Abstract
Background
Fingertip entrapment injuries, which involve lacerations to the pulp and nail and often a fracture of the underlying bone, commonly occur in children, usually as the result of a crushing injury. Treatment is either conservative (wound cleaning and fingertip dressing) or surgical (repair of lacerations, reduction and stabilisation of fractures); however, no consensus currently exists regarding the most appropriate treatment modality.
Objectives
To assess the effects (benefits and harms) of surgical and conservative interventions for fingertip entrapment injuries in children. We aimed to compare: different methods of conservative treatment; surgical versus conservative treatment; different methods of surgical treatment; and different methods of management after initial conservative or surgical treatment.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, the Cochrane Central Register of Controlled Trials (The Cochrane Library), MEDLINE, EMBASE, the World Health Organization Clinical Trials Registry Platform and reference lists of articles up to 30 April 2013. We did not apply any restrictions based on language or publication status.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTs comparing interventions for treating fingertip entrapment injuries in children. The primary outcomes were fingertip function, nail growth, nail deformity and adverse events such as infection.
Data collection and analysis
Two authors independently screened studies for inclusion, assessed the risk of bias in each included trial and extracted data. We resolved disagreements through discussion.
Main results
We included two RCTs examining a total of 191 young children, 180 of whom were included in the analyses. The two trials tested different comparisons. Both trials were at high risk of bias, particularly from lack of blinding of participants and personnel, and of outcome assessment. The trials did not record fingertip function, nail growth or nail deformity. The quality of the evidence for the reported outcomes was judged to be 'low' using the GRADE approach (i.e. further research is very likely to have an important impact on our confidence in the estimate of the effect and is likely to change the estimate).
One trial compared a seven‐day course of antibiotics with no antibiotics after formal surgical repair of fingertip entrapment injuries. One child in each group had an infection at day seven (1/66 antibiotic group versus 1/69 no antibiotic group; RR 1.05, 95% CI 0.07 to 16.37). Both participants with infections had a more severe injury (partial fingertip amputation).
The other trial compared two different dressings (silicone net and paraffin gauze) for use after either surgical or initial conservative management of fingertip entrapment injuries. It reported that two of 20 children in the silicone group versus one of 25 in the paraffin group had complications of wound infection (RR 2.50, 95% CI 0.24 to 25.63) and that one of 20 children in the silicone group versus two of 25 in the paraffin group had skin necrosis (RR 0.63, 95% CI 0.06 to 6.41). All complications healed with conservative treatment. The results for mean healing times and mean number of dressing changes were similar between groups but benefits of either silicone or paraffin dressings could not be excluded (silicone mean 4.1 weeks versus paraffin mean 4.0 weeks; MD 0.10 weeks, 95% CI ‐0.61 to 0.81); (silicone mean 4.3 dressing changes versus paraffin mean 4.2 dressing changes; MD 0.10, 95% CI ‐0.57 to 0.77). The trial found that a silicone dressing was less likely to adhere to the wound or cause distress for the child at the one‐week dressing change.
Authors' conclusions
There is a lack of evidence from RCTs to inform all key treatment decisions for the management of fingertip entrapment injuries in children.
Given that the quality of evidence is low from one trial, we do not have conclusive evidence that prophylactic use of antibiotics after surgical repair fails to reduce risk of infection. The two children who experienced infection had more severe wounds.
Similarly, the low quality evidence from one trial has not enabled us to draw firm conclusions regarding the effect on healing time or complications (infection, skin necrosis) at four‐week follow‐up between a silicone net dressing and a paraffin gauze dressing when applied post‐surgery or after simple wound irrigation; however, the silicone net dressing may be easier to remove in the first week.
Further RCTs are required in this area, preferably comparing surgical with conservative methods of managing fingertip entrapment injuries. Outcome assessment should include fingertip function, nail growth and nail deformity for a minimum of three months post treatment.
Plain language summary
Treatments for fingertip entrapment injuries in children
Fingertip entrapment injuries commonly happen in children when their fingertip is caught between the door and the door surround as the door closes. This damages the finger nail, surrounding tissue and bone, all of which are important structures in the protection of the fingertip and for nail growth. These injuries are also called trapped finger injuries, crush fingertip injuries or door jamb injuries.
Sometimes these injuries are treated without surgery ('conservatively') by cleaning them and dressing the wound. Alternatively, the injuries are treated with surgery, which typically involves a general anaesthetic, cleaning of the wound and removal of damaged tissue, and stitches to repair any cuts on the fingertip or the nail.
We searched the medical literature until 30 April 2013 for studies comparing different methods of treating fingertip entrapment injuries. Our review includes evidence from two studies where participants were randomly allocated to one of two conditions. The studies included 191 children with results available for a total of 180 children. Both the studies had weaknesses that could undermine the reliability of the results. Since the studies compared different methods, we could not combine their results.
One study looked at the routine use of antibiotics in children with a surgically repaired fingertip injury to prevent infection. Due to the small number of children experiencing infection this study does not provide conclusive evidence of the effect of giving or withholding antibiotics. Only one child in each group had an infection after a week. Both children had had more severe injuries.
The other study compared two different dressing types for use in fingertip entrapment injuries. The low number of complications was comparable in the two treatment groups. Due to the low number of participants in the study we could not be certain that length of time the injuries took to heal and the number of dressing changes were the same in the treatment groups. However, it also found that the dressing made of silicone caused less distress for the child when being changed after the first week, probably because it stuck less to the wound than the paraffin dressing.
Overall, there is not enough evidence about how to best treat fingertip entrapment injuries in children. We recommend that further research is carried out, especially to see if surgery leads to better outcomes than simple wound cleaning and dressing. These studies should evaluate the effect of the treatment on fingertip function, nail growth and nail deformity for a minimum of three months after treatment.
Background
Description of the condition
Fingertip entrapment injuries are amongst the most common causes for children attending hospital emergency departments. Hand injuries occur at an annual rate of 11.6 per thousand (Shah 2012), of which fingertip injuries comprise between 21% (Fetter‐Zarzeka 2002) and two thirds of all injuries (De Alwis 2006; Inglefield 1995a). The hand is the most frequently injured part of the body after the head in this age group (Ljungberg 2003).
The vast majority of fingertip entrapment injuries occur when the finger is crushed by a closing door (Macgregor 1999). This injury usually occurs in the home (De Alwis 2006; Doraiswamy 2000;Inglefield 1995a), where the door may be closed by the child themselves (13%), an adult (25%) or another child (60%) (Doraiswamy 2000). Frequently, the fingertip is trapped on the hinge side of the door. The middle finger is the most frequently injured (25% to 41% of injuries), followed by the ring finger, little finger, index finger and thumb, respectively (Doraiswamy 2000; Gellman 2009; Inglefield 1995a). Injuries occur in both dominant and non‐dominant hands, with 54% to 66% involving fingers of the right hand (Doraiswamy 2000;Fetter‐Zarzeka 2002). Fingertip injuries are most common in children under five years of age, with this age group comprising 38% of all fingertip injuries compared with 32% in children aged five to 10 years (Doraiswamy 1999).
Fingertip entrapment injuries involve damage to one or more of the following: the finger pulp, nail or bone. The degree of damage to each of these structures depends on the specific injury. The nailbed is damaged in 15% to 26% of injuries (De Alwis 2006; Ljungberg 2003) and a phalangeal (finger bone) fracture occurs in 14% to 50% of cases (Doraiswamy 2000; Gellman 2009; Ljungberg 2003). More severe cases involve avulsion, where tissue or bone is partially or completely pulled away from the body by the force of the injury. If this injury involves complete removal of the fingertip, it is considered an amputation.
The nail serves an important function as part of the fingertip. In addition to cosmetic appearance, the nail gives protection to the fingertip, helps in fine motor skills such as the pincer grip, scratching and picking up small objects, and plays a role in tactile sensation (Gellman 2009;Inglefield 1995a). As a result of a fingertip entrapment injury, the germinal matrix (the region proximal to the nail plate from which it grows) and the sterile matrix (which supports the nail plate from below) can be damaged, affecting future nail growth and leading to dysfunction and disfigurement.
Damage to the nailbed, resulting in altered nail growth, is the major consequence of fingertip entrapment injuries. While damage to the pulp and bone also occur, the future repercussions of these aspects of the injury are less significant. Altered nail growth can result in cosmetic abnormalities, as well as altered sensation and difficulty scratching and pinching.
The tendons of the fingertip are not usually severed (Doraiswamy 2000). Clinically, injuries are frequently only described in terms of the level of injury. The PNB (pulp, nail, bone) classification allows fingertip injuries to be qualitatively assessed and comparisons between different injuries to be drawn, such as the degree of pulp loss, level of nail damage and amount of bone injury (Evans 2000). The PNB classification is summarised in Table 1.
1. The PNB (pulp, nail, bone) classification of fingertip injuriesa.
| Pulp | Nail | Bone | |||
| No injury | 0 | No injury | 0 | No injury | 0 |
| Laceration | 1 | Sterile matrix laceration | 1 | Tuft fracture | 1 |
| Crush | 2 | Germinal and sterile matrix laceration | 2 | Comminuted non‐articular fracture | 2 |
| Loss: distal transverse | 3 | Crush | 3 | Articular fracture | 3 |
| Loss: palmar oblique partial | 4 | Proximal nailbed dislocation | 4 | Displaced basal fracture | 4 |
| Loss: dorsal oblique | 5 | Loss: distal third | 5 | Tip exposed | 5 |
| Loss: lateral | 6 | Loss: distal two thirds | 6 | Loss: distal half | 6 |
| Loss: complete | 7 | Loss: lateral | 7 | Loss: subtotal (tendons intact) | 7 |
| ‐‐ | 8 | Loss: complete | 8 | Loss: complete | 8 |
aAdapted from Evans 2000. The PNB classification describes fingertip injuries according to the damage to the three main components of the fingertip. A score is allocated according to the extent or type of injury to each component. Thus PNB 110 = lacerated pulp, sterile matrix laceration to nail, but no injury to bone.
Description of the intervention
Treatment of fingertip entrapment injuries can be either surgical (operative) or conservative (non‐operative). A conservative approach involves irrigation of the injured area with saline and then dressing of the wound with fingertip dressings. Trephination (draining through a small hole) of a haematoma (collection of blood outside the blood vessels) under the nail (subungual haematoma) may be performed to reduce the pain associated with pressure in this area. No form of sedation or anaesthesia is usually required for this process. Treatment usually occurs in a hospital emergency department or in a family doctor's surgery. A variety of dressings may be used, including dressings made from silicone or paraffin gauze. Splints may be used to protect the injured area. Follow‐up of children with these injuries in a clinical setting is rare.
Typically, a surgical approach involves the child undergoing a general anaesthetic, having the injury debrided (the wound cleaned and damaged tissue removed) and then repaired and sutured. This would occur in an operating theatre and is usually performed by a hand surgeon (plastic or orthopaedic). Indications for treatment and variations in technique are often based on practitioner preferences (Gellman 2009). These include whether a nail plate that has remained attached is removed; the material and gauge of sutures used to repair the nailbed and skin; whether antibiotics are given perioperatively; and whether a nail splint (the removed nail or a prosthetic foil) or finger tip splint are used or not. The same variety of dressings are used for surgical treatment as are available for conservative treatment. Follow‐up after repair is usually limited to a single clinic appointment, often between two and 12 weeks postoperatively (West 2011).
As discussed in Description of the condition, fingertip entrapment injuries vary in severity, involving damage to a range of structures in the fingertip (the pulp, nail, and bone). The severity and location of the injury is likely to influence management decisions.
How the intervention might work
One key issue we aimed to cover in this review was whether to treat fingertip entrapment injuries surgically or conservatively. Surgical treatment involves meticulous repair of the fingertip injury in a way that aims to promote rapid wound healing. Surgical repair is thought to result in better nail regeneration and growth, which in turn should result in better functional and cosmetic outcomes in the long term. However, surgical management usually involves general anaesthesia, which is associated with additional risks to the child. These risks are avoided by conservative treatment methods, which also avoid the cost and social impacts of hospital admission and surgical procedures but may result in poorer outcomes.
Why it is important to do this review
Despite the relative frequency of this injury, there is no consensus on the best course of management, with decisions usually based upon the inclination of the individual clinician and not on any local, regional, national or international evidence‐based policy. Both surgical and conservative methods have received support in the literature; some argue that conservative treatment is often acceptable (Inglefield 1995a), while others advocate surgical repair for all but the most minimal injuries (De Alwis 2006). Others argue that trephination of a subungual haematoma and dressing alone has a similar outcome to surgical intervention (Gellman 2009). A study of 283 children aged over six months presenting with such injuries in Glasgow reported that 48% were treated conservatively and 52% were treated surgically, without giving the underlying rationale for treatment decisions (Doraiswamy 1999). The frequent use of surgical repair is likely to contribute to the average cost of £2500 per injury estimated for the UK National Health Service in 2007 (Garvin 2007). Thus, a systematic review of randomised controlled trials was required to ascertain the best course of treatment for this common presentation.
Objectives
To assess the effects (benefits and harms) of surgical and conservative interventions for fingertip entrapment injuries in children.
We aimed to compare:
Different methods of conservative treatment
Surgical versus conservative treatment
Different methods of surgical treatment
Different methods of management after initial conservative or surgical treatment
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs (e.g. allocation by alternation or date of birth) evaluating interventions for treating fingertip entrapment injuries in children.
Types of participants
Children with a fingertip entrapment injury. We included RCTs of children less than 12 years old as the mechanism of injury differs in older populations. We adopted a common‐sense approach to exclusion based upon age, wherein we considered each trial in terms of the primary objectives of the review. Thus we would have included RCTs that focused on children but enrolled a small proportion (< 10%) of adults or older children if either: a) separate data had been available for paediatric participants or b) the mechanism of injury was similar to that seen in paediatric populations and the older participants were balanced between comparison groups.
We excluded trials focusing exclusively on the management of fingertip injuries involving amputation or avulsion. However, while the focus of this review was on those injuries that did not result in amputation (see Table 2), we included trials with a proportion of participants with partial or complete amputations where such participants were balanced between the comparison groups and where the mechanism of injury was within the scope of this review.
2. Fingertip injuries of interest to this review using the PNB classification.
| Pulp | Nail | Bone | |||
| No injury | 0 | No injury | 0 | No injury | 0 |
| Laceration | 1 | Sterile matrix laceration | 1 | Tuft fracture | 1 |
| Crush | 2 | Germinal and sterile matrix laceration | 2 | Comminuted non‐articular fracture | 2 |
| ‐‐ | Crush | 3 | Articular fracture | 3 | |
| ‐‐ | Proximal nailbed dislocation | 4 | Displaced basal fracture | 4 | |
Types of interventions
We included trials comparing interventions used for treating fingertip entrapment injuries in children. Examples of conservative interventions include simple irrigation and dressing, trephination of a subungual haematoma and dressing, and the use of splints to protect the injured area. Surgical treatment involves debridement and repair, which can be performed in a variety of ways. Factors of interest included the removal of an attached nail, the type and gauge of suture used to repair the different structures of the fingertip, the use of perioperative antibiotics and the use of a splint to protect the injured area. Some interventions, such as the type of dressing, use of antibiotics and the type of protective splint, apply to both conservative and surgical treatments.
Types of outcome measures
The measurement of both subjective and objective outcomes is difficult in young children. Therefore we anticipated that outcomes would usually be reported by parents.
Primary outcomes
Fingertip function (dexterity; likely to be measured subjectively based upon parents' comments)
Nail growth (likely to be measured in terms of growth or time, or dichotomously, e.g. nail present or absent at follow‐up)
Nail deformity (likely to be measured subjectively, or using a grading system unique to each trial, as no universally‐adopted system currently exists)
Adverse events (e.g. wound infection, distal necrosis of fingertip, hypertrophic scarring, growth arrest)
Secondary outcomes
Child or parent satisfaction, or both (e.g. with the intervention; with appearance)
Pain and sensation (these are unlikely to be reported because of the age of the typical patient; however, patient distress may be recorded at the time of the intervention)
Time to healing of injury (likely to be reported subjectively)
Requirement for secondary procedures to improve function or appearance (likely to be surgical interventions performed after the injury is fully healed).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (April 2013), the Cochrane Central Register of Controlled Trials (The Cochrane Library, 2013 Issue 4), MEDLINE (1946 to April Week 3 2013), and EMBASE (1980 to 2013 Week 17). We also searched the WHO International Clinical Trials Registry Platform (to April 2013) for ongoing trials. We did not apply any restrictions based on language or publication status.
The search strategies for The Cochrane Library, MEDLINE, EMBASE and the WHO International Clinical Trials Registry Platform are listed in Appendix 1. The MEDLINE strategy combined subject‐specific search terms with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying RCTs in MEDLINE (Lefebvre 2011).
Searching other resources
We searched reference lists of relevant articles.
Data collection and analysis
Selection of studies
Using a study eligibility form, both authors independently screened all identified studies for possible inclusion in the review. We then compared individual lists of included trials and resolved any disagreements through discussion. We contacted trial authors of two studies (Alpern 2005; Strauss 2008) to inform trial selection.
Data extraction and management
Both authors extracted data independently using a form piloted on several selected trials beforehand and resolved disagreements through discussion. One author (RC) entered the data into Review Manager (RevMan) software.
Assessment of risk of bias in included studies
Both authors assessed the risk of bias independently using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2011). Using this tool we assessed selection bias due to inadequate sequence generation or allocation concealment; performance bias due to lack of blinding of participants and personnel; detection bias due to lack of blinding of outcome assessment; attrition bias resulting from incomplete outcome data; reporting bias in the form of selective reporting; and 'other bias'.
Measures of treatment effect
For each trial, we calculated the risk ratio (RR) and 95% confidence intervals (CIs) for dichotomous outcomes, and mean differences (MD) and 95% CIs for continuous outcomes. Where continuous data were measured using different scales, we calculated the standardised mean difference (SMD) where such data were pooled.
Unit of analysis issues
Most injuries were expected to involve single fingers. However, we anticipated that unit of analysis could have been an issue if trials presented data for individual fingers rather than for individual participants (unit of randomisation) where some participants had more than one injured finger. If such an issue arose and appropriate corrections had not been made, we planned to present the data for such trials where the disparity between the units of analysis and randomisation was small (and thus the proportion of participants with multiple finger involvement was very small). However, this was not relevant for any trials included in the review. If data had been pooled, it would have been necessary to perform a sensitivity analysis to examine the effects of excluding incorrectly reported trials from the analysis.
Dealing with missing data
Where data were missing from published reports, we planned to contact authors via email. Where possible, we performed intention‐to‐treat analysis.
Assessment of heterogeneity
We planned to assess statistical heterogeneity using the visual inspection of forest plots in Review Manager (RevMan) combined with the Chi² test (with statistical significance set at P < 0.10), and the I² statistic (with an I² between 50% to 90% likely to represent substantial heterogeneity and 75% to 100%, representing considerable (very substantial) heterogeneity) (section 9.5.2; Higgins 2011). However, as none of the included trials compared similar interventions, we did not conduct statistical assessment of heterogeneity.
Assessment of reporting biases
If appropriate in a future update, we will explore publication bias using a funnel plot if there are at least 10 trials reporting the same outcome.
Data synthesis
If appropriate in a future update, we plan to pool results from trials with comparable participant characteristics and interventions using the fixed‐effect model. We will consider using the random‐effects model if there is significant or substantial unexplained heterogeneity, or both.
Subgroup analysis and investigation of heterogeneity
If sufficient data are available in a future update, we will investigate heterogeneity by subgroup analyses based on the aspects listed below.
Anatomical level and classification of injury (in particular, different involvement of pulp, nail and bone components).
Length of follow‐up. We will consider up to three months as short term (i.e. relating to a single nail growth cycle) and over three months as long term.
Age of the child. We will compare the age group that accounts for the majority of these injuries (0 to 4 years) with the older age groups (5 to 8 years, and 9 to 12 years). The mechanism of injury is likely to be different in older children.
We will use the test for subgroup differences available in Review Manager (RevMan) to determine if the results for subgroups are statistically significantly different.
Sensitivity analysis
If appropriate in a future update, we will undertake sensitivity analysis to determine the impact of bias within individual trials on the meta‐analysis. The effect of removing trials with a high risk of bias will be analysed, with inadequate allocation concealment leading to selection bias being of primary interest. If, on visual inspection of an analysis, a trial appears to be the source of substantial heterogeneity, we will conduct a sensitivity analysis to assess the effect of excluding this trial from the analysis.
Assessing the quality of the evidence
We used the GRADE approach to assess the quality of evidence related to each of the primary outcomes listed in the Types of outcome measures (Higgins 2011). If sufficient data are available in a future update, we will present the main results of this review in 'Summary of findings' tables.
Results
Description of studies
Results of the search
The search was completed in April 2013. We screened a total of 363 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (17 records); Cochrane Central Register of Controlled Trials (90), MEDLINE (148), EMBASE (108) and the WHO International Clinical Trials Registry Platform (9). We also identified eight potentially eligible studies from other sources (reference lists of potentially eligible studies).
The search resulted in the identification of 33 potentially eligible studies, for each of which full reports were obtained (35 reports). Upon trial selection, we included two trials: Altergott 2008 (published in two reports) and O'Donovan 1999; and excluded 30 studies (listed in the Characteristics of excluded studies). One unpublished trial is awaiting classification (Alpern 2005). We did not identify any trials as ongoing. Figure 1 is a flow diagram summarising the trial selection process.
1.
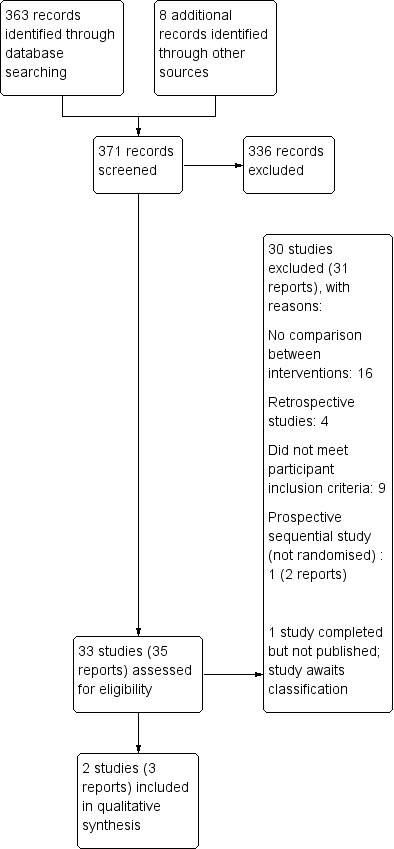
Study flow diagram
Overall, we included two trials, excluded 30 studies, identified one trial awaiting classification and no ongoing studies.
Included studies
The two included trials were published as full reports in journals, one in 1999 and one in 2008. We have summarised key information about the trials below and provided fuller details of methods, participants, interventions and outcomes for the individual trials in the Characteristics of included studies table.
Design
The two trials (Altergott 2008; O'Donovan 1999) were described as randomised; however, O'Donovan 1999 did not describe the method of randomisation. Participants and personnel were not blinded in either of the trials.
Sample size
The two trials had a total sample size of 191: Altergott 2008 included 146 children and O'Donovan 1999 included 45 children.
Setting
Both were single centre trials. Altergott 2008, which was conducted in the United States of America, recruited participants from September 2000 to July 2004. O'Donovan 1999, which was conducted in Ireland, recruited over an unspecified four‐month period.
Participants
Both trials had paediatric populations. In Altergott 2008, the mean age was 3.2 years in the antibiotic group and 3.0 years in the no antibiotic group. The mean age in both intervention and control groups in O'Donovan 1999 was 4.6 years. The youngest participant in each trial was six months of age.
Altergott 2008 included fingertip injuries distal to the distal interphalangeal joint requiring surgical repair. O'Donovan 1999 included fingertip injuries involving the pulp, nail complex or distal phalanx. The majority of children in both trials had injuries that did not involve amputation of the fingertip, in keeping with the scope of this review (see Table 2). However, both trials included a proportion of participants that had undergone a partial or total amputation; in both cases these participants were balanced between the intervention and control groups. We have summarised inclusion and exclusion criteria in the Characteristics of included studies table.
Interventions
Each trial compared a different intervention. Altergott 2008 compared prophylactic antibiotics with no antibiotics following surgical repair of fingertip injuries. O'Donovan 1999 compared a silicone net dressing with paraffin gauze following either surgical (31 participants) or initial conservative (14 participants) management of fingertip injuries.
Outcomes
Follow‐up was for seven days in Altergott 2008 and four weeks in O'Donovan 1999. Neither trial reported on this review's primary outcomes of fingertip function, nail growth and nail deformity. Both trials recorded infection rate as an outcome: this was the primary outcome in Altergott 2008, while O'Donovan 1999 recorded it as a complication. A secondary outcome in Altergott 2008 was antibiotic compliance within the prophylactic antibiotic group. O'Donovan 1999 measured the number of dressing changes required until the wound healed, as well as perceived level of patient stress, wound adhesion and the rate of complications.
Excluded studies
We have listed brief details and reasons for the exclusion of 30 studies in the Characteristics of excluded studies table. We excluded 16 studies because they did not make a comparison between two or more interventions. Four studies were excluded because they were conducted retrospectively. We excluded nine studies because they were either not conducted in paediatric participants or did not focus on the injuries of interest to this review (Table 2). Also, we excluded one trial because although it was conducted prospectively it was not randomised or quasi‐randomised.
Studies awaiting classification
Alpern 2005 awaits classification. This trial aimed to compare different types of local anaesthetic for fingertip injuries in children. It was registered in 2005 with clinicaltrials.gov and was seemingly completed in 2007; however, we did not find any published report of its results. We contacted the author directly and they indicated that the trial manuscript is currently under revision for publication. We summarised details of the trial in the Characteristics of studies awaiting classification table.
Risk of bias in included studies
We summarised the risk of bias on seven items for each of the included trials in Figure 2 and described them in the 'Risk of bias' tables in the Characteristics of included studies section. In Figure 2, a (+) judgement indicates that we considered there to be low risk of bias for the specific item, while a (‐) judgement indicates a high risk of bias. An unclear (?) verdict indicates that we were unable to determine the impact of the specific bias item on the trial.
2.
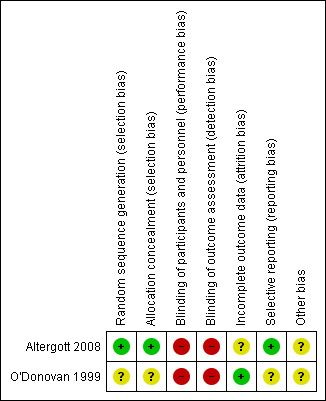
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial. See each trial's individual Risk of Bias table for explanation.
Allocation
Altergott 2008 had a low risk of selection bias relating to sequence generation and allocation concealment. O'Donovan 1999 was at unclear risk of bias as the allocation method was described as randomised, but no further details were provided.
Blinding
Participants and personnel were not blinded at any point in either of the studies, nor were outcome assessors. Both studies were therefore judged to be at high risk of performance bias and detection bias.
Incomplete outcome data
In Altergott 2008, 7% of participants in the intervention group and 8% of participants in the control group were lost to follow‐up. Although the trial reported the reasons for attrition, the trial authors did not report the distribution of these reasons between the groups. It was unclear what impact attrition bias had upon the trial's findings. O'Donovan 1999 followed all participants up to the conclusion of the trial, and so the trial was at low risk of attrition bias.
Selective reporting
A trial protocol for Altergott 2008 was available through the WHO International Clinical Trials Registry Platform. The outcomes reported matched those from the protocol, and the risk of reporting bias was judged to be low. O'Donovan 1999 reported all outcomes outlined in the methods section; however, no trial protocol was available for comparison and it was unclear if the trial was at risk of reporting bias.
Other potential sources of bias
Injury severity
In Altergott 2008, participant enrolment was at the discretion of the clinical team (where inclusion criteria applied). The trial authors considered that this approach had the potential to skew the participant population towards less severe injuries, with more complicated injuries not being enrolled in the trial. We agreed with this assessment.
Conversely, in O'Donovan 1999 only those participants who were referred to the plastic surgery department could potentially be enrolled in the trial. As more minor injuries may have been managed in the emergency department without referral, it is possible that this method resulted in a participant population skewed towards more severe injuries.
However, provided there was allocation concealment, skewing of the patient population in terms of injury severity in either Altergott 2008 or O'Donovan 1999 is unlikely to have impacted the internal validity of either trial. Rather, it would limit the applicability of the results each trial reports when a broader patient population with injuries ranging in severity is considered.
Length of follow‐up
Altergott 2008 followed up participants for seven days and assessed them for the presence of infection at this time. However, the trial authors noted that after the trial conclusion a further four participants were found to have an infection on chart review. As these infections occurred outside the time period of the trial, the trial authors did not include them in the trial's results. This suggests a potential bias from an inappropriately short follow‐up period; it is unclear what impact on the results a longer follow‐up would have had.
In contrast to Altergott 2008, where patients were discharged with a scheduled follow‐up visit at 48 hours and final follow‐up at seven days, participants in O'Donovan 1999 had weekly dressing changes performed in dressing clinics for four weeks. Such a disparity in follow‐up length may reflect the lack of standardisation in general clinical practice.
Effects of interventions
We listed the outcomes reported in the included trials in the Characteristics of included studies section. Also, we have presented outcome data reported at final follow‐up for each trial in Data and analyses. Pooling of data was not undertaken as the two included trials reported different comparisons. Neither of these measured the primary outcomes of fingertip function (either subjectively or objectively), nail growth or nail deformity. Neither trial assessed the secondary outcomes of participant or parent satisfaction, or fingertip sensation.
Different methods of conservative treatment
O'Donovan 1999 compared two types of finger dressings and included 14 participants (31%) who were treated conservatively. However, separate data for these participants were not available and therefore we could not directly compare the different dressings in a population receiving only conservative treatment.
Surgical versus conservative treatment
No trials compared surgical with conservative treatment.
Different methods of surgical treatment
No trials directly compared different methods of surgical treatment.
Different methods of management after initial conservative or surgical treatment
Prophylactic antibiotics
In Altergott 2008, the use of prophylactic antibiotics was compared with no prophylactic antibiotics after formal surgical repair in 146 children. Altergott 2008 found no difference in presence of infection at the seventh postoperative day as determined by review via telephone and confirmed by visual examination in person (1/66 antibiotic group versus 1/69 no antibiotic group; RR 1.05, 95% CI 0.07 to 16.37; see Analysis 1.1). The authors noted that each of the two injuries that became infected, both partial amputations, had been repaired with a larger than average number of sutures (infected cases had eight and nine sutures respectively; in non‐infected cases the mean number of sutures was 4.9, SD 2.0). Both participants made a full recovery after treatment for their infection. In terms of antibiotic compliance, 86.2% (59/66) of the children in the antibiotic group had consumed at least 75% of the prescribed doses at the day seven telephone interview.
1.1. Analysis.
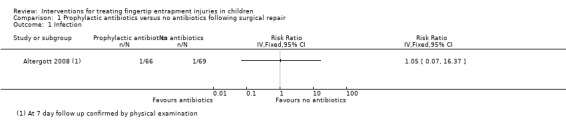
Comparison 1 Prophylactic antibiotics versus no antibiotics following surgical repair, Outcome 1 Infection.
Silicone dressings versus paraffin dressings
O'Donovan 1999 compared silicone net dressings with paraffin gauze dressings after either surgical management (debridement only, nailbed repair, composite grafts, or local (V‐Y) flaps) or initial conservative management (simple wound irrigation) of fingertip entrapment injuries.
There were no significant differences between the two dressings in the reported complications of wound infection (2/20 silicone group versus 1/25 paraffin group; RR 2.50, 95% CI 0.24 to 25.63; see Analysis 2.1) or skin necrosis (1/20 silicone group versus 2/25 paraffin group; RR 0.63, 95% CI 0.06 to 6.41; see Analysis 2.1). All complications healed with conservative management; however, one patient with an amputated fingertip in the paraffin group had an "active cellulitis" that required hospital readmission.
2.1. Analysis.
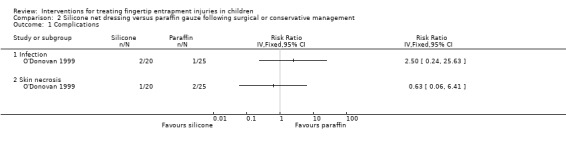
Comparison 2 Silicone net dressing versus paraffin gauze following surgical or conservative management, Outcome 1 Complications.
O'Donovan 1999 found no differences between groups in either the mean healing times (silicone mean 4.1 weeks versus paraffin mean 4.0 weeks; MD 0.10 weeks, 95% CI ‐0.61 to 0.81; see Analysis 2.2) or the mean number of dressing changes (silicone mean 4.3 versus paraffin mean 4.2; MD 0.10, 95% CI ‐0.57 to 0.77; see Analysis 2.3).
2.2. Analysis.
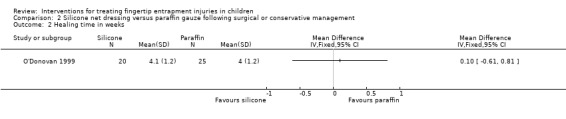
Comparison 2 Silicone net dressing versus paraffin gauze following surgical or conservative management, Outcome 2 Healing time in weeks.
2.3. Analysis.
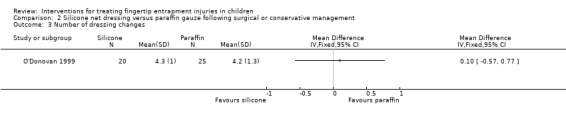
Comparison 2 Silicone net dressing versus paraffin gauze following surgical or conservative management, Outcome 3 Number of dressing changes.
When the dressings were compared in terms of level of distress experienced by the child during a dressing change, a low level of perceived stress (defined as "happy" or only "mildly upset"), was significantly more common in the silicone dressing group at the week one dressing change (19/20 silicone group versus 9/25 paraffin group; RR 2.64, 95% CI 1.55 to 4.49; see Analysis 2.4). At the week two dressing change, the silicone dressing was again favoured; however, this difference was not statistically significant. No difference was found at the week three or week four dressing changes. A similar pattern favouring the silicone group was reported for observed adhesion of the dressing to the wound (see Analysis 2.5). Dressings were significantly more likely to have "slipped off" or were "gently teased off" in the silicone dressing group than in the paraffin group at the week one dressing change (18/20 silicone versus 12/25 paraffin; RR 1.88, 95% CI 1.22 to 2.89). At the week two dressing change, the silicone dressing was again favoured in terms of adhesion; however, this difference was not statistically significant. No difference was found at the week three or week four dressing changes; just one paraffin dressing had to be soaked for removal on each occasion.
2.4. Analysis.
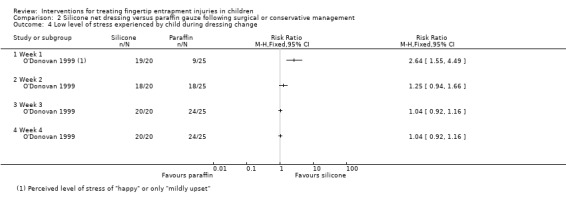
Comparison 2 Silicone net dressing versus paraffin gauze following surgical or conservative management, Outcome 4 Low level of stress experienced by child during dressing change.
2.5. Analysis.
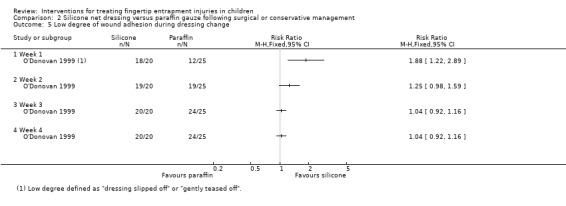
Comparison 2 Silicone net dressing versus paraffin gauze following surgical or conservative management, Outcome 5 Low degree of wound adhesion during dressing change.
Discussion
Summary of main results
This review, which covers all surgical and conservative interventions for treating fingertip entrapment injuries in children, includes two single‐centre trials that tested different comparisons and reported results for a total of 180 young children. Each of the trials focused on outcomes measurable over a short time frame rather than primary outcomes of this review such as fingertip function, nail growth and nail deformity, which tend to be measured over longer periods of time.
One trial (Altergott 2008) compared a seven‐day course of prophylactic antibiotics with no antibiotics after surgical repair. One child in each group had an infection at day seven. Both infections were in children who had a partial amputation of their fingertip.
The other trial (O'Donovan 1999) compared silicone versus paraffin dressings after initial conservative or surgical management. The trial found similar results in the two groups in terms of complications (infection, skin necrosis) at four‐week follow‐up, and in the mean injury healing times and mean number of dressing changes. However, it found that at the week one dressing change the silicone net dressing adhered less to the wound and caused less distress for the child.
No trials compared surgical versus conservative management or different methods of surgical management. Aspects of surgical interventions that were of particular interest to this review such as removal of an attached nail, the type and gauge of suture used and the use of a splint to protect the injured area were not evaluated in either of the included trials.
Overall completeness and applicability of evidence
The available evidence from RCTs is very limited and comes from two small single‐centre non‐blinded trials that did not report on our primary outcomes of fingertip function, nail growth or nail deformity. Altergott 2008 reported on wound infection at the day seven follow‐up. This time period was too short, as illustrated by the subsequent finding of later infections from via chart review.
The age distribution in both trials was characteristic of the usual population with these injuries. While the intended focus of this review was those injuries that did not result in amputation, as described in the Types of participants section both trials included a minority of participants with partial or complete amputations. This potentially limits the applicability of the evidence when considering less severe injuries, which were the intended injury population of this review. As discussed under Other potential sources of bias, the different treatment settings and enrolment methods in the two trials may have skewed the populations in terms of injury severity.
Quality of the evidence
We used the GRADE approach to assess the quality of evidence relating to each outcome for which results were available (Higgins 2011). There was a notable absence of evidence for our key primary outcomes of fingertip function, nail growth and nail deformity. We downgraded the quality of evidence for each reported outcome by two levels to 'low quality'; once for limitations in design and implementation (given that neither trial was blinded, introducing performance and detection bias), and once for imprecision (given that results for each outcome were based on a small number of events in a single trial). This indicates that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Potential biases in the review process
We undertook systematic processes as outlined in order to minimise the potential for bias in this review. While our literature search was extensive, it is possible that we did not identify some RCTs particularly those only reported in abstract form, communicated at conferences or published in non‐English language journals. Due to our inclusion criteria we may have overlooked mixed‐population trials examining interventions in fingertip entrapment injuries where a number of paediatric participants were included and analysed within a larger adult population. However, it is almost certain that we have not overlooked paediatric trials that would provide definitive evidence for application to routine clinical practice.
Some adjustment to the inclusion criteria was required to accommodate the populations in the included trials. This review aimed to focus on injuries that did not result in amputation. However, while we excluded trials exclusively examining the management of fingertip amputation, both included trials had a proportion of injuries severe enough to cause amputation. We included these trials because amputated cases were in the minority, were evenly distributed across the comparison groups, and the mechanism of injury was within the scope of this review. However, the inclusion of these trials effectively shifts the review towards more severe injuries. Secondly, O'Donovan 1999 included both surgically and conservatively‐treated participants. Thus we adjusted the scope of our fourth comparison to "different methods of management after initial conservative or surgical treatment" to reflect this.
Agreements and disagreements with other studies or reviews
We did not identify any other systematic reviews on fingertip injuries in children during our literature search.
Authors' conclusions
Implications for practice.
There is a lack of evidence from RCTs to inform all key treatment decisions for the management of fingertip entrapment injuries in children.
The low quality of evidence from one trial means that we do not have conclusive evidence that prophylactic use of antibiotics after surgical repair fails to reduce risk of infection. The two children who experienced infection had more severe wounds (partial fingertip amputation). Similarly, the low quality evidence from another trial has not enabled us to draw firm conclusions regarding the effect on healing time or complications (infection, skin necrosis) at four‐week follow‐up between a silicone net dressing and a paraffin gauze dressing when applied post‐surgery or after simple wound irrigation. However, the silicone net dressing may be less likely to adhere to the wound, and its removal less likely to cause distress for the child in the first week. There is no evidence about longer term outcomes, including fingertip function, nail deformity or nail growth.
Implications for research.
The absence of high‐quality evidence regarding interventions in fingertip entrapment injuries in children demonstrated in this review highlights the need for further research in this area. One key area of focus for future RCTs is the comparison of surgical management with conservative management for fingertip injuries in children. While blinding of participants and personnel and outcome assessment is difficult for this comparison, it should be done where possible for other comparisons. Outcome assessment should include fingertip function, nail growth and nail deformity at a minimum of three months post treatment.
What's new
| Date | Event | Description |
|---|---|---|
| 14 May 2019 | Amended | Declarations of interest updated. |
Acknowledgements
This review was produced within the Cochrane Bone, Joint and Muscle Trauma Group. We thank Alwyn Abraham, Lesley Gillespie, Keith Hill, Maggie Wilkinson and Helen Handoll for valuable comments on drafts of the protocol and review. We also acknowledge the help of Joanne Elliott in developing the search strategies and Lindsey Elstub and Laura MacDonald for editorial support.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley Online Library)
#1 MeSH descriptor: [Finger Injuries] explode all trees (87) #2 (fingertip or finger tip or finger‐tip):ti,ab,kw (339) #3 (finger near/3 (nail or nail bed or nail‐bed)):ti,ab,kw (23) #4 (distal and phalan* and (fract or injur*)):ti,ab,kw (8) #5 MeSH descriptor: [Nails] explode all trees and with qualifiers: [Injuries ‐ IN]2 #6 #1 or #2 or #3 or #4 or #5 (442) #7 MeSH descriptor: [Child] explode all trees (65) #8 MeSH descriptor: [Infant] explode all trees (11959) #9 MeSH descriptor: [Adolescent] explode all trees (69709) #10 MeSH descriptor: [Adult] explode all trees (845) #11 #9 not #10 (69631) #12 MeSH descriptor: [Pediatrics] explode all trees (459) #13 (paediatr* or pediatr* or neonate* or baby or babies or infant* or child* or toddler* or teenage* or adolescent*):ti,ab,kw (137302) #14 #7 or #8 or #11 or #12 or #13 (137311) #15 #6 and #14 (90) [trials]
MEDLINE (Ovid Online)
1 Finger Injuries/ (7770) 2 (fingertip or finger tip or finger‐tip).tw. (2709) 3 (finger adj3 (nail or nailbed or nail‐bed)).tw. (189) 4 (distal and phalan* and (fract* or injur*)).tw. (607) 5 Nails/in [Injuries] (323) 6 or/1‐5 (10624) 7 exp Child/ (1476682) 8 exp Infant/ (897755) 9 Adolescent/ not exp Adult/ (457239) 10 exp Pediatrics/ (41291) 11 (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or toddler* or teenage* or adolescen*).tw. (1314186) 12 or/7‐11 (2366976) 13 and/6,12 (1986) 14 Randomized controlled trial.pt. (346797) 15 Controlled clinical trial.pt. (85759) 16 randomized.ab. (249438) 17 placebo.ab. (137469) 18 Drug therapy.fs. (1603091) 19 randomly.ab. (178468) 20 trial.ab. (257183) 21 groups.ab. (1160728) 22 or/14‐21 (2992626) 23 exp Animals/ not Humans/ (3804093) 24 22 not 23 (2543370) 25 and/13,24 (145)
EMBASE (Ovid Online)
1 Finger Injury/ (5101) 2 (fingertip or finger tip or finger‐tip).tw. (3323) 3 (finger adj3 (nail or nailbed or nail‐bed)).tw. (251) 4 (distal and phalan* and (fract* or injur*)).tw. (690) 5 Nail/ (4740) 6 injur*.ti,ab. (589562) 7 5 and 6 (155) 8 or/1‐4,7 (8996) 9 exp Child/ (1659196) 10 exp Infant/ (516239) 11 Adolescent/ not exp Adult/ (453190) 12 exp Pediatrics/ (69487) 13 (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or toddler* or teenage* or adolescen*).tw. (1621497) 14 or/9‐13 (2460390) 15 8 and 14 (1437) 16 Randomized Controlled Trial/ (341042) 17 Clinical Trial/ (877056) 18 Controlled Clinical Trial/ (395530) 19 Randomization/ (61250) 20 Single Blind Procedure/ (17288) 21 Double Blind Procedure/ (114243) 22 Crossover Procedure/ (36732) 23 Placebo/ (216837) 24 Prospective Study/ (231233) 25 ((clinical or controlled or comparative or placebo or prospective* or randomi#ed) adj3 (trial or study)).tw. (683902) 26 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (166520) 27 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (153035) 28 (cross?over* or (cross adj1 over*)).tw. (65427) 29 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (211245) 30 RCT.tw. (11295) 31 or/16‐30 (1788623) 32 Case Study/ or Abstract Report/ or Letter/ (884994) 33 31 not 32 (1751882) 34 15 and 33 (101)
WHO International Clinical Trials Registry Platform
Advanced search Recruitment status: ALL
1 finger injuries (title) (2) 2 finger injuries (condition) (2) 3 fingertip OR finger‐tip OR finger tip (title) (2) 4 fingertip OR finger‐tip OR finger tip (condition) (8) 5 nail injury (title) (0) 6 nail injury (condition) (0) 7 entrapment (title) (1) 8 entrapment (condition) (0) 9 finger nail (title) (0) 10 finger nail (condition) (0) 11 nail bed (title) (0) 12 nail bed (condition) (0)
Data and analyses
Comparison 1. Prophylactic antibiotics versus no antibiotics following surgical repair.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Infection | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 2. Silicone net dressing versus paraffin gauze following surgical or conservative management.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Complications | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Infection | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Skin necrosis | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Healing time in weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of dressing changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Low level of stress experienced by child during dressing change | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Week 1 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Week 2 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Week 3 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Week 4 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Low degree of wound adhesion during dressing change | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Week 1 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Week 2 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Week 3 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Week 4 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Altergott 2008.
| Methods | Randomised using computer‐generated randomisation list. Participants and assessors were not blinded at follow‐up. Trial terminated earlier than expected due to staffing issues. Loss to follow‐up: 7/146 (4 unable to be reached by telephone, 2 insufficient data provided, 1 requesting withdrawal from trial). In addition, 4/146 removed from trial because they received antibiotics for an unrelated reason during the trial period. | |
| Participants | Children's Hospital, Los Angeles, CA, USA Period of recruitment: September 2000 to July 2004. 146 participants enrolled, 135 followed to trial completion. All participants under 18 years of age presenting to the emergency department with fingertip injuries distal to the distal interphalangeal joint, undergoing surgical repair. Exclusion criteria: time from injury to repair greater than 8 hours; diabetes; oncological disorder; immune deficiency; bleeding disorder; regular steroid use; grossly contaminated wound; currently taking antibiotics; previous allergy to cephalosporins. Participant characteristics provided for the 135 followed up at 7 days. Injuries included ranged in severity from simple laceration to partial amputation (51/135 participants) and complete amputation (6/135 participants). The mechanism of injury was a crush injury in the majority of cases (112/135). 77 male, 58 female participants. Mean age 3.1 years, range 6 months to 6.1 years. |
|
| Interventions | Intervention and randomisation occurred after surgical repair of lacerations using a standardised protocol. 1. Treatment group. Prophylactic antibiotics given (oral cephalexin 50 mg/kg daily in three divided doses for seven days) (randomised = 71; analysed = 66). 2. Control group. No prophylactic antibiotics given (randomised = 75; analysed = 69). Both groups received the same post‐repair instructions regarding elevation, keeping the dressing dry, and returning if signs of wound infection developed. |
|
| Outcomes | Length of follow‐up: wound review after 48 hours; phone call after 7 days. Primary outcome: infection rate after 7 days, as determined by the presence of erythema, tenderness, warmth, purulent discharge or regional lymphadenopathy. If participants' caregiver reported any of these signs via phone at 7 days they were asked to re‐present for confirmation by trial investigators. Secondary outcomes: compliance with antibiotics if in treatment group. |
|
| Notes | Following conclusion of the trial the authors conducted a chart review and found that four cases had become infected outside the seven day window. This suggests that the length of follow‐up was too short and any future studies should be designed to reflect this. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated to treatment or control group using computer‐generated randomisation. |
| Allocation concealment (selection bias) | Low risk | Allocation was made using a randomisation list generated prior to recruitment. Participants were allocated using this list after recruitment. Participants and personnel had no foreknowledge of allocation prior to assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither participants nor personnel were blinded. Investigators were aware at follow‐up if participants had been allocated to the treatment arm as they assessed compliance with antibiotics. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded to participant allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition occurred due to inability to contact participants (4 participants); participants found not to have met inclusion criteria during the trial (e.g. taking antibiotics for an unrelated reason) (4 participants); insufficient data recorded by assessors (2 participants); and requesting withdrawal from trial (1 participant). Participants lost to follow‐up were balanced across groups; 5 (7%) in the intervention group and 6 (8%) in the control group. However, group‐specific reasons for attrition were not reported and therefore balance between the groups cannot be determined. Participants who were lost to follow‐up were statistically significantly older than other participants. An intention‐to‐treat analysis was not conducted. |
| Selective reporting (reporting bias) | Low risk | Results of all outcomes described in the methods were reported. The primary outcome was the same as that published with the WHO International Clinical Trials Registry Platform prior to trial commencement. |
| Other bias | Unclear risk | Participant enrolment in the trial was at the discretion of the clinical team (when inclusion criteria applied). There is the potential for bias if the treating team was more or less likely to enrol participants with more or less severe injuries. |
O'Donovan 1999.
| Methods | Compared two different dressing types for fingertip injuries. Participants were randomised to trial dressing or control dressing irrespective of surgical or conservative treatment; method of randomisation was not stated. Participants and personnel were not blinded to allocation prior to assignment, during the intervention or at follow‐up. All participants enrolled completed the trial; there was no loss to follow‐up. |
|
| Participants | Our Lady's Hospital for Sick Children, Dublin, Ireland. Recruitment over a four‐month period; dates not stated. 45 participants referred by the Emergency Department to the Plastic Surgery department with fingertip injuries involving only the pulp, nail complex or distal phalanx. Participants underwent either surgical or conservative management of their injuries. Exclusion criteria were proximal tendon or nerve injuries, or complex hand injuries involving multiple digits. Injuries ranged from simple lacerations to subtotal or complete amputations (5/45 participants). Participant gender was not reported. Mean age 4.6 years, range 6 months to 11 years. |
|
| Interventions | Intervention occurred post surgical or conservative management of fingertip injury. 1. Intervention group. Participants' wounds dressed with silicone net dressing, dry gauze and cotton bandage (randomised = 20; analysed = 20). 2. Control group. participants' wounds dressed with paraffin gauze, dry gauze and cotton bandage (randomised = 25; analysed = 25). Participants were allocated to intervention or control group irrespective of the mechanism of injury, degree of wound contamination, presence of bony involvement, or surgical or conservative treatment. Conservative treatment (wound irrigation and dressings only) was used for 14 participants (6/20 in the intervention group, 8/25 in the control group). Surgical treatment was used for 31 participants (14/20 in the intervention group, 17/25 in the control group). Surgical treatment included debridement only (7/45 cases), formal nailbed repair where tip vascularity was well preserved (19/45 cases), composite grafts where the amputated tip was replaced (3/45 cases), or local V‐to‐Y advancement flaps where there was exposed bone (2/45 cases). Participants in both groups had their inner dressings changed no more than once per week. |
|
| Outcomes | Participants were followed for four weeks from intervention. Outcomes were mean number of dressing changes until wound healed, as determined by the plastic surgery registrar (criteria not reported); perceived level of stress associated with dressing change using 0 to 3 scoring system where 0 is "happy" and 3 is "hysterical"; degree of wound adhesion using 0 to 3 scoring system where 0 is "dressing slipped off" and 3 is "heavily soaked and still stuck"; and the rate of complications such as infection, uninjured tissue maceration or necrosis. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation method. States "patients were randomly allocated". |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation method. States "patients were randomly allocated into one of two treatment groups, either Mepitel [silicone] or paraffin gauze dressings, regardless of whether the injury was treated conservatively or surgically." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded to allocation at assignment or during the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded to participant group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "All 45 patients complied with the management regime until wound healing was achieved". |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available to compare intended outcomes with those reported in the trial. All outcomes described in the methods were reported on. Outcomes were not described in terms of primary and secondary so it is not possible to determine if outcome priority changed when it was found that neither wound healing time nor infection rate was statistically different between groups. |
| Other bias | Unclear risk | Only participants that had been referred to the plastic surgery unit from the emergency department could potentially be enrolled in the trial. As a proportion of minor fingertip injuries may have been treated in the emergency department without plastics referral, this potentially skews the participant population towards more severe injuries. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barton 1979 | This study examines the outcome following phalangeal shaft fractures; however, no comparison between different interventions is made. |
| Chale 2006 | A randomised comparison of different anaesthesia options in finger lacerations; however, fingertip entrapment injuries are explicitly excluded and the population is not paediatric. |
| Cheng 2004 | A retrospective comparison of outcomes in fractured digits treated with three separate surgical interventions. No randomisation. |
| Claudet 2007 | An epidemiological report discussing entrapment injuries. No comparison made between interventions. |
| Das 1978 | A comparison of outcomes in fingertip injuries treated with three different surgical treatments. The method of group allocation and randomisation is unclear, and the study explicitly excludes those injuries that do not result in pulp loss. This study was excluded because it does not include those injuries that are the focus of this review (as shown in Table 2). |
| De Boer 1981 | A quasi‐randomised comparison of fingertip dressings. The mechanism of injury in participants was unclear. The study states that "four children were among the patients" in one group, inferring that the majority were adults and that there were no children in the other comparison group. |
| Doraiswamy 1999 | A prospective epidemiological report of fingertip injuries. No comparison made between interventions. |
| Douglas 1972 | A quasi‐randomised study comparing conservative with surgical management of digital amputations. These injuries are not consistent with the fingertip injuries of interest to this review (Table 2). |
| Duncan 1993 | A retrospective analysis of outcomes in hand injuries with open fractures. No randomisation used in group allocation and the population is not described as paediatric. |
| Foucher 1994 | A retrospective analysis of outcomes following fingertip pulp loss. No comparison made between different interventions. |
| Halim 1998 | A study measuring outcome following use of a particular fingertip dressing. No comparison drawn to other interventions and the mechanism of injury in participants is unclear. |
| Holm 1974 | A retrospective comparison of conservative and surgical management of fingertip injuries. Participants were not randomly allocated to treatment groups. |
| Illingworth 1974 | A description of management of fingertip entrapment injuries at one centre. No comparison made between different interventions. |
| Inglefield 1995 | An epidemiological report including a description of outcomes following a single intervention in treating fingertip entrapment injuries. No comparison made with other interventions. |
| Innis 1995 | An article describing the mechanism of injury in fingertip entrapment injuries. No comparison made between different treatment interventions. |
| Keramidas 2004 | A randomised trial comparing different anaesthetic modalities in fingertip injuries in adults. Paediatric participants explicitly excluded. |
| Ljungberg 2003 | An epidemiological report discussing fingertip entrapment injuries. No comparison drawn between interventions. |
| Ljungberg 2008 | A retrospective analysis of financial cost associated with paediatric fingertip entrapment injuries. No comparison drawn between treatment modalities. |
| Louis 1980 | An article describing management of open fingertip injuries with a single intervention. Paediatric participants not included, and no comparison made with other interventions. |
| Mennen 1993 | An article describing outcome following use of a particular dressing in fingertip injuries. Mechanism of injury and participant age unclear, and no comparison drawn to other interventions. |
| O'Shaughnessy 1990 | A retrospective comparison of outcome following fingertip entrapment injury treated with different interventions. Participants were not randomly allocated to treatment groups. |
| Rosenthal 1983 | An article describing different techniques of managing fingertip injuries. No comparison between interventions made in terms of outcome. |
| Roser 1999 | A prospective study comparing surgical nailbed repair to nail trephination for subungual haematomas. The interventions were compared sequentially rather than concurrently with the first 25 participants recruited managed operatively and the subsequent 26 participants managed conservatively by trephination. As this allocation process was not randomised or pseudo‐randomised, the study was excluded from the review. |
| Schiller 1957 | A case series describing a single intervention. No comparison made with other interventions. |
| Seaberg 1991 | An observational study of subungual hematomas treated with trephination involving paediatric and non‐paediatric participants. No comparison with other interventions. |
| Shetty 1996 | A letter to the editor describing a comparison of three different treatment modalities in fingertip injuries. The randomisation unclear, and the study did not involve paediatric participants. |
| Strauss 2008 | A quasi‐randomised study comparing suture to glue in the repair of finger‐tip injuries. The study did not examine an exclusively paediatric population ‐ although some children were included, the mean age of the study population was 30.76 years. Further, the mechanism of injury in participants was not clearly defined, and while five were described as "crush‐type" lacerations, it is not clear if these cases were in paediatric participants or in participants outside the scope of this review. The corresponding author was contacted but no longer has access to raw study data, making analysis of any potential subgroup of participants meeting inclusion criteria impossible. |
| Vadivelu 2006 | A prospective epidemiological analysis of fractures in hand injuries in children. No comparison made between different treatment modalities. |
| Whittaker 1994 | A prospective randomised trial comparing two dressings in the treatment of fingertip injuries. The study did not examine an exclusively paediatric population; the mean age of the study population was 31 years. Although four participants in the trial group and three in the control group were children, these participants were not analysed separately. Further, the study included participants with a mechanism of injury outside the scope of this review, including puncture injuries and injuries involving toes. |
| Williamson 1987 | A randomised trial comparing different dressings for use in fingertip entrapment injuries. A combination of crushing and slicing mechanisms of injury included. Participants under 14 years of age explicitly excluded. |
Characteristics of studies awaiting assessment [ordered by study ID]
Alpern 2005.
| Methods | A randomised single‐blinded trial comparing transthecal metacarpal block to traditional digital block for the anaesthesia of finger injuries undergoing treatment in the paediatric emergency department. Trial registered with clinicaltrials.gov in August 2005. Enrolment commenced July 2005. Trial completed August 2007. |
| Participants | Children's Hospital of Philadelphia, Philadelphia, PA, USA. Inclusion criteria were participants under 18 years of age, weighing greater than 10 kg, with finger injuries or infections requiring digital regional anaesthesia but not general anaesthesia; English speaking. Intended recruitment size 92 participants. |
| Interventions | Transthecal metacarpal block versus traditional ring block |
| Outcomes | Success of ring block; complications associated with block; pain experienced with the block; repairing physician satisfaction with the procedure. |
| Notes | This trial was registered in 2005 and was seemingly completed in 2007; however, we could not find any published report of its results. We contacted the registered author directly via email who indicated that the trial manuscript is currently under revision for publication. |
Differences between protocol and review
We made minor changes to the background text and included updated incidence figures from contemporary sources.
In the protocol we proposed a common‐sense approach to the exclusion of studies based on participant age. We have now added a clarification of our intended approach.
In the protocol we planned to exclude trials focusing on the management of fingertip entrapment injuries resulting in amputation or avulsion. While this review continues to focus on those injuries that did not result in amputation, we revised this criterion to indicate that we included studies in which a proportion of injuries resulted in amputation if these injuries were in the minority, were balanced between the comparison groups, and the mechanism of injury was within the scope of the review.
Since one trial included both surgically‐ and conservatively‐treated participants, we adjusted the scope of our fourth comparison from "different methods of post‐surgical treatment" to "different methods of management after initial conservative or surgical treatment", allowing for both categories of patients.
In addition to the outcomes listed in the protocol, we collected data on time to wound healing, dressing changes to wound healing, participant distress at dressing change and wound adhesion of dressing at dressing change. Secondary outcomes we did not list in the protocol but included in this review were the time to healing of the injury, and the requirement for secondary procedures to improve function or appearance.
Because no trials compared similar interventions, we could not conduct statistical assessment for heterogeneity, nor was it possible to undertake a meta‐analysis or any subsequent subgroup or sensitivity analysis. We did not construct a funnel plot to assess reporting bias for the same reason. We made provisions for these elements of the review in the protocol; however, due to the scarcity of available evidence we did not conduct them.
Contributions of authors
Robert Capstick and Henk Giele designed the review, collected and interpreted data. Robert Capstick performed data management, data entry, analysed the data and drafted the review. Henk Giele provided general advice for the review and is the review guarantor.
Sources of support
Internal sources
-
University of Oxford, UK.
Computing, administration and library services (RC, HG)
External sources
-
Monash University, Australia.
Computing, administration and library services (RC)
Declarations of interest
Robert Capstick: none known. Henk Giele: I have received grants and payments for duties relating to hand surgery and non‐surgical aspects of Dupuytren's disease, all of which are unrelated to this review and not influencing this review.
Note added 14 May 2019: The Cochrane Funding Arbiters have judged that this review breaches Cochrane's commercial sponsorship policy, published 8 March 2014, in relation to the following criterion: 'The lead author and more than 50% of all authors must not have received other types of financial support from an industry sponsor with an interest in the review.' Specifically, Henk Giele received personal remuneration from Pfizer who manufacture antibiotics, one of the interventions of interest in the review.
Edited (no change to conclusions)
References
References to studies included in this review
Altergott 2008 {published data only}
- Altergott C. Pediatric fingertip injuries: are antibiotics required?. http://clinicaltrials.gov/show/NCT00300092 (accessed 7 April 2014). [CTG: NCT00300092]
- Altergott C, Garcia FJ, Nager AL. Pediatric fingertip injuries: do prophylactic antibiotics alter infection rates?. Pediatric Emergency Care 2008;24(3):148‐52. [DOI] [PubMed] [Google Scholar]
O'Donovan 1999 {published data only}
- O'Donovan DA, Mehdi SY, Eadie PA. The role of Mepitel silicone net dressings in the management of fingertip injuries in children. Journal of Hand Surgery ‐ British Volume 1999;24(6):727‐30. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Barton 1979 {published data only}
- Barton NJ. Fractures of the shafts of the phalanges of the hand. Hand 1979;11(2):119‐33. [DOI] [PubMed] [Google Scholar]
Chale 2006 {published data only}
- Chale S, Singer AJ, Marchini S, McBride MJ, Kennedy D. Digital versus local anesthesia for finger lacerations: a randomized controlled trial. Academic Emergency Medicine 2006;13(10):1046‐50. [DOI] [PubMed] [Google Scholar]
Cheng 2004 {published data only}
- Cheng HS, Wong LY, Chiang LF, Chan I, Yip TH, Wu WC. Comparison of methods of skeletal fixation for severely injured digits. Hand Surgery 2004;9(1):63‐9. [DOI] [PubMed] [Google Scholar]
Claudet 2007 {published data only}
- Claudet I, Toubal K, Carnet C, Rekhroukh H, Zelmat B, Debuisson C, et al. When doors slam, fingers jam! [Quand les portes claquent, les doigts craquent!]. Archives de Pediatrie 2007;14(8):958‐63. [DOI] [PubMed] [Google Scholar]
Das 1978 {published data only}
- Das SK, Brown HG. Management of lost finger tips in children. Hand 1978;10(1):16‐27. [DOI] [PubMed] [Google Scholar]
De Boer 1981 {published data only}
- Boer P, Collinson PO. The use of silver sulphadiazine occlusive dressings for finger‐tip injuries. Journal of Bone & Joint Surgery ‐ British Volume 1981;63B(4):545‐7. [DOI] [PubMed] [Google Scholar]
Doraiswamy 1999 {published data only}
- Doraiswamy NV. Childhood finger injuries and safeguards. Injury Prevention 1999;5(4):298‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Douglas 1972 {published data only}
- Douglas BS. Conservative management of guillotine amputation of the finger in children. Australian Paediatric Journal 1972;8(2):86‐9. [DOI] [PubMed] [Google Scholar]
Duncan 1993 {published data only}
- Duncan RW, Freeland AE, Jabaley ME, Meydrech EF. Open hand fractures: an analysis of the recovery of active motion and of complications. Journal of Hand Surgery ‐ American Volume 1993;18(3):387‐94. [DOI] [PubMed] [Google Scholar]
Foucher 1994 {published data only}
- Foucher G, Dallaserra M, Tilquin B, Lenoble E, Sammut D. The Hueston flap in reconstruction of fingertip skin loss: Results in a series of 41 patients. Journal of Hand Surgery ‐ American Volume 1994;19(3):508‐15. [DOI] [PubMed] [Google Scholar]
Halim 1998 {published data only}
- Halim AS, Stone CA, Devaraj VS. The Hyphecan cap: A biological fingertip dressing. Injury 1998;29(4):261‐3. [DOI] [PubMed] [Google Scholar]
Holm 1974 {published data only}
- Holm A, Zachariae L. Fingertip lesions. An evaluation of conservative treatment versus free skin grafting. Acta Orthopaedica Scandinavica 1974;45(3):382‐92. [DOI] [PubMed] [Google Scholar]
Illingworth 1974 {published data only}
- Illingworth CM. Trapped fingers and amputated finger tips in children. Journal of Pediatric Surgery 1974;9(6):853‐8. [DOI] [PubMed] [Google Scholar]
Inglefield 1995 {published data only}
- Inglefield CJ, D'Arcangelo M, Kolhe PS. Injuries to the nail bed in childhood. Journal of Hand Surgery ‐ British Volume 1995;20(2):258‐61. [DOI] [PubMed] [Google Scholar]
Innis 1995 {published data only}
- Innis PC. Office evaluation and treatment of finger and hand injuries in children. Current Opinion in Pediatrics 1995;7(1):83‐7. [DOI] [PubMed] [Google Scholar]
Keramidas 2004 {published data only}
- Keramidas EG, Rodopoulou SG, Tsoutsos D, Miller G, Ioannovich J. Comparison of transthecal digital block and traditional digital block for anesthesia of the finger. Plastic and Reconstructive Surgery 2004;114(5):1131‐4. [DOI] [PubMed] [Google Scholar]
Ljungberg 2003 {published data only}
- Ljungberg E, Rosberg HE, Dahlin LB. Hand injuries in young children. Journal of Hand Surgery ‐ British Volume 2003;28(4):376‐80. [DOI] [PubMed] [Google Scholar]
Ljungberg 2008 {published data only}
- Ljungberg EM, Carlsson KS, Dahlin LB. Cost per case or total cost? The potential of prevention of hand injuries in young children ‐ retrospective and prospective studies. BMC Pediatrics 2008;8:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Louis 1980 {published data only}
- Louis DS, Palmer AK, Burney RE. Open treatment of digital tip injuries. JAMA 1980;244(7):697‐8. [PubMed] [Google Scholar]
Mennen 1993 {published data only}
- Mennen U, Wiese A. Fingertip injuries management with semi‐occlusive dressing. Journal of Hand Surgery ‐ British Volume 1993;18(4):416‐22. [DOI] [PubMed] [Google Scholar]
O'Shaughnessy 1990 {published data only}
- O'Shaughnessy M, McCann J, O'Connor TP, Condon KC. Nail re‐growth in fingertip injuries. Irish Medical Journal 1990;83(4):136‐7. [PubMed] [Google Scholar]
Rosenthal 1983 {published data only}
- Rosenthal EA. Treatment of fingertip and nail bed injuries. Orthopedic Clinics of North America 1983;14(4):675‐97. [PubMed] [Google Scholar]
Roser 1999 {published data only}
- Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. Journal of Hand Surgery ‐ American Volume 1999;24(6):1166‐70. [DOI] [PubMed] [Google Scholar]
- Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children (Abstract). Orthopaedic Transactions 1997;21(1):121. [DOI] [PubMed] [Google Scholar]
Schiller 1957 {published data only}
- Schiller C. Nail replacement in finger tip injuries. Plastic and Reconstructive Surgery 1957;19(6):521‐30. [DOI] [PubMed] [Google Scholar]
Seaberg 1991 {published data only}
- Seaberg DC, Angelos WJ, Paris PM. Treatment of subungual hematomas with nail trephination: A prospective study. American Journal of Emergency Medicine 1991;9(3):209‐10. [DOI] [PubMed] [Google Scholar]
Shetty 1996 {published data only}
- Shetty PC, Dicksheet S, Scalea T. Fingertip injuries: immediate reconstruction versus delayed healing [letter]. American Journal of Emergency Medicine 1996;14(1):103‐4. [DOI] [PubMed] [Google Scholar]
Strauss 2008 {published data only}
- Strauss EJ, Weil WM, Jordan C, Paksima N. A prospective, randomized, controlled trial of 2‐octylcyanoacrylate versus suture repair for nail bed injuries. Journal of Hand Surgery 2008;33(2):250‐3. [DOI] [PubMed] [Google Scholar]
Vadivelu 2006 {published data only}
- Vadivelu R, Dias JJ, Burke FD, Stanton J. Hand injuries in children: a prospective study. Journal of Pediatric Orthopedics 2006;26(1):29‐35. [DOI] [PubMed] [Google Scholar]
Whittaker 1994 {published data only}
- Whittaker S. A dressing for the occasion? A comparative trial of two dressings for digit injuries. Professional Nurse 1994;9(11):729‐33. [PubMed] [Google Scholar]
Williamson 1987 {published data only}
- Williamson DM, Sherman KP, Shakespeare DT. The use of semipermeable dressings in fingertip injuries. Journal of Hand Surgery ‐ British Volume 1987;12(1):125‐6. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Alpern 2005 {published data only}
- Alpern ER. Cochrane systematic review ‐ 2005 study [personal communication]. Email to: E Alpern 11 February 2014.
- Alpern ER. Transthecal metacarpal block versus traditional digital block for painful finger procedures in children. WHOICTRP: http://apps.who.int/trialsearch/Trial.aspx?TrialID=NCT00130104 (accessed 20 Sept 2013).
Additional references
De Alwis 2006
- Alwis W. Fingertip injuries. Emergency Medicine Australasia 2006;18(3):229‐37. [DOI] [PubMed] [Google Scholar]
Doraiswamy 2000
- Doraiswamy NV, Baig H. Isolated finger injuries in children ‐ incidence and aetiology. Injury 2000;31(8):571‐3. [DOI] [PubMed] [Google Scholar]
Evans 2000
- Evans DM, Bernardis C. A new classification for fingertip injuries. Journal of Hand Surgery ‐ British Volume 2000;25(1):58‐60. [DOI] [PubMed] [Google Scholar]
Fetter‐Zarzeka 2002
- Fetter‐Zarzeka A, Joseph MM. Hand and fingertip injuries in children. Pediatric Emergency Care 2002;18(5):341‐5. [DOI] [PubMed] [Google Scholar]
Garvin 2007
- Garvin S, Ridal J. Finger‐trapping: a scoping study. Glasgow (UK): Building Research Establishment Report; 2007 Jan. [Report Number: 231851‐1]
Gellman 2009
- Gellman H. Fingertip‐nail bed injuries in children: current concepts and controversies of treatment. Journal of Craniofacial Surgery 2009;20(4):1033‐5. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Inglefield 1995a
- Inglefield CJ, D'Arcangelo M, Kolhe PS. Injuries to the nail bed in childhood. Journal of Hand Surgery ‐ British Volume 1995;20(2):258‐61. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Macgregor 1999
- Macgregor DM, Hiscox JA. Fingertip trauma in children from doors. Scottish Medical Journal 1999;44(4):114‐5. [DOI] [PubMed] [Google Scholar]
Review Manager (RevMan) [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Shah 2012
- Shah SS, Rochette LM, Smith GA. Epidemiology of pediatric hand injuries presenting to United States emergency departments, 1990 to 2009. Journal of Trauma and Acute Care Surgery 2012;72(6):1688‐94. [DOI] [PubMed] [Google Scholar]
West 2011
- West E, Smith J, Mykula R, Tan E, Capstick R. Paediatric Fingertip Injuries. Regional Audit. Portsmouth, UK: Oxford/Wessex Deanery of Plastic Surgery, June 2011.


