Supplemental Digital Content is Available in the Text.
Keywords: Medical adhesive related skin injury, Peristomal, Peristomal skin complications
Abstract
Stomal and peristomal skin complications (PSCs) are prevalent in persons living with an ostomy; more than 80% of individuals with an ostomy will experience a stomal or peristomal complication within 2 years of ostomy surgery. Peristomal skin problems are especially prevalent, and a growing body of evidence indicates that they are associated with clinically relevant impairments in physical function, multiple components of health-related quality of life, and higher costs. Several mechanisms are strongly linked to PSCs including medical adhesive-related skin injuries (MARSIs). Peristomal MARSIs are defined as erythema, epidermal stripping or skin tears, erosion, bulla, or vesicle observed after removal of an adhesive ostomy pouching system. A working group of 3 clinicians with knowledge of peristomal skin health completed a scoping review that revealed a significant paucity of evidence regarding the epidemiology and management of peristomal MARSIs. As a result, an international panel of experts in ostomy care and peristomal MARSIs was convened that used a formal process to generate consensus-based statements providing guidance concerning the assessment, prevention, and treatment of peristomal MARSIs. This article summarizes the results of the scoping review and the 21 consensus-based statements used to guide assessment, prevention, and treatment of peristomal MARSIs, along with recommendations for research priorities.
INTRODUCTION
Creation of an ostomy is a life-changing event, resulting in alterations in body image, urinary or fecal elimination, peristomal skin status, and multiple components of health-related quality of life.1,2 While the exact prevalence is not known, there are estimated to be up to 1 million people with an ostomy in the United States alone.3 The negative effects on health-related quality of life are well documented, and the effects are magnified in individuals experiencing stoma-related complications.1,2,4 More than 80% of individuals with an ostomy will experience some types of stomal or peristomal complications within 2 years of undergoing surgery, with a heightened risk found among those with impaired mobility and/or suffering from obesity.5–7 Taneja and colleagues8 evaluated 128 individuals and found that 36.7% experienced a peristomal skin complication (PSC) during the first 90 days following ostomy surgery; these patients had a higher likelihood of subsequent hospital admissions and health care costs were approximately $80,000 (USD) higher than patients without PSC. Peristomal skin complications vary, with the most common types including peristomal moisture-associated skin damage (MASD), irritant dermatitis, hypersensitivity and allergic responses of the skin, and mechanical damage related to the use of medical adhesives in various pouching systems.9
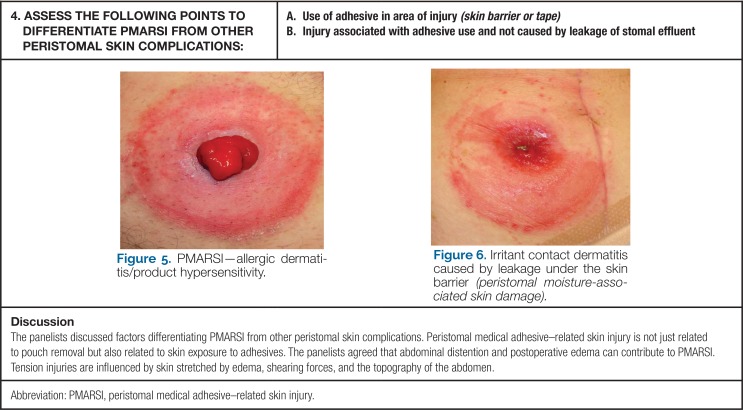
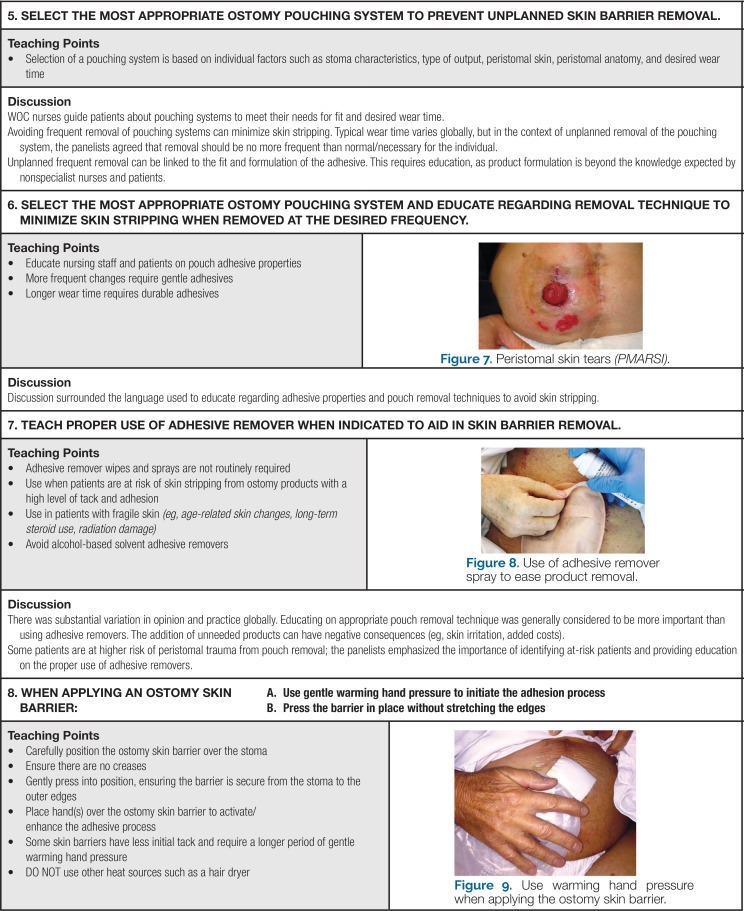
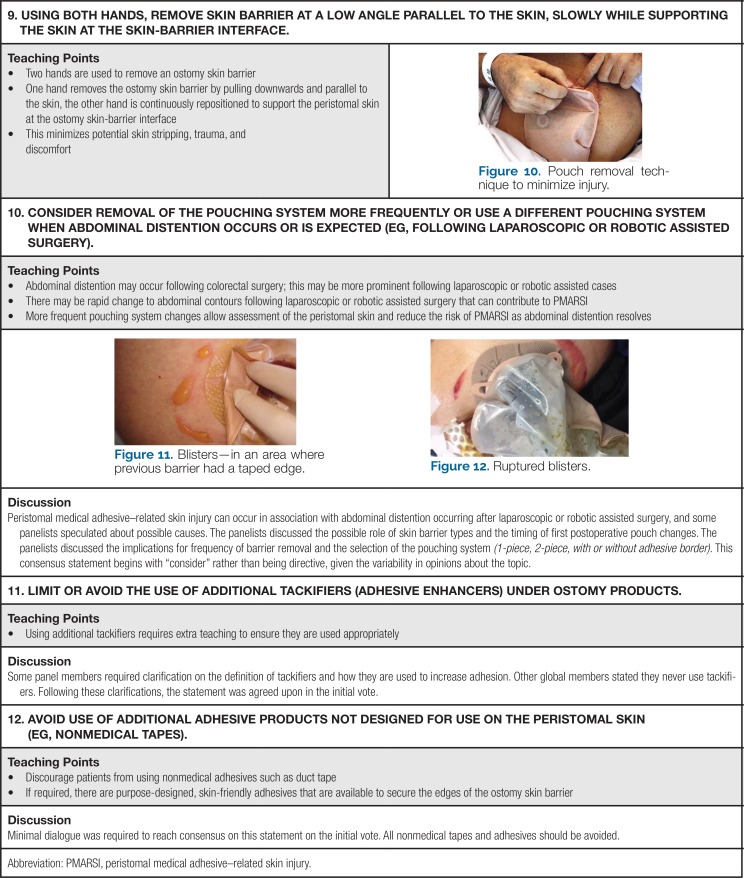
McNichol and colleagues10 reviewed the literature and found that skin injuries related to medical adhesives are prevalent but underreported. They defined medical adhesive-related skin injuries (MARSIs) as any alteration in skin integrity characterized by erythema and/or other skin damage including skin tears, erosion, bulla, or vesicle that persists for 30 minutes or more after removal of a medical device containing adhesive. They identified 3 main types of MARSI: mechanical, dermatitis, and other. Extending the MARSI definition, peristomal medical adhesive-related skin injury (PMARSI) can be defined as an alteration in skin integrity with erythema and/or other skin alterations such as skin tears, erosion, bulla, or vesicle that is apparent after removal of an adhesive ostomy pouching system. Our definition does not include the 30-minute assessment period promulgated by McNichol's group because many individuals with an ostomy cannot leave their ostomy pouching system off for such a prolonged period of time. We hypothesize that skin stripping, defined as removing or tearing of the epidermis with removal of the adhesive faceplate, is a particularly prevalent form of PMARSI. Though evidence is lacking, we have observed that these injuries are frequently associated with unintentional traumatic removal of adhesive products. Patient teaching is an essential prevention strategy for this type of peristomal complication. Other prevalent forms of PMARSI include tension injuries or blisters. They are usually caused by shearing forces due to distension of the skin beneath an adhesive product that does not stretch. Peristomal tension injuries are often associated with postoperative peristomal edema.10
In a recent consensus document, the International Skin Tear Advisory Panel (ISTAP) defined skin tears as traumatic wounds attributable to mechanical forces such as removal of adhesives.11 The ISTAP classified skin tear severity into 3 types: type 1 tears are linear losses of skin flaps with no loss of skin that can be repositioned so that they cover the wound bed; type 2 tears are characterized by partial loss of the skin so that the flap of residual skin does not cover the wound base when repositioned; and type 3 tears are characterized by total loss of the flap. Peristomal skin tears occur predominantly when the adhesive portion of the pouching system is removed from the skin. The amount of force required to cause skin injury depends on the individual's overall risk factors for skin tear development and related factors such as adhesive forces required to remove a particular pouch and use of additional adhesive products of adhesive enhancing product on the peristomal skin.
Irritant contact dermatitis is the development of erythema, edema, and possible vesicles to the peristomal skin as a result of contact with chemical irritants.9,10 Peristomal irritant contact dermatitis may occur when stool or urine is trapped under an adhesive (as with peristomal moisture-associated dermatitis), or it may be attributable to irritants in the adhesive product.10
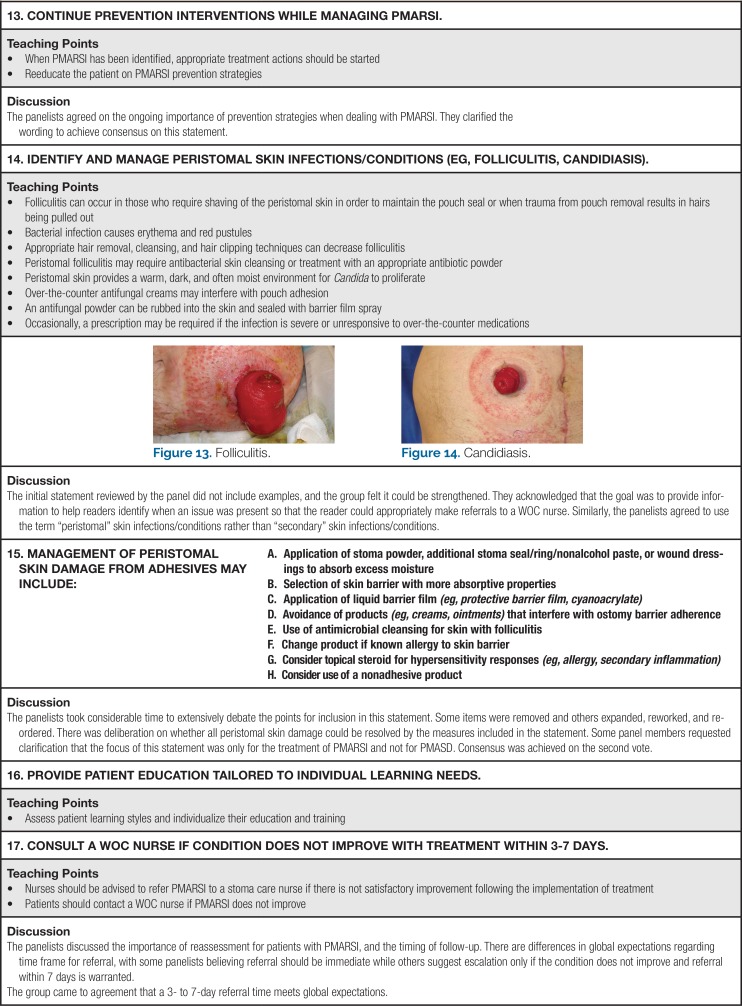
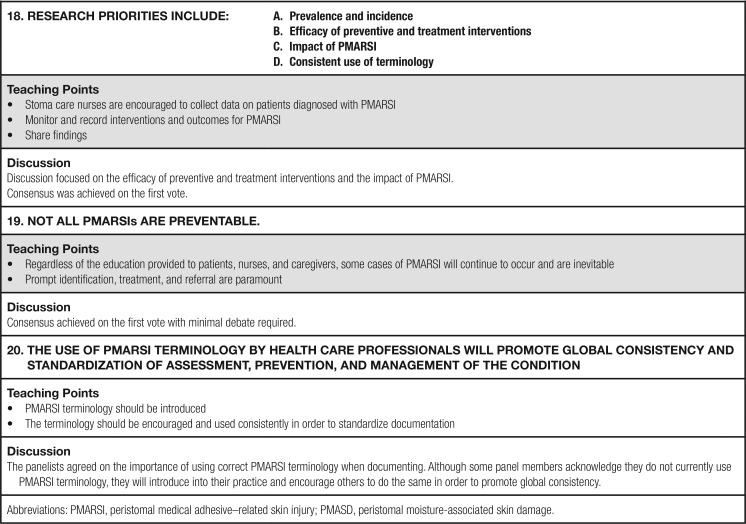
Allergic dermatitis seen in PMARSI is a cell-mediated immunologic response to an adhesive and may appear as areas of erythema. In contrast, vesicular pruritic dermatitis corresponds to the area of exposure. Maceration can result from moisture (stoma effluent, serosanguinous fluid, or perspiration) being trapped under adhesive products, making the skin more susceptible to injury. Folliculitis is another consequence of PMARSI consisting of an inflammatory reaction in the hair follicle caused by entrapped bacteria or by traumatic hair removal. Folliculitis presents as pustules or papules surrounding the hair follicles.
Clinicians have identified MARSI as an important area for research and education.12 In response to the dearth of evidence about PMARSI and its presumed prevalence, a consensus panel was brought together to identify areas of agreement and gaps in knowledge related to PMARSI. The panel used a structured and guided process leading to 21 consensus statements focusing on the assessment, prevention, management, and research priorities regarding PMARSIs. The consensus meeting was sponsored by Hollister Incorporated (Libertyville, Illinois).
SCOPING LITERATURE REVIEW
Prior to the meeting, panelists reviewed a summary of current literature relevant to MARSI and ostomy care. The literature summary was based on a scoping review of publications indexed in CINAHL and MEDLINE electronic databases during the 10-year period prior to the meeting date. Search terms were “peristomal wounds,” “medical adhesive-related skin injury,” “peristomal skin tear,” “skin tear,” and “adhesive skin injury.” Inclusion criteria were research reports using an experimental, quasi-experimental design, best practice guidelines, systematic, scoping or integrative reviews, consensus documents, or chapters from academic references. Elements were restricted to works published in the English language. Individual case studies and abstracts were excluded. Prior to the meeting, panel members were encouraged to provide any relevant literature in their own languages for translation and review prior to the consensus meeting. One hundred six papers were initially identified and their abstracts were reviewed for relevance by 3 individuals (K.L., G.S., M.G.); disagreements concerning relevance to PMARSI were resolved by discussion. Ten elements were identified for additional review, and 8 met criteria for inclusion; they included 3 original research studies (2 cross-sectional surveys and 1 epidemiologic study), 2 consensus meetings (one provided guidelines for all forms of MARSI and one provided additional guideline specific to WOC nurses), and 2 integrative literature reviews (Table 1).10,12,14–19
TABLE 1. Scoping Literature Review Study.
| Reference | Study: Design/Type of Literature Review/Practice Guideline | Subjects and Setting | Pertinent Outcomes |
|---|---|---|---|
| Beitz and Colwell13 | Study: Cross-sectional survey, content validation of management options for various peristomal skin complications | 281 WOC nurses practicing in the United States | Nurses specialized in ostomy care ranked interventions for managing stoma and peristomal complications. Highest-ranking interventions for PMARSI relevant conditions were: Peristomal irritant contact dermatitis
Allergic or hypersensitivity response
Peristomal trauma
|
| Beitz and Colwell14 | Study: Cross-sectional survey | 281 WOC nurses practicing in the United States | Analysis of narrative comments received in the survey described previously. Frequently advocated interventions for PMARSI-related conditions were: Peristomal candidiasis
Peristomal folliculitis
|
| Farris et al15 | Study: Epidemiologic study of patients care for in a single-site study on 2 nursing units in the United States | Two inpatient care units in single acute care facility in the United States; data based on 1189 skin assessments over a 28-d data collection period | Measured prevalence of multiple corms of MARSI, including PMARSI over a 28-d period
|
| Lund16 | Integrative literature review | Not applicable | Summarized the challenges of using medical adhesives in premature, full-term, and chronically hospitalized infants Included ostomy pouching systems as relevant medical devices |
| McNichol et al10 | Practice guideline | 23 key opinion leaders | Reported the results of multidisciplinary consensus panel meeting. Participants agreed on 25 statements about assessment, prevention, and management of MARSI and identified gaps in research Included a systematic literature review of topic |
| Ousey and Wasek12 | Study: Cross-sectional survey | 918 clinicians (nurses, community nurses, district nurses, wound care specialty practice nurses, general practice physicians, geriatricians, podiatrists); all clinicians indicated practicing in the United Kingdom | Queried professional opinion of clinician perspectives on medical adhesive-related skin injuries, pertinent findings
|
| Yates et al17 | Consensus | ≥250 WOC nurses practicing in North America | Reported 8 consensus statements about medical adhesives relevant to WOC nursing. Included a review of the state of the science in adhesive product technology Authors recommend conducting point prevalence for MARSI and taking action based on data |
| Zulkowski18 | Integrative literature review | Not applicable | Described types of skin damage relevant to WOC nursing practice, distinguishing characteristics and general recommendations for prevention and treatment |
Abbreviations: MARSI, medical adhesive-related skin injury; PMARSI, peristomal medical adhesive-related skin injury.
Beitz and Colwell13,14 surveyed 281 WOC nurses practicing in the United States concerning stomal and peristomal complications and their management. The questionnaire included forced-choice responses submitted to content validation procedures and open-ended items subjected to a descriptive, quantitative analysis. Findings from these studies included recommendations for management of various forms of PMARSI including irritant contact dermatitis, allergic contact dermatitis, peristomal skin damage, candidiasis, and folliculitis.
Farris and colleagues15 reported an epidemiologic study of various forms of MARSI, including PMARSI, on 2 inpatient units in a single acute care facility in the Midwestern United States. They reported multiple outcomes for various forms of MARSI, including daily prevalence of any form of MARSI, prevalence by type of MARSI (including prevalence of PMARSI), location and prevalence of MARSI, and proportion of medical devices with adhesive associated with MARSI. They identified 2 MARSI events associated with pouching systems.
Ousey and Wasek12 reported findings from a cross-sectional survey of 918 British nurses concerning their professional opinions related to MARSI, including prevalence of “fragile skin” and causes of skin injury including MASD, pressure/shear, and MARSI. Respondents estimated that more than half of their patients (60.6%) have fragile skin. While MARSI was recognized as a common cause of skin injury, 70.5% indicated that they did not document its presence as part of routine charting.
Two articles included in our scoping review were practice guidelines.10,17 McNichol and colleagues10 generated 25 statements providing guidance for MARSI that focused on assessment, prevention, selection, application, and removal of adhesive products, treatment, and future research directions for MARSI. This guideline is intended for all clinicians and all care settings. Yates and colleagues17 reported results of a consensus process conducted that focused on various aspects of MARSI pertinent to WOC nursing practice. Building on the earlier statements promulgated by McNichol's group,10 a task force of 3 individuals produced 8 consensus statements specific to WOC nursing practice. Key assessments involved in distinguishing MARSI from other types of skin injury were provided, underscoring the importance of completing a focused history and examination with users of any adhesive products. Agreement was reached on the appropriate methods for removal of adhesive products, methods of application of ostomy skin barriers, and avoidance of additional adhesive enhancers (tackifiers) under ostomy products. Two statements relevant to the use of adhesives in areas of edema around wounds may also be relevant in ostomy care, particularly in settings where laparoscopic and robotic assisted surgeries are common.
Lund16 discussed use of medical adhesive devices in neonates and infants, including premature infants. This integrative review reported the myriad challenges associated with the use of adhesives in this extreme of age, including use of ostomy pouches. Zulkowski18 reviewed the literature related to MASD, MARSI, and skin tears. This integrative review identified research-based evidence and expert opinion concerning distinguishing characteristic of these various forms of skin damage and provide general recommendations for prevention and treatment.
Considered collectively, findings of our scoping review indicated sparse research specific to MARSI and PMARSI (Table 1). This paucity in research is reflected in variability of terminology used to identify MARSI, low rates of documentation of skin injuries attributed to medical adhesives, absence of instruments to measure presence and severity of various forms of MARSI, and lack of guidelines for its assessment, prevention, and care. Two documents provided guidelines for caring of patients with MARSI,10,17 but both indicated recommendations were based on a formal consensus of expert opinion rather than research-based evidence. The 3 original research reports were cross-sectional surveys that investigated professional opinions related to nomenclature, clinical relevance, prevalence, and preferred prevention and management strategies for PSCs and MARSI. No randomized or nonrandomized clinical trials were reported that compared any intervention for MARSI or PMARSI with placebo or a comparison intervention. In addition, 2 of the 3 original research reports and both practice guidelines were limited to North American respondents and experts. Based on this review, we concluded that an international consensus building process was needed to provide additional guidance for assessment, prevention, and management of the various forms of MARSI and to identify gaps in knowledge and priorities for additional research.
CONSENSUS CONFERENCE
Using structured processes as outlined by Murphy and coworkers,19 14 expert panelists from 9 countries (Box 1) were convened to review, discuss, and vote on proposed consensus statements related to assessment, prevention, treatment, and research priorities for PMARSI. In an effort to create a diverse panel, participants were invited based on their clinical expertise in stoma care, practice settings, and countries of origin. The panelists represented a broad range of practice settings, including private practice, community, and acute care; all worked with adult patients and had expertise with stoma care products and their use. Their credentials included WOC nurse, ET nurse (now NSWOC), stoma care nurse, and stoma therapy nurse. We will subsequently refer to panelists as WOC nurses. Panelists' experience ranged from 7 to 41 years, with a median of 20 years. The panel members practiced in Australia, Canada, and Denmark, France, Germany, Italy, Japan, the United Kingdom, and the United States. The meeting was conducted in English and held in Windsor, United Kingdom.
BOX 1.
Consensus Panel Members
The meeting was moderated by a doctoral-prepared nurse practitioner with experience in facilitation and general knowledge of MARSI and PMARSI (M.G.). A smaller group (K.L., G.S., M.G.) wrote proposed statements in advance of the meeting to expedite panel discussion and voting; in addition, panelists were encouraged to propose their own statements during the latter part of the meeting. The glossary of terms used by the panelists is shown in Table 2. An electronic audience response system was used to allow anonymity when voting. Individual statements were read by the moderator and then discussed by the panel members. Each proposed statement was introduced to the panel, followed by a short initial discussion for clarification of intended meaning. The panelists then voted to accept the statement as written. If the statement was accepted as written by 80% of panelists (11 of 14), consensus was achieved. If less than 80% of panelists accepted the statement as originally proposed, the facilitator led a discussion designed to revise the statement to achieve agreement among no less than 80% of panelists. This process continued for up to 3 rounds of discussion; if the group was unable to reach consensus after 3 rounds of discussion and revision, the statement was classified as “unable to reach consensus” and removed from additional consideration. Upon completion of voting for each of the statements, the panel reviewed all final statements to confirm they were comprehensive and reflected their discussions accurately.
TABLE 2. Glossarya.
| Term | Definition |
|---|---|
| Allergic contact dermatitis | Immunologic response to an irritant or allergen; presents with peristomal papules and vesicles, redness, discoloration, oozing or dryness, burning, or itching |
| Bulla/vesicle | Blisters containing clear fluid; in the peristomal skin, they often present as circumscribed epidermal elevations <0.5 cm in diameter; vesicles >0.5 cm classified as bulla |
| Erosion | Partial or complete loss of the epidermis of the skin resulting in a denuded, moist surface; given proper treatment, eroded skin will heal by primary intention (ie, without scarring) |
| Folliculitis | Pustular lesions and inflammation of the hair follicles |
| Irritant contact dermatitis | Inflammation, with or without erosion, attributable to exposure to stoma effluent, chemical preparations including solvents, skin cleansers or adhesives may present with papules and vesicles, redness or discoloration, oozing or dryness, erythema, edema, or epidermal loss |
| Maceration | Softening and breakdown of skin resulting from prolonged exposure to moisture; affected skin is soft, pale, and wrinkled; patients may complain of pain or itching |
| Peristomal moisture-associated skin damage | Inflammation and/or denudation of the skin adjacent to a stoma associated with exposure to urinary or fecal effluent |
| Skin (epidermal) stripping | Removal of the stratum corneum typically due to removal of a medical adhesive (ostomy skin barrier) |
| Skin tear | Traumatic skin injury caused by mechanical forces, such as removal of the skin barrier of a pouching system containing adhesives. Skin tears may be classified based on depth; they do not extend through the subcutaneous layer |
| Tension injury | Blisters caused by shearing forces as the skin interacts with an inflexible adhesive ostomy barrier; may be associated with postoperative abdominal distention and/or peristomal edema. |
The panel reached consensus on 21 statements about PMARSI, covering assessment (Box 2), prevention (Box 3), management (Box 4), and research priorities. The consensus meeting was characterized by rich discussion of factors affecting clinicians' efforts to prevent and manage PMARSI within their practices in health care systems that varied (in some cases widely) between countries (see Supplemental Digital Content 1, available at: http://links.lww.com/JWOCN/A49).
BOX 2.
Assessment for PMARSI
BOX 3.
PMARSI Prevention
BOX 4.
Management of PMARSI
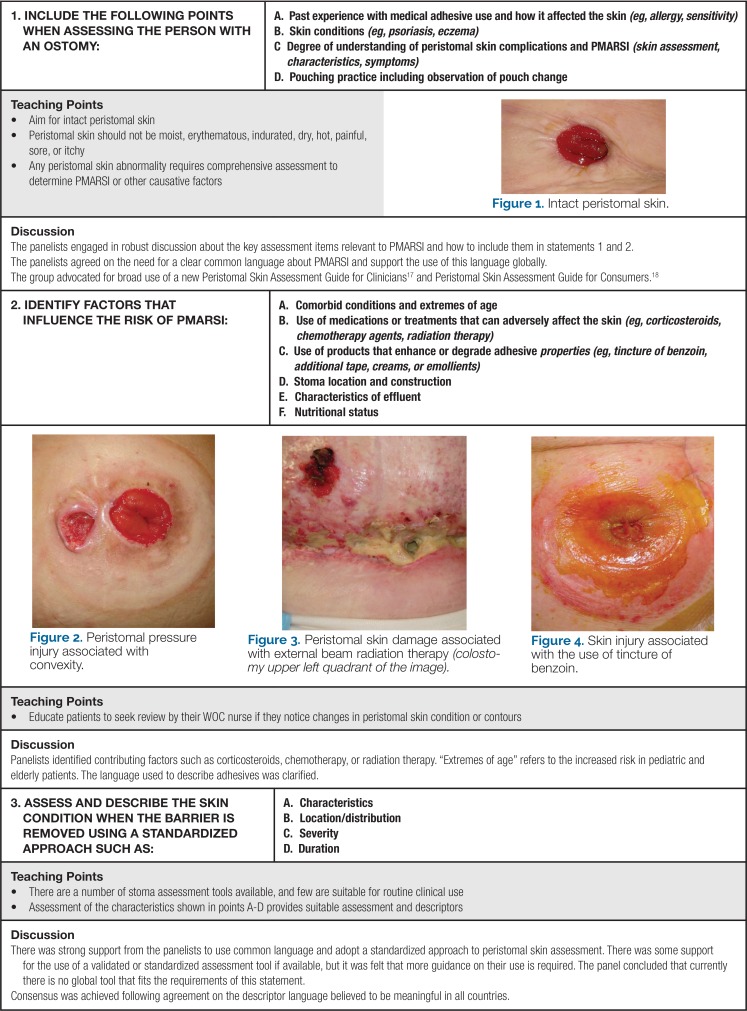
Assessment
Box 2 presents the 4 consensus statements outlining best practice for assessment of PMARSI, along with highlights of the panel discussion, and illustration of normal peristomal skin and PMARSI. Skin assessment is a foundational component of identifying and preventing PSCs. A complete assessment should include a detailed history of previous PSCs, underlying skin conditions such as psoriasis or eczema, and previous pouching practices. The clinician should take note of factors known to contribute to PMARSI such as comorbid conditions, extremes of age, use of medications known to adversely affect the skin, use of products that increase or degrade adhesive properties, stoma location and construction, characteristics of effluent, and nutritional status. Whenever possible, these factors should be managed to minimize the individual's susceptibility to PMARSI or other PSCs.
Ideally, peristomal skin assessment is conducted using a validated method.20 Unfortunately, no validated instrument for assessing PSCs has achieved widespread acceptance in clinical practice and none of the existing tools address PMARSI in its entirety.10 Assessments should be completed to ensure that other causes of PSCs, such as disease-related complications, are ruled out when assessing PMARSIs. The Ostomy Skin Tool is a validated peristomal skin assessment tool developed as a standardized measuring instrument for assessing the extent and severity of peristomal skin damage; however, the tool does not specifically address mechanical injury.21 The tool is designed to assess peristomal skin at a particular point in time and determine if there has been improvement or degradation over time. Skin condition is described in 3 domains: discoloration (D), erosion (E), and tissue overgrowth (T). Each section is scored and combined to give a total score out of 15. Greater scores are indicative of greater PSCs.
A second validated tool is the Study on Peristomal Skin Lesions (SACs) tool. The tool was developed in an attempt to standardize the language for the assessment and classification of PSCs. The tool identifies the type and location of PSCs. It was revised and published as SACs 2.0 in 2016.22
Woo and associates23 developed a mnemonic teaching tool (MINDS) that categorizes peristomal skin injury into classifications of tissue injury: mechanical (M), infection (I), noxious/chemical irritants (N), diseases (D), and skin allergens (S). The MINDS framework is limited in that it restricts mechanical peristomal skin injury to skin stripping, with no focus on the other aspects of skin injury related to MARSI. The tool has not been validated.
Pittman and associates24 developed and evaluated psychometric properties of the Ostomy Complication Severity Index. This 9-item tool was designed to evaluate multiple stomal and peristomal complications, along with leakage from the pouching system. One item queries a prevalent PSC, irritant dermatitis (peristomal MASD), and the related factor of ostomy pouch leakage. The instrument does not evaluate other PSCs such as PMARSI.
McCann25 reported development and content validity testing of an instrument designed to aid in the description of peristomal skin disorders based on their depth and location based on the stoma as a central reference point. Depth is measured on a scale of L1 to LX, and the location is measured using a clock face, with the stoma acting as the central point on the clock, with 12 o'clock lying in a straight line superior to the stoma, and 6 o'clock in a straight line inferior to the stoma. This instrument was designed to describe rather than identify the underlying etiologies of PSCs such as PMARSI.
As part of an enhanced recovery after surgery project, Miller and coworkers26 emphasized that health care professionals, persons with an ostomy, and their caregivers must be able to identify potential causes for PSCs and be aware of the available resources should issues arise. The expert panel concurred that health care professionals, individuals, and their caregivers should be educated on the assessment of PMARSI and what actions to take if a PMARSI occurs.
Prevention
Consensus statements, discussion, teaching recommendations, and relevant photographs of the peristomal skin relevant to prevention of PMARSI are presented in Box 3. Determination of what is normal is an important component when assessing peristomal skin health. Rolstad and Erwin-Toth27 asserted that many persons with ostomies and their health care professionals frequently perceive PSCs as an inevitable part of living with an ostomy. A robust discussion among the panelists focused on the need for routine assessment of the peristomal skin at every pouching, regular reporting of abnormal findings to a health care professional, and prompt intervention when PSCs occur. Furthermore, while a screening assessment of the peristomal skin is neither complex nor time-consuming, a parsimonious and methodical approach is needed.
Selection of a pouching system that meets individuals' needs is appropriate for their ostomy type and abdominal skin contours and is well fitted for their stoma is a fundamental component of PSC prevention.28 The selection of a pouching system is based on individual patient circumstances including assessment of the stoma, ostomy effluent, peristomal skin, peristomal anatomy, and desired wear time. Persons with ostomies, caregivers, and health care professionals should possess basic knowledge of strategies to apply, empty and change a pouching system, ensure its proper fit, and identify circumstances when referral to a stoma care specialist is warranted before PSCs occur.
Management
Box 4 presents consensus statements, highlights of panel discussion, and pertinent images relevant to management of PMARSI. Early recognition of PMARSI or any PSC and prompt referral to a nurse specializing in ostomy care before PMARSI worsens are essential for effective management of PMARSI. Management of any PSC including PMARSI begins with identifying and removing modifiable contributing factors.28 Once the cause has been removed or minimized, management strategies can be put in place. Prevention and management strategies are closely linked. Management of PMARSI includes assessment of the individual's technique when applying or removing the skin barrier (ostomy faceplate). Management is based on identification of the type of PMARSI (skin stripping, tension injury, skin tear, irritant/allergic contact dermatitis, maceration, and folliculitis). Health care professionals, individuals, and/or their caregivers should be advised to refer PMARSI to a nurse specialized in ostomy care if satisfactory improvement does not occur following initiation of treatment. In order to obtain a greater understanding of the extent of PMARSI and the related complications, ostomy nurse specialists should conduct prevalence and incidence studies to ascertain the true burden of PMARSI on those living with a stoma.
DISCUSSION
A growing body of evidence demonstrates that PSCs, including PMARSI, are associated with increased morbidity and enhanced risk for hospital readmission following stoma surgery, impaired psychosocial status and health-related quality of life, and higher costs to the individual and the health care system.1,2,4,7–9,29 However, individuals living with a PSC may not identify early signs of altered skin integrity as an issue and may not seek the advice of a health care professional until the problem worsens.13,27,30 In order to address the paucity of evidence related to MARSI, and PMARSI in particular, and the need for additional guidance to best practices in this area, an expert panel constructed 21 consensus-based recommendations for the assessment, prevention, and management of PMARSI. While panel members reached consensus related to a number of issues surrounding this area of practice, they also acknowledged the paucity of research in this area and the likelihood that some statements may require revision or rejection as additional research emerges.
CONCLUSION
A global panel of experienced nurses specialized in ostomy care identified key areas of agreement about PMARSI and how to prevent, manage, and investigate this important type of PSC. These 21 recommendations provide the best available guidance for clinical practice and suggest topics for further research.
Supplementary Material
Footnotes
The authors received support from an unrestricted grant from Hollister Incorporated, where Dr Salvadalena is an employee.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (JWOCNOnline.com).
REFERENCES
- 1.Nichols T. Health utility, social interactivity and peristomal skin status: a cross-sectional study. J Wound Ostomy Continence Nurs. 2018;45(5):438–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichols TR. Quality of life in persons living with an ostomy assessed using the SF36v2: mental component summary vitality, social function, role-emotional and mental health. J Wound Ostomy Continence Nurs. 2016;43(6):6161–7122. [DOI] [PubMed] [Google Scholar]
- 3.UOAA. Living with an ostomy: FAQs. https://www.ostomy.org/living-with-an-ostomy. Accessed October 22, 2018.
- 4.Nichols TR. Quality of life in US residents with ostomies as assessed using the SF36v2. J Wound Ostomy Continence Nurs. 2015;42(1):71–78. [DOI] [PubMed] [Google Scholar]
- 5.Pittman J, Kozell K, Gray M. Should WOC nurses measure health-related quality of life in patients undergoing intestinal ostomy surgery? J Wound Ostomy Continence Nurs. 2009;36(3):254–265. [DOI] [PubMed] [Google Scholar]
- 6.Almutairi D, LeBlanc K, Alvai A. Peristomal skin complications: what dermatologists need to know. Int J Dermatol. 2018;57(3):257–264. [DOI] [PubMed] [Google Scholar]
- 7.Colwell JC, Pittman J, Raizman R, Salvadalena G. A Randomized Controlled Trial Determining Variances in Ostomy Skin Conditions and the Economic Impact (ADVOCATE Trial). J Wound Ostomy Continence Nurs. 2018;45(1):37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taneja C, Netsch D, Rolstad BS, Inglese G, Lamerato L, Oster G. Clinical and economic burden of peristomal skin complications in patients with recent ostomies. J Wound Ostomy Continence Nurs. 2017;44(4):350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ratliff CR, Scarana KA, Donovan AM. Descriptive studies of peristomal complications. J Wound Ostomy Continence Nurs. 2005;32(1):33–37. [DOI] [PubMed] [Google Scholar]
- 10.McNichol L, Lund C, Rosen T, Gray M. Medical adhesives and patient safety: state of the science: consensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Continence Nurs. 2013;40(4):365–380. [DOI] [PubMed] [Google Scholar]
- 11.Campbell K, Leblanc K, Woo K. Best practice recommendations for the prevention and management of skin tears in aged skin: an overview. Wounds Int. 2018;45(6):540–542. https://www.woundsinternational.com/download/wint_article/7524. Accessed February 8, 2019. [DOI] [PubMed] [Google Scholar]
- 12.Ousey K, Wasek S. Clinician perspectives on medical adhesive-related skin injuries. Wounds UK. 2016;12(4):42–46. [Google Scholar]
- 13.Beitz JM, Colwell JC. Stomal and peristomal complications: prioritizing management approaches in adults. J Wound Ostomy Continence Nurs. 2014;41(5):1–10. [DOI] [PubMed] [Google Scholar]
- 14.Beitz JM, Colwell JC. Management approaches to stomal and peristomal complications: a narrative descriptive study. J Wound Ostomy Continence Nurs. 2016;43(3):263–268. [DOI] [PubMed] [Google Scholar]
- 15.Farris MK, Petty M, Hamilton J, Walters SA, Flynn MA. Medical adhesive-related skin injury prevalence among adult acute care patients: a single-center observational study. J Wound Ostomy Continence Nurs. 2015:42(6):589–598. [DOI] [PubMed] [Google Scholar]
- 16.Lund C. Medical adhesives in the NICU. Newborn Infant Nurs Rev. 2014;14(4):160–165. [Google Scholar]
- 17.Yates S, McNichol L, Heinecke SB, Gray M. Embracing the concept, defining the practice, and changing the outcome: setting the standard for medical adhesive-related skin injury interventions in WOC nursing practice. J Wound Ostomy Continence Nurs. 2017;44(1):13–17. [DOI] [PubMed] [Google Scholar]
- 18.Zulkowski K. Understanding moisture-associated skin damage, medical adhesive-related skin injuries, and skin tears. Adv Skin Wound Care. 2017;30(8):372–381. [DOI] [PubMed] [Google Scholar]
- 19.Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess. 1998;2(3):i–iv, 1-88. [PubMed] [Google Scholar]
- 20.Haugen V, Ratliff C. Tools for assessing peristomal skin complications. J Wound Ostomy Continence Nurs. 2013;40(2):131–134. [DOI] [PubMed] [Google Scholar]
- 21.Martins L, Ayello EA, Claessens I, et al. The ostomy skin tool: tracking peristomal skin changes. Br J Nurs. 2010;19(15):930, 932-934. [DOI] [PubMed] [Google Scholar]
- 22.Antonini M, Arena R, Mancini S, et al. Peristomal skin changes: what treatment should be adopted? Results of an observational multi-centre study. WCET J. 2018;38(1):30–34. [Google Scholar]
- 23.Woo KY, Sibbald RG, Ayello EA, et al. Peristomal skin complications and management. Adv Skin Wound Care. 2009;22:522–532. [DOI] [PubMed] [Google Scholar]
- 24.Pittman J, Bakas T, Elliott M, Sloan R, Rawl SM. Psychometric evaluation of the ostomy complication severity index. J Wound Ostomy Continence Nurs. 2014;41(2):147–157. [DOI] [PubMed] [Google Scholar]
- 25.McCann E. The ostomy files: a content-validated tool to effectively document peristomal skin lesions. Ostomy Wound Manage. 2010;56(10):22–38.21030726 [Google Scholar]
- 26.Miller TE, Thacker JK, White WD. et al; Enhanced Recovery Study Group. Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118(5):1052–1061. [DOI] [PubMed] [Google Scholar]
- 27.Rolstad BS, Erwin-Toth PL. Peristomal skin complications: prevention and management. Ostomy Wound Manage. 2004;50(9):68–77. [PubMed] [Google Scholar]
- 28.Goldberg M, Colwell J, Burns S, et al. WOCN Society Clinical Guideline: management of the adult patients with a fecal or urinary ostomy: an executive summary. J Wound Ostomy Continence Nurs. 2018;45(1):50–58. [DOI] [PubMed] [Google Scholar]
- 29.Neil N, Inglese G, Manson A, Townshend A. A cost-utility model of care for peristomal skin complications. J Wound Ostomy Continence Nurs. 2016;43(10):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WOCN Society. Peristomal skin assessment guide for clinicians. psag.wocn.org/index.html#home. Accessed October 15, 2018.
- 31.Online medical dictionary. https://www.online-medical-dictionary.org. Accessed December 15, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.