Abstract
Background
Transcranial electrical stimulation is a promising technique to facilitate behavioural improvements in neurological and psychiatric populations. Recently there has been interest in remote delivery of stimulation within a participant’s home.
Objective
The purpose of this review is to identify strategies employed to implement and monitor in-home stimulation and identify whether these approaches are associated with protocol adherence, adverse events and patient perspectives.
Methods
MEDLINE, Embase Classic + Embase, Emcare and PsycINFO databases and clinical trial registries were searched to identify studies which reported primary data for any type of transcranial electrical stimulation applied as a home-based treatment.
Results
Nineteen published studies from unique trials and ten on-going trials were included. For published data, internal validity was assessed with the Cochrane risk of bias assessment tool with most studies exhibiting a high level of bias possibly reflecting the preliminary nature of current work. Several different strategies were employed to prepare the participant, deliver and monitor the in-home transcranial electrical stimulation. The use of real time videoconferencing to monitor in-home transcranial electrical stimulation appeared to be associated with higher levels of compliance with the stimulation protocol and greater participant satisfaction. There were no severe adverse events associated with in-home stimulation.
Conclusions
Delivery of transcranial electrical stimulation within a person’s home offers many potential benefits and appears acceptable and safe provided appropriate preparation and monitoring is provided. Future in-home transcranial electrical stimulation studies should use real-time videoconferencing as one of the approaches to facilitate delivery of this potentially beneficial treatment.
Keywords: Non-invasive brain stimulation, Transcranial direct current stimulation, Rehabilitation, Home therapy, Remote monitoring, Telemedicine
Introduction
Transcranial electrical stimulation (tES) is a technique used to modulate cortical function and human behaviour. It involves weak current passing through the scalp via surface electrodes to stimulate the underlying brain. A common type of tES is transcranial direct current stimulation (tDCS). Several studies have demonstrated tDCS is capable of modulating cortical function, depending on the direction of current flow [1–3]. When the anode is positioned over a cortical region, the current causes depolarisation of the neuronal cells, increasing spontaneous firing rates [4]. Conversely, positioning the cathode over the target cortical region causes hyperpolarisation and a decrease in spontaneous firing rates [4]. This modulation of cortical activity can be observed beyond the period of stimulation and is thought to be mediated by mechanisms which resemble long term potentiation and depression [5]. Along similar lines, transcranial alternating current stimulation (tACS) and transcranial random noise stimulation (tRNS) are also forms of tES. Both tACS and tRNS are thought to interact with ongoing oscillatory cortical rhythms in a frequency dependent manner to influence human behaviour [6–8].
The ability of tES to selectively modulate cortical activity offers a promising tool to induce behavioural change. Indeed, several studies have demonstrated that tES may be a favourable approach to reduce impairment following stroke [9], improve symptoms of neglect [10], or reduce symptoms of depression [11]. While these results appear promising, there remains debate around technical aspects of stimulation along with individual participant characteristics that may influence the reliability of a stimulation response [12–22]. However, current evidence does suggest that effects of stimulation may be cumulative, with greater behavioural improvements observed following repeated stimulation sessions [20]. Furthermore, tES has shown potential as a tool for maintenance stimulation, with potential relapses of depression managed by stimulation which continued over several months [23, 24]. Therefore, it may be that repeated stimulation sessions will become a hallmark of future clinical and research trials aiming to improve behavioural outcomes. This would require participants to attend frequent treatment sessions applied over a number of days, months or years. Given that many participants who are likely to benefit from stimulation are those with higher levels of motor or cognitive impairment, the requirement to travel regularly for treatment may present a barrier, limiting potential clinical utility or ability to recruit suitable research participants [25]. In addition, regular daily treatments would also hinder those who travel from remote destinations to receive this potentially beneficial neuromodulation. Therefore, there is a requirement to consider approaches to safely and effectively deliver stimulation away from the traditional locations of research departments or clinical facilities.
One benefit of tES over other forms of non-invasive brain stimulation, such as repetitive transcranial magnetic stimulation, is the ability to easily transport the required equipment. This opportunity may allow for stimulation to be delivered in a participant’s home, which could represent the mode of delivery for future clinical applications. However, it may be unreasonable to expect that a participant would be capable of managing delivery of tES alone and would likely require some form of training and/or monitoring [25]. Although tES is considered relatively safe [26], stimulation should be delivered within established guidelines to avoid adverse events [27]. Inappropriate delivery of stimulation could result in neural damage, detrimental behavioural effects, irritation, burns or lesions of the skin [28–33]. Therefore, in order to deliver stimulation safely to the appropriate cortical region, it is likely that in-home stimulation may require some form of monitoring [25].
It is currently unclear what the best approach is to implement and monitor in-home tES. An early paper proposed several guidelines to perform in home tES [34]. However, these guidelines were not based on evidence from published clinical trials as there were none available at the time of publication. One recent systematic review sought to discuss current work in this area and highlighted the need for further research to investigate safety, technical monitoring and assessment of efficacy [35]. Given the recent, and growing, interest in home-based brain stimulation, we felt it was now pertinent to conduct a review to specifically identify strategies employed to implement and monitor the use of in-home tES in neurological and psychiatric populations. The secondary questions were to report protocol adherence, adverse events and patient perspectives of in-home tES. Understanding optimal treatment fidelity for in-home brain stimulation will be instrumental to achieving higher levels of tES useability and acceptance within a participant’s home.
Methods
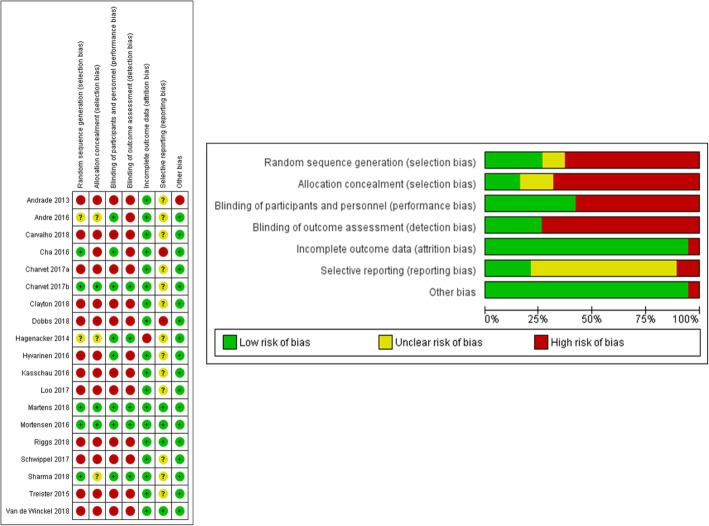
This systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Fig. 1) and is registered with the International Prospective Register of Systematic Reviews (PROSPERO Registration number CRD42018091960). The literature search of studies that involve in-home tES was performed in the following databases; MEDLINE (1946 to February 2019), Embase Classic + Embase (1947 to February 2019), Emcare (1995 to February 2019) and PsycINFO (1806 to February 2019). In addition, trial registries (clinicaltrials.gov, anzctr.org.au and who.int/ictrp/en/) were searched to identify current in-home tES studies. The search was carried out in February 2019 using combinations of keywords relating to in-home tES (search strategy available on PROSPERO, CRD42018091960).
Fig. 1.
PRISMA flow diagram of study inclusion for this systematic review
Studies were included if (i) they presented primary data using any type of tES including tDCS, tRNS or tACS as the treatment approach regardless of types of montage as well as whether it was applied with or without additional therapy (ii) the tES treatment was carried out as a home-based treatment (iii) the study involved humans of any age with neurological or psychiatric conditions which included, but was not limited to, stroke, Parkinson’s disease, traumatic brain injury and depression (iv) the study reported on compliance with treatment protocol, adverse events or participant satisfaction with home stimulation (v) the type of study was either a randomised controlled trial, randomised cross-over trial, observational study, case series, or qualitative study, and (vi) the study was published or available in the English language. All other studies that did not fulfil the inclusion criteria were excluded.
The review process was carried out in three steps. First, one reviewer (N.S.) screened titles and abstracts according to eligibility criteria and excluded studies which were obviously not related to the search criteria. Second, full text articles were retrieved and screened by two reviewers (B.H. and N.S.) with a third reviewer (S.H.) resolving any discrepancies that arose. The reference lists of included articles were then screened to identify any additional articles that may not have been found during the original search. Third, quality assessment of each included study was carried out using the Cochrane risk of bias assessment [36]. Two reviewers (B.H. and N.S.) assessed bias individually and discrepancies were resolved via discussion. The variables extracted from the included papers were; (1) subject demographics and clinical characteristics (age, gender, sample size, clinical condition(s)), (2) details on strategies to facilitate in-home tES treatment, (3) type of stimulator used, (4) size and positioning of electrodes, (5) parameters of stimulations for in-home sessions (current and duration), (6) monitoring approaches, (7) adverse events, (8) study protocol compliance, which was defined as the percentage of correctly completed stimulation sessions relative to the total number of intended sessions, and (9) perception of patients towards in-home tES treatment. Where required, authors were contacted to obtain additional data. Data were then synthesised using a narrative approach to describe approaches to achieve optimal treatment fidelity. This included strategies employed both prior to, and during, the treatment period to effectively implement in-home tES and approaches to monitor use of in-home tES during the treatment period to ensure it is both effective and safe. Where reported, adverse events, protocol adherence and participant perspectives were also synthesised using a narrative approach and discussed with reference to approaches to implement and monitor in-home tES.
Results
Study description
A total of 957 related studies were identified, with 65 duplicates removed, leaving 892 studies for title and abstract screening. Following title and abstract screening, 48 studies remained and full text articles of those studies were screened for eligibility. Out of these 48 studies, 28 were discarded as 11 studies were found to have the wrong study design (three review articles, one book chapter, six methodological or guideline papers and one protocol paper) and one had the wrong study population. The other 16 studies were considered duplicates as they were conference abstracts related to full text studies already included in the review. Thus, in total, this systematic review included 20 studies. One additional study [37] was excluded from this review as it was identified through communication with the author that the data came from a trial that was already included within the review [38]. As B Dobbs, N Pawlak, M Biagioni, S Agarwal, M Shaw, G Pilloni, M Bikson, A Datta and L Charvet [38] reported all outcomes of interest to this review, it was decided that data would be extracted from this study. As a result, there were 19 studies identified with data from unique trials (Fig. 1).
Description of included studies
All 19 studies are summarised in Table 1. Although the inclusion criteria for this review included several variations of tES, all identified studies used tDCS as the form of brain stimulation, with none using tACS or tRNS. The studies were relatively recent, all being published within the past 5 years (2013–2018), while 84% were published within the last 2 years (2016–2018). Of the included studies, five were identified as randomised controlled trials [39–43], two randomised cross-over trials [44, 45], two observational studies [46, 47], ten case series [38, 48–56].
Table 1.
Descriptions of studies based on sample populations and stimulation parameters
| Study | Study Design and Population | Stimulation Parameters | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Design | Size | Gender | Age (years) | Condition | Type | Target Area | Electrodes | Current | Session | Duration | |
| Andrade 2013 | Case series | 1 | 1F | 25 | Schizophrenia | Zeebeetronics | F3 (Anodal tDCS) | 25cm2 | 1–3 mA | 3 years | 20–30 min |
| Andre 2016 | RCT | 22 | NS | 63–94 | Dementia | NeuroConn | DLPFC (Anodal tDCS) | 35cm2 | 2 mA | 4 sessions | 20 min |
| Carvalho 2018 | Case series | 1 | 1F | 57 | Neuropathic pain | Neuroelectric Starstim | M1 (Anodal tDCS) | 35cm2 | 2 mA | 5 sessions | 20 min |
| Cha 2016 | RCT | 24 | 24F | 52.9 ± 12.2 | MdDS | Transcranial Technologies | DLPFC | 35cm2 | 1 mA | 20 sessions | 20 min |
| Charvet 2017a | Observational | 25 | 21F, 4 M | 51.0 ± 12.7 | MS | Soterix Mini-Clinical Trials | DLPFC (Anodal tDCS) | 35 cm2 | 1.5 mA | 10 sessions | 20 min |
| Charvet 2017b1 | RCT | 27 | 16F, 11 M | 44.2 | MS | Soterix Mini-Clinical Trials | DLPFC (Anodal tDCS) | 25 cm2 | 2 mA | 20 sessions | 20 min |
| Clayton 2018 | Case series | 1 | 1F | 54 | MS, Bipolar | NS | DLPFC (Anodal tDCS) | NS | 2 mA | 40 sessions | 20 min |
| Dobbs 2018 | Case series | 16 | 4F, 12 M | 66.9 ± 5.4 | PD | Soterix Mini-Clinical Trials | DLPFC (Anodal tDCS) | 25cm2 | 2 mA | 10 sessions | 20 min |
| Hagenacker 2014 | RCT - crossover | 17 | 10F, 7 M | 32–82 | Trigeminal neuralgia | Neuronica | M1 (Anodal tDCS) | 16cm2 | 1 mA | 14 sessions | 20 min |
| Hyvarinen 2016 | Observational | 43 | 20F, 23 M | 51 ± 15.4 | Tinnitus | Sooma | Auditory or bifrontal tDCS | 35cm2 | 2 mA | 10 sessions | 20 min |
| Kasschau 2016 | Case series | 20 | 17F, 3 M | 30–69 | MS | tDCS mini-Clinical Trial | DLPFC | 25cm2 | 1.5 mA | 10 sessions | 20 min |
| Loo 2017 | Case series | 10 | NS | NS | Depression | NS | DLPFC | NS | 2 mA | 20 sessions | 30 min |
| Martens 2018 | RCT - crossover | 27 | 8F,19M | 42 ± 14.5 | MCS | CEFALY tDCS | DLPFC | 35cm2 | 2 mA | 20 sessions | 20 min |
| Mortenson 2016 | RCT | 16 | 7F, 9 M | 44–76 | Stroke | NeuroConn | M1 (Anodal tDCS) | 35cm2 | 1.5 mA | 5 sessions | 20 min |
| Riggs 2018 | Case series | 4 | 2F, 2 M | 44–63 | Multiple conditions | Soterix Mini-Clinical Trials | DLPFC/M1 (Anodal tDCS) | 25cm2 | 1–1.5 mA | 10 sessions | 20 min |
| Schwippel 2017 | Case series | 1 | 1 M | 31 | Hallucinations | Neuroconn | Tempoproparietal (Anodal tDCS) | 35cm2 | 2 mA | 400 sessions | 20 min |
| Sharma 2018 | RCT | 12 | NS | 64.7 ± 7.1 | PD | NS | DLPFC | NS | 2 mA | 10 sessions | 20 min |
| Treister 2015 | Case series | 11 | 7F, 4 M | 60.6 ± 16.3 | Neurological pain | NS | M1 (Anodal tDCS) | NS | 1.5 mA | 12 sessions | 20 min |
| Van de Winckel 2018 | Case series | 6 | 3F, 3 M | 61 ± 10 | Stroke | StartSim | M1 bihemispheric | 20cm2 | 1.5 mA | 5 sessions | 20 min |
DLPFC = Dorsolateral prefrontal cortex; F = female; M = male; MCS = Minimally conscious state; MdDS = Mal De Debarquement Syndrome; MS = Multiple sclerosis; M1 = primary motor cortex; NS = not stated; PD = Parkinson’s disease; RCT = Randomised controlled trial; tDCS = transcranial Direct Current Stimulation
1, data only reported for study two
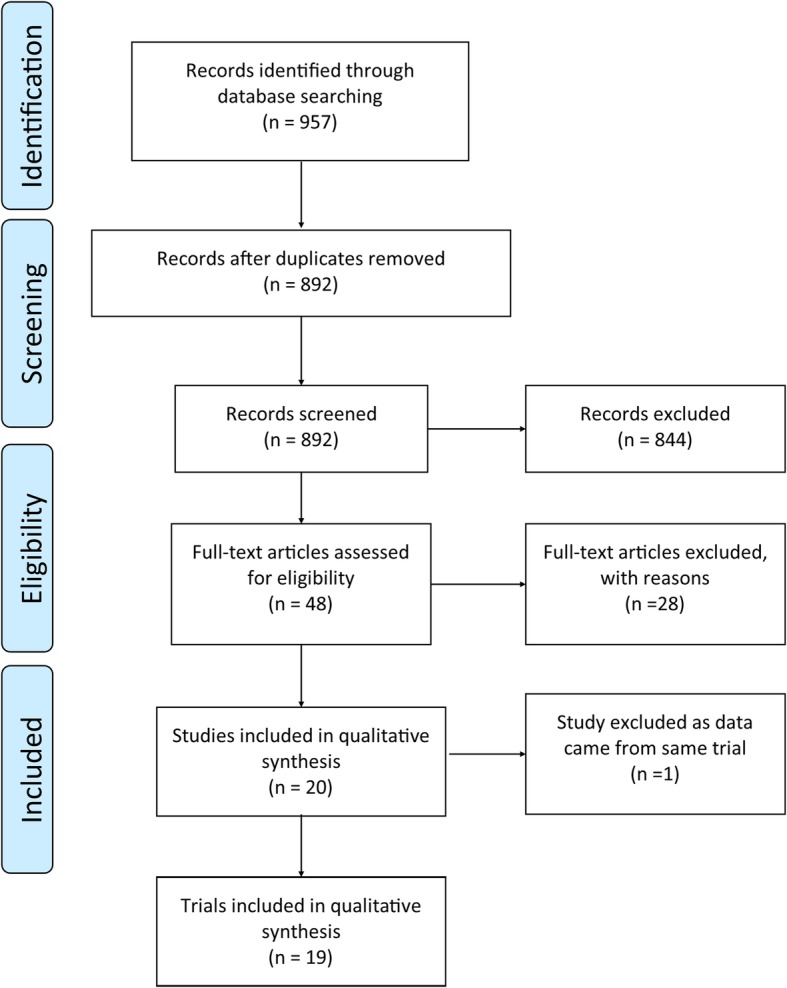
Risk of bias in included studies
Review of internal validity using the Cochrane risk of bias assessment tool in seven domains is summarised in Fig. 2. In keeping with the low level of research design, which likely reflects the preliminary nature of current work, the majority of studies had a high risk of bias. Few studies (26.3%) demonstrated low risk for random sequence generation [39–41, 43, 45], allocation concealment (15.8%) [40, 41, 45], blinding of personnel and participants (42.1%) [39–46] and blinding of outcome assessments (26.3%) [40, 41, 43–45]. However, a large proportion of studies (94.7%) demonstrated low risk of bias for incomplete outcome data, with only one study identified as high risk of bias due to an increased number of participants who withdrew from the study [44]. Selective reporting was generally (68.4%) identified as an unclear level of bias [40, 42–44, 46–49, 51–55], with two studies identified as high risk of bias [38, 39], and one as low risk of bias [41] in this category. One study was identified as high risk of bias under the domain of other sources of bias due to substantial variation in duration and intensity of stimulation based on response to treatment [52]. However, we note that the overall purpose of this study was different compared to all other included studies as it was a maintenance program for symptoms of schizophrenia.
Fig. 2.
Cochrane risk of bias tool was used to assess quality of included studies
Participants’ characteristics and stimulation protocols
There were various patient populations included in this review for in-home tES (Table 1). Four studies were performed with people who had Multiple Sclerosis (MS) [40, 47, 48, 54], two with Parkinson’s disease (PD) [38, 43] and two with stroke [41, 56]. Other populations included tinnitus [46], dementia [42], minimally conscious state [45], Mal de Debarquement syndrome [39], trigeminal neuralgia [44], neuropathic pain [55], depression [49], multimodal hallucinatory perceptions [53], schizophrenia [52], various neurological pain conditions [51] and a case series of four chronically ill patients which included myasthenia gravis, depression, chronic pain and stroke [50].
In-home tES treatment was provided over a wide range of different durations from 4 [42] to 400 sessions [53], with the most common approach to apply in-home tES for 10–20 sessions [38–40, 43–51]. One study did not report the number of treatment sessions which ranged from once to twice daily over a period of 3 years [52]. The duration for each treatment was 20–30 min for all included studies, with the majority applying stimulation at 1-2 mA. Only one study exceeded 2 mA, with stimulation intensity increased up to 3 mA to control symptoms of Schizophrenia [52].
Approaches to achieve optimal treatment fidelity for in-home brain stimulation
Across the 19 included studies, there were a range of strategies used both prior to, and during, the treatment period to implement in-home tES (Table 2). The most common approach was to conduct training sessions prior to beginning in-home tES. This frequently included practicing the placement and positioning of electrodes on the scalp, sponge preparation, starting the stimulator, troubleshooting common problems and provision of training videos [39, 46, 53]. Furthermore, several studies extended the training sessions to include a caregiver, or support person, who was able to assist during the home treatment phase. For some studies, the assistance of a caregiver, or support person, was a requirement for all participants [44, 48, 50, 55], and others specifying it only for those participants with higher disability [38, 40, 47].
Table 2.
Strategies identified to implement in-home tES
| Study | Strategies to implement in-home tES | |||||
|---|---|---|---|---|---|---|
| Training session | Caregiver training | Customised headband | Remote computer access (stimulator set-up) | Home visit | Stimulation delivered by research team | |
| Kasschau 2016 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Riggs 2018 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Dobbs 2018 | ✓ | ✓ | ✓ | ✓ | ||
| Sharma 2018 | ✓ | ✓ | ✓ | ✓ | ||
| Van de Winckel 2018 | ✓ | ✓ | ✓ | ✓ | ||
| Charvet 2017a | ✓ | ✓ | ✓ | ✓ | ||
| Charvet 2017b | ✓ | ✓ | ✓ | ? | ||
| Carvalho 2018 | ✓ | ✓ | ||||
| Hagenacker 2014 | ✓ | ✓ | ||||
| Cha 2016 | ✓ | ✓ | ||||
| Hyvarinen 2016 | ✓ | ✓ | ||||
| Schwippel 2017 | ✓ | |||||
| Treister 2015 | ✓ | |||||
| Loo 2017 | ✓ | |||||
| Mortenson 2016 | ✓ | |||||
| Martens 2018 | ✓ | |||||
| Andrade 2013 | ||||||
| Andre 2016 | ||||||
| Clayton 2018 | ||||||
Note; Andrade 2013, Andre 2016 and Clayton 2018 did not report any strategy to implement in-home tES
✓; Reported as a strategy to implement in-home tES
?; Charvet 2017b reported each participant was provided a laptop that enabled connection to a study technician. It is not stated whether this included remote computer access
During delivery of in-home tES, several monitoring approaches were identified as strategies to achieve optimal treatment fidelity (Table 3). The most common treatment monitoring approach was to use videoconferencing to observe, in real time, the in-home treatment being conducted by the patients or their caregivers [38–40, 43, 47–50, 54–56]. This provided researchers opportunity to visualise tES set-up, correct electrode placement and troubleshoot issues that arose. Monitoring in-home stimulation in this manner may also assist with compliance with the treatment protocol. Five studies which utilised videoconferencing as a method to monitor in-home tES also used a remote desktop access approach for each treatment [38, 43, 47, 48, 50, 56]. This allowed research staff to have strict dose control for the delivery of tES and remotely solve any technology-based issues that arose. Four studies used passive (not in real time) monitoring approaches which included recording use of tES through websites such as Survey Monkey [39] or with self-report treatment diaries [44–46].
Table 3.
Monitoring approaches and protocol compliance of the studies
| Study | Monitoring approaches | Compliance |
|---|---|---|
| Mortenson 2016 | Direct in-person monitoring | 100% |
| Clayton 2018 | Real-time videoconferencing | 100% |
| Carvalho 2018 | Real-time videoconferencing | 100% |
| Van de Winckel 2018 | Real-time videoconferencing Remote administration of tDCS delivery |
100% |
| Riggs 2018 | Real-time videoconferencing Remote administration of tDCS delivery |
100% |
| Dobbs 2018 | Real-time videoconferencing Remote administration of tDCS delivery |
100% |
| Sharma 2018 | Real-time videoconferencing Remote administration of tDCS delivery |
100% |
| Charvet 2017a | Real-time videoconferencing Remote administration of tDCS delivery |
> 96% |
| Cha 2016 | Real-time videoconferencing Daily online-tracking and reporting system |
96% |
| Kasschau 2016 | Real-time videoconferencing Remote administration of tDCS delivery |
96% |
| Charvet 2017b1 | Real-time videoconferencing Remote administration of tDCS delivery |
93% |
| Hyvarinen 2016 | Daily self-report treatment diary | 91% |
| Loo 2017 | Initial sessions real-time videoconferencing Daily phone or email contact |
90% |
| Martens 2018 | Daily self-report abnormalities, questionnaire | 81% |
| Hagenacker 2014 | Daily self-report treatment diary | 76% |
1, data only reported for study two
Protocol compliance
Table 3 shows that most studies reported a high level of compliance with the in-home tES treatment program which was defined as the percentage of correctly completed stimulation sessions relative to the total number of intended sessions. Seven studies had 100% compliance, with three additional studies having 95% compliance or greater and a further three studies reporting 90–95% compliance. These results suggest that it is possible to implement an in-home tES study and obtain an excellent level of compliance. An observation from this review is that studies which provided regular and repeated real-time videoconferencing to monitor each in-home treatment session achieved compliance levels of 93% or greater [38–40, 43, 47, 48, 50, 54–56]. One study delivered in-home tES with research staff attending a participant’s home as opposed to the study participant performing stimulation independently, achieving 100% compliance [41].
The studies which did not use real-time videoconferencing to monitor each in-home treatment session reported different approaches that achieved comparatively lower compliance levels (see Table 3). These strategies included a single real-time videoconference call for the first in-home treatment session only, daily phone calls and emails and self-reported treatment diaries [44–46, 49]. Although there may be some indication that strategies to monitor in-home tES may influence protocol compliance, there are likely to be additional factors which contribute to this outcome. For example, it is important to acknowledge that protocol compliance may be affected by the duration of the experiment with high levels of compliance likely to be more difficult to achieve with more home stimulation sessions. Within this review, those studies with relatively higher levels of protocol compliance generally conducted 5–20 sessions, while those with relatively lower levels of compliance conduced 10–20 sessions.
As opposed to monitoring strategies, where videoconferencing appears to be a factor that may enable high levels of protocol compliance, there did not appear to be any association between a particular strategy to implement in-home tES and protocol compliance (Table 2). For example, some of the studies which reported relatively high levels of compliance used various strategies to implement in-home tES such as training sessions for participants and caregivers [38, 43, 47, 48, 50, 55, 56], customised headbands [38–40, 43, 47, 48, 50, 56] and remote computer access [38, 43, 47, 48, 50, 56], while others did not report any strategies [54]. However, it may be that use of multiple strategies is best. Of the studies which used three or more strategies to prepare the participant and deliver the in-home tES program, reported compliance levels were between 93 and 100% [38, 40, 43, 47, 48, 50, 56]. For studies which used two strategies or less, compliance levels appeared more variable and were as low as 76% [44].
Adverse events
Eighteen studies reported outcomes for adverse events (Table 4). The most common event was tingling sensations during the stimulation, which was reported in 12 studies [38–41, 43, 44, 46, 48, 52, 54–56]. Other common adverse events were itching or skin irritation, burning sensation, head pain, difficulties in concentrating, blurred vision, facial muscle twitching and changes in mood. There did not appear to be any association between adverse events and strategies to implement or monitor in-home tES. One study reported occurrence of a seizure, however the authors suggest this was not associated with stimulation as the participant was receiving a sham condition (no stimulation) and had a history of epilepsy [45]. Excluding the occurrence of this seizure which did not appear to be associated with delivery of tDCS, none of the reported adverse events would be considered severe or requiring medical attention.
Table 4.
Reported adverse events for in-home tES
| Adverse Events | |
|---|---|
| Andrade 2013 | Tingling sensation at the electrode site |
| Andre 2016 | No adverse events occurred |
| Carvalho 2018 | Minor and transient scalp burn, tingling and skin redness |
| Cha 2016 | Tingling, itching, redness, headache, tiredness, confusion, nausea. |
| Charvet 2017a | Not stated |
| Charvet 2017b1 | Pain > 6/10 (n = 2). Tingling (43%), itching (21%), burning sensation (23%), head pain or pressure (2%), dizziness (< 1%), difficulty concentrating (4%), blurred vision (<1%) and facial muscle twitch (<1%). |
| Clayton 2018 | Minimal and transient tingling and itchiness at the site of electrodes |
| Dobbs 2018 | Tingling (43%), burning (29%), head pain (8%), itching (8%), headache (6%), difficulty concentrating (1%) |
| Hagenacker 2014 | Slight itching or tingling |
| Hyvarinen 2016 | Tinnitus loudness and annoyance (5%), skin burn (2%); irritation (2%), mood changes (2%), tingling sensation (5%), uncomfortable sensation (47%), poor sleep (7%) |
| Kasschau 2016 | Tingling (60%), itching (24%), burning (30%), headache (3%), nausea (3%), head pain (3%), dizziness (<1%), difficulty concentrating (1%), blurred vision (<1%), forgetfulness (<1%). |
| Loo 2017 | No significant adverse events occurred |
| Martens 2018 | Skin redness (37%), sleepiness (11%), seizure (4%)* |
| Mortenson 2016 | Mild itching, tingling, burning sensation, headache and sleepiness |
| Riggs 2018 | No adverse events occurred |
| Schwippel 2017 | No adverse events occurred |
| Sharma 2018 | Tingling (20%), itching (6.5%), burning (8.3%), dizziness (0.4%), headache (2.2%), sleepiness (0.4%, nausea (0.4%) |
| Treister 2015 | No serious adverse events occurred |
| Van de Winckel 2018 | Mild tingling at electrode site at beginning of treatment (83%) |
1, data only reported for study two
*Unlikely related to stimulation as it occurred in the sham group in a participant with history of epilepsy
Participants’ satisfaction
Participants’ satisfaction towards the treatment was only reported by six studies [39, 46, 48, 50, 55, 56]. For five studies where real-time monitoring was provided, but a range of different strategies were employed to prepare participants for home stimulation, authors reported that participants generally had positive experiences with using in-home tES [39, 48, 50, 55, 56]. These studies were performed in various clinical populations that included neuropathic pain, Mal de Debarquement Syndrome, stroke, depression, myasthenia gravis, chronic pain and Multiple Sclerosis. Themes that emerged included users reporting that there were no difficulties in the treatment set-up, being comfortable with the stimulation device, being satisfied with the overall experience and expressing a desire to continue this home-based treatment after the study [48, 50, 55, 56] with purchase of their own stimulator [39]. However, some participants with Mal de Debarquement Syndrome, a condition characterised by feelings of rocking or swaying after exposure to motion, reported feeling uncomfortable applying the stimulation independently and reported frustration setting up the device and achieving appropriate levels of impedance to start stimulation [39]. The fourth study reported the perspectives of people with tinnitus who used in-home tES and were provided with self-reported treatment diaries to monitor stimulation [46]. The authors reported six out of 35 participants felt it was difficult to apply stimulation despite being providing with a one-day training session and instruction notes.
Registered clinical trials
The search of trial registries (clinicaltrials.gov, anzctr.org.au and who.int/ictrp/en/) identified ten clinical studies which are currently ongoing or completed, but not yet published (Table 5). These studies implemented in-home tES in various neurological and psychiatric conditions. Four studies stated that videoconferencing (or telemedicine) will form part of the monitoring strategy to implement in-home tES. Few studies have identified that they will be reporting on the occurrence of adverse events, protocol compliance or patients’ perspective. However, it is worth noting that limited information is required to be provided in clinical trial registries.
Table 5.
Clinical trials which are currently investigating in-home tES in neurological or psychiatric conditions
| Registration No. | Status | Population | Intervention | Strategies to implement or monitor in-home tES | Results to be reported | ||
|---|---|---|---|---|---|---|---|
| Adverse events | Compliance | Patients’ perspective | |||||
| NCT03499314 | Recruiting | Multiple Sclerosis | Anodal tDCS and dexterity training (20 sessions) | Real-time videoconferencing | ? | ? | ? |
| NCT03189472 | Recruiting | Parkinson’s Disease | tDCS (5 weeks) | Real-time videoconferencing Individual ‘unlock’ codes for stimulation Remote computer access |
? | ? | ? |
| NCT02959502 | Recruiting | Alzheimer’s Dementia | tDCS and cognitive training (40 sessions, 8 weeks) |
Caregiver will be trained in tDCS. No monitoring strategy reported | ? | ? | ? |
| NCT02894736 | Recruiting | Major Depression | tDCS | Monitoring strategy not reported | ? | ? | ? |
| NCT02746705 | Recruiting | Multiple Sclerosis | tDCS and cognitive training (20 sessions, 4 weeks) | Real-time videoconferencing | ? | ? | ? |
| NCT02652988 | Recruiting | Fibromyalgia | tDCS (60 sessions, 12 weeks) | Not reported | ? | ? | ? |
| NCT02346396 | Recruiting | Neuropathic chronic pain | tDCS (20 sessions, 4 weeks) | Monitoring strategy not reported | ? | ? | ? |
| ISRCTN56839387 | Completed | Chronic Pain | tDCS (5 sessions) | Not reported | ? | ? | ? |
| ACTRN12618000443291 | Recruiting | Stroke | tDCS and arm exercise (14 sessions, 2 weeks) | Real-time videoconferencing | ? | ✓ | ? |
| ACTRN12615000592549 | Recruiting | Tourette Syndrome | tDCS (18 sessions, 9 weeks) | Remotely supervised (strategy not stated) | ? | ? | ? |
tDCS transcranial direct current stimulation
Tick = reported in trial registry
? = not clearly reported in trial registry
Discussion
It is clear that in-home tES is an area of current research interest. Of the studies identified in this review, the majority were published within the last few years. Generally, these studies have been conducted in relatively small samples of patients, suggesting that current work is mostly around testing feasibility, safety and tolerability of this approach. As a result, many studies were found to have high levels of bias due to the less rigorous research designs employed. Nevertheless, this review identified a number of key findings from current evidence which will inform future in-home tES research and clinical practice. First, several different strategies were identified to implement and monitor in-home tES. The requirement to monitor stimulation appears to be a critical component to the successful implementation of in-home tES. Second, studies that employ real-time videoconferencing as a strategy to monitor in-home tES seemed to be associated with increased compliance with stimulation protocols and could possibly contribute to greater patient satisfaction with this form of treatment. Finally, from the available evidence, there does not appear to be any indication of severe adverse events associated with stimulation, suggesting that in-home tES is safe. Considering these findings in light of the promising advantages of delivering tES within a participant’s home, we suggest future studies continue to explore this approach.
The primary aim of this review was to identify approaches to implement and monitor in-home tES and achieve optimal treatment fidelity. We were particularly motivated to investigate this research question because in-home tES is likely to require significant consideration to ensure stimulation is performed correctly and in accordance with the treatment program, while maintaining patient safety. Therefore, strategies to implement and monitor in-home tES will be essential to ensure correct set-up and electrode preparation prior to stimulation, as well as to troubleshoot any issues that arise. It is clear from the available evidence that several approaches have been employed and these are likely to be critical aspects of future work for in-home tES. It is of particular note that studies which used real-time videoconferencing to monitor stimulation remotely were associated with higher levels of compliance (93–100%) with the in-home tES program [38–40, 43, 47, 48, 50, 54–56]. These are impressive levels of protocol compliance that are comparable to, or even greater, than that reported in previous clinical trials or research studies [9, 57, 58]. It should be noted that several of these studies did follow similar methodology as they followed an earlier guidelines paper that proposed a comprehensive approach to implement in-home tES [34]. However, despite similarity in their methodology, it is interesting to note that higher levels of compliance were observed across several different clinical populations and unique datasets. It is perhaps not surprising this approach resulted in greater compliance with the treatment protocol. Regular contact and viewing each treatment session in real-time likely ensured that technical or set-up difficulties were appropriately dealt with in an efficient and timely manner, preventing these challenges from affecting treatment compliance. There is also likely to be opportunity for research staff to motivate and encourage participants to continue with the treatment protocol where regular videoconferencing sessions are performed. These positive outcomes are supported by various telehealth studies where videoconferencing has been used to monitor treatments undertaken remotely in a patient’s home [59, 60]. However, in contrast to monitoring with real-time videoconferencing, we note that compliance with treatment protocols did not appear to reflect any particular strategy employed to prepare the participant for the in-home tES and deliver the program such as training participants or caregivers in the use of in-home tES, or the use of customised headbands. However, this in no way should undermine the importance of training sessions or additional approaches to prepare participants for performing in-home tES. Indeed, there is some indication that use of multiple strategies (at least three different approaches) to prepare the participant and deliver the in-home tES program may be associated with greater protocol compliance. However, this requires further investigation. Therefore, at this stage we suggest a multifaceted approach combining several of the identified strategies to prepare and train the participant to use tES in their own home along with real-time videoconferencing to monitor stimulation may be best. Future work should continue to explore approaches to ensure delivery of in-home tES is an acceptable, easy and safe.
Aside from videoconferencing, there were several other methods that have been used to monitor in-home tES treatments. For example, participants were required to self-report treatments using either treatment diaries [44–46] or online tracking systems [39]. While self-reported approaches do provide a record of in-home tES use, the accuracy of this approach relies upon regular reporting and accurate recall. As self-reported approaches do not obtain real-time information relating to in-home tES sessions, research staff are unable to monitor treatment sessions. This may prevent the ability to ensure correct electrode preparation, set-up and starting of the stimulator. These difficulties faced during the treatment phase by the study participants might contribute to the lower compliance. One interesting observation is that the use of real-time videoconferencing for monitoring in-home tES may have to be ongoing, and regular, to help achieve best protocol compliance. This observation is supported by CK Loo, A Alonzo and J Fong [49], where compliance was reported as 90% with a protocol which included a videoconference performed for the initial in-home tES session only, with the remaining sessions monitored through phone and email contact.
There is also some indication that regular videoconferencing sessions may contribute to greater patient satisfaction with using in-home tES. Few studies, which did use videoconferencing to monitor in-home tES, reported that study participants were able to set-up the stimulator and begin treatment without difficulty and were interested in continuing treatment with in-home tES [39, 48, 50, 55, 56]. However, patient perspectives were not commonly reported by the studies included in this review and this is an area for future investigation. Ensuring higher levels of satisfaction may assist with improving compliance with home treatment programs and may help facilitates clinical translation of this approach.
While a concern regarding in-home tES may be greater risk of injury from stimulation, results from this review suggest that no severe adverse events associated with receiving stimulation occurred during in-home tES and that any reported adverse events were akin to those reported for tES trials performed in clinics or research facilities [26, 61]. Common adverse events that were reported included tingling, burning and itching sensations especially at the electrode placement site. One study did report that participants experienced poor sleep and mood changes [46]. It is not clear why these adverse events occurred in this study involving stimulation applied to either the auditory cortex or frontal cortex in people with tinnitus. However, we do note that this study used a passive monitoring approach of self-reported treatment diaries. This may have limited the ability of the research team to track the progression of these symptoms at each session and discuss approaches to manage, or prevent, their occurrence. Furthermore, we note that one seizure was reported but was unlikely related to the home tES as it occurred to a participant receiving sham stimulation who had a history of epilepsy. While there does not appear to be a relationship between monitoring strategies for in-home tES and the occurrence of adverse events, we suggest that real-time monitoring approaches, such as videoconferencing, should be used to ensure patient safety and limit potential for adverse events to occur.
A limitation of the current study is that it does not account for the various patient groups that were included. It is likely that different pathology and patient characteristics could influence treatment compliance and satisfaction with in-home tES. As the current literature around in-home tES continues to grow, it is recommended future studies investigate how different patient groups respond and accept in-home tES. It may be that specific monitoring approaches or strategies to implement in-home tES are required for different patient populations to ensure high levels of treatment compliance and satisfaction are achieved.
Conclusion
Although in-home tES is a relatively new area of research, current evidence indicates that this is a feasible, acceptable and safe approach to deliver non-invasive brain stimulation treatment for a range of neurological and psychiatric conditions. This review indicates that the use of videoconferencing to monitor in-home tES can result in excellent levels of treatment fidelity and potentially greater participant satisfaction. While there are different approaches to implement and monitor in-home tES, we suggest real-time monitoring through videoconferencing should be included as one of these strategies in future studies. The area of in-home tES research is rapidly developing, driven in part by the ability to deliver consecutive stimulation sessions without overburdening people who are unwell by requiring that they travel frequently to receive treatment. We suggest future studies continue to explore patient groups which may benefit from this treatment approach and continue to monitor critical aspects of protocol compliance, adverse events and participant satisfaction. This information will help shape delivery of in-home tES to ensure that best possible services are provided.
Acknowledgments
Funding
N.S. is supported by a Research Themes Investment Scheem grant funded by the University of South Australia.
B.H. is supported by National Health and Medical Research Council (NHMRC) fellowship (1125054).
This study was supported by a Sylvia and Charles Viertel Charitable Foundation Clinical Investigator.
Award (VTL2016CI009).
Availability of data and materials
Please contact author for data requests. All primary data wee extracted from the refereced sources.
Abbreviations
- PRISMA
Preferred reporting items for systematic reviews and meta-analysis
- tACS
Transcranial alternating current stimulation
- tDCS
Transcranial direct current stimulation
- tES
Transcranial electrical stimulation
- tRNS
Transcranial random noise stimulation
Authors’ contributions
NS conducted the literature search and review, drafted the manuscript and reviewed the final version. SH was involved in study design, assisted during the systematic review of included studies and reviewed the final version of the manuscript. BH was involved in study design, assisted during the systematic review of included studies, drafted the manuscript and reviewed the final version. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable as used secondary data from published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nandini Sandran, Email: nandini.sandran@unisa.edu.au.
Susan Hillier, Email: susan.hillier@unisa.edu.au.
Brenton Hordacre, Phone: +61883021286, Email: brenton.hordacre@unisa.edu.au.
References
- 1.Purpura DP, McMurtry JG. Intracellular activities and evoked potential changes during polarization of motor cortex. J Neurophysiol. 1965;28:166–185. doi: 10.1152/jn.1965.28.1.166. [DOI] [PubMed] [Google Scholar]
- 2.Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol Lond. 2000;527:633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nitsche MA, Paulus W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology. 2001;57:1899–1901. doi: 10.1212/WNL.57.10.1899. [DOI] [PubMed] [Google Scholar]
- 4.Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, et al. Transcranial direct current stimulation: state of the art 2008. Brain Stimul. 2008;1:206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Liebetanz D, Nitsche MA, Tergau F, Paulus W. Pharmacological approach to the mechanisms of transcranial DC-stimulation-induced after-effects of human motor cortex excitability. Brain. 2002;125:2238–2247. doi: 10.1093/brain/awf238. [DOI] [PubMed] [Google Scholar]
- 6.Antal A, Boros K, Poreisz C, Chaieb L, Terney D, Paulus W. Comparatively weak after-effects of transcranial alternating current stimulation (tACS) on cortical excitability in humans. Brain Stimul. 2008;1:97–105. doi: 10.1016/j.brs.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Terney D, Chaieb L, Moliadze V, Antal A, Paulus W. Increasing human brain excitability by transcranial high-frequency random noise stimulation. J Neurosci. 2008;28:14147–14155. doi: 10.1523/JNEUROSCI.4248-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paulus W. Transcranial electrical stimulation (tES – tDCS; tRNS, tACS) methods. Neuropsychol Rehabil. 2011;21:602–617. doi: 10.1080/09602011.2011.557292. [DOI] [PubMed] [Google Scholar]
- 9.Allman C, Amadi U, Winkler AM, Wilkins L, Filippini N, Kischka U, et al. Ipsilesional anodal tDCS enhances the functional benefits of rehabilitation in patients after stroke. Sci Transl Med. 2016;8:330re331. doi: 10.1126/scitranslmed.aad5651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Shea J, Revol P, Cousijn H, Near J, Petitet P, Jacquin-Courtois S, et al. Induced sensorimotor cortex plasticity remediates chronic treatment-resistant visual neglect. eLife. 2017;6. [DOI] [PMC free article] [PubMed]
- 11.Shiozawa P, Fregni F, Benseñor IM, Lotufo PA, Berlim MT, Daskalakis JZ, et al. Transcranial direct current stimulation for major depression: an updated systematic review and meta-analysis. Int J Neuropsychopharmacol. 2014;17:1443–1452. doi: 10.1017/S1461145714000418. [DOI] [PubMed] [Google Scholar]
- 12.Hordacre B, Moezzi B, Ridding MC. Neuroplasticity and network connectivity of the motor cortex following stroke: a transcranial direct current stimulation study. Hum Brain Mapp. 2018;39:3326–3339. doi: 10.1002/hbm.24079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hordacre B, Moezzi B, Goldsworthy MR, Rogasch NC, Graetz LJ, Ridding MC. Resting state functional connectivity measures correlate with the response to anodal transcranial direct current stimulation. Eur J Neurosci. 2017;45:837–845. doi: 10.1111/ejn.13508. [DOI] [PubMed] [Google Scholar]
- 14.Hordacre B, Goldsworthy MR, Vallence A-M, Darvishi S, Moezzi B, Hamada M, et al. Variability in neural excitability and plasticity induction in the human cortex: a brain stimulation study. Brain Stimul. 2017;10:588–595. doi: 10.1016/j.brs.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Hordacre B, Ridding MC, Goldsworthy MR. Response variability to non-invasive brain stimulation protocols. Clin Neurophysiol. 2015;126:2249–2250. doi: 10.1016/j.clinph.2015.04.052. [DOI] [PubMed] [Google Scholar]
- 16.López-Alonso V, Fernández-del-Olmo M, Costantini A, Gonzalez-Henriquez JJ, Cheeran B. Intra-individual variability in the response to anodal transcranial direct current stimulation. Clin Neurophysiol. 2015;126:2342–2347. doi: 10.1016/j.clinph.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 17.López-Alonso V, Cheeran B, Río-Rodríguez D, Fernández-del-Olmo M. Inter-individual variability in response to non-invasive brain stimulation paradigms. Brain Stimul. 2014;7:372–380. doi: 10.1016/j.brs.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Wiethoff S, Hamada M, Rothwell JC. Variability in response to transcranial direct current stimulation of the motor cortex. Brain Stimul. 2014;7:468–475. doi: 10.1016/j.brs.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Ridding MC, Ziemann U. Determinants of the induction of cortical plasticity by non-invasive brain stimulation in healthy subjects. J Physiol Lond. 2010;588:2291–2304. doi: 10.1113/jphysiol.2010.190314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monte-Silva K, Kuo M-F, Hessenthaler S, Fresnoza S, Liebetanz D, Paulus W, et al. Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimul. 2013;6:424–432. doi: 10.1016/j.brs.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Goldsworthy MR, Hordacre B. Dose-dependency of transcranial direct current stimulation: implications for neuroplasticity induction in health and disease. J Physiol. 2017;595:3265–3266. doi: 10.1113/JP274089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jamil A, Batsikadze G, Kuo HI, Labruna L, Hasan A, Paulus W, et al. Systematic evaluation of the impact of stimulation intensity on neuroplastic after-effects induced by transcranial direct current stimulation. J Physiol. 2017;595:1273–1288. doi: 10.1113/JP272738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin DM, Alonzo A, Ho KA, Player M, Mitchell PB, Sachdev P, et al. Continuation transcranial direct current stimulation for the prevention of relapse in major depression. J Affect Disord. 2013;144:274–278. doi: 10.1016/j.jad.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Valiengo L, Bensenor IM, Goulart AC, de Oliveira JF, Zanao TA, Boggio PS, et al. The sertraline versus electrical current therapy for treating depression clinical study (select-TDCS): results of the crossover and follow-up phases. Depress Anxiety. 2013;30:646–653. doi: 10.1002/da.22079. [DOI] [PubMed] [Google Scholar]
- 25.Hordacre B. The role of telehealth to assist in-home tDCS: opportunities, promising results and acceptability. Brain Sci. 2018;8:102. doi: 10.3390/brainsci8060102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matsumoto H, Ugawa Y. Adverse events of tDCS and tACS: a review. Clin Neurophysiol Pract 2017; 2:19–25. [DOI] [PMC free article] [PubMed]
- 27.Woods AJ, Antal A, Bikson M, Boggio PS, Brunoni AR, Celnik P, et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clin Neurophysiol. 2016;127:1031–1048. doi: 10.1016/j.clinph.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liebetanz D, Koch R, Mayenfels S, Konig F, Paulus W, Nitsche MA. Safety limits of cathodal transcranial direct current stimulation in rats. Clin Neurophysiol. 2009;120:1161–1167. doi: 10.1016/j.clinph.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 29.Jackson MP, Truong D, Brownlow ML, Wagner JA, McKinley RA, Bikson M, et al. Safety parameter considerations of anodal transcranial direct current stimulation in rats. Brain Behav Immun. 2017;64:152–161. doi: 10.1016/j.bbi.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frank E, Wilfurth S, Landgrebe M, Eichhammer P, Hajak G, Langguth B. Anodal skin lesions after treatment with transcranial direct current stimulation. Brain Stimul. 2010;3:58–59. doi: 10.1016/j.brs.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez N, Opisso E, Pascual-Leone A, Soler MD. Skin lesions induced by transcranial direct current stimulation (tDCS) Brain Stimul. 2014;7:765–767. doi: 10.1016/j.brs.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 32.Palm U, Feichtner KB, Hasan A, Gauglitz G, Langguth B, Nitsche MA, et al. The role of contact media at the skin-electrode interface during transcranial direct current stimulation (tDCS) Brain Stimul. 2014;7:762–764. doi: 10.1016/j.brs.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 33.Wang J, Wei Y, Wen J, Li X. Skin burn after single session of transcranial direct current stimulation (tDCS) Brain Stimul. 2015;8:165–166. doi: 10.1016/j.brs.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 34.Charvet LE, Kasschau M, Datta A, Knotkova H, Stevens MC, Alonzo A, et al. Remotely-supervised transcranial direct current stimulation (tDCS) for clinical trials: guidelines for technology and protocols. Front Syst Neurosci. 2015;9:26. doi: 10.3389/fnsys.2015.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palm U, Kumpf U, Behler N, Wulf L, Kirsch B, Worsching J, et al. Home use, remotely supervised, and remotely controlled transcranial direct current stimulation: a systematic review of the available evidence. Neuromodulation. 2017. [DOI] [PubMed]
- 36.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions 5.1. 0. The Cochrane collaboration. 2011. pp. 33–49. [Google Scholar]
- 37.Agarwal S, Pawlak N, Cucca A, Sharma K, Dobbs B, Shaw M, et al. Remotely-supervised transcranial direct current stimulation paired with cognitive training in Parkinson's disease: an open-label study. J Clin Neurosci. 2018;57:51–57. doi: 10.1016/j.jocn.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 38.Dobbs B, Pawlak N, Biagioni M, Agarwal S, Shaw M, Pilloni G, et al. Generalizing remotely supervised transcranial direct current stimulation (tDCS): feasibility and benefit in Parkinson’s disease. J NeuroEng Rehabil. 2018;15:114. doi: 10.1186/s12984-018-0457-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cha YH, Urbano D, Pariseau N. Randomized single blind sham controlled trial of adjunctive home-based tDCS after rTMS for mal De Debarquement syndrome: safety, efficacy, and participant satisfaction assessment. Brain Stimul. 2016;9:537–544. doi: 10.1016/j.brs.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 40.Charvet LE, Dobbs B, Shaw MT, Bikson M, Datta A, Krupp LB. Remotely supervised transcranial direct current stimulation for the treatment of fatigue in multiple sclerosis: results from a randomized, sham-controlled trial. Mult Scler J. 2017:1–10. [DOI] [PMC free article] [PubMed]
- 41.Mortensen J, Figlewski K, Andersen H. Combined transcranial direct current stimulation and home-based occupational therapy for upper limb motor impairment following intracerebral hemorrhage: a double-blind randomized controlled trial. Disabil Rehabil. 2016;38:637–643. doi: 10.3109/09638288.2015.1055379. [DOI] [PubMed] [Google Scholar]
- 42.Andre S, Heinrich S, Kayser F, Menzler K, Kesselring J, Khader PH, et al. At-home tDCS of the left dorsolateral prefrontal cortex improves visual short-term memory in mild vascular dementia. J Neurol Sci. 2016;369:185–190. doi: 10.1016/j.jns.2016.07.065. [DOI] [PubMed] [Google Scholar]
- 43.Sharma K, Agarwal S, Mania D, Cucca A, Migdadi H, Charvet L, et al. Remotely supervised transcranial direct current stimulation (RS-tDCS) to mitigate fatigue and cognitive decline: a novel protocol for Parkinson's disease. Mov Disord. 2018;33.
- 44.Hagenacker T, Bude V, Naegel S, Holle D, Katsarava Z, Diener HC, et al. Patient-conducted anodal transcranial direct current stimulation of the motor cortex alleviates pain in trigeminal neuralgia. J Headache Pain. 2014;15:78. doi: 10.1186/1129-2377-15-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martens G, Lejeune N, O'Brien AT, Fregni F, Martial C, Wannez S, et al. Randomized controlled trial of home-based 4-week tDCS in chronic minimally conscious state. Brain Stimul. 2018;11:982–990. doi: 10.1016/j.brs.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 46.Hyvärinen P, Mäkitie A, Aarnisalo AA. Self-administered domiciliary tDCS treatment for tinnitus: a double-blind sham-controlled study. PLoS One. 2016;11:e0154286. doi: 10.1371/journal.pone.0154286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Charvet L, Shaw M, Dobbs B, Frontario A, Sherman K, Bikson M, et al. Remotely supervised transcranial direct current stimulation increases the benefit of at-home cognitive training in multiple sclerosis. Neuromodulation. 2017. [DOI] [PMC free article] [PubMed]
- 48.Kasschau M, Reisner J, Sherman K, Bikson M, Datta A, Charvet LE. Transcranial direct current stimulation is feasible for remotely supervised home delivery in multiple sclerosis. Neuromodulation. 2016;19:824–831. doi: 10.1111/ner.12430. [DOI] [PubMed] [Google Scholar]
- 49.Loo CK, Alonzo A, Fong J. Principles in use of home-based tDCS in depression. Brain Stimul. 2017;10:397. doi: 10.1016/j.brs.2017.01.177. [DOI] [Google Scholar]
- 50.Riggs A, Patel V, Paneri B, Portenoy RK, Bikson M, Knotkova H. At-home transcranial direct current stimulation (tDCS) with telehealth support for symptom control in chronically-ill patients with multiple symptoms. Front Behav Neurosci. 2018;12. [DOI] [PMC free article] [PubMed]
- 51.Treister R, Lang M, Klein M, Oaklander AL. Transcranial direct current stimulation (tDCS) for treating chronic pain; preliminary results of open-label, self-administered, at-home treatment. J Neurol Sci. 2015;357:e244. doi: 10.1016/j.jns.2015.08.851. [DOI] [Google Scholar]
- 52.Andrade C. Once- to twice-daily, 3-year domiciliary maintenance transcranial direct current stimulation for severe, disabling, clozapine-refractory continuous auditory hallucinations in schizophrenia. J ECT. 2013;29:239–242. doi: 10.1097/YCT.0b013e3182843866. [DOI] [PubMed] [Google Scholar]
- 53.Schwippel T, Wasserka B, Fallgatter AJ, Plewnia C. Safety and efficacy of long-term home treatment with transcranial direct current stimulation (tDCS) in a case of multimodal hallucinations. Brain Stimul. 2017;10:873–874. doi: 10.1016/j.brs.2017.04.124. [DOI] [PubMed] [Google Scholar]
- 54.Clayton AM, Howard J, Dobbs B, Shaw MT, Charvet LE. Remotely supervised transcranial direct current stimulation after ECT improves mood and cognition in a patient with multiple sclerosis: a case study. J ECT. 2018;34:e15. doi: 10.1097/YCT.0000000000000474. [DOI] [PubMed] [Google Scholar]
- 55.Carvalho S, Leite J, Pinto CB, Morse LR, Zafonte R, Fregni F. Feasibility of remotely-supervised tDCS in a person with neuropathic pain due to spinal cord injury. J Spinal Cord Med. 2018:1–2. [DOI] [PMC free article] [PubMed]
- 56.Van de Winckel A, Carey JR, Bisson TA, Hauschildt EC, Streib CD, Durfee WK. Home-based transcranial direct current stimulation plus tracking training therapy in people with stroke: an open-label feasibility study. J NeuroEng Rehabil. 2018;15:83. doi: 10.1186/s12984-018-0427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Loo CK, Alonzo A, Martin D, Mitchell PB, Galvez V, Sachdev P. Transcranial direct current stimulation for depression: 3-week, randomised, sham-controlled trial. Br J Psychiatry. 2012;200:52–59. doi: 10.1192/bjp.bp.111.097634. [DOI] [PubMed] [Google Scholar]
- 58.Sampaio-Junior B, Tortella G, Borrione L, Moffa AH, Machado-Vieira R, Cretaz E, et al. Efficacy and safety of transcranial direct current stimulation as an add-on treatment for bipolar depression: a randomized clinical TrialTranscranial direct current stimulation for bipolar DepressionTranscranial direct current stimulation for bipolar depression. JAMA Psychiatry. 2018;75:158–166. doi: 10.1001/jamapsychiatry.2017.4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Crotty M, Killington M, van den Berg M, Morris C, Taylor A, Carati C. Telerehabilitation for older people using off-the-shelf applications: acceptability and feasibility. J Telemed Telecare. 2014;20:370–376. doi: 10.1177/1357633X14552382. [DOI] [PubMed] [Google Scholar]
- 60.Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, et al. Effect of telehealth on use of secondary care and mortality: findings from the whole system demonstrator cluster randomised trial. BMJ. 2012;344. [DOI] [PMC free article] [PubMed]
- 61.Bikson M, Grossman P, Thomas C, Zannou AL, Jiang J, Adnan T, et al. Safety of transcranial direct current stimulation: evidence based update 2016. Brain Stimul. 2016;9:641–661. doi: 10.1016/j.brs.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact author for data requests. All primary data wee extracted from the refereced sources.