Abstract
This study examined attention-deficit/hyperactivity disorder (ADHD) comorbidity in military veterans with a high prevalence of posttraumatic stress disorder (PTSD) and evaluated the relationships between the 2 disorders and exposure to traumatic events. The sample included 222 male and female military veterans who were administered structured clinical interviews based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Results show that 54.5% met the criteria for current PTSD, 11.5% of whom also met the criteria for current adult ADHD. Level of trauma exposure and ADHD severity were significant predictors of current PTSD severity. Evaluation of the underlying structure of symptoms of PTSD and ADHD using confirmatory factor analysis yielded a best-fitting measurement model that comprised 4 PTSD factors and 3 ADHD factors. Standardized estimates of the correlations among PTSD and ADHD factors suggested that the largest proportion of shared variance underlying PTSD-ADHD comorbidity is related to problems with modulating arousal levels that are common to both disorders (ie, hyperarousal and hypoarousal).
1. Introduction
Posttraumatic stress disorder (PTSD) is an extreme psychobiological reaction to a traumatic event characterized by marked disturbances in cognitive, affective, behavioral, and physiological functioning. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM–IV–TR) [1] defines PTSD by 3 core symptom clusters: (1) intrusive reexperiencing of traumatic events, (2) avoidance of reminders of traumatic events and emotional numbing, and (3) general hyperarousal (ie, sleep problems, irritability/anger, difficulty concentrating, hypervigilance, and startle response). Epidemiologic and clinical studies have shown that an overwhelming majority of individuals diagnosed with PTSD meet the criteria for at least 1 additional Axis I disorder (ie, >80%), and a substantial percentage meet the criteria for 3 or more other psychiatric diagnoses [2–4]. Based on epidemiologic data from the National Comorbidity Survey [3], lifetime prevalence estimates of the most common Axis I disorders comorbid with PTSD included major depressive disorder (48%–49%), substance use disorders (27%–52%), and other anxiety disorders (specific phobias, social phobia, panic disorder, agoraphobia: 7%–31%).
There is also accumulating evidence suggesting that substantial comorbidity exists between PTSD and attentiondeficit/hyperactivity disorder (ADHD), with prevalence estimates ranging from 12% to 37% across the lifespan [5–8]. The DSM–IV–TR defines ADHD by 2 primary symptom dimensions, inattention and hyperactivity-impulsivity. Despite evidence of considerable comorbidity between PTSD and ADHD, relatively few studies have examined the nature of the overlap between these 2 disorders. Thus, the primary objectives of the current study were to examine ADHD comorbidity and trauma exposure in a sample of military veterans with a high prevalence of PTSD and to investigate the specific nature of associations among symptoms of these 2 disorders. An improved understanding of the covariation between symptoms of PTSD and ADHD represents an important step toward advancing the mental health treatment of individuals who present with both disorders and developing risk reduction and prevention programs for populations at risk for high trauma exposure.
1.1. The relationship between PTSD-ADHD comorbidity and exposure to psychological trauma
There is mixed evidence regarding the role of trauma exposure in PTSD–ADHD comorbidity. Adler and colleagues [5] suggested that ADHD may be one risk factor that increases vulnerability for developing PTSD after trauma exposure, based on their finding that patients with PTSD reported higher levels of childhood ADHD relative to patients with panic disorder. Some longitudinal studies have found that early exposure to trauma was significantly associated with a diagnosis of childhood ADHD [9] as well as a lifetime diagnosis of ADHD [10]. Similarly, a longitudinal study by Koenen and colleagues [11] found that individuals were 50% more likely to experience a psychological trauma if they had problems with hyperactivity, antisocial behavior, and difficult temperament during childhood as compared with individuals without such a history. Furthermore, there is evidence that children and adolescents diagnosed with ADHD are at greater risk for sustaining severe injuries [12–14] and that adolescent and adult drivers with ADHD are much more likely to have traffic violations and motor vehicle accidents relative to drivers without ADHD [15]. Additional studies have found elevated rates of physical and sexual abuse among children diagnosed with ADHD relative to a comparison group without ADHD [16–18] or children diagnosed with adjustment disorder [19]. In contrast, Wozniak and colleagues [20] reported no significant differences in the rate of trauma exposure or the development of PTSD between children diagnosed with ADHD and controls.
1.2. Potential mechanisms underlying PTSD-ADHD comorbidity
A number of hypotheses have been advanced regarding potential mechanisms underlying the high levels of comorbidity of PTSD with other psychiatric disorders [21], several of which are relevant for understanding the comorbidity between PTSD and ADHD. First, it has been proposed that the presence of certain psychiatric disorders may function as a risk factor for the development of PTSD, and these disorders may have been present before the trauma exposure[22]. There is evidence suggesting that the presence of early childhood risk factors (eg, pretrauma psychopathology including antisocial behavior, hyperactivity, and conduct disorder; family psychiatric history; and general childhood adversity) may play an important role in the development of PTSD [11,23]. Childhood ADHD may function as a risk factor for trauma exposure, such that children with ADHD may place themselves in riskier situations relative to their non-ADHD peers, thereby increasing their risk for certain types of trauma exposure, including physical injuries, physical and sexual abuse, neglect, and parental conflict [18,24]. In addition, children who are exposed to traumatic events might be more vulnerable to experiencing an exacerbation of ADHD symptoms. In support of this hypothesis, childhood physical and sexual abuse have been linked to increased externalizing problems including hyperactivity, impulsivity, aggression, anger, and physical attacks [25–27].
Another possible explanation for psychiatric comorbidity is the common-factor hypothesis, which postulates that the observed covariations between seemingly distinct disorders reflect manifestations of a common, unobserved latent psychopathology dimension [28–30]. One candidate for a common factor underlying PTSD–ADHD comorbidity is likely related to shared temperament or personality traits that confer the risk for psychopathology. The personality trait of neuroticism/negative emotionality (NEM) is a fairly nonspecific factor that contributes to a broad array of mental disorders, and it has been linked to disorders spanning the internalizing and externalizing spectrums [31–33]. Research examining the relationship between personality/temperament and ADHD has suggested that this diagnostic group is often characterized by high NEM, low constraint (CON), low conscientiousness or low effortful control, low reactive control, and low agreeableness [34–36]. Moreover, problems with CON, behavioral disinhibition, and executive control have been hypothesized to play a central etiologic role in ADHD [37–39]. Thus, problems in the domain of high NEM and behavioral disinhibition (ie, low CON) may underlie the expression of ADHD. Similarly, research on structural models of PTSD and its comorbidity by Miller and colleagues [40–42] suggests that high NEM is the primary personality risk factor involved in the development of PTSD and that externalizing forms of posttraumatic psychopathology reflect a tendency toward both high NEM and low CON. Based on the common-factor hypothesis, we expected that the strongest associations between PTSD and ADHD would be those thought to reflect generalized distress (ie, negative affectivity, NEM, or dysphoria) as opposed to traumaspecific symptoms.
1.3. Associations between specific symptom clusters of PTSD and ADHD
Another important step toward improving our understanding of the specific nature of PTSD–ADHD comorbidity is to examine the associations between symptoms of the 2 disorders. There are no known factor analytic studies that have examined the factor structure of PTSD and ADHD simultaneously. Only 2 studies have examined the associations between specific symptom clusters of PTSD and ADHD, and both studies focused on children. Ford and colleagues [19] found that children with ADHD showed significantly higher parent-reported reexperiencing and hyperarousal symptom scores than did children with adjustment disorder; however, the 2 groups did not differ in their hyperarousal symptom levels after accounting for the one overlapping symptom between ADHD and PTSD (ie, concentration problems). It is unclear if the higher reexperiencing symptoms in the ADHD group are a robust and reliable finding considering that ratings of PTSD symptoms were based on parent report only. Husain et al[43] reported stronger associations between the inattentive symptoms of ADHD and all PTSD symptom clusters relative to the hyperactive-impulsive symptoms in a sample of Sarajevan children who were exposed to the Bosnian War. The study of Husain et al also revealed the strongest association between ADHD inattention symptoms and PTSD hyperarousal symptoms, suggesting that this relationship may be driving the observed covariation between ADHD and PTSD.
1.4. The present study
Given the limited and inconsistent findings from previous investigations of the associations between PTSD and ADHD, combined with the lack of research using adult clinical samples, additional research is needed to help elucidate the patterns of covariation between specific symptoms of the 2 disorders. The current study was designed to address this gap in the literature by conducting a confirmatory factor analysis (CFA) of the structural associations among concurrent symptoms of PTSD and ADHD. Several characteristics of this data set make it particularly well suited for investigating PTSD–ADHD comorbidity. First, in contrast to most previous studies that included a limited number of patients diagnosed with PTSD, this study used a large clinical sample of veterans with a high prevalence of current and lifetime PTSD. Second, psychiatric diagnoses and symptom ratings were generated by trained clinicians using standardized, semistructured clinical interviews. Finally, this study also included a thorough assessment of exposure to a broad range of potentially traumatic events, allowing for examination of the rates of different types of trauma exposure among veterans diagnosed with PTSD and ADHD.
The first aim of the present study was to evaluate the relationships among PTSD, ADHD, and exposure to traumatic events. We hypothesized that ADHD would be associated with greater PTSD severity and/or higher levels of exposure to traumatic events, and we tested whether ADHD severity is a significant predictor of PTSD severity that is independent of trauma exposure. In addition, we expected to find elevated rates of specific types of trauma (ie, physical abuse, sexual abuse, motor vehicle accidents, and serious physical injuries) in veterans diagnosed with current ADHD as compared with those without ADHD. The second study aim was to evaluate the structural associations among symptoms of PTSD and ADHD using CFA. We advanced 2 hypotheses regarding the underlying association between symptoms of PTSD and ADHD. First, based on the common-factor hypothesis combined with evidence suggesting that high NEM is the major personality risk factor for both disorders, we expected that the ADHD inattention, hyperactivity, and impulsivity factors would show significant positive associations with the components of PTSD that are most closely aligned with generalized distress (ie, dysphoria/emotional numbing and hyperarousal factors). Second, given the assumption that the fundamental features of PTSD and ADHD are generally distinct [44], we expected that none of the ADHD factors would demonstrate significant associations with the cardinal features of PTSD that are most directly linked to trauma (ie, intrusive reexperiencing of traumatic events and effortful avoidance of reminders of traumatic events).
2. Methods
2.1. Participants
The sample consisted of 242 veterans who screened positive for current PTSD during a telephone administration of the PTSD Checklist–C (PCL–C) [45]. Recruitment, through posted flyers, clinical referrals, and a PTSD recruitment database, took place during a 34–month period between 2006 and 2009 from 2 campuses of the US Department of Veterans Affairs Boston Healthcare System. Of the 341 potential participants screened for the study, 242 met the eligibility criteria (as described in Section 2.2) and were enrolled. Twenty failed to complete the study protocol and were excluded from data analysis, leaving a final sample of 222. Of the 20 excluded participants, 12 were terminated by study staff because of problems conforming to interview requirements, and 8 withdrew from study participation.
Study participants were predominantly male (n = 201, or 90%) and self-reported their race and ethnicity as follows: 174 (79%) were white; 44 (20%), black or African American; 15 (7%), American Indian or Alaskan Native; 8 (4%), Hispanic or Latino; and 7 (3%), unknown racial origin (totals are >100% because participants could select more than 1 race). The mean (SD) age of participants was 50.8 years (10.7) (range, 23–68 years). Of the final sample of 222 veterans, 121 (54.5%) participants met the criteria for a current diagnosis of PTSD and 167 (75.2%) for a lifetime diagnosis, according to DSM-IV-TR criteria [1], as determined by the Clinician-Administered PTSD Scale (CAPS) (see Section 2.3.2). The index Criterion A event, as specified by the clinician conducting the assessment, was combatrelated in 101 (45%) of the cases, 20 participants (9%) endorsed physical assault, 17 (8%) endorsed childhood sexual trauma, 15 (7%) endorsed the sudden death of a friend or loved one, and 12 (5%) endorsed sexual trauma as an adult only being the index trauma. Several other types of trauma were endorsed (eg, natural disaster, serious accident, and being stalked), each occurring in less than 4% of the sample. Based on participants’ responses to the Traumatic Life Events Questionnaire (TLEQ; which assesses DSM-IV-TR PTSD Criteria A1 and A2]), the mean (SD) total number of traumatic events endorsed by participants in the sample was 22 (15), and the mean (SD) number of different types of traumatic events was 8 (4). This former figure reflects participants’ reports of multiple incidents of the same type of trauma. The overall prevalence of current adult ADHD was 11%, as determined by the Adult ADHD Clinical Diagnostic Scale version 1.2 (ACDS v1.2). Of the 23 veterans who met the full DSM-IV-TR criteria for current adult ADHD, 15 (65%) met the criteria for predominantly inattentive type, 4 (17.5%) met the criteria for predominantly hyperactive-impulsive type, and 4 (17.5%) met the criteria for combined type.
2.2. Procedure
This research was reviewed and approved by the institutional review board and research and development committees at the Veterans Affairs Boston Healthcare System and the Boston University School of Medicine Institutional Review Board. Participants provided written voluntary informed consent and were compensated for their time and effort. A telephone screen was administered to all interested veterans to determine study eligibility. Male and female veterans were eligible for participation if they were between the ages of 18 and 68 years and screened positive for current PTSD on the PCL–C [45] according to the standard DSM-IV-TR scoring rule (ie, endorsement of 1 B, 3 C, and 2 D criterion symptoms at a level of ≥3 on a 5–point severity scale). The study protocol involved administration of a series of self-report measures (demographic information, TLEQ) and structured diagnostic interviews, including the CAPS and the ACDS. The diagnostic interviews were administered by doctoral- and masters-level clinical psychologists and clinical psychology trainees. All interviews were digitally recorded on videotape, and approximately one third of them were randomly selected and independently coded by a second rater. Before study administration, all interviewers and secondary raters were required to attain a minimum of 90% diagnostic agreement for all major Axis I disorders according to 3 “gold standard” training videos. Throughout the course of the study, the interviews were reviewed in weekly reliability meetings to discuss factors related to diagnostic disagreement, to examine the source of dimensional (ie, symptom level) rating discrepancies, and to establish consensus ratings for any discrepant items. These meetings were moderated by the principal investigator or a doctoral-level clinical psychologist with expertise in administering DSM-IV–based structured clinical interviews. κ for current PTSD diagnosis was 0.61. The intraclass correlation coefficient for current PTSD symptom severity was 0.93. κ for current ADHD diagnosis was 0.58 when all DSM-IV-TR diagnostic criteria were applied (ie, Criteria A, B, C, and D; see Section 2.3.3). The intraclass correlation coefficient for current ADHD symptom severity was 0.97.
2.3. Measures
2.3.1. Traumatic Life Events Questionnaire
The TLEQ [46] is a self-report measure that assesses exposure to 22 types of potentially traumatic events (ie, to assess DSM-IV-TR PTSD Criterion A1). For each traumatic event that is endorsed, respondents are subsequently asked to provide (1) the number of times the event was experienced using a 7–point scale ranging from “never” to “more than 5 times” and (2) whether they experienced intense fear, helplessness, or horror in response to the event (ie, to assess DSM-IV-TR PTSD Criterion A2). The TLEQ has good test-retest reliability during a 2-week interval (mean κ, 0.63; mean percent agreement, 86%), excellent content and convergent validity with interview based measures of trauma exposure (mean percent agreement, 92%), and good predictive validity [46].
2.3.2. Clinician-Administered PTSD Scale
Participants were administered the CAPS [47], the gold-standard diagnostic interview for the assessment of PTSD, to determine current and lifetime PTSD diagnostic status and symptom severity according to the DSM-IV-TR criteria [1]. The CAPS is a 30–item structured interviewed designed to assess the 17 PTSD symptoms, its associated features, and functional impairment. PTSD diagnostic status was determined with a validated scoring rule [48]; namely, at least 1 reexperiencing symptom, 3 avoidance and numbing symptoms, and 2 hyperarousal symptoms each with a frequency score of 1 or greater and an intensity score of 2 or greater had to be endorsed to achieve the diagnosis. Severity scores were calculated by summing the frequency and intensity ratings (each ranges from 0 to 4) for each of the 17 items (range, 0–136) [48]. The CAPS has shown high internal consistency (α = 0.85–0.87) and good test-retest reliability (0.77–0.96) for the 3 symptom clusters [47], as well as strong convergent validity with the Structured Clinical Interview for DSM-IV PTSD module and the PTSD Symptom Scale-Interview version (0.83 and 0.73, respectively [49]).
2.3.3. Adult ADHD Clinical Diagnostic Scale version 1.2
Participants were administered the ACDS v1.2 [50] to assess current ADHD symptoms in adulthood. The ACDS v1.2 is a semistructured interview that assesses the 18 DSM-IV-TR symptoms of ADHD in both childhood and adulthood, using child- and adult-specific prompts. For this study, a diagnosis of adult ADHD was assigned for individuals who met all of the DSM-IV-TR criteria. Specifically, a DSM-IV-TR clinical diagnosis of ADHD requires an individual to have at least 6 symptoms of inattention and/or hyperactivity-impulsivity that have persisted for at least 6 months (Criterion A), with some symptoms of ADHD present before age 7 years (Criterion B), some impairment from ADHD symptoms in at least 2 areas of living during the past 6 months (Criterion C), and clinically significant impairment in at least 1 of these areas (Criterion D). Consistent with previous studies that have used the ACDS v1.2[7], the age criterion was operationalized to require that participants endorse the presence of at least 2 ADHD symptoms before age 7 years.
Minor modifications were made to the instrument to standardize the metric across a variety of other measures administered in the current study, including changes in the metric of the rating scale from “not present,” “mild,” “moderate,” or “severe” to a 0 to 2 format (ie, 0, absent; 1, subthreshold; and 2, clinically significant). Also, the period assessed in the present study was changed from adulthood (past 12 months) as specified in the ACDS v1.2 to current (past month) to align with the other study measures. Although ADHD symptom severity was assessed during the past month, a current diagnosis of ADHD also required evidence of impairing ADHD symptoms that have been present for at least 6 months per DSM-IV-TR criteria. An additional probe was added to assess childhood onset of symptoms (before age 7 years) for each ADHD symptom. Item level severity scores (0–2) were summed across the 9 inattentive and 9 hyperactive-impulsive symptoms to obtain a total severity score for each participant (range, 0–36). Although the psychometric properties of the ACDS v1.2 have not been formally described, the ACDS v1.2 has been used to assess adult ADHD in a large, nationally representative household survey in the United States (ie, the National Comorbidity Survey Replication) [7] as well as in multiple clinical studies of adult ADHD [51–53]. In the current study, the internal consistency of the 3 symptom dimensions of ADHD ranged from high to moderate for the inattention, hyperactive, and impulsive symptoms (α = 0.87, 0.74, and 0.68, respectively).
2.4. Statistical analyses
First, we conducted a hierarchical regression analysis to test the incremental effects of trauma exposure and severity of current ADHD symptoms on current PTSD severity. In step 1 of the model, the total number of traumatic events endorsed by participants was entered as a predictor of current PTSD severity. In step 2, current ADHD symptom severity was added as a second predictor of current PTSD severity. In addition, we conducted χ2 tests to examine whether the frequency of trauma exposure and types of traumatic events (ie, physical abuse, sexual abuse, and motor vehicle accidents/other serious accidents) endorsed by veterans differ by ADHD diagnostic status in this PTSD–selected sample.
Next, we investigated the associations between current symptoms of PTSD and ADHD using CFA. This approach offers advantages over bivariate correlations or multiple regression analyses in its ability to estimate the relationships among PTSD and ADHD variables after adjusting for measurement error and an error theory [28]. Thus, the factor correlations derived from CFA represent better estimates of the true population association between these constructs compared with simple bivariate correlation matrices. The CFA was conducted using the Mplus statistical modeling software (version 5.1) [54]. The 17 PTSD items on the CAPS and the 18 items on the ACDS were submitted to CFA to compare competing models reflecting alternative representations of PTSD and ADHD. Given the categorical nature of the ACDS ADHD items (ie, rated on a 3–point scale), the mean and variance-adjusted weighted least-square estimator was used. Participants with partial missing data were included in the analyses because the variance-adjusted weighted least-square estimator invokes a 4–step procedure to model such cases directly, building on direct maximum likelihood estimation. The largest percentage of missing data for a single item was 6.8%, which was the case for 2 hyperactivity symptoms (“on the go/acts like driven by a motor” and “talks excessively”). We first evaluated the latent structure of PTSD and ADHD separately, and then the best-fitting models for PTSD and ADHD were combined in a single measurement model. Specifically, we first tested the structure of the ACDS scale using CFA to compare 1-factor, 2-factor (ie, inattention and hyperactivity-impulsivity), and 3-factor models (ie, inattention, hyperactivity, and impulsivity) of ADHD. Next, we tested the structure of the CAPS by comparing the fit of the 2 leading 4–factor models of PTSD, namely, the “Numbing” model proposed by King et al[55] and the “Dysphoria” model proposed by Simms et al[56]. The Numbing model of King et al is defined by 4 factors: reexperiencing (DSM-IV-TR PTSD Criteria B1–B5), effortful avoidance (C1–C2), emotional numbing (C3–C7), and hyperarousal (D1–D5). The Dysphoria model of Simms et al defines the reexperiencing and effortful avoidance factors in the same manner as the Numbing model; however, it differs in that 3 of the hyperarousal items are moved onto the emotional numbing factor, yielding a dysphoria factor (C3–C7, D1–D3) and a revised hyperarousal factor (D4–D5).
Model fit was evaluated using fit statistics from several classes of fit indices: absolute (χ2), parsimony (root mean square error of approximation [RMSEA]), and comparative fit (Tucker–Lewis index [TLI] and comparative fit index [CFI]). The cutoff guidelines recommended by Hu and Bentler [57] and Kline [58] were used to determine the acceptability of each model. Specifically, RMSEA values less than 0.06 were considered indicators of good model fit, and CFI and TLI values of 0.90 or greater and 0.95 or greater were considered as indicators of adequate and good model fit, respectively. Finally, to examine the statistical significance between the magnitude of pairs of correlations within the best-fitting model (eg, the difference in the magnitude of the association between inattention and emotional numbing vs hyperarousal), we computed t statistics for comparing the magnitude of dependent correlations (ie, within a single sample) as described by Cohen and Cohen [59].
3. Results
3.1. Relationships between PTSD, ADHD, and exposure to traumatic events
We hypothesized that ADHD may be associated with greater exposure to traumatic events and conducted a hierarchical regression analysis to test the incremental effects of trauma exposure and current ADHD severity on current PTSD severity. As shown in Table 1, the results of the regression analysis revealed a significant main effect of trauma exposure that accounted for 5% of the variance in current PTSD severity. Current ADHD severity was also a significant predictor of PTSD, accounting for an additional 7% of the variance in current PTSD severity above and beyond trauma exposure. The overall regression model was significant (F2, 215 = 15.05, P < .001), with higher levels of trauma exposure and ADHD symptom severity positively associated with greater PTSD symptom severity. Collinearity statistics fell well within the acceptable range for both predictors (tolerance, 1.00; variable inflation factor, 1.00), with no evidence of significant multicollinearity in the model.1
Table 1.
Exposure to traumatic events and current ADHD symptom severity predict current PTSD symptom severity
| Independent variable | B | SE (B) | β | t | P | R2 | ΔR2 |
|---|---|---|---|---|---|---|---|
| Step 1 | |||||||
| No. of traumatic events | 0.40 | 0.12 | 0.23 | 3.40 | .001 | 0.05 | - |
| Step 2 | |||||||
| No. of traumatic events | 0.40 | 0.11 | 0.23 | 3.54 | <.001 | ||
| Severity of ADHD sx | 1.67 | 0.40 | 0.27 | 4.20 | <.001 | 0.12 | 0.07 |
sx indicates symptoms.
Next, we examined possible diagnostic differences in the frequency of trauma exposure across several types of traumatic events endorsed by veterans (ie, combat, sexual abuse, physical abuse, natural disaster, and motor vehicle accident/other serious accident). χ2 Tests revealed significant differences between veterans diagnosed with current ADHD relative to those never diagnosed with ADHD in the overall rate of sexual abuse (χ21 [n = 204] = 4.17; P = .04, 2-tailed), such that individuals with ADHD endorsed higher rates of sexual abuse (ie, occurring during childhood or adulthood) than those without the disorder (73.9% vs51.4%). No significant differences were found for the other types of trauma with respect to ADHD diagnostic status.
3.2. Confirmatory factor analysis of PTSD and ADHD
The top portion of Table 2 displays the results of the χ2 difference tests and fit indices evaluating the 3 competing models of the structure of ADHD using CFA. The results suggested that the 3-factor model of ADHD provided the best representation of the ACDS factor structure. More specifically, the 2–factor model yielded significantly poorer fit relative to the 3–factor model, and the 1–factor model was associated with degraded fit relative to the 2–factor model. As shown in the second part of Table 2, the Numbing and Dysphoria models of PTSD yielded fit statistics that were roughly equivalent; however, only the fit indices for the Numbing model fell within the range of adequate model fit. Thus, the Numbing model was determined to best capture the CAPS factor structure in this sample. The best-fitting models for PTSD and ADHD were subsequently combined in a single measurement model that included 4 intercorrelated factors of reexperiencing, effortful avoidance, emotional numbing, and hyperarousal dimensions of PTSD and 3 intercorrelated factors of inattention, hyperactivity, and impulsivity dimensions of ADHD. The fit statistics associated with this model fell just short of the recommended cutoff guidelines for acceptable fit (see Table 2), which may have been due to unrepresented associations between specific PTSD and ADHD symptoms. As often occurs in large samples, the χ2 tests were significant for all models evaluated, which can reflect small differences between the model and the observed associations among the data.
Table 2.
Goodness-of-fit indices for CFA of ADHD and PTSD
| Model | df | χ2 | P | RMSEA | TLI | CFI | Models compared | χ2 Difference test |
|---|---|---|---|---|---|---|---|---|
| a. 1-factor ADHD | 49 | 256.89 | <.001 | 0.14 | 0.85 | 0.78 | - | - |
| b. 2-factor ADHD | 52 | 125.19 | <.001 | 0.08 | 0.95 | 0.92 | b vs a | 47.57 (P <.001) |
| c. 3-factor ADHD | 53 | 109.55 | <.001 | 0.07 | 0.96 | 0.94 | c vs b | 17.02 (P <.001) |
| d. 4-factor PTSD (Numbing) | 113 | 179.32 | <.001 | 0.05 | 0.92 | 0.93 | - | - |
| e. 4-factor PTSD (Dysphoria) | 113 | 204.34 | <.001 | 0.06 | 0.88 | 0.90 | - | - |
| f. Best-fitting ADHD + PTSD | 100 | 183.63 | <.001 | 0.06 | 0.92 | 0.84 | - | - |
| g. D3 cross-loading on INAT | 101 | 163.45 | <.001 | 0.05 | 0.94 | 0.88 | - | - |
| h. Hypothesized paths only | 76 | 124.00 | <.001 | 0.05 | 0.94 | 0.91 | h vs g | 5.77 (P = .123) |
Numbing indicates the model of PTSD by King et al; Dysphoria, the model of PTSD by Simms et al; D3, difficulty concentrating; INAT, ADHD inattention factor.
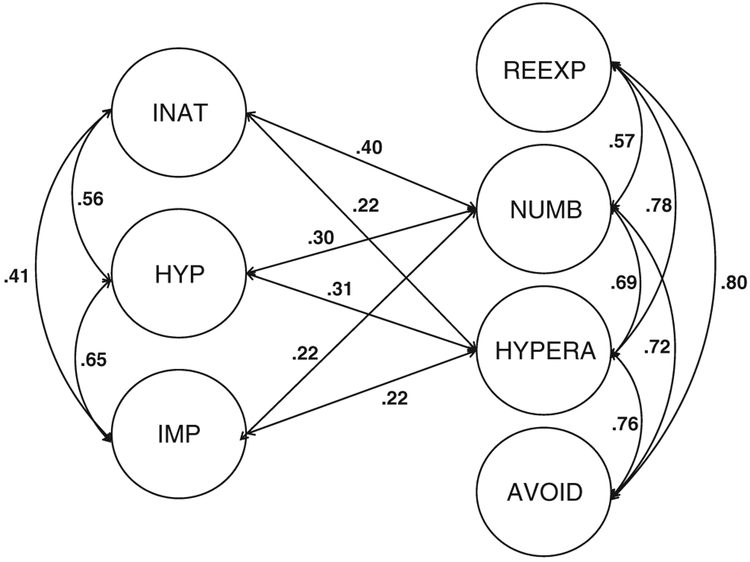
Next, to account for the item overlap between the DSM-IV-TR criteria for PTSD and ADHD (ie, difficulty concentrating/sustaining attention), PTSD criterion D3 was allowed to cross-load on the ADHD inattention factor. This resulted in only slight improvement in model fit, such that the values for RMSEA and TLI shifted into the acceptable range, but the value for CFI remained slightly below the cutoff for acceptable fit. The association between the ADHD inattention factor and the PTSD hyperarousal factor was reduced from 0.39 to 0.21 by accounting for the shared variance on this overlapping item (ie, allowing D3 to cross-load on the inattention factor). This fully saturated structural model was then used as a base model for comparison with a nested model that only included the associations between the factors of PTSD and ADHD that were hypothesized to be significant (ie, the covariances were fixed to zero between each of the ADHD factors and the PTSD reexperiencing and avoidance factors). This hypothesized model demonstrated slightly better fit to the data relative to the parent model, as indicated by a higher value for CFI, which shifted into the range of acceptable fit. Furthermore, results of the χ2 difference test showed that fit was not significantly damaged by removing the paths that were not hypothesized (χ2diff(3) = 5.77, P =.123), suggesting that the hypothesized model is more parsimonious than the saturated model but equivalent in model fit. All of the fit indices of the final model fell within the range of adequate model fit. Further efforts to simplify the model degraded the fit, leading us to accept the final model comprised of paths between 3 ADHD factors (inattention, hyperactivity, and impulsivity) and 2 PTSD factors (emotional numbing and hyperarousal), as depicted in Fig. 1.
Fig. 1.
Final model of CFA of ADHD and PTSD, which only includes hypothesized factor covariances. Standardized estimates of the correlations among latent factors are reported. INAT indicates inattention factor; HYP, hyperactivity factor; IMP, impulsivity factor; REEXP, reexperiencing factor; AVOID, effortful avoidance factor; NUMB, emotional numbing factor; HYPERA, hyperarousal factor. All correlations were significant at P < .05.
The following standardized estimates of the correlations among PTSD and ADHD factors are based on the saturated model that allows D3 to cross-load on the inattention factor. Consistent with our hypotheses, the ADHD inattention factor showed significant association with PTSD emotional numbing and hyperarousal factors (r’s = 0.40 and 0.21, respectively). The magnitude of the association between the inattention and emotional numbing factors was significantly greater than the corresponding association with the hyperarousal factor (t218 = 3.72, P < .001). Also in line with our predictions, the inattention factor was not significantly related to the reexperiencing factor (r = 0.10). One unexpected finding was that the inattention factor was significantly related to avoidance (r = 0.19), and the magnitude of this association was significantly stronger than its association with reexperiencing (t218 = 2.15, P =.03). As expected, the hyperactivity factor was significantly correlated with emotional numbing and hyperarousal factors (r’s = 0.30 and 0.33, respectively), but not with reexperiencing or avoidance factors (r’s = 0.16 and 0.11, respectively). Emotional numbing and hyperarousal factors evidenced an equivalent strength of association with hyperactivity (t218 =0.57, P = .60). Results revealed a very similar pattern of associations for the impulsivity factor, in that it was significantly related to both emotional numbing and hyperarousal (r’s = 0.22 and 0.25, respectively), but not with reexperiencing or avoidance (r’s = 0.06 and 0.10, respectively). Similarly, the magnitude of the associations with impulsivity did not differ significantly for emotional numbing and hyperarousal (t218 = 0.56, P = .60).
4. Discussion
This study examined ADHD comorbidity in a clinical sample of military veterans who screened positive for PTSD and investigated associations among PTSD, ADHD, and exposure to traumatic events. Of those participants who met the DSM-IV-TR criteria for PTSD, a considerable proportion(11.5%) also met the DSM-IV-TR criteria for current ADHD. The conditional prevalence estimate of current ADHD in those individuals diagnosed with current PTSD was more in line with the prevalence rate reported in a large epidemiologic sample (ie, 13.4%) [7] than that reported in a prior clinical sample of military veterans (ie, 28%) [5], although both of these studies used clinician-assessed interview methods to determine ADHD diagnosis.
As hypothesized, the rate of sexual abuse was significantly higher among veterans diagnosed with ADHD relative to those without ADHD. This finding adds to a growing body of evidence suggesting that having an ADHD diagnosis is associated with a higher prevalence rate of sexual abuse. Although a causal relationship has not been established between ADHD and sexual abuse, studies have documented a higher prevalence of ADHD among samples of sexually abused children [8,60,61]. Similarly, higher rates of childhood sexual abuse have been reported among children diagnosed with oppositional defiant disorder and ADHD [19] as well as adults with ADHD [62]. Prospective studies are needed to elucidate the nature of the association between ADHD and sexual abuse. Possible mechanisms underlying the specific relationship between ADHD and sexual abuse might include the following: (1) self-regulatory problems associated with ADHD (eg, distractibility and impulsivity) may place an individual at greater risk for sexual maltreatment; (2) sexual abuse and subsequent PTSD symptoms may exacerbate existing ADHD-related deficits such as inattention, disorganization, impulse regulation, or hyperactivity; or (3) environmental risk factors (eg, poverty, family conflict, and parental psychopathology) associated with ADHD and conduct disorders may increase the risk for sexual maltreatment [19].
In contrast to previous studies [14–15,18], we did not detect higher rates of other types of traumatic events such as physical abuse, motor vehicle accidents, or serious physical injuries among veterans with ADHD. Considering the relatively small number of veterans diagnosed with ADHD in this sample (n = 23), the failure to replicate this prior work is likely attributable to a lack of statistical power to detect differences in the rates of trauma between ADHD and non-ADHD groups. We also found that both overall level of trauma exposure and ADHD severity exerted significant, independent effects on PTSD severity. More specifically, current ADHD severity accounted for additional variance in current PTSD severity above and beyond trauma exposure. Given that trauma exposure is presumed to be a necessary causal agent of PTSD symptoms, it is notable that ADHD symptom severity explained more variance in PTSD severity than level of trauma exposure. The significant association between ADHD and PTSD symptom severity is likely an indirect effect that may reflect the expression of preexisting vulnerabilities that the 2 disorders share in common, such as negative emotionality.
4.1. The factor structure of PTSD and ADHD
The CFA of the 17 PTSD items on the CAPS and the 18 items on the ACDS revealed a best-fitting model reflecting3 ADHD factors (inattention, hyperactivity, impulsivity) and 4 PTSD factors (reexperiencing, avoidance, emotional numbing, hyperarousal). Our finding that ADHD was best represented by a 3-factor model replicates several prior CFA studies that factor analyzed DSM-IV-TR–based items of ADHD in college student populations [63–65]. To our knowledge, only one other study by Kessler and colleagues[66] has conducted a factor analysis of the ACDS (ie, a principal axis factor analysis). Given that the study of Kessler et al included 14 non-DSM items in their factor analysis related to difficulties with planning, organization, inattention, and mood lability (ie, executive function [EF]deficits), our results cannot be directly compared. None-theless, it is interesting to note that the factor analysis of Kessler et al revealed a 3–factor solution consisting of an inattention-hyperactivity factor, an impulsivity factor, and an EF factor. The fact that we found the Numbing model of PTSD [55] to be slightly better fitting than the Dysphoria model [56] might be related to using an intervieweradministered instrument (the CAPS) to measure PTSD in this sample rather than a self-report instrument as suggested by Palmieri et al [67]; however, results of a recent meta-analysis by Yufik and Simms [68] failed to find support for the hypothesis that PTSD symptom structure varies as a function of PTSD measure or trauma type. Our final measurement model of PTSD and ADHD (a) allowed PTSD Criterion D3 (ie, difficulty concentrating) to cross-load on the ADHD inattention factor to account for item overlap and (b) only included the associations between the factors of PTSD and ADHD that were hypothesized to be significant (ie, paths between each of the ADHD factors and emotional numbing and hyperarousal). The fact that the association between the ADHD inattention factor and the PTSD hyperarousal factor was significantly attenuated (from r = 0.39 to 0.21) when PTSD Criterion D3 was allowed to cross-load on the ADHD inattention factor suggests that the item overlap accounted for a significant amount of shared variance between these 2 factors.
Examination of the patterns of covariation among current PTSD and ADHD symptom clusters showed evidence of strong associations between the inattention and emotional numbing factors, hyperactivity and hyperarousal factors, and hyperactivity and emotional numbing factors. This suggests that the largest proportion of shared variance underlying the co-occurrence of PTSD and ADHD is related to problems with modulating arousal levels that are common to both disorders (ie, hyperarousal and hyperactivity on one end of the continuum, as well as hypoarousal and emotional numbing on the other end of the continuum). This finding is consistent with previous research. For example, some theories of ADHD postulate that difficulty in regulating arousal or activation levels is a core deficit of the disorder [69–70], and recent neuroimaging studies by Frewen and Lanius [71] and Lanius et al [72] have suggested that a “deficiency in the ability to adaptively regulate levels of affective arousal and distress in the context of stressors” may be central to PTSD. Lanius et al further proposed that reexperiencing and hyperarousal reactivity can be viewed as a form of deficient neuroregulatory control over emotional arousal (ie, emotional undermodulation), whereas states of dissociation, anhedonia, and emotional numbing can be conceptualized as forms of enhanced neuroregulatory suppression of emotional arousal (ie, emotional overmodulation).
As hypothesized, symptoms of inattention, hyperactivity, and impulsivity showed weak, nonsignificant associations with reexperiencing symptoms. In contrast, the finding that the ADHD inattention factor was moderately associated with avoidance symptoms was unexpected, particularly given the lack of association between inattention and reexperiencing symptoms. One possible explanation for this result is that ADHD inattentiveness and PTSD avoidance symptoms might reflect similar disturbances in cognitive control mechanisms, which could manifest as problems with distractibility and disorganization in ADHD [38] and difficulty suppressing emotionally distracting and intrusive thoughts in PTSD [73].
4.2. Limitations
These findings should be considered within the context of several limitations of the current study. First, given that the study used a clinical sample composed of veterans predominantly with military-related PTSD, caution should be used in generalizing the current findings to survivors of other types of trauma or to civilian samples. Although roughly 68% of the sample endorsed combat-related trauma, most participants also endorsed multiple types of trauma. The fact that this sample was selected for PTSD and did not include a comparison group of non–trauma-exposed individuals further limits the generalizability of the study findings to epidemiologic samples. Specifically, the eligibility criteria for the study required that participants endorse at least 1 Criterion A traumatic event and screen positive for PTSD on the PCL–C, as administered via telephone. At the same time, we believe that this selected group of veterans characterized by high rates of PTSD represents a good sample for investigating the nature of the overlap between PTSD and ADHD because it provides sufficient interindividual variability in severity of the constructs of interest. Second, assessment of the presence of ADHD symptoms before the age of 7 years required exclusive reliance on participants’ retrospective report of symptoms and may be subject to recall bias [74]. This problem is not unique to this study, however, given that the clinical diagnosis of ADHD in adults is typically based on retrospective reports of childhood symptoms. Importantly, there is empirical support suggesting that self-report is a reliable way of identifying adults with ADHD [75] and that well-operationalized, adverse childhood experiences are recalled with sufficient accuracy to provide useful information in retrospective studies [76]. Third, given the relatively small number of participants diagnosed with ADHD in this sample, caution should be used when interpreting findings from the analyses comparing ADHD and non-ADHD groups on the frequency of different types of trauma exposure. Fourth, to our knowledge, this is the first CFA study of PTSD and ADHD comorbidity; thus, additional studies are needed to test whether the same factor structure can be replicated in independent samples. Fifth, given the cross-sectional nature of the current sample, the results cannot bear on our understanding of the etiologic mechanisms involved in PTSD–ADHD comorbidity. Nevertheless, the current results do help to shed light on the degree and nature of associations among the symptoms of the 2 disorders and illuminate future directions for research in this understudied area.
Finally, mild traumatic brain injury (TBI) may be a potentially important confounding variable to consider when investigating PTSD–ADHD comorbidity in future research. Although data on TBI were not collected as part of this study, it is noteworthy that mild TBI and PTSD can be associated with mild neuropsychological impairment (eg, attention, learning and memory, and executive functioning) [77], and impairments in these same neuropsychological domains also represent core deficits in ADHD [37]. TBI has been of particular concern for military personnel deployed to contemporary war zones, considering the high rates of head injuries among Operation Enduring Freedom and Operation Iraqi Freedom veterans. Given that Operation Enduring Freedom/Operation Iraqi Freedom veterans comprised only 14% of the current sample, it is unlikely that TBI represents a major confounding variable in this study.
4.3. Clinical implications and directions for future research
More research is needed to determine how the cooccurrence of PTSD and ADHD may interact and influence the symptom presentation and course of either disorder. These results suggest that it is important to assess trauma history as part of a comprehensive ADHD assessment and to screen for ADHD when assessing for PTSD. Specifically, high rates of PTSD–ADHD comorbidity in clinical populations suggest that careful evaluation of both disorders is important in the event that one of the disorders can be ruled out to reduce the risk for improper psychiatric medication prescription or other inappropriate treatment interventions. Ford and Connor [44] offered several helpful guidelines for differentiating between primary symptoms of PTSD vs ADHD, including careful assessment of the chronologic sequence and timing of traumatic experiences in relation to the symptom course. Increased awareness by clinicians with respect to recognizing the potential for true cases of comorbid PTSD and ADHD may help to reduce the chances that symptoms of either disorder may become exacerbated if left untreated. Our ability to effectively treat these disorders is further complicated by the fact that mood disorders, substance use disorders, and anxiety disorders frequently cooccur in adults with PTSD [3] as well as adults with ADHD[7]. Although it was beyond the scope of this study, it will be important for future CFA studies to examine how the presence of these other commonly co-occurring conditions may affect the extent of covariation among symptoms of PTSD and ADHD.
The CFA results of this study suggest that the intersection of PTSD and ADHD cannot be adequately understood through the examination of overlapping DSM-IV-TR symptom criteria alone. Rather, it seems important for future studies to consider a broader constellation of overlapping symptoms between the 2 disorders (ie, beyond DSM-IV-TR criteria) that may serve to complicate the process of differential diagnosis and potentially lead to misdiagnosis, including difficulty in sustaining attention, difficulty listening, failure to complete duties, difficulty in organization, forgetfulness, avoidance of mental tasks, memory dysfunctions, irritability, anger, restlessness, and sleeplessness. One promising direction for future investigation is to examine relevant cognitive and emotional processes or areas of dysfunction that are shared by the 2 disorders to help elucidate the clinical impairment associated with having these disorders independently vs concurrently. For example, studying problems of emotion regulation (ER)2 and EF3 that are known to be involved in both PTSD and ADHD may be a fruitful line of research for identifying domains of impairment shared by the 2 disorders as well as those that are not adequately captured by the current DSM-IV-TR diagnostic criteria. Moreover, increased recognition that deficits in ER and EF underlie both PTSD and ADHD also has clear treatment implications. The development of an integrated treatment approach for treating comorbid PTSD and ADHD seems warranted, with the goal of simultaneously targeting key areas of impairment across the 2 disorders. Relevant components from existing treatment protocols might include dialectical behavior therapy skills training [80] to address problems with ER, as well as cognitive training techniques [81–82] for reducing attentional bias toward threat in PTSD and improving attention and disinhibition problems in ADHD.
4.4. Conclusions
The current findings highlight that a subset of veterans with PTSD experience concurrent problems with ADHD, yet little is known about possible causal and noncausal factors contributing to this co-occurrence. An evaluation of the underlying structure of symptoms of PTSD and ADHD suggests that the largest proportion of shared variance underlying this co-occurrence is related to problems with modulating arousal levels that are common to both disorders. An improved understanding of shared cognitive, emotional, and neurobiological mechanisms underlying the comorbidity of PTSD and ADHD could potentially have a profound impact on the diagnosis and treatment of these debilitating disorders.
Acknowledgment
Funding for this study was provided by a VA Merit Review Award to Mark W. Miller. Kelly M. Harrington was supported by National Institute of MentalHealth Training Grant T32MH019836.
Footnotes
A post hoc test was conducted to rule out the hypothesis that the association between symptoms of PTSD and ADHD merely may be reflecting the presence of depressive symptoms. Specifically, current depression severity was entered in step 3 of the hierarchical regression analysis. Results revealed that current ADHD severity remained a significant predictor of current PTSD severity even when controlling for current depression symptoms (P = .02).
According to Thompson [78], ER is defined as “the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, especially their intensive and temporal features, to accomplish one’s goals.”
According to Willcutt et al [79], EFs are defined as qneurocognitive processes that maintain an appropriate problem-solving set to attain a later goal," including cognitive control, problem solving, planning and executing tasks, organization, cognitive flexibility, self-monitoring, and behavioral inhibition.
References
- [1].American Psychiatric Association. Diagnostic and Statistical Manual Of Mental Disorders Text Revision (DSM-IV-TR). 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- [2].Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol 2001;110: 585–99. [DOI] [PubMed] [Google Scholar]
- [3].Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048–60. [DOI] [PubMed] [Google Scholar]
- [4].Orsillo SM, Weathers FW, Litz BT, Steinberg HR, Huska J, Keane TM. Current and lifetime psychiatric disorders among veterans with war-zone related posttraumatic stress disorder. J Nerv Ment Dis 1996;184:307–13. [DOI] [PubMed] [Google Scholar]
- [5].Adler LA, Kunz M, Chua HC, Rotrosen J, Resnick SG. Attention-deficit/hyperactivity disorder in adult patients with posttraumatic stress disorder (PTSD): is ADHD a vulnerability factor? J Atten Disord 2004;8:11–6. [DOI] [PubMed] [Google Scholar]
- [6].Famularo R, Fenton R, Kinscherff R, Augustyn M. Psychiatric comorbidity in childhood posttraumatic stress disorder. Child Abuse Negl 1996;20:953–61. [DOI] [PubMed] [Google Scholar]
- [7].Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163:716–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].McLeer S, Callaghan M, Henry D, Wallen J. Psychiatric disorders in sexually abused children. J Am Acad Child Psy 1994;33:313–9. [DOI] [PubMed] [Google Scholar]
- [9].Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Faraone SV, et al. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the National Comorbidity Survey Replication. Biol Psychiatry 2005;57: 1442–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Copeland WE, Keeler G, Angold A, Costello J. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry 2007;64: 577–84. [DOI] [PubMed] [Google Scholar]
- [11].Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder: results form a longitudinal birth cohort. Psychol Med 2007;37:181–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Brehaut JC, Miller A, Raina P, McGrail KM. Childhood behavior disorders and injuries among children and youth: a population-based study. Pediatrics 2003;111:262–9. [DOI] [PubMed] [Google Scholar]
- [13].DiScala C, Lescohier I, Barthel M, Li G. Injuries to children with attention deficit hyperactivity disorder. Pediatrics 1998;102:1415–21. [DOI] [PubMed] [Google Scholar]
- [14].Lam LT. Attention deficit disorder and hospitalization due to injury among older adolescents in New South Wales, Australia. J Atten Disord 2002;6:77–82. [DOI] [PubMed] [Google Scholar]
- [15].Barkley RA. Driving impairments in teens and adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am 2004;27: 233–60. [DOI] [PubMed] [Google Scholar]
- [16].Briscoe-Smith AM, Hinshaw SP. Linkages between child abuse and attention-deficit/hyperactivity disorder in girls: behavioral and social correlates. Child Abuse Negl 2006;30:1239–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lam LT. Attention deficit disorder and hospitalization owing to intra-and interpersonal violence among children and young adolescents. J Adolesc Health 2005;36:19–24. [DOI] [PubMed] [Google Scholar]
- [18].Ouyang L, Fang X, Mercy J, Perou R, Grosse SD. Attention-deficit/hyperactivity disorder symptoms and child maltreatment: a population-based study. J Pediatr 2008;153:851–6. [DOI] [PubMed] [Google Scholar]
- [19].Ford JD, Racusin R, Ellis CG, Daviss WB, Reiser J, Fleischer A, et al. Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreat 2000;5:205–17. [DOI] [PubMed] [Google Scholar]
- [20].Wozniak J, Crawford MH, Biederman J, Faraone SV, Spencer TJ, Taylor A, et al. Antecedents and complications of trauma in boys with ADHD: findings from a longitudinal study. J Am Acad Child Psy 1999;38:48–55. [DOI] [PubMed] [Google Scholar]
- [21].Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2000;61(Suppl 7):22–32. [PubMed] [Google Scholar]
- [22].Keane TM, Kaloupek DG. Comorbid psychiatric disorders in PTSD: implications for research. Ann NY Acad Sci 1997;821:24–34. [DOI] [PubMed] [Google Scholar]
- [23].Koenen KC, Fu QJ, Lyons MJ, Toomey R, Goldberg J, Eisen SA, et al. Juvenile conduct disorder as a risk factor for trauma exposure and posttraumatic stress disorder. J Trauma Stress 2005;18:23–32. [DOI] [PubMed] [Google Scholar]
- [24].Knutson JF. Psychological characteristics of maltreated children: putative risk factors and consequences. Annu Rev Psychol 1995;46: 401–31. [DOI] [PubMed] [Google Scholar]
- [25].Dubowitz H, Black M, Harrington D, Verschoore A. A follow-up study of behavior problems associated with child sexual abuse. Child Abuse Negl 1993;17:743–54. [DOI] [PubMed] [Google Scholar]
- [26].Margolin G, Gordis E. The effects of family and community violence on children. Annu Rev Psychol 2000;51:445–79. [DOI] [PubMed] [Google Scholar]
- [27].Osofsky J Prevalence of children’s exposure to domestic violence and child maltreatment: Implications for prevention and intervention. Clin Child Fam Psychol Rev 2003;6:161–70. [DOI] [PubMed] [Google Scholar]
- [28].Brown TA. Confirmatory factor analysis for applied research. New York: The Guilford Press; 2006. [Google Scholar]
- [29].Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry 1999;56:921–6. [DOI] [PubMed] [Google Scholar]
- [30].Thurstone LL. Multiple-factor analysis. Chicago: University of Chicago Press; 1947. [Google Scholar]
- [31].Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence In: Lahey BB, Moffitt TE, & Caspi A, editors. Causes of conduct and juvenile delinquency. New York: The Guilford Press; 2003. p. 76–117. [Google Scholar]
- [32].Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: reflections and directions. J Abnorm Child Psychol 2003;31:285–91. [DOI] [PubMed] [Google Scholar]
- [33].Rhee SH, Cosgrove VE, Schmitz S, Haberstick BC, Corley RC, Hewitt JK. Early childhood temperament and the covariation between internalizing and externalizing behavior in school-aged children. Twin Res Hum Genet 2007;10:33–44. [DOI] [PubMed] [Google Scholar]
- [34].Martel MM, Nigg JT. Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. J Child Psychol Psychiatry 2006;47:1175–83. [DOI] [PubMed] [Google Scholar]
- [35].Nigg JT, John OP, Blaskey LG, Huang-Pollock CL, Willcutt EG, Hinshaw SP, et al. Big five dimensions and ADHD symptoms: links between personality traits and clinical symptoms. J Pers Soc Psychol 2002;83:451–69. [DOI] [PubMed] [Google Scholar]
- [36].Volkow ND, Wang GJ, Newcorn JH, Kollins SH, Wigal TL, Telang F, et al. Motivation deficit in ADHD is associated with dysfunction of the dopamine reward pathway. Mol Psychiatry 2010, doi: 10.1038/mp.2010.97 Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997;121:65–94. [DOI] [PubMed] [Google Scholar]
- [38].Martel MM, Nigg JT, von Eye A. How do trait dimensions map onto ADHD symptom domains? J Abnorm Child Psych 2009;37:337–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Nigg J Is ADHD a disinhibitory disorder? Psychol Bull 2001;127: 571–98. [DOI] [PubMed] [Google Scholar]
- [40].Miller MW. Personality and the etiology and expression of PTSD: a three-factor model perspective. Clin Psychol-Sci Pr 2003;10:373–93. [Google Scholar]
- [41].Miller MW, Kaloupek DG, Dillon AL, Keane TM. Externalizing and internalizing subtypes of combat-related PTSD: a replication and extension using the PSY-5 scales. J Abnorm Psychol 2004;113:636–45. [DOI] [PubMed] [Google Scholar]
- [42].Miller MW, Resick PA. Internalizing and externalizing subtypes in female sexual assault survivors: implications for the understanding of complex PTSD. Behav Ther 2007;38:58–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Husain SA, Allwood MA, Bell DJ. The relationship between PTSD symptoms and attention problems in children exposed to the Bosnian war. J Emot Behav Disord 2008;16:52–62. [Google Scholar]
- [44].Ford JD, Connor DF. ADHD and posttraumatic stress disorder. Curr Atten Disord Rep 2009;1:60–6. [Google Scholar]
- [45].Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; 1993. San Antonio, TX. [Google Scholar]
- [46].Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess 2000;12:210–24. [DOI] [PubMed] [Google Scholar]
- [47].Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. J Trauma Stress 1995;8:75–90. [DOI] [PubMed] [Google Scholar]
- [48].Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychol Assess 1999;11:124–33. [Google Scholar]
- [49].Foa EB, Tolin DF. Comparison of the PTSD Symptom Scale-Interview version and the Clinician-Administered PTSD Scale. J Trauma Stress 2000;13:181–91. [DOI] [PubMed] [Google Scholar]
- [50].Adler L, Cohen J. Diagnosis and evaluation of adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am 2004;27:187–201. [DOI] [PubMed] [Google Scholar]
- [51].Spencer T, Biederman J, Wilens T, Faraone S, Prince J, Gerard K, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58: 775–82. [DOI] [PubMed] [Google Scholar]
- [52].Spencer T, Biederman J, Wilens T, Prince J, Hatch M, Jones J, et al. Effectiveness and tolerability of tomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155:693–5. [DOI] [PubMed] [Google Scholar]
- [53].Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434–43. [DOI] [PubMed] [Google Scholar]
- [54].Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Los Angeles, CA: Muthén & Muthén, 1998–2009. [Google Scholar]
- [55].King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: evidence for the dimensionality of posttraumatic stress disorder. Psychol Assess 1998; 10:90–6. [Google Scholar]
- [56].Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. J Abnorm Psychol 2002;111:637–47. [DOI] [PubMed] [Google Scholar]
- [57].Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1–55. [Google Scholar]
- [58].Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- [59].Cohen J, Cohen P. Bivariate correlation and regression Applied multiple regression/correlation analysis for the behavioral sciences, 2nd ed. Hillsdale (N.J.): Erlbaum; 1983. p. 25–78. [Google Scholar]
- [60].Merry SN, Andrews LK. Psychiatric status of sexually abused children 12 months after disclosure of abuse. J Am Acad Child Psychiatry 1994;33:939–44. [DOI] [PubMed] [Google Scholar]
- [61].Weinstein D, Staffelbach D, Biaggio M. Attention-deficit hyperactivity disorder and posttraumatic stress disorder: differential diagnosis in childhood sexual abuse. Clin Psychol Rev 2000;20:359–78. [DOI] [PubMed] [Google Scholar]
- [62].Rucklidge JJ, Brown DL, Crawford S, Kaplan BJ. Retrospective reports of childhood trauma in adults with ADHD. J Atten Disord 2006;9:631–41. [DOI] [PubMed] [Google Scholar]
- [63].Glutting JJ, Youngstrom EA, Watkins MW. ADHD and college students: exploratory and confirmatory factor structures with student and parent data. Psychol Assess 2005;17:44–55. [DOI] [PubMed] [Google Scholar]
- [64].Proctor BE, Prevatt F. Confirming the factor structure of attention-deficit/hyperactivity disorder symptoms in college students using student and parent data. J Learn Disabil 2009;42:250–9. [DOI] [PubMed] [Google Scholar]
- [65].Span SA, Earleywine M, Strybel TZ. Confirming the factor structure of attention deficit hyperactivity disorder symptoms in adult, nonclinical samples. J Psychopathol Behav 2002;24:129–36. [Google Scholar]
- [66].Kessler RC, Green JG, Adler LA, Barkley RA, Chatterji S, Faraone SV, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: analysis of expanded symptom criteria from the adult ADHD diagnostic scale. Arch Gen Psychiatry 2010;67:1168–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center Ground Zero. J Abnorm Psychol 2007;116:329–41. [DOI] [PubMed] [Google Scholar]
- [68].Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. J Abnorm Psychol 2010;119: 764–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Martel MM. Research review: A new perspective on attention-deficit/hyperactivity disorder: emotion dysregulation and trait models. J Child Psychol Psychiatry 2009;50:1042–51. [DOI] [PubMed] [Google Scholar]
- [70].Sergeant JA, Oosterlaan J, van der Meere J. Information processing and energetic factors in attention-deficit/hyperactivity disorder In: Quay HC, & Hogan AE, editors. Handbook of disruptive behavior disorders. New York: Kluwer/Plenum; 1999. p. 75–104. [Google Scholar]
- [71].Frewen PA, Lanius RA. Toward a psychobiology of posttraumatic self-dysregulation: reexperiencing, hyperarousal, dissociation, and emotional numbing. Ann NY Acad Sci 2006;1071:110–24. [DOI] [PubMed] [Google Scholar]
- [72].Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry 2010;167:640–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Banich MT, Mackiewicz KL, Depue BE, Whitmer AJ, Miller GA, Heller W. Cognitive control mechanisms, emotion, and memory: a neural perspective with implications for psychopathology. Neurosci Biobehav Rev 2009;33:613–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Henry B, Moffitt TE, Caspi A, Langley J, Silva PA. On the “remembrance of things past”: a longitudinal evaluation of the retrospective method. Psychol Assess 1994;6:92–101. [Google Scholar]
- [75].Murphy P, Schachar R. Use of self-ratings in the assessment of symptoms of attention deficit hyperactivity disorder in adults. Am J Psychiatry 2000;157:1156–9. [DOI] [PubMed] [Google Scholar]
- [76].Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry 2004;45:260–73. [DOI] [PubMed] [Google Scholar]
- [77].Vasterling JJ, Verfaellie M, Sullivan KD. Mild traumatic brain injury and posttraumatic stress disorder in returning veterans: perspectives from cognitive neuroscience. Clin Psychol Rev 2009;29:674–84. [DOI] [PubMed] [Google Scholar]
- [78].Thompson RA. Emotion regulation: a theme in search of a definition. In: & Fox NA, editor. The development of emotion regulation: biological and behavioral considerations. Monographs of the Society for Research in Child Development; 1994. p. 25–52. 59(2/3). [PubMed] [Google Scholar]
- [79].Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 2005;57:1336–46. [DOI] [PubMed] [Google Scholar]
- [80].Linehan MM. Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- [81].Mohlman J Attention training as an intervention for anxiety: review and rationale. Behav Therapist 2004;27:37–41. [Google Scholar]
- [82].Shipherd JC, Salters-Pedneault K. Attention, memory, intrusive thoughts, and acceptance in PTSD: an update on the empirical literature for clinicians. Cogn Behav Pract 2008;15:349–63. [Google Scholar]