Abstract
The typical imaging findings in hepatocellular carcinoma (HCC) are arterial hyperenhancement with washout on portal venous and/or equilibrium phases. Larger HCCs can have atypical imaging findings including fibrous capsule or mosaic appearance. We describe an unusual biopsy proven HCC in a cirrhotic liver with imaging features mimicking cavernous hemangioma which also demonstrated some atypical features such as thick capsule. In addition to knowing the typical imaging findings of HCC, it is important to be familiar with its atypical imaging findings especially in larger lesions.
Keywords: Hepatocellular carcinoma, Cavernous hemangioma, MRI, Atypical
Introduction
Hepatocellular carcinoma (HCC) is the most common primary hepatic malignancy [1], arising in the background of cirrhosis and chronic liver disease.
The diagnostic imaging criteria for HCC are well defined by current imaging algorithms (AASLD, OPTN, and LI-RADS) and rely primarily on the characteristic appearance of HCC on dynamic multiphasic contrast-enhanced computed tomography (CT) or magnetic resonance images [2], [3], [4], [5]. The imaging diagnostic criteria for HCC include early enhancement in the arterial phase and contrast medium washout in the portal venous or equilibrium phase [6]. Equilibrium phase CT and magnetic resonance imaging (MRI) could also show a thin rim-enhancing capsule appearance [6].
Atypical findings on imaging have been described in multiple studies [7], [8], [9] and include hemorrhage, calcification, central scar or gross fat. Also there are variant subtypes of HCC which demonstrate atypical imaging characteristics on dynamic CT or MRI [1]. Larger HCCs (more than 3 cm) may have certain imaging features that are not frequently seen in smaller HCCs [10].
In this case report we describe an unusual appearance of a well-differentiated HCC, which mimicked a cavernous hemangioma on imaging.
Case presentation
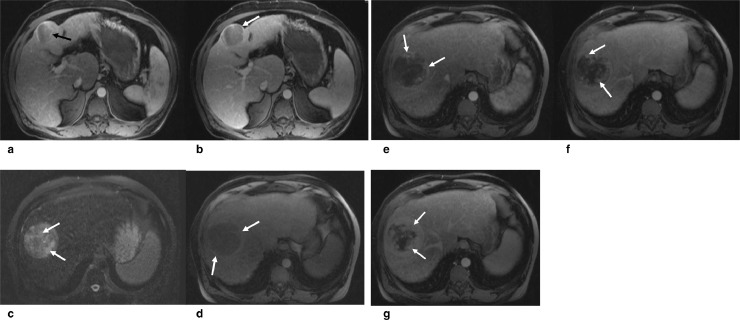
A 58-year-old man with no significant past medical history underwent CT of the abdomen for abdominal pain which showed hepatic cirrhosis and 2 lesions in segments 4B and 7/8 (Fig. 1a, 1b). The lesion in segment 7/8 was initially diagnosed as a cavernous hemangioma due to the enhancement pattern, while the lesion in segment 4B was concerning for HCC. These lesions were further evaluated with dynamic MRI. On MRI, the 5.8 cm partially exophytic mass in the segment 4B of the liver demonstrated mild hyperenhancement on arterial phase with subsequent washout and rim enhancing capsule appearance on equilibrium images, consistent with an Organ Procurement and Transplantation Network class 5 HCC (Fig. 2a, 2b). The 8 cm lesion in segment 7/8 showed heterogeneous and moderately T2 hyperintense signal and suggestion of hemorrhage manifested by a mildly hyperintense rim on precontrast T1-weighted images (Fig. 2c, 2d). In addition, there was a distinct hypointense rim surrounding the mass, which demonstrated delayed enhancement and capsule appearance. On postcontrast images a nodular discontinuous peripheral enhancement was seen in the arterial phase with subsequent progressive inward enhancement in the equilibrium and delayed images (Fig. 2e, 2f, and 2g). The enhancement pattern again raised the possibility of cavernous hemangioma, however, due to some ancillary imaging features such as mosaic architecture, mildly T1 hyperintense rim and delayed enhancing capsule appearance (Fig. 2g), the possibility of HCC was raised and biopsy was recommended which confirmed the presence of a well-differentiated HCC.
Fig. 1.
(a and b) 58-year-old man with no significant past medical history, underwent contrast enhanced CT of the abdomen for evaluation of abdominal pain. CT showed hepatic cirrhosis and two lesions in segments 4B (a) and 7/8 (b). The lesion in segment 7/8 shows nodular peripheral areas of hyperenhancement (arrows in b) and therefore a diagnosis of cavernous hemangioma was suggested for this lesion.
Fig. 2.
(a and b) Dynamic contrast enhanced MRI of the same patient shows a 5.8 cm partially exophytic mass in the segment 4B with mild hyperenhancement on arterial phase (a, arrow), and subsequent washout and rim enhancing capsule (arrow in b) on equilibrium phase, consistent with an OPTN class 5 HCC. (c, d, e, f, g) Dynamic contrast-enhanced MRI of the second lesion in segment 7/8 shows mildly increased but heterogeneous T2 signal intensity (c, arrows) and mildly hyperintense rim on precontrast T1-weighted image (d, arrows). Postcontrast images show a nodular discontinuous peripheral enhancement in the arterial phase (e, arrow) with subsequent progressive inward enhancement in the equilibrium and delayed images (f and g, arrows). Delayed enhancing capsule can be clearly seen in figure g.
Discussion
In this article we describe a case of HCC that showed enhancement characteristics of a cavernous hemangioma, which may have led to a missed diagnosis of cancer. Typically, cavernous hemangiomas show peripheral nodular discontinuous enhancement which progresses centripetally (inward) on delayed images [11]. They also appear hyperintense relative to liver parenchyma, but less than the intensity of cerebrovascular fluid or of a hepatic cyst on T2-weighted image and are hypointesnse relative to liver tissue on noncontrast T1-weighted image [12]. Like a cavernous hemangioma, the described atypical HCC in our case showed nodular discontinuous peripheral enhancement in the arterial phase with subsequent progressive inward enhancement in the equilibrium and delayed images. Without the ability to assess ancillary features on MRI, this lesion was inaccurately classified as a hemangioma on initial CT. However on T2-weighted MR images, the lesion demonstrated very heterogeneous signal, which was not as bright as expected. The presence of mildly T1 hyperintense rim and delayed enhancing capsule were other features that were suggestive of an etiology other than cavernous hemangioma in our case.
As imaging modalities continue to improve, fewer biopsies are required for making diagnosis of both benign and malignant lesions. HCC in particular has very well-defined imaging features and a clear imaging algorithm for making a noninvasive diagnosis. The features are so well recognized in fact that the imaging appearance is sufficient for directing treatment and transplant allocation. As discussed above, the major features of HCC include arterial phase hyperenhancement, washout appearance, and capsule appearance [6], [13]. In our case, a diagnosis based upon the enhancement features alone would have led to a misdiagnosis.
Multiple prior studies [7], [8], [9] have described atypical imaging findings of HCCs and include hemorrhage, calcification, central scar or gross fat. Also certain characteristic features have been reported in larger HCCs (larger than 3 cm) more frequently than the smaller ones. These features include: fibrous capsule that appears hypointense on T1W and T2W images with enhancement during the portal venous or delayed phases [14], [15], mosaic appearance due to areas of necrosis and hemorrhage, extra capsular extension into adjacent parenchyma and vessels, satellite nodules and lymph nodal, and distant metastases [10]. When typical features are absent or atypical features are present, biopsy may be warranted to exclude a different malignancy [5].
In assessing lesions in cirrhotic and at-risk patients, use of algorithms such as LI-RADS version 2014 [4] is helpful in coming to a final diagnosis and management plan. The lesion in our case demonstrated several ancillary features that were potentially worrisome for malignancy, including mosaic architecture, capsule appearance, and internal blood products. The summation of these ancillary features and the presence of background liver disease prompted the radiologist to suggest biopsy to confirm diagnosis.
Additionally, it should be noted that cavernous hemangioma in cirrhotic liver is very uncommon [16] and with progressive cirrhosis, they decrease in size and become more fibrotic, and are more difficult to recognize radiologically and pathologically [16], [17]. Rarity of cavernous hemangioma in cirrhotic livers was another reason that raised the concern for an atypical HCC rather than a cavernous hemangioma in our patient.
In conclusion, although it is important to know the classic CT and MR appearance of HCC, it is also important to know that many HCCs do not have the classic imaging characteristics especially when they are larger than 3 cm. It is probably a reasonable approach to regard any hypervascular, noncystic focal hepatic lesion in a cirrhotic liver as being suggestive of HCC.
References
- 1.Chung Y.E., Park M.S., Park Y.N., Lee H.J., Seok J.Y., Yu J.S. Hepatocellular carcinoma variants: radiologic-pathologic correlation. AJR Am J Roentgenol. 2009;193:7–13. doi: 10.2214/AJR.07.3947. [DOI] [PubMed] [Google Scholar]
- 2.Bruix J., Sherman M., American Association for the Study of Liver Diseases Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fowler K.J., Karimova E.J., Arauz A.R., Saad N.E., Brunt E.M., Chapman W.C. Validation of organ procurement and transplant network (OPTN)/united network for organ sharing (UNOS) criteria for imaging diagnosis of hepatocellular carcinoma. Transplantation. 2013;95:1506–1511. doi: 10.1097/TP.0b013e31828eeab2. [DOI] [PubMed] [Google Scholar]
- 4.American College of Radiology (ACR). Liver Imaging Reporting and Data System (LI-RADS) [accessed 24.08.14]. 2013. Available from http://www.acr.org/Quality-Safety/Resources/LIRADS
- 5.Willatt J.M., Hussain H.K., Adusumilli S., Marrero J.A. MR imaging of hepatocellular carcinoma in the cirrhotic liver: challenges and controversies. Radiology. 2008;247:311–330. doi: 10.1148/radiol.2472061331. [DOI] [PubMed] [Google Scholar]
- 6.Wald C., Russo M.W., Heimbach J.K., Hussain H.K., Pomfret E.A., Bruix J. New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology. 2013;266:376–382. doi: 10.1148/radiol.12121698. [DOI] [PubMed] [Google Scholar]
- 7.Grazioli L., Olivetti L., Fugazzola C. The pseudocapsule in hepatocellular carcinoma: correlation between dynamic MR imaging and pathology. Eur Radiol. 1999;9:62–67. doi: 10.1007/s003300050629. [DOI] [PubMed] [Google Scholar]
- 8.Szklaruk J., Silverman P.M., Charnsangavej C. Imaging in the diagnosis, staging, treatment, and surveillance of hepatocellular carcinoma. AJR. 2003;180:441–454. doi: 10.2214/ajr.180.2.1800441. [DOI] [PubMed] [Google Scholar]
- 9.Brancatelli G., Federle M.P., Grazioli L., Carr B.I. Hepatocellular carcinoma in noncirrhotic liver: CT, clinical, and pathologic findings in 39 U.S. residents. Radiology. 2002;222:89–94. doi: 10.1148/radiol.2221010767. [DOI] [PubMed] [Google Scholar]
- 10.Digumarthy S.R., Sahani D.V., Saini S. MRI in detection of hepatocellular carcinoma. Cancer Imaging. 2005;5:20–24. doi: 10.1102/1470-7330.2005.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ros P.R., Lubbers P.R., Olmsted W.W. Hemangioma of the liver: heterogeneous appearance on T2-weighted images. AJR Am J Roentgenol. 1987;149:1167–1170. doi: 10.2214/ajr.149.6.1167. [DOI] [PubMed] [Google Scholar]
- 12.Klotz T., Montoriol P.F., Da Ines D. Hepatic haemangioma: common and uncommon imaging features. Diagn Interv Imaging. 2013;94:849–859. doi: 10.1016/j.diii.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Bruix J., Sherman M., Practice Guidelines Committee, American Association for the Study of Liver Diseases Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 14.Kadoya M., Matsui O., Takashima T. Hepatocellular carcinoma: correlation of MR imaging and histopathologic findings. Radiology. 1992;183:819–825. doi: 10.1148/radiology.183.3.1316622. [DOI] [PubMed] [Google Scholar]
- 15.Grazioli L., Olivetti L., Fugazzola C. The pseudocapsule in hepatocellular carcinoma: correlation between dynamic MR imaging and pathology. Eur Radiol. 1999;9:62–67. doi: 10.1007/s003300050629. [DOI] [PubMed] [Google Scholar]
- 16.Brancatelli G., Federle M.P., Blachar A., Grazioli L. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology. 2001;219:69–74. doi: 10.1148/radiology.219.1.r01ap3269. [DOI] [PubMed] [Google Scholar]
- 17.Tung G.A., Vaccaro J.P., Cronan J.J., Rogg J.M. Cavernous hemangioma of the liver: pathologic correlation with high-field MR imaging. AJR Am J Roentgenol. 1994;162:1113–1117. doi: 10.2214/ajr.162.5.8165993. [DOI] [PubMed] [Google Scholar]