Abstract
Pet treats and pet food can be contaminated with Salmonella and other pathogens, though they are infrequently implicated as the source of human outbreaks. In 2013, the New Hampshire Department of Health and Human Services investigated a cluster of Salmonella Typhimurium infections associated with contaminated locally made pet treats. Case-patients were interviewed with standardized questionnaires to assess food, animal, and social histories. Laboratory and environmental investigations were conducted, including testing of clinical specimens, implicated product, and environmental swabs. Between June and October 2013, a total of 43 ill persons were identified. Sixteen patients (37%) were hospitalized. Among 43 case-patients interviewed, the proportion exposed to dogs (95%) and pet treats (69%) in the 7 days prior to illness was statistically higher than among participants in a U.S. population-based telephone survey (61%, p < 0.0001 and 16%, p < 0.0001, respectively). On further interview, 38 (88%) reported exposure to Brand X Chicken Jerky, the maker of Brand X chicken jerky, or the facility in which it was made. Product testing isolated the outbreak strain from four of four Brand X Chicken Jerky samples, including an unopened package purchased at retail, opened packages collected from patient households, and unpackaged jerky obtained from the jerky maker. A site visit revealed inadequate processing of the chicken jerky, bare-hand contact with the finished product prior to packaging, and use of vacuum-sealed packaging, which may have enabled facultative anaerobic bacteria to proliferate. Seven (78%) of nine environmental swabs taken during the site visit also yielded the outbreak strain. Brand X Chicken Jerky was voluntarily recalled on September 9, 2013. Consumers should be made aware of the potential for locally made products to be exempt from regulation and for animals and animal food to carry pathogens that cause human illness, and be educated to perform hand hygiene after handling pet food or treats.
Introduction
Salmonella is a gram-negative bacterium that can cause gastrointestinal illness in both humans and animals (Heymann, 2008). More than 43,000 cases are reported in the United States annually, though the actual burden of illness is estimated at > 1 million cases when accounting for under-reporting, and lack of diagnosis or laboratory confirmation (Scallan et al., 2011). Most human infections of Salmonella are caused by the ingestion of contaminated food; however, pets and pet foods are an increasingly recognized source of Salmonella and cause of Salmonella infections (FDA, n.d.; Sanchez et al., 2002; CDC, 2006; Finley et al., 2006, 2008; Behravesh et al., 2010; KuKanich et al., 2011; Imanishi et al., 2014). Approximately 11% or 127,155 of the estimated annual Salmonella illnesses in the United States are thought to be attributable to animal contact (Hale et al., 2012). The proportion of illnesses specifically attributable to pet food and pet treats is unknown. Outbreaks implicating pet treats have been described; however, they are often small and geographically widespread (Clark et al., 2001; Pitout et al., 2003; CDC, 2006).
We describe a human outbreak of Salmonella enterica serotype Typhimurium (Salmonella Typhimurium) infections attributed to locally made, underprocessed chicken jerky pet treats. This outbreak investigation is noteworthy because it is the largest human outbreak of salmonellosis associated with pet treats reported in the literature. Timely patient interview, inspection of the production facility, and laboratory testing of specimens from retail, patient homes, and the production facility led to identification and recall ofthe contaminated product within 2 weeks of initiation of the outbreak investigation.
Materials and Methods
Outbreak detection
On August 20, 2013, the New Hampshire (NH) Department of Health and Human Services (DHHS) identified an increase in Salmonella Typhimurium cases with indistinguishable pulsed-field gel electrophoresis (PFGE) patterns by restriction enzymes Xbal (JPXX01.0302) and BlnI (JPXA26.0183). All isolates received in the NH Public Health Laboratories (PHL) routinely undergo PFGE and are submitted to PulseNet, a national molecular subtyping network that is used for foodborne disease surveillance. Because the PFGE patterns were common among Salmonella Typhi-murium, the initial eight isolates were sent to the U.S. Centers for Disease Control and Prevention (CDC) for further differentiation using multiple locus variable-number tandem repeat analysis (MLVA). On August 28, CDC confirmed the eight isolates were also indistinguishable by MLVA, suggesting that a local community outbreak was occurring. By August 30, the NH PHL identified 9 more patients with Salmonella Typhimurium Xbal pattern JPXX01.0302, bringing the total to 17 cases.
Case finding and investigation
A confirmed case was defined as isolation of the outbreak strain of Salmonella Typhimurium (Xbal/BlnI pattern JPXX01.0302/JPXA26.0183) from a person with illness onset between June 1,2013 and October 31,2013 and who either resided in or visited NH during the week before illness onset. A probable case was defined as diarrhea (> 3 loose stools in 24 h) in any person with illness onset between June 1, 2013 and October 31, 2013 and self-reported exposure to the implicated product or epidemiologic link to a confirmed case.
Prior to recognition of the outbreak, all salmonellosis cases were interviewed with a routine standard enteric disease questionnaire. To further generate hypotheses about possible sources of the outbreak, 13 cases were re-interviewed with a standardized hypothesis-generating questionnaire, which asked about > 200 potential exposures, including pets and pet food. Data from questionnaires were entered into a database and the frequencies of exposures among cases were compared to data for the general U.S. population collected by the CDC FoodNet program (CDC, n.d.). Frequencies, frequency comparisons, and corresponding binomial probabilities were calculated using SAS software (SAS Institute, Cary, NC). Upon identification of pet treats as a possible hypothesis for the outbreak’s source, administration of a pet treat–specific questionnaire was attempted for all cases.
Environmental investigation and traceback
Based on results of hypothesis-generating questionnaires, site visits to local pet food stores and farmers markets were conducted to identify locally made and distributed pet treats. Implicated product was purchased from stores, collected from patient households, and from the manufacturing facility. DHHS staff conducted a site visit and inspection of the facility where the implicated product was produced. The production process was reviewed and environmental swabs of equipment and surfaces along the production chain were collected. Receipts for raw chicken purchased and used to produce the chicken jerky pet treats were collected and provided to CDC and the U.S. Department of Agriculture Food Safety and Inspection Service to determine if the source chicken had been associated with other illnesses or outbreaks.
Laboratory testing
Stool specimens from ill individuals were collected by private healthcare providers and sent to clinical microbiology laboratories for analysis. Once identified, Salmonella isolates were submitted to the PHL for serotyping and PFGE, using protocols established by PulseNet (CDC, 2013). Product and environmental samples were also submitted to the PHL and were tested for pathogens using standard Food and Drug Administration (FDA) protocols (Andrews et al., 2011). Salmonella isolates obtained from these samples were sent to CDC for MLVA testing.
Results
Case finding and investigation
A total of 43 ill persons were identified from 6 different counties, with the majority of cases coming from Merrimack County (n = 23, 53%). Thirty-five patients met the confirmed case definition and eight were classified as probable cases (Fig. 1). One probable case-patient had a positive Salmonella Typhimurium laboratory result; however, the Xbal pattern was not indistinguishable from the outbreak strain. One confirmed case-patient was co-infected with Salmonella In-fantis Xbal JFXX01.0025; no other matches to this serotype-PFGE pattern were identified in NH. MLVA was completed for 33 cases infected with the outbreak strain, and all were considered similar or indistinguishable. Twenty-eight cases (65%) were female and the median age of cases was 43 years (range: < 1–76). Sixteen patients (37%) were hospitalized.
FIG. 1.
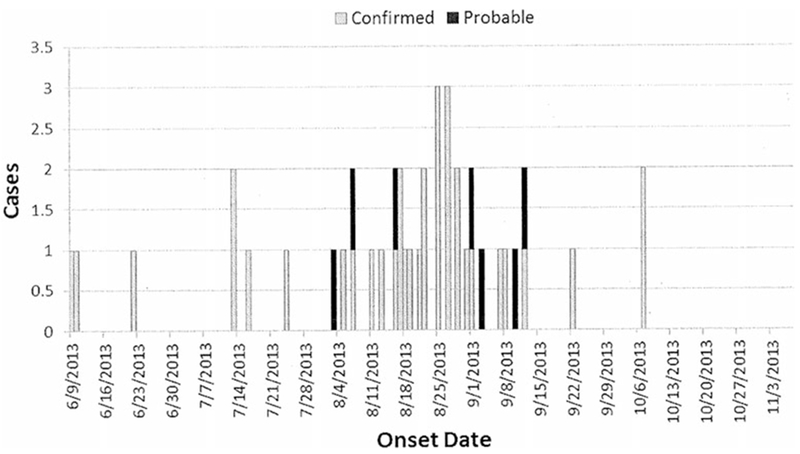
Outbreak of Salmonella Typhimurium in New Hampshire, case-patient illness onset dates (n = 42), June–October 2013. Includes 35 confirmed and 7 probable cases. Onset date is missing for one probable case.
Hypothesis-generating interviews revealed that 13 (93%) of the first 14 case-patients had exposure to dogs in the 7 days prior to illness onset and 76% had exposure to pet treats. No specific dog foods of interest were identified in interviews; however, common patterns emerged such as the purchase of “natural” and “organic” pet foods, and shopping at local pet stores and farmers markets rather than national chains. One case reported making homemade pet food and that the only pet food purchased outside the home was a chicken jerky product from a local pet store. A site visit to this store confirmed that the only chicken jerky sold was locally made (Brand X).
The pet-treat-specific questionnaire was administered to a total of 37 (86%) cases, representing 29 (83%) confirmed and 8 (100%) probable cases. However, all cases were reached for at least one interview: the initial enteric disease questionnaire, the hypothesis-generating questionnaire, or the pet-treat-specific questionnaire (Table 1). Across all interviews, 41 (95%) cases reported exposure to a dog within the 7 days prior to illness, and 27 (69%) reported exposure to any pet treats. Both proportions are statistically higher than the U.S. population, among which 61% of persons report exposure to dogs (p < 0.0001) and 16% report exposure to pet treats (p < 0.0001) in the previous 7 days (CDC, n.d.) (Clark et al., 2001). Ultimately, 38 (88%) case-patients reported exposure to Brand X Chicken Jerky, and the majority (79%) were exposed to the product in their own homes. A high proportion of case-patients reported handling Brand X Chicken Jerky themselves (68%). Only 9% reported always washing their hands after handling pet treats. Seven case-patients (18%) reported gastrointestinal illness in a household dog in the 7 days prior to illness onset, though no stool cultures or other tests to identify Salmonella were performed on any ill dogs.
Table 1.
Outbreak of Salmonella Typhimurium in New Hampshire: Summary of Risk Factors for Infection Among Case Patients (n = 43)a
| Total cases |
Confirmed cases |
Probable cases |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk factor | n | Total | % | n | Total | % | n | Total | % |
| Dogb | 41 | 43 | 95.3b | 33 | 35 | 94.3 | 8 | 8 | 100.0 |
| Household petc | 34 | 38 | 89.5 | 26 | 30 | 87.1 | 8 | 8 | 100.0 |
| Ill dog | 7 | 38 | 18.4 | 5 | 31 | 16.1 | 2 | 7 | 28.6 |
| Brand X Jerky or its manufacturerd | |||||||||
| Yes | 38 | 43 | 88.4 | 30 | 35 | 85.7 | 8 | 8 | 100.0 |
| No | 1 | 43 | 2.3 | 1 | 35 | 2.9 | 0 | 8 | 0.0 |
| Unknown/LTF | 4 | 43 | 9.3 | 4 | 35 | 11.4 | 0 | 8 | 0.0 |
| Location of jerky exposure | |||||||||
| Household | 30 | 38 | 79.0 | 22 | 30 | 73.3 | 8 | 8 | 100.0 |
| Outside of home | 5 | 38 | 13.2 | 5 | 30 | 16.7 | 0 | 8 | 0.0 |
| Social connectiond | 3 | 38 | 7.9 | 3 | 30 | 10.0 | 0 | 8 | 0.0 |
| Handled any pet treatsb | 27 | 39 | 69.2b | 20 | 31 | 64.5 | 7 | 8 | 87.5 |
| Handled Brand X Jerky | 26 | 38 | 68.4 | 19 | 30 | 63.3 | 7 | 8 | 87.5 |
| Regular purchaser of Brand X Jerky | 10 | 40 | 25.0 | 9 | 32 | 28.1 | 1 | 8 | 12.5 |
| Wash hands after handling treats | |||||||||
| Never | 12 | 32 | 37.5 | 9 | 24 | 37.5 | 3 | 8 | 37.5 |
| Rarely | 5 | 32 | 15.6 | 5 | 24 | 20.8 | 0 | 8 | 0.0 |
| Most of the time | 12 | 32 | 37.5 | 7 | 24 | 29.2 | 5 | 8 | 62.5 |
| Always | 3 | 32 | 9.4 | 3 | 24 | 12.5 | 0 | 8 | 0.0 |
Includes 35 confirmed and 8 probable cases. Risk factors were exposures reported in the 7 days preceding illness.
These numbers are statistically significant compared to the U.S. population FoodNet Survey in which 61% of Americans reported exposure to dogs in the previous 7 days (p < 0.0001) and 16.2% reported exposure to pet treats in the previous 7 days (p < 0.0001) (CDC, n.d.).
Defined as living in the house > 50% of the time.
Defined as personal contact with the jerky maker or the location in which the jerky was made.
Environmental investigation and traceback
The chicken jerky pet treat was manufactured in a private home by Company A and all production activities took place in the residential kitchen and two nearby rooms. The product was sold beginning in January 2013 and was available for sale in 6 retail stores in NH. Because Company A only produced a single pet-food item (chicken jerky) containing a single ingredient and produced no human food, it was exempt from food licensing and routine food safety inspection by both DHHS and the NH Department of Agriculture, Markets, and Food (DAMF) (NHDHHS, n.d., 2012; NHDAMF, n.d.).
Site visit to the facility revealed that the manufacturer obtained raw, boneless chicken breasts from a warehouse club store, sliced the chicken to approximately ¼-inch slices using a meat slicer, and then dehydrated the strips for 34–36 h at 160°F (the maximum temperature setting for the dehydrator cabinets). Product temperatures were not taken during or after the dehydration process. Doneness of the jerky was determined by a subjective test whereby the manufacturer would break a piece of the chicken to see that it snapped. The manufacturer used an electronic scale to weigh the product into 8-ounce portions and a vacuum sealer to package the finished product. Gloves were not used when handling the finished product and there were no protocols in place to wash, rinse, and sanitize food equipment. Traceback of the chicken used to make the chicken jerky did not identify a common source of raw chicken among NH cases or other cases with the same strain of Salmonella Typhimurium identified by PulseNet.
Product and environmental testing
DHHS collected two opened packages of Brand X Chicken Jerky from case-patient households, one unopened package from a pet store, and unpackaged finished product from the manufacturing facility. Nine environmental swabs were collected from along the production chain and results are listed in Table 2. All four jerky samples and seven of nine environmental samples yielded the outbreak strain of Salmonella Typhimurium, and were similar by MLVA. The only environmental samples not yielding Salmonella were the meat slicer and one of the dehydrator samples.
Table 2.
Outbreak of Salmonella Typhimurium in New Hampshire: Summary of Environmental Testing Results (n = 9)
| Environmental swab location | Salmonella | Outbreak strain |
|---|---|---|
| Meat slicer | (−) | n/a |
| Inside dehydrator 1 | (+) | (+) |
| Inside dehydrator 2 | (+) | (+) |
| Dehydrator trays | (−) | n/a |
| Measuring bowl | (+) | (+) |
| Scale | (+) | (+) |
| Vacuum sealer (inside) | (+) | (+) |
| Plastic bin to store product | (+) | (+) |
| Kitchen sink drain | (+) | (+) |
n/a, not applicable.
Product recall
On the basis of epidemiologic and traceback evidence, the manufacturer issued a voluntary recall of Brand X Chicken Jerky pet treats on September 9, 2013 and permanently ceased production. On September 10, DHHS issued a press release alerting the public to the outbreak and associated recall. Three additional case-patients became ill more than one incubation period after the recall, one of which was a household contact to a confirmed case.
Discussion
At the time of this report, this was the largest outbreak of Salmonella associated with pet treats identified in the United States. This outbreak was noteworthy in that, contrary to other outbreaks of pet food and pet treats (Pitout et al., 2003; Finley et al., 2008; Behravesh et al., 2010; Clark et al., 2001; Imanishi et al, 2014), it was localized and infected a large number of humans despite small-scale production. Epidemiologic, laboratory, and environmental evidence implicated locally made Brand X Chicken Jerky pet treats. Only three additional cases occurred after a voluntary recall of this product. Isolation of the outbreak strain from unopened packages, opened packages from patient homes, unpackaged chicken jerky, and environmental swabs from the Company A facility all yielded the outbreak strain and suggested extensive contamination of this product and the environment in which it was produced.
Though pet treats are less commonly implicated as the cause of outbreaks, it is known that they can be contaminated with Salmonella and other pathogens (Sanchez et al., 2002; CDC, 2006; Finley et al., 2006; KuKanich et al., 2011). In fact, the U.S. FDA’s first use of the mandatory recall authority granted by the 2011 Food Safety Modernization Act was for the recall of pet treats contaminated with Salmonella, though no human illness was ever identified (FDA, 2013). There have only been 3 published reports of human illness associated with pet treats, all occurring in the last 15 years. These outbreaks have involved some of the most common Salmonella serotypes (Newport, Infantis, Typhimurium), and it is possible that pet treats may be an under-recognized source of sporadic infections and undetected outbreaks. In at least one of these outbreaks, caused by dehydrated beef and salmon pet treats, inadequate dehydration temperature was also a factor contributing to contamination (Clark et al., 2001; Pitout et al., 2003; CDC, 2006). These outbreaks raise the authors’ concerns about the regulation of pet treats, in particular locally made pet treats, for which the level of regulation can vary from state to state. In NH, pet treats containing only a single ingredient do not require registration, and no pet treats or feed require facility inspection or production process review (NHDAMF, n.d.).
Spread of illness in this outbreak likely occurred through direct contact with the contaminated product, contact with an ill or asymptomatic but infected dog, or contact with contaminated surfaces in the home or in the jerky manufacturing facility. The contribution of zoonotic exposure is unknown. Only 17% of cases reported a pet ill with gastroenteritis, though an infected dog can shed Salmonella intermittently in its feces for up to 6 weeks even if asymptomatic (Sanchez et al., 2002; Finley et al., 2006). One case-patient reported consuming the pet treats. The small percentage of cases reporting hand washing after handling pet treats suggests that direct contact to the contaminated treats was the most significant source of transmission. Though illnesses occurred throughout the summer, a majority of cases became ill in August (57%), which could suggest the pet treats were most heavily contaminated at that point in time.
Several observations made during inspection of the Company A manufacturing facility were identified as contributing factors to contamination of the chicken jerky with Salmonella. To kill Salmonella, raw animal foods should be cooked to an internal temperature of 165°F or above for 15 seconds (FDA, 2009). The temperature of the dehydrator was set only to 160°F, and no internal temperature verification was conducted during the cooking of the chicken; there was no evidence that the time and temperature needed to kill Salmonella was ever reached. The recovery of Salmonella from the environmental swabs of food contact surfaces in the manufacturing facility illustrate that these surfaces were not being adequately cleaned and sanitized. Among these surfaces were plastic bins used to store extra chicken jerky before packaging, which the manufacturer reported using bare hands to fill. It is likely that jerky from numerous batches comingled in the bins and if only one batch had been contaminated, it could have contaminated much of the chicken jerky produced by the facility. “Best if used by” dates were stamped on the Brand X Chicken Jerky retail packaging; however, it was not clear how this date was determined, and there were no product-rotation procedures. Finally, as Salmonella is a facultative anaerobe, if present on a product that has been vacuum-packed like the chicken jerky, the reduced oxygen state in the package would make conditions more favorable for its growth. Company A did not recognize conditions that may contribute to foodborne illness and take appropriate preventive and corrective actions. This was illustrated by lack of procedures to validate cooking time and temperatures, poor sanitization, and no food safety assessment for the process of making the chicken jerky.
In previous pet food and pet treat Salmonella outbreaks, pet food products were often found to be contaminated with multiple Salmonella serotypes (Finley et al., 2008; Behravesh et al., 2010). Though only one Salmonella serotype was recovered from the jerky and the manufacturing environment in this instance, there were a number of MLVA patterns recovered from the manufacturing facility environment, one case-patient was co-infected with Salmonella Infantis, and one case-patient had a PFGE pattern similar, but not exactly the same as the other patients.
In the United States, there has been increasing interest in locally sourced human and pet foods. From 2009 to 2013, the number of farmers’ markets in the United States increased by 54% (from 5274 markets to 8144) (USDA, n.d.) and as of 2013, 42 states including NH had some type of “cottage food” or “homestead food” law. These laws allow in-home production of certain “non-hazardous” foods intended for sale, as opposed to requiring they be prepared in an inspected commercial kitchen (Condra et al., 2013). Many of these laws, including NH’s, have been passed in recent years (NHDHHS, 2012). Some of the drivers of the local food movement include perceptions of safer, more nutritious food, recalls of commercial human and pet foods (FDA, n.d.), support of the local economy and local agriculture, reduced environmental impact, and the avoidance of food containing preservatives or other additives. Not all of these perceived benefits have been scientifically documented, including that locally produced food is as safe as or safer than food produced elsewhere that is regulated for safety, and the benefits gained by local production may depend on the type and amount of food produced.
The increased interest and production of local foods creates a unique food safety issue that is highlighted by this outbreak. Though pet foods are regulated differently than foods intended for human consumption, many of the processing concerns identified in this outbreak would be safety concerns for home producers of even “nonhazardous foods” frequently allowed under homestead or cottage food laws (i.e., cross-contamination of ready-to-eat product, lack of glove use, gross environmental contamination, inadequate temperature control, improper packaging). This home-based company began production in response to worries about the safety of chicken jerky pet treats manufactured in China (FDA, 2012). Their product was marketed as a safe, natural, local alternative to commercially prepared pet treats, claiming food for pets should be as safe as food intended for humans. When increasing the scale of production of any product for sale to the public, there are inherent changes in food safety risk. Some of these risks cannot be mitigated in a home kitchen without significant investments in new or retrofitted equipment and changes to kitchen design. This outbreak demonstrates that local, small-scale food production operations can result in food safety vulnerabilities, when appropriate processing procedures are not followed. Food safety education for home producers could lessen these vulnerabilities.
Conclusions
This outbreak demonstrates that contaminated pet treats can be an efficient transmitter of Salmonella to humans. Consumers should be aware that locally made products, especially pet foods, may be exempt from food safety regulations and may not inherently be safer than other products, and that in general, animals and animal food can carry pathogens that cause human illness. To reduce risk of human illness caused by Salmonella, regulation and education of pet food manufacturers of any size to ensure basic knowledge of safe food-processing practices, as well as education of consumers about the importance of hand hygiene after feeding pets or handling pet food or feces, could be considered.
Acknowledgments
We wish to thank the following persons for their contributions to study design, data collection, and specimen collection and testing: Shannon Casey, Christine Villeneuve, and Betty Wendt (City of Nashua, NH Health Department); Christine Adamski and Mary Lee Greaves, (New Hampshire Department of Health and Human Services); Elizabeth A. Talbot, MD (Dartmouth College, Hanover NH); and the PulseNet Team and MLVA Laboratory at the U.S. Centers for Disease Control and Prevention. This work was supported, in part, by the Centers for Disease Control and Prevention, Epidemiology and Laboratory Capacity Cooperative Agreement (grant number 3U50CI000874–02S3) and the Food and Drug Administration, Food Emergency Response Network Microbiological Cooperative Agreement (grant number U18FD0038220). The findings and conclusions in this report are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Footnotes
Disclosure Statement
No competing financial interests exist.
References
- Andrews WH, Jacobson A, Hammack T. Bacteriological Analytical Manual. Chapter 5: Salmonella. Silver Spring, MD: U.S. Food and Drug Administration, 2011. [Google Scholar]
- Behravesh C, Ferraro A, Deasy M III, Dato V, Moll M, Sandt C, Rea NK, Rickert R, Marriott C, Warren K, Urdaneta V, Salehi E, Villamil E, Ayers T, Hoekstra RM, Austin JL, Ostroff S, Williams IT, and the Salmonella Schwarzengrund Outbreak Investigation Team. Human Salmonella infections linked to contaminated dry dog and cat food, 2006–2008. Pediatrics 2010;126:477–483. [DOI] [PubMed] [Google Scholar]
- [CDC] Centers for Disease Control and Prevention. Foodborne Active Surveillance Network (FoodNet) Population Survey Atlas of Exposures. Atlanta, Georgia: US Department of Health and Human Services, 2006–7. Available at: http://www.cdc.gov/foodnet/PDFs/FNExpAtl03022011.pdf, n.d., accessed May 5, 2014. [Google Scholar]
- CDC. Human salmonellosis associated with animal-derived pet treats—United States and Canada, 2005. MMWR 2006;55: 702–705. [PubMed] [Google Scholar]
- CDC. Standard Operating Procedure for PulseNet PFGE of Escherichia coli O157:H7, Escherichia coli non-O157 (STEC), Salmonella serotypes, Shigella sonnei and Shigella flexneri. 2013. Available at: http://www.cdc.gov/pulsenet/PDF/ecoli-shigella-salmonella-pfge-protocol-508c.pdf, accessed December 15, 2014.
- Clark C, Cunningham J, Ahmed R, Woodward D, Fonseca K, Isaacs S,Ellis A, Anand C, Ziebell K, Muckle A, Sockett P, Rodgers F. Characterization of Salmonella associated with pig ear dog treats in Canada. J Clin Microbiol 2001;3911:3962–3968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condra A Cottage Food Laws in the United States. Boston: Harvard Food Law and Policy Clinic, Harvard Law School, 2013. [Google Scholar]
- [FDA] United States Food and Drug Administration. FDA 2009 Food Code: Chapter 3 Subpart 401.11 (A)(3). 2009. Available at: http://www.fda.gov/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/ucm186451.htm#part3-4, accessed April 1, 2014.
- FDA. FDA Investigates Animal Illnesses Linked to Jerky Pet Treats. 2012. Available at: http://www.fda.gov/AnimalVeterinary/SafetyHealth/ProductSafetyInformation/ucm319463.htm, accessed December 9, 2014.
- FDA. The Food Safety Modernization Act (FSMA): Annual Report to Congress on the Use of Mandatory Recall Authority—2013. FSMA Reports and Studies. 2013. Available at: http://www.fda.gov/Food/GuidanceRegulation/FSMA/ucm382490.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery, accessed April 30, 2014.
- FDA. USFDA Recalls and Withdrawals. n.d. Available at: http://www.fda.gov/animalVeterinary/safetyhealth/recallswithdrawals/default.htm, accessed May 5, 2014.
- Finley R, Reid-Smith R, Ribble C, Popa M, Vandermeer M, and Aramini J. The occurrence and anti-microbial susceptibility of Salmonellae isolated from commercially available pig ear pet treats. Zoonoses Public Health 2008;55:455–461. [DOI] [PubMed] [Google Scholar]
- Finley R, Reid-Smith R, Weese JS, Angulo FJ. Human health implications of Salmonella-contaminated natural pet treats and raw pet food. Clin Infect Dis 2006;42:686–691. [DOI] [PubMed] [Google Scholar]
- Hale CR, Scallan E, Cronquist AB, Dunn J, Smith K, Robinson T,Lathrop S, Tobin-D’Angelo M, Clogher P. Estimates of enteric illness attributable to contact with animals and their environments in the United States. Clin Infect Dis 2012; 54(Suppl 5):S472–S479. [DOI] [PubMed] [Google Scholar]
- Heymann DL (ed.). Control of Communicable Diseases Manual, 19th ed. Washington, DC: American Public Health Association, 2008. [Google Scholar]
- Imanishi M, Rotstein D, Reimschuessel R, Schwensohn C, Woody D, Davis S, Hunt A, Arends K, Achen M, Cui J, Zhang Y, Denny L, Phan Q, Joseph L, Tuite C, Tataryn J, Behravesh C. Outbreak of Salmonella enterica serotype Infantis infection in humans linked to dry dog food in the United States and Canada, 2012. J Am Vet Med Assoc 2014;244:545–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KuKanich KS. Update on Salmonella spp contamination of pet food, treats, and nutritional products and safe feeding recommendations. J Am Vet Med Assoc 2011;238:1430–1434. [DOI] [PubMed] [Google Scholar]
- [NHDAMF] New Hampshire Department of Agriculture, Markets, and Food New Hampshire. Title XL Agriculture, Horticulture, and Animal Husbandry. RSA 435: Animal Care, Breeding and Feed. Section 19 IV. Available at: http://www.gencourt.state.nh.us/rsa/html/XL/435/435-mrg.htm, n.d., accessed May 21, 2014.
- [NHDHHS] New Hampshire Department of Health and Human Services. New Hampshire He-P 2300: Sanitary Production and Distribution of Food. Part He-P 2301.01. Available at: http://www.gencourt.state.nh.us/rules/state_agencies/he-p2300.html, n.d., accessed April 30, 2014.
- NHDHHS. New Hampshire Title X Public Health: Sanitary Production and Distribution of Food. Chapter 143-A: Food Service Licensure. Section 5 Exemption VII. 2012. Available at: http://www.gencourt.state.nh.us/rsa/html/X/143-A/143-A-5.htm, accessed April 30, 2014.
- Pitout JD, Reisbig MD, Mulvey M, Chui L, Louie M, Crowe L, Church DL, Elsayed S, Gregson D, Ahmed R, Tilley P, Hanson ND. Association between handling of pet treats and infection with Salmonella enterica serotype Newport expressing the AmpC beta-lactamase, CMY-2. J Clin Microbiol 2003;41:4578–4582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez S, Hofacre CL, Lee MD, Maurer JJ, Doyle MP. Animal sources of salmonellosis in humans. Am Vet Med Assoc 2002;221:492–497. [DOI] [PubMed] [Google Scholar]
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL. Foodborne illness acquired in the United States—Major pathogens. Emerg Infec Dis 2011;17:7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [USDA] United States Department of Agriculture: Agricultural Marketing Service (USDA). National Count of Farmers Market Directory Listings Graph: 1994–2013. n.d. Available at: http://www.ams.usda.gov/AMSv1.0/ams.fetchTemplateData.do?template=TemplateS&navID=WholesaleandFarmersMarkets&leftNav=WholesaleandFarmersMarkets&page=WFMFarmersMarketGrowth&description=Farmers%20Market%20Growth&acct=frmrdirmkt, accessed March 25, 2014.


