Abstract
Background: The neonatal period is the most susceptible phase of life. In Ethiopia changes in neonatal mortality are not as significant as changes in post-neonatal and child mortality. The aim of this study was to assess the causes and factors associated with neonatal mortality at Jimma Medical Center.
Materials and methods: A cross-sectional study was conducted for 11 days from February 12, 2018 at the Neonatal ICU of Jimma Medical Center. Data were extracted from the medical records of neonates admitted during a three year period from September 07, 2014 to August 31, 2017, using pretested checklists. Bivariate and multivariate logistic regressions were used to determine factors associated with neonatal mortality and P-values <0.05 were considered statistically significant.
Results: Of 3,276 neonates admitted during the study period, 412 (13.3%) died, equating to a rate of 30 deaths per 1,000 institutional live births. The majority (249, 60.4%) of deceased neonates had low birth weight, while 230 (55.8%) were premature and 169(41%) had Respiratory Distress Syndrome (RDS). Residency being outside Jimma city (AOR 1.89, 95% CI: 1.43, 2.51) and the length of stay <7Days (AOR 3.93, 95% CI: 2.82, 5.50), low birth weight (AOR 1.54, 95% CI: 1.06, 2.25), prematurity (AOR 2.2, 95% CI: 1.41, 3.42), RDS (AOR 4.15, 95% CI: 2.9, 5.66), perinatal asphyxia (AOR 4.95, 95% CI: 3.6, 7.34), and congenital malformations (AOR 4, 95% CI: 2.55, 2.68) were significantly associated with neonatal mortality.
Conclusions: A significant proportion of neonates attending the neonatal ICU died. Parental residency, the length of stay, low birth weight, prematurity, RDS, perinatal asphyxia, and congenital malformations were factors associated with neonatal mortality, which could be avoidable. Therefore, preventive measures such as enhancing the utilization of antenatal care services and, early identification and referral of high risk pregnancy and neonates could reduce the neonatal deaths
Keywords: causes, neonate, mortality, Jimma, Ethiopia, NICU
Introduction
The neonatal period, from birth to the first 28 days of life, is the most hazardous period of life because of the various diseases that the neonate faces. The risk of dying is highest in this period of life.1 Globally, in 2017 alone, an estimated 6.3 million children and young adolescents died, mostly from preventable causes. Of these approximately 85% of deaths occurred in the first five years of life and nearly half (47%) of the under five deaths occurred in the first month of life. In other words, the probability of dying in the first 28 days of life was estimated at 18 deaths per 1,000 live births globally.2
Over the last two decades, the world has made substantial progress in the reduction of mortality among children. Globally, the neonatal mortality rate fell by 51% which means 37 deaths per 1,000 live births in 1990 to 18 in 2017. However, the change in neonatal mortality is not as significant as the change in children aged 1–59 months (63%).2 Africa contributed to one third of the world’s neonatal mortality burden. In this region about 75% of deaths occurred during the first week of life almost half being within the first 24 hrs. Among (Sustainable Developmental Goals (SDG) regions, Sub-Saharan Africa had the highest neonatal mortality rate in 2017 at 27 deaths per 1000 live births.2–4
According to the Ethiopian Demographic Health Survey (EDHS) 2016, the under-5, infant and neonatal mortality rate is 67, 48 and 29 deaths per 1,000 live births respectively. In other words, in Ethiopia 1 in every 35 children dies within the first month, 1 in every 21 children dies before celebrating the first birthday, and 1 of every 15 children dies before reaching the fifth birthday. Childhood mortality has declined substantially since 2000. Neonatal mortality declined from 49 deaths per 1,000 live births in 2000 to 29 deaths per 1,000 births in 2016, a reduction of 41% over the past 16 years. However, the change in neonatal mortality is not as significant as the change in post-neonatal and child mortality.5 In Ethiopia, the main causes of neonatal deaths were birth asphyxia, prematurity and sepsis.6–9
Knowing the disease patterns and causes in the Neonatal Intensive Care Unit (NICU) and the disease-wise mortality rate can inform the requisite efforts to reduce morbidity and mortality. Therefore, the aim of this study was to assess the causes and factors associated with neonatal mortality among neonates admitted to the Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center.
Materials and methods
Study design and period
An institutional based retrospective cross-sectional study was conducted from February 12, to 23, 2018 using the medical records of neonates admitted to Neonatal ICU of Jimma University Medical Center (JUMC).
Study setting and period
The study was carried out at Neonatal ICU of Jimma University Medical Center, located in Jimma town. The town is located 357 km towards the southwest of Addis Ababa, the capital of Ethiopia. JUMC is the only tertiary and referral teaching hospital in the south western part of the country, and currently provides different services for approximately 18 million people in the catchment area. The neonatal ICU is one of the ICU services that the hospital is currently running. The unit has 20 neonatal beds and 14 Kangaroo mother care (KMC) beds. the unit also has 2 incubators,10 radiant warmers, 4 continuous positive airway pressure (CPAP), phototherapy and oxygen concentrator machines. Additionally, there is pulse oximetry, glucometer and neonatal resuscitation equipment. Advanced procedures such as exchange transfusions and Lumber punctures are performed at the center. The unit is staffed with pediatricians, pediatric residents and neonatal nurses and located adjacent to the labour ward to receive high-risk newborns from this unit. Furthermore, the unit also receives neonates referred from other health facilities and homes. The maternal services including antenatal care follow up, delivery services, early detection and treatment of high-risk pregnant mothers are currently run by the center. According to Jimma town municipality reports during the last three years, there were 19,250 institutional delivery cases in Jimma town, from which 13,568 mothers give birth at JUMC, which resulted in 13,705 total live births.
Study population
The study populations were all neonates admitted to the Neonatal Intensive Care Unit (NICU) of JUMC from September 11, 2014 to September 10, 2017.
Inclusion and exclusion criteria
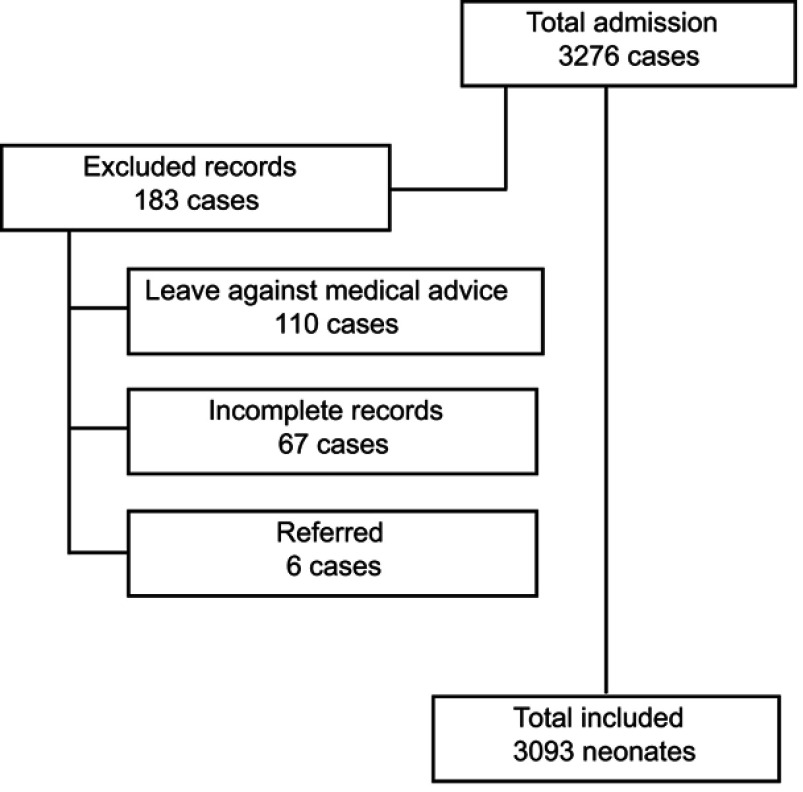
Medical records of neonates with a missing diagnosis of admission and missing clinical outcomes, other than death and improved discharge were excluded from the study (Figure 1).
Figure 1.
Flow chart of the inclusion and exclusion criteria.
Sample size
All available medical records of neonates that fulfilled the inclusion criteria were included in the study.
Data collection procedures
Data were extracted by reviewing medical records of newborns using a structured checklist adapted from the previous related study.8 The checklist contained variables including age, sex, address of parents, gestational age, birth weight, length of stay, causes of admission, causes of death and medical outcomes. The quality of the data collected was guaranteed by pretesting using the medical records of 5% of the newborns before actual data collection. The data were collected by professional nurses and training was given to the data collectors on how to collect data from the records to augment data accuracy and validity. The data collection was closely supervised by the supervisors to check for its completeness and clarity before data entry.
Data analysis
The Collected data were cleaned, coded and entered into Epidata 3.1 and exported, to SPSS for windows version 23.0 for cleaning and analyses, data were summarized, by using simple frequency tables, graphs, and charts. Bivariate analysis of candidate associated factors for multivariate analysis at the p-value of <0.25 and multivariate analysis was employed, in order to assess the relative effect of independent variables on dependent variables and statistically significant association was declared at the p-value of less than 0.05.
Operational definitions
Neonatal conditions were divided into five major categories, four adapted from the Global Burden of Diseases (GBD 2017) classification catalog, and one category, Low Birth Weight (LBW) added from the National strategy for newborn and child survival in Ethiopia.35,36 The presentation conditions included under these five categories is presented in the Table 1. Specific neonatal conditions with high frequency were selected and used for multivariate analysis. In JUMC, the causes of neonatal admissions and deaths were recorded based on clinical presentation and supportive laboratory results. In this study any neonatal conditions or diagnosis identified or recorded for deceased neonates were considered as causes of death and its contributing factors. In other words, causes of deaths were defined as the underlying neonatal factors or conditions, which presented in the admitted or deceased neonate. Variables such as birth weight; gestational age and maturity were classified based on WHO classification criteria.1 The gestational age was estimated using Maternal Report of the Last Normal Menstrual Period(LNMP) and confirmed by ultrasound for those mother who gave birth at the center while the Ballard score was used to estimate the gestational age of the newborn delivered outside the center and newborn delivered to those mothers who did not remember or know the date of their last normal menstrual period. The neonatal mortality rate was number of deaths during the first 28 completed days of life per 1,000 live births in a given period.
Table 1.
Major categories of neonatal diseases and definitions
| Categories | Definitions | Conditions included |
|---|---|---|
| Birth asphyxia & other perinatal complications | Any of the following conditions identified to occur in a newborn during the perinatal period. | -Birth asphyxia -Birth trauma -Hypoglycemia/Hypothermia -Meconium aspiration syndrome(MAS) -Pathological jaundice |
| Neonatal sepsis & Infections | Any neonatal conditions identified as neonatal sepsis and other neonatal infections. | -EONS -LONS -Any other infectionsa |
| Preterm birth complication | Any complications occurred in preterm newborns which attributed to prematurity | -Prematurity - Respiratory complication -Metabolic complications (Hypoglycemia/Hypothermia) - Infections and Sepsis - Other complications related to preterm birth |
| Low birth weight | Any child with birth weight is less than 2,500 g or recorded as LBW. | -Low birth weight (EVLBWa, LBW LBW) |
| Other neonatal condition | All neonatal conditions other than those listed in the above categories. | eg Congenital malformations, baby of high risk mothers, anemia, Circumcision site bleeding, baby admitted for observation and etc. |
Note: aAny other infection; includes any infections other than EONS and LONS.
Abbreviations: EONS, early onset neonatal sepsis; LONS, late onset neonatal sepsis; EVLBW, extremely very low birth weight; VLBW, very low birth weight; LBW, low birth weight; JUMC, Jimma University Medical Center.
Ethical considerations
Ethical clearance to conduct the study was obtained from the institutional review board of the Institute of Health, Faculty of Health Sciences, Jimma University. Further permission was obtained from the medical director of JUMC and the department head of pediatrics and gynecology for the utilization of medical records. We guaranteed confidentiality by excluding names or any other personal identifiers from data-collection sheets and reports. The identifier for each eligible subject was replaced by a code and no master code exists that allows the research data to be linked with the identifiers.
Results
The total number of neonates admitted to the NICU during the period under the study was 3,276, of which 110 neonates left against medical advice, 67 neonates had deficient
records and 6 neonates were referred to other facilities and were excluded from the study. A total of 3,093 neonates with improved/death hospital outcomes were included for further analysis.
Socio-demographic characteristics
The present study shows that, more than half, 1837(59.4%) of the neonates were males, while 1256(40.6%), were females giving a male to female ratio of 1.46:1. The majority, 2349(76.0%) of the newborns admitted within 24 hrs of life while 135(4.3%) were admitted within 8–21 days of life. The mean age at admission was 1.84(SD±2.4) days. With regard to the residential addresses of parents, the majority 2135(69%) came from places outside Jimma town, while 958(31%) of them were from Jimma town. For the period under the study it was observed that the magnitude of admissions increased from 453(14.6%) admissions during 2014/15 to 1085(35.1%) during the year 2016/2017. The highest admission of neonates was observed in 2015 which accounted for half (50%) of the total neonatal admissions studied (Table 2). Less than one third, 864(27.9%) of the neonates were preterm whereas 2229(72.1%) were term neonates. Regarding gestational ages of the neonates, the majority 222(71.9%)had a gestational age between 37–42 weeks. The birth weight of the newborns studied were comprised of, nearly one third 1108(35.8%) within the Low Birth Weight (LBW) range. Amongst these 29(1.0%), and 236(7.6%) had extremely or very low birth weights, respectively. Seventy two percent of the neonates were discharged within 7 days of admission, and the median length of stay was 5 days. Out of 3093 neonates admitted 412 died, giving a death rate of 13.3%. In other words, there were 30 deaths per 1,000 live births at the JUMC for the period under the study. The mortality rate was higher among neonates of extremely low birth weight, gestational age <28 weeks, very low birth weight and preterm which accounted 27/29(93%), 23/25(92%), 124/236(52.5%) and 230/864(26.6%) respectively (Table 2).
Table 2.
Demographic characteristics of neonates admitted to JUMC
| Characteristics | Frequency | Percent | Mean±SD | |
|---|---|---|---|---|
| Sex | Male | 1,837 | 59.4% | |
| Female | 1,256 | 40.6% | ||
| Total | 3,093 | 100% | ||
| Age | <24 hrs | 2,349 | 76.0% | |
| 2–7 days | 609 | 19.7% | ||
| ≥8–14 days | 135 | 4.3% | ||
| Total | 3,093 | 100% | 1.84±2.4 | |
| Parents’ residency | From Jimma | 958 | 31.0% | |
| Out of Jimma | 2,135 | 69.0% | ||
| Total | 3,093 | 100% | ||
| Year of visit | 2014/2015 | 453 | 14.6% | |
| 2015/2016 | 1,555 | 50.3% | ||
| 2016/2017 | 1,085 | 35.1% | ||
| Total | 3,093 | 100% | ||
| Gestational age | <28 weeks | 25 | 0.8% | |
| 28 – <32 weeks | 219 | 7.1% | ||
| 32 – <37 weeks | 620 | 20.0% | ||
| 37 – <42 weeks | 2,222 | 71.9% | ||
| >42 weeks | 7 | 0.2% | ||
| Total | 3,093 | 100% | ||
| Maturity | Preterm | 864 | 27.9% | |
| Term | 2,229 | 72.1% | ||
| Total | 3,093 | 100% | ||
| Birth weight | EVLBW | 29 | 1.0% | |
| VLBW | 236 | 7.6% | ||
| LBW | 843 | 27.3% | ||
| NBW | 1,864 | 60.3% | ||
| Macrosomia | 121 | 3.9% | ||
| Total | 3,093 | 100% | ||
| Length of say | <7 Days | 2,231 | 72.1% | |
| >7 Days | 862 | 27.8% | ||
| Total | 3,093 | 100% | ||
| Median | 5 | |||
| Hospital Outcomes | Died | 412 | 13.3% | |
| Improved | 2,681 | 86.7% | ||
| Total | 3,093 | 100% | ||
Abbreviations: EVLBW, extremely very low birth weight; VLBW, very low birth weight; LBW, low birth weight; NBW, normal birth weight; JUMC, Jimma University Medical Center.
Causes of neonatal admission and death
Nearly half (1,488, 48.1%) of admissions were due to birth asphyxia & other perinatal complications. Of these 138 died, accounting for 4.5% of total neonatal mortality.In contrast low birth weight newborns, accounted for 1108(35.8%) of admissions and contributed to 249(8.1%)of neonatal deaths. Furthermore, neonatal sepsis and infections were the third causes of a visit to the neonatal ICU, accounting for 919(29.7%) and 129(4.2%) neonatal admissions and deaths, respectively (Table 3).
Table 3.
Aggregated categories of causes of admission and death by outcomes among neonates admitted to Neonatal ICU of JUMC
| Categoriesa | Outcomes at discharge | Total | |
|---|---|---|---|
| Death | Improved | ||
| No(%) | No(%) | No(%) | |
| All causes | 412(13.3) | 2681(86.7) | 3093(100) |
| Birth asphyxia & other perinatal complications | 138(4.5) | 1350(43.6) | 1488(48.1) |
| Low birth weight | 249(8.1) | 859(27.8) | 1108(35.8) |
| Neonatal sepsis and infections | 129(4.2) | 790(25.5) | 919(29.7) |
| Preterm birth complications | 222(7.2) | 561(18.1) | 783(25.3) |
| Other neonatal conditions | 87(2.8) | 481(15.6) | 568(18.4) |
Note: aOne neonate can be categorized in more than one categories
Top causes of neonatal admission and death
All available admission diagnoses were extracted to evaluate the proportional cause of admission and death among neonates., Low birth weight, neonatal sepsis, and hypothermia were the top three conditions that accounted for 1108(35.8%), 884(28.6%), and 809(26.2%) of neonatal ICU admissions, respectively. Furthermore, 157(5.1%), 112(3.6%), and 86(2%) of the neonates were admitted due to meningitis, sub-glial haemorrhage, and macrosomia, respectively (Table 4).
Table 4.
Top ten leading causes of admissions and mortalities among neonates admitted to JUMC
| Ranks | Causes of admission (n=3093) | No(%) | Ranks | Causes of death (n=412) | No(%) |
|---|---|---|---|---|---|
| 1 | Low birth weight | 1108(35.8) | 1 | Low birth weight | 249(60.4) |
| 2 | Neonatal Sepsis | 884(28.6) | 2 | Prematurity | 230(55.8) |
| 3 | Hypothermia | 809(26.2) | 3 | RDS | 169(41.0) |
| 4 | Hypoglycemia | 548(17.7) | 4 | Neonatal sepsis | 129(31.3) |
| 5 | RDS | 413(13.4) | 5 | Hypothermia | 120(29.1) |
| 6 | PNA | 286(9.2) | 6 | PNA and birth trauma | 108(26.2) |
| 7 | Baby of a high-risk mother | 172(5.6) | 7 | MAS | 53(12.9) |
| 8 | Meningitis | 157(5.1) | 8 | Hypoglycemia | 49(11.9) |
| 9 | Sub-glial Hemorrhage | 112(3.6) | 9 | Congenital malformation | 33(8.0) |
| 10 | Macrosomia | 86(2) | 10 | Pathologic Jaundice | 31(7.5) |
Abbreviations: RDS, respiratory distress syndrome; MAS, meconium aspiration syndrome; PNA, perinatal asphyxia; JUMC, Jimma University Medical Center.
With respect to the top ten leading causes of deaths, out of 1,108 neonates admitted with Low birth weight, 249(60.4%) died. Among premature neonates,230(55. %)of them died. Total neonates with sepsis were 884 and 129(31.3%) died. Hypothermia accounted for 809 (28.6%) admissions and169(41%) deaths. Moreover, Respiratory Distress Syndrome (RDS), 169(41.0%) was the fourth ranked cause observed among the deceased neonates; whereas hypoglycaemia, 49(11.9%), congenital malformations 33(8%), and pathologic jaundice, 31(7.5%) were the least ranked three conditions respectively (Table 4).
Multivariate analysis of socio demographic characteristics of neonate admitted to the NICU of JUMC
Using Multivariate analysis, to test the association of socio demographic variables with neonatal mortalities, four variables were found to be significantly associated with neonatal death. These variables were address of parents, the length of stay, gestational ages, and birth weight and maturity levels. neonates who came from addresses outside the city had a 1.89 times higher increased risk of mortality (AOR 1.89, 95% CI1.4–2.5) compared to their counterparts resident in the city. Neonates who stayed for less than one week in the NICU had 3.9 fold higher odds of neonatal mortality (AOR 3.9, 95%CI2.8–5.50), compared to those who stayed for more than one week. The risk of mortality decreased as the gestational age increased. The highest risk was observed in those neonates delivered before 28 weeks of gestation (AOR 19.2, 95%CI 3.9–90.9). The same was true for the birth weight; the risk of mortality decreased as the birth weight increased and the highest risk was seen in a neonate who had birth weight less 1,000 g (AOR 44.8, 9%CI9.43–200). The odds of neonatal death in preterm birth was two times higher compared to term births as shown in Table 5.
Table 5.
Multivariate analysis of socio demographic characteristics of neonate admitted to the NICU of JUMC
| Variables | Died | Survived | COR(CI,95) | AOR(CI,95) | P-value | |
|---|---|---|---|---|---|---|
| No(%) | No(%) | |||||
| Sex | Male | 236(7.6) | 1601(51.8) | 1 | 1 | |
| Female | 176(5.7) | 1080(34.9) | 1.11(0.90, 1.36) | 0.99(0.78, 1.26) | 0.934 | |
| Age | <24 hrs | 337(10.9) | 2011(65.0) | 1.26(0.74, 2.15) | 0.62(0.35, 1.10) | 0.101 |
| 2–7 days | 59(1.9) | 550(17.8) | 0.80(0.45, 1.45) | 0.58(0.31, 1.07) | 0.081 | |
| ≥8 days | 16(0.5) | 120(3.9) | 1 | 1 | ||
| Address | Out of Jimma | 326(10.5) | 1809(58.5) | 1.83(1.422, 2.35) | 1.89(1.43, 2.51) | |
| From Jimma | 86(2.8) | 872(28.2) | 1 | 1 | 0.000 | |
| Length of stay | <7 Days | 346(11.2) | 1885(60.9) | 2.21(1.68, 2.92) | 3.93(2.82, 5.50) | |
| >7 Days | 66(2.1) | 796(25.7) | 1 | 1 | 0.000 | |
| Gestational age | <28 weeks | 23(0.7) | 2(0.1) | 129.7(30.3, 554.3) | 19.16(3.9, 90.9) | 0.000 |
| >42 weeks | 1(0.0) | 6(0.2) | 1.88(0.23, 15.70) | 3.58(0.39, 33.3) | 0.260 | |
| 28 - <32 weeks | 93(3.0) | 126(4.1) | 8.33(6.12, 11.33) | 3.06(1.79, 5.26) | 0.000 | |
| 32 - <37 weeks | 114(3.7) | 506(16.4) | 2.54(1.97, 3.27) | 1.89(1.23, 2.92) | 0.004 | |
| 37 - <42 weeks | 181(5.9) | 2041(66.0) | 1 | 1 | ||
| Birth weight | <1,000 g | 27(0.9) | 2(0.1) | 142.8(33.7, 606) | 44.84(9.43, 200) | 0.000 |
| <2,500 g | 98(3.2) | 745(24.1) | 1.39(1.07, 1.81) | 0.88(0.59, 1.33) | 0.541 | |
| >4,000 g | 2(0.1) | 119(3.9) | 0.18(0.04, 0.73) | 0.16(0.04, 0.66) | 0.011 | |
| 2,500–4,000 g | 161(5.2) | 1703(55.1) | 1 | 1 | ||
| <1,500 g | 124(4.0) | 112(3.6) | 11.71(8.66, 15.85) | 6.87(4.05, 11.6) | 0.000 | |
| Maturity | Preterm | 230(7.4) | 634(20.5) | 4.08(3.30, 5.05) | 2.11(1.39, 3.23) | |
| Term | 182(5.9) | 2047(66.2) | 1 | 1 | 0.001 | |
Note: Preterm: those who delivered before 37 weeks of Gestation, Term:those delivered at above 37 weeks of gestation.
Multivariate and univariate analysis of factors associated with neonatal mortalities
Univariate logistic regression analysis was performed separately for each neonatal condition and any risk factors that showed significant association (P<0.25) with the outcome were selected for multivariate analysis. While testing the association of causes of neonatal admissions with the neonatal mortality using binary logistic regressions seven variables were significantly associated with neonatal mortalities. Neonatal sepsis, hypothermia and meconium aspiration syndrome(MAS) were not significantly associated with mortality in univariate analysis. In multivariate analysis, only five variables were found to be the significant predictors of the neonatal mortalities. The odds of neonatal mortalities among preterm neonates were 2.2 times higher than that of term neonates (AOR 2.2, 95%CI 1.41, 3.42). Neonates who had a history of birth asphyxia had five fold higher odds of death (AOR4.9, 95%CI 3.6, 7.34) and low birth weight had 1.54 times increased risk of mortality (AOR 1.54, 95%CI 1.06, 2.25). The odds of death among newborns who had a history of congenital malformations and RDS were four times that of neonates who did not have the conditions (AOR 4, 95%CI 2.55–2.68) and (AOR 4.15,95%CI 2.9–5.66) respectively (Table 6).
Table 6.
Multivariate and Univariate analysis of factors associated with Neonatal mortalities among neonate admitted to JUMC
| Variables | Died | Survived | COR(CI,95) | AOR(CI,95) | P-value | |
|---|---|---|---|---|---|---|
| No(%) | No(%) | |||||
| Prematurity | Yes | 230(7.4) | 634(20.5) | 4(3.29,5.05) | 2.2(1.41,3.42) | 0.000 |
| No | 182(5.9) | 2047(66.2) | 1 | 1 | ||
| Neonatal sepsis and Infection | Yes | 129(4.2) | 790(25.5) | 1.1 (0.87,1.36) | ||
| No | 283(9.1) | 1891(61.1) | 1 | |||
| Birth asphyxia and birth trauma | Yes | 108(3.5) | 348(11.3) | 2.4(1.86,3.04) | 4.95(3.6,7.34) | 0.000 |
| No | 304(9.8) | 2333(75.4) | 1 | 1 | ||
| Low birth weight | Yes | 249(8.1) | 859(27.8) | 3.24(2.6,4.01) | 1.54(1.06,2.25) | 0.025 |
| No | 163(5.3) | 1822(58.9) | 1 | 1 | ||
| Hypothermia | Yes | 120(3.9) | 689(22.3) | 1.2(0.94,1.49) | 0.97(0.74–1.27) | 0.816 |
| No | 292(9.4) | 1992(64.4) | 1 | 1 | ||
| Hypoglycemia | Yes | 49(1.6) | 499(16.1) | 0.59(0.43,0.80) | 0.81(0.57–1.15) | 0.231 |
| No | 363(11.7) | 2182(70.5) | 1 | 1 | ||
| Congenital malformation | Yes | 33(1.1) | 122(3.9) | 1.8(1.23,2.7) | 4(2.55–2.68) | 0.000 |
| No | 379(12.3) | 2559(82.7) | 1 | 1 | ||
| MAS | Yes | 53(1.7) | 322(10.4) | 1.1(0.79,1.48) | ||
| No | 359(11.6) | 2359(76.3) | 1 | |||
| Pathologic Jaundice | Yes | 31(1.0) | 300(9.7) | 0.65(0.44–0.95) | 0.82(0.54–1.25) | 0.357 |
| No | 381(12.3) | 2381(77) | 1 | |||
| RDS | Yes | 169(5.5) | 252(8.1) | 6.7(5.29–8.48) | 4.15(2.9–5.66) | 0.000 |
| No | 243(7.9) | 2429(78.5) | 1 | |||
| Others conditions | Yes | 54(1.7) | 359(11.6) | 0.98(0.72–1.32) | ||
| No | 358(11.6) | 2322(75.1) | 1 | |||
Abbreviations: RDS, respiratory distress syndrome; MAS, meconium aspiration syndromes; JUMC, Jimma University Medical Center.
Discussion
According to the Ethiopian demographic health survey (EDHS) 2016, in Ethiopia 1 in every 35 children dies within the first month of birth.5 The present study assessed causes and factors associated with neonatal mortality among neonates admitted to NICU of Jimma University Medical Center.
The present study reported that low birth weight 35.8%, neonatal sepsis 28.6% and hypothermia 26.2% were found to be the three predominant causes of neonatal admissions. The proportions of these causes of admission vary across different studies conducted in Ethiopia.8–11 Similar to this study neonatal sepsis and low birth weight were found to be within the top three leading causes of neonatal admissions in other several studies conducted outside Ethiopia.12–17 This implies that major causes of neonatal admissions were attributed to avoidable and curable neonatal conditions and would be preventable if detected early and proper care were in place.
In the present study, the overall neonatal mortality rate was 12.6% (30 deaths per 1,000 live births). This finding is inconsistent with several studies carried out in different parts of Ethiopia. The current finding is slightly lower than the studies conducted in northwestern parts of Ethiopian and significantly lower than the study carried out in Addis Ababa which was 14.3%, 15.9%, and 23.2% respectively. Similarly, the finding in this study is significantly lower than the neonatal mortality rate reported by WHO in 2018 which is 40% and also lower compared to studies conducted in Eritrea 8.2%, Pakistan 6.8%, South Africa 3.8% and India 7.16%. Commonly, the mortality rates of the newborn in NICU fluctuate between 3.1% and 29% in the world.8,11–20–22 The discrepancy observed between the mortality rates estimated by several centers and countries might be due to the difference in the distribution of skilled human resources, quality of care delivered by the centers, equipment availability, and socioeconomic status, as well as geographical locations.
The major causes of neonatal mortality in the current study were low birth weight 8%, prematurity, 7.4%, RDS 5.4%. Case fatality for neonatal sepsis was 4.2%. The similar causes of neonatal mortalities were reported in several studies conducted in other centers and countries.8–11,15,16,23–27 Most of the neonatal problems would be avoidable if proper antenatal care implementation and on time linkage of high risk pregnant women to health institutions were in place,28 This implies that antenatal care services in the area were not satisfactory in anticipating and linking high risk pregnant women to health institutions where an appropriate neonatal care service was available.
In multivariate analysis of neonatal conditions prematurity, low birth weight, birth asphyxia, congenital malformations and respiratory distress syndrome were identified as predictors of neonatal mortalities. Similarly significant associations have been observed in a study conducted in Gondar, Addis Ababa, Iran, Brazil and other several studies.8,9,24,26,29–32 These indicated that most of the neonatal deaths are due to preventable causes of death that could be addressed by anticipating risky pregnancies and the provision of proper and on time interventions.
Furthermore, the multivariate analysis of socio demographic factors has also found that those neonates who came from centers outside the city had increased risk of mortality. This is comparable with a similar finding from another study carried out in our country.26 This may be related to delay in making a decision to seek care and delay in reaching care due to the availability of and cost of transportations which would affect the on time arrival of laboring mothers to the hospitals and lack of pre hospital emergency care. Since most mothers and newborns are referred to the center after they had already developed complications, this could contribute significantly to loss of life during neonatal periods.
Our finding in the present study also indicated that neonatal mortality was also related to the length of hospital stay, gestational age and birth weights of the newborn. This finding is in line with other studies.33,34 The lower the gestational and birth weight the higher chance of death and this is due to the fact that underweight and preterm newborn had immaturity of immune systems and other body defense mechanisms which control newborn disease susceptibility.1 This implies that anticipating high risk newborn babies and early treatment would reduce the deaths of such physiologically and anatomically vulnerable neonates. Other possible explanations for this might also be due to delay in receiving adequate health care due to poor facilities and lack of medical supplies in low income countries.
The strengths of this study include the fact that it used large sample sizes and statistical analyses appropriate to the study design and with the results matching the method described. Limitations include the use of medical records of newborns and since the study is institutionally based, the results might lack generalizability to the entire population in the catchment area. This study was mainly focused on neonatal factors that could be related to neonatal mortalities, for this reason other possible factors not adjusted for during the current study may influence observed associations. In all cross-sectional studies, we can infer association but not causation from our results.
In conclusion, this study found that babies born outside the city, gestational ages, the length of stay in the ICU, prematurity, low birth weight, RDS, and congenital malformations all had a significant association with neonatal mortality. Therefore, it is recommended that early detection and anticipating high risk pregnancies and high-risk newborns and provision of timely and appropriate intervention could reduce neonatal mortalities. Furthermore, it is important that further community based interventional studies be conducted on a larger scale to broaden the understanding obtained from this initial study.
Acknowledgments
Professor Gillian Murphy, Emeritus Professor senior visitor, Departments of Oncology, University of Cambridge, CRUK Cambridge Institute.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kliegman RM, Stanton BF. St Geme S. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016:794–825. [Google Scholar]
- 2.UNICEF, WHO, World Bank Group, Nations U. Levels and Trends in Child Mortality: Report 2018. New York: UNICEF; 2018. [Google Scholar]
- 3.Assamala. African Regional Health Report 2014 [Internet]. World Health Organisation; 2014. Available from: http://www.who.int/intellectualproperty/documents/thereport/ENPublicHealthReport.pdf. [Google Scholar]
- 4.Okechukwu AA, Achonwa A. Morbidity and mortality patterns of admissions into the special care baby unit of university of abuja teaching hospital, Gwagwalada, Nigeria. Niger J Clin Pract. 2009;12:389–394. [PubMed] [Google Scholar]
- 5.DHS Program. Ethiopia Demographic and Health Survey – 2016. Rockville (MD): ICF; 2016. [Google Scholar]
- 6.Liu L, Mathers C, Oza S, et al. MCEE-WHO methods and data sources for child causes of death 2000-2015. World Health Organization [Internet]. Available from: http://www.who.int/healthinfo/global_burden_disease/en/ Accessed February1, 2016.
- 7.Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A. Neonatal mortality in Ethiopia: trends and determinants.. BMC Public Health. 2013;13(1):1. doi: 10.1186/1471-2458-13-483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital, Northwest Ethiopia [Internet]. Pediatric Health Med Ther. 2017;8:57–64. Available from: https://www.dovepress.com/patterns-of-admission-and-factors-associated-with-neonatal-mortality-a-peer-reviewed-article-PHMT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mengesha HG, Sahle BW. Cause of neonatal deaths in Northern Ethiopia: a prospective cohort study.. BMC Public Health. 2017;1–8. doi: 10.1186/s12889-016-3979-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tekleab AM, Amaru GMTY. Reasons for admission and neonatal outcome in the neonatal care unit of a tertiary care hospital in Addis Ababa: a prospective study. Res Rep Neonatol. 2016;201:17–23. doi: 10.2147/RRN.S95455 [DOI] [Google Scholar]
- 11.Sime H, Workneh N, Girma E. Morbidity and Mortality of Neonates Admitted in Jimma University Specialized Hospital Paediatrics Neonatal Ward: A One Year Retrospective Analysis. Ethiopian Journal of Pediatrics and Child Health. 2014;10(10):44–54. [Google Scholar]
- 12.Okposio MM, Ighosewe OI. Morbidity and mortality pattern among neonates admitted to the general paediatric ward of a secondary health care centre in the Niger delta region of Nigeria. Sri Lanka J Child Health. 2016;45(2):84–89. doi: 10.4038/sljch.v45i2.7981 [DOI] [Google Scholar]
- 13.Saini N, Chhabra S, Chhabra S, Garg L, Garg N. Pattern of neonatal morbidity and mortality: a prospective study in a District Hospital in Urban India [Internet]. J Clin Neonatol. 2016;5(3):183 Available from:: http://www.jcnonweb.com/text.asp?2016/5/3/183/191258. [Google Scholar]
- 14.Pal A, Batra S, Kaur J. A study of neonatal admission pattern and outcome from rural Haryana. A Study of Neonatal Admission Pattern and Outcome from Rural Haryana. Glob J Res Anal. 2018;7(February):73–75. [Google Scholar]
- 15.Ranjan A, Singh A. Pattern of morbidity and mortality of neonates admitted in tertiary level neonatal intensive care unit in Nalanda Medical College and Hospital, Patna, Bihar, India. Int J Contemp Pediatr. 2016;3(3):854–857. Available from: http://www.ijpediatrics.com. [Google Scholar]
- 16.Yasmeen S, Ahmad K, Waheed I, Gul R. Spectrum of neonatal admissions and their outcome in a tertiary Care hospital. Pak Armed Forces Med J. 2017;67(6):1044–1049. [Google Scholar]
- 17.Shahidullah M, Hasan MZ, Jahan I, Ahmed F, Chandra A. Perinatal characteristics and outcome of Neonates at NICU of a tertiary level hospital in Bangladesh. Bangladesh J Child Health. 2017;41(1):34–39. doi: 10.3329/bjch.v41i1.33634 [DOI] [Google Scholar]
- 18.Chow S, Chow R, Popovic M, et al. A selected review of the mortality rates of Neonatal Intensive Care Units [Internet]. Front Public Health. 2015;3(October). Available from: http://journal.frontiersin.org/Article/10.3389/fpubh.2015.00225/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.P V S, Thammanna PS, Sandeep M. Morbidity pattern and hospital outcome of neonates admitted in a tertiary care teaching hospital, Mandya. Int J Sci Study. 2015;3(6):3–6. [Google Scholar]
- 20.Shah S, Zemichael O, Meng HD. Factors associated with mortality and length of stay in hospitalised neonates in Eritrea, Africa: a cross-sectional study. BMJ Open. 2012;2(5):1–9. doi: 10.1136/bmjopen-2011-000792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ali SR, Hospital I, Ahmed S, Lohana H. Disease patterns and outcomes of neonatal admissions at a secondary care hospital in Pakistan. Sultan Qaboos University Med J. 2013;13(3):424–428. [PMC free article] [PubMed] [Google Scholar]
- 22.UNICEF. IGME Child Mortality Estimates:2018. New York: UNICEF ;2018. [Google Scholar]
- 23.Pepler PT, Uys DW, Nel DG. Predicting mortality and length-of-stay for neonatal admissions to private hospital neonatal intensive care units: a Southern African retrospective study. Afr Health Sci. 2012;12(2):166–173. doi: 10.4314/ahs.v12i2.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Demitto MDO, Gravena AAF, Dell’Agnolo CM, Antunes MB, Pelloso SM. High risk pregnancies and factors associated with neonatal death. Rev Esc Enferm. 2017;51:1–7. [DOI] [PubMed] [Google Scholar]
- 25.Walana W, Ks AE, Naafu B, et al. Health pattern, causes and treatment outcomes of neonatal admission in the tamale teaching hospital. Clin Mother Child. 2016;13:4. [Google Scholar]
- 26.Worku B, Kassie A, Mekasha A, Tilahun B, Worku A. predictors of early neonatal mortality at a neonatal intensive care unit of a specialized referal teaching hospita in Ethiopia. Ethiop J Health Dev. 2012;26(3):200–207. [Google Scholar]
- 27.Gaiva MAM, Fujimori E, Sato APS. Maternal and Child Risk Factors Associated With Neonatal Mortality. Texto Contexto - Enferm. 2016;25(4):2–9. doi: 10.1590/0104-07072016002290015 [DOI] [Google Scholar]
- 28.Cunningham FG, Leveno KJ, Bloom SL, Bloom SL, Hauth JC, Larry Gilstrap III KDW. Section V. Fetus and Newborn: chapter 29; Diseases and Injuries of the Fetus and Newborn In: Williams_Obstetrics_-22_Edition [Internet]. 22nd ed. McGrew-Hill’s; 2007. Available from: http://mk:@MSITStore:E:%5Cneonatology%5Cwilliams_obstetrics_-22_edition—2005-0071413154-mcgraw-. [Google Scholar]
- 29.Ansari-Moghaddam A, Sadeghi-Bojd S, Imani M, Movahedinia S, Pourrashidi A, Mohammadi M. A multivariate analysis of factors associated with infant mortality in South-East of Iran. J Pak Med Assoc. 2014;64(10):1123–1126. [PubMed] [Google Scholar]
- 30.Sabzehei MK, Basiri B, Shokouhi M, Eghbalian F. Causes and risk factors associated to neonatal mortality in Neonatal Intensive Care Unit (NICU) in Besat Hospital Hamadan-Iran in 2015 to 2016. Int J Pediatr. 2018;6(9):8185–8194. [Google Scholar]
- 31.Emília M, Claudia A, Dalva M, et al. Factors associated with hospitalization during neonatal period. J Pediatr [Internet]. 2018;94(4):390–398. Sociedade Brasileira de Pediatria;. doi: 10.1016/j.jped.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 32.Kousar T, Memon Y, Sheikh S, Memon S, Sehto R. Risk factors and causes of death in Neonates. Rawal Med J. 2010;35(2):205–208. [Google Scholar]
- 33.Overman DM. Neonatal outcomes and length of stay: a firm grasp of the obvious? [Internet]. J Thorac Cardiovasc Surg. Elsevier; 2015;152(3):727–728. doi: 10.1016/j.jtcvs.2016.05.061 [DOI] [PubMed] [Google Scholar]
- 34.Berry MA, Shah PS, Brouillette RT, Hellmann J. Predictors of mortality and length of stay for neonates admitted to children’s hospital neonatal intensive care units. J Perinatol. 2008;28(4):297–302. doi: 10.1038/sj.jp.7211904 [DOI] [PubMed] [Google Scholar]
- 35.IHME, Global Burden of Disease Study. Population Estimates 1950-2017, report 2017. 2017. Available from: http://ghdx.healthdata.org/record/global-burden-disease-study-2017-gbd-2017-population-estimates-1950-2017.
- 36.FMOH. National strategy for newborn and child survival in Ethiopia: 2015/16-2019/20.2015.