Abstract
Objectives:
Both psychiatric polypharmacy and multimorbidity are common in depressed adults. We examine recent patterns of psychotropic polypharmacy with attention to concurrent multimorbidity in the treatment of depressive disorders in outpatient psychiatric care.
Methods:
Data from the 2006–2015 National Ambulatory Medical Care Survey offer nationally representative samples of office-based psychiatric care in adults with depressive disorders (ICD-9-CM codes 296.20–296.26, 296.30–296.36, 300.4, 311, and 301.10–301.13) (n=6,685 unweighted). These data allowed estimation of the prevalence of polypharmacy (within-class, between-class, and both) involving four major psychotropic classes: antidepressants, antipsychotics, mood-stabilizers, and sedative-hypnotics. We further evaluated the proportion of within-class and between-class psychotropic prescription combinations that were potentially justifiable, taking FDA-approved indications and multimorbidity into consideration.
Results:
Prescribing two or more psychotropic medications for depressed adults remained substantial and stable ranging from 59.0% in 2006–2007 to 58.0% in 2014–2015. The most common within-class polypharmacy types were: antidepressants (22.7%) and sedative-hypnotics (14.8%). The most common between-class polypharmacy types were: an antidepressant and a sedative-hypnotic (30.7%), an antidepressant and an antipsychotic (16.4%), and an antipsychotic and a sedative-hypnotic (9.0%). In visits in which between-class psychotropics were prescribed, 53.9% were potentially justified by FDA-approved augmentation and/or adjunctive treatment strategies or by psychiatric multimorbidities.
Conclusion:
Psychotropic polypharmacy affects more than half of depressed adults. Between-class polypharmacy is the most common pattern and in over 50% of instances may be justified by augmentation strategies or considerations of psychiatric multimorbidity. Future research is needed to address effectiveness, safety, and cost-effectiveness of polypharmaceutical care for depression, especially those occurring with psychiatric co-morbididities.
Keywords: Depression, psychotropics, polypharmacy, psychiatric co-morbidities, pharmacoepidemiology
INTRODUCTION
Depressive disorders are frequently chronic, recurring, and disabling, and are a major source of disability and comorbidity in the US and globally.1 Antidepressants are the first line treatment for depression in most clinical guidelines.2,3 For patients who do not respond to antidepressants, many guidelines4–6 support alternative pharmacological therapies, such as switching to another antidepressant or augmentation with either an additional antidepressant or a second-generation antipsychotic.7
In the US, about one in six adults (16.7%) reported taking psychotropic medications in 2013,8 and a substantial number of adults are prescribed two or more psychotropics concomitantly (hereafter referred to as psychotropic polypharmacy).9 The proportion of all office-based psychiatrist visits in which two or more psychotropic medications were prescribed increased from 42.6% in 1996–1997 to 59.8% in 2005–2006.9 While some guidelines support psychotropic polypharmacy of specific types in some specific clinical conditions based on findings from randomized controlled trials (RCTs) (e.g., the FDA has approved use of several antipsychotics for treatment-resistant major depressive disorders),4–7,10 many patients receive two or more psychotropic agents that are not FDA approved, but may be justified by co-morbidities.9,11–13
Justification for psychotropic polypharmacy in depressed adults may be based on evidence of enhanced efficacy for treatment resistant disorders or treatment of specific multimorbidities (e.g. insomnia).14–16 Unjustified psychotropic polypharmacy in adults with depression may result in unnecessary adverse drug events and even potential drug addiction.14–16 Because little is known about current trends of psychotropic polypharmacy and, more specifically, its relationship to multimorbidity, we sought to describe the diverse clinical contexts polypharmaceutical care for depression.
Most studies of polypharmacy published in the past decade do not address these issues,9,12,17–20 because they focused on pediatric populations,12,17,19 while others9,20 investigated all psychiatric disorders taken together17–20 without specific consideration of depressive disorders and their specific multimorbidities,7,21 or failed to distinguish between within-class and between-class of polypharmacy.12,17,18,20 While prescribing two or more medications from a single psychotropic class may be justified as an evidence-based augmentation strategy,15,16 prescribing medications from different psychotropic classes may result in drug-drug interactions, potentially leading to adverse effects on cognitive or functional outcomes. For instance, the recent Beers criteria guideline strictly advises that neither antidepressants nor antipsychotics should be co-prescribed with other CNS-active drugs because they increase the risk of falls and fractures in older adults.22 Furthermore, several studies used data from a single clinic18 or a state,19 limiting the generalizability of the results, and virtually all of the previous studies9,12,17–20 used data gathered prior to 2009.
To address these limitations, we examine recent trends in psychotropic polypharmacy for adults with depressive disorders in a nationally representative sample of visits by adults to office-based psychiatrists taking greater consideration of both multimorbidity and the distinction between within-class and between-class polypharmacy. We thus sought to address the following questions: 1) What are national rates and longitudinal trends of polypharmaceutical psychotropic prescribing for adults with depressive disorders? 2) What are the frequencies of within-class and between-class psychotropic polypharmacy for adults with depressive disorders? And, 3) what proportion of the polypharmaceutical prescriptions are potentially justified by evidence of the effectiveness of between-class augmentation or by multimorbidity? This study thus seeks to provide an enriched account of psychotropic polypharmacy among adults with depressive disorders in office-based psychiatrist visits.
METHODS
Data source and study sample
We used data from the 2006–2015 National Ambulatory Medical Care Surveys (NAMCS), which is administrated by National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC).23 The NAMCS conducts an annual survey of visits to office-based physicians in outpatient settings, and is designed to be a nationally representative sample of office-based outpatient medical care.23 We limited our sample to adults aged 18 or older with depressive disorders (ICD-9-CM diagnostic codes 296.20–296.26, 296.30–296.36, 300.4, 311, and 301.10–301.13), who had office visits to a psychiatrist (n=7,162 unweighted). We further excluded observation with any missing covariates (6.7%), leaving a final sample size of 6,685 office visits. Since we used publicly available deidentified data, our study was exempted by the Institutional Review Board (#2000021850) at Yale School of Medicine. Further details of the survey, including descriptions, questionnaires, sampling methodology and datasets, are publicly available on the NAMCS website (https://www.cdc.gov/nchs/ahcd/index.htm).
Measures
Psychotropic medications.
The NAMCS documented up to eight medications prescribed at each visit during surveys conducted in 2006–2011, up to 10 medications from 2012–2013, and up to 30 medications from 2014–2015. For consistency, we examined the first eight medications listed as prescribed for each visit. We identified four major classes of psychotropic prescriptions using the following generic names:9,24 (1) antidepressants which included: amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, trimipramine, nefazodone, trazodone, vilazodone, vortioxetine, citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, phenelzine, tranylcypromine, rasagiline, selegiline, desvenlafaxine, duloxetine, levomilnacipran, venlafaxine, milnacipran, bupropion, and mirtazapine; (2) antipsychotics which included: haloperidol, chlorpromazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine, thiothixene, loxapine, molindone, pimozide, aripiprazole, asenapine, clozapine, iloperidone, lurasidone, olanzapine, paliperidone, quetiapine, risperidone, and ziprasidone; (3) mood stabilizers which included: carbamazepine, lamotrigine, lithium, and valproic sodium/divalproex sodium; and (4) sedative-hypnotics which included: alprazolam, butabarbital, chlordiazepoxide, chloral hydrate, clorazepate, clonazepam, diazepam, diphenhydramine, eszopiclone, estazolam, flurazepam hydrochloride, hydroxyzine, lorazepam, meprobamate, oxazepam, phenobarbital, secobarbital, temazepam, triazolam, zaleplon, and zolpidem tartrate.
Psychiatric co-morbidities.
Up to three clinical diagnoses were collected in NAMCS for each visit using the International Classification of Diseases, 9th edition, Clinical Modification (ICD-9-CM) diagnostic codes. We constructed indicator variables for the following psychiatric disorders: (1) anxiety (300.0X); (2) insomnia (307.42 and 780.51–780.52); (3) post-traumatic stress disorder (PTSD) (309.81); (4) bipolar disorders (296.00–296.16, 296.40–296.80, and 296.89); and (4) schizophrenia and other psychoses (295 and 297–299).
Covariates.
We considered a number of covariates in characterizing polypharmacy subgroups,2,7,25,26 including: age (18–44, 45–64, 65–74, 75+), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), region of residence (Northeast, Midwest, South, or West), repeated visits within the past 12 months (dichotomized as <6 or 6+). receipt of psychotherapy or mental health counseling (yes/no), and time spent with a doctor (<15, 15–20, 21–30, or >30 minutes).
Data analysis
First, we estimated frequency of all psychotropic medication prescriptions written for adults with depressive disorders during psychiatrist visits from 2006 to 2015. We descriptively compared visits classified as involving no prescription, 1 prescription, 2, 3–4, and ≥5 psychotropic prescriptions, and traced the frequency of such prescriptions over time. Second, we estimated the frequency of visits characterized by within-class psychotropic polypharmacy for each of four major psychotropic class from 2006 to 2015. Third, we estimated the frequency of between-class psychotropic polypharmacy in the population of interest.
We further present data on the most common combinations of between-class psychotropic prescriptions. Furthermore, we compared selected demographic and clinical characteristics among adults with depressive disorders who had at least two psychotropic medications prescribed during their visit to a psychiatrist (i.e., who were prescribed polypharmacy) differentiating those with: 1) within-class polypharmacy; 2) between-class polypharmacy; and 3) both within- and between-class polypharmacy. We compared the groups on bivariate analyses using Pearson’s chi-squared statistic, with a p-value of 0.01 (two-sided) for tests of statistical significance.
Finally, we identified between-class polypharmacy combinations, especially those associated with FDA-approved augmentation strategies or rational responses to diagnostic multimorbidities, which could plausibly justify polypharmacy, and calculated the proportion of between-class polypharmacy treatment regimens. For example, we considered dual psychiatric diagnoses as potential justification for the use of between-class psychotropic polypharmacy. For example, co-prescribing of antidepressant and antipsychotic medications could be justifiable for patients diagnosed with both depression and schizophrenia. We also considered co-prescribing of antidepressant and antipsychotic medications for those with depression and PTSD, as antidepressants are approved by the FDA for PTSD,27 and antipsychotic therapy has shown efficacy for treating PTSD in many, although not all RCTs.28–31 We did not indicate potential justification of antipsychotic medication use for depressive disorders when used without antidepressants since this neither has FDA approval nor a supporting body of research evidence. We used Stata 15.1 MP/6-Core32 for all analyses, and we employed the svy commands in Stata to account for the complex survey sampling design of the NAMCS (i.e., unequal probability of selection, clustering and stratification).
RESULTS
National trends of psychotropic prescriptions
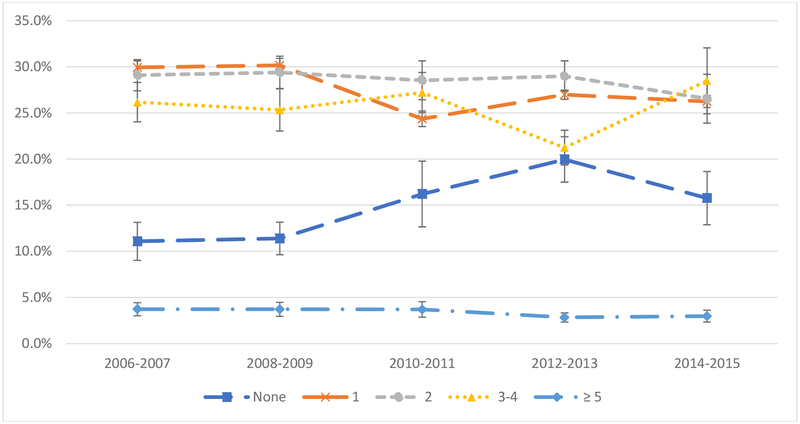
Figure 1 presents national trends of any psychotropic prescriptions in visits to psychiatrists among adults with depressive disorders. Of these visits, 84.9% had at least one psychotropic medication prescribed between 2006 and 2015. The proportion of patients prescribed only one psychotropic medication decreased from 29.9% in 2006–2007 to 24.4% in 2010–2011, but then increased to 26.2% in 2014–2015. Proportions of visits in which no medication was prescribed increased from 11.1% in 2006–2007 to 20.0% in 2012–2013, but then dropped to 15.8% in 2014–2015. Proportions of visits in which two and three to four psychotropics prescribed remain stable at 28.3% and 25.9%, respectively, across the time periods. Approximately 3.3% of visits had five or more psychotropics prescribed across years from 2006 to 2015.
Figure 1. National trends of psychotropic prescribing among US adults with depressive disorders in visits to office-based psychiatrists (n=6,685 unweighted), 2006–2015 NAMCS.
Note: Bars represent 95% confidence intervals.
National trends of within-class psychotropic polypharmacy
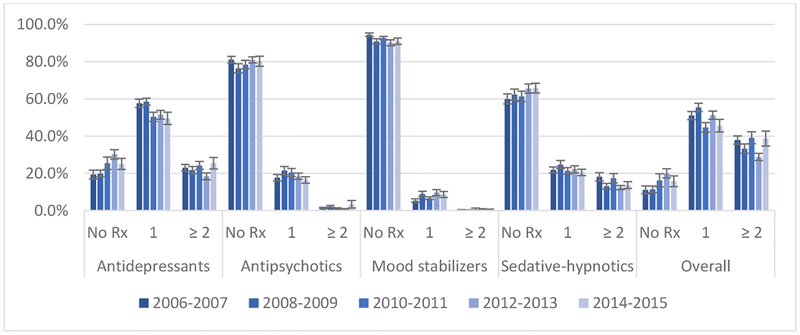
Figure 2 presents national trends of within-class psychotropic prescriptions by major psychotropic class among adults with depressive disorders in psychiatrist visits. Overall, 35.7% of visits were associated with two or more within-class psychotropic prescriptions between 2006 and 2015. Antidepressants were the most common within-class psychotropic class prescribed (22.7%), followed by sedative-hypnotics (14.8%). Within-class polypharmacy was not common for antipsychotics (<4.0%) or mood stabilizers (<1.0%).
Figure 2. National trends of within-class psychotropic prescriptions among US adults with depressive disorders in visits to office-based psychiatrists (n=6,685 unweighted), 2006–2015 NAMCS.
Note: Bars represent 95% confidence intervals.
National trends of between-class psychotropic polypharmacy
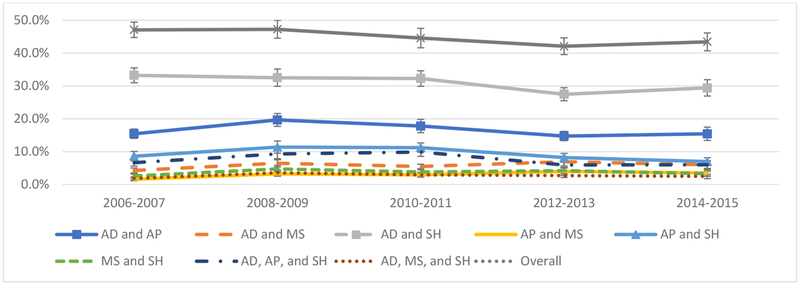
Figure 3 shows national trends of psychiatrist visits in which between-class psychotropics were prescribed in adults with depressive disorders. Overall, psychiatrist visits in which between-class psychotropics were prescribed decreased slightly, from 47.0% in 2006–2007 to 43.4% in 2014–2015. The most common type of a between-class polypharmacy involved antidepressants and sedative-hypnotics (30.7%), followed by the combination of antidepressants and antipsychotics (16.4%), antipsychotics and sedative-hypnotics (9.0%), and the triple combination of antidepressants, antipsychotics, and sedative-hypnotics (7.4%). These trends were relatively stable from 2006 to 2015.
Figure 3. National trends of two or more between-class psychotropic prescriptions among US adults with depressive disorders visits to office-based psychiatrists (n=6,685 unweighted), 2006–2015 NAMCS.
Note: Bar represents 95% confidence intervals. AD=antidepressants; AP=antipsychotics; MS=mood stabilizers; and SH=sedative-hypnotics. Other combinations are not reported here as they have <3% across all time periods.
Characteristics of visits by psychotropic polypharmacy
Table 1 demonstrates selected demographic and clinical characteristics few of which were significantly different across the three types of psychotropic polypharmacy. Psychiatrist visits in which multiple psychotropics prescribed primarily involved adults under 65 (86.6%), females (66.6%), and non-Hispanic whites (80.3%). There were two significant differences between groups in this large sample at p<0.01. The overall rate of co-diagnosed psychiatric disorders was differed by group such that the proportion with between-class psychotropic polypharmacy was higher (32.4%) than the proportion with within-class psychotropic polypharmacy (23.2%) (p<0.001). This pattern is particularly pronounced in the diagnosis of anxiety disorder, where the between-class psychotropic polypharmacy rate was significantly greater (23.7%) than the proportion with within-class polypharmacy (15.9%) (p=0.002).
Table 1.
Selected characteristics (weighted column %) of adults ages 18 and older with depressive disorders who received two or more psychotropics in office-based psychiatrist visits, 2006–2015 NAMCS.
| Within-class polypharmacy (1) | Between-class polypharmacy (2) | Both (1) and (2) | Total | P-value† | |
|---|---|---|---|---|---|
| Sample size | |||||
| Unweighted sample | 782 | 1,438 | 1,481 | 3,701 | |
| Weighted visits | 1,683,269 | 2,848,188 | 2,978,984 | 7,510,441 | |
| Age | |||||
| 18–44 | 38.4 | 38.0 | 35.0 | 36.9 | 0.049 |
| 45–64 | 50.8 | 45.9 | 52.7 | 49.7 | |
| 65–74 | 7.5 | 9.9 | 7.8 | 8.5 | |
| 75+ | 3.3 | 6.3 | 4.4 | 4.9 | |
| Gender | |||||
| Female | 64.3 | 63.4 | 70.9 | 66.6 | 0.0 16 |
| Male | 35.8 | 36.6 | 29.1 | 33.4 | |
| Race/ethnicity | |||||
| Non-Hispanic White | 84.1 | 77.3 | 81.0 | 80.3 | 0.206 |
| Non-Hispanic Black | 3.8 | 6.8 | 5.1 | 5.5 | |
| Hispanic | 8.9 | 11.7 | 9.6 | 10.2 | |
| Othera) | 3.3 | 4.1 | 4.3 | 4.0 | |
| Region | |||||
| Northeast | 36.5 | 31.8 | 27.8 | 31.3 | 0.093 |
| Midwest | 13.8 | 17.1 | 17.1 | 16.4 | |
| South | 30.0 | 31.8 | 36.8 | 33.4 | |
| West | 19.7 | 19.3 | 18.3 | 19.0 | |
| Repeat of visits in the past 12 months | |||||
| < 6 visits | 53.5 | 48.8 | 44.9 | 48.3 | 0.023 |
| ≥ 6 visits | 46.5 | 51.2 | 55.1 | 51.7 | |
| Psychotherapy provided | |||||
| Yes | 64.4 | 64.1 | 68.0 | 65.7 | 0.436 |
| No | 35.6 | 35.9 | 32.0 | 34.3 | |
| Time spent with doctor | |||||
| < 15 min. | 15.8 | 9.3 | 12.9 | 12.2 | 0.036 |
| 15–20 min. | 28.2 | 27.8 | 32.5 | 29.8 | |
| 21–30 min. | 25.9 | 28.7 | 23.6 | 26.0 | |
| > 30 min. | 30.2 | 34.2 | 31.1 | 32.1 | |
| Co-diagnosed psychiatric disorder | 23.2 | 32.4 | 37.9 | 32.5 | <0.001 |
| Anxiety | 15.9 | 23.7 | 26.4 | 23.0 | 0.002 |
| PTSD | 5.0 | 4.7 | 6.2 | 5.4 | 0.350 |
| Bipolar disorder | 2.3 | 2.6 | 4.2 | 3.2 | 0.091 |
| Insomnia | 2.4 | 0.8 | 2.1 | 1.7 | 0.356 |
| Schizophrenia | 0.6 | 1.7 | 1.8 | 1.5 | 0.210 |
Note:
compares proportion differences by psychotropic polypharmacy type using a weight-corrected Pearson’s chi-squared statistic; and
includes Asians, American Indian/Alaska Natives (AIANs), Native Hawaiian or Other Pacific Islanders (NHOPI), and other mixed races.
Potentially justified between-class psychotropic polypharmacy
Table 2 presents potential justification of between-class psychotropic prescriptions in adults with depressive disorders by the most common type of combinations. Overall, 53.9% of psychiatrist visits with between-class psychotropic prescriptions (3.1 million visits) could potentially be justified. For a combination of antidepressant and sedative-hypnotic classes, 30.2% were potentially justified on the basis of insomnia or a co-morbid anxiety disorder. For a combination of antidepressant and antipsychotic classes, 100.0% were potentially justified by the use of antipsychotics for treating depression, while 14.9% were potentially justified among those with the combination of antipsychotic and mood stabilizer classes, and 11.0% among those with a combination of an antidepressant and a mood stabilizer classes.
Table 2.
Potential justification of between-class psychotropic prescriptions among US adults with depressive disorders who received any combination of between-class psychotropic prescriptions in visits to office-based psychiatrists (n=2,919 unweighted), 2006–2015 NAMCS.
| Psychiatric co-morbidity | Unweighted sample | Weighted visits | P-value† | % Potentially justified |
|---|---|---|---|---|
| Antidepressant and sedative-hypnotic | 1,986 | 4,012,039 | ||
| Depression and anxiety | 537 | 1,147,008 | <0.001 | 30.2% |
| Depression and insomnia | 36 | 75,286 | 0.008 | |
| Antidepressant and antipsychotic | 1,100 | 2,146,574 | ||
| Depression | 1,100 | 2,146,574 | - | 100.0% |
| Depression and bipolar disorder | 49 | 113,881 | 0.001 | |
| Depression and PTSD | 92 | 132,233 | 0.313 | |
| Depression and schizophrenia | 43 | 75,001 | 0.002 | |
| Depression, bipolar disorder, and schizophrenia | 2 | 1,039 | 0.138 | |
| Depression, PTSD, and bipolar disorder | 2 | 958 | 0.215 | |
| Depression, PTSD, and schizophrenia | 0 | 0 | - | |
| Depression, bipolar disorder, and schizophrenia | 2 | 1,039 | 0.138 | |
| Antipsychotic and sedative-hypnotic | 588 | 1,178,803 | ||
| Depression, bipolar disorder, and anxiety | 4 | 3,706 | 0.942 | 1.3% |
| Depression, bipolar disorder, and insomnia | 1 | 746 | 0.604 | |
| Depression, schizophrenia, and anxiety | 3 | 11,323 | 0.120 | |
| Depression, schizophrenia, and insomnia | 0 | 0 | - | |
| Antidepressant, antipsychotic, and sedative-hypnotic | 488 | 960,778 | ||
| Depression, bipolar disorder, and anxiety | 2 | 1,225 | 0.277 | 1.4% |
| Depression, bipolar disorder, and insomnia | 1 | 746 | 0.471 | |
| Depression, schizophrenia, and anxiety | 3 | 11,323 | 0.065 | |
| Depression, schizophrenia, and insomnia | 0 | 0 | - | |
| Antidepressant and mood stabilizer | 420 | 764,505 | ||
| Depression and bipolar disorder | 42 | 83,930 | <0.001 | 11.0% |
| Mood stabilizer and sedative-hypnotic | 249 | 480,427 | ||
| Depression, bipolar disorder, and anxiety | 2 | 726 | 0.716 | 0.2% |
| Depression, bipolar disorder, and insomnia | 0 | 0 | - | |
| Antipsychotic and mood stabilizer | 201 | 407,472 | ||
| Depression and bipolar disorders | 26 | 60,889 | <0.001 | 14.9% |
| Depression, schizophrenia, and bipolar disorders | 1 | 128 | 0.323 | |
| Overall potentially justification of between-class psychotropic prescriptions | 1,569 | 3,143,208 | 53.9% |
Note:
The p-value is based on the cross-tabulation of diagnosis (yes/no) and between-class prescriptions (yes/no), and is based on the weight-corrected Pearson’s chi-squared test.
DISCUSSION
This study investigated recent patterns and trends of psychotropic polypharmacy in the context of multimorbidity among US adults with depressive disorders in a nationally representative sample of office-based visits to a psychiatrist from 2006 to 2015. Overall, the proportion of visits in which two or more psychotropics were prescribed remained stable at 59.0% in 2006–2007 and 58.0% in 2014–2015. A previous study9 reported that visits for any psychiatric disorder in which two or more psychotropics were prescribed, increased from 42.6% in 1996 to 59.8% in 2006, prior to the period examined here. While these studies are not strictly comparable due to sampling from different populations, it appears that visits in which two or more psychotropics prescribed remained substantial as well as stable in office-based psychiatry practice in the past decade, after an increase in the previous decade.
Second, we identified frequencies and patterns of within-class polypharmacy in adults with depressive disorders. The most common within-class psychotropic co-prescriptions were for antidepressants and sedative-hypnotics across the study periods. Characterization of within-class polypharmacy showed that prescribing two or more antidepressants was the most common pattern. Such pattern may be justified as an augmentation strategy,7, even though an RCT33 investigating two antidepressant combinations did not find significant difference on clinical effectiveness when compared to antidepressant monotherapy (although notably this study did not focus on treatment unresponsive cases), and a recent RCT published in 2017 showed that augmentation with a second antipsychotic was more effective on some measures than switching to another antidepressant, and more effective than augmenting with another antidepressant.6 Besides antidepressants, sedative-hypnotics were the second most common type of within-class polypharmacy in depressed adults, and we are unaware of any potential justification for this practice.
Third, the overall proportion of patients receiving between-class polypharmacy decreased slightly from 47.0% in 2006–2007 to 43.4% in 2014–2015, with the three most common patterns of between-class psychotropic prescriptions appearing as: an antidepressant and a sedative-hypnotic, an antidepressant and an antipsychotic, and an antipsychotic and a sedative-hypnotic. The combination of an antidepressant and an antipsychotic is an increasingly recognized strategy for treating unresponsive depression,7 which was also supported by the recent VAST-D RCT study.6,34 Furthermore, current guidelines suggest that augmented or adjunctive treatment of an antidepressant with one of four second-generation antipsychotics (aripiprazole, quetiapine, olanzapine plus fluoxetine, and brexipiprazole) are recommended, as the FDA approved such medication use for depressed adults who do not respond adequately to antidepressants in the US.7 While the FDA approvals took effect since 2007 (e.g., aripiprazole in 2007 and olanzapine with fluoxetine in 2009), these approvals did not change the polypharmacy rate. In the case of augmentation with an antipsychotic or mood stabilizer, it is also possible that unrecognized bipolar disorder contributes to apparently resistant depression among those treated with antidepressant prescriptions.35
The combination of an antidepressant and a sedative-hypnotic is potentially rational treatment based on co-morbid insomnia and other sleep disturbances, which are often considered important symptoms of depressive disorders.36–38 This combination may also reflect individualized treatment of patients with both depressive and anxiety disorders. In our study sample, more than 23% of patients with between-class polypharmacy had a diagnosis of a co-morbid depression and anxiety disorders, which may have resulted in potentially justifiable use of both antidepressant and sedative-hypnotic classes.
The combination of an antipsychotic and a sedative-hypnotic may also be accounted for by co-morbid psychiatric disorders in this population in which 27.9% of the study sample had co-occurring psychiatric disorders including anxiety, post-traumatic stress disorder, bipolar disorders, and schizophrenia. Thus, the combination of antipsychotic and sedative-hypnotic medications may have been co-prescribed to treat other psychiatric disorders. In our study, we also noticed that the combination of an antidepressant and a sedative-hypnotic was prescribed for some patients with both depression and anxiety. As most antidepressants also have antianxiety properties, this practice raises the question why a sedative-hypnotic would be used to target anxiety symptoms. In this regard, further research is needed to evaluate any advantage of this polypharmacy regimen and to address the potential risk of abuse or dependency of sedative-hypnotics.
Thus, in this study of outpatient psychiatric care, approximately 53.9% of visits, in which between-class psychotropics were prescribed, were potentially justified by treatment resistance or psychiatric multimorbidity. This finding, however, may have underestimated the actual proportion due to the features of survey design methodology. The NAMCS only collects up to three diagnoses using the ICD-9-CM diagnostic codes in randomly sampled visits. Thus, it may not capture all psychiatric co-morbid conditions, some of which may have been documented in previous visits or in different clinics. Alternatively, between-class psychotropic prescriptions may also be justified in cases in which the diagnosis changes over time. However, our study could not assess this possibility due to the cross-sectional nature of data.
Several clinical and policy implications derive from these findings. First, as a previous study revealed,39 psychiatric multimorbidity is common in real-world outpatient psychiatric care. While most RCTs are limited to patients with a single psychiatric disorder, our observational study suggest that many depressed adults have concurrent psychiatric disorders complicating their treatment and perhaps indicating a justifiable need to for polypharmacy. Additional RCTs are needed to assess the balance of improved patient outcomes, cost-effectiveness and safety in depressed adults in the context of multimorbidity. Such studies would further inform policy guidelines (e.g., implementing value-based quality of care models for prescribing psychotropics) and justify current prescribing practices.
Second, there have been efforts at discouraging presumably unnecessary psychotropic polypharmacy through quality assurance and performance improvement initiatives,40,41 physician training programs,42 and by developing and disseminating explicit criteria16 to reduce polypharmacy (e.g., Beers criteria22 for older adults). Despite these efforts, our study suggests that the psychotropic polypharmacy is still common in adults with depressive disorders and that such polypharmacy is potentially justified as individualized treatments of multimorbidity.
Several limitations in this study deserve comment. First, the study was limited to office-based psychiatric practice, and therefore, the results may not generalizable to other treatment settings (e.g., inpatient or emergency department settings). Second, as stated briefly earlier, the NAMCS documents a maximum of three diagnoses in a sampled visit, which may have led to incomplete documentation of multimorbidity in patient records. If patients were diagnosed with other psychiatric disorders in earlier visits or at different clinical sites, NAMCS may not capture such information. Furthermore, NAMCS cannot determine whether adults with depressive disorders initially received some of their currently prescribed psychotropic medications from different clinics. For these reasons, our findings may underestimate the magnitude of multimorbidity and psychotropic prescribing patterns.
Despite these limitations, the strengths of our study include delineating nationally consistent high levels of psychotropic polypharmacy over several years and highlighting the importance of multimorbidity as an important contextual consideration in the treatment of adults with depressive disorders. Our study shows that between-class psychotropic polypharmacy remains common in depressed adults, and that more than half of such polypharmacy is potentially justifiable by augmenting and/or adjunctive treatment strategies or multimorbidity. This study points to a need future research which addresses the effectiveness as well as potential adverse effects of polypharmacy for depression especially as it occurs in the context of psychiatric multimorbidity.
Highlights.
Psychiatric multimorbidity is common among depressed adults. Yet, little is known about to what extent between-class psychotropic polypharmacy may potentially be justified by multimorbidities in this population.
Altogether 53.9% of between-class polypharmacy is potentially justified by augmenting and/or adjunctive treatment strategies or psychiatric multimorbidity.
Understanding long-term effectiveness and patient safety of psychotropic polypharmacy in the context of multimorbidity is needed.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.World Health Organization. Depression: Fact sheet. 2017; http://www.who.int/mediacentre/factsheets/fs369/en/.
- 2.Rhee TG, Schommer JC, Capistrant BD, Hadsall RL, Uden DL. Potentially Inappropriate Antidepressant Prescriptions Among Older Adults in Office-Based Outpatient Settings: National Trends from 2002 to 2012. Adm Policy Ment Health. 2017: 10.1007/s10488-10017-10817-y. [DOI] [PubMed] [Google Scholar]
- 3.Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Veterans Affairs and Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Major Depressive Disorder. 2016; https://www.healthquality.va.gov/guidelines/MH/mdd/MDDFullFinal5192016.pdf.
- 5.Patkar AA, Pae CU. Atypical antipsychotic augmentation strategies in the context of guideline-based care for the treatment of major depressive disorder. CNS Drugs. 2013;27 Suppl 1:S29–37. [DOI] [PubMed] [Google Scholar]
- 6.Mohamed S, Johnson GR, Chen P, et al. Effect of Antidepressant Switching vs Augmentation on Remission Among Patients With Major Depressive Disorder Unresponsive to Antidepressant Treatment: The VAST-D Randomized Clinical Trial. JAMA. 2017;318(2):132–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhee TG, Mohamed S, Rosenheck RA. Antipsychotic prescriptions among adults With major depressive disorder in office-based outpatient settings: National trends from 2006 to 2015. J Clin Psychiatry. 2018;79(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore TJ, Mattison DR. Adult Utilization of Psychiatric Drugs and Differences by Sex, Age, and Race. JAMA Intern Med. 2017;177(2):274–275. [DOI] [PubMed] [Google Scholar]
- 9.Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry. 2010;67(1):26–36. [DOI] [PubMed] [Google Scholar]
- 10.Diagnosis Fava M. and definition of treatment-resistant depression. Biol Psychiatry. 2003;53(8):649–659. [DOI] [PubMed] [Google Scholar]
- 11.Karow A, Lambert M. Polypharmacy in treatment with psychotropic drugs: the underestimated phenomenon. Curr Opin Psychiatr. 2003;16(6):713–718. [Google Scholar]
- 12.Comer JS, Olfson M, Mojtabai R. National trends in child and adolescent psychotropic polypharmacy in office-based practice, 1996–2007. J Am Acad Child Adolesc Psychiatry. 2010;49(10):1001–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiechers IR, Kirwin PD, Rosenheck RA. Increased risk among older veterans of prescribing psychotropic medication in the absence of psychiatric diagnoses. Am J Geriatr Psychiatry. 2014;22(6):531–539. [DOI] [PubMed] [Google Scholar]
- 14.Millan MJ. On ‘polypharmacy’ and multi-target agents, complementary strategies for improving the treatment of depression: a comparative appraisal. Int J Neuropsychopharmacol. 2014;17(7):1009–1037. [DOI] [PubMed] [Google Scholar]
- 15.Moller HJ, Seemuller F, Schennach-Wolff R, Stubner S, Ruther E, Grohmann R. History, background, concepts and current use of comedication and polypharmacy in psychiatry. Int J Neuropsychopharmacol. 2014;17(7):983–996. [DOI] [PubMed] [Google Scholar]
- 16.Preskorn SH, Lacey RL. Polypharmacy: when is it rational? J Psychiatr Pract. 2007;13(2):97–105. [DOI] [PubMed] [Google Scholar]
- 17.McIntyre RS, Jerrell JM. Polypharmacy in children and adolescents treated for major depressive disorder: a claims database study. J Clin Psychiatry. 2009;70(2):240–246. [DOI] [PubMed] [Google Scholar]
- 18.Glezer A, Byatt N, Cook R, Jr., Rothschild AJ. Polypharmacy prevalence rates in the treatment of unipolar depression in an outpatient clinic. J Affect Disord. 2009;117(1–2):18–23. [DOI] [PubMed] [Google Scholar]
- 19.Fontanella CA, Warner LA, Phillips GS, Bridge JA, Campo JV. Trends in psychotropic polypharmacy among youths enrolled in Ohio Medicaid, 2002–2008. Psychiatr Serv. 2014;65(11):1332–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frye MA, Ketter TA, Leverich GS, et al. The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. J Clin Psychiatry. 2000;61(1):9–15. [DOI] [PubMed] [Google Scholar]
- 21.Bhalla IP, Rosenheck RA. A Change in Perspective: From Dual Diagnosis to Multimorbidity. Psychiatr Serv. 2018;69(1):112–116. [DOI] [PubMed] [Google Scholar]
- 22.American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015;63(11):2227–2246. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Ambulatory Health Care Data. 2017; https://www.cdc.gov/nchs/ahcd/index.htm, 2017.
- 24.American Society of Health-System Pharmacists. American Hospital Formulary Service (AHFS) Drug Information. In. Bethesda, MD: American Society of Health-System Pharmacists; 2017. [Google Scholar]
- 25.Rhee TG, Capistrant BD, Schommer JC, Hadsall RS, Uden DL. Effects of depression screening on diagnosing and treating mood disorders among older adults in office-based primary care outpatient settings: An instrumental variable analysis. Prev Med. 2017;100:101–111. [DOI] [PubMed] [Google Scholar]
- 26.Rhee TG, Choi YC, Ouellet GM, Ross JS. National prescribing trends for high-risk anticholinergic medications in older adults. J Am Geriatr Soc. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non-SSRIs in post-traumatic stress disorder: an update with recommendations. Drugs. 2004;64(4):383–404. [DOI] [PubMed] [Google Scholar]
- 28.Liu XH, Xie XH, Wang KY, Cui H. Efficacy and acceptability of atypical antipsychotics for the treatment of post-traumatic stress disorder: a meta-analysis of randomized, double-blind, placebo-controlled clinical trials. Psychiatry Res. 2014;219(3):543–549. [DOI] [PubMed] [Google Scholar]
- 29.Ahearn EP, Juergens T, Cordes T, Becker T, Krahn D. A review of atypical antipsychotic medications for posttraumatic stress disorder. Int Clin Psychopharmacol. 2011;26(4):193–200. [DOI] [PubMed] [Google Scholar]
- 30.Villarreal G, Hamner MB, Canive JM, et al. Efficacy of Quetiapine Monotherapy in Posttraumatic Stress Disorder: A Randomized, Placebo-Controlled Trial. Am J Psychiatry. 2016;173(12):1205–1212. [DOI] [PubMed] [Google Scholar]
- 31.Krystal JH, Rosenheck RA, Cramer JA, et al. Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: a randomized trial. JAMA. 2011;306(5):493–502. [DOI] [PubMed] [Google Scholar]
- 32.Stata Statistical Software: Release 15 [computer program]. College Station, TX: StataCorp LP; 2017. [Google Scholar]
- 33.Rush AJ, Trivedi MH, Stewart JW, et al. Combining medications to enhance depression outcomes (CO-MED): acute and long-term outcomes of a single-blind randomized study. Am J Psychiatry. 2011;168(7):689–701. [DOI] [PubMed] [Google Scholar]
- 34.Mohamed S, Johnson GR, Vertrees JE, et al. The VA augmentation and switching treatments for improving depression outcomes (VAST-D) study: Rationale and design considerations. Psychiatry Res. 2015;229(3):760–770. [DOI] [PubMed] [Google Scholar]
- 35.Correa R, Akiskal H, Gilmer W, Nierenberg AA, Trivedi M, Zisook S. Is unrecognized bipolar disorder a frequent contributor to apparent treatment resistant depression? J Affect Disord. 2010;127(1–3):10–18. [DOI] [PubMed] [Google Scholar]
- 36.Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mendlewicz J Sleep disturbances: core symptoms of major depressive disorder rather than associated or comorbid disorders. World J Biol Psychiatry. 2009;10(4):269–275. [DOI] [PubMed] [Google Scholar]
- 38.Murphy MJ, Peterson MJ. Sleep Disturbances in Depression. Sleep Med Clin. 2015;10(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhalla IP, Stefanovics EA, Rosenheck RA. Clinical Epidemiology of Single Versus Multiple Substance Use Disorders: Polysubstance Use Disorder. Med Care. 2017;55 Suppl 9 Suppl 2:S24–S32. [DOI] [PubMed] [Google Scholar]
- 40.Goren JL, Parks JJ, Ghinassi FA, et al. When is antipsychotic polypharmacy supported by research evidence? Implications for QI. Jt Comm J Qual Patient Saf. 2008;34(10):571–582. [DOI] [PubMed] [Google Scholar]
- 41.Little MO, Morley A. Reducing polypharmacy: evidence from a simple quality improvement initiative. J Am Med Dir Assoc. 2013;14(3):152–156. [DOI] [PubMed] [Google Scholar]
- 42.Tamura BK, Bell CL, Lubimir K, Iwasaki WN, Ziegler LA, Masaki KH. Physician intervention for medication reduction in a nursing home: the polypharmacy outcomes project. J Am Med Dir Assoc. 2011;12(5):326–330. [DOI] [PMC free article] [PubMed] [Google Scholar]