Abstract
Group consultations are an important care option that is starting to gain traction in the USA and Australia. This review summarises the likely benefits accruing from a systems approach to implementing group consultations widely in the NHS and other socialised healthcare systems. Existing evidence is mapped to five distinct systems approaches: (1) development; (2) different age groups; (3) patient-centred pathway of care; (4) NHS system changes; and (5) education. Implications are discussed for patients and staff, who both benefit from group consultations once embedded; ranging from improved access and efficiency to more enjoyable multidisciplinary team working, improved resource management, and maintained/better outcomes. Moreover, even patients who don't attend group consultations can benefit from system effects of long-term implementation. Changing behaviour and health systems is challenging, but change requires systematic experimentation and documentation of evidence. We conclude that group consultations have unique potential for delivering system-wide benefits across the NHS.
KEYWORDS: Group consultation, shared medical appointment, group clinic
Introduction
Group consultations are an important care option that is starting to gain traction in the USA and Australia, with some practise now in the UK.1–11 Group consultations are an overarching term to describe care models where several patients are seen by one or more clinicians concurrently. They can be contrasted with conventional models of care: usual 1:1 clinics; education groups where only education is delivered; and round robin annual review clinics, with serial 1:1 consultation. Group consultations are used to manage the rising burden of chronic conditions like diabetes.12
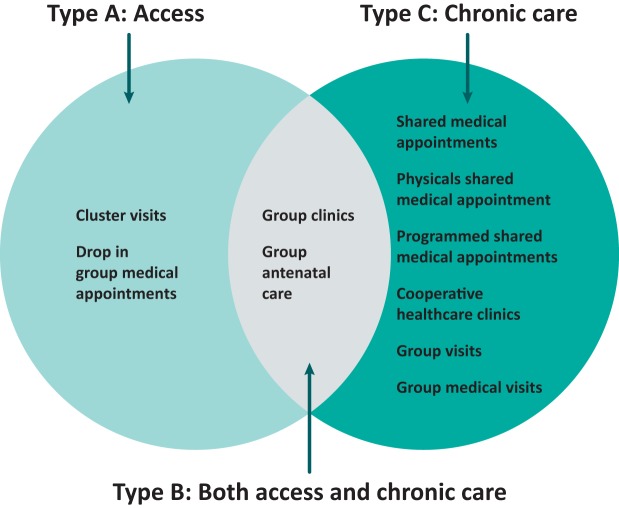
Ideally, group consultations should deliver all the care options available through usual models, plus the unique benefits of peer support. There are many different labels, but group consultation models share more similarities than differences. We will classify group consultation models (Fig 1) into those that improve access (type A, for access);13,14 those that deliver continuity for chronic conditions (type C, for continuity);11,15–18 and a subgroup of hybrid group consultations models that deliver both (type B, for both).19,20
Fig 1.
Group consultation models.
In a type A group care model aimed at improving access for pregnant women, patients could attend a ‘drop-in group medical appointment’15 or formalised group antenatal care through ‘Centering Pregnancy’20 or ‘Expect With Me’.21 The outcomes are likely to be determined by the scale, and skill of the facilitator and clinician. Type C chronic care in groups is called ‘shared medical appointments’ in the Cleveland Clinic in the USA, which offers them in every department. It is very likely that the key elements or ‘active ingredients’ for behaviour change22 are shared with effective ‘cooperative health care clinics’18 and type B ‘group clinics’ for inflammatory arthritis,23 where both patients with chronic stable and active newly diagnosed or flaring arthritis can be seen together.
The General Practice Development Programme24 and NHS alliance report commissioned by NHS England25 use the term ‘group consultations’: this label is well accepted and understood by NHS patients. We will use this term throughout this review, except where there is evidence that only applies to one of the models.
There is academic, clinical and patient interest in group consultations models. A recent editorial in the British Medical Journal called them ‘a promising response to escalating demand for healthcare’26 and there is national media interest. This transformative innovation, like others, needs four key drivers for effective widespread introduction:27 system specific evidence of value; easy ways to pilot and adapt models; regulatory change or incentives; and relevant patient and clinician education.
We will consider how UK implementation of group consultations has already used the elements of a systems approach described in Engineering Better Care;28 in development, across different age groups, within pathways of care, and embedding the model within the whole NHS integration within undergraduate and postgraduate education.
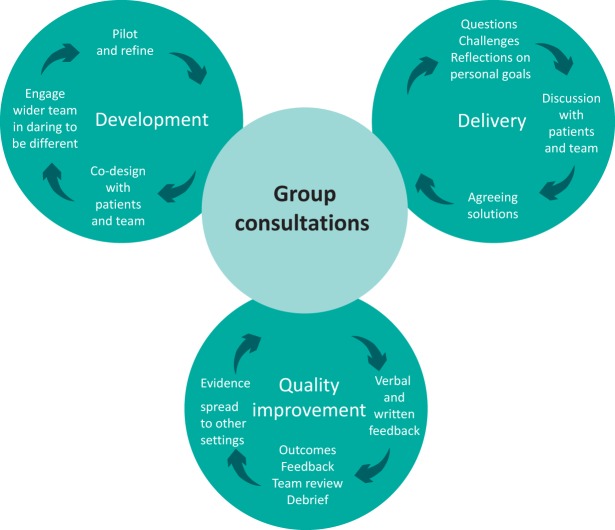
System approach within group consultation development
When introducing a new system, there is an opportunity to design something from scratch, described by Engineering Better Care as ‘iteration before implementation’ and ‘design as an exploratory process’;28 although, most commonly we are improving existing systems. Group consultations are different enough from usual care that they present an unrivalled opportunity to reflect on what works from existing systems; what can be improved and how to best implement and deliver the process and outcomes needed (see Fig 2) using this approach. Group consultations often contain an invaluable internal feedback loop as patient co-design is integral.29 Challenges that arise in a group setting can be solved in a group setting, with patients fully involved. The current UK training model (www.groupconsultations.com) also embeds team and patient reflection, as quality assurance processes, so that continuous learning supports ‘understanding, designing, delivering and maintaining success’.28
Fig 2.
Group consultations as a system.
Patients have been an integral part of the UK co-design process. For example, there was enthusiasm from patients in the first pilot testing of inflammatory arthritis group consultations in Northumbria30 and in primary care in Slough.31 Despite initial concerns about this clinical innovation, the pilot consultations were rated very highly by both patients and staff (median 10/10), equivalent to existing clinics. National recognition with the British Society for Rheumatology Innovation in Development Award 2009, secured agreement to commission the service, so group clinics have been a routine care option since 2010, with 40% of follow-up workload delivered in groups.24 The model has spread organically with three consultants delivering across four hospitals so far. Patient feedback is gathered at each clinic and any challenges discussed during the session with solutions adapting the model agreed, eg the decision to give intramuscular steroid injections during, rather than after, the clinic. Reluctant patients often become enthusiastic once they actually see the model in practice,32 and play a genuine role in understanding, designing, delivering and maintaining success – ‘Systems are centred on people.’28
Successful piloting in community hospitals for consultant-led inflammatory arthritis group consultations raised the question whether other conditions, in other settings, and by other clinicians could be successful. This led to primary care piloting of osteoporosis group clinics led by specialist nurses and pharmacists, and implementation of a randomised controlled trial (RCT) of pharmacist-led groups.32 – ‘Design is an exploratory process.’28
Croydon Clinical Commissioning Group was one of the early UK adopters of primary care group consultations, initially using shared medical appointments in a few practices to pilot successfully for long-term conditions, including diabetes mellitus and chronic obstructive airways disease.33 With increasing experience and recognition that successful group consultations do not have to be restricted to single conditions, (indeed capacity to mix conditions is a critical success factor),17 the model is now being rolled out to all 57 practices – ‘Iteration before implementation.’28
Health Education England has supported regional training in the north west and north east of England for nurse-led group consultation training leading to more than 100 practices having been trained. A regional training model could deliver a step change in uptake nationally across England, although slightly different approaches are needed in Scotland, Wales and Northern Ireland. The chief medical officers of all four home nations and strategy lead for NHS England support the vision: ‘to offer training to every NHS general practice within 5 years, as well as effective use elsewhere along the patient journey’ (personal communication).
Every group consultation raises new questions from patients about their chronic conditions and many answers come from their peers. There are also often questions about the care delivery process and group consultation embeds a process for providing solutions, which both reinforces learning and drives quality improvement. By making outcome collection routine, group consultations can make demonstrating good care easier. What good care looks like in this setting can differ from the expectations of clinicians only used to usual care, so it is important that first-hand experience is triangulated with patient feedback – ‘Thinking changes practice, process helps.’28
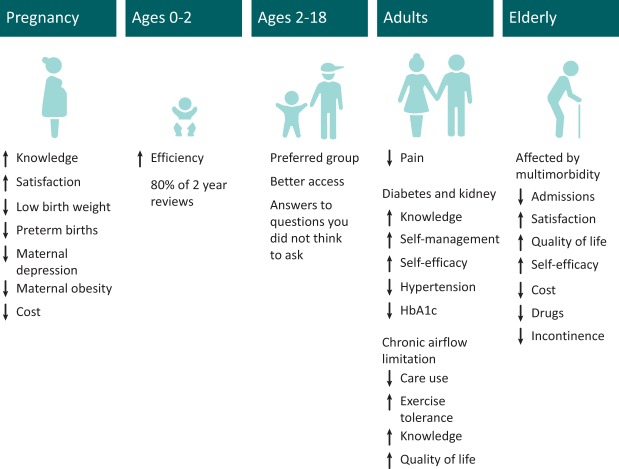
A patient-centred system approach across different age groups
There is growing evidence of high-quality care through group consultations, with outcomes the same as or better than for usual care, across a wide range of healthcare settings and conditions, for both chronic conditions and acute presentations (Fig 3) including perinatal, children, adults and older people.
Fig 3.
Group consultations across different age groups.
Perinatal
Some of the most compelling evidence for group consultation efficacy and cost-effectiveness is from perinatal care where results from several large randomised trials indicate that group consultations increase knowledge, satisfaction, healthier pregnancy weight gain trajectories and postpartum weight loss, and rates of breastfeeding; as well as decrease preterm and small babies for gestational age births, maternal depression, sexually transmitted disease and rapid repeat pregnancy.34,35 There is also evidence of cost savings, with more than US $22,000 for every preterm birth averted as a function of group prenatal care.36 Others have implemented group consultations in prenatal care and shown favourable outcomes for use in special populations such as military personnel and Hispanic women with gestational diabetes. Group prenatal care has been implemented in clinical settings across the USA and throughout the world.
It is important to note that although many studies of group prenatal care have demonstrated improved outcomes relative to standard individual care, a recent meta-analysis indicates there is no difference across studies (combined), in terms of adverse birth outcomes, except for certain subgroups, such as African American women.34 Importantly, there are no adverse effects associated with group prenatal care.35 Based on this existing evidence base, the American College of Obstetricians and Gynecologists recently released its first committee opinion on group prenatal care.37
Children
Hertfordshire NHS Trust found that switching to group 2-year child development review saved 22% of health visitor team time compared to 1:1 reviews. After 12 months, over 80% of 2-year child development reviews were conducted as group reviews.38 Across ages 2–18 years, patients report better care and a preference for groups.39 Feldman first described group consultations in children, which she named ‘cluster visits’.13
Adults
There is growing evidence across a range of chronic conditions. For example, multiple RCTs showing improved outcomes in diabetes group care compared to usual care including tighter HbA1c control, improved hypertension,40 knowledge, self-management, self-efficacy and less consistent effects on weight and cholesterol.4–10 At the same time, a recent review highlights the need for more rigorous scientific evidence for diabetes.7 Groups improve blood pressure, medicine compliance, physical activities, diet, self-reported health and self-efficacy in a trial of 1,024 hypertensive patients.41 They improve exercise tolerance in patients with chronic obstructive pulmonary disease.42 Groups improve knowledge, quality of life and hospitalisations in two small studies in chronic cardiac failure,43,44 and improve diet and low-density lipoprotein levels in coronary artery disease,45 with 82% patients preferring group follow-up after piloting a post-cardiac surgery model.46 Knowledge was improved for patients involved in chronic kidney disease groups and show a trend to better self-management/efficacy in a two site pilot RCT.47 In chronic pain, groups improve pain, sleep quality and perceived stress;48 and reduce cost of acupuncture.49 Mixed chronic disease groups lower emergency care use.50–53 Groups improve patient knowledge and quality of life.23,54 They are safe and effective for pharmacist international normalized ratio monitoring.55 Satisfaction levels are as high as usual care or higher, despite higher productivity.24,56–58 Finally, they can enhance access to primary care for disempowered and traumatised groups, including indigenous Australians, where patients most enjoyed the ‘yarn up’ with peer support, which reduced the ‘scary’ and culturally ‘unnatural’ nature of 1:1 consultations with a general practitioner,59 and Canadian Inuits where similar effects were observed.14
Older people
Older people have more long-term conditions,60 and so benefit especially from the shared time and peer support of group consultations. The differing levels of care (self-care, disease-specific management and case management) are likely to all be supported by access to group care. Supporting evidence includes improved outcomes and fewer emergency admissions54 and a lower incidence of urinary incontinence and medication.61
Introducing group consultations widely offers patients more choice; this is why patients are often very strong advocates, once they have experience.62
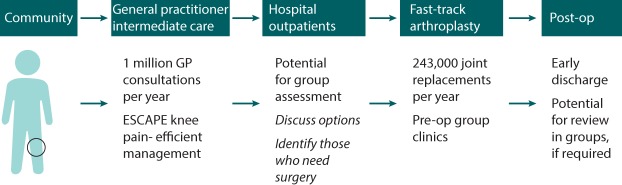
Patient-centred system pathways
An example of a patient who presents with joint pain is shown (Fig 4). Group consultation is possible at many stages of the pathway, and this illustrates the potential. The patient may initially be seen in nurse-, pharmacist-, or GP-led group consultations in primary care, offered group acupuncture63 or increasingly managed in a physiotherapy-led ESCAPE knee pain programme now that the group approach is being rolled out nationally.64 Once there is progressive pain, they might be referred to rheumatology and seen in group clinics24 where it is envisaged that novel disease-modifying drugs for osteoarthritis might well be managed; or directly as now to orthopaedics. Henrik Husted was the pioneer of fast-track arthroplasty65 and a step change in patient and staff mind-set was needed to achieve a 2-day length of stay for total joint replacement.66 This was achieved by a group consultation, including the physiotherapist, ward nurse, orthopaedic surgeon and patients.67 After discharge and, potentially, group consultation review, the patient with a good outcome can return to the community, accessing primary care as needed in the future; whereas those with a poor outcome or who are unfit for surgery have the option of pain group clinics, which can achieve positive outcomes such as returning to work through facilitating self-management.68
Fig 4.
Group consultations along the patient pathway. GP = general practitioner; op = operation.
NHS system change
We have described the benefits of group consultations for patients and staff as same/better care, better efficiency and access, and more enjoyable. It is important to avoid underestimating the challenge of changing to this model of care. Table 1 shows common barriers and solutions to implementation, together with the positive impacts of successful implementation.69 The common factors that thriving sites shared were attitudinal, including reactions to the model, organisational culture and intrinsic climate.70 Struggling sites tended to be bureaucratic and to not embrace innovation, and so responded very differently to the same implementation barriers. While Novick and colleagues articulate this especially clearly for their experience in the USA, exactly the same issues are encountered in the NHS and elsewhere.
Table 1.
Barriers and solutions to widespread implementation of group consultations
| Barrier 70 | Solution 70 | Positive group impact – patients 69,75 | Positive group impact – providers 69 , 75 |
|---|---|---|---|
| Reluctance to attend/share | Clinician & team encouragement | More time makes patients feel well-supported | Develops provider confidence |
| Inertia to novel paradigm | Leadership – patient & provider ‘champions’ | Combats isolationWitness others’ illness | Leadership development |
| Identifying suitable space | Tackling problems (eg imaginative use of existing/community spaces) | Inspired by others copingEquitable patient-clinician relationshipEnhances trust in clinician by observing patient interaction | Develops creative thinking |
| Scheduling | Motivation and systems thinking | Greater and more tailored choice | Better team-working & efficiency |
| Staffing | Buy-in: climate & communication | Patients experience more joined-up care | Clinicians learn to meet patients’ needs better |
| Facing challenges | Anticipating changes | Patients perceive attention to removing of obstacles in care | Clinician & peer education robustly transfers knowledge |
At the Cleveland Clinic every department is mandated to include group consultations and 100% compliance is achieved with massive benefits for that system. This suggests the default should be for practices and hospitals to offer group consultations. The only question is when the NHS will be ready for that step. Where other systemic changes have been made in the NHS, for example, many chronic diseases being managed in primary care by practice nurses;71 propagation of fast-track joint replacement driven by higher efficiency, lower cost and better outcomes;69and independent prescribing by pharmacists, nurses and allied health professionals,72 specific training is needed. This must be supported and funded to deliver success.
Education system change
Currently, medical school curricula do not include group consultations, but there is evidence that both third-year students as well as patients benefit from including undergraduates in group consultations.73 This suggests it is feasible to incorporate group consultations in undergraduate curricula. Similarly, curriculum inclusion drives learning and adoption,74 so both undergraduate and postgraduate curricula should also include group consultation learning outcomes.
Discussion and conclusions
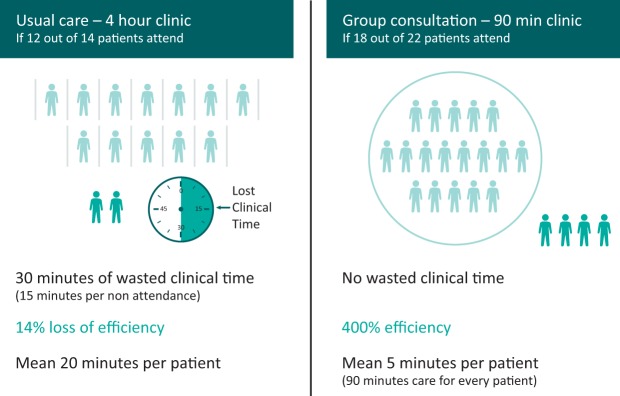
There is much to learn from a systems approach. The main point is that patients will benefit from better outcomes and access, and be empowered, while simultaneously reducing provider costs, thus improving value through both quality improvement and cost reduction.74 However, the benefits are not restricted to those who attend group consultations. Established systems incorporating group care options are able to improve access through conventional care pathways because of their ability to absorb service pressures at a maximum efficiency; this is due to non-repetition of advice that is common across patients. There are also no wasted care opportunities if patients fail to attend. Groups in routine practice can deliver 300–400% efficiency compared to usual care (see Fig 5).
Fig 5.
Group consultation efficiency.
A second important benefit from a systems perspective is that group consultations create greater system flexibility to deal with patients with different care needs. In any care setting, some patients will need 1:1 consultation. In fact, any patient may need a 1:1 consultation, some of the time. Having group consultations embedded into the care mix allows more provider flexibility, ensuring those most needing 1:1 consultations can get them in a timely fashion. Furthermore, among the patients who can benefit from group consultations, the types of patient map to the group consultation models: type A, basically want to get seen faster; type C, need more ‘hand holding’ – have lots of questions and take a lot of consultant time; and type B, can need both. The type A drop-in model reduces costs and increases provider efficiency while patients see a consultant faster. Type C consultations with the same patients in a group on repeat visits is ideal for patients who tend to want more time with the doctor and have more queries, which makes them hard to serve well 1:1. Type B is ideal where geography and other resource constraints determine mixed delivery as optimal. Therefore, group consultations increase system flexibility by finding ways to serve patients with different needs.
A third important system perspective benefit is that group consultations combine aspects of doctor–patient consultations and patient support groups, which are typically offered in very separate and often disjointed parts of a care delivery system.
A fourth important benefit is returning to the varying labels used, having reviewed the key evidence it becomes clearer how the elements are consistent and so should be generalisable. For example, the tight control strategy, which was developed in diabetes (DCCT/EDIC),75 was then applied to rheumatoid arthritis (TICORA)76 and psoriatic arthritis (TICOPA).77 Observational data for inflammatory arthritis shows that delivering a similar tight control strategy with group peer support for mixed inflammatory arthritis achieves outcomes at least as good, but with 400% efficiency. As long as group consultations are implemented efficiently, achieving at least the same, if not better outcomes than usual care they are a ripe target for pragmatic observational scaling-up studies. Naturally, in observational studies, patients who opt in to group care may differ systematically from those who don't. Once sufficient scale is obtained, appropriate RCTs can follow.
Finally, previous systematic reviews have highlighted some gaps in the evidence.1–11 Also, some of the studies are small and underpowered as pointed out by Edelman et al.9 Further, as Booth et al highlighted ‘although there is consistent and promising evidence for an effect of group clinics for some biomedical measures, this effect does not extend across all outcomes’, but scaling-up can confirm both feasibility and real-world efficacy.10 There remains an absence of evidence for assessing new patients, especially presenting to secondary care, and a paucity of educational research on group consultations. More work is also needed on measuring and understanding the peer support effects and how much this affects future consultation behaviour. Furthermore, as patients progress from one age group to another, this model has the potential to create a generation of more expert patients. Therefore, these areas present opportunities for future research, which may become a priority now that these models have been shown to have such potential for the NHS.
We believe that the NHS as the prototypical socialised healthcare system has a unique opportunity to embed group consultations as an alternative routine care option and that doing so will further improve patient access and outcomes, as well as provider efficiency and morale. Group consultations improve value by simultaneously improving quality and reducing cost.7,8,78,79 By collaborating to create and share improved pathways, processes and patient experience while integrating data collection and improvement within the system, a systems approach to care using group consultations can support holistic patient-centred care. This can enhance communication and information retention and improve the quality of health and care delivery.
We conclude that group consultations have significant potential for delivering system-wide benefits across the NHS, in delivering great potential good within a resource-limited system.
Author contributions
The manuscript was drafted by Tania Jones and Fraser Birrell, with critical review by all authors, who agreed the final version and are jointly accountable for its contents.
Acknowledgements
Alison Manson, Georgina Craig and Dr Abi Morbi for help with preparation of figures and compiling evidence. Professor David Asch for providing examples of effective behaviour change.
References
- 1.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2005;18:CD003417. [DOI] [PubMed] [Google Scholar]
- 2.Jaber R, Braksmajer A, Trilling J. Group visits for chronic illness care: models, benefits and challenges. Fam Pract Manag 2006;13:37–40. [PubMed] [Google Scholar]
- 3.Jaber R, Braksmajer A, Trilling JS. Group visits: a qualitative review of current research. J Am Board Fam Med 2006;19:276–90. [DOI] [PubMed] [Google Scholar]
- 4.Riley SB, Marshall ES. Group visits in diabetes care: A systematic review. Diabetes Educ 2010;3:936–4. [DOI] [PubMed] [Google Scholar]
- 5.Burke RE, Ferrara SA, Fuller AM, Kelderhouse JM, Ferrara LR. The effectiveness of group medical visits on diabetes mellitus type 2 (dm2) specific outcomes in adults: a systematic review. JBI Libr Syst Rev 2011;9:833–5. [DOI] [PubMed] [Google Scholar]
- 6.Steinsbekk A, Rygg LØ, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 2012;12:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edelman D, McDuffie JR, Oddone E. et al. Shared medical appointments for chronic medical conditions: A systematic review. Washington: Department of Veterans Affairs (US), 2012. www.hsrd.research.va.gov/publications/esp/shared-med-appt.pdf. [PubMed] [Google Scholar]
- 8.Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. Can Med Assoc J 2013;185:E635–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edelman D, Gierisch JM, McDuffie JR, Oddone E, et al. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med 2015;30:99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Booth A, Cantrell A, Preston L, Chambers D, Goyder E. What is the evidence for the effectiveness, appropriateness, and feasibility of group clinics for patients with chronic conditions? A systematic review. Health Services and Delivery Research Journal 2015;3:1–372. [PubMed] [Google Scholar]
- 11.Egger G, Stevens J, Ganora C, Morgan B. Programmed shared medical appointments. Aust J Gen Pract 2018;47:70–5. [DOI] [PubMed] [Google Scholar]
- 12.Sadikot SM, Das AK, Wilding J. et al. Consensus recommendations on exploring effective solutions for the rising cost of diabetes. Diabetes Metab Syndr 2017;11:141–7. [DOI] [PubMed] [Google Scholar]
- 13.Feldman M. Care of the well child: cluster visits. Am J Nurs 1974;74:1485–8. [PubMed] [Google Scholar]
- 14.Noffsinger E. Increasing efficiency, accessibility, and quality of care through drop-in group medical appointments. Group Practice Journal 1999;48:12–8. [Google Scholar]
- 15.Noffsinger EB, Scott JC. Understanding today's group visit models. Perm J 2000;4:99–112. [Google Scholar]
- 16.Noffsinger EB. Physicals shared medical appointments: a revolutionary access solution. Group Practice Journal 2002;51:16–26. [Google Scholar]
- 17.Scott JC, Robertson BJ. Kaiser Colorado's Cooperative Health Care Clinic: a group approach to patient care. Manag Care Q 1996;4:41–5. [PubMed] [Google Scholar]
- 18.Blumenfeld A, Tischio M. Centre of excellence for headache care: group model at Kaiser Permanente. Headache 2003;43:431–40. [DOI] [PubMed] [Google Scholar]
- 19.Ickovics JR, Kershaw TS, Westdahl C, et al. Group prenatal care and preterm birth weight: results from a matched cohort study at public clinics. Obstet Gynecol 2003;102:1051–7. [DOI] [PubMed] [Google Scholar]
- 20.Birrell F. Group clinics can deliver effective care for rheumatoid arthritis: A feasible model for an annual review clinic. Rheumatology 2009;48:i17. [Google Scholar]
- 21.Cunningham SD, Lewis JB, Thomas JL, Grilo SA, Ickovics JR. Expect with me: development and evaluation design for an innovative model of group prenatal care to improve perinatal outcomes. BMC Pregnancy Childbirth 2017;17:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abraham C, Michie S. A taxonomy of behaviour change techniques used in interventions. Health Psychology 2008;27:379–87. [DOI] [PubMed] [Google Scholar]
- 23.Birrell F. Optimal management for inflammatory arthritis: achieving remission through one-to-one and group clinic strategies. In: Wallace M, Sommer CL, Cohen SP, Kress M. (eds), Pain 2016: Refresher Courses: 16th World Congress on Pain. Washington: IASP, 2016:201–8. [Google Scholar]
- 24.General Practice Development Programme 10 High Impact Actions. NHS England, 2016. www.england.nhs.uk/gp/gpfv/redesign/gpdp [Accessed 18 May 2018]. [Google Scholar]
- 25.Group consultations: a way to spend more time with patients. NHS Alliance: 2015. www.nhsalliance.org/making-time-in-general-practice/appendix-4 [Accessed 18 May 2018]. [Google Scholar]
- 26.Hayhoe B, Verma A. & Kumar S. Shared medical appointments A promising response to escalating demand for healthcare. BMJ 2017;358:j4034. [DOI] [PubMed] [Google Scholar]
- 27.Ramdas K, Darzi A. Adopting innovations in care delivery – the case of shared medical appointments. N Engl J Med 2017;376:1105–7. [DOI] [PubMed] [Google Scholar]
- 28.Clarkson J, Bogle D, Dean J. et al. Engineering better care: a systems approach to health and care design and continuous improvement. London: Royal Academy of Engineering, 2018. [Google Scholar]
- 29.Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based co-design and healthcare improvement: realising participatory design in the public sector. The Design Journal 2015;18:227–48. [Google Scholar]
- 30.Birrell J, Clark I, Easterbrook C, et al. Patients say yes to group clinics. BMJ 2017;358:j4034.28855156 [Google Scholar]
- 31.Slough group clinics evaluation. Slough CCG, 2016. www.england.nhs.uk/wp-content/uploads/2016/03/releas-capcty-case-study-2-153.pdf [Accessed 18 May 2018]. [Google Scholar]
- 32.Baqir W. Pharmacy-led osteoporosis group clinics in the community. Rheumatology 2016;55(Suppl 1):i17. [Google Scholar]
- 33.Hacker J. Croydon: Group consultation pilot - results of independent evaluation. Croydon CCG, 2016. [Google Scholar]
- 34.Carter EB, Temming LA, Akin J, et al. Group prenatal care compared with traditional prenatal care: A systematic review and meta-analysis. Obstetrics & Gynecology 2016;128:551–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Catling CJ, Medley N, Foureur M, et al. Group versus conventional antenatal care for women. Cochrane Database Syst Rev 2015;2:CD007622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gareau S, Lòpez-De Fede A, Loudermilk BL. et al. Group prenatal care results in Medicaid savings with better outcomes: A propensity score analysis of centering pregnancy participation in South Carolina. Matern Child Health J 2016;20:1384–93. [DOI] [PubMed] [Google Scholar]
- 37.McCue BK, Borders AE, Choby B. Group prenatal care. ACOG Committee Opinion No. 731. Obstet Gynecol 2018;131:616–8. [DOI] [PubMed] [Google Scholar]
- 38.Evaluation of two-year child development group reviews. NHS Hertfordshire Community Trust, 2017. www.groupconsultations.com/Herts2017 [Accessed 30 May 2018]. [Google Scholar]
- 39.Wall-Haas CL, Kulbok P, Kirchgessner J, Rovnyak V. Shared medical appointments: facilitating care for children with asthma and their caregivers. J Pediatr Health Care 2012;26:37–44. [DOI] [PubMed] [Google Scholar]
- 40.Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Annals of Internal Medicine 2010;152:689–96. [DOI] [PubMed] [Google Scholar]
- 41.Junling G, Yang L, Junming D, Pinpin Z, Hua F. Evaluation of group visits for Chinese hypertensives based on primary health care center. Asia Pac J Public Health 2015;27:NP350–60. [DOI] [PubMed] [Google Scholar]
- 42.De Vries B, Darling-Fisher C, Thomas AC, Belanger-Shugart EB. Implementation and outcomes of group medical appointments in an outpatient specialty care clinic. J Am Acad Nurse Pract 2008;20:163–9. [DOI] [PubMed] [Google Scholar]
- 43.Yehle KS, Sands LP, Rhynders PA, Newton GD. The effect of shared medical visits on knowledge and self-care in patients with heart failure: a pilot study. Heart Lung 2009;38:25–33. [DOI] [PubMed] [Google Scholar]
- 44.Bartley KB, Haney R: Shared medical appointments: improving access, outcomes, and satisfaction for patients with chronic cardiac diseases. J Cardiovasc Nurs 2010;25:13–9. [DOI] [PubMed] [Google Scholar]
- 45.Masley S, Phillips S, Copeland JR. Group office visits change dietary habits of patients with coronary artery disease-the dietary intervention and evaluation trial (DIET). J Fam Pract 2001;50:235–9. [PubMed] [Google Scholar]
- 46.Harris M. Shared medical appointments after cardiac surgery-the process of implementing a novel pilot paradigm to enhance comprehensive postdischarge care. J Cardiovasc Nurs 2010;25:124–9. [DOI] [PubMed] [Google Scholar]
- 47.Montoya V, Sole ML, Norris AE. Improving the care of patients with chronic kidney disease using group visits: a pilot study to reflect an emphasis on the patients rather than the disease. Nephrol Nurs J 2016;43:207–22. [PubMed] [Google Scholar]
- 48.Gardiner P, Dresner D, Barnett KG, Sadikova E, Saper R. Medical group visits: a feasibility study to manage patients with chronic pain in an underserved urban clinic. Glob Adv Health Med 2014;3:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.White A, Richardson M, Richmond P, Freedman J, Bevis M. Group acupuncture for knee pain: evaluation of a cost-saving initiative in the health service. Acupuncture in Medicine 2012;30:170–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beck A, Scott J, Williams P, et al. A randomized trial of group outpatients visits for chronically ill older HMO members: the cooperative health care clinic. J Am Geriatr Soc 1997;45:543–9. [DOI] [PubMed] [Google Scholar]
- 51.Coleman EA, Eilertsen TB, Kramer AM, et al. Reducing emergency visits in older adults with chronic illness. A randomized, controlled trial of group visits. Effective Clinical Practice 2001;4:49–57. [PubMed] [Google Scholar]
- 52.Crane S, Collins L, Hall J, Rochester D, Patch S. Reducing utilization by uninsured frequent users of the emergency department: combining case management and drop-in group medical appointments. J Am Board Fam Med 2012;25:184–1. [DOI] [PubMed] [Google Scholar]
- 53.Scott JC, Conner DA, Venohr I. et al. Effectiveness of a group outpatient visit model for chronically ill older health maintenance organization members: a 2-year randomized trial of the cooperative health care clinic. J Am Geriatr Soc 2004;52:1463–70. [DOI] [PubMed] [Google Scholar]
- 54.Seesing FM, Drost G, Groenewoud J, van der Wilt GJ, van Engelen BG. Shared medical appointments improve QOL in neuromuscular patients: a randomized controlled trial. Neurology 2014;83:240–6. [DOI] [PubMed] [Google Scholar]
- 55.Griffin BL, Burkiewicz JS, Peppers LR, Warholak TL. International normalized ratio values in group versus individual appointments in a pharmacist-managed anticoagulation clinic. Am J Health Syst Pharm 2009;66:1218–23. [DOI] [PubMed] [Google Scholar]
- 56.Cohen S. Patient satisfaction and perception of value with shared medical appointments. Communicating Nursing Research 2012;45:397. [Google Scholar]
- 57.Seager MJ, Egan RJ, Meredith HE, Bates SE, Norton SA, Morgan JD. Shared medical appointments for bariatric surgery follow-up: a patient satisfaction questionnaire. Obesity Surgery 2012;22:641–5. [DOI] [PubMed] [Google Scholar]
- 58.Egger G, Dixon J, Meldrum H, et al. Patients' and providers' satisfaction with shared medical appointments. Australian Family Physician 2015;44:674–9. [PubMed] [Google Scholar]
- 59.Stevens J, Binns A, Dixon J, Morgan R, Egger G. Shared medical appointments for Aboriginal and Torres Strait Islander men. Australian Family Physician 2016;45:425–9. [PubMed] [Google Scholar]
- 60.Department of Health Supporting people with long-term conditions: An NHS and social care model to support local innovation and integration. London: Department of Health, 2005. [Google Scholar]
- 61.Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. J Am Geriatr Soc 1999;47:775–83. [DOI] [PubMed] [Google Scholar]
- 62.Price A. Amy Price on shared medical appointments – just say no. BMJ, 2017. http://blogs.bmj.com/bmj/2017/09/18/amy-price-on-shared-medical-appointments-just-say-no [Accessed 12 May 2018]. [Google Scholar]
- 63.Asprey A, Paterson C, White A. ‘All in the same boat’: a qualitative study of patients' attitudes and experiences in group acupuncture clinics. Acupuncture in Medicine 2012;30:163–9. [DOI] [PubMed] [Google Scholar]
- 64.Hurley MV, Carter A. ESCAPE into the community – a community-based rehabilitation programme for elderly people with chronic joint pain. Perspect Public Health 2016;136:67–9. [DOI] [PubMed] [Google Scholar]
- 65.Husted H, Hansen HC, Holm G, et al. Length of stay in total hip and knee arthroplasty in Denmark I: volume, morbidity, mortality and resource utilization. A national survey in orthopaedic departments in Denmark. [In Danish] Ugeskr Laeger 2006;168:2139–43. [PubMed] [Google Scholar]
- 66.14th Annual Report. National Joint Registry, 2017.. www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2014th%20Annual%20Report%202017.pdf [Accessed 11 May 2018]. [Google Scholar]
- 67.Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl 2012;83:1–39. [DOI] [PubMed] [Google Scholar]
- 68.Cottom S. Survey of Pain Association Scotland self-management groups. Pain News 2016;14:129–30. [Google Scholar]
- 69.Kirsh SR, Aron DC, Johnson KD, et al. A realist review of shared medical appointments: How, for whom, and under what circumstances do they work? BMC Health Serv Res 2017;17:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Novick G, Womack JA, Lewis J, et al. Perceptions of barriers and facilitators during implementation of a complex model of group prenatal care in six urban sites. Res Nurs Health 2015;38:462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Libr Syst Rev 2009;7:492–582. [DOI] [PubMed] [Google Scholar]
- 72.Graham-Clarke E, Rushton A, Noblet T, Marriott J. Facilitators and barriers to non-medical prescribing – A systematic review and thematic synthesis. PLoS One 2018;13:e0196471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Birrell F, Jones T, Li KHC, Russell-Westhead M. Teaching undergraduates chronic disease management through group clinics: sometimes, more is more. ASME Annual Scientific Meeting 2018 Abstract Book 2018. [Google Scholar]
- 74.Baker KF, Jandial S, Thompson B, Walker D, Taylor K, Foster HE. Use of structured musculoskeletal examination routines in undergraduate medical education and postgraduate clinical practice – a UK survey. BMC Med Educ 2016;16:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nathan DM, DCCT/EDIC Research Group The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care 2014;37:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grigor C, Capell H, Stirling A, et al. Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet 2004;364:263–9. [DOI] [PubMed] [Google Scholar]
- 77.Coates LC, Moverley AR, McParland L, et al. Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK multicentre, open-label, randomised controlled trial. Lancet 2015;386:2489–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Noffsinger E. Running group visits in your practice. Springer, 2009. [Google Scholar]
- 79.Noffsinger E. The ABCs of group visits: an implementation manual for your practice. Springer, 2012. [Google Scholar]