Abstract
Objective:
To determine the association between fracture collapse with altered gait after intertrochanteric (IT) fracture using the trochanteric fixation nail (TFN) and helical blade.
Design:
Prospective cohort study.
Setting:
Academic Level I trauma center.
Patients:
Seventy-two patients with IT hip fractures (OTA/AO 31) treated between 2012 and 2016. The average age was 79.7 years (range, 51–94 years); there were 59 women and 13 men.
Intervention:
All patients were treated with cephalomedullary nailing using the TFN (DePuy-Synthes, West Chester, PA) with a helical blade.
Main Outcome Measures:
At follow-up appointments, temporospatial gait parameters were measured and recorded. Radiographs were analyzed at the time of surgery and at each follow-up visit. Amount of radiographic femoral neck shortening was measured radiographically. Patients completed the Harris Hip Score, visual analog scale for pain, Short Form-36 Physical Component Score, and Short Form-36 Mental Component Score.
Results:
The mean length of follow-up between the surgery and the gait analysis was 8.6 months (±0.7 months). The mean amount of shortening was 4.7 mm (±0.6 mm). Out of the 72 patients analyzed, there were 15 patients (20.8%) who shortened more than 8 mm, 7 patients (9.7%) who shortened 10 mm or more, and 2 patients (2.8%) who shortened more than 20 mm. Mean shortening was 3.0 mm for stable OTA/AO 31-A1 fractures, whereas the unstable patterns (OTA/AO 31-A2, 31-A3) demonstrated a mean shortening of 5.9 mm (P = 0.02). There was significant correlation between increased shortening and decreased cadence (P = 0.008), increased double support time (P < 0.001), decreased step length (P = 0.001), and increased single support asymmetry (P = 0.04) during gait analysis. The threshold of 8 mm of shortening predicted decreased cadence (P = 0.008), increased double support time (P < 0.001), and decreased step length (P = 0.006). Analysis of patient-reported outcome scores, including the Harris Hip Score, visual analog scale, SF-36 Physical Component Score, and SF-36 Mental Component Score, revealed no significant association with shortening.
Conclusions:
Results from this study indicate that shortening after cephallomedullary nailing of IT hip fractures using the TFN with a helical blade is associated with altered gait, specifically decreased cadence, increased double support time, decreased step length, and increased single support time asymmetry.
Keywords: gait analysis, hip fractures, hip fracture outcomes, outcomes
INTRODUCTION
Hip fractures are an increasing public health concern as the population continues to age. The increased morbidity and mortality in the 12-month period after hip fracture is largely related to decreased mobility.1 However, very few studies have analyzed the radiographic factors associated with gait impairment after intertrochanteric (IT) hip fractures. As the medical management of hip fracture patients continues to improve the quality-adjusted life expectancy postinjury, efforts have shifted toward improving functionality and quality-of-life after surgical fixation. Improving gait and mobility after surgical fixation of IT fractures is one important target of research efforts.
Several cephalomedullary nails are designed to allow for collapse to improve bony apposition and compression, as opposed to length stable implants that have high failure rates.2 There is evidence that severe shortening, or telescoping, of the femoral neck and IT region after IT fractures results in decreased mobility,3 but the quantitative effect on gait has not been established. This shortening may affect gait by altering the abduction length–tension relationship. This can result in abductor weakness and ultimately a Trendelenburg gait.
The objective of this study was to determine the association between fracture collapse with altered gait after IT fractures treated with the trochanteric fixation nail (TFN; DePuy-Synthes, West Chester, PA) using the helical blade. We hypothesized that increased radiographic femoral neck shortening would result in decreased cadence, increased double support time, decreased step length, increased single support asymmetry, and inferior outcome scores.
PATIENTS AND METHODS
After institutional review board approval, all patients with IT fractures treated with cephalomedullary nailing were prospectively enrolled in the study between 2012 and 2016. Additional inclusion criteria consisted of age older than 50 years, low-energy fracture, and the ability to ambulate at least 10 feet during gait analysis. Patients were excluded if they sustained other osseous injuries either concomitantly with the IT fracture or at any point during the study period. Patients were asked to follow-up at 6 weeks, 3 months, 6 months, and 12 months, which is the typical follow-up at our institution for monitoring patients after hip fractures.
A total of 72 patients were prospectively enrolled in the study and successfully completed at least one gait analysis. The mean age was 79.8 years (range, 51–94 years), and there were 59 female and 13 male patients included. There were 30 OTA/AO 31-A1 fractures, 31 31-A2 fractures, and 11 31-A3 fractures.
All patients in the study were treated with cephalomedullary nails, specifically the Trochanteric Fixation Nail System (DePuy Synthes), which is designed to allow telescoping for controlled fracture collapse. All cases used a helical blade. Patients were allowed to weight bear as tolerated after the surgery.
At follow-up appointments, patients’ gait parameters were recorded while ambulating using the Intelligent Device for Energy Expenditure and Activity (IDEEA) system to provide temporospatial gait analysis, including cadence and time spent in double stance phase. The IDEEA system has been validated and used in hip fracture patients previously.4,5 Thingstad et al6 studied gait in patients 4 months after hip fracture and identified 4 domains that explained the majority of variation in gait patterns in these patients. These domains included double support time, asymmetry in single support time = 100 × (|ln left/right)|), walk ratio (step length/cadence), and variability in step velocity. Therefore, we chose the following variables to analyze from the IDEEA output: double-limb support time, asymmetry in single support time, cadence, step length, and walk ratio.
Patients also completed the Harris Hip Score (HHS), visual analog scale, Short Form-36 Physical Component Score and Short Form-36 Mental Component Score at each follow-up visit. Injury radiographs were reviewed and fractures were classified according to the OTA/AO classification.7
Radiographic Analysis
Radiographs were analyzed at the time of surgery and at each follow-up visit. The amount of telescoping along the helical blade was measured after correcting for image magnification and rotation8 (Fig. 1).
FIGURE 1.
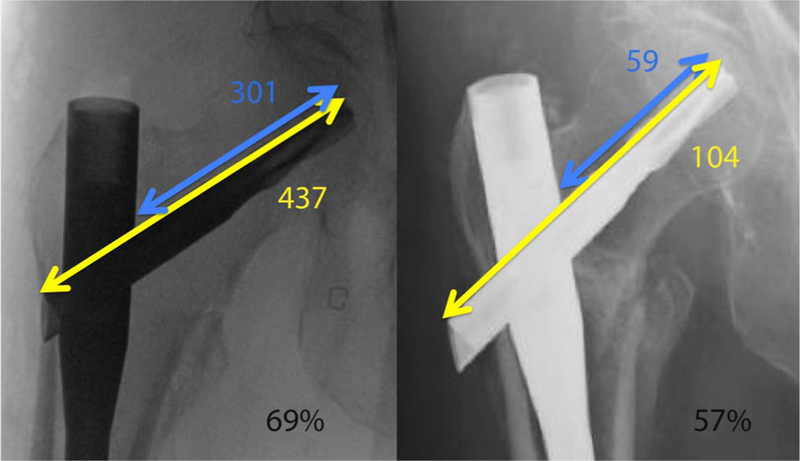
Measurement method for determining the amount of shortening along the helical blade. A, The amount of blade protruding medial to the barrel of the nail is measured and compared with the measurement of the entire blade once the nail has been placed intraoperatively. B, This is repeated for the follow-up radiograph 6 months after surgery. The change in percentage between these 2 measurements is applied to the actual length of the blade, which was recorded in the operative record. In this example, the percentage changed from 69% to 57% along a blade of length 90 mm, indicating that 10.8 mm of shortening had occurred [(0.69–0.57) × 90 = 10.8 mm]. Editor’s Note: A color image accompanies the online version of this article.
Statistical Analysis
Statistical analyses were performed using STATA software version 14.0 (StataCorp LP, College Station, TX). Descriptive statistics were calculated for patients’ demographic information. The data are reported as the mean ± 1 standard error for each outcome. All analyses that generated P-values were 2-tailed. Univariate linear regression was used to assess whether shortening is associated with the gait domains measured. Wilcoxon rank sum test was used to test if shortening >8 mm is associated with the gait domains or functional outcome scores. Finally, a linear regression model was created to assess whether the effect of shortening remains an independent predictor of poor gait pattern when controlling for age, sex, and time out from surgery.
RESULTS
All patients had radiographs taken at the time of each gait analysis. The mean length of follow-up between the surgery and the gait analysis was 8.6 months (±0.7 months) with a minimum of 6 weeks. The mean length of shortening along the helical blade at the last follow-up was 4.7 mm (±0.6 mm).
Of the 72 patients analyzed, there were 15 patients (20.8%) who shortened more than 8 mm, 7 patients (9.7%) who shortened 10 mm or more, and 2 patients (2.8%) who shortened more than 20 mm. Figure 2 demonstrates a case of 11 mm of shortening. Eighteen patients (25%) shortened less than 1 mm and the maximum amount of shortening was 21.8 mm.
FIGURE 2.

An 88-year-old woman sustained an IT fracture from a ground level fall (A and B). She was treated with a cephalomedullary nail, and the fracture was reduced to near-anatomic position (C and D). At 3-month follow-up (E and F), the patient was noted to have over 1.0 cm of shortening across the helical blade of the intramedullary nail.
Shortening was significantly associated with fracture pattern. Mean shortening was 3.0 mm for stable OTA/AO 31A1 fractures, whereas the unstable patterns (OTA/AO 31-A2, 31-A3) demonstrated a mean shortening of 5.9 mm (P = 0.02).
Comparison of Radiographic Shortening With Gait Characteristics
The gait domains measured are listed in Table 1.9, 10 Patients with increased shortening demonstrated increased double-leg stance time (P < 0.001) (Fig. 3), decreased cadence (P = 0.008), decreased step length (P = 0.001), and increased single limb asymmetry (P = 0.04) during gait analysis at the final follow-up. Shortening was not significantly associated with walk ratio (P = 0.20). A threshold of 8 mm of shortening predicted decreased cadence (P = 0.008), increased double support time (P < 0.001), and decreased step length (P = 0.006) at the final follow-up.
TABLE 1.
| Domain | Cohort Average | Standard Error | Range | Normative Average Range (Age > 70 years) |
|---|---|---|---|---|
| Cadence (steps/min) | 93.7 | 1.9 | 58.5–127.7 | 102–114 |
| Double-leg stance time (ms) | 353.2 | 12.6 | 210.5–693.2 | 290–320 |
| Step length (m) | 0.40 | 0.01 | 0.24–0.61 | 0.54–0.69 |
| Single support time asymmetry | 11.0 | 1.5 | 0–93.3 | N/A |
| Walk ratio | 0.43 | 0.01 | 0.26–0.97 | 0.64 |
NA, not available.
FIGURE 3.
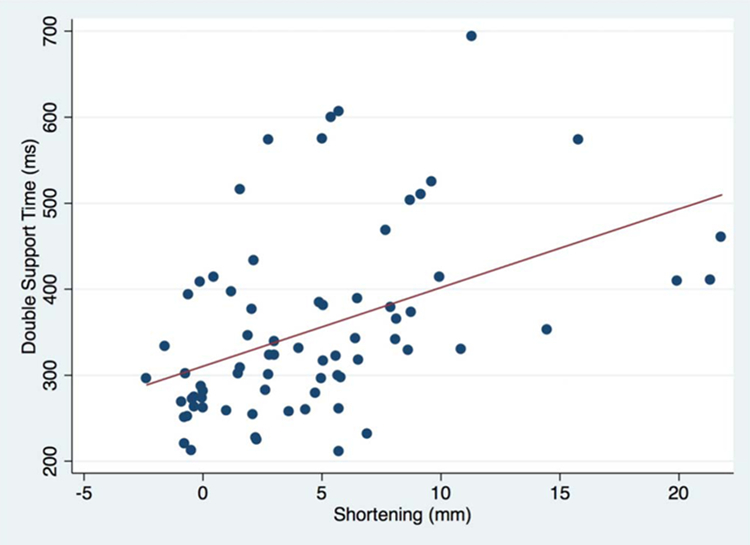
Scatter plot of mean double stance time (in milliseconds) by amount of femoral neck shortening (in millimeter) (P < 0.001). Editor’s Note: A color image accompanies the online version of this article.
Shortening remained an independent predictor of decreased cadence after controlling for age, sex, fracture pattern stability, and time from operation in a multivariable linear regression model (P = 0.031). Similarly, shortening was an independent predictor of increased double support time (P = 0.001) and decreased step length (P = 0.009) after controlling for age, sex, fracture pattern stability, and days from the operation.
Outcome Scores
Analysis of patient-reported outcome scores, including the HHS, visual analog scale, SF-36 Physical Component Score, and SF-36 Mental Component Score, revealed no significant association with shortening.
DISCUSSION
The purpose of this study was to determine whether radiographic outcomes, most importantly the amount of shortening along the axis of the femoral neck, are associated with a patient’s gait parameters and functional outcome after fixation of IT hip fractures. The results from this cohort of elderly patients indicate that femoral neck shortening is associated with increased double support time, increased single support asymmetry, decreased cadence, and increased step length.
There has been renewed interest in studying gait characteristics and rehabilitation in hip fracture patients recently.6,11 However, the literature is limited with regards to the effect of shortening on functional outcomes after IT hip fractures.12 In 2015, Thingstad et al6 examined gait parameters in 249 subjects after hip fracture to identify which gait variables most appropriately represent the gait in this patient population. The authors concluded that in addition to gait speed, assessment of double support time, walk ratio, variability of step velocity, and single support asymmetry are the key elements when attempting to represent the overall gait in hip fracture patients.13 The same group also reported that extracapsular hip fractures were associated with slower gait speed, decreased double stance time, and higher asymmetry compared with intracapsular fractures on postoperative assessment.
In femoral neck fractures fixed with open reduction internal fixation, shortening greater than 5 mm has been associated with inferior clinical outcomes.12,14 The literature pertaining specifically to extracapsular hip fractures is even more limited. In 2016, Fang et al3 found no association between shortening or collapse and mortality in IT fractures treated with sliding hip screws. However, patients with increased fracture collapse and shortening were unable to maintain their preinjury walking function.3 The incidences of both significant shortening (>10 mm; 9.7%) in this patient cohort are similar to previous reports15,16 and indicate that this radiographic outcome is not a rare event. Platzer et al17 studied IT fractures in nonelderly patients and found an association between fracture type and shortening, as we identified in this cohort. However, the authors also found that patients with shortening over 2 cm had lower HHS. We could not reproduce this finding in our cohort, but only 2 of our patients had greater than 2 cm of shortening.
This study adds to the body of literature that demonstrates worse outcomes with increased fracture collapse in the postoperative period after IT fracture fixation. There has been a recent interest in comparing devices used for IT fracture fixation and development of devices that limit postoperative collapse. In a retrospective review from 2016, Stern et al18 compared the helical blade to a lag screw option for cephalomedullary nails and reported a higher incidence of cut out with the blade compared with the screw. In 2017, Sanders et al19 completed a multicenter randomized controlled trial comparing the InterTAN intramedullary nail (Smith-Nephew, Memphis, TN), which uses a locked dual screw device, to a sliding hip screw. These authors found that the InterTAN-treated patients had less femoral shortening and improved mobility in a subset of patients that had high preinjury function. In addition, Serrano et al8 demonstrated less collapse with the dual screw device compared with the Gamma Nail (Stryker, Mahwah, NJ), which is a single screw cephalomedullary nail design. A large randomized study that compares locked dual screw fixation with standard telescoping cephalomedullary nails is needed to directly compare patient outcomes and gait patterns.
This study has several limitations. First, given the sporadic nature of trauma, we were unable to attain preinjury gait analysis parameters on IT fracture patients. Ideally, the preinjury and postfixation gait characteristics would be compared to more definitively attribute a slower cadence or a longer double support time to the shortening or collapse that occurs. Preinjury functional status is perhaps the most significant confounder in this study, in that this characteristic had the most potential to influence the amount of shortening a patient experienced and their ability to ambulate well postoperatively. Although age is not a perfect method for controlling for functional status, when age was added to a multivariable analysis, radiographic shortening remained a significant independent predictor of slower cadence and increased double support time. Future studies should include assessment of preinjury ambulatory status. Given the high degree of comorbidities in hip fracture patients, the time of follow-up was highly variable, and it was not possible to assess each patient at the regular, staged intervals postoperatively and may lead to variability in our HHS resulting from length of time to final follow-up. Studies with long-term follow-up are needed. Patients who returned for follow-up and were nonambulatory were excluded, thus introducing the potential for selection bias. Additionally, we were not able to measure pelvic tilt in this cohort of patients. Although the method used to measure shortening along the helical blade allowed for correction of rotation, it does not account for cutout of the blade within the femoral head, which could affect gait mechanics as well.
Despite these limitations, this study demonstrates that there is a high incidence of shortening after IT fracture fixation with the TFN using helical blade fixation, and that shortening along the blade is associated with worse gait parameters in the short term after hip fracture.
Acknowledgments
Supported by the Samuel and May Rudin Foundation.
Footnotes
The authors report no conflict of interest.
Presented in part at the Annual Meeting of the Orthopaedic Trauma Association, October 11–14, 2017, Vancouver, Canada, and the Annual Meeting of the American Academy of Orthopaedic Surgeons 2018, March 14–18, 2017, San Diego, CA.
Level of Evidence: Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
REFERENCES
- 1.Iosifidis M, Iliopoulos E, Panagiotou A, et al. Walking ability before and after a hip fracture in elderly predict greater long-term survivorship. J Orthop Sci 2016;21:48–52. [DOI] [PubMed] [Google Scholar]
- 2.Berkes MB, Little MT, Lazaro LE, et al. Catastrophic failure after open reduction internal fixation of femoral neck fractures with a novel locking plate implant. J Orthop Trauma 2012;26:e170–e176. [DOI] [PubMed] [Google Scholar]
- 3.Fang C, Gudushauri P, Wong TM, et al. Increased fracture collapse after intertrochanteric fractures treated by the dynamic hip screw adversely affects walking ability but not survival. Biomed Res Int 2016;2016:4175092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paul O, Barker JU, Lane JM, et al. Functional and radiographic outcomes of intertrochanteric hip fractures treated with calcar reduction, compression, and trochanteric entry nailing. J Orthop Trauma 2012;26:148–154. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Barker JU, Briggs SM, et al. An evaluation of accuracy and repeatability of a novel gait analysis device. Arch Orthop Trauma Surg 2007;127:223–227. [DOI] [PubMed] [Google Scholar]
- 6.Thingstad P, Egerton T, Ihlen EF, et al. Identification of gait domains and key gait variables following hip fracture. BMC Geriatr 2015;15:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007;21: S1–S133. [DOI] [PubMed] [Google Scholar]
- 8.Serrano R, Blair JA, Watson DT, et al. Cephalomedullary nail fixation of intertrochanteric femur fractures: are two proximal screws better than one? J Orthop Trauma 2017;31:577–582. [DOI] [PubMed] [Google Scholar]
- 9.Hollman JH, McDade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011;34:111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rota V, Perucca L, Simone A, et al. Walk ratio (step length/cadence) as a summary index of neuromotor control of gait: application to multiple sclerosis. Int J Rehabil Res 2011;34:265–269. [DOI] [PubMed] [Google Scholar]
- 11.Guven M, Kocadal O, Akman B, et al. Proximal femoral nail shows better concordance of gait analysis between operated and uninjured limbs compared to hemiarthroplasty in intertrochanteric femoral fractures. Injury 2016;47:1325–1331. [DOI] [PubMed] [Google Scholar]
- 12.Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br 2008;90:1487–1494. [DOI] [PubMed] [Google Scholar]
- 13.Thingstad P, Taraldsen K, Saltvedt I, et al. The long-term effect of comprehensive geriatric care on gait after hip fracture: the trondheim hip fracture trial–a randomised controlled trial. Osteoporos Int 2016; 27:933–942. [DOI] [PubMed] [Google Scholar]
- 14.Weil YA, Khoury A, Zuaiter I, et al. Femoral neck shortening and varus collapse after navigated fixation of intracapsular femoral neck fractures. J Orthop Trauma 2012;26:19–23. [DOI] [PubMed] [Google Scholar]
- 15.Song HK, Yoon HK, Yang KH. Presence of a nail in the medullary canal; is it enough to prevent femoral neck shortening in trochanteric fracture? Yonsei Med J 2014;55:1400–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Studer P, Suhm N, Wang Q, et al. Displaced trochanteric fragments lead to poor functional outcome in pertrochanteric fractures treated by cephalomedullary nails. Injury 2015;46:2384–2388. [DOI] [PubMed] [Google Scholar]
- 17.Platzer P, Thalhammer G, Wozasek GE, et al. Femoral shortening after surgical treatment of trochanteric fractures in nongeriatric patients. J Trauma 2008;64:982–989. [DOI] [PubMed] [Google Scholar]
- 18.Stern LC, Gorczyca JT, Kates S, et al. Radiographic review of helical blade versus lag screw fixation for cephalomedullary nailing of lowenergy peritrochanteric femur fractures: there is a difference in cutout. J Orthop Trauma 2017;31:305–310. [DOI] [PubMed] [Google Scholar]
- 19.Sanders D, Bryant D, Tieszer C, et al. A multicenter randomized control trial comparing a novel intramedullary device (InterTAN) versus conventional treatment (sliding hip screw) of geriatric hip fractures. J Orthop Trauma 2017;31:1–8. [DOI] [PubMed] [Google Scholar]


