Abstract
Background/Objective
Unwanted mental intrusions (UMIs), typically discussed in relation to Obsessive-Compulsive Disorder (OCD), are highly prevalent, regardless of the specific nationality, religion, and/or cultural context. Studies have also shown that UMIs related to Body Dysmorphic Disorder (BDD), Illness anxiety/Hypochondriasis (IA-H), and Eating Disorders (EDs) are commonly experienced. However, the influence of culture on these UMIs and their transdiagnostic nature has not been investigated.
Method
Participants were 1,473 non-clinical individuals from seven countries in Europe, the Middle-East, and South America. All the subjects completed the Questionnaire of Unpleasant Intrusive Thoughts, which assesses the occurrence and discomfort of four UMI contents related to OCD, BDD, IA-H, and EDs, and symptom questionnaires on the four disorders.
Results
Overall, 64% of the total sample reported having experienced the four UMIs. The EDs intrusions were the most frequently experienced, whereas hypochondriacal intrusions were the least frequent but the most disturbing. All the UMIs were significantly related to each other in frequency and disturbance, and all of them were associated with clinical measures of OCD, BDD, IA-H, and EDs.
Conclusions
UMIs are a common phenomenon across different cultural contexts and operate transdiagnostically across clinically different disorders.
Keywords: Obsessive-Compulsive spectrum disorders, Cross-cultural study, Unwanted mental intrusions, Transdiagnostic, Cross-sectional study
Resumen
Introducción/Objetivo
Las intrusiones mentales no deseadas (IM), clásicamente estudiadas en relación con el trastorno obsesivo-compulsivo (TOC), tienen una prevalencia elevada independientemente de la nacionalidad, religión, y/o el contexto cultural. Las investigaciones muestran que también es habitual experimentar IM sobre contenidos relacionados con el trastorno dismórfico corporal (TDC), la ansiedad por la enfermedad/hipocondría (AE-H) y los trastornos alimentarios (TCA). Sin embargo, la influencia de la cultura sobre estas IM y su naturaleza transdiagnóstica no se han investigado.
Método
Participaron 1.473 personas de siete países de Europa, Oriente Medio y Suramérica. Todas completaron el Cuestionario de Pensamientos Intrusos Desagradables, que evalúa la ocurrencia y malestar asociados a cuatro contenidos de IM relacionados con TOC, TDC, AE-H y TCA, y cuestionarios sobre síntomas de los cuatro trastornos.
Resultados
El 64% de la muestra total había experimentado las cuatro modalidades de IM. Las IM-TCA fueron las más frecuentes y las hipocondríacas las menos, pero las más molestas. Todas las IM mantuvieron relaciones entre sí, tanto en frecuencia como en molestia, y todas se asociaron con las medidas clínicas de TOC, TDC, AE-H y TCA.
Conclusiones
Las IM son una experiencia habitual en diferentes contextos culturales y operan de modo transdiagnóstico en trastornos clínicamente distintos.
Palabras clave: Trastornos del espectro obsesivo-compulsivo, Estudio transcultural, Intrusiones mentales no deseadas, Transdiagnóstico, Estudio transversal
Unwanted mental intrusions (UMIs) are discrete, undesired, and unexpected cognitive events that are consciously experienced in the form of thoughts, images, sensations, and impulses. They interfere with the normal flow of thoughts, tend to be recurrent, and promote subjective resistance efforts (Clark & Rhyno, 2005). Like worry and rumination, UMIs are a modality of maladaptive conscious thought processes, although there are subtle but important differences among them. Worry has been defined as “a chain of thoughts and images, negatively affect-laden and relatively uncontrollable” (Borkovec, Robinson, Pruzinsky, & Depree, 1983, p. 10), and rumination has been defined as “the tendency to repetitively analyze one's problems, concerns, and feelings of distress without taking action to make positive changes” (Nolen-Hoeksema & Watkins, 2011, p. 596). The content of rumination tends to be more past-oriented than the content of either worry or unwanted intrusive thoughts (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). Moreover, although the three thought modalities are highly uncontrollable, individuals have a stronger desire to engage in neutralizing behaviors in response to unwanted intrusive thoughts than in response to either worry or rumination (Fergus, 2013). Wahl, van den Hout, and Lieb (2019) showed that when individuals are instructed to ruminate on an idiosyncratic UMI, they have stronger urges to be engaged in neutralization efforts, compared to those who engage in rumination on negative mood. Finally, although worry, rumination, and UMIs were initially proposed as typically occurring in Generalized Anxiety Disorder, Depression, and OCD and related disorders, respectively, they are currently thought to be transdiagnostic across several different disorders in which anxiety and negative mood states are prominent.
Regarding UMIs, current cognitive models of Obsessive-Compulsive Disorder (OCD) postulate that those with obsessive content (e.g., concerning injury/harm, religion, sexuality, contamination, doubt, scrupulosity, relationships, etc.) constitute the “normal” variants of clinically significant obsessions (Clark & Radomsky, 2014). A corollary of this assumption is that obsessive UMIs should be experienced by the vast majority of people. Therefore, they would be a normative, common cognitive conscious experience that occurs independently of the cultural and/or social context. The research has supported this. Radomsky et al. (2014) found that in 13 countries across 6 continents, the majority of nonclinical individuals (93.6%) reported experiencing UMIs with obsessional content. In the same sample, Moulding et al. (2014) observed that, although there were differences in the overall rates of these intrusive thoughts across sites, the relationships between their frequency and the meanings people attributed to them did not differ among the participants. These findings showed, first, that obsessional intrusive thoughts are highly prevalent in the nonclinical population and that these cognitive phenomena are experienced regardless of nationality, religion, or culture. Second, they support the applicability of the cognitive model of OCD to different cultures, that is, the generalizability of a Western-derived psychological model to non-Western cultures.
Even though most of the research on UMIs has been conducted on obsessional contents, UMIs have been described as occurring in other disorders, such as Body Dysmorphic Disorder (BDD; Giraldo-O’Meara & Belloch, 2017, 2018; Onden-Lim & Grisham, 2014), Health/Illness Anxiety-Hypochondriasis (IA-H; Arnáez et al., 2017, Fergus, 2013, Muse et al., 2010), and Eating Disorders (EDs; Belloch et al., 2016, Blackburn et al., 2012, García-Soriano et al., 2014, Halmi et al., 2003). Onden-Lim and Grisham (2014) found that up to 84% of non-clinical community individuals had intrusive images with similar contents to those reported by BDD patients. Giraldo-O’Meara and Belloch (2018) found similar results in community participants and in patients with BDD, thus supporting the universality and dimensionality of dysmorphic UMIs from normalcy to psychopathology. Regarding hypochondriasis, Muse et al. (2010) showed that patients with hypochondriasis experienced distressing intrusive images and thoughts about illnesses and death with a high frequency. In studies with non-clinical community individuals, Arnáez et al. (2017) found that UMIs related to illnesses and death were also common, and Fergus (2013) reported that these intrusive cognitions shared unique relations with health anxiety after accounting for negative affect. With regard to EDs, data from several studies (e.g., Avargues-Navarro et al., 2017, Belloch et al., 2016, Blackburn et al., 2012, García-Soriano et al., 2014, Halmi et al., 2003) indicate that both patients with EDs and non-clinical community individuals experience recurrent cognitions in the form of thoughts, images, and impulses about food, diet, physical exercise, and appearance. Taken together, all the above-mentioned studies support the notion expressed by Clark and Rhyno (2005) that the experience of UMIs “can encompass any topic...that is pertinent to the individual or situation at hand” (p.3). From this perspective, UMIs can be said to be a transdiagnostic factor operating across different clinical disorders and, accordingly, may be a universal experience free from cultural and/or social influences.
Nonetheless, with the exception of OCD-related intrusions, the studies about UMIs related to BDD, IA-H, and EDs have been conducted in single cities in Europe and Australia. Consequently, these studies did not explore whether the four UMI contents are universally experienced and cause comparable levels of disturbance across different cultures. This was the primary aim of the current study.
A second aim was to test whether UMIs might be a transdiagnostic factor operating across different clinical disorders such as OCD, BDD, IA-H, and EDs, given that transdiagnostic approaches to psychopathology seek to identify fundamental and/or core processes and constructs underlying diverse disorders (e.g., Nolen-Hoeksema & Watkins, 2011). To date, the published research has separately studied the four different intrusive-cognition contents in both non-clinical and clinical samples, but without examining whether the frequency and distress associated with the experience of one specific UMI content correlate with the distress and frequency of other UMI contents. This approach seems to be more adequate to ascertain whether UMI could operate transdiagnostically across the four sets of disorders and then be a vulnerability factor to the development of mental disorders such as OCD, BDD, HYP, and EDs. To explore this, we sought to examine the experience of the UMIs with contents related to these disorders in the same individual.
Method
Participants
A sample of 1,473 participants in 10 cities in seven countries and three continents volunteered to participate in the current study. The sites were located in the Middle East (Herzliya, Tel Aviv in Israel; Ankara in Turkey; and Tehran in Iran), Europe (Firenze and Padova in Italy; Algarve in Portugal; Valencia and Madrid in Spain), and South America (Buenos Aires in Argentina). Of the total sample, 74% participants (N= 1,086) were women, and 26% (n= 387) were men (χ2= 331.705, p<.0001). Their ages ranged from 18 to 64 years (M= 28.09, SD= 11.24 years), with the Israeli and Argentinian participants being the oldest, whereas the Italian, Iranian, and Turkish participants were the youngest (F6, 1458 =142.95, p< .0001). The majority of the participants in all the countries had university studies. See Table 1 for additional participant characteristics.
Table 1.
Demographic information by site.
| Continent | Country | Age M (SD) |
Gender % Female |
Education: % University studies |
n |
|---|---|---|---|---|---|
| Mediterranean Europe | Spain | 28.10 (10.25)a | 70.9a | 77.8 | 326 |
| Portugal | 30.58 (12.14)a | 68.6a | 64.7 | 255 | |
| Italy | 22.06 (2.37)b | 70.3a | 61.6 | 209 | |
| Middle-East Asia | Iran | 22.63 (4.38)b | 70.9a | 100 | 55 |
| Israel | 40.79 (12.52)c | 48.6b | 72.4 | 105 | |
| Turkey | 21.54 (4.50)b | 86.1c | 92.6 | 366 | |
| South America | Argentina | 40.70 (11.22)c | 81.5ac | 79.6 | 157 |
| Overall | 28.09 (11.12) | 73.7 | 78.3 | 1473 |
Note. Values which share the same superscript letter were not significantly different from each other. Differing superscript letters indicate post-hoc between-groups differences (Bonferroni).
Instruments
Socio-demographic data sheet. The data required were the following: age, gender, years of education, marital status, and socio-economic level. Two additional questions about the participants’ current mental-health status were also included.
For the self-report questionnaire measures that follow, published translations with established norms were used.
Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002). This is an 18-item self-report questionnaire that assesses distress associated with obsessive-compulsive symptoms (washing, checking, ordering, obsessing, hoarding, and neutralizing). The total score ranges from 0 to 72, and in this study, the Cronbach's α was .91.
Body Dysmorphic Disorder Questionnaire (BDDQ; Phillips, Atala, & Pope, 1995). This screening measure for BDD can be completed either as a self-report or by an interviewer. In this study, the BDDQ was applied as a self-report questionnaire. It includes 11 items with various response formats. The internal consistency in this study was α= .76.
Whiteley Index (WI; Pilowsky, Spence, Cobb, & Katsikitis, 1984). This self-report was one of the first dimensional measures developed to assess health anxiety and its items are based on clinicians’ experiences of illness characteristics of severe health anxiety or hypochondriasis. It contains 14 True/False items yielding a total score range of 0–14. In this study, the reliability value was α= .94 (total score).
Eating Attitudes Test (EAT-26; Garner, Olmsted, Bohr, & Garfinkel, 1982). This self-report assesses attitudes and behaviors related to EDs. The total score measures symptom severity. Internal consistency in the current study was α= .91.
Questionnaire of Unpleasant Intrusive Thoughts (QUIT). The QUIT is a newly developed measure. A preliminary Spanish version of the QUIT was designed on the basis of previously validated self-report questionnaires that assess OCD-related intrusions (García-Soriano, Belloch, Morillo, & Clark, 2011), BDD-related intrusions (Giraldo-O’Meara & Belloch, 2017, 2018), hypochondriasis or illness and death-related intrusions (Arnáez et al., 2017), and EDs-related intrusions (Belloch et al., 2016). The most frequent and disturbing mental intrusions experienced by non-clinical and clinical individuals in the aforementioned studies were selected for inclusion in the QUIT. All these self-report instruments follow the structure of the Revised Obsessional Intrusions Inventory (ROII; Purdon & Clark, 1993) and the International Intrusive Thoughts Interview Schedule (IITIS; Clark et al., 2014, Moulding et al., 2014, Radomsky et al., 2014), which assess the frequency of UMIs with obsessional contents as well as their functional consequences. Pilot studies of the QUIT were conducted in Spanish and Portuguese community samples (n= 438; Pascual-Vera and Roncero, 2017, Pascual-Vera and Belloch, 2018a, Pascual-Vera and Belloch, 2018b) and in Turkish university students (n=259; Akin & Inozu, 2018).
Similar to the ROII, the QUIT starts with a detailed definition of UMIs and the different ways they can be experienced (i.e., as images, thoughts/doubts, impulses, or physical sensations). After the initial description, four separate sets of intrusions are presented: Obsessional-related (OCD-related; 12 items), appearance defect-related (BDD-related; 9 items), illness and death/hypochondriasis-related (IA-H-related; 10 items) and eating disorders-related (EDs-related; 8 items). Respondents must evaluate each intrusion from a set on its frequency (from 0= never, to 6= always, frequently throughout the day) and the discomfort (from 0= not at all, to 4= extremely disturbing) it produces when it occurs. The number and frequency of UMIs reported by the participant in each set were computed as the average frequency of the intrusions actually experienced by the respondent at least once in his/her lifetime; that is, the total scores for each set were divided by the number of items with a frequency ≥ 1. Internal consistency of the four UMI contents were between good and excellent in terms of their frequency and disturbance across the different countries (Table 2).
Table 2.
Internal consistency (Cronbach's alpha) of the QUIT scores across countries.
| Country | OCD-related intrusions |
BDD-related intrusions |
IA/H-related intrusions |
EDs-related intrusions |
||||
|---|---|---|---|---|---|---|---|---|
| F | D | F | D | F | D | F | D | |
| Spain | .84 | .83 | .90 | .89 | .90 | .92 | .88 | .90 |
| Portugal | .80 | .85 | .89 | .90 | .87 | .90 | .88 | .90 |
| Italy | .83 | .87 | .89 | .91 | .89 | .91 | .88 | .89 |
| Iran | .85 | .81 | .87 | .91 | .87 | .84 | .84 | .89 |
| Israel | .92 | .91 | .93 | .93 | .94 | .92 | .92 | .93 |
| Turkey | .79 | .81 | .91 | .90 | .88 | .90 | .92 | .90 |
| Argentina | .89 | .91 | .92 | .95 | .91 | .94 | .92 | .92 |
Note. OCD: Obsessive-compulsive Disorder; BDD: Body Dysmorphic Disorder; IA-H: Illness Anxiety/Hypochondriasis; EDs: Eating Disorders. F= Frequency; D= Disturbance.
Procedure
Participants were recruited by the authors in each site from several sources: undergraduate students who attended their lectures at the University, advertisements on the University Campus, and the web page of each research group, requesting voluntary participation in a study on values and beliefs about thoughts. Those who explicitly agreed to participate and provided informed written consent were scheduled to attend an assessment session. In this session, the booklet containing the self-report instruments was administered to groups of 25-35 individuals in the presence of one of the authors. A common data template was created to enter the same labels and categories across sites. The research protocol was approved by the research ethics boards of each research site.
Data cleaning and missing data
Having diagnosed mental health problems in the past six months, undergoing psychological or pharmacological treatment (criterion a), or not being in the 18-to-65 age range (criterion b) were non-inclusion criteria. A total of 123 individuals (criterion a n = 108; criterion b n = 15) were not included in the data analyses.
Data analyses
One-factor ANOVAs were used to examine the mean number of intrusions experienced by site. Post-hoc tests were also computed using a T3 Dunnett correction for post-hoc analyses. The frequency and disturbance with which the four UMI were experienced across the seven countries were examined using two different two-way mixed MANOVAs. The within-subjects factor was the content of the UMI (4 levels), and the between-groups factor was the site of the participants (7 levels), with the dependent variable being the frequency or the disturbance. These analyses were performed with the Huynh-Feldt correction because Mauchly's tests of sphericity were violated. To explore the transdiagnostic nature of UMIs, Spearman correlations were calculated of the frequency and disturbance caused by the four UMI contents, as well as the UMIs and symptom measures of the different disorders. To overcome the difficulties in interpreting the results, given the different sample sizes across sites, Cohen's (1988) criteria were used to evaluate the significance of the correlations: large correlations are defined as those ≥.50, medium correlations are from .30 to .49, and small correlations are .10 to .29. Additionally, differences in correlations were tested using Fisher's r to z transformation.
Results
Prevalence of the four UMI content areas
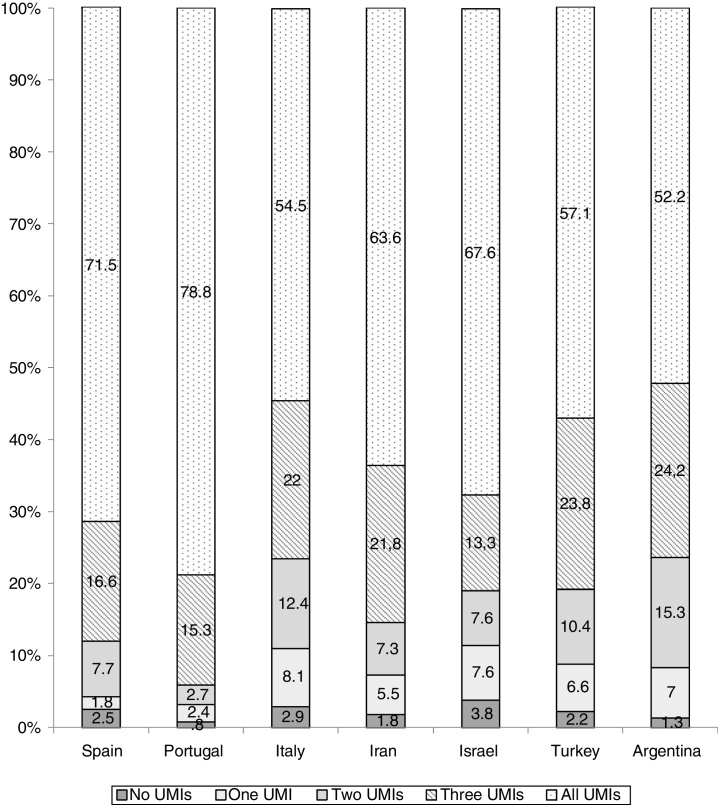
Overall, 64.2% (n = 945, Mage = 27.74, SD = 10.95; 73% women) of the sample reported having experienced the four sets of UMI once or more in their lives (see Figure 1 for a breakdown by site). Furthermore, 2% (n = 31) of the participants did not experience any UMIs, and 5% (n = 75) reported having only one UMI modality or content. The percentage rates of participants who experienced the four UMI modalities differed across countries (χ2 = 78.349, p < .0001). Between-group comparisons showed that the highest rates of participants who experienced the four UMIs were from Portugal and Spain, whereas the lowest rate was from Argentinian participants.
Figure 1.
Percentage rates of the experienced unwanted mental intrusions content- numbers by site.
The number of UMIs from the four sets experienced differed across countries (see Table 3). Participants from Italy and Israel experienced fewer OCD-related intrusions than individuals from the other countries, whereas the number of BDD-intrusions was higher among Portuguese and Turkish participants. The IA-H intrusions were the least endorsed by Italian and Argentinian participants, but Spanish, Portuguese, Iranian, and Israeli individuals endorsed a similar number of these intrusions. Finally, Spanish, Portuguese, and Israeli participants endorsed EDs-related intrusions more, but Italian participants reported the smallest number of these UMIs. In the full data set, participants endorsed up to 57% of OCD-related, 50% of BDD-related, 46% of IA-H-related, and 51% of EDs-related intrusions.
Table 3.
Number of unwanted mental intrusions endorsed by country.
| Country | OCD intrusions (range 0-12) |
BDD intrusions (range 0-9) |
IA/H intrusions (range 0-10) |
EDs intrusions (range 0-8) |
|---|---|---|---|---|
| Spain | 7.24 (3.09)a | 4.84 (3.08)a | 5.19 (3.29)a | 4.56 (2.62)a |
| Portugal | 6.98 (2.70)a | 4.93 (2.90)b | 5.90 (3.11)a | 4.92 (2.49)a |
| Italy | 5.41 (2.93)b | 4.08 (2.84)a.c | 3.03 (2.88)c | 2.95 (2.60)c |
| Iran | 7.29 (3.29)a | 4.81 (2.79)a | 5.63 (2.90)a | 3.80 (2.44)a.b |
| Israel | 5.23 (6.64)b | 3.80 (3.18)a.c | 5.43 (3.52)a | 4.22 (2.92)a |
| Turkey | 7.24 (3.09)a | 4.99 (3.17)b | 4.28 (3.30)b | 3.75 (3.03)b |
| Argentina | 6.95 (3.04)a | 3.19 (3.19)c | 3.57 (3.18)b.c | 3.65 (2.64)b |
| F6.1472 | 16.157* | 9.528* | 22.646* | 13.409* |
| η2 | .062 | .037 | .084 | .052 |
Note. *p ≤ .001. Data are Means (SD). Values which share the same superscript letter were not significantly different from each other. Differing superscript letters indicate post-hoc differences (T3 Dunnett correction for 7 post-hoc analyses – 1 per site). OCD: Obsessive-compulsive Disorder; BDD: Body Dysmorphic Disorder; IA-H: Illness Anxiety/Hypochondriasis; EDs: Eating Disorders.
Differences in the frequency and disturbance caused by the OCD, BDD, IA-H, and EDs-related mental intrusions in the participants from the different countries
The MANOVA results showed main effects for country (F6,938 =14.84, p≤.001; η2=.087) and for the frequency of the four UMI categories (F2.77, 2602 =62.26, p≤.001; η2=.062). Moreover, an interaction effect between the category of the UMI contents and the sample location on frequency was also observed, indicating that the pattern of UMI frequencies differed between sites (F16.64, 2602=5.801, p≤.001; η2=.036). Table 3 shows which countries were significantly different from each other in the frequency of the four sets of UMI. Between-group comparisons (i.e., country of the sample) indicated that Iranian and Turkish participants endorsed the highest mean frequency of OCD-related intrusions, whereas Israeli participants endorsed the lowest frequency. Post-hoc analyses indicate that both Italian and Argentinian participants experienced OCD-related intrusions with a frequency similar to that of the Israeli participants. By contrast, in every site, the BDD-related intrusions were experienced with the same frequency, with the exception of Turkish individuals, who reported higher rates of dysmorphic-related intrusions. In the case of hypochondriacal intrusions, Iranian participants reported the highest frequency, and Italian participants the lowest. Finally, Turkish participants experienced EDs-related intrusions more frequently than the Israeli and Italian participants, who did not differ in their respective rates of EDs-UMI frequency.
At the within-group comparison level (i.e., UMI content), the results indicate that the four UMIs were experienced with different rates of frequency across countries. Overall, the EDs intrusions were the most frequently experienced, whereas the IA-H-related intrusions were the least frequent. No differences were observed between the frequency of the OCD and BDD intrusions. Regarding the specific location of the sample, some similarities and differences emerged: Spanish, Israeli, Argentinian, and Italian participants experienced OCD intrusions and EDs-related intrusions with similar frequency, and Iranian participants experienced all the UMIs with similar frequency, regardless of their respective contents.
Regarding the discomfort caused by the UMI, the MANOVA produced main effects for both the sample site (F6, 681=9.77, p≤.001, η2 =.079) and the disturbance caused by the four UMIs (F2.73, 1865 = 9.08, p≤.001; η2 =.013), with an interaction effect between disturbance and site (F16.43, 1865 =5.63, p≤.001; η2 =.047). Between-group comparisons (see Table 4) showed both similarities and differences in the discomfort caused by the four types of UMIs across countries. On the whole, the OCD-related intrusions were endorsed as the most disturbing for Portuguese participants, whereas the BDD-related intrusions were similarly disturbing across sites, with the exception of Israeli participants, who experienced the lowest rates of discomfort. Spanish, Portuguese and Iranian participants reported the greatest discomfort when having IA-H-related intrusions, whereas Israelis and Argentinian participants reported the least. Similarly, Spanish, Portuguese and Iranian participants reported the greatest discomfort with the EDs-related intrusions, whereas Turkish participants reported the least. No differences were observed in the discomfort caused by EDs-related intrusions across the other sites.
Table 4.
Differences in the frequency and disturbance of four sets of mental intrusions across countries.
| Location of sample | Frequency of mental intrusions | Disturbance due to mental intrusions | ||||||
|---|---|---|---|---|---|---|---|---|
| OCD | BDD | IA-H | EDs | OCD | BDD | IA-H | EDs | |
|
Spain (frequency: n=233; disturbance: n=157) |
2.26 (0.77)ac/1 |
2.14 (0.99)a/1 |
1.83 (0.87)b/1 |
2.36 (1.04)c/1 |
1.99 (0.59)a.b/1 |
1.97 (0.78)a/1 |
2.15 (0.91)b/1 |
1.93 (0.80)a/1 |
| Portugal (frequency: n=201; disturbance: n=161) |
2.24 (0.71)a/1 |
2.13 (0.94)ab/1 |
1.97 (0.82)b/1 |
2.59 (1.06)c/1.3 |
2.16 (0.69)a/2 |
1.99 (0.84)b/1 |
2.39 (0.90)c/1 |
2.00 (0.87)ab/1 |
| Italy (frequency: n=114; disturbance: n=90) |
2.06 (0.78)a/13 |
1.99 (0.88)a/1 |
1.54 (0.59)b/3 |
2.13 (0.96)a/2 |
1.90 (0.70)a/3 |
1.91 (0.76)a/1 |
1.94 (0.87)a/2 |
1.75 (0.79)a/2 |
| Iran (frequency: n=35; disturbance: n=26) |
2.76 (0.97)a/2 |
2.37 (1.17)a/1.2 |
2.79 (1.27)a/2 |
2.66 (1.56)a/1.2.3 |
2.01 (0.63)a/1.2.3 |
1.90 (0.85)a/1.2 |
2.28 (0.97)a/1 |
1.95 (0.90)a/2 |
| Israel (frequency: n=71; disturbance: n=54) |
1.85 (0.77)ab/3 |
1.77 (0.82)a/1 |
1.76 (0.75)a/1 |
2.12 (0.98)b/2 |
1.49 (0.46)a/3 |
1.47 (0.63)a/2 |
1.55 (0.55)a/3 |
1.66 (0.68)a/2 |
| Turkey (frequency: n=209; disturbance: n=133) |
2.57 (0.74)a/2 |
2.57 (1.04)a/2 |
1.82 (0.73)b/1 |
2.82 (1.20)c/3 |
2.01 (0.55)a/1 |
1.99 (0.72)a/1 |
2.03 (0.78)a/2 |
1.52 (0.58)b/2.3 |
| Argentina (frequency: n=82; disturbance: n=67) |
1.97 (0.82)ac/1.3 |
1.78 (0.87)ab/1 |
1.57 (0.88)b/1.3 |
2.22 (1.12)c/1 |
1.65 (0.63)a/3 |
1.73 (0.86)a/1.2 |
1.57 (0.68)a/3 |
1.81 (0.87)a/2 |
Note. Data are Mean (SD). Values which share the same superscript were not significantly different from each other. Superscripts a.b.c indicate post-hoc within-group (UMIs content) differences (Bonferroni). Superscripts 1.2.3 indicate post-hoc among location differences (same UMI content) (Bonferroni). Same superscript means no differences.
OCD: Obsessive-compulsive Disorder; BDD: Body Dysmorphic Disorder; IA/H: Illness Anxiety/Hypochondriasis; EDs: Eating Disorders.
At the within-group comparison level (i.e., UMI content), the four UMI types provoked different disturbance levels in the participants from the different sites. The four UMIs provoked a similar degree of disturbance, regardless of their content, in Iranian, Israeli, Argentinian, and Italian participants, whereas the IA-H-related intrusions caused more distress than the BDD-related and EDs-related intrusions in Spanish participants. The IA-H-related intrusions were also the most disturbing to the Portuguese participants, but Turkish participants experienced similar disturbance when experiencing OCD, BDD and IA-H-related intrusions, whereas EDs-related intrusions disturbed them less.
Relationships between the frequency and disturbance caused by obsessional, dysmorphic, hypochondriac, and EDs-related unwanted intrusions
In each site, the four sets of UMI were associated in terms of both their frequency (r range from .32 to .70; all p's≤.01) and disturbance (r range from .26 to .71; all p's≤.01). For the UMIs’ frequency, the largest coefficients were found between BDD and EDs intrusions in Spain (r= .58), Portugal (r=.47), Iran (r=.63), and Italy (r=.57), and between OCD and BDD intrusions in Israel (r=.70) and Turkey (r=.53), whereas in Argentina the largest coefficient was between OCD and IA-H intrusions (r=.60). By contrast, the smallest coefficients were observed between IA-H and EDs intrusions in all countries (r range from .32 to .48). Regarding the discomfort caused by the UMIs, the largest coefficients were observed between BDD and EDs intrusions in Spain (r=.63), Iran (r=.63), Israel (r=.71), Turkey (r=.51) and Italy (r=.70), and between BDD and IA-H intrusions in Argentina (r= .56) and Portugal (r=.50). Although remaining statistically significant (p≤.05), the smallest correlations were between IA-H and EDs intrusions in Spain (r=.26), Portugal (r=.33), Israel (r=.39), Argentina (r=.30), and Turkey (r=.19), and between OCD and EDs intrusions in Iran (r=.42) and Italy (r=.52).
Relationships among the frequency and discomfort provoked by UMIs and symptom measures of the different disorders
Table 5 shows the associations between the frequency and discomfort due to the UMIs and symptom measures of OCD, BDD, Hypochondriasis and EDs. Each set of UMIs correlated with its corresponding clinical measure on both the frequency and discomfort scores. Moreover, cross-associations were also found between the frequency and the disturbance caused by the four UMIs and their non-specific clinical measures (i.e., OCI-R and frequency of BDD-related intrusions). The largest coefficients were found between the OCI-R score and the frequency of OCD-related intrusions, and between the clinical measure of BDD and the frequency of EDs intrusions. The smallest coefficients were observed for the relationship between the WI and both the disturbance caused by IA-H-related intrusions and the frequency of BDD-related intrusions.
Table 5.
Correlations between the UMIs frequency and discomfort with symptom measures.
| OCD intrusions |
BDD intrusions |
IA/H intrusions |
EDs intrusions |
Symptom measures |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency | Disturb. | Frequency | Disturb. | Frequency | Disturb. | Frequency | Disturb. | OCI-R | BDDQ | WI | EAT-26 | ||
| OCI-R | r | .55** -- |
.43** -- |
.43** .30** |
.33** .24** |
.31** .24** |
.27** .07 |
.40** .35** |
.226** .04 |
1 | |||
| n | 761 | 713 | 633 | 591 | 662 | 614 | 638 | 492 | 808 | ||||
| BDDQ | r | .39** .31** |
.24** .49** |
.41** -- |
.25** -- |
.28** .37** |
.10 .07 |
.57** .49** |
.41** .31** |
.32** | 1 | ||
| n | 125 | 117 | 116 | 112 | 117 | 106 | 126 | 121 | 132 | 132 | |||
| WI | r | .19** .14** |
.01 .14* |
.10** .18** |
.03 .11* |
.27** -- |
.10* -- |
.07 .05 |
.00 .05 |
.22** | .20* | 1 | |
| n | 734 | 689 | 609 | 571 | 636 | 591 | 615 | 472 | 776 | 132 | 783 | ||
| EAT-26 | r | .26** .34** |
.19** .26** |
.35** .43** |
.26** .35** |
.31** .34** |
.17** .22** |
.45** -- |
.46** -- |
.27** | .37** | .30** | 1 |
| n | 710 | 666 | 588 | 550 | 612 | 571 | 593 | 451 | 749 | 754 | 732 | 119 | |
Note. * p ≤ .05 ** p ≤ .01. The coefficients in italics correspond to partial correlations. Disturb.: Disturbance due to UMIs. OCI-R: Obsessive-Compulsive Inventory-Revised; BDDQ: Body Dysmorphic Disorder Questionnaire; WI: Whiteley Index; EAT-26: Eating Attitudes Test. OCD: Obsessive-compulsive Disorder; BDD: Body Dysmorphic Disorder; IA/H: Illness Anxiety/Hypochondriasis; EDs: Eating Disorders.
The correlation coefficients between the frequency of OCD intrusions and the OCI-R scores were significantly higher than the correlations observed between the OCI-R and the frequency of BDD intrusions (z=2.83, p=.002) and EDs intrusions (z=3.58 p=.001). By contrast, the association between the frequency of BDD intrusions and the BDDQ was smaller than the association observed between the BDDQ and the frequency of EDs intrusions (z=1.68, p=.04). Regarding IA-H intrusions, the correlation between the WI and the frequency of these intrusions was higher than the association between the WI and the frequency of BDD intrusions (z=3.06, p=.001). Finally, the correlation coefficient between the EAT-26 and the frequency of EDs intrusions was significantly higher than the associations found between the EAT-26 and the frequency of OCD intrusions (z=3.38, p=.001), BDD intrusions (z=2.09, p=.01), and IA-H intrusions (z=2.79, p=.001).
To test for specificity, partial correlations were also calculated examining whether each of the four UMI sets was related to the symptom measures, by partialling-out its corresponding symptom measure (e.g., correlations between OCD intrusions and symptom measures when controlling for OCD symptoms; correlations between BDD intrusions and symptoms measures controlling for BDD symptoms, etc.). As Table 5 shows, the pattern of relationships was comparable to the one observed without partialling out the symptom measures, with some minor exceptions for the WI, which was related to the disturbance caused by the OCD and BDD intrusions. The four self-report questionnaires assessing the symptoms were correlated, with small to medium coefficients.
Discussion
This study aimed to examine for the first time two key inter-related issues about four different contents of unwanted mental intrusions: first, their universality across different cultural and social contexts, and second, their putative transdiagnostic value.
To date, the universality of UMIs and the differences in their expression depending on the cultural and social context have only been examined in the case of OCD-related intrusions (Clark et al., 2014, Moulding et al., 2014, Radomsky et al., 2014). Our findings showed that more than half of the participants in the seven countries involved in the study reported having had the four types of UMI contents. Furthermore, it was more common for participants to experience more than one UMI than to experience only one, which suggests that the propensity to have UMIs, regardless of their content, is a source of individual differences. This propensity might help to explain, at least in part, the comorbidities among disorders where UMIs play a key role; that is, the tendency to have unwanted intrusions may be a common vulnerability factor that comes into play in a number of disorders.
There were both similarities and differences across the sites in terms of the frequency and disturbance caused by the OCD, BDD, IA-H, and EDs-related mental intrusions. Overall, Iranian and Turkish participants showed the highest frequency on all the UMIs, whereas Spanish and Portuguese participants reported the most discomfort associated with the four UMIs. By contrast, Argentinian, Israeli, and Italian participants experienced the lowest frequencies and least discomfort. As such, whereas the UMIs were experienced similarly across sites, we can suggest that there were three patterns of responses across countries: the first includes Iranian and Turkish individuals, the second involves Portuguese and Spanish subjects, and the third affects participants from Argentina, Israel, and Italy. We cannot know whether these patterns reflect deeper socio-cultural factors because we did not include specific culturally-relevant constructs that would allow us to make culturally-specific predictions. Nonetheless, some reasons for the three observed patterns in the participants’ responses can be tentatively suggested. For example, the individuals in the first group (Iran and Turkey) share Muslim values that are not prevalent in the other countries that participated in the study. Islamic rules are a determinant of self-identity and everyday life, and mental intrusions about following certain rules while praying in a near-ritualistic manner, or about the need to maintain a high degree of mental and physical purity, could explain the observed similarities between the participants from these two countries (Shams, 2018).
The association between obsessional symptoms and religiosity has been noted in studies performed in Middle-Eastern countries. Religious obsessions are predominant in these samples, compared to their low prevalence in the rest of the continents, as were checking and cleaning compulsions (e.g., Fontenelle et al., 2004, Okasha, 2004). Karadag, Oguzhanoglu, Özdel, Ateşci, and Amuk. (2006) observed that Egyptians, who live in a predominantly Muslim society, reported a high degree of egodystonicity related to checking and cleaning compulsions, which might result from culturally bounded religious practices that emphasize cleanliness and purity. Similarly, Yorulmaz, Yilmaz, and Gençöz (2004) showed that Turkish individuals experienced more morality thought-action fusion beliefs than what was reported in other nations, which might be a reflection of Turkish culture as well as a concept of morality linked to religious values. Nonetheless, given that the Iranian and Turkish participants in our study were among the youngest participants in the entire sample, the role of age in our findings cannot be ruled out. In the case of Spanish and Portuguese participants, the similarities could be explained by the fact that they shared not only the same geographical space in past centuries, but also that they have a common history that includes Christian Catholic religion and values. Again, age could be a factor because participants from these two countries were in a similar age range. Regarding the third group (Argentina, Israel, and Italy), the similarities between Argentinian and Israeli participants could have to do with age because participants from these countries were the oldest members of the entire sample. However, contradicting this suggestion, the Italian participants were among the youngest. Thus, other reasons related to the immigration of Italian individuals to Argentina, especially in the 19th century, and Israel could lie behind the similarities among the participants from these three countries.
On the whole, the study findings showed more similarities than differences across sites with respect to the occurrence and related disturbance of the four UMI types examined. The findings suggest that experiencing UMIs is quite common, regardless of their specific contents and the nationality or cultural context. Additionally, age differences among the samples, rather than cultural variables, could explain some of the observed differences. In any case, our results about the universality of UMIs agree with studies indicating that the disorders with which they are related, OCD, BDD, Hypochondriasis, and EDs, are present in almost every culture and social context, with only slight differences in their respective prevalence rates (i.e., Eli and Warin, 2018, Nedeljkovic et al., 2012). From this perspective, the data on EDs-related intrusions as the most frequently experienced across the different countries agree with perspectives of Anorexia Nervosa as a Western ‘culture-bound syndrome’ transportable to other cultures through a “westernization” process. For example, Cheney (2011) argued that, among young US women from immigrant backgrounds, thinness becomes an emblem of “whiteness”, such that a disordered eating pattern is viewed as a means to improve social relationships, mobility, and power.
The second aim of the study was to examine the putative transdiagnostic nature of UMIs. We focused on four specific contents, OCD, BDD, IA-H, and EDs-related, because of the phenomenological similarities of the disorders with which they are associated. These similarities include higher comorbidity rates than what would be expected by chance, analogous cognitive explanatory models for each disorder, comparable response to similar treatments, and similar ages of onset. The four disorders also share the experience of UMIs, which might be instigators of their respective clinical symptoms and/or of rumination on their presence and the associated negative causes and consequences (Wahl et al., 2019). Our findings showed close relationships among the four UMI types, both in the frequency of appearance and in the discomfort they caused. These results support the notion that having a disturbing UMI about a specific theme or content is associated with having disturbing UMIs about other different contents, suggesting that the tendency or propensity to experience UMIs related to OCD, BDD, IA-H, and EDs could be a vulnerability factor for these disorders (Pascual-Vera et al., 2017). The associations between BDD and OCD-related intrusions and between BDD and EDs-related intrusions suggest that a complex network of relationships exists between the disorders in which the UMIs play a key role. The current psychiatric diagnostic systems based on categorical rather than dimensional and network (i.e., Borsboom, 2017) perspectives, which exclude or minimize the search for shared psychopathological aspects underlying different clinical manifestations, are unable to adequately explain these relationships that are commonly observed in clinical practice. For example, as Halmi et al. (2003) suggested in their study about OCD symptoms in patients with Anorexia Nervosa (AN), some common phenotype characteristics shared by most AN and OCD patients suggest that these disorders may share common brain behavioral pathways.
The relationship between the frequency and discomfort provoked by the four UMI types and the respective symptom measures of OCD, BDD, Hypochondriasis, and EDs was an expected result. Nonetheless, we found that these clinical measures were also correlated with the frequency of all the UMI types, regardless of their specific content, with the only exception of the Whiteley Index, which was associated with the frequency of OCD and BDD intrusions, but not with the EDs-related ones. The association found between the Whiteley Index and the frequency of both OCD and BDD-related intrusions supports the inclusion of Hypochondriasis in the obsessive-compulsive spectrum disorders (Kogan et al., 2016, Stein et al., 2016). The lack of relationships between the WI and EDs-intrusions would suggest that thoughts about the “dangers” of eating or not doing exercise in trying to reach and/or maintain a desired state of thinness are different from preoccupations about one's health status. In fact, some studies found that, unlike OCD-related intrusions, EDs-related intrusions are egosyntonic, even being viewed as positive reminders of the “right behaviors” in terms of eating habits, both for non-clinical participants and for patients with Anorexia Nervosa (Belloch et al., 2012, Belloch et al., 2016, García-Soriano et al., 2014).
Several limitations of the study should be mentioned. First, the study was designed to assess the prevalence of and disturbance caused by four UMI contents in different countries. Thus, it did not include culturally-relevant constructs to draw culturally-specific conclusions. Second, the study results rely on a questionnaire. We tried to control the possible biases associated with the uses of self-report questionnaires by designing the QUIT on the basis of previously validated self-report measures, employing highly rigorous translation and back translation, administration, coding, and data entry protocols across all sites. The difference in sample sizes across countries is another limitation. Nonetheless, it is important to note that this study includes a diverse range of non-western countries that have hardly been represented in the research. Other representative cross-cultural studies are needed to generalize results from Western-driven studies and advance our knowledge about how psychological phenomena vary across different cultural and social contexts.
Limitations notwithstanding, the present results support the universality and prevalence of unwanted mental intrusions in different content areas (obsessive, dysmorphic, hypochondriacal, and EDs-related) across a variety of countries and cultural contexts. Moreover, the data obtained refer not only to the frequency or occurrence of these intrusions, but also to the disturbance they cause, an aspect that was not previously studied and that has more importance for the possible clinical implications of UMIs than the mere determination of the presence of UMIs. The adoption of a within-subject design is an additional strength because it further supports the notion that these UMIs could operate transdiagnostically across clinically different disorders, specifically OCD, BDD, IA-H, and the EDs. Additionally, this could help us to better understand the comorbidities usually found between these disorders through the detection of individuals with an increased propensity to experience disturbing mental intrusions. Future research should specifically test the dimensionality of the four sets of UMIs, as well as their transdiagnostic nature, in clinical samples representative of the four disorders to which they are related.
Funding
This work was supported by the Spanish Ministerio de Economía y Competitividad, MINECO (Grant PSI2013-44733-R) and by the Generalitat Valenciana (GVA), Conselleria d’Educació, Cultura i Esport (Grant PROMETEO/2013/066).
References
- Akin B., Inozu M. Psychometric properties of the Turkish Form of the Questionnaire of Unwanted Intrusive Thoughts: Transdiagnostic approach in unwanted intrusive thoughts. Journal of Anatolian Psychiatry. Advanced publication online. 2018;19:55–63. [Google Scholar]
- Arnáez S., García-Soriano G., Belloch A. Hypochondriasis and illness intrusions: Development and validation of an assessment instrument. Behavioral Psychology. 2017;25:65–86. [Google Scholar]
- Avargues-Navarro M.L., Borda-Mas M., Asuero-Fernández R., Pérez-San-Gregorio M.Á., Martín-Rodríguez A., Beato-Fernández L., Bardone-Cone A.M., Sánchez-Martín M. Purging behaviors and therapeutic prognosis of women with eating disorders treated in a healthcare context. International Journal of Clinical and Health Psychology. 2017;17:120–127. doi: 10.1016/j.ijchp.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belloch A., Roncero M., Perpiñá C. Ego-syntonicity and ego-dystonicity associated with upsetting intrusive cognitions. Journal of Psychopathology and Behavioral Assessment. 2012;34:94–106. https://doi.org/10.1007/s10862-011-9255-4. [Google Scholar]
- Belloch A., Roncero M., Perpiñá C. Obsessional and eating disorder-related intrusive thoughts: Differences and similarities within and between individuals vulnerable to OCD or to EDs. European Eating Disorders Review. 2016;24:446–454. doi: 10.1002/erv.2458. https://doi.org/10.1002/erv.2458. [DOI] [PubMed] [Google Scholar]
- Blackburn J.F., Thompson A.R., May J. Feeling good about being hungry: Food-related thoughts in eating disorders. Journal of Experimental Psychopathology. 2012;3:243–257. https://doi.org/10.5127/jep.018711. [Google Scholar]
- Borboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec T.D., Robinson E., Pruzinsky T., Depree J.A. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- Cheney A.M. ‘Most girls want to be skinny”: Body (dis) satisfaction among ethnically diverse women. Qualitative Health Research. 2011;21:1347–1359. doi: 10.1177/1049732310392592. [DOI] [PubMed] [Google Scholar]
- Clark D.A., Abramowitz J., Alcolado G.S., Alonso P., Belloch A., Bouvard M., Coles M.E., Doron G., Fernández-Álvarez H., García-Soriano G., Ghisi M., Gómez B., Inozu M., Moulding R., Radomsky A.S., Shams G., Sica C., Simos G., Wong W. Part 3 - A question of perspective: The association between intrusive thoughts and obsessionality in 11 countries. Journal of Obsessive-Compulsive and Related Disorders. 2014;3:292–299. https://doi.org/10.1016/j.jocrd.2013.12.006. [Google Scholar]
- Clark D.A., Radomsky A.S. Introduction: A global perspective on unwanted intrusive thoughts. Journal of Obsessive-Compulsive and Related Disorders. 2014;3:265–268. https://doi.org/10.1016/j.jocrd.2014.02.001. [Google Scholar]
- Clark D.A., Rhyno S. Unwanted intrusive thoughts in non-clinical individuals. In: Clark D.A., editor. Intrusive thoughts in clinical disorders. Theory, research and treatment. Guilford Press; New York, NY: 2005. pp. 1–29. [Google Scholar]
- Eli K., Warin M. Anthropological Perspectives on Eating Disorders: Deciphering Cultural Logics. Transcultural Psychiatry. 2018;55:443–453. doi: 10.1177/1363461518784385. hptts://doi.org/10.1177/1363461518784385. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Huppert J.D., Leiberg S., Langner R., Kichic R., Hajcak G., Salkovskis P.M. The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment. 2002;14:485–496. https://doi.org/10.1037/1040-3590.14.4.485. [PubMed] [Google Scholar]
- Fontenelle L.F., Mendlowicz M.V., Marques C., Versiani M. Trans-cultural aspects of obsessive–compulsive disorder: A description of a Brazilian sample and a systematic review of international clinical studies. Journal of Psychiatric Research. 2004;38:403–411. doi: 10.1016/j.jpsychires.2003.12.004. https://doi.org/10.1016/j.jpsychires.2003.12.004. [DOI] [PubMed] [Google Scholar]
- Fergus T.A. Repetitive thought and health anxiety: Tests of specificity. Journal of Psychopathology and Behavioral Assessment. 2013;35:366–374. https://doi.org/10.1007/s10862-013-9340-y. [Google Scholar]
- García-Soriano G., Belloch A., Morillo C., Clark D.A. Symptom dimensions in obsessive-compulsive disorder: From normal cognitive intrusions to clinical obsessions. Journal of Anxiety Disorders. 2011;25:474–482. doi: 10.1016/j.janxdis.2010.11.012. https://doi.org/10.1016/j.janxdis.2010.11.012. [DOI] [PubMed] [Google Scholar]
- García-Soriano G., Roncero M., Perpiñá C., Belloch A. Intrusive thoughts in obsessive-compulsive disorder and eating disorder patients: A differential analysis. European Eating Disorders Review. 2014;22:191–199. doi: 10.1002/erv.2285. https://doi.org/10.1002/erv.2285. [DOI] [PubMed] [Google Scholar]
- Garner D.M., Olmsted M.P., Bohr Y., Garfinkel P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychological Medicine. 1982;12:871–878. doi: 10.1017/s0033291700049163. https://doi.org/10.1017/S0033291700049163. [DOI] [PubMed] [Google Scholar]
- Giraldo-O’Meara M., Belloch A. The Appearance Intrusions Questionnaire: A self-report questionnaire to assess the universality and intrusiveness of preoccupations about appearance defects. European Journal of Psychological Assessment. Advanced publication online. 2017 https://doi.org/10.1027/1015-5759/a000406. [Google Scholar]
- Giraldo-O’Meara M., Belloch A. Escalation from normal appearance related intrusive cognitions to clinical preoccupations in body dysmorphic disorder: A cross-sectional study. Psychiatry Research. 2018;265:137–143. doi: 10.1016/j.psychres.2018.04.047. https://doi.org/10.1016/j.psychres.2018.04.047. [DOI] [PubMed] [Google Scholar]
- Halmi K.A., Sunday S.R., Klumpp K.L., Strober M., Leckman J.F., Fichter M., Kaplan A., Woodside B., Treasure J., Berrettini W.H., Shabboat M., Bulik C.M., Kaye W.H. Obsessions and compulsions in anorexia nervosa subtypes. International Journal of Eating Disorders. 2003;33:308–319. doi: 10.1002/eat.10138. [DOI] [PubMed] [Google Scholar]
- Karadaĝ F., Oguzhanoglu N.K., Özdel O., Ateşci F.Ç., Amuk T. OCD symptoms in a sample of Turkish patients: A phenomenological picture. Depression and Anxiety. 2006;23:145–152. doi: 10.1002/da.20148. https://doi.org/10.1002/da.20148. [DOI] [PubMed] [Google Scholar]
- Kogan C.S., Stein D.J., Maj M., First M.B., Emmelkamp P.M., Reed G.M. The classification of anxiety and fear-related disorders in the ICD-11. Depression and Anxiety. 2016;33:1141–1154. doi: 10.1002/da.22530. https://doi.org/10.1002/da.22530. [DOI] [PubMed] [Google Scholar]
- Moulding R., Coles M.E., Abramowitz J.S., Alcolado G.M., Alonso P., Belloch A., Bouvard M., Clark D.A., Doron G., Fernández-Álvarez H., García-Soriano G., Ghisi M., Gómez B., Inozu M., Radomsky A., Shams G., Sica C., Simos G., Wong W. Part 2. They scare because we care: The relationship between obsessive intrusive thoughts and appraisals and control strategies across 15 cities. Journal of Obsessive-Compulsive and Related Disorders. 2014;3:280–291. https://doi.org/10.1016/j.jocrd.2014.02.006. [Google Scholar]
- Muse K., McManus F., Hackmann A., Williams M., Williams M. Intrusive imagery in severe health anxiety: Prevalence, nature and links with memories and maintenance cycles. Behaviour Research and Therapy. 2010;48:792–798. doi: 10.1016/j.brat.2010.05.008. https://doi.org/10.1016/j.brat.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nedeljkovic M., Moulding R., Foroughi E., Kyrios M., Doron G. Cultural issues in understanding and treating obsessive compulsive and spectrum disorders. In: Steketee G., editor. Oxford Handbook of Obsessive Compulsive and Spectrum Disorders. Oxford University Press; Oxford: 2012. pp. 1–66. [Google Scholar]
- Nolen-Hoeksema S., Watkins E.R. A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science. 2011;6:589–609. doi: 10.1177/1745691611419672. https://doi.org/10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Wisco B.E., Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Okasha A. OCD in Egyptian adolescents: The effect of culture and religion. Psychiatric Times. 2004;21:1–5. [Google Scholar]
- Onden-Lim M., Grisham J.R. Intrusive imagery experiences in a high dysmorphic concern population. Journal of Psychopathology and Behavioral Assessment. 2014;35:99–105. https://doi.org/10.1007/s10862-012-9318-1. [Google Scholar]
- Pascual-Vera B., Belloch A. El carácter transdiagnóstico de las intrusiones mentales: Una revisión y una propuesta basada en datos. Revista de Psicopatología y Psicología Clínica. 2018;23:135–148. doi:10.5944/rppc.vol.23.num.1.2018.18494. [Google Scholar]
- Pascual-Vera B., Belloch A. Functional links of obsessive, dysmorphic, hypochondriac, and eating-disorders related mental intrusions. International Journal of Clinical and Health Psychology. 2018;18:43–51. doi: 10.1016/j.ijchp.2017.09.001. https://doi.org/10.1016/j.ijchp.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual-Vera B., Roncero M., Belloch Are unwanted mental intrusions a transdiagnostic variable? Psicothema. 2017;29:166–171. doi: 10.7334/psicothema2016.199. https://doi.org/10.7334/psicothema2016.199. [DOI] [PubMed] [Google Scholar]
- Phillips, K.A., Atala, K.D., & Pope, H.G. (1995). Diagnostic instruments for body dysmorphic disorder. In American Psychiatric Association (Ed.), New research program and abstracts. 148th meeting of the American Psychiatric Association 157. Miami: American Psychiatric Association.
- Pilowsky I., Spence N., Cobb J., Katsikitis M. The Illness Behavior Questionnaire as an aid to clinical assessment. General Hospital Psychiatry. 1984;6:123–130. doi: 10.1016/0163-8343(84)90070-7. https://doi.org/10.1016/0163-8343(84)90070-7. [DOI] [PubMed] [Google Scholar]
- Purdon C., Clark D.A. Obsessive intrusive thoughts in non-clinical subjects Part I. Content and relation with depressive, anxious and obsessional symptoms. Behaviour Research and Therapy. 1993;31:713–720. doi: 10.1016/0005-7967(93)90001-b. https://doi.org/10.1016/0005-7967(93)90001-B. [DOI] [PubMed] [Google Scholar]
- Radomsky A.S., Alcolado G.M., Abramowitz J.S., Alonso P., Belloch A., Bouvard M., Clark D.A., Coles M.E., Doron G., Fernández-Álvarez H., García-Soriano G., Ghisi M., Gómez B., Inozu M., Moulding R., Shams G., Sica C., Simos G., Wong W. Part 1-You can run but you can’t hide: Intrusive thoughts on six continents. Journal of Obsessive-Compulsive and Related Disorders. 2014;3:269–279. https://doi.org/10.1016/j.jocrd.2013.09.002. [Google Scholar]
- Shams G. Roozbeh Hospital; Tehran: 2018. Cognitive behavior therapy: The role of culture and religion in OCD. Monthly brain, cognitive and behaviour seminar. [Google Scholar]
- Stein D.J., Kogan C.S., Atmaca M., Fineberg N.A., Fontenelle L.F., Grant J.E., Matsunaga H., Reddy Y.C.J., Simpson H.B., Thomsen P.H., van den Heuvel O.A., Veale D., Woods D.W., Reed G.M. The classification of obsessive-compulsive and related disorders in the ICD-11. Journal of Affective Disorders. 2016;190:663–674. doi: 10.1016/j.jad.2015.10.061. https://doi.org/10.1016/j.jad.2015.10.061. [DOI] [PubMed] [Google Scholar]
- Wahl K., van den Hout M., Lieb R. Rumination on unwanted intrusive thoughts affects the urge to neutralize in nonclinical individuals. Journal of Obsessive-Compulsive and Related Disorders. 2004;20:4–12. https://doi.org/10.1016/j.jocrd.2018.02.002. [Google Scholar]
- Yorulmaz O., Yilmaz A.E., Gençöz T. Psychometric properties of the thought-action fusion scale in a Turkish sample. Behaviour Research and Therapy. 2004;42:1203–1214. doi: 10.1016/j.brat.2003.08.005. https://doi.org/10.1016/j.brat.2003.08.005. [DOI] [PubMed] [Google Scholar]