Abstract
Background and Aims
Er:YAG laser has become optional for enamel and dentin preparation for a decade. However, it is unclear if Er:YAG laser is acceptable for enamel conditioning prior to an application of a pit-and-fissure sealant. This in vitro study thus aimed to investigate shear bond strength of a sealant to enamel etched with Er:YAG laser, as well as to demonstrate an alteration of enamel surface after the laser was applied.
Materials and Methods
One hundred and twenty extracted human premolars were divided into 4 groups (N = 30 per group) in which the enamel surfaces were treated with 1) 37% phosphoric acid, 2) Er:YAG laser 80 mJ/pulse, 2 Hz, 3) Er:YAG laser 120 mJ/pulse, 10 Hz, and 4) Er:YAG laser 140 mJ/pulse, 2 Hz. Prior to sealant application. Shear bond strength was determined by using a universal testing machine. Statistical analysis was performed using One-way ANOVA. Modification of enamel surface after laser ablation was also investigated using scanning electron microscope.
Results
Phosphoric acid-etched enamel yielded the highest shear bond strength when bonded with a sealant. Ablation of enamel with Er:YAG laser did not significantly improve sealant bonding since it demonstrated lower shear bond strength, compared to acid-etched enamel. Despite the presence of cracks after Er:YAG laser application, dissolution of enamel substances was limited.
Conclusion
Our study has shown a reduced shear bond strength of dental sealant to an Er:YAG laser-irradiated enamel, compared with phosphoric acid-etched enamel.
Keywords: Er:YAG laser, laser etching, pit and fissure sealant, enamel conditioning, shear bond strength
Introduction
To date, preventive dentistry has become an area of a recent focus as a conservative dental treatment plays a crucial role in minimizing a loss of tooth structure due to a pathologic cause. This conceptual treatment modality includes an implication of enamel adhesion with dental adhesives in dental practice with an ultimate purpose to reduce the incidence of dental disease i.e. dental caries as well as to preserve tooth structure 1–4). Sealing deep pits and fissures over occlusal surface, as well as other tooth surface in which deep grooves exist, with resin-based materials is thus recommended as a preventive measure that helps prevent a colonization of caries-related bacterial species on the tooth surface 5–7).
An adhesion of resin-based material to enamel surface was reported in 1955 by Buonocore in which an enamel conditioning with phosphoric acid prior was first introduced 8). Numbers of studies have validated the use of phosphoric acid for etching tooth surface and its subsequent effects on increasing the bond strength between resin and etched enamel 9–13). The reported effectiveness of enamel bonding to dental resin has increasingly enabled clinicians to utilize phosphoric acid as a standard protocol for enamel surface conditioning prior to a dental sealant placement procedure. However, among limitations of the usage of dental sealant, its ease of placement is usually compromised by the moisture contamination that impairs the retention of materials, resulting in the decreased efficacy of its use 14, 15). Therefore, a new treatment strategy has been introduced to possibly overcome a clinical situation in which the moisture control might be challenging during the clinical procedures.
The application of laser in clinical, dental treatments had been addressed in the last decades, and it is currently implicated as an alternative treatment modality in several dental fields. Er:YAG laser was first used in dentistry for hard tissue ablation and was reported to be biologically safe to the dental pulp 16–19). It might therefore be another approach for tooth preparation, as opposed to using an invasive method i.e. diamond burs. The use of Er:YAG laser for cavity preparation generates less vibration than using high-speed conventional handpiece, leading to a more satisfactory treatment outcome 20). The efficacy of Er:YAG laser used for enamel ablation and the effect of its altered surface on the bond strength with dental adhesives has also been extensively investigated 21–23). However, it is still controversial if Er:YAG laser is a suitable tool for enamel surface conditioning prior to the placement of dental sealants.
The objective of this experimental study was to determine an in vitro shear bond strength of dental sealant to the enamel surface pre-treated with Er:YAG laser irradiation. In addition, we investigated the microscopic features of enamel surface ablated with Er:YAG laser, compared to phosphoric acid-etched enamel. Despite a significantly lower shear bond strength of dental sealant bonded to Er:YAG-ablated enamel than that of acid-etched enamel, a physical alteration of superficial enamel surface might have some clinical implications and worth further investigations.
Materials and methods
Specimen preparation
The proposal of this study was reviewed and approved by Khon Kaen University Ethics Committee for human research based on the declaration of Helsinki. The dismissal of the consent was hence approved. One hundred and twenty human premolars extracted for an orthodontic purpose were used. All collected teeth must meet the following inclusion criteria:
-
-
Intact tooth crown with no crack line located on the enamel surface.
-
-
No cavitated lesion located on the smooth surface of buccal cusp.
-
-
No existing restoration i.e. amalgam, tooth-colored materials on the crown.
All teeth were curetted to remove gingival tissues and calculus, rinsed with distilled water prior to storage at room temperature in a 1% chloramine-T solution until use. All premolars were randomly divided into 4 groups (N = 30 per group) and the roots were cut 2 mm below cemento-enamel junction by using high speed handpiece with fissure diamond burs. Each tooth crown was embedded in a self-cured acrylic block made of polymerized vinyl chloride (PVC) pipe with 0.5-inch diameter and 1-inch length. Flat surfaces of buccal cusp were placed perpendicular to the long axis of PVC pipe in order to make the bound surface parallel to the applied shear force.
Enamel surface conditioning procedures
Four different surface treatment methods were performed (30 specimens/group) separately on the teeth designated as Group 1, 2, 3, and 4. Prior to enamel surface conditioning, all teeth were cleaned with a rubber cup and pumice using a low-speed handpiece for 20 seconds each, and rinsed with water. A 3-mm diameter circular shape was then drawn by a pencil on the enamel surface to specify the area in which phosphoric acid or Er:YAG laser irradiation was applied. Specific protocols were described below:
Group 1: Phosphoric acid etching – 37% phosphoric acid (Teethmate” F-1, Kuraray, Osaka, Japan) was applied for 20 seconds. All specimens were then rinsed with water for 30 seconds and air-dried for 5 seconds to ensure that the chalky-white surface was appeared.
Group 2: 80 mJ/pulse Er:YAG etching – Er:YAG laser machine (Fotona Dualis XS Erbium YAG 2940 nm, Ljubljana, Slovenia) was setup with the fixed parameters: wavelength of 2.94 µm, pulse energy of 80 mJ/pulse, pulse repetition rate of 2 Hz. Laser energy was delivered via a fiber tip placed 1 mm far from enamel surface under a very short pulse (VSP) mode. A laser focal point was emitted from a laser handpiece and allowed to move in a circular motion for 30 seconds with an integrated water coolant until the flaky surface was visible in the area located on the enamel as shown in Figure 1A.
Figure 1:
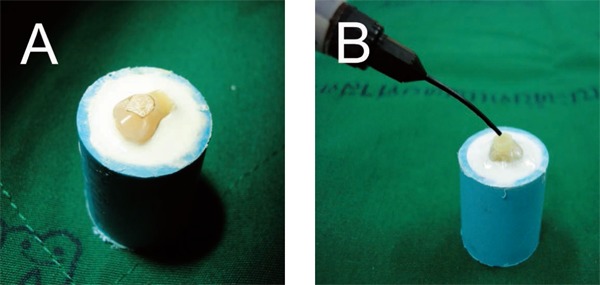
Sample preparation prior to sealant application. (A) Flaky enamel surface was achieved after Er:YAG laser ablation. (B) A light-cured dental sealant was applied into an orthodontic elastic placed on etched enamel surface.
Group 3: 120 mJ/pulse Er:YAG etching – Er:YAG laser machine was setup with the following parameters: wavelength of 2.94 µm, pulse energy of 120 mJ/pulse, pulse repetition rate of 10 Hz. Laser irradiation of enamel surface was performed as mentioned above.
Group 4: 140 mJ/pulse Er:YAG etching – Er:YAG laser machine was setup similarly but with a pulse energy of 140 mJ/pulse, pulse repetition rate of 2 Hz. Laser irradiation of enamel surface was performed likewise.
Sealant placement and a determination of shear bond strength
A 2-mm diameter hole was made on a clear adhesive tape using a rubber dam punch. A punctured tape was placed over the etched area of enamel surface with the adhesive surface placing toward the specimen. A 1/8 inch orthodontic elastic band with 1-mm thickness was then placed on the punctured hole. A light-cured pit and fissure sealant (Teethmate” F-1, Kuraray, Osaka, Japan) was dropped from a nozzle into an elastic band until it reached the upper margin of the band as demonstrated in Figure 1B. A placed sealant was cured by using a halogen light curing unit (Curing Light XL3000, 3M ESPE, St. Paul, MN, USA) for 40 seconds prior to a removal of elastic band by using cotton pliers. After sealant placement, all prepared specimens were incubated in distilled water at 37°C for 24 hours, and followed by 500-cycle thermocycling process between 5°C and 55°C using a thermocycler (TC-301 Thermocycler, King Mongkut's Institute of Technology, Bangkok, Thailand)
Shear bond strength was next determined using a universal testing machine (LLOYD instruments, Ametek Inc., FL, USA) with a crosshead speed of 0.5 mm per minute until the sealant failed to retain on the enamel. The maximum force was recorded in Newton (N) and converted to shear bond strength value in megapascal (MPa) by dividing the maximum force applied with a contact area of sealant to enamel in mm2. Sealant contact area was calculated by using πr2, in which r indicates a radius of a punctured hole (1 mm). Data were represented as mean ± standard deviation derived from 30 samples per group.
Scanning electron microscopic (SEM) analysis of the etched enamel
In order to examine the effect of surface conditioning on microscopic change of enamel surface, extracted premolars were prepared similarly under 4 protocols described earlier (N = 8 per group) using phosphoric acid etching as a comparison. Samples were coated with gold particles (sputter-carbon coater, K500X-012, Kent, UK) and observed under scanning electron microscope (S-3000N, Hitachi, Japan) at 100–2000 fold magnification levels.
Statistical analysis
Shear bond strength of sealants to enamel surfaces treated with different surface conditioning methods were statistically compared using One-way ANOVA with Bonferroni's post-hoc test. Statistically-significant difference was reported when P-value (P) was below 0.05. Statistical analysis was performed using GraphPad Prism Version 7 (GraphPad Software Inc., La Jolla, CA, USA).
Results
Shear bond strength derived from each experimental group is shown in Table 1. Notably, bonding between a sealant and phosphoric acid-etched enamel showed the maximum strength (11.03 ± 4.07 MPa) and was statistically different from those bonded with Er:YAG laser-irradiated enamel surfaces (P < 0.001). Despite the variability of laser setup, Er:YAG laser irradiation generated shear bond strength values in all experimental groups with no statistical difference between groups, as demonstrated in Table 2.
Table 1: Shear bond strength (MPa) of a pit-and-fissure sealant to enamel treated with different protocols.
| Sample | Mean (MPa) | Standard Deviation | 95% Confidence Interval |
|---|---|---|---|
| 37 % Phosphoric acid | 11.03 | 4.07 | 9.51 – 12.55 |
| Er:YAG 80 mJ/pulse 2 Hz. | 5.08 | 2.11 | 4.26 – 5.90 |
| Er:YAG 120 mJ/pulse 10 Hz. | 6.18 | 2.54 | 5.20 – 7.17 |
| Er:YAG 140 mJ/pulse 2 Hz. | 5.13 | 2.65 | 4.04 – 6.23 |
Table 2: Determination of statistically significant difference between treatment groups using One-way ANOVA with Bonferroni's post-hoc test.
| Multiple comparison between groups | Mean Difference | P-value | 95% Confidence Interval |
|
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Phosphoric acid vs Er:YAG 80* | 5.849 | < 0.001 | 3.313 | 8.721 |
| Phosphoric acid vs Er:YAG 120* | 4.738 | < 0.001 | 2.202 | 7.608 |
| Phosphoric acid vs Er:YAG 140* | 6.039 | < 0.001 | 3.399 | 9.033 |
| Er:YAG 80 vs Er:YAG 120 | −1.109 | 0.800 | −2.810 | 0.938 |
| Er:YAG 80 vs Er:YAG 140 | 0.112 | 1.000 | −1.666 | 2.257 |
| Er:YAG 120 vs Er:YAG 140 | 1.239 | 0.644 | −0.739 | 3.585 |
Asterisk (*) indicates a significant difference at P < 0.05.
We next investigated a microscopic change of enamel surface after 4 different protocols of surface conditioning were applied, prior to resin bonding. Of note, enamel etching with 37% phosphoric acid created a surface microroughness with the presence of unaffected enamel (Figure 2A). Higher magnifications of a microscopic feature showed the presence of both honey-comb and cobble-stone appearances (Figure 2B).
Figure 2:
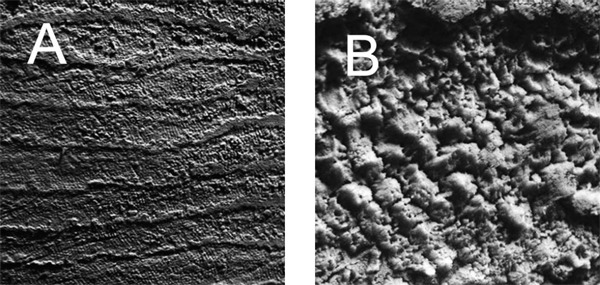
SEM evaluation of 37% phosphoric acid-etched enamel. (A) 100X magnification level. (B) 1000X magnification level showed enamel projections caused by the dissolution of enamel rods and peripheries.
When Er:YAG laser irradiation was applied on enamel, a superficial alteration of enamel structure was detected under SEM. A low pulse energy of Er:YAG laser (80 mJ/pulse, 2 Hz) created subtle change on enamel as visible under 100X magnification (Figure 3A). The dissolution of enamel substances surrounding the prism peripheries was clearly evident, with most of the surface was not ablated (Figure 3B). However, less enamel projections were abundantly shown when Er:YAG laser irradiation was used for enamel surface conditioning, compared with phosphoric acid-etched enamel. Interestingly, we found a drastic change of enamel surface after a higher power of Er:YAG (120 mJ/pulse, 10 Hz; and 140 mJ/pulse, 2 Hz) was used. Remarkably, enamel surface scaling and cracking were found at a 100X magnification level (Figure 4A, 5A). Despite the abundance of enamel flaking, the majority of enamel prisms remained slightly irradiated (Figure 4B, 5B).
Figure 3:
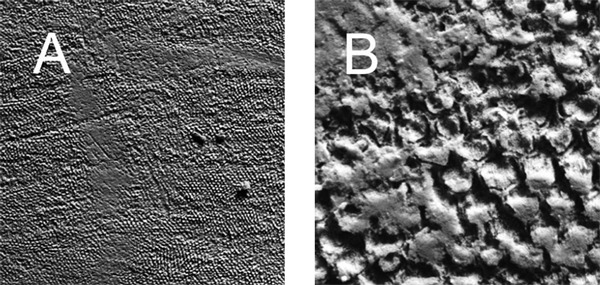
SEM evaluation of 80 mJ/pulse, 10 Hz. Er:YAG laser-irradiated enamel. (A) 100X magnification level. (B) 1000X magnification level showed partial removal of surface enamel.
Figure 4:
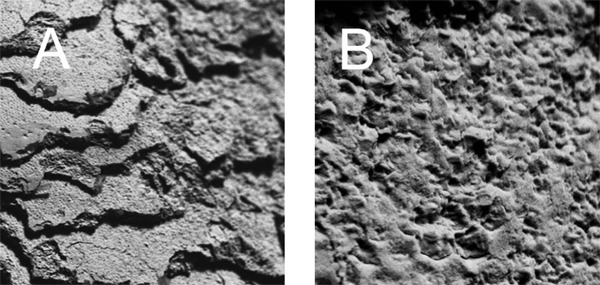
SEM evaluation of 120 mJ/pulse, 2 Hz. Er:YAG laser-irradiated enamel. (A) 100X magnification level demonstrated craters and cracks present on enamel surface. (B) 1000X magnification level revealed superficial enamel fusion and surface cracks.
Figure 5:
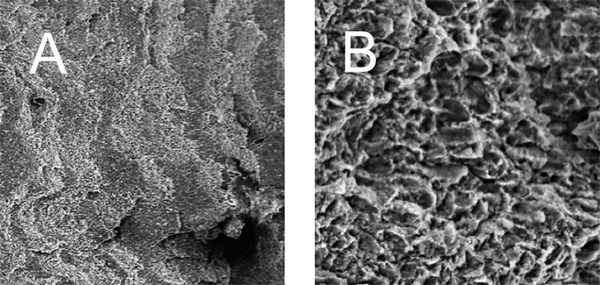
SEM evaluation of 140 mJ/pulse, 10 Hz. Er:YAG laser-irradiated enamel. (A) 100X magnification level showed enamel cracks, similar to Figure 4A. (B) 1000X magnification level demonstrated limited enamel dissolution and the presence of surface cracking.
Discussion
Development of laser technology has increasingly rendered modalities of dental treatment more rapid and convenient and brought more satisfactory clinical outcomes for the patients 16, 20). However, whether the use of laser in dentistry for ablating tooth surface has fetched a successful clinical results remains elusive. Although the number of in vitro investigations has shown the feasibility of laser application for roughening an enamel 21–24), it is not clear yet if the resultant laser-modified enamel surface improves the shear bond strength with resin-based materials used in restorative and preventive dentistry.
In this in vitro study, we used unground surfaces of extracted premolars for experimental execution in order to mimic a clinical scenario in which a fresh, untreated enamel surface is directly bound to the dental sealants. Previous clinical study showed the combination effect of acid etching and Er:YAG laser etching on improving sealant retention 25). However, a weak bond between dental adhesive and an Er:YAG laser-ablated enamel surface, relative to acid etching, as reported by previous laboratory investigations has rendered the utilization of Er:YAG laser for enamel surface conditioning controversial 22, 26, 27). In agreement with recent reports, we found that the shear bond strength between Er:YAG laser-irradiated enamel to a sealant was significantly lower than that of phosphoric acid-etched enamel. Surprisingly, variable settings of Er:YAG laser machine did not result in a statistical difference between the mean shear bond strength among 3 groups (Group 2, Group 3, and Group 4). Our findings thus suggest the independence of interfacial bond strength between irradiated enamel and sealant on the laser power. In addition, an impaired shear bond strength of dental sealant to Er:YAG laser-irradiated enamel, as demonstrated by our in vitro findings, indicates that the clinical effectiveness of a pitand-fissure sealant in dental caries prevention might be reduced when Er:YAG laser is used.
A roughness of enamel surface created by using Er:YAG laser has been investigated by several lines of studies. Introduction of Er:YAG laser power to a tooth surface generates a micro-explosion of enamel and dentin, a microscopic appearance that is thought to be responsible for enhancing a mechanical bond of tooth structures to resin materials 21, 22, 28, 29). In addition, a cuffing was reportedly found in the area of peritubular dentin 22). Our SEM investigation showed a significant alteration of an enamel after Er:YAG laser irradiation. Destruction of enamel surface and superficial cracking were found when a high pulse energy was used for surface conditioning (Figure 4B, 5B). Despite the presence of surface scaling and fissuring, the shear bond strength was compromised when compared to an acid-etched control. Our data clearly suggest that surface roughening by means of laser ablation alone is not sufficient to retain a pit and fissure sealant on the enamel surface. Rather, the dissolution of mineral contents from enamel structure is required for resin adherence to the tooth 8).
It is also of our interest as to whether the use of Er:YAG laser transforms both organic and inorganic compositions constituting enamel structure. Recent studies have shown the inhibitory effect of laser irradiation on enamel demineralization, possibly due to the altered calcium-to-phosphate ratio (Ca:P) after laser irradiation 30–33). Intriguingly, the application of high-powered carbon dioxide laser on the enamel induces the fusion of hydroxyapatite crystals, similar phenomena found after Er:YAG laser ablation, thereby rendering enamel recalcitrant to acidic environment 34, 35). Furthermore, melting of hydroxyapatite by laser energy results in micropore sealing on enamel surface, a consequent phenomenon caused by the deposition of denatured enamel organic matrix 34, 35). Fusion of enamel matrix might be associated with the reduced penetration of resin into enamel prisms. Even though reduced susceptibility of Er:YAG laser-treated enamel to dental caries is seemingly beneficial to the host, its clinical application must be of a careful consideration since it might compromise the bond strength of adhesive to irradiated tooth substrate. Thus, the use of Er:YAG laser aiming at prevention of dental caries still needs further study, particularly clinical trials to determine an in vivo effect of Er:YAG laser-irradiated enamel on resin bond strength as well as its acid resistance since enamel surface modification by Er:YAG laser may have a clinical implication in acid tolerance property of an enamel.
To recapitulate, our in vitro investigation has shown an altered adhesion of dental sealant to an Er:YAG laser-irradiated enamel. Shear bond strength of a sealant to phosphoric acid-etched enamel was significantly greater than that of Er:YAG laser-irradiated enamel. Abundant formation of enamel projections, found in acid-etched enamel, might be required for resin adhesion to tooth substrate. Despite the presence of cracks and fissures, sealant was poorly retained on the Er:YAG laser-irradiated enamel. However, the effect of Er:YAG laser on promoting caries tolerance property and a change of inorganic contents of the enamel make its use very promising and therefore needs further investigations. Considering its potential benefits on modifying enamel structure, Er:YAG laser might become a clinical tool used in preventive dentistry that provides a predictable, satisfactory treatment outcome.
Acknowledgments
We thank Associate Professor Sajee Sattayut at the Department of Oral Maxillofacial Surgery, Faculty of Dentistry, Khon Kaen University, for Er:YAG laser technical advice, and Associate Professor Numchai Sooksantisakoonchai, a former lecturer at the Department of Prosthodontics, for kindly providing a statistical assistance.
Funding resources
This study was financially supported by Research Funding Resource of Khon Kaen University Faculty of Dentistry.
References
- 1: Christensen GJ: Preventive restorative dentistry. Int Dent J, 1990; 40: 259-66. [PubMed] [Google Scholar]
- 2: Simonsen RJ: Pit and fissure sealant: review of the literature. Pediatr Dent, 2002; 24: 393-414. [PubMed] [Google Scholar]
- 3: Simonsen RJ: Preventive resin restorations and sealants in light of current evidence. Dent Clin North Am, 2005; 49: 815-23. [DOI] [PubMed] [Google Scholar]
- 4: Green DJ, Banerjee A: Contemporary adhesive bonding: bridging the gap between research and clinical practice. Dent Update, 2011; 38: 439-40, 443,-6, 449-50. [DOI] [PubMed] [Google Scholar]
- 5: Handelman SL, Buonocore MG, Heseck DJ: A preliminary report on the effect of fissure sealant on bacteria in dental caries. J Prosthet Dent, 1972; 27: 390-2. [DOI] [PubMed] [Google Scholar]
- 6: Handelman SL, Washburn F, Wopperer P: Two-year report of sealant effect on bacteria in dental caries. J Am Dent Assoc, 1976; 93: 967-70. [DOI] [PubMed] [Google Scholar]
- 7: Jeronimus DJ, Jr., Till MJ, Sveen OB: Reduced viability of microorganisms under dental sealants. ASDC J Dent Child, 1975; 42: 275-80. [PubMed] [Google Scholar]
- 8: Buonocore MG: A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res, 1955; 34: 849-53. [DOI] [PubMed] [Google Scholar]
- 9: Rock WP, Weatherill S, Anderson RJ: Retention of three fissure sealant resins. The effects of etching agent and curing method. Results over 3 years. Br Dent J, 1990; 168: 323-5. [DOI] [PubMed] [Google Scholar]
- 10: Symons AL, Chu CY, Meyers IA: The effect of fissure morphology and pretreatment of the enamel surface on penetration and adhesion of fissure sealants. J Oral Rehabil, 1996; 23: 791-8. [DOI] [PubMed] [Google Scholar]
- 11: Peutzfeldt A, Nielsen LA: Bond strength of a sealant to primary and permanent enamel: phosphoric acid versus self-etching adhesive. Pediatr Dent, 2004; 26: 240-4. [PubMed] [Google Scholar]
- 12: Lührs AK, Guhr S, Schilke R, Borchers L, Geurtsen W.et al.: Shear bond strength of self-etch adhesives to enamel with additional phosphoric acid etching. Oper Dent 2008;33:155-62. [DOI] [PubMed] [Google Scholar]
- 13: Asselin ME, Sitbon Y, Fortin D, Abelardo L, Rompre PH: Bond strength of a sealant to permanent enamel: evaluation of 3 application protocols. Pediatr Dent, 2009; 31: 323-8. [PubMed] [Google Scholar]
- 14: Feigal RJ, Hitt J, Splieth C: Retaining sealant on salivary contaminated enamel. J Am Dent Assoc, 1993; 124: 88-97. [DOI] [PubMed] [Google Scholar]
- 15: Barroso JM, Torres CP, Lessa FC, Pécora JD, Palma-Dibb RG.et al.: Shear bond strength of pit-and-fissure sealants to saliva-contaminated and noncontaminated enamel. J Dent Child, 2005; 72: 95-9. [PubMed] [Google Scholar]
- 16: Reyto R: Lasers and air abrasion. New modalities for tooth preparation. Dent Clin North Am, 2001; 45: 189-206. [PubMed] [Google Scholar]
- 17: van As G: Erbium laser in dentistry. Dent Clin N Am, 2004; 48: 1017-59. [DOI] [PubMed] [Google Scholar]
- 18: Mehl A, Kremers L, Salzmann K, Hickel R: 3D-volume ablation rate and thermal side effects with Er:YAG and Nd:YAG laser. Dent Mater, 1997; 13: 246-51. [DOI] [PubMed] [Google Scholar]
- 19: Armengol V, Jean A, Marion D: Temperature rise during Er:YAG and Nd:YAP laser ablation of dentin. J Endod, 2000; 26: 138-41. [DOI] [PubMed] [Google Scholar]
- 20: Takamori K, Furukawa H, Morikawa Y, Katayama T, Watanabe S: Basic study on vibrations during tooth preparations caused by high-speed drilling and Er:YAG laser irradiation. Lasers Surg Med, 2003; 32: 25-31. [DOI] [PubMed] [Google Scholar]
- 21: Wanderley RL, Monghini EM, Pécora JD, Palma-Dibb RG, Borsatto MC: Shear bond strength to enamel of primary teeth irradiated with varying Er:YAG laser energies and SEM examination of the surface morphology: an in vitro study. Photomed Laser Surg, 2005; 23: 260-7. [DOI] [PubMed] [Google Scholar]
- 22: Dunn WJ, Davis JT, Bush AC: Shear bond strength and SEM evaluation of composite bonded to Er:YAG laser-prepared dentin and enamel. Dent Mater, 2005; 21: 616-24. [DOI] [PubMed] [Google Scholar]
- 23: Kumar P, Goswami M, Dhillon JK, Rehman F, Thakkar D.et al.: Comparative evaluation of microhardness and morphology of permanent tooth enamel surface after laser irradiation and fluoride treatment – An in vitro study. Laser Ther, 2016; 25: 201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24: Rodríguez-Vilchis LE, Contreras-Bulnes R, Olea-Mejìa OF, Sánchez-Flores I, Centeno-Pedraza C: Morphological and structural changes on human dental enamel after Er:YAG laser irradiation: AFM, SEM, and EDS evaluation. Photomed Laser Surg, 2011; 29: 493-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25: Durmus B, Giray F, Peker S, Kargul B: Clinical evaluation of a fissure sealant placed by acid etching or Er:YAG laser combined with acid etching. Oral Health Prev Dent, 2017; 15: 157-62. [DOI] [PubMed] [Google Scholar]
- 26: Attrill D, Farrar S, King T, Dickinson M, Davies R.et al.: Er:YAG (λ = 2.94 µm) Laser etching of dental enamel as an alternative to acid etching. Lasers Med Sci, 2000; 20: 154-61. [Google Scholar]
- 27: Contreras-Bulnes R, Scougall-Vilchis RJ, Rodríguez-Vilchis LE, Centeno-Pedraza C, Olea-Mejìa OF, Alcántara-Galena M. Evaluation of self-etching adhesive and Er:YAG laser conditioning on the shear bond strength of orthodontic brackets. Sci World J 2013;8:719182. 10.1155/2013/719182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28: Aoki A, Ishikawa I, Yamada T, Otsuki M, Watanabe H.et al.: Comparison between Er:YAG laser and conventional technique for root caries treatment in vitro. J Dent Res, 1998; 77: 1404-14. [DOI] [PubMed] [Google Scholar]
- 29: Ceballo L, Toledano M, Osorio R, Tay FR, Marshall GW: Bonding to Er-YAG-laser-treated dentin. J Dent Res, 2002; 81: 119-22. [PubMed] [Google Scholar]
- 30: Oho T, Morioka T: A possible mechanism of acquired acid resistance of human dental enamel by laser irradiation. Caries Res, 1990; 24: 86-92. [DOI] [PubMed] [Google Scholar]
- 31: Fowler BO, Kuroda S: Changes in heated and in laser-irradiated human tooth enamel and their probable effects on solubility. Calcif Tissue Int, 1986; 38: 197-208. [DOI] [PubMed] [Google Scholar]
- 32: Contreras-Arriaga B, Rodríguez-Vilchis LE, Contreras-Bulnes R, Olea-Mejìa OF, Scougall-Vilchis RJ.et al.: Chemical and morphological changes in human dentin after Er:YAG laser irradiation: EDS and SEM analysis. Microsc Res Tech, 2015; 78: 1019-25. [DOI] [PubMed] [Google Scholar]
- 33: Aljdaimi A, Devlin H, Dickinson M, Alfutimie A. Effect of 2.94 µm Er:YAG laser on the chemical composition of hard tissues. Microsc Res Tech 2018; 10.1002/jemt.23051. [DOI] [PubMed] [Google Scholar]
- 34: McCormack SM, Fried D, Featherstone JD, Glena RE, Seka W: Scanning electron microscope observations of CO2 laser effects on dental enamel. J Dent Res, 1995; 74: 1702-8. [DOI] [PubMed] [Google Scholar]
- 35: Hsu CY, Jordan TH, Dederich DN, Wefel JS: Effects of low-energy CO2 laser irradiation and the organic matrix on inhibition of enamel demineralization. J Dent Res, 2000; 79: 1725-30. [DOI] [PubMed] [Google Scholar]


