Abstract
This article provides an overview and description of implementation activities of the multicomponent, community-wide initiatives of the Teenage Pregnancy Prevention Program initiated in 2010 by the Office of Adolescent Health and the Centers for Disease Control and Prevention. The community-wide initiatives applied the Interactive Systems Framework for dissemination and implementation through training and technical assistance on the key elements of the initiative: implementation of evidence-based teen pregnancy prevention (TPP) interventions; enhancing quality of and access to youth-friendly reproductive health services; educating stakeholders about TPP; working with youth in communities most at risk of teen pregnancy; and mobilizing the community to garner support. Of nearly 12,000 hours of training and technical assistance provided, the majority was for selecting, implementing, and evaluating an evidence-based TPP program. Real-world implementation of a community-wide approach to TPP takes time and effort. This report describes implementation within each of the components and shares lessons learned during planning and implementation phases of the initiative.
Keywords: Teen pregnancy, Teen pregnancy prevention, Community-wide initiatives, Adolescent sexual and reproductive health, Interactive systems framework, Training, Technical assistance, Implementation
Although the teen birth rate declined 64% between 1991 and 2015 from 61.8 to 22.3 per 1,000 female adolescents aged 15–19 years [1], the United States continues to have one of the highest teen pregnancy rates among developed nations [2], and racial/ethnic and geographic disparities in teen birth rates persist [3,4]. Because of the high rates and persistent disparities in teen births, teen pregnancy prevention is one of six major evidence-based policy initiatives currently funded across the federal government [5]. In 2010, the U.S. Centers for Disease Control and Prevention (CDC) declared teen pregnancy one of its seven “winnable battles” and a public health priority because of the potential for large-scale impact on health and the availability of known, effective strategies [6]. The Department of Health and Human Services (HHS) Office of Adolescent Health (OAH) is responsible for implementing and administering the Teenage Pregnancy Prevention Program, which has two funding tiers: the replication of evidence-based intervention (EBI) models (tier 1) and the testing of new or innovative approaches (tier 2) [7]. In 2010, as one of the tier 2’s approaches, CDC, in partnership with OAH, funded eight state- and community-based organizations to develop and implement a multicomponent, community-wide approach to teen pregnancy prevention (TPP) in communities with a history of high teen birth rates (>45.5 births per 1,000 females aged 15e19 years). CDC and the Office of Population Affairs also supported a Title X organization to implement the same community-wide approach in a ninth community. Funded state- and community-based organizations received between $700,000 to $1.5 million per year through a 5-year cooperative agreement to implement project activities. To meet the needs of the nine state- and community-based organizations and their local partners, the CDC also funded five national organizations to provide training and technical assistance (TTA). Table 1 lists the state- and community-based organizations and their targeted communities and the national organizations included in these initiatives.
Table 1.
State- and community-based organizations and national organizations in the community-wide teen pregnancy prevention initiatives
| State- and community-based organizations | |
|---|---|
| Organization name | Target community |
| Adolescent Pregnancy Prevention Coalition of North Carolinaa | Gaston County, North Carolina |
| Fund for Public Health in New Yorka | South Bronx, New Yorkb |
| Family Planning Councila | Philadelphia, Pennsylvania |
| City of Hartforda | Hartford, Connecticut |
| Georgia Campaign for Adolescent Power and Potentiala | Richmond County, Georgia |
| Massachusetts Alliance on Teen Pregnancya | Springfield and Holyoke Massachusetts |
| University of Texas Health Science Center at San Antonioaa | South San Antonio, Texas |
| South Carolina Campaign to Prevent Teen Pregnancya | Spartanburg County, South Carolina; Horry County, South Carolina |
| Mobile County Health Departmentc | Mobile County, Alabama |
| National training and technical assistance organizationsd | |
| Organization name | Area of expertise |
| Advocates for Youth | Community mobilization |
| CAI Global, Inc | Clinical services |
| Healthy Teen Network | Evidence-based programs |
| The National Campaign to Prevent Teen and Unplanned Pregnancy | Stakeholder education |
| JSI, Inc | Working with diverse communities |
Funded by the Office of Adolescent Health.
Community Districts 2 and 3, Hunts Point and Morrisania.
Funded by the Office of Population Affairs.
Funded by the Centers for Disease Control and Prevention.
Description of Initiatives
The purpose of the initiatives was to use a community-wide, multicomponent approach to reduce teen pregnancy and birth rates in communities with rates exceeding the national average. The current initiative model includes five primary elements (Figure 1). Although individual elements are based on research and implementation of prior TPP efforts, the overall model has not been previously carried out.
Figure 1.
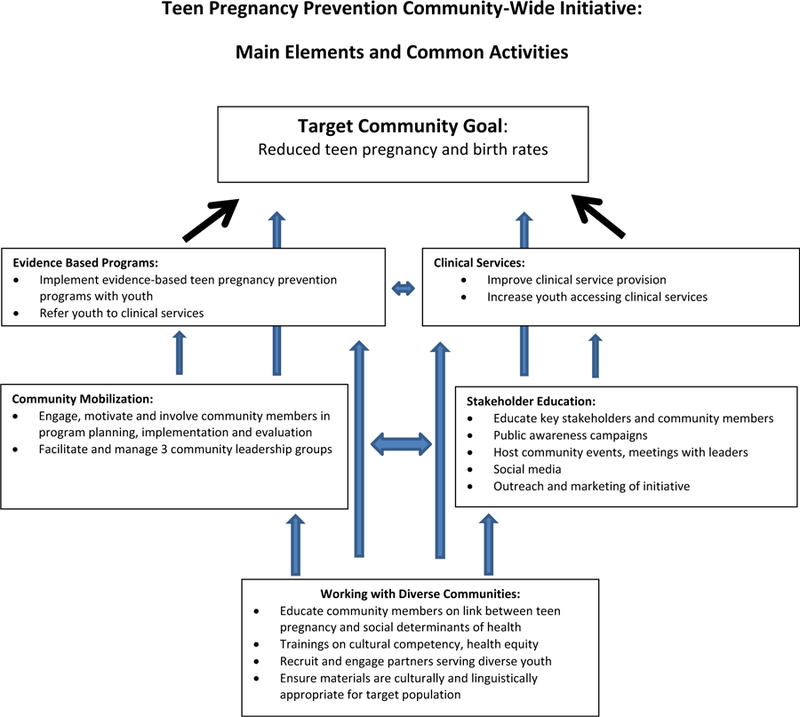
Key elements of the multicomponent, community-wide initiatives. Evidence-based interventions and clinical services are the main pillars of the initiative. The supporting elements (community mobilization, stakeholder education, and working with diverse communities) seek to enhance the likelihood that the evidence-based intervention and clinical services elements will have the desired impact on teen birth rates and ensures all strategies within each component are culturally appropriate and tailored to the needs of the community. Common activities implemented within each element are listed.
The first element is implementation of EBIs to prevent teen pregnancy. Interventions that have been rigorously evaluated and found to impact behaviors associated with pregnancy and/or reduce the likelihood of pregnancy or sexually transmitted infections among teens have been identified through a review carried out for HHS [8]. State- and community-based organizations were expected to partner with youth-serving organizations (program partners) who would implement these EBIs.
In addition, given indications of the importance of increasing contraceptive use among teens to declining teen birth rates nationally [9,10], increasing teen access to high-quality sexual and reproductive health services was identified as the second key element of the model. State- and community-based organizations were to work with local health centers to improve implementation of evidence-based guidelines for adolescent reproductive health care [11]. Implementation of these guidelines has been linked to greater use of highly effective contraception and youth satisfaction with services received [12–18]. The initiatives also were to connect youth participating in EBIs to participating health centers for sexual and reproductive health services, as needed.
Implementing teen pregnancy prevention efforts in a community can be a sensitive and even controversial issue. Wide-spread implementation of these efforts may require the approval of local community leaders (e.g., school officials) and can be derailed when community members object to how the teen pregnancy prevention efforts are carried out. In light of this, the initiatives were designed to involve and engage the communities from the start. Community mobilization efforts, which represent the third initiative element, sought to engage community members, youth, and local leaders in planning the initiatives and providing feedback on how and where initiative activities were implemented [19]. The fourth element, educating key stake-holder (e.g., school boards, youth serving organization leadership) about the need for teen pregnancy prevention, extent of community support for TPP efforts, and the types of interventions supported by research, was to be carried out by the state- and community-based organizations as well as participating community members. Mobilizing community members to become actively involved in change efforts and educating key leaders in the community about change efforts have been found to be factors in the success of community efforts [20–22].
Finally, the fifth element, which focused on working with diverse communities, sought to engage community members from different backgrounds to participate in community mobilization and stakeholder education, as well as ensure that EBI’s and sexual and reproductive health services were culturally appropriate and tailored to meet the needs of all youth in the community. Failing to engage key segments of the community or providing youth with interventions that are not culturally sensitive may reduce the likelihood that efforts have a positive impact [23,24] (Figure 1).
To ensure that capacity was built within the state- and community-based organizations and their partners to implement the five elements of the community-wide initiative and to ensure quality implementation, we applied a multitiered TTA framework modeled after the Interactive Systems Framework for Dissemination and Implementation (ISF, Figure 2). Previous application provides support for using the ISF to help local providers implement interventions [25–27]. The ISF, a multisystem, capacity-building model, was developed to help prevention practitioners and researchers bridge the gap between what is known about effective approaches from research and how activities are implemented in the field [28]. The ISF is represented by three systems: (1) prevention synthesis and translation; (2) prevention support; and (3) prevention delivery. The prevention synthesis and translation system distills the research and makes it accessible to practitioners in the field who may not have access to journals through which information about best practices is disseminated. The delivery system provides prevention services in the community, and the support system helps to build the capacity of the delivery system [28]. All three systems of the ISF are represented in the initiatives through the national training organizations, state- and community-based organizations, and local partners–the direct service providers in the community.
Figure 2.
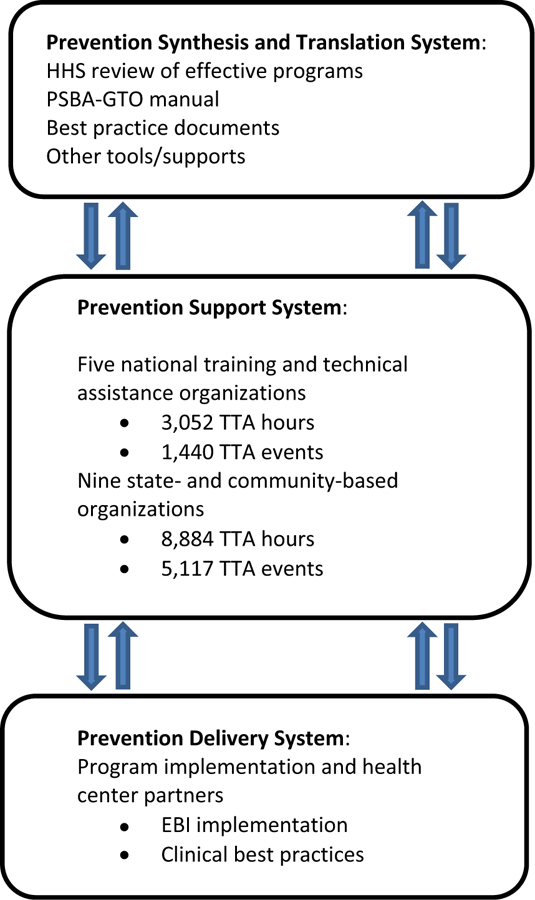
Training and technical assistance model. The Prevention Synthesis and Translation system distills the research and provides user-friendly materials for local prevention partners. The national training and technical assistance organizations (prevention support system) provide training and technical assistance to the nine state- and community-based organizations. The state- and community-based organizations (also prevention support system), in turn, provide training and technical assistance to their local partners (prevention delivery system) to support EBI implementation and clinical improvements. Training and technical assistance hours provided by the prevention support system are included in the model. EBI = evidence-based intervention; HHS = Department of Health and Human Services; PSBA-GTO = Promoting Science-Based Approaches to Teen Pregnancy Prevention-Getting to Outcomes; TTA = training and technical assistance.
Understanding how this community-wide, comprehensive model for TPP is implemented in the real world and what support organizations need for implementation is important for others interested in replicating this approach in its entirety or interested in implementing individual elements (e.g., enhancing sexual and reproductive health services). In this article, we present an overview of the initiatives and a description of activities implemented by state- and community-based organizations and their partners to increase understanding of the elements of the community-wide approach. We describe the tools and resources developed as part of the synthesis and translation system, the types and amount of TTA provided at the support system, and describe implementation as reported by the state- and community-based organizations. Other articles in this issue provide a more detailed examination of implementation data across the state- and community-based organizations specific to EBIs and clinical services or detail aspects of implementation as carried out by individual state- and community-based organizations [29–35]. An evaluation of the impact of these initiatives on intervention and comparison communities’ teen birth rates is underway.
Methods
State- and community-based organizations were required to develop community-wide plans and implement strategies within each of the five elements of the approach. The national organizations provided capacity-building support. All TTA was tracked to demonstrate the effort needed to support implementation of a community-wide approach to teen pregnancy prevention.
Program Implementation Requirements
The first year of the project (2010) was dedicated solely to planning given the importance of developing a solid foundation within the community to support implementation activities. State- and community-based organizations were required to formalize partnerships with at least 10 youth-serving organizations (or program partners) to implement EBIs which were shown to be effective and were identified by the HHS TPP evidence review [8] and with at least five health centers willing to implement practice changes to increase adolescent access to youth-friendly sexual and reproductive health services. To support community mobilization, state- and community-based organizations established and maintained three community groups: (1) the core partnership leadership team, made up of TPP leaders in the community, to develop a plan for the overall initiative; (2) the community action team, consisting of business owners, parents, and other community members; and (3) the youth leadership teams who ensured the strategies and activities were informed by, and acceptable to, youth in the community.
State- and community-based organizations assessed the needs of partners using tools developed by CDC and the national organizations. For example, the needs assessment tool for program partners measured and monitored the organizations’ capacity for program implementation, adaptation, evaluation, and continuous quality improvement. Health center assessment tools measured implementation of clinical best practices and evidence-based clinical guidelines. The baseline assessments were used to identify needs and develop individualized TTA plans for each partner. Needs assessments were conducted annually to monitor progress and update TTA plans [11,31,33]. Each state- and community-based organization conducted additional assessments of their community to supplement the baseline assessments using existing data sources and collecting information from focus groups, interviews, or surveys of adults and youth in their community.
Supporting and Implementing the Community-Wide Initiatives Using the Interactive Systems Framework
To ensure state- and community-based organizations and their partners had capacity to implement the strategies and activities of the initiatives, the national organizations (representing the synthesis and translation system of the ISF) synthesized the research and developed user-friendly tools, resources, and best practice documents. The national organizations also acted in the prevention support system and provided TTA to the state- and community-based organizations for a specific element of the initiative (Table 1). The needs of the state- and community-based organizations were assessed and reviewed annually to inform TTA plans. State- and community-based organizations (also representing the prevention support system in the ISF) then provided TTA to their program and health center partners (the prevention delivery system in the ISF) to implement EBIs and improve clinical practices.
Data Sources—Program Implementation
Training and technical assistance
During 2011–2015, the implementation years, state- and community-based organizations and the national organizations entered TTA events into a web-based system. Information about the type of event (training or technical assistance encounter), topic of TTA, and time spent providing TTA was recorded.
End-of-project interviews
An interview with each of the 9 project coordinators (e.g., individual who oversaw the initiative in each community) was conducted during the latter part of the final year of the project. Interviews were conducted by a staff member of one of the national organizations and asked about primary activities undertaken as part of each element, as well as notable successes and challenges of implementation. National organization staff summarized the interviews and provided the summaries to each project coordinator for edits.
End-of-project reports
State-and community-based organizations and national organizations submitted a final project report documenting progress on project objectives from 2010 to 2015.
Performance measures
Performance measures were developed to assess intermediate outcomes of the initiatives (http://www.cdc.gov/teenpregnancy/pdf/about/state-community-awardee-performance-measure-reporting-tool-627kb.pdf). The measures assessed included, but were not limited to number and demographics of youth receiving EBIs, number and types of EBIs implemented, the number and demographics of youth accessing services at health centers, and contraceptive coverage rates. Performance measures also collected information on short-term outcomes related to the leadership teams, including the number of meetings held for each team and the number of individuals per team. Data were submitted to CDC annually.
Results
Evidence-based program implementation
Prevention support system—national organizations.
The national organization for this element, Healthy Teen Network, facilitated train the trainer sessions on select EBIs and training skills workshops to build training capacity at state- and community-based organizations. Healthy Teen Network also provided TTA on a 10-step process for state- and community-based organizations to use with their program partners to select, implement, and evaluate EBIs using the prevention synthesis and translational tool developed by CDC, Promoting Science-Based Approaches to Teen Pregnancy Prevention-Getting to Outcomes (PSBA-GTO) [36]. TTA records indicate that the Healthy Teen Network provided 587 TTA events in over 1,103.75 hours of TTA from 2011 to 2015. Almost 86% of the TTA events were on the PSBA-GTO process (294 events) and select EBI trainings (211 events). The Healthy Teen Network provided 121 hours of TTA in 27 TTA events to increase general training and facilitation skills.
Prevention support system—state- and community-based organizations.
State- and community-based organizations provided 6,749 hours of TTA in 3,685 TTA events to their program partners to support implementation of EBIs and referral of youth to health centers. Program partners were led through the 10 steps of PSBA-GTO to: (1) select an EBI that best meet the needs of the youth and agency capacity (7% of TTA events); (2) develop a plan, receive training on, and implement the program (34% of TTA events); (3) evaluate the process and outcomes (22% of TTA events); and (4) use data for program improvement and sustainability (17% of TTA events). Overall, 3,048 TTA events (83% of TTA events) were dedicated to the PSBA-GTO process. State- and community-based organizations also facilitated linkages between program partners and health center partners and pro- vided training to program partners on how to make effective referrals (2% of TTA events).
Prevention delivery system.
With support from state- and community-based organizations, 139 program partners implemented EBIs. Performance measure data show program partners implemented more than 2,800 cycles of EBIs across the 10 communities, reaching 53,428 youth during 2011e2015. Comprehensive sexuality education programs were most often implemented (71%), with abstinence-based programs (14%), youth development programs (9%), and clinic focused program also implemented (6%). The programs were implemented most frequently in schools (66%) and community-based organizations (16%), but also in other settings such health centers, foster care agencies, and juvenile justice agencies. See article by House et al. in this issue for details about EBI implementation.
Clinical services component implementation
Prevention synthesis and translation system.
As part of synthesizing and translating research for use, the national grantee for this component, CAI Inc., in partnership with CDC, developed a list of evidence-based practices to guide state- and community-based organization work with their health center partners (this and other best practice lists developed for the initiatives are available at http://www.cdc.gov/teenpregnancy/practitioner-tools-resources/index.html). The best practice list provided a guide for state- and community-based organizations to support health center partners to implement practice improvements. Best practice categories included: (1) contraceptive access; (2) provision of contraception on the same day requested; (3) cervical cancer screening; (4) emergency contraception; (5) sexually transmitted diseases and HIV testing; (6) confidentiality and consent; (7) the health center environment; and (8) cost and billing practices. See the study by Romero et al. (this issue) for more details about development of clinical best practices.
Prevention support system—national organizations.
CAI provided 640 hours of TTA across 402 events. Thirty-four percent of TTA events addressed best practices in the delivery of adolescent reproductive health care; 17% related to using a continuous quality improvement approach to improving services; 22% of TTA events involved managing relationships between state- and community-based organizations and health center partners and conducting monitoring and evaluation of the clinical services component; 9% covered financial issues; 7% covered workforce development to support health centers to implement best practices; and 9% covered guidance on linking with other agencies that can serve as referral sources for teens in need of reproductive health care and developing marketing and outreach efforts.
Prevention support system—state- and community-based organization.
State- and community-based organizations provided 2,136 hours of TTA in 1,432 events to their health center partners to conduct needs assessments, set project objectives, and plan for implementation of best practices (19% of TTA events); evaluation and continuous quality improvement (31% of TTA events); and improvements in delivering health care services (26% of TTA events). TTA on delivery health care services included TTA on improving the clinical environment and accessibility for youth; training on contraceptive counseling and long-acting reversible contraception (LARC) insertions; conducting sexual health assessments; ensuring the full range of contraceptives onsite; and implementing best practices in adolescent sexual and reproductive health services.
Prevention delivery system.
The health centers carried out changes to health center policies and practices related to adolescent reproductive health. Based on end-of-project interviews, they most commonly indicated enhancing access to contraceptive services (i.e., making it easier for teens to attend by changing clinic operating hours to more teen-convenient times or providing teens with walk-in or same-day appointments). Another common approach to increasing access was screening existing teen clients whose presenting issue did not relate to contraception to determine if they were in need of contraceptive care. State- and community-based organizations reported that many of their health center partners sought to increase teen access to the full range of contraception particularly long-acting reversible contraceptives (LARCs). Specific efforts most commonly described included training providers to insert intrauterine devices and implants, facilitating referrals from health centers that do not provide LARC methods to those that do, and identifying funding sources for LARC methods because they have greater upfront costs than do other methods. Four grantees reported significant efforts to increase same-day provision of hormonal contraption and/or LARCs by addressing appointment scheduling policies and issues around keeping LARCs stocked and available.
End-of-project interviews also indicated that many health center partners sought to create an environment inside the health center that was youth-friendly or comfortable for teens. The most frequent efforts included scheduling teen-only hours, developing teen-only waiting areas decorated to appeal to young people, and hiring or assigning dedicated staff with expertise in working with adolescents to conduct intakes and provide care. Two communities developed new clinics that served only teens and provided both primary and reproductive health care. Efforts to reduce costs to teens for reproductive health services also were frequently reported including seeking out federal or state programs with which the health center had not been previously involved or identifying private donors.
Efforts to enhance adolescent confidentiality were rarely mentioned in end-of-project interviews. No efforts to address best practices in the categories of cervical cancer screening, emergency contraception, or STD and human immunodeficiency virus testing were described.
Community mobilization implementation
Prevention synthesis and delivery system.
As part of synthesizing and translating research for use, the national training organization for this element, Advocates for Youth (referred to as Advocates), in partnership with CDC, reviewed the literature and developed a list of 14 key community engagement strategies that are based on best practices in community mobilization, collaborative partnerships, and coalition building. These strategies address the importance of strong leadership and support, community and youth partnerships, and evaluating and sustaining community-wide efforts. Advocates also developed guidance documents on how to support and manage the community leadership teams and a sustainability model to guide efforts to sustain implementation after grant funding ended.
Prevention support system—national organizations.
Advocates provided 542 hours of TTA in 212 events to state- and community-based organizations: 35% of events were related to organizational capacity building; 25% on development and maintenance of the three leadership teams; and 9% on community engagement and planning. TTA on organizational capacity building focused on developing sustainability plans for the initiatives.
Prevention support system—state- and community-based organization.
State- and community-based organizations developed and maintained three leadership teams to provide input and lead various activities in the community. State- and community-based organizations hosted a mean of 6.10 core partnership leadership team meetings each year with a mean of 13.76 members; 6.56 community leadership team meetings with 17.71 members; and 17.59 youth leadership team meetings with members. Each leadership team developed an action plan. Final interviews reported that youth leadership team members conducted clinical mystery shopper visits to assess the youth-friendliness of health centers. Youth leadership team members also helped develop communication campaigns, managed social media outreach, and organized community-wide events. Many community and youth leadership teams received training on adolescent and sexual health and received media training so they could act as spokespersons for the initiative at community events (See [19] for additional information on lessons learned from the community mobilization groups).
Stakeholder education implementation
Prevention synthesis and translation system.
The National Campaign for Teen and Unplanned Pregnancy (referred to as the National Campaign), with CDC, conducted a literature review and distilled the research into key strategies for educating stakeholders (e.g., faith-based leaders, child welfare administrators, parents). These strategies provided guidance about what state- and community-based organizations could do to engage and educate specific groups in their communities.
Prevention support system—national organizations.
The National Campaign provided TTA on the development of the communication strategy in each of the communities, whether print, television, or digital. The National Campaign provided 454 hours of TTA in 182 TTA events to support stakeholder education efforts.
Prevention delivery system.
State- and community-based organization end-of-project interviews report state- and community-based organizations implemented communication strategies to promote their initiatives and raise awareness of local health centers. Three communities developed TPP public awareness campaigns focused on dual protection and parent-child communication. Community-specific communication materials, tag lines, logos, and Web sites were developed with input from the youth and the community. Outreach and marketing examples include participating in community events and health fairs, social media (i.e., Facebook, YouTube, Twitter), radio ads, billboards, ads on public transportation, videos, or postcards distributed at partnership organizations. All state- and community-based organizations used social media and regularly posted to Twitter, Facebook, and YouTube. Communication efforts were implemented community wide, with tailored messages dependent on the stakeholder group and with higher saturation goals in pockets of the community with higher teen birth rates.
State- and community-based organizations reported hosting conferences or town hall meetings to educate and raise awareness on teen pregnancy prevention. Six state- and community-based organizations hosted trainings for parents on parent-child communication or sexual and reproductive health. In addition, all state- and community-based organizations met with school superintendents, the Mayor’s office, city council, or other community leaders to educate them on teen pregnancy prevention and the goals of the initiative.
Working with diverse communities
Prevention synthesis and translation system.
In collaboration with CDC, JSI Research and Training Institute, Inc. (JSI) reviewed published literature and developed a list of 37 key strategies guided by best practices, organized by element, to work with diverse communities. These strategies helped state- and community-based organizations fully engage diverse youth and the community in the initiatives. JSI developed a series of tools, resources, case studies, and TTA materials to further facilitate the adoption of these strategies.
Prevention support system—national organizations.
JSI provided trainings on trauma-informed approaches, cultural competency and engaging males in program and clinical services. JSI also facilitated root-cause analysis workshops with that helped identify local contributing and underlying causes of teen pregnancy and identified feasible actions to address these conditions. In total, 263 hours of TTA was provided for the working with diverse communities’ element.
Prevention delivery system.
State- and community-based organizations sought out and engaged partners working with youth most at risk for teen pregnancy, including juvenile justice systems, homeless shelters, foster care systems, alternative schools, and parenting teens themselves. Through TTA, state- and community-based organizations also ensured that EBIs and reproductive health services were culturally and linguistically appropriate and met the needs of youth from diverse communities. National organizations and state- and community-based organizations worked with program partners to translate materials into other languages and adapt EBIs when needed and provide training to clinical providers on cultural competency, engaging males in reproductive health services, and serving gay, lesbian, or bisexual teens. All state- and community-based organizations targeted and recruited individuals’ representative of the community onto leadership teams.
Discussion
Overall, 1,440 TTA events (3,052 hours) were provided by the national organizations to the state- and community-based organizations and their local partners to implement the community-wide teen pregnancy prevention initiatives. The national organizations distilled the research and developed best practice documents that helped guide the strategies implemented in the community. TTA occurred at the prevention support system of the ISF, whereas implementation of EBIs and clinical improvements at the practice level and the delivery of services to youth were made at the prevention delivery system among over 100 local organizations. Over 40% of TTA events provided to state- and community-based organizations covered EBIs; 28% clinical services; 15% community mobilization; 12% stakeholder education; and 3% working with diverse communities. Over 5,100 TTA events (8,850 hours) were provided by state- and community-based organizations to program and health center partners. Over 72% of the TTA events to local program and health center partners covered EBIs; 28% of TTA events covered clinical services.
In the community-wide initiatives, the most TTA support was provided to local organizations implementing EBIs. To support EBI implementation, state- and community-based organizations were provided general skills in training facilitation and the ability to train educators on specific EBIs. At the prevention delivery level, almost three fourths of TTA events covered EBIs and just over a quarter covered clinical services. This finding may be due to the original funding announcement’s emphasis on EBI implementation using the 10 steps of the PSBA-GTO model for all local organizations. Although using PSBA-GTO may have resulted in increased TTA provision compared with the other elements, recent research suggests that implementation support such as was provided by PSBA-GTO leads to increased performance and fidelity [37]. EBI implementation also required staff at local organizations to be trained in specific EBIs that were frequently multiday trainings. Even after an EBI selection and training, ongoing support was needed for fidelity monitoring, evaluation, and quality improvement.
The most frequently reported TTA topic for health centers was quality improvement (31% of TTA events). Consistent with CDC and Office of Population Affairs guidelines for conducting quality improvement [38], state- and community-based organizations helped health centers collect information needed for their own quality improvement purposes as well as performance monitoring as required by CDC. To extract data needed for performance measurement, it was necessary to analyze encounter and claims data and client medical records. Thus, it was important for data to be accurately entered into the electronic medical records (EMRs). After initial attempts to collect data, it became clear that service codes were not being entered correctly or consistently. Significant TTA was needed to ensure health center staff were using the correct service codes and entering the codes routinely into their EMRs. State- and community-based organizations also helped health centers review their data and to use to improve quality of care. Based on our experience, TTA providers should be hired with expertise on EMRs or need to be trained on it themselves—they need to understand EMRs and ideally be able to help health centers improve the data recorded in the EMR and be able to provide support in analyzing the data. Even if a health center is not using service codes for quality improvement purposes, making sure all services provided are correctly documented in the EMR is important for optimal reimbursement of services.
The tools, resources, strategies, and TTA provided by national organizations and CDC were critical for building the capacity of state- and community-based organizations. Some synthesis and translation activities occurred before the initiative (e.g., HHS review of effective programs, PSBA-GTO manual), but efforts to translate best practices in each component facilitated TTA in the support system and implementation in the delivery system. Without the TTA of the national organizations (prevention support system), most state- and community-based organizations likely would not have had the capacity to meet the requirements for the project or needs of program and health center partners. Extensive training of trainers on EBIs for staff at state- and community-based organizations made possible training facilitators at their program partners. Many state- and community-based organizations had not previously worked with health centers. Recruiting, hiring, and training state- and community-based organization staff on clinical best practices and quality improvement was needed before interacting with the health center partners.
With the support of national organizations, state- and community-based organizations ensured that tools, strategies, and resources developed by the national organizations, or others were integrated into local initiatives. HHS’s review of effective programs and clinical best practices compiled by CDC and the national organizations provided guidance for EBI selection and recommendations for clinical practice. By distilling relevant published literature, strategies guided by best practice documents for community mobilization, stakeholder education, and working with diverse communities provided state- and community-based organizations with concrete, actionable strategies that could be integrated into their plans. Community mobilization and stakeholder education efforts developed the foundation for partnerships and raising awareness among community leaders and members. The strategies developed by the national organizations provided guidance on how to work with, and tailor your message, for different stakeholders and how to effectively manage the leadership teams in the community. Research that measures the impact of these strategies on teen pregnancy and birth will improve efforts to reduce teen pregnancy further.
Limitations in this report include the nature of self-reported data which may be biased in favor of the reporter and may be differentially reported across reporters. Although training was provided on how to track TTA, it is possible that not all organizations tracked TTA in the same way. This article only reports on TTA provided by the national organizations not that provided by CDC. Further analysis of the data is needed to determine if the initiatives has had an impact on birth rates.
The community-wide initiatives for teen pregnancy prevention were ground-breaking efforts to incorporate comprehensive approaches to a public health problem using tiered TTA based on the Interactive Systems Framework. We found that comprehensive implementation takes time and significant TTA to ensure organizations have the capacity to integrate best practices and strategies at the practitioner level. This community-wide approach has the potential to advance TPP and could be applied to other public health problems. To better meet the needs of youth in communities and to further reduce teen pregnancy and birth rates, elements of the community-wide initiatives and lessons learned were incorporated into new funding opportunity announcements issued by the OAH and the CDC in spring 2015.
For more information on the community-wide initiatives or on the Teenage Pregnancy Prevention program administered by the HHS Office of Adolescent Health, readers are encouraged to visit the http://www.cdc.gov/teenpregnancy and http://www.hhs.gov/ash/oah/.
IMPLICATIONS AND CONTRIBUTION.
Implementation of a comprehensive, evidence-based community-wide approach to teen pregnancy prevention required significant training and technical assistance. A tiered training and technical assistance approach was helpful for distilling the research and translating it to practice in the communities.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, U.S. Department of Health and Human Services.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest to disclose.
Publisher's Disclaimer: Disclaimer: Publication of this article was supported by the Office of Adolescent Health. The opinions or views expressed in this supplement are those of the authors and do not necessarily represent the official position of the funder.
References
- [1].Hamilton BE, Ventura SJ, Osterman MJ. Births: Preliminary data for 2015. Natl Vital Stat Rep 2016;65. [PubMed] [Google Scholar]
- [2].Sedgh G, Finer LB, Bankole A, et al. Adolescent pregnancy, birth, and abortion rates across countries: Levels and recent trends. J Adolesc Health 2015;56:223–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Romero L, Pazol K, Warner L, et al. Reduced disparities in birth rates among teens aged 15–19 Years - United States, 2006–2007 and 2013–2014. MMWR Morb Mortal Wkly Rep 2016;65:409–14. [DOI] [PubMed] [Google Scholar]
- [4].Ventura SJ, Hamilton BE, Matthews TJ. National and state patterns of teen births in the United States, 1940–2013. Natl Vital Stat Rep 2014;63:1–34. [PubMed] [Google Scholar]
- [5].Haskins R, Baron J. Part 6: The Obama Administration’s evidence-based social based policy initiatives: an Overview. In: Evidence for Social Policy and Practice: Perspectives on How Research and Evidence Can Influence Decision Making in Public Services London: NESTA; 2011. [Google Scholar]
- [6].Prevention C. f. D. C. a. Winnable battles Centers for Disease Control and Prevention; 2014. Available at: http://www.cdc.gov/winnablebattles/. Accessed July 3, 2016. [Google Scholar]
- [7].Kappeler EM, Farb AF. Historical context for the creation of the office of adolescent health and the teen pregnancy prevention program. J Adolesc Health 2014;54(3 Suppl):S3–9. [DOI] [PubMed] [Google Scholar]
- [8].Goesling B, Colman S, Trenholm C, et al. Programs to reduce teen preg-nancy, sexually transmitted infections, and associated sexual risk behaviors: A systematic review. J Adolesc Health 2014;54:499–507. [DOI] [PubMed] [Google Scholar]
- [9].Lindberg L, Santelli J, Desai S. Understanding the decline in adolescent fertility in the United States, 2007–2012. J Adolesc Health 2016;59: 577–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. Am J Public Health 2007;97:150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Romero LM, Middleton D, Mueller T, et al. Improving the implementation of evidence-based clinical practices in adolescent reproductive health care services. J Adolesc Health 2015;57:488–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Brindis CD, Geierstanger SP, Wilcox N, et al. Evaluation of a peer provider reproductive health service model for adolescents. Perspect Sex Reprod Health 2005;37:85–91. [DOI] [PubMed] [Google Scholar]
- [13].Christner J, Davis P, Rosen DS. Office-based interventions to promote healthy sexual behavior. Adolesc Med State Art Rev 2007;18:544–57, viii. [PubMed] [Google Scholar]
- [14].Morrison A, Mackie CM, Elliott L, et al. The Sexual Health Help Centre: a service for young people. J Public Health Med 1997;19:457–63. [DOI] [PubMed] [Google Scholar]
- [15].Reddy DM, Fleming R, Swain C. Effect of mandatory parental notification on adolescent girls’ use of sexual health care services. JAMA 2002;288: 710–4. [DOI] [PubMed] [Google Scholar]
- [16].Sadler LS, Daley AM. A model of teen-friendly care for young women with negative pregnancy test results. Nurs Clin North Am 2002;37: 523–35. [DOI] [PubMed] [Google Scholar]
- [17].Secura G, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med 2014;371: 1316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Winter L, Breckenmaker LC. Tailoring family planning services to the special needs of adolescents. Fam Plann Perspect 1991;23:24–30. [PubMed] [Google Scholar]
- [19].Saunders EJ. Mobilizing communities in support of teen pregnancy prevention: “Communitywide initiatives” findings. Health Promot Pract 2016. [Epub ahead of print], 10.1177/1524839916662602. [DOI] [PubMed]
- [20].Hawkins JD, Brown EC, Oesterle S, et al. Early effects of communities that care on targeted risks and initiation of delinquent behavior and substance use. J Adolesc Health 2008;43:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health 2000;21: 369–402. [DOI] [PubMed] [Google Scholar]
- [22].Wandersman A, Florin P. Community interventions and effective prevention. Am Psychol 2003;58:441–8. [DOI] [PubMed] [Google Scholar]
- [23].Kreuter MW, Lukwago SN, Bucholtz RD, et al. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Educ Behav 2003;30:133–46. [DOI] [PubMed] [Google Scholar]
- [24].Villarruel AM, Jemmott LS, Jemmott JB 3rd. Designing a culturally based intervention to reduce HIV sexual risk for Latino adolescents. J Assoc Nurses AIDS Care 2005;16:23–31. [DOI] [PubMed] [Google Scholar]
- [25].Duffy JL, Prince MS, Johnson EE, et al. Enhancing teen pregnancy prevention in local communities: Capacity building using the interactive systems framework. Am J Community Psychol 2012;50:370–85. [DOI] [PubMed] [Google Scholar]
- [26].Lesesne CA, Lewis KM, White CP, et al. Promoting science-based approaches to teen pregnancy prevention: Proactively engaging the three systems of the interactive systems framework. Am J Community Psychol 2008;41:379–92. [DOI] [PubMed] [Google Scholar]
- [27].Rolleri LA, Wilson MM, Paluzzi PA, Sedivy VJ. Building capacity of state adolescent pregnancy prevention coalitions to implement science-based approaches. Am J Community Psychol 2008;41:225–34. [DOI] [PubMed] [Google Scholar]
- [28].Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: The interactive systems framework for dissemination and implementation. Am J Community Psychol 2008;41: 171–81. [DOI] [PubMed] [Google Scholar]
- [29].Bhuiya N, House LD, Desmarais J, et al. Strategies to build readiness in community mobilization efforts for implementation in a multi-year teen pregnancy prevention initiative. J Adolesc Health 2017;60:S51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Galloway CT, Duffy JL, Dixon RP. Exploring african-american and latino teens’ perceptions of contraception and access to reproductive health care services. J Adolesc Health 2017;60:S57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].House LD, Tevendale HD, Martinez-Garcia G. Implementing evidence-based teen pregnancy-prevention interventions in a community-wide initiative: building capacity and reaching youth. J Adolesc Health 2017; 60:S18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Plastino K, Quinlan J, Todd J, Tevendale HD. Stakeholder education and community mobilization garner support for sex education. J Adolesc Health 2017;60:S24–9. [DOI] [PubMed] [Google Scholar]
- [33].Romero LM, Olaiya O, Hallum-Montes R, et al. Efforts to increase implementation of evidence-based clinical practices to improve adolescent-friendly reproductive health services. J Adolesc Health 2017;60:S30–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].O’Uhuru DJ, Santiago V, Murray LE, et al. Bronx teens connection’s clinic linkage model: connecting youth to quality sexual and reproductive health care. J Adolesc Health 2017;60:S38–44. [DOI] [PubMed] [Google Scholar]
- [35].Sotolongo J, House LD, Swanson S, Davis SEH. Integrated community strategies for linking youth to adolescent reproductive health services: a case study. J Adolesc Health 2017;60:S45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Lesesne CA, Lewis KM, Fisher D, et al. Promoting science-based approaches to teen pregnancy prevention using Getting to Outcomes for Teen Pregnancy Prevention (PSBA-GTO) Atlanta, GA: Centers for Disease Control and Prevention; 2016. [Google Scholar]
- [37].Chinman M, Acosta J, Ebener P, et al. Can implementation support help community-based settings better deliver evidence-based sexual health promotion programs? a randomized trial of getting to outcomes(R). Implement Sci 2016;11:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep 2014;63(Rr-04):1–54. [PubMed] [Google Scholar]


