Abstract
Objective
Psychosocial factors likely contribute to racial and ethnic inequalities in cardiovascular diseases (CVDs). However, precise social, psychological, and physiological pathways linking race and ethnicity to the development of CVDs are not well understood. Systemic inflammation, commonly indexed by C-reactive protein (CRP), is a biomarker for CVD risk and progression. The objective of this study was to identify mediating pathways from race and ethnicity to CRP through social, psychological, and behavioral variables.
Methods
Using data from 12,382 participants aged 51 and older in the Health and Retirement Study, structural equation models tested for direct and indirect effects of race and ethnicity on CRP measured over four years through educational disadvantage, everyday discrimination, depressive symptoms, external locus of control, and smoking.
Results
Educational disadvantage mediated Black-White and Hispanic-White disparities in baseline CRP directly, as well as indirectly through elevated depressive symptoms, higher external locus of control, and smoking. Educational disadvantage also mediated Black-White and Hispanic-White disparities in CRP change directly, as well as indirectly through higher external locus of control and smoking. Independent of education, discrimination mediated Black-White differences in baseline CRP via elevated depressive symptoms, higher external locus of control, and smoking. Discrimination also mediated Black-White disparities in CRP change via external locus of control.
Conclusions
Results from this population-based, longitudinal study support the view that racially patterned social disadvantage is prospectively associated with longitudinal inflammatory processes, and some of these effects are independently mediated by psychological and behavioral factors. Biopsychosocial pathways to health disparities also differ between minority groups.
Keywords: United States, Inflammation, Minority health, Discrimination, Education, Depression
Highlights
-
•
C-reactive protein (CRP) increased over 4 years among 12,382 adults aged 51 and older.
-
•
Blacks and Hispanics had higher initial CRP than Whites, but only Blacks showed greater CRP increase than Whites.
-
•
Lower education, less perceived control, and smoking contributed to each disparity in some way.
-
•
Depressive symptoms were only a mediator of cross-sectional disparities.
-
•
Discrimination was only a mediator of Black-White disparities.
1. Introduction
Racial and ethnic inequalities have been documented for a wide array of health outcomes, including cardiovascular disease (CVD), which represents a leading cause of death among adults in the U.S. (Kochanek, Murphy, & Xu, 2015). However, pathways linking race and ethnicity to the development of CVD are poorly understood. To date, most studies have focused on individual components of what is likely a much larger set of interrelated biopsychosocial processes. An improved understanding of pathways linking the experiences of racial and ethnic minority groups to increased risk could reveal opportunities for interventions to reduce CVD morbidity and combat racial and ethnic health inequalities. The current study examines mediators of racial and ethnic inequalities in systemic inflammation, which is an important indicator of CVD risk and progression (Ridker, Rifai, Rose, Buring, & Cook, 2002) that is disproportionately experienced by Black and Hispanic adults, compared with non-Hispanic Whites (Albert, 2007; Crimmins, Kim, Alley, Karlamangla, & Seeman, 2007; Mitchell & Aneshensel, 2016).
As a social construct, self-identified race and ethnicity is a proxy for exposure to racism, the organized system that phenotypically categorizes population groups and preferentially allocates societal resources to groups regarded as superior (Bonilla-Silva, 1997). Substantial research on health inequalities across racial and ethnic groups has focused on interpersonal discrimination as one pathway by which racism can affect health, but interpersonal discrimination is only one aspect of racism that can affect health (Williams & Mohammed, 2009). Institutional discrimination is another aspect of racism that may contribute to health disparities via racially patterned socioeconomic disadvantage. Socioeconomic status can be operationalized as educational attainment, income and/or occupation, but educational attainment is the main gateway to later occupational and economic status (Pearlin, Schieman, Fazio, & Meersman, 2005). In addition, educational attainment is least likely to be affected by health events after young adulthood (Crimmins, Hayward, & Seeman, 2004) and shows the strongest and most consistent independent relationships with CVD risk and health (Winkleby, Jatulis, Frank & Fortmann, 1992). Thus, the current study examined both interpersonal discrimination and educational attainment as social factors relevant to racial and ethnic inequalities in health.
The biopsychosocial approach to understanding racial and ethnic inequalities in health builds on a more general stress-coping model (Lazarus & Folkman, 1984) and posits that conceptualizing racially patterned social experiences as “stressful” may help to explain group differences in health outcomes (Clark, Anderson, Clark, & Williams, 1999). Indeed, interpersonal discrimination and low educational attainment both represent stressors with the potential to trigger psychological and physiological stress responses. Socioeconomic stressors are among the most impactful of stressful life experiences (Pearlin et al., 2005), and the experience of discrimination may be particularly harmful due to its unpredictability and uncontrollability (Williams & Mohammed, 2009).
Randomized controlled experiments directly testing whether interpersonal discrimination or low socioeconomic status causes negative psychological sequelae are not readily available. However, longitudinal studies indicate that discrimination predicts subsequent depressive symptoms, independent of baseline depressive symptoms, and not vice versa (Brown et al., 2000; Pavalko, Mossakowski, & Hamilton, 2003). Studies using instrumental variable analyses or natural experiments support the view that low educational attainment causes depressive symptoms (Chevalier & Feinstein, 2007; McFarland & Wagner, 2015; Mezuk, Myers, & Kendler, 2013). In addition to depressive symptoms, observational data indicate that individuals with lower educational attainment report less perceived control (Bailis, Segall, Mahon, Chipperfield, & Dunn, 2001; Bruce & Thornton, 2004; Pearlin, Nguyen, Schieman, & Milkie, 2007; Pudrovska, Schieman, Pearlin, & Nguyen, 2005; Schieman, 2001), slower increases in perceived control during young adulthood, and faster declines in perceived control in older adulthood (S. K. Lewis, Ross, & Mirowsky, 1999; Mirowsky & Ross, 2007; Schieman, 2001). Qualitative studies also consistently identify a perceived lack of control as a common response to discriminatory situations (Broman, Mavaddat, & Hsu, 2000; Bullock & Houston, 1987). Together, these studies support the hypothesis that interpersonal discrimination and lower educational attainment can be conceptualized as “stressful” and are linked to negative psychological sequelae, including depressive symptoms and low perceived control.
Stress-related activation of the sympathetic nervous system (i.e., norepinephrine release), as well as chronic activation of the hypothalamic-pituitary-adrenal axis (i.e., glucocorticoid resistance), both up-regulate inflammatory processes that can have broad effects on cardiovascular health (Slavich & Irwin, 2014). A common marker of systemic inflammation is the level of circulating C-reactive protein (CRP), which is an acute-phase protein synthesized by the liver and secreted in response to inflammation. Growing evidence indicates that psychosocial factors are associated with inflammatory response, as indexed by CRP. For example, educational disadvantage has been linked to higher CRP levels in epidemiological studies (Ranjit et al., 2007). In addition, a recent prospective study of approximately 2500 women found that greater discrimination predicted higher CRP levels over seven years (Beatty Moody, Brown, Matthews, & Bromberger, 2014), extending previous cross-sectional findings (Friedman, Williams, Singer, & Ryff, 2009; T. T.; Lewis, Aiello, Leurgans, Kelly, & Barnes, 2010). Finally, both depressive symptoms (Howren, Lamkin, & Suls, 2009; Kop et al., 2002) and low perceived control (Elliot, Mooney, Infurna, & Chapman, 2017) have been associated with higher CRP.
A related mechanism by which racially patterned social stress (e.g., discrimination, socioeconomic disadvantage) could contribute to disparities in cardiovascular disease risk is described by the Environmental Affordances Model (Mezuk, Abdou et al., 2013). This model proposes that certain negative health behaviors can serve as self-regulatory coping strategies that help to preserve mental health in the short term but can have deleterious effects on physical health in the long term (Jackson & Knight, 2006; Jackson, Knight, & Rafferty, 2010). Smoking is one such negative health behavior with a well-documented history of negative impacts on cardiovascular health. Furthermore, despite many years of smoking cessation interventions, non-Hispanic Blacks and Hispanics are less likely to receive and use these interventions than Whites, even after controlling for socioeconomic status and healthcare utilization (Cokkinides, Halpern, Barbeau, Ward, & Thun, 2008). Thus, the Environmental Affordances Model predicts that health behaviors may also mediate links between social variables and health, as well as contribute to smaller indirect effects involving psychological variables.
The current study sought to examine psychosocial mediators of racial and ethnic health inequalities using longitudinal data from a large, nationally representative sample of Black, Hispanic, and White adults participating in the Health and Retirement Study (HRS). A mediation model simultaneously examined multiple pathways from race and ethnicity to CRP over four years through social (i.e., interpersonal discrimination, educational attainment), behavioral (i.e., smoking), and psychological (i.e., depressive symptoms, external locus of control) factors.
2. Method
2.1. Participants
Data were obtained from the Health and Retirement Study (HRS), a nationally representative sample of Americans over age 50 followed since 1992 (Sonnega & Weir, 2014). Details of the HRS longitudinal panel design, sampling, and all assessment instruments are available on the HRS website (http://hrsonline.isr.umich.edu). Participants in HRS are interviewed every two years. In 2006, the HRS initiated an enhanced face-to-face interview, which included collecting biomarker data and giving participants a psychosocial questionnaire, which they were asked to return via mail. A random one half of the sample was selected to participate in these procedures in 2006, and the other half was selected to participate in 2008. These individuals then participated in a follow-up face-to-face interview four years later (i.e., 2010 for participants originally interviewed in 2006, 2012 for participants originally interviews in 2008). In the current study, data obtained in 2006 and 2008 were combined to form a baseline wave, and data obtained in 2010 and 2012 were combined to form a follow-up wave. Biomarker response rates were 83.0% in 2006, 87.0% in 2008, 85% in 2010, and 87.0% in 2012 (http://hrsonline.isr.umich.edu).
Of participants aged 51 or older, the current study included only participants who self-identified as non-Hispanic Black, Hispanic (of any race), or non-Hispanic White. Two participants were excluded for non-availability of data on race and ethnicity, and 282 participants were excluded for non-membership in one of these three groups. Characteristics of the 12,382 individuals included in the current study are provided in Table 1. Data on education were available for 12,364 participants, data on discrimination were available for 11,197 participants, data on depressive symptoms were available on 12,380 participants, data on external locus of control were available on 11,199 participants, and data on smoking were available for 12,293 participants. Biomarker data were available for 11,747 participants at baseline (2006 or 2008) and 8307 participants at follow-up (2010 or 2012). All participants provided written informed consent, and all study procedures were approved by the University of Michigan institutional review board.
Table 1.
Sample characteristics at baseline displayed as mean (standard deviation) unless otherwise indicated.
| Whole sample (N = 12,382) | Non-Hispanic Black (N = 1626) | Hispanic (N = 1117) | Non-Hispanic White (N = 9639) | Group differences | |
|---|---|---|---|---|---|
| Baseline wave (% 2006) | 51.3 | 50.2 | 46.9 | 52.0 | B=W < H |
| Age (51–101 years) | 68.8 (9.9) | 67.6 (9.6) | 66.2 (9.4) | 69.4 (9.9) | H < B < W |
| Gender (% women) | 58.9 | 64.1 | 61.0 | 57.8 | W < H=B |
| Smoking (% yes) | 13.0 | 17.4 | 12.5 | 12.4 | H=W < B |
| C-reactive protein (NHANES-equivalent) | W < H < B | ||||
| % Low (<1 μg/mL) | 28.9 | 25.3 | 23.3 | 30.1 | |
| % Moderate (1–3 μg/mL) | 33.9 | 26.7 | 36.9 | 34.7 | |
| % High (>3 μg/mL) | 37.3 | 48.0 | 39.8 | 35.1 | |
| Education (0–17 years) | 12.5 (3.2) | 11.6 (3.2) | 8.9 (4.5) | 13.1 (2.6) | H < B < W |
| Discrimination (1–6) | 1.6 (0.7) | 1.8 (0.9) | 1.6 (0.8) | 1.6 (0.7) | W=H < B |
| Depressive symptoms (0–10) | 1.4 (2.0) | 1.8 (2.1) | 2.1 (2.4) | 1.3 (1.8) | W < B < H |
| External locus of control (1–6) | 2.2 (1.2) | 2.3 (1.2) | 2.6 (1.3) | 2.2 (1.2) | W < B < H |
Note. NHANES = National Health and Nutrition Examination Survey; B = Non-Hispanic Black; H = Hispanic; W = Non-Hispanic White.
2.2. Measures
2.2.1. Race and ethnicity
Race was assessed with the question “What race do you consider yourself to be: White, Black or African American, American Indian, Alaska Native, Asian, Native Hawaiian, Pacific Islander, or something else?” Ethnicity was assessed with the question, “Do you consider yourself Hispanic or Latino?” The current study included three, mutually exclusive categories: non-Hispanic Black, non-Hispanic White, and Hispanic (of any race). The largest category, non-Hispanic White, was selected as the reference group.
2.2.2. CRP
A detailed description of the HRS biomarker study is available (Crimmins et al., 2013). In brief, high-sensitivity assays primarily conducted at the University of Vermont were used to detect CRP levels in blood spots. As per HRS recommendations, the current study used National Health and Nutrition Examination Survey (NHANES)-equivalent values of CRP, which are based on serum blood. In line with American Heart Association and Centers for Disease Control and Prevention guidelines, CRP levels were categorized in terms of CVD risk: low (<1 mg/L), moderate (1–3 mg/L), and high (>3 mg/L) (Pearson et al., 2003).
2.2.3. Social variables
Educational attainment was self-reported from 0 to 17 years and centered at the sample median (12 years) to facilitate parameter interpretation. Interpersonal discrimination at baseline was assessed with the five-item Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997), administered as part of the psychosocial questionnaire. Items included, “You are treated with less courtesy or respect than other people,” “You receive poorer service than other people at restaurants or stores,” “People act as if they think you are not smart,” “People act as if they are afraid of you,” and “You are threatened or harassed.” Items are rated for frequency on a 6-point Likert-type scale (1 = Almost every day to 6 = Never). In the current study, mean scores were reversed prior to analysis so that higher scores correspond to greater discrimination. The Everyday Discrimination Scale has been validated across a variety of populations (Barnes et al., 2004; Gonzales et al., 2016; Williams et al., 1997). Alpha for this measure in the current sample was 0.80.
2.2.4. Psychological and behavioral variables
Depressive symptoms in the week leading up to the baseline visit were assessed with eight items from the Center for Epidemiologic Studies Depression scale (CES-D; Radloff, 1977), which were modified into a yes/no format. Higher scores correspond to more depressive symptoms. External locus of control at baseline was assessed with five items from the Perceived Control scale (Lachman & Weaver, 1998), administered as part of a leave-behind questionnaire. Items included, “I often feel helpless in dealing with the problems of life,” “Other people determine most of what I can and cannot do,” “What happens in my life is often beyond my control,” “I have little control over the things that happen to me,” and “There is really no way I can solve problems I have.” Items are rated for agreement on a 6-point Likert-type scale (1 = Strongly disagree to 6 = Strongly agree). Scores represent the average score across items, and higher scores correspond to more external locus of control. Alpha for this measure in the current sample was 0.86. Current smoking at baseline was operationalized as self-reported smoking status, with current non-smokers as the reference group.
2.2.5. Covariates
Analyses controlled for baseline age (centered at the sample median, 68 years), gender (male as reference category), and year of baseline assessment (2006 as reference category).
2.3. Analytic strategy
Descriptive statistics were computed in SPSS. Associations between race/ethnicity and CRP over four years were examined using structural equation models in Mplus. All models were weighted using HRS biomarker sample weights, which correct for over- or under-sampling and allow results to be generalizable to the larger population from which the sample was drawn (i.e., U.S. adults over age 50). Models were estimated using maximum likelihood estimation with robust standard errors (MLR). Missing data were managed with full information maximum likelihood (FIML). While FIML effectively handles non-random missingness related to variables included in the model, it does not account for missingness due to unobserved variables.
Baseline and follow-up CRP were estimated using latent difference score (LDS) models (McArdle & Nesselroade, 1994). Rather than calculating raw difference scores, the LDS model defined a latent variable corresponding to the residual of follow-up CRP, which was not predicted by baseline CRP. In the LDS model, features of CRP change that are of interest (e.g., mean CRP change, inter-individual variability in CRP change, relationship between baseline CRP and CRP change) are modeled as explicit parameters (McArdle, 2009).
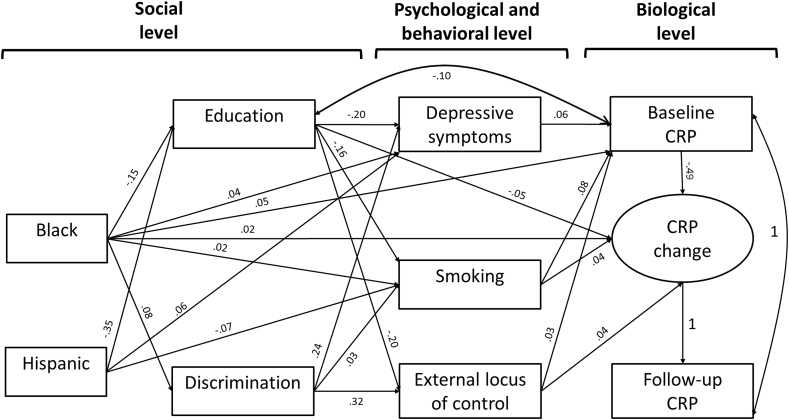
An initial model examined associations between Black race and Hispanic ethnicity and CRP over four years within a single model, controlling for age, gender, and baseline year. Next, the social (i.e., education, discrimination), psychological (i.e., depressive symptoms, external locus of control) and behavioral (i.e., smoking) variables were added to this model to examine psychosocial pathways linking race and ethnicity to CRP over four years. As shown in Fig. 1, baseline CRP and CRP change were regressed onto Black race and Hispanic ethnicity, all psychological, behavioral, and social variables, and all covariates in a single mediation model. In addition, each of the psychological and behavioral variables was regressed onto social variables, race and ethnicity, and covariates. Social variables were regressed onto race, ethnicity and covariates. Direct effects are associations between race and ethnicity and CRP over four years that are independent of all mediators and covariates. Indirect effects are specific effects of race and ethnicity on CRP over four years that operate through the mediator(s) and are calculated as the product of all regression paths within a given pathway. Total effects are the sum of all direct and indirect effects. The fit of all models was evaluated with the following commonly-used indices: comparative fit index (CFI), root-mean-square error of approximation (RMSEA), and standardized root-mean square residual (SRMR). CFI >0.95, RMSEA <0.06, and SRMR <0.05 were used as criteria for adequate model fit (Hu & Bentler, 1999).
Fig. 1.
Schematic of significant paths in the mediation model. Values shown are standardized estimates. For simplicity, covariates (i.e., age, gender, baseline assessment wave) and a correlation between contemporaneously-measured depressive symptoms and external locus of control are not shown. Note. CRP = C-reactive protein.
3. Results
3.1. CRP and race and ethnicity
Fit of the initial model examining the effects of race and ethnicity on baseline and follow-up CRP independent of covariates was perfect: CFI = 1.000; RMSEA = 0.000 (90% CI: 0.000 to 0.000), SRMR = 0.000. Independent of covariates, CRP increased over the four-year follow-up period (standardized estimate = 0.505; 95% CI: 0.467–0.543; p < 0.001). As shown in Table 2, individuals with higher baseline CRP evidenced smaller increases. Both Black and Hispanic individuals had significantly higher baseline CRP than non-Hispanic White individuals did. Black, but not Hispanic, individuals also showed a greater increase in CRP over the four-year study period. Higher baseline CRP was also associated with the later evaluation wave and female gender. Greater increase in CRP was also associated with female gender.
Table 2.
Demographic predictors of baseline CRP and four-year change in CRP.
| Standardized estimate | 95% CI | p | |
|---|---|---|---|
| Baseline CRP | |||
| Wave | 0.022 | 0.004–0.040 | 0.046 |
| Age | −0.018 | −0.036–0.000 | 0.092 |
| Female | 0.097 | 0.079–0.116 | <0.001 |
| Black | 0.075 | 0.059–0.091 | <0.001 |
| Hispanic | 0.033 | 0.016–0.050 | 0.001 |
| CRP change | |||
| Baseline CRP | −0.479 | −0.491 to −0.467 | <0.001 |
| Wave | 0.011 | −0.009–0.030 | 0.360 |
| Age | −0.004 | −0.025–0.017 | 0.778 |
| Female | 0.030 | 0.010–0.049 | 0.013 |
| Black | 0.034 | 0.017–0.052 | 0.001 |
| Hispanic | 0.003 | −0.016–0.022 | 0.773 |
Note. CRP = C-reactive protein; CI = Confidence Interval.
3.2. Psychosocial pathways from race and ethnicity to CRP
The mediation model fit well: CFI = 0.989; RMSEA = 0.047 (90% CI: 0.038–0.055), SRMR = 0.013. Associations between race and ethnicity and CRP were partially mediated by the social, psychological, and behavioral factors, as evidenced by attenuated direct effects and multiple significant indirect effects detailed in Table 3. Standardized estimates of significant paths are summarized in Fig. 1. Together, these mediators explained 34.67% of the association between Black race and baseline CRP and 32.35% of the association between Black race and CRP change. The association between Hispanic ethnicity and baseline CRP was fully mediated by the psychosocial variables, as the positive association between Hispanic ethnicity and baseline CRP (see Table 2) became negative and non-significant in the mediation model (see Table 3).
Table 3.
Standardized direct and indirect effects of race and ethnicity on CRP, estimated within a single model.
| Black race |
Hispanic ethnicity |
|||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | p | Estimate | 95% CI | p | |
| Baseline CRP | ||||||
| Direct effect | 0.049 | 0.033–0.065 | <0.001 | −0.012 | −0.030–0.006 | 0.285 |
| Specific indirect effects through: | ||||||
| Education | 0.015 | 0.012–0.018 | <0.001 | 0.036 | 0.029–0.043 | <0.001 |
| Education, depressive symptoms | 0.002 | 0.001–0.002 | <0.001 | 0.004 | 0.002–0.006 | <0.001 |
| Education, external locus of control | 0.001 | 0.000–0.002 | 0.014 | 0.000 | 0.000–0.000 | 0.014 |
| Education, smoking | 0.002 | 0.001–0.003 | <0.001 | 0.005 | 0.003–0.006 | <0.001 |
| Discrimination | 0.001 | 0.000–0.003 | 0.211 | 0.000 | −0.001–0.000 | 0.539 |
| Discrimination, depressive symptoms | 0.001 | 0.001–0.002 | <0.001 | 0.000 | 0.000–0.000 | 0.486 |
| Discrimination, external locus of control | 0.001 | 0.000–0.001 | 0.021 | 0.000 | 0.000–0.000 | 0.494 |
| Discrimination, smoking | 0.000 | 0.000–0.000 | 0.046 | 0.000 | 0.000–0.000 | 0.501 |
| Depressive symptoms | 0.002 | 0.001–0.004 | 0.003 | 0.003 | 0.002–0.005 | 0.001 |
| External locus of control | 0.000 | −0.001–0.000 | 0.335 | 0.001 | 0.000–0.001 | 0.155 |
| Smoking | 0.002 | 0.000–0.004 | 0.045 | −0.006 | −0.008 to −0.004 | <0.001 |
| CRP change | ||||||
| Direct effect | 0.023 | 0.005–0.040 | 0.038 | −0.018 | −0.038–0.002 | 0.148 |
| Specific indirect effects through: | ||||||
| Education | 0.007 | 0.004–0.011 | <0.001 | 0.017 | 0.009–0.025 | <0.001 |
| Education, depressive symptoms | 0.000 | 0.000–0.001 | 0.123 | 0.002 | 0.000–0.003 | 0.121 |
| Education, external locus of control | 0.001 | 0.000–0.002 | 0.018 | 0.003 | 0.001–0.004 | 0.017 |
| Education, smoking | 0.001 | 0.000–0.002 | 0.003 | 0.002 | 0.001–0.004 | 0.003 |
| Discrimination | 0.000 | −0.002–0.002 | 0.964 | 0.000 | 0.000–0.000 | 0.964 |
| Discrimination, depressive symptoms | 0.000 | 0.000–0.001 | 0.135 | 0.000 | 0.000–0.000 | 0.525 |
| Discrimination, external locus of control | 0.001 | 0.000–0.002 | 0.024 | 0.000 | 0.000–0.000 | 0.496 |
| Discrimination, smoking | 0.000 | 0.000–0.000 | 0.081 | 0.000 | 0.000–0.000 | 0.509 |
| Depressive symptoms | 0.001 | 0.000–0.002 | 0.141 | 0.001 | 0.000–0.003 | 0.143 |
| External locus of control | 0.000 | −0.001–0.000 | 0.330 | 0.001 | 0.000–0.002 | 0.162 |
| Smoking | 0.001 | 0.000–0.002 | 0.081 | −0.003 | −0.005 to −0.001 | 0.006 |
Note. CRP = C-Reactive Protein; CI = Confidence Interval.
3.2.1. Baseline CRP
There were nine significant indirect effects of Black race on baseline CRP. First, Black race was associated with lower educational attainment, and lower educational attainment was associated with higher baseline CRP. In addition to this single-mediator path, Black race was associated with higher baseline CRP through all three of the psychological and behavioral correlates of lower educational attainment: more depressive symptoms, greater external locus of control, and smoking. Specifically, lower educational attainment was associated with more depressive symptoms, greater external locus of control, and smoking. In turn, each of these psychological and behavioral variables independently predicted higher baseline CRP. Next, Black race was associated with higher baseline CRP through all three of the psychological and behavioral correlates of discrimination: more depressive symptoms, greater external locus of control, and smoking. Specifically, greater discrimination was associated with more depressive symptoms, greater external locus of control, and smoking. As noted above, more depressive symptoms, greater external locus of control, and smoking each independently predicted higher baseline CRP. There was no association between discrimination and baseline CRP independent of these psychological and behavioral variables.
Independent of the social variables (i.e., education and discrimination), Black race was also associated with higher baseline CRP through depressive symptoms and smoking. Specifically, Black individuals reported more depressive symptoms and were more likely to smoke, independent of education and discrimination. In turn, both depressive symptoms and smoking were associated with higher baseline CRP. Black individuals did not report more external locus of control independent of education and discrimination.
There were six significant indirect effects of Hispanic ethnicity on baseline CRP. First, Hispanic ethnicity was associated with lower educational attainment, and lower educational attainment was associated with higher baseline CRP. In addition to this single-mediator path, Hispanic ethnicity was associated with higher baseline CRP through all three of the psychological and behavioral correlates of lower educational attainment: more depressive symptoms, greater external locus of control, and smoking. Specifically, lower educational attainment was associated with more depressive symptoms, greater external locus of control, and smoking. In turn, each of these psychological and behavioral variables independently predicted higher baseline CRP. Independent of education, Hispanic ethnicity was also associated with more depressive symptoms. In turn, more depressive symptoms predicted higher baseline CRP. Finally, there was a single negative indirect effect of Hispanic ethnicity on baseline CRP. Independent of the social and psychological variables, Hispanic individuals were less likely to smoke, and smoking was associated with higher baseline CRP.
3.2.2. CRP change
There were four significant indirect effects of Black race on CRP change. First, Black race was associated with lower educational attainment, and lower educational attainment was associated with greater increase in CRP. In addition to this single-mediator path, Black race was associated with lower educational attainment, which predicted greater external locus of control and smoking, and both greater external locus of control and smoking predicted greater increase in CRP. Independent of education, Black race was also associated with greater discrimination. In turn, greater discrimination predicted greater external locus of control, and greater external locus of control predicted greater increase in CRP.
While there were no total or direct effects of Hispanic ethnicity on CRP change, there were four significant indirect effects. Specifically, Hispanic ethnicity was associated with lower education, and lower education was associated with greater increase in CRP. Lower education was also associated with greater external locus of control and smoking, each of which predicted greater increase in CRP over the four-year study period. Finally, there was a single negative indirect effect of Hispanic ethnicity on CRP change. Independent of the social and psychological variables, Hispanic individuals were less like to smoke, and smoking was associated with greater increase in CRP.
3.2.3. Sensitivity analysis
While the choice to model the psychological variables (i.e., depressive symptoms and external locus of control) as outcomes of the social variables (i.e., education and discrimination) was based on both theoretical (Clark et al., 1999) and empirical (Brown et al., 2000; Pavalko et al., 2003) work, these variables were measured concurrently in the primary model in order to allow for an examination of longitudinal change in the CRP outcome. The fit of models in which the ordering of (1) discrimination and depressive symptoms; or (2) discrimination and external locus of control was reversed were worse than the fit of the original model, in which depressive symptoms and external locus of control were both regressed onto discrimination (see Supplementary Table 1). However, adding in a modification that allowed for a correlation between education and depressive symptoms in the alternative model in which depressive symptoms predicted concurrently-measured discrimination resulted in the best overall fit.
Because cross-sectional mediation paths involving discrimination and the psychological factors (depressive symptoms and external locus of control) may be upwardly biased due to their concurrent measurement, a sensitivity analysis was conducted to compare cross-sectional coefficients between discrimination, depressive symptoms, and external locus of control measured at baseline (2006/2008) to longitudinal coefficients between baseline discrimination (2006/2008), follow-up depressive symptoms (2010/2012) and follow-up external locus of control (2010/2012). These longitudinal coefficients were slightly smaller than the corresponding cross-sectional coefficients shown in Fig. 1 (0.22 versus 0.24 for discrimination → depressive symptoms; 0.27 versus 0.32 for discrimination → external locus of control), indicating some upward bias. Finally, an additional sensitivity analysis confirmed that discrimination reported in 2006/2008 prospectively predicted both depressive symptoms (standardized estimate = 0.094; 95% CI: 0.072–0.116; p < 0.001) and external locus of control (standardized estimate = 0.118; 95% CI: 0.093–0.143; p < 0.001) four years later, controlling for previous values of depressive symptoms and external locus of control, respectively.
4. Discussion
This national, population-based, longitudinal study provides evidence for deleterious effects of racially and ethnically patterned psychosocial disadvantage on systemic inflammation. In line with the biopsychosocial framework, educational disadvantage was associated with worse CRP for both Black and Hispanic adults directly, as well as indirectly through the links between educational disadvantage and negative psychological and behavioral sequelae: higher depressive symptoms, greater external locus of control, and smoking. Independent of education, discrimination was also associated with worse CRP via depressive symptoms, external locus of control, and smoking for Black adults. Together, these results support the view that social disadvantage is associated with inflammatory processes for racial and ethnic minorities, though the current data cannot prove causation. Results further suggest that a portion of these associations is mediated by depressive symptoms, external locus of control, and smoking.
4.1. Social factors
Findings from this study support existing evidence that educational disadvantage contributes to racial and ethnic disparities in health (Phelan, Link, & Tehranifar, 2010). Our findings further indicate that at least one pathway by which racially patterned educational disadvantage might adversely affect health involves the negative psychological and behavioral correlates of lower educational attainment. Substantial literature demonstrates associations between lower educational attainment and adult depression (Akhtar-Danesh & Landeen, 2007; Eaton, Muntaner, Bovasso, & Smith, 2001; Kaplan, Roberts, Camacho, & Coyne, 1987; Ladin, 2008; Sargeant, Bruce, Florio, & Weissman, 1990), lower educational attainment and lower perceived control (Mirowsky & Ross, 2007), and lower educational attainment and smoking (Hu, Davies, & Kandel, 2006).
Education may promote psychological resilience by enhancing a vast array of personal and social resources, such as literacy (Nguyen et al., 2017), higher-status occupations (Link, Lennon, & Dohrenwend, 1993), higher income (Quesnel-Vallée & Taylor, 2012), embeddedness in cohesive social structures (Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997), and cultural entitlement (ten Kate, de Koster, & van der Waal, 2017). Through its socioeconomic benefits, education may reduce exposure to adversity throughout life and provide resources to handle crises (Turner & Noh, 1983; Wheaton, 1980). As a developmental environment, schooling also provides graded opportunities to succeed in increasingly challenging tasks, nurturing a sense of control (Mirowsky & Ross, 2007). It has been proposed that the negative association between education and smoking may reflect the use of smoking as a coping strategy in the face of environmental stressors (Mezuk, Abdou et al., 2013; Pomerleau & Pomerleau, 1984), and individuals with lower educational attainment are also less likely to benefit from anti-smoking campaigns (Escobedo & Peddicord, 1996). The fact that associations between education and CRP were not entirely mediated by the psychological and behavioral variables examined in this study points to additional pathways. For example, higher educational attainment is a prominent predictor of health behaviors beyond smoking, such as healthy eating and exercise (Hampson, Goldberg, Vogt, & Dubanoski, 2007). Additional research is needed to more fully characterize the protective effects of educational attainment.
In contrast to education, discrimination did not predict CRP above and beyond its psychological and behavioral consequences. The stress of discrimination accumulates over time (Essed, 1990a, 1990b; Williams et al., 1997), and discrimination has previously been linked to elevated depressive symptoms and external locus of control (Zahodne, Sol, & Kraal, 2019; Banks, Kohn-Wood, & Spencer, 2006; Earnshaw et al., 2016), as well as behaviors that may serve as self-regulatory coping strategies to preserve mental health in the face of social stressors, such as smoking (Mezuk, Abdou et al., 2013). The current study is consistent with these previous results indicating that discrimination is associated with negative psychological sequelae and negative health behaviors. Further, these findings warrant future longitudinal investigations of systemic inflammation as a potential downstream negative health effect of discrimination. A recent cross-sectional study in HRS documented a positive association between the experience of major discrimination and CRP (Cobb, Parker & Thorpe, 2018). The current study extends this previous work by focusing on everyday discrimination, incorporating follow-up CRP data, and examining psychological and behavioral mediators of the association between discrimination and CRP.
4.2. Psychological and behavioral factors
The results of this study are also consistent with previous work indicating that psychological factors predict subsequent inflammatory responses (Elliot et al., 2017; Stewart, Rand, Muldoon, & Kamarck, 2009). Specifically, depressive symptoms are consistently associated with elevated levels of CRP (Danner, Kasl, Abramson, & Vaccarino, 2003; Elovainio et al., 2006; Gimeno et al., 2009). The current study extends a previous longitudinal analysis of depressive symptoms and CRP in the HRS (Niles, Smirnova, Lin & Donovan, 2018) by examining its social antecedents and racial differences, as well as by including other related psychological and behavioral factors. Depressive symptoms increase sympathetic nervous activity, decrease parasympathetic nervous activity, and increase sedentary behavior and body mass index, all of which have been shown to promote inflammation (Di Gregorio et al., 2005; Kop & Gottdiener, 2005). Depressive symptoms may also directly promote inflammatory responses by activating the immune response (Maes, 1995; Maier & Watkins, 1998). While some longitudinal studies indicate that depressive symptoms predict subsequent inflammatory response, but not vice versa (Stewart et al., 2009), other studies indicate that depressive symptoms and inflammation exhibit a bi-directional relationship (Dantzer, O'Connor, Freund, Johnson, & Kelley, 2008; Matthews et al., 2010). Studies with greater longitudinal follow-up are needed to more directly characterize the nature of the relationship between depressive symptoms and CRP.
While fewer studies have examined associations between external locus of control and inflammatory response, a recent analysis in the HRS also documented a positive association between external locus of control and subsequent CRP (Elliot et al., 2017). The current study extends this previous work by considering racial and ethnic differences in perceived control. Having a sense of control may lead to less inflammation by reducing the impact of stressors, in line with experimental studies of other positive psychological factors such as optimism and self-esteem (Brydon, Walker, Wawrzyniak, Chart, & Steptoe, 2009; O'Donnell, Brydon, Wright, & Steptoe, 2008). In the current study, external locus of control was associated with a greater four-year increase in CRP, independent of baseline CRP, which supports a prospective association between perceived control and subsequent inflammation. However, additional experimental work is needed to confirm the direction of effects.
Finally, substantial evidence supports an association between smoking and inflammatory markers, including CRP (Tibuakuu et al., 2017; Tracy et al., 1997). Smoking modulates inflammation by activating a biological pathway that results in increased transcription of genes involved in the immune response (Goncalves et al., 2011; Rom, Avezov, Aizenbud, & Reznick, 2013). Interestingly, levels of CRP among former smokers are similar to those of individuals who have never smoked, supporting the beneficial health effects of smoking cessation (Tibuakuu et al., 2017).
4.3. Racial and ethnic differences
This study found differences in longitudinal CRP between Black and Hispanic participants. Compared to non-Hispanic Whites, Black participants showed higher levels of CRP at baseline and greater increases in CRP over the four-year study period. In contrast, there was only a significant Hispanic-White difference in baseline CRP. Indeed, Hispanic-White differences in inflammatory response are not always reported in studies of older adults (Albert, 2007), which has been interpreted in the context of intragroup variability among Hispanics and/or the “Hispanic paradox” of comparable or favorable health outcomes despite lower socioeconomic status (Crimmins et al., 2007; Mitchell & Aneshensel, 2016). Most strongly supported for Mexican Americans, the “Hispanic paradox” may reflect selective migration (Markides & Eschbach, 2005).
Another potential contributor to the “Hispanic paradox” involves smoking behavior (Perez-Stable et al., 2001). In the U.S., Hispanic adults are less likely to smoke than non-Hispanic Whites, though there is great variability in smoking behaviors across Hispanic subgroups (Kaplan et al., 2014), and Hispanic smokers are less likely to be advised to quit than non-Hispanic Whites (Lopez-Quintero, Crum, & Neumark, 2006). Independent of education and discrimination, Hispanic participants in this study were less likely to smoke than non-Hispanic Whites, while Black participants were more likely to smoke than non-Hispanic Whites. This difference resulted in a positive indirect effect of Black race on CRP through smoking and a negative indirect effect of Hispanic ethnicity on CRP through smoking. Furthermore, greater exposure to social exposures (i.e., low educational attainment and/or discrimination) among both Blacks and Hispanics was associated with higher baseline CRP and greater increase in CRP over time through smoking, suggesting additional points of intervention among disadvantaged subgroups.
Finally, while educational disadvantage mediated associations between both Black race and Hispanic ethnicity and higher CRP, discrimination only mediated associations involving Black race. In the U.S., Black individuals report higher levels of discrimination than non-Hispanic Whites across age, gender, and socioeconomic status (Forman, Williams, Jackson, & Gardner, 1997). In contrast, many studies report no difference in reports of discrimination across Hispanics and non-Hispanic Whites (T. T. Lewis, Yang, Jacobs, & Fitchett, 2012). This finding may reflect the items included in the Everyday Discrimination Scale, which were developed based on qualitative interviews with Black women (Essed, 1990a, 1990b; Williams et al., 1997). The lack of a significant Hispanic-White difference in discrimination may also reflect intragroup variability among Hispanic adults, as the perception of discrimination varies according to ethnic identity, immigrant status, and age of immigration among Hispanics (Pérez, Fortuna, & Alegria, 2008).
4.4. Limitations and strengths
Limitations of this study include the availability of only two time points of biomarker data, which precluded our ability to use growth curve modeling to more reliably evaluate associations involving cross-sectional level of inflammation versus changes in inflammation. However, the use of longitudinal biomarker data in this study strengthens our interpretation that psychosocial factors are prospectively associated with CVD risk, though these data cannot prove causation. Another limitation is the use of concurrent self-report measures of discrimination, depressive symptoms, and locus of control to predict concurrent CRP and four-year change in CRP. Indeed, a sensitivity analysis replacing concurrently-measured depressive symptoms and external locus of control with their values four years later indicated that the original mediation paths may be slightly upwardly biased. However, additional analyses confirmed that discrimination prospectively predicted both psychological factors four years later, controlling for previous values. Nonetheless, future studies should consider the contribution of response bias to associations between self-report variables and include additional longitudinal measures collected over varying time scales to clarify the direction of effects.
Another limitation was that smoking was the only health behavior examined in this study. We recommend that future research incorporate additional health behaviors to more fully model the complexity of racial and ethnic disparities (Mezuk, Abdou et al., 2013). In addition, only self-reported health conditions were available. Future work is needed to confirm effects in the context of additional, directly-measured information on specific health conditions. Because this study focused on only three racial and ethnic groups with adequate representation in the HRS, future studies are also needed to investigate long-term biological impacts of social and psychological stress among other groups. Finally, other limitations of the current study include possible selection bias above and beyond that addressed via sampling weights, assuming linear associations among the continuous variables (e.g., education), information bias from self-report, confounding due to uncontrolled for variables (e.g., region of residence, national origin), and chance findings from multiple comparisons.
Strengths of this study include its large sample of older adults from three racial and ethnic groups. The use of sampling weights allow the current results to be generalizable to the larger population of U.S. adults over age 50. The primary contribution of this study is its theoretically guided integration of biological, psychological, behavioral, and social variables into an empirical model. Links revealed by this model, as well as differences in these pathways between two minority groups (i.e., non-Hispanic Black and Hispanic), provide additional information regarding potential biopsychosocial pathways from race and ethnicity to CVD risk that can guide future work. Because this model reflects only a subset of a more comprehensive biopsychosocial model of racial and ethnic disparities in health, additional work is needed to integrate other structural (e.g., neighborhood disadvantage), behavioral (e.g., diet), and biological (e.g., cortisol) factors.
While the psychosocial factors examined in this study fully mediated the association between Hispanic ethnicity and baseline CRP, the fact that they only explained a portion of the association between Black race and CRP further underscores the need for more comprehensive models. The size of independent associations between each psychological factor (i.e., depressive symptoms and external locus of control) and CRP were between one third and three quarters of the size of the association between current smoking and baseline CRP, and the size of association between external locus of control and CRP change was the same as that between smoking and CRP change. Thus, the psychological factors examined in this study explained a substantial proportion of racial and ethnic variation in CRP and may warrant as much attention as other modifiable factors.
5. Conclusion
In conclusion, this nationally representative, longitudinal study helps to clarify health inequalities by detailing pathways through which the psychosocial experiences of Black and Hispanic adults are associated with systemic inflammation. By modeling multiple biopsychosocial pathways from race and ethnicity to CRP within a single model, this study provides an important replication of previous findings from studies that focused on only a subset of these pathways. Such replication is important for confirming that targeting only one pathway is unlikely to fully eliminate racial disparities and for demonstrating that certain related constructs (e.g., psychological and behavioral factors such as depressive symptoms, external locus of control, and smoking) may represent distinct opportunities for behavioral health interventions. In addition, this study makes a novel contribution to the literature on health disparities by demonstrating specific ways in which these biopsychosocial pathways to health disparities may differ for different minority groups (i.e., Hispanic versus non-Hispanic Black), which could guide more culturally-relevant prevention and intervention efforts. Because CRP is an important indicator of CVD risk, pathways involving education, discrimination, depressive symptoms, external locus of control, and smoking indicate that interventions targeted at these levels may have potential cardiovascular health benefits.
Ethics approval
This study used publicly-available data from the Health and Retirement Study, which was approved by the University of Michigan Institutional Review Board.
Acknowledgments
This research was supported in part by grants from the National Institutes on Aging [grant numbers R01AG054520, R00AG047963]. The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. The authors report no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100391.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Akhtar-Danesh N., Landeen J. Relation between depression and sociodemographic factors. International Journal of Mental Health Systems. 2007;1(1):4. doi: 10.1186/1752-4458-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Akhtar-Danesh, N., & Landeen, J. (2007). Relation between depression and sociodemographic factors. International Journal of Mental Health Systems, 1(1), 4. https://doi.org/10.1186/1752-4458-1-4 [DOI] [PMC free article] [PubMed]
- Albert M.A. Inflammatory biomarkers, race and ethnicity and cardiovascular disease. Nutrition Reviews. 2007;65(s3):S234–S238. doi: 10.1111/j.1753-4887.2007.tb00369.x. [DOI] [PubMed] [Google Scholar]; Albert, M. A. (2007). Inflammatory Biomarkers, Race and ethnicity and Cardiovascular Disease. Nutrition Reviews, 65(s3), S234-S238. [DOI] [PubMed]
- Bailis D.S., Segall A., Mahon J.J., Chipperfield J.G., Dunn E.M. Perceived control in relation to socioeconomic and behavioral resources for health. Social Science & Medicine. 2001;52(11):1661–1676. doi: 10.1016/s0277-9536(00)00280-x. [DOI] [PubMed] [Google Scholar]; Bailis, D. S., Segall, A., Mahon, J. J., Chipperfield, J. G., & Dunn, E. M. (2001). Perceived control in relation to socioeconomic and behavioral resources for health. Social Science & Medicine, 52(11), 1661-1676. [DOI] [PubMed]
- Banks K.H., Kohn-Wood L.P., Spencer M. An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Mental Health Journal. 2006;42(6):555–570. doi: 10.1007/s10597-006-9052-9. [DOI] [PubMed] [Google Scholar]; Banks, K. H., Kohn-Wood, L. P., & Spencer, M. (2006). An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Mental Health Journal, 42(6), 555-570. [DOI] [PubMed]
- Barnes L.L., Mendes De Leon C.F., Wilson R.S., Bienias J.L., Bennett D.A., Evans D.A. Racial differences in perceived discrimination in a community population of older Blacks and Whites. Journal of Aging and Health. 2004;16:315–337. doi: 10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]; Barnes, L.L., Mendes De Leon, C.F., Wilson, R.S., Bienias, J.L., Bennett, D.A., & Evans, D.A. (2004). Racial differences in perceived discrimination in a community population of older Blacks and Whites. Journal of Aging and Health, 16, 315-337. [DOI] [PubMed]
- Beatty Moody D.L., Brown C., Matthews K.A., Bromberger J.T. Everyday discrimination prospectively predicts inflammation across 7-years in racially diverse midlife women: Study of women's health across the nation. Journal of Social Issues. 2014;70(2):298–314. doi: 10.1111/josi.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]; Beatty Moody, D. L., Brown, C., Matthews, K. A., & Bromberger, J. T. (2014). Everyday Discrimination Prospectively Predicts Inflammation across 7-Years in Racially Diverse Midlife Women: Study of Women’s Health across the Nation. Journal of Social Issues, 70(2), 298-314. [DOI] [PMC free article] [PubMed]
- Bonilla-Silva E. Rethinking racism: Toward a structural interpretation. American Sociological Review. 1997;62:465–480. [Google Scholar]; Bonilla-Silva E. (1997) Rethinking racism: Toward a structural interpretation. American Sociological Review. 62.465-480.
- Broman C.L., Mavaddat R., Hsu S. The experience and consequences of perceived racial discrimination: A study of Americans. Journal of Black Psychology. 2000;26(2):165–180. [Google Scholar]; Broman, C. L., Mavaddat, R., & Hsu, S. (2000). The experience and consequences of perceived racial discrimination: A study of Americans. Journal of Black Psychology, 26(2), 165-180.
- Brown T.N., Williams D.R., Jackson J.S., Neighbors H.W., Torres M., Sellers S.L. “Being Black and feeling blue”: The mental health consequences of racial discrimination. Race and Society. 2000;2(2):117–131. [Google Scholar]; Brown T. N., Williams D.R., Jackson J.S., Neighbors H.W., Torres M., Sellers S.L., Brown K.T.. (2000) “Being Black and feeling blue”: The mental health consequences of racial discrimination. Race & Society. 2(2).117-131.
- Bruce M.A., Thornton M.C. It's my world? Exploring Black and white perceptions of personal control. The Sociological Quarterly. 2004;45(3):597–612. [Google Scholar]; Bruce, M. A., & Thornton, M. C. (2004). It’s my world? Exploring Black and White perceptions of personal control. The Sociological Quarterly, 45(3), 597- 612.
- Brydon L., Walker C., Wawrzyniak A.J., Chart H., Steptoe A. Dispositional optimism and stress-induced changes in immunity and negative mood. Brain, Behavior, and Immunity. 2009;23(6):810–816. doi: 10.1016/j.bbi.2009.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]; Brydon, L., Walker, C., Wawrzyniak, A. J., Chart, H., & Steptoe, A. (2009). Dispositional optimism and stress-induced changes in immunity and negative mood. Brain, Behavior, and Immunity, 23(6), 810-816. [DOI] [PMC free article] [PubMed]
- Bullock S.C., Houston E. Perceptions of racism by Black medical students attending White medical schools. Journal of the National Medical Association. 1987;79(6):601–608. [PMC free article] [PubMed] [Google Scholar]; Bullock, S. C, & Houston, E. (1987). Perceptions of racism by Black medical students attending White medical schools. Journal of the National Medical Association, 79(6), 601-608. [PMC free article] [PubMed]
- Chevalier A., Feinstein L. 2007. UCD geary institute discussion series. [Google Scholar]; Chevalier, A., & Feinstein, L. (2007). UCD Geary Institute Discussion Paper Series.
- Clark R., Anderson N.B., Clark V.R., Williams D.R. Racism as a stressor for African Americans. A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]; Clark, R., Anderson, N.B., Clark, V.R., & Williams, D.R. (1999). Racism as a stressor for African Americans. A biopsychosocial model. American Psychologist, 54, 805-816. [DOI] [PubMed]
- Cobb R.J., Parker L.J., Thorpe R.J. Self-reported instances of major discrimination, race/ethnicity, and inflammation among older adults: Evidence from the health and retirement study. Journal of Gerontology: Biological and Medical Sciences. 2018 Dec 1 doi: 10.1093/gerona/gly267. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]; Cobb, R.J., Parker, L.J., & Thorpe, R.J. (in press). Self-reported instances of major discrimination, race/ethnicity, an dinflammation among older adults: evidence from the Health and Retirement Study. Journal of Gerontology: Biological and Medical Sciences . [DOI] [PMC free article] [PubMed]
- Cokkinides V.E., Halpern M.T., Barbeau E.M., Ward E., Thun M.J. Racial and ethnic disparities in smoking-cessation interventions: Analysis of the 2005 national health interview survey. American Journal of Preventive Medicine. 2008;34:404–412. doi: 10.1016/j.amepre.2008.02.003. [DOI] [PubMed] [Google Scholar]; Cokkinides, V.E., Halpern, M.T., Barbeau, E.M., Ward, E., & Thun, M.J. (2008). Racial and ethnic disparities in smoking-cessation interventions: analysis of the 2005 National health Interview Survey. American Journal pf Preventive Medicine, 34, 404-412. [DOI] [PubMed]
- Crimmins E., Faul J., Kim J.K., Guyer H., Langa K., Ofstedal M.B. Survey Research Center University of Michigan; Ann Arbor, MI: 2013. Documentation of biomarkers in the 2006 and 2008 health and retirement study. [Google Scholar]; Crimmins, E., Faul, J., Kim, J. K., Guyer, H., Langa, K., Ofstedal, M. B., ... & Weir, D. (2013). Documentation of biomarkers in the 2006 and 2008 Health and Retirement Study. Ann Arbor, MI: Survey Research Center University of Michigan.
- Crimmins E.M., Hayward M.D., Seeman T. In: Critical perspectives on racial and ethnic differences in health in late life. National research council (US) panel on race, ethnicity, and health in later life. Anderson N.B., Bulatao R.A., Cohen B., editors. National Academies Press (US); Washington (DC): 2004. [PubMed] [Google Scholar]; Crimmins, E.M., Hayward, M.D., & Seeman, T. (2004). Critical perspectives on racial and ethnic differences in health in late life. National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life; Anderson NB, Bulatao RA, Cohen B, editors. Washington (DC): National Academies Press (US); 2004. [PubMed]
- Crimmins E.M., Kim J.K., Alley D.E., Karlamangla A., Seeman T. Hispanic paradox in biological risk profiles. American Journal of Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]; Crimmins, E. M., Kim, J. K., Alley, D. E., Karlamangla, A., & Seeman, T. (2007). Hispanic paradox in biological risk profiles. American Journal of Public Health, 97(7), 1305-1310. [DOI] [PMC free article] [PubMed]
- Danner M., Kasl S.V., Abramson J.L., Vaccarino V. Association between depression and elevated C-reactive protein. Psychosomatic Medicine. 2003;65(3):347–356. doi: 10.1097/01.psy.0000041542.29808.01. [DOI] [PubMed] [Google Scholar]; Danner, M., Kasl, S. V., Abramson, J. L., & Vaccarino, V. (2003). Association between depression and elevated C-reactive protein. Psychosomatic Medicine, 65(3), 347-356. [DOI] [PubMed]
- Dantzer R., O'Connor J.C., Freund G.G., Johnson R.W., Kelley K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nature Reviews Neuroscience. 2008;9(1):46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dantzer R., O’Connor J.C., Freund G.G., Johnson R.W., Kelley K.W. (2008). From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience; 9(1): 46 -56. [DOI] [PMC free article] [PubMed]
- Di Gregorio G.B., Yao–Borengasser A., Rasouli N., Varma V., Lu T., Miles L.M. Expression of CD68 and macrophage chemoattractant protein-1 genes in human adipose and muscle tissues: Association with cytokine expression, insulin resistance, and reduction by pioglitazone. Diabetes. 2005;54(8):2305–2313. doi: 10.2337/diabetes.54.8.2305. [DOI] [PubMed] [Google Scholar]; Di Gregorio G.B., Yao-Borengasser A., Rasouli N., Varma V., Lu T., Miles L.M., …, Kern P.A. Expression of CD68 and macrophage chemoattractant protein-1 genes in human adipose and muscle tissues: Association with cytokine expression, insulin resistance, and reduction by pioglitazone. Diabetes54(8), 2305-2313. [DOI] [PubMed]
- Earnshaw V.A., Rosenthal L., Carroll-Scott A., Santilli A., Gilstad-Hayden K., Ickovics J.R. Everyday discrimination and physical health: Exploring mental health processes. Journal of Health Psychology. 2016;21(10):2218–2228. doi: 10.1177/1359105315572456. [DOI] [PMC free article] [PubMed] [Google Scholar]; Earnshaw, V. A., Rosenthal, L., Carroll-Scott, A., Santilli, A., Gilstad-Hayden, K., & Ickovics, J. R. (2016). Everyday discrimination and physical health: Exploring mental health processes. Journal of Health Psychology, 21(10), 2218-2228. [DOI] [PMC free article] [PubMed]
- Eaton W.W., Muntaner C., Bovasso G., Smith C. Socioeconomic status and depressive syndrome: The role of inter- and intra-generational mobility, government assistance, and work environment. Journal of Health and Social Behavior. 2001;42(3):277–294. [PMC free article] [PubMed] [Google Scholar]; Eaton, W. W., Muntaner, C., Bovasso, G., & Smith, C. (2001). Socioeconomic status and depressive syndrome: the role of inter- and intra-generational mobility, government assistance, and work environment. Journal of Health and Social Behavior, 42(3), 277-294. [PMC free article] [PubMed]
- Elliot A.J., Mooney C.J., Infurna F.J., Chapman B.P. Associations of lifetime trauma and chronic stress with C-reactive protein in adults ages 50 Years and older: Examining the moderating role of perceived control. Psychosomatic Medicine. 2017;79(6):622–630. doi: 10.1097/PSY.0000000000000476. [DOI] [PubMed] [Google Scholar]; Elliot, A. J., Mooney, C. J., Infurna, F. J., & Chapman, B. P. (2017). Associations of Lifetime Trauma and Chronic Stress with C-reactive Protein in Adults Ages 50 Years and Older: Examining the moderating role of perceived control. Psychosomatic Medicine, 79(6), 622-630. [DOI] [PubMed]
- Elovainio M., Keltikangas-Järvinen L., Pulkki-Råback L., Kivimäki M., Puttonen S., Viikari L. Depressive symptoms and C-reactive protein: The cardiovascular risk in young Finns study. Psychological Medicine. 2006;36(6):797–805. doi: 10.1017/S0033291706007574. [DOI] [PubMed] [Google Scholar]; Elovainio, M., Keltikangas-Jarvinen, L., Pulkki-Raback, L., Kivimaki, M., Puttonen, S., Viikari, L., ... & Raitakari, O. T. (2006). Depressive symptoms and C-reactive protein: The cardiovascular risk in young Finns study. Psychological Medicine, 36(6), 797-805. [DOI] [PubMed]
- Escobedo L.G., Peddicord J.P. Smoking prevalence in US birth cohorts: The influence of gender and education. American Journal of Public Health. 1996;86:231–236. doi: 10.2105/ajph.86.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]; Escobedo, L.G., & Peddicord, J.P. (1996). Smoking prevalence in US birth cohorts: the influence of gender and education. American Journal of Public Health, 86, 231-236. [DOI] [PMC free article] [PubMed]
- Essed P. Hunter House Publishers; 1990. Everyday racism: Reports from women of two cultures. [Google Scholar]; Essed, P. (1990a). Everyday racism: Reports from women of two cultures. Hunter House Publishers.
- Essed P. Vol. 2. Sage; 1990. (Understanding everyday racism: An interdisciplinary theory). [Google Scholar]; Essed, P. (1990b). Understanding everyday racism: An interdisciplinary theory (Vol. 2). Sage.
- Forman T.A., Williams D.R., Jackson J.S., Gardner C. Race, place, and discrimination. In: Gardner C., editor. Perspectives on social problems. JAI Press; 1997. pp. 231–261. 9. [Google Scholar]; Forman, T. A., Williams, D. R., Jackson, J. S., & Gardner, C. (1997). Race, place, and discrimination. In C. Gardner (Ed.), Perspectives on Social Problems (pp. 9: 231-261). JAI Press.
- Friedman E.M., Williams D.R., Singer B.H., Ryff C.D. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: The MIDUS study. Brain, Behavior, and Immunity. 2009;23(5):684–692. doi: 10.1016/j.bbi.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; Friedman, E. M., Williams, D. R., Singer, B. H., & Ryff, C. D. (2009). Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: The MIDUS study. Brain, Behavior, and Immunity, 23(5), 684-692. [DOI] [PMC free article] [PubMed]
- Gimeno D., Kivimäki M., Brunner E.J., Elovainio M., De Vogli R., Steptoe A. Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the whitehall II study. Psychological Medicine. 2009;39(3):413. doi: 10.1017/S0033291708003723. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gimeno, D., Kivimaki, M., Brunner, E. J., Elovainio, M., De Vogli, R., Steptoe, A., … Marmot, M.G. (2009). Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychological Medicine, 39(3), 413. [DOI] [PMC free article] [PubMed]
- Goncalves R.B., Coletta R.D., Silvério K.G., Benevides L., Casati M.Z., da Silva J.S. Impact of smoking on inflammation: Overview of molecular mechanisms. Inflammatory Research. 2011;60:409–424. doi: 10.1007/s00011-011-0308-7. [DOI] [PubMed] [Google Scholar]; Goncalves, R.B., Coletta, R.D., Silverio, K.G., et al. (2011). Impact of smoking on inflammation: overview of molecular mechanisms. Inflammatory Research, 60, 409-424. [DOI] [PubMed]
- Gonzales K.L., Noonan C., Goins R.T., Henderson W.G., Beals J., Manson S.M. Assessing the everyday discrimination scale among American Indians and Alaska natives. Psychological Assessment. 2016;28:51–58. doi: 10.1037/a0039337. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gonzales, K.L., Noonan, C., Goins, R.T., Henderson, W.G., Beals, J., … & Roubideaux, Y. (2016). Assessing the Everyday Discrimination Scale among American Indians and Alaska Natives. Psychological Assessment, 28, 51-58. [DOI] [PMC free article] [PubMed]
- Hampson S.E., Goldberg L.R., Vogt T.M., Dubanoski J.P. Mechanisms by which childhood personality traits influence adult health status: Educational attainment and healthy behaviors. Health Psychology. 2007;26(1):121. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hampson, S. E., Goldberg, L. R., Vogt, T. M., & Dubanoski, J. P. (2007). Mechanisms by which childhood personality traits influence adult health status: Educational attainment and healthy behaviors. Health Psychology, 26(1), 121. [DOI] [PMC free article] [PubMed]
- Howren M.B., Lamkin D.M., Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosomatic Medicine. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]; Howren, M.B., Lamkin, D.M., & Suls, J. (2009). Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosomatic Medicine, 71, 171-186. [DOI] [PubMed]
- Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]; Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1-55.
- Hu M.C., Davies M., Kandel D.B. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. American Journal of Public Health. 2006;96:299–308. doi: 10.2105/AJPH.2004.057232. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hu, M.C., Davies, M., & Kandel, D.B. (2006). Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. American Journal of Public Health, 96, 299-308. [DOI] [PMC free article] [PubMed]
- Jackson J.S., Knight K.M. Race and self-regulatory health behaviors: The role of the stress response and the HPA Axis in physical and mental health disparities. In: Schaie K.W., Cartensen L., editors. Social structures, aging, and self-regulation in the elderly. Springer; New York: 2006. pp. 189–207. [Google Scholar]; Jackson, J.S., Knight, K.M. Race and Self-regulatory Health Behaviors: The Role of the Stress Response and the HPA Axis in Physical and Mental Health Disparities. In: Schaie, KW.; Cartensen, L., editors. Social Structures, Aging, and Self-Regulation in the Elderly. Springer; New York: 2006. p. 189-207.
- Jackson J.S., Knight K.M., Rafferty J.A. Race and unhealthy behaviors: Chronic stress, the HPA Axis, and physical and mental health disparities over the life-course. American Journal of Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jackson, J.S., Knight, K.M., & Rafferty, J.A. (2010). Race and unhealthy behaviors: chronic stress, the HPA Axis, and physical and mental health disparities over the life-course. American Journal of Public Health, 100, 933-939. [DOI] [PMC free article] [PubMed]
- Kaplan R.C., Bangdiwala S.I., Barnhart J.M., Castañeda S.F., Gellman M.D., Lee D.J. Smoking among US Hispanic/Latino adults: The Hispanic community health study/study of Latinos. American Journal of Preventive Medicine. 2014;46:496–506. doi: 10.1016/j.amepre.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kaplan, R.C., Bangdiwala, S.I., Barnhart, J.M., et al. (2014). Smoking among US Hispanic/Latino adults: the Hispanic Community Health Study/Study of Latinos. American Journal of Preventive Medicine, 46, 496-506. [DOI] [PMC free article] [PubMed]
- Kaplan G.A., Roberts R.E., Camacho T.C., Coyne J.C. Psychosocial predictors of depression: Prospective evidence from the human population laboratory studies. American Journal of Epidemiology. 1987;125(2):206–220. doi: 10.1093/oxfordjournals.aje.a114521. [DOI] [PubMed] [Google Scholar]; Kaplan, G. A., Roberts, R. E., Camacho, T. C., & Coyne, J. C. (1987). Psychosocial predictors of depression: Prospective evidence from the human population laboratory studies. American Journal of Epidemiology, 125(2), 206-220. [DOI] [PubMed]
- ten Kate J., de Koster W., van der Waal J. Why are depressive symptoms more prevalent among the less educated? The relevance of low cultural capital and cultural entitlement. Sociological Spectrum. 2017;37:63–76. [Google Scholar]; ten Kate, J., de Koster, W., & van der Waal, J. (2017). Why are depressive symptoms more prevalent among the less educated? The relevance of low cultural capital and cultural entitlement. Sociological Spectrum, 37, 63-76.
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kawachi, I., Kennedy, B. P., Lochner, K., & Prothrow-Stith, D. (1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87(9), 1491-1498. [DOI] [PMC free article] [PubMed]
- Kochanek K.D., Murphy S.L., Xu J. Deaths: Final data for 2011. National vital statistics Reports : From the Centers for disease Control and prevention, national Center for health statistics. National Vital Statistics System. 2015;63(3):1–120. [PubMed] [Google Scholar]; Kochanek, K. D., Murphy, S. L., & Xu, J. (2015). Deaths: Final Data for 2011. National Vital Statistics Reports : From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 63(3), 1-120. [PubMed]
- Kop W.J., Gottdiener J.S. The role of immune system parameters in the relationship between depression and coronary artery disease. Psychosomatic Medicine. 2005;67:S37–41. doi: 10.1097/01.psy.0000162256.18710.4a. [DOI] [PubMed] [Google Scholar]; Kop W.J., Gottdiener J.S. (2005). The role of immune system parameters in the relationship between depression and coronary artery disease. Psychosomatic Medicine.;67,S37- 41. [DOI] [PubMed]
- Kop W.J., Gottdiener J.S., Tangen C.M., Fried L.P., McBurnie M.A., Walston J. Inflammation and coagulation factors in persons >65 years of age with symptoms of depression but without evidence of myocardial ischemia. The American Journal of Cardiology. 2002;89:419–424. doi: 10.1016/s0002-9149(01)02264-0. [DOI] [PubMed] [Google Scholar]; Kop, W.J., Gottdiener, J.S., Tangen, C.M., Fried, L.P., McBurnie, M.A., Walston, J., …, Tracy, R.P., 2002. Inflammation and coagulation factors in persons >65 years of age with symptoms of depression but without evidence of myocardial ischemia. Am. J. Cardiol. 89, 419-424. [DOI] [PubMed]
- Lachman M.E., Weaver S.L. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74(3):763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]; Lachman, M. E., & Weaver, S. L. (1998). The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology, 74(3), 763-773. [DOI] [PubMed]
- Ladin K. Risk of late-life depression across 10 European Union Countries: Deconstructing the education effect. Journal of Aging and Health. 2008;20(6):653–670. doi: 10.1177/0898264308321002. [DOI] [PubMed] [Google Scholar]; Ladin, K. (2008). Risk of late-life depression across 10 European Union Countries: Deconstructing the education effect. Journal of Aging and Health, 20(6), 653-670. [DOI] [PubMed]
- Lazarus R.S., Folkman S. 1984. Coping and adaptation; pp. 282–325. (The Handbook of Behavioral Medicine). [Google Scholar]; Lazarus, R. S., & Folkman, S. (1984). Coping and adaptation. The Handbook of Behavioral Medicine, 282-325.
- Lewis T.T., Aiello A.E., Leurgans S., Kelly J., Barnes L.L. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity. 2010;24(3):438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lewis, T. T., Aiello, A. E., Leurgans, S., Kelly, J., & Barnes, L. L. (2010). Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity, 24(3), 438-443. [DOI] [PMC free article] [PubMed]
- Lewis S.K., Ross C.E., Mirowsky J. Establishing a sense of personal control in the transition to adulthood. Social Forces. 1999;77(4):1573–1599. [Google Scholar]; Lewis, S. K., Ross, C. E., & Mirowsky, J. (1999). Establishing a sense of personal control in the transition to adulthood. Social Forces, 77(4), 1573- 1599.
- Lewis T.T., Yang F.M., Jacobs E.A., Fitchett G. Racial and ethnic differences in responses to the everyday discrimination scale: A differential item functioning analysis. American Journal of Epidemiology. 2012;175(5):391–401. doi: 10.1093/aje/kwr287. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lewis, T. T., Yang, F. M., Jacobs, E. A., & Fitchett, G. (2012). Racial and ethnic Differences in Responses to the Everyday Discrimination Scale: A Differential Item Functioning Analysis. American Journal of Epidemiology, 175(5), 391-401. [DOI] [PMC free article] [PubMed]
- Link B.G., Lennon M.C., Dohrenwend B.P. Socioeconomic status and depression: The role of occupations involving direction, control, and planning. American Journal of Sociology. 1993;98:1351–1387. [Google Scholar]; Link, B.G., Lennon, M.C., & Dohrenwend, B.P. (1993). Socioeconomic status and depression: the role of occupations involving direction, control, and planning. American Journal of Sociology, 98, 1351-1387.
- Lopez-Quintero C., Crum R.M., Neumark Y.D. Racial/ethnic disparities in report of physician-provided smoking cessation advice: Analysis of the 2000 national health interview survey. American Journal of Public Health. 2006;96:2235–2239. doi: 10.2105/AJPH.2005.071035. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lopez-Quintero, C, Crum RM, Neumark YD. (2006). Racial/ethnic disparities in report of physician-provided smoking cessation advice: analysis of the 2000 National Health Interview Survey. American Journal of Public Health, 96, 2235-2239. [DOI] [PMC free article] [PubMed]
- Maes M. Evidence for an immune response in major depression: A review and hypothesis. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 1995;19(1):11–38. doi: 10.1016/0278-5846(94)00101-m. [DOI] [PubMed] [Google Scholar]; Maes, M. (1995). Evidence for an immune response in major depression: A review and hypothesis. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 19(1), 11-38. [DOI] [PubMed]
- Maier S.F., Watkins L.R. Cytokines for psychologists: Implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychological Review. 1998;105:83–107. doi: 10.1037/0033-295x.105.1.83. [DOI] [PubMed] [Google Scholar]; Maier, S. F. & Watkins, L. R. (1998). Cytokines for psychologists: implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychological Review, 105, 83-107. [DOI] [PubMed]
- Markides K.S., Eschbach K. Aging, migration, and mortality: Current status of research on the hispanic paradox. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]; Markides, K.S., & Eschbach, K. (2005). Aging, migration, and mortality: current status of research on the Hispanic paradox. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 68-75. [DOI] [PubMed]
- Matthews K.A., Schott L.L., Bromberger J.T., Cyranowski J.M., Everson-Rose S.A., Sowers M. Are there bi-directional associations between depressive symptoms and C-reactive protein in mid-life women? Brain, Behavior, and Immunity. 2010;24(1):96–101. doi: 10.1016/j.bbi.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]; Matthews, K.A., Schott, L.L., Bromberger, J.T., Cyranowski, J.M., Everson-Rose, S.A., & Sowers, M. (2010). Are there bi-directional associations between depressive symptoms and C-reactive protein in mid-life women? Brain, Behavior, and Immunity, 24(1), 96-101. [DOI] [PMC free article] [PubMed]
- McArdle J.J. Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology. 2009;60(1):577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]; McArdle, J. J. (2009). Latent Variable Modeling of Differences and Changes with Longitudinal Data. Annual Review of Psychology, 60(1), 577-605. [DOI] [PubMed]
- McArdle J.J., Nesselroade J.R. Using multivariate data to structure developmental change. In: Cohen S.H., Reese H.W., editors. The West Virginia University conferences on life-span developmental psychology. Life-span developmental psychology: Methodological contributions. Lawrence Erlbaum Associates; Hillsdale, NJ: 1994. pp. 223–267. [Google Scholar]; McArdle, J. J., & Nesselroade, J. R. (1994). Using multivariate data to structure developmental change. In S. H. Cohen & H. W. Reese (Eds.), The West Virginia University conferences on life-span developmental psychology. Life-span developmental psychology: Methodological contributions (pp. 223-267). Hillsdale, NJ: Lawrence Erlbaum Associates.
- McFarland M.J., Wagner B.G. Does a college education reduce depressive symptoms in American young adults? Social Science & Medicine. 2015;146:75–84. doi: 10.1016/j.socscimed.2015.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]; McFarland, M.J., & Wagner, B.G. (2015). Does a college education reduce depressive symptoms in American young adults? Social Science & Medicine, 146, 75-84. [DOI] [PMC free article] [PubMed]
- Mezuk B., Abdou C.M., Hudson D., Kershaw K.N., Rafferty J.A., Lee H. “White box” epidemiology and the social neuroscience of health behaviors: The environmental Affordances model. Society and Mental Health. 2013;3(2) doi: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mezuk, B., Abdou, C.M., Hudson, D., Kershaw, K.N., Rafferty, J.A., Lee, H., & Jackson, J.S. (2013). “White box” epidemiology and the social neuroscience of health behaviors: the Environmental Affordances Model. Society and Mental Health, 3(2). [DOI] [PMC free article] [PubMed]
- Mezuk B., Myers J.M., Kendler K.S. Integrating social science and behavioral genetics: Testing the origin of socioeconomic disparities in depression using a genetically informed design. American Journal of Public Health. 2013;103(S1):S145–S151. doi: 10.2105/AJPH.2013.301247. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mezuk, B., Myers, J. M., & Kendler, K. S. (2013). Integrating social science and behavioral genetics: Testing the origin of socioeconomic disparities in depression using a genetically informed design. American Journal of Public Health, 103(S1), S145-S151. [DOI] [PMC free article] [PubMed]
- Mirowsky J., Ross C.E. Life course trajectories of perceived control and their relationship to education. American Journal of Sociology. 2007;112(5):1339–1382. doi: 10.1086/511800. [DOI] [Google Scholar]; Mirowsky, J., & Ross, C. E. (2007). Life course trajectories of perceived control and their relationship to education. American Journal of Sociology, 112(5), 1339-1382. https://doi.org/10.1086/511800
- Mitchell U.A., Aneshensel C.S. Social inequalities in inflammation: Age variations in older persons. Journal of Aging and Health. 2016:1–19. doi: 10.1177/0898264316645546. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mitchell, U. A., & Aneshensel, C. S. (2016). Social Inequalities in Inflammation: Age Variations in Older Persons. Journal of Aging and Health, 1-19. [DOI] [PMC free article] [PubMed]
- Nguyen T.T., Tchetgen E.J.T., Kawachi I., Gilman S.E., Walter S., Glymour M.M. The role of literacy in the association between educational attainment and depressive symptoms. SSM - Population Health. 2017;3:586–593. doi: 10.1016/j.ssmph.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; Nguyen, T. T., Tchetgen, E. J. T, Kawachi, I., Gilman, S. E., Walter, S., & Glymour, M. M. (2017). The role of literacy in the association between educational attainment and depressive symptoms. SSM - Population Health, 3, 586-593. [DOI] [PMC free article] [PubMed]
- Niles A.N., Smirnova M., O'Donovan A. Gender differences in longitudinal relationships between depression and anxiety symptoms and inflammation in the health and retirement Study. Psychoneuroendocrinology. 2018;95:149–157. doi: 10.1016/j.psyneuen.2018.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]; Niles, A.N., Smirnova, M., & O’Donovan, A. (2018). Gender differences in longitudinal relationships between depression nan danxiety symptoms and inflammation in the Health an dRetirement Study. Psychoneuroendocrinology, 95, 149-157. [DOI] [PMC free article] [PubMed]
- O'Donnell K., Brydon L., Wright C.E., Steptoe A. Self-esteem levels and cardiovascular and inflammatory responses to acute stress. Brain, Behavior, and Immunity. 2008;22(8):1241–1247. doi: 10.1016/j.bbi.2008.06.012. [DOI] [PubMed] [Google Scholar]; O’Donnell, K., Brydon, L., Wright, C. E., & Steptoe, A. (2008). Self-esteem levels and cardiovascular and inflammatory responses to acute stress. Brain, Behavior, And Immunity, 22(8), 1241-1247. [DOI] [PubMed]
- Pavalko E.K., Mossakowski K.N., Hamilton V.J. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women's physical and emotional health. Journal of Health and Social Behavior. 2003:18–33. [PubMed] [Google Scholar]; Pavalko, E. K., Mossakowski, K. N., & Hamilton, V. J. (2003). Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women's physical and emotional health. Journal Of Health And Social Behavior, 18-33. [PubMed]
- Pearlin L.I., Nguyen K.B., Schieman S., Milkie M.A. The life-course origins of mastery among older people. Journal of Health and Social Behavior. 2007;48:164–179. doi: 10.1177/002214650704800205. [DOI] [PubMed] [Google Scholar]; Pearlin, L. I., Nguyen, K. B., Schieman, S., & Milkie, M. A. (2007). The life-course origins of mastery among older people. Journal of Health and Social Behavior, 48, 164 -179. doi:10.1177/002214650704800205 [DOI] [PubMed]
- Pearlin L.I., Schieman S., Fazio E.M., Meersman S.C. Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]; Pearlin, L. I., Schieman, S., Fazio, E. M., & Meersman, S. C. (2005). Stress, health, and the life course: Some conceptual perspectives. Journal Of Health And Social Behavior, 46(2), 205-219. [DOI] [PubMed]
- Pearson T.A., Mensah G.A., Alexander R.W., Anderson J.L., Cannon R.O., Criqui M. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the centers for disease control and prevention and the american heart association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]; Pearson, T. A., Mensah, G. A., Alexander, R. W., Anderson, J. L., Cannon, R. O., Criqui, M., … American Heart Association. (2003). Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation, 107(3), 499-511. [DOI] [PubMed]
- Perez-Stable E.J., Ramirez A., Villareal R., Talavera G.A., Trapido E., Suarez L. Cigarette smoking behavior among US Latino men and women from different countries of Origin. American Journal of Public Health. 2001;91(9):1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]; Perez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, et al. Cigarette smoking behavior among US Latino men and women from different countries of Origin. American Journal of Public Health. 2001;91(9):1424-1430. [DOI] [PMC free article] [PubMed]
- Pérez D.J., Fortuna L., Alegría M. Prevalence and correlates of everyday discrimination among U.S. Latinos. Journal of Community Psychology. 2008;36(4):421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]; Perez, D. J., Fortuna, L., & Alegria, M. (2008). Prevalence and correlates of everyday discrimination among U.S. Latinos. Journal of Community Psychology, 36(4), 421-433. [DOI] [PMC free article] [PubMed]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior. 2010;51(1_suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]; Phelan, J. C., Link, B. G., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior, 51(1_suppl), S28-S40. [DOI] [PubMed]
- Pomerleau O.F., Pomerleau C.S. Neuroregulators and the reinforcement of smoking: Towards a biobehavioral explanation. Neuroscience & Biobehavioral Reviews. 1984;8:505–513. doi: 10.1016/0149-7634(84)90007-1. [DOI] [PubMed] [Google Scholar]; Pomerleau, O.F., & Pomerleau, C.S. (1984). Neuroregulators and the reinforcement of smoking: towards a biobehavioral explanation. Neuroscience & Biobehavioral Reviews, 8, 505-513. [DOI] [PubMed]
- Pudrovska T., Schieman S., Pearlin L.I., Nguyen K. The sense of mastery as a mediator and moderator in the association between economic hardship and health in later life. Journal of Aging and Health. 2005;17:634–660. doi: 10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]; Pudrovska, T., Schieman, S., Pearlin, L. I., & Nguyen, K. (2005). The sense of mastery as a mediator and moderator in the association between economic hardship and health in later life. Journal of Aging and Health, 17, 634 - 660. doi:10.1177/0898264305279874 [DOI] [PubMed]
- Quesnel-Vallée A., Taylor M. Socioeconomic pathways to depressive symptoms in adulthood: Evidence from the national longitudinal survey of youth 1979. Social Science & Medicine. 2012;74(5):734–743. doi: 10.1016/j.socscimed.2011.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]; Quesnel-Vallee, A., & Taylor, M. (2012). Socioeconomic pathways to depressive symptoms in adulthood: Evidence from the national longitudinal survey of youth 1979. Social Science & Medicine, 74(5), 734-743. [DOI] [PMC free article] [PubMed]
- Radloff L.S. The CES-D scale. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]; Radloff, L. S. (1977). The CES-D Scale. Applied Psychological Measurement, 1(3), 385-401.
- Ranjit N., Diez-Roux A.V., Shea S., Cushman M., Ni H., Seeman T. Socioeconomic position, race and ethnicity, and inflammation in the multi-ethnic study of atherosclerosis. Circulation. 2007;116(21):2383–2390. doi: 10.1161/CIRCULATIONAHA.107.706226. [DOI] [PubMed] [Google Scholar]; Ranjit, N., Diez-Roux, A. V, Shea, S., Cushman, M., Ni, H., & Seeman, T. (2007). Socioeconomic position, race and ethnicity, and inflammation in the multi-ethnic study of atherosclerosis. Circulation, 116(21), 2383-2390. [DOI] [PubMed]
- Ridker P.M., Rifai N., Rose L., Buring J.E., Cook N.R. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. New England Journal of Medicine. 2002;347(20):1557–1565. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]; Ridker P.M., Rifai N., Rose L., Buring J.E., and Cook N.R., Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. New England Journal of Medicine 347(20), 2002, 1557-1565. [DOI] [PubMed]
- Rom O., Avezov K., Aizenbud D., Reznick A.Z. Cigarette smoking and inflammation revisited. Respiratory Physiology & Neurobiology. 2013;187:5–10. doi: 10.1016/j.resp.2013.01.013. [DOI] [PubMed] [Google Scholar]; Rom, O., Avezov, K., Aizenbud, D., & Reznick, A.Z. (2013). Cigarette smoking and inflammation revisited. Respiratory Physiology & Neurobiology, 187, 5-10. [DOI] [PubMed]
- Sargeant J.K., Bruce M.L., Florio L.P., Weissman M.M. Factors associated with 1-year outcome of major depression in the community. Archives of General Psychiatry. 1990;47(6):519. doi: 10.1001/archpsyc.1990.01810180019004. [DOI] [PubMed] [Google Scholar]; Sargeant, J. K., Bruce, M. L., Florio, L. P., & Weissman, M. M. (1990). Factors Associated With 1-Year Outcome of Major Depression in the Community. Archives of General Psychiatry, 47(6), 519. [DOI] [PubMed]
- Schieman S. Age, education, and the sense of control: A test of the cumulative advantage hypothesis. Research on Aging. 2001;23:153–178. [Google Scholar]; Schieman, S. (2001). Age, education, and the sense of control: A test of the cumulative advantage hypothesis. Research on Aging, 23, 153-178. doi:10.1177/0164027501232002
- Slavich G.M., Irwin M.R. From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin. 2014;140(3):774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]; Slavich, G. M., & Irwin, M. R. (2014). From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychological Bulletin, 140(3), 774-815. [DOI] [PMC free article] [PubMed]
- Sonnega A., Weir D.R. The health and retirement study: A public data resource for research on aging. Open Health Data. 2014;2(1) doi: 10.5334/ohd.am. [DOI] [Google Scholar]; Sonnega, A., & Weir, D. R. (2014). The health and retirement study: A public data resource for research on aging. Open Health Data, 2(1). https://doi.org/10.5334/ohd.am
- Stewart J.C., Rand K.L., Muldoon M.F., Kamarck T.W. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain, Behavior, and Immunity. 2009;23(7):936–944. doi: 10.1016/j.bbi.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]; Stewart, J.C., Rand, K.L., Muldoon, M.F., Kamarck, T.W. (2009). A prospective evaluation of the directionality of the depression-inflammation relationship. Brain, behavior, and immunity, 23(7), 936-944. [DOI] [PMC free article] [PubMed]
- Tibuakuu M., Kamimura D., Kianoush S., DeFilippis A.P., Al Rifai M., Reynolds L.M. The association between cigarette smoking and inflammation: The genetic epidemiology network of arteriopathy (GENOA) study. PLoS One. 2017;12 doi: 10.1371/journal.pone.0184914. [DOI] [PMC free article] [PubMed] [Google Scholar]; Tibuakuu, M., Kamimura, D., Kianoush, S., DeFilippis, A.P., Al Rifai, M., … & Blaha, M.J. (2017). The association between cigarette smoking and inflammation: the Genetic Epidemiology Network of Arteriopathy (GENOA) study. PLoS One, 12, e0184914. [DOI] [PMC free article] [PubMed]
- Tracy R.P., Psaty B.M., Macy E., Bovill E.G., Cushman M., Cornell E.S. Lifetime smoking exposure affects the association of C-reactive protein with cardiovascular disease risk factors and subclinical disease in healthy elderly subjects. Arteriosclerosis, Thrombosis, and Vascular Biology. 1997;17(10):2167–2176. doi: 10.1161/01.atv.17.10.2167. [DOI] [PubMed] [Google Scholar]; Tracy, R. P., Psaty, B. M., Macy, E., Bovill, E. G., Cushman, M., Cornell, E. S., & Kuller, L. H. (1997). Lifetime smoking exposure affects the association of C-reactive protein with cardiovascular disease risk factors and subclinical disease in healthy elderly subjects. Arteriosclerosis, Thrombosis, and Vascular Biology, 17(10), 2167-2176. [DOI] [PubMed]
- Turner R.J., Noh S. Class and psychological vulnerability among women: The significance of social support and personal control. Journal of Health and Social Behavior. 1983:2–15. [PubMed] [Google Scholar]; Turner, R. J., & Noh, S. (1983). Class and psychological vulnerability among women: The significance of social support and personal control. Journal Of Health And Social Behavior, 2-15. [PubMed]
- Wheaton B. The sociogenesis of psychological disorder: An attributional theory. Journal of Health and Social Behavior. 1980:100–124. [PubMed] [Google Scholar]; Wheaton, B. (1980). The sociogenesis of psychological disorder: An attributional theory. Journal Of Health And Social Behavior, 100-124. [PubMed]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]; Williams, D.R., & Mohammed, S.A. (2009). Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine, 32, 20. [DOI] [PMC free article] [PubMed]
- Williams D.R., Yu Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]; Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. Journal of Health Psychology, 2(3), 335-351. [DOI] [PubMed]
- Winkleby M.A., Jatulis E.E., Frank E., Fortman S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health. 1992;82:816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]; Winkleby, M.A., Jatulis, E.E., Frank, E., & Fortman,, S.P. (1992). Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health, 82, 816-820. [DOI] [PMC free article] [PubMed]
- Zahodne L.B., Sol K., Kraal A.Z. Psychosocial pathways to racial/ethnic inequalities in late-life memory trajectories. Journal of Gerontology: Psychological Sciences. 2019;74(3):409–418. doi: 10.1093/geronb/gbx113. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zahodne L.B., Sol K., and Kraal A.Z., Psychosocial pathways to racial/ethnic inequalities in late-life memory trajectories. Journal of Gerontology: Psychological Sciences 74(3), 2019, 409-418. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.