Abstract
PURPOSE:
The purpose of this study was to examine the incidence and economic burden of peristomal skin complications (PSCs) following ostomy surgery.
DESIGN:
Retrospective cohort study based on electronic health records and administrative data stores at a large US integrated healthcare system.
SUBJECTS AND SETTINGS:
The sample comprised 168 patients who underwent colostomy (ICD-9-CM 46.1X) (n = 108), ileostomy (46.2X) (n = 40), cutaneous ureteroileostomy (56.5X), or other external urinary diversion (56.6X) (n = 20) between January 1, 2012, and December 31, 2014. The study setting was an integrated health services organization that serves more than 2 million persons in the northeastern United States.
METHODS:
We scanned electronic health records of all study subjects to identify those with evidence of PSCs within 90 days of ostomy surgery and then examined healthcare utilization and costs over 120 days, beginning with date of surgery, among patients with and without evidence of PSCs. Testing for differences in continuous measures between the 3 ostomy groups was based on one-way analysis of variance; testing for differences in such measures between the PSC and non-PSC groups was based on a t statistic, and the χ2 statistic was used to test for differences in categorical measures.
RESULTS:
Sixty-one subjects (36.3%) had evidence of PSCs within 90 days of ostomy surgery (ileostomy, 47.5%; colostomy, 36.1%; urinary diversion, 15.0%; P < .05 for differences between groups). Among patients with evidence of PSCs, the mean (SD) time from surgery to first notation of this complication was 26.4 (19.0) days; it was 24.1 (13.2) days for ileostomy, 27.2 (21.1) days for colostomy, and 31.7 (25.7) days for urinary diversion (P = .752). Patients with PSCs were more likely to be readmitted to hospital by day 120 (55.7% vs 35.5% for those without PSCs; P = .011). The mean length of stay for patients readmitted to hospital was 11.0 days for those with PSCs and 6.8 days for those without PSCs (P = .111). The mean total healthcare cost over 120 days was $58,329 for patients with evidence of PSCs and $50,298 for those without evidence of PSCs (P = .251).
CONCLUSIONS:
Approximately one-third of ostomy patients developed PSCs within 90 days of their surgery. Peristomal skin complications are associated with a greater likelihood of hospital readmission. Our findings corroborate results of earlier studies.
Keywords: Colostomy, Complications, Cost analysis, Ileostomy, Ostomy, Peristomal skin, Stoma, Urostomy
INTRODUCTION
More than 750,000 persons in the United States are currently living with ostomies, and approximately 130,000 undergo creation of a new ostomy every year.1 Maintenance of the peristomal skin is often challenging for both patients and providers, and peristomal skin complications (PSCs) are prevalent.2 The severity of these complications varies from mild erythema to eroded or ulcerated skin. The etiology of PSCs can be complex, and contributing factors include peristomal moisture-associated skin damage caused by prolonged exposure to urinary or fecal effluent, mechanical skin injury such as medical adhesive–related skin injuries, pressure injury, bacterial or fungal infections, hypersensitivity or allergy to ostomy products, and immune or autoimmune disorders such as pyoderma gangrenosum.3
Reported rates of PSC incidence following ostomy surgery range from 10% to 70%.4 Reasons for discrepancies in these estimates include relatively small and/or heterogeneous sample sizes, differences in the types of ostomies studied (eg, fecal vs urinary, end vs loop), differences in the types of complications considered and how cases were identified, and variability in assessment periods. Estimates of the lifetime prevalence of PSCs range from 6% to 80%, depending on the type of ostomy and how PSCs are defined.5
Peristomal skin complications are usually preventable; there is evidence suggesting that their severity can be limited by adequate training and active engagement of patients in the care of their stomas, along with emphasis on the importance of seeking treatment on a timely basis when problems arise.6–8 For example, Stokes and colleagues6 reported that patients who attended a preoperative educational session on the management of new ostomies led by certified wound, ostomy, and continence nurses (CWOCNs) experienced significantly fewer PSCs within 30 days of ostomy surgery versus those who did not attend this session. In addition, several studies have shown that many patients with PSCs do not realize they have them.7,8 Regular follow-up visits to a qualified healthcare professional such as a WOC nurse are critical to identifying problems early and often avoiding long-term debilitating and expensive complications of PSCs.
Despite the prevalence of PSCs in patients with ostomies, relatively little is known about their economic burden. In an earlier retrospective study conducted at Henry Ford Health System in Detroit, Michigan, we found that 36.7% of 128 patients who underwent colostomy, ileostomy, or urostomy between 2008 and 2012 developed PSCs within 90 days of their surgery.9 We also found that patients experiencing these complications had substantially higher costs of postsurgical care than those who did not develop PSCs.9 The generalizability of these findings to other healthcare systems and to the present day (with potentially more aggressive case management) is unknown. In this study, we examined the risk and burden of PSCs following ostomy surgery in another large US integrated healthcare system during a more recent time period.
METHODS
Data were obtained from information systems of Geisinger Health System (GHS), a physician-led, fully integrated health services organization that serves more than 2 million persons throughout central and northeastern Pennsylvania. On a licensed basis for research purposes, the system provides customized, de-identified data extracted from electronic health records (EHRs) through its wholly owned subsidiary, MedMining. Data extracts from GHS include information from both inpatient and outpatient facilities, and standard data elements include patient demographics, vital signs, flow sheet measure types, results of lab tests, ICD-9-CM diagnosis codes, ICD-9-CM and HCPCS procedure codes, medications, mortality (including day of death), and actual costs to providers. In addition to information from the GHS EHR, for persons who are members of Geisinger Health Plan (GHP), a GHS-owned health maintenance organization, information is also available from all medical, hospital, and pharmacy claims. Approximately 460,000 persons are enrolled in GHP in any given year, including almost 80,000 persons who are in Medicare Advantage/Risk plans.
Our source population consisted of all persons who were members of GHP anytime between January 1, 2012, and December 31, 2014. This time period was chosen because it allowed us to meet our requirement of a minimum sample size of 100 patients. We limited our attention to persons who were members of GHP to maximize the likelihood of complete data capture for all study subjects. Persons who are members of GHS but not GHP have the option of receiving their care from non-GHS providers and facilities, which would not be captured by GHS clinical data systems.
From among the source population, we selected persons aged 18 years or older who underwent colostomy (ICD-9-CM 46.1X), ileostomy (46.2X), cutaneous ureteroileostomy (56.5X), or other external urinary diversion (56.6X) anytime between January 1, 2012, and December 31, 2014. Persons who were not continuously enrolled in GHP for at least 120 days following their date of ostomy surgery, or who died during this period, were excluded from the study sample. We excluded persons who died because most were terminally ill and expired relatively soon after surgery (mean time from surgery to death, 35 days).
Study Procedures
Trained medical record technicians scanned each subject's EHR to determine if the patient experienced a PSC within 90 days of surgery. Ascertainment of PSCs was based on notation of any of a number of predefined key words and terms such as “dermatitis,” “excoriated,” and “maceration.” Information was extracted using case report forms that we designed, and the completed forms were independently reviewed by 2 CWOCNs. Study subjects were designated as having experienced a PSC only if there was agreement between both study nurses.
Levels of healthcare utilization (hospitalizations, outpatient visits, and stays in long-term care facilities, based on information in GHP paid healthcare claims) were then tallied for each study subject over a 120-day period following surgery. Costs of inpatient and outpatient care were similarly tallied over 120 days beginning with the date of hospital admission for ostomy surgery, based on the recorded cost of encounters to GHS providers and facilities. We employed a 120-day observation period to ensure that the period of follow-up subsequent to the occurrence of a PSC would be at least 30 days (ie, for a patient with incident PSC on day 90). Also, because the attribution of specific services to particular disease conditions is methodologically problematic and difficult to operationalize, we tallied utilization and costs on an all-cause basis.
Data Analysis
We examined baseline characteristics for study patients including age on date of ostomy surgery, gender, race, year of surgery, type of surgery (colostomy, ileostomy, urostomy), whether the procedure was described as permanent or temporary, and total days in hospital during the index admission. We also examined the cumulative incidence of PSCs on an overall basis as well as by type of procedure to day 120. Closure of stoma during follow-up was treated as a “competing risk” as of the date on which this procedure was performed, since these patients were deemed no longer to be at risk of developing a PSC. A competing risk is an event that precludes the occurrence of an event of interest or may modify the probability that it will occur; stoma closure thus constitutes a competing risk for PSCs, since patients are at risk of these complications only while their stoma remains open. For subjects with and without evidence of PSCs, respectively, we examined the number of patients receiving various types of services, as well as the number of times these services were rendered, which we summarized using means, standard deviations, medians, and interquartile ranges.
Costs of healthcare services also were tallied for subjects with and without PSCs, on an overall basis and by type of service. Total healthcare costs were operationally defined to include the cost of all direct medical services covered by GHS. Costs were analyzed using the Kaplan-Meier Sample Average (KMSA) estimator.10,11 With this method, the follow-up period is divided into segments of equal length, and the mean cost of all uncensored patients (ie, patients who are alive and contributing to follow-up) during each time interval is multiplied by the Kaplan-Meier estimate of the proportion of patients surviving to the beginning of the interval. These products are then summed across all intervals to yield a KMSA estimator of costs.
All analyses were conducted using SAS Proprietary Software, Release 9.1 (SAS Institute Inc, Cary, North Carolina). Summary statistics were examined for patients with and without PSCs; statistical tests for differences between 2 groups were undertaken. These results should be interpreted cautiously, however, due to the small sample size and low statistical power. Testing for differences in continuous measures between the 3 ostomy groups was based on the F statistic from one-way analysis of variance; testing for differences in such measures between the PSC and non-PSC groups was based on a t statistic. A χ2 statistic was used to test for differences in categorical measures between groups.
RESULTS
We identified 249 persons aged 18 years or older who underwent colostomy, ileostomy, cutaneous ureteroileostomy, or other external urinary diversion between January 1, 2012, and December 31, 2014, and were members of GHP on the day of their ostomy procedure. Among these persons, 168 met all study entry criteria (including survival and GHP continuous enrollment through day 120). Our sample comprised 108 (64.3% of all eligible study subjects) patients who underwent colostomy, 40 (23.8%) who underwent ileostomy, and 20 (11.9%) who underwent urostomy. The mean (SD) age of study subjects was 63.9 (13.6) years at the time of ostomy surgery (Table 1). Approximately equal numbers of men and women underwent colostomy and ileostomy; women constituted 80% of all urostomy patients, however. Approximately one-fourth of study subjects (23.2%) had ostomies that were described as temporary, and 39.9% had procedures that were reported to be permanent; status could not be determined for 36.9% of study subjects.
TABLE 1. Demographic and Pertinent Clinical Characteristics of Study Subjects, by Type of Ostomya.
| Characteristic | Colostomy (N = 108) | Ileostomy (N = 40) | Urinary Diversion (N = 20) | All Subjects (N = 168) | P |
|---|---|---|---|---|---|
| Age at index admission, y | |||||
| Mean (SD) | 63.6 (13.0) | 62.9 (16.7) | 67.5 (8.8) | 63.9 (13.6) | .441 |
| Gender | |||||
| Male | 53 (49.1) | 21 (52.5) | 4 (20.0) | 78 (46.4) | .039 |
| Female | 55 (50.9) | 19 (47.5) | 16 (80.0) | 90 (53.6) | ... |
| Race | |||||
| African American | 3 (2.8) | 1 (2.5) | 0 (0.0) | 4 (2.4) | .754 |
| White | 105 (97.2) | 39 (97.5) | 20 (100.0) | 164 (97.6) | ... |
| Year of ostomy surgery | |||||
| 2012 | 28 (25.9) | 13 (32.5) | 4 (20.0) | 45 (26.8) | .489 |
| 2013 | 44 (40.7) | 18 (45.0) | 7 (35.0) | 69 (41.1) | ... |
| 2014 | 36 (33.3) | 9 (22.5) | 9 (45.0) | 54 (32.1) | ... |
| Type of ostomy | |||||
| Permanent | 30 (27.8) | 18 (45.0) | 19 (95.0) | 67 (39.9) | <.001 |
| Temporary | 34 (31.5) | 5 (12.5) | 0 (0.0) | 39 (23.2) | ... |
| Unknown | 44 (40.7) | 17 (42.5) | 1 (5.0) | 62 (36.9) | ... |
aUnless otherwise indicated, all values are number (%) of subjects.
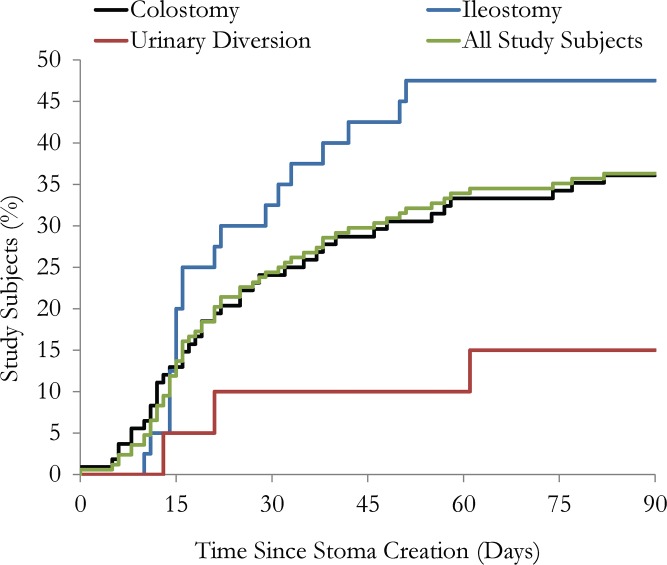
Sixty-one patients (36.3%) had evidence of PSCs within 90 days of surgery, including 19 of 40 patients (47.5%) who underwent ileostomy, 39 of 108 patients (36.1%) who underwent colostomy, and 3 of 20 patients (15.0%) who underwent urostomy (P = .0475; Table 2, Figure 1). The mean age was similar for patients with and without PSCs (64.4 years vs 63.6 years, respectively; P = .698). The mean (SD) time from surgery to first notation of a PSC was 26.4 (19.0) days; it was 24.1 (13.2) days for patients with ileostomies, 27.2 (21.1) days for those with colostomies, and 31.7 (25.7) days for those with urinary diversions (P = .752). Nine of 61 patients (14.8%) with PSCs developed a complication during their index admission; the remainder did so following hospital discharge. The mean length of stay did not differ for the index admission based on evidence of a PSC (12.7 days for patients with PSCs vs 13.3 days for patients without PSCs; P = .769).
TABLE 2. Utilization of Selected Healthcare Services During 120-Day Period Following Ostomy Surgery, by Absence/Presence of PSC (Analyses Based on Administrative Data)a.
| Colostomy | Ileostomy | Urinary Diversion | All Subjects | P | |||||
|---|---|---|---|---|---|---|---|---|---|
| No PSC (N = 69) | PSC (N = 39) | No PSC (N = 21) | PSC (N = 19) | No PSC (N = 17) | PSC (N = 3) | No PSC (N = 107) | PSC (N = 61) | ||
| Length of stay, index admission | |||||||||
| Mean (SD) | 14.0 (19.0) | 10.9 (8.7) | 16.5 (16.0) | 17.0 (15.4) | 6.8 (2.3) | 8.7 (5.5) | 13.3 (17.1) | 12.7 (11.3) | .769 |
| Median (IQR) | 9.0 (6.0-14.0) | 8.0 (5.0-16.0) | 9.0 (5.0-19.0) | 14.0 (5.0-21.0) | 6.0 (6.0-7.0) | 6.0 (5.0-15.0) | 8.0 (6.0-14.0) | 14.0 (5.0-17.0) | |
| Readmissions | |||||||||
| Patients, n (% with any) | 27 (39.1) | 22 (56.4) | 7 (33.3) | 9 (47.4) | 4 (23.5) | 3 (100.0) | 38 (35.5) | 34 (55.7) | .011 |
| Number of readmissionsb | |||||||||
| Mean (SD) | 1.4 (0.7) | 1.4 (0.6) | 1.1 (0.4) | 1.6 (0.5) | 1.0 (0.0) | 2.7 (2.1) | 1.3 (0.6) | 1.5 (0.8) | .162 |
| Median (IQR) | 1.0 (1.0-2.0) | 1.0 (1.0-2.0) | 1.0 (1.0-1.0) | 2.0 (1.0-2.0) | 1.0 (1.0-1.0) | 2.0 (1.0-5.0) | 1.0 (1.0-1.0) | 1.0 (1.0-2.0) | |
| Days in hospitalb | |||||||||
| Mean (SD) | 7.5 (9.0) | 7.5 (6.4) | 5.6 (5.3) | 9.6 (7.9) | 4.0 (1.2) | 41.0 (27.7) | 6.8 (8.0) | 11.0 (13.3) | .111 |
| Median (IQR) | 5.0 (1.0-9.0) | 5.5 (3.0-10.0) | 4.0 (1.0-12.0) | 7.0 (4.0-12.0) | 4.0 (3.0-5.0) | 26.0 (24.0-73.0) | 5.0 (1.0-8.0) | 8.0 (3.0-12.0) | |
| Outpatient care | |||||||||
| Physician's office | |||||||||
| Patients, n (% with any) | 64 (92.8) | 38 (97.4) | 21 (100.0) | 18 (94.7) | 16 (94.1) | 2 (66.7) | 101 (94.4) | 58 (95.1) | .849 |
| Number of visitsb | |||||||||
| Mean (SD) | 6.3 (4.0) | 7.4 (6.3) | 6.3 (3.1) | 5.7 (2.0) | 6.0 (3.6) | 5.0 (1.4) | 6.3 (3.8) | 6.8 (5.3) | .513 |
| Median (IQR) | 6.0 (3.0-9.0) | 6.0 (3.0-10.0) | 5.0 (4.0-8.0) | 6.0 (4.0-7.0) | 5.0 (3.5-9.0) | 5.0 (4.0-6.0) | 5.0 (3.0-9.0) | 9.0 (4.0-8.0) | |
| Emergency room | |||||||||
| Patients, n (% with any) | 14 (20.3) | 10 (25.6) | 2 (9.5) | 2 (10.5) | 4 (23.5) | 0 (0.0) | 20 (18.7) | 12 (19.7) | .876 |
| Number of visitsb | |||||||||
| Mean (SD) | 1.6 (1.9) | 1.3 (0.9) | 1.0 (0.0) | 2.0 (1.4) | 1.0 (0.0) | 0.0 (0.0) | 1.4 (1.6) | 1.4 (1.0) | .974 |
| Median (IQR) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 2.0 (1.0-3.0) | 1.0 (1.0-1.0) | 0.0 (0.0-0.0) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | |
| Other outpatient visits | |||||||||
| Patients, n (% with any) | 50 (72.5) | 37 (94.9) | 19 (90.5) | 18 (94.7) | 12 (70.6) | 3 (100.0) | 81 (75.7) | 58 (95.1) | .001 |
| Number of visitsb | |||||||||
| Mean (SD) | 3.6 (2.9) | 4.8 (5.1) | 2.2 (2.0) | 3.1 (2.2) | 4.0 (4.5) | 2.3 (0.6) | 3.3 (3.0) | 4.1 (4.3) | .232 |
| Median (IQR) | 3.0 (2.0-5.0) | 3.0 (2.0-5.0) | 1.0 (1.0-3.0) | 3.0 (2.0-4.0) | 2.0 (1.5-4.5) | 2.0 (2.0-3.0) | 2.0 (1.0-4.0) | 4.0 (2.0-4.0) | |
Abbreviations: IQR, interquartile range; PSC, peristomal skin complication.
aUnless otherwise indicated, all values are mean (SD).
bAmong patients receiving this service.
Figure 1.
Time to peristomal skin complication, by type of ostomy surgery.
Information on healthcare utilization over the 120-day period following ostomy surgery is presented in Table 2 for patients with and without evidence of PSCs. Information on healthcare costs is provided in Table 3. Patients with PSCs were more likely to be rehospitalized following their index admission (55.7% vs 35.5%, respectively; P = .011). Patients with PSCs who were readmitted to the hospital did not have significantly longer stays than did those without PSCs (11.0 days for readmissions with evidence of PSCs vs 6.8 days for those without such evidence; P = .111). The mean (SD) time to first readmission for any reason was 42 days among patients with PSCs versus 58 days for patients without PSCs (P = .0399). The mean number of outpatient visits was broadly similar in the 2 groups (P = .513). Among the 72 patients who were rehospitalized during the 120-day period of follow-up, 21 underwent closure procedures; the mean time to hospital readmission for closure of stoma for these 21 patients was 83 days.
TABLE 3. Healthcare Costs During 120-Day Period Following Ostomy Surgery, by Absence/Presence of PSC (Analyses Based on Administrative Data).
| Colostomy | Ileostomy | Urinary Diversion | All Subjects | P | |||||
|---|---|---|---|---|---|---|---|---|---|
| No PSC (N = 69) | PSC (N = 39) | No PSC (N = 21) | PSC (N = 19) | No PSC (N = 17) | PSC (N = 3) | No PSC (N = 107) | PSC (N = 61) | ||
| Inpatient care | |||||||||
| Index hospitalization | |||||||||
| Mean (SD) | 36,033 (38,300) | 34,995 (27,401) | 52,592 (48,842) | 52,000 (31,831) | 29,018 (5,982) | 43,006 (31,702) | 38,168 (38,133) | 40,686 (29,577) | .635 |
| Median (IQR) | 23,391 (17,679-43,601) | 26,717 (15,876-41,679) | 36,727 (22,161-55,453) | 45,798 (29,335-67,726) | 27,020 (25,088-30,434) | 24,985 (24,421-79,611) | 25,369 (18,839-43,601) | 31,484 (19,040-48,001) | |
| Readmissions | |||||||||
| Mean (SD) | 9,763 (25,609) | 8,893 (11,390) | 4,530 (8,639) | 8,540 (13,073) | 2,374 (5,519) | 77,727 (50,524) | 7,562 (21,182) | 12,168 (21,085) | .176 |
| Median (IQR) | 0 (0-11,198) | 4,099 (0-18,156) | 0 (0-6,706) | 0 (0-12,622) | 0 (0-0) | 64,089 (35,423-133,671) | 0 (0-7,570) | 4,361 (0-18,366) | |
| Other inpatient | |||||||||
| Mean (SD) | 178 (614) | 87 (345) | 91 (411) | 378 (794) | 0 (0) | 102 (95) | 133 (528) | 178 (532) | .594 |
| Median (IQR) | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-407) | 0 (0-0) | 118 (0-188) | 0 (0-0) | 0 (0-0) | |
| Total inpatient | |||||||||
| Mean (SD) | 45,974 (52,920) | 43,975 (27,073) | 57,212 (49,205) | 60,918 (38,557) | 31,392 (7,649) | 120,835 (34,908) | 45,863 (48,180) | 53,032 (35,408) | .272 |
| Median (IQR) | 29,101 (19,665-51,403) | 37,104 (23,362-54,891) | 38,715 (22,181-62,196) | 52,963 (32,301-83,043) | 29,491 (25,088-36,073) | 115,033 (89,192-158,280) | 30,496 (22,181-50,387) | 44,746 (30,110-63,477) | |
| Outpatient care | |||||||||
| Mean (SD) | 4,815 (8,081) | 6,458 (6,973) | 6,067 (11,644) | 3,525 (2,546) | 4,846 (6,208) | 1,428 (1,295) | 5,066 (8,576) | 5,297 (5,951) | .838 |
| Median (IQR) | 2,013 (941-4,543) | 4,229 (2,128-7,908) | 2,664 (1,269-3,121) | 3,208 (2,021-4,414) | 2,423 (2,104-4,644) | 1,702 (18-2,564) | 2,387 (981-4,543) | 3,305 (2,021-5,808) | |
| Total care | |||||||||
| Mean (SD) | 50,789 (52,106) | 50,432 (27,411) | 63,279 (47,735) | 64,443 (39,071) | 36,238 (11,047) | 122,263 (33,944) | 50,928 (47,486) | 58,329 (35,057) | .251 |
| Median (IQR) | 35,190 (25,583-58,204) | 45,480 (32,137-62,602) | 51,563 (37,481-65,747) | 52,963 (33,582-83,707) | 36,321 (27,792-42,869) | 117,598 (90,894-158,299) | 36,818 (26,334-58,204) | 49,361 (33,582-68,519) | |
Abbreviations: IQR, interquartile range; PSC, peristomal skin complication.
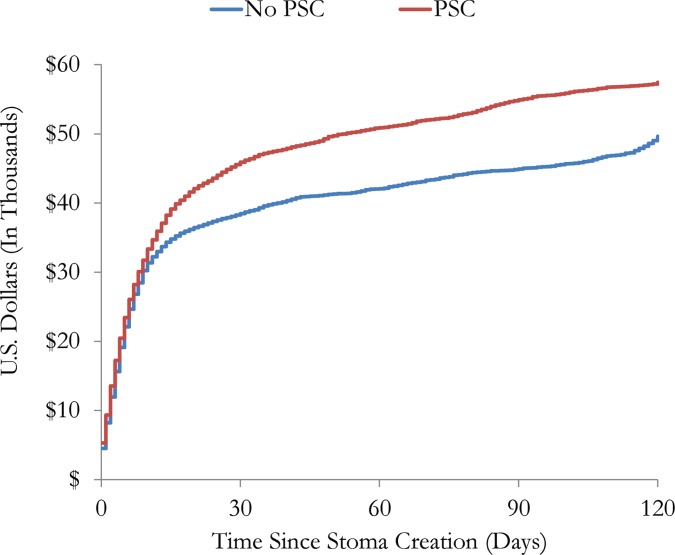
Total healthcare costs over 120 days averaged $58,329 (median = $49,361) among patients with PSCs and $50,928 (median = $36,818) among those without evidence of PSCs (P = .25; Table 3). Inpatient care accounted for the largest share of total costs. Kaplan-Meier sample average estimates of cumulative costs over 120 days by PSC status are presented in Figure 2.
Figure 2.
Mean total cumulative cost from day of ostomy surgery to day 120, by peristomal skin complication status.
DISCUSSION
We conducted a retrospective study at a large integrated healthcare system to examine the risk and economic burden of PSCs among 168 patients who underwent ostomy surgery during a recent 3-year period. We found that approximately one-third of subjects had evidence of PSCs in the 90-day period following surgery. We also found that patients who developed PSCs were more likely to be readmitted to the hospital than those without this complication and that mean total healthcare cost over 120 days was about $7400 higher among patients with PSCs.
Our findings appear to be consistent with those reported in our earlier study based on data from another large integrated US health system.9 In particular, the overall incidence of PSCs following ostomy surgery in this study (36.3%) is almost identical to the rate reported in our earlier study (36.7%) that analyzed data from another US-based healthcare system. Both of these estimates of incidence are within the range of other studies that investigated the economic burden of PSC (10%-70%).4
Our estimates of PSC risk by type of procedure, however, differ from those of prior reports. In a cross-sectional study by Herlufsen and colleagues,12 for example, the incidence of PSCs was found to be highest in patients with an ileostomy (57%), followed by urostomy (48%) and colostomy (35%). Ratliff and Donovan13 assessed all patients who had undergone ileal conduits, ileostomy, and colostomy, respectively, for the presence of PSCs when they returned for their 2-month postoperative evaluation. The incidence of PSCs was 15% among patients with ileal conduits, 9% among those with ileostomies, and 1% among those with colostomy. In this study and our previous investigation,9 we found that the incidence of PSCs was lowest among patients who had undergone urostomy. However, the number of patients undergoing urostomy was low and our study design and duration of follow-up differed from those of prior studies.
Consistent with our earlier findings,9 we found that patients who experienced PSCs were more likely to be rehospitalized over the 120-day period following their index admission (55.7% for patients with PSCs vs 35.5% for those without these complications) and that their length of stay when readmitted was nominally longer (11.0 days for patients with PSCs vs 6.8 days for those with no evidence of PSCs). To the best of our knowledge, no studies other than the present one and our earlier investigation have reported rates of healthcare utilization and costs among patients who experience PSCs in the United States. Several studies have examined the risk of hospital readmission following ostomy surgery, however. For example, Wick and colleagues14 evaluated the risks and costs of hospital readmission following colorectal surgery. Among 1482 patients with ostomies, 37.2% were readmitted to the hospital within 90 days of their index admission; mean length of stay was 8 days. In a study based on Medicare claims data, Gore and colleagues15 reported a 31% rate of readmission over 90 days among urostomy patients. Tyler and colleagues16 examined the rate of readmission within 30 days of surgery for colostomy and ileostomy, respectively, using data from Healthcare Cost and Utilization Project. They reported that approximately 13.5% of colostomy patients and 24.7% of ileostomy patients were readmitted to hospital within 30 days of surgery; corresponding percentages in our study over the 120-day follow-up period were 45.4% and 40.0%, respectively.
In our earlier study, we reported that patients with PSCs had longer and more costly index admissions than those who did not develop these complications (21.5 days for patients with PSCs vs 13.9 days for those without these complications; $161,507 vs $97,817, respectively).9 In this study, however, the cost of index admissions was similar between the 2 groups ($40,686 vs $38,168). This difference in cost may be a result of shorter hospital stays in more recent years. This trend toward shorter hospital stays has been widely acknowledged and noted extensively in the literature.17–19 Shorter hospital stay may be attributed to improvements in surgical techniques, more planned versus emergent surgeries, more aggressive case management following surgery along with discharge-aimed guidelines upon admission, and rehabilitation in transitional care units and in patients' homes versus in the acute care setting. We suspect these factors explain why healthcare costs between patients with PSCs and those without this complication were higher in our earlier study than in the present one.
LIMITATIONS
Limitations of our study should be noted. Our sample was small and apparent variability in our results (eg, between procedures) may only reflect “noise” in the data. Second, it is important to bear in mind that patients with PSCs may differ in many important respects from those who do not develop these complications (eg, surgical technique, effluent characteristics, stoma characteristics, body mass index, comorbid disease processes) and that differences in healthcare utilization and costs that we observed in the 2 groups simply may reflect the effects of confounding. Third, our data were collected via retrospective chart review, and information in patients' medical records can be of variable quality, incomplete, and/or difficult to interpret.
CONCLUSIONS
Approximately one-third of patients in our study developed PSCs within 90 days of ostomy surgery, consistent with findings from earlier studies. Patients with PSCs also were found to have a greater likelihood of hospital readmission. Consistent with findings regarding hospital readmission, total costs of care over 120 days also were nominally (albeit not significantly) higher among patients who experienced PSCs (the difference was >$7000). For patients who have undergone ostomy surgery, prevention of PSCs using advanced pouching systems, optimized education, and ongoing communication during the transition to home may provide opportunities for improved outcomes and cost savings.
ACKNOWLEDGMENT
Funding for this research was provided by Hollister Incorporated, Libertyville, Illinois.
Footnotes
Conflicts of Interest: Ms Taneja and Dr Oster are employed by Policy Analysis Inc (PAI), an independent contract research organization with previous and ongoing engagements with Hollister Incorporated, as well as other biomedical firms. Ms Eaves and Mr Inglese are employed by Hollister Incorporated. Dr Netsch and Ms Rolstad received compensation from webWOC Programs' contractual agreement with PAI for their consultation with respect to this study.
REFERENCES
- 1.United Ostomy Associations of America, Inc (UOAA). About us.http://www.ostomy.org/About_the_UOAA.html. Accessed July 6, 2017.
- 2.Gray M, Colwell JC, Doughty D, et al. Peristomal moisture-associated skin damage in adults with fecal ostomies: a comprehensive review and consensus. J Wound Ostomy Continence Nurs. 2013;40(4):389–399. [DOI] [PubMed] [Google Scholar]
- 3.Nybaek H, Jemec GB. Skin problems in stoma patients. J Eur Acad Dermatol Venereol. 2010;24:249–257. [DOI] [PubMed] [Google Scholar]
- 4.Colwell JC, Ratliff CR, Goldberg M, et al. MASD part 3: peristomal moisture-associated dermatitis and periwound moisture-associated dermatitis. J Wound Ostomy Continence Nurs. 2011;38(5):541–555. [DOI] [PubMed] [Google Scholar]
- 5.Nybaek H, Bang Knudsen D, Norgaard Laursen T, Karlsmark T, Jemec GB. Skin problems in ostomy patients: a case-control study of risk factors. Acta Derm Venereol. 2009;89:64–67. [DOI] [PubMed] [Google Scholar]
- 6.Stokes AL, Tice S, Follett S, et al. Institution of a preoperative stoma education group class decreases rate of peristomal complications in new stoma patients. J Wound Ostomy Continence Nurs. 2017;44(4):363–367. [DOI] [PubMed] [Google Scholar]
- 7.Martins L, Tavernelli K, Sansom W, et al. Strategies to reduce treatment costs of peristomal skin complications. Gastrointest Nurs. 2012;10(10):24–32. [DOI] [PubMed] [Google Scholar]
- 8.Erwin-Toth P, Thompson SJ, Davis JS. Factors impacting the quality of life of people with an ostomy in North America: results from the Dialogue Study. J Wound Ostomy Continence Nurs. 2012;39:417–422. [DOI] [PubMed] [Google Scholar]
- 9.Taneja C, Netsch D, Rolstad BS, Inglese G, Lamerato L, Oster G. Clinical and economic burden of peristomal skin complications in patients with recent ostomies. J Wound Ostomy Continence Nurs. 2017;44:350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Etzioni R, Urban N, Baker M. Estimating the costs attributable to a disease with application to ovarian cancer. J Clin Epidemiol. 1996;49:95–103. [DOI] [PubMed] [Google Scholar]
- 11.Lin DY, Feuer EJ, Etzioni R, Wax Y. Estimating medical costs from incomplete follow-up data. Biometrics. 1997;53:419–434. [PubMed] [Google Scholar]
- 12.Herlufsen P, Olsen AG, Carlsen B, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs. 2006;15(16):854–862. [DOI] [PubMed] [Google Scholar]
- 13.Ratliff CR, Donovan AM. Frequency of peristomal complications. Ostomy Wound Manage. 2001;47(8):26–29. [PubMed] [Google Scholar]
- 14.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54(12):1475–1479. [DOI] [PubMed] [Google Scholar]
- 15.Gore JL, Lai J, Gilbert SM. Readmissions in the postoperative period following urinary diversion. World J Urol. 2011;29:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tyler JA, Fox JP, Dharmarajan S, et al. Acute health care resource utilization for ileostomy patients is higher than expected. Dis Colon Rectum. 2014;57(12):1412–1420. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg MT. Patient education following urinary/fecal diversion. In: Carmel JE, Colwell JC, Goldberg MT, eds. Wound, Ostomy and Continence Nurses Society Core Curriculum: Ostomy Management. Philadelphia, PA: Wolters Kluwer; 2016:131–139. [Google Scholar]
- 18.Lee L, Mata J, Ghitulescu GA, et al. Cost-effectiveness of enhanced recovery versus conventional perioperative management for colorectal surgery. Ann Surg. 2015;262(6):1026–1033. [DOI] [PubMed] [Google Scholar]
- 19.Ratliff CR, Scarano KA, Donovan AM, Colwell JC. Descriptive study of peristomal complications. J Wound Ostomy Continence Nurs. 2005;32(1):33–37. [DOI] [PubMed] [Google Scholar]