ABSTRACT
Previous meta-analyses have associated dairy products with a lower risk of metabolic syndrome (MetS). Since then, new studies evaluating not only total dairy but also different subtypes have been published in this field. The objective of the present work was to systematically review and meta-analyze the epidemiologic studies regarding the associations between the consumption of total dairy products and subtypes (milk, yogurt, and cheese) and the incidence of MetS. Relevant studies were identified through Medline and Cochrane databases. Eligible studies were prospective cohort studies that examined the association between dairy product consumption and/or different subtypes of dairy and the risk of MetS. Random-effects or fixed-effects models were assigned to calculate the pooled RR estimates with 95% CIs. From the 2994 identified articles, 12 and 11 studies were included for the qualitative and quantitative synthesis, respectively. After comparing the highest with the lowest categories, total dairy product consumption was inversely associated with the risk of MetS (9 study comparisons; RR: 0.73; 95% CI: 0.64, 0.83). Low-fat dairy and total yogurt consumption were inversely associated with the risk of MetS (low-fat dairy: 2 study comparisons; RR: 0.77; 95% CI: 0.65, 0.91; total yogurt consumption: 4 study comparisons; RR: 0.74; 95% CI: 0.66, 0.82). The linear RR per 1 serving of yogurt/d was 0.77 (95% CI: 0.60, 1.00). Low-fat yogurt and whole-fat yogurt were inversely associated with the risk of MetS (low-fat yogurt: 2 study comparisons; RR: 0.72; 95% CI: 0.62, 0.84; whole-fat yogurt: 2 study comparisons; RR: 0.81; 95% CI: 0.70, 0.94). Total milk consumption was inversely associated with the risk of MetS (6 study comparisons; RR: 0.79; 95% CI: 0.64, 0.97). Whole-fat dairy consumption was not associated with MetS risk. Our findings suggest that the consumption of total and low-fat dairy products, milk, and yogurt is inversely associated with the risk of MetS. The study protocol is available at https://www.crd.york.ac.uk/PROSPERO/ as CRD42018082480.
Keywords: dairy products, metabolic syndrome, milk, yogurt, cheese
Introduction
Metabolic syndrome (MetS) is a cluster of ≥3 different cardiovascular risk factors, including abdominal obesity, blood pressure, glucose, and serum TG and HDL-cholesterol concentrations in a pathological range (1). This syndrome is directly associated with 2 of the most prevalent diseases worldwide: type 2 diabetes and cardiovascular disease (2). The prevalence of MetS has increased in the last decades around the globe, affecting nearly one-quarter of the total adult population (3).
The etiology of MetS is not well known. However, different modifiable risk factors, such as physical activity, smoking habits, alcohol consumption, and following a healthy diet, seem to influence the risk of this complex metabolic disease (4). From a nutritional point of view, the available evidence suggests that different healthy dietary patterns and specifically some food groups, such as dairy products, may have potential beneficial effects on MetS prevention (3).
A growing number of studies have reported an inverse association between total dairy product consumption and the risk of developing MetS. Two previous meta-analyses summarized the results showing a 14% (RR: 0.86; 95% CI: 0.79, 0.92) and a 15% (RR: 0.85; 95% CI: 0.73, 0.98) lower risk of MetS incidence when comparing the highest with the lowest categories of total dairy consumption (5, 6). However, there are significant differences in the compositions of dairy product subtypes, which could exert different roles in MetS prevention. However, to our knowledge, no previous meta-analysis has taken this into consideration. Therefore, we conducted a systematic review and meta-analysis of prospective cohort studies to evaluate the associations between total dairy product consumption and different dairy subtypes and the prevention of MetS.
Methods
The Cochrane Handbook for Systematic Reviews of Interventions was used to conduct the present systematic review and meta-analysis. Moreover, Meta-analysis of Observational Studies in Epidemiology (MOOSE) was used to report the results. The study protocol is available at https://www.crd.york.ac.uk/PROSPERO/ (registration number: CRD42018082480).
Search strategy and data sources
Through 28 November 2017, a comprehensive search of 2 databases (Medline and the Cochrane Library) was performed, which was limited to studies conducted in humans and without any language restriction. Supplemental Table 1 shows the complete search strategy. To supplement the electronic search, a manual review of all the retrieved article references was conducted.
Study selection
The first step in the study selection was to remove duplicates on the basis of article references. Second, the eligibility criteria of the studies were evaluated through comprehensive screening of all titles and abstracts. The inclusion criteria were as follows: prospective cohort studies with ≥1 y of follow-up conducted in adults (aged >18 y), total dairy products and/or different dairy subtypes (full-fat or low-fat total dairy; milk, full-fat, or low-fat milk; yogurt, full-fat, or low-fat yogurt; and cheese) as the exposure, and MetS as the outcome with reports of the effect estimates (ORs or RRs and 95% CIs) for categories of dairy product consumption. When different articles carried out in the same cohort were identified, we included the one with the highest sample size or longer follow-up period (7). Published proceedings and abstracts were not included.
Data extraction
The full text of articles that passed the eligibility process were carefully reviewed by 2 independent researchers (NB-T and GM-S). A predefined proforma was filled out for each one of the included studies in order to extract the relevant information: author(s); year of publication; journal; title of the article; setting; study name (if provided); follow-up; sample size; participant characteristics; exposure; dietary assessment; number of cases; outcome; assessment method; RRs, ORs, or HRs; 95% CIs or SEs; statistical analyses; and findings. Additional relevant information was requested from some authors (8). If necessary, inconsistencies between researchers in terms of data extraction were resolved by consensus or discussion with a third author (JS-S).
Risk-of-bias (quality) assessment
The Newcastle-Ottawa Scale was used to assess the risk of bias in the retrieved prospective cohort studies (9). This tool consists of a rating scale from 0 to 9 points that are given according to 3 domains: selection of the population (ranging from 0 to 4 points), assessment of the outcome (ranging from 0 to 3 points), and comparability of the groups (ranging from 0 to 2 points). We considered a study to be of high quality when the total score was ≥7 points.
Statistical analyses
The inverse variance method with random-effects (when ≥5 comparisons were available) or fixed-effects models (when <5 comparisons were available) was used to pool the natural log of transformed RRs, ORs, and HRs, comparing extreme categories of dairy product consumption. For the present analysis, we considered the HRs and ORs to be equivalent to RRs, as has been done by others (10).
The linear and nonlinear dose-response relations were assessed using generalized estimation models and spline curve modeling (MKSPLINE procedure) when >2 comparisons were available (total dairy products, total yogurt, and total milk). This procedure requires the mean or median consumption of ≥3 categories and the number of MetS cases, participants, or person-years by category and effect estimates. For studies that did not report some of the aforementioned data, we estimated these variables, if possible, following the imputation method described by Bekkering et al. (11) Becerra-Tomás et al. (12). Therefore, we only included in the analysis those studies reporting all the needed information. For these analyses, grams of total dairy, yogurt, and milk were converted to servings per day, considering 1 serving as 200, 125, and 200 g, respectively, unless authors specified another serving size.
Interstudy heterogeneity was estimated using the Cochran's Q statistic and quantified by I2 statistic. A P value <0.10 and I2 ≥50% indicated significant heterogeneity. To test the influence of each study on the summary risk estimates, we removed one study at a time and recalculated the pooled risk estimates. All of the data analyses were performed using Review Manager (RevMan) version 5.3 and Stata version 15 (StataCorp).
Results
Study selection
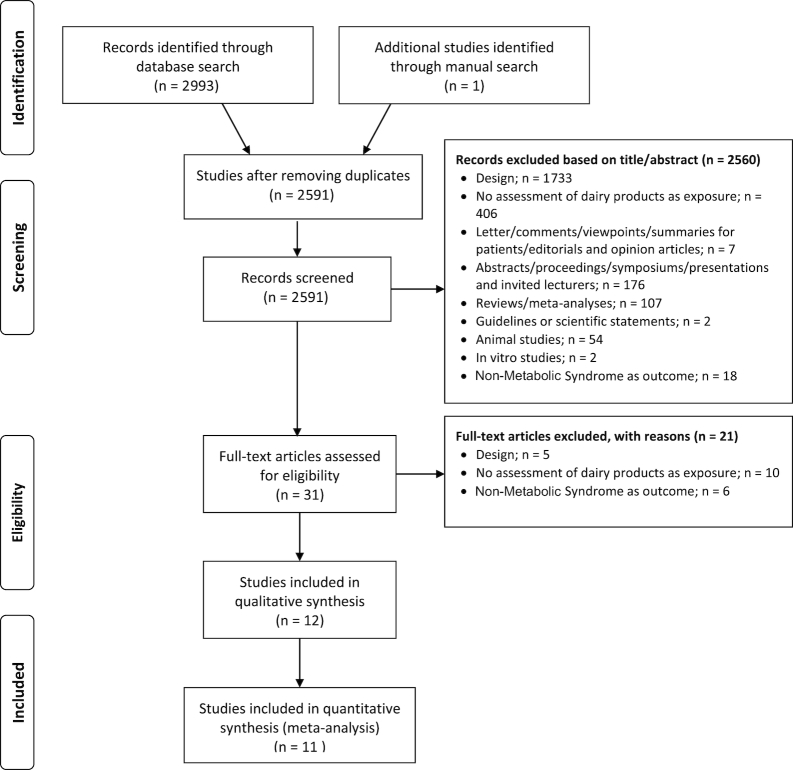
A total of 2993 potential studies were found using the search strategy shown in Supplemental Table 1. In addition, we added one study from a manual search of the references from other studies. Before screening 2591 studies by reviewing titles and abstracts, 402 duplicate articles were removed. Next, 31 studies were fully reviewed; and finally, 12 and 11 studies were included for the qualitative and quantitative syntheses, respectively (Figure 1).
FIGURE 1.
Flow chart of the literature search.
Studies characteristics
The characteristics of the included prospective cohort studies are reported in Table 1. We identified a total of 12 prospective studies reporting the relation between total dairy and dairy product subtypes and the risk of MetS; 8 for total dairy products, 2 for low-fat and whole-fat dairy products, 3 for total yogurt, 2 for low-fat and whole-fat yogurt, 5 for milk, and 2 for cheese. All of the studies were published between 2002 and 2017. By geographical region, 2 studies were conducted in Spain (13, 14), 1 in Brazil (15), 1 in France (16), 3 in Korea (8, 17, 23), 1 in Australia (18), 2 in the United States (19, 20), 1 in the Netherlands (21), and 1 in Taiwan (22). Participants were all aged ≥18 y, including both women and men. Follow-up period ranged from 2.8 to 10 y. For dairy product assessment, 92% of the studies used a validated FFQ. With regard to the MetS definition, 3 studies used the updated harmonized criteria (13, 14, 17), 3 used the National Cholesterol Education Program Adult Treatment Panel III criteria (8, 15, 23), 1 used the International Diabetes Federation criteria (18), 1 used the American Heart Association guidelines (19), 1 used no official definition (20), and 1 study reported information using 2 different MetS definitions (16) (National Cholesterol Education Program Adult Treatment Panel III and the International Diabetes Federation).
TABLE 1.
Characteristics of prospective cohort studies evaluating the association between dairy product consumption and the incidence of MetS1
| Study, year | Country | Study name | Participants, n | Age, y | Follow-up, y | Dairy assessment | Dairy definition | Total incidence | Adjustments | Founding source | NOS, score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Shin H et al., 2013 (8) | Korea | Anseong and Ansan cohort of the KoGES | Sample size: 7240; men: 3620; women: 3620 | 40–69 | 3.79 | Validated FFQ | Dairy products: milk, yogurt, and cheese | 1240 | Sex, age, smoking, physical activity, energy, alcohol, education, and income | Agency | 7 |
| Babio N et al., 2015 (13) | Spain | Prevención con Dieta Mediterránea (PREDIMED) | Sample size: 1868; men: 888; women: 980 | 55–80 | 3.2 | Validated FFQ | Total dairy: low-fat/skim milk and skim yogurt, whole milk, condensed milk, whole yogurt, custard, and all types of cheeses, including petit Swiss, ricotta, cottage, and semicured/cured cheeses, such as cheddar, Manchego, and Emmentaler. | 930 | Intervention group, sex, age, leisure time physical activity, BMI, smoking habit, hypoglycemic, hypolipidemic, antihypertensive, and insulin treatment at baseline, vegetables, fruit, legumes, cereals, fish, red meat, cookies, olive oil, and nuts (all grams per day), as well as alcohol (grams per day and quadratic term), the prevalence of MetS components at baseline, including abdominal obesity (yes/no), hypertriglyceridemia (yes/no), low HDL cholesterol (yes/no), hypertension (yes/no), and high fasting plasma glucose (yes/no) | Agency-Industry | 8 |
| Sayón-Orea et al., 2015 (14) | Spain | Seguimiento Universidad de Navarra (SUN) | Sample size: 8063; men: 1812; women: 6251 | 20–90 | 6 | Validated FFQ | Total yogurt: whole-fat yogurt and low-fat yogurt | 306 | Age, sex, baseline weight, total energy intake, alcohol intake, soft drinks, red meat, French fries, fast food, Mediterranean diet, physical activity, sedentary behavior, hours sitting, smoking status, snacking between meals, and following special diet | Agency-industry | 7 |
| Damião R et al., 2016 (15) | Brazil | - | Sample size: 151; men: 84; women: 67 | 40–49 | 7 | Validated FFQ | Dairy milk | 57 | Age, sex, physical activity, smoking, education level, alcohol, total energy intake, and total fat intake | Agency | 7 |
| Fumeron F et al., 2011 (16) | France | Devenir des Spondyloart rites Indifférenciées Récentes DESIR | Sample size: 3435; men: 1710; women: 1725 | 30–65 | 9 | Validated FFQ | Dairy products, except cheese | 667 | Gender, age, smoking, physical activity, fat intake, and mean BMI | Agency | 7 |
| Baik et al., 2013 (17) | Korea | KoGES | Sample size: 5251 | 40–69 | 6 | Validated FFQ | No description | 1325 | Sex, age, smoking, physical activity, fat intake, alcohol, education, income, occupation, study sites, FTO genotypes, and food groups | Agency | 9 |
| Louie et al., 2013 (18) | Australia | Blue Mountains Eye Study (BMES) | Sample size: 1824 | >49 | 10 | Validated FFQ | Total dairy: dairy subcategorization includes regular milk, reduced-fat/skim milk, low-fat cheese, regular cheese, reduced-fat dairy dessert (e.g., low-fat yogurt), and medium-fat dairy dessert (e.g., custard and regular yogurt) | 155 | Sex, age, smoking, physical activity, energy, glycemic load, fiber from vegetables, family history of type 2 diabetes, and calcium | Industry | 6 |
| Lutsey et al., 2008 (19) | United States | Atherosclerosis Risk in Communities (ARIC) | Sample size: 9514; men: 4197; women: 5317 | 45–64 | 9 | Validated FFQ | No description | 3782 | Age, sex, race, education, center, total calories, smoking status (current, former, or never), pack-years, physical activity, meat, fruits and vegetables, whole grains, and refined grains (all as time-varying covariates) | Agency | 7 |
| Pereira et al., 2002 (20) | United States | Coronary Artery Risk Development in Young Adults | Sample size: 909 | 18–30 | 10 | Validated FFQ | Dairy: milk, milk drinks, butter, cream, cheeses (90% of total dairy intake), and yogurts, dips, ice cream, puddings, and dairy-based desserts | 293 overweight cases | Age, sex, race, calorie intake per day, study center, baseline BMI, daily alcohol intake, smoking status, daily physical activity, use of vitamin supplement, daily polyunsaturated fat consumption, daily caffeine intake, fiber per 1000 kcal, frequency of whole and refined grains, meat, fruit, vegetables, and soda and dietary intake of magnesium, calcium, and vitamin D | Agency | 7 |
| Snijder et al., 2008 (21) | Netherlands | The Hoorn study | Sample size: 885 | 50–75 | 6.4 | Validated FFQ | The variable dairy desserts included yogurt, curds, and custard; the variable milk included low-fat, skim, and whole milk; the variable yogurt included all low-fat, skim, and whole yogurts | 215 | Age, sex, smoking, physical activity, energy, and alcohol consumption | Agency | 7 |
| Lin et al., 2013 (22) | Taiwan | — | Sample size: 888 | ∼77 | 2.8 | Medical histories and health behaviors by personal interview using the questionnaires | Milk | Yes or no | Serum creatinine, ALT, and uric acid concentrations were included as continuous variables in the regression model; age, sex, initial MetS score, smoking, drinking, exercise, vegetable intake, milk intake, and teeth brushing | Agency | 6 |
| Kim D et al., 2017 (23) | Korea | Korean Genome and Epidemiology | Sample size: 5510 Men: 2859 Women: 2651 |
40–69 | 10 | Validated FFQ | Total dairy: milk, yogurt and cheese | 2013 | Age, sex, BMI, residential location, educational level, household income, smoking status, alcohol intake and physical activity, nutrient intakes such as energy and energy-adjusted Ca and fiber | Agency | 7 |
1ALT, Alanine aminotransferase; FTO, Fat Mass and Obesity-Associated gene; MetS, metabolic syndrome; NOS, Newcastle-Ottawa Scale.
The mean quality assessment score for all of the studies was 7.1 (range: 6–9). Two studies received a poor-quality score of 6 points (18, 22), 8 studies received a 7-point score (8, 14–16, 19–21, 24), and 2 studies reported quality scores of 8 (13) and 9 (17), indicating a good quality.
Meta-analysis of prospective cohort studies
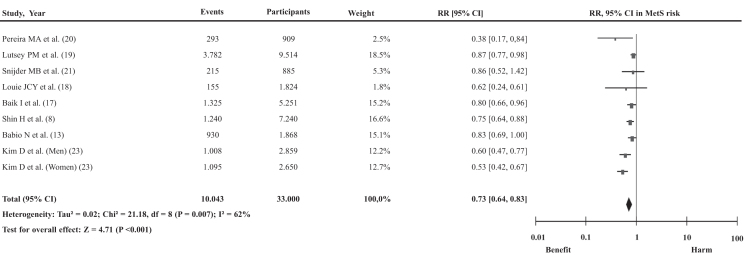
Figure 2 shows the association between total dairy product consumption and the risk of MetS incidence. The pooled analysis of 9 comparisons generated a summary RR of 0.73 (95% CI: 0.64, 0.83), with substantial heterogeneity (P < 0.001, I2 = 62%) when comparing the highest with the lowest categories of dairy product consumption. The removal of one study at a time did not modify the association. However, the removal of the study by Kim and Kim (23) conducted in women (I2 = 38%, P = 0.13) did explain most of the interstudy heterogeneity (Supplemental Table 2). Seven studies were included in the dose-response analysis of total dairy consumption and the risk of MetS incidence (8, 13, 17, 19–21, 23.). The pooled risk showed a nonlinear association between the consumption of 1 serving of dairy products/d and the risk of MetS (P for departure from linearity = 0.046) (Supplemental Figure 1).
FIGURE 2.
Association between total dairy product consumption and the risk of MetS incidence. The diamond represents the pooled risk estimate. Interstudy heterogeneity was tested by using the Cochran Q statistic (χ2) at a significance level of P < 0.10 and quantified by the I2 statistic. MetS, metabolic syndrome.
Supplemental Figure 2 shows the association between low-fat dairy product consumption and the risk of MetS after pooling the results of 2 studies. There was a significant inverse association between low-fat dairy product consumption and MetS risk when comparing the highest with the lowest consumption categories (0.77; 95% CI: 0.65, 0.91), with evidence of substantial heterogeneity (P = 0.002, I2 = 89%).
Supplemental Figure 3 shows the association between whole-fat dairy product consumption and the risk of MetS. The analysis included 2 studies showing a pooled RR of 0.93 (95% CI: 0.79, 1.08), with evidence of substantial heterogeneity (P = 0.002, I2 = 89%).
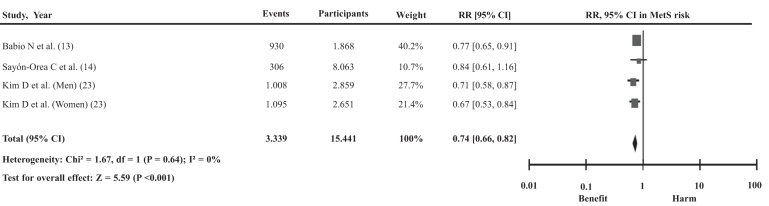
Figure 3 shows the association between total yogurt consumption and the risk of MetS after pooling the results of 4 studies. The pooled analysis showed a 26% lower risk of MetS incidence when comparing the highest with the lowest consumption categories (0.74; 95% CI: 0.66, 0.82), with no evidence of heterogeneity (P = 0.64, I2 = 0%). The removal of one study at a time did not modify the association between total yogurt consumption and the risk of developing MetS nor the interstudy heterogeneity (Supplemental Table 2). Three studies were included in the dose-response analysis of total yogurt consumption and the risk of MetS (13, 14, 24). The pooled risk showed a linear association between 1 serving of total yogurt consumption/d and the risk of MetS (0.77; 95% CI: 0.60, 1.00; P = 0.046; P for departure from linearity = 0.556) (Supplemental Figure 4).
FIGURE 3.
Association between total yogurt consumption and the risk of MetS incidence. The diamond represents the pooled risk estimate. Interstudy heterogeneity was tested by using the Cochran Q statistic (χ2) at a significance level of P < 0.10 and quantified by the I2 statistic. MetS, metabolic syndrome.
Supplemental Figure 5 shows the association between low-fat yogurt consumption and the risk of MetS incidence. The pooled analysis of 2 comparisons generated a summary RR of 0.72 (95% CI: 0.62, 0.84), with no evidence of substantial heterogeneity (P = 0.60, I2 = 0%) when comparing the highest with the lowest categories of consumption. For low-fat yogurt, the summary RR was 0.72 (95% CI: 0.62, 0.84), with no heterogeneity (P = 0.60, I2 = 0%).
Supplemental Figure 6 shows the association between whole-fat yogurt consumption and the risk of MetS incidence. The pooled RR was 0.81 (95% CI: 0.70, 0.94) for the 2 included studies, with no evidence of heterogeneity (P = 0.26, I2 = 20%).
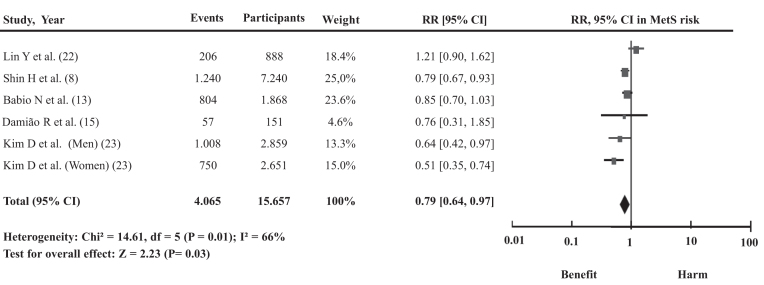
Figure 4 shows the association between total milk consumption and the risk of MetS. After pooling 5 studies (6 comparisons), an inverse association between total milk consumption and the risk of MetS was identified when comparing the highest with the lowest categories. The pooled RR was 0.79 (95% CI: 0.64, 0.97), with evidence of heterogeneity (P = 0.01, I2 = 66%). The exclusion of one study at a time did not modify the association. However, the removal of the study by Lin et al. (22) (I2 = 39%, P = 0.16) did explain most of the interstudy heterogeneity (Supplemental Table 2). Three studies were included in the dose-response analysis of total milk consumption and the risk of MetS incidence (13, 15, 24). The pooled risk showed a nonlinear association for 1 serving of total milk consumption/d and the risk of MetS (P for departure from linearity = 0.01) (Supplemental Figure 7).
FIGURE 4.
Association between total milk consumption and the risk of MetS incidence. The diamond represents the pooled risk estimate. Interstudy heterogeneity was tested by using the Cochran Q statistic (χ2) at a significance level of P < 0.10 and quantified by the I2 statistic. MetS, metabolic syndrome.
We identified one prospective cohort study analyzing the association between cheese consumption, categorized in tertiles, and MetS risk (13). Moreover, one study analyzed the association between cheese consumption using continuous variables and the risk of MetS (16). As a consequence, a meta-analysis comparing the highest with the lowest categories was not performed, because only one study was available for the analysis. On the one hand, in the Prevención con Dieta Mediterránea (PREDIMED) study, a positive association between cheese consumption and MetS incidence was reported (RR: 1.31; 95% CI: 1.10, 1.56; comparing the third with the first tertile). On the other hand, in the Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) study, a lower risk of MetS was observed (RR: 0.82; 95% CI: 0.71, 0.95) with an increase in cheese consumption from one category to the next.
Discussion
We conducted a systematic review and meta-analysis of prospective cohort studies to investigate the relation between the intake of total dairy products and different subtypes of dairy and the risk of developing MetS. On the basis of the results of the analysis, comparing the highest with the lowest categories of dairy product consumption, we found an inverse association between total dairy, low-fat dairy, yogurt (total and its different subtypes), and total milk and the incidence of MetS. However, whole-fat dairy was not associated with the risk of MetS. The results of the dose-response analysis showed a decreased risk of developing MetS for each additional serving of yogurt per day.
Our results with regard to total dairy products are in line with those of the 2 previous meta-analyses (5, 6), even including the new published studies, and support our hypothesis that dairy product consumption is inversely associated with the risk of MetS. However, the previous meta-analyses had the limitation of including in the analysis studies that had different dairy subtypes as an exposure, instead of total dairy products. As a consequence, the results could not be attributed to total dairy product consumption. The present meta-analysis is the first, to our knowledge, that takes this aspect into account, showing a 27% lower risk of MetS associated with total dairy product intake.
To the best of our knowledge, this is the first time that a meta-analysis evaluating the association between different subtypes of dairy products, such as yogurt and milk, and the risk of MetS has been performed. It is important to note that few studies have been included for dairy product subtype analysis, which highlights the necessity of investigating the association between specific dairy products and MetS incidence, taking into account the fat content. Only 2 studies were found to evaluate low-fat dairy, whole-fat dairy, different types of yogurt, and MetS incidence, and only one study reported information comparing the highest with the lowest categories of cheese consumption. Moreover, it is important to point out that there was evidence of substantial heterogeneity in all dairy product categories, except for total and low-fat yogurt consumption. However, the observed heterogeneity disappeared after excluding one study (I2 = 38%, P = 0.13) (23) in the case of total dairy and another one in the case of total milk (I2 = 39%, P = 0.16) (22). The reasons are unclear, but could be related to sex [inclusion of only women (23)] or due to the comparison only between consumers and nonconsumers (22).
The potentially beneficial metabolic effects of dairy product consumption, such as milk, yogurt, and cheese, on MetS risk could be explained through their complex nutrient matrix. Calcium, the most concentrated mineral in dairy products, seems to interact with SFAs, forming FA-insoluble soaps, consequently decreasing fat absorption (25), lowering TG concentrations, and improving the HDL- to LDL-cholesterol ratio (26). Moreover, calcium has been related to decreased blood pressure in intervention studies (27, 28). These potentially beneficial effects of decreasing fat accumulation and blood pressure and regulating lipid metabolism have also been related to the milk-derived bioactive peptides modulating satiety and, consequentially, total energy intake, reducing weight gain (27, 29, 30).
Dairy products also contain saturated fats that have been related to increased peripheral HDL-cholesterol plasma concentrations and decreased VLDL cholesterol and remnant chylomicrons (31, 32). Polar lipids (phospholipids and sphingolipids) located in the membrane of dairy fat globules have been suggested to have anti-inflammatory properties, which could partially explain the inverse association with MetS (33). Dairy fat also contains SFAs and MUFAs that could improve insulin sensitivity and glycemic response (34, 35). This modulation of plasma glucose has also been related to probiotic bacteria. Fermented dairy products, such as yogurt and cheese, contain different bacterial strains (36) that may modulate gut microbiota and insulin sensitivity. In fermented milk and cheese, menaquinones seem to exert similar effects (34, 35). Moreover, probiotic bacteria from fermented dairy products could also modulate different inflammation reactions, reducing the abundance of pathogenic bacteria and increasing the production of some metabolites, such as SCFAs, through the fermentation of dietary fiber from fruits, vegetables, nuts, and legumes (37).
This meta-analysis has different strengths. It is the first systematic review and meta-analysis evaluating prospective studies reporting the relations between total dairy and different subtypes of dairy products and the risk of MetS. We followed stringent eligibility criteria using different databases to maximize the inclusion of high-quality, comparable studies. Most of the included studies were adjusted for important confounders, such as energy intake, smoking habit, age, sex, and physical activity. We assessed the linear and nonlinear dose-response between total dairy, yogurt, milk, and MetS incidence, although few studies were included.
The present meta-analysis also has potential limitations that should be considered. First, the analysis was based on observational studies and, for that reason, residual effects cannot be excluded from the results. Second, authors used different MetS criteria, which could change the effect estimates. However, due to the limited studies included in the analysis (<10), we could not conduct a subgroup analysis to clarify if this limitation affected the final results. The development of new MetS prevention strategies using a unified definition worldwide would be helpful. Third, although the dietary assessments were carried out with a validated FFQ in most of the prospective studies, a possible measurement error in recording the information during the assessment must be assumed. Fourth, we could not conduct subgroup analyses to explore the sources of interstudy heterogeneity observed in most of the analyses because there were not enough studies evaluating the relation between total and different subtypes of dairy products and the incidence of MetS. It is dubious that exploring heterogeneity will produce reliable results unless this would include >10 studies (38). Finally, in dairy subtype analyses, few studies were included. Therefore, it is likely that the publication of new studies evaluating different subtypes could change the magnitude or the direction of the effect estimates.
In conclusion, the results of the present systematic review and meta-analysis of prospective studies suggest that consumption of total and low-fat dairy, total yogurt and its different subtypes, and total milk is related to a reduced risk of MetS development. Furthermore, the consumption of whole-fat dairy has not been associated with the incidence of the syndrome. Due to the alarming prevalence of MetS, new dietary strategies to prevent this syndrome are imperative. The present results might provide deeper insight into dietary recommendations with regard to the consumption of dairy products and different dairy subtypes. Long-term randomized controlled trials conducted in different types of study populations (taking into account age, sex, health status, and ethnicity) and analyzing the effect of different dairy subtypes according to the fat and sugar composition are warranted to provide a definitive cause-effect relation between total dairy and different dairy subtypes and MetS incidence.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—GM-S, NB-T, NB, and JS-S: had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis and drafted the manuscript; NB, JS-S: study concept and design; GM-S, NB-T: statistical analyses; GM-S, NB-T, NB, and JS-S: critically revised the manuscript for important intellectual content and read and approved the final manuscript.
Notes
This supplement was sponsored by the Interprofessional Dairy Organization (INLAC), Spain.
The sponsor had no role in the design of the studies included in the supplement; in the collection, analyses, or interpretation of the data; in the writing of the manuscripts; or in the decision to publish the results. Publication costs for this supplement were defrayed in part by the payment of page charges. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
Supported by the Fondo de Investigación para la Salud, Instituto Carlos III, Madrid (projects PI13/00462 and PI16/00501) and Recercaixa (project 2013ACUP00194). None of the funding sources took part in the design, collection, analysis, or interpretation of the data or in the decision to submit the manuscript for publication.
Author disclosures: GM-S and NB-T, no conflicts of interest. NB received payments from Danone S.A. for the purposes of scientific and technical consulting but not for the preparation of this study. In addition, she is one of the members of the Scientific Advisory Board of the European Union program for the promotion of milk and milk products within the framework of appropriate dietary practices. JS-S is a member of Danone S.A.’s Scientific Advisory Board and the Executive Committee of Danone Institute Spain. He received payments from Danone S.A. for the purposes of scientific and technical consulting but not for the preparation of this manuscript.
GM-S and NB-T contributed equally to this work.
Supplemental Tables 1 and 2 and Supplemental Figures 1–7 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
References
- 1. Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart J-C, James WPT, Loria CM, Smith SC. Harmonizing the metabolic syndrome. Circulation. 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 2. Dunkley AJ, Charles K, Gray LJ, Camosso-Stefinovic J, Davies MJ, Khunti K. Effectiveness of interventions for reducing diabetes and cardiovascular disease risk in people with metabolic syndrome: systematic review and mixed treatment comparison meta-analysis. Diabetes Obes Metab. 2012;14:616–25. [DOI] [PubMed] [Google Scholar]
- 3. Pérez-Martínez P, Mikhailidis DP, Athyros VG, Bullo M, Couture P, Covas MI, de Koning L, Delgado-Lista J, Díaz-López A, Drevon CA et al.. Lifestyle recommendations for the prevention and management of metabolic syndrome: an international panel recommendation. Nutr Rev. 2017;75:307–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wannamethee SG, Shaper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: effects of lifestyle changes. J Am Geriatr Soc. 2006;54:1909–14. [DOI] [PubMed] [Google Scholar]
- 5. Chen G-C, Szeto IMY, Chen L-H, Han S-F, Li Y-J, van Hekezen R, Qin L-Q. Dairy products consumption and metabolic syndrome in adults: systematic review and meta-analysis of observational studies. Sci Rep. 2015;5:14606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim Y, Je Y. Dairy consumption and risk of metabolic syndrome: a meta-analysis. Diabet Med. 2016;33:428–40. [DOI] [PubMed] [Google Scholar]
- 7. Fumeron F, Lamri A, Abi Khalil C, Jaziri R, Porchay-Baldérelli I, Lantieri O, Vol S, Balkau B, Marre M, Ducimetière P et al.. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: results from a French prospective study, Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care. 2011;34:813–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shin H, Yoon YS, Lee Y, Kim C, Oh SW. Dairy product intake is inversely associated with metabolic syndrome in Korean adults: Anseong and Ansan cohort of the Korean Genome and Epidemiology Study. J Korean Med Sci. 2013;28:1482–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Internet]. Ottawa (Canada): Ottawa Hospital Research Institute; 2014. Available from: www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Accessed: 2018 16 May]. [Google Scholar]
- 10. Martínez-González MÁ, Hershey MS, Zazpe I, Trichopoulou A. Transferability of the Mediterranean diet to non-Mediterranean countries: what is and what is not the Mediterranean diet. Nutrients. 2017;9:E1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bekkering GE, Harris RJ, Thomas S, Mayer A-MB, Beynon R, Ness AR, Harbord RM, Bain C, Smith GD, Sterne JAC. How much of the data published in observational studies of the association between diet and prostate or bladder cancer is usable for meta-analysis?. Am J Epidemiol. 2008;167:1017–26. [DOI] [PubMed] [Google Scholar]
- 12. Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, Rahelic D, Sievenpiper JL, Salas-Salvadó J, Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials, Crit Rev Food Sci Nutr. 2019;24:1–21. [DOI] [PubMed] [Google Scholar]
- 13. Babio N, Becerra-Tomás N, Martínez-González MÁ, Corella D, Estruch R, Ros E, Sayón-Orea C, Fitó M, Serra-Majem L, Arós F et al.. Consumption of yogurt, low-fat milk, and other low-fat dairy products is associated with lower risk of metabolic syndrome incidence in an elderly Mediterranean population. J Nutr. 2015;145:2308–16. [DOI] [PubMed] [Google Scholar]
- 14. Sayón-Orea C, Bes-Rastrollo M, Martí A, Pimenta AM, Martín-Calvo N, Martínez-González MA. Association between yogurt consumption and the risk of metabolic syndrome over 6 years in the SUN study. BMC Public Health. 2015;15:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Damião R, Castro TG, Cardoso M, Gimeno SG, Ferreira SRG. Dietary intakes associated with metabolic syndrome in a cohort of Japanese ancestry. Br J Nutr. 2006;96:532–8. [PubMed] [Google Scholar]
- 16. Fumeron F, Lamri A, Abi Khalil C, Jaziri R, Porchay-Baldérelli I, Lantieri O, Vol S, Balkau B, Marre M; Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) Study Group. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: results from a French prospective study: Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care. 2011;34:813–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baik I, Lee M, Jun N-R, Lee J-Y, Shin C. A healthy dietary pattern consisting of a variety of food choices is inversely associated with the development of metabolic syndrome. Nutr Res Pract. 2013;7:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Louie JCY, Flood VM, Rangan aM, Burlutsky G, Gill TP, Gopinath B, Mitchell P. Higher regular fat dairy consumption is associated with lower incidence of metabolic syndrome but not type 2 diabetes. Nutr Metab Cardiovasc Dis. 2013;23:816–21. [DOI] [PubMed] [Google Scholar]
- 19. Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities Study. Circulation. 2008;117:754–61. [DOI] [PubMed] [Google Scholar]
- 20. Pereira MA, Jacobs DR, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA study. J Am Med Assoc. 2002;287:2081–9. [DOI] [PubMed] [Google Scholar]
- 21. Snijder MB, Van Dam RM, Stehouwer CDA, Hiddink GJ, Heine RJ, Dekker JM. A prospective study of dairy consumption in relation to changes in metabolic risk factors: the Hoorn study. Obesity. 2008;16:706–9. [DOI] [PubMed] [Google Scholar]
- 22. Lin Y-H, Chang H-T, Tseng Y-H, Lin M-H, Chen Y-C, Yang H-W, Chen T-J, Hwang S-J. Characteristics and health behavior of newly developed metabolic syndrome among community-dwelling elderly in Taiwan. Int J Gerontol. 2013;7:90–6. [Google Scholar]
- 23. Kim D, Kim J. Dairy consumption is associated with a lower incidence of the metabolic syndrome in middle-aged and older Korean adults: the Korean Genome and Epidemiology Study (KoGES). Br J Nutr. 2017;117:148–60. [DOI] [PubMed] [Google Scholar]
- 24. Kim J. Dairy food consumption is inversely associated with the risk of the metabolic syndrome in Korean adults. J Hum Nutr Diet. 2013;26(Suppl 1):171–9. [DOI] [PubMed] [Google Scholar]
- 25. Boon N, Hul GBJ, Stegen JHCH, Sluijsmans WEM, Valle C, Langin D, Viguerie N, Saris WHM. An intervention study of the effects of calcium intake on faecal fat excretion, energy metabolism and adipose tissue mRNA expression of lipid-metabolism related proteins. Int J Obes (Lond). 2007;31:1704–12. [DOI] [PubMed] [Google Scholar]
- 26. Lorenzen JK, Nielsen S, Holst JJ, Tetens I, Rehfeld JF, Astrup A. Effect of dairy calcium or supplementary calcium intake on postprandial fat metabolism, appetite, and subsequent energy intake. Am J Clin Nutr. 2007;85:678–87. [DOI] [PubMed] [Google Scholar]
- 27. Bucher HC, Cook RJ, Guyatt GH, Lang JD, Cook DJ, Hatala R, Hunt DL. Effects of dietary calcium supplementation on blood pressure: a meta-analysis of randomized controlled trials. JAMA. 1996;275:1016–22. [DOI] [PubMed] [Google Scholar]
- 28. van Mierlo LAJ, Arends LR, Streppel MT, Zeegers MPA, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to calcium supplementation: a meta-analysis of randomized controlled trials. J Hum Hypertens. 2006;20:571–80. [DOI] [PubMed] [Google Scholar]
- 29. Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E. Dairy augmentation of total and central fat loss in obese subjects. Int J Obes (Lond). 2005;29:391–7. [DOI] [PubMed] [Google Scholar]
- 30. Zemel MB, Richards J, Milstead A, Campbell P. Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes Res. 2005;13:1218–25. [DOI] [PubMed] [Google Scholar]
- 31. van Schalkwijk DB, Pasman WJ, Hendriks HFJ, Verheij ER, Rubingh CM, van Bochove K, Vaes WHJ, Adiels M, Freidig AP, de Graaf AA. Dietary medium chain fatty acid supplementation leads to reduced VLDL lipolysis and uptake rates in comparison to linoleic acid supplementation. PLoS One. 2014;9:e100376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bonham MP, Linderborg KM, Dordevic A, Larsen AE, Nguo K, Weir JM, Gran P, Luotonen MK, Meikle PJ, Cameron-Smith D et al.. Lipidomic profiling of chylomicron triacylglycerols in response to high fat meals. Lipids. 2013;48:39–50. [DOI] [PubMed] [Google Scholar]
- 33. Lordan R, Zabetakis I. Invited review: the anti-inflammatory properties of dairy lipids. J Dairy Sci. 2017;100:4197–212. [DOI] [PubMed] [Google Scholar]
- 34. Ejtahed HS, Mohtadi-Nia J, Homayouni-Rad A, Niafar M, Asghari-Jafarabadi M, Mofid V. Probiotic yogurt improves antioxidant status in type 2 diabetic patients. Nutrition. 2012;28:539–43. [DOI] [PubMed] [Google Scholar]
- 35. Parvez S, Malik KA, Ah Kang S, Kim H-Y. Probiotics and their fermented food products are beneficial for health. J Appl Microbiol. 2006;100:1171–85. [DOI] [PubMed] [Google Scholar]
- 36. McSweeney PLH, Ottogalli G, Fox PF. Diversity of cheese varieties: an overview, Cheese: Chemistry, Physics and Microbiology. 2004;2:1–23. [Google Scholar]
- 37. Veiga P, Pons N, Agrawal A, Oozeer R, Guyonnet D, Brazeilles R, Faurie J-M, van Hylckama Vlieg JET, Houghton LA, Whorwell PJ et al.. Changes of the human gut microbiome induced by a fermented milk product. Sci Rep. 2015;4:6328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Higgins JPT, , Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011], [Internet]. [cited 2018 May 23] The Cochrane Collaboration; 2011. Available from: http://handbook.cochrane.org. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.