Abstract
Objective
Health-related quality of life (HRQoL) is a patient-centred benchmark promoted by clinical guidelines in atrial fibrillation (AF). Income is associated with health outcomes, but how income effects HRQoL in AF has limited investigation.
Methods
We enrolled a convenience cohort with AF receiving care at a regional healthcare system and assessed demographics, medical history, AF treatment, income, education and health literacy. We defined income as a categorical variable (<$20 000; $20 000–$49 999; $50 000–$99 999; >$100 000). We used two complementary HRQoL measures: (1) the atrial fibrillation effect on quality of life (AFEQT), measuring composite and domain scores (daily activity, symptoms, treatment concerns, treatment satisfaction; range 0–100); (2) the 12-item Short Form Survey (SF-12), measuring general HRQoL with physical and mental health domains (range 0–100). We related income to HRQoL and adjusted for relevant covariates.
Results
In 295 individuals with AF (age 71±10, 40% women), we observed significant differences in HRQoL by income. Higher mean composite AFEQT scores were observed for higher income groups: participants with income <$20 000 had the lowest HRQoL (n=35, 68.2±21.4), and those with income >$100 000 had the highest HRQoL (n=64, 81.9±17.0; p=0.04). We also observed a significant difference by income in the AFEQT daily activity domain (p=0.02). Lower income was also associated with lower HRQoL in the mental health composite score of the SF-12 (59.7±21.5, income <$20 000 vs 79.3±16.3, income >$100 000; p<0.01).
Conclusion
We determined that income was associated with HRQoL in a cohort with prevalent AF. Given the marked differences, we consider income as essential for understanding patient-centred outcomes in AF.
Keywords: atrial fibrillation, epidemiology, public health
Key messages.
What is already known about this subject?
Atrial fibrillation (AF) has an adverse impact on health-related quality of life (HRQoL). HRQoL is becoming an increasingly emphasised patient-centred benchmark in treatment guidelines and clinical trials for AF.
What does this study add?
Our manuscript describes the association of income and HRQoL in individuals with AF.
How might this impact on clinical practice?
Understanding the association between annual income and HRQoL in AF can help guide strategies to improve patient-centred outcomes.
Introduction
Atrial fibrillation (AF) is a challenging arrhythmia with adverse impact on health-related quality of life (HRQoL).1 Patients with AF experience unfavourable symptoms of varying degree and severity that may be disabling. Treatment for AF requires long-term adherence to challenging medications, such as anticoagulants or anti-arrhythmic drugs, which have significant potential for side effects. AF is associated with a range of negative outcomes—stroke, myocardial infarction, heart failure, decreased functional status and multiple others—that contribute to significant social and medical costs.2–4 The symptoms, treatment and outcomes associated with AF have a heavy toll on patients’ quality of life. Accordingly, HRQoL has emerged as a benchmark in AF treatment guidelines and a patient-centred outcome in clinical trials for patients with AF.1
Income is associated with health outcomes, but how income relates to HRQoL in AF has had limited investigation. Socioeconomic status (SES), often determined by income and education, is associated with risk factors and outcomes for multiple cardiovascular and non-cardiovascular diseases.5 6 A large community-based cohort identified unemployment as a risk factor for AF.7 Individuals with higher SES were 50% more likely to transition from warfarin to a direct oral anticoagulant, a change that decreases the specific self-care burdens associated with warfarin.8 In a cohort of over 166 000 people with AF on warfarin therapy, lower SES was associated with an 18% higher rate of haemorrhage and a 28% higher rate of haemorrhage-related mortality relative to people with higher SES.9 Lower SES has also been shown to be associated with higher mortality in individuals with AF.10
In the present study, we examined the association between income and HRQoL in a cohort with prevalent AF. Our objectives were twofold. First, we sought to quantify the degree to which self-reported annual income was associated with HRQoL in individuals with AF. We hypothesised that, among people with AF, those with lower income would have lower HRQoL in comparison with people with higher income.
Methods
Cohort ascertainment
Study participants were enrolled via their affiliation with the University of Pittsburgh Medical Center, a large, regional healthcare system with a uniform electronic health record spanning multiple sites in Pittsburgh, Pennsylvania, and the surrounding region. Participants were identified by screening of the electronic health record and direct contact at ambulatory visits, referral by physicians and other providers, and self-referral via the University of Pittsburgh’s Center for Assistance in Research eRecord, which serves as a web-based portal for institutional-based clinical research. Eligibility criteria for this study consisted of age ≥18 years; a documented history of non-valvular AF, as established by the electronic health record; a CHADS2-VASc (congestive heart failure [CHF], hypertension [HTN], stroke, vascular disease [history of MI, PVD, or aortic atherosclerotic disease] and diabetes) score ≥211; English-speaking at a level appropriate to provide informed consent and participate in this research. From September 2016 through May 2018, a total of 1093 eligible participants were identified, 486 were approached by the study team and 339 agreed to participate. Study participants lacking income data were excluded from this analysis.
Demographics including age, sex and race were obtained by participant self-report. Body mass index (BMI) was extracted from the medical record. Clinical history including medical history relevant to the CHADS2-VASc, medications and AF treatment were assessed by a combination of self-report and review of the electronic medical record. Medication use collected included use of anti-arrhythmic medications including: flecainide, sotalol, amiodarone, propafenone, dofetilide and lidocaine. Prior treatment variables included history of pulmonary vein isolation, electrical cardioversion, or cardioversion by medication. Annual household income was obtained by self-report and categorised into four groups based on distribution (<$19 000; $20 000–$49 999; $50 000–$99 999; >$100 000) and summarised in online Supplementary table 1. Similarly, highest completed education level was obtained by self-report and divided into four groups based on distribution (≤high school or vocational training; some part of college or an associate degree; bachelor’s degree; or any graduate or professional school degree or enrolment), as summarised in online Supplementary table 2. Health literacy was assessed with the short-test of functional health literacy in adults (S-TOFHLA).12
Health-related quality of life
We ascertained HRQoL with two complementary measures: the atrial fibrillation effect on quality of life (AFEQT)13 and the 12-item Short Form Survey (SF-12).14 The AFEQT allows individuals with AF to quantify disease-specific HRQoL. The AFEQT is a validated, 20-item questionnaire that measures HRQoL in AF across four domains: symptoms, daily activities, treatment concern and treatment satisfaction. A summary measure and the four domains are each scored from 0 to 100, with higher scores indicating superior quality of life. The SF-12 was used to assess general physical and mental HRQoL. The SF-12 is an instrument that contains eight subscales including: physical functioning, role limitation due to physical problems, bodily pain, general health, vitality, social functioning, role limitation due to emotional problems and mental health with scores ranging from 0 to 100. The SF-12 was assessed in a subset of the participants (n=185).
Statistical methods
We summarised continuous variables as mean±SD and categorical variables by their frequency (n, %). We compared patient characteristics across the four income groups using the χ2 test for categorical variables and analysis of variance for continuous variables. We completed a test for trend using the Jonchkeere-Terpstra test ordered for differences among classes. We report the measures of HRQoL (AFEQT composite, AFEQT domain scores and SF-12 subscales) as mean±SD across each of the income groups. Multivariable regression was performed to test differences in HRQoL by income when adjusting for relevant covariates. We tested with adjustments for different combinations of variable including: (1) model I: age and sex; (2) model II: age, sex, race, BMI, CHF, HTN, stroke, vascular disease, education and S-TOFHLA; (3) model III: model II (age, sex, race, BMI, CHF, HTN, stroke, vascular disease, education and S-TOFHLA) plus AF treatment (consisting in procedures and anti-arrhythmic medications). We checked the variance inflation factor (VIF) of all variables in multivariable models and no pair of independent variables had a VIF greater than 1.3, indicating no problems with multicollinearity. An adjusted test for trend using a constrained interference for linear mixed effects (CLME) test was also performed15 16 (online Supplementary table 3). Statistical analyses were performed using SAS V.9.4.
Results
Patient characteristics
There were 339 participants enrolled in this study. Following exclusions for missing income data (n=44), 295 participants were included for these analyses. Table 1 describes the study cohort (age 71.3±9.9, 40.0% women, 95.3% white race). The majority of the cohort had HTN (71.2% of participants) while CHF and diabetes were less prevalent (approximately 20%). There was no difference between income groups when evaluating AF treatments. We observed statistically significant differences in education and sex when between income groups using test for trend. Lower income was associated with lower education attainment.
Table 1.
Patientcharacteristics in individuals with atrial fibrillation, by income
| Characteristic | All participants | <$20 000 | $20 000–$49 000 | $50 000–$99 999 | >$100 000 | P value (standard) | P value (trend) |
| n=295 | n=35 | n=99 | n=97 | n=64 | |||
| Age | 71.3±9.9 | 69.9±11.4 | 73.2±10.2 | 71.6±9.2 | 68.8±9.4 | 0.04 | 0.06 |
| Sex (Male) | 177 (60.0%) | 16 (45.7%) | 55 (55.6%) | 66 (68.0%) | 40 (62.5%) | 0.09 | 0.04 |
| White race | 281 (95.3%) | 34 (97.1%) | 92 (92.9%) | 95 (97.9%) | 60 (93.8%) | 0.01 | 0.64 |
| BMI | 31.4±7.41 | 33.2±9.09 | 31.4±7.50 | 31.4±7.77 | 30.5±5.39 | 0.41 | 0.13 |
| CHF | 54 (18.3%) | 9 (25.7%) | 23 (23.2%) | 17 (17.5%) | 5 (7.8%) | 0.05 | <0.01 |
| HTN | 210 (71.2%) | 29 (82.9%) | 69 (69.7%) | 71 (73.2%) | 41 (64.1%) | 0.24 | 0.16 |
| DM | 65 (22.0%) | 7 (20.0%) | 22 (22.2%) | 22 (22.7%) | 14 (21.9%) | 0.99 | 0.84 |
| Stroke/TIA | 22 (7.5%) | 2 (5.7%) | 11 (11.1%) | 3 (3.1%) | 6 (9.4%) | 0.16 | 0.68 |
| Vascular disease | 56 (19.0%) | 4 (11.4%) | 26 (26.3%) | 16 (16.5%) | 10 (15.6%) | 0.13 | 0.42 |
| Education | <0.01 | <0.01 | |||||
| ≤HS or vocational | 100 (33.9%) | 21 (60.0%) | 47 (47.5%) | 28 (28.9%) | 4 (6.3%) | ||
| Some college | 62 (21.0%) | 7 (20.0%) | 24 (24.2%) | 22 (22.7%) | 9 (14.1%) | ||
| Bachelor’s | 70 (23.7%) | 6 (17.1%) | 18 (18.2%) | 29 (29.9%) | 17 (26.6%) | ||
| Graduate | 63 (21.4%) | 1 (2.9%) | 10 (10.1%) | 18 (18.6%) | 34 (53.1%) | ||
| S-TOHFLA Score | 29.6±4.92 | 27.3±5.88 | 28.9±6.26 | 30.2±3.51 | 31.0±2.89 | <0.01 | <0.01 |
| Treatment | |||||||
| Pulmonary vein isolation | 59 (20.0%) | 6 (17.1%) | 20 (20.2%) | 15 (15.5%) | 18 (28.1%) | 0.25 | 0.28 |
| Electrical cardioversion | 58 (19.7%) | 6 (17.1%) | 18 (18.2%) | 19 (19.6%) | 15 (23.4%) | 0.83 | 0.38 |
| Cardioversion by medication | 5 (1.7%) | 0 (0.0%) | 0 (0.0%) | 3 (3.1%) | 2 (3.1%) | 0.23 | 0.07 |
| Anti-arrhythmics (any) | 72 (24.4%) | 6 (17.1%) | 21 (21.2%) | 25 (25.8%) | 20 (31.3%) | 0.35 | 0.07 |
Standard p value using χ2 tests for categorical variables and ANOVA for continuous variables. P value trend test using the Jonckheere-Terpstra test for ordered differences among classes.
BMI, body mass index; CHF, congestive heart failure; DM, diabetes mellitus; HS, high school; HTN, hypertension; S-TOFHLA, short-test of functional health literacy in adults; TIA, transient ischaemic attack.
Income and HRQoL
All results are presented here are derived from model III, however results these findings were consistent across the three sets of models. When examining the association between income and HRQoL as measured by AFEQT, we observed a graded relation with higher income associated with higher HRQoL (68.2±21.4 for income <$20 000 vs 81.9±17.0 for income >$100 000; p=0.04, figure 1). When examining AFEQT by domain, the largest differences across income groups was observed for daily activity domain (57.3±26.3 for income <$20 000 vs 79.8±23.9 for income >$100 000; p=0.02, figure 2). These associations persisted in multivariable-adjusted models that included age, sex, race, BMI, CHF, HTN, stroke, vascular disease, education, AF treatment, and health literacy.
Figure 1.
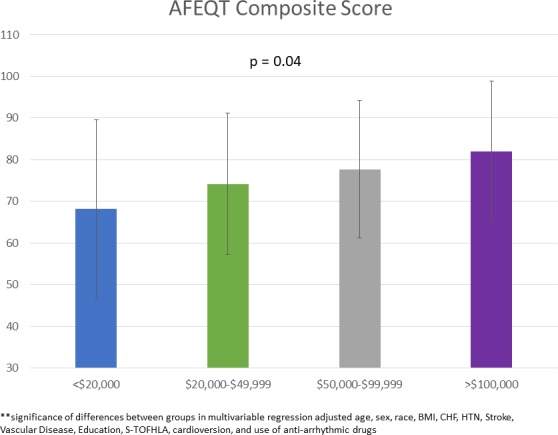
Distribution of atrial fibrillation effect on quality of life (AFEQT) composite score, by income. Bar graph relating composite AFEQT score to income as a categorical variable. Graded relationship with lower annual income associated with inferior health-related quality of life. Error bars represent SD. BMI, body mass index; CHF, congestive heart failure; HTN, hypertension; S-TOFHLA, short-test of functional health literacy in adults.
Figure 2.
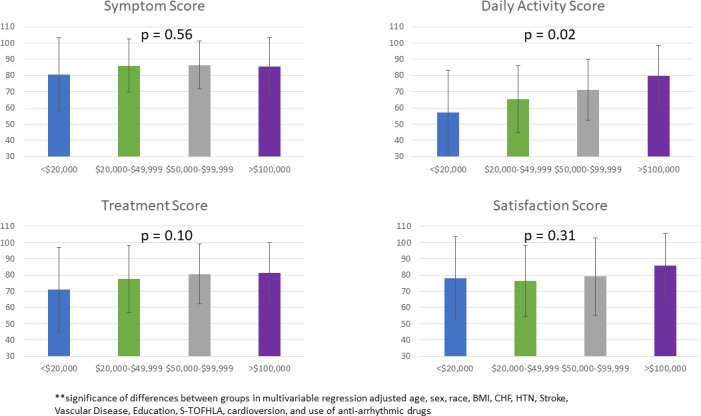
Distribution of atrial fibrillation effect on quality of life (AFEQT) domain scores, by income. bar graph relating AFEQT domain scores to income as a categorical variable. Significant graded relationship with lower annual income associated with inferior health-related quality of life in the daily activity domain. Error bars represent SD. BMI, body mass index; CHF, congestive heart failure; HTN, hypertension; S-TOFHLA, short-test of functional health literacy in adults.
When evaluating the relation between income and HRQoL as measured by SF-12, we similarly observed a graded relation between income and HRQoL. Higher levels of income were associated with higher mental health composite scores (43.2±11.8, 49.8±10.3, 52.1±8.0 and 53.2±7.2 for income <$19 000; $20 000–$49 999; $50 000–$99 999; >$100 000, respectively; p<0.01) but were less strongly associated with physical health composite scores (p=0.07), as summarised in table 2. In addition, we identified a strong association between income and the SF-12 subscores of role limitation physical (0.01), general health (p<0.01), vitality (p=0.01), social functioning (p=0.01), role limitation emotional (p<0.01), mental health (p<0.01) and mental health composite (p<0.01).
Table 2.
Adherence, stress, health and quality of life scores in individuals with atrial fibrillation, by income
| Characteristic | All participants | <$20 000 | $20 000–$49 000 | $50 000–$99 999 | >$100 000 | P value (adjusted)* | P value (adjusted)† | P value (adjusted)‡ |
| n=295 | n=35 | n=99 | n=97 | n=64 | ||||
| AFEQT | ||||||||
| Symptom score | 85.4±17.1 | 80.7±22.6 | 86.0±16.5 | 86.4±14.9 | 85.5±17.9 | 0.63 | 0.57 | 0.56 |
| DA score | 69.4±25.1 | 57.3±26.3 | 65.3±23.6 | 71.1±24.4 | 79.8±23.9 | <0.01 | 0.02 | 0.02 |
| Treatment score | 78.5±20.4 | 71.0±26.0 | 77.5±20.7 | 80.5±18.5 | 81.2±18.7 | 0.06 | 0.08 | 0.1 |
| Satisfaction score | 79.5±22.7 | 78.1±25.3 | 76.5±21.9 | 79.0±23.9 | 85.8±19.9 | 0.07 | 0.31 | 0.31 |
| Total score | 76.3±17.8 | 68.2±21.4 | 74.2±17.0 | 77.7±16.5 | 81.9±17.0 | <0.01 | 0.03 | 0.04 |
| SF-12 | n = 185 | n = 22 | n = 61 | n = 64 | n = 38 | |||
| Physical functioning | 59.7±36.6 | 44.3±36.9 | 52.5±39.5 | 62.9±34.2 | 75.0±29.6 | <0.01 | 0.07 | 0.08 |
| Role limitation physical | 56.7±27.1 | 39.2±24.2 | 52.7±24.5 | 61.7±28.2 | 64.8±26.0 | <0.01 | <0.01 | 0.01 |
| Pain | 68.1±33.4 | 46.6±33.9 | 67.2±31.8 | 71.1±34.0 | 77.0±30.4 | <0.01 | 0.03 | 0.05 |
| General health | 54.5±27.5 | 35.0±28.9 | 51.8±27.4 | 59.5±23.8 | 61.8±28.0 | <0.01 | <0.01 | <0.01 |
| Vitality | 45.8±25.1 | 35.2±26.3 | 41.0±24.6 | 48.4±23.5 | 55.3±24.8 | <0.01 | <0.01 | 0.01 |
| Social functioning | 76.4±27.7 | 56.8±31.0 | 73.0±28.2 | 83.2±24.4 | 81.6±24.4 | <0.01 | <0.01 | 0.01 |
| Role limitation emotional | 77.0±23.9 | 56.3±29.3 | 74.2±23.0 | 81.4±22.3 | 85.9±16.2 | <0.01 | <0.01 | <0.01 |
| Mental health | 72.8±19.3 | 59.7±21.5 | 71.7±19.4 | 74.4±18.3 | 79.3±16.3 | <0.01 | <0.01 | <0.01 |
| Physical health composite | 40.6±11.6 | 34.3±10.7 | 38.9±12.1 | 42.0±11.2 | 44.4±10.2 | <0.01 | 0.04 | 0.07 |
*P value adjusted for covariates age and sex.
†P value adjusted for covariates including: age, sex, race, BMI, CHF, HTN, stroke, vascular disease, education, S-TOFHLA.
‡P value adjusted for covariates including: age, sex, race, BMI, CHF, HTN, stroke, vascular disease, education, S-TOFHLA, cardioversion and use of anti-arrhythmic drugs.
§Continuous variables summarised as mean±SD; significance test performed using ANOVA.
AFEQT, atrial fibrillation effect on quality-of-life; SF-12, 12-item Short Form Survey; S-TOHFLA, short-test of functional health literacy in adults.
Discussion
In a cohort of individuals receiving clinical care for non-valvular AF, we identified strong associations between income and HRQoL as measured by two complementary, well-validated assessments of HRQoL, the AF-specific AFEQT and the more general SF-12. In addition, we found that the domain of HRQoL most significantly associated with income was daily activity. In the daily activity domain, individuals with annual income <$20 000 had nearly 40% lower HRQoL compared with the highest income group. Our results remained significant when adjusting for covariates encompassing demographics, clinical history and both pharmacological and electrophysiological AF treatment. Our results are consistent with the study of HRQoL in other cohorts with chronic diseases.17–19 We observed similar associations between income and mental and physical components of the SF-12 as that identified in cohorts with diabetes or a history of stroke.20 21
Multiple reasons likely explain the associations we observed. First, lower income can limit individuals’ ability to access medications or treatments that in turn may alleviate symptoms and improve clinical outcomes. Inability to access such resources may ultimately lead to inferior HRQoL. However, participants in this study were recruited from the same clinics with similar access to clinical treatments and physicians, and there was no significant difference between income groups when looking at medications or electrophysiological treatments. It is possible that the uniform treatment across income groups in our cohort accounts for the absence of differences in HRQoL treatment or symptom domain. Second, out-of-pocket expenses related to AF may have more effect on people with lower income. While our study did not measure the financial costs allocated by patients, we expect that out-of-pocket expenditures would have a higher toll on HRQoL for individuals with limited income. Third, income may be related to additional social factors that mediate or moderate the associations we observed. In particular, in our data, income is associated with education and health literacy. Such factors may provide intermediate mechanisms by which income may impact HRQoL. AF is a complex condition, and limited health literacy may affect individuals’ understanding of the condition, rationale for treatment, expectations of treatment and adherence, and such factors may in turn result in lower HRQoL.22 Fourth, the profound social burden associated with AF may include missed work and disability as we expect that individuals with lower income would experience a greater severity of the concomitant financial stress surrounding such events.23 Finally, our study lacks a control group measuring changes in HRQoL in individuals without AF. Without a control group for comparison we cannot accurately define the magnitude of decreased HRQoL due to AF specifically. However, the AFEQT provides information regarding AF-specific HRQoL measures, and we observed a graded relation such that decreased income was associated with lower HRQoL as quantified with AF-specific measures. We additionally note that the magnitude of changes in SF-12 components was similar in our study as that observed in cohorts with diabetes or a history of stroke.20 21
Income has been previously associated with decreased quality of life in both chronic medical conditions and cardiovascular disease.24–27 However, data specifically evaluating this association in individuals with AF are sparse. A large, community-based cohort with extended follow-up of over 20 years did identify family income as associated with increased risk of incident AF.28 Our study contributes to the literature demonstrating the impact of social factors such as income on patient-centred outcomes in AF.
Understanding the association between income and HRQoL in individuals with AF can guide strategies to improve outcomes. Our findings are relevant to the assessment and interpretation of HRQoL, which is now routine in clinical trials and registries for AF. Many clinical trials and registries have treated income as a silent covariate, either not examining the effect of income or not assessing income at all. Our findings suggest that income should not be ignored in understanding these relationships. Specifically, our results support the assessment of income as a social determinant that may influence patient-centred outcomes in the treatment of AF. Likewise, our results suggest that interventions that aim to improve HRQoL need to include individuals with lower income in order to assess efficacy and generalisability to a more vulnerable patient population. Additional research is essential to incorporate other social determinants of health in the assessment of AF risk, symptom recognition, treatment and adverse outcomes. In particular, investigations of income and increased risks for morbidity and mortality in AF are needed. In summary, HRQoL is a focus of guidelines-based care, and our results establish the importance of patient income in the care and management of AF.
The strengths of our study include our recruitment of a moderate-sized cohort of individuals with prevalent AF and our employment of well-validated, complementary measures of HRQoL. This study also has important limitations. Our primary limitation concerns generalisability, as this cohort was recruited as a single-centre study. Additionally, there was limited racial and ethnic diversity in our cohort, which may further limit generalisability. Second, we relied on a single measurement of self-reported income as our independent variable. It is possible that some individuals had financial assets or higher net worth than characterised by income, and that such resources would confound our assessments of income with HRQoL. However, we would expect that such misclassification would affect those with lower income primarily, and thereby would not diminish the strong associations between income and HRQoL that we observed here. Third, we cannot exclude residual confounding by unmeasured variables that may impact income and HRQoL. For example, individuals with greater physical disability or burden of comorbidity may have decreased employment and lower general quality of life. Fourth, we assessed HRQoL at a single time point, and recognise that a patient-centred outcome such as quality of life may evolve with the experience and treatment of a chronic disease.
Finally, our analysis consisted of a cross-sectional assessment which precludes determination of the existence or direction of a causal relation between income and HRQoL. Indeed, the relationship between income and HRQoL for patients with AF may be complex and bidirectional with both—lower income leading to lower HRQoL and lower HRQoL leading to lower income. The ways AF and AF treatment may have influenced patients’ work history and earning capacity were beyond the scope of our data collection. Similarly, the ways different type of workers (eg, labourers vs managers) have the physical capacity or job flexibility to withstand symptoms of AF and AF treatment were beyond the scope of our data collection. Ultimately, such data would be needed over time to ascertain causation and directionality for the findings we have presented.
In conclusion, we found a strong association in individuals with AF between higher income and higher HRQoL as measured by both the AFEQT and SF-12. Our findings suggest that ascertainment of income is relevant to the treatment and assessment of quality of life in AF. Studies of patient-centred outcomes in AF should include income. Exploring the mechanisms underlying this relationship may provide opportunities for intervention.
Footnotes
Contributors: EG: conception, design, drafting of the manuscript and manuscript revision. AA: analysis, manuscript revision. MS: analysis, manuscript revision. AMP: data collection, design, manuscript revision. MP-O: manuscript revision. JWM: conception, design and drafting of the manuscript, manuscript revision for important intellectual content and final approval of the manuscript.
Funding: This work was supported by Grant 2015084 from the Doris Duke Charitable Foundation and by NHLBI award R56143010.
Competing interests: None declared.
Patient consent for publication: All participants provided written informed consent.
Ethics approval: The University of Pittsburgh Institutional Review Board approved the study protocol.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The anonymized individual participant data will be shared onreasonable request.
References
- 1.Cherian TS, Shrader P, Fonarow GC, et al. . Effect of Atrial Fibrillation on Mortality, Stroke Risk, and Quality-of-Life Scores in Patients With Heart Failure (from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation [ORBIT-AF]). Am J Cardiol 2017;119:1763–9. 10.1016/j.amjcard.2017.02.050 [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Wolf PA, D'Agostino RB, et al. . Impact of Atrial Fibrillation on the Risk of Death : The Framingham Heart Study. Circulation 1998;98:946–52. [DOI] [PubMed] [Google Scholar]
- 3.Anter E, Jessup M, Callans DJ, et al. . And heart failure: treatment considerations for a dual epidemic. Circulation 2009;119:2516–25. [DOI] [PubMed] [Google Scholar]
- 4.Passman R, Bernstein RA. New appraisal of atrial fibrillation burden and stroke prevention. Stroke 2016;47:570–6. 10.1161/STROKEAHA.115.009930 [DOI] [PubMed] [Google Scholar]
- 5.Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu. Rev. Public Health 2011;32:39–69. 10.1146/annurev-publhealth-031210-101234 [DOI] [PubMed] [Google Scholar]
- 6.Havranek EP, Mujahid MS, Barr DA, et al. . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 7.Soliman EZ, Zhang Z-M, Judd S, et al. . Comparison of risk of atrial fibrillation among employed versus unemployed (from the reasons for geographic and racial differences in Stroke study). Am J Cardiol 2017;120:1298–301. 10.1016/j.amjcard.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sholzberg M, Gomes T, Juurlink DN, et al. . The influence of socioeconomic status on selection of anticoagulation for atrial fibrillation. Plos One 2016;11:e0149142–12. 10.1371/journal.pone.0149142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cressman AM, Macdonald EM, Yao Z, et al. . Socioeconomic status and risk of hemorrhage during warfarin therapy for atrial fibrillation: a population-based study. American Heart Journal 2015;170:133–40. 10.1016/j.ahj.2015.03.014 [DOI] [PubMed] [Google Scholar]
- 10.Kargoli F, Shulman E, Aagaard P, et al. . Socioeconomic status as a predictor of mortality in patients admitted with atrial fibrillation. Am J Cardiol 2017;119:1378–81. 10.1016/j.amjcard.2017.01.041 [DOI] [PubMed] [Google Scholar]
- 11.GYH L, Nieuwlaat R, Pisters R, et al. . Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach. CHEST 2010;137:263–72. [DOI] [PubMed] [Google Scholar]
- 12.Baker DW, Williams MV, Parker RM, et al. . Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42. 10.1016/S0738-3991(98)00116-5 [DOI] [PubMed] [Google Scholar]
- 13.Spertus J, Dorian P, Bubien R, et al. . Development and validation of the atrial fibrillation effect on quality-of-life (AFEQT) questionnaire in patients with atrial fibrillation. Circ Arrhythm Electrophysiol 2011;4:15–25. 10.1161/CIRCEP.110.958033 [DOI] [PubMed] [Google Scholar]
- 14.Gandek B, Ware JE, Aaronson NK, et al. . Cross-validation of item selection and scoring for the SF-12 health survey in nine countries. J Clin Epidemiol 1998;51:1171–8. 10.1016/S0895-4356(98)00109-7 [DOI] [PubMed] [Google Scholar]
- 15.Jelsema CM, Peddada SD. CLME : An R Package for Linear Mixed Effects Models under Inequality Constraints. J. Stat. Soft. 2016;75:1–32. 10.18637/jss.v075.i01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farnan L, Ivanova A, Peddada SD. Linear mixed effects models under inequality constraints with applications. PLoS ONE 2014;9:e84778–8. 10.1371/journal.pone.0084778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brennan DS, Spencer AJ. Health-related quality of life and income-related social mobility in young adults. Health Qual Life Outcomes 2014;12:52–6. 10.1186/1477-7525-12-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huguet N, Kaplan MS, Feeny D. Socioeconomic status and health-related quality of life among elderly people: results from the joint Canada/United states survey of health. Soc Sci Med 2008;66:803–10. 10.1016/j.socscimed.2007.11.011 [DOI] [PubMed] [Google Scholar]
- 19.Lemos CF, Rodrigues MP, Veiga JRP. Family income is associated with quality of life in patients with chronic kidney disease in the pre-dialysis phase: a cross sectional study. Health Qual Life Outcomes 2015;13:1–9. 10.1186/s12955-015-0390-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellis C, Grubaugh AL, Egede LE. Factors associated with SF-12 physical and mental health quality of life scores in adults with stroke. J Stroke Cerebrovasc Dis 2013;22:309–17. 10.1016/j.jstrokecerebrovasdis.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 21.Arditi C, Zanchi A, Peytremann-Bridevaux I. Health status and quality of life in patients with diabetes in Switzerland. Prim Care Diabetes 2018:1–2. 10.1016/j.pcd.2018.11.016 [DOI] [PubMed] [Google Scholar]
- 22.Aronis KN, Edgar B, Lin W, et al. . Health literacy and atrial fibrillation: relevance and future directions for patient-centred care. Eur Cardiol 2017;12:52–14. 10.15420/ecr.2017:2:2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghushchyan V, Nair KV, Page RL. Indirect and direct costs of acute coronary syndromes with comorbid atrial fibrillation, heart failure, or both. Vasc Health Risk Manag 2015;11:25–10. 10.2147/VHRM.S72331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J-H, Park E-C. Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Public Health 2015;15:1–15. 10.1186/s12889-015-2014-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CLK L, Guo VY, Wong CKH, et al. . Poverty and health-related quality of life of people living in Hong Kong: comparison of individuals from low-income families and the general population. J Public Health 2016;54:fdw046–23. [DOI] [PubMed] [Google Scholar]
- 26.Klein J, Lüdecke D, Hofreuter-Gätgens K, et al. . Income and health-related quality of life among prostate cancer patients over a one-year period after radical prostatectomy: a linear mixed model analysis. Qual Life Res 2017;26:2363–73. 10.1007/s11136-017-1582-9 [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Ou F, Gao S, et al. . Effect of low income on health-related quality of life: a cross-sectional study in northeast China. Asia Pac J Public Health 2015;27:NP1013–25. [DOI] [PubMed] [Google Scholar]
- 28.Misialek JR, Rose KM, Everson-Rose SA, et al. . Socioeconomic status and the incidence of atrial fibrillation in whites and blacks: the Atherosclerosis Risk in Communities (ARIC) study. J Am Heart Assoc 2014;3:e001159–9. 10.1161/JAHA.114.001159 [DOI] [PMC free article] [PubMed] [Google Scholar]


