Psychology. 1999;108(4):701–706. doi: 10.1037//0021-843x.108.4.701. [DOI] [PubMed] [Google Scholar]; Whisman MA. Marital dissatisfaction and psychiatric disorders: results from the National Comorbidity Survey. J Abnorm Psychol. 1999;108(4):701-706. doi: 10.1037/0021-843X.108.4.701 [DOI] [PubMed]
- Whiteford H.A., Degenhardt L., Rehm J., Baxter A.J., Ferrari A.J., Erskine H.E. Global burden of disease attributable to mental and substance use disorders: Findings from the global burden of disease study 2010. The Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]; Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013:382(9904): 1575-1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed]
- Zebrak K.A., Green K.M. Mutual influences between parental psychological distress and alcohol use and children problem behavior in a cohort of urban African Americans. Journal of Family Issues. 2016;37(13):1869–1890. doi: 10.1177/0192513X14553055. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zebrak KA, Green KM. Mutual influences between parental psychological distress and alcohol use and children problem behavior in a cohort of urban African Americans. J Fam Issues. 2016;37(13):1869-1890. doi: 10.1177/0192513X14553055 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.