Abstract
BACKGROUND
Hospitalizations for severe infections associated with substance use disorder (SUD) are increasing. People with SUD often remain hospitalized for many weeks instead of completing intravenous antibiotics at home; often, they are denied skilled nursing facility admission. Residential SUD treatment facilities are not equipped to administer intravenous antibiotics. We developed a medically enhanced residential treatment (MERT) model integrating residential SUD treatment and long-term IV antibiotics as part of a broader hospital-based addiction medicine service. MERT had low recruitment and retention, and ended after six months. The goal of this study was to describe the feasibility and acceptability of MERT, to understand implementation factors, and explore lessons learned.
METHODS
We conducted a mixed-methods evaluation. We included all potentially eligible MERT patients, defined by those needing ≥2 weeks of intravenous antibiotics discharged from February 1 to August 1, 2016. We used chart review to identify diagnoses, antibiotic treatment location, and number of recommended and actual IV antibiotic-days completed. We audio-recorded and transcribed key informant interviews with patients and staff. We conducted an ethnographic analysis of interview transcripts and implementation field notes.
RESULTS
Of the 45 patients needing long-term intravenous antibiotics, 18 were ineligible and 20 declined MERT. 7 enrolled in MERT and three completed their recommended intravenous antibiotic course. MERT recruitment barriers included patient ambivalence towards residential treatment, wanting to prioritize physical health needs, and fears of untreated pain in residential. MERT retention barriers included high demands of residential treatment, restrictive practices due to PICC lines, and perceptions by staff and other residents that MERT patients “stood out” as “different.” Despite the challenges, key informants felt MERT was a positive construct.
CONCLUSIONS
Though MERT had many possible advantages; it proved more challenging to implement than anticipated. Our lessons may be applicable to future models integrating post-hospital intravenous antibiotics and SUD care.
Introduction
United States hospitalizations for severe infections such as endocarditis and osteomyelitis among people with substance use disorder (SUD) have doubled in the last decade.1 Treatment for such infections typically requires six to eight weeks of intravenous (IV) antibiotics, and may require heart-valve surgery or other invasive procedures.
Many people can complete a prolonged course of IV antibiotics at home or in a post-acute care skilled nursing facility (SNF). However, people with SUD are often deemed unsafe to discharge home with IV antibiotics because of social risks such as homelessness or continued drug use; and often, they are denied admission to post-acute care facilities.2, 3 Thus, many with SUD have hospitalizations that extend weeks or months to complete an antibiotic course.4
Despite this, outcomes remain poor. People with SUD are more likely to be denied valve surgery, leave the hospital against medical advice, and die.2, 5 Hospital systems commonly do not provide SUD treatment, yet hospitalization can be a reachable moment to initiate and coordinate SUD treatment.6
Just as hospitals are not equipped to provide SUD treatment, SUD treatment settings are not equipped to provide complex medical care.4 Residential addiction treatment settings are not routinely staffed by physicians or nurses and do not have expertise to provide wound care, intravenous antibiotics, or other physical health care.
Studies examining alternative care models to address combined antibiotic and SUD needs are limited. One single-site, retrospective study retrospectively reviewed 205 medical charts of patients discharged to a residential addiction treatment setting where they received IV antibiotics between 2006 and 2011.7 Seventy-three percent of patients completed their course of antibiotics, with sizable savings in hospital days and costs. However, this study did not report patient characteristics, preferences, or outcomes of those who did not enter this care model. This study did not describe patient or SUD treatment provider experiences, nor did it describe implementation experience.
We developed and implemented a medically enhanced residential treatment (MERT) model as part of a broader hospital-based addiction medicine service4. MERT aimed to deliver IV antibiotics in residential addiction treatment for patients with SUD who were medically stable for discharge but needed ongoing long-term IV antibiotics. While the overall hospital-based addiction medicine service thrived, MERT had low recruitment and retention. Ultimately we decided to end MERT after six months. The goal of this study was to describe the feasibility and acceptability of MERT; and, given limited acceptability, to understand implementation barriers and explore lessons learned.
Methods
MERT was part of a multicomponent hospital-based addiction medicine intervention, the Improving Addiction Care Team (IMPACT) that includes care from addiction medicine physicians, social workers, and peers with lived experience in recovery. All MERT patients received care from IMPACT. Earlier studies describe IMPACT rationale and design.4, 6 Our institutional review board approved all study procedures.
Setting
MERT was a collaboration between a university hospital, a community-based SUD treatment agency, and a specialty infusion pharmacy. The hospital is a 522-bed urban academic medical center in Oregon. During the study period, the hospital had an Outpatient Parenteral Antibiotic Therapy (OPAT) program. OPAT managed all patients leaving the hospital with intravenous antibiotics and included direct medical care from infectious disease providers and intensive case management. OPAT monitored antibiotic complications, completion, and follow up needs (e.g. laboratory tests).
The community-based SUD treatment agency (CODA) is a non-profit agency that provides outpatient treatment, medication for addiction treatment (MAT) (e.g. methadone, buprenorphine), medically supervised withdrawal, and residential treatment. The residential site that housed MERT includes 42 men’s beds and 22 women’s beds. Prior to MERT, residential treatment did not have nursing or medical staff. Residential treatment enforced the traditional 30-day “blackout period” during which unsupervised visitors, personal mobile devices, and internet use is prohibited. CODA agreed to prioritize MERT patients waiting for a residential bed.
The specialty infusion pharmacy is a private company whose nurses deliver home infusion services including antibiotic administration and real-time support in the case of complications (e.g. catheter malfunction). The company had not previously worked in residential treatment.
Intervention Description
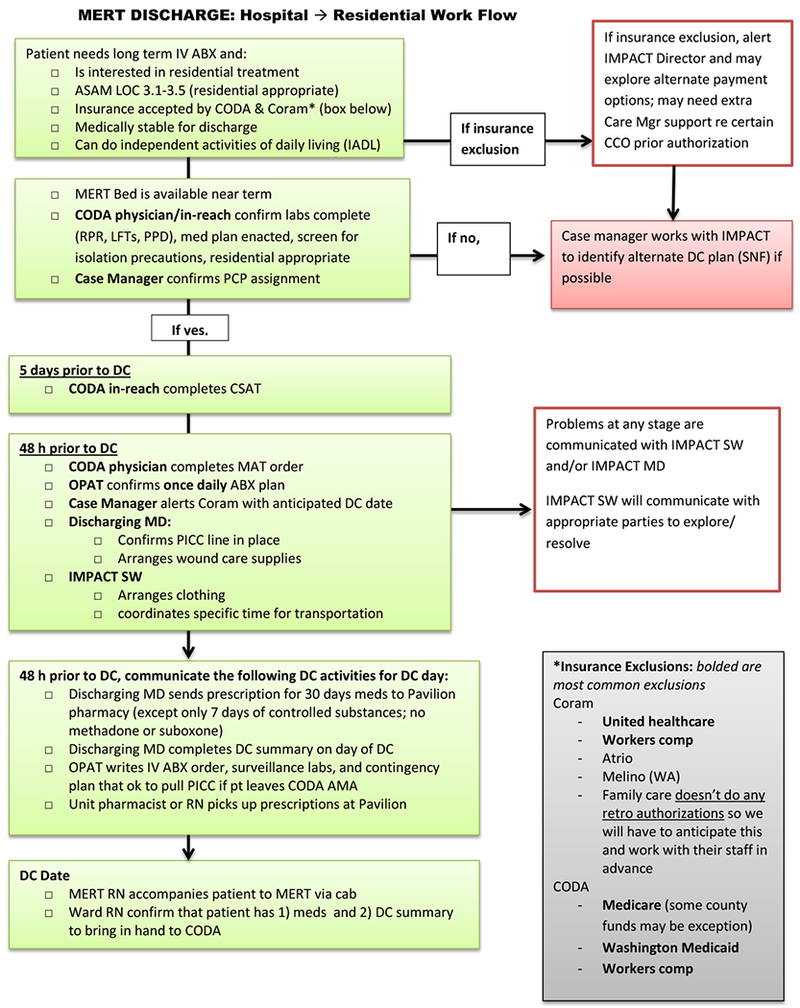
MERT was located within a traditional residential addiction treatment setting where residents were expected to participate in 20 hours of groups and 1 hour of individual therapy each week. Home infusion nurses administered daily antibiotic infusions and performed weekly dressing changes of peripherally inserted central catheters (PICC). The MERT registered nurse (RN) did an in-person handoff with hospital nurses and IMPACT prior to discharge and accompanied patients directly from hospital to MERT. All team members were informed of the workflow (appendix). The MERT RN coordinated post-hospital medical care and attended all off-campus follow-up visits. MERT patients and MERT RN participated in weekly telemedicine rounds with the hospital-based infectious disease team. We made establishing with a primary care provider (and in some cases a mental health provider) a requirement for MERT.
Hospital-based infectious disease teams referred all patients needing long-term IV antibiotics (defined as ≥2 weeks) with SUD to IMPACT, and all were considered for MERT. MERT patients had to agree to enroll in residential SUD treatment; meet residential treatment criteria based on addiction severity (ASAM level of care 3.1-3.5); perform activities of daily living independently; require no more than once daily antibiotic infusions; limit prescription opioids for pain to no more than three times daily with a taper plan; and, have insurance that would cover residential addiction treatment at CODA.
During hospitalization, an IMPACT social worker assessed all potential MERT patients’ interest in MERT and worked to enhance treatment motivation. The MERT registered nurse (RN) visited all interested patients in their hospital room to discuss treatment expectations and to review the anticipated residential care plan.
Intervention Financing
MERT was funded by Oregon Health & Science University and a Medicaid coordinated care organization.4 We estimated that MERT would serve approximately 30 patients/year and 3 individuals at any time. We contracted to pay infusion pharmacy for 6-days/week of infusion costs (insurance covers once-weekly home infusion) and we supported additional CODA residential staffing that included 0.1 physician, 0.7 RN, 0.2 residential manager time.4 The hospital infectious disease OPAT team provided in-kind support for 30 minutes/week telehealth rounds.
Implementation Process
We constructed stakeholder partnerships that were integral to the design,4 implementation, and evaluation phases of MERT. We held on-site planning visits at the hospital and residential settings that included all partners. During implementation we held biweekly meetings with IMPACT clinicians and residential staff to identify potentially eligible patients and discuss barriers and potential solutions. As we identified barriers (e.g. residential staff discomfort with wound care), we provided staff trainings to address them. We also modified the intervention to better serve complex patient-care needs. For example, IMPACT helped patients change insurance and tailored antibiotics to once daily regimens if possible. In one case, IMPACT worked with federal marshals and local parole officers to squash warrants to avoid incarceration and permit entrance into residential. We held quarterly meetings with all partners across organizations and roles (e.g. clinical care, implementation, evaluation).
Evaluation
We conducted a mixed-methods evaluation of MERT implementation. We employed a sequential explanatory research design,8 using qualitative data to gain a deeper understanding of quantitative results. Our evaluation included all IMPACT patients who were potentially eligible for MERT, as defined by those needing at least 2 weeks of IV antibiotics who were discharged between February 1 and August 1, 2016.
Quantitative data collection and analysis
We collected demographic data including age, gender, race, and insurance from hospital administrative data. We collected data on housing and substance use from an IMPACT study registry. We performed chart review to identify primary hospital diagnosis, antibiotic treatment location (MERT, hospital, SNF, home); number of recommended IV antibiotic days and actual IV antibiotic days completed. We used a study registry to identify reasons people did not attempt MERT and confirmed reasons by chart review.
We defined antibiotic completion if the actual number of treatment days was greater than or equal to the number of days of IV antibiotics recommended. We considered salvage therapy if patients transitioned to oral therapy prior to completing the recommended IV antibiotic course. We considered therapy incomplete if participants completed neither IV antibiotics nor salvage therapy.
Qualitative data collection and analysis
We performed semi-structured interviews with key informants to understand barriers, facilitators, and effects of MERT. We also reviewed MERT development and implementation field notes. We used purposive sampling to identify six key informants including: an IMPACT social worker, the CODA-IMPACT liaison, an IMPACT physician, CODA’s executive director, the residential manager, and the MERT RN. We conducted qualitative interviews with four patients who needed long-term IV antibiotics, two who went to MERT and two who did not. Patient participants completed interviews approximately 30 days after hospital discharge.
All interviews were audio recorded and transcribed. We conducted an ethnographic analysis of interview transcripts and field notes, focusing on insights that may best describe the phenomenon and inform future interventions.9 Two authors independently coded all transcripts and reconciled codes by consensus. We reviewed preliminary findings with key informants as a form of member checking. The full team, including experts in qualitative methods and SUD, finalized results.
Results
Recruitment
During the study period there were 45 patients needing long-term IV antibiotics (Table 1). Eighteen were ineligible, 20 declined, and 7 discharged to MERT. Patients were ineligible for various reasons, including active warrants, insurance, need for multiple daily antibiotic infusions, inability to perform independent activities of daily living, ongoing physical rehabilitation needs. Most patients who declined were unwilling to commit to residential treatment (Figure 1).
Table 1.
Demographics of patients needing IV antibiotics and SUD treatment, comparing MERT and non-MERT individuals by antibiotic treatment location
| All (n=45) |
Hospital (n=24) |
MERT (n=7) |
SNF (n=11) |
Home (n=3) |
|
|---|---|---|---|---|---|
| Mean age in years (range) | 39 (21-69) | 37 (21-69) | 38 (28-57) | 43 (25-55) | 36 (27-46) |
| Female Gender n (%) | 20 (44%) | 12 (46%) | 2 (29%) | 4 (36%) | 2 (67%) |
| Non-Hispanic White n (%) | 38 (84%) | 20 (83%) | 6 (86%) | 10 (91%) | 2 (67%) |
| Any Insurance (%) | 45 (100%) | ||||
| Oregon Medicaid | 33 (73%) | 19 (79%) | 4 (57%) | 8 (73%) | 2 (67%) |
| Insecure housing n (%) | 23 (51%) | 17 (71%) | 2 (29%) | 3 (27%) | 1 (33%) |
| Substance Use Disorder (%)* | |||||
| Opioid | 37 (82%) | 23 (96%) | 7 (100%) | 5 (45%) | 2 (67%) |
| Methamphetamine | 27 (60%) | 17 (71%) | 2 (29%) | 7 (64%) | 1 (33%) |
| Cocaine | 5 (11%) | 3 (16%) | 1 (14%) | 0 | 1 (33%) |
| Alcohol | 5 (11%) | 2 (8%) | 0 | 3 (27%) | 0 |
| Benzodiazepine | 3 (7%) | 0 | 2 (29%) | 1 (9%) | 0 |
| Any Severe SUD (%)* | 38 (84%) | 23 (96%) | 6 (86%) | 8 (73%) | 1(33%) |
| Polysubstance use (%) | 28 (62%) | 18 (75%) | 5 (71%) | 4 (36%) | 1 (33%) |
| Infection site | |||||
| Endocarditis | 16 (36%) | 11 (46%) | 1 (14%) | 4 (36%) | 0 |
| Osteomyelitis | 14 (31%) | 6 (25%) | 3 (43%) | 4 (36%) | 1 (33%) |
| Bacteremia | 9 (20%) | 6 (25%) | 0 | 1 (9%) | 2 (67%) |
| Other | 6 (13%) | 1 (4%) | 3 (43%) | 2 (18%) | 0 |
Defined by Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) criteria as assessed by IMPACT clinicians
Figure 1:
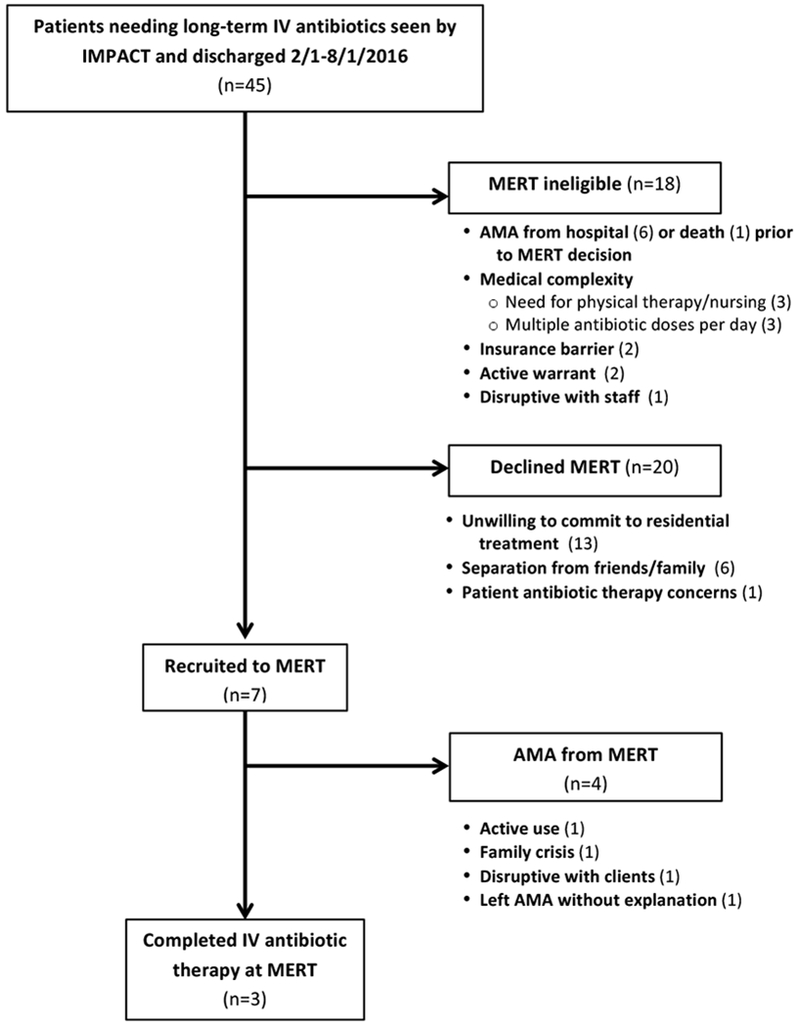
Participant flow diagram.
Key informants repeatedly described that MERT was “hard to sell.” Many patients expressed ambivalence towards residential treatment, especially after acute hospitalization. As an IMPACT physician recalled:
“Many patients would say, I want to address my medical issues now and then I’ll address my addiction issues after… we heard [that] over and over.”
For some, ambivalence was exacerbated by a changing medical plan and discharge date, which made coordinating a residential bed difficult. Facing so many “what-if’s,” some patients’ motivation waned. Some had concerns about the demands of a highly structured treatment program and others did not want to be separated from friends, family, pets and home.
Patients also worried about getting adequate pain control in residential, and feared that by agreeing to MERT, they would have to forgo pain medication. As one patient who attended MERT recalled,
“Having my surgery on my back, and then 10 days later, “let’s stick you in a treatment facility”… where I had to walk around and take classes…. I was initially worried about my physical ability to do so…. I was gonna be in a significant amount of pain… [and] the transition from my oxycodone and dilaudid to methadone concerned me at first…”
Retention
Of the 7 patients who went to MERT, 4 left against medical advice (AMA) before completing the recommended antibiotic course. Key informants highlighted “culture shock” with the transition from the hospital to MERT. They repeatedly described that the 20-hours of per week of groups was challenging for MERT patients. As MERT’s residential manager described:
“Patients were in the hospital for long periods of time, so there was a lot of downtime… and once they got into treatment… you’re talking about a pretty strict schedule. They were expected to get up at a certain time, your meal is at a certain time, you have to go take your medications. And you have to do that as opposed to a nurse getting everything to you, and I can watch TV and sleep in… it is a different mindset that you really had to be ready for.”
In some cases, staff perceived MERT patients’ lesser participation in residential as disruptive to the treatment environment.
Attitudes of residential staff towards medical complexity may have influenced retention. An IMPACT social worker recalled his sense that, “[some] counselors were refusing to work with the MERT patients… because of the medical complexities. Not because they didn’t like them or want them, but because they were hard, difficult, complex people.” Residential staff often felt “on edge” because patients had PICC lines, which they feared were “a direct portal right to their heart, they could overdose at any moment.” These fears increased staffs’ vigilance and led them to implement added restrictions for MERT patients. As the residential program manager described:
“[Staff] couldn’t let them out into the community. We couldn’t let them … be outside and do exercise walks, or those kinds of things because it was really high risk… It’s hard to watch your peers be able to come and go in the community, and you not be able to participate.”
These restrictions were repeatedly identified as a key barrier to MERT completion rates, and led to MERT patient dissatisfaction. As one patient described, MERT felt “like jail” and he felt “completely lied to.” IMPACT leadership, inpatient addiction medicine, and infectious disease teams only learned about these restrictions after MERT had ended.
Finally, key informants described that MERT patients were often “isolated” from other residents. They speculated that this resulted partly from fear of contagion given visible wounds, stigma towards those with medical illness, resentment of “special treatment” that allowed MERT patients to be accompanied to off-campus medical appointments, and use of MAT that was uncommon amongst other residents. The IMPACT-CODA liaison described:
“A lot of the patients at residential sort of pushed against that. The IMPACT patients, like, you just sort of got here. And you took someone else’s bed… you don’t have to go to groups because you have to go to an appointment. Or just like, you get specialized care. And that just really rubbed against patients the wrong way.”
Potential Utility
Though overall IV antibiotic completion was low (44%), a majority of participants either completed ≥80% of recommended IV antibiotics (64%) and/or completed salvage therapy (24%). A combination of discharge to MERT, SNF, or home allowed for 384 days of IV antibiotics delivered outside of the hospital. Though numbers are too small for statistical comparisons, information about antibiotic completion rates and out-of-hospital IV antibiotic days are presented in table 2.
Table 2.
Antibiotic completion rates and out-of-hospital IV antibiotic days by planned antibiotic treatment location*
| All (n=45) |
Hospital (n=24) |
MERT (n=7) |
SNF (n=11) |
Home (n=3) |
|
|---|---|---|---|---|---|
| Completed recommended IV antibiotic course, % (n) | 44% (20) | 42% (11) | 43% (3) | 64% (7) | 33% (1) |
| Completed at least 80% of recommended IV antibiotic course, % (n) | 64% (29) | 67% (16) | 43% (3) | 73% (8) | 67% (2) |
| Salvage therapy with oral antibiotics, % (n)** | 24% (11) | 21% (5) | 29% (2) | 18% (2) | 67% (2) |
| Total out-of-hospital IV antibiotic days | 384 | 0 | 101 | 226 | 57 |
All participants initiated their course of IV antibiotics in the hospital. This table describes the intended location for completion of IV antibiotic treatment.
Salvage therapy includes those who were transitioned from IV to oral antibiotics
Despite the challenges, nearly all respondents felt that the MERT construct was positive and worth pursuing again. Respondents felt that the patients who completed MERT benefitted greatly. As the MERT RN emphasized, “there wasn’t anything else like it … the people it did impact, it profoundly impacted.” Respondents praised MERT’s success with highly motivated patients, particularly those with external motivating factors such as reuniting with their family or avoiding legal issues.
This sentiment was echoed by one patient who completed the program:
“I’m so grateful for this program cause instead of being in the hospital… and just basically doing nothing except getting your injection every day… out here, not only do I get to address my addiction, but I have the opportunity to go to NA meetings or AA meetings… Initially, I probably went into the program saying ‘hey, well I’ll just wait for my antibiotics to be done and then I can leave.’ Well, no. After a couple a days, I’m like that’s not what I really want. I want to finish this program. I need to do things differently.”
Finally, independent of MERT’s explicit goal to facilitate access to IV antibiotics, respondents noted that having an on-site nursing increased residential treatment’s ability to care for more medically complex patients, including expanded use of MAT in residential (which he estimated “almost doubled”) and more staff familiarity caring for patients with wounds, diabetes, or other common medical problems.
MERT alternatives
The majority of participants did not go to MERT, and instead went to SNF or stayed in the hospital. However, these settings had different limitations. SNFs commonly resisted accepting patients with SUD or homelessness, and SNFs felt they had limited ability to administer methadone due to their interpretation of federal regulations. SNF staff typically had no addiction training and the SNF environment was largely unmonitored with reports of active drug use on premises. Many SNF patients also felt ostracized due to their SUD. Hospital was a more controlled environment; however prolonged admissions are extremely costly. Furthermore, even with IMPACT, hospital care had limited ability to prepare patients for post-hospital trigger-rich environments. As one staff participant described: “Just leaving the hospital… as soon as you drive down Burnside [street], you’re in a more trigger rich environment. And you begin to lose people.”
Discussion
Though MERT had many possible theoretical advantages, it proved more challenging to implement than anticipated. Recruitment barriers included patient’s medical complexity, patient concerns about physical health and pain, and ambivalence towards residential treatment. Retention barriers included high demands of residential treatment, restrictive residential practices due to PICC lines, and the perception that MERT patients “stood out” as “different.” Despite the challenges, the majority of patients completed IV antibiotic or salvage therapy and MERT saved a modest number of hospital days. Most providers felt that there was some value in the care model that should inform future trial.
Our experience builds on existing research in several important ways. An earlier study by Jewell and colleagues7 describes a program that continued successfully for 6 years with higher retention rates (73% completing IV-antibiotics versus our 43%) and relatively low patient-volumes (<3 patients/month). While an important precedent, Jewell and colleagues do not describe recruitment – describing experiences only of those who went to their program – nor do they elaborate on patient/staff experience. Our finding that many patients did not want residential treatment serves as an important caution that programs such as Jewell’s may not be a solution for many patients and health systems.
Differences in the Jewell program and ours highlight potentially important differences in settings and implementation strategies. Higher retention rates in Jewell could be related to pre-existing on-site nursing staff in residential treatment, which may have increased residential staffs’ comfort managing medical problems and mitigated the perception that patients with medical illness were ‘different.’ Also, Jewell included a fixed monthly rate to reserve residential bed-capacity and an additional payment for each day a bed was occupied. In MERT, additional staff were financed up-front and were an expense even if there were no MERT patients. A daily rate may have incentivized residential staff to retain patients in residential and reduced financial strain on the hospital in that the hospital would pay for a resource proportional to its use. Importantly, the Jewell program was implemented in a more integrated system. The effort necessary to initiate and maintain MERT in non-integrated systems may be substantially greater. Finally, the challenges we had with patients who discharged to SNF echo others’ description of post-acute barriers for patients with SUD in SNF.10
Our experience designing and implementing IMPACT supports that hospitalization is a reachable moment to engage patients and initiate addiction care.6 However, residential treatment may represent a higher bar, particularly given the intensive residential addiction treatment demands; the restrictions on visitors, cell phones and internet; and limitations on opioid pain medications. Fear of unmet pain needs is a common concern amongst hospitalized patients with SUD.11 Others have questioned whether such restrictions are necessary.12 Our experience suggests that these barriers may dissuade patients from entering or completing residential treatment.
Our study has several key limitations. First, it took place at a single-academic medical center and single residential treatment program in Oregon, limiting the generalizability of our findings. Our six-month experience included a small number of participants. Though we did not have large enough numbers to compare outcomes across various settings, we present outcomes for patients who remained inpatient or discharged to MERT, SNF, and home. Our qualitative evaluation focused on MERT and was not designed to thoroughly explore other treatment settings, a topic of future investigation. Despite these limitations, our experience may be important to others trying to improve care for people requiring intravenous antibiotics with SUD.
Our experience has several key implications. The finding that hospitalized patients declined residential treatment is important and suggests the need for flexible, patient-centered post-acute care models that can engage patients who range from pre-contemplative to action stages of change. Findings that residential staff felt “on edge” and that patients with medical problems “stood out” in residential treatment underscore the need for training to support integrated physical and behavioral health models. Though we hired an on-site MERT nurse and part-time physician who led some training, we underestimated the time and support residential staff would need to feel comfortable working with recently hospitalized patients. Future efforts might benefit from more dedicated time and resources for staff education, including all-staff trainings about PICC lines, MAT, and pain. Finally, though MERT was developed based on a patient needs assessment and broad stakeholder input4, our experience raises the question of whether a more iterative design process that included ongoing feedback from adults with SUD and residential staff may have led to a more successful intervention. Our experience highlights the need to anticipate and adapt to barriers relating to patients with SUD (e.g. concerns about pain management), organizations (e.g. changing hospital discharge dates and residential bed capacity), and the program itself (e.g. staff attitudes).
Despite our challenges, we believe there may still be benefit to creating options for patients to receive long-term IV antibiotics outside of the hospital. Even with low recruitment and retention, we saved over 300 hospital days with the majority of patients completing IV antibiotics or salvage therapy. Our findings underscore the need for more flexible, patient-centered treatment models. Future programs might integrate addiction supports into post-acute medical care. Given high prevalence of homelessness among people with SUD, a model that warrants exploration is to integrate IV antibiotics and substance use treatment in medical respite facilities.13 Medical respite – which is proliferating across the US - provides post-acute medical care for homeless persons who are too ill to recover from a physical illness on the streets.14 Medical respite could be staffed with nurses to provide infusions and case management; physicians to prescribe opioid agonist therapy; and, recovery supports, including peers in recovery. Alternatively, studies might explore modifying physical health treatment plans to accommodate patients’ behavioral health needs, for example, exploring off-label once weekly antibiotic infusions for patients who decline SNF or threaten to leave the hospital AMA.
Future implementation research should explore alternative models of integrated treatment for patients with SUD requiring long-term intravenous antibiotics. It is unlikely that a single solution will emerge, especially given variations in settings and resources across communities. However, the lessons of our experience, including patient ambivalence towards residential treatment and the challenges of delivering physical healthcare in a residential addiction setting, are likely to be applicable in future models.
Acknowledgements:
Authors would like to thank Claire Dorfman, Alison Noice, Luke Strnad, Tara Williams, and Catherine Maria Michalczyk for their support of this work. Authors would also like to acknowledge Daren Ford, Onesha Cochran, Jeff Ottenbecher, Lisa Rivers, Pen Barnes, and the entire IMPACT clinical team. Dr. Korthuis’ time was supported through grants from the NIH National Institute on Drug Abuse (UG3DA044831, U10DA015815). This publication was made possible with support from the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1 RR024140 01 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Funding: OHSU and CareOregon funded this work. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: No authors have any conflicts of interest to disclose
References:
- 1.Ronan MV and Herzig SJ. Hospitalizations Related To Opioid Abuse/Dependence And Associated Serious Infections Increased Sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fanucchi L and Lofwall MR. Putting Parity into Practice - Integrating Opioid-Use Disorder Treatment into the Hospital Setting. N Engl J Med. 2016;375(9):811–813. [DOI] [PubMed] [Google Scholar]
- 3.Feigal J, Park B, Bramante C, Nordgaard C, Menk J and Song J. Homelessness and discharge delays from an urban safety net hospital. Public Health. 2014;128(11):1033–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Englander H, Weimer M, Solotaroff R, et al. Planning and Designing the Improving Addiction Care Team (IMPACT) for Hospitalized Adults with Substance Use Disorder. J Hosp Med. 2017;12(5):339–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slater MS, Komanapalli CB, Tripathy U, Ravichandran PS and Ungerleider RM. Treatment of endocarditis: a decade of experience. Ann Thorac Surg. 2007;83(6):2074–2079; discussion 2079–2080. [DOI] [PubMed] [Google Scholar]
- 6.Velez CM, Nicolaidis C, Korthuis PT and Englander H. “It’s been an Experience, a Life Learning Experience”: A Qualitative Study of Hospitalized Patients with Substance Use Disorders. J Gen Intern Med. 2017;32(3):296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jewell C, Weaver M, Sgroi C, Anderson K and Sayeed Z. Residential addiction treatment for injection drug users requiring intravenous antibiotics: a cost-reduction strategy. J Addict Med. 2013;7(4):271–276. [DOI] [PubMed] [Google Scholar]
- 8.Ivankova NV, Creswell JW and Stick SL. Using Mixed-Methods Sequential Explanatory Design: From Theory to Practice. Field Methods. 2006;18(1):3–20. [Google Scholar]
- 9.Goodson L and Vassar M. An overview of ethnography in healthcare and medical education research. J Educ Eval Health Prof. 2011;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wakeman SE and Rich JD. Barriers to Post-Acute Care for Patients on Opioid Agonist Therapy; An Example of Systematic Stigmatization of Addiction. J Gen Intern Med. 2017;32(1):17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merrill JO, Rhodes LA, Deyo RA, Marlatt GA and Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collier S and Gavriel M. Mobile phones in residential treatment: implications for practice. J Subst Abuse Treat. 2015;55:45–51. [DOI] [PubMed] [Google Scholar]
- 13.Beieler AM, Dellit TH, Chan JD, et al. Successful implementation of outpatient parenteral antimicrobial therapy at a medical respite facility for homeless patients. J Hosp Med. 2016;11(8):531–535. [DOI] [PubMed] [Google Scholar]
- 14.Zerger S, Doblin B and Thompson L. Medical respite care for homeless people: a growing national phenomenon. J Health Care Poor Underserved. 2009;20(1):36–41. [DOI] [PubMed] [Google Scholar]
- 15.Kathol RG, Butler M, McAlpine DD and Kane RL. Barriers to physical and mental condition integrated service delivery. Psychosom Med. 2010;72(6):511–518. [DOI] [PubMed] [Google Scholar]


