Abstract
Background:
Prurigo nodularis (PN) is a poorly understood, understudied pruritic dermatosis that reduces quality of life.
Objective:
To characterize the demographics and comorbidities associated with PN.
Methods:
Cross-sectional study of patients 18 years and older who were seen at the Johns Hopkins Health System between December 6, 2012, and December 6, 2017.
Results:
Over the past 5 years, 909 patients with PN were seen at Johns Hopkins Health System. African American patients were 3.4 times more likely to have PN than white patients were (odds ratio [OR], 3.4; 95% confidence interval [CI], 2.9–3.9; P \.001). A comparison of the study patients and race-matched controls revealed that PN was significantly associated with a variety of systemic, cardiovascular, and psychiatric comorbidities, including chronic kidney disease, chronic hepatitis C, chronic obstructive pulmonary disease, congestive heart failure, depression, and atopic dermatitis. Black patients with PN were 10.5 times more likely (OR, 10.5; 95% CI, 7.9–13.9; P \.001) to have HIV than were race-matched controls with atopic dermatitis, and 8 times more likely (OR, 8.0; 95% CI, 5.7–11.1; P \ .001) to have HIV than were African American patients with psoriasis.
Limitations:
Our data describe patients seen by 1 hospital system. Our data identify associated conditions and comorbidities but are unable to support a causal relationship.
Conclusion:
PN disproportionately affects African Americans and is associated with several systemic conditions, including HIV, chronic kidney disease, and diabetes. (J Am Acad Dermatol 2018;79:714–9.)
Keywords: atopic dermatitis, chronic kidney disease, HIV, itch, PN, prurigo nodularis, pruritus, psoriasis
CAPSULE SUMMARY
Prurigo nodularis (PN) is a pruritic dermatosis of unknown etiology.
PN is associated with an increased risk of chronic kidney disease, diabetes, hepatitis C, HIV, and several psychiatric comorbidities.
Clinicians should be aware of associations with psychiatric, metabolic, and infectious disease when treating patients with PN.
Prurigo nodularis (PN) is a pruritic dermatosis of unknown etiology that is characterized by chronic scratching behavior.1 It presents as symmetrically distributed hyperkeratotic and intensely pruritic nodules and papules, most commonly involving the extensor surfaces of the extremities and trunk.2 Like other chronically pruritic conditions, PN carries a significant burden of disease, disrupting sleep quality and contributing to mood disorders such as anxiety and depression.2,3
Despite its effects on health-related quality of life, PN remains poorly understood and understudied throughout the literature. In fact, to date, there are only a few small-scale studies describing the strength of the association of various comorbidities with PN.3,4 Currently, the most comprehensive study characterizing a cohort of patients with PN involves 108 primarily white patients in Germany.3 One explanation for the dearth of available data is that PN is relatively uncommon; thus, studies analyzing chronic itch often group PN together with other pruritic conditions.2 Furthermore, the pathogenesis of PN has not yet been elucidated, limiting dermatologists’ understanding and management of the disease.2
Because PN carries a significant burden of disease and has not been well characterized, it is important to gather more data on this patient population.2 To help provide a better understanding of this condition, we performed a cross-sectional study of demographic characteristics, ethnic differences, and associated comorbid conditions of patients with PN who were seen at the Johns Hopkins Health System (JHHS) over the past 5 years.
METHODS
Institutional review board approval was waived, as only anonymous aggregate-level data counts were used. Retrospective data on patient demographics and comorbidities were collected by using the Slicer Dicer feature of the electronic medical record system EPIC. Johns Hopkins has a large and diverse catchment area that includes the city of Baltimore and surrounding suburban areas across the state of Maryland and neighboring states; in addition, many patients travel long distances both domestically and internationally to receive care at JHHS.
Using Slicer Dicer, we anonymously searched for the total number of patients age 18 or older in whom PN had been diagnosed at JHHS over the past 5 years (from December 6, 2012, through December 6, 2017). We then applied additional filters for various comorbid chronic conditions to determine the percentages of patients with PN and each comorbidity. The list of comorbidities was derived from the 2015 Medicare report of the most prevalent chronic medical conditions in the United States.5 Atopic dermatitis (AD) was also added to this list of comorbidities, as it is associated with PN.
Patients with PN were compared with 3 groups of controls: patients with a diagnosis of AD, patients with a diagnosis of psoriasis, and all patients without PN who were seen at JHHS within the same time frame. Odds ratios were calculated to evaluate the strength of association between PN and the various comorbidities versus that in our control groups. Statistical significance was set at a P value less than .05 (Supplemental Table I; available at http://www.jaad.org). Odds ratios and P values were not calculated for comorbidities with 0 patients in that category.
Subgroup analyses stratified by race were performed for the aforementioned outcomes (Supplemental Tables II and III; available at http://www.jaad.org). Age distributions for all patients with PN, African American patients with PN, and white patients with PN were determined by calculating the percentage of patients in 4 different age brackets for each year of the study and averaging those percentages together.
RESULTS
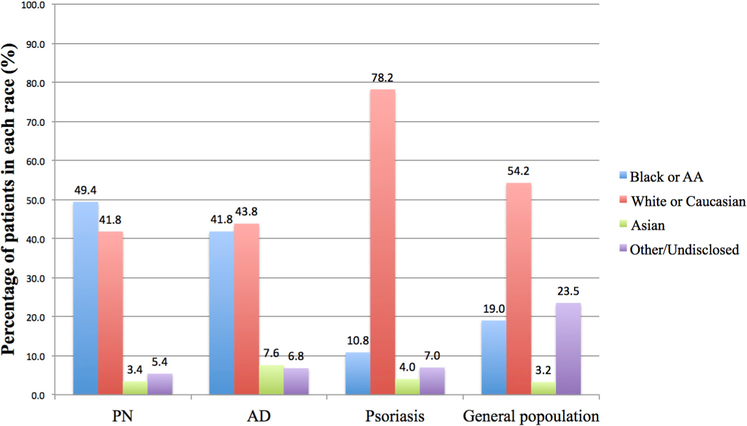
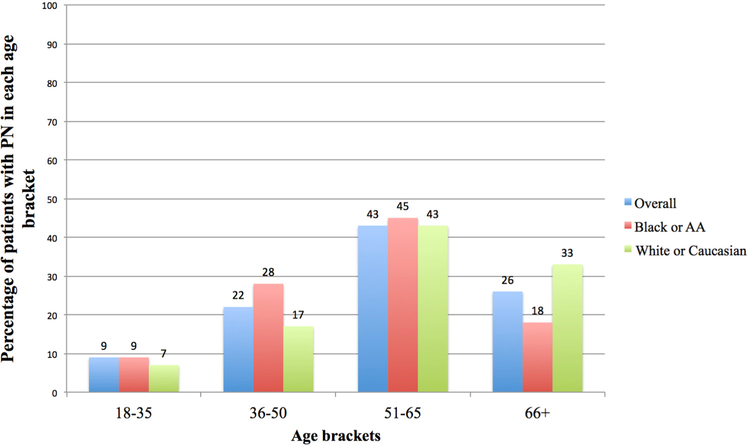
Over the past 5 years, 909 patients with a diagnosis of PN presented to JHHS. Of these 909 patients with PN, 49.4% were African American, 41.8% were white, and 3.4% were Asian (Fig 1). African American patients were 3.4 times more likely to have PN than white patients were (odds ratio [OR],3.4; 95% confidence interval [CI], 2.9–3.9; P \.001). Of the African American patients, 54.6% were female and 45.4% were male. Of the white patients, 50.5% were female and 49.5% were male. Of the Asians, 41.9% were female and 58.1% were male. The age distribution was similar among African American and white patients with PN, with the majority of patients with PN (43%−45%) being 51 to 65 years old (Fig 2). In both our African American and white study groups, PN was statistically significantly associated with a variety of systemic, cardiovascular, and psychiatric conditions when those groups were compared with race-matched controls; these diseases included chronic kidney disease, chronic hepatitis C, chronic obstructive pulmonary disease (COPD), congestive heart failure, depression, and AD (Supplemental Tables II and III). Whereas 10.7% of patients with PN had concomitant AD, only 4.2% of patients with PN had concomitant psoriasis.
Fig 1.
Racial backgrounds of all patients 18 years and older with a diagnosis of prurigo nodularis (PN), atopic dermatitis (AD), or psoriasis and within the general population who presented to the Johns Hopkins Hospital System over the past 5 years. AA, African American.
Fig 2.
Age distribution of patients with prurigo nodularis (PN) overall, in African Americans (AAs), and in white patients. Most patients (43%−45%) with PN were between 51 and 65 years old.
Among African Americans, PN was also statistically significantly associated with HIV infection, hypertension, and ischemic heart disease, whereas neither psoriasis nor AD was statistically significantly associated of with HIV, hypertension, or ischemic heart disease; such associations were not seen in our white study group. Compared with psoriasis, PN was not associated with osteoarthritis, rheumatoid arthritis, atrial fibrillation, hyperlipidemia, or osteoporosis. Compared with AD, PN was not associated with rheumatoid arthritis or asthma. There were too few Asian patients in our PN cohort to determine associated comorbidities.
DISCUSSION
This study represents one of the most detailed analyses of patients with PN reported in the literature. Our study found that PN disproportionately affects African Americans as compared with the general population (Fig 1). In addition, sex distribution varied by race, with more females affected among African American patients, more males affected among Asian patients, and males and females affected relatively equally among white patients. When both African American and white patients were compared with race-matched controls, having PN was associated with a statistically significantly increased risk of various systemic, cardiovascular, and psychiatric conditions (Supplemental Tables I–III).
Half of the patients with PN who were seen at JHHS over the last 5 years were African American. By comparison, only 19.0% of all patients seen at JHHS are African American (Fig 1). Indeed, many of the underlying conditions thought to contribute to the development of PNdsuch as AD, type 2 diabetes mellitus, chronic kidney disease, and chronic liver diseasedhave a higher incidence in African Americans.2,6–8 Our study also found that compared with all the control groups, both African American and white patients with PN had a statistically significantly increased risk of having the 4 aforementioned conditions (Supplemental Tables II and III).
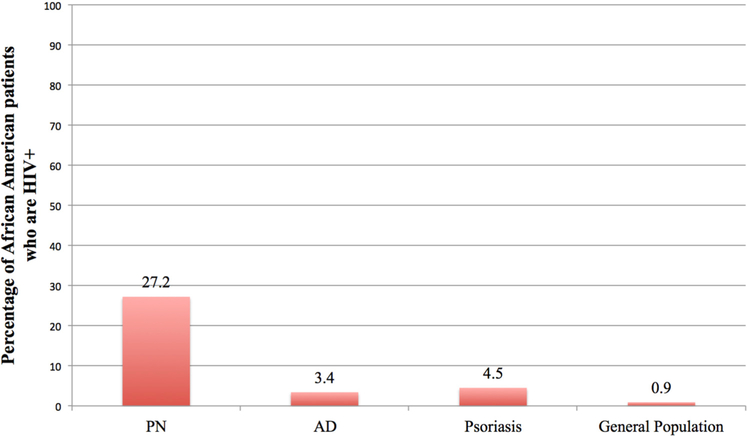
We found that PN in African Americans is also statistically significantly associated with HIV infection, a finding that was not observed in our white cohort. Our study found that black patients with PN were 10.5 times more likely (OR, 10.5; 95% CI, 7.9–13.9; P \.001) to have HIV than were race-matched controls with atopic dermatitis, and 8 times more likely (OR, 8.0; 95% CI, 5.7–11.1; P \ .001) to have HIV than were African American patients with psoriasis (Fig 3). Although the racial differences are a significant finding, the association with HIV infection is not surprising, as HIV is a recognized major systemic cause of generalized chronic pruritus.9 Indeed, a previous article described an association between HIV infection and PN on the basis of a study of patients treated at a clinic in French Guiana.10 The study found that 35.7% of patients with PN in French Guiana had a concomitant diagnosis of HIV.10 In our study, 27.2% of African American patients with PN had HIV. In line with the most recent US Centers for Disease Control and Prevention guidelines, all patients age 13 to 64 years should undergo HIV testing at least once in their lifetime as long as the prevalence of undiagnosed HIV in that patient population is greater than 0.1%.11 Thus, clinicians should consider an HIV work-up in patients with PN who have not yet been tested for HIV during their lifetime.
Fig 3.
Percentages of African American patients with prurigo nodularis (PN), atopic dermatitis (AD), or psoriasis and in the general population who are HIV positive. African American patients with PN were 10.5 times more likely to have HIV than were race-matched patients with AD and 8 times more likely to have HIV than were race-matched patients with psoriasis.
Our study also found that when patients with PN are compared with race-matched controls with AD or psoriasis, PN is statistically significantly associated with a variety of cardiovascular conditions; these conditions include hypertension, ischemic heart disease, and congestive heart failure (Supplemental Table I). To our knowledge, these associations are novel. There are several explanations that could account for this finding. Hypertension is highly associated with concomitant diabetes mellitus and chronic kidney disease, both of which are systemic causes of chronic pruritus that could contribute to PN.9 Hypertension is also a well-documented risk factor for the development of congestive heart failure.12 However, these associations warrant further study in future research.
PN was also statistically significantly associated with COPD in both African American and white patients (Supplemental Tables II and III). It is known that patients with psoriasis are at greater risk of developing COPD than the general population, with the severity of psoriasis correlating with the strength of this association.13 The authors of the study that demonstrated this finding hypothesized that the inflammatory response seen in patients with psoriasis leads to increased levels of the proinflammatory cytokines interleukin 1 (IL-1), IL-6, IL-8, and tumor necrosis factor-a, which predisposes smokers to a proinflammatory state in the lungs.13 Future studies should further explore this association in patients with PN.
We found that a statistically significant percentage of African American and white patients with PN had major depressive disorder when compared with race-matched controls (Supplemental Tables II and III). In fact, patients with PN were almost 3 times more likely to have concomitant depression when compared with patients with AD and 2.5 times more likely to have depression when compared with patients with psoriasis (Supplemental Table I). This finding suggests a psychologic component to PN, and it is consistent with previous reports describing a relationship between chronic itch and mood disorders. Of all patients with chronic pruritus, 70% have some type of psychiatric comorbidity, and the severity of depression in patients with chronic pruritus correlates with intensity of itch.14,15 The concomitant psychologic component of PN likely contributes to the challenging nature of treating this disease.
There are several limitations to this study. Our data describe patients who were seen by 1 hospital system in the United States and thus are not generalizable to the general population or to patients living in remote or rural areas. Our data also identify associated conditions and comorbidities but are unable to support a causal relationship between these comorbidities and the development of PN. Associated conditions may be a consequence of uncontrolled factors, such as socioeconomic status or history of intravenous drug use. Substratification by age could not be performed given the relatively small total number of patients with PN and given the fact that each comorbidity existed in different age brackets. Finally, we lacked information on racial biases in referral patterns, which may have affected the interpretation of our results.
There are few studies currently available on the epidemiology of PN. Our findings indicate that PN disproportionately affects African Americans between the ages of 50 and 65 years and that PN is associated with a number of systemic and psychiatric conditions. Patients with PN who have not already undergone HIV screening should be considered for an HIV work-up.
Supplementary Material
Funding sources:
Dr Kwatra received a grant from the Skin of Color Society.
Abbreviations used:
- AD
atopic dermatitis
- COPD
chronic obstructive pulmonary disease
- JHHS
Johns Hopkins Health System
- IL
interleukin
- PN
prurigo nodularis
Footnotes
Disclosure: Dr Kwatra is an advisory board member for Menlo and Trevi Therapeutics. Dr Pereira has a grant from the European Academy of Dermatology and Venereology (EADV grant 2016–012). Dr Kang served on the advisory board for Menlo Therapeutics and received an honorarium for his service. Ms Boozalis, Ms Tang, Dr Patel, Dr Semenov, and Dr Stander have no conflicts of interest to disclose.
The content in this manuscript has not been published or submitted for publication elsewhere. All the authors have contributed significantly and are in agreement with the content of the manuscript.
Reprints not available from the authors.
REFERENCES
- 1.Pereira MP, Steinke S, Zeidler C, et al. European Academy of Dermatology and Venereology European prurigo project: expert consensus on the definition, classification and terminology of chronic prurigo. J Eur Acad Dermatol Venereol. 2018. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2.Fostini AC, Girolomoni G, Tessari G. Prurigo nodularis: an update on etiopathogenesis and therapy. J Dermatolog Treat. 2013;24(6):458–462. [DOI] [PubMed] [Google Scholar]
- 3.Iking A, Grundmann S, Chatzigeorgakidis E, Phan NQ, Klein D, St €ander S. Prurigo as a symptom of atopic and non-atopic diseases: aetiological survey in a consecutive cohort of 108 patients. J Eur Acad Dermatol Venereol. 2013;27(5):550–557. [DOI] [PubMed] [Google Scholar]
- 4.Winhoven SM, Gawkrodger DJ. Nodular prurigo: metabolic diseases are a common association. Clin Exp Dermatol. 2007; 32(2):224–225. [DOI] [PubMed] [Google Scholar]
- 5.US Centers for Medicare and Medicaid Services. Chronic conditions. Available at: https://www.cms.gov/ResearchStatistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main.html. Accessed December 27, 2017.
- 6.Merriman JA, Mueller EA, Cahill MP, et al. Temporal and racial differences associated with atopic dermatitis staphylococcus aureus and encoded virulence factors. mSphere. 2016;1(6): e00295–e00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21): e393. [DOI] [PubMed] [Google Scholar]
- 8.Alhmada Y, Selimovic D, Murad F, et al. Hepatitis C virus-associated pruritus: etiopathogenesis and therapeutic strategies. World J Gastroenterol. 2017;23(5): 743–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tarikci N, Kocatürk E, Güngör Ş, Topal IO, Can PÜ, Singer R Pruritus in systemic diseases: a review of etiological factors and new treatment modalities. ScientificWorldJournal. 2015; 2015:803752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magand F, Nacher M, Cazorla C, Cambazard F, Marie DS, Couppie P. Predictive values of prurigo nodularis and herpes zoster for HIV infection and immunosuppression requiring HAART in French Guiana. Trans R Soc Trop Med Hyg. 2011; 105(7):401–404. [DOI] [PubMed] [Google Scholar]
- 11.US Centers for Disease Control Prevention. Revised recommendation for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14). [PubMed] [Google Scholar]
- 12.Kannan A, Janardhanan R. Hypertension as a risk factor for heart failure. Curr Hypertens Rep. 2014;16(7):447. [DOI] [PubMed] [Google Scholar]
- 13.Li X, Kong L, Li F, et al. Association between psoriasis and chronic obstructive pulmonary disease: a systematic review and meta-analysis. PLoS One. 2015;10(12): e0145221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schneider G, Driesch G, Heuft G, Evers S, Luger TA. St, Stematic review and meta-analysisadolescents, and pregnant women in health-care settings. Clin Exp Dermatol. 2006;31(6):762–767. [DOI] [PubMed] [Google Scholar]
- 15.Gupta MA, Gupta AK. Depression modulates pruritus perception: a study of pruritus in psoriasis, atopic dermatitis and chronic idiopathic urticaria. Ann N Y Acad Sci. 1999;885(1):394–395. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.