Abstract
Background
Fractures of the femoral shaft in children are relatively uncommon but serious injuries that disrupt the lives of children and their carers and can result in significant long‐term disability. Treatment involves either surgical fixation, such as intramedullary nailing or external fixation, or conservative treatment involving prolonged immobilisation, often in hospital.
Objectives
To assess the effects (benefits and harms) of interventions for treating femoral shaft fractures in children and adolescents.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma (BJMT) Group Specialised Register (accessed 16 August 2013), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2013 Issue 7), MEDLINE (1946 to August Week 1 2013), EMBASE (1980 to 2012 week 9), CINAHL (16 August 2013), clinical trials registries, conference proceedings and reference lists; and contacted trial authors and experts in the field.
Selection criteria
Randomised and quasi‐randomised controlled trials comparing conservative and surgical interventions for diaphyseal fractures of the femur in children under 18 years of age. Our primary outcomes were functional outcome measures, unacceptable malunion, and serious adverse events.
Data collection and analysis
Two authors independently screened and selected trials, assessed risk of bias and extracted data. We assessed the overall quality of the evidence for each outcome for each comparison using the GRADE approach. We pooled data using a fixed‐effect model.
Main results
We included 10 trials (six randomised and four quasi‐randomised) involving a total of 527 children (531 fractures). All trials were at some risk of bias, including performance bias as care provider blinding was not practical, but to a differing extent. Just one trial was at low risk of selection bias. Reflecting both the risk of bias and the imprecision of findings, we judged the quality of evidence to be 'low' for most outcomes, meaning that we are unsure about the estimates of effect. Most trials failed to report on self‐assessed function or when children resumed their usual activities. The trials evaluated 10 different comparisons, belonging to three main categories.
Surgical versus conservative treatment
Four trials presenting data for 264 children aged 4 to 12 years made this comparison. Low quality evidence (one trial, 101 children) showed children had very similar function assessed using the RAND health status score at two years after surgery (external fixation) compared with conservative treatment (spica cast): mean 69 versus 68. The other three trials did not report on function. There was moderate quality evidence (four trials, 264 children, aged 4 to 12 years, followed up 3 to 24 months) that surgery reduced the risk of malunion (risk ratio (RR) 0.29, 95% confidence interval (CI) 0.15 to 0.59, 4 trials). Assuming an illustrative baseline risk of 115 malunions per 1000 in children treated conservatively, these data equate to 81 fewer (95% CI 47 to 97 fewer) malunions per 1000 in surgically‐treated children. Conversely, low quality evidence indicated that there were more serious adverse events such as infections after surgery (RR 2.39, 95% CI 1.10 to 5.17, 4 trials). Assuming an illustrative baseline risk of 40 serious adverse events per 1000 for conservative treatment, these data equate to 56 more (95% CI 4 to 167 more) serious adverse events per 1000 children treated surgically. There was low quality evidence (one trial, 101 children) of similar satisfaction levels in children and parents with surgery involving external fixation and plaster cast only. However, there was low quality evidence (one trial, 46 children) that more parents were satisfied with intramedullary nailing than with traction followed by a cast, and that surgery reduced the time taken off from school.
Comparisons of different methods of conservative treatment
The three trials in this category made three different comparisons. We are very unsure if unacceptable malunion rates differ between immediate hip spica versus skeletal traction followed by spica in children aged 3 to 10 years followed up for six to eight weeks (RR 4.0, 95% CI 0.5 to 32.9; one trial, 42 children; very low quality evidence). Malunion rates at 5 to 10 years may not differ between traction followed by functional orthosis versus traction followed by spica cast in children aged 5 to 13 years (RR 0.98, 95% CI 0.46 to 2.12; one trial, 43 children; low quality evidence). We are very unsure (very low quality evidence) if either function or serious adverse events (zero events reported) differ between single‐leg versus double‐leg spica casts (one trial, 52 young children aged two to seven years). Low quality evidence on the same comparison indicates that single‐leg casts are less awkward to manage by parents, more comfortable for the child and may require less time off work by the caregiver.
Comparisons of different methods of surgical treatment
The three trials in this category made three different comparisons. Very low quality evidence means that we are very unsure if the rates of malunion, serious adverse events, time to return to school or parental satisfaction actually differ in children whose fractures were fixed using elastic stable intramedullary nailing or external fixation (one trial, 19 children). The same applies to the rates of serious adverse events and time to resume full weight‐bearing in children treated with dynamic versus static external fixation (one trial, 52 children). Very low quality evidence (one trial, 47 children) means that we do not know if malunion, serious adverse events and time to resume weight‐bearing actually differ between intramedullary nailing versus submuscular plating. However, there could be more difficulties in plate removal subsequently.
Authors' conclusions
There is insufficient evidence to determine if long‐term function differs between surgical and conservative treatment. Surgery results in lower rates of malunion in children aged 4 to 12 years, but may increase the risk of serious adverse events. Elastic stable intramedullary nailing may reduce recovery time.
There is insufficient evidence from comparisons of different methods of conservative treatment or of different methods of surgical treatment to draw conclusions on the relative effects of the treatments compared in the included trials.
Plain language summary
Different methods of treating fractures of the shaft of the thigh bone in children and adolescents
Although uncommon, fractures of the femoral shaft (thigh bone) in children may require prolonged treatment in hospital and sometimes surgery. This can cause significant discomfort and can disrupt the lives of the children and their familles. This review compared different methods of treating these fractures. Surgical treatment comprises different methods of fixing the broken bones, such as internally‐placed nails, or pins incorporated into an external frame (external fixation). Non‐surgical or conservative treatment usually involves different types of plaster casts with or without traction (where a pulling force is applied to the leg).
We searched for studies in the medical literature until August 2013. The review includes 10 randomised or quasi‐randomised controlled trials that recruited 527 children. Four trials compared different surgical versus non‐surgical treatments; three compared different methods of non‐surgical treatment and three compared different methods of surgical treatment. Generally we are unsure about the results of these trials because some were at risk of bias, some results were contradictory and usually there was too little evidence to rule out chance findings. Most trials failed to report on self‐assessed function or when children resumed their usual activities.
Comparing surgical versus non‐surgical treatment
Low quality evidence (one trial, 101 children) showed children had similar function at two years after having surgery, involving external fixation, compared with those treated with a plaster cast. The other three trials did not report this outcome. There was moderate quality evidence (four trials, 264 children, aged 4 to 12 years, followed up for 3 to 24 months) that surgery reduced the risk of malunion (the leg is deformed) compared with non‐surgical treatment. However, low quality evidence (four trials) indicated that there were more serious adverse events such as infections after surgery. There was low quality evidence (one trial, 101 children) of similar satisfaction levels in children and parents with surgery involving external fixation and plaster cast only. However, there was low quality evidence (one trial, 46 children) that more parents were satisfied with surgery involving an internal nail than with traction followed by a cast and that surgery reduced the time taken off from school.
Comparing various non‐surgical treatments
Very low quality evidence means that we are very unsure if the rates of malunion differ or not between children treated with immediate plaster casts versus with traction followed by plaster cast (one trial, 42 children), or between children treated with traction followed by either a functional orthosis (a brace or cast that allows some movement) or a cast (one trial, 43 children). We are very unsure if either function or serious adverse events differ between young children (aged two to seven years) immobilised in single‐leg versus double‐leg casts (one trial, 52 children). However, single‐leg casts appear to be easier to manage by parents and more comfortable for the child.
Comparing various surgical treatments
Very low quality evidence means that we are very unsure if the rates of malunion, serious adverse events, time to return to school or parental satisfaction actually differ in children whose fractures were fixed using internal nails or external fixation (one trial, 19 children). The same applies to the rates of serious adverse events and time to resume full weight‐bearing in children treated with dynamic (less rigid) versus static external fixation (one trial, 52 children). Very low quality evidence (one trial, 47 children) means that we do not know if malunion, serious adverse events and time to resume weight‐bearing actually differ between intramedullary nailing versus submuscular plating. However, there could be more difficulties in plate removal subsequently.
Conclusions
This review found insufficient evidence to determine if long‐term function differs between surgical and conservative treatment of thigh bone fractures in children aged 4 to 12 years. It found surgery resulted in lower rates of malunion but increased the risk of serious adverse events, such as infections. It found internal nailing may speed up recovery.
The review found there was insufficient evidence from comparisons of different methods of non‐surgical treatment to clearly show that any type of non‐surgical treatment is better than any other. The same conclusion applies to comparisons of different methods of surgical treatment.
Summary of findings
Summary of findings for the main comparison. Surgical interventions compared to conservative interventions for treating femoral shaft fractures in children and adolescents.
| What are the effects of surgical interventions compared with conservative interventions for treating femoral shaft fractures in children and adolescents? | ||||||
| Participant or population: Children and adolescents with femoral shaft fractures Settings: In hospital; high‐ and middle‐income countries Interventions: Surgical interventions (external fixation, intramedullary pin fixation, elastic stable intramedullary nailing‐ESIN)¹ Comparisons: Conservative interventions (spica cast, dynamic skeletal traction casting, skeletal traction followed by casting)¹ | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conservative interventions | Surgical interventions | |||||
| Functional outcomes Follow‐up: 2 years | The mean functional outcome score was 68 points on the RAND child health status scale | The mean functional outcome score was 1 point higher (2.2 lower to 4.2 higher) | 101 (1 study) | ⊕⊕⊝⊝ low² | This trial compared external fixation versus immediate hip spica cast | |
| Unacceptable malunion Assessed by imaging Follow‐up: 3 to 24 months | 115 per 1000³ | 34 per 1000 (18 to 68) | RR 0.29 (0.15 to 0.59) | 264 (4 studies) | ⊕⊕⊕⊝ moderate⁴ | |
| Serious adverse events Follow‐up: 3 to 24 months | 40 per 1000³ | 96 per 1000 (44 to 207) | RR 2.39 (1.10 to 5.17) | 264 (4 studies) | ⊕⊕⊝⊝ low⁵ | Note: there was great variety and severity of the reported adverse events. Where confirmed, superficial infection that was readily resolved by antibiotics was not included. |
| Time to return to usual activities⁶(time to return to school) | The mean time to return to school with conservative treatment was 31.5 days | The mean time to return to school was 32.8 days fewer (42.5 to 23.1 days fewer) | 46 (1 study) | ⊕⊕⊝⊝ low₇ | This trial compared elastic stable intramedullary nail (ESIN) versus traction followed by spica cast | |
| Child satisfaction Assessed by an ordinal rating scale (11 points): very unhappy to very happy Follow‐up: 2 years | The mean child satisfaction score with immediate spica cast was 6.8 on the 11‐point ordinal scale | The mean child satisfaction with external fixation was 0.8 higher (0.61 lower to 2.21 higher) | 101 (1 study) | ⊕⊕⊝⊝ low₈ | This trial compared external fixation versus immediate hip spica cast | |
| Parent satisfaction Rated as excellent or good Follow‐up: 24 weeks | 739 per 1000 | 990 per 1000 (776 to 1000) | RR 1.34 (1.05 to 1.73) | 46 (1 study) | ⊕⊕⊝⊝ low⁹ | This trial compared external fixation versus immediate hip spica cast. In another study, parental satisfaction did not differ between external fixation versus immediate spica cast on an 11‐point ordinal scale (mean difference ‐0.10, 95% CI ‐0.49 to 0.29) |
| Resource use and other costs | See comment | See comment | Not estimable | ‐ | See comment | The length of hospital stay reported in 4 studies varied considerably, with direction and size of effects markedly different. One study, conducted in the Phillipines, reported surgical treatment was approximally 4 times more costly ($844 versus $216 at 2008 costs) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1. The four trials making this comparison compared different methods of surgery with different conservative intervention. The four specific comparisons were:
- External fixation versus immediate hip spica cast (101 children aged 4 to 10 years)
- Intramedullary pin fixation plus spica cast versus skeletal traction followed by spica cast (66 children aged 6 to 11 years)
- Elastic stable intramedullary nail (ESIN) versus traction followed by spica cast (46 children aged 6 to 12 years)
- Elastic stable intramedullary nailing (ESIN) versus dynamic skeletal traction spica casting (DSTSC) (51 children aged 5 to 12 years)
2. This was downgraded two levels for very serious imprecision. There were no serious study limitations (although the trial was at high risk of performance bias, we did not think this affected effect estimates), and no serious indirectness (this trial included children aged 4 to 10 years and used standard methods; it was conducted in high‐income countries but there is no reason to expect significantly different estimates in other settings where external fixation is offered and in older children or adolescents). 3. The assumed risk is based on the medium control risk across the studies.
4. This was downgraded one level for serious imprecision: while the 95% Ci of the effect estimate appreciably favoured conservative treatment, the number of events and participants was smaller than the optimal information size. There were no serious study limitations; the quasi‐randomised study was judged to be at high risk of selection bias but contributed only 13% weight in the pooled analysis. Removal of the data from this trial did not alter the pooled results significantly. There was no serious indirectness: the trials included children aged 3 years to adolescence and used standard methods. 5. This was downgraded one level for serious study limitations (removal of the quasi‐randomised study at high risk of selection bias altered the pooled effect estimates from favouring conservative treatment to no significant difference between interventions); and one level for serious imprecision (while the 95% CI of the effect estimate favoured conservative treatment, the number of events and participants was smaller than the optimal information size). 6. This outcome was presented in various ways; such as time to end of treatment; time to independent walking; time to return to school. We present the lattermost here.
7. This was downgraded one level for serious study limitations (reflecting performance and detection bias from lack of blinding), and one level for serious imprecision (though the 95% CI of the effect estimate indicated appreciable benefit for surgery, data were from only one small trial that did not fulfil the requirements for an optimal information size).
8. This was downgraded two levels for very serious imprecision: the 95% CI of the effect estimate indicated appreciable benefit with both interventions and data were from only one small trial.
9. This was downgraded one level for inconsistency in results and one level for serious imprecision: the 95% CI of the effect estimate indicates non‐appreciable and appreciable benefits with nailing. but data were from only one small study.
Background
Description of the condition
The femur is the thigh‐ or upper‐leg bone. The shaft, or diaphysis, is the long central portion of the femur that lies between the top end (proximal femur) at the hip and the lower end (distal femur) at the knee. Shaft or diaphyseal fractures of the femur are uncommon but significant injuries in children, constituting less than 2% of all skeletal injuries in children (Flynn 2006). The injury requires prolonged immobilisation or surgery that can result in significant morbidity. It is the most common orthopaedic injury amongst children requiring hospital admission (Loder 2006). These fractures are sustained more commonly in early childhood and adolescence (Flynn 2006). In normal children a significant force is required to sustain this injury and consequently displaced fractures are common. The commonest causes of femoral shaft fractures are falls and road traffic accidents; however, in children under walking age, abuse needs to be considered (Bridgman 2004).
A common method used to classify diaphyseal femur fractures in children is descriptive labelling into: 1) transverse, spiral or oblique; 2) comminuted (multiple fragments) or non‐comminuted; and 3) open (fractured bone is exposed to the outside) or closed fractures (Flynn 2006). Open fractures are further subclassified as Gustilo and Anderson Type I to III based on the velocity of injury, contamination and soft tissue disruption (Gustilo 1976). Type III of the Gustilo and Anderson classification is further subdivided as A, B and C based on severity of soft tissue injury, energy of trauma, periosteal stripping and need for vascular reconstruction (Gustilo 1984). According to the Arbeitsgemeineschaft fur Osteosynthesefragen (AO) paediatric comprehensive classification of long bone fractures (Slongo 2007), femoral shaft fractures are classified as category 32‐D. Sub‐categories 32‐D 4.1 (complete transverse with an obliquity of 30º or less) and 32‐D 5.1 (complete oblique or spiral more than 30º) are simple fractures. Wedge/multi‐fragmentary fractures are subcategorised into 32‐D 4.2 (multi‐fragmentary transverse 30º or less) and 32 D 5.2 (multi‐fragmentary oblique or spiral more than 30º). Fracture instability can result from oblique/spiral fracture geometry, comminution and soft tissue disruption.
Description of the intervention
These fractures may be treated conservatively (without surgery) or surgically. The choice of treatment is influenced by age and other modifiers such as the size of the child, the ability to tolerate a spica cast, stability of fracture reduction, fracture pattern, the weight of the child, the nature of injury (open/pathological fractures), the presence or absence of neighbouring injuries, polytrauma and open injuries.
Displaced fractures can be reduced (the fractured parts are put back into place) using closed (traction, manipulation) or open (the bone is surgically exposed, allowing direct repositioning) techniques.
The main types of conservative interventions are:
Pavlik harness: this is a sling with chest, shoulder and leg straps commonly used for developmental dysplasia of the hip. It is useful for immobilising the fracture in flexion and abduction and is comfortable for children under six months of age.
Bryant's traction: this allows an infant to be placed on a splint bed frame with traction on the lower limbs at 90º to the hips, with the knees mildly flexed. Monitoring the vascular status is vital to avoid complications and this form of traction can be used in children under three years of age and less than 20 pounds in weight.
Hip spica casting: a plaster cast is applied from the subcostal region to the toes on the affected side, with or without preliminary traction. A safe and effective position is 30º of abduction, 30º to 40º of flexion and external rotation at the hip.
Functional cast bracing is another type of cast which allows movement of the adjacent joints (hip and knee). It is considered more suitable for lower shaft fractures.
The main types of surgical interventions are:
Intramedullary nailing: one or more titanium or stainless steel nails are inserted into the medullary canal of the femur. Flexible intramedullary nailing uses pre‐bent nails that are introduced from either side of the femur on the diaphyseal side of the growth plate. In contrast, the rigid trochanteric nail is inserted down through the greater trochanter, thus through the growth plate, and into the medullary canal.
External fixation: pins inserted, usually percutaneously (through the skin) or with small incisions, into the femur, are attached to an external frame.
Plate fixation: a metal plate is fixed by screws to the femur.
Treatment choices in children younger than two years are generally Bryant's traction, a Pavlik harness and immediate spica casting. Treatment for children aged between three and five years is often an immediate spica cast with a move towards flexible nailing in certain societies. Occasionally for an unstable fracture an initial period of traction may be required prior to application of a spica cast to prevent shortening, more so in older children. In children older than six years, flexible intramedullary nailing is currently favoured. The main disadvantage is that these nails are less suitable for unstable fracture patterns and in heavier children. In contrast, the rigid trochanteric nail, which affords stronger fixation, is generally preferred in children over the age of 12 years as they have minimal residual longitudinal growth potential at the greater trochanter. Thus growth disturbance is not an issue. External fixation and plating are reserved for specific indications across all age groups such as open or unstable fractures or multiple injuries.
The above interventions are detailed in standard orthopaedic textbooks (Flynn 2006) and in the American Academy of Orthopaedic Surgeons (AAOS) practice guidelines (Kocher 2010).
How the intervention might work
Union occurs rapidly in a fractured shaft of femur in children and these injuries have a good remodelling potential, whereby the bone naturally returns to its normal shape. This remodelling potential allows for some tolerance regarding the initial deformity of the healed bone. For example, acceptable angulation in the coronal plane (deformity either out to the back or front of the normal line along the length of the femur), and in the sagittal plane (deformity to either side along the length of the femur) ranges from 30º at birth, to 15º at 10 years (Flynn 2006). Similarly, remodelling with up to 15 mm of shortening can be compensated in children up to 12 years by growth acceleration (Malkawi 1986). Rotational malposition of greater than 10º especially in the upper one third of the femur is considered malaligned (Resch 1989). Malalignment, angulation and leg‐length discrepancy are the main consequences of failed treatment for these fractures. These can manifest as in‐toeing (foot points inwards) or out‐toeing (foot points outwards), shortening, and rotated limbs.
A Pavlik harness, different methods of traction (Bryant's, skin and skeletal traction), functional bracing and hip spica maintain the length and alignment of the femur while union occurs. By allowing movement of the adjacent joints, functional bracing may allow earlier mobilisation and return to normal activities. All these methods rely on the ability of the bone to remodel in children.
There has been a noticeable shift away from conservative management in recent years for paediatric femoral shaft fractures. Economic considerations and convenience have played a role in this swing to operative management since it allows shorter hospital stays and less care during recuperation. Surgery, however, comes at the risk of surgical complications, including infection, neurovascular injury and damage to the growth plate. Often a second operation is required for implant removal.
By stabilising the fracture, intramedullary nails should enable earlier weight‐bearing. Flexible nails allow a small degree of motion at the fracture site that helps to produce bridging callus formation. Rigid intramedullary nails act as load‐sharing devices, providing adequate fixation for larger and heavier children and adolescents.
External fixation may be associated with pin track infection. Although the surgery required is less invasive, the external frame may be less acceptable to patients. There is also some risk of subsequent fracture at a pin site for a short period after external fixator removal.
Plate fixation provides immobilisation by placement of screws on either side of the fracture; however soft tissue stripping for their application may lead to overgrowth. Additionally rigid fixation may inhibit callus formation through 'stress shielding' and delay bony union. Potentially, minimally invasive bridge plating with contemporary locked plates avoids some of these disadvantages and is gaining popularity in the treatment of older children.They have been advocated for pathological and complex fractures (Hedequist 2008).
Why it is important to do this review
Femoral shaft fractures in children and adolescents, although comparatively rare, are serious injuries almost invariably requiring hospital admission and often causing prolonged disruption to the life of the child and their family. These fractures may also result in lifelong deformity and disability. There is no universally accepted protocol for the treatment of these fractures (Kocher 2010). In particular, the recent shift to operative management in some age groups needs to be validated, especially for resource‐compromised settings. There is a clear need for a systematic review of the evidence in order to inform clinical practice in this area.
Objectives
To assess the effects (benefits and harms) of interventions for treating femoral shaft fractures in children and adolescents.
We compared interventions within the following broad categories:
Surgical versus conservative treatment
Different methods of conservative treatment
Different methods of surgical treatment
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials (where the method of allocating participants to a treatment is not strictly random and where allocation can be predicted: e.g. by date of birth, hospital record number, alternation).
Types of participants
Children and adolescents below the age of 18 years with femoral shaft fractures.
Types of interventions
Trials comparing different interventions used for treating femoral shaft fractures in children and adolescents.
Interventions include:
Pavlik harness
Bryant's traction
Immediate hip spica cast
Traction followed by spica cast
Functional bracing (cast brace)
External fixation
Compression/locked plate
Flexible intramedullary nailing
Rigid intramedullary nail
Types of outcome measures
Primary outcomes
Functional outcome measures, such as the Pediatric Outcomes Data Collection Instrument (PODCI: PODCI 2005) (and also known as the Pediatric Orthopaedics Society of North America (POSNA) outcomes instruments scale (Daltroy 1998)), the RAND child health status scale and the Activity Scale for Kids (ASK; Young 2000).
Unacceptable malunion (angular, rotational and shortening), leg‐length discrepancy, limp.
Serious adverse events: compartment syndrome, deep infections, non‐union, nerve injury, knee ankylosis, persistent pain or need for second surgical intervention other than routine implant removal.
Secondary outcomes
Time for recuperation or return to usual activities.
Child satisfaction.
Parent satisfaction.
Resource use and other costs.
Timing of outcome measure
Whenever possible, we collected data for outcomes assessed at follow‐up in the short term (less than three months) and longer term (longer than three months and ideally at least at one year).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (accessed 16 August 2013), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2013 Issue 7), MEDLINE (1946 to August Week 1 2013), MEDLINE In‐Process & Other Non‐Indexed Citations (15 August 2013), EMBASE (1980 to 2012 week 9) and CINAHL (16 August 2013). We applied no language restrictions. In MEDLINE, we combined a subject‐specific strategy with the sensitivity‐ and precision‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011) (seeAppendix 1). Search strategies for the Cochrane Central Register of Controlled Trials, EMBASE and CINAHL are also shown in Appendix 1. We also searched the WHO International Clinical Trials Registry Platform and the metaRegister of Controlled Trials (mRCT) for ongoing and recently completed trials (to August 2013). We handsearched all available online conference proceedings of the following societies:
Paediatric Orthopaedic Society of India (annual meetings 2001 ‐ 2013)
Pediatric Orthopaedic Society of North America (annual meetings 2007 ‐ 2013)
The paediatric section of Asia Pacific Orthopaedic Association (the 8th Combined Congress of the Spine and Pediatric Sections, 2013)
The European Paediatric Orthopaedic Society (annual meetings 2006 ‐ 2013)
British Society for Children's Orthopaedic Surgery abstracts published in the Bone and Joint Journal (formerly the Journal of Bone & Joint Surgery British Volume) Orthopaedic Proceedings (2002 ‐ 2013)
Searching other resources
We searched reference lists of articles. We also contacted experts in the field and the contact authors of identified trials for information on existing or ongoing trials.
Data collection and analysis
The intended methodology for data collection and analysis was described in our published protocol (Madhuri 2011), which was based on the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011a).
Selection of studies
Two authors (AG and VD) independently assessed potentially eligible trials for inclusion. We obtained the full text of trials that fulfilled our inclusion criteria and those that were unclear from perusal of the abstracts. We resolved disagreements by discussion and consultation with a third author (VM).
Data extraction and management
All authors independently extracted information on study characteristics and results using a piloted data extraction form, resolving any disagreement through discussion. We attempted to contact trial authors where there were incomplete details on study methods or data. VD and VM entered the data into Review Manager 5 (RevMan) software (Review Manager 2014), and PT independently checked this.
Assessment of risk of bias in included studies
All authors independently assessed the risks of bias in each included trial using The Cochrane Collaboration's 'Risk of bias' assessment tool (Higgins 2011b) on the following six domains: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other biases. We considered subjective outcomes (e.g. participant‐reported function, parent and child satisfaction) and objective outcomes (unacceptable malunion, serious adverse events, time to return to usual activities) separately in our assessment of blinding and completeness of outcome data. Other potential biases assessed were major imbalances in key baseline characteristics (e.g. isolated versus combined fractures, age and gender); and performance bias such as that resulting from lack of comparability in the experience of care providers. We tried to contact the trial authors for clarification when methodological details were unclear. We resolved differences by discussion.
For each of these six domains, we assigned a judgement regarding the risk of bias as low risk, high risk or unclear risk, based on the criteria summarised in Table 8.5.c of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b) (see Appendix 2). We recorded these assessments in the standard 'Risk of bias' tables in RevMan, and summarised them in 'Risk of bias' summary figures and graphs. We used these judgements when assessing limitations in study design of the trials contributing to important outcomes in 'Summary of findings' tables.
Measures of treatment effect
We calculated risk ratios (RRs) and 95% confidence intervals (95% CIs) for dichotomous outcomes, and mean differences (MDs) with 95% CIs for continuous outcomes, wherever available.
Unit of analysis issues
Although the unit of randomisation in these trials is usually the individual participant, trials including children with bilateral fractures may present results for fractures or limbs rather than for individuals. Where such unit of analysis issues arose and appropriate corrections had not been made, or could not be obtained from trial authors, we pooled the data from such trials where the disparity between the units of analysis and randomisation was small. Had the disparity been moderate or large, and had data been pooled, we would have performed a sensitivity analysis to examine the effects of excluding incorrectly reported trials from the analysis.
Dealing with missing data
We attempted to obtain missing data from trial authors. Where possible, we extracted data to allow an intention‐to‐treat (ITT) analysis in which all randomised participants are analysed in the groups to which they were originally assigned. If there was discrepancy in the number randomised and the numbers analysed in each treatment group, we calculated the percentage loss to follow‐up in each group and reported this information. Had drop‐outs exceeded 10% for any trial, and if the differential drop‐out rate in the intervention arms was significant, we would have assigned the worst outcome to those lost to follow‐up for dichotomous outcomes and assessed the impact of this in sensitivity analyses with the results of completers. Where possible, we calculated missing standard deviations from other available data such as standard errors (Higgins 2011c). However, we did not impute missing values in order to present these in the analyses. We did not make any assumptions about loss to follow‐up for continuous data and analysed results for those who completed the trial.
Assessment of heterogeneity
We judged the appropriateness of pooling data by assessing clinical heterogeneity in terms of the trial participants, interventions and outcomes of the included studies. For pooled data we assessed heterogeneity between trials by visual examination of the forest plot, primarily to check for overlapping confidence intervals, and used the Chi² test for homogeneity and the I² statistic to assess inconsistency (the percentage of the variability in effect estimates that is due to heterogeneity rather than random error). We based our judgements of substantial heterogeneity on the guidance provided in Deeks 2011; in general we interpreted an I² value of 50% or more to denote substantial heterogeneity, although we acknowledge that this cut‐off is arbitrary. We therefore interpreted I² values between 30% and 60% as significant depending on whether the inconsistency in results was due to differences in the direction of effects estimates between trials, rather than if inconsistency in results was due to differences in the magnitude of effect estimates favouring an intervention (Deeks 2011).
Assessment of reporting biases
We attempted to reduce reporting bias by: a) performing a comprehensive search for published, unpublished and ongoing trials; b) placing no language restrictions on the search strategy; c) checking for multiple trial reports of the same trial; d) attempting to obtain the protocol or the trial registration document of trials; and e) contacting the authors in cases where the pre‐specified primary (favourable or adverse) outcomes are not reported.
We assessed all included studies for adequacy of reporting of data for pre‐stated outcomes and for selective reporting of outcomes. We incorporated judgements about reporting biases in the risk of bias assessments for each trial.
Had there been at least 10 trials included in a meta‐analysis for primary outcomes, we would have assessed the likelihood of potential publication bias using funnel plots.
Data synthesis
We analysed data using Review Manager 5 (Review Manager 2014). Since all the included trials studied different sets of comparisons, and not all these trials reported the same outcomes, we were not able to synthesise data for the comparisons of different conservative interventions and between surgical interventions. However, we synthesised data for surgical versus conservative interventions where comparable data for outcomes were subgrouped by the specific comparison used in the trials, to derive pooled, weighted risk ratios in Mantel‐Haenszel fixed‐effect meta‐analyses. We would have used the random‐effects model for data synthesis when heterogeneity was identified as significant and could not be explained by subgroup analyses. Had I² values revealed substantial inter‐trial variability in effect estimates not accounted for by chance (I² values 75% or more), or had trials differed substantially in clinical or methodological attributes, we would have presented the results of the trials in a forest plot, without summating their effect estimates.
We intended to combine continuous data measured using the same scale using the mean difference. We planned to use the standardised mean difference (SMD) in meta‐analyses where data were measured on different scales that could not be converted to a common scale. If the scales used in the trials had differed in the direction of scoring, we would have multiplied the mean values from one set of scales by ‐1 in order to ensure that the direction of scores across trials were comparable (Deeks 2008). We would have attempted to interpret the combined standardised mean differences by re‐expressing them as odds ratios and numbers needed to treat (or harm) for an additional beneficial (or harmful) outcome, using the methods described in Schünemann 2011.
Subgroup analysis and investigation of heterogeneity
Had there been sufficient trials to enable data synthesis, we would have undertaken the following subgroup analyses:
Polytrauma versus isolated injuries;
Open versus closed injuries;
Age groups: two years or less, three to five years, 6 to 11 years and 12 to 18 years;
Fracture pattern: stable versus unstable;
Short‐term (3 months) versus long‐term follow‐up (more than one year) as determined by the pattern of reporting.
However, we only presented available data for trials comparing surgical versus conservative treatments, subgrouped by the specific comparison. For fixed‐effect meta‐analyses, we assessed subgroup differences by interaction tests (Altman 2003). Had we used random‐effects meta‐analyses, we would have used non‐overlapping confidence intervals to indicate a statistically significant difference in treatment effect between the subgroups.
Sensitivity analysis
We conducted sensitivity analyses to investigate the robustness of the results for the primary outcomes by excluding trials at high risk of bias for the one comparison where it was possible to pool data, and used the results of this sensitivity analysis to grade study limitations when making overall assessments of study quality for the 'Summary of findings' tables.
We had also planned to undertake sensitivity analyses if trials reported drop‐out rates of 10% or greater, to ascertain differences in outcomes of ITT analysis (all drop‐outs would have been assigned to the worst outcome for dichotomous outcomes) and analysis of completers.
For pooled data, if significant heterogeneity had been detected that arose from one or two outlying studies with results that conflicted with the other studies with clinical or methodological characteristics that differed from the other trials, we would have performed analyses with and without these outlying studies as part of a sensitivity analysis.
Summarising and interpreting results
We used the GRADE approach to interpret findings (Schünemann 2011) and used GRADE Profiler (GRADE 2004) to import data from Review Manager 5 (Review Manager 2014) to create 'Summary of findings' tables for each comparison if possible and relevant. These tables provide information concerning the quality of the evidence, the magnitude of effect of the interventions examined, and the sum of available data on all primary outcomes, and for the secondary outcomes of time for recuperation/return to normal activities, resource use and costs, and parent and child satisfaction. We consider these outcomes critically important for patient care and decision‐making.
Results
Description of studies
Results of the search
The search was completed in August 2013. We screened a total of 1044 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (31 records); Cochrane Central Register of Controlled Trials (107), MEDLINE (297), EMBASE (287), and CINAHL (322). We also identified two records from searching the WHO International Clinical Trials Registry Platform.
The search resulted in the identification of 22 potentially eligible studies (some published in multiple reports), for which we obtained full‐text reports where possible. Of these, we included 10 trials (Bar‐On 1997; Domb 2002; Hsu 2009; Leu 2012; Malo 1999; Mehdinasab 2008; Park 2012; Shemshaki 2011; Siddiqui 2008; Wright 2005) and excluded another 10 studies (Agarwal 2004; Ali 2005; Altay 2011; Ansari 2011; Buechsenschuetz 2002; Curtis 1995; Flynn 2004; Flynn 2011; Gupta 2007; Ramseier 2007). Two trials, both of which were reported in conference abstracts only, currently await assessment (Shaikh 2012; Ucar 2013); see Characteristics of studies awaiting classification. We did not identify any ongoing trials. All trial reports were in English aside from Malo 1999, which was reported in a French language journal and was translated by the French Cochrane Centre.
Details of the process of screening and selecting studies for inclusion in the review are illustrated in Figure 1.
1.

Study flow diagram
Included studies
Details of the methods, participants, interventions and outcome measures of individual trials are provided in the Characteristics of included studies and are summarised below. We attempted unsuccessfully to contact trial authors of six trials (Bar‐On 1997; Hsu 2009; Leu 2012; Malo 1999; Mehdinasab 2008; Park 2012) for clarification of study methods and characteristics.
Setting
Nine trials were single‐country trials, recruiting children from Canada (Malo 1999), Iran (Mehdinasab 2008; Shemshaki 2011), Israel (Bar‐On 1997), Korea (Park 2012), Pakistan (Siddiqui 2008), the Philippines (Hsu 2009), and the USA (Domb 2002; Leu 2012). Wright 2005 had four centres in four countries (Canada, Australia, USA and New Zealand). Trial recruitment usually took place over several years. The earliest participant was recruited into Malo 1999 (recruiting between July 1982 and June 1984) and the latest recruited into Shemshaki 2011 (recruiting between February 2009 and January 2010). Recruitment spanned seven years in Wright 2005: October 1994 to October 2000.
Participants
The 10 included trials randomised 527 children with 531 fractures. Respectively, Bar‐On 1997, Domb 2002 and Park 2012 included one, one and two participants with bilateral femoral fractures. Overall, the age of the participants included in this review ranged from 3 to 17.4 years. Bar‐On 1997 did not report the sex of the participants; in the other nine studies, the number of boys was at least twice that of the girls. All children had sustained closed femoral shaft fractures, except in Hsu 2009, which included 12 children with grade I open fractures, and Park 2012, which included three open fractures (two 'grade I', and one 'grade II').
Interventions
The trials were grouped by comparison as follows:
Surgical versus conservative treatment
Each of the four trials comparing surgical versus conservative treatment differed in the interventions under comparison, as described below.
External fixation versus immediate hip spica cast (Wright 2005): a multi‐centre trial of 108 children aged 4 to 10 years;
Intramedullary pin fixation plus spica cast versus skeletal traction followed by spica cast (Mehdinasab 2008): 70 children aged 6 to 11 years;
Elastic stable intramedullary nail (ESIN) versus traction followed by spica cast (Shemshaki 2011): 46 children aged 6 to 12 years;
Elastic stable intramedullary nailing (ESIN) versus dynamic skeletal traction spica casting (DSTSC) (Hsu 2009): 51 children aged 5 to 12 years.
Different methods of conservative treatment
Immediate hip spica cast versus skin traction followed by spica cast (Siddiqui 2008): 42 children aged 3 to 10 years;
Traction followed by functional orthosis versus traction followed by spica cast (Malo 1999): 43 children aged 5 to 13 years;
Single‐leg versus double‐leg spica cast (Leu 2012): 52 children two to seven years.
Different methods of surgical treatment
Elastic stable intramedullary nail (ESIN) versus external fixation (Bar‐On 1997): 19 children (20 fractures) aged 5.2 to 13.2 years;
Dynamic external fixation versus static external fixation (Domb 2002): 52 children (53 fractures) aged 3 to 12 years;
Intramedullary nailing versus submuscular plating (Park 2012): 47 children (49 fractures) aged 11 to 17.4 years.
There were no eligible trials examining the use of Pavlik's harness or Bryant's traction. Both of these methods are used for infants. There were also no eligible trials examining locked femoral plating, which is often used for unstable and upper femur fractures, or rigid trochanteric intramedullary nailing, which is typically used for adolescents.
Outcomes
Primary outcomes
Wright 2005 and Leu 2012 reported on functional status and used the RAND child health status scale (Eisen 1980) and the Activities Scale for Kids (Young 2000) (ASK; www.activitiesscaleforkids.com/) score, respectively.
All included trials except Domb 2002 and Leu 2012 reported rates of malunion, but specific criteria used to define malunion were not reported in four trials (Bar‐On 1997; Malo 1999; Mehdinasab 2008; Shemshaki 2011). Siddiqui 2008 defined malunion as an unsatisfactory outcome with shortening greater than 2 cm and angulation within 20º in the sagittal plane and greater than 15º in the coronal plane at the time of cast removal. Wright 2005 defined malunion assessed at two years as any of: limb‐length discrepancy (as assessed by computed tomography (CT)) of greater than 2 cm, greater than 15º of anterior or posterior angulation, or greater than 10º of varus or valgus angulation (as assessed from radiographs).
Serious adverse events or complications other than malunion were reported by Bar‐On 1997,Domb 2002, Hsu 2009, Leu 2012, Park 2012, Shemshaki 2011 and Wright 2005.
Secondary outcomes
Time for recuperation or return to usual activities was reported by Bar‐On 1997 (time to achieve full weight‐bearing, full range of movement, and return to school), Domb 2002 (time to resume full weight‐bearing), Mehdinasab 2008 (time to independent walking), Shemshaki 2011 (time to start walking independently, and return to school) and Wright 2005 (duration of treatment: number of days child wore external fixator or hip spica).
Child satisfaction was measured formally in Wright 2005, and parent satisfaction was reported in Bar‐On 1997,Shemshaki 2011 and Wright 2005. However, the method used to assess this outcome was not reported in Bar‐On 1997. Aspects relating to child and parental satisfaction were recorded using a custom scoring tool in Leu 2012.
In Hsu 2009, resource use and other costs (excluding surgeons fees and costs borne by families) were formally calculated and reported as total cost in dollars. Aspects of resource use were reported in other trials. These included length of hospital stay (Hsu 2009; Malo 1999; Mehdinasab 2008; Shemshaki 2011; Wright 2005) and caregiver's time off work (Leu 2012).
Excluded studies
The reasons for exclusion for the 10 studies are described in the Characteristics of excluded studies. Of the two RCTs, Ansari 2011 randomised only adults, while separate data were unavailable for the few children with femur fracture in Agarwal 2004. The remaining eight studies were not RCTs; these included Curtis 1995, which was claimed to be randomised but, on closer scrutiny, was not randomised because allocation of interventions was at the discretion of the surgeon, and data were gathered from retrospective chart review.
Risk of bias in included studies
None of the trials was at low risk of bias for all domains. Wright 2005 was free of risk of bias in all domains bar one (performance bias, where the risk of bias was unclear) (see Figure 2 and Figure 3).
2.
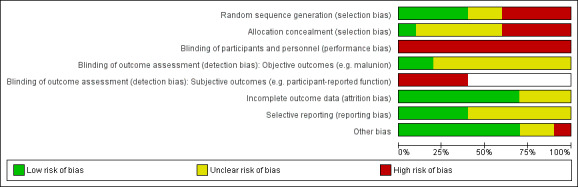
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Bar‐On 1997,Domb 2002,Mehdinasab 2008 and Park 2012 were quasi‐randomised trials where allocation was predictable and were therefore judged as being at high risk of selection bias. Only Wright 2005 was judged as being at low risk of selection bias. The other trials were at unclear risk of selection bias. In two trials (Malo 1999; Siddiqui 2008), this applied to both random sequence generation and allocation concealment: Malo 1999 described drawing by lots but gave no explanation for the imbalance in allocation (15 versus 28); and Siddiqui 2008 gave no information on the method of randomisation. The other three trials (Hsu 2009; Leu 2012; Shemshaki 2011) described a suitable method of sequence generation but there was insufficient mention of adequate safeguards for concealing allocation.
Blinding
All trials were open‐label in design due to the different comparisons used, and were judged to be at high risk of performance bias. Two trials (Malo 1999; Shemshaki 2011) used independent outcome assessors and were judged to be at low risk of detection bias for objective outcomes. The remainder were judged unclear for the risk of detection bias for objective outcomes such as malunion, serious adverse events and the time for recuperation or to return to usual activities. Bar‐On 1997, Leu 2012, Shemshaki 2011 and Wright 2005 were judged to be at high risk of detection bias for participant‐reported outcomes; the remaining trials did not report subjective outcomes.
Incomplete outcome data
Bar‐On 1997, Mehdinasab 2008 and Park 2012 were judged to be at unclear risk of attrition bias because of incomplete information, including that relating to participants with bilateral fractures in Bar‐On 1997 and Park 2012. In Mehdinasab 2008 and Park 2012, there was also no information on group allocation of four excluded participants. The other seven trials were judged to be at low risk of attrition bias.
Selective reporting
Although two trials (Leu 2012; Shemshaki 2011) were registered, it was retrospective in both cases. Although outcomes mentioned in the methods section or the objectives of all the trials were reported, we considered that six trials (Bar‐On 1997; Domb 2002; Hsu 2009; Malo 1999; Mehdinasab 2008; Siddiqui 2008) were at unclear risk of bias where outcomes such as malunion were inadequately defined or pre‐specified, or obvious outcomes (e.g. complications) were not reported.
Other potential sources of bias
It is unclear from the descriptions in Mehdinasab 2008 and Shemshaki 2011 whether the surgical skills in the operating teams were similar. Leu 2012 was at high risk for recall bias.
Effects of interventions
See: Table 1
Surgical versus conservative interventions
Four studies (Hsu 2009; Mehdinasab 2008; Shemshaki 2011; Wright 2005) compared surgical versus conservative treatment.
Primary outcomes
Only Wright 2005 assessed functional outcomes: they found that RAND scores did not differ between external fixation and spica cast recipients at two years (mean 69 versus 68; mean difference (MD) 1.00, 95% CI ‐2.15 to 4.15; 101 children; Analysis 1.1).
1.1. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 1 Functional outcome at 2 years ‐ RAND scores (characteristics of scale unclear).
Malunion rates were reported in all four trials. Surgical interventions significantly reduced the absolute risk of malunion by 84% (95% CI 76% to 92%) and the relative risk of malunion by 71% when compared with conservative interventions (7/130 versus 31/134; RR 0.29, 95% CI 0.15 to 0.59; 264 children, 4 to 24 months follow‐up; Analysis 1.2, Figure 4).
1.2. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 2 Malunion.
4.
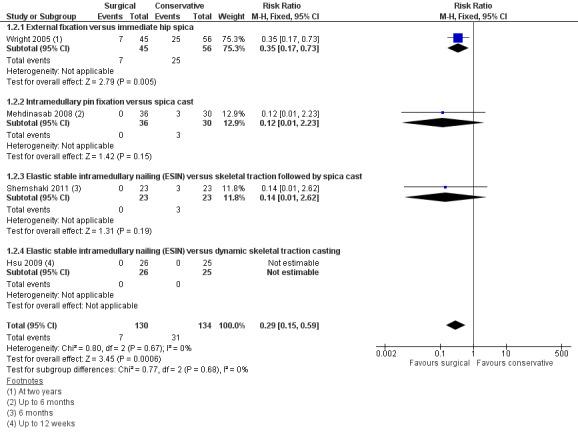
Forest plot of comparison: 1 Surgical versus conservative treatment, outcome: 1.2 Malunion
Serious adverse events, which were reported in all four trials, were more common in the surgical group (19/130 versus 8/134; RR 2.39, 95% CI 1.10 to 5.17; 264 children; Analysis 1.3). In Wright 2005, there were two refractures after removal of the external fixator and five hospital readmissions for repeat closed reduction and adjustment to the external fixator in the surgical group, and six children received surgery after unacceptable loss of reduction in the conservative treatment group. Not included in the analysis were 20/45 (44%) children treated with external fixation in Wright 2005 who developed pin track infections, all of which resolved uneventfully with antibiotics. In Mehdinasab 2008, six children in the surgery group had pain and discomfort at the pin end site (pin‐end irritation) until the pins were extracted. Not included was one child in this group who had a superficial infection that was treated by antibiotics. Three children in the surgery group of Shemshaki 2011 had infection; there was no indication of the severity of these infections or their treatment. Not included was one child in this group who had a transitional nerve injury that repaired spontaneously. Hsu 2009 reported one case of nail migration and two cases of skin irritation in the surgery group and two pin‐tract infections (traction pin) for the conservative treatment group; the severity of these complications was not reported but all resolved without surgery.
1.3. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 3 Serious adverse events.
Secondary outcomes
Time for recuperation or return to usual activities was reported using various measures in three trials, with data presented for two in Analysis 1.4. Although Wright 2005 did not report on time to resume normal activities, a proxy (duration of treatment) showed a longer time wearing the external fixator than the spica cast (77 versus 58 days: MD 19.00 days, 95% CI 9.21 to 28.79; 101 children; Analysis 1.4). Mean time to independent walking was less for surgery group participants in both Mehdinasab 2008 (60.2 versus 75.3 days) and Shemshaki 2011 (35.2 versus 80.0 days). The time to return to school was also significantly shorter in the surgical group of Shemshaki 2011 (31.5 versus 64.3 days; MD ‐32.80 days, 95% CI ‐42.50 to ‐23.10 days; 46 children; Analysis 1.4).
1.4. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 4 Time for recuperation or return to usual activities.
Wright 2005 recorded child and parent satisfaction using an 11‐point ordinal scale, with 'very happy' or 'very satisfied' at the top end respectively. Children's and parents' satisfaction did not differ significantly between intervention (child satisfaction: MD 0.80, 95% CI ‐0.61 to 2.21; 101 children; Analysis 1.5; parent satisfaction: MD 0.10, 95% CI ‐0.49 to 0.29; 101 children; Analysis 1.6). In Shemshaki 2011, all parents of children (23/23) treated with surgery rated the treatment as excellent or good compared with 17/23 (74%) treated with traction followed by spica cast (RR 1.34, 95% CI 1.05 to 1.73, 46 children; Analysis 1.7).
1.5. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 5 Child satisfaction (scale 1 ‐ 11; 11 = 'very happy').
1.6. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 6 Parent satisfaction (1 ‐ 11; 11 = 'very satisfied').
1.7. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 7 Parent satisfaction (excellent or good).
All four trials reported on length of hospital stay, full data being available from three trials. Since the latter were significantly heterogeneous, these were not pooled (Analysis 1.8). In Wright 2005, the surgical group (external fixation) stayed around two days longer in hospital (5.9 versus 4.1 days; MD 1.80 days, 95% CI ‐0.32 to 3.92 days; 101 children), whereas in Shemshaki 2011, the surgical group (elastic intramedullary nailing) spent around 13 days less time in hospital (6.9 versus 20.5 days; MD ‐13.60 days, 95% CI ‐16.25 to ‐10.95 days; 46 children). Hsu 2009 found a significantly increased length of stay in the surgery (elastic intramedullary nailing) group (17 versus 6 days; MD 11.00 days, 95% CI 7.77 to 14.23 days; 51 children) which was attributable to a significantly longer time to surgery in the surgery group that was primarily due to "financial constraints in acquiring the necessary supplies". Mehdinasab 2008 reported a considerably shorter hospital stay for the surgical group (4.6 versus 23.7 days).
1.8. Analysis.

Comparison 1 Surgical versus conservative treatment, Outcome 8 Hospital stay (days).
Hsu 2009 reported the total costs for surgery using the elastic intramedullary nailing (hardware, supplies, anaesthesia, radiographs, medicines including antibiotics, and hospital stay; and excluding physicians' fees or patient‐borne costs) were higher than for conservative treatment with dynamic skeletal traction spica casting ($844 versus $216) at 2008 costs.
Comparisons of different conservative interventions
Three randomised trials (Leu 2012; Malo 1999; Siddiqui 2008) compared different surgical interventions.
Immediate hip spica cast versus skin traction followed by spica cast
Siddiqui 2008 only reported on 'unsatisfactory' outcome, which was based on prespecified criteria for malunion (shortening or unacceptable angulation) at cast removal or a complication requiring a change in management. Since the latter was correction for unacceptable angulation by wedging the cast, this outcome is presented as malunion at cast removal (six to eight weeks from injury) in this review. More children in the immediate hip spica cast group had malunion at cast removal than those in the skeletal traction followed by hip spica cast at cast removal, but the small sample size did not preclude the probability that this was due to chance (4/21 versus 1/21; RR 4.00, 95% CI 0.49 to 32.87, 42 children; Analysis 2.1). No other outcomes sought in this review were reported.
2.1. Analysis.

Comparison 2 Immediate hip spica cast versus skeletal traction followed by spica cast, Outcome 1 Malunion at cast removal (6 ‐ 8 weeks from injury).
Traction followed by functional orthosis versus traction followed by spica cast
Malo 1999 found similar malunion rates assessed at five or more years in the functional orthosis and spica cast groups (6/15 versus 11/27; RR 0.98, 95% CI 0.46 to 2.12; 42 children, Analysis 3.1). Functional outcomes and development of serious complications were not reported in this study.
3.1. Analysis.

Comparison 3 Traction followed by functional orthosis versus traction followed by spica cast, Outcome 1 Malunion (assessed at 5 to 10 years).
Length of hospital stay, a measure of resource use, was the only secondary outcome reported in Malo 1999. Duration of hospitalisation was similar in the two groups (mean duration was 26.3 days in the orthosis group and 26.8 days in the spica cast group; MD ‐0.50 days, 95% CI ‐4.68 to 3.68 days; 45 children, Analysis 3.2).
3.2. Analysis.

Comparison 3 Traction followed by functional orthosis versus traction followed by spica cast, Outcome 2 Hospital stay (days).
Single‐leg versus double‐leg spica cast
Leu 2012 did not find a significant difference in ASK scores at cast removal (mean 44 days in both groups) between the single‐leg and double‐leg casts (mean 26.15% versus 24.58%; Analysis 4.1). Four children had a change in treatment: one child in the single‐leg cast group had a recast for loss of fracture reduction; one in the double‐leg cast group has surgery on immediate loss of reduction on first application of the cast, and two children had their casts converted to single‐casts on request by their parents (Analysis 4.2). None of the children had any serious adverse events, such as compartment syndrome or major skin problems (Analysis 4.3). Malunion was not reported but there were no statistically significant differences between the two groups in radiological outcomes of extent of shortening (reported P = 0.40) or angulation (reported P = 0.28).
4.1. Analysis.
Comparison 4 Single‐leg versus double‐leg spica cast, Outcome 1 Performance version of ASK (%: 100% = best result).
| Performance version of ASK (%: 100% = best result) | |||
|---|---|---|---|
| Study | Single‐leg spica cast | Double‐leg spica cast | Reported P value |
| Leu 2012 | 24.56% (8 to 58); n = 16 | 26.15% (5 to 61); n = 21 | 0.39 |
4.2. Analysis.

Comparison 4 Single‐leg versus double‐leg spica cast, Outcome 2 Change in treatment.
4.3. Analysis.

Comparison 4 Single‐leg versus double‐leg spica cast, Outcome 3 Serious adverse effects.
Leu 2012 reported the results of the individual questions of a 10‐question custom survey completed by the families on 'Ease of patient function and care giving' after cast removal. The results of four questions are presented in Analysis 4.4; these show that single‐leg casts tended to allow more comfort when sitting and greater ease on leaving the family home. Fewer caregivers needed to take time off work in the single‐cast group (11/21 versus 15/19; RR 0.66, 95% CI 0.41 to 1.06; 40 children, Analysis 4.5) and for less time (mean 10.38 versus 19.0 days; reported P = 0.049).
4.4. Analysis.
Comparison 4 Single‐leg versus double‐leg spica cast, Outcome 4 Comfort and ease of care during cast use (VAS: visual analogue score 0 to 10 where 10 = most difficult).
| Comfort and ease of care during cast use (VAS: visual analogue score 0 to 10 where 10 = most difficult) | ||||
|---|---|---|---|---|
| Study | Outcome |
Single‐leg spica
mean VAS score N = 21 |
Double‐leg spica mean VAS score N = 23 | Reported P value |
| Leu 2012 | Comfort in chair | 4.38 (Range 1 to 10) | 6.26 (Range 1 to 10) | 0.032 |
| Leu 2012 | Difficulty leaving residence | 5.00 (Range 1 to 10) | 6.74 (Range 1 to 10) | 0.066 |
| Leu 2012 | Difficulty keeping child clean | 6.05 (Range 1 to 10) | 6.04 (Range 1 to 10) | 0.42 |
| Leu 2012 | Difficulty keeping cast clean | 6.10 (Range 1 to 10) | 6.00 (Range 1 to 10) | 0.40 |
4.5. Analysis.

Comparison 4 Single‐leg versus double‐leg spica cast, Outcome 5 Caregiver took time off work.
Comparisons of different surgical interventions
Three quasi‐randomised trials (Bar‐On 1997; Domb 2002; Park 2012) compared different surgical interventions.
Elastic stable intramedullary nailing (ESIN) versus external fixation
Although Bar‐On 1997 did not report on functional outcomes, all children had unrestricted activity at final follow‐up (mean 14 months; range 12 to 22 months). None of the nine children treated with ESIN but four of 10 children treated with external fixation had malunion (malalignment) at final follow‐up: RR 0.12, 95% CI 0.01 to 2.00; Analysis 5.1). The criteria for malunion were not reported. None of the children had a limp; two children in the external fixation group had a limb‐length discrepancy of 1 cm. There were fewer children with serious adverse events in the ESIN group (2/9 versus 5/10; RR 0.44, 95% CI 0.11 to 1.75; Analysis 5.2).
5.1. Analysis.
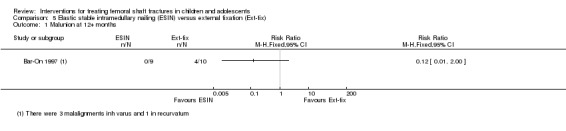
Comparison 5 Elastic stable intramedullary nailing (ESIN) versus external fixation (Ext‐fix), Outcome 1 Malunion at 12+ months.
5.2. Analysis.

Comparison 5 Elastic stable intramedullary nailing (ESIN) versus external fixation (Ext‐fix), Outcome 2 Serious adverse events.
Children in the ESIN group returned to school on average eight weeks earlier than those in the external fixation group (ESIN: mean 5 weeks (range 2 to 12 weeks); external fixation: mean 13 weeks (3 to 32 weeks)), and were also fully weight‐bearing three weeks earlier (ESIN: mean 7 weeks (range 3 to 10 weeks); external fixation: mean 10 weeks (5 to 17 weeks)). All parents of children treated with ESIN reported satisfaction with treatment while two parents of the eight children with isolated fractures treated with external fixation said they would select non‐surgical treatment if faced again with the same decision. Resource use and costs were not reported in this trial.
Dynamic external fixation versus static external fixation
Domb 2002 did not report on functional outcomes or final malunion. One child in the dynamic fixator group and three children in the static fixator group had serious adverse events (1/25 versus 3/28 fractures; RR 0.37, 95% CI 0.04 to 3.36; Analysis 6.1).
6.1. Analysis.

Comparison 6 Dynamic external fixation (Ext‐fix) versus static external fixation (Ext‐fix), Outcome 1 Serious adverse events.
Of the secondary outcomes sought for this review, Domb 2002 reported only on the time to resume full weight‐bearing, which was longer in the dynamic external fixation group (73.31 versus 62.9 days, MD 10.41 days, 95% CI ‐0.99 to 21.81 days; 53 children, Analysis 6.2). Of note is that, contrary to the intended method, dynamisation was performed not at the time of early callus formation (mean 23 days) but at an average of 50 days (range 20 to 121 days), which thus indicates some deviation from original intention.
6.2. Analysis.

Comparison 6 Dynamic external fixation (Ext‐fix) versus static external fixation (Ext‐fix), Outcome 2 Time to resume full weight‐bearing.
Trochanteric‐entry intramedullary nailing versus submuscular plating
Park 2012 did not report on functional outcomes. No malunion was seen in either group (43 children) at final mean follow‐up of 21 months (Analysis 7.1). Two children in the nail group had a serious adverse event, both of which required a re‐operation, whereas there were none in the plating group (2/21 versus 0/22; RR 5.23, 95% CI 0.27 to 102.87; 43 children, Analysis 7.2).
7.1. Analysis.

Comparison 7 Intramedullary nailing versus submuscular plating, Outcome 1 Unacceptable malunion.
7.2. Analysis.

Comparison 7 Intramedullary nailing versus submuscular plating, Outcome 2 Serious adverse events.
Park 2012 found a significantly shorter time to weight‐bearing in the nailing group compared with the plating group: mean 57.3 versus 89.2 days; reported P value < 0.05). Hardware removal was not a listed outcome in our protocol. However, it is noteworthy that all 16 removals of nails that had occurred by the end of follow‐up were uneventful while there were serious difficulties encountered in removing three of the 17 plates.
Discussion
Summary of main results
This review summarises the evidence from 10 trials (527 children) that conducted 10 different sets of comparisons, across three main comparison groups. We were able to pool data only from the four trials comparing surgical versus conservative intervention for the review's primary outcomes of malunion and serious adverse events. Most of the trials were at risk of bias in one or more domains; all were at risk of performance bias because of the impracticalities of blinding care providers. The sample sizes in all the trials, except Wright 2005 for their primary outcome of malunion, were also not sufficient to rule out chance effects.
Comparison of surgical and conservative intervention
Four trials (maximum data for 264 children, aged between 4 and 12 years) compared surgery versus conservative treatment, using different combinations of interventions. Surgery was either external fixation (one trial) or nailing (three trials) and conservative treatment was either spica cast, skeletal traction followed by casting (two trials) or dynamic skeletal traction spica casting. Only one trial reported functional outcomes. The evidence for this comparison is presented in Table 1.
Primary outcomes
Low quality evidence (one trial, 101 children, aged between 4 and 10 years) showed that RAND child health status scores may not differ significantly between surgery (external fixation) and conservative treatment (immediate spica cast). There were no data on functional outcome measures for the other three trials making this comparison.
Moderate quality evidence (four trials) showed that rates of unacceptable malunion were reduced in surgical interventions. Assuming an illustrative baseline risk of 115 malunions per 1000, the results equated to 81 fewer (95% CI 47 to 97 fewer) malunions per 1000 children treated with surgery.
Low quality evidence (four trials) showed that serious adverse events differed significantly between the two groups, being higher overall in the surgical group. Assuming an illustrative baseline risk of 40 serious adverse effects per 1000 for conservative treatment, these resulted equated to 56 more (95% CI 4 to 167 more) serious adverse events per 1000 surgically‐treated children. Notably, the variety and severity of the adverse events differed considerably in the four trials.
Secondary outcomes
There is low quality evidence (one trial, 46 children) that surgery (Elastic stable intramedullary nail (ESIN)) may reduce the time for children to return to school compared with conservative treatment (traction followed by spica cast).
There is low quality evidence (one trial, 46 children) that parental satisfaction may be greater in surgery (with ESIN) than conservative treatment (traction followed by spica cast). However, another study (101 children) found that parental satisfaction was almost the same in the two treatment groups (external fixation versus spica cast).
There is low quality evidence that child satisfaction probably did not differ significantly between surgery (external fixation) versus conservative treatment (immediate spica cast).
There were conflicting results for length of hospital stay from the four studies, which meant that we cannot draw any conclusions on this outcome. We do not know if the total costs are higher for surgery versus conservative treatment, but the study comparing ESIN with conservative treatment with dynamic skeletal traction spica casting found hospital costs, excluding physicians' fees, in the Philippines (2008) were 400% higher for surgery.
None of the other comparisons reported data on resource uses, costs or other financial considerations
Comparisons of different conservative interventions
The three small randomised trials in this category made three different comparisons. Only one trial reported functional outcomes. We have not presented 'Summary of findings' tables for these comparisons.
Very low quality evidence (one trial, 42 children, aged between 3 and 10 years) means that we do not know if malunion at cast removal, measured at six to eight weeks, actually differs between immediate hip spica casts versus skin traction followed by spica casts.
Very low quality evidence (one trial, 43 children, aged between 5 and 15 years) means that we do not know if long‐term malunion actually differs between traction followed by functional orthosis versus traction followed by spica casts. Very low quality evidence from the same trial indicates little difference in length of stay in hospital, but otherwise there is no evidence on resource use or costs.
Very low quality evidence (one trial, 52 children, aged between two and seven years) means that we do not know if function, measured using the Activity Scale for Kids (ASK) score, at cast removal or serious adverse events (zero reported for both interventions) actually differs between single‐leg versus double‐leg spica casts. Low quality evidence from the same trial indicates that single‐leg casts are less awkward to manage by parents, more comfortable for the child and may require less time off work by the caregiver.
Comparisons of different surgical interventions
The three small quasi‐randomised trials in this category made three different comparisons. None reported functional outcomes nor child satisfaction with treatment. We have not presented 'Summary of findings' tables for these comparisons.
Very low quality evidence (one trial, 19 children, aged between 5.2 and 13.2 years) means that we do not know if malunion, measured at 12 to 22 months, serious adverse events, time to return to school or parental satisfaction actually differ between ESIN versus external fixation.
Very low quality evidence (one trial, 52 children, aged between 3 and 12 years) means that we do not know if serious adverse events and time to resume full weight‐bearing actually differ between dynamic external fixation versus static external fixation. The disparity between the planned (early callus formation) and actual timing (mean 50 days compared with 23 days) of dynamisation hampers interpretation of the results of this trial.
Very low quality evidence (one trial, 47 children, aged between 11 and 17.4 years) means that we do not know if malunion, serious adverse events and time to resume weight‐bearing actually differ between intramedullary nailing versus submuscular plating. The difficulties encountered in extracting three plates subsequently (18%), however, sound a cautionary note for the use of submuscular plating.
Overall completeness and applicability of evidence
Completeness
This review attempted to categorise choices available for treating shaft of femur fractures in children and adolescents and examined the available evidence to inform such choices. Only a limited number of these choices were addressed by randomised controlled trials. Most of the studies did not involve infants, toddlers and older adolescents. No included trials evaluated key interventions such as Pavlik's harness or Bryant's traction. Critical outcomes such as functional outcome measures were underreported in the included trials. Important outcome measures such as time to return to normal activity, resource use, direct and indirect costs from societal and individual perspectives; opportunity costs, and satisfaction with treatment were also not reported, or were inadequately reported. The timing of final outcome assessment, such as at cast removal in Leu 2012 and Siddiqui 2008, was also inadequate in several trials, and failed to provide a full picture of final function and, especially given that children's bones remodel over time, the incidence of unacceptable malunion.
Applicability
The range of interventions assessed in the included trials provide evidence to inform clinical decision‐making and cover the interventions that can be offered via specialist orthopaedic teams in high‐, middle‐ and low‐income settings. However, the choice of intervention to be used will require a shared decision‐making approach where the suitability of the intervention, depending on the clinical presentation, has to be balanced by considerations of the potential benefits and harms, as well as the value placed on early return to usual activities, the burdens associated with interventions, and the financial implications of each intervention, as these are likely to differ between and within settings, and between individual parent‐child dyads.
The available evidence applies to closed fractures only: most of the trials excluded open fractures except Bar‐On 1997, Hsu 2009 and Park 2012. However, Bar‐On 1997 recruited no children with open fractures and Park 2012 recruited only three children with open fractures: two Gustilo grade I and one Gustilo grade II. Hsu 2009 recruited 12 children (24%) with grade I open fractures but excluded those with more severe grades.
Quality of the evidence
We assessed the overall quality of the evidence using the GRADE approach (Schünemann 2011). This approach integrates evaluations regarding serious study limitations, with judgements regarding unexplained inconsistency in the results; indirectness; deviations from accepted practice in the way interventions and comparisons were given, the populations studied, the choice of outcomes and the methods of ascertainment; imprecision in the effect estimates in terms of statistical significance as well as clinical importance; and the likelihood that publication bias affected the estimates.
Surgical versus conservative treatment
The description and explanation for our assessment for the quality of the evidence for this comparison is provided in the Footnotes of the Table 1. The evidence for all of the outcomes was low quality ("further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate") except for malunion, where we judged the evidence to be moderate quality ("further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate").
Comparisons of different conservative interventions
The evidence for malunion in a comparison of immediate hip spica casts versus skin traction followed by spica casts was downgraded one level for serious study limitations, mainly reflecting unclear risks of selection bias and high risk of performance bias, and two levels for imprecision. Thus, we concluded that the evidence was of very low quality, meaning that we are very uncertain about the estimate for malunion.
The evidence for malunion in a comparison of traction followed by functional orthosis versus traction followed by spica casts was downgraded one level for serious study limitations, mainly reflecting unclear risks of selection bias and high risk of performance bias, and two levels for imprecision. The evidence for resource use, presented in terms of length of hospital stay, was downgraded one level for serious study limitations, one level for indirectness, and one level for imprecision.Thus, we concluded that the evidence was of very low quality, meaning that we are very uncertain about these estimates.
For function and serious adverse events, the evidence for the comparison of single‐leg versus double‐leg spica casts was downgraded one level for serious study limitations, mainly reflecting high risks of bias associated with lack of blinding, one level for indirectness reflecting the short follow‐up, and one level for imprecision. The evidence for the outcomes relating to cast wear and time off by the caregiver was downgraded two levels for serious study limitations reflecting high risks of bias associated with lack of blinding and attrition. Despite the plausibility of the results for outcomes during cast wear, as implied by the low quality rating we are uncertain about the estimates.
Comparisons of different surgical interventions
The three comparisons were separately tested by three small quasi‐randomised trials. For all reported outcomes, the evidence was downgraded two levels for serious study limitations, mainly reflecting high risks of selection and performance biases, and one level for imprecision. Thus, we concluded that the evidence was of very low quality, meaning that we are very uncertain about the results.
Potential biases in the review process
This review followed the criteria and methods set out in our published protocol (Madhuri 2011),and followed recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). Our search was comprehensive and included the handsearching of conference proceedings and checks for ongoing trials. Additionally, we sent requests for information and full trial reports to authors of trials that were reported only in conference proceedings, or where there was a doubt regarding completeness of the data. It is possible that we have missed some potentially eligible trials but, if so, these may still not be suitable for inclusion, particularly if unpublished and inadequately reported. We guarded against study selection bias by the independent selection of eligible trials by two authors. We also adhered to the standard methods required of Cochrane Reviews (MECIR 2011).
Agreements and disagreements with other studies or reviews
We identified two systematic reviews from searching the Database of Reviews of Effectiveness (Centre for Reviews and Dissemination) in The Cochrane Library, and the Cochrane Database of Systematic Reviews, using the terms "femoral" AND "shaft" AND "fractures".
Alho 1996 was a meta‐analysis of retrospective case series. Wright 2000 searched MEDLINE till 1996 for English language reports and selected 15 cohort studies of children and adolescents with femoral fractures, but identified no randomised controlled trials (RCTs). Wright 2000 concluded that early application of a hip spica cast was associated with a shorter duration of hospital stay and low rates of malunion compared with traction. The RCT in our review compared early spica with skeletal traction followed by spica cast, but was under‐powered to detect significant differences between the two interventions. Wright 2000 also concluded that internal fixation gave low rates of malunion compared with early hip spica casting but was associated with high rates of over‐lengthening. Mehdinasab 2008, included in the present review, reported low quality evidence that intramedullary pin followed by spica casting may reduce malunion rates compared to traction followed by spica cast. We are not aware of any systematic reviews of RCTs addressing the objectives of this present review.
Authors' conclusions
Implications for practice.
This review did not find evidence from RCTs to inform clinical decisions regarding the management of femoral shaft fractures in those under three years or over 15 years of age, or those with open fractures.
There is insufficient evidence to determine if long‐term function differs between surgical and conservative treatment. Moderate quality evidence indicates that overall malunion rates would be lower in surgical interventions compared with conservative interventions in children aged between 3 and 12 years. Low quality evidence indicates that this benefit may be offset by increased incidence of serious adverse events. Elastic stable intramedullary nailing may reduce recovery time, such as return to school. The choice of intervention selected will also have to factor in the preference of the child and parents for surgical versus conservative interventions, the effects of disruption on their lives, as well as local costs for the interventions and their affordability.
There is insufficient evidence from comparisons of different methods of conservative treatment or of different methods of surgical treatment to draw conclusions on the relative effects of the treatments compared in the included trials.
Implications for research.
Further, methodologically sound, randomised trials are required to inform on the appropriate selection of interventions in children and adolescents with femoral shaft fractures. Future trials should conform to international standards in their design, conduct and reporting, should use standard definitions for outcomes, and estimate adequate sample sizes to ensure that potentially useful interventions are accurately identified. Assessing long‐term functional outcome, return to normal activities and parent and child satisfaction are crucial; as is cost analysis, especially for contrasting interventions. Parrticularly given the high incidence of reported radiographically‐defined malunion in conservatively‐treated children, research is needed to validate radiographic standards for malunion and to establish the extent of the relationship between malunion and later problems and long term functional outcome.
The selection of priority areas for research should take into account the current coverage of the evidence, current practice and differences in practice, and should involve consultation with patients and their families as to their preferences and values. Multicentre trials that reflect professional consensus on treatment uncertainties should facilitate sufficient recruitment and also implementation. Although the identification of priority topics requires input from others, we suggest two priority topics for research are:
Elastic stable intramedullary nailing (ESIN) versus hip spica cast. The trial population should include preschool children, and we suggest that any trial should be powered for this group as well as for older children.
ESIN versus submuscular plates. For this comparison, we suggest a special focus on pre‐adolescent children and thus any trial should be powered for this group as well as for older children.
What's new
| Date | Event | Description |
|---|---|---|
| 14 May 2019 | Amended | Declarations of interest updated. |
Acknowledgements
We acknowledge with gratitude the constructive comments and guidance on the protocol provided by Lindsey Elstub, Joanne Elliott, Mario Lenza, Neil Wilson and Helen Handoll. We also thank the senior author of Bar‐On 1997 for unpublished data, and Philippe Ravaud and Florence Aim of the French Cochrane Centre for translating Hsu 2009 from French. We thank Joanne Elliott for providing search results for the review and feedback on this aspect. We would also like to thank Lindsey Elstub, Helen Handoll, Laura MacDonald, Cathie Sherrington and Neil Wilson for their feedback and editorial help with the review.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (Wiley Online Library)
#1 MeSH descriptor: [Femoral Fractures] this term only (183) #2 MeSH descriptor: [Femur] this term only (522) #3 MeSH descriptor: [Fractures, Bone] this term only (1097) #4 MeSH descriptor: [Fracture Fixation] explode all trees (1077) #5 MeSH descriptor: [Fracture Healing] this term only (358) #6 #3 or #4 or #5 (2124) #7 #2 and #6 (32) #8 ((femur* or femor*) near/4 (fracture* or fixat* or stabili*)):ti,ab,kw (1211) #9 #1 or #7 or #8 (1220) #10 MeSH descriptor: [Pediatrics] explode all trees (473) #11 MeSH descriptor: [Infant] explode all trees (12193) #12 MeSH descriptor: [Adolescent] this term only (70293) #13 (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or teenage* or adolescen*):ti,ab,kw (140155) #14 #10 or #11 or #12 or #13 (140164) #15 (#9 and #14) in Trials (107)
MEDLINE (OvidSP)
1 Femoral Fractures/ (12732) 2 Femur/ (30265) 3 Fractures, Bone/ or exp Fracture Fixation/ or Fracture Healing/ (86520) 4 2 and 3 (2024) 5 ((femur* or femor*) adj4 (fracture* or fixat* or stabili*)).tw. (17746) 6 or/1,4‐5 (24918) 7 exp Pediatrics/ (42918) 8 exp Infant/ (935710) 9 exp Child/ (1543840) 10 Adolescent/ not exp Adult/ (479309) 11 (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or teenage* or adolescen*).tw. (1461444) 12 or/7‐11 (2546681) 13 6 and 12 (3635) 14 Randomized controlled trial.pt. (383304) 15 Controlled clinical trial.pt. (88946) 16 randomized.ab. (298690) 17 placebo.ab. (160672) 18 Drug Therapy.fs. (1741540) 19 randomly.ab. (211731) 20 trial.ab. (314769) 21 groups.ab. (1348102) 22 or/14‐21 (3370535) 23 exp Animals/ not Humans/ (4021928) 24 22 not 23 (2888552) 25 13 and 24 (297)
EMBASE (OvidSP)
1 Femur Fracture/ or Femur Shaft Fracture/ (16187) 2 Femur/ or Femur Shaft/ (32128) 3 Fracture/ or Fracture Treatment/ or Fracture Fixation/ or Fracture Healing/ (89328) 4 2 and 3 (2540) 5 ((femur* or femor*) adj4 (fracture* or fixat* or stabili*)).tw. (20559) 6 or/1,4‐5 (29301) 7 exp Pediatrics/ (71896) 8 exp Infant/ (529301) 9 exp Child/ (1703687) 10 Adolescent/ not exp Adult/ (465163) 11 (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or teenage* or adolescen*).tw. (1674415) 12 or/7‐11 (2528651) 13 and/6,12 (3882) 14 Randomized controlled trial/ (353771) 15 Clinical trial/ (887803) 16 Controlled clinical trial/ (404378) 17 Randomization/ (63137) 18 Single blind procedure/ (18070) 19 Double blind procedure/ (116998) 20 Crossover procedure/ (38092) 21 Placebo/ (223384) 22 Prospective study/ (246361) 23 ((clinical or controlled or comparative or placebo or prospective* or randomi#ed) adj3 (trial or study)).tw. (713794) 24 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (174815) 25 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (157338) 26 (cross?over* or (cross adj1 over*)).tw. (67509) 27 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (222673) 28 RCT.tw. (12318) 29 or/14‐28 (1851009) 30 Case Study/ or Abstract Report/ or Letter/ (902012) 31 29 not 30 (1813676) 32 13 and 31 (287)
CINAHL (Ebsco)
S1 (MH "Femoral Fractures") (2,224) S2 (MH "Femur") (4,682) S3 MH Fractures OR MH Fracture Fixation OR MH Fracture Healing (16,762) S4 S2 and S3 (555) S5 ( femur* N4 fracture* or femur* N4 fixat* or femur* N4 stabili* ) or ( femor* N4 fracture* or femor* N4 fixat* or femor* N4 stabili* ) (4,118) S6 S1 or S4 or S5 (4,357) S7 (MH "Pediatrics+") (10,080) S8 (MH "Infant+") (148,652) S9 (MH "Child+") (376,247) S10 MH Adolescence NOT MH Adult (130,333) S11 TX (paediatr* or pediatr* or neonate* or bab*3 or infant* or child* or teenage* or adolescen*) (713,657) S12 S7 or S8 or S9 or S10 or S11 (713,704) S13 S6 and S12 (874) S14 (MH "Clinical Trials+") (165,068) S15 (MH "Evaluation Research+") (19,689) S16 (MH "Comparative Studies") (72,882) S17 (MH "Crossover Design") (10,801) S18 PT Clinical Trial (74,400) S19 (MH "Random Assignment") (35,418) S20 S14 or S15 or S16 or S17 or S18 or S19 (261,753) S21 TX ((clinical or controlled or comparative or placebo or prospective or randomi?ed) and (trial or study)) (453,418) S22 TX (random* and (allocat* or allot* or assign* or basis* or divid* or order*)) (62,773) S23 TX ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) (687,750) S24 TX ( crossover* or 'cross over' ) or TX cross n1 over (13,537) S25 TX ((allocat* or allot* or assign* or divid*) and (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)) (78,957 S26 S21 or S22 or S23 or S24 or S25 (1,055,070) S27 S20 or S26 (1,118,691) S28 S13 and S27 (322)
Appendix 2. Assessment of risk of bias tool
| Domain | Description | Review authors’ judgement | Notes for specific assessments made for the review topic |
| Sequence generation | Describe the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups. | Was the allocation sequence adequately generated? | |
| Allocation concealment | Describe the method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment. | Was allocation adequately concealed? | |
| Blinding of participants, personnel and outcome assessorsAssessments should be made for each main outcome (or class of outcomes). | Describe all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective. | Was knowledge of the allocated intervention adequately prevented during the study? | Separate assessments / entries will be made for subjective (e.g. pain, patient‐reported function) and objective or 'hard' outcomes (e.g. adverse events) |
| Incomplete outcome dataAssessments should be made for each main outcome (or class of outcomes). | Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether attrition and exclusions were reported, the numbers in each intervention group (compared with total randomised participants), reasons for attrition/exclusions where reported, and any re‐inclusions in analyses performed by the review authors. | Were incomplete outcome data adequately addressed? | Separate assessments / entries will be made for subjective (e.g. pain, patient‐reported function) and objective or 'hard' outcomes (malunion, adverse events time to resume usual activities,) |
| Selective outcome reporting | State how the possibility of selective outcome reporting was examined by the review authors, and what was found. | Are reports of the study free of suggestion of selective outcome reporting? | |
| Other sources of bias | State any important concerns about bias not addressed in the other domains in the tool. If particular questions/entries were pre‐specified in the review’s protocol, responses should be provided for each question/entry. |
Was the study apparently free of other problems that could put it at a high risk of bias? | Two entries are pre‐specified. 1. Bias relating to major imbalances in key baseline characteristics (e.g. isolated versus combined fractures, age and gender). 2. Performance bias, such as lack of comparability in the experience of care providers. |
Appendix 3. Details of Dynamic Skeletal Traction Spica Casting (DSTSC)
From Hsu 2009:
"For phase II DSTSC, patients were placed in Buck’s traction on admission and then immediately placed in a DSTSC apparatus using ketamine sedation. Under sterile conditions, a Kirschner wire (0.062 in) was placed through the distal tibia anterior to the fibula at a distance 5–7 cm proximal to the tip of the lateral malleolus for skeletal traction. Xeroform (InvaCare, Elyria, OH) gauze was then applied followed by a felt pad which was secured using disc plates and Jurgan pin balls (Jurgan Development & Mfg, Madison, WI) to prevent lateral pin migration. The Kirschner wire was then attached to a traction bow and placed under tension. While maintaining manual traction, the patient was placed in a half hip spica cast with the fractured side and normal leg both casted above the knee. Femurs were positioned according to fracture level and were abducted 35–45°, externally rotated 10–15°,and flexed 20–30° (up to 45° for proximal fractures). The knee joint was free on the normal side and kept in full extension on the fracture side. The length of the traction brace was adjusted based on the child’s size, and the device was incorporated into a spica cast with plaster. Sheet wadding was applied to the brace at points of contact with the cast to facilitate later removal. The traction brace was aligned with the proper rotation along the longitudinal axis of the extremity, and then a traction bow was attached to the brace along with a tensioning device and 18‐gauge wire. Traction was provided by a coiled steel spring, and the device was tensioned by turning the wing nut until the desired amount overlap was achieved on radiographs. Traction force was measured using a handheld, spring‐loaded scale, and approximately 3.5–5.5 kg of traction was needed to achieve proper fracture overlap. The injured leg was supported by a cloth hammock while in the traction device and a few drops of 70% alcohol were placed at the pin sites through the overlying dressings. After discharge, patients were evaluated in the outpatient clinic and traction was adjusted until healing was sufficient to remove the apparatus and pin under sedation (about three to four weeks). Healing was typically achieved after eight to ten weeks, and after removal of the DSTSC system, patients used crutches if necessary to aid in walking for one month".
Data and analyses
Comparison 1. Surgical versus conservative treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Functional outcome at 2 years ‐ RAND scores (characteristics of scale unclear) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 External fixation versus immediate spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Malunion | 4 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.15, 0.59] |
| 2.1 External fixation versus immediate hip spica | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.17, 0.73] |
| 2.2 Intramedullary pin fixation versus spica cast | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.01, 2.23] |
| 2.3 Elastic stable intramedullary nailing (ESIN) versus skeletal traction followed by spica cast | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.62] |
| 2.4 Elastic stable intramedullary nailing (ESIN) versus dynamic skeletal traction casting | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Serious adverse events | 4 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.10, 5.17] |
| 3.1 External fixation versus immediate hip spica | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.52, 4.02] |
| 3.2 Intramedullary pin fixation plus spica cast versus skeletal traction followed by spica cast | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 10.89 [0.64, 185.79] |
| 3.3 Elastic stable intramedullary nailing (ESIN) versus skeletal traction followed by spica cast | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.38, 128.33] |
| 3.4 Elastic stable intramedullary nailing (ESIN) versus dynamic skeletal traction casting | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.26, 7.92] |
| 4 Time for recuperation or return to usual activities | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 External fixation versus immediate hip spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Elastic stable intramedullary nailing (ESIN) versus skeletal traction followed by spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Child satisfaction (scale 1 ‐ 11; 11 = 'very happy') | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 External fixation versus immediate hip spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Parent satisfaction (1 ‐ 11; 11 = 'very satisfied') | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 External fixation versus immediate hip spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Parent satisfaction (excellent or good) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Elastic stable intramedullary nailing (ESIN) versus skeletal traction followed by spica cast | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Hospital stay (days) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 External fixation versus immediate hip spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Elastic stable intramedullary nailing (ESIN) versus skeletal traction followed by spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Elastic stable intramedullary nailing (ESIN) versus dynamic skeletal traction spica cast | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Immediate hip spica cast versus skeletal traction followed by spica cast.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Malunion at cast removal (6 ‐ 8 weeks from injury) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Traction followed by functional orthosis versus traction followed by spica cast.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Malunion (assessed at 5 to 10 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 4. Single‐leg versus double‐leg spica cast.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Performance version of ASK (%: 100% = best result) | Other data | No numeric data | ||
| 2 Change in treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Serious adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Comfort and ease of care during cast use (VAS: visual analogue score 0 to 10 where 10 = most difficult) | Other data | No numeric data | ||
| 5 Caregiver took time off work | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 5. Elastic stable intramedullary nailing (ESIN) versus external fixation (Ext‐fix).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Malunion at 12+ months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Serious adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 6. Dynamic external fixation (Ext‐fix) versus static external fixation (Ext‐fix).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serious adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Time to resume full weight‐bearing | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 7. Intramedullary nailing versus submuscular plating.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unacceptable malunion | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Serious adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bar‐On 1997.
| Methods | Quasi‐randomised, parallel‐group, single‐centre, open‐label, controlled trial Country: Israel Setting: Hadassah Medical Centre, Jerusalem Duration: Recruitment over one year. Study submitted in March 1997 and published in November 1997 |
|
| Participants |
Participants: 19 children with 20 fractures (none were open) Age: 5 to 15 years of age Sex: no information Inclusion criteria: Children with fractures of the shaft of the femur
|
|
| Interventions |
Intervention:
Fractures were fixed with either stainless steel (6) or titanium nails (4); the first of the flexible nails was inserted from the lateral side, proximally in the 3 proximal‐third fractures, and from the distal end in the 7 mid‐ or distal‐third fractures. The second nail was inserted from the medial distal aspect. One fracture site had to be exposed to allow engagement of the distal fragment; the other 9 nailings were performed closed. One of the ESIN participants also had flexible nailing of an ipsilateral segmental tibial fracture. The ESIN procedures included the first 10 procedures done at the centre. Control:
Fractures were fixed with either of the 2 different external fixation devices Orthofix (7 fractures) (Orthofix SRL, Bussolengo (Vr), Italy) or an AO external fixator (3 fractures) (Mathys Medical Ltd, Bettlach, Switzerland). Operations were performed or directly supervised by surgeons with subspecialty training in either trauma or paediatric orthopaedics. The operations were performed on either a normal or a fracture table, and fluoroscopic control was used in all cases. |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: not stated Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote from report: "randomly allocated sequentially for management either by external fixation (EF) or by flexible intramedullary nailing (FIN)" Comment: Although baseline characteristics reported for both the groups were similar, quasi‐random allocation was used, and residual confounding is possible |
| Allocation concealment (selection bias) | High risk | Comment: Not reported but quasi‐random allocation used, precluding concealment of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: This was an open‐label trial and performance bias was possible. |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Comment: This was an open‐label trial with unclear allocation concealment. Also, the surgeons who were responsible for the management of the cases appear to have been the outcome assessors. However, it is unclear if this led to biases in detecting the objective outcomes in this review. |
| Blinding of outcome assessment (detection bias) Subjective outcomes (e.g. participant‐reported function) | High risk | Comment: This was an open‐label trial with unclear concealment of allocation that is prone to detection bias for subjective outcomes. The method of ascertaining parent satisfaction was also not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: 19 participants with 20 fractures were recruited in the study and all were followed up till a mean of 14 months ranging from 12 to 22 months. However, there was an incomplete report of the results, with potential for unit of analysis issues. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The trial was not prospectively registered. All pre‐stated outcomes were reported but not well defined. |
| Other bias | Low risk | Comment: Procedures were performed by trained personnel. No other biases were detected |
Domb 2002.
| Methods | Quasi‐randomised, parallel‐group, single‐centre, open‐label, controlled trial Country: USA Setting: Johns Hopkins School of Medicine, Baltimore, Maryland Duration: 1995 to 1999 |
|
| Participants |
Participants: 52 children with 53 fractures Age: 3 to 12 years of age (mean 7 years) Sex: 14 girls, 49 boys (1 child was counted twice) Inclusion criteria: children with "diaphyseal" fractures of femur Exclusion criteria: Not stated |
|
| Interventions |
Intervention:
Control:
All surgeries were performed using general anaesthesia by paediatric orthopaedic surgeons. The fractures were stabilised by 2 pins above and 2 pins below the fracture site. The external fixation was assembled using a unilateral frame and one longitudinal bar. Of the 25 in the dynamic group, 21 were dynamised at an average of 50 days after surgery (range 20 to 121 days). This was later that when early callus formation was seen (mean 23 days). 4 were not dynamised because participants did not return for follow‐up at the appropriate interval. |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: EBI Medical systems, Parsippany, New Jersey Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: " randomised according to their medical record number at the time of surgery" Comment: This does not permit concealment of allocation and is a quasi‐randomised method |
| Allocation concealment (selection bias) | High risk | Comment: Allocation concealment was not possible in this trial. Different fixators were used for each group and the surgeon knew which group the participant would fall into |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: This was an open‐label study |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Comment: This was an open‐label, quasi‐randomised trial with no mention of blind assessment. However, it is unclear if this led to biases in detecting the objective outcomes in this review. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All the participants were followed up till completion of the trial |
| Selective reporting (reporting bias) | Unclear risk | Comment: The trial was not prospectively registered. All pre‐stated outcomes were reported but not well defined. |
| Other bias | Low risk | Comment: The source of funding was EBI Medical Systems, Parsippany NJ. This company manufactures the EBI external fixator which was a part of this trial. However, the results and conclusions did not favour the EBI fixator. All surgeries were performed by paediatric orthopaedic surgeons. |
Hsu 2009.
| Methods | Randomised, single‐centre, open‐label, controlled trial Country: Philippines Setting: Department of Orthopaedic Surgery, Davao Medical Center, Davao City, Mindanao Duration: 2002 to 2006 |
|
| Participants |
Participants: 51 children (12 had grade 1 open fractures) Age: 5 to 12 years of age Sex: 10 girls, 41 boys Inclusion criteria: Children with a femoral fracture (age 5 to 12) Exclusion criteria:
|
|
| Interventions |
Intervention:
The standard technique for ESIN in children with femoral fractures was used. Retrograde insertion. Control:
Full details of procedures used for DSTSC provided in Appendix 3 |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Not stated Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "assigned by flipping a coin in order to reduce selection bias, and treatment was administered by the same two surgeons to reduce individual variability" |
| Allocation concealment (selection bias) | Unclear risk | Quote:"There were no major differences in fracture characteristics between groups and injury presentation" Comment: Unsure if residual confounding could be accurately measured. There was no mention of adequate safeguards; e.g. to prevent the coin being tossed again. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: This was an open‐label trial |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Quote: "Radiographs of all patients were measured and re‐measured by three separate examiners to verify the recorded data" Comment: As these examiners were viewing radiographs in groups treated either with flexible nails or dynamic skeletal traction spica cast, they would not be blind to treatment – rather the use of 3 examiners might have assessed inter‐observer judgment effects. However, is unclear if the lack of blinding introduced detection bias for the objective outcomes of malunion, and serious adverse events. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All participants included in the trial were followed up |
| Selective reporting (reporting bias) | Unclear risk | There was reference made to a protocol approved before data collection started. However, the trial was not prospectively registered and not all pre‐stated outcomes were reported |
| Other bias | Low risk | Comment: Treatment was provided by the same 2 surgeons to reduce variability. No other sources of bias detected |
Leu 2012.
| Methods | Randomised, open‐label, single‐centre, parallel‐assignment controlled trial Country: United States of America Setting: Department of Orthopaedic Surgery, The John Hopkins University/Johns Bayview Medical Center, Baltimore, MD Duration: May 2006 to August 2009 |
|
| Participants |
Participants: 52 children Age: 2 to 7 years of age Sex: 17 girls, 35 boys Inclusion criteria: Children with an acute diaphyseal femoral fracture Exclusion criteria:
|
|
| Interventions |
Intervention:
Control:
The standard technique for spica cast in children with femoral fractures was used. |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Nil Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "..were assigned to one of the two treatment groups via random selection of an opaque envelope that contained the word 'single' or 'double'." Comment: adequate randomisation was done |
| Allocation concealment (selection bias) | Unclear risk | Quote: "random selection of an opaque envelope that contained the word 'single' or 'double". Inadequate safeguards |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was an open‐label study |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | This was an open‐label study and the outcome assessors were not blinded. However, it is unclear if this led to biases in detecting the objective outcomes reported in this trial and used in the review. |
| Blinding of outcome assessment (detection bias) Subjective outcomes (e.g. participant‐reported function) | High risk | In this open‐label trial, participant‐rated satisfaction using the specially constructed visual analogue scales and functional outcomes rated by children on the Activites Scale for Kids were likely to have introduced bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of the twenty‐four patients in the single‐leg group, one could not have radiographs made at our institution; therefore, only the custom and activities surveys were evaluated for that child. In the single‐leg group, twenty‐one custom surveys and twenty‐one activities surveys were available for analysis. Of the twenty‐eight patients in the double‐leg group, twenty‐seven had radiographs, twenty‐three had custom surveys, and sixteen had activities surveys for comparison. With the contact information provided, it was not possible to reach the parents of the patients in either group who did not have custom surveys, activities surveys, or both. No family enrolled in the study refused to complete the surveys." Comment: Denominators for each outcome were reported with little difference between the 2 groups, except for ASK (see Other bias) |
| Selective reporting (reporting bias) | Low risk | Trial was retrospectively registered, but all relevant pre‐stated outcomes were reported |
| Other bias | High risk | Quote: "that substantial bias could have been introduced by the fact that the surveys were conducted at different points of time in the patients’ treatment" Comment: high risk for recall bias |
Malo 1999.
| Methods | Randomised, parallel‐group, open‐label, assessor‐blinded, controlled trial Country: Canada Setting: Orthopaedics Service, Department of Surgery, St Justine hospital, Montreal Duration: July 1982 to June 1984 |
|
| Participants |
Participants: 43 Age: 5 to 13 years of age Sex: 19 girls, 24 boys Inclusion criteria: Children with femoral shaft fractures Exclusion criteria: Open fractures, pathological, subtrochanteric, physeal injuries, including moderate to severe head injuries, medical conditions precluding early mobilisation |
|
| Interventions |
Intervention:
Control:
|
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcome reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Not stated Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote from report (translated from French): "The allocation of the type of final treatment was determined by a list previously produced by lots." Unequal allocation (spica cast = 28; functional orthosis = 15) is not explained. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of the method of allocation concealment. As stated above, the numbers randomised were unequal in the 2 arms and it is unclear if these imbalances were due to failure to recruit the estimated numbers and the use of simple as opposed to block randomisation. The estimated sample size was not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: The trial was open‐label. |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Low risk | Quote from report (translated from French): "A full and final assessment of 42 patients was performed by an independent observer with a minimum 5 years follow up." Comment: Outcomes were assessed blind to allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 1 child in the spica cast group was lost to follow‐up because their parents had moved. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The trial was not prospectively registered and only limited outcomes (long‐term malunion and number of hospital days and duration of wear of brace or cast) were reported. However, there is no indication in the report that other outcomes were to have been assessed. |
| Other bias | Low risk | Comment: No other potential biases were detected |
Mehdinasab 2008.
| Methods | Quasi‐randomised, open‐label, parallel‐group, controlled trial Country: Iran Setting: Two hospitals (Mehr Hospital, Kianpars, Ahwaz and Dept. of Orthopedics, Imam Khomeini Hospital, Azadegan Avenue, Ahwaz) Duration: May 2003 to February 2006 |
|
| Participants |
Participants: 70 children Age: 6 to 11 years of age Sex: 15 girls, 51 boys (of the 66 children followed up) Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention:
A 4 to 5 mm slightly bent pin was inserted retrograde first, into proximal fragment with the hip in flexion, adduction, and internally rotated and after reduction, into distal fragment. Pin end was bent above the greater trochanter subcutaneously. Control of reduction was performed by a C‐ arm fluoroscopy. Then a hip spica cast was applied Control:
In the operating room, under local anaesthesia after insertion of a 3 or 4 mm Steinman pin into proximal tibia, 90‐90 skeletal traction and leg support with sling was applied. Following primary callus formation and early union that was characterised by loss of pain, tenderness and motion at the fracture site, pin was removed and 1½ spica cast was applied |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Not stated Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Randomizing of patients into two groups was performed consecutively based on their order of presentation and hospitalization." Comment: Quasi‐randomised. Baseline characteristics of the 2 groups are not provided |
| Allocation concealment (selection bias) | High risk | Comment: Not concealed. Alternate participants were allotted to either treatment group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: This was an open‐label study and prone to the risk of performance bias |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Comment: This was an open‐label study. However, it is unclear if this led to biases in detecting the objective outcomes reported in this trial and used in the review |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Out of seventy 6‐11 years old children who were admitted and treated for closed femoral shaft fractures, four patients were lost to follow up and were excluded from study, but 66 cases (51 boys and 15 girls) were available and followed‐up for 6 months." Comment: Only 4 children were lost to follow‐up; outcome data for continuous outcomes were reported without measures of dispersion; some data inconsistencies (e.g. number with pin end irritation were present). |
| Selective reporting (reporting bias) | Unclear risk | Comment: Although the trial was not prospectively registered, the outcomes to be evaluated stated in the Methods were incompletely reported (no measures of dispersion) |
| Other bias | Unclear risk | Comment: The trial was conducted in 2 hospitals. Unclear if same standards applied in each hospital |
Park 2012.
| Methods | Quasi‐randomised, open‐label, controlled trial; 2 centres Country: Republic of Korea Setting: Kyungpook National University hospital, Daegu (the other participating hospital was not identified) Duration: January 2006 to December 2009 |
|
| Participants |
Participants: 47 children with 49 fractures (2 bilateral); reporting for 43 children with 45 fractures (3 were open fractures) Age: 11 to 17.4 years Sex: 9 girls, 34 boys Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention: Trochanteric entry intramedullary nail (N = 21 children, 22 fractures) Control: Submuscular locked plate (N = 22 children, 22 fractures) |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: National University research fund 2011 Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were alternatively treated by IN [intramedullary nail] or SP [submuscular plate], according to the time of arrival" Comment: quasi‐randomised |
| Allocation concealment (selection bias) | High risk | Not mentioned; alternate allocation precludes concealment of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: this was an open‐label study and prone to the risk of performance bias |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Comment: this was an open‐label study. However, it is unclear if this led to biases in detecting the objective outcomes reported in this trial and used in the review |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data were provided for 4 participants (2 died post‐operatively and 2 had insufficient follow‐up) including group allocation. Although there was one participant with bilateral fractures in each group, there were no details on the specific outcome of these participants. |
| Selective reporting (reporting bias) | Low risk | Comment: although the trial was not prospectively registered, the outcomes to be evaluated stated in the Methods were completely reported |
| Other bias | Low risk | No other sources of bias were evident |
Shemshaki 2011.
| Methods | Randomised, open‐label, assessor‐blinded, controlled trial Country: Iran Setting: Two university hospitals in Isfahan Duration: February 2009 to January 2010 |
|
| Participants |
Participants: 46 children Age: 6 to 12 years of age Sex: 15 girls, 31 boys Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention:
The standard TEN technique was applied. 2 titanium elastic nails were retrogradely inserted through the distal part of the femur. Control:
Participants in the spica cast group were treated with skeletal traction for about 3 weeks and then with a spica cast. The pin was removed after sufficient callus consolidation had been achieved, and a 1½ hip spica was applied in the operating room under general anaesthesia. |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Isfahan University of Medical Sciences Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using random allocation software, patients were divided into two groups of TEN and spica cast and were treated by a single orthopedic surgeon." |
| Allocation concealment (selection bias) | Unclear risk | Comment: Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: The study was open‐label |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Low risk | Comment: The study was assessor blinded (according to the trials registration document) |
| Blinding of outcome assessment (detection bias) Subjective outcomes (e.g. participant‐reported function) | High risk | Comment: Methods of assessing parent satisfaction were not clear in this open label study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "51 met the inclusion criteria (four patients had open fractures). Five patients did not agree to participate in the study protocol, so 46 children with simple closed femoral fractures (23 in each group) entered and completed the study." |
| Selective reporting (reporting bias) | Low risk | Comment: The study was retrospectively registered; however, all the outcomes in the methods were reported and met the stated objectives |
| Other bias | Unclear risk | Comment: The trial was conducted in 2 hospitals. Unclear if the "single surgeon" referred to operated on all participants or if each hospital had a separate surgeon. Data from both hospital not presented separately to evaluate comparable outcomes |
Siddiqui 2008.
| Methods | Randomised, parallel‐group, open‐label, controlled trial Country: Pakistan Setting: Dow University of Health Sciences & Civil Hospital, Karachi Duration: June 2004 to May 2006 |
|
| Participants |
Participants: 42 children Age: 3 to 10 years of age Sex: 13 girls, 29 boys Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention:
Participants were kept on long leg POP slabs for about 24 to 48 hours. After this period,a 1½ spica cast was applied in the operation theatre under general anaesthesia. The spica was kept for 6 to 8 weeks. Control:
Before the application of spica cast, a Thomas’ splint adhesive plaster was applied both medially and laterally from mid thigh to foot. Traction was applied for 3 to 4 weeks with radiological confirmation done weekly to ensure no over‐riding. The spica cast was applied for another 3 to 4 weeks before physiotherapy commenced. |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Not stated Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "They were randomly assigned to two groups:" Comment: Unclear what method was used to generate the random sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: This trial was not blinded and allocation may not have been concealed; performance bias is likely |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Comment: This was an open‐label study. However, it is unclear if this led to biases in detecting the objective outcome (malunion) reported in this trial and used in the review |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All participants were followed up until completion of the trial (at cast removal) |
| Selective reporting (reporting bias) | Unclear risk | Comment: This trial was not prospectively registered, and only unsatisfactory outcome (malunion) was reported; however, there is no indication in the report that other outcomes were to have been assessed. |
| Other bias | Low risk | Comment: No other potential biases were detected |
Wright 2005.
| Methods | Multi‐centre, parallel‐group, open‐label, assessor‐blinded, randomised controlled trial Country: Multi‐centre international trial (Canada, USA, Australia and New Zealand) Setting: Hospital for Sick Children, Toronto, Canada; Royal Children’s Hospital, Melbourne, Australia; Los Angeles Children’s Hospital, Los Angeles, USA; and Starship Children’s Hospital, Auckland, New Zealand Duration: October 1994 to October 2002 |
|
| Participants |
Participants: 108 children Age: 4 to 10 years Sex: 32 girls, 76 boys Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention:
Control:
Children in the external‐fixator group were given general anaesthesia for a closed reduction of the fracture and application of a dynamised Orthofix external fixator (Orthofix, McKinney, TX, USA) |
|
| Outcomes |
Outcomes reported in the trial and used in this review:
Outcomes reported in the trial but not used in this review:
Outcomes sought for this review but not reported in the trial:
|
|
| Notes |
Funding: Medical Research Council (MRC) of Canada (grants MT12788, MA‐12788, MA‐12788 renewal, and 95048) and the Canadian Orthopaedic Research Education Association. Funders had no role in the conduct or reporting of trial. Canadian Institutes of Health Research provided peer review of the grant application Notes:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"A biostatistician who had no further involvement in the trial created the computer‐generated randomisation schedule using SAS (version 8.2)" Quote: "To ensure masking at randomisation, children were allocated in blocks of variable size by three strata:hospital, surgeon, and age (4–6 years and 7–10 years)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Opaque envelopes, which were sequentially numbered, were kept in the operating room. Once consent for inclusion in the study was obtained, the envelopes were opened by the operating surgeon to allow for appropriate preparation for the operating‐room staff." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Trial was open‐label |
| Blinding of outcome assessment (detection bias) Objective outcomes (e.g. malunion) | Unclear risk | Quote: "Clinical assessments at 3 months, 9 months, 15 months, and 24 months after the fracture were done by physicians unaware of the child’s treatment regimen, previous assessments, and study protocol. Children wore tights to mask treatment allocation. For assessment of the primary outcome of fracture malunion a single reader, unaware of the treatment children received, the date of the radiograph, and the study protocol, reviewed all radiographs using a standard protocol at a central location" Comment: Outcome assessment appears to have been done blind to treatment allocation but the treatments being compared were external fixator and Immediate spica cast ‐ the pins tracks in the external fixator group would have been likely to be evident on radiographs. However, it is unclear if this biased outcome estimates . |
| Blinding of outcome assessment (detection bias) Subjective outcomes (e.g. participant‐reported function) | High risk | Comment: Treatments were not blinded and could have influenced subjective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of 108 enrolled children, 101 (94%) completed the 2‐year assessment" Comment: in the hip spica group 56/60 (93%) and in the external fixation group 45/48 (94%) reached the 2‐year assessment |
| Selective reporting (reporting bias) | Low risk | Comment: The trial was not registered in a clinical trials registry, but the primary and secondary outcome measures mentioned in the Methods were reported in the results |
| Other bias | Low risk | Comment: No other biases were detected |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agarwal 2004 | RCT: separate data for the few children with femur fracture are unavailable. It is unlikely that a full report will ever be published |
| Ali 2005 | Not RCT: non‐probability sampling was used |
| Altay 2011 | Not RCT: retrospective study |
| Ansari 2011 | RCT: study population were only adult participants |
| Buechsenschuetz 2002 | Not RCT: retrospective study |
| Curtis 1995 | Not RCT: although described as randomised and prospective, "patients were divided randomly according to surgeon's preference", and data collection and case selection were done retrospectively |
| Flynn 2004 | Not RCT: case series |
| Flynn 2011 | Not RCT: prospective cohort |
| Gupta 2007 | Not RCT: case series |
| Ramseier 2007 | Not RCT: retrospective study |
Characteristics of studies awaiting assessment [ordered by study ID]
Shaikh 2012.
| Methods | Quasi‐randomised (non probability purposive sampling) clinical trial |
| Participants |
Participants: 60 children Age: 2 to 10 years Sex: both sexes Inclusion criteria: all femoral shaft fractures Exclusion criteria: none listed |
| Interventions |
Intervention Group 1: 24‐hour skin traction followed by spica cast Intervention Group 2: 20‐ to 30‐day traction followed by spica cast |
| Outcomes |
Outcomes reported: Primary outcomes:
Secondary outcomes:
Outcomes sought but not reported: Prmary outcomes
Secondary outcome
|
| Notes | Only abstract available. Study details awaited |
Ucar 2013.
| Methods | Randomised controlled trial |
| Participants |
Participants: 29 children Mean age: 8 years Group 1 and 8.2 years group 2 Sex: both sexes Inclusion criteria: all femoral shaft fractures Exclusion criteria: none listed |
| Interventions |
Intervention Group 1: closed reduction and titanium elastic nailing (n = 15). Follow‐up 24.8 months Intervention Group 2: mini open reduction and titanium elastic nailing (n = 14). Follow‐up 28.8 months |
| Outcomes |
Outcomes reported that could be used: Primary outcomes:
Secondary outcomes:
Outcomes sought but not reported: Secondary outcomes:
|
| Notes | Only abstract available. Study details awaited |
Differences between protocol and review
1. Child/parent satisfaction: it was felt that the expectations of the child may be different from that of the parent. In some trials, the outcomes were separately reported, hence this single outcome was split into two outcomes.
2. We re‐ordered the presentation of the comparisons in analyses, results and discussion compared to the order used in the protocol, in order to evaluate and discuss the comparisons in a clinically meaningful manner.
Contributions of authors
Vrisha Madhuri: conceived the review, drafted and wrote the protocol and review, assessed risk of bias, checked extracted data and corrected the final draft. Vivek Dutt: drafted and wrote the protocol and the review, selected trials, extracted data, assessed risk of bias, entered data, interpreted data and corrected the final draft. Abhay Gahukamble: drafted the protocol, selected trials, extracted data, assessed risk of bias. Prathap Tharyan: checked the protocol, checked excluded studies, extracted and entered data, assessed risk of bias, interpreted data, constructed 'Summary of findings' tables and wrote the final version of the review. All authors approved the final version of the review.
Sources of support
Internal sources
-
Christian Medical College, Vellore, India.
Salaries of all authors; logistic support
-
South Asian Cochrane Network and Centre, Vellore, India.
Protocol development and review completion workshops
External sources
-
Effective Health Care Research Consortium, UK.
Funding for the South Asian Cochrane Centre to build capacity to undertake systematic reviews via a programme grant to the Liverpool School of Tropical Medicine (Paul Garner) from UKaid (Department for International Development) in aid of developing countries. PT is a programme partner.
Declarations of interest
Vrisha Madhuri: was Course Chairman for an AO paediatric course 2013 and was Co‐Chairman in 2009. There were no personal or institutional financial gains; however local travel and accomodation were arranged by the education wing of the AO Foundation India. An honorarium for the days of the course was paid by the International AO Education but it was not received personally or by the institution; it went into the AO Education Fund India. AO Foundation and their education activities are related to Synthes company, which manufactures implants for fixing femur fractures. on Vivek Dutt: none known Abhay D Gahukamble: none known Prathap Tharyan: none known
Note added 14 May 2019: The Cochrane Funding Arbiters have judged that this review breaches Cochrane's commercial sponsorship policy, published 8 March 2014, in relation to the following criterion: 'The lead author and more than 50% of all authors must not have received other types of financial support from an industry sponsor with an interest in the review.' Specifically, although not having a personal financial gain, the lead author (VM) had travel costs, accommodation and an honorarium paid from the AO Foundation which is linked with Synthes, a company that manufactures implants for fixing femur fractures.
Edited (no change to conclusions)
References
References to studies included in this review
Bar‐On 1997 {published data only}
- Bar‐On E, Sagiv S, Porat S. External fixation or flexible intramedullary nailing for femoral shaft fractures in children. A prospective, randomised study. Journal of Bone and Joint Surgery ‐ British Volume 1997;79(6):975‐8. [DOI] [PubMed] [Google Scholar]
- Bar‐on E, Sagiv S, Howard CB, Porat S. External fixation vs flexible intramedullary nailing of femoral shaft fractures in children: a prospective randomized study [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1997;79 Suppl 3:344. [DOI] [PubMed] [Google Scholar]
- Bar‐on E, Sagiv S, Howard CB, Porat S. External fixation vs flexible intramedullary nailing of femoral shaft fractures in children: a prospective randomized study [abstract]. Orthopaedic Transactions 1997;21(2):673. [DOI] [PubMed] [Google Scholar]
Domb 2002 {published data only}
- Domb BG, Sponseller PD, Ain M, Miller NH. Comparison of dynamic versus static external fixation for pediatric femur fractures. Journal of Pediatric Orthopedics 2002;22(4):428‐30. [PubMed] [Google Scholar]
Hsu 2009 {published data only}
- Hsu AR, Diaz HM, Penaranda NR, Cui HD, Evangelista RH, Rinsky L, et al. Dynamic skeletal traction spica casts for paediatric femoral fractures in a resource‐limited setting. International Orthopaedics 2009;33(3):765‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leu 2012 {published data only}
- Leu D. Spica casting in pediatric femur fractures: study of single leg versus double leg spica casts. http://apps.who.int/trialsearch/trial.aspx?trialid=NCT01293916 (accessed 21 July 2014). [DOI] [PubMed]
- Leu D, Sargent MC, Ain MC, Leet AI, Tis JE, Sponseller PD. Spica casting for pediatric femoral fractures: a prospective, randomized controlled study of single‐leg versus double‐leg spica casts. Journal of Bone and Joint Surgery ‐ American Volume 2012;94(14):1259‐64. [DOI] [PubMed] [Google Scholar]
Malo 1999 {published data only}
- Malo M, Grimard G, Morin B. Treatment of diaphyseal femoral fractures in children: a clinical study [Traitement des fractures diaphysaires du femur chez l'enfant: Un essai clinique]. Annales de Chirurgie. 1999;53(8):728‐34. [PubMed] [Google Scholar]
Mehdinasab 2008 {published data only}
- Mehdinasab SA, Nejad SAM, Sarrafan N. Short term outcome of treatment of femoral shaft fractures in children by two methods: Traction plus casting, versus intramedullary pin fixation: a comparative study. Pakistan Journal of Medical Sciences 2008;24(1):147‐51. [Google Scholar]
Park 2012 {published data only}
- Park KC, Oh CW, Byun YS, Oh JK, Lee HJ, Park KH, et al. Intramedullary nailing versus submuscular plating in adolescent femoral fracture. Injury 2012;43(6):870‐5. [DOI] [PubMed] [Google Scholar]
Shemshaki 2011 {published data only}
- Shemshaki H. Titanium elastic nailing versus hip spica cast in treatment of femoral fractures in children. http://apps.who.int/trialsearch/trial.aspx?trialid=NCT01190696 (accessed 18 July 2014). [DOI] [PMC free article] [PubMed]
- Shemshaki HR, Mousavi H, Salehi G, Eshaghi MA. Titanium elastic nailing versus hip spica cast in treatment of femoral‐shaft fractures in children. Journal of Orthopaedics and Traumatology 2011;12(1):45‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siddiqui 2008 {published data only}
- Siddiqui MA, Pirwani MA, Naz N, Rehman AU, Soomro YH. Skin traction followed by spica cast versus early spica cast in femoral shaft fractures of children. Pakistan Journal of Surgery 2008;24(1):38‐41. [Google Scholar]
Wright 2005 {published data only}
- Wong J, Boyd R, Keenan NW, Baker R, Selber P, Wright JG, et al. Gait patterns after fracture of the femoral shaft in children, managed by external fixation or early hip spica cast. Journal of Pediatric Orthopaedics 2004;24(5):463‐71. [DOI] [PubMed] [Google Scholar]
- Wright JG, Wang EEL, Owen JL, Stephens D, Graham HK, Hanlon M, et al. Treatments for paediatric femoral fractures: a randomised trial. Lancet 2005;365(9465):1153‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agarwal 2004 {published data only}
- Agarwal A, Hammer A, Deep K, Morar Y, Jones CB, Nascone JW. Is elastic intramedullary nailing technique better in children? A prospective randomised trial [abstract]. American Academy of Orthopaedic Surgeons Annual Meeting; 2006 Mar 22‐26; Chicago (IL). www3.aaos.org/education/anmeet/anmt2006/podium/ppr06_22.cfm (accessed 26 March 2008) 2006.
- Agarwal A, Hammer AJ, Deep D, Morar Y. Is elastic intramedullary nailing technique better in children? A prospective randomized trial. European Journal of Trauma 2004;30(3):214. [Google Scholar]
- Agarwal A, Selven, Hammer AJ, Deep K, Morar Y. Is elastic intramedullary nailing technique better in children? A prospective randomised trial [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 2006;88(Suppl 1):119. [Google Scholar]
Ali 2005 {published data only}
- Ali M, Raza A. Union and complications after Thomas splint and early hip spica for femoral shaft fractures in children. Journal of College of Physicians and Surgeons Pakistan 2005;15(12):799‐801. [PubMed] [Google Scholar]
Altay 2011 {published data only}
- Altay MA, Erturk C, Cece H, Isikan UE. Mini‐open versus closed reduction in titanium elastic nailing of paediatric femoral shaft fractures: a comparative study. Acta Orthopaedica Belgica 2011;77(2):211‐7. [PubMed] [Google Scholar]
Ansari 2011 {published data only}
- Ansari Moein CM, Duis HJ, Oey PL, Kort GAP, Meulen W, Werken Chr. Intramedullary femoral nailing through the trochanteric fossa versus greater trochanter tip: a randomized controlled study with in‐depth functional outcome results. European Journal of Trauma and Emergency Surgery 2011;37(6):615‐22. [DOI] [PubMed] [Google Scholar]
Buechsenschuetz 2002 {published data only}
- Buechsenschuetz KE, Mehlman CT, Shaw KJ, Crawford AH, Immerman EB. Femoral shaft fractures in children: traction and casting versus elastic stable intramedullary nailing. Journal of Trauma‐Injury Infection and Critical Care 2002;53(5):914‐21. [DOI] [PubMed] [Google Scholar]
Curtis 1995 {published data only}
- Curtis JF, Killian JT, Alonso JE. Improved treatment of femoral shaft fractures in children utilizing the pontoon spica cast: a long‐term follow‐up. Journal of Pediatric Orthopedics 1995;15(1):36‐40. [DOI] [PubMed] [Google Scholar]
Flynn 2004 {published data only}
- Flynn JM, Luedtke LM, Ganley TJ, Dawson J, Davidson RS, Dormans JP, et al. Comparison of titanium elastic nails with traction and a spica cast to treat femoral fractures in children. Journal of Bone and Joint Surgery ‐ American Volume 2004;86(4):770‐7. [DOI] [PubMed] [Google Scholar]
Flynn 2011 {published data only}
- Flynn JM, Garner MR, Jones KJ, D'Italia J, Davidson RS, Ganley TJ, et al. The treatment of low‐energy femoral shaft fractures: a prospective study comparing the "walking spica" with the traditional spica cast. Journal of Bone and Joint Surgery ‐ American Volume 2011;93(23):2196‐202. [DOI] [PubMed] [Google Scholar]
Gupta 2007 {published data only}
- Gupta MN, Salaria AQ, Gupta R, Sharma S, Bala S, Basit MA. Treatment of fracture shaft of femur in children (a comparative study of operative versus conservative management). JK Practitioner 2007;14(1):28‐30. [Google Scholar]
Ramseier 2007 {published data only}
- Ramseier LE, Bhaskar AR, Cole WG, Howard AW. Treatment of open femur fractures in children: Comparison between external fixator and intramedullary nailing. Journal of Pediatric Orthopaedics 2007;27(7):748‐50. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Shaikh 2012 {published data only}
- Shaikh AH, Gulzar SA, Ahmed KZ, Bilal FS. A comparative study between early spica cast and skin traction followed by spica cast. Medical Channel 2012;18(2):88‐92. [Google Scholar]
Ucar 2013 {published data only}
- Ucar BY, Gem M, Azboy I, Demirtas A, Bulut M, Alemdar C, et al. Osteosynthesis with TEN in pediatric femoral fractures; closed or mini‐open?. Injury 2013;44(S2):33. [Google Scholar]
Additional references
Alho 1996
- Alho A. Concurrent ipsilateral fractures of the hip and femoral shaft: a meta‐analysis of 659 cases. Acta Orthopaedica Scandinavica. 1996;67(1):19‐28. [DOI] [PubMed] [Google Scholar]
Altman 2003
- Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326(7382):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bridgman 2004
- Bridgman S, Wilson R. Epidemiology of femoral fractures in children in the West Midlands region of England 1991 to 2001. Journal of Bone and Joint Surgery ‐ British Volume 2004;86(8):1152‐7. [DOI] [PubMed] [Google Scholar]
Daltroy 1998
- Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. Journal of Pediatric Orthopedics 1998;18(5):561‐71. [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Eisen 1980
- Eisen M, Donald CA, Ware JEJ, Brook RH. Conceptualization and measurement of health for children in the health insurance study;. Conceptualization and measurement of health for children in the health insurance study; RAND R‐2313‐HEW. Santa Monica, CA, USA: RAND Health, 1980. [Google Scholar]
Flynn 2006
- Flynn JM, Skaggs D. Chapter 22: Femoral shaft fractures. In: Kasser J, Beaty J editor(s). Rockwood & Wilkins' Fractures in Children. Philadelphia: Lippincott Williams & Wlkins, 2006:893‐936. [Google Scholar]
GRADE 2004 [Computer program]
- Version 3.2 for Windows. Jan Brozek, Andrew Oxman, Holger Schünemann. GRADEpro. Version 3.2 for Windows. Jan Brozek, Andrew Oxman, Holger Schünemann, 2008.
Gustilo 1976
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty‐five open fractures of long bones: retrospective and prospective analyses. Journal of Bone and Joint Surgery‐American Volume 1976;58(4):453‐8. [PubMed] [Google Scholar]
Gustilo 1984
- Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. Journal of Trauma‐Injury, Infection and Critical Care 1984;24(8):742‐6. [DOI] [PubMed] [Google Scholar]
Hedequist 2008
- Hedequist D, Bishop J, Hresko T. Locking plate fixation for pediatric femur fractures. Journal of Pediatric Orthopedics 2008;28(1):6‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kocher 2010
- Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of pediatric diaphyseal femur fracture. Journal of Bone and Joint Surgery ‐ American Volume 2010;92(8):1790‐2. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J (editors). Chapter 6: Searching for studies. Box 6.4.c. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Loder 2006
- Loder RT, O'Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur fractures in children. Journal of Pediatric Orthopedics 2006;26(5):561‐6. [DOI] [PubMed] [Google Scholar]
Malkawi 1986
- Malkawi H, Shannak A, Hadidi S. Remodeling after femoral shaft fractures in children treated by the modified Blount method. Journal of Pediatric Orthopedics 1986;6(4):421‐9. [DOI] [PubMed] [Google Scholar]
MECIR 2011
- Chandler J, Churchill R, Higgins J, Lasserson T, Tovey D. Methodological Expectations of Cochrane Intervention Reviews (MECIR). Methodological standards for the conduct of new Cochrane Intervention Reviews. Version 2.1, 8 December 2011. Available at: www.editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/MECIR_conduct_standards%202.1.pdf (accessed 4 November 2012).
PODCI 2005
- American Academy of Orthopaedic Surgeons. Pediatric Outcomes Questionnaire (Pediatric Outcomes Data Collection Instrument). www.aaos.org/research/outcomes/Pediatric.pdf August 2005.
Resch 1989
- Resch H, Oberhammer J, Wanitschek P, Seykora P. Rotational deformities following pediatric femoral shaft fracture [Der Rotationsfehler nach kindlicher Oberschenkelschaftfraktur]. Aktuelle Traumatologie 1989;19(2):77‐81. [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH (editors). Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org ..
Slongo 2007
- Slongo TF, Audigé L. Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF). Journal of Orthopaedic Trauma 2007;21(10 Suppl):S135‐60. [DOI] [PubMed] [Google Scholar]
Wright 2000
- Wright JG. The treatment of femoral shaft fractures in children: a systematic overview and critical appraisal of the literature. Canadian Journal of Surgery 2000;43(3):180‐9. [PMC free article] [PubMed] [Google Scholar]
Young 2000
- Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the activities scale for kids. Journal of Clinical Epidemiology 2000;53:125‐37. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Madhuri 2011
- Madhuri V, Gahukamble AD, Dutt V, Tharyan P. Interventions for treating femoral shaft fractures in children and adolescents. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.CD009076] [DOI] [PMC free article] [PubMed] [Google Scholar]


