Abstract
Introduction
Japan has experienced extremely low human papillomavirus vaccine (HPVV) coverage following the suspension of proactive governmental recommendations in 2013. Several studies have reported that recommendations from physicians increase adolescents’ vaccine acceptance. In this survey, we evaluated the attitudes and intentions of Japanese physicians related to adolescent immunizations, particularly HPVV.
Methods
We conducted a cross-sectional study using a mailed questionnaire targeting 330 Japanese physicians including 78 pediatricians, 225 internists and 27 obstetricians and gynecologists (OB/GYNs) in Kawasaki City, Japan in 2016. The survey measured physicians’ reported frequency of educating adolescents about vaccines as well as their own perceptions and intentions related to adolescent immunizations.
Results
Valid responses were obtained from 148 (45%) physicians. Though 53% agreed that the HPVV should be recommended, only 21% reported educating about HPVV. The majority of respondents (90%) agreed that they would restart HPVV for adolescents if the government reinstated its recommendation.
Conclusions
Although Japanese physicians reported support for adolescent immunizations, they were less likely to recommend or discuss HPVV compared with other adolescent vaccines. Responses indicated this was, at least in part, due to the lack of governmental support for HPVV, indicating that their recommendations would improve with government endorsement of the vaccine.
Keywords: Adolescent vaccination, Human papillomavirus vaccine, Vaccination coverage, Physician, Japan
1. Introduction
Maintaining immunization coverage is important for preventing morbidity and mortality caused by vaccine preventable diseases (VPDs). Recently, low immunization coverage among adolescents including human papillomavirus vaccine (HPVV) has been reported in some countries, including Japan [[1], [2], [3], [4]]. Health care system barriers include variable immunization laws and regulations that govern vaccine requirements and exemption policies in Japan [5,6]. Some studies also reported personal or provider related barriers to HPVV in Japan such as lower vaccine acceptance among parents and lack of physician recommendation [7,8]. Even in the United States (US), a country with a strong immunization program and recommendations, several studies report barriers that make increasing adolescent immunization coverage difficult including safety concerns, lack of knowledge about HPVV, no provider recommendation, personal beliefs, lack of access to healthcare services and competing priorities in an adolescent's schedule (e.g., extra-curricular activities, low priority for seeking medical care) [[9], [10], [11], [12], [13]]. Provider-related barriers have also been reported in the US, such as lack of knowledge about HPVV, negative attitudes toward adolescent immunizations, inconsistent strength of recommendation, and missed opportunities [[14], [15], [16], [17], [18], [19], [20], [21]].
In Japan, HPVV and diphtheria tetanus toxoid vaccine (DT) have been recommended as routine immunizations for adolescents under the National immunization Programs (NIP) since 2013 and 1981, respectively. Vaccines that are included in NIP are supplied by the national government free of charge to Japanese citizens. In 2016, DT coverage was 76.9% - lower than routine vaccines targeting infants and young children [22]. When HPVV was first introduced by NIP in 2013, it was recommended for girls 12–16 years of age; HPVV coverage was around 70% [23]. In addition, 9-valent HPVV (HPV9) is not licensed in Japan; instead, only 2-valent HPVV (HPV2) and 4-valent HPVV (HPV4) versions are available. Both are administered in a 3-dose series at 0, 1 to 2, and 6 months. Since the Ministry of Health, Labour and Welfare (MHLW) suspended their proactive recommendation for HPVV in 2013, HPVV coverage has dropped to 0.6% for this same group, despite availability of the vaccine. The HPVV recommendation was removed after reports of adverse events following immunization (AEFI) [24]. Individuals reported experiencing conditions such as complex regional pain syndrome (CRPS) and postural orthostatic tachycardia syndrome (POTS) following receipt of HPVV. The precipitous drop in HPVV caused by vaccine safety concerns in Japan is similar to the negative impact of vocal anti-vaccine contingencies in Denmark [25] and Ireland [26]. Recently, the formation of powerful cross-sectoral alliances has led to rapid improvement in vaccine uptake in Ireland [26]. However, in Japan, despite a lack of evidence to support these conditions as being causally associated with receipt of HPVV, the recommendation has not been reinstated by the MHLW. HPVV is still classified as a NIP vaccine even after suspension of proactive governmental recommendations, and both HPV2 and HPV4 are supplied to adolescents without cost; however, HPVV is infrequently administered.
Inactivated influenza vaccines (IIV) are also available to adolescents as a voluntary vaccine. “Voluntary vaccines” are categorized as non-NIP and must be paid for “out of pocket” by individuals. As a result, adolescent IIV coverage is only about 40% [27]. Additional vaccines licensed and recommended for adolescents in other countries like quadrivalent meningococcal vaccine (ACYW-135), tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine and serogroup B Meningococcal (MenB) vaccine are not a part of the immunization program in Japan.
Several studies have reported that physician recommendations increase adolescent vaccine acceptance [9,11,[14], [15], [16]], particularly in the case of HPVV [[17], [18], [19], [20], [21]]. Most vaccines for adolescents are delivered by physicians in public and private clinics in Japan. However, to the best of our knowledge, few researchers have investigated the role of physician attitudes and intentions related to adolescent immunizations in Japan. Kawasaki City is one of the largest cities located in the suburbs of Tokyo, Japan. Despite vaccination coverages rates above 90% for most NIP covered vaccines in Kawasaki City (e.g., Haemophilus influenzae type B vaccine, 13-valent pneumococcal conjugate vaccine, diphtheria-tetanus-acellular pertussis and inactivated poliovirus vaccine, measles-rubella vaccine), rates for 3 doses of HPVV was only 0.3% in 2015 [28], similar to coverage rates in other large cities in Japan. In comparison, DT coverage was 70.5% in 2015, and IIV is not captured for children in Kawasaki City because it is categorized as a “non-NIP” vaccine. In this exploratory survey, we evaluated physicians’ attitudes and intentions regarding adolescent immunizations by specialty in order to better understand the potential role of physicians in strategies to improve adolescent immunization uptake, particularly HPVV.
2. Methods
2.1. Study design and procedures
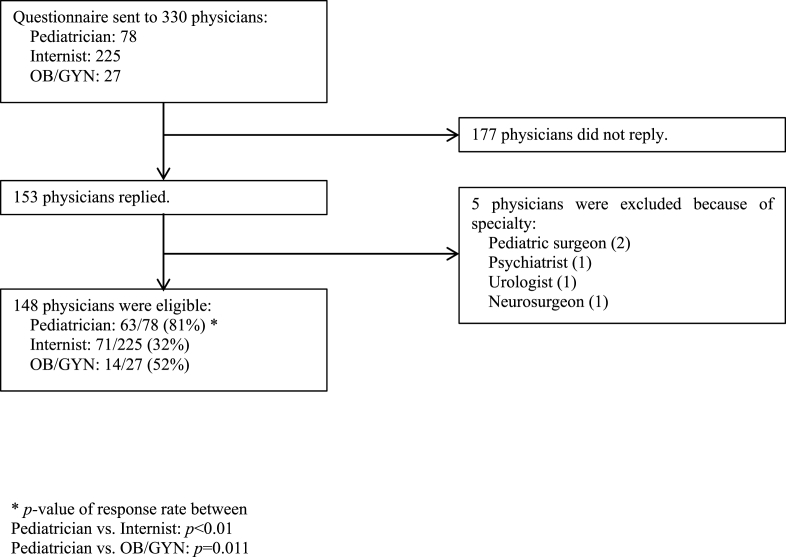
A cross-sectional survey was mailed through the postal service to 330 Japanese physicians parcticing in 299 medical facilities between October and November in 2016. We sent the survey to medical facilities that were registered to the immunization cooperative healthcare facility in Kawasaki City. Facilities ranged in size from small clinics to large hospitals. Surveys were addressed to the facility and not a particular physician. Directions indicated that if more than one physician from the same specialty worked at the same clinic or hospital, only one physician within that specialty should reply. This was done to prevent greater numbers of responses by providers from large facilities, which may be similar by virtue of their similar practice environment, from biasing the conclusions of the study. We sent up to 3 survey forms by mail to each facility depending on the number of specialties of interest represented by providers (pediatrics, internal medicine, obstetrics - gynecology). Invitations were sent to 78 pediatric, 225 internal medicine and 27 obstetricians and gynecologist (OB/GYN) departments. We included OB/GYNs and internists because HPVV are sometimes provided by both provider groups in Japan. While physician sub-specialists, such as dermatologists, orthopedists or brain surgeons can immunize adolescents against IIV, we excluded them from the list of invited participants for this survey. Reminder postcards were sent to all practices 6 weeks after the first invitation. A total of 153 physicians replied to the survey; however, 5 were excluded because their specialties were outside of our inclusion criteria: (Pediatric surgeon (2), Psychiatrist (1), Urologist (1), Neurosurgeon (1)). Valid responses were obtained from the remaining 148 participants (45%) of 330 invited physicians (Fig. 1).
Fig. 1.
Survey summary.
2.2. Questionnaire
The survey tool was developed by adapting items from previously published studies [9,29] and was subsequently reviewed by a small number of practicing physicians in Japan for accuracy of translation. The survey included questions about the frequency of providing education to adolescent patients or guardians and personal perceptions and intentions of adolescent immunizations. We defined an adolescent as a person between 10 and 19 years of age. Nine questions about the frequency of providing education addressed 3 major topics: vaccines, VPDs, and sexual health (Table 2). Two questions about sexual health were added to understand the context in which HPVV is discussed. Responses were measured using a 4-point scale (Regularly, Sometimes, Previously, Never). Three questions addressed physicians' perceptions related to vaccine recommendations, concerns about vaccine safety and vaccine effectiveness (Table 3). Lastly, one question assessed physician intention to recommend HPVV if the MHLW were to reinstate their recommendation (Table 4). Responses to the majority of questions related to physicians’ perceptions and intentions were measured using a 5-point Likert scale (Strongly agree, Somewhat agree, Undecided, Somewhat disagree, Strongly disagree) while intended HPVV recommendation behavior was measured using 4 response categories (Recommended actively, If patients or guardians request, Not yet determined, Never recommend). This survey was approved by the institutional review board of St. Marianna University School of Medicine.
Table 2.
Educational practices related to adolescent vaccines, VPDs∗4 and sexual health.
| General Topic | Specific topic | % education group∗1 (education/total number) |
|||||
|---|---|---|---|---|---|---|---|
| Total | Pediatrician | Internist | OB/GYN∗4 | p | |||
| Adolescent vaccines | HPVV∗4 | 21 (26/122) | 22 (11/49) | 17 (10/59) | 36 (5/14) | Ped ∗4vs. Int∗4: p = 0.64 Ped vs. OB/GYN: p = 0.64 Int vs. OB/GYN: p = 0.44 |
|
| DT∗4 | 62∗3a (82/133) | 81 (51/63) | 49 (31/63) | 0 (0/7) | Ped vs. Int: p < 0.01 Ped vs. OB/GYN: p < 0.01 Int vs. OB/GYN: p = 0.15 |
||
| IIV∗4 | 89∗3b (117/132) | 90 (53/59) | 91 (58/64) | 67 (6/9) | Ped vs. Int: p = 1 Ped vs. OB/GYN: p = 0.23 Int vs. OB/GYN: p = 0.23 |
||
| VPDs | Cervical cancer | 24 (29/121) | 28 (13/47) | 15 (9/60) | 50 (7/14) | Ped vs. Int: p = 0.30 Ped vs. OB/GYN: p = 0.30 Int vs. OB/GYN: p = 0.026 |
|
| Diphtheria | 28 (37/132) | 37 (23/62) | 22 (14/63) | 0 (0/7) | Ped vs. Int: p = 0.24 Ped vs. OB/GYN: p = 0.24 Int vs. OB/GYN: p = 0.33 |
||
| Tetanus | 47 (62/132) | 61 (38/62) | 38 (24/63) | 0 (0/7) | Ped vs. Int: p = 0.025 Ped vs. OB/GYN: p = 0.007 Int vs. OB/GYN: p = 0.087 |
||
| Influenza | 86∗3c (112/131) | 91 (53/58) | 84 (54/64) | 56 (5/9) | Ped vs. Int: p = 0.28 Ped vs. OB/GYN: p = 0.044 Int vs. OB/GYN: p = 0.13 |
||
| Sexual health | General education∗2 | 12 (15/123) | 6 (3/49) | 13 (8/60) | 29 (4/14) | Ped vs. Int: p = 0.45 Ped vs. OB/GYN: p = 0.11 Int vs. OB/GYN: p = 0.045 |
|
| HPV∗4 related STIs∗4 | 17 (21/123) | 16 (8/49) | 12 (7/60) | 43 (6/14) | Ped vs. Int: p = 0.58 Ped vs. OB/GYN: p = 0.13 Int vs. OB/GYN: p = 0.039 |
||
*1 Education group includes respondents who chose “regularly” or “sometimes”.
*2 General education indicates any educational topics related to sexual health, not specifically HPV or STIs.
*3 Statistical analysis.
a p < 0.01 vs. HPVV.
b p < 0.01 vs. HPVV, p < 0.01 vs. DT.
c p < 0.01 vs. Cervical cancer, p < 0.01 vs. Diphtheria, p < 0.01 vs. Tetanus.
*4 Abbreviations.
VPDs: vaccine preventable diseases, OB/GYN: Obstetrics/Gynecology, Ped: Pediatrician, Int: Internist.
HPVV: human papillomavirus vaccine, DT: diphtheria tetanus toxoid vaccine, IIV: inactivated influenza vaccine.
HPV: human papillomavirus, STIs: sexual transmitted infections.
Table 3.
Perceptions related to recommendations, safety, and efficacy of adolescent vaccines.
| Survey Questions | % agreement group*1 (agreement/total number) |
|||
|---|---|---|---|---|
| HPVV∗2 | DT∗2 | IIV∗2 | p | |
| Vaccine recommendation The MHLW∗2 should restart the proactive recommendation of HPVV. | 53 (78/147) | |||
| DT, IIV should be recommended for adolescent actively. | 83 (118/142) | 80 (114/142) | DT vs. IIV: p = 0.58 | |
|
Concern about vaccine safety I have concerns about the safety of this vaccine. |
26 (38/146) | 2 (3/139) | 1 (2/141) | HPVV vs. DT: p < 0.01 HPVV vs. IIV: p < 0.01 DT vs. IIV: p = 0.82 |
|
Concern about vaccine effectiveness I have concerns about the effectiveness of this vaccine. |
12 (17/147) | 5 (7/140) | 20 (28/142) | HPVV vs. DT: p = 0.09 HPVV vs. IIV: p = 0.06 DT vs. IIV: p < 0.01 |
*1 Agreement group includes respondents who chose “strongly agree” or “somewhat agree” when answering these questions.
*2 Abbreviations.
MHLW: Ministry of Health, Labour and Welfare, HPVV: human papillomavirus vaccine, DT: diphtheria tetanus toxoid vaccine, IIV: inactivated influenza vaccine.
Table 4.
Responses related to approach to policy changes and education.
| Survey Questions | % positive responses∗1 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Pediatrician | Internist | OB/GYN*2 | p | |||||
| % HPVV*2 acceptance group (acceptance/total number) [% “Recommended actively”, % “If patients/guardians request”] | |||||||||
| [HPVV] | |||||||||
|
Change of policy (%) If the MHLW*2 reinstates the proactive recommendation of HPVV, I would restart HPVV for adolescents. |
90 (117/130) [44, 46] | 89 (48/54) [39, 50] | 90 (56/62) [47, 43] | 93 (13/14) [50, 43] | Ped*2 vs. Int*2: p = 1 Ped vs. OB/GYN: p = 1 Int vs. OB/GYN: p = 1 |
||||
| % agreement group (agreement/total number) | |||||||||
| [HPVV] | |||||||||
|
Lack of confidence for education skill about STIs*2related HPV*2(%) I don't have enough education skills about STIs related HPV. |
48 (70/146) | 51 (31/61) | 52 (37/71) | 14 (2/14) | Ped vs. Int: p = 1 Ped vs. OB/GYN: p = 0.05 Int vs. OB/GYN: p = 0.05 |
||||
| [DT*2] | |||||||||
|
Lack of awareness of importance to DT for prevention of diphtheria (%) DT vaccine is not required because incidence of diphtheria is extremely rare. |
9 (13/142) | 3 (2/62) | 12 (8/69) | 27 (3/11) | Ped vs. Int: p = 0.20 Ped vs. OB/GYN: p = 0.07 Int vs. OB/GYN: p = 0.20 |
||||
|
Lack of awareness of importance to DT for prevention of tetanus (%) DT vaccine is not required because incidence of tetanus is extremely rare. |
9 (13/142) | 2 (1/62) | 12 (8/69) | 36 (4/11) | Ped vs. Int: p = 0.070 Ped vs. OB/GYN: p = 0.004 Int vs. OB/GYN: p = 0.07 |
||||
| [IIV*2] | |||||||||
|
Lack of awareness of importance to IIV for prevention of influenza (%) IIV is not required because incidence of severe influenza is extremely rare. |
3 (4/142) | 0 (0/61) | 3 (2/70) | 18 (2/11) | Ped vs. Int: p = 0.50 Ped vs. OB/GYN: p = 0.07 Int vs. OB/GYN: p = 0.18 |
||||
*1 % positive responses includes respondent choices of “recommend actively” or “if patients/guardians agree” for HPVV policy question (identified as “HPVV acceptance group” in text) or “strongly agree” or “somewhat agree” for confidence and awareness questions (identified as “agreement group” in text).
*2 Abbreviations.
OB/GYN: Obstetrics/Gynecology, HPVV: human papillomavirus vaccine, MHLW: Ministry of Health, Labour and Welfare.
Ped: Pediatrician, Int: Internist, STIs: sexual transmitted infections, HPV: human papillomavirus.
DT: diphtheria, tetanus toxoid vaccine, IIV: inactivated influenza vaccine.
2.3. Statistical analysis
We measured the frequency of providing vaccine or VPD education and perceptions for each adolescent vaccine or VPD and compared results by physician specialty. We categorized physicians to the “education group” when they chose “Regularly” or “Sometimes” for frequency of providing vaccine education. Similarly, we categorized physicians to the “agreement group” when they chose “Strongly agree” or “Somewhat agree” for positive perceptions of adolescent vaccines. To distinguish between providers that would give HPVV, either upon request or through active promotion, from those who will not give the vaccine, we categorized those who chose “Recommended actively” or “If patients or guardians request” as the “HPVV acceptance group.”
Differences between each vaccine and VPD were analyzed respectively using multiple comparison Ryan's method [30]. In addition, eligible physicians were divided into three groups by their specialties and differences were analyzed by the pairwise Fisher-test with Holm correction. Estimated parameters were considered significant if their associated p-values were ≤0.05. All analyses were conducted using R version 3.3.2 (2016, The R Foundation for Statistical Computing, http://www.R-project.org/).
3. Results
3.1. Characteristics of study subjects
Median age of physician respondents was 55 years old (Range: 34–88), and 78% were male (Table 1). These demographics were similar to 2016 national statistics in which the median age of physicians who belong clinics in Japan was 59.6 years old and 81% were male [31]. In addition, in this survey, percent of males practicing in each specialty was 68% pediatricians, 92% internists, and 57% OB/GYNs. These demographics were also similar to national data in which 68% of pediatricians, 86% of internists, and 76% of OB/GYNs in Japan were male [31]. The response rate from pediatricians was significantly higher than other groups (81% versus 32% internists and 52% OB/GYNs) (Fig. 1). As a result, the study population was composed of 43% pediatricians, 48% internists, and 9% OB/GYNs. The median years of experience as a physician was 30 years (Range: 9 to 60). Eighty-three percent practiced in private clinics, and 91% provided vaccines to less than 50 teen patients per month. Fourteen (9%) physicians did not supply any vaccine to their adolescent patients in a one month period. However, we included all of them when analyzing responses about intention to recommend any vaccines including HPVV. The majority (64%) of these respondents were OB/GYNs who typically only provide HPVV. As such, their intentions related to HPVV in the context of the suspended governmental recommendation in Japan are important to understand.
Table 1.
Characteristics of study participants (N = 148).
| Variable | N (%) |
|---|---|
| Age (y) Median (IQR) Range |
55 (47–62) 34-88 |
| Gender Female Male |
32 (22) 116 (78) |
| Specialty Pediatrician Internist OB/GYN |
63 (43) 71 (48) 14 (9) |
| Years of experience as physician Median (IQR) Range |
30 (20–36) 9-60 |
| Affiliation Clinic Hospital |
123 (83) 25 (17) |
| Number of teen patients vaccinated per month 0 1-49 50-99 100-199 200-299 No answer |
14 (9) 122 (82) 8 (5) 1 (1) 1 (1) 2 (2) |
3.2. Provision of education
3.2.1. Education about adolescent vaccines
Overall, only 21% respondents reported that they provide HPVV education, significantly fewer than the proportion who provided education about IIV and DT (Table 2). Similar trends were observed within each specialty but there were no significant differences in the frequency of HPVV education among specialties. OB/GYNs were significantly less likely than other specialties to educate about DT (Table 2).
3.2.2. Education about VPDs
Overall, a significantly higher proportion of respondents reported providing education about influenza compared with other VPDs, and among specialist types, significant differences were detected for different diseases (Table 2). Specifically, pediatricians were most likely to educate about tetanus and influenza infection; whereas, OB/GYNs were most likely to educate about cervical cancer.
3.2.3. Education about sexual health
Only a few providers educated about sexual health. Frequency of education about human papillomavirus (HPV)-related sexually transmitted infections (STIs) was also low among pediatricians and internists; however, OB/GYNs educated significantly more frequently than internists (Table 2).
3.3. Perceptions about the safety, effectiveness, and recommendation of adolescent vaccines
Although almost all (92%) respondents acknowledged the lack of recommendation for HPVV immunization by the Japanese MHLW, 53% providers also agreed that the government's proactive recommendations for HPVV should be re-established (Table 3). A higher proportion of respondents (26%) reported having concerns about HPVV safety compared to DT or IIV; however, they were less concerned (12%) about HPVV effectiveness (Table 3). A significantly higher proportion of respondents (20%) reported concerns about IIV effectiveness compared to DT. There was no significant difference between specialties related to perceptions about the effectiveness, or safety of adolescent vaccines (data not shown).
3.4. Intentions related to adolescent vaccine questions
Almost all (90%) respondents indicated that they would restart HPVV for adolescents if the MHLW reinstates their proactive recommendation (HPVV acceptance group) (Table 4). Forty-four percent of physicians chose the answer “recommended actively”. When compared across physicians’ specialties, pediatricians (51%) and internists (52%) reported being significantly less confident educating about STIs related to HPV than OB/GYNs (14%) (Table 4). Results related to vaccines other than HPVV differed among specialist types. Specifically, OB/GYN felt DT and IIV immunizations were less important than other specialties (Table 4). Significant differences were also observed among specialists related to the prevention of tetanus (Table 4).
4. Discussion
In this exploratory survey, we evaluated attitudes and intentions regarding adolescent vaccines including HPVV, DT and IIV among a sample of Japanese physicians in Kawasaki City.
Importantly, we observed significant differences in the frequency of education about HPVV compared to the other adolescent vaccines included in the NIP. This lack of education may due to a few factors. First, this finding may, at least in part, be due to suspension of the proactive recommendation by the Japanese government in 2013. Most Japanese physicians do not inoculate girls in the HPVV target age because few parents ask for it. In this survey, the majority of physicians indicated that they would recommend HPVV for adolescents if the MHLW recommendation were to be reinstated. Second, HPVV safety concerns among physicians may also play a role. Many Japanese public media outlets have reported concerns about HPVV safety [24] raising fears in Japanese society as a whole. In this survey, 26% of physicians reported concerns about the safety of HPVV, significantly higher than concerns reported about the other NIP adolescent vaccines. Although these may not be the only factors contributing to low HPVV rates in Japan, physician recommendation is recognized as one of the most powerful predictors of HPVV acceptance [21]. Several studies have reported that provider-focused interventions, including provision of information about adolescent vaccines, have the potential to improve immunization coverage [7,8,[32], [33], [34], [35], [36]]. Although the majority of such studies were completed outside of Japan, given the percent of physicians indicating HPVV safety concerns in our sample, informational resources and provider education are likely to be one area that will need attention in order to improve HPVV coverage rates in Japan. In addition, changing policy may be an even more important intervention. Only half of the physicians in our sample (53%) agreed that the MHLW should restart proactive recommendation of HPVV. On the other hand, almost all respondents indicated they would recommend HPVV for adolescents if the government reinstates its proactive recommendation for HPVV even if they reported low confidence discussing HPV. This paradoxical result demonstrates the significant influence governmental recommendations have on decision-making among Japanese physicians and further highlights the profound impact of the lack of governmental support for reinstating the HPVV recommendation as highlighted by Larson [37]. Notably, around one third of OB/GYN did not think the DT vaccine is necessary because the diseases it prevents are rare. Additionally, 47% of physicians did not believe the government should restart proactive recommendations for the HPVV. These results suggest hesitancy toward adolescent vaccines that should be further evaluated. Some Japanese physicians may have inadequate knowledge about VPDs themselves and would benefit from education.
We also observed important differences in educational practices and intention to vaccinate between physician specialties. The findings likely reflect differences in clinical expertise and align with those of other studies. In our study, pediatricians and internists more frequently provided education about tetanus infection and DT than OB/GYNs. Sakai et al. reported that pediatrician density was positively and significantly associated with immunization coverage for diphtheria, tetanus and acellular pertussis (DTaP) vaccine and measles vaccine series in Japan [38]. On the other hand, OB/GYNs educated more frequently about HPVV-related issues including cervical cancer and sexual health. Indeed, in a survey of 49 physicians in the US, including 40 pediatricians, Alexander et al. reported that one-third of adolescent patients had annual health maintenance visits to their clinic without any discussion of sexual health. They also reported that Asian-American physicians were significantly less likely to have discussions related to sexual health with adolescents than physicians categorized as non-Asian [39]. However, the comparison was based on responses from small number of Asian-American physicians (only 3 physicians), and to the best of our knowledge, the influence of discussions about sexual health by Japanese physicians on HPVV uptake has not been assessed. Similar to the findings of other groups, few pediatricians reported providing education about sexual health and nearly half indicated a lack of confidence when discussing STIs and HPV. However, growing evidence suggests that HPVV recommendations that highlight cancer prevention may be associated with greater HPVV acceptance [40,41]. Given that many providers are not currently discussing sexual health and other studies indicate the effectiveness of discussions about HPVV as an opportunity to prevent cancer, if the HPVV recommendation is reinstated, provision of education and supporting messages related cancer prevention may be more effective.
These results also highlight the importance of engaging other specialists who provide care to adolescents. In particular, as discussed above, our sample of OB/GYNs indicated frequently providing education about STIs and may, therefore, be well-positioned to offer a strong endorsement of HPVV. Mazzoni et al. reported that an educational intervention targeting OB/GYNs providing outpatient care increased immunization coverage rates for both HPVV and IIV [42]. However, while any physician can vaccinate in Japan, those with experience doing so may be more equipped to deal with parental concerns and anxieties both before and after vaccination. Therefore, educating about these issues would be an important consideration in expanding the types of providers who give vaccines regularly.
Sawada et al. recently reported that the intentions of Japanese OB/GYNs regarding HPVV have become more positive compared to 2014 when they were first surveyed. Specifically, 61% versus 73.6% of OB/GYNs surveyed believed that the Japanese government should restart the proactive recommendation of HPVV in 2014 versus 2017, respectively [43,44]. They also reported higher rates of intention to recommend the HPVV (65.2% in 2014 to 70.1% in 2017) despite the lack of support by the MHLW. Their increasing endorsement may be due to WHO position statements about OB/GYN involvement in HPVV delivery and the publication of an epidemiological study completed in Japan [43]. Together, these findings suggest that HPVV rates may be improved in Japan if OB/GYNs can be engaged by either increasing their opportunities to administer this vaccine or by partnering with pediatricians and internists to share messaging related to the importance of HPVV. Even in the absence of a recommendation from the MHLW in Japan, providers could increasingly rely on the WHO and scientific/medical professional bodies statements when talking with parents about the importance of HPVV. Likewise, as pointed out by Larson [37], using data related to declining rates of cervical cancer in Europe and North America along with conversations related to the lack of screening opportunities in Japan may also empower Japanese-based providers to increase HPVV rates despite the current government position.
Our study presents one of the few assessments of attitudes and intentions to vaccination related to adolescent immunizations among Japanese physicians. While our results identify factors associated with education and recommendation behavior that could inform future interventions, our survey has a few important limitations. First, we mailed a cross-sectional survey to medical facilities through the postal service without addressing to particular physicians within in each facility. This could have led to the survey not reaching the best people to complete the survey. In addition, if more than one physician from the same specialty worked at the same clinic or hospital, we requested that only one arbitrary physician from each specialty in each facility complete the survey to prevent a confounding impact from larger facilities. However, because an arbitrary physician's point of view might not reflect that of the majority in the facility, the results may not be generalizable to other physicians working at similar. Further, sending a mailed survey to a large facility without addressing a specific individual may have caused fewer to be delivered to a qualified participant, inadvertently selecting against larger facilities. The extent to which these biases would be reflected in the data is uncertain. However, this is an exploratory study, so despite these limitations, the results can provide information to inform larger studies designed in a way to address these limitations. Our overall response rate approached 50% which is within the range frequently reported for survey-based studies among physicians. However, the response rate was low for internists and OB/GYNs. As such, their responses may not be generalizable to all internists and OB/GYNs. The difference in response rate may also impact the reliability of our comparisons between specialties. We conducted sample size calculations and estimated that a sample of 32 participants in each group would provide 80% power to detect difference among physicians' specialties (effect size, 0.5). Our study had only 14 OB/GYNs, thus limiting the statistical power to detect a difference. However, we did not exclude them from this survey because they have knowledge, particularly related to HPVV that evaluating their attitudes and intentions related to adolescent vaccines could provide meaningful information. Additionally, we only surveyed physicians from one city in Japan, so results may not be generalizable to other localities. The questions regarding HPV education related to STIs. We did not specifically ask about HPV education related to the link between HPV and cervical cancer or the role of vaccination in preventing cervical cancer or pre-cancerous conditions requiring medical attention. In future studies, we intend to explore the differences between physicians' attitudes and intentions related to reliance on STIs versus cervical cancer when discussing HPVV. Lastly, our survey instrument was adapted from tools utilized in previously published studies evaluating attitudes related to adolescent vaccines but may not have measured all factors that influence recommendation behavior in this population.
5. Conclusions
Although Japanese physicians had positive perceptions about adolescent immunizations, they were less supportive of HPVV under the current policy environment in Japan. Our results suggest that Japanese physicians would benefit from governmental endorsement of HPVV, education about HPVV safety, and the availability of resources related to adolescent immunizations to support their communication with parents. Overall, these results suggest that the strongest of these relates to endorsement by the Japanese government. Therefore, advocacy to move the Japanese government to reinstate its proactive recommendation of HPVV for adolescents may be the most effective way to protect future generations of Japanese citizens from the consequences of infection with HPV.
Conflicts of interest
All authors declare no conflict of interests.
Authors’ contributions
Tomohiro Katsuta designed and implemented the study, analyzed and interpreted the data, and wrote the initial draft of the manuscript.
Kristen A. Feemster assisted with study design, data analysis and interpretation, and manuscript preparation. Charlotte A. Moser and Paul A. Offit assisted with study design, data interpretation, and manuscript preparation.
Funding
This work was supported by endowment funds from the Children's Hospital of Philadelphia. We have not received funds for the completion or publication of this study from any pharmaceutical company or other agency.
Declarations of interest
None.
References
- 1.Walker T.Y., Elam-Evans L.D., Yankey D., Markowitz L.E., Williams C.L., Mbaeyi S.A. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 Years - United States, 2017. MMWR Morb. Mortal. Wkly. Rep. 2018;67:909–917. doi: 10.15585/mmwr.mm6733a1. [DOI] [PMC free article] [PubMed] [Google Scholar]; T.Y. Walker, L.D. Elam-Evans, D. Yankey, L.E. Markowitz, C.L. Williams, S.A. Mbaeyi, et al National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13-17 Years - United States, 2017. MMWR Morb Mortal Wkly Rep. 67 (2018) 909-917. [DOI] [PMC free article] [PubMed]
- 2.Wigle J., Fontenot H.B., Zimet G.D. Global delivery of human papillomavirus vaccines. Pediatr. Clin. 2016;63:81–95. doi: 10.1016/j.pcl.2015.08.004. [DOI] [PubMed] [Google Scholar]; J. Wigle, H.B. Fontenot, G.D. Zimet. Global Delivery of Human Papillomavirus Vaccines. Pediatr Clin North Am. 63 (2016) 81-95. [DOI] [PubMed]
- 3.Brotherton J.M.L., Zuber P.L.F., Bloem P.J.N. Primary prevention of HPV through vaccination: update on the current global status. Curr Obstet Gynecol Rep. 2016;5:210–224. [Google Scholar]; J.M.L. Brotherton, P.L.F. Zuber, P.J.N. Bloem. Primary prevention of HPV through vaccination: Update on the current global status. Curr Obstet Gynecol Rep 5 (2016) 210-224.
- 4.Hanley S.J.B., Yoshioka E., Ito Y., Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385:2571. doi: 10.1016/S0140-6736(15)61152-7. [DOI] [PubMed] [Google Scholar]; S.J.B. Hanley, E. Yoshioka, Y. Ito, R. Kishi, HPV vaccination crisis in Japan, Lancet. 385 (2015) 2571. [DOI] [PubMed]
- 5.Saitoh A., Okabe N. Recent progress and concerns regarding the Japanese immunization program: addressing the "vaccine gap. Vaccine. 2014;32:4253–4258. doi: 10.1016/j.vaccine.2014.06.022. [DOI] [PubMed] [Google Scholar]; A. Saitoh, N. Okabe, Recent progress and concerns regarding the Japanese immunization program: Addressing the "vaccine gap", Vaccine. 32 (2014) 4253-4258. [DOI] [PubMed]
- 6.Saitoh A., Okabe N. Progress and challenges for the Japanese immunization program: beyond the "vaccine gap. Vaccine. 2018;36:4582–4588. doi: 10.1016/j.vaccine.2018.01.092. [DOI] [PubMed] [Google Scholar]; A. Saitoh, N. Okabe. Progress and challenges for the Japanese immunization program: Beyond the "vaccine gap". Vaccine. 36 (2018) 4582-4588. [DOI] [PubMed]
- 7.Hanley S.J.B., Yoshioka E., Ito Y., Konno R., Sasaki Y., Kishi R. An exploratory study of Japanese fathers' knowledge of and attitudes towards HPV and HPV vaccination: does marital status matter? Asian Pac. J. Cancer Prev. APJCP. 2014;15:1837–1843. doi: 10.7314/apjcp.2014.15.4.1837. [DOI] [PubMed] [Google Scholar]; S.J.B. Hanley, E. Yoshioka, Y. Ito, R. Konno, Y. Sasaki, R. Kishi, et al An Exploratory Study of Japanese Fathers' Knowledge of and Attitudes towards HPV and HPV Vaccination: Does Marital Status Matter? Asian Pac. J. Cancer Prev. 15 (2014) 1837-1843. [DOI] [PubMed]
- 8.Hanley S.J.B., Yoshioka E., Ito Y., Konno R., Hayashi Y., Kishi R. Acceptance of and attitudes towards human papillomavirus vaccination in Japanese mothers of adolescent girls. Vaccine. 2012;30:5740–5747. doi: 10.1016/j.vaccine.2012.07.003. [DOI] [PubMed] [Google Scholar]; S.J.B. Hanley, E. Yoshioka, Y. Ito, R. Konno, Y. Hayashi, R. Kishi, et al Acceptance of and attitudes towards human papillomavirus vaccination in Japanese mothers of adolescent girls. Vaccine. 30 (2012) 5740-5747. [DOI] [PubMed]
- 9.Gargano L.M., Herbert N.L., Painter J.E., Sales J.M., Morfaw C., Rask K. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum. Vaccines Immunother. 2013;9:2627–2633. doi: 10.4161/hv.25823. [DOI] [PMC free article] [PubMed] [Google Scholar]; L.M. Gargano, N.L. Herbert, J.E. Painter, J.M. Sales, C. Morfaw, K. Rask, et al, Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines, Hum Vaccin Immunother. 9 (2013) 2627-2633. [DOI] [PMC free article] [PubMed]
- 10.Szilagyi P.G., Rand C.M., McLaurin J., Tan L., Britto M., Francis A. Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 2008;121:S15–S24. doi: 10.1542/peds.2007-1115C. [DOI] [PubMed] [Google Scholar]; P.G. Szilagyi, C.M. Rand, J. McLaurin, L. Tan, M. Britto, A. Francis, et al, Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 121 (2008) S15-24. [DOI] [PubMed]
- 11.Darden P.M., Thompson D.M., Roberts J.R., Hale J.J., Pope C., Naifeh M. Reasons for not vaccinating adolescents: national immunization survey of teens, 2008-2010. Pediatrics. 2013;131:645–651. doi: 10.1542/peds.2012-2384. [DOI] [PubMed] [Google Scholar]; P.M. Darden, D.M. Thompson, J.R. Roberts, J.J. Hale, C. Pope, M. Naifeh, et al, Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008-2010, Pediatrics. 131 (2013) 645-651. [DOI] [PubMed]
- 12.The Children's Hospital of Philadelphia Vaccine Education Center. fifth ed. Vaccines and Teens; Philadelphia: 2017. [Google Scholar]; The Children's Hospital of Philadelphia Vaccine Education Center, Vaccines and Teens, 5th ed., Philadelphia, 2017.
- 13.Dorell C., Yankey D., Strasser S. Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, national immunization survey: teen. Clin. Pediatr. 2009;50:1116–1124. doi: 10.1177/0009922811415104. [DOI] [PubMed] [Google Scholar]; C. Dorell, D. Yankey, S. Strasser, Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, national immunization survey: teen, 2009, Clin pediatr. 50 (2011) 1116-1124. [DOI] [PubMed]
- 14.Darden P.M., Jacobson R.M. Impact of a physician recommendation. Hum. Vaccines Immunother. 2014;10:2632–2635. doi: 10.4161/hv.29020. [DOI] [PMC free article] [PubMed] [Google Scholar]; P.M. Darden, R.M. Jacobson, Impact of a physician recommendation, Hum Vaccin Immunother. 10 (2014) 2632-2635. [DOI] [PMC free article] [PubMed]
- 15.Opel D.J., Heritage J., Taylor J.A., Mangione-Smith R., Salas H.S., DeVere V. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132:1037–1046. doi: 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]; D.J. Opel, J. Heritage, J.A. Taylor, R. Mangione-Smith, H.S. Salas, V. DeVere, et al., The Architecture of Provider-Parent Vaccine Discussions at Health Supervision Visits, Pediatrics. 132 (2013) 1037-1046. [DOI] [PMC free article] [PubMed]
- 16.Edwards K.M., Hackell J.M. Countering vaccine hesitancy. Pediatrics. 2016;138 doi: 10.1542/peds.2016-2146. [DOI] [PubMed] [Google Scholar]; K.M. Edwards, J.M. Hackell, Countering Vaccine Hesitancy, Pediatrics. 138 (2016) e20162146. doi: 10.1542/peds.2016-2146. [DOI] [PubMed]
- 17.Kahn J.A., Ding L., Huang B., Zimet G.D., Rosenthal S.L., Frazier A.L. Mothers' intention for their daughters and themselves to receive the human papillomavirus vaccine: a national study of nurses. Pediatrics. 2009;123:1439–1445. doi: 10.1542/peds.2008-1536. [DOI] [PubMed] [Google Scholar]; J.A. Kahn, L. Ding, B. Huang, G.D. Zimet, S.L. Rosenthal, A.L. Frazier, Mothers' intention for their daughters and themselves to receive the human papillomavirus vaccine: a national study of nurses, Pediatrics. 123 (2009) 1439-1445. [DOI] [PubMed]
- 18.Caskey R., Lindau S.T., Alexander G.C. Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey. J. Adolesc. Health. 2009;45:453–462. doi: 10.1016/j.jadohealth.2009.04.021. [DOI] [PubMed] [Google Scholar]; R. Caskey, S.T. Lindau, G.C. Alexander, Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey, J Adolesc Health. 45 (2009) 453-462. [DOI] [PubMed]
- 19.Rosenthal S.L., Weiss T.W., Zimet G.D., Ma L., Good M.B., Vichnin M.D. Predictors of HPV vaccine uptake among women aged 19-26: importance of a physician's recommendation. Vaccine. 2011;29:890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]; S.L. Rosenthal, T.W. Weiss, G.D. Zimet, L. Ma, M.B. Good, M.D. Vichnin., Predictors of HPV vaccine uptake among women aged 19-26: importance of a physician's recommendation, Vaccine. 29 (2011) 890-895. [DOI] [PubMed]
- 20.Ylitalo K.R., Lee H., Mehta N.K. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am. J. Public Health. 2013;103:164–169. doi: 10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]; K.R. Ylitalo, H. Lee, N.K. Mehta, Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey, Am J Public Health. 103 (2013) 164-169. [DOI] [PMC free article] [PubMed]
- 21.Feemster K.A., Middleton M., Fiks A.G., Winters S., Kinsman S.B., Kahn J.A. Does intention to recommend HPV vaccines impact HPV vaccination rates? Hum. Vaccines Immunother. 2014;10:2519–2526. doi: 10.4161/21645515.2014.969613. [DOI] [PMC free article] [PubMed] [Google Scholar]; K.A. Feemster, M. Middleton, A.G. Fiks, S. Winters, S.B. Kinsman, J.A. Kahn, Does intention to recommend HPV vaccines impact HPV vaccination rates? Hum Vaccin Immunother. 10 (2014) 2519-2526. [DOI] [PMC free article] [PubMed]
- 22.Ministry of Health Labour and Welfare, Immunization rate in Japan, http://www.mhlw.go.jp/topics/bcg/other/5.html (Japanese) (accessed 6 July 2018).
- 23.Hanley S.J.B., Yoshioka E., Ito Y., Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385:2571. doi: 10.1016/S0140-6736(15)61152-7. [DOI] [PubMed] [Google Scholar]; S.J.B. Hanley, E. Yoshioka, Y. Ito, R. Kishi. HPV vaccination crisis in Japan. The Lancet. 385 (2015) 2571. [DOI] [PubMed]
- 24.Tsuda K., Yamamoto K., Leppold C., Tanimoto T., Kusumi E., Komatsu T. Trends of media coverage on human papillomavirus vaccination in Japanese newspapers. Clin. Infect. Dis. 2016;63:1634–1638. doi: 10.1093/cid/ciw647. [DOI] [PubMed] [Google Scholar]; K. Tsuda, K. Yamamoto, C. Leppold, T. Tanimoto, E. Kusumi, T. Komatsu, et al., Trends of media coverage on human papillomavirus vaccination in Japanese newspapers, Clin Infect Dis. 63 (2016) 1634-1638. [DOI] [PubMed]
- 25.Suppli C.H., Hansen N.D., Rasmussen M., Valentiner-Branth P., Krause T.G., Mølbak K. Decline in HPV-vaccination uptake in Denmark – the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 2018;18:1360. doi: 10.1186/s12889-018-6268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]; C.H. Suppli, N.D. Hansen, M. Rasmussen, P. Valentiner-Branth, T.G. Krause, K. Molbak. Decline in HPV-vaccination uptake in Denmark - the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 18 (2018) 1360. doi: 10.1186/s12889-018-6268-x. [DOI] [PMC free article] [PubMed]
- 26.Corcoran B., Clarke A., Barrett T. Rapid response to HPV vaccination crisis in Ireland. Lancet. 2018;391:2103. doi: 10.1016/S0140-6736(18)30854-7. [DOI] [PubMed] [Google Scholar]; B. Corcoran, A. Clarke, T. Barrett. Rapid response to HPV vaccination crisis in Ireland. The Lancet. 391 (2018) 2103. [DOI] [PubMed]
- 27.National institute of Infectious Deseases Influenza vaccination coverage in the 2014/15 influenza season and seroprevalence of influenza prior to the 2015/16 influenza season, Japan-FY 2015 National Epidemiological Surveillance of Vaccine-Preventable Diseases. Infect. Agents Surveill. Rep. 2016;37:223–225. [Google Scholar]; National institute of Infectious Deseases, Influenza vaccination coverage in the 2014/15 influenza season and seroprevalence of influenza prior to the 2015/16 influenza season, Japan-FY 2015 National Epidemiological Surveillance of Vaccine-Preventable Diseases, Infectious Agents Surveillance Report. 37 (2016) 223-225.
- 28.Kawasaki City Immunization rate in Kawasaki City. http://www.city.kawasaki.jp/350/page/0000092026.html (Japanese) (accessed 10 October 2018); Kawasaki City, Immunization rate in Kawasaki City, HYPERLINK "http://www.city.kawasaki.jp/350/page/0000092026.html%20" \o "http://www.city.kawasaki.jp/350/page/0000092026.html"http://www.city.kawasaki.jp/350/page/0000092026.html (Japanese) (accessed 10 October 2018).
- 29.Hofstetter A.M., Rosenthal S.L. Factors impacting HPV vaccination: lessons for health care professionals. Expert Rev. Vaccines. 2014;13:1013–1026. doi: 10.1586/14760584.2014.933076. [DOI] [PubMed] [Google Scholar]; A.M. Hofstetter, S.L. Rosenthal. Factors impacting HPV vaccination: lessons for health care professionals. Expert Rev Vaccines. 13 (2014) 1013-1026. [DOI] [PubMed]
- 30.Ryan T.A. Significance tests for multiple comparison of proportions, variances, and other statistics. Psychol. Bull. 1960;57:318–328. doi: 10.1037/h0044320. [DOI] [PubMed] [Google Scholar]; T.A. Ryan. Significance tests for multiple comparison of proportions, variances, and other statistics, Psychol bull. 57 (1960) 318-328. [DOI] [PubMed]
- 31.Ministry of health, Labour and Welfare, demographics of Japanese physicians in, 2016. https://www.mhlw.go.jp/toukei/saikin/hw/ishi/16/index.html (Japanese) (accessed 5 March 2019); Ministry of Health, Labour and Welfare, Demographics of Japanese physicians in, 2016, https://www.mhlw.go.jp/toukei/saikin/hw/ishi/16/index.html, (Japanese) (accessed 5 March 2019).
- 32.Gilkey M.B., Dayton A.M., Moss J.L., Sparks A.C., Grimshaw A.H., Bowling J.M. Increasing provision of adolescent vaccines in primary care: a randomized controlled trial. Pediatrics. 2014;134:e346–353. doi: 10.1542/peds.2013-4257. [DOI] [PMC free article] [PubMed] [Google Scholar]; M.B. Gilkey, A.M. Dayton, J.L. Moss, A.C. Sparks, A.H. Grimshaw, J.M. Bowling, et al, Increasing provision of adolescent vaccines in primary care: a randomized controlled trial, Pediatrics. 134 (2014) e346-353. [DOI] [PMC free article] [PubMed]
- 33.Perkins R.B., Zisblatt L., Legler A., Trucks E., Hanchate A., Gorin S.S. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine. 2015;33:1223–1229. doi: 10.1016/j.vaccine.2014.11.021. [DOI] [PubMed] [Google Scholar]; R.B. Perkins, L. Zisblatt, A. Legler, E. Trucks, A. Hanchate, S.S. Gorin, Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls, Vaccine. 33 (2015) 1223-1229. [DOI] [PubMed]
- 34.Walling E.B., Benzoni N., Dornfeld J., Bhandari R., Sisk B.A., Garbutt J. Interventions to improve HPV vaccine uptake: a systematic review. Pediatrics. 2016;138 doi: 10.1542/peds.2015-3863. [DOI] [PubMed] [Google Scholar]; E.B. Walling, N. Benzoni, J. Dornfeld, R. Bhandari, B.A. Sisk, J. Garbutt, et al., Interventions to Improve HPV Vaccine Uptake: A Systematic Review, Pediatrics. 138 (2016) e20153863. doi: 10.1542/peds.2015-3863. [DOI] [PubMed]
- 35.Fiks A.G., Grundmeier R.W., Mayne S., Song L., Feemster K., Karavite D. Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt. Pediatrics. 2013;131:1114–1124. doi: 10.1542/peds.2012-3122. [DOI] [PMC free article] [PubMed] [Google Scholar]; A.G. Fiks, R.W. Grundmeier, S. Mayne, L. Song, K. Feemster, D. Karavite, et al., Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt, Pediatrics. 131 (2013) 1114-1124. [DOI] [PMC free article] [PubMed]
- 36.Alexander A.B., Best C., Stupiansky N., Zimet G.D. A model of health care provider decision making about HPV vaccination in adolescent males. Vaccine. 2015;33:4081–4086. doi: 10.1016/j.vaccine.2015.06.085. [DOI] [PubMed] [Google Scholar]; A.B. Alexander, C. Best, N. Stupiansky, G.D. Zimet, A model of health care provider decision making about HPV vaccination in adolescent males, Vaccine. 33 (2015) 4081-4086. [DOI] [PubMed]
- 37.Cosgrove H.J. Larson. Japanese media and the HPV vaccine saga. Clin. Infect. Dis. 2017;64:533–534. doi: 10.1093/cid/ciw796. [DOI] [PubMed] [Google Scholar]; H.J. Larson. Cosgrove, Japanese Media and the HPV Vaccine Saga, Clin Infect Dis. 64 (2017) 533-534. [DOI] [PubMed]
- 38.Sakai R., Fink G., Wang W., Kawachi I. Correlation between pediatrician supply and public health in Japan as evidenced by vaccination coverage in 2010: secondary data analysis. J. Epidemiol. 2015;25:359–369. doi: 10.2188/jea.JE20140121. [DOI] [PMC free article] [PubMed] [Google Scholar]; R. Sakai, G. Fink, W. Wang, I. Kawachi, Correlation between pediatrician supply and public health in Japan as evidenced by vaccination coverage in 2010: secondary data analysis, J Epidemiol. 25 (2015) 359-369. [DOI] [PMC free article] [PubMed]
- 39.Alexander S.C., Fortenberry J.D., Pollak K.I., Bravender T., Davis J.K., Ostbye T. Sexuality talk during adolescent health maintenance visits. JAMA pediatr. 2014;168:163–169. doi: 10.1001/jamapediatrics.2013.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]; S.C. Alexander, J.D. Fortenberry, K.I. Pollak, T. Bravender, J.K. Davis, T. Ostbye, et al, Sexuality talk during adolescent health maintenance visits, JAMA pediatr. 168 (2014) 163-169. [DOI] [PMC free article] [PubMed]
- 40.Gilkey M.B., Zhou M., McRee A.L., Kornides M.L., Bridges J.F.P. Parents' views on the best and worst reasons for guideline-consistent HPV vaccination. Cancer Epidemiol. Biomark. Prev. 2018;27:762–767. doi: 10.1158/1055-9965.EPI-17-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]; M.B. Gilkey, M. Zhou, A.L. McRee, M.L. Kornides, J.F.P. Bridges. Parents' Views on the Best and Worst Reasons for Guideline-Consistent HPV Vaccination. Cancer Epidemiol, Biomarkers Prev. 27 (2018) 762-767. [DOI] [PMC free article] [PubMed]
- 41.Centers for Disease Control and Prevention Talking to parents about HPV vaccine. 2016. https://www.cdc.gov/hpv/hcp/for-hcp-tipsheet-hpv.html accessed 23 March 23 2019.; Centers for Disease Control and Prevention, Talking to parents about HPV vaccine. 2016, https://www.cdc.gov/hpv/hcp/for-hcp-tipsheet-hpv.html, (accessed 23 March 23 2019).
- 42.Mazzoni S.E., Brewer S.E., Pyrzanowski J.L., Durfee M.J., Dickinson L.M., Barnard J.G. Effect of a multi-modal intervention on immunization rates in obstetrics and gynecology clinics. Am. J. Obstet. Gynecol. 2016;214:617 e1–7. doi: 10.1016/j.ajog.2015.11.018. [DOI] [PubMed] [Google Scholar]; S.E. Mazzoni, S.E. Brewer, J.L. Pyrzanowski, M.J. Durfee, L.M. Dickinson, J.G. Barnard, et al., Effect of a multi-modal intervention on immunization rates in obstetrics and gynecology clinics, Am J Obstet Gynecol. 214 (2016) 617 e1-7. [DOI] [PubMed]
- 43.Sawada M., Ueda Y., Yagi A., Morimoto A., Nakae R., Kakubari R. HPV vaccination in Japan: results of a 3-year follow-up survey of obstetricians and gynecologists regarding their opinions toward the vaccine. Int. J. Clin. Oncol. 2018;23:121–125. doi: 10.1007/s10147-017-1188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]; M. Sawada, Y. Ueda, A. Yagi, A. Morimoto, R. Nakae, R. Kakubari, et al, HPV vaccination in Japan: results of a 3-year follow-up survey of obstetricians and gynecologists regarding their opinions toward the vaccine, Int J. clin. oncol. 23 (2018) 121-125. doi: 10.1007/s10147-017-1188-9. [DOI] [PMC free article] [PubMed]
- 44.Egawa-Takata T., Ueda Y., Morimoto A., Tanaka Y., Matsuzaki S., Kobayashi E. Human papillomavirus vaccination of the daughters of obstetricians and gynecologists in Japan. Int. J. Clin. Oncol. 2016;21:53–58. doi: 10.1007/s10147-015-0869-5. [DOI] [PubMed] [Google Scholar]; T. Egawa-Takata, Y. Ueda, A. Morimoto, Y. Tanaka, S. Matsuzaki, E. Kobayashi, et al Human papillomavirus vaccination of the daughters of obstetricians and gynecologists in Japan. Int J Clin Oncol. 21(2016) 53-58. [DOI] [PubMed]