Abstract
We evaluated the visual and refractive outcomes after phakic visian toric implantable collamer lens (ICL) insertion in stable keratoconus (KC). This retrospective study investigated toric ICL implantation in 14 eyes of 8 patients with stable KC. After 6mo, the mean uncorrected distance visual acuity improved significantly from 0.77 to 0.15 logMAR. The mean best corrected distance visual acuity (BCDVA) improved from 0.18±0.1 to 0.15±0.1 logMAR. Fifty percent of eyes maintained their preoperative BCDVA; 42.8% gained one line. There was no statistical difference in high order or coma aberration. The mean refractive manifest spherical equivalent (MSE), mean refractive manifest spherical error, mean manifest astigmatism decreased significantly postoperatively. At 6mo postoperatively, our achieved mean spherical equivalent was approximately 74%. No intraoperative or postoperative complications occurred. Toric ICL implantation was effective, predictable and safe to correct refractive error and improve visual acuity in patients with stable KC.
Keywords: coma, keratoconus, lens implantation, intraocular
INTRODUCTION
Keratoconus (KC) is a progressive type of non-inflammatory corneal degeneration characterized by stromal thinning and ectasia of the cornea leading to a decrease in visual acuity as a result of myopia, irregular astigmatism and corneal scarring[1]–[2]. Various visual rehabilitation options are available including contact lenses, intracorneal ring segments (ICRS), phakic intraocular lenses (pIOL), and photorefractive keratectomy[3]. Corneal cross linking (CXL) can be combined with all of these techniques to stabilize KC[4]–[6].
The implantable collamer lens (ICL; Visian; STAAR Surgical, Nidau, Switzerland), which is used as a posterior chamber pIOL, is made from collamer, a biocompatible hydrophilic copolymer of collagen and hydroxyethyl methacrylate with an ultraviolet light-filtering chromophore[7]. A toric ICL is typically indicated for the correction of myopia in adults aged 21-40y with myopia up to -18.0 diopters (D) with up to 6.0 D of astigmatism. Toric ICL cannot correct irregular corneal astigmatism; therefore, it is an alternative method to correct myopia and myopic astigmatism in eyes with stable KC for partial visual rehabilitation[8].
SUBJECTS AND METHODS
Ethical Approval
The study complied the principles outlined in the Declaration of Helsinki. Written consent was obtained from all patients. None of our patients received any stipend. Clinical study registration number: ACTRN12618000909224.
In this retrospective study, the visual and refractive outcomes of patients with KC who underwent ICL (STAAR Surgical Inc., Switzerland) implantation to correct myopia and myopic astigmatism were investigated. Patients were considered eligible if they were over 21y of age, had a stable refraction for 1y after CXL, contact lenses intolerant, and significant improvement in best corrected distance visual acuity (BCDVA) with refraction. Eligible patients had no other ocular and general pathology and no greater than stage 2 KC according to the Amsler-Krumeich classification[9]. Additional inclusion criteria were clear central cornea, central or centralized (with ICRS) cone, an anterior chamber depth (ACD) greater than 3.0 mm (from the endothelium), a mesopic pupil size of less than 6.5 mm.
The lens power calculation was performed by online calculation software (STAAR Surgical Co., Switzerland). The calculation is based on: manifest refraction (the axis of astigmatism is the axis obtained by manifest refraction), corneal curvature, corneal thickness and ACD measured by Pentacam (OCULUS Optikgeräte GmbH, Wetzlar, Germany). High order aberration (HOA) are measured by an Optical Path difference (OPD III scan, NIDEK Inc., Gamagori, Japan).
The suitable ICL size was determined based on the horizontal white-to-white distance measured with a caliper. Emmetropia was selected as the postoperative target refraction.
Current V4C ICL design was used. Under local anesthesia, dilating agents were administered. For the toric ICL implantation, the axis was marked using Neuhann-Nuijts One-Step Toric Marker (Asico, Westmont, IL, USA) while the patient was lying upright to prevent cyclotorsion. Small 3.2 mm clear temporal corneal incision was made. After injection of viscoelastic material (Provisc, Alcon, Fort Worth, TX, USA), ICL was injected and allowed to slowly unfold. Haptics were tucked under the iris and the toric ICL was aligned to the desired axis. Toric ICL are manufactured to minimize rotation and require the surgeon to rotate the lens no more than 22.0° from the horizontal meridian. All toric ICLs have a diagram to demonstrate the amount and direction of rotation from the horizontal axis. Irrigation and aspiration of the viscoelastic material were performed. Hydration of the surgical incisions was performed at the end of surgery. Postoperatively, moxifloxacin 0.5% (Vigamox; Alcon, Fort Worth, TX, USA) was prescribed four times daily for 1wk, and prednisolone acetate 1% (PredForte; Allergan, Inc., Dublin, Ireland) was prescribed six times daily for 1wk. The dose of prednisolone was then tapered on weekly basis over a period of 4wk.
Postoperative evaluation included a slit lamp examination, uncorrected distance visual acuity (UCDVA), manifest refraction, BCDVA, corneal topography and HOA during 6-month follow-up visit.
Statistical Analysis
Data was revised for its completeness and consistency. Double data entry on SPSS program (version 20, USA) was done. Quantitative data was summarized by mean, standard deviation while qualitative data was summarized by frequencies and percentages. Student's t-test, paired t-test were used in analysis of this paper. P<0.05 was considered statistically significant.
RESULTS
The study included 14 eyes of 8 patients. The mean age was 29.6y (range: 21 to 44y). CXL was performed on ten eyes (71.4%). All patients (100%) underwent a complete follow-up from baseline up to 6mo after ICL implantation. ICRS were inserted in one eye 6mo prior to phakic ICL to improve corneal shape decrease corneal irregularity and improve BCDVA. The same toric ICLs was implanted in all eyes; six patients underwent bilateral implantation while the remaining two patients had unilateral toric ICL implantation. The mean preoperative spherical equivalent (SE) power was -4.8±2.25 D (range: -2 to -9.4 D). Preoperatively, the mean spherical power was -3.7±1.9 D (range: -0.75 to -6.5 D) and the mean cylindrical power was 2.3±1.60 D (range: 0.75 to 5.5 D). Mean steep K (Ksteep) at 3 mm was 45.3±2.8 (range 43.4-47.7). Mean average pupillary power was 44.8±3.2 (range 40.4-51.6). Mean RMS of spherical, coma-like, and HOA were 0.09, 0.49, and 0.60 microns, respectively, for a 4.0-mm simulated pupil diameter. Surface regularity index (SRI) was 1.13±0.3 (range 0.57-1.48).
Visual Outcomes
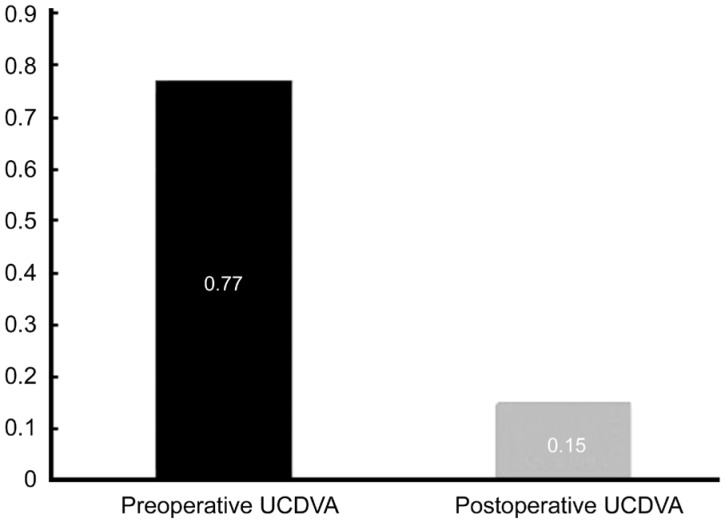
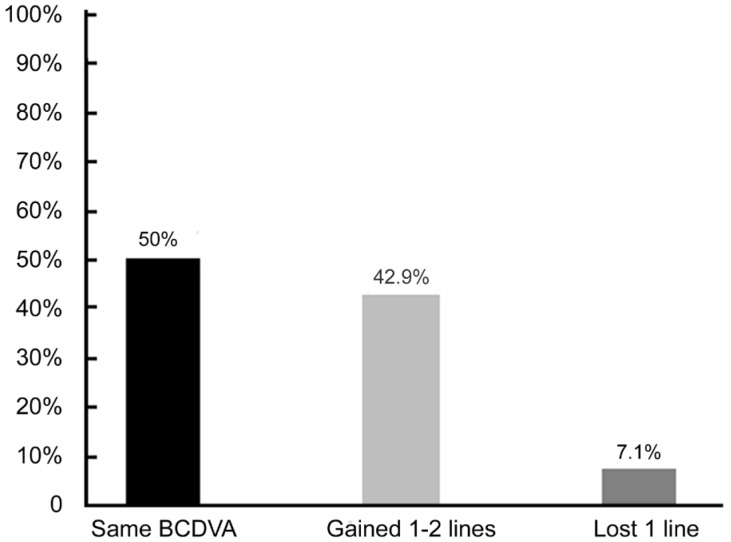
The mean UCDVA improved significantly from 0.77±0.2 logMAR to 0.15±0.1 (P<0.01 highly significant; Figure 1). The mean BCDVA was 0.18±0.1 logMAR preoperatively compared to 0.15±0.1 postoperatively. Fifty percent of eyes (7/14) maintained the same preoperative BCDVA; 42.9% of eyes (6/14) gained 1-2 lines and 7.1% (1/14) lost one line (Figure 2).
Figure 1. Comparison between preoperative and postoperative UCDVA logMAR.
P<0.01 were highly significant.
Figure 2. Postoperative changes of BCDVA line.
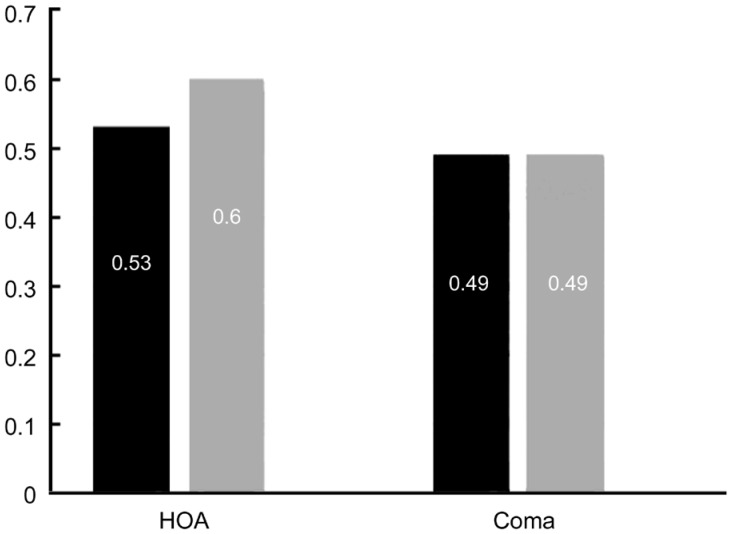
Coma aberration which is the most common aberration in KC, showed no statistical difference between preoperative and postoperative values (0.49±0.6 vs 0.49±0.4 respectively). There was no statistically significant difference in HOA (RMS) between before and after surgery (0.6±0.2 compared to 0.53±0.3 respectively; Figure 3).
Figure 3. Comparison between preoperative and postoperative mean coma and HOA aberrations.
P>0.05 weren't significant.
Refractive Outcomes
The mean preoperative manifest spherical equivalent (MSE) decreased from -4.8±2.25 to -0.3±0.4 D, which was statistically significant (P<0.01 highly significant). The mean preoperative manifest spherical error decreased from -3.7±1.9 to -0.2±0.5 D, which also was statistically significant (P<0.01 highly significant). The mean preoperative manifest astigmatism decreased significantly from -2.3±1.6 to -0.6±-0.5 D (P<0.01 highly significant).
At 6mo after surgery our achieved mean SE was about 74% of our attempted mean SE. Sixty-five percent of eyes were within ±0.75 D of the attempted SE correction and 85% were within ±1.0 D of the attempted SE correction.
DISCUSSION
Corneal regularity is a very important factor for postoperative potential visual acuity. Highly aberrated eyes are accompanied with poor BCDVA and accordingly poor postoperative UCDVA. SRI is an indicator for corneal irregularity, which increase with increasing irregular astigmatism and is highly correlated with potential visual acuity. A toric ICL corrects only spherical and cylindrical errors of refraction, it cannot correct HOAs caused by an irregular corneal shape. Patients who have a good spectacle corrected visual acuity would benefit from toric ICL implantation. Cases who have a cornea that is too irregular to have a good corrected distance visual acuity (CDVA) except with rigid contact lenses, will not improve after toric ICL implantation. All our cases with Ksteep less than 52.0 D and SRI less than 1.5.
Regarding effectiveness (preoperative BCDVA comparing with postoperative UCDVA), about 93% (13/14) of eyes maintained their same preoperative BCDVA or gained 1-2 lines, only 7% (1/14) of eyes lost one line of preoperative BCDVA (due to residual spherical error). No intraoperative or postoperative complication occurred.
A toric ICL does not induce HOAs, since after toric ICL implantation, our patients still had the same amount of HOA despite correcting the high amount of myopia and myopic astigmatism. We were able to correct up to 6.5 D of myopia and up to 5.0 D of astigmatism with precise axis alignment.
Regarding predictability, at 6mo after surgery our achieved SE was about 74% of our attempted SE. Sixty-five percent of eyes were within ±0.75 D of the attempted SE correction and 85% were within ±1.0 D of the attempted SE correction.
Our study demonstrated a clinically significant improvement in postoperative UCDVA in all patients; this is in concurrence with the results of other studies[10]–[12]. About 50% of the eyes in our study maintained their preoperative BCDVA and 43% gained 1-2 lines, only 7% of eyes lost one line of BCDVA. In a study by Kamiya et al[10], 44% of their eyes showed no change in in BCDVA and 48% gain 1-2 lines and only 7% lost one line. A study by Navas et al[11] which had a long follow up period (38mo), showed that 9/11 (82%) of their eyes gained 1-3 lines of BCDVA, 1/11 (9%) presented no change and 1/11 (9%) lost one line. Kurian et al[12] assessed postoperative BCDVA of their patients at 6mo. Totally 40% had no change, 30% gained two lines, 10% gained three or more lines and 20% of eyes lost one line.
The aberrations associated with an irregular cornea in KC that are uncorrected by the pIOL have an effect on the final visual quality. A phakic toric ICL can correct a high degree of myopic astigmatism without inducing new HOA. This was documented in our study as there were no clinically significant changes in HOA or coma aberration at 6mo postoperatively.
At 6mo after surgery our achieved SE was about 74% of our attempted SE. Sixty-five percent of eyes were within ±0.75 D of the attempted SE correction and 85% were within ±1.0 D of the attempted SE correction. The postoperative mean SE decreased to -0.3±0.4 D at 6mo and the mean manifest spherical error decreased to -0.2±0.5 D at 6mo. The mean manifest astigmatism decreased to -0.6±-0.5 D at 6mo follow up. In a study by Kurian et al[12], the preoperative mean refractive SE decreased to -0.44±1.21 D at 6mo. Shafik Shaheen et al[13] had a postoperative SE of -0.25 D at 3y of follow up in 16 eyes that had early KC. Antonios et al[14] showed that the mean SE improved to -0.83±0.76 D. The mean cylinder also improved to 1.03±0.60 D and these values were maintained during the follow-up over 12mo. In a longer follow up period, Doroodgar et al[15] reported 82% of eyes were within ±0.50 D, and 97.05% were within ±1.0 D of attempted correction. Mean MSE was -0.07±0.5 and -0.01±0.48 D, at 1 and 4y respectively. None of their patients showed decrease in UCVA. Twenty-four eyes have increased in UCVA by ≥1 line. At 24mo follow up, Abdelmassih et al[16] concluded that UCVA improved significantly from 1.06 to 0.76 logMAR and the BCVA from 0.42 to 0.26 logMAR. Keratometric values and UCVA were stable, whereas BCVA, sphere, and cylinder values showed a significant improvement in the period between 6mo and 2y.
An accurate ICL calculation is very challenging in moderate and advanced KC. Refractive outcome depends on accurate manifest refraction and intraoperative accurate axis alignment measurements.
In conclusion, implantation of the toric ICL was an effective, predictable and safe option to correct refractive error and to improve visual acuity in patients with stable KC and regular cornea. High corneal irregularity limits the potential visual acuity and may need another surgery to make the cornea more regular.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Conflicts of Interest: Emerah SH, None; Sabry MM, None; Saad HA, None; Ghobashy WA, None.
REFERENCES
- 1.Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 2.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 3.Fernández-Vega-Cueto L, Romano V, Zaldivar R, Gordillo CH, Aiello F, Madrid-Costa D, Alfonso JF. Surgical options for the refractive correction of keratoconus: myth or reality. J Ophthalmol. 2017;2017:7589816. doi: 10.1155/2017/7589816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dirani A, Fadlallah A, Syed ZA, Chelala E, Khoueir Z, Cherfan G, Jarade E. Non-topography-guided photorefractive keratectomy for the correction of residual mild refractive errors after ICRS implantation and CXL in keratoconus. J Refract Surg. 2014;30(4):266–271. doi: 10.3928/1081597X-20140320-05. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira TB, Güell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30(5):336–341. doi: 10.3928/1081597X-20140319-01. [DOI] [PubMed] [Google Scholar]
- 6.Sakla H, Altroudi W, Muñoz G, Albarrán-Diego C. Simultaneous topography-guided partial photorefractive keratectomy and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2014;40(9):1430–1438. doi: 10.1016/j.jcrs.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009;127(7):845–850. doi: 10.1001/archophthalmol.2009.67. [DOI] [PubMed] [Google Scholar]
- 8.Kamiya K, Shimizu K, Ando W, Asato Y, Fujisawa T. Phakic toric implantable collamer lens implantation for the correction of high myopic astigmatism in eyes with keratoconus. J Refract Surg. 2008;24(8):840–842. doi: 10.3928/1081597X-20081001-12. [DOI] [PubMed] [Google Scholar]
- 9.Sinjab MM. Quick guide to the management of keratoconus; a systematic step-by-step approach. Berlin, Germany: Springer-Verlag; 2012. pp. 13–58. [Google Scholar]
- 10.Kamiya K, Shimizu K, Kobashi H, Komatsu M, Nakamura A, Nakamura T, Ichikawa K. Clinical outcomes of posterior chamber toric phakic intraocular lens implantation for the correction of high myopic astigmatism in eyes with keratoconus: 6-month follow-up. Graefes Arch Clin Exp Ophthalmol. 2011;249(7):1073–1080. doi: 10.1007/s00417-010-1540-5. [DOI] [PubMed] [Google Scholar]
- 11.Navas A, Tapia-Herrera G, Jaimes M, Graue-Hernández EO, Gomez-Bastar A, Ramirez-Luquín T, Ramirez-Miranda A. Implantable collamer lenses after intracorneal ring segments for keratoconus. Int Ophthalmol. 2012;32(5):423–429. doi: 10.1007/s10792-012-9582-9. [DOI] [PubMed] [Google Scholar]
- 12.Kurian M, Nagappa S, Bhagali R, Shetty R, Shetty BK. Visual quality after posterior chamber phakic intraocular lens implantation in keratoconus. J Cataract Refract Surg. 2012;38(6):1050–1057. doi: 10.1016/j.jcrs.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Shafik Shaheen M, El-Kateb M, El-Samadouny MA, Zaghloul H. Evaluation of a toric implantable collamer lens after corneal collagen crosslinking in treatment of early-stage keratoconus: 3-year follow-up. Cornea. 2014;33(5):475–480. doi: 10.1097/ICO.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 14.Antonios R, Dirani A, Fadlallah A, Chelala E, Hamade A, Cherfane C, Jarade E. Safety and visual outcome of visian toric ICL implantation after corneal collagen cross-linking in keratoconus: up to 2y of follow-up. J Ophthalmol. 2015;2015:514834. doi: 10.1155/2015/514834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doroodgar F, Niazi F, Sanginabadi A, Niazi S, Baradaran-Rafii A, Alinia C, Azargashb E, Ghoreishi M. Comparative analysis of the visual performance after implantation of the toric implantable collamer lens in stable keratoconus: a 4-year follow-up after sequential procedure (CXL+TICL implantation) BMJ Open Ophthalmol. 2017;2(1):e000090. doi: 10.1136/bmjophth-2017-000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdelmassih Y, El-Khoury S, Chelala E, Slim E, Cherfan CG, Jarade E. Toric ICL implantation after sequential intracorneal ring segments implantation and corneal cross-linking in keratoconus: 2-year follow-up. J Refract Surg. 2017;33(9):610–616. doi: 10.3928/1081597X-20170621-02. [DOI] [PubMed] [Google Scholar]