ABSTRACT
Dairy product consumption has been related to type 2 diabetes (T2D) incidence, although data from epidemiological studies have shown mixed results regarding the association of dairy products and T2D risk. This overview of systematic reviews and meta-analyses aimed to examine the scientific literature available on the association between dairy product consumption and T2D risk. A literature search was conducted in the MEDLINE (via PubMed), EMBASE, Cochrane Central Database of Systematic Reviews, and Web of Science databases from their inception to April, 2018. Forest plots summarized the risk ratios (RRs) reported by meta-analyses on high compared with low and dose–response dairy product consumption. The risk of bias was assessed using the AMSTAR2 tool. We included 12 meta-analyses, reporting data from 4–22 cohort studies and from 4–23 populations. The participants’ ages ranged from 20 to 88 y, and participants were followed up for from 4 to 30 y. Studies included 64,227–566,875 participants and reported 4810–44,474 cases of T2D. Most studies reported an inverse association between T2D incidence and dairy product consumption, especially for 1) total dairy products (range: 0.86–0.91), 2) low-fat dairy products (range: 0.81–0.83), 3) low-fat milk (RR: 0.82), and 4) yogurt (range: 0.74–0.86). Dose–response analyses showed a decreased T2D risk for 1) 200–400 g/d of total dairy products (range: 0.93–0.97) and 2) 200 g/d of low-fat dairy products (range: 0.88–0.91). Total dairy product consumption is associated with a lower risk of T2D, especially for yogurt and low-fat dairy consumption. The association with cheese is moderate. Moreover, dose–response analyses showed that the risk of T2D decreased by each unit increase in consumption of total dairy products and low-fat dairy products.
Keywords: dairy products, milk, cheese, yogurt, diabetes mellitus, type 2 diabetes, meta-analysis, review
Introduction
Type 2 diabetes (T2D) is one of the most common chronic diseases associated with multiple factors, including weight gain, dietary pattern, and physical inactivity (1, 2). Approximately 366 million people worldwide have diabetes (3), its global estimated prevalence is 8.5% (4), and the age-adjusted incidence is ∼6.7 per 1000 persons (5); moreover, by 2030, T2D will affect an estimated 552 million people worldwide (3). Progression of T2D results in other associated complications, the management of which imposes social, medical, and economic burdens (3, 6). Early control of T2D is crucial in preventing progression of the disease. Indeed, many of the complications could be alleviated through simple and inexpensive dietary modifications (7, 8).
The link between dietary factors and the risk of T2D has long been studied. Previous meta-analyses have shown that overall diet quality, such as the Mediterranean diet score or Dietary Approaches to Stop Hypertension (DASH), is associated with a significant decrease in T2D risk (9–11). In terms of specific food groups, the dairy group has gained attention owing to the health effects associated with some of its components. For example, calcium and magnesium, 2 minerals found in dairy products, are associated with a lower incidence of T2D and insulin resistance (12). Whey protein showed insulinotropic effects and glucose-lowering properties through insulin and incretin secretion (13, 14). Vitamin D is supplied in fortified dairy products. Fortification of dairy foods with vitamin D is performed systematically in some countries (15) and nonsystematically in others (16), is associated with multiple metabolic health benefits, and recent findings suggest that dietary fatty acids such as trans-palmitoleic acid are inversely associated with T2D risk and that SCFAs have an important role in the control of body weight and insulin sensitivity (17–20). However, other studies reported that the aforementioned health benefits might be offset by SFAs. Nevertheless, the detrimental effects of SFAs could be nullified when they are consumed as part of complex food matrices, such as those in milk, yogurt, cheese, and other dairy foods (21).
Data from epidemiological studies have shown mixed results regarding the association of dairy products and dairy subtypes with T2D risk. For instance, whereas some concluded that total dairy consumption was negatively associated with T2D risk (9, 22–26), others showed nonsignificant associations or inconclusive results (27, 28). In addition, prior meta-analyses showed an inverse association between yogurt consumption and risk of T2D (22–25, 27, 28). However, the conclusions on yogurt dose–response remain unclear (23, 27, 28). Among other studies of subtypes of dairy products, some meta-analyses found an inverse association of low-fat dairy products (22, 23, 25, 29) and low-fat milk (22, 23) with T2D risk, but not all reports reached the same conclusions (26), especially with regard to whole-fat dairy products (22–25, 29). Although meta-analyses and systematic reviews are meant to be conclusive, the evidence is not sufficient to draw conclusions and a more comprehensive evaluation is necessary. Therefore, from an overarching perspective, we conducted an overview of existing systematic reviews and meta-analyses to clarify conflicting results and examine the scientific literature available for the association between milk and dairy product consumption (high compared with low and dose–response) and T2D risk, including different subtypes of dairy products.
Methods
This overview of systematic reviews and meta-analyses is reported according to the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) (30) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (31) statements, following the recommendations of the Cochrane Collaboration Handbook (32), and was registered through the International Prospective Register of Systematic Reviews (PROSPERO) as CRD42018091910.
Search strategy
We used 3 methods to search for systematic reviews or meta-analyses that were relevant for this study. First, we systematically searched the MEDLINE (via PubMed), EMBASE, Cochrane Database for Systematic Reviews, and Web of Science databases from their inception until April, 2018. Systematic reviews and meta-analyses addressing the association of dairy product consumption with T2D were eligible. Second, the literature search was complemented by screening references included in previous systematic reviews and meta-analyses. Finally, we searched the websites of organizations aimed at conducting meta-analyses or at compiling meta-analyses (the Cochrane Database of Systematic Reviews; the TRIP database). The search strategy is presented in Supplemental Table 1.
Study selection
Inclusion criteria were as follows: 1) participants: adult population; 2) study design: meta-analyses of observational studies (including cohort and case-control studies); 3) exposure: dairy product consumption (total dairy, milk, cheese, yogurt, or other dairy products such as ice cream, butter, sherbet, and cream); and 4) outcome: incidence of T2D.
The exclusion criteria were as follows: 1) studies written in languages other than English or Spanish and 2) narrative reviews and reviews that did not follow the methodology of a systematic review (33). No date restriction was applied to the study selection.
Data extraction and quality assessment
The following data were extracted from the original reports: 1) first author and year of publication; 2) number of studies included; 3) length of follow-ups; 4) sample characteristics (age distribution, number of subjects, and number of cases); 5) type of dairy product assessed; 6) risk ratio (RR) estimates; 7) heterogeneity reported and its P value; and 8) AMSTAR 2 risk of bias category (29). Moreover, the individual studies included in each meta-analysis and the covariates used in their analyses were extracted (Supplemental Table 2).
The AMSTAR 2 tool (34) was used to evaluate the risk of bias in the included meta-analyses and to detect weaknesses in specific domains that could threaten the validity of the included systematic reviews and meta-analyses. The checklist consists of 16 criteria, each referring to a relevant methodological aspect of a study. Plausible scores were “no” (0 points) when the study did not meet the criteria, “yes” (1 point) when the study met the criteria, and “partial yes” (0.5 points) when studies reported partial information on the scored item. The quality score for each study could range from 0 to 16. According to the number of criteria the studies met, the quality score was categorized into 5 groups as follows: excellent, 15–16 points; very good, 12–14 points; good, 9–11 points; acceptable, 6–8 points; and deficient, 3–5 points.
The literature search, data extraction, and quality assessment were independently performed by 2 reviewers (IC-R and CA-B); inconsistencies were resolved by consensus and involved a third researcher when consensus was not reached (VM-V).
Data synthesis
Forest plots were used to summarize the pooled RR estimates for the association between dairy product consumption and T2D incidence. From the included meta-analyses, dose–response and high compared with low dairy consumption analyses were separately depicted in forest plots including information by type of dairy product (total dairy product, milk, cheese, and yogurt). Information on the amount of dairy product reported by each meta-analysis related with T2D RR was included in the forest plots. For inclusion in the forest plot, the pooled RR reported by each meta-analysis should include ≥4 studies. Forest plot graphs were performed using StataSE software, version 15 (StataCorp).
Results
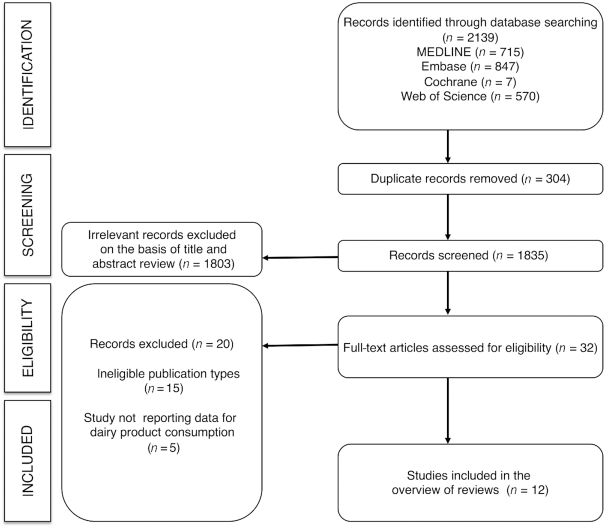
The PRISMA flow diagram is presented in Figure 1. From the 1761 full-text articles identified, 12 systematic reviews and meta-analyses (9, 22–25, 27–29, 35–38) quantifying the association between dairy consumption and T2D and meeting the inclusion criteria were included in the overview of reviews. Table 1 presents descriptive information for the included studies.
FIGURE 1.
Literature search: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
TABLE 1.
Characteristics of the systematic reviews and meta-analyses included in this review1
| Reference | n | Age (y) | Follow-up (y) | n (cases) | Exposure observed | RR (95% CI) | I 2 (%) | P | Risk of bias (AMSTAR) |
|---|---|---|---|---|---|---|---|---|---|
| Aune et al. (22) | 17 cohort studies (18 populations) | 20–75 | 5–23 | 426,055 (26,976) 196,799 (7222) 278,875 (11,168) 167,982 (15,149) 242,960 (17,620) 254,892 (19,082) NA | Total dairy products2 400 g/d dairy products3 High-fat dairy products2 200 g/d dairy products3 Low-fat dairy products2 200 g/d low-fat dairy products Milk2 200 g/d milk3 Cheese2 50 g/d cheese3 Yogurt2 200 g/d yogurt Other products: Whole milk2 200 g/d whole milk3 Low-fat or skim milk2 Per 200 g/d low-fat or skim milk3 Cottage cheese2 Cream2 Fermented dairy products2 Ice cream2 Sherbet2 Sour cream2 | 0.89 (0.82, 0.96)* 0.93 (0.87, 0.99)* 0.96 (0.87, 1.06) 0.98 (0.94, 1.03) 0.83 (0.76, 0.90)* 0.91 (0.86, 0.96)* 0.87 (0.70, 1.07) 0.87 (0.72, 1.04) 0.91 (0.84, 0.98)* 0.92 (0.86, 0.99)* 0.86 (0.75, 0.98)* 0.78 (0.60, 1.02) 1.12 (0.99, 1.27) 1.06 (0.93, 1.20) 0.82 (0.69, 0.97)* 0.89 (0.84, 0.95)* 0.91 (0.79, 1.04) 0.96 (0.84, 1.11) 0.88 (0.79, 0.98)* 0.83 (0.73, 0.95)* 0.90 (0.79, 1.03) 0.98 (0.82, 1.16) | 42.1 33.1 15.8 7.6 0 40.2 70.5 93.6 0 0 58.9 69.9 0 22.5 40.1 0 0 4.9 0 0 0 0 | 0.05 0.13 0.31 0.37 0.67 0.10 0.002 <0.0001 0.57 0.79 0.02 0.003 0.79 0.28 0.19 0.57 0.43 0.31 0.99 0.37 0.60 0.54 | Good |
| Chen et al. (27) | 11 cohort studies (14 populations) | 21–79 | 5–30 | 459,790 (35,863) | Total dairy products2 1 serving/d yogurt3 | 0.98 (0.96, 1.01) 0.82 (0.70, 0.96)* | 58.8 63.2 | 0.003 0.005 | Good |
| Elwood et al. (35) | 4 cohort studies (4 populations) | NA | 8–20 | 120,263 (4851) | Milk2 | 0.92 (0.86, 0.97)* | NA | NA | Acceptable |
| Elwood et al. (36) | 5 cohort studies (5 populations) | NA | 7–25 | 184,454 (7121) | Milk2 | 0.85 (0.75, 0.96)* | NA | 0.122 | Acceptable |
| Gao et al. (23) | 15 cohort studies and 1 case control study (18 populations) | 21–79 | 5–23 | 457,893 (27,095) 260,700 (9398) 260,700 (9398) 327,039 (21,755) 88,323 (2898) 84,019 (2515) 178,429 (14,810) 254,552 (18,532) NA NA NA | Total dairy products2 200 g/d total dairy products3 Full-fat dairy products2 200 g/d full-fat dairy products3 Low-fat dairy products2 200 g/d low-fat dairy products3 Milk2 200 g/d milk3 Full-fat milk2 200 g/d full-fat milk3 Low-fat milk2 200 g/d low-fat milk3 Cheese2 30 g/d cheese3 Yogurt2 50 g/d yogurt3 Cream2 Ice cream2 Fermented dairy products2 | 0.89 (0.81, 0.98)* 0.94 (0.91, 0.97)* 0.95 (0.85, 1.07) 0.95 (0.88, 1.04) 0.81 (0.74, 0.89)* 0.88 (0.84, 0.93)* 0.89 (0.78, 1.01) 0.89 (0.79, 1.01) 1.12 (0.99, 1.27) 1.27 (0.97, 1.67) 0.82 (0.69, 0.97)* 0.83 (0.70, 1.00) 0.82 (0.77, 0.87)* 0.80 (0.69, 0.93)* 0.85 (0.75, 0.97)* 0.91 (0.82, 1.00) 0.96 (0.84, 1.12) 0.84 (0.73, 0.95)* 0.94 (0.75, 1.18) | 65.4 51.9 38.1 52.2 1.8 16.3 51.8 66.3 0 0 40.1 14.0 0 59 55.4 74 NA NA NA | 0.000 0.002 0.126 0.041 0.416 0.32 0.043 0.005 0.792 0.58 0.188 0.21 0.82 0.02 0.02 0.001 NA NA NA | Very good |
| Gijsbers et al. (28) | 22 cohort studies (23 populations) | 36–67 | 2.6–30 | 489,113 (38,993) 327,895 (24,034) 405,667 (27,597) 145,472 (17,241) 336,102 (21,995) 267,607 (20,098) 369,697 (32,936) 438,140 (36,125) 258,571 (19,730) 258,571 (19,730) 231,642 (16,759) | 200 g/d total dairy products3 200 g/d high-fat dairy products3 200 g/d low-fat dairy products3 200 g/d total milk3 200 g/d high-fat milk3 200 g/d low-fat milk3 10 g/d cheese3 50 g/d yogurt3 5 g/d cream3 10 g/d ice cream3 10 g/d sherbet3 | 0.97 (0.95, 1.00) 0.98 (0.93, 1.04) 0.96 (0.92, 1.00) 0.97 (0.93, 1.02) 0.99 (0.88, 1.11) 1.01 (0.97, 1.05) 1.00 (0.99, 1.02) 0.94 (0.90, 0.97)* 0.99 (0.97, 1.01) 0.84 (0.78, 0.85)* 1.00 (0.97, 1.02) | 66.4 51.6 68.0 57.4 84.1 71.6 61.7 73.3 33.6 85.7 33.1 | <0.001 0.016 <0.001 0.007 <0.001 0.002 0.002 0.000 0.198 0.000 0.214 | Very good |
| Khoramdad et al. (29) | 13 cohort studies (14 populations) | 40–88 | 5.5–20 | 79,241 (3231) 150,185 (6086) 76,510 (2683) | Milk2 Cheese2 Yogurt2 | 0.89 (0.82, 0.97)* 0.92 (0.82, 1.04) 0.74 (0.65, 0.84)* | 0 17.3 51.1 | 0.515 0.304 0.085 | Very good |
| Khoramdad et al. (37) | 14 cohort studies (16 populations) | 20–79 | 5–10 | 154,843 (6865) 10,137 (1171) 92,213 (5117) | Total dairy products2 High-fat dairy products2 Low-fat dairy products2 | 0.88 (0.80, 0.96)* 0.98 (0.78, 1.24) 0.81 (0.68, 0.96)* | 32.9 53.6 65.6 | 0.166 0.116 0.033 | Very good |
| Pimpin et al. (38) | 4 cohort studies (11 populations) | 26–65 | 12.3–23 | 201,628 (23,954) | 14 g/d butter3 | 0.96 (0.93, 0.99)* | 46.8 | 0.131 | Very good |
| Schwingshackl et al. (9) | 21 cohort studies (NA) | 20–88 | 4.1–30 | 566,872 (44,474) | Total dairy products2 200 g/d of dairy products3 | 0.91 (0.85, 0.97)* 0.97 (0.94, 0.99)* | 63.0 74.0 | <0.0001 <0.00001 | Very good |
| Tian et al. (24) | 9 cohort studies (11 populations) | 25–80 | 4.1–25 | 282,771 (10,381) 222,335 (9226) 207,026 (7896) | Total dairy products2 Whole milk2 Yogurt2 | 0.89 (0.84, 0.94)* 0.87 (0.78, 0.96)* 0.83 (0.70, 0.98)* | 48.81 52.20 62.06 | 0.03 0.01 0.007 | Good |
| Tong et al. (25) | 7 cohort studies (8 populations) | 39–57 | 5–20 | 263,838 (10,808) 119,623 (4810) 119,623 (4810) 202,424 (6230) 138,233 (3960) | Total dairy products2 1 serving/d total dairy products3 High-fat dairy products2 1 serving/d high-fat dairy products3 Low-fat dairy products2 1 serving/d low-fat dairy products3 Whole milk2 Yogurt2 | 0.86 (0.79, 0.92)* 0.94 (0.92, 0.97)* 1.00 (0.89, 1.10) 0.98 (0.92, 1.05) 0.82 (0.74, 0.90)* 0.90 (0.85, 0.95)* 0.95 (0.86, 1.05) 0.83 (0.74, 0.93)* | 29.7 NA NA NA NA NA NA NA | NA NA NA NA NA NA NA NA | Good |
1*P < 0.05. NA, not available; RR, risk ratio.
2High compared with low consumption.
3Per each consumption increment of the named dairy product.
The identified systematic reviews and meta-analyses were published between 2008 and 2017. The number of studies ranged from 4 to 22 cohort studies and included data from 4–23 populations. In addition, 1 systematic review and meta-analysis included 1 case-control study. The age of the included participants ranged between 20 and 88 y of age, and the follow-up duration ranged from 4 to 30 y. The sample size ranged from 64,227 to 566,875, and the reported cases of T2D ranged from 4810 to 44,474. The original studies included in the systematic reviews and meta-analyses were developed in the United States (12 studies), United Kingdom (3 studies), Australia (2 studies), China (2 studies), and Sweden (2 studies). In addition, 1 study from each of the following countries was reported: Finland, France, Germany, Iran, Japan, Netherlands, Puerto Rico, and Spain. Finally, 1 study including data from Europe and another with multicountry data were included.
Ten systematic reviews and meta-analyses reported an exposure comparison between high and low dairy product consumption (9, 22–25, 27, 29, 35–37) and 7 reported dose–response consumptions (9, 22, 23, 25, 27, 28, 38). Most of the studies reported data on the association of total dairy product, milk, and yogurt consumption (9, 22–25, 27–29, 35–37) with T2D incidence. Four studies reported cheese consumption (22, 23, 28, 37); data from high-fat dairy, low-fat dairy, and fermented products (including yogurt, cheese, and buttermilk) were reported in other studies (22, 23, 24, 29). In addition, 3 reported ice cream consumption (22, 23, 28), 1 reported butter (38), and others examined sherbet (frozen dessert containing sweetened, diluted fruit with 0.5–2% dairy fat content), cream, and sour cream consumption (22, 23, 28, 38).
The heterogeneity as measured by I2 in the systematic reviews and meta-analyses ranged from 0.0% to 93.6%. The list of original studies addressing the association of dairy consumption with T2D that were included in the systematic reviews and meta-analyses is given in Supplemental Table 2.
Risk of bias
As evaluated by the AMSTAR 2 tool, 16.7% of the systematic reviews and meta-analyses showed an acceptable risk of bias, 33.3% had a good risk of bias, and 50.0% had a very good risk of bias. When individual domains were analyzed, all studies had shortcomings in reporting the list of excluded studies and the funding information of the original studies (Supplemental Table 3).
Data synthesis
High compared with low consumption analyses
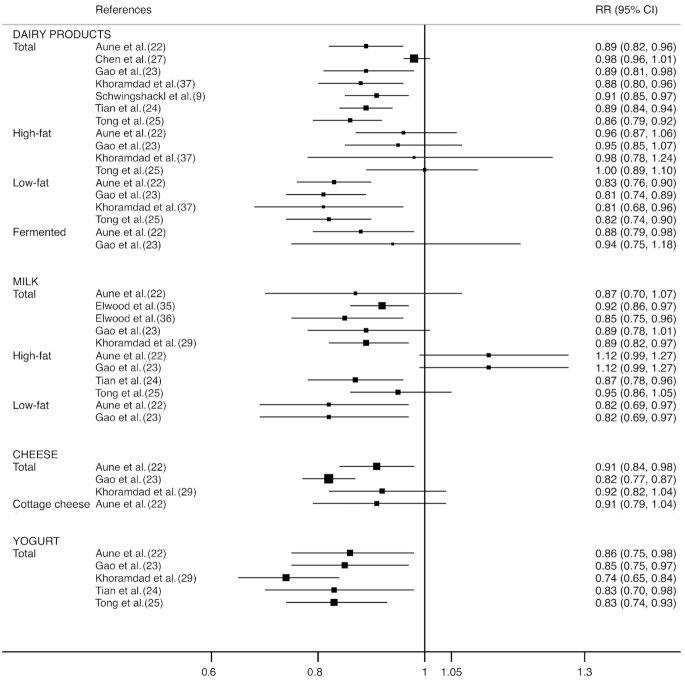
Figure 2 displays a forest plot with the summary effect on T2D risk for high compared with low consumption of each dairy product. For total dairy products, RRs ranged from 0.81 to 1.00, showing a significant effect in 6 out of 7 studies (85.7%) (RR range: 0.86–0.91). All of the studies analyzed reported a significant inverse association for low-fat dairy products (RR range: 0.81–0.83). No study found a significant association for high-fat dairy products, and 1 out of 2 studies of fermented dairy products showed a significant association (RR: 0.88; 95% CI: 0.79, 0.98) (18).
FIGURE 2.
Forest plot for the association between high compared with low dairy product consumption and risk of type 2 diabetes by type of dairy product. RR, risk ratio.
For milk consumption, RRs ranged from 0.82 to 1.12, 3 out of 5 studies (60%) found significant effects for total milk consumption (RR range: 0.85–0.92), and all studies found significant effects for low-fat milk consumption (RR: 0.82; 95% CI: 0.69, 0.97) (18, 19). Furthermore, a significant effect was found in 1 out of 4 studies of high-fat milk consumption (RR: 0.87; 95% CI: 0.78, 0.96) (20) (see Figure 2).
For cheese and cottage cheese consumption, RRs ranged from 0.82 to 0.92 and were significant in 2 of 4 studies (RR: 0.82; 95% CI: 0.77, 0.87; and RR: 0.91; 95% CI: 0.82, 0.98). The study for cottage cheese did not find statistical significance (RR: 0.91; 95% CI: 0.79, 1.04).
For yogurt consumption, the RRs ranged from 0.74 to 0.86, and all 5 studies analyzed showed a significant association with T2D.
Dose–response analyses
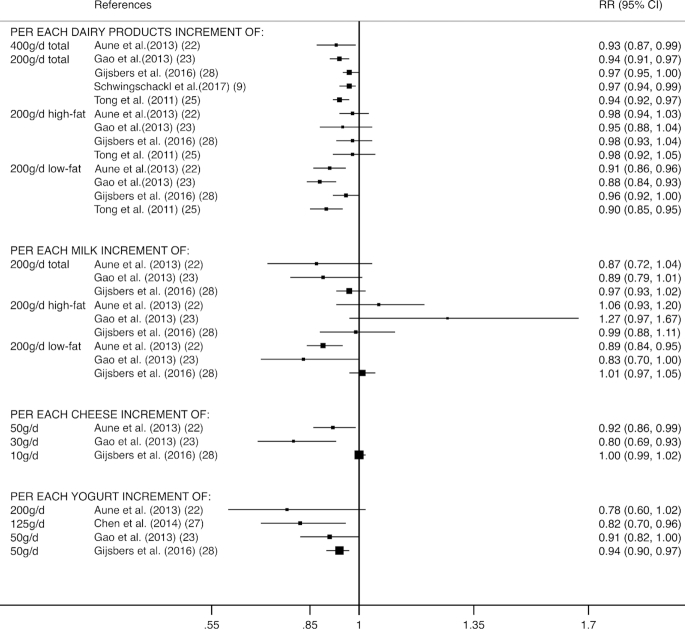
A forest plot with dose–response analyses for the consumption of each dairy product is depicted in Figure 3. For dairy product consumption, RRs ranged from 0.88 to 0.98, showing a significant association in 4 out of 5 studies for 200–400 g/d of total dairy product consumption (RR range: 0.93–0.97) and 3 out of 4 studies for 200 g/d of low-fat dairy product consumption (RR range: 0.88–0.91). No studies including high-fat dairy product consumption showed significant effects.
FIGURE 3.
Forest plot for the association of dose–response dairy product consumption with risk of type 2 diabetes by type and amount of dairy product. RR, risk ratio.
For milk consumption, RRs ranged from 0.83 to 1.27, showing a significant effect in 1 study out of 3 for 200 g/d of low-fat milk consumption (RR: 0.89; 95% CI: 0.84, 0.95) (18). Studies including total milk and high-fat milk showed no significant effects.
For cheese consumption, RRs ranged from 0.80 to 1.00 and were significant in 2 of the 3 studies (RR: 0.80; 95% CI: 0.69, 0.93; and RR: 0.92; 95% CI: 0.86, 0.99).
For yogurt consumption, RRs ranged from 0.78 to 0.94, showing a significant effect in 2 studies out of 4 (RR: 0.82; 95% CI: 0.70, 0.96; and RR: 0.94; 95% CI: 0.90, 0.97).
Discussion
This overview of systematic reviews and meta-analyses provides a synthesis of the state of knowledge for the association between dairy product consumption and risk of T2D. The data from this study provide evidence supporting the association of total dairy product consumption with a lower risk of T2D, as this evidence is more robust for yogurt consumption and low-fat dairy. The association with cheese is moderate, and no association was found for high-fat dairy. Moreover, our data support a dose–response association in which the risk of T2D is decreased by each unit increase in consumption of total dairy products (200–400 g) or low-fat dairy products (200 g/d).
In this overview, 6 out of the 7 studies comparing high with low consumption of total dairy products reported a lower T2D risk. In contrast, Chen et al. (27) reported no significant association of total dairy product consumption with T2D risk in their meta-analyses of 14 studies (RR: 0.98; 95% CI: 0.96, 1.01) and in their separate updated analysis of 3 cohorts (RR: 1.00; 95% CI: 0.98, 1.02). However, previous studies that included a shorter follow-up showed an inverse association of low-fat and total dairy consumption with T2D in the same populations (39, 40). The authors suggested that the potential benefits of dairy were less evident with longer follow-up periods, which was later supported by Gijsbers et al. (28) in a subgroup analysis (>10 y follow-up) where they found no associations with total or low-fat dairy consumption. In the studies that quantified the association, 200 g/d of total dairy products was associated with lower (3–6%) T2D risk (9, 23, 25, 28), and only 1 study found a 6% lower T2D risk per 400 g/d (22). This association was probably mostly driven by low-fat dairy products where all (22, 23, 25) except one (26) (with a borderline association) of the systematic reviews and meta-analyses found a significant association of 200 g/d of low-fat dairy with a lower (4–12%) T2D risk. Consistent results were found for a lower T2D risk (17–19%) when comparing high with low consumption for all the studies reviewed (22, 23, 25, 29).
For milk consumption, low-fat milk was consistently associated with a lower risk of T2D (22, 23, 25), except in the study of Gijsbers et al. (28), where 200 g/d (0.83 servings/d) was not associated with T2D risk. However, there was no evidence for an association with high-fat milk consumption (22, 23, 28). For total milk consumption, only Elwood et al. (35, 36) and Khoramdad et al. (37) reported a protective effect on T2D risk. However, based on the risk of bias, the smaller number of studies analyzed, and the confounder variables that the studies included, we are not able to draw any robust conclusion for their recommendations. Further research is warranted to shed some light on this issue.
Dairy products are an important source of calcium, magnesium, vitamin D, and protein and are suggested to have favorable health effects on body weight (41), glucose (42), and hypertension (43). Although calcium has been associated with lower blood glucose, few original studies have been able to adjust for calcium or magnesium to show independent effects. Thus, we must interpret the results with caution and in the context of when the studies were conducted. Not only has global dairy consumption changed over the last few decades (44), but dietary guidelines that were based on a low-fat diet might have influenced the consumption towards a low-fat type of dairy products. However, strong evidence has shown that when addressing the effects of fat, health benefits are heavily dependent on the macronutrient that is replaced (45). Therefore, adjusting for other dietary factors is important because dairy consumption might be associated with other dietary practices that can bias the results (46). Unfortunately, some but not all studies have been able to do so, which makes interpretation of the results difficult.
For yogurt consumption, all the studies included in this overview reported a consistent and clear protective effect when comparing high with low consumption, and lower (14–26%) T2D risk. In the linear dose–response studies, 3 out of 4 studies showed a significant and inverse association with T2D risk; however, the dose reported varied across studies (50–200 g/d or 0.5–2 servings/d) with a suggested nonlinear association (22), as shown by the latest meta-analysis (26), which indicated that a consumption of 80–125 g/d was related to a 14% lower T2D risk. Of note, we were unable to distinguish between plain and sugar-sweetened yogurt and high- or low-fat yogurt; however, a recent study in a Spanish population showed that both low- and high-fat yogurt were associated with T2D (47). Researchers have attempted to elucidate whether the different types of dairy SFAs, including odd-numbered SFAs (15:0 and 17:0), methyl-branched-chain SFAs, and trans-palmitoleic acid, may have health benefits (18, 46, 48–50). Two studies found that trans-palmitoleic acid was associated with a lower incidence of T2D (18), which may offset the unfavorable effects of SFAs in high-fat dairy products. However, in light of the evidence from the observational studies, our results do not support the association of high-fat dairy products and T2D risk in any direction, suggesting that more research is needed in that regard.
For cheese consumption, Aune et al. (22) and Gao et al. (23) reported a significant inverse association with T2D risk at dosages of 30 and 50 g/d (0.33 and 0.5 servings/d), respectively. However, no association was found per 10 g/d, and mixed results were found when comparing high and low consumption, with significant heterogeneity between the various individual cohorts (22, 23, 29). We were not able to differentiate among the different types of cheese, which have different fat and sodium contents; thus, more evidence is needed to reach firm conclusions about cheese consumption recommendations for T2D.
Some limitations should be considered in this overview of systematic reviews and meta-analyses. First, some primary studies are included in most systematic reviews and meta-analyses in this synthesis of evidence, thus, the influence of these studies is inflated; fortunately, this overlapping evidence comes from the largest and well-designed cohort studies. Second, the results of the included systematic reviews and meta-analyses seem to be consistent although the included systematic reviews and meta-analyses were published across a wide date range (from 2008 to 2017), and included a range of follow-up durations from 2.6 to 30 y. In addition, the meta-analyses that included a sensitivity analysis (22, 23) considering <10 y and >10 y of follow-up found no differences in pooled RR. Third, the amount of dairy product consumption for the dose–response analyses varied across studies; thus, these results should be interpreted with caution. Finally, because the search was limited to articles published in English or Spanish and unpublished literature was not consulted, the language restrictions and unpublished studies might slightly modify our results. Moreover, owing to the inherent nature of the methods used in this review, publication bias could not be tested.
In conclusion, the results of this synthesis suggest that dairy consumption, particularly low-fat dairy and yogurt (80–125 g/d), is associated with a lower risk of T2D. This is important from a public health point of view because the results may inform practitioners, policy-makers, and diabetes scientific associations’ recommendations. However, the evidence is still null or weak with regard to high-fat dairy, and more research is warranted to differentiate fat content in dairy products (high or low) and fat and sweetener content of yogurt. Studies with the ability to adjust for other food components and conduct substitution analysis may provide the strongest evidence given the lack of randomized control trials.
Supplementary Material
Acknowledgments
All authors read and approved the final manuscript.
Notes
This supplement was sponsored by the Interprofessional Dairy Organization (INLAC), Spain. The sponsor had no role in the design of the studies included in the supplement; in the collection, analyses, or interpretation of the data; in the writing of the manuscripts; or in the decision to publish the results. This study was partially funded by the University of Granada Plan Propio de Investigación 2016, Excellence actions: Unit of Excellence on Exercise and Health (UCEES), Plan Propio de Investigación 2018, Programa Contratos-Puente, the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades, and European Regional Development Funds (ref. SOMM17/6107/UGR). Publication costs for this supplement were defrayed in part by the payment of page charges. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
Author disclosures: CA-B, IC-R, VM-V, MS-P, JRR, and AG, no conflicts of interest.
Supplemental Tables 1–3 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances.
References
- 1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. [DOI] [PubMed] [Google Scholar]
- 2. Stevens JW, Khunti K, Harvey R, Johnson M, Preston L, Woods HB, Davies M, Goyder E. Preventing the progression to type 2 diabetes mellitus in adults at high risk: a systematic review and network meta-analysis of lifestyle, pharmacological and surgical interventions. Diabetes Res Clin Pract. 2015;107:320–31. [DOI] [PubMed] [Google Scholar]
- 3. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Global Report on Diabetes. Geneva: World Health Organization; 2016. [Google Scholar]
- 5. Centers for Disease Control and Prevention. Incidence of diagnosed diabetes. [Internet] Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation; 2018; [cited 20 Sep, 2018]. Available from: https://www.cdc.gov/diabetes/data/statistics-report/incidence-diabetes.html. [Google Scholar]
- 6. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pasin G, Comerford KB. Dairy foods and dairy proteins in the management of type 2 diabetes: a systematic review of the clinical evidence. Adv Nutr. 2015;6:245–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maghsoudi Z, Ghiasvand R, Salehi-Abargouei A. Empirically derived dietary patterns and incident type 2 diabetes mellitus: a systematic review and meta-analysis on prospective observational studies. Public Health Nutr. 2016;19:230–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schwingshackl L, Hoffmann G, Lampousi AM, Knüppel S, Iqbal K, Schwedhelm C, Bechthold A, Schlesinger S, Boeing H. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32:363–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115:780–800. [DOI] [PubMed] [Google Scholar]
- 11. Schwingshackl L, Missbach B, Konig J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr. 2015;18:1292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dong JY, Xun P, He K, Qin LQ. Magnesium intake and risk of type 2 diabetes: meta-analysis of prospective cohort studies. Diabetes Care. 2011;34:2116–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jakubowicz D, Froy O. Biochemical and metabolic mechanisms by which dietary whey protein may combat obesity and type 2 diabetes. J Nutr Biochem. 2013;24:1–5. [DOI] [PubMed] [Google Scholar]
- 14. Jakubowicz D, Froy O, Ahren B, Boaz M, Landau Z, Bar-Dayan Y, Ganz T, Barnea M, Wainstein J. Incretin, insulinotropic and glucose-lowering effects of whey protein pre-load in type 2 diabetes: a randomised clinical trial. Diabetologia. 2014;57:1807–11. [DOI] [PubMed] [Google Scholar]
- 15. Pilz S, März W, Cashman KD, Kiely ME, Whiting SJ, Holick MF, Grant WB, Pludowski P, Hiligsmann M, Trummer C et al.. Rationale and plan for vitamin D food fortification: a review and guidance paper. Front Endocrinol. 2018;9:373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Itkonen S, Erkkola M, Lamberg-Allardt C. Vitamin D fortification of fluid milk products and their contribution to vitamin D intake and vitamin D status in observational studies—a review. Nutrients. 2018;10:1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The NS, King IB, Couch SC, Crandell JL, Dabelea D, Liese AD, Mayer-Davis EJ. Plasma trans-palmitoleic acid is associated with cardio-metabolic risk factors in youth with type 1 diabetes. Diabetes Metab. 2018;44:181–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mozaffarian D, de Oliveira Otto MC, Lemaitre RN, Fretts AM, Hotamisligil G, Tsai MY, Siscovick DS, Nettleton JA. trans-Palmitoleic acid, other dairy fat biomarkers, and incident diabetes: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr. 2013;97(4):854–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mozaffarian D, Cao H, King IB, Lemaitre RN, Song X, Siscovick DS, Hotamisligil GS. trans-Palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: a cohort study. Ann Intern Med. 2010;153:790–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Canfora EE, Jocken JW, Blaak EE. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. 2015;11:577–91. [DOI] [PubMed] [Google Scholar]
- 21. Drouin-Chartier JP, Côté JA, Labonté MÈ, Brassard D, Tessier-Grenier M, Desroches S, Couture P, Lamarche B. Comprehensive review of the impact of dairy foods and dairy fat on cardiometabolic risk. Adv Nutr. 2016;7:1041–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr. 2013;98:1066–83. [DOI] [PubMed] [Google Scholar]
- 23. Gao D, Ning N, Wang C, Wang Y, Li Q, Meng Z, Liu Y, Li Q. Dairy products consumption and risk of type 2 diabetes: systematic review and dose-response meta-analysis. PLoS ONE. 2013;8:e73965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tian S, Xu Q, Jiang R, Han T, Sun C, Na L. Dietary protein consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Nutrients. 2017;9:982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tong X, Dong JY, Wu ZW, Li W, Qin LQ. Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur J Clin Nutr. 2011;65:1027–31. [DOI] [PubMed] [Google Scholar]
- 26. Drouin-Chartier JP, Brassard D, Tessier-Grenier M, Côté JA, Labonté MÈ, Desroches S, Couture P, Lamarche B. Systematic review of the association between dairy product consumption and risk of cardiovascular-related clinical outcomes. Adv Nutr. 2016;7:1026–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen M, Sun Q, Giovannucci E, Mozaffarian D, Manson JE, Willett WC, Hu FB. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med. 2014;12:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr. 2016;103:1111–24. [DOI] [PubMed] [Google Scholar]
- 29. Khoramdad M, Alimohamadi Y, Safiri S, Pakzad R, Shakiba E, Shafiei J, Firouzi A. Dairy products consumption and risk of type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Iranian Red Crescent Med. 2017;19:e14140. [Google Scholar]
- 30. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB, for the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 31. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. [DOI] [PubMed] [Google Scholar]
- 32. Higgins JPT, Deeks JJ. Selecting studies and collecting data. In: Higgins JPT, Green S, editors. Cochrane Handbook of Systematic Reviews of Interventions, Version 5.1.0. Cochrane Collaboration; 2011; [updated Mar 2011]. Available from: https://handbook-5-1.cochrane.org/. [Google Scholar]
- 33. Pae CU. Why systematic review rather than narrative review?. Psychiatry Investig. 2015;12(3):417–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E et al.. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Elwood PC, Givens DI, Beswick AD, Fehily AM, Pickering JE, Gallacher J. The survival advantage of milk and dairy consumption: an overview of evidence from cohort studies of vascular diseases, diabetes and cancer. J Am Coll Nutr. 2008;27:723–34. [DOI] [PubMed] [Google Scholar]
- 36. Elwood PC, Pickering JE, Givens DI, Gallacher JE. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids. 2010;45:925–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Khoramdad M, Rahimi M, Cheraghi Z, Izadi N, Alimohamadi Y, Firouzi A, Shafiei J. The effect of dairy products subgroups consumption on the risk of diabetes: a systematic review and meta-analysis. Iranian Red Crescent Med. 2017;19:e42064. [Google Scholar]
- 38. Pimpin L, Wu JH, Haskelberg H, Del Gobbo L, Mozaffarian D. Is butter back? A systematic review and meta-analysis of butter consumption and risk of cardiovascular disease, diabetes, and total mortality. PLoS One. 2016;11:e0158118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB. Dairy consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med. 2005;165:997–1003. [DOI] [PubMed] [Google Scholar]
- 40. Pittas AG, Dawson-Hughes B, Li T, Van Dam RM, Willett WC, Manson JE, Hu FB. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care. 2006;29:650–6. [DOI] [PubMed] [Google Scholar]
- 41. Pereira MA, Jacobs DR Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA study. JAMA. 2002;287:2081–9. [DOI] [PubMed] [Google Scholar]
- 42. Tremblay A, Gilbert JA. Milk products, insulin resistance syndrome and type 2 diabetes. J Am Coll Nutr. 2009;28:91S–102S. [DOI] [PubMed] [Google Scholar]
- 43. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG et al.. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Eng J Med. 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 44. Canadian Dairy Information Centre (CDIC). Per capita global consumption of fluid milk. [Internet]. 2015; [cited 10 Jun, 2018]. Available from: http://www.dairyinfo.gc.ca/index_e.php?s1=dff-fcil&s2=cons&s3=consglo&s4=tm-lt. [Google Scholar]
- 45. Zong G, Li Y, Wanders AJ, Alssema M, Zock PL, Willett WC, Hu FB, Sun Q. Intake of individual saturated fatty acids and risk of coronary heart disease in US men and women: two prospective longitudinal cohort studies. BMJ. 2016;355:i5796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yu E, Hu FB. Dairy products, dairy fatty acids, and the prevention of cardiometabolic disease: a review of recent evidence. Curr Atheroscler Rep. 2018;20:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Díaz-López A, Bulló M, Martínez-González MA, Corella D, Estruch R, Fitó M, Gómez-Gracia E, Fiol M, Garcia de la Corte FJ, Ros E et al.. Dairy product consumption and risk of type 2 diabetes in an elderly Spanish Mediterranean population at high cardiovascular risk. Eur J Nutr. 2016;55:349–60. [DOI] [PubMed] [Google Scholar]
- 48. Micha R, King IB, Lemaitre RN, Rimm EB, Sacks F, Song X, Siscovick DS, Mozaffarian D. Food sources of individual plasma phospholipid trans fatty acid isomers: the Cardiovascular Health Study. Am J Clin Nutr. 2010;91:883–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mozaffarian D. Natural trans fat, dairy fat, partially hydrogenated oils, and cardiometabolic health: the Ludwigshafen Risk and Cardiovascular Health Study. Eur Heart J. 2016;37:1079–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fontecha J, Rodriguez-Alcalá LM, Calvo MV, Juárez M. Bioactive milk lipids. Curr Nutr Food Sci. 2011;7:155–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.