Abstract
Background:
The extent to which racial/ethnic disparities in pneumonia care occur within or between hospitals is unclear.
Objective:
Examine within and between-hospital racial/ethnic disparities in quality indicators and mortality for patients hospitalized for pneumonia.
Research Design:
Retrospective cohort study.
Subjects:
1,183,753 non-Hispanic white, African American and Hispanic adults hospitalized for pneumonia between January 2005 and June 2006.
Measures:
8 pneumonia care quality indicators and in-hospital mortality.
Results:
Performance rates for the 8 quality indicators ranged from 99.4% (oxygenation assessment within 24 hours) to 60.2% (influenza vaccination). Overall hospital mortality was 4.1%. African American and Hispanic patients were less likely to receive pneumococcal and influenza vaccinations, smoking cessation counseling, and first dose of antibiotic within 4 hours than white patients at the same hospital (ORs=.65-.95). Patients at hospitals with the racial composition of those attended by average African Americans and Hispanics were less likely to receive all indicators except blood culture within 24 hours than patients at hospitals with the racial composition of those attended by average whites. Hospital mortality was higher for African Americans (OR=1.05, 95% CI=1.02,1.09) and lower for Hispanics (OR=.85, 95% CI=.81,.89) than for whites within the same hospital. Mortality for patients at hospitals with the racial composition of those attended by average African Americans (OR=1.21, 95% CI=1.18,1.25) or Hispanics (OR=1.18, 95% CI=1.14,1.23) was higher than for patients at hospitals with the racial composition of those attended by average whites.
Conclusions:
Racial/ethnic disparities in pneumonia treatment and mortality are larger and more consistent between hospitals than within hospitals.
Keywords: Health disparities, pneumonia, quality of care
Pneumonia leads to 1.2 million hospital admissions annually in the United States at a cost exceeding $8 billion, and, combined with influenza, represents the 8th leading cause of death in the country.1–3 Although certain processes of care recommended for patients who develop pneumonia are cost-effective prevention strategies (e.g., pneumococcal and influenza vaccination),4–9 and others have been associated with reduced mortality for patients hospitalized for pneumonia (e.g., appropriate and timely initial antibiotic therapy),10–14 there is wide variation across hospitals in the performance of many of the quality measures recommended for patients with pneumonia.15 Moreover, there has been concern that these quality measures are not performed uniformly across patients from all racial and ethnic groups. Given that pneumonia accounts for over 5% of the overall difference in potential life-years lost to death between African Americans and Non-Hispanic whites,16 it is important to understand whether systematic racial and ethnic differences exist in the management of pneumonia.
The current study investigates whether there are racial and ethnic disparities in quality of care and outcomes for patients hospitalized for pneumonia. Previous studies have found that racial/ethnic minorities are less likely than whites to receive some, but not all, recommended processes of care for pneumonia.17–23 For example, minorities hospitalized for pneumonia are less likely than whites to receive antibiotics within 8 hours of presentation or smoking cessation counseling.20–22 In contrast, minorities and whites are equally likely to have blood cultures conducted prior to receiving antibiotics and to receive appropriate antibiotics.21, 22 Whether there are racial disparities in pneumonia-related mortality is unclear, as documented mortality rates for African Americans hospitalized for pneumonia have been similar19, 24, 25 or lower21, 26, 27 than for patients of other races.
Prior investigations of disparities in pneumonia care have been limited in that they examined relatively few quality indicators, included data from a small number of hospitals, or combined all minority patients into a single category or compared just one minority group (e.g., African Americans) with whites.20–23 Prior work has also provided little information about whether disparities in pneumonia care occur because racial/ethnic minorities receive lower quality of care than whites within the same hospital (i.e., within-hospital disparities) and/or because minorities are more likely than whites to receive care in hospitals that deliver poorer quality of care overall (i.e., between-hospital disparities). Two studies have documented that hospitals serving higher concentrations of African American and Hispanic patients have lower performance on pneumonia quality indicators,17, 18 while a third found that differences between minority and white patients in pneumonia quality indicators were attenuated after controlling for site of care.20 These studies indicate that disparities in pneumonia care are due, at least in part, to differences in where minority and white patients receive care. However, these studies offer no information on the relative magnitude of within- and between-hospital disparities.
The objectives of the current study were to examine racial/ethnic disparities in pneumonia care and in-hospital mortality for African American, Hispanic, and non-Hispanic white adults hospitalized for pneumonia, and to examine the extent to which such disparities occur within and between hospitals. By examining 8 process quality indicators and mortality in a sample of patients from over 95% of acute-care hospitals in the United States, our goal was to provide a comprehensive account of racial/ethnic variation in the management of pneumonia.
Methods
Patient Sample
Patient-level data from the Quality Improvement Organization Clinical Data Warehouse, an electronic data repository created by the Centers for Medicare & Medicaid (CMS), were analyzed. Greater than 95% of acute care hospitals paid under the CMS Inpatient Prospective Payment System (therefore excluding military or Veterans Affairs hospitals) submit all-payer data (including Medicare and non-Medicare) to this repository on over one million pneumonia cases per year.28 All elements in the database were abstracted from medical records by chart reviews conducted by hospital personnel using uniform instructions. All abstracted medical record data were subject to randomly selected and independently performed validation audits conducted by a CMS contractor on a quarterly basis. Specification manuals containing the complete guidelines for data abstraction are available online.29
We selected pneumonia cases that occurred between January 2005 and June 2006. The initial sample included all patients aged 18 years or older with a principal diagnosis of pneumonia at the time of discharge, as identified by the International Classification of Disease 9th Revision – Clinical Modification (ICD−9−CM) codes 481–483.8, 485, 486, or 487.0. The sample also included patients with a principal diagnosis of septicemia (ICD-9-CM 038.0–038.9) or respiratory failure (ICD-9-CM 518.81 or 518.84) and a secondary diagnosis of pneumonia. Although these codes do not guarantee a diagnosis of community-acquired pneumonia, patients with hospital acquired pneumonia were largely excluded by selecting patients based on their principal diagnosis and using a medical review to confirm a working diagnosis of pneumonia at the time of admission. Patients were further defined as at risk for healthcare associated pneumonia if they stayed in a hospital, nursing home, or extended care facility within the last 90 days, or if they received dialysis, wound care, tracheostomy care, or ventilator care within the last 30 days. Twenty-nine percent of patients in the sample met these criteria.
As in previous studies examining pneumonia care, we excluded patients who did not have pneumonia as a working diagnosis at admission (physician documentation of the diagnosis of pneumonia written before or at admission), died on the day of admission, received comfort measures only (documentation of palliative care), left the hospital against medical advice, were transferred from or discharged to another acute care hospital, or received no antibiotic therapy during their hospital stay.13, 21, 30 These characteristics were existing elements in the database. We also excluded patients who were from U.S. territories; had AIDS or HIV; had missing race/ethnicity or gender; had a race/ethnicity other than non-Hispanic white, African American, or Hispanic; remained hospitalized longer than 90 days; or had missing data on all study outcomes.
Measures
Patient characteristics.
Patient age, sex, race/ethnicity, insurance status, and presence of comorbid conditions were included in the analyses. Hospitals reported patient race as white, Black or African American, American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, and other; Hispanic or Latino ethnicity was reported as a separate variable. We created 4 mutually exclusive racial/ethnic categories: non-Hispanic whites, non-Hispanic African Americans, Hispanics (of all races), and other race/ethnicity. The other race/ethnicity group was excluded from analyses due to the relatively small proportion of patients in this group (3%) and the difficulty of drawing conclusions about them due to their heterogeneous nature (23% were American Indian or Alaska Native, 50% were Asian, 6% were Native Hawaiian or Pacific Islanders, and 21% were other). Hospitals reported all sources of payment as Medicare, Medicaid, and/or other, or indicated no insurance/not documented/unable to determine. We created an insurance variable with 3 mutually exclusive categories: Medicaid with or without other insurance, other insurance, and no insurance/unable to determine. The following comorbid conditions were identified using ICD-9-CM codes specified by Romano and colleagues31: cancer, liver disease, myocardial infarction, heart failure, chronic pulmonary disease, cerebrovascular disease (including hemiplegia or paraplegia), renal disease, peripheral vascular disease, dementia, rheumatologic disease, peptic ulcer disease, and diabetes.
Hospital characteristics.
Hospital characteristics were obtained from the 2005 CMS Inpatient Prospective Payment System Impact File and a CMS database maintained via the Online Survey Certification and Reporting System.32 Hospital characteristics included rural or urban location, bed size, teaching status, and geographic location (4 U.S. census regions). Number of beds and teaching status were highly correlated and were therefore combined into a single categorical variable: large/teaching, large/non-teaching, small-medium/teaching, and small-medium/non-teaching. “Large” hospitals were those with >268 beds (75th percentile).
Quality indicators.
We assessed 8 processes of care designated by CMS and the Joint Commission as quality indicators for the treatment of pneumonia: 1) oxygenation assessment within 24 hours of admission, 2) administration of pneumococcal vaccination, 3) blood culture within 24 hours of admission, 4) blood culture before first dose of antibiotic, 5) smoking cessation counseling, 6) first antibiotic dose administered within 4 hours of presentation, 7) appropriate antibiotic selection within 24 hours of admission, and 8) administration of influenza vaccination.33 According to CMS and Joint Commission specifications, oxygenation assessment and appropriate antibiotic selection were indicated for all patients. Blood culture within 24 hours was restricted to patients who were transferred or admitted to the intensive care unit within 24 hours of hospital arrival. Blood culture before antibiotic was restricted to patients who received a blood culture in the emergency department. Smoking cessation counseling was applicable to patients who had documentation in their medical record of having smoked cigarettes anytime during the previous year. Appropriate antibiotic selection was applicable to immunocompetent patients with community-acquired pneumonia. Excluded from this measure were immunocompromised patients (i.e, those with AIDS, cystic fibrosis, prior hospitalization within 14 days, or chemotherapy, systemic immunosuppressive therapy, leukemia, lymphoma, or radiation therapy within the past 3 months) and those at-risk for healthcare associated pneumonia, as defined previously. Pneumococcal vaccination was applicable to those 65 or older and influenza vaccination was applicable to those 50 or older who were discharged between October and February. Patients were counted as achieving the pneumococcal and influenza vaccination measures if they received them during their hospital stay, or if they were not vaccinated due to documented contraindications, documented vaccination prior to admission, or refusal of the vaccination.
Completion rates of each quality indicator were calculated by dividing the number of patients who had an indicator completed by the number of patients who were eligible for it. We also calculated a composite measure to assess the extent to which patients received all quality indicators for which they were eligible. We utilized an “observed-minus-expected” (O-E) composite measure to take into account that overall performance was higher on some indicators than on others (e.g. overall performance was 99.4% for oxygenation assessment and 60.2% for influenza vaccination).34 Observed scores were the number of indicators each patient had completed divided by the number for which they were eligible (possible range of 0 – 100%). Expected scores were the average population performance rate for the indicators that were applicable to each patient. The composite consisted of the observed scores minus the expected scores. For example, a patient who was eligible for 6 indicators and had 3 completed would have an observed score of 50%. If the average population performance rate across the 6 measures for which the patient was eligible was 80% (i.e., the expected score), the patient’s O-E composite would be −30%. This would indicate that 30% fewer quality indicators were completed for that patient than would be expected given the population completion rates for the relevant indicators.
In-hospital mortality.
We also examined in-hospital mortality, which was defined as deaths that occurred within 30 days of admission while the patient was in the hospital. Vital status after discharge was not available to ascertain overall 30-day mortality.
Statistical Analyses
We examined unadjusted differences in completion rates for each quality indicator, the O-E composite, and hospital mortality across the 3 racial/ethnic groups using chi-square tests for categorical outcomes and analysis of variance for continuous outcomes. We used generalized linear mixed model regression to examine the effects of patient race/ethnicity on these measures, adjusting for patient (i.e., age, sex, insurance status, and comorbid conditions) and hospital (i.e., rural versus urban, bed size/teaching status, and geographic region) characteristics. Linear models were used for the O-E composite measure and logistic models for the other measures. Random intercepts were used for each hospital.
We partitioned the effect of patient race/ethnicity into within-hospital and between-hospital components. Within-hospital effects were estimated by including 2 patient-level terms, one for African Americans and one for Hispanics. These terms were computed as a standard dummy variable for each minority group (1 = patient belongs to the minority group, 0 = patient does not belong to that group) minus the proportion of patients in our analytic sample who were treated for pneumonia at the hospital and who belong to that minority group. The within-hospital effects provide an estimate of the difference in outcome for a patient of a given race/ethnicity compared to an otherwise identical white patient at the same hospital. The between-hospital effects were estimated by including 2 hospital-level variables indicating the proportion of African American and Hispanic pneumonia patients in our analytic sample at the hospital where the patient was treated. The between-hospital effects estimate the effect of a hospital’s proportion of African American or Hispanic pneumonia patients on the study outcomes. Use of this approach allows for direct estimation of the within-hospital and between-hospital effects of race/ethnicity without making assumptions about the association of within-hospital and between-hospital effects, as do methods that estimate these effects individually.35, 36
Rescaling of between-hospital effects.
The between-hospital effects estimate the differences in outcomes for patients at a hospital where 100% of patients belong to a given racial/ethnic group compared to a hospital where 0% of patients belong to that group. Given that few hospitals have predominantly-minority patient populations, we rescaled the between-hospital effects to reflect the racial composition of hospitals attended by typical patients of each racial/ethnic group in our sample. For example, for African Americans we identified the median African American concentration such that half of the African Americans in the sample attended hospitals with that concentration or more of African Americans and half attended hospitals with fewer African Americans. Similarly, we identified the median concentration of African Americans at hospitals attended by whites. We scaled the between hospital effects by multiplying the between-hospital parameter estimates by the difference in these two values. For dichotomous outcomes, scaled odds ratios were computed in the standard way: by exponentiating the scaled parameter estimates. The scaled between hospital effects indicate the effect of hospital racial/ethnic concentration for the typical patient from each racial/ethnic group compared to the typical white patient. All analyses were conducted using SAS Version 9.1 (SAS Institute Inc, Cary, NC).
Human Subjects Review
The use of the data and analytic plan for the current study were approved by the Institutional Review Board at the Veterans Affairs Pittsburgh Healthcare System.
Results
Our sample was drawn from 4,527 hospitals, of which 54.3% were urban and 68.1% were small-to-medium/non-teaching (Table 1). Of the 1,761,953 patients hospitalized for pneumonia at these hospitals, 1,183,753 (67.2%) met all eligibility criteria (Figure 1). The final study population was 82.5% non-Hispanic white, 11.4% African American, and 6.1% Hispanic. Overall, 53.7% of all patients were women, 82.3% had insurance other than Medicaid, and their mean age was 70 years (Table 2). There was significant variation in demographic characteristics across racial/ethnic subgroups (Table 2).
Table 1:
Hospital Characteristics
| Frequency (N = 4,527) |
||
|---|---|---|
| Hospital Characteristics | Number | Percent |
| Urban | 2,456 | 54.3 |
| Bed Size/Teaching Status | ||
| Large/Teaching | 747 | 16.5 |
| Large/Non-Teaching | 393 | 8.7 |
| Small-Medium/Teaching | 303 | 6.7 |
| Small-Medium/Non-Teaching | 3,084 | 68.1 |
| Geographic Region | ||
| Northeast | 622 | 13.7 |
| Midwest | 1,347 | 29.8 |
| South | 1,745 | 38.5 |
| West | 813 | 18.0 |
Figure 1:
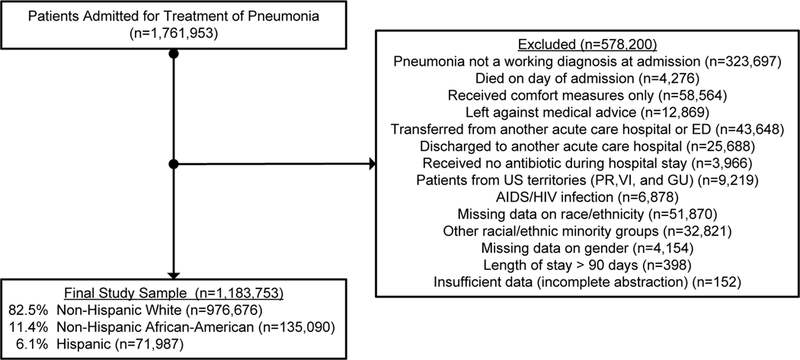
Identification of the Study Sample
Table 2:
Baseline Characteristics of a National Sample of Adults Hospitalized for Pneumonia
| Patient Characteristics | Total Sample (N=1,183,753) |
Non-Hispanic White (n=976,676) |
Non-Hispanic African American (n=135,090) |
Hispanic (n=71,987) |
*p value |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, mean (SD) | 70 (17) | 71 (16) | 61 (18) | 66 (19) | <.0001 |
| Women (%) | 53.7 | 53.6 | 54.5 | 52.6 | <.0001 |
| Insurance status (%) | <.0001 | ||||
| Medicaid with or without other Insurance | 13.9 | 11.1 | 25.8 | 29.1 | <.0001 |
| Other Insurance (Medicare or private) | 82.3 | 85.9 | 66.5 | 63.0 | <.0001 |
| No insurance or unable to determine | 3.8 | 3.0 | 7.6 | 7.9 | <.0001 |
| Comorbid Conditions (%) | |||||
| Chronic pulmonary disease | 50.3 | 52.5 | 39.5 | 41.0 | <.0001 |
| Heart failure | 26.8 | 27.4 | 24.1 | 23.4 | <.0001 |
| Diabetes | 25.1 | 23.7 | 30.5 | 34.1 | <.0001 |
| Cancer | 7.6 | 7.8 | 7.3 | 5.9 | <.0001 |
| Myocardial infarction | 6.4 | 6.7 | 4.6 | 4.7 | <.0001 |
| Renal disease | 4.9 | 4.5 | 7.3 | 6.0 | <.0001 |
| Cerebrovascular disease | 4.9 | 4.8 | 6.0 | 5.1 | <.0001 |
| Peripheral vascular disease or hemiplegia or paraplegia | 4.4 | 4.6 | 3.8 | 3.4 | <.0001 |
| Rheumatologic disease | 3.2 | 3.2 | 3.3 | 3.0 | <.0001 |
| Dementia | 1.6 | 1.6 | 1.5 | 1.4 | <.0001 |
| Peptic ulcer disease | 1.1 | 1.1 | 1.1 | 1.2 | 0.11 |
| Liver disease | 1.0 | 0.9 | 0.9 | 2.2 | <.0001 |
| Types of Hospitals Attended | |||||
| Urban (%) | 75.0 | 72.3 | 85.7 | 91.3 | <.0001 |
| Bed size/teaching status (%) | |||||
| Large/teaching | 31.8 | 28.4 | 49.7 | 44.1 | <.0001 |
| Large/non-teaching | 17.2 | 17.3 | 16.5 | 16.9 | <.0001 |
| Small-medium/teaching | 8.0 | 8.1 | 7.9 | 7.1 | <.0001 |
| Small-medium/non-teaching | 43.0 | 46.2 | 26.0 | 32.0 | <.0001 |
| Geographic region (%) | |||||
| Northeast | 18.6 | 19.1 | 16.0 | 16.7 | <.0001 |
| Midwest | 25.1 | 27.0 | 21.3 | 6.9 | <.0001 |
| South | 41.5 | 39.5 | 55.0 | 42.7 | <.0001 |
| West | 14.8 | 14.4 | 7.6 | 33.7 | <.0001 |
Comparisons across the three racial/ethnic groups were made using analysis of variance for age and chi-square tests for all other variables.
Patients were most often hospitalized in urban areas (75.0%) and were most often treated at small-to-medium, non-teaching (43.0%) or large, teaching hospitals (31.8%). African American and Hispanic patients were treated at urban and large/teaching hospitals significantly more often than white patients (Table 2). African American and Hispanic patients were also more likely than whites to be admitted to hospitals with diverse patient populations. For whites, the median concentration of African American pneumonia patients admitted to the same hospital was 4%; in contrast, the median concentration of African American patients at hospitals attended by African Americans was 27%. The median concentrations of Hispanic pneumonia patients at hospitals attended by whites and Hispanics were 1% and 29%, respectively. The differences of these values (27%−4%=23% and 29%−1%−28%, respectively) were used to scale the between-hospital effects.
Quality Indicators
Overall performance rates on quality indicators ranged from 99.4% for oxygenation assessment within 24 hours to 60.2% for influenza vaccination (Table 3). Although there were statistically significant (p<.001) differences across racial/ethnic groups for all 8 indicators, only 4 of the indicators displayed clinically meaningful differences (Table 3). Specifically, pneumococcal vaccination was completed for 67.7% of whites, compared to 53.8% for African Americans and 52.9% for Hispanics, with a similar pattern observed for influenza vaccination. First antibiotic dose within 4 hours was also achieved more frequently for whites (77.9%) than for African Americans (70.0%) or Hispanics (70.7%). Finally, smoking cessation counseling was completed for more whites (81.6%) than for Hispanics (76.1%).
Table 3:
Unadjusted Performance on Quality Indicators by Race and Ethnicity
| Quality Indicator | Total Sample (N=1,183,753) |
Non-Hispanic White (n=976,676) |
Non-Hispanic African American (n=135,090) |
Hispanic (n=71,987) | ||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | N | (%) | |
| Oxygenation assessment within 24 hours | ||||||||
| Eligible | 1,183,577 | 976,542 | 135,063 | 71,972 | ||||
| Completed | 1,176,152 | (99.4) | 970,748 | (99.4) | 134,075 | (99.3) | 71,329 | (99.1) |
| Pneumococcal vaccination | ||||||||
| Eligible | 743,166 | 647,964 | 55,984 | 39,218 | ||||
| Completed | 489,540 | (65.9) | 438,702 | (67.7) | 30,102 | (53.8) | 20,736 | (52.9) |
| Blood culture within 24 hours | ||||||||
| Eligible | 403,876 | 331,600 | 49,085 | 23,191 | ||||
| Completed | 325,796 | (80.7) | 265,338 | (80.0) | 41,064 | (83.7) | 19,394 | (83.6) |
| Blood culture before antibiotic | ||||||||
| Eligible | 902,555 | 736,176 | 108,547 | 57,832 | ||||
| Completed | 769,485 | (85.3) | 631,240 | (85.7) | 90,032 | (82.9) | 48,213 | (83.4) |
| Smoking cessation counseling | ||||||||
| Eligible | 262,227 | 210,059 | 40,018 | 12,150 | ||||
| Completed | 212,866 | (81.2) | 171,391 | (81.6) | 32,228 | (80.5) | 9,247 | (76.1) |
| First antibiotic dose within 4 hours | ||||||||
| Eligible | 977,587 | 799,390 | 116,835 | 61,362 | ||||
| Completed | 748,147 | (76.5) | 622,940 | (77.9) | 81,834 | (70.0) | 43,373 | (70.7) |
| Appropriate antibiotic selection | ||||||||
| Eligible | 792,888 | 653,204 | 88,686 | 50,998 | ||||
| Completed | 647,109 | (81.6) | 533,943 | (81.7) | 71,972 | (81.2) | 41,194 | (80.8) |
| Influenza vaccination | ||||||||
| Eligible | 395,532 | 334,902 | 37,732 | 22,898 | ||||
| Completed | 238,044 | (60.2) | 208,699 | (62.3) | 18,196 | (48.2) | 11,149 | (48.7) |
| Observed – Expected Composite | ||||||||
| Mean (Standard Deviation) | −0.3 | (19.1) | 0.4 | (18.9) | −3.5 | (19.5) | −4.0 | (20.0) |
Note: Overall tests for differences by race/ethnicity are significant for all measures. All pairwise comparisons between racial/ethnic minority groups and whites are significantly different at p < .0001.
Unadjusted performance on the O-E composite was significantly lower (p<.001) for African Americans and Hispanics than for whites (Table 3). Whites, on average, received 0.4% more quality indicators than would be expected given population performance rates. In contrast, African Americans and Hispanics received 3.5% and 4.0% fewer quality indicators, respectively, than expected.
In adjusted models, the within-hospital effects of patient race/ethnicity indicated that the odds of receiving a pneumococcal vaccination was significantly lower for African Americans (OR=.65) and Hispanics (OR=.73) compared to whites treated in the same hospital (Table 4). This was also the case for smoking cessation counseling (OR=.87 and .85 for African Americans and Hispanics, respectively), first antibiotic dose within 4 hours (OR=.89 and .95), and influenza vaccinations (OR=.70 and .78). Within-hospital effects for the remaining measures were less consistent, with performance being roughly equivalent or better for at least one minority subgroup compared to whites. According to the O-E composite, African Americans and Hispanics each had significantly (p<.001) fewer quality indicators completed than expected, compared to whites at the same hospital (−1.6% and −0.9%, respectively).
Table 4:
Adjusted within-hospital and between-hospital effects of race and ethnicity on quality indicators†
|
Within-Hospital Effects†† |
Between-Hospital Effects††† |
Scaled Between-Hospital Effects†††† |
|||||
|---|---|---|---|---|---|---|---|
| Measure | Race/Ethnicity | OR | (95% CI) | OR | (95% CI) | Scaled OR | (95% CI) |
| Oxygenation assessment | African American | 1.19 | (1.10,1.30) | 0.18 | (0.13,0.26) | 0.68 | (0.62,0.73) |
| within 24 hours | Hispanic | 1.01 | (0.90,1.14) | 0.17 | (0.11,0.26) | 0.61 | (0.54,0.68) |
| Pneumococcal | African American | 0.65 | (0.64,0.67) | 0.16 | (0.12,0.20) | 0.66 | (0.62,0.69) |
| Vaccination | Hispanic | 0.73 | (0.71,0.76) | 0.34 | (0.26,0.45) | 0.74 | (0.69,0.80) |
| Blood culture | African American | 1.04 | (1.01,1.08) | 1.06 | (0.86,1.29) | 1.01 | (0.97,1.06) |
| within 24 hours | Hispanic | 1.06 | (1.01,1.11) | 1.11 | (0.88,1.39) | 1.03 | (0.97,1.10) |
| Blood culture | African American | 0.97 | (0.95,0.99) | 0.61 | (0.54,0.70) | 0.89 | (0.87,0.92) |
| before antibiotic | Hispanic | 1.01 | (0.98,1.04) | 0.67 | (0.59,0.78) | 0.90 | (0.86,0.93) |
| Smoking | African American | 0.87 | (0.83,0.90) | 0.51 | (0.39,0.68) | 0.86 | (0.80,0.92) |
| cessation counseling | Hispanic | 0.85 | (0.80,0.90) | 0.55 | (0.40,0.77) | 0.85 | (0.77,0.93) |
| First antibiotic | African American | 0.89 | (0.87,0.90) | 0.43 | (0.38,0.49) | 0.82 | (0.80,0.85) |
| dose within 4 hours | Hispanic | 0.95 | (0.93,0.97) | 0.57 | (0.50,0.65) | 0.85 | (0.82,0.89) |
| Appropriate | African American | 1.04 | (1.02,1.06) | 0.63 | (0.55,0.71) | 0.90 | (0.87,0.92) |
| antibiotic selection | Hispanic | 1.10 | (1.07,1.14) | 0.61 | (0.53,0.71) | 0.87 | (0.84,0.91) |
| Influenza | African American | 0.70 | (0.68,0.72) | 0.19 | (0.15,0.24) | 0.69 | (0.65,0.72) |
| Vaccination | Hispanic | 0.78 | (0.76,0.81) | 0.39 | (0.30,0.50) | 0.77 | (0.72,0.83) |
|
Estimate |
(95% CI) |
Estimate |
(95% CI) |
Scaled Estimate |
(95% CI) |
||
| O-E Composite | African American | −1.6 | (−1.77,−1.53) | −11.8 | (−13.29,−10.23) | −2.7 | (−3.06,−2.35) |
| Hispanic | −0.9 | (−1.07,−0.73) | −8.7 | (−10.41,−6.94) | −2.4 | (−2.91,−1.94) | |
Models adjusted for patient age, gender, insurance status, comorbidities, and hospital urban/rural status, size/teaching status, and U.S. region.
Within-hospital ORs represent the odds of an outcome for patients of the given race/ethnic group compared to white patients within the same hospital.
Between-hospital ORs represent the odds of an outcome for patients treated at hospitals where 100% of pneumonia patients are of the given race/ethnic group compared to patients at hospitals where 0% of pneumonia patients or of that group.
Scaled between-hospital ORs are transformations of the original between-hospital ORs and are provided to aid interpretation of the effects with regard to the racial composition of hospitals observed in our sample. They represent the effect of hospital racial composition for the typical patient from each racial/ethnic group compared to the typical white patient (see Methods for full details).
There were consistent between-hospital effects of racial/ethnic patient concentration on the quality indicators. Patients who received care at hospitals that served higher concentrations of African American or Hispanic patients had significantly lower odds of receiving 7 of the 8 quality indicators, with the exception of blood culture within 24 hours (Table 4). These effects were substantial, even after rescaling them to reflect the racial composition of hospitals observed in our sample: scaled ORs ranged from .66 to .90 for African American patient concentration and from .61 to .90 for Hispanic patient concentration (Table 4). Performance on the O-E composite was also significantly lower (p<.001) for patients who attended hospitals with higher concentrations of African American or Hispanic patients (scaled estimates = −2.7% and −2.4%, respectively).
Hospital Mortality
Unadjusted hospital mortality was significantly higher (p<.001) for African Americans (4.5%) and Hispanics (4.6%) compared to whites (4.1%). In adjusted models, within-hospital effects indicated that African Americans had significantly higher odds of mortality compared to whites treated at the same hospital (OR=1.05, 95% CI=1.02–1.09), while Hispanics had significantly lower odds of mortality (OR=0.85, 95% CI=.81-.89). Between-hospital effects indicated that patients at hospitals with 100% African American patients and 100% Hispanic patients were 2.31 (95% CI=2.05–2.61) and 1.83 (95% CI=1.60–2.09) times more likely to experience hospital death, compared to patients at hospitals with 0% of each minority subgroup (scaled OR [95% CI]=1.21 [1.18,1.25] and 1.18 [1.14,1.23], respectively).
Discussion
This study provides evidence of within-hospital and between-hospital racial/ethnic disparities in processes of care and hospital mortality for patients hospitalized for pneumonia. Compared to white patients at the same hospital, African Americans and Hispanics had lower odds of receiving pneumococcal vaccination, smoking cessation counseling, first antibiotic dose within 4 hours, and influenza vaccination. Moreover, patients at hospitals serving higher concentrations of African American and Hispanic patients had lower odds of receiving 7 of 8 recommended quality indicators. Mortality was higher for African Americans than for whites within the same hospital, as well as for patients treated at hospitals with higher concentrations of African Americans or Hispanics. Hispanics had lower mortality than whites within the same hospital. Although this might seem surprising, it is consistent with the “Hispanic paradox”, which refers to the fact that Hispanics often have better health outcomes than the general population even though one would expect poorer health outcomes given their relative socio-economic position.37, 38
Our focus on whether disparities occur within and/or between hospitals is relevant to on-going efforts to understand the source of racial/ethnic disparities so that appropriate steps can be taken to address them.39 Although we found evidence of within-hospital and between-hospital disparities, the between-hospital disparities were more striking. Not only were between-hospital disparities observed for more processes of care (7 vs. 4), they tended to be of greater magnitude. For instance, the within-hospital disparity on blood culture before antibiotic for African American patients (OR=.97) was almost 10% smaller than the corresponding between-hospital disparity (scaled OR=.89). Similar differences in magnitude existed for first antibiotic dose administered within 4 hours (within-hospital and scaled between-hospital OR: .89 and .82 for African American race; .95 and .86 for Hispanic ethnicity).
The consistent and large between-hospital disparities observed in the current study support the argument that racial/ethnic disparities exist because minority patients are concentrated in lower-performing medical facilities.17–20, 40, 41 There are several reasons why facilities with high concentrations of minority patients may provide lower-quality care, such as being larger, having lower nurse-staffing levels, and obtaining more revenue from Medicaid.17, 18 It is also possible that patients at such hospitals have poorer health overall, which could contribute to poorer outcomes (e.g., mortality). We attempted to account for some of these factors by controlling for hospital size, location, and teaching status, source of payment at the patient level, and comorbid illnesses. Nevertheless, we still observed considerable between-hospital disparities on the majority of outcomes.
Our results suggest that efforts to reduce racial/ethnic disparities in pneumonia care should focus on improving performance at hospitals with large minority patient populations. Existing quality-improvement programs typically encompass all hospitals, regardless of performance, and tend to utilize financial incentive programs that reward top performing hospitals and penalize low performing hospitals. Financial incentives based on relative performance across institutions, however, may inadvertently increase disparities between institutions.42 Incentive programs aimed at improving low-performing hospitals may therefore need to be designed to reward absolute improvements rather than relative performance.
This study had several limitations. Although we were able to control for patients’ age, sex, insurance status, and comorbid conditions, we were unable to adjust for severity of the pneumonia.43 Given that the database contained limited patient demographic information, we were also unable to control for potential confounders such as patient socio-economic status. The observed racial and ethnic differences may therefore have been driven by differences in economic resources. The lack of extensive patient background information is one downside to using a national database of almost all pneumonia cases versus collecting in-depth data on a smaller sample.
When interpreting the study findings, one should also keep in mind that cases of healthcare associated pneumonia were included in all analyses except those examining appropriate antibiotic selection, which is the only process of care that CMS and the Joint Commission have restricted to patients with community-acquired pneumonia. Furthermore, one should consider that for quality indicators such as vaccinations, patients satisfied the measure if they received the vaccination prior to hospitalization, making it possible that some of the observed disparities are due to differences in outpatient care prior to hospitalization. Finally, with the data available to us we were only able to assess in-hospital rather than 30-day mortality. Although it would have been preferable to assess 30-day mortality, in-hospital mortality has been shown to be an acceptable substitute when 30-day mortality data are unavailable.44
This study also had several strengths. Most notable is that it utilized a large national database that included patient-level data on pneumonia hospitalizations from over 4,000 hospitals, making our findings highly generalizable. Additional strengths were that we examined disparities in 8 quality indicators and hospital mortality across the 3 largest racial/ethnic groups in the United States, thus providing a more comprehensive assessment of disparities in pneumonia care and outcomes than previous studies. We also partitioned the effects of patient race into within-hospital and between-hospital effects, which was not possible in prior studies that relied on hospital-level data.17, 18
Our findings indicate that racial/ethnic disparities in pneumonia care occur both within and between hospitals, but that between-hospital disparities are more consistent across measures and are often of greater magnitude. Our comprehensive study of pneumonia quality indicators in a large number of hospitals adds substantial support to the emerging consensus that racial/ethnic disparities are largely due to such patients being treated in low-performing hospitals. Targeted efforts to improve quality of care at hospitals serving large minority populations are likely to be the most effective way to reduce racial/ethnic disparities in pneumonia management.
Acknowledgements
The analyses upon which this publication is based were performed in part under Contract Number HHSM-500 2006-OK003C, entitled “Utilization and Quality Control Peer Review Organization for the State of Oklahoma”, sponsored by the Centers for Medicare & Medicaid Services, Department of Health & Human Services. This work was also supported by resources and the use of facilities at the Veterans Affairs Pittsburgh Healthcare System in Pittsburgh, PA. The content of this publication does not necessarily reflect the views or policies of the Department of Health & Human Services, Department of Veterans Affairs, or the U.S. Government, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented. (Publication No. 4–673-OK-0608). Dr. Hausmann was supported by VA Health Services Research and Development Career Development Award #RCD 06–287. Dr. Ibrahim is the recipient of a VA Health Services Research and Development Award and the Harold Amos Robert Wood Johnson Scholar Award. Dr. Ibrahim is also supported by a K24 Award (1K24AR055259–01) from the National Institutes of Musculoskeletal and Skin Disorders. Dr Mehrotra’s salary was supported by a career development award (KL2-RR024154–01) from the National Center for Research Resources, a component of the National Institutes of Health. There are no conflicts of interest to disclose.
References
- 1.DeFrances CJ, Lucas CA, Bule VC, Golosinskiy A. 2006 National Hospital Discharge Survey July 30 2008. 5. [PubMed] [Google Scholar]
- 2.Minino AM, Heron MP, Murphy SL, Kochanek KD. Deaths: Final Data for 2004 August 21 2007. Volume 55, Number 19. [PubMed] [Google Scholar]
- 3.Lave JR, Lin CC, Hughes-Cromick P, Fine MJ. The cost of treating patients with community-acquired pneumonia. Sem Respir Crit Care Med. 1999;20:189–198. [Google Scholar]
- 4.Muennig PA, Khan K. Cost-effectiveness of vaccination versus treatment of influenza in healthy adolescents and adults. Clin Infect Dis. December 1 2001;33(11):1879–1885. [DOI] [PubMed] [Google Scholar]
- 5.Lee PY, Matchar DB, Clements DA, Huber J, Hamilton JD, Peterson ED. Economic analysis of influenza vaccination and antiviral treatment for healthy working adults. Ann Intern Med. August 20 2002;137(4):225–231. [DOI] [PubMed] [Google Scholar]
- 6.Rothberg MB, Rose DN. Vaccination versus treatment of influenza in working adults: a cost-effectiveness analysis. Am J Med. January 2005;118(1):68–77. [DOI] [PubMed] [Google Scholar]
- 7.Sisk JE, Whang W, Butler JC, Sneller VP, Whitney CG. Cost-effectiveness of vaccination against invasive pneumococcal disease among people 50 through 64 years of age: role of comorbid conditions and race. Ann Intern Med. June 17 2003;138(12):960–968. [DOI] [PubMed] [Google Scholar]
- 8.Vold Pepper P, Owens DK. Cost-effectiveness of the pneumococcal vaccine in the United States Navy and Marine Corps. Clin Infect Dis. January 2000;30(1):157–164. [DOI] [PubMed] [Google Scholar]
- 9.Sisk JE, Moskowitz AJ, Whang W, et al. Cost-effectiveness of vaccination against pneumococcal bacteremia among elderly people. Jama. October 22–29 1997;278(16):1333–1339. [PubMed] [Google Scholar]
- 10.Malone DC, Shaban HM. Adherence to ATS guidelines for hospitalized patients with community-acquired pneumonia. Ann Pharmacother. October 2001;35(10):1180–1185. [DOI] [PubMed] [Google Scholar]
- 11.Menendez R, Ferrando D, Valles JM, Vallterra J. Influence of deviation from guidelines on the outcome of community-acquired pneumonia. Chest. August 2002;122(2):612–617. [DOI] [PubMed] [Google Scholar]
- 12.Gleason PP, Meehan TP, Fine JM, Galusha DH, Fine MJ. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med. November 22 1999;159(21):2562–2572. [DOI] [PubMed] [Google Scholar]
- 13.Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. March 22 2004;164(6):637–644. [DOI] [PubMed] [Google Scholar]
- 14.Bratzler DW, Ma A, Nsa W. Initial antibiotic selection and patient outcomes: observations from the National Pneumonia Project. Clin Infect Dis. December 1 2008;47 Suppl 3:S193–201. [DOI] [PubMed] [Google Scholar]
- 15.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. N Engl J Med. July 21 2005;353(3):265–274. [DOI] [PubMed] [Google Scholar]
- 16.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. November 14 2002;347(20):1585–1592. [DOI] [PubMed] [Google Scholar]
- 17.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. June 11 2007;167(11):1177–1182. [DOI] [PubMed] [Google Scholar]
- 18.Jha AK, Orav EJ, Zheng J, Epstein AM. The characteristics and performance of hospitals that care for elderly Hispanic Americans. Health Aff (Millwood). Mar-Apr 2008;27(2):528–537. [DOI] [PubMed] [Google Scholar]
- 19.Gaskin DJ, Spencer CS, Richard P, Anderson GF, Powe NR, Laveist TA. Do hospitals provide lower-quality care to minorities than to whites? Health Aff (Millwood). Mar-Apr 2008;27(2):518–527. [DOI] [PubMed] [Google Scholar]
- 20.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. June 25 2007;167(12):1233–1239. [DOI] [PubMed] [Google Scholar]
- 21.Mortensen EM, Cornell J, Whittle J. Racial variations in processes of care for patients with community-acquired pneumonia. BMC Health Serv Res. August 10 2004;4(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fine JM, Fine MJ, Galusha D, Petrillo M, Meehan TP. Patient and hospital characteristics associated with recommended processes of care for elderly patients hospitalized with pneumonia: results from the medicare quality indicator system pneumonia module. Arch Intern Med. April 8 2002;162(7):827–833. [DOI] [PubMed] [Google Scholar]
- 23.Ayanian JZ, Weissman JS, Chasan-Taber S, Epstein AM. Quality of care by race and gender for congestive heart failure and pneumonia. Med Care. December 1999;37(12):1260–1269. [DOI] [PubMed] [Google Scholar]
- 24.O’Meara ES, White M, Siscovick DS, Lyles MF, Kuller LH. Hospitalization for pneumonia in the Cardiovascular Health Study: incidence, mortality, and influence on longer-term survival. J Am Geriatr Soc. July 2005;53(7):1108–1116. [DOI] [PubMed] [Google Scholar]
- 25.Haas JS, Dean ML, Hung Y, Rennie DJ. Differences in mortality among patients with community-acquired pneumonia in California by ethnicity and hospital characteristics. Am J Med. June 1 2003;114(8):660–664. [DOI] [PubMed] [Google Scholar]
- 26.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. Jama. January 17 2001;285(3):297–303. [DOI] [PubMed] [Google Scholar]
- 27.Pippins JR, Fitzmaurice GM, Haas JS. Hospital characteristics and racial disparities in hospital mortality from common medical conditions. J Natl Med Assoc. September 2007;99(9):1030–1036. [PMC free article] [PubMed] [Google Scholar]
- 28.DeFrances CJ, Hall MJ. Advance Data, No. 385: 2005 National hospital discharge survey: CDC; July 12 2007. [PubMed] [Google Scholar]
- 29.Specifications manual for national hospital quality measures, Versions 1.0–1.05. http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1141662756099. Accessed February 3, 2009.
- 30.Lindenauer PK, Behal R, Murray CK, Nsa W, Houck PM, Bratzler DW. Volume, quality of care, and outcome in pneumonia. Ann Intern Med. February 21 2006;144(4):262–269. [DOI] [PubMed] [Google Scholar]
- 31.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. October 1993;46(10):1075–1079; discussion 1081–1090. [DOI] [PubMed] [Google Scholar]
- 32.FY 2005 CMS IPPS Impact File. http://www.cms.hhs.gov/AcuteInpatientPPS/HIF/list.asp. Accessed June 4, 2008.
- 33.Hospital Compare Home Page. http://www.hospitalcompare.hhs.gov/. Accessed February 20, 2009.
- 34.Min LC, Wenger NS, Fung C, et al. Multimorbidity is associated with better quality of care among vulnerable elders. Med Care. June 2007;45(6):480–488. [DOI] [PubMed] [Google Scholar]
- 35.Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- 36.Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London: Sage; 1999. [Google Scholar]
- 37.Turra CM, Goldman N. Socioeconomic differences in mortality among U.S. adults: insights into the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. May 2007;62(3):S184–192. [DOI] [PubMed] [Google Scholar]
- 38.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. October 2005;60 Spec No 2:68–75. [DOI] [PubMed] [Google Scholar]
- 39.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: A conceptual framework. Am J Public Health. December 2006;96(12):2113–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. March 2008;121(3):e407–415. [DOI] [PubMed] [Google Scholar]
- 41.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. October 25 2005;112(17):2634–2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Jama. May 14 2008;299(18):2180–2187. [DOI] [PubMed] [Google Scholar]
- 43.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. January 23 1997;336(4):243–250. [DOI] [PubMed] [Google Scholar]
- 44.Rosenthal GE, Baker DW, Norris DG, Way LE, Harper DL, Snow RJ. Relationships between in-hospital and 30-day standardized hospital mortality: implications for profiling hospitals. Health Serv Res. March 2000;34(7):1449–1468. [PMC free article] [PubMed] [Google Scholar]


