Key Points
Question
What proportion of cancer cases is attributable to excess body weight in each state in the United States?
Findings
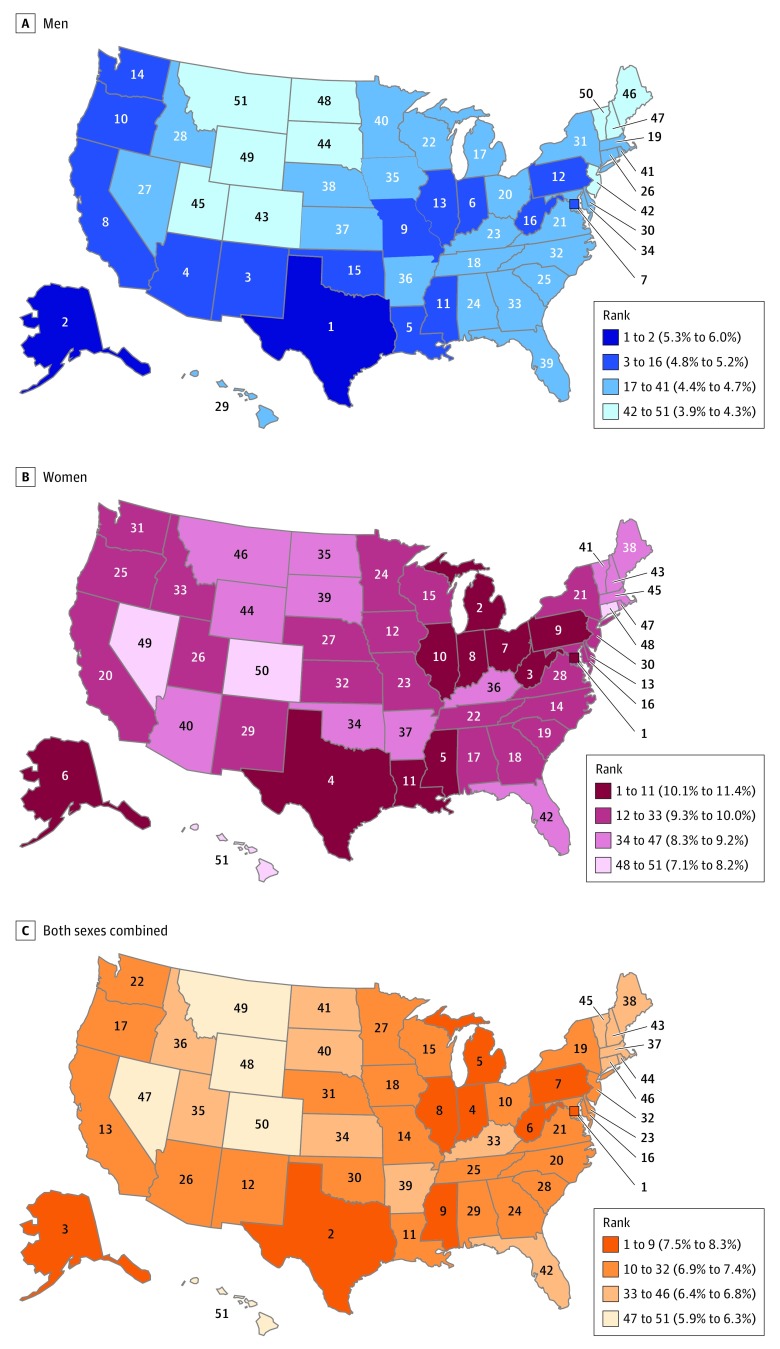
This nationwide cross-sectional study of US adults found that the proportion of cancers attributable to excess body weight ranges from 3.9% to 6.0% among men and from 7.1% to 11.4% among women, with the highest proportions found in several southern and midwestern states, Alaska, and the District of Columbia.
Meaning
There is a need for broad implementation of known interventions to reduce excess body weight, and potentially, the risk of associated cancers and other diseases.
This cross-sectional study analyzes the proportion of cancer cases attributable to excess body weight in each US state using data from several databases.
Abstract
Importance
Excess body weight (EBW) is an established cause of cancer. Despite variations in the prevalence of EBW among US states, there is little information on the EBW-related cancer burden by state; this information would be useful for setting priorities for cancer-control initiatives.
Objective
To calculate the population attributable fraction (PAF) of incident cancer cases attributable to EBW among adults 30 years or older in 2011 to 2015 in all 50 states and the District of Columbia.
Design, Setting, and Participants
State-level, self-reported body mass index (BMI [calculated as weight in kilograms divided by height in meters squared]) data from the Behavioral Risk Factor Surveillance System were adjusted by sex, age, race/ethnicity, and education using objectively measured BMI values from the National Health and Nutrition Examination Survey. Age- and sex-specific cancer incidence data by state were obtained from the US Cancer Statistics database. All analyses were performed between February 15, 2018, and July 17, 2018.
Main Outcomes and Measures
Sex-, age-, and state-specific adjusted prevalence estimates for 4 high BMI categories and corresponding relative risks from large-scale pooled analyses or meta-analyses were used to compute the PAFs for each US state for esophageal adenocarcinoma, multiple myeloma, and cancers of the gastric cardia, colorectum, liver, gallbladder, pancreas, female breast, corpus uteri, ovary, kidney and renal pelvis, and thyroid.
Results
Each year, an estimated 37 670 cancer cases in men (4.7% of all cancer cases excluding nonmelanoma skin cancers) and 74 690 cancer cases in women (9.6%) 30 years or older in the United States were attributable to EBW from 2011 to 2015. In both men and women, there was at least a 1.5-fold difference in the proportions of cancers attributable to EBW between states with the highest and lowest PAFs. Among men, the PAF ranged from 3.9% (95% CI, 3.6%-4.3%) in Montana to 6.0% (95% CI, 5.6%-6.4%) in Texas. The PAF for women was approximately twice as high as for men, ranging from 7.1% (95% CI, 6.7%-7.6%) in Hawaii to 11.4% (95% CI, 10.7%-12.2%) in the District of Columbia. The largest PAFs were found mostly in southern and midwestern states, as well as Alaska and the District of Columbia.
Conclusions and Relevance
The proportion of cancers attributable to EBW varies among states, but EBW accounts for at least 1 in 17 of all incident cancers in each state. Broad implementation of known community- and individual-level interventions is needed to reduce access to and marketing of unhealthy foods (eg, through a tax on sugary drinks) and to promote and increase access to healthy foods and physical activity, as well as preventive care.
Introduction
Excess body weight (EBW) is known to be associated with 13 cancer types.1 Incidence rates of several EBW-related cancer types have increased in the United States in the past few decades,2,3 which may be in part owing to the increase in EBW prevalence.4 Since the 1960s, more than one-third of Americans have been overweight,5 with a body mass index (BMI [calculated as weight in kilograms divided by height in meters squared]) of 25 to 29.9. However, the prevalence of obesity (BMI ≥30) considerably increased from 13% in the 1970s to 38% in 2014 for obesity overall and from 1% to 8% for class 3 obesity (BMI ≥40).5
The population attributable fraction (PAF) is an estimate of the proportion of a given outcome attributable to a given risk factor. Several studies have estimated the PAF for EBW-related cancer in the United States.4,6,7,8 We recently showed that 7.8% (n = 123 300) of all cancers (excluding nonmelanoma skin cancers) among adults 30 years and older in 2014 were attributable to EBW, with a higher burden among women (10.9%; n = 85 680 cases) than men (4.8%; n = 37 670 cases).6 To our knowledge, however, only 1 modeling study has estimated the PAF for EBW-related cancer by state, despite substantial variations in EBW prevalence across states.4 Nevertheless, that study was limited because it provided EBW-related PAFs for cancer mortality, years lived with disability (YLD), and disability-adjusted life-years (DALYs) but not for incident cancer cases. PAFs for mortality may not fully capture the burden of cancers with relatively longer survival (eg, breast cancer). For example, the estimated PAF for cancer mortality was higher for men than women in Kentucky in 2016 (6.8% vs 6.3%)9 despite a higher obesity prevalence in women than in men.10 Furthermore, the proportion of YLD and DALYs attributable to EBW are more difficult to interpret and are based on more assumptions (eg, complications of cancer)9 than PAFs for incident cancer cases.
In this article, we estimate the contemporary PAF and the number of incident cancer cases attributable to EBW by sex in all 50 states and the District of Columbia using representative exposure and cancer occurrence data. This information would be useful to help states set priorities for cancer control initiatives.
Methods
This study was based on deidentified publicly available data and did not require institutional review board approval or patient written consent. The list of cancer types associated with EBW were obtained from a report published by the International Agency for Research on Cancer (Table 1).1 Relative risks (RRs) were obtained from large-scale pooled analyses or meta-analyses of studies mostly conducted in North America and/or Europe (Table 1).11,12,13,14,15
Table 1. Cancer Types Associated With Excess Body Weight and Corresponding Relative Risks.
| Cancer Type | ICD-10 Codes | Relative Risk (95% CI) per 5-Unit Increase in BMI | Region of Relative Risk |
|---|---|---|---|
| Colorectum | C18-C20, C26.0 | 1.04 (1.02-1.06)11 | North America |
| Esophagus | C15 (adenocarcinoma only)a | 1.48 (1.35-1.62)12 | North America, Europe |
| Stomach | C16.0 (cardia only) | 1.31 (1.18-1.45)12 | North America, Europe |
| Liver | C22.0, C22.2-C22.4, C22.7, C22.9 | 1.59 (1.35-1.87)12 | Europe |
| Gallbladder | C23 | 1.29 (1.20-1.39)12 | North America |
| Pancreas | C25 | 1.14 (1.07-1.21)13 | North America, Europe, Australia |
| Breast (female) | C50 (postmenopausal only) | 1.10 (1.08-1.12)12 | North America |
| Corpus uteri | C54-C55 | 1.50 (1.42-1.59)12 | Worldb |
| Ovary | C56 | 1.08 (1.05-1.10)12 | Worldb |
| Kidney and renal pelvis | C64-C65 | 1.29 (1.20-1.39)12 | North America |
| Thyroid | C73 | 1.09 (1.04-1.14)14 | United States |
| Multiple myeloma | C90.0, C90.2c | 1.09 (1.03-1.16)15 | North America, Europe |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ICD-10, International Classification of Diseases, Tenth Revision.
The International Classification of Diseases for Oncology, third edition (ICD-O-3) histologic codes for esophageal adenocarcinoma includes histologic codes 8140 to 8147, 8160 to 8162, 8180 to 8221, 8250 to 8507, 8514, 8520 to 8551, 8560, 8570 to 8574, 8576, and 8940 to 8941. We did not include meningioma because the number of invasive meningioma was too sparse (data not shown).
Most studies were conducted in North America and/or Europe.
The ICD-O-3 morphology codes for multiple myeloma are 9731 through 9732 and 9734.
The numbers of new invasive cancer cases for 13 cancer types diagnosed from 2011 to 2015 in the United States, including information on sex, age group (30-49, 50-59, 60-69, 70-79, and ≥80 years), and state, were obtained from the United States Cancer Statistics (USCS) Public Use database as reported by the Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries (NCPR) and the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results (SEER) Program, which collectively approached complete coverage of the US population.16 We used the SEER*Stat software (version 8.3.4) to extract the cancer cases from the USCS database. The increased risk of breast cancer associated with EBW has been reported for postmenopausal women only (Table 1). In our analysis, owing to the lack of information on menopausal status in the USCS database, women younger than 50 years were considered premenopausal and were not included in the calculation of breast cancers attributable to EBW. To estimate the number of esophageal adenocarcinomas and gastric cardia cancers at the state level, we applied the corresponding proportions from national data to minimize any effects of variations in misclassification or lack of detailed histological/anatomical information across states. Because gallbladder cancer by state is rare, we grouped this cancer with liver cancer and used a weighted cancer-specific RR (1.55 per 5-unit increase in BMI; 95% CI, 1.39-1.79), with the proportions of liver (0.87) and gallbladder (0.13) cancer cases used as the weight.
Data on BMI were obtained from the 2001 to 2004 Behavioral Risk Factor Surveillance System (BRFSS), a nationwide telephone survey of adults 18 years or older designed to provide reliable state-level estimates of health-related behavioral risk factors, including BMI.17 The 2001 to 2004 time frame was used to allow for an approximately 10-year lag period between BMI prevalence and cancer occurrence at the population level, although the lag period is unknown for some cancer types.18,19 The BMI data from 2001 to 2004 were obtained for age groups 20 to 39, 40 to 49, 50 to 59, 60 to 69, and 70 or more years, corresponding to age groups 30 to 49, 50 to 59, 60 to 69, 70 to 79, and 80 or more years at the time of cancer diagnosis in 2011 to 2015. However, BMI in the BRFSS is based on self-reported height and weight, and the information may be misreported.20 Therefore, we adjusted the BMI values obtained from the BRFSS by sex, age group, race/ethnicity, and education level20,21,22 using 2001 to 2004 data from the National Health and Nutrition Examination Survey (NHANES), a nationally representative survey with objective measurements of height and weight.23 Adjusted EBW prevalence by sex, BMI category, and state is shown in the eFigure in the Supplement.
In an additional analysis, we used contemporary exposure data from 2011 to 2014—after making adjustments using 2011 to 2014 NHANES data—to compare our results with recently published PAF estimates for EBW and cancer at the national level, which used NHANES data on BMI from the same period.6 Furthermore, PAFs based on contemporary data might provide insights on the magnitude of PAFs in the near future. We used SAS-callable SUDAAN software (release 11.0.1) to provide mean BMIs and prevalence estimates, accounting for the complex survey design.
Statistical Analysis
We categorized high BMI into 4 standard groups: 25.0 to 29.9 (overweight), 30.0 to 34.9 (class 1 obesity), 35.0 to 39.9 (class 2 obesity), and 40.0 or greater (class 3 obesity). To allow for uncertainty in the data, we applied a simulation method and generated numbers from repeated draws for all RRs, exposure levels, and the number of cancer cases, with 1000 times replication for each sex, age group, and state stratum.24 To calculate overall PAFs, we applied the weighted-sum method and used adjusted RRs to avoid bias owing to confounding.25,26 The sex-, age group-, and state-specific PAFs were calculated using the prevalence of 4 categories of high BMI (P1 to 4) in each sex, age group, and state stratum and the corresponding RR (RR1 to 4) for all 1000 replications using the following approximate formula:
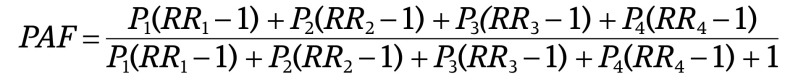 |
The sex-, age group–, and state-specific PAFs were then multiplied by the number of cancer cases in each stratum; the results were summed over age groups to calculate the number of cancer cases attributable to EBW by sex and state. Overall sex- and state-specific PAFs were calculated by dividing this number by the total number of cases of the corresponding cancer in each sex and state. Because the numbers of cancer cases attributable to EBW overall and by sex and individual cancer type were from separate simulation models and rounded to the nearest 10, the number of cancer cases by sex or for individual cancer types may not sum to the totals. We calculated the number and proportion of cancer cases attributable to EBW in the United States by summing the number of cancer cases attributable to EBW in all 50 states and the District of Columbia and dividing this number by the total number of corresponding cancer cases at the national level. The reported proportions and number of cancer cases attributable to EBW are the medians of the corresponding values from 1000 replications, and limits of 95% CIs are 25th and 975th ordered values. We used Stata statistical software (StataCorp, version 13) for the simulation and consequent calculations. More detailed information on exposure data and statistical analysis is provided in the eMethods in the Supplement.
Results
Each year, about 37 670 cancer cases in men (4.7% of all cancer cases excluding non–melanoma skin cancers) and 74 690 cancer cases in women (9.6%) 30 years or older in the United States were attributable to EBW from 2011 to 2015. By state, the PAF in men ranged from 3.9% (95% CI, 3.6%-4.3%) in Montana to 6.0% (95% CI, 5.6%-6.4%) in Texas (Table 2). The PAF in women was about twice as high as in men, ranging from 7.1% (95% CI, 6.7%-7.6%) in Hawaii to 11.4% (95% CI, 10.7%-12.2%) in the District of Columbia. For both men and women, however, the highest PAFs were found in several states in the South and Midwest, Alaska, and the District of Columbia, and the lowest PAFs were found in the Mountain (including Nevada, Wyoming, Montana, and Colorado) and New England regions and Hawaii; PAFs for men were also high in west coast states (Figure).
Table 2. Proportion and Average Annual Number of Incident Cancer Cases Attributable to Excess Body Weight (EBW) in Adults 30 Years or Older, 2011-2015a.
| Stateb | Men | Women | Men and Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PAF, % (95% CI) | Rank | Cases | PAF, % (95% CI) | Rank | Cases | PAF, % (95% CI) | Rank | Cases | ||||
| Attribc | Totald | Attribc | Totald | Attribc | Totald | |||||||
| United States | 4.7 (4.7-4.8) | NA | 37 670 | 794 675 | 9.6 (9.5-9.7) | NA | 74 690 | 777 046 | 7.2 (7.1-7.2) | NA | 112 380 | 1 571 721 |
| District of Columbia | 5.0 (4.4-5.5) | 7 | 70 | 1354 | 11.4 (10.7-12.2) | 1 | 170 | 1449 | 8.3 (7.9-8.8) | 1 | 230 | 2802 |
| Texas | 6.0 (5.6-6.4) | 1 | 3090 | 51 741 | 10.4 (9.9-10.8) | 4 | 5160 | 49 822 | 8.1 (7.8-8.4) | 2 | 8250 | 101 563 |
| Alaska | 5.6 (5.1-6.1) | 2 | 70 | 1330 | 10.4 (9.7-11.1) | 6 | 130 | 1284 | 7.9 (7.5-8.4) | 3 | 210 | 2614 |
| Indiana | 5.0 (4.7-5.4) | 6 | 820 | 16 262 | 10.3 (9.8-10.8) | 8 | 1690 | 16 466 | 7.7 (7.4-8.0) | 4 | 2510 | 32 728 |
| Michigan | 4.7 (4.4-5.0) | 17 | 1260 | 26 982 | 10.7 (10.2-11.1) | 2 | 2780 | 26 048 | 7.6 (7.3-7.9) | 5 | 4040 | 53 030 |
| West Virginia | 4.8 (4.4-5.1) | 16 | 280 | 5863 | 10.5 (10.0-11.0) | 3 | 580 | 5523 | 7.6 (7.3-7.9) | 6 | 860 | 11 387 |
| Pennsylvania | 4.8 (4.5-5.1) | 12 | 1860 | 38 602 | 10.1 (9.6-10.6) | 9 | 3900 | 38 634 | 7.5 (7.2-7.8) | 7 | 5760 | 77 235 |
| Illinois | 4.8 (4.5-5.1) | 13 | 1560 | 32 514 | 10.1 (9.6-10.6) | 10 | 3340 | 32 972 | 7.5 (7.2-7.8) | 8 | 4900 | 65 486 |
| Mississippi | 4.9 (4.5-5.3) | 11 | 410 | 8266 | 10.4 (9.9-11.0) | 5 | 740 | 7110 | 7.5 (7.1-7.8) | 9 | 1150 | 15 376 |
| Ohio | 4.6 (4.3-4.9) | 20 | 1440 | 31 398 | 10.3 (9.8-10.7) | 7 | 3200 | 31 235 | 7.4 (7.1-7.7) | 10 | 4650 | 62 633 |
| Louisiana | 5.1 (4.7-5.5) | 5 | 660 | 12 926 | 10.1 (9.6-10.6) | 11 | 1120 | 11 115 | 7.4 (7.1-7.8) | 11 | 1790 | 24 041 |
| New Mexico | 5.2 (4.8-5.6) | 3 | 230 | 4339 | 9.5 (9.0-10.0) | 29 | 420 | 4437 | 7.4 (7.1-7.7) | 12 | 650 | 8776 |
| California | 4.9 (4.6-5.3) | 8 | 3890 | 79 246 | 9.6 (9.2-10.1) | 20 | 7720 | 80 154 | 7.3 (7.0-7.6) | 13 | 11 620 | 159 400 |
| Missouri | 4.9 (4.5-5.2) | 9 | 790 | 16 089 | 9.6 (9.1-10.0) | 23 | 1530 | 15 913 | 7.2 (6.9-7.5) | 14 | 2310 | 32 002 |
| Wisconsin | 4.6 (4.3-4.9) | 22 | 730 | 15 904 | 9.8 (9.4-10.3) | 15 | 1490 | 15 199 | 7.2 (6.9-7.4) | 15 | 2230 | 31 103 |
| Maryland | 4.5 (4.1-4.8) | 34 | 650 | 14 457 | 9.8 (9.3-10.3) | 16 | 1460 | 14 856 | 7.2 (6.9-7.5) | 16 | 2100 | 29 312 |
| Oregon | 4.9 (4.6-5.3) | 10 | 500 | 10 070 | 9.6 (9.1-10.1) | 25 | 960 | 10 031 | 7.2 (6.9-7.6) | 17 | 1460 | 20 101 |
| Iowa | 4.5 (4.2-4.9) | 35 | 400 | 8859 | 10.0 (9.4-10.5) | 12 | 830 | 8346 | 7.2 (6.9-7.5) | 18 | 1230 | 17 205 |
| New York | 4.5 (4.2-4.8) | 31 | 2430 | 53 537 | 9.6 (9.1-10.1) | 21 | 5220 | 54 327 | 7.1 (6.8-7.4) | 19 | 7650 | 107 864 |
| North Carolina | 4.5 (4.2-4.8) | 32 | 1180 | 26 162 | 9.8 (9.4-10.3) | 14 | 2470 | 25 077 | 7.1 (6.8-7.4) | 20 | 3650 | 51 240 |
| Virginia | 4.6 (4.3-4.9) | 21 | 850 | 18 436 | 9.5 (8.9-10.0) | 28 | 1800 | 18 979 | 7.1 (6.8-7.4) | 21 | 2650 | 37 415 |
| Washington | 4.8 (4.4-5.1) | 14 | 830 | 17 266 | 9.4 (8.8-9.8) | 31 | 1600 | 17 105 | 7.1 (6.8-7.4) | 22 | 2430 | 34 370 |
| Delaware | 4.6 (4.2-4.9) | 30 | 130 | 2890 | 9.9 (9.3-10.5) | 13 | 270 | 2689 | 7.1 (6.8-7.5) | 23 | 400 | 5579 |
| Georgia | 4.5 (4.2-4.8) | 33 | 1070 | 23 787 | 9.7 (9.2-10.2) | 18 | 2180 | 22 460 | 7.0 (6.7-7.3) | 24 | 3240 | 46 247 |
| Tennessee | 4.7 (4.4-5.0) | 18 | 830 | 17 800 | 9.6 (9.1-10.1) | 22 | 1590 | 16 526 | 7.0 (6.8-7.3) | 25 | 2420 | 34 325 |
| Arizona | 5.1 (4.7-5.4) | 4 | 740 | 14 617 | 9.0 (8.5-9.5) | 40 | 1300 | 14 441 | 7.0 (6.7-7.3) | 26 | 2040 | 29 058 |
| Minnesota | 4.4 (4.1-4.7) | 40 | 630 | 14 216 | 9.6 (9.1-10.1) | 24 | 1310 | 13 699 | 7.0 (6.7-7.2) | 27 | 1940 | 27 914 |
| South Carolina | 4.6 (4.3-4.9) | 25 | 610 | 13 342 | 9.7 (9.2-10.2) | 19 | 1180 | 12 208 | 7.0 (6.7-7.3) | 28 | 1790 | 25 550 |
| Alabama | 4.6 (4.3-4.9) | 24 | 610 | 13 356 | 9.8 (9.3-10.3) | 17 | 1160 | 11 819 | 7.0 (6.7-7.3) | 29 | 1770 | 25 175 |
| Oklahoma | 4.8 (4.5-5.2) | 15 | 470 | 9768 | 9.2 (8.8-9.7) | 34 | 850 | 9233 | 7.0 (6.7-7.3) | 30 | 1330 | 19 002 |
| Nebraska | 4.5 (4.2-4.8) | 38 | 220 | 4789 | 9.6 (9.0-10.1) | 27 | 430 | 4501 | 7.0 (6.7-7.3) | 31 | 650 | 9289 |
| New Jersey | 4.3 (4.0-4.6) | 42 | 1060 | 24 317 | 9.4 (8.9-9.8) | 30 | 2340 | 24 949 | 6.9 (6.6-7.2) | 32 | 3390 | 49 266 |
| Kentucky | 4.6 (4.3-5.0) | 23 | 620 | 13 348 | 9.1 (8.7-9.5) | 36 | 1150 | 12 624 | 6.8 (6.5-7.1) | 33 | 1760 | 25 972 |
| Kansas | 4.5 (4.1-4.8) | 37 | 330 | 7494 | 9.3 (8.8-9.8) | 32 | 660 | 7104 | 6.8 (6.6-7.1) | 34 | 1000 | 14 598 |
| Utah | 4.2 (3.9-4.6) | 45 | 210 | 4958 | 9.6 (9.1-10.1) | 26 | 440 | 4567 | 6.8 (6.5-7.1) | 35 | 650 | 9525 |
| Idaho | 4.6 (4.2-4.9) | 28 | 180 | 3900 | 9.3 (8.8-9.8) | 33 | 340 | 3631 | 6.8 (6.5-7.1) | 36 | 520 | 7531 |
| Massachusetts | 4.7 (4.4-5.0) | 19 | 810 | 17 196 | 8.6 (8.1-9.0) | 45 | 1600 | 18 721 | 6.7 (6.4-7.0) | 37 | 2410 | 35 916 |
| Maine | 4.2 (3.9-4.6) | 46 | 180 | 4203 | 9.1 (8.5-9.6) | 38 | 380 | 4210 | 6.7 (6.4-6.9) | 38 | 560 | 8413 |
| Arkansas | 4.5 (4.1-4.8) | 36 | 380 | 8471 | 9.1 (8.6-9.6) | 37 | 670 | 7303 | 6.6 (6.3-6.9) | 39 | 1040 | 15 774 |
| South Dakota | 4.3 (4.0-4.7) | 44 | 100 | 2264 | 9.1 (8.6-9.6) | 39 | 190 | 2115 | 6.6 (6.3-7.0) | 40 | 290 | 4380 |
| North Dakota | 4.2 (3.9-4.6) | 48 | 80 | 1911 | 9.2 (8.7-9.8) | 35 | 160 | 1701 | 6.6 (6.3-6.9) | 41 | 240 | 3612 |
| Florida | 4.4 (4.1-4.7) | 39 | 2550 | 57 413 | 8.8 (8.3-9.3) | 42 | 4700 | 53 431 | 6.5 (6.3-6.8) | 42 | 7240 | 110 844 |
| New Hampshire | 4.2 (3.9-4.6) | 47 | 170 | 3941 | 8.8 (8.3-9.3) | 43 | 340 | 3913 | 6.5 (6.2-6.8) | 43 | 510 | 7854 |
| Rhode Island | 4.4 (4.0-4.7) | 41 | 130 | 2871 | 8.4 (8.0-8.9) | 47 | 260 | 3119 | 6.5 (6.2-6.8) | 44 | 390 | 5990 |
| Vermont | 4.0 (3.6-4.3) | 50 | 70 | 1782 | 8.9 (8.4-9.5) | 41 | 160 | 1808 | 6.5 (6.2-6.8) | 45 | 230 | 3590 |
| Connecticut | 4.6 (4.2-4.9) | 26 | 460 | 9947 | 8.2 (7.8-8.7) | 48 | 850 | 10 355 | 6.4 (6.2-6.7) | 46 | 1310 | 20 301 |
| Nevada | 4.6 (4.2-4.9) | 27 | 270 | 5954 | 8.2 (7.7-8.7) | 49 | 470 | 5747 | 6.3 (6.0-6.6) | 47 | 740 | 11 701 |
| Wyoming | 4.1 (3.7-4.5) | 49 | 60 | 1350 | 8.7 (8.2-9.3) | 44 | 100 | 1198 | 6.3 (5.9-6.6) | 48 | 160 | 2548 |
| Montana | 3.9 (3.6-4.3) | 51 | 120 | 2947 | 8.5 (8.0-9.0) | 46 | 230 | 2671 | 6.1 (5.8-6.4) | 49 | 340 | 5618 |
| Colorado | 4.3 (3.9-4.6) | 43 | 460 | 10 847 | 7.7 (7.3-8.1) | 50 | 840 | 10 804 | 6.0 (5.7-6.3) | 50 | 1300 | 21 651 |
| Hawaii | 4.6 (4.3-5.0) | 29 | 160 | 3396 | 7.1 (6.7-7.6) | 51 | 240 | 3417 | 5.9 (5.6-6.2) | 51 | 400 | 6813 |
| Range (across states) | 3.9-6.0 | NA | 60-3890 | 1330-79 246 | 7.1-11.4 | NA | 100-7720 | 1198-80 154 | 5.9-8.3 | NA | 160-11 620 | 2548-159 400 |
Abbreviations: Attrib, attributable number of cases; NA, not applicable; PAF, population attributable fraction.
Estimates are based on prevalence of excess body weight in 2001 through 2004.
States are ordered by PAFs for both sexes combined (rank = 1 for highest PAF, rank = 51 for lowest PAF).
Numbers of cancer cases attributable to EBW are rounded to the nearest 10.
Total cases represent average annual number of all cancer cases except nonmelanoma skin cancers. The number and proportion of cancers attributable to EBW in the United States were calculated, respectively, by summing up the cancer cases attributable to EBW in all 50 states and the District of Colombia and dividing that number by total number of cancer cases in each sex.
Figure. Rank and Proportion of Incident Cancer Cases in the 50 US States and District of Columbia Attributable to Excess Body Weight in Adults 30 Years or Older, 2011-2015.
The figures show estimates based on the prevalence of excess body weight from 2001 to 2004. States are categorized using the Jenks natural breaks classification method.
Substantial proportions of some individual cancer types were attributable to EBW. Overall, at least 25% of all cases of esophageal, liver and gallbladder, kidney and renal pelvis (except for Hawaii, 23.7%, [n = 270]), and corpus uteri cancers in all states, even those with the lowest corresponding PAFs, were attributable to EBW (eTable 1 in the Supplement). The PAF for corpus uteri cancer ranged from 36.5% to 54.9% across states and was 50.0% or more in 19 states (eTable 1). States with greater PAFs for all cancers combined generally had greater PAFs for most cancer types.
The patterns of variation in PAFs across states did not substantially change when we used BMI prevalence from 2011 to 2014 instead of from 2001 to 2004, although the PAFs slightly increased (eTable 2 in the Supplement). Specifically, the PAFs ranged from 4.2% in Montana to 6.4% in Texas among men and from 7.8% in Hawaii to 11.8% in Texas and the District of Columbia among women. Similarly, the annual number of cancer cases attributable to EBW in the country increased to 40 110 (5.0%) among men and to 83 320 (10.7%) among women.
Discussion
The proportion of cancer cases overall that could be attributable to EBW ranged from a high of 8.3% in the District of Columbia to a low of 5.9% in Hawaii, with some southern and midwestern states, Alaska, and the District of Columbia showing the highest PAFs, reflecting variation in the obesity prevalence.22 Variations in PAFs for individual cancer types across states generally followed those for all cancer combined. The overall PAF for EBW was higher in women than in men nationally and in all states, largely reflecting the associations of EBW with increased risk for several female-specific cancers (corpus uteri, female breast, and ovary) and the relatively higher prevalence of obesity in women than men nationally (41.1% vs 37.9%), particularly class 3 obesity (9.7% vs 5.6%),27 and across states in this analysis.
Adherence to comprehensive guidelines on weight, nutrition, and physical activity, including those of the American Cancer Society,28 has been associated with a reduced risk of total cancer incidence and mortality in prospective observational studies.29,30,31 However, many Americans do not meet the recommendations.6 Because individual behavioral choices often occur within the context of the community, reducing the obesity epidemic will require primary prevention interventions at individual and community levels to promote healthy diet and physical activity.12,32,33,34 At the individual level, the US Preventive Services Task Force recommends EBW screening for adults by primary care physicians and offering or referring individuals to intensive behavioral interventions if they are obese (BMI, ≥30); if they are overweight (BMI, 25.0-29.9) with hypertension, dyslipidemia, abnormal blood glucose, or diabetes; or if they are normal weight (BMI, 18.5-24.9) with abnormal blood glucose or diabetes.35 Because obesity in many children extends into adulthood,36 the US Preventive Services Task Force also recommends screening for obesity in children 6 years and older and behavioral interventions for those who are obese.37 However, counseling for obesity is generally underutilized, reflecting limited access to care, primary care physicians’ time constraints, and insufficient training for delivering effective behavioral counseling.38,39,40 For example, less than 50% of children aged 6 to 17 years in the United States receive this counseling, with a lower prevalence in low-income groups.40 Although there is no systematic information on obesity counseling across states, a study has shown variations in prevalence among children across census regions, with approximately 40% lower prevalence in the South, Midwest, and West than in the Northeast.40
To adequately address the obesity epidemic at the community level, policymakers in each state should promote a combination of various successful interventions targeting different settings, including communities, schools, workplaces, public service venues, health care facilities, and media.34,41,42 Some examples include increasing accessible and safe infrastructure for physical activity and facilitating the establishment of grocery stores for fresh fruit and vegetables in underserved areas through zoning and licensing regulations and incentive programs32,33,34 because EBW is more common in lower socioeconomic groups in the United States.43,44 Taxes on sugary beverages have shown promising results in reducing EBW,32,45,46,47 but only a small number of local or state governments have enacted such taxation.48,49,50 From 2009 to 2015, states with the highest number of enacted public health laws to promote healthy diet or physical activity in communities, schools, or workplaces were some of those with relatively high EBW–related cancer burden, including Texas, Illinois, Louisiana, Maryland, and California.48 However, many other states passed very few such laws, and many enacted laws across states focused on only a few policy areas, such as school-based policies.48,49,50 Insufficient support from legislators, complex legislative and/or judicial processes, and opposition from the food industry are a hinderance to more comprehensive strategies in many states.48,51,52 More research is also needed to identify tailored, more efficient, and mutually reinforcing interventions, particularly for underserved populations.
In this analysis, the numbers and proportions of cancer attributable to EBW at the national level (calculated by combining cancer cases attributable to EBW in all 50 states and the District of Colombia) based on contemporary BMI data (BRFSS 2011-2014 data) are comparable to our recently published estimates using NHANES BMI data from the same time period (PAF of 4.8% for men, 10.9% for women, and 7.8% for both sexes combined).6 A slightly higher PAF for men is largely owing to the use of an updated RR for liver and gallbladder cancer in this study, which was slightly higher than the RR in previous study (1.55 vs 1.30 per 5-unit increase in BMI). However, the PAFs estimates based on BRFSS data from 2011 to 2014 were slightly higher than the estimates based on BRFSS data from 2001 to 2004 data owing to an increase in EBW prevalence between these 2 time periods. The PAFs for EBW-related cancers based on more recent BRFSS data (2011-2014) likely reflect the attributable fraction of cases a decade from now, assuming a 10-year lag period between EBW prevalence and cancer occurrence.
It is noteworthy that states with relatively low overall cancer incidence rates will have a high PAF for cancer associated with EBW if they have a high EBW prevalence. For example, although the overall age–standardized cancer rate in women was higher in Connecticut than in Alaska (526.7 vs 447.7 per 100 000 people in 2010-2014),3 Connecticut had a lower PAF for cancer associated with EBW than Alaska (8.2% vs 10.4%), reflecting its lower EBW prevalence (adjusted prevalence of 57.7% vs 64.3%, respectively, in 2001-2004).
Strengths of this study include the use of representative exposure and cancer occurrence data and RRs of specific types of cancer for each level of EBW to calculate PAF estimates by state, along with their CIs. In addition, self-reported BMIs were adjusted using objectively measured BMIs to provide more accurate PAF estimates.
Limitations
This study has several limitations. First, although we combined several years of exposure and cancer occurrence data, PAFs for some cancer types in less populated states were based on a relatively small number of cases. Nevertheless, variations in PAFs for those cancer types across states were generally consistent with variation in PAFs for all cancers combined. Second, the BRFSS data included cell phones in the sampling frame beginning with the 2011 survey owing to an increase in the proportion of US households relying exclusively on cell phones.17 However, this change is unlikely to have had a substantial effect on our results because we adjusted BRFSS prevalence data using NHANES data from the same period. Third, although BMI is shown to be a good proxy for assessing EBW1 and is commonly used in large-scale epidemiological studies, when measuring body fat is challenging, it is an indirect measure of EBW because it includes both body fat and lean body mass.12 Fourth, RRs for many cancer types in this study were based on meta-analyses of studies with various designs and different adjustment strategies. We also used similar RRs for both sexes and various age groups. Although when reported, there is no substantial difference between men and women in RRs for EBW and cancer,12 RRs by age group are generally unknown and might be heterogeneous. Furthermore, EBW in adolescence or childhood may be more important than EBW in adulthood in increasing the risk of cancer, such as colorectal cancer,53 which is likely unaccounted for by RRs from studies of mostly older adults and by BMI data for adults that was used for calculating PAFs. Fifth, as shown by our supplementary analysis, the choice of the lag period between BMI prevalence and cancer occurrence can affect PAFs when prevalence changes over time. The actual lag periods are unknown for some cancer types, underscoring the need for further research. Finally, we could not control for possible changes in the population owing to interstate migration during the lag period.
Conclusions
We found that with an approximately 1.5-fold difference in the PAF between states with the highest and lowest PAFs, 1 in 17 to 1 in 12 of all incident cancers in US states were attributable to EBW. However, this proportion was substantially higher for some cancer types. Increases in obesity prevalence over the past 40 years strongly suggest that the burden of EBW will further increase in the decades to come. Health care clinicians and policymakers at the state and federal levels must support efforts to substantially reduce the prevalence of EBW and the associated health burden, as well as disparities through comprehensive and broad implementation of known interventions at individual and community levels. Further research to identify tailored and more efficient strategies for reducing the prevalence of EBW is also needed.
eMethods.
eReferences.
eTable 1. Estimated number and proportion of incident cancer cases attributable to excess body weight in adults aged ≥30 years during entire 2011-2015, by sex, state, and cancer site
eTable 2. Proportion and average annual number of incident cancer cases attributable to excess body weight in adults aged ≥30 years, 2011-2015, based on prevalence of excess body weight in 2011-2014
eFigure. Excess body mass prevalence in adults aged ≥20 years by sex and BMI category, 2001-2004
References
- 1.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K; International Agency for Research on Cancer Handbook Working Group . Body fatness and cancer--viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794-798. doi: 10.1056/NEJMsr1606602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steele CB, Thomas CC, Henley SJ, et al. Vital signs: trends in incidence of cancers associated with overweight and obesity—United States, 2005-2014. MMWR Morb Mortal Wkly Rep. 2017;66(39):1052-1058. doi: 10.15585/mmwr.mm6639e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30. doi: 10.3322/caac.21442 [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators . The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444-1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fryar CD, Carroll MD, Ogden CL Prevalence of overweight, obesity, and extreme obesity among adults aged 20 and over: United States, 1960–1962 through 2011–2014. National Center for Health Statistics Data, Health E-Stats. July 2016. https://www.cdc.gov/nchs/data/hestat/obesity_adult_13_14/obesity_adult_13_14.pdf. Accessed November 19, 2018.
- 6.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31-54. doi: 10.3322/caac.21440 [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Panagiotou OA, Graubard BI. Estimating population attributable fractions to quantify the health burden of obesity. Ann Epidemiol. 2015;25(3):201-207. doi: 10.1016/j.annepidem.2014.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song M, Giovannucci E. Preventable incidence and mortality of carcinoma associated with lifestyle factors among white adults in the United States. JAMA Oncol. 2016;2(9):1154-1161. doi: 10.1001/jamaoncol.2016.0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute for Health Metrics and Evaluation (IHME) GBD results tool. http://ghdx.healthdata.org/gbd-results-tool. Accessed 06/19/2018.
- 10.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health BRFSS prevalence & trends data. 2015. https://www.cdc.gov/brfss/brfssprevalence/ Accessed June 19, 2018.
- 11.World Cancer Research Fund International/American Institute for Cancer Research Continuous update project report: diet, nutrition, physical activity and colorectal cancer. http://www.aicr.org/continuous-update-project/reports/colorectal-cancer-2017-report.pdf. Accessed July 2, 2018.
- 12.World Cancer Research Fund International/American Institute for Cancer Research Diet, nutrition, physical activity and cancer: a global perspective. Continuous update project expert report 2018. https://www.wcrf.org/dietandcancer. Accessed July 2, 2018.
- 13.Genkinger JM, Spiegelman D, Anderson KE, et al. A pooled analysis of 14 cohort studies of anthropometric factors and pancreatic cancer risk. Int J Cancer. 2011;129(7):1708-1717. doi: 10.1002/ijc.25794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitahara CM, McCullough ML, Franceschi S, et al. Anthropometric factors and thyroid cancer risk by histological subtype: pooled analysis of 22 prospective studies. Thyroid. 2016;26(2):306-318. doi: 10.1089/thy.2015.0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teras LR, Kitahara CM, Birmann BM, et al. Body size and multiple myeloma mortality: a pooled analysis of 20 prospective studies. Br J Haematol. 2014;166(5):667-676. doi: 10.1111/bjh.12935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention NPCR and SEER incidence database: United States cancer statistics incidence public use databases. analytic database-1998-2015. Updated November 2017. http://www.cdc.gov/cancer/uscs/public-use. Accessed February 15, 2018.
- 17.Centers for Disease Control and Prevention (CDC) Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep. 2012;61(22):410-413. [PubMed] [Google Scholar]
- 18.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569-578. doi: 10.1016/S0140-6736(08)60269-X [DOI] [PubMed] [Google Scholar]
- 19.Brenner DR, Poirier AE, Grundy A, Khandwala F, McFadden A, Friedenreich CM. Cancer incidence attributable to excess body weight in Alberta in 2012. CMAJ Open. 2017;5(2):E330-E336. doi: 10.9778/cmajo.20160039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the national health and nutrition examination survey, 2001-2006. Prev Chronic Dis. 2009;6(4):A121. [PMC free article] [PubMed] [Google Scholar]
- 21.Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99(5):250-257. doi: 10.1177/014107680609900517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le A, Judd SE, Allison DB, et al. The geographic distribution of obesity in the US and the potential regional differences in misreporting of obesity. Obesity (Silver Spring). 2014;22(1):300-306. doi: 10.1002/oby.20451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention National center for health statistics. national health and nutrition examination survey. https://wwwn.cdc.gov/nchs/nhanes/default.aspx. Accessed May 21, 2018.
- 24.Greenland S. Interval estimation by simulation as an alternative to and extension of confidence intervals. Int J Epidemiol. 2004;33(6):1389-1397. doi: 10.1093/ije/dyh276 [DOI] [PubMed] [Google Scholar]
- 25.Benichou J. A review of adjusted estimators of attributable risk. Stat Methods Med Res. 2001;10(3):195-216. doi: 10.1177/096228020101000303 [DOI] [PubMed] [Google Scholar]
- 26.Darrow LA, Steenland NK. Confounding and bias in the attributable fraction. Epidemiology. 2011;22(1):53-58. doi: 10.1097/EDE.0b013e3181fce49b [DOI] [PubMed] [Google Scholar]
- 27.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723-1725. doi: 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kushi LH, Doyle C, McCullough M, et al. ; American Cancer Society 2010 Nutrition and Physical Activity Guidelines Advisory Committee . American cancer society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1):30-67. doi: 10.3322/caac.20140 [DOI] [PubMed] [Google Scholar]
- 29.Warren Andersen S, Blot WJ, Shu XO, et al. Adherence to cancer prevention guidelines and cancer risk in low-income and African American populations. Cancer Epidemiol Biomarkers Prev. 2016;25(5):846-853. doi: 10.1158/1055-9965.EPI-15-1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCullough ML, Patel AV, Kushi LH, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(6):1089-1097. doi: 10.1158/1055-9965.EPI-10-1173 [DOI] [PubMed] [Google Scholar]
- 31.Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, Rohan TE. Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. Am J Clin Nutr. 2015;101(3):558-569. doi: 10.3945/ajcn.114.094854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet. 2015;385(9985):2410-2421. doi: 10.1016/S0140-6736(14)61745-1 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention State initiatives supporting healthier food retail: an overview of the national landscape. Division of Nutrition, Physical Activity, and Obesity. https://www.cdc.gov/obesity/downloads/healthier_food_retail.pdf. Accessed March 26, 2018.
- 34.Khan LK, Sobush K, Keener D, et al. ; Centers for Disease Control and Prevention . Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58(RR-7):1-26. [PubMed] [Google Scholar]
- 35.Curry SJ, Krist AH, Owens DK, et al. ; US Preventive Services Task Force . Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(11):1163-1171. doi: 10.1001/jama.2018.13022 [DOI] [PubMed] [Google Scholar]
- 36.Song M, Hu FB, Wu K, et al. Trajectory of body shape in early and middle life and all cause and cause specific mortality: results from two prospective US cohort studies. BMJ. 2016;353:i2195. doi: 10.1136/bmj.i2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grossman DC, Bibbins-Domingo K, Curry SJ, et al. ; US Preventive Services Task Force . Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA. 2017;317(23):2417-2426. doi: 10.1001/jama.2017.6803 [DOI] [PubMed] [Google Scholar]
- 38.Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA. 2014;312(17):1779-1791. doi: 10.1001/jama.2014.14173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sim LA, Lebow J, Wang Z, Koball A, Murad MH. Brief primary care obesity interventions: a meta-analysis. Pediatrics. 2016;138(4):e20160149. doi: 10.1542/peds.2016-0149 [DOI] [PubMed] [Google Scholar]
- 40.Odulana A, Basco WT, Bishu KG, Egede LE. Dietary and physical activity counseling trends in U.S. children, 2002-2011. Am J Prev Med. 2017;53(1):9-16. doi: 10.1016/j.amepre.2017.01.039 [DOI] [PubMed] [Google Scholar]
- 41.Cauchi D, Glonti K, Petticrew M, Knai C. Environmental components of childhood obesity prevention interventions: an overview of systematic reviews. Obes Rev. 2016;17(11):1116-1130. doi: 10.1111/obr.12441 [DOI] [PubMed] [Google Scholar]
- 42.Peeters A, Backholer K. How to influence the obesity landscape using health policies. Int J Obes (Lond). 2017;41(6):835-839. doi: 10.1038/ijo.2017.24 [DOI] [PubMed] [Google Scholar]
- 43.Ogden CL, Fakhouri TH, Carroll MD, et al. Prevalence of obesity among adults, by household income and education - United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2017;66(50):1369-1373. doi: 10.15585/mmwr.mm6650a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household - United States 2011-2014. MMWR Morb Mortal Wkly Rep. 2018;67(6):186-189. doi: 10.15585/mmwr.mm6706a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Colchero MA, Popkin BM, Rivera JA, Ng SW. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016;352:h6704. doi: 10.1136/bmj.h6704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Silver LD, Ng SW, Ryan-Ibarra S, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: A before-and-after study. PLoS Med. 2017;14(4):e1002283. doi: 10.1371/journal.pmed.1002283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gulland A. WHO calls for tax on sugary drinks to tackle child obesity. BMJ. 2016;352:i475. doi: 10.1136/bmj.i475 [DOI] [PubMed] [Google Scholar]
- 48.Pomeranz JL, Siddiqi A, Bolanos GJ, Shor JA, Hamad R. Consolidated state political party control and the enactment of obesity-related policies in the United States. Prev Med. 2017;105:397-403. doi: 10.1016/j.ypmed.2017.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pomeranz JL, Wilde P, Huang Y, Micha R, Mozaffarian D. Legal and administrative feasibility of a federal junk food and sugar-sweetened beverage tax to improve diet. Am J Public Health. 2018;108(2):203-209. doi: 10.2105/AJPH.2017.304159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention Chronic disease state policy tracking system. https://chronicdata.cdc.gov/Nutrition-Physical-Activity-and-Obesity/CDC-Nutrition-Physical-Activity-and-Obesity-Legisl/nxst-x9p4. Accessed March 14, 2018.
- 51.American Cancer Society Cancer Action Network How do you measure up? A progress report on state legislative activity to reduce cancer incidence and mortality, 15th Edition. https://www.fightcancer.org/sites/default/files/National%20Documents/HDYMU-2017.pdf. Accessed March 14, 2018.
- 52.Merrill TG, Lopez W, Perl SB, Bassett MT. The judicial threat to public health innovation—the sword of Boreali. N Engl J Med. 2018;378(6):499-501. doi: 10.1056/NEJMp1712636 [DOI] [PubMed] [Google Scholar]
- 53.Levi Z, Kark JD, Katz LH, et al. Adolescent body mass index and risk of colon and rectal cancer in a cohort of 1.79 million Israeli men and women: a population-based study. Cancer. 2017;123(20):4022-4030. doi: 10.1002/cncr.30819 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eReferences.
eTable 1. Estimated number and proportion of incident cancer cases attributable to excess body weight in adults aged ≥30 years during entire 2011-2015, by sex, state, and cancer site
eTable 2. Proportion and average annual number of incident cancer cases attributable to excess body weight in adults aged ≥30 years, 2011-2015, based on prevalence of excess body weight in 2011-2014
eFigure. Excess body mass prevalence in adults aged ≥20 years by sex and BMI category, 2001-2004