Abstract
Background:
Contraceptive nonadherence is an important contributor to unintended pregnancy in the United States. While the elimination of patient cost sharing has been cited as means to improve contraceptive access, little is known about the relationship between cost sharing and ongoing adherence and continuation of chosen methods. The purpose of this study was to examine the relationship between copayment amount and adherence to pharmacy-dispensed contraception in young women.
Methods:
We conducted a retrospective cohort study of 39,142 women ages 19–29 with a new prescription for the contraceptive pill, patch, or ring at Kaiser Permanente Northern California during 2011–2014. We examined 12-month nonadherence as measured by timely prescription refills and used multivariable Cox proportional hazards models to assess the association between copayment amount and the risk of nonadherence.
Results:
Ninety-four percent of women used the pill, and 6% used the patch or ring. Forty percent of patients had no copayment and 25% had a copayment of ≥ $30. Nearly 75% of women were non-adherent during the study period. In 2013 and 2014, women with a copayment had a 9% increased risk of nonadherence (adjusted hazard ratio, 1.09; 95% confidence interval, 1.04, 1.14) compared with women with no copayment.
Conclusions:
Prescription copayments may serve as a barrier to adherence of pharmacy-dispensed contraception. Given recent changes to Affordable Care Act contraceptive coverage requirement, these findings can be used to support state-level and health system-level policies for no-cost contraception, and to determine the potential public health impact of this policy change.
Keywords: contraceptive behavior, costs, women’s health
Nearly 70% of women using contraception in the United States use nonpermanent methods, primarily short-acting hormonal methods (eg, the pill, patch, implant, injectable, and vaginal ring) and condoms.1 Modern hormonal contraception is very effective at preventing pregnancy. However, incorrect and inconsistent contraceptive method use as well as method switching are common, placing women at risk for unintended pregnancy.2–4 Approximately 45% of all pregnancies in the United States are unintended each year, and over 40% of these pregnancies occur while a woman is inconsistently using contraception.5,6 Contraceptive nonadherence is a key concern. One study found that up to 700,000 unintended pregnancies each year could be prevented by increasing adherence to oral contraception alone.7 This is of concern as the oral contraceptive pill is the most commonly used contraceptive method in the United States, with ~26% of contraceptive users relying on the method.1
Several factors have been associated with contraceptive adherence, including individual-level sociodemographic, behavioral, and relationship factors as well as method characteristics.2, 8 Cost sharing is another important factor that may be associated with contraceptive adherence and consistent use, but has received relatively little attention in the literature. Cost sharing is the nonreimbursable financial contribution that patients make when they use health care services, and may be in the form of deductibles, coinsurance, or copayments. Many studies examining an array of chronic disease medications (eg, statin therapy for cholesterol, blood pressure lowering agents, diabetes medications) have shown that increased cost sharing is associated with decreased medication adherence.9, 10
High costs are a key barrier to contraceptive access,6 and studies have shown that out-of-pocket costs contribute to the methods women are able to choose and use.11 A 2004 survey found that one third of US women using reversible contraception would switch methods if they did not have to worry about cost.2 The landmark Contraceptive CHOICE study found that the elimination of cost sharing was associated with increased patient choice of long-acting reversible contraceptive methods that, at the time, generally required high initial out-of-pocket costs.12 Long-acting reversible contraceptives, such as intrauterine devices and subdermal implants, provide highly effective contraception for an extended time and require little intervention on the part of the user. Recently, a study evaluating the impact of the Affordable Care Act (ACA) coverage requirement, which mandates that most private health insurance plans provide coverage for Food and Drug Administration approved prescription contraceptives without cost sharing, found that reductions in cost sharing was associated with greater use of prescription contraceptives, particularly long-term methods.13
Although the impact of cost on patients’ contraceptive choices is well documented, there remains a paucity of data on the association between cost and ongoing adherence and continuation of chosen methods despite suggestions that this relationship could be significant. For example, one study examining the impact of the economic recession on women’s reproductive health found that some women using oral contraception reported that they tried to save money through inconsistently using the pill.2 Outside of this self-report data, only 2 studies have empirically assessed the relationship between cost sharing and contraceptive adherence to our knowledge. One focused on the relatively small female veteran population, and the other used insurance claims data that lacked information on patient-level characteristics, including sociodemographics.14,15 Recently issued regulations that have significantly broadened employers’ ability to be exempt from the ACA contraceptive coverage requirement may lead to a significant increase in out-of-pocket costs for contraceptives.16 It is important to better understand the relationship between cost sharing and contraceptive adherence, which can assist in determining the public health implications of changes to current policy. The purpose of this analysis was to examine the relationship between a key form of cost sharing, prescription copayments, and contraceptive refill adherence in an integrated delivery system. We hypothesized that higher prescription copayments would be associated with lower adherence to pharmacy-dispensed contraception, the contraceptive pill, patch, and ring.
METHODS
Study Design and Population
This retrospective cohort study analyzed data from Kaiser Permanente Northern California, a large integrated health delivery system serving ~4 million patients. Data in this study were drawn from the patient electronic health record (EHR), which combines diagnosis, utilization, pharmacy, and laboratory records from across the care system. The study was approved by the Institutional Review Board of Kaiser Permanente Northern California.
Our cohort consisted of female patients, ages 19–29 with prescription drug coverage and a new prescription dispensed for a pharmacy-dispensed contraceptive method, the oral contraceptive pill, contraceptive patch, or contraceptive ring, between January 2011 and June 2014. All women were “naïve” contraceptive users, meaning that they had no record of a contraceptive method dispensed or inserted in the 12 months before the index prescription date, which was defined as the date of the new contraceptive within the study time frame. Naïve users were examined to capture women likely planning to use their contraceptive method for some time. The oral contraceptive pill, contraceptive patch, and contraceptive ring are pharmacy-dispensed methods designed for a 28-day cycle, which may or may not have a nonactive medication week. Over 95% of health plan members have prescription drug coverage as a benefit, and members must fill their prescriptions at KPNC pharmacies in order to receive the benefit. We studied women 19–29 because of the high unintended pregnancy rate among women in this age group.5 Patients were followed for 12-month postindex date. We excluded patients who did not have at least 12-month KPNC membership before their index contraceptive prescription date and at least 13 months postdate, although a 30-day gap in membership was allowed (n = 61,695). Patients were also excluded if they had > 1 contraceptive method on record on the index date (n = 60) and > 15 prescriptions in a 12-month period (n = 2), as this may indicate contraceptive use for noncontraceptive reasons such as irregular bleeding. We excluded women who had been sterilized or had diagnosis and/or procedure codes for infertility, menopause, or hysterectomy (n = 2413). Finally, women who did not have a 3-month supply of contraception were excluded (n = 6893); ~85% of new prescriptions were for the 3-month supply, which is the typical amount dispensed in this care delivery system.
Measures
Outcome: Nonadherence
Our primary outcome measure was nonadherence to the index contraceptive method over a 12-month period, defined as a lack of timely dispensing of prescription refills (timely refills). Timely refills were defined as refills dispensed by the expected prescription end date based on the dispensed quantity. This approach is similar to the one used by Nelson et al17 in their investigation of real-world patterns of prescription refills for hormonal contraceptives. We allowed patients a grace period, or gap, of up to 14 days following the expected prescription end date to allow for variability in the date of fill and medication use. The prescription end date was adjusted for subsequent refills when a prescription was dispensed before the expected end date. We conducted sensitivity analyses using a grace period of up to 21 days; results were similar to 14 days.
Prescription Copayment
Our independent variable of interest was prescription copayment, which reflects the dollar amount that was paid by the patient for the contraceptive prescription on the index prescription date. We defined copayment amounts in 4 categories based on the observed distribution: $0, <$15, <$30, and ≥ $30. For the regression analyses, copayment was a dichotomous variable indicating whether the patient had a copayment or not.
Other Covariates
We examined several other variables as covariates based on predictors of contraceptive nonadherence in other published studies, including patient age (categorical), self-identified race/ethnicity, socioeconomic status, and whether the patient had an abortion in the past 12 months. Individual-level socioeconomic status was unavailable in the EHR, so the socioeconomic status variable is a geocoded census-level variable based off patients’ zip code indicating whether ≥ 20% of the households were below the federal poverty level.
Statistical Analysis
We reported summary statistics (counts, percentages) to describe cohort characteristics, prescription copayments, and nonadherence. We constructed Kaplan-Meier survival functions to estimate the time to nonadherence (eg, the first untimely prescription refill) among the entire cohort and by copayment amount. Patients with timely refills during the entire 12-month period were right censored. The bivariate association between prescription copayment amount and nonadherence was assessed using the log rank test. A multi-variable Cox proportional hazards model was constructed to determine association between prescription copayment amount and contraceptive nonadherence while adjusting for other key predictors of nonadherence and year of initiation (2011 and 2012; pre-ACA contraceptive mandate/2013 and 2014; post-ACA contraceptive mandate). We also tested for an interaction between copayment and year of method initiation to test for possible effect modification using the log-likelihood statistic. The Cox proportional hazards model predicted nonadherence as defined as the time to first occurrence of an untimely/late refill. The proportional hazards assumption was evaluated by fitting time-dependent covariates and examining the Wald test. On the basis of this assessment, the final models were stratified by the selected contraceptive method (pill vs. patch/ring), giving one set of hazard ratios for covariates that are assumed to be constant across the selected method. We report adjusted hazard ratios (aHR) and 95% confidence intervals (CI). Significance was noted at P-value <0.05. Analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
Our final cohort included 39,142 patients. The vast majority of patients were ages 19–24 (Table 1), with a mean age of 22.4 (SD, 3.3) (data not shown). The cohort was racially and ethnically diverse; less than half were non-Hispanic white. Approximately 10% of women lived in a low-income census tract and 3% had an abortion in the past year. Over 90% of women in this cohort used the oral contraceptive pill.
TABLE 1.
Characteristics of Women With a New Prescription for Pharmacy-dispensed Hormonal Contraception (Contraceptive Pill or Patch/Ring) by Copayment Amount, Kaiser Permanente Northern California, 2011–2014(n = 39,142)
| Characteristics | Total | Copayment for Contraceptive Prescription | P | |||
|---|---|---|---|---|---|---|
| $0 | <$15 | <$30 | ≥$30 | |||
| 37.98 | 21.72 | 13.50 | 26.80 | |||
| Method | < 0.001 | |||||
| Pill | 93.74 | 93.49 | 96.08 | 95.97 | 91.06 | |
| Patch/ring | 6.26 | 6.51 | 3.92 | 4.03 | 8.94 | |
| Age (y) | < 0.001 | |||||
| 19–24 | 72.64 | 76.87 | 75.56 | 75.02 | 63.09 | |
| 25–29 | 27.36 | 23.13 | 24.44 | 24.98 | 36.91 | |
| Race/ethnicity | < 0.001 | |||||
| Non-Hispanic white | 46.33 | 44.61 | 45.41 | 45.56 | 49.90 | |
| Non-Hispanic black | 7.51 | 8.97 | 7.22 | 9.35 | 4.74 | |
| Hispanic | 21.92 | 22.89 | 22.30 | 19.89 | 21.25 | |
| Asian | 17.83 | 16.94 | 18.80 | 18.22 | 18.11 | |
| Other/unknown | 6.42 | 6.60 | 6.27 | 6.98 | 6.01 | |
| Low-income residence* | < 0.001 | |||||
| Yes | 10.71 | 11.65 | 9.84 | 10.23 | 10.31 | |
| No | 89.29 | 88.35 | 90.16 | 89.77 | 89.69 | |
| Abortion in the past | 0.71 | |||||
| 12 mo | ||||||
| Yes | 2.84 | 2.73 | 2.94 | 2.78 | 2.94 | |
| No | 97.16 | 97.27 | 97.06 | 97.22 | 97.06 | |
Residence in census tract with ≥ 20% incomes below the Federal Poverty Level; missing n = 16.
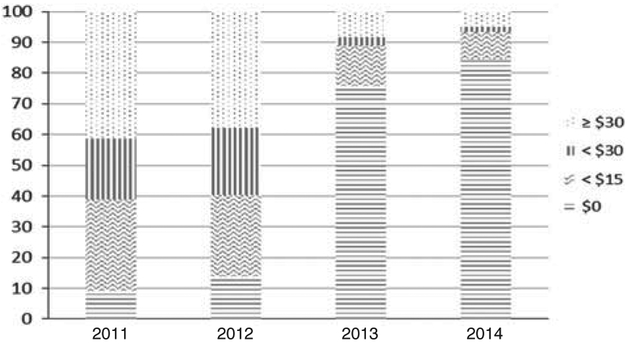
Nearly 40% of the patients had no copay for their prescription contraception, and slightly more than a quarter had a copayment of over $30 (Table 1). The median copay was ~$10 (data not shown). Women using the patch or ring were more likely than pill users to have a copayment of ≥ $30 (P < 0.001). Patient age, race/ethnicity, and socioeconomic status were all significantly associated with copayment. For example, younger women were more likely to have no copayment (P < 0.001), and 45% of black women had no copayment compared with 37% of white women (P < 0.001). As shown in Figure 1, copayments for prescription contraception changed dramatically over the study period. For example, ~9% of women had no copayment in 2011, while over 80% of women had no copayment in 2014.
FIGURE 1.
Copayment amount for pharmacy-dispensed contraception (contraceptive pill or patch/ring) by year of method initiation, Kaiser Permanente Northern California, 2011–2014.
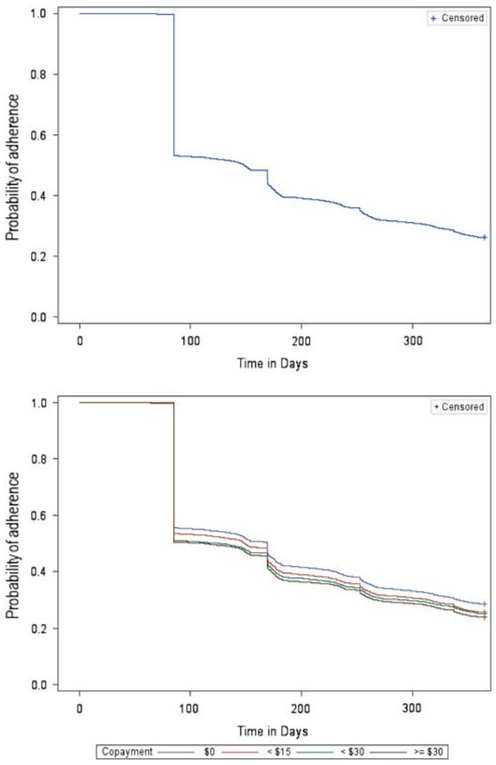
Nonadherence among women with a new prescription for pharmacy-dispensed contraception was high. By 12 months, nearly three fourths of women had an untimely refill of their prescription contraception following the initial prescription fill. The median time to initial nonadherence in this cohort was 148 days. As shown in Figure 2, the largest drop in adherence occurred at ~90 days.
FIGURE 2.
Kaplan-Meier curve demonstrating time to non-adherence to the contraceptive pill, patch or ring, overall (top), and by copayment amount (bottom), Kaiser Permanente Northern California, 2011–2014.
Kaplan-Meier curves demonstrating time to non-adherence showed significant differences by copayment amount (P < 0.001) (Fig. 2). The median time to nonadherence for women with no copayment was 169 days compared with 149 days for women with a copayment <$15, 127 days for women with a copayment <$30, and 113 days for women with a copayment of ≥ $30. At 12 months, nonadherence was highest among women with a copayment of ≥ $30, followed by women with a copayment of <$30, <$15, and women with no copayment (76.1%, 74.4%, 74.8%, 71.5%, respectively).
The multivariable Cox proportional hazards model indicated an interaction between copayment and contraceptive nonadherence by year. In 2011 and 2012, the risk of non-adherence was not significantly different among those with a copayment compared with those without one (aHR, 0.98; 95% CI, 0.94, 1.03) (Table 2). However, in 2013 and 2014, women with a copayment were more likely than those without a copayment to be nonadherent, with an increased risk of ~9% (aHR, 1.09; 95% CI, 1.04, 1.14). Patient race/ethnicity, age, socioeconomic status, and abortion status were also significantly associated with nonadherence during both time periods. The strongest predictor of nonadherence was patient race/ethnicity. Non-Hispanic black women had ~40% increase in risk of contraceptive nonadherence compared with non-Hispanic white women (2011–2012 aHR, 1.40; 95% CI, 1.32, 1.48).
TABLE 2.
Association Between Contraceptive Copayment and Nonadherence to the Contraceptive Pill, Patch, or Ring by Year of Initiation, Kaiser Permanente Northern California, 2011–2014
| 2011/2012 | 2013/2014 | |
|---|---|---|
| aHR (95% CI) | aHR (95% CI) | |
| Copayment | ||
| No ($0) | REF. | REF. |
| Yes (>$0) | 0.98 (0.94, 1.03) | 1.09 (1.04, 1.14) |
| Age (y) | ||
| 19–24 | REF. | REF. |
| 25–29 | 1.08 (1.05, 1.17) | 1.20 (1.15, 1.26) |
| Race/ethnicity | ||
| Non-Hispanic white | REF. | REF. |
| Non-Hispanic black | 1.40 (1.32, 1.48) | 1.40 (1.30, 1.50) |
| Hispanic | 1.19 (1.15, 1.24) | 1.26 (1.20, 1.33) |
| Asian | 1.13 (1.08, 1.18) | 1.13 (1.07, 1.19) |
| Other/unknown | 1.10 (1.03, 1.17) | 1.06 (0.98, 1.14) |
| Low-income census tract | ||
| Yes | 1.07 (1.02, 1.12) | 1.11 (1.04, 1.17) |
| No | REF. | REF. |
| Abortion in the past 12 mo | ||
| Yes | 1.14 (1.05, 1.24) | 1.31 (1.17, 1.46) |
| No | REF. | REF. |
aHR indicates adjusted hazard ratio; CI, confidence interval; REF., reference.
DISCUSSION
In this integrated care delivery system, adherence to pharmacy-dispensed contraception—the pill, patch, or ring—was low. Nearly 75% of young women starting a contraceptive method had at least one untimely refill over the 12-month study period. This finding is consistent with the finding that contraceptive discontinuation and inconsistent use is common in the United States. Of interest, a large drop in adherence occurred at ~3 months, which is the standard dispensed quantity amount in this care delivery system. Our data suggest that a large proportion of women with new contraceptive prescriptions obtain the initial fill, but do not return to refill the prescription. Prior studies have shown that the greater number of packs dispensed is associated with higher continuation.18 However, these studies have been observational, and it is possible that that providers dispense more packs to women with a higher likelihood of continuation.
The proportion of women with no copayment increased dramatically over the study period, which covered the implementation of the contraceptive mandate of the ACA. This finding is consistent with several other studies that have demonstrated a sharp reduction in out-of-pocket costs for prescription contraception since 2013 when the contraceptive mandate was implemented.19–22 We found that patient copayments were a risk factor for nonadherence, but only following the implementation of the contraceptive mandate of the ACA. In 2013 and 2014, ~20% of women in this cohort had a copayment for their contraceptive prescription. These women were at a greater risk of nonadherence than women who had no copayment. Following the implementation of the contraceptive mandate, women who still had a copayment for contraception were likely covered by “grandfathered” plans, which did not require the full range of contraceptive methods to be covered without cost sharing. In 2014, 26% of American workers covered in employer sponsored plans were still in grandfathered plans.23 It is possible that women in these plans differed from women who benefited from the contraceptive mandate in ways that made the expense associated with consistently refilling prescriptions prohibitive. In another investigation of cost sharing and contraceptive adherence, Pace et al15 similarly found that even small amounts of cost sharing increased nonadherence and discontinuation during 2010–2013, although this analysis was unable to control for patient-level factors. It is estimated that 1.64 million unintended pregnancies each year are due to imperfect contraceptive adherence.24 Using this estimate, our findings suggest that removing copayments for contraception has the potential to prevent a nontrivial proportion of unintended pregnancies each year.
Several of the covariates included in our multivariable analyses were significantly associated with contraceptive nonadherence, including patient race/ethnicity, having an abortion in the past year, and census-level socioeconomic status. Patient race/ethnicity was the strongest predictor of nonadherence in our analysis. Both before and after the implementation of the contraceptive mandate, non-Hispanic black and Hispanic women had ~40% and 20% increased risk of nonadherence, respectively, compared with non-Hispanic white women. While several other studies have noted higher contraceptive nonadherence and discontinuation among racial and ethnic minorities, our findings suggest that these disparities persist even an insured population of women with access to contraception.8, 25, 26 Further research is needed to elucidate the specific reasons or barriers to adherence among minority populations and develop tailored interventions that can support consistent method use in these groups.
Our investigation is one of the only studies to look at the relationship between copayments and contraceptive adherence. Strengths of our study include the use of a large and racially/ethnically diverse sample of young women and the use of the robust EHR data which included demographic and reproductive characteristics. However, several limitations should be noted. First, pharmacy data only documents that the refill was obtained; it does not provide information on actual medication use. However, pharmacy data has been noted as an objective source of adherence data and may be less biased than patient self-report.27 Second, we examined the copayment amount for the index prescription. It is possible that a patient’s copayment may have changed over the 12-month follow-up period, particularly following the implementation of the contraceptive mandate. However, it is reasonable to believe patients expect to pay the same amount for their prescription as their first fill given that changes to benefits usually occur on a yearly basis. Another limitation is that we are unable to know the reason for contraception non-adherence. It is possible that women did not fill their prescriptions on time because they desired pregnancy or did not need contraception any longer. It is also possible that women discontinued one method to use another method. However, further analyses indicated that, among women who were nonadherent to their selected method, ~90% did not switch to other methods in the 12-month follow-up period. Finally, the findings of the study are based on one care delivery system and the outcomes of insured women and, as such, may not be generalizable to the larger population of young women using short-acting hormonal contraception.
Contraceptive nonadherence remains an important contributor to unintended pregnancy in the United States. Our results suggest that, copayments may be a barrier to continuous contraceptive use for some young women. Prescription copayments are potentially modifiable and offer a system-level approach to improving contraceptive use and decreasing unintended pregnancy. This information can be used to support state-level and system-level policies for no-cost contraception considering recent changes to ACA contraceptive coverage requirement, and to determine the public health impact of recent changes to this policy.
ACKNOWLEDGMENTS
The authors acknowledge the Kaiser Permanente Northern California, Division of Research Delivery Science Fellowship Program and the Kaiser Permanente Northern California Community Benefit Program.
Footnotes
Earlier versions of the analyses described in this manuscript were presented at the Academy Health Annual Research Meeting, New Orleans, LA, June 26, 2017.
The authors declare no conflict of interest.
REFERENCES
- 1.Daniels K, Daugherty J, Jones J, et al. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013. Natl Health Stat Report. 2015;86:1–14. [PubMed] [Google Scholar]
- 2.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40:94–104. [DOI] [PubMed] [Google Scholar]
- 3.Frost JJ, Darroch JE, Remez L. Improving contraceptive use in the United States. Issues Brief (Alan Guttmacher Inst). 2008:1–8. [PubMed] [Google Scholar]
- 4.Vaughan B, Trussell J, Kost K, et al. Discontinuation and resumption of contraceptive use: results from the 2002 National Survey of Family Growth. Contraception. 2008;78:271–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sonfield A, Hasstedt K, Gold R. Moving Forward: Family Planning in the Era of Health Reform. New York: Guttmacher Institute; 2014. [Google Scholar]
- 7.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998; 179:577–582. [DOI] [PubMed] [Google Scholar]
- 8.Pittman ME, Secura GM, Allsworth JE, et al. Understanding prescription adherence: pharmacy claims data from the Contraceptive CHOICE Project. Contraception. 2011;83:340–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eaddy MT, Cook CL, O’Day K, et al. How patient cost-sharing trends affect adherence and outcomes: a literature review. P T. 2012;37:45–55. [PMC free article] [PubMed] [Google Scholar]
- 10.Sinnott SJ, Buckley C, O’Riordan D, et al. The effect of copayments for prescriptions on adherence to prescription medicines in publicly insured populations; a systematic review and meta-analysis. PLoS One. 2013;8: e64914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gariepy AM, Simon EJ, Patel DA, et al. The impact of out-of-pocket expense on IUD utilization among women with private insurance. Contraception. 2011;84:e39–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Secura GM, Allsworth JE, Madden T, et al. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115.e111–115.e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carlin CS, Fertig AR, Dowd BE. Affordable Care Act’s mandate eliminating contraceptive cost sharing influenced choices of women with employer coverage. Health Aff (Millwood). 2016;35:1608–1615. [DOI] [PubMed] [Google Scholar]
- 14.Kazerooni R, Vu K, Takizawa A, et al. Association of copayment and socioeconomic status with hormonal contraceptive adherence in a female veteran population. Womens Health Issues. 2014;24:e237–e241. [DOI] [PubMed] [Google Scholar]
- 15.Pace LE, Dusetzina SB, Keating NL. Early impact of the Affordable Care Act on oral contraceptive cost sharing, discontinuation, and non-adherence. Health Aff (Millwood). 2016;35:1616–1624. [DOI] [PubMed] [Google Scholar]
- 16.Sobel L, Salganicoff A, Rosenzweig C. New Regulations Broadening Employer Exemptions to Contraceptive Coverage: Impact on Women. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2017. [Google Scholar]
- 17.Nelson AL, Westhoff C, Schnare SM. Real-world patterns of prescription refills for branded hormonal contraceptives: a reflection of contraceptive discontinuation. Obstet Gynecol. 2008;112:782–787. [DOI] [PubMed] [Google Scholar]
- 18.Steenland MW, Rodriguez MI, Marchbanks PA, et al. How does the number of oral contraceptive pill packs dispensed or prescribed affect continuation and other measures of consistent and correct use? A systematic review. Contraception. 2013;87:605–610. [DOI] [PubMed] [Google Scholar]
- 19.Bearak JM, Finer LB, Jerman J, et al. Changes in out-of-pocket costs for hormonal IUDs after implementation of the Affordable Care Act: an analysis of insurance benefit inquiries. Contraception. 2016;93: 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Becker NV, Polsky D. Women saw large decrease in out-of-pocket spending for contraceptives after ACA mandate removed cost sharing. Health Aff (Millwood). 2015;34:1204–1211. [DOI] [PubMed] [Google Scholar]
- 21.Law A, Wen L, Lin J, et al. Are women benefiting from the Affordable Care Act? A real-world evaluation of the impact of the Affordable Care Act on out-of-pocket costs for contraceptives. Contraception. 2016;93:392–397. [DOI] [PubMed] [Google Scholar]
- 22.Sonfield A, Tapales A, Jones RK, et al. Impact of the federal contraceptive coverage guarantee on out-of-pocket payments for contraceptives: 2014 update. Contraception. 2015;91:44–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sobel L, Beamesderfer A, Salganicoff A. Private Insurance Coverage of Contraception. Menlo Park, CA: Kaiser Family Foundation; 2016. [Google Scholar]
- 24.Trussell J, Henry N, Hassan F, et al. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87:154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raine TR, Foster-Rosales A, Upadhyay UD, et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117:363–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stuart JE, Secura GM, Zhao Q, et al. Factors associated with 12-month discontinuation among contraceptive pill, patch, and ring users. Obstet Gynecol. 2013;121:330–336. [DOI] [PubMed] [Google Scholar]
- 27.Triebwasser JE, Higgins S, Secura GM, et al. Pharmacy claims data versus patient self-report to measure contraceptive method continuation. Contraception. 2015;92:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]