Abstract
Background
Middle managers are given scant attention in the implementation literature in health care, where the focus is on senior leaders and frontline clinicians.
Aims
To empirically examine the role of middle managers relevant to innovation implementation and how middle managers experience the implementation process.
Methods
A qualitative study was conducted using the methods of grounded theory. Data were collected through semistructured interviews with middle managers (N = 15) in Nova Scotia and New Brunswick, Canada. Participants were purposively sampled, based on their involvement in implementation initiatives and to obtain variation in manager characteristics. Data were collected and analyzed concurrently, using an inductive constant comparative approach. Data collection and analysis continued until theoretical saturation was reached.
Results
Middle managers see themselves as being responsible for making implementation happen in their programs and services. As a result, they carry out five roles related to implementation: planner, coordinator, facilitator, motivator, and evaluator. However, the data also revealed two determinants of middle managers' role in implementation, which they must negotiate to fulfill their specific implementation roles and activities: (1) They perform many other roles and responsibilities within their organizations, both clinical and managerial in nature, and (2) they have limited decision‐making power with respect to implementation and must work within the parameters set by upper levels of the organization.
Linking Evidence to Action
Middle managers play an important role in translating adoption decisions into on‐the‐ground implementation. Optimizing their capacity to fulfill this role may be key to improving innovation implementation in healthcare organizations.
Keywords: middle managers, implementation, qualitative methods
Background
The organization, delivery, and outcomes of care can be improved using innovations (i.e., new tools, technologies, and practices) whose effectiveness is supported by scientific evidence. However, a substantive literature base has revealed gaps between scientific evidence and what actually happens in the course of clinical care (Grol, 2001; McGlynn et al., 2003). In cancer, for example, the Canadian Strategy for Cancer Control estimated that cancer outcomes in Canada could improve by as much as 30% by appropriately and routinely applying existing scientific evidence in practice (Canadian Strategy for Cancer Control, 2006). Ultimately, the poor uptake of evidence means that many patients do not benefit from optimal care (Curtis, Walker, & Goldacre, 2018; Kryworuchko, Stacey, Bai, & Graham, 2009; Sheldon et al., 2004; Tu et al., 2017).
Achieving the widespread uptake of beneficial innovations may relate less to dissemination and decisions around their use and more to their implementation (Glasgow & Emmons, 2007; Green, Ottoson, Garcia, & Hiatt, 2009)—that is, the transition period following a decision to adopt when an innovation “is actually put into practice” (Rogers, 2003, p. 179). Successful implementation is essential to realizing the sustained use and benefits of innovations (Weiner, Lewis, & Linnan, 2009). Innovation implementation in health care is often characterized by complex and dynamic processes (Van de Ven, Polley, Garud, & Venkataraman, 1999). The role of middle managers—“employees who are supervised by an organization's top managers and who supervise frontline employees” (Birken, Lee, & Weiner, 2012)—in these processes is poorly understood, despite the considerable influence they can potentially exert in day‐to‐day implementation activities. In nonhealth sectors, middle managers are often the individuals who oversee the implementation of innovations (Bourne & Walker, 2005). In health care, however, the literature has focused on the influence of senior administrators and managers on innovation implementation and use (Bradley et al., 2003; Kimberly & Cook, 2008; Mitchell, 2000; Weiner, Shortell, & Alexander, 1997; Yousefi Nooraie, Lohfeld, Marin, Hanneman, & Dobbins, 2017).
Recent theoretical and empirical work suggests that middle managers play an important role in implementation efforts in health care, particularly by bridging informational gaps that exist between senior management and frontline clinicians (Birken et al., 2012, 2016; Engle et al., 2017). Birken et al. (2012) presented a theory that posited that middle managers' organizational position enabled them to address informational gaps in four ways: (a) giving information to employees regarding implementation (diffusing information); (b) making information relevant to employees (synthesizing information); (c) giving employees the tools required for implementation (mediating between strategy and day‐to‐day activities); and (d) encouraging employees to consistently and effectively use innovations (selling innovation implementation). This theory was not empirically derived, yet a recent effort to substantiate the theory suggests it aligns with the practical experiences of middle managers (Birken et al., 2016). Nevertheless, much more research is necessary to further elucidate the roles and experiences of middle managers in innovation implementation in healthcare settings.
Aims
The aims of this study were to empirically examine the role of middle managers relevant to innovation implementation and how middle managers experience the implementation process. An improved understanding of their role will contribute to this nascent area of inquiry and may be important to optimizing implementation in health care.
Methods
Using the methods of grounded theory (Strauss & Corbin, 1990), this study employed semistructured interviews of middle managers working in cancer care in two Canadian provinces. The research design, data collection instrument, and data analysis were informed by Birken et al.'s theory of middle managers' role in innovation implementation in health care (Birken et al., 2012). Approval to conduct the study was gained from the Capital District Health Authority Research, Cape Breton District Health Authority, Guysborough Antigonish Strait Health Authority, South West Health, IWK Health Centre, and Horizon Health Network Research Ethics Boards.
Participants
Participants were middle managers in two Canadian provinces (Nova Scotia and New Brunswick) who managed hospital‐based programs, services, departments, or units wherein a cancer‐related innovation was implemented during their current management tenure. The provinces have populations of approximately 940,000 (Nova Scotia) and 747,000 (New Brunswick); they are characterized by health system differences that might impact innovation implementation (e.g., ratio of academic vs. community clinicians, centralization of healthcare services, and level of health research activity). Managers were purposively recruited to ensure variation in managers' training and profession (clinician, nonclinician), work location (community, academic or tertiary care), and innovation type. Four team members (R.U., A.F., T.R., G.A.P.) identified potential participants based on their familiarity with the provinces' cancer programs and knowledge of recent implementation initiatives, and a research coordinator approached all identified potential participants.
Data Collection and Analysis
Semistructured interviews (Patton, 2002; Rubin & Rubin, 1995) were used to gather data on how middle managers experience the process of innovation implementation and the role they play in these endeavors. An innovation was defined and described to participants as a tool, technology, or practice new to the middle managers' unit, department, or organization (i.e., new to that setting, but may have been implemented elsewhere previously; Klein & Sorra, 1996). Two pilot interviews were conducted to assess and refine the interview script; these were audiotaped, transcribed verbatim, and discussed among team members (R.U., C.K., A.F.) to ensure all topics of interest were explored. The resulting interview guide (see Table S1) was adapted during data collection based on earlier interviews to further explore important concepts and emerging categories (Patton, 2002; Rubin & Rubin, 1995).
One team member (C.K.), experienced in qualitative methods, conducted all interviews face to face in the manager's office or via telephone, depending on practical considerations. Only the interviewer and participant were involved in the interview. For each, the interviewer had a prior understanding of the background and work of the participant and ensured that the participant understood the study objectives and interview procedure. All interviews were audiotaped and transcribed verbatim by a research coordinator with experience in transcription. The audiotapes and transcripts were supplemented with field notes (i.e., memos).
Data were collected and analyzed concurrently, using a constant comparative approach (Strauss & Corbin, 1990). The pilot interviews were included in the analysis, with pilot participants' permission, because no substantive changes were made to the interview guide. Through iterative discussion and review of the first four transcripts, two investigators (C.K., A.F.) developed a codebook (or coding structure) to guide coding and subsequent categorization of data (see Table S2). They used this codebook to independently code the first four transcripts (27%). The codebook was updated throughout analysis as further codes (or concepts) were identified. The remaining 11 transcripts were coded and analyzed by one investigator (C.K.).
Consistent with constant comparative analysis, open and axial coding of interview transcripts occurred simultaneously. This entailed reading the transcribed interviews line by line in their entirety to identify ideas and concepts, grouping the concepts into high‐level categories and subcategories, and making connections between the categories and subcategories. The iterative process involved continually reviewing codes for refining purposes, going back to prior transcripts to constantly compare emerging concepts with prior data, examining concepts and emerging categories across sampling characteristics, and reviewing and refining emerging categories based on their relationship to one another and their ability to explain middle managers' role in implementation. Qualitative software (NVivo; QSR International, Cambridge, MA, USA) was used to assist with data management and to enable comparison and synthesis of codes. Investigators (R.U., C.K., A.F.) met regularly to review the coded data, discuss emerging categories, and probe theoretical saturation. Data collection and analysis continued until theoretical saturation was reached—that is, the point at which no new substantive information was being collected (in other words, the point at which any new information collected does not add anything substantive to the overall story; Strauss & Corbin, 1990). The detailed development of categories was performed through discussion among investigators and continually returning to the analysis.
Numerous techniques were employed to optimize study rigor. These included the following: detailed documentation of methodological and analytic decisions; systematic data coding (C.K., A.F.); development of a codebook and data coding by a cancer system middle manager (A.F.); use of direct quotations to ensure participant perspectives are clearly represented; ongoing review and questioning of data coding, analytic decisions, and resultant categories; and team meetings to discuss and question findings.
Results
In total, 22 middle managers were approached for study participation, with 17 agreeing to participate. However, two interviews were unusable (one because of a faulty audio recording and one because the participant was not in a middle manager role), leaving 15 middle managers who participated in the study: six from Nova Scotia and nine from New Brunswick. Three participants had a nonclinical background (e.g., health administration) and 12 a clinical background (e.g., nursing). Four were male; 11 were female. All were full‐time managers at the time of their participation. Participants worked across a broad range of cancer programs and services (e.g., cancer screening, diagnostic imaging, pathology, surgery, adjuvant therapy, and survivorship) and were involved in the implementation of a variety of innovations (e.g., clinical practice guidelines, cancer screening programs, imaging technologies, therapeutic modalities, electronic tools and systems, and laboratory testing). These cancer programs and services were all hospital‐based and all served adult populations. The interviews lasted between 29 and 56 min.
Three overarching categories emerged related to a middle manager's role in innovation implementation. At the core, middle managers viewed themselves as the people responsible for making implementation happen. However, the data also revealed two determinants of middle managers' roles in implementation, which they must negotiate to fulfill their specific implementation roles and activities: (a) They have many other roles and responsibilities within their organizations, and (b) they have limited decision‐making power when it comes to implementation. The dataset suggested these two determinants were deeply linked to participants' perceived roles and real‐world experiences with implementation. Figure 1 illustrates these findings. No substantive differences emerged across participant training and profession (clinician, nonclinician), work location (academic, community), or province.
Figure 1.
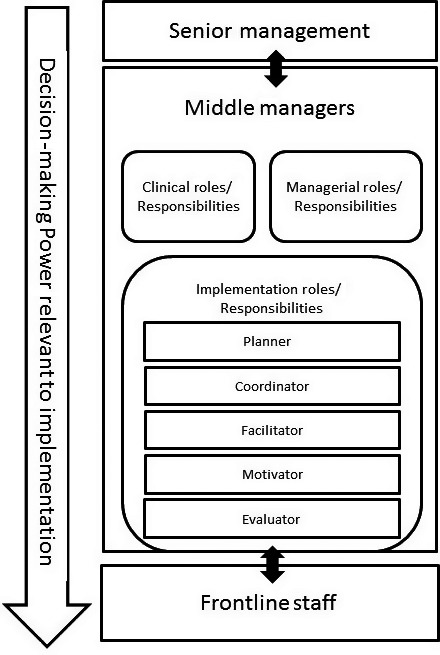
Middle managers' roles in innovation implementation and determinants of fulfilling these roles.
Responsible for Making Implementation Happen.
The data overwhelmingly demonstrated that middle managers perceive themselves as being the ones who are responsible for making implementation happen within their programs and services. That is, their managerial experience is characterized as doing whatever needs to be done to make implementation happen. As one participant succinctly stated, “I am responsible for everything related to [the implementation] … um, it all falls on me to make sure it happens” [P4]. As a result, participants described carrying out five roles related to implementation: planner, coordinator, facilitator, motivator, and evaluator. Table 1 defines these roles and illustrates the multitude of activities participants described doing according to the roles. As planner, participants discussed how they identify what is needed for implementation (e.g., equipment, training, and resources) and then plan appropriately to ensure these needs are addressed. As coordinator, participants described organizing and connecting all the components required to implement an innovation, including making sure all the necessary stakeholders are involved in the initiative. One participant described this as follows:
Table 1.
Making It Happen: Participant Activities According to the Five Roles
| Role | Activities | Representative quotations |
|---|---|---|
|
Planner Anticipating needs and planning accordingly |
|
“I have to prepare, um, a briefing on exactly what the [innovation] is going to be, what does it do … what requirements are going to be needed, what support, I mean from other disciplines, if necessary. The cost of supplies … all of that has to be put together in a package.” [P10] “I would look at, you know, what's needed as far as the impact of the, of what we're doing. But also what's needed with respect to the implementation. The training and education is always a big component of the review and understanding, before we even get started, the challenges … There's an awful lot of process and steps to do it well.” [P14] |
|
Coordinator Organizing and connecting all the required components |
|
“It was my responsibility to coordinate with the staff educator when she was going to do the education and free the staff up and make sure I had coverage to replace.” [P13] “It's identifying the key stakeholders and the key people … like I said, knowing who to go to, knowing who the contact people are.” [P17] |
|
Facilitator Creating the environment to enable more successful implementation |
|
“We also support [innovation] in the sense that we've spent countless hours developing the requirements to the point that, I mean we had it all the way down to operational policies and procedures and the whole thing. Anyway, so if I die tomorrow, they know what to do.” [P11] “It is facilitating … ensuring that there is dedicated time and resources because I would have the knowledge of what is needed, and how do we acquire those resources.” [P2] |
|
Motivator Promoting buy‐in and providing emotional support |
|
“You know, I have to try to keep the staff positive because they are busy and sometimes these new things we implement are, um, they take more time for them, right? So we talk about it at staff meetings, and you know, I always … try to engage them in the process. So I think moral support of staff is really huge.” [P13] “It's the encouraging part of it. You tell them ‘yes, this is what's great about our project,' but if someone is struggling with it, you don't, you know, bring ‘em down about it. You make sure that you provide them with the tools necessary to be able to get to a skill level.” [P12] |
|
Evaluator Monitoring progress and impacts |
|
“Giving them actual data or facts helps … When you have it there, it's like ‘oh wow, I didn't realize that was happening here.'” [P13] “Post implementation we're always looking at the evaluation information to understand ‘did it do what we expected it to do and, if not, why?'” [P14] |
[I] make sure that the right players are at the table … that we have our educators involved, that nursing's involved, clinicians, making sure that the right people are there. And it's a collaborative effort because there's not very much that we do here that doesn't affect somebody else. [P14]
As facilitator, participants emphasized how they sought to create the material or operational conditions that would enable more successful implementation, such as providing or requesting additional finances and establishing new processes and protocols to ensure smooth operations during and after implementation. In contrast, as motivator, participants discussed their role in championing an innovation and providing staff with the emotional support and encouragement they required to change their practices. As an evaluator, participants were responsible for monitoring the implementation and its impacts and reporting to senior management on progress and issues. Participants undertook these five roles irrespective of their personal level of support for an innovation's implementation.
Although the existence of a hierarchy was evident (i.e., participants saw themselves as fulfilling a leadership or supervisory role relevant to implementation), participants also tended to view themselves as part of a team. They often spoke of we rather than I, and when questioned about this, they consistently responded that implementation was a team effort. For example, although they oversaw others and delegated work to others, they understood that implementation is a collaborative effort where any change will inevitably impact others working in close proximity. Thus, they sought to include their staff in change processes and ensure that appropriate organizational members were involved. In general, participants had positive attitudes toward implementation and were willing to take on additional activities to translate adoption decisions into on‐the‐ground actions. This was primarily motivated by the desire to improve patient care.
Many Other Roles and Responsibilities.
Participants described their implementation roles as being in addition to their daily roles and responsibilities. Notably, middle managers often had clinical duties on top of their managerial duties. Thus, implementation typically required taking on extra work although still performing their other roles. Most middle managers had clinical expertise, often required for their manager position. However, without formal training in human resource, project, or change management, they were constantly trying to learn new knowledge and skills that would help them succeed in their multiple roles. This learning was typically self‐directed. Due to performing many roles, many participants felt their engagement in so many activities meant they were unable to perform all of them optimally. This was compounded by the need for additional learning. One participant stated:
The role is so broad in the clinical area … and the expectation is almost to program manage and program plan while at the same time be at the front line and be aware of all the clinical practices that are happening. The span is too big. [P2]
Limited Decision‐Making Power.
Participants described the status quo as one where they have limited decision‐making power with regard to decisions to implement innovations as well as the overarching parameters related to implementation goals and strategies. Senior managers and administrators typically make the adoption decisions, although middle managers provide information to assist in making these decisions and are subsequently expected to work within the set parameters. This was illustrated by one participant when discussing interactions with senior management:
I don't always see eye to eye with, with the ideas that may be coming down the chute but it's sort of, um, try to explain your position and in the long run it's going to be their decision that is going to either move the car ahead or put it on park. So I mean, as far as I'm concerned, my job ends at having given them all the facts and figures that are important to make an appropriate decision. [P8]
The limited decision‐making authority meant that participants were expected to implement innovations even when they perceived the innovations to be a poor fit with the implementation setting or to have limited impact on patient care. At the same time, poor fit and limited impact on patient care both impacted, in negative ways, participants' personal level of support for an innovation.
Nonetheless, at the level of their program or unit, participants described some decision‐making authority as long as they stayed within the specified implementation parameters. For example, middle managers can adjust their program budget and staffing levels and mix to meet specific goals or deliverables set from above. As expressed by one participant, these adjustments can have an important effect on implementation: “We can't make big decisions, but we can make little decisions that make a big impact” [P1]. Participants also noted they have some authority to prioritize which innovation to implement next when multiple implementation projects are on the horizon.
Discussion
This study provides an in‐depth examination of middle managers' experiences with innovation implementation in healthcare settings and their roles in these endeavors. Middle managers clearly perceived themselves as the people responsible for implementation in their respective organizations, and they carry out a breadth of roles to make it happen. Yet, they perceived these roles as on top of their everyday managerial and clinical roles and experienced a lack of overall preparation to undertake them. This, in conjunction with their limited decision‐making authority, may reflect important obstacles to their capacity to optimally lead and navigate implementation processes. This reality has clear implications in terms of actually realizing the potential patient and health system benefits of the innovations organizations choose to adopt.
In recent years, Birken et al. (2012, 2016) have developed and refined a theory on middle managers' role in innovation implementation. Their theory proposes that middle managers are uniquely positioned to disseminate, synthesize, and translate the information that employees need to effectively implement innovations in health care. That is, they are able to close the informational gaps that often impede implementation. The four roles they hypothesize (obtaining and diffusing information, adapting information and the innovation, mediating between strategy and day‐to‐day activities, and selling innovation implementation) are encompassed within the roles and activities defined in this study. In other words, participants perceived themselves as fulfilling the roles represented in Birken et al.'s theory. At the same time, participants clearly described roles and activities that fall outside the scope of that theory. Table 2 maps the study findings to Birken et al.'s four hypothesized roles. As shown in the table, the task‐oriented coordinating (i.e., organizing and connecting all the required components) and facilitating (i.e., creating an environment to enable more successful implementation) roles extend beyond the roles proposed in the prior theory. Moreover, the evaluator role, which was not prominent in the original theory (Birken et al., 2012) but was cited by managers in a subsequent study to substantiate the theory (Birken et al., 2016), was deemed a fundamental role by participants in this study, with multiple and defined activities reaching across the organization. Thus, our findings suggest a broader spectrum of roles and activities than those proposed in Birken et al.'s theory.
Table 2.
Role Findings Mapped to Birken et al.'s Hypothesized Middle Manager Roles in Innovation Implementation
| Obtaining and diffusing information | Adapting information and the innovationa | Mediating between strategy and day‐to‐day activities | Selling innovation implementation | |
|---|---|---|---|---|
| Planner (anticipating needs and planning accordingly) | ++ | |||
| Coordinator (organizing and connecting all the required components) | ||||
| Facilitator (creating the environment to enable more successful implementation) | + | + | ||
| Motivator (promoting buy‐in and providing emotional support) | + | +++ | ||
| Evaluator (monitoring progress and impacts) | + | |||
| Areas of clear divergence | ||||
| Coordination activities found in this study are not apparent within Birken et al.'s hypothesized roles | ||||
| Task‐oriented facilitation activities (e.g., securing finances and resources and connecting the right people) are not apparent within Birken et al.'s hypothesized roles | ||||
+: some alignment between study findings and Birken et al.'s hypothesized roles; ++: moderate alignment between study findings and Birken et al.'s hypothesized roles; +++: high alignment between study findings and Birken et al.'s hypothesized roles.
Also referred to as “synthesizing information”.
In addition to roles and activities, the findings also expand the prior theory by presenting two determinants of their roles, which middle managers have to negotiate and reconcile as they guide implementation efforts. In fact, there is a clear tension between being responsible for implementation yet having limited decision‐making authority. Middle managers' limited decision‐making authority reflects, at least in part, power dynamics across different levels of the organization. From an organizational standpoint, however, a limited ability to make decisions around a certain innovation, particularly when tasked with ensuring its implementation, may negatively impact the levels of moral and material support necessary for effective implementation.
The findings further suggest that middle managers play a potentially crucial and strategic role—which goes beyond mitigating informational gaps—in translating decisions into actions. Although Birken et al.'s (2016) theory emphasizes an important role for middle managers in innovation implementation, our findings suggest these individuals may be a key nexus between an innovation's adoption (i.e., the “decision to make full use of an innovation as the best course of action available” (Rogers, 2003, p. 177) and its implementation. Indeed, in many ways, the findings would suggest middle managers undertake a critical leadership role in implementation efforts. This is an important finding for at least two reasons. First, the scant attention paid to middle managers in the implementation literature (Birken et al., 2012; Parand, Dopson, Renz, & Vincent, 2014) means their contribution to implementation is often seen as negligible. Second, mounting evidence suggests that the important issues related to health and health system improvement may relate less to evidence dissemination and adoption and more to its implementation (Glasgow & Emmons, 2007; Green et al., 2009). Research in management and organizational sciences has demonstrated that the poor uptake of innovations is commonly a failure of the implementation process (Klein & Rails, 1995; Reger, Gustafson, DeMarie, & Mullane, 1994). Middle managers' potentially pivotal role in implementation requires further examination, including how their role relates to context and how differing degrees of involvement contribute to implementation effectiveness.
Several findings concur with those from a recent Canadian study on middle managers' role in hospital quality improvement (QI; Dainty & Sinclair, 2017). In both studies, middle managers felt they had limited training for QI or implementation activities, undertook individual (self‐directed) learning, and considered QI and implementation to be an added part of their position. Others have found that clinician managers often feel persuaded to enter management positions and are subsequently unprepared for their position (Spehar, Frich, & Kjekshus, 2012). Indeed, middle managers in health care are often hired based on clinical skills and credibility and may lack skills, knowledge, and training in key managerial and administrative areas (Federico & Bonacum, 2010). In this study, 12 participants had a clinical background, and most of those reported still having clinical roles and responsibilities. Thus, the hybrid nature of many middle managers in health care may create fundamental tensions due to ill‐defined roles, competing priorities, and incongruity between their skill set and what they are expected to do in their managerial position (Dainty & Sinclair, 2017; Pannick, Sevdalis, & Athanasiou, 2016).
This study presents concepts and categories around middle managers' roles and associated determinants that can be used to build and expand on the existing literature and theory in this area. Future research is needed to further elucidate roles and determinants and how these relate to implementation outcomes. Nonetheless, our findings have important implications for organizations today. First, organizations should consider how they might support middle managers in their pursuit of education and training to ensure they have the knowledge and skills to manage the change process. Most middle managers in our study felt they were inadequately prepared for and lacked any formal knowledge or training regarding implementation. Ongoing mentorship could complement formal education opportunities (Gagliardi, Webster, Perrier, Bell, & Straus, 2014). Second, organizations could include middle managers as more active participants in decision‐making processes rather than organizational actors who merely provide information (“facts and figures”) to help others make decisions. Such involvement may help ensure that implementation decisions better reflect on‐the‐ground needs and realities, that innovations are better aligned with the local setting from the outset, and increase middle managers' own support and buy‐in for implementation in circumstances where this is lacking (Urquhart, Porter, Sargeant, Jackson, & Grunfeld, 2014).
The main study limitation is that it was conducted in only two Canadian provinces and therefore may not be generalizable to other jurisdictions or settings. The purpose of qualitative research, however, is not to achieve generalizable results but to gain rich knowledge about experiences, processes, and context. This study included participants involved in the implementation of a wide range of innovations, incorporated numerous steps to maximize rigor, and attained theoretical saturation. Thus, these findings should have applicability to other similar settings (e.g., publicly funded health care, hospital‐based managers, and hybrid middle managers). A second limitation reflects the composition of the participants, with 12 of 15 having a clinical background. Thus, our findings may be less applicable to middle managers with nonclinical training and experiences. A third limitation is that we sought middle managers' views on their roles in and experiences with innovation implementation, but we did not seek their perceptions on, or objectively assess, implementation effectiveness. Therefore, we are unable to explore whether and how their roles impact implementation outcomes, including effectiveness.
Conclusions
This study provides valuable insight into an area in which we have limited empirical knowledge. The findings suggest middle managers play a leading role in implementation processes. Optimizing their capacity to fulfill this role may be key to improving innovation implementation in healthcare organizations. Indeed, organizational investment in this area, such as providing training and skills development or ongoing mentorship opportunities, may yield substantial return in terms of narrowing evidence to practice gaps in health care. WVN
Linking Evidence to Action.
Middle managers play a potentially crucial and strategic role in translating adoption decisions into on‐the‐ground implementation.
Optimizing middle managers' capacity to fulfill this role may be key to improving innovation implementation in healthcare organizations.
Providing middle managers with training and skills development opportunities may yield substantial return in terms of narrowing evidence to practice gaps in health care.
Supporting information
Table S1. Interview Guide: Exploring Middle Managers' Role in Innovation Implementation.
Table S2. Final Codebook and Associated Definitions.
We gratefully acknowledge study participants who took their valuable time to participate in this study, as well as Margaret Jorgensen for her assistance with study coordination. The study was funded by a research grant from the Canadian Institutes of Health Research. The funder had no role in the design, collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit this manuscript for publication.
References
- Birken, S. A. , Lee, S. Y. , & Weiner, B. J. (2012). Uncovering middle managers' role in healthcare innovation implementation. Implementation Science, 7, 28 10.1186/1748-5908-7-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birken, S. A. , DiMartino, L. D. , Kirk, M. A. , Lee, S. Y. , McClelland, M. , & Albert, N. M. (2016). Elaborating on theory with middle managers' experience implementing healthcare innovations in practice. Implementation Science, 11, 2 10.1186/s13012-015-0362-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourne, L. , & Walker, D. H. T. (2005). The paradox of project control. Team Performance Management, 11, 157–178. [Google Scholar]
- Bradley, E. H. , Holmboe, E. S. , Mattera, J. A. , Roumanis, S. A. , Radford, M. J. , & Krumholz, H. M. (2003). The roles of senior management in quality improvement efforts: What are the key components? Journal of Healthcare Management, 48, 15–29. [PubMed] [Google Scholar]
- Canadian Strategy for Cancer Control (2006). The Canadian strategy for cancer control: A cancer plan for Canada: Discussion paper. Ottawa, ON: CSCC Governing Council. [Google Scholar]
- Curtis, H. J. , Walker, A. J. , & Goldacre, B. (2018). Impact of NICE guidance on tamoxifen prescribing in England 2011–2017: An interrupted time series analysis. British Journal of Cancer, 118(9), 1268–1275. 10.1038/s41416-018-0065-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dainty, K. , & Sinclair, D. (2017). A critical qualitative study of the position of middle managers in health care quality improvement. Journal of Nursing Care Quality, 32(2), 172–179. [DOI] [PubMed] [Google Scholar]
- Engle, R. L. , Lopez, E. R. , Gormley, K. E. , Chan, J. A. , Charns, M. P. , & Lukas, C. V. (2017). What roles do middle managers play in implementation of innovative practices? Health Care Management Review, 42(1), 14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federico, F. , & Bonacum, D. (2010). Strengthening the core: Middle managers play a vital role in improving safety. Healthcare Executive, 25(1), 68–70. [PubMed] [Google Scholar]
- Gagliardi, A. R. , Webster, F. , Perrier, L. , Bell, M. , & Straus, S. (2014). Exploring mentorship as a strategy to build capacity for knowledge translation research and practice: A scoping systematic review. Implementation Science, 9, 122 10.1186/s13012-014-0122-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow, R. E. , & Emmons, K. M. (2007). How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health, 28, 413–433. [DOI] [PubMed] [Google Scholar]
- Green, L. W. , Ottoson, J. M. , Garcia, C. , & Hiatt, R. A. (2009). Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual Review of Public Health, 30, 151–174. [DOI] [PubMed] [Google Scholar]
- Grol, R. (2001). Successes and failures in the implementation of evidence‐based guidelines for clinical practice. Medical Care, 39(8 Suppl. 2), II46–II54. [DOI] [PubMed] [Google Scholar]
- Kimberly, J. , & Cook, J. M. (2008). Organizational measurement and the implementation of innovations in mental health services. Administration Policy in Mental Health, 35(1–2), 11–20. [DOI] [PubMed] [Google Scholar]
- Klein, K. J. , & Rails, R. S. (1995). The organizational dynamics of computerized technology implementation: A review of the empirical literature In Gomez‐Mejia L. R. & Lawless M. W. (Eds.), Implementation management of high technology (pp. 31–79). Greenwich, CT: JAI Press. [Google Scholar]
- Klein, K. J. , & Sorra, J. S. (1996). The challenge of innovation implementation. Academic Management Review, 21(4), 1055–1080. [Google Scholar]
- Kryworuchko, J. , Stacey, D. , Bai, N. , & Graham, I. D. (2009). Twelve years of clinical practice guideline development, dissemination and evaluation in Canada (1994 to 2005). Implementation Science, 4, 49 10.1186/1748-5908-4-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlynn, E. A. , Asch, S. M. , Adams, J. , Keesey, J. , Hicks, J. , DeCristofaro, A. , & Kerr, E. A. (2003). The quality of health care delivered to adults in the United States. New England Journal of Medicine, 348(26), 2635–2645. [DOI] [PubMed] [Google Scholar]
- Mitchell, J. P. (2000). Guideline implementation in the department of defense. Chest, 118(2 Suppl.), 65S–69S. [DOI] [PubMed] [Google Scholar]
- Pannick, S. , Sevdalis, N. , & Athanasiou, T. (2016). Beyond clinical engagement: A pragmatic model for quality improvement interventions, aligning clinical and managerial priorities. BMJ Quality & Safety, 25(9), 716–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parand, A. , Dopson, S. , Renz, A. , & Vincent, C. (2014). The role of hospital managers in quality and patient safety: A systematic review. British Medical Journal Open, 4(9), e005055 10.1136/bmjopen-2014-005055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton, M. Q. (2002). Qualitative research & evaluation methods (3rd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Reger, R. K. , Gustafson, L. T. , DeMarie, S. M. , & Mullane, J. V. (1994). Reframing the organization: Why implementing total quality is easier said than done. Academic Management Review, 19, 565–584. [Google Scholar]
- Rogers, E. M. (2003). Diffusion of innovations (5th ed.). New York, NY: Free Press. [Google Scholar]
- Rubin, H. , & Rubin, I. (1995). Qualitative interviewing: The art of hearing data. Thousand Oaks, CA: Sage. [Google Scholar]
- Sheldon, T. A. , Cullum, N. , Dawson, D. , Lankshear, A. , Lowson, K. , Watt, I. , … Wright, J. (2004). What's the evidence that NICE guidance has been implemented? Results from a national evaluation using time series analysis, audit of patients' notes, and interviews. BMJ, 329(7473), 999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spehar, I. , Frich, J. C. , & Kjekshus, L. E. (2012). Clinicians' experiences of becoming a clinical manager: A qualitative study. BMC Health Services Research, 12, 421 10.1186/1472-6963-12-421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss, A. L. , & Corbin, J. M. (1990). Basics of qualitative research: Grounded theory procedures and techniques. Thousand Oaks, CA: Sage. [Google Scholar]
- Tu, J. V. , Chu, A. , Maclagan, L. , Austin, P. C. , Johnston, S. , Ko, D. T. , … Cardiovascular Health in Ambulatory Care Research Team (2017). Regional variations in ambulatory care and incidence of cardiovascular events. Canadian Medical Association Journal, 189(13), E494–E501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urquhart, R. , Porter, G. A. , Sargeant, J. , Jackson, L. , & Grunfeld, E. (2014). Multi‐level factors influence the implementation and use of complex innovations in cancer care: A multiple case study of synoptic reporting. Implementation Science, 9, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Ven, A. H. , Polley, D. E. , Garud, R. , & Venkataraman, S. (1999). The innovation journey. Oxford, UK: Oxford University Press. [Google Scholar]
- Weiner, B. J. , Shortell, S. M. , & Alexander, J. (1997). Promoting clinical involvement in hospital quality improvement efforts: The effects of top management, board, and physician leadership. Health Services Research, 32(4), 491–510. [PMC free article] [PubMed] [Google Scholar]
- Weiner, B. J. , Lewis, M. A. , & Linnan, L. A. (2009). Using organization theory to understand the determinants of effective implementation of worksite health promotion programs. Health Education Research, 24(2), 292–305. [DOI] [PubMed] [Google Scholar]
- Yousefi Nooraie, R. , Lohfeld, L. , Marin, A. , Hanneman, R. , & Dobbins, M. (2017). Informing the implementation of evidence‐informed decision making interventions using a social network analysis perspective: A mixed‐methods study. BMC Health Services Research, 17(1), 122 10.1186/s12913-017-2067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Interview Guide: Exploring Middle Managers' Role in Innovation Implementation.
Table S2. Final Codebook and Associated Definitions.


