Abstract
Interpersonal difficulties are common among veterans with posttraumatic stress disorder (PTSD) and are associated with poorer treatment response. Treatment outcomes for PTSD, including relationship functioning, improve when partners are included and engaged in the therapy process. Cognitive-behavioral conjoint therapy for PTSD (CBCT) is a manualized 15-session intervention designed for couples in which one partner has PTSD. CBCT was developed specifically to treat PTSD, engage a partner in treatment, and improve interpersonal functioning. However, recent research suggests that an abbreviated CBCT protocol may lead to sufficient gains in PTSD and relationship functioning, and yield lower dropout rates. Likewise, many veterans report a preference for receiving psychological treatments through clinical videoteleconferencing (CVT) rather than traditional face-to-face modalities that require travel to VA clinics. This manuscript describes the development and implementation of a novel randomized controlled trial (RCT) that examines the efficacy of an abbreviated 8-session version of CBCT (“brief CBCT,” or B-CBCT), and compares the efficacy of this intervention delivered via CVT to traditional in-person platforms. Veterans and their partners were randomized to receive B-CBCT in a traditional Veterans Affairs office-based setting (B-CBCT-Office), CBCT through CVT with the veteran and partner at home (B-CBCT-Home), or an in office-delivered, couple-based psychoeducation control condition (PTSD Family Education). This study is the first RCT designed to investigate the delivery of B-CBCT specifically to veterans with PTSD and their partners, as well as to examine the delivery of B-CBCT over a CVT modality; findings could increase access to care to veterans with PTSD and their partners.
Keywords: Cognitive behavioral conjoint therapy, Videoconferencing, Veterans, Home-based care, Couple therapy, Randomized controlled trial
1. Introduction
Approximately 5%–20% of recent veterans have posttraumatic stress disorder (PTSD); the lifetime prevalence among Vietnam era veterans is 17% [1]. PTSD is associated with other psychological problems [2], unemployment [3], and suicidality [4]. Relationship problems associated with PTSD include poor intimate relationship adjustment, parenting problems, intrafamilial violence, and separation/divorce [[5], [6], [7]]. Somatic symptoms, anxiety, insomnia, depression, and low partner self-esteem are also associated with poorer relationship functioning [8].
PTSD treatment outcomes are enhanced when both partners engage in therapy [8,9]. Cognitive-behavioral conjoint therapy for PTSD (CBCT [10]; is a manualized 15-session treatment for couples in which one partner has PTSD, and simultaneously reduces PTSD symptoms and enhances relationship functioning. Preliminary trials of CBCT support its efficacy in veteran and community samples [11].
Couples often encounter obstacles to receiving care, including agency-level barriers (e.g., few rural providers [12]; client-level barriers (e.g., transportation, child care, fear of stigmatization), and PTSD-specific obstacles (e.g., avoidance; [[13], [14], [15]]. Clinical videoteleconferencing (CVT) provides a safe, effective, and cost-efficient way of delivering evidence-based treatments remotely (e.g., Refs. [[16], [17], [18]]. Studies of CVT delivered clinic-to-clinic demonstrate reductions in some barriers to care. Extending CVT to include home-based service delivery, where patients remain at home and connect to clinicians at their office, could address remaining impediments. However, more research is needed on the effectiveness of home-based CVT for couples [19]. This study will address this gap.
In the pilot phase of this study, two-thirds of couples dropped out around session seven. This is consistent with data from the CBCT dissemination within the Veteran's Health Administration (S.Glynn, personal communication, July 2018). Moreover, studies of the first eight sessions of CBCT yielded significant pre-to post-treatment reductions in PTSD with large effect sizes (g = 1.07; [20,21]. A rigorous evaluation of the efficacy, acceptability, and feasibility of a briefer version of CBCT (B-CBCT) for veteran couples is needed to establish its efficacy and effectiveness.
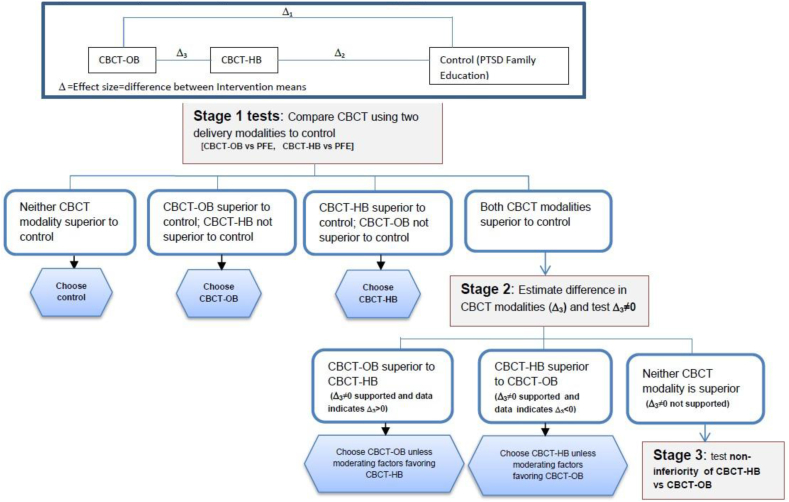
The primary aim of this 4-year RCT is to evaluate the superiority of an 8-session version of CBCT, B-CBCT, delivered via two modalities (B-CBCT-OB and B-CBCT-HB) compared with PFE (Fig. 1). The primary hypothesis is that both CBCT modalities will yield significantly greater reductions in PTSD symptoms, couples' relationship distress, and functional impairment when compared with PFE. The CBCT modalities are compared to the control condition on a range of secondary outcomes, including PTSD diagnosis, patient-rated PTSD symptoms, depression, anger, and couples' conflict ratings. The second aim of this study is to compare results from the B-CBCT-HB and B-CBCT-OB conditions on the same three primary outcomes of PTSD symptoms, couples’ relationship distress, and functional impairment. We hypothesize that B-CBCT-HB will be non-significantly different from B-CBCT-OB (see Fig. 1, Stage 2 tests). The third aim of this study is to compare engagement and process variables among the three conditions. Our tertiary hypothesis is that therapy process outcomes, such as enrolment, therapeutic alliance, and treatment satisfaction, will be significantly higher in B-CBCT-HB compared to the two office-based conditions, and dropout will be lower in B-CBCT-HB compared to the two office-based conditions. We expect the relationship between these process variables and B-CBCT-HB to be stronger than in the other conditions because there are fewer barriers and stressors involved in obtaining home-based treatment (e.g., not needing to travel, wait in a waiting room, coordination of schedules among all parties).
Fig. 1.
Study design diagram and hypothesis testing algorithm.
2. Method
2.1. Study design
This randomized controlled trial (RCT) compares B-CBCT delivered via traditional office-based (B-CBCT-OB) and home-based CVT (B-CBCT-HB) modalities to an office-based 8-session couple-based psychoeducation control condition (PTSD Family Education; PFE; [22]). The primary analyses compare each B-CBCT modality with the control condition: B-CBCT-OB vs. PFE control and B-CBCT-HB vs. PFE control (Stage 1 analyses in Fig. 1). These comparisons are considered primary in the sense that establishing superiority of each modality to control is a necessary condition before consideration of each modality's relationship to each other. Should both B-CBCT modalities be superior to PFE, the outcomes obtained via the two CBCT modalities will be compared to determine if they are not statistically different. Progression to Stage 2 testing (comparison of the two CBCT modalities) will occur only if Stage 1 analyses show that both modalities are superior to control; progression to Stage 3 (future non-inferiority testing between the two B-CBCT modalities) occurs only if no statistically significant differences are found in Stage 2.
A dedicated non-inferiority trial comparing B-CBCT-OB to B-CBCT-HB was ruled out because, at study conception, there was only one RCT that had established CBCT's superiority over a waiting list condition [21]. No RCTs had examined the efficacy of CBCT in a veteran population or examined a B-CBCT protocol, which is a necessary step for establishing an acceptable non-inferiority margin (i.e., delta). Results of this study will guide future B-CBCT non-inferiority studies (Stage 3 analysis in Fig. 1) by formally testing the superiority of B-CBCT to a control, and by providing an estimate of the observed difference between B-CBCT delivery modalities (Stage 3).
2.2. Participants and recruitment
Participating couples (N = 180) at a US Department of Veterans’ Affairs (VA)-based clinical site in San Diego are randomly assigned to one of three treatment arms (B-CBCT-OB, B-CBCT-HB or PFE) and assessed at five time points: pre-treatment, mid-treatment, post-treatment, 3-months post-treatment, and 6-months post-treatment. To be included in the study, dyads must include a veteran (age 18 or older) with a current PTSD diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; [23], with symptoms present for at least 3 months (to allow for potential natural recovery assessed by the Clinician-Administered PTSD Scale-5; CAPS-5; [24], and an intimate partner (age 18 or older, any gender, and any sexual orientation) who is willing to participate in the intervention. If on psychiatric medication, the veteran must be on a stable regimen for at least 2 months. Both members of the couple must be willing to: (1) be randomized to any of the three treatment conditions, (2) have assessment and treatment sessions audio-recorded, (3) not receive other individual psychotherapy for PTSD or conjoint psychotherapy during the treatment portion of the study. Exclusion criteria in either member of the dyad include: (1) current substance use disorder (past 3 months) as assessed by the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, De la Fuente, & Grant, 1993) and Drug Abuse Screening Test (DAST [25]; (2) current uncontrolled psychotic disorder; (3) imminent suicidality or homicidality; (4) any severe cognitive impairment (5) probable partner PTSD (i.e., ≥33 on the PCL-5); or (6) any perpetration of severe physical or sexual relationship aggression in the past year, including fear and intimidation (as assessed by the Revised Conflict Tactics Scale [CTS-2-S [26]], the Extended-Hurt, Insult, Threaten, Scream [E-HITS [27]], item 6 of the Couple Questionnaire [ [28]], and two items assessing current and past fear and/or intimidation of their partner). Participants who do not meet study criteria are offered referrals to alternate services, as well as assistance in contacting the referral sites as needed.
A sample of 180 veterans eligible to receive services from the VA San Diego Healthcare System (VASDHS) is being recruited through multiple clinics, including the Family Mental Health Program (FMHP), the PTSD Clinic, and Primary Care Mental Health Clinic. Participants are also recruited from other non-VA clinics providing services to veterans, including Department of Defense (DoD) and community agencies (e.g., Vet Centers, university counseling centers), the VA electronic medical records database, and self-referrals through advertisement, such as posting materials (e.g., pull-tab flyers) in strategic community locations.
2.3. Assessment
A brief phone screen is administered to determine preliminary eligibility at the initial contact with each potential participant. Individuals are given a comprehensive overview of the study, including discussing treatment modalities and screening for inclusion/exclusion criteria. Based on initial eligibility review, both members of the couple are invited to the VASDHS site to complete informed consent procedures and a baseline assessment interview designed to gather background information (e.g., trauma history, prior treatment history) and to screen for psychiatric disorders and intimate partner violence. A master's or doctoral-level clinician administers the CAPS-5 to the PTSD-positive screened veteran. All interview assessments are audio-recorded for fidelity purposes. Couples are assessed at: (1) baseline, (2) midpoint of treatment, (3) immediately post-treatment, (4) 3-months post-treatment, and (5) 6-months post-treatment. Participants also complete weekly measures of PTSD severity, relationship satisfaction, and intimate partner violence. All assessment sessions are conducted on site at the VASDHS. A complete list of measures and the assessment schedule are detailed in Table 1.
Table 1.
Assessment measures.
| Measures | Baseline | Mid-Txt | Post-Txt | 3M Post-Txt | 6M Post-Txt | Veteran | Partner | Interview (I) or Self-Report (SR) |
|---|---|---|---|---|---|---|---|---|
| Adverse Childhood Experiences (ACE [29]; | X | X | X | SR | ||||
| Alabama Parenting Questionnaire (APQ-9 [30]; | X | X | X | X | X | X | X | SR |
| Alcohol Use Disorders Identification Test (AUDIT [31]; | X | X | X | SR | ||||
| Beck Depression Inventory (BDI-II [32]; | X | X | X | X | X | X | X | SR |
| Beck Scale for Suicidal Ideation (BSS [33]; | X | X | X | X | X | X | SR | |
| Changes in Sexual Functioning Questionnaire-Male/Female Versions (CSFQ-M/F [34]; | X | X | X | X | X | X | X | SR |
| Client Satisfaction Questionnaire-8 (CSQ-8 [35]; | X | X | X | SR | ||||
| Clinical Administered PTSD Scale for DSM-5 (CAPS-5 [24]; | X | X | X | X | X | I | ||
| Collateral PTSD Checklist for DSM-5 Last Month (PCL-5 [24]; modified to have the partner rate the veteran's symptoms | X | X | X | X | X | X | SR | |
| Conflict Tactics Scale-Short Form (CTS-2-S [26]; | X | X | X | X | X | X | X | I/SR |
| Couples Satisfaction Index (CSI-32 [36]; | X | X | X | X | X | X | X | SR |
| Demographics (developed by study team) | X | X | X | I | ||||
| Drug Abuse Screening Test (DAST-10 [25]; | X | X | X | SR | ||||
| Experiences in Close Relationships-Revised (ECR-R [37]; | X | X | X | X | X | X | SR | |
| Insomnia Severity Index (ISI [38]; | X | X | X | X | X | X | X | SR |
| Intimate Partner Violence Assessment-Extended (IPV-E [28]; modified by the study team to include additional items) | X | X | X | SR | ||||
| Intimate Partner Violence Assessment-Three Items (IPV-3 [28]; | X | X | X | X | X | X | I | |
| Intimate Partner Violence Screening Tool-Extended (E-HITS [27]; | X | X | X | SR | ||||
| Inventory of Psychosocial Functioning-Brief (B-IPF [39]; | X | X | X | X | X | X | X | SR |
| Life Events Checklist for DSM-5 (LEC-5 [24]; | X | X | X | I | ||||
| Life Events & Treatment Information Questionnaire (LETI; developed by study team) | X | X | X | X | X | I | ||
| Posttraumatic Cognitions Inventory-9 (PTCI-9; Wells et al., 2017) | X | X | X | X | X | X | SR | |
| Posttraumatic Cognitions Inventory-Full (PTCI [40]; | X | X | SR | |||||
| PRIME Screen-Revised (PS-R [41]; | X | X | X | X | X | X | SR | |
| PTSD Checklist for DSM-5 (PCL-5 [24]; | X | X | X | X | X | X | X | SR/I |
| Significant Others' Response to Trauma Scale (SORTS [42]; | X | X | X | X | X | SR | ||
| State-Trait Anger Expression Inventory-2 (STAXI-2 [43]; | X | X | X | X | X | X | X | SR |
| Telehealth Satisfaction [44]; p.7) | X | X | X | X | X | X | SR | |
| Treatment Preferences (developed by study team) | X | X | SR |
To minimize the risk of bias, independent evaluators (IE) blind to participants’ study condition are trained to administer the CAPS-5 to fidelity via practice interviews until a minimum interrater reliability rating of 80% is achieved with the original assessors. CAPS-5 reliability is monitored through weekly meetings in an ongoing fashion to prevent drift. A random selection of 15% of all CAPS-5 interviews is being reviewed for reliability between assessors. The assessment reliability monitors assess adherence to overall assessment procedures and scoring the measure; interrater reliability will be calculated.
2.4. Treatment selection
In-office delivered PFE was chosen as the control intervention for this study because it is a psychoeducation-oriented, couple intervention that contains the essential and non-specific elements of psychotherapy (e.g., therapist interaction, partner-to-veteran interaction), but does not include specific and active ingredients documented to improve PTSD or couple functioning (e.g., skills training). Additionally, providing psychoeducation, such as PFE, to couples requesting therapy is the standard of care within the VA system. Furthermore, PFE was recently used as a comparison condition in a RCT evaluating the Structured Approach Therapy (SAT) for PTSD intervention [45]. Results showed that, although veterans in both the experimental (SAT) and control (PFE) groups demonstrated significant reductions in PTSD post-treatment and at 3-month follow-up, SAT was more efficacious (as evidenced by its greater rates of improvement). An 8-session version of PFE was selected to control for time spent in therapy to be comparable with the 8-session B-CBCT protocol.
3. Treatments
3.1. Brief CBCT-Office-based
CBCT is a manualized couple-based intervention for PTSD designed to simultaneously reduce PTSD symptoms and to enhance relationship functioning [10]. The original therapy consists of 15, 75-min sessions organized into three phases that build upon one another and includes both in- and out-of-session exercises to increase skill acquisition. Phase 1 (sessions 1–2) focuses on the rationale for the therapy and establishing safety within the relationship (e.g., recognizing early warning signs of anger, use of conflict management strategies). Phase 2 (sessions 3–7) focuses on increasing relational satisfaction and undermining avoidance that maintains PTSD and diminishes relationship satisfaction. Couples develop a list of people, places, situations, and feelings that they avoid as a result of PTSD and begin in vivo approach exercises that are assigned in a graduated manner. Special attention is paid to the selection of in vivo approach activities that address behavioral and experiential avoidance, and concurrently double as shared rewarding activities for the couple. Enhanced dyadic communication is used as an antidote to PTSD-related emotional numbing and avoidance, as well as a means of increasing emotional intimacy.
In the original version of CBCT, Phase 3 (sessions 8–15) focuses on examining beliefs that each member of the couple may hold that contribute to PTSD symptoms and relationship problems, culminating with a discussion of the potential for benefit-finding and growth and a review of gains made and challenges expected in the future. Given preliminary evidence of the efficacy of phases 1 and 2 of CBCT alone, the current study modified the original 15-session protocol and developed an 8-session CBCT protocol (B-CBCT). A brief version of CBCT may help to increase providers’ uptake of the intervention, decrease dropout, and increase the reach of the intervention to veterans. The modified intervention includes sessions 1–7 from the original protocol and an additional session (8) that reviews gains, consolidates skills learned, and identifies and plans for potential challenges in the future. A structured training procedure and adherence/competence rating form have been developed for both B-CBCT conditions based on the updated 8-session protocol.
3.2. Brief CBCT-Home-based
Home-based CBCT utilizes the same 8-session version of CBCT for PTSD described above (B-CBCT), with additional considerations given to the use of technology in the delivery of the intervention. B-CBCT-HB is delivered to couples via their personal computer or tablet located in a private, quiet setting within the home or their preferred private location. Couples without a video-capable home computer, or one that cannot be located in a private area of the home, are provided with an Android-compatible or iOS tablet. Prior to session 1, study staff or VA computer staff conducts a test call with all couples randomized to receive home-based therapy. To assure patient confidentiality and HIPAA compliance, VA-approved CVT software is utilized. The most recent VA Guidance for Home-Based Telemental Health Standard Operating Procedures [46] is used in order to best implement CBCT via CVT- HB. Descriptive data on the type and amount of assistance required for successful home-based delivery is tracked.
3.3. Office-based PTSD Family Education (PFE)
PFE is a manualized PTSD-focused psychoeducation intervention for couples consisting of eight 90-min couples’ sessions adapted from the Support and Family Education (SAFE) program [47] and the Behavioral Family Therapy (BFT) program [48]. PFE involves educating family members about trauma and other comorbid conditions using didactics, discussion, and written materials. Skills training is not included in PFE and clinicians providing PFE are specifically trained to avoid skills training and other therapeutic interventions beyond psychoeducation. A structured training protocol and a rating form have been developed to assess PFE fidelity and competence.
3.4. Treatment delivery
B-CBCT-OB and PFE are delivered in a traditional office-based setting at the VA; both members of the dyad and the therapist are all present in the therapist's office. In contrast, B-CBCT-HB is delivered by a therapist located in a VA office, with the dyad connecting via CVT from their private location of choice (e.g., their home). In all three conditions, participants receive a complete set of therapy-related materials during the initial baseline assessment. Participants complete weekly session assessments prior to meeting with their therapist to track progress and to assess safety. In the office-based conditions, participants complete paper-and-pencil versions of the weekly measures, whereas home-based participants are contacted by study staff via phone immediately prior to logging into the computer for the therapy appointment to verbally report answers to each self-report questionnaires that they completed. Weekly scores are tracked and the provider has access to assessment data prior to the start of the session, regardless of modality. All treatment sessions across the three conditions are audio-recorded for purposes of assessing fidelity and provision of supervision. In the event of a therapeutic crisis between two sessions (e.g., infidelity, potential dissolution of the relationship, or other unforeseen event), the therapist and couple can collaboratively decide to complete an “ASAP” session to focus on managing the emergent situation. ASAP sessions will be used sparingly and couples are told that no more than two ASAP sessions can occur during the course of the 8-session intervention. Sessions are coded as ASAP sessions, do not replace a manualized session, and are not evaluated as part of the fidelity process. Theses ASAP session will be tracked and reported in the primary outcome paper. Therapy then resumes the following scheduled session and covers the content of the next consecutive session.
3.5. Therapist selection
Treatment is provided by clinicians who have a Master's degree or higher and a minimum of two years of clinical experience. These clinicians are trained to administer both B-CBCT and the PFE protocols, and are assigned to treat couples randomized to each condition in equal numbers based primarily on couples' and therapists' availability. Each therapy requires a two-day intensive workshop led by an expert in the respective treatments. Following the initial workshop, audio-recorded pilot cases were reviewed by expert trainers to ensure that each therapy was delivered with adherence and competence to study protocols. Following completion of pilot cases, therapists who were deemed qualified to provide the therapies began attending weekly group consultation teleconferences to ensure ongoing fidelity to the treatments.
3.6. Treatment fidelity monitoring
Ongoing close supervision (adherence and competence) is closely monitored to ensure that the therapy being delivered adheres to the study protocol. In order to ensure that the treatment is administered in accordance with the respective treatment manual, all sessions in the study are recorded for supervision purposes and for possible selection for fidelity rating. In addition to weekly consultation to assure ongoing treatment fidelity, 20% of available participant IDs will be randomly selected for review by CBCT and PFE experts in order to evaluate fidelity, with equal numbers of each treatment arm evaluated. In addition 10% of the recordings selected for treatment fidelity monitoring will be randomly selected for double rating to determine inter-rater reliability (kappa) for treatment adherence and competence.
3.7. Planned statistical analyses
3.7.1. Preliminary analyses
Preliminary analyses will examine distributional characteristics of study variables and provide a description of the study sample and allow for assessment of randomization. Demographic, baseline clinical characteristics of the individual veteran and/or couple dyad, and other putative prognostic variables (e.g., diagnostic profile, health functioning) will be compared for imbalance across the treatment groups using analysis of variance (or a nonparametric equivalent) for continuous variables and chi-square tests for categorical variables. If, despite randomization, significant group differences at baseline are identified, those variables will be included as covariates in subsequent analyses.
3.7.2. Power analysis
The primary comparisons in which each active treatment is compared to control involve directional hypotheses with two multiple comparisons (CBCT-OB superior to PFE, CBCT-HB superior to PFE). Assuming four post-randomization measurement time points, level of significance α = 0.05, one-tailed comparison adjusted for multiple comparisons, correlation between pairs of measurements within participants (interclass correlation) no larger than ρ = 0.5, we estimated that with 48 couples per group (total n = 144), we will have 80%–85% power to detect a standardized effect size of 0.45–0.48 SD (i.e., Cohen's d effect size measured in units of standard deviation). Based on data from our previous studies with similar populations, we estimate the SD of CAPS scores to be 20, yielding a CAPS raw score intervention difference that can be detected of 9.0–9.7 units for individual veteran analyses and 7.6–8.1 for couple-based analyses. The IPF total and scale scores also have SD of approximately 20, yielding same power estimates as for CAPS scores. To compare relationship distress outcomes for the dyad, we estimate 80%–85% power to detect a 0.38–0.41 SD difference between active treatment and control group means. The final sample size estimate was inflated by 20%–180 couples (60 per group) to account for the attrition and the dilution effect of ITT analyses.
3.7.2.1. Analyses for efficacy outcomes (Hypothesis 1)
Longitudinal trajectories of outcomes from baseline to mid-treatment, post-treatment, 3-month, and 6-monh follow-up time points will be compared using multivariable, multilevel generalized linear mixed models (GLMM), which accommodate a wide range of distributional assumptions, including continuous, categorical/dichotomous, ordinal, and count predictors. In addition, GLMM allow for missing and multilevel data, such as possible cluster effects due to correlations among repeated measures, correlation within couples, and correlation between participants within therapists, through inclusion of random effects in the model [49].
The primary efficacy outcome variables are: (1) clinician-rated PTSD symptoms (CAPS-5 severity scores), (2) relationship distress (CSI; [36], and (3) functional impairment (B-IPF; [39]. Secondary variables include PTSD diagnostic status (CAPS-5), self-reported PTSD symptoms (PCL-5; Blake et al., 2013), depression scores (BDI-II; [32], anger (STAXI-2; [43], and relationship conflict (CTS-2-S; [26]. Each of the primary and secondary outcome measures will be examined separately in a series of multilevel models. Each model will examine the predictive value of the primary variable of interest: (1) time (fixed effects), (2) treatment group (fixed effects), and (3) the cross-level interaction of time*treatment group (fixed effects). Baseline scores on the dependent measure will also be included as a model covariate, to control for their effect. For couple-based outcomes (e.g., CSI scores), between-dyad, within-dyad, and mixed variables will be coded in the model as described by Ref. [50].
For Stage 1 analyses addressing the primary hypothesis, pairwise unadjusted (or covariate-adjusted, if necessary) differences in least squares means for each outcome variable will be compared at mid-treatment, post-treatment, and at the 3- and 6-month follow-up time points using appropriate model contrasts (i.e., CBCT-OB vs. PFE and CBCT-HB vs. PFE). Next, in Stage 2 analyses addressing the secondary hypothesis (), unadjusted and least squares adjusted means from the GLMM contrast comparisons, along with corresponding 95% CIs, will provide estimates of the magnitude (effect sizes), direction, and statistical significance of differences in outcome measures for CBCT-OB compared to CBCT-HB. Progression to a future fully powered non-inferiority trial (Stage 3, Fig. 1) occurs only if both CBCT delivery modalities are superior to the control intervention. In that event, this study provides necessary input information (e.g., variance-covariance and effect size estimates) for the design of the subsequent non-inferiority study. If only one CBCT delivery modality is superior to the control intervention, then the additional test for non-superiority between CBCT arms is not required (see Fig. 1 for additional information). While the study chose three primary outcome measures (i.e., CAPS-5, CSI and B-IPF scores), if there are mixed findings regarding the superiority of the CBCT conditions compared to PFE, the results from based on the CAPS-5 scores will be more heavily weighted in decision-making as the primary focus of the treatment is towards reducing posttraumatic symptoms. To address possible Type I errors due to multiple dependent variables, we specify a priori the primary measures corresponding to the stated a priori hypotheses within the following specified domains: PTSD symptoms, relationship satisfaction and functional impairment.
3.7.2.2. Primary analyses for process outcomes
To address tertiary hypotheses, measures of treatment process outcomes include ease of treatment delivery (as rated by participants and therapists), treatment satisfaction (as measured by the Couples Satisfaction Questionnaire, CSQ), therapeutic alliance (for both participants' and therapists’ Working Alliance Inventory, WAI), safety issues (tracked by clinical team) and general program management issues tracked by the coordinator. Additional measures of feasibility are recruitment (percentage who agree to participate out of number approached), compliance (percentage of session attended, percentage of homework assignments completed), and retention (dropout rate). GLMM will be used to compare the feasibility outcomes between each of the two CBCT delivery modalities at the post-treatment time point. The longitudinal profile of adherence as a dichotomous outcome at each visit (e.g., attended/did not attend a given session) within the active intervention period will also be modeled using GLMM. Ninety-five percent CIs for proportions (within groups) and differences in proportions (between groups) obtained from the GLMM analyses will be used to estimate the dichotomous feasibility outcomes (e.g., proportion of couples who participate to number approached; proportion of couples who dropped out to number who complete treatment). Ninety-five percent CIs on means and differences in means will be used to describe continuous feasibility outcomes. Frequency distributions describing the reasons for noncompliance and discontinuation of study participation will be developed. For secondary analyses using additional outcome variables within a given domain, we will report both unadjusted p-values and adjusted p-values using a Tukey-type correction for multiple outcomes. Further, secondary outcomes and exploratory analyses will be evaluated qualitatively in terms of consistency with primary results and conservatively in terms of statistical significance of results. Sensitivity of study results to adjustment for multiplicity of outcomes will be evaluated.
4. Discussion
This RCT examines the efficacy of an abbreviated couple intervention for PTSD (B-CBCT) delivered in-office versus through a home-based CVT modality against an in-office delivered, psychoeducation-focused active control condition (PFE). It offers several innovations, including the testing of a briefer version of CBCT that is more scalable, the use of strong methodology to examine the efficacy of the CVT modality to deliver couple therapy, and the use of functioning as one of the primary outcomes. The findings of this study could have a major impact on the delivery of PTSD services within the VA system and in the public sector, where brief evidence-based treatments that incorporate family are hard to access.
The study is particularly novel for several reasons. First, the study was developed specifically to address the barriers to treatment engagement and retention that veterans frequently face when trying to obtain psychological care for PTSD. Based on recent research suggesting many veterans are only receiving the first two phases of CBCT in the VA's dissemination project, and large effect sizes for the first two phases of treatment, study staff conducted an evidence-based adaptation and shortened the length of the CBCT protocol - from 15 to 8 sessions - in order to provide a more feasible and practical intervention that may be more appealing to veterans and their partners, as well as more cost-effective.
Second, this study is one of the first to conduct an RCT to examine the efficacy of couple therapy delivered through the CVT modality. Although the efficacy of the CVT modality has been established across a variety of different treatments [51], the vast majority of research on CVT is on individual therapy delivered via office-based CVT; almost no research has been done on the efficacy of couple therapy when delivered via telehealth, particularly home-based telehealth. Although office-based CVT allows veterans to obtain care from their local VA facilities rather than having to travel to a larger hospital, even travel to a local clinic can require significant travel and result in a number of other barriers to care. Veterans are interested in flexible, home-based care with lower travel and time burden [52], and this study examines the efficacy of the couple's intervention delivered via home-based CVT as the dyad remains remain in the comfort and privacy of their own home to receive treatment. The described study will also explore the feasibility and efficacy of the CVT modality's use within the veteran's home, which could reduce travel time and cost to clinics. Further, home-based CVT and the inclusion of a partner in therapy may increase treatment retention and engagement. Findings of this study may establish the clinical utility and efficacy of providing couple-based counseling for PTSD through CVT to veterans and their partners.
Finally, most PTSD treatment studies focus on symptom improvement as the primary outcome metric. However, it is also critically important to examine domains related to life functioning, in addition to symptom improvements, in order to better assess the multidimensional impact of psychosocial interventions. This study incorporates a multi-domain assessment protocol that includes measures of psychological health and psychosocial functioning, and relationship functioning in particular. Although the relationship between PTSD and reduced functioning has long been established [53], the impact of PTSD treatments on quality of life and psychosocial functioning has received far less attention [21,53]; Schnurr et al., 2016; [54]. This study will offer a comprehensive evaluation of the effects of CBCT treatment among veterans with PTSD and their partners across several different domains.
In addition to its novelty, this study has several important strengths that will enhance the impact of the study findings. The study methodology incorporates a control condition (PFE) that will allow for the evaluation of the active components of B-CBCT in comparison to general couple-focused contact and PTSD education. Furthermore, the study is a highly controlled RCT that will allow for testing the efficacy of the brief CBCT protocol and the use of the CVT delivery modality. This well-controlled design will also provide the opportunity to conduct future non-inferiority analyses should the first two aims suggest that there are no significant differences between CVT and in-person treatment modalities. The use of staged analysis within the study data plan will serve to maximize data utility and the impact of the findings. Overall, our phased study design will allow us to address multiple research questions within the same study protocol, establishing a novel time- and cost-effective method of conducting treatment outcome research.
Importantly, these study findings will have direct implications for the treatment of PTSD within healthcare systems. Results will expand the current research on CBCT with respect to its clinical effectiveness. Currently, the VA and the community more generally offers few evidence-based interventions for couple therapy, especially those that target specific clinical symptoms (e.g., PTSD) rather than general relationship functioning. Further examination of the efficacy of CBCT, especially in a shorter, more scalable format, may result in a more expedient adoption of the protocol. This would allow those affected by PTSD to choose this type of therapy should they be interested in a relatively brief intervention for PTSD that includes their partner. This study may also establish the efficacy of a home-based service delivery option and provide information on the feasibility and protocol modifications required for delivering a couple-based intervention over home-based CVT. We hope this information will inform future training and policy decisions. Indeed, this project will be a necessary first step towards broad clinical implementation of evidence-based PTSD couples services, particularly in the home setting via CVT.
There is a broader public health need for brief, highly accessible mental health interventions that are effective and easily implemented throughout different healthcare systems. Individuals with PTSD and their loved ones encounter real-life barriers that prevent them from accessing or fully benefiting from evidence-based interventions. Brief psychological treatments offered in-home via technology may encourage more individuals to seek out, and engage in, mental health services. This may be particularly important for those who live in rural communities, as home-based telehealth provides an opportunity to reduce health care disparities among individuals who are most impacted by barriers to receiving high-quality mental health treatment. Examining and incorporating technology into the mental health system is a public health issue, as the impact of these initiatives will affect all consumers of psychological treatment.
Funding
This work was supported by Award Number 1I01RX002093-01 from the Rehabilitation Research & Development Service of the VA Office of Research and Development.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100369.
Contributor Information
Leslie A. Morland, Email: leslie.morland@va.gov.
Alexandra Macdonald, Email: amacdon1@citadel.edu.
Kathleen M. Grubbs, Email: Kathleen.grubbs@va.gov.
Margaret-Anne Mackintosh, Email: Margaret.mackintosh@va.gov.
Candice M. Monson, Email: candice.monson@psych.ryerson.ca.
Lisa H. Glassman, Email: lisahayley@gmail.com.
Julia Becker, Email: julia.becker.cretu@gmail.com.
Frederic Sautter, Email: fsautter@gmail.com.
Brian Buzzella, Email: brian.buzzella@va.gov.
Elizabeth Wrape, Email: Elizabeth.wrape@va.gov.
Stephanie Y. Wells, Email: Stephanie.wells2@va.gov.
Benjamin M. Rooney, Email: Benjamin.rooney@va.gov.
Shirley Glynn, Email: sglynn@g.ucla.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Marmar C.R., Schlenger W., Henn-Haase C., Qian M., Purchia E., Li M., Corry N., Williams C.S., Ho C.-L., Horesh D., Karstoft K.-I., Shalev A., Kulka R.A. Course of posttraumatic stress disorder 40 years after the Vietnam war: findings from the national Vietnam veterans longitudinal study. JAMA Psychiatry. 2015;72(9):875–881. doi: 10.1001/jamapsychiatry.2015.0803. [DOI] [PubMed] [Google Scholar]
- 2.Elhai J.D., Contractor A.A., Palmieri P.A., Forbes D., Richardson J.D. Exploring the relationship between underlying dimensions of posttraumatic stress disorder and depression in a national, trauma-exposed military sample. J. Affect. Disord. 2011;133(3):477–480. doi: 10.1016/j.jad.2011.04.035. [DOI] [PubMed] [Google Scholar]
- 3.Smith M.W., Schnurr P.P., Rosenheck R.A. Employment outcomes and PTSD symptom severity. Ment. Health Serv. Res. 2005;7(2):89–101. doi: 10.1007/s11020-005-3780-2. https://www.ncbi.nlm.nih.gov/pubmed/15974155 Retrieved from. [DOI] [PubMed] [Google Scholar]
- 4.Jakupcak M., Cook J., Imel Z., Fontana A., Rosenheck R., McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan war veterans. J. Trauma. Stress. 2009;22(4):303–306. doi: 10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- 5.Jordan B.K., Marmar C.R., Fairbank J.A., Schlenger W.E., Kulka R.A., Hough R.L., Weiss D.S. Problems in families of male Vietnam veterans with posttraumatic stress disorder. J. Consult. Clin. Psychol. 1992;60(6):916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- 6.Monson C.M., Taft C.T. PTSD and intimate relationships. PTSD Research Quarterly. 2005;16(4):1–7. https://www.ptsd.va.gov/professional/newsletters/research-quarterly/V16N4.pdf Retrieved from. [Google Scholar]
- 7.Monson C.M., Taft C.T., Fredman S.J. Military-related PTSD and intimate relationships: from description to theory-driven research and intervention development. Clin. Psychol. Rev. 2009;29(8):707–714. doi: 10.1016/j.cpr.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westerink J., Giarratano L. The impact of posttraumatic stress disorder on partners and children of Australian Vietnam veterans. Aust. N. Z. J. Psychiatr. 1999;33(6):841–847. doi: 10.1046/j.1440-1614.1999.00638.x. [DOI] [PubMed] [Google Scholar]
- 9.Ray S.L., Vanstone M. The impact of PTSD on veterans' family relationships: an interpretative phenomenological inquiry. Int. J. Nurs. Stud. 2009;46(6):838–847. doi: 10.1016/j.ijnurstu.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Monson C.M., Fredman S.J. first ed. The Guilford Press; New York, NY: 2012. Cognitive-behavioral Conjoint Therapy for Post Traumatic Stress Disorder: Harnessing the Healing Power of Relationships. [Google Scholar]
- 11.Macdonald A., Pukay-Martin N.D., Wagner A.C., Fredman S.J., Monson C.M. Cognitive-behavioral conjoint therapy for PTSD improves various PTSD symptoms and trauma-related cognitions: results from a randomized controlled trial. J. Fam. Psychol. 2016;30(1):157–162. doi: 10.1037/fam0000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Department of Veterans Affairs . 2012. About the office of rural health.www.ruralhealth.va.gov/about/index.asp Retrieved from. [Google Scholar]
- 13.Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N. Engl. J. Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 14.Seal K.H., Maguen S., Cohen B., Gima K.S., Metzler T.J., Ren L., Bertenthal D., Marmar C.R. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J. Trauma. Stress. 2010;23(1):5–16. doi: 10.1002/jts.20493. [DOI] [PubMed] [Google Scholar]
- 15.Vogt D. Mental health-related beliefs as a barrier to service use for military personnel and veterans: a review. Psychiatr. Serv. 2011;62(2):135–142. doi: 10.1176/ps.62.2.pss6202_0135. [DOI] [PubMed] [Google Scholar]
- 16.Morland L.A., Frueh B.C., Pierce K., Miyahira S. PTSD and telemental health: updates and future directions. PTSD Clinical Quarterly. 2003;16(12):1–5. https://www.ptsd.va.gov/professional/treatment/overview/ptsd-telemental.asp Retrieved from. [Google Scholar]
- 17.Morland L.A., Greene C.J., Rosen C.S., Foy D., Reilly P., Shore J., He Q., Frueh B.C. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J. Clin. Psychiatry. 2010;71(7):855–863. doi: 10.4088/JCP.09m05604blu. [DOI] [PubMed] [Google Scholar]
- 18.Yuen E.K., Gros D.F., Price M., Zeigler S., Tuerk P.W., Foa E.B., Acierno R. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J. Clin. Psychol. 2015;71(6):500–512. doi: 10.1002/jclp.22168. [DOI] [PubMed] [Google Scholar]
- 19.Mohr D.C., Burns M.N., Schueller S.M., Clarke G., Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen. Hosp. Psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fredman S.J., Macdonald A., Monson C.M., Rhoades G.K., Dondanville K.A., the Consortium to Alleviate PTSD . 2018. Findings from an Open Trial of Intensive Couple Therapy for PTSD Delivered for Active Duty Military and Veteran Couples. (under review) [Google Scholar]
- 21.Monson C.M., Fredman S.J., Macdonald A., Pukay-Martin N.D., Resick P.A., Schnurr P.P. Effect of cognitive-behavioral couple therapy for PTSD: a randomized controlled trial. J. Am. Med. Assoc. 2012;308(7):700–709. doi: 10.1001/jama.2012.9307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sautter F.J., Glynn S.M., Cretu J.B., Senturk D., Vaught A.S. Efficacy of structured approach therapy in reducing PTSD in returning veterans: a randomized clinical trial. Psychol. Serv. 2015;12(3):199–212. doi: 10.1037/ser0000032. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association . fifth ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 24.Weathers F.W., Blake D.D., Schnurr P.P., Kaloupek D.G., Marx B.P., Keane T.M. 2013. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)www.ptsd.va.gov Instrument available from: the National Center for PTSD at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skinner H.A. The drug abuse screening test. Addict. Behav. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 26.Straus M.A., Douglas E.M. A short form of the revised conflict tactics scales and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- 27.Chan C.C., Chan Y.C., Au A., Cheung G.O.C. Reliability and validity of the “Extended-Hurt, Insult, Threaten, Scream”(E-HITS) screening tool in detecting intimate partner violence in hospital emergency departments in Hong Kong. Hong Kong J. Emerg. Med. 2010;17(2):109–117. [Google Scholar]
- 28.Christensen A. University of California; Los Angeles: 2009. Couple Questionnaire. Unpublished Questionnaire. Los Angeles. [Google Scholar]
- 29.Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 30.Elgar F.J., Waschbusch D.A., Dadds M.R., Sigvaldason N. Development and validation of a short form of the Alabama Parenting Questionnaire. J. Child Fam. Stud. 2007;16(2):243–259. [Google Scholar]
- 31.Saunders J.B., Aasland O.G., Babor T.F., De la Fuente J.R., Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 32.Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; San Antonio, TX: 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- 33.Beck A.T., Kovacs M., Weissman A. Assessment of suicidal intention: the scale for suicide ideation. J. Consult. Clin. Psychol. 1979;47:43–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 34.Keller A., McGarvey E.L., Clayton A.H. Reliability and construct validity of the changes in sexual functioning questionnaire short-form (CSFQ-14) J. Sex Marital Ther. 2006;32(1):43–52. doi: 10.1080/00926230500232909. [DOI] [PubMed] [Google Scholar]
- 35.Larsen D.L., Attkisson C.C., Hargreaves W.A., Nguyen T.D. Assessment of client/patient satisfaction: development of a general scale. Eval. Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 36.Funk J.L., Rogge R.D. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index (CSI) J. Fam. Psychol. 2007;21:572–583. doi: 10.1037/0893-3200.21.4.572. [DOI] [PubMed] [Google Scholar]
- 37.Fraley R.C., Waller N.G., Brennan K.A. An item-response theory analysis of self-report measures of adult attachment. J. Personal. Soc. Psychol. 2000;78:350–365. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- 38.Morin C.M., Belleville G., Bélanger L., Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kleiman S.E., Bovin M.J., Black S.K., Rodriguez P., *Brown L.G., *Brown M.E., Lunney C.A., Weathers F.W., Schnurr P.P., Spira J., Keane T.M., Marx B.P. Psychological Services; 2019. Psychometric Properties of a Brief Measure of Posttraumatic Stress Disorder-Related Impairment: the Brief Inventory of Psychosocial Functioning. (in press) [DOI] [PubMed] [Google Scholar]
- 40.Foa E.B., Ehlers A., Clark D.M., Tolin D.F., Orsillo S.M. The posttraumatic cognitions inventory (PTCI): development and validation. Psychol. Assess. 1999;11(3):303. [Google Scholar]
- 41.Kobayashi H., Nemoto T., Koshikawa H., Osono Y., Yamazawa R., Murakami M., Mizuno M. A self-reported instrument for prodromal symptoms of psychosis: testing the clinical validity of the PRIME Screen—revised (PS-R) in a Japanese population. Schizophr. Res. 2008;106(2–3):356–362. doi: 10.1016/j.schres.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 42.Fredman S.J., Vorstenbosch V., Wagner A.C., Macdonald A., Monson C.M. Partner accommodation in posttraumatic stress disorder: initial testing of the significant others' responses to trauma scale (SORTS) J. Anxiety Disord. 2014;28(4):372–381. doi: 10.1016/j.janxdis.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Speilberger C.D. Psychological Assessment Resources; Odessa, FL: 1988. Manual for the State Trait Anger Expression Inventory. [Google Scholar]
- 44.Anderson C. October). Quality and performance: results of the FY10 CVT satisfaction survey pilot. VHA Telehealth Quarterly: Quarterly Newsletter of VHA Office of Telehealth Services. 2010;10(1):7. [Google Scholar]
- 45.Sautter F.J., Glynn S.M., Arseneau J.R., Cretu J.B., Yufik T. Structured approach therapy for PTSD in returning veterans and their partners: pilot findings. Psychological Trauma. 2014;6(1):S66–S72. [Google Scholar]
- 46.Shore P. VA Northwest Health Network Office; Portland, OR: 2011. Home-based Telemental Health (HBTMH) Standard Operating Procedures Manual. (VISN 20) [Google Scholar]
- 47.Sherman M.D. The Support and Family Education (SAFE) program: mental health facts for families. Psychiatr. Serv. 2003;54(1):35–37. doi: 10.1176/appi.ps.54.1.35. [DOI] [PubMed] [Google Scholar]
- 48.Mueser K.T., Glynn S.M. Allyn & Bacon; Needham Heights, MA: 1995. Behavioral Family Therapy for Psychiatric Disorders. [Google Scholar]
- 49.Hedeker D., Gibbons R.D. John Wiley & Sons; Hoboken, NJ: 2006. Longitudinal Data Analysis. [Google Scholar]
- 50.Campbell L., Kashy D.A. Estimating actor, partner, and interaction effects for dyadic data using PROC MIXED and HLM: a user–friendly guide. Pers. Relat. 2002;9(3):327–342. [Google Scholar]
- 51.Backhaus A., Agha Z., Maglione M.L., Repp A., Ross B., Zuest D., Thorp S.R. Videoconferencing psychotherapy: a systematic review. Psychol. Serv. 2012;9(2):111–131. doi: 10.1037/a0027924. [DOI] [PubMed] [Google Scholar]
- 52.Whealin J.M., King L., Shore P., Spira J.L. Diverse veterans' pre- and post-intervention perceptions of home telemental health for posttraumatic stress disorder delivered via tablet. Int. J. Psychiatry Med. 2017;52(1):3–20. doi: 10.1177/0091217417703291. [DOI] [PubMed] [Google Scholar]
- 53.Schnurr P.P., Hayes A.F., Lunney C.A., McFall M., Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. J. Consult. Clin. Psychol. 2006;74(4):707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- 54.Shnaider P., Vorstenbosch V., Macdonald A., Wells S.Y., Monson C.M., Resick P.A. Associations between functioning and PTSD symptom clusters in a dismantling trial of cognitive processing therapy in female interpersonal violence survivors. J. Trauma. Stress. 2014;27(5):526–534. doi: 10.1002/jts.21954. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.