Abstract
Background: To better understand the structural drivers of women living with HIV’s reproductive rights and choices, this study examined the structural correlates, including non-consensual HIV disclosure, on WLWH’s pregnancy decisions and describes access to preconception care. Analyses drew on data (2014-present) from SHAWNA, a longitudinal community-based cohort with WLWH across Metro-Vancouver, Canada. Multivariable logistic regression was used to model the effect of non-consensual HIV disclosure on WLWH’s pregnancy decisions. Of 218 included in the analysis, 24.8% had felt discouraged from becoming pregnant and 11.5% reported accessing preconception counseling. In multivariable analyses, non-consensual HIV disclosure was positively associated with feeling discouraged from wanting to become pregnant (AOR: 3.76; 95%CI 1.82–7.80). Non-consensual HIV disclosure adversely affects WLWH’s pregnancy decisions. Supporting the reproductive rights of WLWH will require further training among general practitioners on reproductive health of WLWH and improved access to women-centred, trauma-informed care, including non-judgmental preconception counseling.
Keywords: HIV, pregnancy, stigma, reproductive health, preconception counseling
INTRODUCTION
With the advent of antiretroviral therapy (ART), and resulting improvements in life expectancy(1, 2), health and quality of life(3), and prevention of sexual and vertical HIV transmission(4, 5), an increasing number of women living with HIV (WLWH) are considering their reproductive options(6, 7). Globally, there has been a steady increase in the proportion of WLWH desiring children(6, 8–12). For example, a US-based study reported a 150% increase in fertility desires among American WLWH after the introduction of ART(7). Similarly, Canada has seen a steady growth in the proportion of WLWH conceiving(13), with fertility desires and pregnancy decisions approaching that of the general population of Canadian women in some settings(14).
There are a growing number of both qualitative and empirical studies examining the fertility desires and intentions among WLWH globally. Existing studies have largely reported on individual and interpersonal factors shaping fertility desires/pregnancy intentions(6), many of which are similar to those of women not living with HIV. Such factors include: younger age(8, 9, 14), lower education(9), parity(10, 15, 16), marital status(10, 16), partners’ fertility desires(6) and ethnicity(11). HIV-specific individual and interpersonal factors, such as HIV serostatus disclosure(17), and taking ART(16) are also documented to increase WLWH’s pregnancy intentions. In Ontario, Canada, a 2009 study among WLWH reported that 69% of WLWH desired to give birth and 57% had positive pregnancy intentions, with place of birth, ethnicity, younger age and number of lifetime births predicting fertility decisions(11). Similarly, a 2007 study amongst WLWH in the Canadian province of British Columbia documented fertility intentions approaching that of the general population; 25.8% of WLWH intended to become pregnant compared to 37.5% in the general population(14). In this study, rates of fertility intentions were higher among WLWH who were younger, non-Indigenous and had a regular partner(14). Understanding the pregnancy decisions of Indigenous WLWH in British Columbia are important given that Indigenous WLWH in Canada remain disproportionately affected by HIV(18). Indigenous women in Canada have higher fertility rates compared to their non-Indigenous counterparts, and often experience additional barriers to health care, including due to systemic racism, stigma and a lack of culturally safe services (19, 20). This is particularly important to explore in our sample of WLWH, over half (55%) of whom are Indigenous.
Only a handful of studies have examined the role of structural barriers on WLWHs’ pregnancy decisions. Of these largely qualitative studies, society and cultural influences (e.g., societal and family pressure for childbearing)(17, 21), and health worker attitudes(22) have been found to influence fertility desires. HIV stigma, fear of HIV disclosure to family members and health care providers have been highlighted as a major concern for WLWH in the perinatal period, and found to deter women from accessing perinatal care(23–26). Similarly, there are qualitative research to suggest that HIV stigma and discrimination strongly undermines WLWH’s access to a variety of PMTCT services(23). Our literature review identified only one empirical study that documented the (negative) influence of HIV stigma on WLWHs’ pregnancy intentions in the United States(27). Despite the potential detrimental influence of stigma on WLWHs’ reproductive decisions and health access, two recent systematic and literature reviews on stigma and fertility desires/intentions identified gaps in empirical research on the impact of structural drivers, including stigma(28), on WLWHs’ pregnancy decisions(6). The role of stigma and discrimination on WLWH’s reproductive choices are particularly pertinent in criminalized settings, where HIV non-disclosure before a sexual encounter can potentially result in an aggravated sexual assault conviction. At odds with Canada’s reputation for liberal policies, Canada is a world-leader in the enforcement of HIV non-disclosure laws(29). The aggressive enforcement of these laws against PLWH are postulated to fuel HIV stigma (from the public and health care providers), and compromise engagement in critical HIV and health care services; (30) however, there is currently a dearth of empirical research, including in the Canadian context, on the relationship of criminalization, stigma and access to care.
To address the impacts of traumatic experiences (e.g., intimate partner violence, traumatic events of stigma/discrimination) there have been increasing calls for trauma-informed approaches to care, including as part of HIV care(31–33) and perinatal care(34, 35). Trauma-informed care approaches recognize and respond to the impacts of traumatic events and embrace the core principles of trauma-informed care: trustworthiness, safety, peer-support, collaboration, empowerment, and respect for cultural/historic and gender issues in care(36).
Given increases in the number of WLWH of reproductive age in Canada who desire pregnancy(37) and recent evidence that half of WLWH reporting having their HIV status disclosed without their consent(38) there is a clear need to better understand the contextual factors that serve as barriers or enabling environments for WLWH’s reproductive choices and care access. In light of the dearth of empirical studies examining the structural determinants of fertility decisions, this study sought to examine the structural factors (including non-consensual HIV disclosure), which encourage or discourage WLWH’s pregnancy decisions. Additionally, given the potential role of conception-focused discussions in shaping the perceptions and decisions around pregnancy, this study also aimed to describe access to preconception services among WLWH in Vancouver.
METHODS
Community-Based Research Cohort (SHAWNA)
Data for this study were drawn from a community-based, open prospective cohort, Sexual Health and HIV/AIDS: Women’s Longitudinal Needs Assessment (SHAWNA). SHAWNA is a partnership of more than 20 women’s HIV and community service providers, guided by two advisory boards: a Community Stakeholder Advisory Board and a Positive Women’s Advisory Board of 12–15 WLWH from Metro-Vancouver. After 6 months of extensive consultations with WLWH, HIV care providers and policy experts, the SHAWNA project was launched in 2014 with the aim to longitudinally assess community-identified needs including the social, policy, legal, gender and geographical gaps in sexual health and HIV care among women living with HIV (WLWH) in Metro Vancouver. The study also aims to evaluate the impact of various care models on subgroups of marginalized women, including Indigenous women, migrant/refugee women, as well as gender and sexual minorities.
Beginning in 2014, SHAWNA began recruiting WLWH (trans-inclusive), aged 14 and older, who live in and/or access services in Metro Vancouver. Participants are recruited via outreach by Peer Research Associates (PRAs) of WLWH and community partners including: self-referrals and referrals from HIV care providers, peer navigators, HIV/AIDS organizations and clinical outreach. This includes a close collaboration with British Columbia’s primary referral centre for WLWH (Oak Tree clinic, BC Women’s hospital). Study participants are offered the opportunity to interview at one of two community research offices, or a safe and discreet location of their choice. At enrolment and every six months thereafter, WLWH complete a questionnaire administered by our trained community/ PRAs, eliciting a wide range of topics including: individual, biological and behavioural variables, such as: age, sexual orientation, ethnicity, fertility variables, and clinical HIV measurements (e.g., adherence, viral load, CD4 count). Social and structural variables include experiences of gender-based violence.
Experiences of physical, mental, and sexual and reproductive health (SRH), navigating SRH services, including experiences of stigma, and access to HIV care, are asked by a sexual health research nurse, along with viral load/CD4 monitoring and sexually transmitted infections/ Hepatitis C virus (STI/HCV) serology, to facilitate support, education and referral. If needed, project nurses offer onsite treatment for symptomatic STIs, free serology and cervical cancer screening (regardless of enrollment in the study), and facilitate education support and referrals. At each visit, participants receive $50 Canadian remuneration for their time, expertise and travel. The study holds ethical approval through Providence Health Care/University of British Columbia Research Ethics Board and BC Women’s Hospital,
Primary outcome:
The primary outcome, was based on the question “Has your HIV diagnosis affected your decision to become pregnant or to not become pregnant?”. The index category, ever felt discouraged from wanting to become pregnant due to one’s HIV diagnosis, was defined based on a response of “Yes, my HIV status discouraged me from wanting to become pregnant”. The reference category combined the following responses: “Yes, my HIV diagnosis encouraged me to want to become pregnant” or “No, it has not affected me”.
Explanatory variables:
Independent variables were selected based on their a priori known or hypothesized relationship with fertility decisions. Individual variables included: Age and age of HIV diagnosis, and duration of known HIV infection (measured continuously, in years); sexual orientation (i.e., identifying as gay, lesbian, bisexual, asexual or two-spirit at baseline); Indigeneity (First Nations, Métis or Inuit), Im/migrant status (born outside of Canada); Education (defined as high-school graduate vs. less than high school). In addition to our outcome, we included ever had a live birth (yes versus no), and currently desire pregnancy (yes versus no) as a relevant fertility-related variable. The following interpersonal variables were also examined: having an intimate male partner, ever experienced physical/sexual violence, and HIV disclosure at diagnosis (all defined as yes versus no). Among the structural factors collected, health services access variables included ever accessing preconception counseling or women-specific care. To quantify the impact of stigma, we assessed the role of HIV disclosure without consent, based on the question “Has anyone ever ‘outed’ you for knowing or suspecting you were HIV positive” (yes versus no). Examples of individuals who were responsible for disclosing without consent include: housing staff or residents, HIV outreach, jail/prison staff, police, intimate partners, friends. Verbal or physical abuse due to one’s HIV diagnosis (ever versus never to both stigma variables) was used as another proxy measure for stigma.
Statistical Analyses:
The analytic sample was restricted to baseline data of cis-gender women who were of reproductive age (15–49 years) at the time of their HIV diagnosis. Descriptive statistics calculated included frequencies and proportions for categorical variables, and measures of central tendencies (i.e., mean, medians and interquartile ranges (IQR)) for continuous data. Our analysis was guided by the reproductive justice framework, which merges elements of social justice and reproductive rights to acknowledge numerous structural barriers/ ‘oppressions’, such as poverty, stigma, discriminatory laws and race, that can shape women’s reproductive choices(39). The reproductive justice framework posits that all women and girls have the right to enabling environments that support their reproductive rights, including their right to have children, prevent pregnancies and access essential sexual and reproductive health care(39). Aligned with the reproductive justice framework, bivariate analyses were conducted to determine the independent associations of individual, social and structural factors with ever feeling discouraged from wanting to become pregnant because of one’s HIV diagnosis. Pearson’s chi-squared tests (or Fisher’s exact test for small cell counts) were used for categorical variables and Wilcoxon rank-sum test for continuous variables. To measure the strength of association between explanatory variables and the outcome, Odds Ratios (ORs) with 95% Confidence Intervals (CIs) were calculated. As in previous studies(40, 41), a conservative p- value- cutoff of <0.10 was used to consider a priori hypothesized explanatory variables for inclusion in the multivariable model. We began with a full model that included all variables with a p-value of <0.10 in bivariate analysis. A backward stepwise approach was then used to construct the final multivariable model. This began with the full model and included the sequential removal of variables starting with the highest p-value (indicating the least statistical significance) and an assessment of the Akaike’s Information Criteria (AIC) value with the removal of each variable. The AIC value indicates the combination of variables that best explain the variability in the outcome. The final model presented in our paper is the model with the lowest associated AIC value. This model building procedure has been justified elsewhere(42). The final model was tested for multicollinearity. All p-values are two-sided, and SAS software version 9.4 was used for all statistical analyses (SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
Of the 218 cisgender WLWH of reproductive age at diagnosis included in the study, almost one quarter (n=54, 24.8%) reported that their HIV diagnosis made them feel discouraged them from wanting to become pregnant and over half (n=114, 52.3%) had experienced HIV disclosure without consent. As displayed in Table 1, the majority of our participants in our sample were Indigenous (55.1%), 36.2% white and 8.3% were African/Caribbean/Black/Other, with no significant differences in feeling discouraged from wanting to become pregnant between these groups. The median age at HIV diagnosis was 30.9 (24.0–36.5) and the median duration of infection was 14.2 years (Interquartile range (IQR): 8.1–20.0); neither were significantly associated with feeling discourage from wanting to become pregnant in bivariate analysis. While 76.6% had ever had a live birth, only 11.5% had ever reported receiving preconception counseling. Among those who ever received preconception counseling, the majority received these from women-specific HIV care providers (Oak Tree Clinic or the Women’s Health Collective) (64%), followed by general practitioners/public health nurses (24%) and HIV specialists (12%) (See Figure 1). Half (50.0%) of our sample had accessed women-specific HIV care. Table 2 details the information participants reported receiving in preconception counseling sessions.
Table 1 .
Sample characteristics for the associations between individual, interpersonal and structural factors and ever felt discouraged from wanting to become pregnant, among 218 WLWH of reproductive age at diagnosis, in SHAWNA cohort in Metro Vancouver, Canada (2014‒2016).
| Variable |
Total sample (n = 218) |
Felt discouraged from wanting to become pregnant due to HIV status |
|
|---|---|---|---|
| Yes 54 ( 24.8%) | No 164 (75. 2 %) | ||
| INDIVIDUAL AND BEHAVIOURAL FACTORS | |||
| Age at diagnosis | 30.9 (24.0‒36.5) | 30.0 (25.0‒35.0) | 31.0 (24.0‒37.0) |
| Age at baseline | 45.0 (38.0‒52.0) | 44.0 (37.9‒52.6) | 45.0 (38.4‒52.0) |
| Duration of known HIV infection ( years) | 14.2 (8.10‒20.0) | 15.5 (6.4‒20.7) | 14.0 (8.3‒19.7) |
| Sexual orientation | |||
| Gay, lesbian, bisexual, asexual, two-spirit | 55 (25.2) | 20 (36.3) | 35 (63.6) |
| Straight | 163 (74.8) | 34 (20.9) | 129 (79.1) |
| Married or common-law partner | 47 (21.6) | 9 (19.1) | 38 (80.9) |
| Not in a married or common-law relationship | 171 (78.4) | 45 (26.3) | 126 (73.7) |
| Indigenous*+ | 120 (55.1) | 27 (22.5) | 93 (77.5) |
| White | 79 (36.2) | 18(22.8) | 61 (77.2) |
| African/ Black/ Caribbean | 10 (4.6) | 6 (60.0) | 4 (40.0) |
| Education: High school graduate* | 99 (45.4) | 25 (25.3) | 74 (74.7) |
| Education: Less than high school education | 118 (54.1) | 29 (53.7) | 89 (54.3) |
| Ever had a l ive birth* | 167 (76.6) | 42 (25.1) | 125 (74.9) |
| Never had a live birth | 49 (22.5) | 12 (24.5) | 37 (75.5) |
| INTERPERSONAL FACTORS | |||
| Have an intimate male partner* | 80 (36.7) | 20 (25.0) | 60 (75.0) |
| Do not have an intimate male partner | 135 (61.9) | 34 (25.2) | 101 (74.8) |
| Physical/ sexual Intimate partner violence ever* | 168 (77.1) | 44 (26.2) | 124 (73.8) |
| Never experienced physical/ sexual intimate partner violence | 46 (21.1) | 8 (17.4) | 38 (82.6) |
| Disclosed HIV status at diagnosis* | 113 (51.8) | 30 (26.5) | 83 (73.5) |
| Did not disclose HIV status at diagnosis | 93 (42.7) | 22 (23.7) | 71 (76.3) |
| STRUCTURAL FACTORS | |||
| HIV disclosure without consent * | 114 (52.3) | 42 (36.8) | 72 (63.2) |
| No HIV disclosure without consent | 100 (45.9) | 12 (12.0) | 88 (88.0) |
| Ever verbally or physically abused because of HIV status * 16 missing | 80 (36.7) | 28 (35.0) | 52 (65.0) |
| Never verbally or physically abused because of HIV status | 122 (56.0) | 25 (20.5) | 97 (79.5) |
| Ever received preconception counseling* | 25 (11.5) | 9 (36.0) | 16 (64.0) |
| Never received preconception counseling | 190 (87.2) | 45 (23.7) | 145 (76.3) |
| Ever accessed women-specific HIV services | 109 (50.0) | 30 (27.5) | 79 (72.5) |
| Never accessed women-specific HIV services | 109 (50.0) | 24 (22.0) | 85 (78.0) |
Variable has missing responses at baseline
Indigenous peoples of Canada: First Nations, Métis and Inuit peoples. The Indigenous peoples of Canada represent diverse cultures and languages however, for the purposes of this analysis Indigenous was used to refer to these groups collectively
Figure. 1.
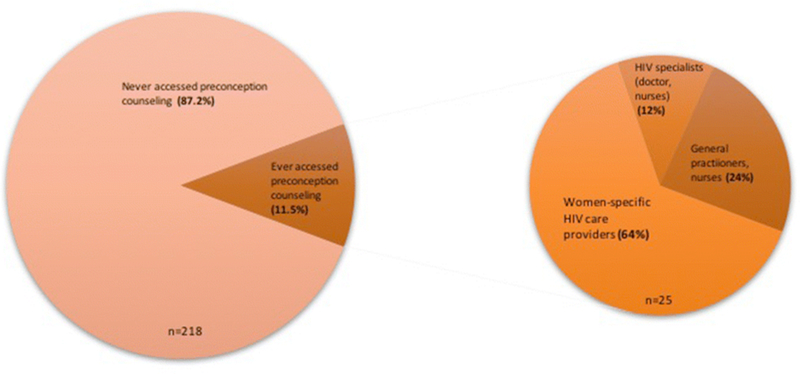
Proportion of the 218 SHAWNA participants reporting having ever accessed preconception counseling, by health care provider type
Table 2 .
Information received at pre-conception counselling, among 25 women l iving with HIV who reported ever receiving pre-conception counseling
| Information received in preconception discussions | n (%) |
|---|---|
| How to medically manage HIV before pregnancy | 20 (80) |
| How to medically manage HIV during childbirth and breastfeeding | 18 (72) |
| How to reduce the risk of vertical transmission | 16 (64) |
| How to reduce the risk of horizontal transmission | 17 (68) |
| Methods to increase pregnancy success | 16 (64) |
| How to prepare yourself for pregnancy/parenting physically (e.g., pre-pregnancy STI tests, nutrition | 14 (56) |
| How to prepare for pregnancy emotionally | 12 (48) |
| How to become pregnant if partner is living with HIV | 9 (36) |
In bivariate analysis, the following variables were significantly associated with our outcome at p<0.10: HIV disclosure without consent (Odds ratio (OR)= 4.28; 95% Confidence Interval (CI) 2.10–8.73), sexual orientation (OR=2.17; 95%CI 1.11–4.22), and ever experienced verbal or physical abuse due to one’s HIV status (OR=2.09; 95%CI 1.11–3.95).
In multivariable analyses, women reporting non-consensual HIV sero-status disclosure had 3.76-fold increased odds of reporting that their HIV diagnosis made them feel discouraged them from wanting to become pregnant (AOR: 3.76; 95%CI 1.82–7.80) (Table 3).
Table 3 .
Bivariate ( unadjusted odds ratios ( OR)) and multivariable associations (adjusted odds ratios (AOR)) and 95 % confidence intervals (95 % CI) of individual, interpersonal and structural factors and feeling discouraged from wanting to become pregnant due to one’ s HIV status among women l iving with HIV in Metro Vancouver (2014‒2016).
| Variable |
||
|---|---|---|
| OR ( 95 % CI | AOR ( 95 % CI) | |
| INDIVIDUAL SOCIO-DEMOGRAPHIC FACTORS | ||
| Age of HIV diagnosis | 0.98 (0.94‒1.02) | - |
| Age at baseline | 0.99 (0.96‒1.03) | - |
| Duration of HIV infection | 1.00 (0.96‒1.05) | |
| Sexual orientation ( LGBQ 2 S vs straight) asexual, two-spirit | 2.17 (1.11‒4.22)* | 1.77 (0.87‒3.60) |
| Married or common-law | 0.66 (0.30‒1.48) | - |
| Indigenous+ | 0.98 (0.50‒1.94) | - |
| African/ Caribbean/ Black | 3.39 (1.17‒9.81) | |
| White | REF | |
| High school graduate vs. less than high school | 1.04 (0.56‒1.92) | - |
| Ever had a live birth | 1.04 (0.50‒2.17) | - |
| INTERPERSONAL FACTORS | ||
| Have an intimate male partner | 0.99 (0.52‒1.87) | - |
| Intimate partner violence ever | 1.69 (0.73‒3.89) | - |
| Disclosed status when tested HIV positive | 1.17 (0.62‒2.20) | - |
| STRUCTURAL FACTORS | ||
| HIV disclosure without consent | 4.28 (2.10‒8.73)* | 3.76 (1.82‒7.80) |
| Ever abused because of HIV status | 2.09 (1.11‒3.95)* | - |
| Received preconception counseling | 1.81 (0.75‒4.38) | - |
| Ever accessed women-specific HIV services | 1.35 0.73‒2.50) | - |
Indigenous peoples of Canada: First Nations, Métis and Inuit peoples. The Indigenous peoples of Canada represent diverse cultures and languages however, for the purposes of this analysis Indigenous was used to refer to these groups collectively
In multivariable analysis, non-consensual HIV disclosure by a third party was associated with WLWH feeling discouraged from wanting to become pregnant.
DISCUSSION
These findings suggest that even in the era of ART, stigma, particularly from non-consensual HIV disclosure, continues to adversely affect WLWH’s reproductive choices. A recent systematic review by Turan and colleagues documented that stigma related to disclosing their status was among WLWHs’ primary concerns in pregnancy and that detrimental effects of HIV-related stigma accumulate across the PMTCT cascade of care(23), citing evidence suggesting that stigma may contribute up to 44% of vertical HIV transmission cases in some settings(43). Having one’s status disclosed without consent, a proxy for HIV stigma, is a serious breach of one’s confidentiality and can exacerbate the fears of stigma, discrimination and violence commonly faced by WLWH when disclosing one’s status(23, 44). Previous negative experiences due to non-consensual HIV disclosure may further discourage women from wanting to become pregnant, due to heightened concerns of judgment of placing their baby at risk of HIV(45). These concerns are valid, as previous research have reported increasing levels of stigma between pregnancy to postpartum period(46), including from intimate partners, family, friends and health care providers(23, 25). We located only one empirical study examining the impact of stigma on pregnancy decisions, which found that women who had experienced HIV disclosure-related stigma had 18.6% decreased odds of wanting to become pregnant(27). The authors hypothesized this was due to WLWHs’ fear of judgement and stigmatization. The criminalization of HIV non-disclosure in Canada and disproportionately severe punishment resulting from a conviction likely fuels stigma towards WLWH and may discourage women from wanting to become pregnant.
Though not significant in our final model, our bivariate results lend further support to the negative impact of stigma on WLWHs’ pregnancy decisions, with sexual minorities (i.e., LGBQ2S) and those who had experienced HIV-related physical or verbal violence having higher odds of feeling discouraged from wanting to become pregnant. There is an urgent need to explore interventions to reduce HIV-related stigma in the community, including the intersecting stigmas stemming from gender and sexual orientation, HIV status, drug use, sex work involvement and ethnicity(47). We did not find any differences in the impact of stigma on the decisions of Indigenous compared to White WLWH, despite evidence suggesting high levels stigma faced by Indigenous people. Surprisingly, the duration of HIV infection and age of HIV diagnosis was not significantly associated with feeling discouraged from wanting to become pregnant; we hypothesized that WLWH diagnosed earlier in the epidemic, before widespread access to ART, would be more likely to feel discouraged from wanting to become pregnant.
Of importance, our findings reveal a concerning gap in access to preconception counseling, highlighting missed opportunities for women to plan safe pregnancies. Preconception counseling is an important opportunity for WLWH to gain a better understanding of Canada’s HIV non-disclosure laws, including the implications of non-disclosure and strategies for disclosing one’s status to their intimate partner in the context of pregnancy planning. Access to preconception counseling may also provide WLWH with an opportunity to discuss prevention of mother-to-child transmission (PMTCT) which could help alleviate WLWHs’ concerns and internal stigma/self-stigmatization around HIV and pregnancy. Finally, conversations with health care providers around how to manage commonly-experience external/enacted stigma and discrimination (e.g., from family and community) in the context of pregnancy and childrearing (e.g., breastfeeding practices) may be beneficial.
The levels of preconception counseling in our sample (11.5%) are low, even when compared to Ontario, Canada, where 31% of WLWH sampled had received preconception counseling(48). This is despite the fact that half of our sample had accessed women-specific HIV care. While it is possible that participants may not have been HIV positive when pregnant/planning pregnancy or were diagnosed during pregnancy, these numbers remain low given the Society of Obstetricians and Gynaecologists Association of Canada (SOGC) guidelines that recommend conception-focused discussions be offered at regular intervals to WLWH of reproductive age. We believe that the majority of missed opportunities for preconception counseling are likely to have occurred in the community (e.g., general practitioners), as the majority of women first access the main women HIV care provider in this setting (Oak Tree Clinic) once they have become pregnant. As HIV has now become a chronic condition manageable with ART, it is critical that health care providers receive adequate training to support positive sexual and reproductive health care needs and rights of WLWH, including safe motherhood. This includes the need for health care providers to recognize the pregnancy intentions of WLWH and initiate conception-focused discussions with their patients. Evidence from the United States support this: among a sample of WLWH who had accessed preconception counseling, the majority (67%) had initiated personalized discussions around pregnancy with their health care providers themselves.(49) The authors also reported that health care providers were significantly more likely to initiate pregnancy planning discussions with younger WLWH (<30 years), overlooking the significant portion of older WLWH who may also desire pregnancy. Pregnancy discussions may not be offered by health care providers due to competing medical priorities, time limitations, and/or a lack of clarity around roles and practices standards among the range of health care providers (e.g., HIV specialists, OBGYN, general practitioners) who serve WLWH(50). Discussions around the criminalization of HIV disclosure in particular are complex, delicate and have the potential to further stigmatize and marginalize WLWH. There is a clear need for specialized training around counseling WLWH on the criminalization of HIV in the context of pregnancy, as well as additional time in appointments to adequately address this issue. Another reason that health providers may not initiate conception-focused discussions may be their judgment of their patient’s capacity to safely parent, particularly for those struggling with addictions, poverty, mental health issues or violent relationship. Fear of such judgement and internalized stigma may prevent/delay women from disclosing their reproductive desires and intentions with their health providers(51). Indeed, fear of health care provider judgement or disapproval is a common barrier for WLWH in bringing forth such conversations(8), and many women, including in Canada, have experienced judgement from their health care providers throughout pregnancy(51). In settings where marginalized women are overrepresented among WLWH, including Indigenous im/migrant, women who use substances, and gender/sexual minority women, adopting new WHO/UNAIDS guidelines and training for sexual and reproductive health and rights among WLWH from a rights-based perspective is critical(52).
While the causes and solutions to HIV stigma are complex, structural interventions, including at the programmatic level could help better support WLWHs’ reproductive choices. There is a clear need for non-judgmental and compassionate holistic health care provision including SRH and HIV care that integrates reproductive health services (including preconception counseling as well as pregnancy spacing or prevention services). Though the sources of non-consensual HIV disclosure in this study are unclear, our preliminary data (not shown) suggests that some cases of non-consensual HIV disclosure occur by health care and social services providers. It is imperative that health and social services providers working with WLWH are trained in protecting the privacy and confidentiality of WLWH. The removal of criminalized laws on HIV non-disclosure is also essential to reducing the stigma around HIV, and may help reduce WLWH’s fears around conception.
The majority of our participants have experienced at least one potentially traumatic event (e.g., intimate partner violence, verbal or physical abuse because of their HIV status, and non-consensual HIV disclosure, intergenerational trauma) highlighting an urgent need to increase access to women-centred, trauma-informed care, including preconception counseling, for WLWH in Metro Vancouver. Complementing a trauma-informed care approach, women-centred care is a comprehensive approach to health care which acknowledges the diversity of women’s experiences and aims to holistically address women’s health concerns in the context of the broader social and structural barriers to health care (e.g., gender-based violence, poverty, challenges to safe disclosure) that women experience(53). Given the high levels of multiple forms of social and structural violence experienced by marginalized WLWH of reproductive age (e.g., childhood abuse/neglect, intimate partner physical, sexual and emotional violence, stigma, poverty, homelessness, intergenerational trauma from colonization), health care providers need to be sensitive and responsive to the multiple forms of trauma women may endure, and offer physically and emotionally safe spaces and care. Accurate and non-judgmental conception-focused discussions need to be initiated by health care providers and offered to women of all ages(49) and sexual orientations. In our setting, there may be a need to train health care providers (particularly those working in the community) on the sexual and reproductive needs and rights of WLWH. Aligned with WHO/UNAIDS International Sexual and Reproductive Health and Rights & HIV guidelines for WLWH and the Society of Gynecologists and Obstetricians of Canada (SOGC) Canadian HIV Pregnancy Planning Guidelines(52, 54), pregnancy discussions should be offered when women are first diagnosed and on a regular basis as women’s reproductive needs and wants change over their lifetime(54). It is imperative that preconception counseling accurately cover all relevant information outlined in the existing preconception counseling guidelines, including: how to increase pregnancy success, appropriate ART use during pregnancy, prevention of vertical and horizontal transmission, general pregnancy issues given many other co-morbidities that women with HIV can have, as well as the psychosocial aspects of HIV and pregnancy(14, 54). Our results demonstrate that less than half of participants (48%) reported discussing the emotional/psychosocial aspects of pregnancy, which generally encompass HIV stigma and discrimination pre- and post-partum and the implications of Canada’s HIV non-disclosure laws. Such information would be critical in supporting WLWH’s reproductive decisions, especially those who have experienced HIV disclosure without consent and fear further stigma arising from pregnancy.
Limitations
This study has a number of strengths and limitations. First, given our lifetime outcome, our analysis was cross-sectional and may be susceptible to biases inherent to cross sectional studies, such as limiting our ability to make temporal inferences. For example, it is unclear when events of non-consensual HIV disclosure occurred and if these proceeded WLWHs’ pregnancy decisions. However, given the median age of HIV diagnosis in our sample is 31 years, it is likely that these events occurred during women’s reproductive years. Second, as with all observational research our outcome may be susceptible to social desirability, potentially leading to an underreporting of this variable and biasing our results towards the null. Despite this bias, a quarter of our sample reported feeling discouraged from wanting to become pregnant and this remained strongly and significantly associated with our outcome in multivariable analysis. Both the community-based nature of the SHAWNA project and our community interview and sexual health research nursing team (many of our team are WLWH themselves) are well-trusted and have a strong rapport with the community. Finally, preconception counseling access may be subject to recall bias, potentially resulting in an underreporting of these discussions as well as the types of information received. However, in light of the SOGC guidelines that recommend that practitioners routinely initiate conception-focused discussions, there should not be a significant lag between WLWHs’ last discussion around pregnancy intentions/desires and the time of our interview.
CONCLUSIONS
Despites advances in ART and parallel shifts in fertility trends among WLWH, stigma from non-consensual HIV disclosure remains a significant barrier to WLWHs’ reproductive choice. There is a clear need to increase access to women-centred care that embraces the principles of trauma-informed care to offer integrated HIV & reproductive health services, inclusive of preconception counseling. There may be a need to better educate health care providers in the community about the reproductive desires of WLWH, and ensure that accurate, comprehensive and non-judgmental conception-focused discussions are initiated by health care providers in an ongoing manner, consistent with Canada’s HIV pregnancy planning guidelines. In addition, given the complexity of the counseling in some cases, women should also be given the opportunity to consult with experts in this area when appropriate.
Acknowledgments:
We thank all those who contributed their time and expertise to this project, particularly participants, community partners, the SHAWNA Positive Women’s Advisory Board and Community Advisory Board, and the SHAWNA Project team: Sarah Moreheart, Brittany Udall, Jennifer Morris, Flo Ranville, Heidi Safford, Lauren Martin, Ray Croy, Bridgette Simpson, Anita Dhanoa, Monique Desroches, Lydia Hamel, Lulu Gurney, and Patience Chamboko. We also acknowledge Melissa Braschel, Abby Rolston, Sylvia Machat, Peter Vann, Erin Seatter, and Patricia McDonald for their research and administrative support. KS is supported by a Canada Research Chair in Global Sexual Health and HIV/AIDS and Michael Smith Foundation for Health Research. This research was supported by the Canadian Institutes of Health Research (MOP-133617) and MacAIDS. KS is supported by a Canada Research Chair in Global Sexual Health and HIV/AIDS and Michael Smith Foundation for Health Research. PD is supported by the Canadian Institutes for Health Research and Michael Smith Foundations for Health Research Postdoctoral Fellowship Award. JM received research support, paid to the institution, from the Public Health Agency of Canada, the BC-Ministry of Health, the US NIH (NIDA R01DA036307 and CTN 248), the Canadian Institues of Health Research, Janssen & Janssen, and Merk.
REFERENCES
- 1.Antiretroviral Therapy Cohort C. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet 2008;372(9635):293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hogg RS, Heath KV, Yip B, Craib KJ, O’Shaughnessy MV, Schechter MT, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA 1998;279(6):450–4. [DOI] [PubMed] [Google Scholar]
- 3.Jin Y, Liu Z, Wang X, Liu H, Ding G, Su Y, et al. A systematic review of cohort studies of the quality of life in HIV/AIDS patients after antiretroviral therapy. Int J STD AIDS 2014;25(11):771–7. [DOI] [PubMed] [Google Scholar]
- 4.Nosyk B, Zang X, Min JE, Krebs E, Lima VD, Milloy MJ, et al. Relative effects of antiretroviral therapy and harm reduction initiatives on HIV incidence in British Columbia, Canada, 1996–2013: a modelling study. The lancet HIV 2017. [DOI] [PMC free article] [PubMed]
- 5.Chi BH, Stringer JS, Moodley D. Antiretroviral drug regimens to prevent mother-to-child transmission of HIV: a review of scientific, program, and policy advances for sub-Saharan Africa. Curr HIV/AIDS Rep 2013;10(2):124–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. A systematic review of factors influencing fertility desires and intentions among people living with HIV/AIDS: implications for policy and service delivery. AIDS Behav 2009;13(5):949–68. [DOI] [PubMed] [Google Scholar]
- 7.Sharma A, Feldman JG, Golub ET, Schmidt J, Silver S, Robison E, et al. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. Am J Obstet Gynecol 2007;196(6):541.e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haddad LB, Machen LK, Cordes S, Huylebroeck B, Delaney A, Ofotokun I, et al. Future desire for children among women living with HIV in Atlanta, Georgia. AIDS Care 2016;28(4):455–9. [DOI] [PubMed] [Google Scholar]
- 9.Jones DL, Cook R, Potter JE, Miron-Shatz T, Chakhtoura N, Spence A, et al. Fertility Desires among Women Living with HIV. PLoS One 2016;11(9):e0160190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jose H, Madi D, Chowta N, Ramapuram J, Bhaskaran U, Achappa B, et al. Fertility Desires and Intentions among People Living with HIV/AIDS (PLWHA) in Southern India. Journal of clinical and diagnostic research : JCDR 2016;10(6):Oc19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loutfy MR, Hart TA, Mohammed SS, Su D, Ralph ED, Walmsley SL, et al. Fertility desires and intentions of HIV-positive women of reproductive age in Ontario, Canada: a cross-sectional study. PLoS One 2009;4(12):e7925-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finocchario-kessler S, Sweat MD, Keller JM, Anderson JR, Finocchario-Kessler S, Sweat MD, et al. Understanding high fertility desires and intentions among a sample of urban women living with HIV in the United States. AIDS and behavior 2010;14(5):1106–14. [DOI] [PubMed] [Google Scholar]
- 13.Health Canada. HIV and AIDS in Canada: surveillance report to June 30,2002 Ottawa: Division of HIV/AIDS Epidemiology and Surveillance, Centre for Infectious Disease Prevention and Control (CIDPC), Health Canada; 2002. [Google Scholar]
- 14.Ogilvie GS, Palepu A, Remple VP, Maan E, Heath K, MacDonald G, et al. Fertility intentions of women of reproductive age living with HIV in British Columbia, Canada. AIDS 2007;21 Suppl 1:S83–8. [DOI] [PubMed] [Google Scholar]
- 15.Fabiani M, Nattabi B, Ayella EO, Ogwang M, Declich S. Differences in fertility by HIV serostatus and adjusted HIV prevalence data from an antenatal clinic in northern Uganda. Trop Med Int Health 2006;11(2):182–7. [DOI] [PubMed] [Google Scholar]
- 16.Burgess A, Purssell E. What is the relationship between increased access to HAART, relationship status and fertility decisions amongst HIV positive women? A Literature Review and Meta-Analysis. Journal of clinical nursing 2017. [DOI] [PubMed]
- 17.Demissie DB, Tebeje B, Tesfaye T. Fertility desire and associated factors among people living with HIV attending antiretroviral therapy clinic in Ethiopia. BMC Pregnancy Childbirth 2014;14:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Public Health Agency of Canada. HIV and AIDS in Canada: Surveillance Report to December 31, 2013 Ottawa: Public Health Agency of Canada; 2014. [Google Scholar]
- 19.Donnelly LR, Bailey L, Jessani A, Postnikoff J, Kerston P, Brondani M. Stigma Experiences in Marginalized People Living With HIV Seeking Health Services and Resources in Canada. J Assoc Nurses AIDS Care 2016;27(6):768–83. [DOI] [PubMed] [Google Scholar]
- 20.Benoit C, Carroll D, Chaudhry M. In search of a healing place: Aboriginal women in Vancouver’s Downtown Eastside. Soc Sci Med 2003;56:821–33.−−33. [DOI] [PubMed] [Google Scholar]
- 21.Oosterhoff P, Anh NT, Hanh NT, Yen PN, Wright P, Hardon A. Holding the line: family responses to pregnancy and the desire for a child in the context of HIV in Vietnam. Cult Health Sex 2008;10(4):403–16. [DOI] [PubMed] [Google Scholar]
- 22.Cooper D, Harries J, Myer L, Orner P, Bracken H, Zweigenthal V. “Life is still going on”: reproductive intentions among HIV-positive women and men in South Africa. Soc Sci Med 2007;65(2):274–83. [DOI] [PubMed] [Google Scholar]
- 23.Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav 2013;17(7):2528–39. [DOI] [PubMed] [Google Scholar]
- 24.Duff P, Kipp W, Wild TCC, Rubaale T, Okech-Ojony J. Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. J Int AIDS Soc 2010;13(1):37-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greene S, Ion A, Kwaramba G, Smith S, Loutfy MR. “Why are you pregnant? What were you thinking?”: How women navigate experiences of HIV-related stigma in medical settings during pregnancy and birth. Social work in health care 2016;55(2):161–79. [DOI] [PubMed] [Google Scholar]
- 26.Ion A, Elston D. Examining the Health Care Experiences of Women Living with Human Immunodeficiency Virus (HIV) and Perceived HIV-Related Stigma. Womens Health Issues 2015;25(4):410–9. [DOI] [PubMed] [Google Scholar]
- 27.Craft SM, Delaney RO, Bautista DT, Serovich JM. Pregnancy decisions among women with HIV. AIDS Behav 2007;11(6):927–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darlington CK, Hutson SP. Understanding HIV-Related Stigma Among Women in the Southern United States: A Literature Review. AIDS Behav 2017;21(1):12–26. [DOI] [PubMed] [Google Scholar]
- 29.Bernard E, Bennet-Carlson R. Criminalization of HIV non-disclosure, exposure and transmission: background and current landscape Geneva: UNAIDS; 2012. [Google Scholar]
- 30.Patterson SE, Milloy MJ, Ogilvie G, Greene S, Nicholson V, Vonn M, et al. The impact of criminalization of HIV non-disclosure on the healthcare engagement of women living with HIV in Canada: a comprehensive review of the evidence. J Int AIDS Soc 2015;18:20572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brezing C, Ferrara M, Freudenreich O. The syndemic illness of HIV and trauma: implications for a trauma-informed model of care. Psychosomatics 2015;56(2):107–18. [DOI] [PubMed] [Google Scholar]
- 32.Duff PK, Money DM, Ogilvie GS, Ranville F, Kestler M, Braschel MC, et al. Severe menopausal symptoms associated with reduced adherence to antiretroviral therapy among perimenopausal and menopausal women living with HIV in Metro Vancouver. Menopause (New York, NY) 2017. [DOI] [PMC free article] [PubMed]
- 33.Ratzlaff A, Deering K, Pick N, Kestler M, Ranville F, Braschel M, et al. , editors. Women living with HIV identify critical need for trauma-informed HIV Care models to support ART use in Metro Vancouver, Canada Canadian Association for HIV Research; 2017; Vancouver. [Google Scholar]
- 34.Gelaye B, Zhong QY, Basu A, Levey EJ, Rondon MB, Sanchez S, et al. Trauma and traumatic stress in a sample of pregnant women. Psychiatry research 2017;257:506–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Torchalla I, Linden IA, Strehlau V, Neilson EK, Krausz M. “Like a lots happened with my whole childhood”: violence, trauma, and addiction in pregnant and postpartum women from Vancouver’s Downtown Eastside. Harm Reduct J 2015;11:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.SAMHSA’s Traumatic and Justic Strategic Initiatve. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach 2014.
- 37.Canada PHAo. HIV and AIDS in Canada: Surveillance Report to December 31, 2013 . Ottawa, Canada: Minister of Public Works and Government Services Canada; ; 2014. [Google Scholar]
- 38.Barreto D, Krusi A, Ranville F, Safford H, Pooyak S, Braschel M, et al. HIV disclosure without consent linked to increased risk of violence against women living with HIV in Metro Vancouver, British Columbia. Women and HIV workshop; February 2017; Seattle, USA2017. [Google Scholar]
- 39.Ross L. What is Reproductive Justice? : Sistersong Women on Color Reproductive Health Collective and Pro-Choice Public Education Project; 2007.
- 40.Wood E, Tyndall MW, Spittal PM, Li K, Anis AH, Hogg RS, et al. Impact of supply-side policies for control of illicit drugs in the face of the AIDS and overdose epidemics: investigation of a massive heroin seizure. CMAJ 2003;168(2):165–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Stockman JK, Morris MD, Martinez G, Lozada R, Patterson TL, Ulibarri MD, et al. Prevalence and Correlates of Female Condom Use and Interest Among Injection Drug-Using Female Sex Workers in Two Mexico-US Border Cities. AIDS AND BEHAVIOR 2012;16(7):1877–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lima VD, Harrigan R Fau - Murray M, Murray M Fau - Moore DM, Moore Dm Fau - Wood E, Wood E Fau - Hogg RS, Hogg Rs Fau - Montaner JS, et al. Differential impact of adherence on long-term treatment response among naive HIV-infected individuals (1473–5571 (Electronic)). [DOI] [PubMed]
- 43.Prudden H, Dzialowy N, Foss A, Black V, Wallace C, Nyblade L . Modelling the impact of stigma on the Prevention of Mother to Child HIV Transmission for a setting in South Africa. Technical Report: London School of Hygiene and Tropical Medicine; 2011. [Google Scholar]
- 44.Rujumba J, Neema S, Byamugisha R, Tylleskar T, Tumwine JK, Heggenhougen HK. “Telling my husband I have HIV is too heavy to come out of my mouth”: pregnant women’s disclosure experiences and support needs following antenatal HIV testing in eastern Uganda. J Int AIDS Soc 2012;15(2):17429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kendall T. Reproductive rights violations reported by Mexican women with HIV. Health Hum Rights 2009;11(2):77–87. [PubMed] [Google Scholar]
- 46.Ion A, Wagner AC, Greene S, Loutfy MR. HIV-related stigma in pregnancy and early postpartum of mothers living with HIV in Ontario, Canada. AIDS Care 2017;29(2):137–44. [DOI] [PubMed] [Google Scholar]
- 47.Logie C, James L, Tharao W, Loutfy M. Associations Between HIV-Related Stigma, Racial Discrimination, Gender Discrimination, and Depression Among HIV-Positive African, Caribbean, and Black Women in Ontario, Canada. AIDS patient care and STDs 2013;27(2):114–22. [DOI] [PubMed] [Google Scholar]
- 48.Loutfy MR, Blitz S, Zhang Y, Hart TA, Walmsley SL, Smaill FM, et al. Self-Reported Preconception Care of HIV-Positive Women of Reproductive Potential: A Retrospective Study. Journal of the International Association of Providers of AIDS Care 2014;13(5):424–33. [DOI] [PubMed] [Google Scholar]
- 49.Finocchario-Kessler S, Dariotis JK, Sweat MD, Trent ME, Keller JM, Hafeez Q, et al. Do HIV-infected women want to discuss reproductive plans with providers, and are those conversations occurring? AIDS Patient Care STDS 2010;24(5):317–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoyt MJ, Storm DS, Aaron E, Anderson J. Preconception and contraceptive care for women living with HIV. Infectious diseases in obstetrics and gynecology 2012;2012:604183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coll AS, Potter JE, Chakhtoura N, Alcaide ML, Cook R, Jones DL. Providers’ perspectives on preconception counseling and safer conception for HIV-infected women. AIDS Care 2016;28(4):513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.World Health Organization. Consolidated guidelines on sexual and reproductive health and rights of women living with HIV 2017. [PubMed]
- 53.of BWsHHCaBCC, Excellence for Women’s Health. A women’s health strategy for British Columbia: advancing the health of girls and women Vancouver: BC Women’s Hospital & Health Centre and British Columbia Centre of Excellence for Women’s Health; 2004. [Google Scholar]
- 54.Loutfy MR, Margolese S, Money DM, Gysler M, Hamilton S, Yudin MH. Canadian HIV Pregnancy Planning Guidelines: No. 278, June 2012. Int J Gynaecol Obstet 2012;119(1):89–99. [DOI] [PubMed] [Google Scholar]


