Objective
Staphylococcus epidermidis is prone to causing a relapse of peritonitis within 4 weeks of completion of therapy of a prior episode due to colonization of the peritoneal dialysis (PD) catheter with biofilm. The aim of the study was to discuss the optimal treatment of relapsing peritonitis caused by staphylococcus epidermidis.
Methods
Twelve consecutive patients with diagnosed relapsing staphylococcus epidermidis peritonitis at the Renal Division, the First Affiliated Hospital of Baotou Medical College, were retrospectively included in the study. The diagnosis of peritoneal dialysis peritonitis according to the International Society for Peritoneal Dialysis (ISPD) was based on at least 2 of the following: (1) clinical features consistent with peritonitis, i.e. abdominal pain and/or cloudy dialysis effluent; (2) dialysis effluent white cell count >100/µL or >0.1×109/L (after a dwell time of at least 2 hours), with >50% polymorphonuclear; and (3) positive gram stain or culture from peritoneal dialysis effluent (PDE). In the study, relapsing peritonitis was defined as an episode that occurs within 4 weeks of completion of therapy of a prior episode with the same organism or one sterile episode. Primary response was defined as resolution of abdominal pain, clearing of dialysate, and PDE neutrophil count <100/mL on day 10 with antibiotics alone. All patients met ISPD criteria for relapsing staphylococcus epidermidis peritonitis. The follow-up time was from January 2014 to June 2018. Peritonitis episodes was treated with standard antibiotic protocol of our center at that time. Antibiotic regimens for individual patient were administrated when identification of the organism and subsequent antibiotic sensitivities were available. Five of the 12 patients received intraperitoneal vancomycin with the dose of 1 g every five days for five times. Another seven patients were treated with 1 g cefazolin daily by intraperitoneal injection for 14 days. In addition to systemic antibiotics therapy, PD nurses carried out standardized retraining for these patients with peritonitis. They all were cured and discharged. However, all of these patients suffered a relapse of staphylococcus epidermidis peritonitis within 4 weeks of the withdrawal. They were administrated the initial treatment regimen, clinical conditions of who showed improvement again and dialysis effluent white cell count and classification were normal. Eight of the twelve patients refused the removal of the PD catheter, treated with intermittent periodic vancomycin with the dose of 1 g every two weeks for twice and following dose of 1 g every four weeks for six times.
Results
From 2014 to 2018, the overall relapsing staphylococcus epidermidis peritonitis rate was 1 episode/330 patient-months in our peritoneal dialysis center. We found that the twelve patients suffered the frequent relapse of staphylococcus epidermidis peritonitis within 4 weeks of completion of therapy of a prior episode. Two of them were switched to long-term hemodialysis after catheter removal. Two older patients with diabetic nephropathy died of multiple organ failure rather than relapsing peritonitis. Eight patients who refused the removal of the PD catheter have not a relapse of peritonitis during a therapeutic period, however, which reoccurred within four weeks of vancomycin withdrawal. The eight patients were ultimately removed catheter and had simultaneous re-insertion of a new catheter. After that, staphylococcus epidermidis peritonitis have not occurred.
Conclusions
Relapsing staphylococcus epidermidis peritonitis would relapse within 4 weeks once the intermittent periodic antibiotic therapy was discontinued, characterized by repeat relapse as well as improvement after treatment. Thus, with regard to the treatment of relapsing peritonitis caused by staphylococcus epidermidis, we suggested that PD catheter removal should be considered due to colonization of the PD catheter with biofilm.
Keywords
Staphylococcus epidermidis, Relapse, The optimal treatment, Catheter removal.
Objective
Acute kidney injury (AKI) is a common and severe clinical syndrome of abrupt loss of kidney function that is strongly associated with higher mortality and morbidity. In regarding to AKI outcomes, we need to focus not only on survival, but also on long-term renal function recovery. With the unification of AKI definition and diagnostic criteria, from the RIFLE criteria, AKIN criteria and the newly developed clinical practice guidelines of KDIGO, the AKI epidemiology study has made great progress. A large number of studies have shown that AKI is associated with increased morbidity and mortality in patients with long-term CKD/ESRD.
Methods
The study aimed to track the long-term prognosis of AKI patients whose basic renal function was normal, further identify the clinical features and risk factors associated with the prognosis of AKI patients, and calculate the proportion of renal function progression during follow-up period. We retrospectively analyzed clinical date of 166 patients who got AKI episode during hospitalization from Jan 1 2011 to Dec 31 2014 in the First Affiliated Hospital of Fujian Medical University.
Inclusion criteria: all patients more than 18 years old with at least two or more Serum creatinine (Scr) examinations during hospitalization were selected, and were discharged alive and followed up for more than 2 years after discharge.
Exclusion criteria: patients with less than 2 years of follow-up, basal renal function GFR <60 ml/min, hospitalization less than 24 hours, and an incomplete history. AKI was defined as an increase in Scr by 0.3 mg/dl within 48 hours or a 50% increase in Scr from the baseline within 7 days according to the KDIGO criteria. We selected patients who had at least two Scr tests within any 7-day. All these patients had normal basic renal function and had follow-up for more than two years after discharge. The complete recovery of renal function was defined that Scr was restored to no more than 44.2 mmol/L in hospital. Partial recovery was defined that Scr in the hospital exceeded the basic creatinine value of 44.2 mmol/L, but was less than the highest creatinine value in which condition patients did not require dialysis. Progression was defined that the Scr value of the patient was not decreased or increased, or that the patient was still dependent on dialysis. Then identify the clinical features and risk factors associated with the prognosis of AKI patients using multivariate logistic regression, and calculate the proportion of renal function progression during follow-up period.
Results
Finally 166 patients (average age was 58.1 ± 16.6) were included in the observational study, among whom 114 patients were men, 52 patients were women, and 87 patients were at AKI stage 1, 39 patients were at AKI stage 2, 40 patients were at AKI stage 3, while 37 patients had pre-renal cause, 113 patients had renal cause and 16 patients had post-renal cause. Of the 113 cases of renal cause, the etiology were nephrotic syndrome, drug-related, contrast agent related, cardiorenal syndrome, hepatorenal syndrome, sepsis, epidemic hemorrhagic fever, rhabdomyolysis, acute interstitial nephritis, and multiple myeloma renal damage. According to the renal function after two years, patients were divided into recover and non-recover group. Non-recover group included partial recovery and progression group. The recover group contained 102 patients while non-recover group contained 64 patients. Of the 37 cases with prerenal function, 22.5% (23/37) were recoverd, while there were 71.6% (73/113) recoverd in the renal cause group and 5.9% (6/16) in the post-renal cause group. No statistically significant difference was found in the AKI stage and etiology in different groups. Renal function recovery group's age, basic creatinine, discharge creatinine, complications, cardiovascular disease, infection, hypovolemic shock, and urinary tract abnormity were significantly less than that of non-recoverd group. Two groups were statistically significant (P > 0.05), while the comparison of other clinical features had no statistical difference.
Renal function when discharged (P = 0.002, OR = 2.980) and Infection (P = 0.003, OR = 2.786) were the risk factors of failing to recovery after two years. As the definition and standard of AKI are unified, there are more and more studies on the risk factors of AKI causing CKD. Most studies indicated that the main risk factors are age, basic complications such as diabetes, chronic kidney disease, severity of AKI, multiple organ failure, the dose of renal replacement therapy and pattern, anemia, sepsis and renal toxicity of drugs. Howere many of the studies were based on retrospective study, and due to the lack of the unity of the baseline renal function and prognosis judgement to the kidney, the primary disease and comorbidities and other confounding variables impacting on the results of the study, they had different emphases for different studied. To completely eliminate these influencing factors, a matching prospective study might be a feasible solution, and large prospective studies are expected to focus on the exploration of the risk factors for renal prognosis in AKI and its correlation with the occurrence and development of CKD/ESRD. Renal function during following-up: 84 patients' renal function returned to normal when discharged, but 1 year later 12 (14.3%) patients' renal function progressed to CKD3 stage and more, while there were 20 patients (23.8%) did so two years later. 54 patients were partial recovery and 28 patients were worsen when discharged, 1 year later 22 (40.7%) and 12 (42.9%) patients' renal function progressed to CKD3 stage and more respectively, while there were 28 patients (51.9%) and 16 (57.1%) did so two years later respectively.
Conclusion
The risk factors of AKI long-term renal outcome were renal function when discharged and infection. After AKI episode, even renal function was fully recoverd, it had great possibility to progress to CKD, we should strength the follow-up observation. This is a reminder that AKI patients who have returned to normal renal function after the AKI episode cannot be optimistic about fully overcoming the risk of renal dysfunction, especially for patients with multiple chronic complications who need to continue to be closely monitored. This study found that discharge renal function not being fully recovered in patients with AKI is the risk factor for kidney function getting deterioration, which may to some extent reflect that the CKD can be directly developed by the AKI progress. But whether the legacy of AKI episode or the patient's chronic complications such as hypertension, diabetes and other causes of CKD risk factors that lead the progress to CKD is still difficult to judge, which need further studies.
Keywords
Acute kidney injury (AKI), Chronic kidney disease (CKD), Long-term renal outcome.
Objective
To investigate the effect of the key transcription factor Sox9 on renal tubular epithelial cell regeneration. To determine whether Sox9 level upregulation can protect kidney damage, promote kidney repair, slow renal function deterioration, and focus on the role of Sox9 in renal tubular epithelial cell regeneration.
Method
1) Establishment of AKI rat model: ketamine and pentobarbital anesthetized mice, open the abdomen through the midline incision, expose the left kidney, separate the left renal artery, clamp the renal artery with non-invasive arterial clamp, reperfusion 90 minutes later, establish acute ischemic AKI model.
2) Experimentalgroup: Adult male and female rats were randomly selected and randomly divided into three groups: AKI group, AKI+overexpressing group, and AKI+down-regulating group. (Sox9 overexpresses the protein expressed by injection of sox9; Downregulation of Sox9 detects the expression of sox9 in renal tissue by detecting the infection rate of the AAV2/9 vector carrying Sox9).
3) In the AKI and renal cortex multiple injections of Sox9 over- or under-regulated AAV2/9 virus before and after: 1) Regular monitoring of 24-hour unit urine volume. 2) Before AKI (Day0), venous blood was taken regularly from 1 day, 2 days, 7 days, 14 days, and 28 days to detect serum creatinine (Cre), urea nitrogen (urea nitrogen, UN) by radioimmunoassay. Cystatin C and Interleukin-6 (IL-6) levels. 2) Puncture kidney tissue, biopsy, HE staining, examination of morphological changes of proximal renal tubular epithelial cells, immunohistochemical method, detection of the number, cell morphology and classification of Sox9-labeled cells in rhesus monkey kidney tissue, influence on cell construction 3) Measurement of Sox9 changes in the kidney; Sox9 protein and gene levels in kidney tissues of Day0, Day1, Day3, Day7, Day14, Day28 were determined by Western Blot and PCR.
Results
1. The renal function indexes of the rats were measured, and the serum creatinine and urea nitrogen levels were compared. The serum creatinine level of AKI+ overexpressing Sox9 group gradually decreased. The AKI+ downregulated Sox9 group serum creatinine level continued to increase; AKI serum creatinine showed a slow upward trend.
2. Kidney: Day14 acquired AKI+ overexpressed Sox9 group renal tubular epithelial cells edema, necrosis, tubular dilation significantly reduced, showing the increase and repair of proximal tubule epithelial cells; AKI+ down-regulated Sox9 group Day14 can be seen after the crescent Into, renal tubular epithelial cells are massively edematous and necrotic.
3. Overexpression of Sox9 in AKI+ peaked at 24–48 h after injury, which was 20 times higher than that in AKI group; while AKI+ down-regulated Sox9 and AKI did not detect Sox9; and we found that AKI+ overexpressed Sox9 blood on Day 28 Decreased creatinine levels remained at baseline and sox9 levels remained elevated.
Conclusion
As a transcription factor, Sox9 belongs to the Y-box family of sex-determining regions and plays a vital role in various tissues and organs including the kidney. Sox9 is a transcription factor necessary for AKI normal epithelial repair process. Up-regulation of sox9 plays a key role in AKI repair of renal tubular epithelial regeneration, promotes renal tubular epithelial cell regeneration and promotes renal repair, and slows renal function deterioration.
Keywords
Acute kidney injury, Sox9 gene, Promote, Renal tubular epithelial cell regeneration.
Objective
To investigate the reason and targeted to take effective measures to reduce the number of hospitalization of continuous ambulatoryperitoneal dialysis (CAPD) patients.
Method
A single center, retrospective clinical study was performed. A total of 331 cases of CAPD patients between January 2014 and December 2016 were enrolled. Rehospitalization was difined as the interval from the last discharge is more than 30 days, and the reason is the different or same from the last hospitalization. All cases were eligible for the study. The general data, clinical data, the reason for hospitalization after the regular peritoneal dialysis treatment of the patients were collected. SPSS 17.0 for Windows was used for statistical analyses.
Results
Among the 331 CAPD patients, 205 males and 126 females, average age was 54.6 ± 19.5 years and average dialysis age was 20 ± 9.7 months. The primary incidence were chronic glomerulonephritis (237 cases), diabetic nephropathy (62 cases), hypertension kidney damage (14 cases), polycystic kidney disease (2 cases), and 16 cases of unknown etiology. Rehospitalization rate is 40.5% (134 patients), rehospitalization for total 233 times. The main causes were infection (48.5%), including pulmonary infection (38.6%) and peritoneal dialysis related peritonitis (9.9%). The cardiovascular disease (20.6%) second, including acute heart failure (12%) and coronary heart disease (8.6%). There were also other reasons such as cerebrovascular accident (6.4%), uremia encephalopathy (6%), inadequate dialysis (6%), peritoneal dialysis tube loss of function (3.4%).
Conclusions
Infection, cardiovascular disease and cerebrovascular disease are the main causes leading to the rehospitalization of CAPD patients. Reasonable diet, strict sterile operation, adequate dialysis and active treatment of related complications will help to reduce the rehospitalization rate of CAPD patients.
Keywords
Continuous ambulatory peritoneal dialysis, Rehospitalization, Cause.
Objective
A well functional vascular acess (VA) can ensure the quality of dialysis and the life of dialysis patients. It is essential for maintenance hemodialysis (MHD) patients. However, it is known that many newly formed fistulae do not mature and have a higher restenosis rate to provide qualitative hemodialysis. The histology of intimal hyperplasia is a primary cause of AVF immaturation and failure, and characterized by an abundance of vascular smooth muscle cells. Platelet derived growth factor (PDGF) can promote the cells proliferation and migration and regulate vascular smooth muscle cell phenotype transformation. Although appropriative autophagy seems to be critical to the cell survival and preserve cell function, excessive autophagy cause the disease to occur. Little known about the relationship between autophagy and AVF intima hyperplasia. To investigate the role of autophagy in the pathogenesis of autologous arteriovenous fistula stenosis, providing the prevention and treatment of AVF stenosis in the future.
Methods
Venous vascular tissues were collected during the surgery of AVF angioplasty or recreation for MHD patients in the Third Hospital of Hebei Medical University from November 2016 to November 2017. The samples were divided into experimental group A, experimental group B and control group. We resected the stenosis and the adjacent stenosis part of the venous in AVF recreating operation and setted into the experimental group A (n = 10) and the experimental group B (n = 10). The control group (n = 10) venous tissues were discarded in AVF angioplasty operation. Histological changes were examined and the thickness of intima was measured after H-E staining of the venous tissues. Immunohistochemistry was used to examine the leval of Beclin-1, LC3II and PDGF-bb expression in the intima of venous tissues. Then we analyze the relation between the thickness of intima and growth factors expression. All data was analyzed by statistical analysis software SPSS 21.0 and expressed as mean ± SE (x±s). Probability values less than 0.05 were required for statistical significance.
Results
To analyszed the age and sex, there was no statistical difference between the two groups (P > 0.01).
1. HE staining: The thickness of intima and media in the vein were various degrees of thickened, and the thickness of intima was more obvious. The hyperplasia intima was composed of a large number of disordered smooth muscle cells under high magnification. We measured the mean ratio of intima/media thickness in the each group. There was related significant difference in each grops (p > 0.01).
- 2. Immunohistochemical Staining:
- 2.1. Beclin-1 is mainly expressed in the cytoplasm of VSMCs. The Beclin-1 strongly positive expressed in intima of the experimental group A, medium positive in media of the experimental group A. The medium positive expression was found in the intima and media of experimental group B. The expression of the intima and middle in the control group was weakly positive. The expression level of Beclin-1 in the experimental group A was higher than that of the experimental group B, with remained significance (P > 0.01).
- 2.2. LC3 II is mainly expressed in the cytoplasm of VSMCs. The protein of LC3 II strongly positive expressed in intima of the experimental group A, medium positive in media of the experimental group A. The medium positive expression was founded in theintima and media of experimental group B. The expression of the intima and middle in the control group was weakly positive. The expression level of LC3 II in the experimental group A was higher than that of the experimental group B, with remained significance (P > 0.01).
- 2.3. PDGF-bb is mainly expressed in the cytoplasm of VSMCs. The protein of PDGF- bb strongly positive expressed in intima of the experimental groupA, and the medium positive expression was found in the experimental group B. The expression of the intima and middle membrane in the control group was weakly positive. Compared of the expression of each groups, and there was statistical significance (P > 0.01).
- 2.4. Negative control for immunochemistry staining.
No positive staining expression was founded in both intima and media.
3. Correlation Analysis:
There was a positive correlation between PDGF-bb and Beclin-1 expression in each group (r = 0.883, P = 0.001; r = 0.919, P = 0.000; r = 0.947, P = 0.000). And the expression of Beclin-1 in each group was positively correlated with LC3 II (r = 0.859, P = 0.001; r = 0.896, P = 0.000; r = 0.997, P = 0.000).
Conclusions
1. Autophagy is involved in the process of wall reconstruction and lumen stenosis after the creation of AVF.
2. Moderate autophagy may contribute to the maturation of the internal fistula, but abnormal autophagy may lead to phenotypic transformation, proliferation and migration of VSMCs.
3. PDGF may be involved in cell phenotype transformation of vascular smooth muscle cellsby inducing autophagy. In future, it may be a new target for the prevention and treatment of AVF stenosis.
Keywords
Autophagy, Pathogenesis, AVF stenosis, LC3 II, PDGF-bb.
Objective
The current clinical guidelines recommend indirect access blood flow (Qa) measurement as one of the most important components in vascular access maintenance programs. The most extensively validated and accepted method of assessing the adequacy of flow is the ultrasound dilution (UD) method. However, the ultrasound detector is expensive and not available in all hemodialysis centers in China. Doppler ultrasound (DU) is the most widely used method of vascular access and has high accuracy in evaluating fistula stenosis. This study aims to evaluate the efficiency of access blood flow measurement with doppler ultrasound in comparison with ultrasound dilution and to examine the relationship between Qa and certain clinical characteristics.
Methods
103 Patients (77 men and 26 women) with well-functional arteriovenous fistula who were undergoing regular hemodialysis were included in this study. The arteriovenous anastomosis was located in the distal third of the forearm (between the radial artery and the cephalic vein) in 72 AVFs (distal RCAVFs) and in the proximal forearm in 31AVFs (proximal RCAVFs). The reference method of ultrasound dilution is used to measure access blood flow (Qa), cardiac output and recirculation at a QB between 200–300 ml/min. Doppler ultrasound was performed before dialysis to measure flow volume and diameter of cephalic vein and brachial artery. Clinical and laboratory data were collected at the same time.
Results
Patients were 56.5 ± 14.2 years old, had spent 62.5 ± 60.1 (median 35.1) months on dialysis, and had a body mass index of 23.2 ± 3.9 kg/m2. Median time from AVF creation to Qa measurement was 32 months (range 2.5–252.6). The mean Qa value obtained using ultrasound dilution (UD-Qa) was 955 ± 440 ml/min (range 280–2380). Mean CO was 6.5 ± 1.5 L/min (range 2.8–16.1) and CI was 3.7 ± 1.1 L/min/m2 (range 1.5–7.5). No patients had detectable recirculation measured by ultrasound dilution whether with stenosis or not.
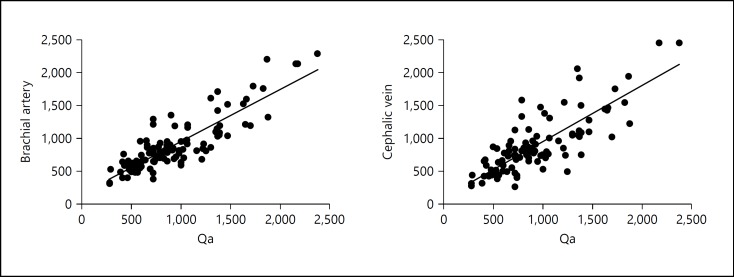
Access blood flow obtained with DU was 915 ± 406 mL/min at the brachial artery and 914 ± 468 mL/min at the cephalic vein. Figure 1 presents a graphical representation of the linear regression model. Using the Qa value obtained from the UD as a reference point, the brachial artery corresponded to 73.3%, and the cephalic vein was at 65.1%. The measurement bias between the two methods was defined as the difference in Qa values obtained between UD and DU in Bland-Altman mathematical model. The measurements taken from the brachial artery using doppler ultrasound with respect to the UD-Qa resulted in a mean value of 896 ± 398 mL/min, with a mean bias of −39 ± 229 ml/min. The mean value at the cephalic vein was 900 ± 460 mL/min, with a bias of −46 ± 282 ml/min. UD measurements classified 87.4% of patients as having a Qa ≥500 ml/min, and 12.6% as having a Qa <500 ml/min. The results from DU were 90.3% and 9.7% at the brachial artery, whereas those at the cephalic vein were 83.5% and 16.5%, respectively.
Fig. 1.
Graphical representation using linear regression for comparing measurements of vascular flow using Doppler ultrasound and Ultrasound dilution (for Abstract No 6).
Qa was significantly lower in patients with diabetes mellitus (compared with no diabetes mellitus, 734 ± 287 vs 1064 ± 464 ml/min, P > 0.001), in distal RCAVFs (compared with proximal RCAVFs, 888 ± 379 vs 1111 ± 533), and in female patients (compared with male, 784 ± 306 vs 1012 ± 466 ml/min, P = 0.006). Qa was also significantly higher in AVFs with long-term use (>5 years 1129 ± 517 vs <years 896 ± 399 ml/min, P = 0.043). There were no differences in Qa between groups defined by body mass index (>25, 994 ± 456 ml/min vs <25, 838 ± 379 ml/min, P = 0.119), and patient age (>65 years, 911 ± 381 ml/min vs <65 years, 976 ± 468 ml/min, P = 0.488). Using mixed models to correct for autocorrelation, we examined the univariate relationship between Qa and each clinical characteristic in turn. We found that diabetic status was significantly associated with lower Qa, patient sex and the interval between AVF creation and Qa measurement were not significantly associated with Qa.
Conclusions
According to our results, DU is a useful automated and non-invasive method for measuring Qa as compared to UD. In patients with RCAVFs, Qa measurements in the brachial artery showed a greater correlation with values taken from UD. Patients with diabetes had a significant lower Qa and a higher prevalence of stenosis. Vascular access maintenance programs might be more helpful in those high-risk patients. Further work is on our schedule to determine whether such factors would associate with fistula dysfunction and patency loss.
Keywords
Hemodialysis, Access blood flow (Qa), Doppler ultrasound, Indicator dilution techniques.
Objective
The volume of hemodialysis patients with hypertension has always been a problem, and some hypertensive patients show asfluidoverload, but someone not. We intend to analyze the difference of predialysis fluidoverload and non-fluidoverload in patients with hypertension by bioelectrical impedance, which may help to provide references for clinical blood pressure control.
Methods
From 300 maintain hemodialysis patients in the blood purification center of Mingji hospital, 51 patients were enrolled because of dialysis for above 3 months and the predialysis systolic blood pressure was greater than 160 mm Hg. These patients are divided into volume-increasing group (group A) and non-volume-increasing group (group B), then blood pressure, laboratory examination, bioelectrical impedance measured parameters (static fluid load and tissue nutritional condition, vector analysis, illmarker, phase angle) and clinical outcomes were compared between the two groups.
Results
There were 34 males and 17 females in the 51 hypertensive patients with an average of 60 years old.78.4% of the patients had received dialysis treatment for one to teen years. The primary renal diseases were glomerulonephritis, diabetic nephropathy and hypertension nephropathy, accounting for 37%, 27% and 21%, respectively. Bioelectrical impedance vector analysis indicated that there were 19 patients with fluidoverload (group A) and 32 patients not (group B). Between the two groups there was no significant difference in systolic and diastolic blood pressure before dialysis (systolic blood pressure: 167 ± 25 vs. 162 ± 15 mm Hg, p = 0.444; diastolic blood pressure: 83.7 ± 17.3 vs. 84.4 ± 15 mm Hg, p = 0.895). However there was a significant difference in age (66 ± 16 vs. 57 ± 15 years, p = 0.054). Patients with volume-increasing hypertension were older, and appeared lower plasma albumin (37.1 ± 5.7 vs. 41.1 ± 3.9 g/l, p = 0.005), pre-albumin (218.9 ± 83 vs. 356.1 ± 93 mg/l, p = 0.000) and hemoglobin (93.5 ± 19.1 vs. 112.2 ± 15 g /l, p = 0.001). Bioelectrical impedance vector analysis was used to assess tissue nutritional status. However, no difference was found. 7 cases of malnutrition in group A (37%) and 12 cases in group B (37.5%), showing no statistical difference. Outcome of the two groups perhaps is deferent. Two important parameters of bioelectrical impedance analysis, phase Angle and illnessmarker, which had been widely confirmed to be closely related to patient prognosis, were significantly different. The fluidoverload patients presented higher illnessmarker (0.881 ± 0.042 vs. 0.826 ± 0.046, p = 0.000) and lower phase Angle (3.4 ± 1.0 vs. 4.9 ± 1.3, p = 0.000). Though Kaplan-Meier survival curve analysis revealed that the survival rate of the two groups was not statistically different (P = 0.207), a trend is that with the extension of follow-up time, the mortality difference between the two groups showedincreasing.
Calculation formula of illnessmarker parameters: Illnessmarker = bioimpedence (200 kHz)/bioimpedence (5 kHz).
Conclusions
Hemodialysis patients with hypertension partly show volume increase, compared with the non-volume-increasing group, serum nutrition indicators appear significant different, such as albumin, hemoglobin, albumin. So we think nutrition may contribute to hypertension pathogenesis mechanism, poor nutritional status of patients are more likely to suffer from high blood pressure with fluidoverload. In addition, there is potential difference in prognosis between the two groups. The patients with non-volume-increasing hypertension perhaps have better outcomes than the other group. We hypothesize that improving the nutrition of dialysis patients helps to controlhypertension andthus improve prognosis. Further research is needed to confirm this conclusion.
Keywords
Hemodialysis, Hypertension, Bioelectrical impedance, Fluid load.
Objective
to explore the effects of 15G and 16G puncture on arterial pressure monitoring and online urea clearance monitoring (OCM) in hemodialysis patients.
Methods
fifty patients with dry body weight over 70 Kg who were treated with maintenance hemodialysis using arteriovenous internal fistula were dialyzed with their fixed blood flow, and three times of hemodialysis were performed with 15G and 16G puncture needles, respectively, to compare the mean test values of arterial pressure and dialysis sufficiency.
Results
by comparison, it was found that the average blood flow was 325 ± 25 ml/min at the time of dialysis, and the mean arterial pressure was −149 ± 21 mm Hg at the time of 15G internal fistula puncture needle use, while the mean arterial pressure was −182 ± 31 mm Hg at the time of 16G internal fistula needle use. There were significant differences in arterial pressure statistics between the two groups (P > 0.01). When the 15G puncture needle was used in Kt/V, the online Kt/V was 1.12 ± 0.18; when the 16G needle was used, the online Kt/V was 1.04 ± 0.21, showing statistical differences (P > 0.050 kg of blood).
Conclusion
15G puncture needle can significantly reduce arterial pressure and improve the dialysis sufficiency of patients with body weight higher than 70 kg.
Keywords
Puncture needle, Arterial pressure test, Hemodialysis, On-line urea clearance rate monitoring.
Objective
The main causes of arteriovenous fistula inmaturation and dysfunction are stenosis and thrombosis, which are often associated with stenosis and are most likely to form thrombosis near the narrow area. The intimal hyperplasia of arteriovenous fistula is considered as the main manifestation of arteriovenous fistula stenosis. The changes of coagulation system, hemodynamics and inflammation play an important role in the occurrence and development of arteriovenous fistula stenosis. This study was to
investigate whether there was a correlation between postoperative stenosis of arteriovenous fistula and preoperative basic items and inflammatory items.
Methods
From July 2014 to June 2016, 216 patients who received arteriovenous fistula formation in the nephrology department of Zhejiang Provincial People's Hospital were included. These patients received arteriovenous fistula formation. Before operation, patients' BMI, blood pressure, albumin, calcium, phosphate, lipid, PTH, super CRP and CBC were tested. 12 weeks after arteriovenous fistula formation, the patients were screened with Doppler ultrasound and seperated to arteriovenous fistula stenosis group or normal arteriovenous fistula group. Arteriovenous fistula stenosis was diagnosed as diameter narrowing greater than 50% of normal vessel. The basic items and inflammatory items were compared between the two groups, and the items which had obviously difference between two groups were found out. Then the patients in arteriovenous fistula stenosis group were divided into 3 groups according to the degree of stenosis: ≥50%, <75%, ≥75%, <90% and ≥90%. The relationship between items which had obviously difference and the stenosis degree of arteriovenous fistula was analyzed.
Results
There were 47 patients in arteriovenous fistula stenosis group and 169 patients in normal arteriovenous fistula group. Most preoperative items had no difference between two groups, but the neutrophil-lymphocyte ratio (NLR) and the HDL had statistically significant difference between two groups. HDL in arteriovenous fistula stenosis group was 0.888 ± 0.187 mmol/l (ranged from 0.59 to 1.16 mmol/l), when HDL in normal arteriovenous fistula group was 1.374 ± 0.279 mmol/l (ranged from 0.92 to 1.99 mmol/l). NLR in arteriovenous fistula stenosis group was 3.956 ± 0.943 (ranged from 2.688 to 5.754), when NLR in normal arteriovenous fistula group was 1.790 ± 0.335 (ranged from 1.214 to 2.644). The maximum NLR in normal arteriovenous fistula group was 2.644, when the minimum NLR of arteriovenous fistula stenosis group was 2.688. NLR more than 2.688 maybe the boundary to predict post-operative arteriovenous fistula stenosis. HDL level had no relationship with arteriovenous fistula stenosis (P > 0.05), but NLR level had (r = 0.7194, p > 0.0001). In arteriovenous fistula stenosis group, the degree of arteriovenous fistula stenosis increased with NLR level.
Conclusion
For hemodialysis patients, the neutrophil-lymphocyte ratio before arteriovenous fistula formation may predict the post-operation arteriovenous fistula stenosis. For patients with NLR more than 2.688 before arteriovenous fistula formation, we should pay more attention to post-operation arteriovenous fistula stenosis.
Keywords
Arteriovenous fistula, Stenosis, Neutrophils-lymphocyte ratio.